Purchase generic kaletra
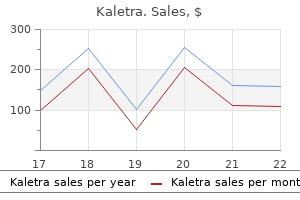
This study indicates that the administration of local anesthetic injections might contribute to overall professional stress for some dentists symptoms xanax is prescribed for order genuine kaletra. Anxious patients may not be the only ones anxious about local anesthetic injections. Dower and coauthors32 found that two-thirds of dentists described anxious patients as the main source of their anxiety, and 16% identified children as the main source of anxiety. Compassion fatigue Moreover, a type of emotional burnout called compassion fatigue may affect many health care workers. In fact, if patients feel pain during restorative treatment, we sometimes internalize the feeling as failure. As dentists and professionals, we provide an extraordinary service to our patients. Our ability to provide exceptional treatment with a caring attitude is a most rewarding art. However, we also have the ability to not accept failure because we have the means to prevent it. Unfortunately, some of the information that we have today that allows us to prevent patient pain was not available in the past. This book will outline the steps you need to take to overcome failure with this block. Anesthetic agents and dosages Table 1-1 outlines the local anesthetic formulations available in the United States. The American Dental Association has specified a uniform color code to prevent confusion among brands. The maximum allowable dosage applies to complex oral and maxillofacial surgery procedures. The typical maximum dosage is for adults (weighing 150 pounds) who are undergoing typical restorative and endodontic procedures. Local anesthetic agents, common names, and milligrams per cartridge are presented in Table 1-2. Both columns show the number of cartridges that would be required for an adult weighing 150 pounds (67 kg). These rubber stoppers are not color coded and are not indicative of the drug the cartridge contains. Orabloc articaine formulation Orabloc (Patterson Dental) is an articaine local anesthetic containing a vasoconstrictor and is available in two epinephrine formulations-1:200,000 and 1:100,000. As far as we are aware, no research has been performed on Orabloc in comparison with other commercially available products. Media hype: "Local anesthetics cause tooth cell death" Zhuang and coauthors,36 using pig teeth and young permanent tooth pulp cells, found that prolonged exposure to high doses of local anesthetics interfered with the mitochondria of tooth cells and led to cell death. The researchers noted that further clinical studies are required before there is enough data to change clinical guidelines. They also urged parents not to be alarmed or withdraw their children from treatment if they need it. In general, a small amount of anesthetic solution remained in both cartridges after delivery of the solution with an aspirating syringe. The amount of anesthetic solution expressed was basically the same for both articaine and lidocaine. Classification of local anesthetics and clinical implications Generally, local anesthetic agents are classified as short, intermediate, or long-acting based on their pKa, lipid solubility, and protein binding. Lidocaine, articaine, mepivacaine, and prilocaine, all with vasoconstrictors, are considered intermediate in action. However, Pateromichelakis and Prokopiou38 found that studies on isolated nerves can be poor guides to the clinical comparisons of local anesthetics. For example, clinical studies indicate that the duration of these drugs is different when used in nerve blocks versus infiltration or intraosseous injections. While classified as long-acting agents, this duration only holds true for nerve blocks-not for maxillary infiltration, intraligamentary, or intraosseous anesthesia. Factors influencing local anesthetic effectiveness Genetics Some patients may not respond adequately to local anesthetic administration. Perhaps, one day in the future, we may be able to use genomic testing to improve the efficacy of local anesthetics by selecting drugs that offer the most appropriate pharmacologic usefulness. Women with red hair have been reported to be more sensitive to some types of pain and may be resistant to subcutaneous lidocaine. In a follow-up study, Binkley and coauthors50 found that genetic variations associated with red hair color were also associated with fear of dental pain and anxiety. However, Myles and coauthors51 found no evidence that patient hair color affects requirements or recovery characteristics in a broad range of surgical procedures. Importantly, women with red hair and women with two red hair color alleles reported significantly higher levels of dental anxiety compared with women with dark hair or women with no red hair color alleles. Women with red hair also reported greater pain on needle insertion during the injection. It may be that the clinical impression of failed anesthesia in red-haired individuals is owed to the higher anxiety levels perceived in this population. During dental treatment, this population may be more likely to report nonpainful sensations (pressure, vibration, etc) as painful. Tofoli and coauthors57 found that injection discomfort and effectiveness of local anesthetics were not related to phases of the menstrual cycle or use of oral contraceptives. However, Loyd and coauthors58 reported that a sexually dimorphic peripheral mechanism may modulate trigeminal pain processing and may be related to the luteal phase of the menstrual cycle. Catastrophizing Some patients may have an exaggerated negative mental set that occurs during an actual or anticipated painful experience. That is, these patients are already predisposed to have a painful experience during dental treatment. Pathways of dental fear Five pathways related to dental fear have been recognized60: (1) the conditioning pathway occurs as a result of direct traumatic experiences. A recent study60 found that less fear was shown in older patients, men were more likely to cancel dental appointments because of fear, and different ethnic backgrounds adopt different pathways of fear. Pregnancy and breastfeeding For pregnant patients, elective treatment should be deferred, particularly in the first trimester. However, if treatment involving a painful procedure is required, many of the commonly available local anesthetic agents are safe to use. Drugs should be given only if the potential benefit justifies the potential risk to the fetus. A category B classification means that "Either animal-reproduction studies have not demonstrated a fetal risk but there are no controlled studies in pregnant women or animal-reproduction studies have shown an adverse effect that was not confirmed in controlled studies in women in the first trimester (and there is no evidence of a risk in later trimesters). These statements are placed for medicolegal reasons because the anesthetics have not been tested during pregnancy. To put things in perspective, congenital anomalies occur in 3% of the general population, yet the causes can be determined in less than 50% of these cases. They found that the use of local anesthetics, as well as dental treatment during pregnancy, did not present a major risk for anomalies. If the practitioner is unsure about the safety of a drug, he or she could consult the National Institutes of Health LactMed database. This resource provides information on drug transference to breast milk, drug safety, and safe alternative drugs. The most important aspect of care in the pregnant patient in pain is elimination of the source of pain by performing the indicated treatment. However, if treatment involving a painful procedure is required for the pregnant or lactating patient, many of the commonly available local anesthetic agents are safe to use. Elderly patients Nordenram and Danielsson64 found that elderly patients had significantly shorter onset times of anesthesia when compared with younger patients. In general, older patients may also be more tolerant of pain than younger patients.
