Buy lopressor without a prescription
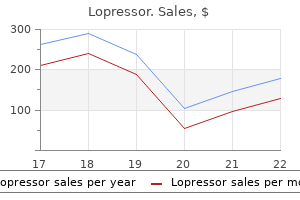
Delta storage pool disease: the malady is heterogeneous and affects the dense granules of platelets understanding prehypertension purchase lopressor 12.5mg. The most frequent complication of hemophilia A is a deforming arthritis caused by repeated bleeding into many joints. Although now uncommon, bleeding into the brain was formerly the most common cause of death. Many different mutations, from single-base substitutions to gross deletions, have been linked to hemophilia B. Severe liver disease may cause impaired secretion of these proteins as a manifestation of a general defect in protein synthesis. Thus, in vitamin K deficiency, activities of all the above-mentioned factors are low. In adults, vitamin K deficiency is uncommon and may reflect inadequate dietary intake. Because bacteria in the colon produce the form of vitamin K that is best absorbed, prolonged antibiotic intake or large colonic resections may lead to vitamin K deficiency. These effects are accompanied by consumption of platelets and coagulation factors and a hemorrhagic diathesis. It is also associated with metastatic cancer, hematopoietic malignancies, cardiovascular and liver disease and many other conditions. With the failure of normal control mechanisms, generation of thrombin leads to intravascular coagulation. With the consequent uncontrolled intravascular coagulation, the delicate balance between coagulation and fibrinolysis is disrupted. This leads to consumption of clotting factors, platelets and fibrinogen as well as a consequent hemorrhagic diathesis. With activation of the clotting cascade, intravascular fibrin microthrombi are deposited in the smallest blood vessels. Stimulation of the fibrinolytic system by fibrin generates fibrin split products, which possess anticoagulant properties and contribute to the bleeding diathesis. Microvascular obstruction is associated with widespread ischemic changes, particularly in the brain, kidneys, skin, lungs and gastrointestinal tract. These organs are also sites of bleeding, which, in the case of the brain and gut, may be fatal. Erythrocytes become fragmented (schistocytes) by passage through webs of intravascular fibrin, resulting in microangiopathic hemolytic anemia. The endothelial cell plays a central role in the inhibition of various components of the clotting mechanism. Fibrinopeptide A and Ddimers are elevated (as markers of coagulation and fibrinolytic activation, respectively). The hereditary tendency to develop thrombosis, regardless of its origin, is referred to as thrombophilia. The bleeding diathesis is evidenced by cerebral hemorrhage, ecchymoses and hematuria. Hypercoagulability May Cause Widespread Thrombosis Hypercoagulability is defined as an increased risk of thrombosis in circumstances that would not cause thrombosis in a healthy person. Disorders that enhance thrombosis have also been considered elsewhere (see Chapters 7, 10 and 11). Activated protein C resistance-factor V Leiden: A point mutation in the factor V gene (factor V Leiden) renders it resistant to proteolysis by activated protein C Compared with healthy persons, the risk for deep venous thrombosis is increased sevenfold in heterozygotes and 80-fold in homozygotes. Antithrombin deficiency: this autosomal dominant disorder, which has incomplete penetrance, occurs in 0. Table 20-5 563 Principal Causes of Neutropenia Decreased Production Irradiation Drug induced (long term and short term) Viral infections Congenital Cyclic Acquired Hypercoagulability Venous stasis contributes to the hypercoagulability associated with prolonged immobilization and congestive cardiac failure. Ineffective Production Megaloblastic anemia Myelodysplastic syndromes Increased Destruction Isoimmune neonatal Autoimmune Idiopathic Drug induced Felty syndrome Systemic lupus erythematosus Dialysis (induced by complement activation) Splenic sequestration Increased margination Antiphospholipid Antibody Syndrome Antibodies directed against several negatively charged phospholipids are associated with the development of antiphospholipid antibody syndrome. This autoimmune disorder features (1) arterial and venous thrombosis, (2) spontaneous abortions and (3) immune-mediated thrombocytopenia or anemia. The antiphospholipid antibody syndrome is the leading acquired hematologic cause of thrombosis. Proposed mechanisms include platelet activation, endothelial cell activation and alterations in the coagulation factor assembly on membranes. White Blood Cells the reader is referred to Chapters 2 through 4 for discussions of white blood cell structure and function. The term agranulocytosis denotes virtual absence of neutrophils caused by depletion of both the marginated pool and the bone marrow reserve. Neutropenia reflects decreased production or increased destruction of neutrophils (Table 20-5). Most cases of neutropenia are asymptomatic and unexplained, and the term chronic benign neutropenia is used. In some cases, the total granulocyte pool is normal, but excessive neutrophils are stored in the marrow or marginated in blood vessels. Radiation or chemotherapeutic drugs interfere with the generation of neutrophils by suppressing marrow cell production. Decreased production of granulocytes can also occur in rare hereditary disorders, including Kostmann syndrome and infantile genetic agranulocytosis. Mutations in the neutrophil elastase gene cause the most common form of congenital agranulocytosis Increased peripheral destruction of granulocytes may be occur in (1) overwhelming infection, (2) hypersplenism and (3) antibody-mediated processes, often involving drugs such as sulfonamides, phenylbutazone and indomethacin. Qualitative Disorders of Neutrophils Are Associated with Impaired Function If granulocyte function is defective, susceptibility to infection may increase despite a normal granulocyte count. Immunological Inflammatory Rheumatoid arthritis Rheumatic fever Vasculitis Monocytosis Is Seen in Malignant and Inflammatory Conditions the main causes of monocytosis include hematologic malignancies, immunologic and inflammatory conditions, infectious diseases and solid cancers. Hematologic malignancies account