Order 250mg kaletra amex
A rectocele is the bulging or displacement of the rectum through a defect in the anterior rectal wall medications derived from plants buy kaletra 250 mg overnight delivery. Damage to the rectovaginal septum or its supporting structures during vaginal childbirth have been implicated in the pathogenesis of rectocele. Rectoceles can cause inability to complete fecal evacuation, perineal pain, sensation of local pressure, and appearance of a bulge at the vaginal opening on straining. Affected patients report the need to apply pressure to the posterior vaginal wall to complete defecation. Kegel exercises are suggested for asymptomatic women, and instructions to avoid repetitive increases in intraabdominal pressure may help prevent progression of the rectocele. Surgery should be considered only for patients in whom contrast is retained during defecography and patients in whom constipation is relieved with digital vaginal pressure to facilitate defecation. Endoscopic ultrasound is used for evaluation of anal sphincters with incontinence and not for constipation. D (S&F ch20) the patient is likely bleeding from peptic ulcer disease secondary to her risk factors, including age, nonsteroidal antiinflammatory drugs, and aspirin. D (S&F ch20) the patient is likely bleeding from peptic ulcer disease secondary to his risk factors, including nonsteroidal antiinflammatory drugs and aspirin. There is no suspicion of cirrhosis in this patient despite history of hepatitis C, which was successfully treated. Studies have shown that a restrictive transfusion strategy (with transfusion only if hemoglobin <7 g/dL) improves outcomes of rebleeding and mortality, compared to a liberal transfusion strategy. Therefore, in patients without massive bleeding or cardiac disease, the recommended transfusion threshold is 7 g/dL. Because the ulcer has an adherent clot, the most appropriate course of action is to attempt removal of the clot with rigorous irrigation and/or a snare, and treat the underling lesion. If the clot cannot be removed, then epinephrine injection can be considered, particularly in high-risk patients. Dual therapy (epinephrine injection plus thermocoagulation/clips) is indicated for an actively bleeding lesion or a non-bleeding visible vessel. B (S&F ch20) the most commonly used probe is the bipolar electrocoagulation probe in which heat is generated through current flowing between wires intertwined at the tip of the probe. Heater probes provide a fixed amount of joules of energy that does not vary with the tissue resistance. A (S&F ch20) this patient has a single gastric ulcer that underwent endoscopic hemostasis. B (S&F ch20) this patient had a recent liver biopsy and is now presenting with hemobilia. Injection with epinephrine, mono or dual endoscopic therapy will not be able to stop the bleeding source. Surgery is not indicated at this time if bleeding control can be achieved by arterial embolization. Scintigraphy may be especially useful in small bowel and colonic sites of active bleeding; however, surgery should not be performed based on scintigraphy localization alone. A barium enema should not be done because it cannot detect active bleeding and will delay and obscure angiography. D (S&F ch20) the patient has recently been started on aspirin, which can precipitate bleeding from a preexisting ulceration. In addition, the repeat test should ideally be performed off proton pump inhibitors for at least 2 weeks. There is no indication to rule out Zollinger-Ellison syndrome, such as recurrent peptic ulcer disease, H. D (S&F ch20) Recent studies suggest that endoscopy is both effective and safe for the therapy of a bleeding diverticulum. After endoscopic hemostasis of a bleeding diverticulum is completed, a permanent submucosal tattoo should be placed around the lesion to allow identification of the site in case colonoscopy is repeated or surgery is performed for recurrent bleeding. After colonoscopic hemostasis, patients should be told to avoid aspirin and other nonsteroidal antiinflammatory drugs and take a daily fiber supplement on a long-term basis. Because the site of bleeding has been localized by colonoscopy, technetium-labeled red blood cell scan would only likely confirm the bleeding segment of the colon. Angiography would be reasonable in this woman to identify and possibly treat the bleeding diverticulum; however, there is morbidity from this procedure, particularly in an elderly woman with known vascular disease. The next step in management is endoscopic hemostasis with injection of epinephrine and hemoclip. If this fails then the patient can be referred to interventional radiology or surgery. Tattooing the area after endoscopic hemostasis is reasonable for future endoscopic or surgical localization. C (S&F ch20) the location in the right colon has been reported as a risk factor for the postpolypectomy bleeding. Other risk factors for postpolypectomy bleed are large polyp (>2 cm), thick stalk, sessile polyp, and use of anticoagulation or aspirin. The presentation here is classic with rows of ectatic mucosal blood vessels in the pylorus. Endoscopic therapy with argon plasma coagulation decreases oozing rates and improves hematocrit levels. Endoscopic therapy is not indicated because rebleeding rates on medical therapy are 5% to 7%. Recognition of the stigmata, early feeding, and consideration for early discharge are recommended. Epinephrine injection is not indicated and biopsy for malignancy can be deferred until a follow-up endoscopy is performed to document endoscopic healing. Malignancy occurs in less than 3% of all benign-appearing gastric ulcers, and would be very uncommon in this prepyloric gastric ulcer. A colonoscopy would be appropriate with a history of hematochezia, but is unlikely to be of help in this patient with hematemesis. In the absence of acute bleeding, neither scintigraphy nor angiography is likely to have a high diagnostic yield. Symptoms, Signs, and Biopsychosocial Issues stigmata of recent hemorrhage in postpolypectomy ulcers are better treated with endoclips (with or without epinephrine injection) because hemoclips do not cause tissue damage, as is seen with thermal coagulation. E (S&F ch20) Ischemic colitis is the most common type of bowel ischemia, accounting for about 75% of intestinal ischemia. Ischemic colitis classically occurs in the elderly with risk factors for a low-flow state, as in those with atherosclerosis. It commonly presents with abdominal pain and hemodynamic disturbances, and affects watershed areas, such as the splenic flexure. New onset inflammatory bowel disease or a missed lesion (either a large mass or innumerable polyps) is very unlikely with a recent normal colonoscopy, and generally does not present with a large amount of bleeding. The diagnosis is made by stool cultures and flexible sigmoidoscopy or colonoscopy. Treatment is with medical management; the use of antibiotics depends on the causative organism. E (S&F ch20) this patient has a white-based duodenal ulcer for which no endoscopic therapy is required. Duodenal ulcer biopsy is not required unless a tumor is seen or a malignant duodenal ulcer is suspected. B (S&F ch20) Painful rectal bleeding particularly when having a bowel movement is characteristic of an anal fissure. Endoscopic appearance is consistent with radiation proctitis with diffuse telengectasias and oozing. There is no presence of ulceration or dilated veins, which makes the other choices less likely. In the setting of constipation, one of the most likely causes for this can be a rectal ulcer. The treatment is a combination of thermal therapy, injection therapy, and suture ligation if needed. The most appropriate therapy for this lesion is epinephrine injection with endoclip placement because this would reduce the high risk of rebleeding and result in the least tissue damage, while actually closing the ulcer (see figure). Gold probe thermocoagulation is less preferred because it leads to increased tissue damage in this ulcer at the gastroesophageal junction.
Diseases
- Dental aberrations steroid dehydrogenase deficienciency
- Hydrocephaly corpus callosum agenesis diaphragmatic hernia
- Cold contact urticaria
- Fara Chlupackova syndrome
- Neutral lipid storage myopathy
- Ectrodactyly cleft palate syndrome
Buy kaletra discount
Options in children younger than 2 years include amphotericin B lipid complex and caspofungin symptoms insulin resistance best order for kaletra. Granulocyte colony-stimulating factor is indicated in neutropenic patients and reduction, discontinuation, or replacement of steroids in patients receiving these agents. Duration of treatment is individual and defined by the complete disappearance of all signs and symptoms and resolution of the underlying deficiency in host defenses. Although not formally investigated, a change in class is advised when a change in antifungal therapy is considered necessary because of refractory disease or a break-through infection on antifungal prophylaxis. While the role of antifungal combination therapies remains to be defined, it may be justified in profoundly compromised patients and those with fulminant or refractory disease. Because of its high solubility in water, voriconazole may also be an option for endophthalmitis, peritonitis, and bone and joint infections. Multi-azole-resistant Aspergillus species, such as Aspergillus calidoustus and A nidulans, have been reported; A terreus, on the other hand, has a reduced susceptibility to amphotericin B and is best treated with voriconazole. Zygomycetes are resistant to voriconazole and caspofungin, and non-Aspergillus hyalohyphomycosis and phaeohyphomycosis are considered resistant to caspofungin. On the basis of pivotal clinical trials conducted in adults, patients 13 years or older may receive posaconazole delayed-release tablets at the adult dose of 300 mg once a day (day 1: 300 mg twice daily). This practical algorithm, however, requires careful attention to contraindications, drug interactions, and adverse effects because appropriate clinical trials in pediatric patients are lacking. Long-term Implications Beyond a considerable short-term case fatality rate of 30% to 50% and the frequent necessity of treatment for months and sometimes years, the long-term prognostic effect of invasive aspergillosis is difficult to evaluate. Cancer treatment may be delayed in the presence of invasive aspergillosis for fear of progression of infection during neutropenia. Unfortunately, this delay of chemotherapy may also increase the probability of relapsed or progressive leukemia. As a case in point, in one case series, the cure rate in patients who were diagnosed and treated for a minimum of 10 days was 64%. Non-Aspergillus Mold Infections A wide variety of previously uncommon opportunistic filamentous fungi are increasingly encountered as causing life-threatening infections in severely immunocompromised children. Apart from the agents of mucormycosis, these emerging pathogens include hyaline filamentous fungi (eg, Fusarium species, Paecilomyces species, Pseudallescheria boydii, and Scedosporium prolificans) and dematiaceous molds (eg, Bipolaris, Exophiala, and Alternaria species). These filamentous fungi cause infections that are virtually indistinguishable from those of Aspergillus species, in clinical presentation and in their appearance in tissue specimens (colorless or lightly pigmented, septate, and branching). However, some of the hyaline molds, most notably Fusarium species, Acremonium species, and Paecilomyces species, disseminate via the bloodstream and can cause fungemia and numerous embolic skin lesions. Infections by the emerging pathogens have extraordinarily high case fatality rates; several of these organisms, including but not limited to Fusarium species and P boydii, have limited susceptibility to amphotericin B. However, while the echinocandins appear to have no useful activity, limited and uncontrolled data indicate an important role of both voriconazole and posaconazole in the management of these infections. Pediatric invasive aspergillosis: a multicenter retrospective analysis of 139 contemporary cases. Treatment of aspergillosis: clinical practice guidelines of the Infectious Diseases Society of America. It may present as uncomplicated catheter-related candidemia or disseminated