for at least half of peripheral blood monocytoses. In such cases, they may be either morphologically normal or immature and dysplastic. Monocytosis often occurs in neutropenic states, probably as a compensatory mechanism. Peripheral blood monocytosis may also accompany malignant lymphomas, either Hodgkin or nonHodgkin types. The benign, nonneoplastic, reactive conditions of mast cells are important to recognize and differentiate from the malignant syndromes. The symptoms of mast cell proliferative diseases are caused by the release of inflammatory mediators (see Chapter 2) and include fl ushing, pruritus and hives. The secretion of heparin also causes bleeding from the nasopharynx or gastrointestinal tract. Reactive mast cell hyperplasia is a nonmalignant process that occurs in immediate- and delayed-type hypersensitivity reactions and in lymph nodes that drain the sites of malignant tumors. The last is a rare autosomal recessive disease that is characterized by abnormal giant lysosomes in leukocytes and numerous other cells. Regardless of the basis for eosinophilia, accumulation of eosinophils in tissues often leads to necrosis, particularly in the myocardium, where it produces endomyocardial disease (see Chapter 11). They are relatively uncommon, with a yearly incidence of 6 to 10 cases per 100,000. The cause is usually unknown, although radiation or benzene exposure has been implicated in limited cases. Characteristic features of all subtypes include hypercellularity of the bone marrow with effective hematopoietic maturation and increased numbers of red cells, granulocytes or platelets. Leukemic cells represent transformed pluripotent stem cells with predominantly granulocytic differentiation. A normal cell contains two separate bcr (chromosome 22) and abl (chromosome 9) genes (right). Bone marrow biopsy shows hypercellularity, with total effacement of the marrow space by predominantly myeloid cells and their precursors. Patients report fatigue, anorexia, weight loss and vague abdominal discomfort due to hepatosplenomegaly. The bone marrow is conspicuously hypercellular due to an increase in granulocyte precursors, mature granulocytes and megakaryocytes. A smear of the bone marrow aspirate from the same patient reveals numerous granulocytes at various stages of development. Proliferation of the neoplastic clone occurs mainly in the bone marrow but may involve such extramedullary sites as the spleen, lymph nodes and liver (myeloid metaplasia).
Diseases
- Fissured tongue
- Stratton Parker syndrome
- Wohlwill Andrade syndrome
- Weaver Williams syndrome
- Chromosome 12, 12p trisomy
- Radiophobia
- Multiple sclerosis ichthyosis factor VIII deficiency
- Myalgic encephalomyelitis
- Neuroepithelioma
- Idiopathic pulmonary fibrosis
Order lopressor with american express
This technique is still commonly used in patients intolerant of endoscopy and in the assessment of oesophageal function and motility blood pressure treatment guidelines order lopressor us. Barium studies also have an important role in the evaluation of patients following gastrointestinal surgery to detect postoperative complications. Upper gastrointestinal endoscopy has effectively replaced radiological studies for imaging the stomach. Radiology continues to play a pivotal role in the investigation of small-bowel pathology, as the small bowel is much less amenable to conventional endoscopy due to its length and tortuosity. This technique has a higher diagnostic accuracy than barium enema and may be used in patients intolerant of colonoscopy or as a screening tool. Introduction Traditionally, barium studies were the mainstay of gastrointestinal tract imaging. Although the technique provides excellent mucosal detail, it has a relatively high false-positive rate (14%) due to mucosal breaks and erosions. In addition, it does not provide extraluminal information and its use is contraindicated in bowel obstruction and in patients with a history of bowel strictures. Many authorities advocate reserving capsule endoscopy for selected cases in which the suspicion of small-bowel disease remains high despite negative evaluations with endoscopy and radiological studies. Postprocessing options with both techniques include multiplanar reformations and maximum intensity projections, which are useful to assess the mesenteric vasculature and highlight enhancing pathology on coronal reconstructions. Other limitations include the need to administer intravenous contrast, possible poor toleration of the enteral contrast agent, and exposure to relatively high levels of ionizing radiation (up to 15 millisievert compared to 2 millisievert for a small-bowel follow-through). Exposure to ionizing radiation is a key consideration when deciding on the most appropriate imaging modality to investigate potential small-bowel disease. Dose optimization strategies include limiting the number of imaging phases acquired, omitting unnecessary images at the peripheries of acquired series that do not contribute to diagnosis, and the use of modern image reconstruction techniques such as iterative reconstruction that reduce radiation dose while still acquiring diagnostic quality images. The two imaging techniques most commonly used to achieve small-bowel distension are magnetic resonance enterography with oral contrast administration and magnetic resonance enteroclysis with infusion of the contrast solution through a nasojejunal tube. Enteric agents are classified as being positive (gadolinium, manganese ions), negative (super-paramagnetic iron oxides), or biphasic (water, polyethylene glycol) according to the signal intensity produced on T1- and T2-weighted images. Biphasic agents are the most commonly used and produce low signal on T1-weighted images, which contrasts well to hyperenhancing inflammatory or neoplastic tissue on postgadolinium sequences. Several new advanced imaging applications have been developed and investigated for small-bowel imaging in recent years including diffusion-weighted imaging, perfusion imaging, and motility imaging. Both diffusion and perfusion imaging have been shown to accurately discriminate normal from abnormal bowel, especially in inflammatory bowel disease. The choice of modality should