candidiasis in a neutropenic child, potentially leading to septic shock. It can affect neonates, children with hematologic malignancies, patients in critical care, and those having risk factors for candidiasis. It can affect almost all organs and tissues of the body, causing multiple local infections. While Candida albicans is still the most frequently isolated species in pediatric patients, certain non-albicans Candida species, such as Candida parapsilosis and Candida glabrata, have become more frequent and may cause problems with their differential susceptibilities to antifungals. Conventional and lipid formulations of amphotericin B, azoles, echinocandins, and flucytosine are the main antifungals for the treatment of candidiasis. It starts from 2-week therapy for a catheter-related candidemia and may last several months in a difficult case of candidal endocarditis or spondylodiscitis. It mainly affects immunocompromised patients but may also affect other subjects with risk factors. Neonates, immunocompromised hosts, and those with vascular catheters are at risk for invasive candidiasis. Blastoconidia (yeast cells) are the infecting form of the organism, whereas hyphae/ pseudohyphae are the invasive form. Among hundreds of different Candida species, Candida albicans is the most frequent isolate, accounting for about half of cases. Other Candida species are Candida parapsilosis, Candida tropicalis, Candida glabrata, and Candida krusei. Candida parapsilosis is especially frequent in neonates, whereas C glabrata is more common in patients with hematologic malignancies. Mucosal or cutaneous candidiasis must be differentiated from other oral lesions and skin exanthemas, such as atopic dermatitis and eczema. Candidal diaper dermatitis is characterized by satellite lesions and appears on regions of skin that are in contact with the diapers of infants around their urogenital area. Candidemia and other forms of invasive candidiasis are difficult to differentiate from bacterial, other fungal, or even viral infections before microbiologic diagnosis is made. In neonates, candidemia resembles bacterial sepsis, and in older children, it has to be differentiated from other bacterial systemic infections. A typical erythematous papular exanthem of acute disseminated candidiasis may differentiate it from bacterial sepsis. Diaper dermatitis is a common mild exanthema around the urogenital area of infants, which comes in contact with diapers. Odynophagia and white plaques on the tongue and buccal surfaces of the mouth can be a problem. Vulvovaginal candidiasis may be seen in sexually active adolescent girls or those exposed to broad-spectrum antibiotics. However, they are the second most frequent cause of mortality and most important cause of neurodevelopmental delay as sequelae of neonatal sepsis, especially when candidemia is followed by the characteristic syndrome of hematogenous Candida meningoencephalitis. The degree of prematurity (ie, low gestational age, low birthweight) is the most important factor associated with increased incidence of candidiasis. Candidemia may be followed in up to 25% by hematogenous meningoencephalitis and in a much higher percentage (up to 60%) by urinary tract infection. Other syndromes that may complicate candidemia in neonates include endocarditis, brain or other organ abscesses, arthritis/osteomyelitis, and renal infection. Other risk factors are fungal colonization, high glucose concentrations, antibiotic and H2-receptor antagonist use, endotracheal intubation, congenital conditions, and necrotizing enterocolitis. The clinical syndromes that Candida causes in older children are similar to those in adults. Invasive candidiasis is also a clinically important syndrome in solid organ transplant recipients. Acute disseminated candidiasis with hemodynamic and inflammatory signs of sepsis, as well as a possible characteristic erythematous papular exanthema, may follow candidemia. Candida glabrata and C tropicalis are more frequent in children with hematologic malignancies than in other patients, probably because of the increased use of azoles and amphotericin B, respectively, in these patients. The attributable mortality of invasive candidiasis has been estimated to be around 10% in children. Chronic disseminated candidiasis (hepatosplenic candidiasis) is a welldescribed syndrome that occurs in children with hematologic malignancies 438 Succinct Pediatrics during and after recovery from neutropenia. It is characterized by persistent fever and upper abdominal pain as well as increased inflammatory index, alkaline phosphatase, and -glutamyltransferase levels, but not transaminase. The disease can last relatively long despite appropriate antifungal therapy and is determined by an ineffective inflammatory response. Organ- or Tissue-Specific Candidal Infections Meningoencephalitis frequently occurs in neonates following about as many as 25% of episodes of neonatal candidemia.
Order 250mg kaletra with mastercard
Lucky Luke dermatitis (also known as cowboy holster dermatitis) affects the skin of the lateral buttock and upper lateral thighs medications 1-z order kaletra paypal, resembling a gun holster appearance. Candidal diaper infections appear as bright red areas with irregular borders that can involve any part of the diaper area and thighs, including the skin folds. If the rash does not have the typical appearance of a candidal rash but has lasted more than 3 days, a candidal infection should be suspected. Additional risk factors for candidal diaper infection include gastrointestinal colonization by Candida, antibiotic exposure, diabetes mellitus, or an immunodeficiency. Intertrigo can appear similar to candidal infections except that no papular satellite lesions are noted. Intertrigo is an inflammatory condition induced by heat, moisture, and friction and characterized by moist, sharply demarcated areas of erythema in the skin folds. Although not caused by an infection, intertrigo can become secondarily infected with Candida or bacteria. Seborrheic dermatitis, while often seen on the scalp, face, neck, and axilla, can be seen in the diaper area. Typically, it manifests as salmon-colored plaques with greasy yellow scale in the inguinal folds. Atopic dermatitis, which often spares the diaper region, can resemble seborrheic dermatitis in its presentation with mild erythema and occasional scaling. Patients usually have a history of previous or concurrent rash on the face or extensor limbs; personal and family histories may include allergies, atopic dermatitis, and asthma. Langerhans cell histiocytosis can mimic seborrheic dermatitis in distribution and initial appearance. Erythematous papules can progress to vesicles, pustules, petechiae, erosions, and ulcerations. Systemic manifestations are typically noted, including hepatosplenomegaly and lymphadenopathy. Typically, psoriatic lesions are not confined to the diaper region and thus will be noted on other areas of skin. Bacterial infections, most commonly caused by Staphylococcus and Streptococcus species, can present in a variety of ways and mimic candidal infections as well as intertrigo. Bright red, well-demarcated patches in the skin folds or perianal region can be seen with streptococcal infections. Additional symptoms that suggest infection with Streptococcus pyogenes include perianal pain, pruritus, and rectal bleeding. Bullous lesions and discrete pustular follicular lesions can be seen with staphylococcal and streptococcal infections. Painful vesicles with or without crust occur with herpes simplex virus infections. Numerous other viral etiologies should be considered when generalized papular or vesicular rashes are noted but not confined solely to the diaper region. Scabies infections occurring in the diaper area appear as pruritic, raised papules. Additional lesions may be seen in the interdigital spaces of the hands and feet, on the abdomen, and in the axillae. Additional etiologies of diaper dermatitis can be caused by metabolic disorders, nutritional deficiencies, and genetic disorders. These include biotin deficiency, acquired or congenital zinc deficiency, cystic fibrosis, and WiskottAldrich syndrome. Consideration of these etiologies should occur when a patient presents with diaper dermatitis that is refractory to treatment. A complete history, including care of the diaper area and adherence to therapy, should first be assessed. The clinician should also obtain a history for associated symptoms, systemic symptoms, past medical history, and family history, because these are essential for helping to identify an etiology. Physical examination, focusing on morphology and location of the rash, often reveals the diagnosis. Rashes that persist longer than 72 hours are highly suspicious for candidal infections. Microbiologic cultures and scrapings are not routinely performed but may be helpful to confirm the etiology. Rashes that appear atypical or do not improve with conventional therapies warrant further workup. A thick layer of petrolatum applied at each diaper change may prevent skin breakdown. Mild diaper dermatitis with erythema and intact skin can often be treated with a cream containing 10% zinc oxide applied as a thick layer; a 40% zinc oxide preparation may be needed for more severe rashes. Antifungals that are effective against Candida include nystatin and any of the -azole drugs. Treatment typically takes 7 to 14 days and should continue for 3 days beyond resolution of the rash. If there is evidence of a secondary bacterial infection, mupirocin offers both antibacterial and antifungal coverage (Evidence Level I). Low-potency topical corticosteroids should be reserved for moderate to severe cases of diaper dermatitis. No evidence supports or refutes the use of topical vitamin A in diaper dermatitis. Diaper dermatitis recalcitrant to the interventions mentioned may warrant consideration of metabolic deficiencies, nutritional deficiencies, malignancies, and other cutaneous disorders. The mainstay in preventing diaper dermatitis is keeping the area as clean and dry as possible. Frequent diaper changes, as often as every 2 hours, are crucial, because urine and stool contribute to skin breakdown. Studies with reusable cloth diapers, conventional disposable diapers, and superabsorbent diapers suggest that superabsorbent disposable diapers are superior to conventional disposable diapers and cloth diapers. However, because of the quality of studies and biases within them, not enough evidence supports one type of diaper over another. Baby wipes that contain alcohol should be avoided, because they can dry out the skin. Over-the-counter lotions and creams that are applied should be free of fragrances and dyes. Topical vitamin A, or its derivatives, for treating and preventing napkin dermatitis in infants. Treatment of candidal diaper dermatitis: a double-blind placebo-controlled comparison of topical nystatin with topical plus oral nystatin. It is a panniculitis, consisting of inflammation of fat cells and the septal fibrotic structures within fat tissue. Clinical presentation is characterized by symmetric, tender, erythematous nodules located most commonly on the anterior and lateral surfaces of the lower legs. Evaluation for underlying causes is necessary, with -hemolytic streptococci representing the most common cause in children. Management primarily focuses on treating underlying causes and supportive measures, including bed rest and analgesics as needed. Overview Erythema nodosum, also known as erythema contusiformis, is an uncommon self-limited hypersensitivity reaction precipitated by both infectious and noninfectious processes. It classically presents as tender, erythematous nodules primarily located on the bilateral lower anterior legs (pretibial areas); however, more extensive disease can occur. Erythema nodosum can occur at any age but most commonly develops between the second and fourth decades of life, particularly between 20 and 30 years of age. Boys and girls are reported to be equally affected in the preadolescent period, but later in life the incidence is higher in women. Causes and Differential Diagnosis Erythema nodosum is considered a hypersensitivity reaction. Myriad presumed etiologic associations have been identified and include infections, drugs, underlying diseases, and malignancies (Box 51-1).