be tailored to the individual patient with consideration of current guidelines. The right panel is from a contemporaneously acquired low-dose study performed at 18% of the conventional radiation dose study and reconstructed with pure model-based iterative reconstruction. Both images demonstrate thickening of distal ileal loops with associated mucosal hyperenhancement and mesenteric fat stranding (arrows). Barium studies There are two barium techniques that are utilized to image the small bowel: the barium follow-through and the small-bowel enema. The barium follow-through involves the oral administration of a barium suspension followed by the acquisition of prone films every 20 to 30 min until barium reaches the terminal ileum. Fluoroscopic compression views of the terminal ileum to separate overlying smallbowel loops are then performed. For the small-bowel enema technique, a nasojejunal tube is inserted and the barium suspension is infused to give better bowel distension. However, they provide very limited extraluminal information and patients often need to undergo further imaging with a cross-sectional technique. Ultrasonography Ultrasonography offers many advantages when imaging the small bowel: absence of ionizing radiation, low cost, and the dynamic realtime nature of the technique provides high temporal resolution. The technique generally involves systematic scanning of the abdomen with the use of graded compression to displace air and overlying bowel loops with a low- to medium-frequency ultrasound probe. Thickened, dilated bowel loops can often be identified but patient factors such as. An apparent stricture (arrowheads) is seen to resolve (left panel to right panel) as it represents an area of peristalsis. Furthermore, ultrasonography is operator dependent and may fail to identify disease in bowel loops located deep within the abdomen and pelvis and to detect complications such as fistulas and strictures. Contrast-enhanced ultrasonography involving the intravenous injection of microbubbles and hydrosonography, whereby the small bowel is distended with oral contrast, are two additional ultrasound techniques that are gaining in popularity. Ultrasound elastography is a novel technique that exploits the fact that pathological processes have altered elastic properties. This change in elasticity is detected and imaged using ultrasound elastography; this technique is currently under evaluation and may play a future role in small-bowel imaging. Many of these play a role in patient assessment when the results of other modalities have been negative or equivocal. Scintigraphy with red blood cells involves labelling red blood cells with a radioactive substance that can be detected on a gamma camera to identify occult sites of gastrointestinal bleeding. This may be done in vivo, whereby the patient is administered 99mTc-pertechnetate following an agent that reduces the radioisotope within the red blood cells or in vitro, whereby the binding process is performed after blood is taken from the patient and then reinjected. Extravasated red blood cells within the small bowel lumen are identified as a focus of activity that increases in intensity over time and moves along the expected anatomical course of the small bowel. Labelled white cell scanning is another nuclear medicine technique occasionally used in small-bowel imaging to detect sites of inflammation. The technique involves the administration of 99mTc-pertechnetate with any radioactivity appearing at the same time as orthotopic gastric mucosa. Detection rates are often increased by the administration of pentagastrin, glucagon, or a H2 blocker around the time of the procedure. Small-bowel involvement is typically transmural with skip lesions being a characteristic feature. The intervening submucosa may be of lower attenuation/signal intensity due to the presence of oedema in acute disease, fat in chronic disease, or an inflammatory infiltrate. Ulceration is identified by clefts in the thickened bowel wall, which may penetrate the wall forming an abscess. Other extraenteric complications include bowel obstruction, bowel stricture, and sinus tract and fistula formation. To the left of the arrow the bowel is dilated; to the right, decompressed small bowel is seen. This appearance is very nonspecific and could be due to an inflammatory or ischaemic stricture, nonsteroidal anti-inflammatory drug diaphragm-like stricture, or metastatic disease. Features of chronic disease include fibrotic strictures, pseudosacculation, and submucosal fat deposition. Transmural extension of inflammation into the mesentery of the affected bowel segment in the acute phase resulting in asymmetric inflammation and fibrosis with pseudosacculation of the antimesenteric border is a hallmark feature. Other associated conditions such as gallstones, sclerosing cholangitis, renal calculi, sacroiliitis, and adenocarcinoma may also be detected. Barium studies may demonstrate fold thickening, coarsening of the villous pattern, and aphthous ulceration, particularly along the mesenteric border. Tumours of the small bowel Small-bowel tumours account for less than 5% of all gastrointestinal tract tumours. They may be classified as benign or malignant and often produce nonspecific clinical symptoms and signs resulting in delayed diagnosis. Presentation may be with bleeding, bowel obstruction, intussusception, and rarely perforation. Carcinoid tumours occur most frequently in the ileum and are typically intensely enhancing luminal polyps or enhancing carpet lesions with mesenteric metastases being characteristic. The mesenteric disease incites a desmoplastic reaction producing a spiculated mass-like appearance, which may calcify. The imaging appearances are protean ranging from a solitary polypoid mass to segmental mural thickening with aneurysmal dilatation due to destruction of the myenteric plexus with associated adjacent lymphadenopathy. Transcoelomic spread may occur from colonic, gastric, or ovarian malignancies while haematogenous metastasis may occur from breast, lung, or melanoma primaries. The typical imaging findings are mild bowel wall thickening with dilatation, marked mucosal hyperenhancement, and mural stratification.