Buy kaletra overnight
Allergic contact dermatitis requires an initial exposure or sensitizing step medications post mi buy line kaletra, followed by the development of immunologic memory, with any subsequent exposure leading to an adverse effect. Causes and Differential Diagnosis Primary irritant contact dermatitis may be caused by numerous exposures ranging from soaps, detergents, and foods to urine and stool in the diaperwearing infant. Frequent wetting and drying in a susceptible individual can lead to irritant contact dermatitis, as in a lip-licking child. The differential diagnosis of irritant contact dermatitis includes atopic dermatitis and allergic contact dermatitis. Allergic contact dermatitis is uncommon in children, and nickel, fragrance, and neomycin are the usual suspects, but any refractory pruritic eruption, particularly if patterned or asymmetric in distribution, should prompt 556 Succinct Pediatrics consideration of allergic contact dermatitis. The differential diagnosis is similar to irritant contact dermatitis but may also include a distinctive pruritic viral exanthem called unilateral laterothoracic exanthem when rash affects the hip or shoulder girdle areas. Clinical Features Both irritant and allergic contact dermatitis look eczematous in appearance with erythema, papulation, and even frank vesiculation. Irritant contact dermatitis will spare protected areas in the diaper where folds, such as the inguinal crease, may be uninvolved, while surrounding skin is acutely inflamed ("affects the peaks, spares the valleys"). Two distinctive presentations of irritant contact dermatitis can easily be mistaken for infection. A history of recurrent diarrhea, frequent cleaning, and particularly use of cloth diapers is supportive. The same context may produce a different picture characterized by more numerous, smaller, papulopustular lesions without ulceration called pseudoverrucous papules. In both cases, minimizing irritancy with barrier protection, topical anti-inflammatories such as hydrocortisone, and elimination of triggers is curative. Allergic contact dermatitis may become impressively edematous and exudative and should present in the distribution and often shape of contact exposure. A potentially misleading feature of allergic contact dermatitis may be the development of an id reaction. An id reaction represents a more diffuse hypersensitivity reaction typically characterized by discrete, monomorphic flesh-colored to erythematous pruritic papules distant from the site of allergic exposure. These papules are most often seen on the extensor arms and hands as well as upper trunk and neck. Because they are present at sites distant from potential allergic trigger, a causal connection may be missed. Evaluation Evaluation requires a careful history directed toward any products potentially touching the affected skin, including soaps, emollients, barriers, clothes, wipes, and even prescription medications. A family history with attention to atopy is noteworthy as atopic children are at greater risk for contact dermatitis of all types. A skin biopsy is usually not helpful because it will not distinguish allergic from irritant contact dermatitis, or either from atopic dermatitis, and cannot identify triggers. Management Management consists first of identification and avoidance of relevant triggers. It is important to note that any exposure, however brief, may trigger allergic contact dermatitis in a sensitized individual, whereas irritant contact dermatitis tends to be more "dose dependent. Burows compresses (aluminum acetate) applied several times daily may be soothing when a significant exudative component is present. Atopic eczema and attentiondeficit/hyperactivity disorder in a population-based sample of children and adolescents. History and physical examination findings often lead to the diagnosis, although occasionally further evaluation is needed. Treatment includes frequent diaper changes, avoidance of products containing potential allergens, and application of topical barrier ointments. Appropriate antimicrobials should be used when an infectious etiology is suspected or confirmed. Consultation with a dermatologic specialist may be needed for persistent diaper dermatitis unresponsive to treatment. Overview Diaper dermatitis refers to a skin problem in the area covered by a diaper, namely the buttocks, genitalia, upper thighs, and lower abdomen. Diaper dermatitis predominantly affects infants and young toddlers but can affect children of any age who wear diapers. Causes and Differential Diagnosis Although diaper dermatitis encompasses any rash in the diaper region, it may not be associated with wearing diapers. Exposure of the skin to urine and stool results in wetness, increased pH, and activation of enzymes that causes breakdown of skin. Friction caused by diapers on the skin, as well as by caregivers during diaper changes, can cause skin breakdown. Exposure to chemicals after ingesting senna-containing laxatives has also been reported to cause contact dermatitis. Kawasaki disease in infants may be heralded by a pronounced rash in the diaper region. Occasionally, infants with violent trauma may present with unusually severe diaper dermatitis. Identifying the etiology of diaper dermatitis enables appropriate treatment to be given and prevention strategies to be implemented. It is characterized by asymptomatic, oval, violaceous papules and nodules on the gluteal surfaces sparing the inguinal folds. Diaper dye dermatitis affects the skin where colored dyes are found in the diapers. Historically, tuberculosis was the most commonly associated etiologic factor in children. This is in contrast to adults, in whom the most common etiologies are drugs, inflammatory bowel disease, and sarcoidosis. Of note, one study in adult patients with sarcoidosis found an association of granulomatous papules on the knees with coexisting erythema nodosum. Differential diagnosis includes other inflammatory diseases of fat, such as Bazin-nodular vasculitis (lobular panniculitis with vasculitis), and cold panniculitis, which may occur in young children following prolonged sucking on cold objects (eg, popsicles, affecting the cheeks). In other cases, unintentional or violent trauma with resultant contusions may resemble erythema nodosum. Clinically, erythematous lesions located on anterior surfaces of the legs are typically larger than those located laterally. Within a few days, they flatten and become purplish in color, then subsequently yellowish green, mimicking the appearance of a deep ecchymosis; hence, the name erythema contusiformis. Erythema nodosum may be associated with fever, sore throat, fatigue, arthralgia, malaise, headache, conjunctivitis, cough, abdominal pain, vomiting, or diarrhea. Prodromal symptoms may appear approximately 568 Succinct Pediatrics 5 to 15 days prior to the onset of erythema nodosum and often provide clues to the underlying etiologic factor. For example, recent sore throat or concurrent fever are common in patients with underlying -hemolytic streptococcal infection. Similarly, diarrhea is reported to be a prodromal symptom in some patients with underlying Yersinia enterocolitica, Leptospira, Campylobacter, or Crohn disease. Arthralgias may be an accompanying symptom in patients with Mycoplasma pneumoniae or Y enterocolitica infection. Typically, the cutaneous eruption persists approximately 1 to 3 weeks in children and 3 to 6 weeks in adults; however, longer duration and recurrence may occur. In one series of erythema nodosum in 35 children, lesions persisted more than 20 days in only 3 patients; underlying causes in the more prolonged cases were Hodgkin disease, Crohn disease, and unknown etiology. This suggests that prolonged cases of erythema nodosum may be caused by an underlying chronic disease with persistent antigenic stimulus. In atypical, persistent, or unclear cases, however, skin biopsy may be necessary to confirm the diagnosis and rule out other possibilities. Workup for underlying processes that might have triggered erythema nodosum is appropriate and should be guided by a detailed history, identifying both prescription and over-the-counter medications, as well as an extensive review of systems and thorough physical examination (Box 51-2). Most experts would recommend tuberculin testing (tuberculin interferon- release assays preferred for those older than 5 years) and evaluation of antistreptolysin O titers in any case without a clear cause.
Syndromes
- Remove excess clothing or blankets. The room should be comfortable, not too hot or cool. Try one layer of lightweight clothing, and one lightweight blanket for sleep. If the room is hot or stuffy, a fan may help.
- Shock (usually when not enough fluid is replaced during the surgery)
- A thin flexible tube called a catheter is passed through the needle, into the artery, and up through the main vessels of the belly area until it is properly placed into a mesenteric artery. The doctor uses x-rays as a guide. The doctor can see live images of the area on a TV-like monitor.