Trusted lopressor 12.5 mg
The broad spectrum of clinical manifestations ranges from barely discernible to severe hypertension online 12.5 mg lopressor visa, destructive, mutilating disease. Immune complexes containing such antibodies are produced in the synovium and activate complement. This increases vascular permeability and the uptake of immune complexes by leukocytes, which in turn release lysosomal enzymes, reactive oxygen species and other injurious products. Activated macrophages in the synovium continue to present antigens to T cells, thereby continuing the production of cytokines, which amplify inflammation and tissue injury. In addition, immune-complex deposits are present in the articular cartilage and the synovium. Abundant T lymphocytes in rheumatoid synovium are frequently Ia positive ("activated") and of the helper type. T cells may directly or indirectly interact with macrophages through production of cytokines that inhibit migration and proliferation of the latter. Vascularity increases, with exudation of fibrin into the joint space, which may result in small fibrin nodules that float in the joint (rice bodies). In this process, the synovium creeps over the surface of the articular cartilage and adjacent structures. This inflammatory synovium, now containing mast cells, is termed a pannus (cloak). The pannus covers the articular cartilage and isolates it from the synovial fluid. Lymphocytes aggregate into masses and eventually develop follicular centers The pannus erodes the articular cartilage and adjacent bone, probably through the action of collagenase produced by the pannus Eventually, the joint is destroyed and undergoes fibrous fusion, termed ankylosis. A characteristic lesion, termed the rheumatoid nodule, is found in extra-articular locations. The influx of lymphocytes, plasma cells and mast cells, together with neovascularization and edema, leads to hypertrophy and hyperplasia of the synovium. Eventually, the joint is destroyed and becomes fused, a condition termed ankylosis. Hyperplastic synovium from a patient with rheumatoid arthritis shows numerous finger-like projections with focal pale areas of fibrin deposition. A microscopic view reveals prominent lymphoid follicles (Allison-Ghormley bodies), synovial hyperplasia and hypertrophy, villous folds and thickening of the synovial membrane by fibrosis and inflammation. A higher power view of the inflamed synovium demonstrates hyperplasia and hypertrophy of the lining cells. Beyond the macrophages is a circle of lymphocytes, plasma cells and other mononuclear cells. The overall appearance resembles a peculiar granuloma surrounding a core of fibrinoid necrosis. Rheumatoid nodules are sometimes found in visceral organs, such as the heart, lungs and intestinal tract and even the dura. Most patients describe slowly developing fatigue, weight loss, weakness and vague musculoskeletal discomfort, which eventually localizes to the involved joints. Unabated disease causes progressive destruction of the joint surfaces and periarticular structures. Eventually, patients manifest severe flexion and extension deformities associated with joint subluxation, which may terminate in joint ankylosis. They are now recommended early in the course of the disease to prevent progression, induce remission and prevent joint deformities and functional disabilities. The group includes ankylosing spondylitis, Reiter syndrome, psoriatic arthritis and arthritis associated with inflammatory bowel disease. Ankylosing Spondylitis Ankylosing spondylitis is an inflammatory arthropathy of the vertebral column and sacroiliac joints. The disease is most common in young men, with a peak incidence at about age 20 years. The result is ultimate destruction of these joints, after which the spine becomes fused posteriorly. A few patients with ankylosing spondylitis rapidly develop crippling spinal disease, but most are able to maintain their employment and live a normal life span. Reiter Syndrome (Reactive Arthritis) Reiter syndrome is a triad that includes (1) seronegative polyarthritis, (2) conjunctivitis and (3) nonspecific urethritis. It occurs almost exclusively in men and usually follows venereal infection or an episode of bacillary dysentery. More than half of the patients develop mucocutaneous lesions similar to those of pustular psoriasis. Polyarticular disease with systemic symptoms: Twenty percent of children with polyarticular arthritis have prominent systemic symptoms, which include high fever, rash, hepatosplenomegaly, lymphadenopathy, pleuritis, pericarditis, anemia and leukocytosis. Pauciarticular arthritis: Children with involvement of only a few large joints such as the knee, ankle, elbow or hip girdle account for half of all juvenile arthritis cases and fall into two general groups. Of these patients, one third have ocular disease, characterized by chronic iridocyclitis (inflammation of the iris and ciliary body). Only a small minority of these children has residual polyarthritis or ocular damage. Joint disease is usually mild and only slowly progressive, although a mutilating form is occasionally encountered. Patients generally present with joint effusion and other manifestations of Lyme disease. Although there may be a transient arthritis with acute infection, patients can develop chronic Lyme arthritis, which is microscopically identical to rheumatoid arthritis. In the remainder of patients, there is an overproduction of uric acid, but the underlying abnormality been identified in only a minority of cases. The consensus today is that multiple genes control the level of serum uric acid and can be associated with gout. Secondary gout is associated with a number of conditions that result in hyperuricemia. Increased production is most often associated with increased nucleic acid turnover, as seen in leukemias and lymphomas as well as after chemotherapy. Dehydration and diuretics increase tubular reabsorption of uric acid and can result in hyperuricemia. Saturnine gout was described in 18th century England, where this disease was prevalent among the upper classes with lead plumbing in their houses (Saturn is the alchemical symbol for lead). Gout is characterized by acute and chronic arthritis and is classified as primary or secondary, depending on the etiology of the hyperuricemia. In primary gout, hyperuricemia is present without any other disease, whereas secondary gout occurs in association with another illness. Of all cases of hyperuricemia, one third are primary and the remainder are secondary. It is rare in children before puberty (other than in uncommon inherited diseases) and in women during the reproductive years. There is a tight balance between uric acid production and the tissue deposition of urates. Positive correlations exist between the prevalence of hyperuricemia in a population and mean weight, protein intake, alcohol consumption and other social variables. Thus, gout is a disease that exemplifies the interplay between genetic predisposition and environmental influences. Purine nucleotides are synthesized de novo from nonpurine precursors or derived from preformed purines in the diet. Purine nucleotides are catabolized to hypoxanthine or incorporated into nucleic acids. Hyperuricemia and gout result from (1) increased de novo purine synthesis, (2) increased cell turnover, (3) decreased salvage of dietary purines and hypoxanthine and (4) decreased uric acid excretion by the kidneys. Neutrophils that have ingested urate crystals release reactive oxygen species and lysosomal enzymes, which mediate tissue injury and promote an inflammatory response. The presence of long, needle-shaped urate crystals that are negatively birefringent under polarized light is diagnostic of gout. A tophus is an extracellular soft tissue deposit of urate crystals surrounded by foreign-body giant cells and an associated inflammatory response of mononuclear cells.