- Polycythemia vera
- High cholesterol levels
- Amyloidosis
- Improper technique used to feel for the pulse
- Bleeding underneath the scalp (cephalohematoma) caused by a difficult delivery
- High or low blood pressure
- Hyperparathyroidism
Discount kaletra 250 mg amex
C (S&F ch53) Refractory ulcer is an ulcer lesion that does not heal within 8 weeks of initiation of antisecretory therapy or beyond 12 weeks for a large ulcer (>2 cm) medications enlarged prostate cheap kaletra 250mg fast delivery. Possible causes for nonhealing ulcer include noncompliance; penetrating ulcer to the pancreas, liver, or other organ; H. C (S&F ch53) this patient has chronic kidney disease with worsening kidney function to the point that her creatinine clearance is less than 50 mL/min. Many pharmaceutical agents for peptic ulcer disease require dose adjustment or discontinuation in this population. All antacids must be used with caution in patients who have chronic kidney disease, due to risk of hypermagnesemia, hypercalcemia, and neurotoxicity (when aluminum-containing antacids is used). Sucralfate is a complex aluminum salt of sulfated sucrose that can cause aluminum accumulation and possible neurotoxicity, similar to aluminum containing antacid. Shortterm, standard-dose therapy with bismuth is acceptable with minor risk of toxicity. However, when administered in high dose or long duration especially in patients with chronic kidney disease, there is the potential for bismuth encephalopathy with neuropsychiatric symptoms. Dose reductions of misoprostol are unnecessary in patients with chronic kidney disease. C (S&F ch53) Size, location, and bleeding stigmata are most important prognostic factors of the ulcer. According to Forrest classification, ulcers with flat pigmentation and clean base do not require endoscopic interventions given low risk of rebleeding (see table at end of chapter). Ulcer size (>2 cm) and location (either high on the lesser curvature of the stomach or in the superior or posterior duodenal bulb) are important prognostic factors associated with poorer outcomes. These are locations where ulcers can erode into major 116 Stomach and Duodenum arteries, such as the left gastric artery and the gastroduodenal artery, respectively. These ulcers occur mostly in older adult patients, often with significant comorbidities, who often present with hemodynamic instability. C (S&F ch54) There are multiple definite and probable risk factors for gastric adenocarcinoma (see box at end of chapter). Incidence of gastric adenocarcinoma is highest in black, Asian, and Pacific Islander population and is lowest in white population (see table at end of chapter) 82. E (S&F ch54) the only statement that is true is E: the most important cofactor in the induction of H. A combination of a virulent bacterial strain, a genetically permissive host, and a favorable gastric environment are necessary for cancer to occur. Pangastritis with high intragastric pH is associated with higher risk of gastric cancer. Patients who are genetically predisposed to developing atrophic gastritis in response to H. Hypochloremic, hypokalemic metabolic alkalosis is a common finding in patients with severe vomiting. Blood transfusion may be required, but over-transfusion should be avoided and goal hemoglobin should be around 7 to 8 g/dL. Her clinical presentation is concerning for gastric outlet obstruction, however, there was no signs of luminal perforation. An abdominal x-ray and nasogastric decompression may be required before the endoscopic intervention but should not precede volume resuscitation in patients with upper gastrointestinal bleeding. Its clinical manifestations include nausea and postprandial vomiting, abdominal fullness, pain, and early satiety. The loss of fluid, hydrogen ions, and chloride ions in the vomitus leads to hypochloremic, hypokalemic metabolic alkalosis. The patient should be volume resuscitated with potassium replacement once urine output is adequate. Nasogastric tube placement for gastric decompression helps relieve vomiting, monitors fluid loss, and allows the stomach to regain its tone. Proton pump inhibitors facilitate ulcer healing, ameliorates inflammatory edema, and assists in resolving obstruction. If conservative management fails, endoscopic dilation should be attempted before surgery. If the ulcer fails to heal, biopsy to rule out malignancy should be performed, however, these tests are of no urgency at this point. Moreover, the etiology of the ulcer in her case is likely from nonsteroidal antiinflammatory drugs. D (S&F ch53) Stress-related gastric and duodenal mucosal injury (stress ulcers) is an illness of the critically ill. D (S&F ch54) the British and American Societies of Gastrointestinal Endoscopy guidelines recommend that all gastric polyps should be biopsied, and all gastric adenomas, symptomatic polyps, and polyps with dysplasia should be removed. Gastric polyps consist predominantly of fundic gland polyps (~50%), hyperplastic polyps (~40%), and adenomatous polyps (~10%). The clinical course of fundic gland polyps is generally benign with very low risk of malignant transformation (~1%) and confined to polyps larger than 1 cm. Hyperplastic polyps are generally benign, often multiple, and are typically found in the background of chronic inflammatory conditions. Hyperplastic polyps rarely undergo malignant transformation and are usually predisposed by dysplastic areas or intestinal metaplasia first. In contrast to other polyps of the stomach, gastric adenomas have a high rate of malignant transformation (11% within 4 years). D (S&F ch54) Hyperplastic polyps larger than 1 cm should be removed due to the risk of malignancy. Endoscopic ultrasound is not required to examine the polyp because it does not add useful information for this pedunculated polyp. To date, there is no reliable serum marker with high enough sensitivity and specificity to help make the diagnosis of gastric cancer. These tumor markers can be used to monitor recurrence of gastric cancer, especially in patients who had elevated levels prior to surgical resection. C (S&F ch54) Accurate staging in gastric cancer is essential for treatment decisions before considering subtotal gastrectomy 117 or endoscopic submucosal dissection. Approximately 50% of gastric cancer have metastatic disease involving the peritoneum, thus laparoscopy with peritoneal lavage for patients with seemingly resectable disease is recommended by National Comprehensive Cancer Network guidelines, especially for whom neoadjuvant chemotherapy is being considered. B (S&F ch54) Overall, the 5-year survival rate in the United States from gastric cancer is 27%. Large tumor size (>5 cm) is a independent risk factor associated with worse survival, independent of nodal status or overall tumor stage. Early gastric cancer is defined as a cancer that does not invade beyond the submucosa, regardless of lymph node involvement. In general, total gastrectomy is performed for proximal gastric tumors and for diffuse gastric cancer, while partial gastrectomy is reserved for tumors in the distal stomach. Approximately half of gastric cancer patients with metastatic disease have cancer involving the peritoneum. As approximately 50% of gastric cancer has metastatic disease involving the peritoneum. Laparoscopy with peritoneal lavage for patients with seemingly resectable disease is recommended by National Comprehensive Cancer Network guidelines, especially patients for whom neoadjuvant chemotherapy is being considered. Total gastrectomy is performed for proximal gastric tumors and for diffuse gastric cancer, while partial gastrectomy is reserved for tumors in the distal stomach. Extended lymph node resection is mainly performed in Japanese centers, not in the Western population. To prevent "understaging," the current recommendation is a minimum D1 lymphadenectomy with removal of at least 15 nodes. In addition, adjuvant chemoradiation is the standard of care and is also warranted in this case, although the optimal chemotherapy regimen is not yet clear. Adjuvant chemotherapy can improve survival and quality of life, and is currently the standard of care postoperatively or even in unresectable case. It has been shown to be superior to best supportive care and can be used for a palliative regimen. Given the lack of convincing evidence, the use of green tea and antioxidants such as carotenoids, vitamin C, and vitamin E cannot be recommended. C (S&F ch54) Gastric cancer is metastatic at the time of diagnosis in up to one third of cases.
Discount generic kaletra canada
Small osmotic gap (<50 mOsm/kg) is suggestive of secretory diarrhea treatment ulcerative colitis kaletra 250mg lowest price, whereas a large (>100 mOsm/kg) osmotic gap is suggestive of osmotic diarrhea. In this patient, the osmotic gap is high at 140 mOsm/kg Symptoms, Signs, and Biopsychosocial Issues flatulence. This patient may have impaired rectal sensation due to neurologic damage from poorly controlled diabetes. Similarly, hard stools due to narcotic use can worsen constipation and fecal impaction. C (S&F ch18) Colonoscopy with colonic biopsies is warranted as a first next step in evaluation of this patient with incontinence as a result of severe diarrhea. E (S&F ch18) this patient most likely has a sphincter defect or weakness due to injury from prior vaginal deliveries and/or surgical hemorrhoidectomy. In order to diagnose this condition, anorectal manometry and anal endosonography are indicated. Barium enema can provide evidence of structural lesion but its utility in evaluating ano-rectal dysfuction is limited. C (S&F ch18) Neuromuscular training, most commonly performed with biofeedback therapy and Kegel exercises, is the most appropriate next step in management (see figure). This has been shown to improve fecal incontinence using a repeated training and feedback to reinforce learning of improved coordination, anorectal perception, and to strengthen the anal sphincter. All the other therapies, including surgical repair, injection of a sphincter-bulking agent, and sacral nerve stimulation, may be effective therapies, but can be reserved as second line treatment due to their more invasive nature. A high resting anal pressure is seen in the presence of an anal fissure or anismus (paradoxical contraction of the external anal sphincter in response to straining or pressure within the anal canal). Inappropriate contraction of the anal sphincter while bearing down is seen in patients with defecatory disorder. C (S&F ch19) this patient has pelvic dyssynergia or functional anorectal outlet obstruction. During normal defecation there is an increase in rectal pressure accompanied by contraction of puborectalis sling, which narrows the anorectal angle; subsequent relaxation of anal sphincter muscles allows evacuation of bowels. In pelvic dyssynergia there is paradoxical contraction of the anal sphincter when patients bear down, which leads to difficulty in evacuation of bowels. If a defecatory disorder is present, initial treatment should include biofeedback; up to 75% of patients with disordered evacuation respond to biofeedback, and many do not respond well to fiber supplementation or oral laxatives. A subtotal colectomy is usually the last resort in patients with slow transit constipation and not with pelvic dyssynergia. Indeed some patients with pelvic dyssynergia, having a wrong diagnosis, end up with constipation after subtotal colectomy. Chest x-ray should be considered if there is a concern for paraneoplastic constipation, where constipation develops suddenly and is not a chronic issue. The patient had a normal colonoscopy and has no concerning features; thus, repeating a colonoscopy is inappropriate. Patients usually present with rectal bleeding and mucous discharge while straining during defecation. Endoscopic findings may include erythema, hyperemia, mucosal ulceration, and polypoid lesions. Defecography, transrectal ultrasonography, and anorectal manometry are helpful in the diagnosis. A (S&F ch19) this is a terminally ill, hospitalized patient on narcotics for pain control. There is evidence in controlled trials that this therapy, as well as diphenoxylate and atropine sulfate, is effective for reducing incontinence. Due to the side effect profile, sedation in the case of tincture of opium, and ischemic colitis and severe constipation in the case of alosetron, these two medications are not good choices for first-line therapy. Docusate and magnesium citrate are laxatives, and since there is no suggestion of fecal impaction in this case, these would not be appropriate therapies and would likely make her condition worse. Female gender, low levels of income and education, nonwhite ethnicity, and a low level of physical activity are risk factors for constipation in the United States. A (S&F ch19) Constipation