Generic lopressor 25 mg with amex
Symptomatic women initially exhibit endocervicitis blood pressure up and down order lopressor 12.5mg on-line, with a vaginal discharge or bleeding and dysuria. Infection often extends to produce acute and chronic salpingitis and eventually pelvic inflammatory disease. The source of infection is usually the ingestion of contaminated meat, milk, vegetables or other food products contaminated with bovine feces, a common source for the serotype. As in shigellosis, the mucosa of the distal ileum and colon are acutely inflamed and focally eroded and are sometimes covered by an inflammatory pseudomembrane. Neisseria gonorrhoeae is a gram-negative diplococcus with surface pili that form a barrier against phagocytosis by neutrophils. The pili contain an IgA protease that digests IgA on the luminal surface of the mucous membranes of the urethra, endocervix and fallopian tube, thereby facilitating attachment of gonococci. In men, gonococci attached to the mucous membrane of the urethra cause urethritis and, sometimes, urethral stricture. Urinary tract infections initially produce an acute inflammatory infiltrate at the site of infection, usually the bladder mucosa, which may ascend to the kidney to produce pyelonephritis (see Chapter 16). In some cases, concomitant capillary thrombosis causes necrosis of overlying mucosa and characteristic ulcers oriented along the long axis of the bowel. These lesions frequently bleed and occasionally perforate, producing infectious peritonitis. The organisms block the respiratory burst of macrophages and multiply within these cells, spreading throughout the body via the lymphatics and bloodstream. Persons with ruptured abdominal organs or acute pyelonephritis suffer gram-negative sepsis because the large numbers of organisms that gain access to the circulation overwhelm the normal defenses. Shigellosis is a self-limited disease that typically presents with abdominal pain and bloody, mucoid stools. Shigellae, which are among the most virulent enteropathogens, produce disease when as few as 10 to 100 organisms are ingested. Replicating shigellae kill infected cells and then spread to adjacent cells and into the lamina propria, producing a patchy inflammatory pseudomembrane, composed of neutrophils, fibrin and necrotic epithelium. The bacteria also produce a potent exotoxin, known as Shiga toxin, which causes severe watery diarrhea by interfering with fluid absorption in the colon. Infection is typically acquired by eating food contaminated with nontyphoidal Salmonella strains and is commonly called Salmonella food poisoning. The organisms proliferate in the small intestine and invade enterocytes in the distal small bowel and colon. The nontyphoidal Salmonella species elaborate several toxins that contribute to the dysfunction of intestinal cells. Salmonella enterocolitis remains a major cause of childhood mortality in less developed countries. The Cholera is a severe diarrheal illness caused by the enterotoxin of Vibrio cholerae, an aerobic, curved gram-negative rod. The organism proliferates in the lumen of the small intestine and causes profuse watery diarrhea, rapid dehydration and, if not treated, shock and death within 24 hours of onset of symptom. Cholera is common in most parts of the world, and major epidemics affecting tens of thousands have occurred in South America and currently in central sub-Saharan Africa. The infection remains endemic in the river deltas of India and Bangladesh, where it causes 500,000 deaths annually. Shellfish ingestion accounts for most of the rare sporadic cases in the United States. They do not themselves invade the mucosa but cause diarrhea by elaborating a potent exotoxin, cholera toxin, which activates adenylyl cyclase of the enterocyte. Replacing lost salts and water is a simple, effective treatment, which can often be accomplished by oral rehydration with preparations of salt, glucose and water. The bacterium is a microaerophilic, curved gram-negative rod, morphologically similar to the vibrios. The overlying skin becomes tense, as edema and gas expand underlying soft tissues. Microscopic examination shows extensive tissue necrosis with dissolution of the cells. A striking feature is the paucity of neutrophils, which are apparently destroyed by the myotoxin. The lesion develops a thick, serosanguinous discharge, which has a fragrant odor and may contain gas bubbles. Hemolytic anemia, hypotension and renal failure may develop and, in the terminal stages, coma, jaundice and shock supervene. Clostridial Diseases Clostridia are gram-positive, spore-forming, obligate anaerobic bacilli. The vegetative bacilli are found in the gastrointestinal tract of herbivorous animals and humans. Anaerobic conditions promote vegetative division, whereas aerobic ones lead to sporulation. Spores pass in animal feces and contaminate soil and plants, where they can survive unfavorable environmental circumstances. Under anaerobic conditions, the spores revert to vegetative cells, thereby completing the cycle. During sporulation, vegetative cells degenerate and the plasmids they contain produce a variety of specific toxins that cause widely differing diseases, depending on the species. Immunization programs using inactivated tetanus toxin have largely eliminated the disease from developed countries. Nonetheless, tetanus remains a frequent and lethal disease in developing countries. The bacteria are omnipresent in the environment, contaminating soil, water, air samples, clothing, dust and meat. Spores survive cooking temperatures and germinate to yield vegetative forms, which proliferate when foods such as meats, gravies and sauces are allowed to stand without refrigeration. The vegetative clostridia sporulate and elaborate a variety of exotoxins, which are cytotoxic to enterocytes and cause the loss of intracellular ions and fluid into the gut. The potent neurotoxin (tetanospasmin) undergoes retrograde transport through the ventral roots of peripheral nerves to the anterior horn cells of the spinal cord, where it binds to receptors on presynaptic terminals of motor neurons in the ventral horns. The release of inhibitory neurotransmitters is blocked, permitting unopposed neural stimulation and sustained contraction of skeletal muscles (tetany). Spastic rigidity often begins in the muscles of the face, giving rise to "lockjaw," which extends to several facial muscles, causing a fixed grin (risus sardonicus). Prolonged spasm of respiratory and laryngeal musculature eventually leads to death. Clostridial growth requires extensive devitalized tissue, as in severe penetrating trauma, wartime injuries and septic abortions. Necrosis of previously healthy muscle is caused by myotoxins, which are phospholipases that Clostridium botulinum spores are widely distributed and are especially resistant to drying and boiling. Botulism can also be contracted from home-cured ham, other meats and nonacidic vegetable products, such as carrot juice that has been left unrefrigerated for several days. Infant botulism is often associated with the consumption of contaminated honey or corn syrup by children. Spores pass in the feces, contaminate soil and plant materials and are ingested or enter sites of penetrating wounds. Meat dishes left to cool at room temperature grow large numbers of clostridia (106 organisms per gram). When contaminated meat is ingested, Clostridium perfringens types A and C produce enterotoxin in the small intestine during sporulation, causing abdominal pain and diarrhea. Clostridia are widespread and may contaminate a traumatic wound or surgical operation. Necrotic tissue at the wound site causes spores to revert to the vegetative form (bacilli). The toxin is transported in peripheral nerves and (retrograde) through axons to the anterior horn cells of the spinal cord. The toxin blocks synaptic inhibition and the accumulation of acetylcholine in damaged synapses leads to rigidity and spasms of the skeletal musculature (tetany). Improperly canned food is contaminated by the vegetative form of Clostridium botulinum, which proliferates under aerobic conditions and elaborates a neurotoxin. When it reaches cholinergic nerve endings at the myoneural junction, it inhibits acetylcholine release. Botulism is characterized by a descending paralysis, first affecting cranial nerves and causing blurred vision, photophobia, dry mouth and dysarthria.
Nelumbo nucifera (Lotus). Lopressor.
- What is Lotus?
- Bleeding, digestion problems, diarrhea, and other conditions.
- Are there safety concerns?
- Dosing considerations for Lotus.
- How does Lotus work?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96164

Order discount lopressor
Hypertension in the upper part of the body results in left ventricular hypertrophy and may produce dizziness blood pressure medication muscle weakness purchase genuine lopressor on-line, headaches and nosebleeds. Hypotension below the coarctation results in weakness, pallor and coldness of lower extremities. After birth, if the shelf does not undergo the normal involution, obliteration of the ductal orifice does not permit free flow around the persistent posterior shelf, thereby creating a juxtaductal obstruction of blood flow to the distal aorta. If the aortic isthmus does not dilate during late fetal life, it remains narrow, resulting in an infantile or preductal coarctation. Most patients with coarctation of the aorta die by age 40 unless they are treated. Complications include (1) heart failure, (2) rupture of a dissecting aneurysm (secondary to cystic medial necrosis of the aorta), (3) infective endarteritis at the point of narrowing or at the site of jet stream impingement on the wall immediately distal to the coarctation, (4) cerebral hemorrhage and (5) stenosis or infective endocarditis of a bicuspid aortic valve. Coarctation of the aorta is successfully treated by surgical excision of the narrowed segment, preferably between 1 and 2 years of age for asymptomatic patients, or by balloon dilation using cardiac catheterization. Good results have been obtained with balloon dilation of the stenotic valve by cardiac catheterization. Pulmonary stenosis may also result from a variety of additional developmental deformities of the heart including peripheral pulmonary stenosis of the pulmonary arteries. Congenital Aortic Stenosis Three types of congenital aortic stenosis are recognized: valvular, subvalvular and supravalvular. A congenitally bicuspid aortic valve is considerably more frequent (4:1) in males than in females and is associated with other cardiac anomalies A bicuspid valve typically features fusion of two of the three semilunar cusps (the right coronary cusp with one of the adjacent two cusps). Over the years, the resulting bicuspid valve tends to become thickened and calcified, generally leading to symptoms in Pulmonary Stenosis Isolated pulmonary stenosis ordinarily involves the valve cusps, which are fused to form an inverted cone or funnel type of constriction (isolated valvular pulmonary stenosis). The artery distal to the valve may develop poststenotic dilation after several years. More severe forms of congenital aortic stenosis involving unicommissural or valves without commissures cause symptoms in early life. In symptomatic cases, aortic valvulotomy has had a high degree of success, although valve replacement is occasionally indicated. Stenosis results from a membranous diaphragm or fibrous ring that surrounds the left ventricular outflow tract immediately below the aortic valve. In many persons with subvalvular aortic stenosis, thickening and immobility of the aortic cusps develops, with mild aortic regurgitation. Surgical treatment of subvalvular aortic stenosis involves excising the membrane or fibrous ridge. The syndrome is characterized by idiopathic