can be functional (primary disorder of colon or rectum) or secondary to a systemic illness or medication. Functional constipation is divided into normal transit constipation, slow transit constipation, and defecatory disorder. Normal transit constipation is characterized by incomplete evacuation; abdominal pain may be present but not a predominant feature. Slow transit constipation is characterized by: Infrequent stools (such as one or fewer per week), lack of urge to defecate, poor response to fiber and laxatives, generalized symptoms. Defecatory disorders are characterized by frequent straining, incomplete evacuation, and a need for manual maneuvers to facilitate defecation. A (S&F ch19) In the management of severe constipation, initial evaluation includes physical examination and obtaining medication history looking for secondary causes of constipation. Initial treatment of constipation is based on nonpharmacologic interventions like exercise, increased fluid and fiber intake through changes in diet, or use of commercial fiber supplements. Osmotic laxatives like magnesium hydroxide or polyethylene glycol are suggested if there is inadequate response to initial measures. Lubiprostone and linaclotide should be considered for patients who have not responded to initial therapy. Anorectal manometry/balloon expulsion test is performed if there is no response to pharmacologic measures. If a defecatory disorder is present, initial treatment should include biofeedback. Patients are diagnosed either early in life with delayed passage of meconium, or later in life with constipation that develops due to a short Symptoms, Signs, and Biopsychosocial Issues constipation in patients with a late-stage advanced illness. Lubiprostone was approved for the treatment of chronic idiopathic constipation for men and women in the United States and women with irritable bowel sydrome with constipation predominance. It was approved for chronic constipation and had also been used in women with irritable bowel syndrome with constipation predominance. Lubiprostone activates the intestinal chloride 2 channels, thereby increasing intestinal fluid secretion and transit. Peripherally acting opioid antagonists like methylnaltrexone have been shown to reverse opioid-induced bowel dysfunction without reversing analgesia or precipitating central nervous system withdrawal signs. Elobixibat (A3309) is a novel investigational, minimally absorbed, ileal bile acid-transporter inhibitor that increases the flow of bile into the colon. Stool softeners, stimulant laxatives, and bulking agents (psyllium and calcium polycarbophil) have grade B evidence for treatment of chronic constipation. B (S&F ch19) this patient has a rectocele that has been causing severe constipation. C (S&F ch21) In unstable patients who cannot tolerate anesthesia, any form of surgical intervention may be contraindicated. In these patients, drainage of the gallbladder may be performed under radiologic guidance via percutaneous cholecystostomy. There is high risk for perforation and abscess formation, and thus antibiotics alone is not adequate treatment. B (S&F ch22) the spinothalamic tract terminates in the medial thalamus and projects as third order neurons to the primary somatosensory cortex (see figure). This is important for sensory discrimination and localization of visceral versus sensory pain. The cingulate cortex, therefore, is important in multicomponent integration of nociceptive information, and this results in variability of experience and reporting of pain. B (S&F ch21) the patient presents with Charcot triad of fever, right upper quadrant pain, and jaundice suggestive of cholangitis. The clinical picture as well as the cholangiogram findings is suggestive of Mirizzi syndrome. Mirizzi syndrome is a common hepatic duct obstruction caused by a gallstone impaction in the gallbladder neck or cystic duct. After decompression of the bile duct with a stent, the next most appropriate step in management is to perform a cholecystectomy for definitive treatment. The clinical history and cholangiogram findings alone are enough to raise the suspicion of this diagnosis. Leaving the stent in for surgery is beneficial because it can help the surgeon identify the common bile duct in order to help avoid ductal injury. It produces asymptomatic unconjugated hyperbilirubinemia and it is important to know the disease to avoid unnecessary diagnostic procedures. Impaired canalicular export of conjugated bilirubin is seen in Dubin-Johnson syndrome.
Cheap kaletra online visa
Travelers should be aware that mosquitoborne illness related to daytime exposure (dengue and yellow fever) may coexist in malarious regions symptoms yeast infection women 250 mg kaletra mastercard, so appropriate precautions should be maintained Table 43-2. Drugs Used in the Prophylaxis of Malaria Drug Atovaquone/ proguanil Use Prophylaxis in all areas Adult Dose 1 adult tablet orally, daily (Adult tablets contain 250 mg atovaquone and 100 mg proguanil hydrochloride. Partial tablet doses may need to be prepared by a pharmacist and dispensed in individual capsules. Take weekly on the same day of the week while in the malarious area and for 4 wk after leaving such areas. Take daily at the same time each day while in the malarious area and for 4 wk after leaving such areas. Contraindicated in people allergic to mefloquine or related compounds (quinine and quinidine) and in people with active depression, a recent history of depression, generalized anxiety disorder, psychosis, schizophrenia, other major psychiatric disorders, or seizures. Use with caution in persons with psychiatric disturbances or a previous history of depression. Take daily at the same time each day while in the malarious area and for 7 d after leaving such areas. Indicated for people who have had prolonged exposure to P vivax, P ovale, or both. Chapter 43 Primaquine Prophylaxis for short-duration travel to areas with principally Plasmodium vivax 30-mg base (52. The clinical presentation is generally acute or subacute respiratory illness similar to other pathogens presenting as pneumonia, but generally severe hypoxemia is a feature. The treatment of choice is trimethoprim/sulfamethoxazole and should be initiated when there is a high level of clinical suspicion prior to final diagnosis. Overview Pneumocystis jiroveci, now classified as an atypical fungus, was formally known as Pneumocystis carinii when it was previously classified as a protozoan. The organism can exist in 2 forms (cyst and trophozoite), which has made classification challenging. Pneumocystis epidemics have also been recognized in malnourished children and neonates and infants in resourcepoor regions, as well as preterm infants. The death rate ranges from 5% to 40% in patients who receive treatment to 100% without therapy. The mode of transmission is still unknown in humans, but animal models have indicated airborne spread. Clinical Features the primary clinical syndrome associated with P jiroveci is pneumonia or pneumonitis presenting in an acute or subacute fashion with clinical symptoms, including nonproductive cough, fever, decreased oxygen saturation, difficulty breathing/shortness of breath, and tachypnea. Other symptoms can include anorexia, fatigue, diarrhea, night sweats, and weight loss. Pneumothorax is a known complication of the disease process, and respiratory failure can also occur. Radiologically, chest radiographs can reveal bilateral diffuse interstitial or alveolar disease; their findings can also be normal. A recent meta-analysis suggests that measurement of serum 1,3-D-glucan may be helpful in establishing diagnosis. More important, a negative test result is good evidence that the diagnosis can be excluded. However, if the assay is positive, consider other entities that may be associated with falsepositive testing, including intravenous amoxicillin-clavulanic acid, treatment of patients with intravenous immune globulin, use of cellulose membranes, filters made from cellulose in hemodialysis, and use of cotton gauze swabs/ packs/pads and sponges. Definitive diagnosis is made with open lung biopsy or bronchoscopy with bronchoalveolar lavage, with lung samples being sent to a histopathologic specialist. Management Treatment should be initiated before an official diagnosis is made when clinical suspicion is high or in severely immunocompromised patients. Although P jiroveci is now classified as a fungus, antifungal treatment is not the drug of choice. Trimethoprim/sulfamethoxazole is the drug of choice and should be given intravenously for moderate to severe infection. However, the oral formulation can be used for patients with mild disease and functional gastrointestinal tract. Trimethoprim/sulfamethoxazole adverse effects during treatment include pancytopenia, hepatitis, and renal impairment. Pentamidine adverse effects during treatment include pancreatitis, cardiac arrhythmias, neutropenia, and renal impairment with electrolyte abnormalities. Urinary/stool samples have limited sensitivity (approximately 25%), so multiple tests are needed. Serologic testing, available through the Centers for Disease Control and Prevention, may be helpful but cannot differentiate between active disease and past infection or reinfection. Praziquantel is the only effective anthelmintic against adult worms and must be repeated in 4 to 6 weeks. Overview Schistosomiasis, or bilharziasis, is an infection caused by the species Schisto soma, a trematode (fluke) helminth that is globally distributed and dependent on freshwater exposure. More than 200 million people are infected across 52 countries in Africa, Asia, the Middle East, and South America, with most infections acquired in sub-Saharan Africa. Causes and Differential Diagnosis Infection typically occurs when people come in contact with freshwater contaminated with cercariae (the larval form of the schistosome) while swimming, bathing, washing clothes, fishing, and farming. Over several weeks, the parasites migrate through host tissue and develop into adult worms. Once mature, the worms mate and the females produce eggs; these eggs travel to the bladder or intestine and are passed into the urine (Schistosoma haematobium) or stool (Schistosoma mansoni, Schistosoma japonicum, Schistosoma mekongi, and Schistosoma intercalatum). Freshwater snails act as intermediate hosts in 502 Succinct Pediatrics which the parasites develop into sporocysts and produce cercariae. Symptoms of schistosomiasis, and therefore differential diagnosis, vary depending on phase of the disease as well as which species of schistosome is causing the infection (Box 45-1). Clinical Features Schistosomiasis presents in 3 distinct forms: acute, chronic, and advanced disease. Eggs shed by the adult worms that do not pass out of the body can become lodged in the intestine or bladder, causing inflammation, granuloma formation, and scarring. Patients may present with symptoms resembling serum sickness, including fever, chills, headache, myalgia, malaise, right upper quadrant abdominal pain, diarrhea, dry cough, lymphadenopathy, and hepatosplenomegaly; significant eosinophilia is routinely noted. The combination of contact with freshwater in sub-Saharan Africa followed in a few weeks by fever and eosinophilia is characteristic of the diagnosis of schistosomiasis and specific enough to warrant initiation of appropriate treatment. Chronic and Advanced Disease Chronic schistosomiasis is far more common than the acute disease. The symptoms and severity of disease are related to the species, number of eggs trapped in tissues, their distribution, and duration of infection. Urogenital Disease Even when parasite burden is relatively low, urinary schistosomiasis is often symptomatic. Urinary tract disease develops after infection with S haematobium and 504 Succinct Pediatrics the subsequent local inflammation after eggs are lodged in the tissues. Hematuria appearing 10 to 12 weeks after infection is often the first sign of disease. Progressive involvement, fibrosis, and calcification of the bladder and ureters can result in hydroureter and hydronephrosis. Eggs trapped in the gut wall lead to inflammation, ulceration, hyperplasia, microabscess formation, and polyposis. Hepatomegaly, secondary to granulomatous inflammation, occurs early in the evolution of chronic disease. Progressive obstruction of blood flow leads to portal hypertension, which ultimately leads to the development of portosystemic collateral vessels. These collateral vessels can lead to varices, variceal bleeding, splenomegaly, and hypersplenism, as well as allow schistosome eggs to embolize to the pulmonary circulation. Eggs lodged in pulmonary arterioles lead to pulmonary hypertension and cor pulmonale; presenting symptoms include dyspnea and pulmonary nodules on chest radiograph.