infantile hypercalcemia, mental retardation and stenotic disease of the aorta, pulmonary artery and other medium- to large-sized arteries. Microscopically, these plaques are areas of endocardial fibroelastotic thickening, frequently accompanied by degeneration of adjacent subendocardial myocytes. Diffuse endocardial thickening involves most of the left ventricle as well as the aortic and mitral valve leaflets. The thickened endocardium tends to obscure the trabecular pattern of the underlying myocardium, and papillary muscles and chordae tendineae are thick and short. In such cases, disruption in the continuity of the conduction system is probably caused by the accompanying cardiac abnormality. It is often associated with a mirror image of the normal leftsided location and configuration. The position of the ventricles is determined by the direction of the embryonic cardiac loop. If the loop protrudes to the right, the future right ventricle develops on the right and the left ventricle comes to occupy its proper position. These include transposition of the great arteries, a variety of atrial and ventricular septal defects, anomalous pulmonary venous drainage and many others. In dextrocardia that occurs with situs inversus, the heart is functionally normal, although minor anomalies are not uncommon. Alternatively, the defect may consist of a fibrous separation of the atrioventricular node from the ventricular conducting tissue. Although the heart rate is abnormally slow, patients with isolated heart block often have little functional difficulty. Later in life, cardiac hypertrophy, attacks of Stokes-Adams syncope (dizziness and unexpected fainting), arrhythmias and heart failure may develop. The disorder is classified as primary or secondary, the latter being far more common. Ischemic Heart Disease Ischemic heart disease is, in most cases, a consequence of coronary artery atherosclerosis. It develops when blood flow is inadequate to meet the oxygen demands of the heart. By contrast, atherosclerotic heart disease is far less frequent in developing countries. It typically occurs in the substernal portion of the chest and may radiate to the left arm, jaw and epigastrium. A patient with typical angina pectoris exhibits recurrent episodes of chest pain, usually brought on by increased physical activity or emotional excitement. The pain is of limited duration (1 to 15 minutes) and is relieved by reducing physical activity or by treatment with sublingual nitroglycerin (a potent vasodilator). Angina is not associated with anatomic changes in the myocardium as long as the duration and severity of ischemic episodes are insufficient to cause myocyte necrosis. The responsible mechanisms are not fully understood but endothelial dysfunction plays a major role. Whereas coronary artery spasm may contribute to the pathogenesis of an acute myocardial infarction or to the size of the infarct, it is generally not the principal cause of infarction. It may occur during rest or sleep and is associated with development of nonocclusive thrombi over atherosclerotic plaques. In some cases of unstable angina, episodes of chest pain become progressively more frequent and longer in duration over a 3- to 4-day period. Unstable angina is also termed preinfarction angina, accelerated angina or "crescendo" angina. Without pharmacologic or mechanical intervention to "open up" the coronary narrowing, many patients with unstable angina progress to myocardial infarction. The development of an infarct is related to the duration of ischemia and the metabolic rate of the ischemic tissue. In experimental coronary artery ligation, foci of necrosis form after 20 minutes of ischemia and become more extensive as the period of ischemia lengthens. Contractile impairment in these patients is due to irreversible loss of myocardium from previous infarcts and hypoperfusion of surviving muscle, which leads to chronic ventricular dysfunction. Many of these patients die suddenly, especially those in whom contractile impairment is not severe. In many cases, lethal arrhythmia is likely triggered by acute ischemia without overt myocardial infarction. However, the presence of a healed infarct or ventricular hypertrophy increases the risk that an episode of acute ischemia will initiate a life-threatening ventricular arrhythmia. Any one of these factors significantly increases the risk of myocardial infarction, but a combination of multiple factors augments the risk more than sevenfold (see Chapter 8). In 1950, the age-adjusted annual death rate from myocardial infarction in the United States was 226 per 100,000 population-50 years later, it was 150. This shift reflects many factors, including reduced smoking, lower dietary saturated fat and new drugs that control hypertension, reduce cholesterol and lyse coronary thrombi. The risk of ischemic heart disease increases in proportion to the number of cigarettes smoked. Increased levels of plasma factors involved in thrombosis or the inhibition of thrombolysis, such as fibrinogen, plasminogen activator inhibitor-1, homocysteine and decreased fibrinolytic activity, contribute to the risk of myocardial infarction. Levels of selected serum markers of inflammation, such as C-reactive protein, are also predictors of ischemic heart disease. During the past several years, there has been a remarkable increase in the incidence of type 2 diabetes in the United States, which mirrors a similar increase in obesity (see Chapter 22). Ischemic heart disease is a consequence of both type 1 and type 2 diabetes, and the risk is twofold to threefold greater than in nondiabetic individuals. Other risk factors for ischemic heart disease include: Obesity: In a major, longitudinal study of one population (Framingham Heart Study), obesity was an independent risk factor for cardiovascular disease, with an increased risk for obese persons over those who are lean of 2 to 2.