Cheap kaletra american express
Her past medical history is significant for breast cancer with recurrence 5 years ago 8h9 treatment buy generic kaletra line, treated with high-dose alkylating chemotherapy and radiation. According to her oncologist, who saw her last 11 months ago, she is in full remission. Her laboratory exam has been unremarkable, including a blood smear, a hemoglobin of 39%, and white blood count 2400/m3, which has been stable for years. Having examined the image of the skin lesion, what is your most important differential diagnosis A 62-year-old man presents to clinic with a 2-week history of a metallic taste in his mouth and oropharyngeal dysphagia for 3 months duration. He denies lymph node swelling, weight loss, regurgitation, halitosis, and odynophagia. His sleep is irregular with frequent awakenings at night, and his wife complains about her husband snoring excessively, in particular when lying on his back. Local abscess with sepsis in a patient with chemotherapy-induced decreased white and red blood cell count C. Postoperatively, he was treated with mesalamine 400 mg tablets, three tablets, three times a day. Within 3 years of the first surgically-induced remission, the patient had a second operation for an anastomotic stricture with obstruction, treated with resection and primary anastomosis. The postoperative course was complicated by dehiscence and abscess formation, resulting in creation of an ileostomy, mucus fistula, and colonic stump of about 60 cm in length. The patient recovered and was treated during the ensuing years with azathioprine 175 mg by mouth, once a day, with metabolites in the therapeutic range. A short course of prednisone 40 mg taper for 50 days had little effect controlling the lesion. Prednisone 60 mg by mouth per day taper and reintroduction of azathioprine at a lower dose to prevent neutropenia D. A 37-year-old man presents to your clinic for further workup of sudden onset of secretory diarrhea with ten to twelve watery bowel movements day and night. With a job as an executive, he finds himself increasingly fatigued, with occasional lapses in focus and confusion; he finds he is unable to follow conversations. Physical exam is remarkable for two light purple, macular and scaling lesions on his forehead and left forearm. A 78-year-old man presents to gastroenterology outpatient clinic for a 4-month history of progressive globus sensation, cough, and halitosis. He feels that food gets stuck in the throat during swallowing and has intermittent nocturnal regurgitation of food. In the left submandibular triangle you discover a soft, mobile nodule that is tender to palpation and indistinguishable from an enlarged left thyroid lobe. The rest of his exam is relevant for a 3/6 systolic murmur, bilateral decreased breath sounds, and a normal abdominal exam. The patient had a colonoscopy 6 years ago that was consistent with three hyperplastic polyps in the rectum and left colonic diverticulosis. Referral to otolaryngology for endoscopic exam of pharynx with visualization of vocal cords and swallowing study D. A 24-year-old female graduate student presents to your outpatient clinic with a 3-year history of irritable bowel syndrome with daytime diarrhea and diffuse, cramping abdominal pain, predominantly located in the left lower quadrant. Her pain is consistently precipitated by food with a delay of 2 hours, followed by two episodes of massive diarrhea. She was managed with a combination of simethicone as needed, omeprazole 20 mg per day, imodium 2 mg by mouth twice a day, and oral hyoscyamine 0. Initially, laboratory exams were normal for complete blood count and comprehensive metabolic panel. Celiac serologies, stool studies for pathogenic bacteria, fecal fat, and white cells all were negative. Due to persistent symptoms, you schedule a lactulose breath test, which is reported positive with 146 ppm after 2 hours. However, within 2 months her symptoms recurred with increased severity, now including a 6-pound weight loss, nausea, severe abdominal distention, and borborygmi. The decision is made to treat with rifaximin 550 mg three times a day for 14 days. The patient is tearful and frustrated with her course of disease and care, which interfers with her studies. You are called to the emergency department to help evaluate a 58-year-old woman with syncope after complaining of sudden onset of left lower quadrant sharp abdominal pain at home. Her physical exam is remarkable for a heart rate of 110 bpm, a markedly distended abdomen with minimally active bowel sounds, and left upper quadrant tenderness to palpation, but no rebound or guarding. The patient is known to have long-standing systemic sclerosis complicated by numerous small bowel diverticuli, ranging in size from 3 cm to 3. An 88-year-old man with a known asymptomatic and stable 2 cm Zenker diverticulum diagnosed 4 years ago presents to your clinic with sensation of progressive leftsided neck fullness and blood in expectorant. The endoscopy revealed a second lumen proximal to the upper esophageal sphincter, and the proximal esophagus was intubated without difficulties. At the time of diagnosis the patient decided to not have the diverticulum surgically removed, given that he was asymptomatic. His past medical history is significant for pulmonary emphysema, deep venous thrombosis, and recent onset of arthritis of his left wrist after a fall 6 years ago, treated with ibuprofen 400 mg by mouth, three times a day. A 23-year-old man from India presents to your clinic with the complaint of intermittent, sharp, nonradiating 9 out of 10 abdominal pain, lasting up to an hour, for the past year. He recently arrived in the United States to fill a postdoctoral position at your university for the next 2 years. On physical exam you find a thin man, clearly uncomfortable with a fever, pronounced bilateral breath sounds, tachycardia, and a tender left lower quadrant to palpation. His enhanced computer enterography is consistent with left lower quadrant massive lymphadenopathy, inflamed terminal ileum with marked narrowing of the lumen, and numerous distinct, prestenotic, round, loose 1 cm filling defects. Besides admission to the hospital and isolation, what has to be done about the terminal ileum filling defects The pain is related to food intake, delayed by 2 hours after eating, most severe during daytime, and associated with nausea but without vomiting. Since the onset of his symptoms, the patient has decreased the frequency of his meals and has lost 46 Topics Involving Multiple Organs approximately 17 pounds of weight. His past medical history is remarkable for a gunshot wound to the abdomen with exploratory laparotomy at the age of 21, hypertension, and chronic renal insufficiency. Social history revealed him to be an active smoker with a 35-year history of tobacco use. He has localized periumbilical tenderness to deep palpation and a negative rectal exam for blood. Referral to pain clinic for trigger point injection colon, but it is otherwise a normal exam. A 55-year-old man with alcoholic cirrhosis presents to the endoscopy suite for massive diuretic refractory ascites. For the past year, the patient required paracentesis every 6 weeks, completed without complication. He was evaluated by the transplant committee but was rejected because of noncompliance regarding smoking cessation, alcohol consumption, and medication management. On physical exam, you note caput medusae, hypoactive bowel sounds, tenderness, ascites with tachypnea, and an umbilical hernia. Following successful insertion of a draining catheter in the right lower quadrant, a total of 7 L of clear yellow fluid is drained. On physical exam you note the now deflated umbilical hernia, which is extremely tender to palpation and is increased in size. Surgical consult, laparoscopic repair, repeat postoperative paracentesis if necessary D. A 24-year-old man is brought to the emergency department by his girlfriend after having swallowed a large number of razor blades of various size and glass fragments in an attempt to commit suicide. He is complaining of epigastric abdominal pain and sore throat with specks of blood staining his sputum. On physical exam, he has a heart rate of 90 bpm and blood pressure of 90/52 mm Hg. An abdominal x-ray shows numerous square radiodense foreign bodies in the right upper quadrant without free air. Do not attempt endoscopic retrieval as foreign bodies are no longer within reach of the standard endoscope B.
Discount kaletra 250mg mastercard
Serologic testing is used to confirm the diagnosis if erythema migrans is not present treatment 0f osteoporosis buy discount kaletra 250mg on-line. Most will be afebrile and have arthritis of a knee that is often subacute in its manifestations with only mild to moderate tenderness and limitation of motion, sometimes despite large effusions. However, in some children the presentation can mimic acute bacterial arthritis with fever and an acutely inflamed and tender joint. Arthrocentesis should not be routine, since it rarely is helpful or necessary in children with a subacute presentation, but arthrocentesis is mandatory in patients who present with acute signs that are consistent with a possible septic arthritis, since it is important to determine the bacterial cause for appropriate treatment. White blood cell counts in synovial fluid of patients with typical Lyme arthritis usually range from 15,000 to 50,000/mcL, but sometimes can be 100,000/mcL or more with a preponderance of neutrophils, requiring culture of joint fluid (negative in Lyme arthritis) and serum 180 Succinct Pediatrics tests for IgG antibodies to B burgdorferi to make an accurate diagnosis. Polymerase chain reaction test of synovial fluid may be useful in select cases in which the diagnosis is in question. A positive result simply means that a component of the bacteria, depending on polymerase chain reaction target, is present (which may persist for some time after treatment with antimicrobials has killed the bacteria). Coinfections Ixodes scapularis ticks can also transmit Babesia microti, the usual cause of babesiosis, and Anaplasma phagocytophilum, the cause of human granulocytic anaplasmosis (formerly termed human granulocytic ehrlichiosis). Consequently, these possible coinfections, though they occur in only some cases of Lyme disease, should be considered in patients with symptoms, signs, or test results that are atypical or unusually severe (eg, very high or prolonged fever, leukopenia, thrombocytopenia, or anemia) or who do not respond as expected to treatment. In addition, these ticks can also transmit Borrelia miyamotoi, an organism in the relapsing fever group of Borrelia, and deer-tick (Powassan) virus, which can cause severe encephalitis. Management Recommended treatment for children with Lyme disease is shown in Table 17-3. Antimicrobial treatment should be continued if this occurs, since the reaction resolves spontaneously in 24 to 48 hours. Single and Multiple Erythema Migrans As outlined in the Table 17-3, treatment with a 14- to 21-day regimen of orally administered antimicrobials is recommended for erythema migrans and highly effective. The preferred drugs are doxycycline (children 8 years; a large trial in adults indicated that 10 days is sufficient treatment) or amoxicillin. Once advanced heart block resolves, treatment may be completed with an oral agent. In rare cases of persistent synovitis despite repeat treatment with antimicrobials, a rheumatologist should be consulted. Firstgeneration cephalosporins, such as cephalexin, are not effective treatment for Lyme disease. Potential advantages of using doxycycline to treat Lyme disease include excellent penetration into the central nervous system compared with alternative oral agents and that it is effective in treating human granulocytic anaplasmosis, an illness that may occur as a coinfection with Lyme disease. Doxycycline is generally not recommended for children younger than 8 years because it may cause staining of their permanent teeth or for women who are either pregnant or lactating. A sun-induced dermatitis occurs in 15% to 30% of patients who take doxycycline, so precautions should be taken to protect their skin from the sun. Although there is some controversy, most experts treat patients with cranial nerve palsies, except for those with concomitant signs or symptoms of meningitis, with orally administered antimicrobials (doxycycline is preferred when possible). Treatment of patients with facial nerve palsy is recommended to prevent other manifestations of Lyme disease. Corticosteroids are not indicated to treat patients with either facial nerve palsy or carditis caused by Lyme disease. If the eye does not close completely, drops to lubricate it should be administered several times a day. It is also important to monitor and manage elevated intracranial pressure in patients in whom there is evidence that it persists despite antimicrobial treatment. Cefuroxime is an alternative agent and particularly useful for empiric treatment while awaiting results of cultures if a patient presents with acute arthritis and methicillin-susceptible Staphylococcus aureus, Streptococcus pneumoniae, or Streptococcus pyogenes as part of the differential diagnosis in addition to Lyme disease. If the arthritis still does not resolve, consider either a persistent immunemediated arthritis (which is relatively rare in children) that is not responsive to antimicrobials because the organism has invariably already been killed or alternative diagnoses; referral to a specialist is usually indicated. Nonsteroidal anti-inflammatory drugs may also be helpful for treating pain or inflammation associated with Lyme arthritis. The cause and even relative frequency of this problem is unclear, because such nonspecific symptoms are relatively common in the general population without Lyme disease, especially among adolescents and adults. Some experts believe there is some degree of association between infection with Lyme disease and subsequent nonspecific symptoms, which are more common in patients with disseminated neurologic or late Lyme disease and those for whom treatment is delayed. Nevertheless, in most affected patients, these nonspecific symptoms resolve over time without additional antimicrobial treatment. There is no evidence that additional antimicrobial treatment is beneficial in persons with only nonspecific symptoms and no clinical signs of Lyme disease. Resistance of B burgdorferi to recommended first-line antimicrobials has not been reported. Multiple studies in both children and adults have documented overdiagnosis and overtreatment of Lyme disease in patients who never had objective signs of Lyme disease but only nonspecific symptoms. Positive laboratory test results alone, especially those done at "Lyme specialty laboratories" that often perform diagnostic tests that are unconventional or use unconventional interpretations of conventional tests, are generally not considered reliable evidence of Lyme disease. Management of Persons Bitten by an Ixodes Tick in Endemic Areas the risk of Lyme disease after a bite by its vector tick, even in areas in which Lyme disease has the highest incidence, is only 2% to 3%. In fact, most persons develop Lyme disease from a bite by a nymphal stage tick that is unrecognized. If there is certainty that the tick is either a nymphal or adult stage of Ixodes that is at least partially engorged, and the bite occurred in an area in which the risk that the tick is infected is at least 20% (which is generally true only in certain areas of New England and the eastern midAtlantic states as well as some parts of Wisconsin and Minnesota), a single dose of doxycycline (4 mg/kg, maximum: 200 mg), given with food to minimize nausea, may be offered to children 8 years and older to prevent Lyme disease (Evidence Level I). Follow-up tests for antibody against B burgdorferi in patients who had a tick bite but have no subsequent signs of Lyme disease are not indicated because the positive predictive value of such tests is poor. Routine testing of ticks for infection with B burgdorferi is also not indicated because there is no evidence that results of such tests are predictive of the risk of infection in the person who was bitten. Long-term Monitoring In general, long-term monitoring is unnecessary because treatment is usually highly effective. Moreover, follow-up depends on assessment of clinical signs and symptoms (persistent arthralgia or myalgia may be treated with 186 Succinct Pediatrics nonsteroidal anti-inflammatory drugs). Patients with early localized disease should be instructed to return if any complications develop (eg, new neurologic findings, such as facial nerve palsy) or if the rash or associated symptoms do not resolve. Patients with early disseminated or late Lyme disease should be seen in follow-up to be certain the signs have resolved and no additional manifestations (eg, new neurologic signs) develop. Facial palsy due to Lyme disease generally resolves completely, but mild, sometimes clinically inapparent, weakness may persist in some patients who undergo careful neurologic testing. Uncommon cases of persistent synovitis that last longer than 3 months or are severe should be referred to a rheumatologist. As with most infections, once antibodies against B burgdorferi develop, they (both IgM and IgG antibodies) may last for many years despite clinical cure. Furthermore, there is substantial variability in results of assays from batch to batch, so assessing whether antibody titers have changed over time as a means of assessing progression or cure of disease is generally unreliable. Persistence of immunoglobulin M or immunoglobulin G antibody responses to Borrelia burgdorferi 10-20 years after active Lyme disease. Diagnosis, treatment, and prevention of Lyme disease, human granulocytic anaplasmosis, and babesiosis: A review. Acute pediatric monoarticular arthritis: distinguishing Lyme arthritis from other etiologies. Outcomes of children treated for Lyme arthritis: results of a large pediatric cohort. The clinical assessment, treatment, and prevention of Lyme disease, human granulocytic anaplasmosis, and babesiosis: clinical practice guidelines by the Infectious Diseases Society of America.