Buy 25mg lopressor with mastercard
Chronic periodontal disease typically occurs in adults with poor oral hygiene or in individuals with a strong family history of the disease heart attack kidney damage purchase 12.5mg lopressor free shipping. Chronic periodontitis causes loss of more teeth in adults than does any other disease, including caries. The condition is caused by the accumulation of bacteria under the gingiva in the periodontal pocket. As the mass of bacteria adhering to the surface of tooth (dental plaque) ages, it mineralizes to form calculus (tartar). Adult periodontitis is mostly associated with Bacteroides gingivalis, Bacteroides intermedius, Actinomyces species and Haemophilus species. Agranulocytosis causes necrotizing ulcers anywhere in the oral and pharyngeal mucosa, but especially in the gingiva. Infectious mononucleosis often results in gingivitis and stomatitis, with exudate and ulceration. Necrosis and ulceration of the gingiva predispose to severe superimposed infection, which may cause loss of teeth and alveolar bone. This newly formed dentin is opposite the area of tooth destruction and was produced by the stimulated odontoblasts. Odontogenic Tumors: Ameloblastoma Ameloblastomas are tumors of odontogenic epithelia and are the most common clinically significant odontogenic tumor. The abundant serous discharge then becomes mucopurulent, after which the surface epithelium is shed. Chronic rhinitis is characterized by nasal mucosal thickening due to persistent hyperemia, mucous gland hyperplasia and lymphocyte and plasma cell infiltration. Often called hay fever, allergic rhinitis may be acute and seasonal or chronic and perennial (see Chapter 4). A common histologic pattern is characterized by islands of odontogenic epithelium with a central stellate reticulum-like area, surrounded by basal cells with a "picket fence" appearance, due to subnuclear vacuoles. The etiology involves multiple factors, including allergy, infections, diabetes mellitus, cystic fibrosis and aspirin intolerance. Sinonasal inflammatory polyps are lined externally by respiratory epithelium and contain mucous glands within a loose mucoid stroma, which is infiltrated by plasma cells, lymphocytes and many eosinophils. Microscopically, ameloblastoma resembles the enamel organ in its various stages of differentiation, and a single tumor may show various histologic patterns. Accordingly, tumor cells resemble ameloblasts at the periphery of epithelial nests or cords, where columnar cells are oriented perpendicularly to the basement membrane. Although incompletely excised tumors may recur, the tumor ordinarily does not metastasize. Some may spread and yet remain histologically benign (metastasizing ameloblastoma). The causes range from the common cold to unusual infections, such as diphtheria and anthrax. The virus replicates in epithelial cells, causing the degenerating cells to be shed. The mucosa is edematous and engorged and is infiltrated by neutrophils and mononuclear cells. Abundant mucus secretion and increased vascular permeability produce rhinorrhea (free discharge of a thin nasal mucus). Viral rhinitis may be followed within a few days by or foreign body that interferes with sinus drainage or aeration renders it liable to infection. If the ostium of a sinus is blocked, secretions or exudate accumulate behind the obstruction. Maxillary sinusitis may also be caused by odontogenic infections, in which case bacteria from the roots of the first and second molars penetrate the thin bony plate that separates them from the floor of the maxillary sinus. Chronic sinusitis is a sequel of acute inflammation, either as a result of incomplete resolution of infection or because of recurrent acute complications. In contrast to acute sinusitis, the purulent exudate in chronic sinusitis almost always includes anaerobic bacteria. Rhinoscleroma is endemic in some Mediterranean countries and in parts of Asia, Africa and Latin America. Microscopically, the granulation tissue is strikingly rich in plasma cells, lymphocytes and foamy macrophages. The characteristic large macrophages, referred to as Mikulicz cells, contain masses of phagocytosed bacilli. Serologic tests are valuable in establishing the diagnosis of rhinoscleroma because specific antibodies are present in many patients. They arise from the sinonasal mucosa, the ectodermally derived lining of the sinonasal tract (Schneiderian membrane). Three morphologically distinct benign papillomas are recognized: inverted, oncocytic (cylindrical or columnar cell) and fungiform (exophytic, septal) papillomas. They are composed of a uniform cellular proliferation, which displays an inflammatory cell infiltrate and scattered microcysts. As the name implies, they show characteristic inversions of the surface epithelium into the underlying stroma. Unless surgical resection extends beyond the boundaries of grossly visible lesions, they frequently recur. Several industrial chemicals including nickel and chromium have been reported to increase the risk of cancer of the nose and sinuses. Squamous tumors in nickel workers usually arise from the middle turbinate, with latencies from 2 to 32 years. Cancers of the nasal cavity and sinuses grow relentlessly and invade adjacent structures. Follicular tonsillitis is characterized by pinpoint exudates that can be extruded from the crypts. Pseudomembranous tonsillitis refers to a necrotic mucosa covered by a coat of exudate, for instance, in diphtheria or in Vincent angina (see above). However, repeated infections can cause enlargement of tonsils and adenoids to a degree that obstructs air passages. In children, repeated bouts of streptococcal tonsillitis may progress to rheumatic fever or glomerulonephritis, and patients may benefit from tonsillectomy. Peritonsillar abscess (quinsy) is a collection of purulent material behind the posterior capsule of the tonsil, usually due to infection with - and -hemolytic streptococci. Untreated, peritonsillar abscesses may result in several life-threatening situations, such as rupture into the airway, weakening of the carotid artery wall or penetration into the mediastinum, the base of the skull or the cranial vault. Adenoids represent chronic inflammatory hyperplasia of the pharyngeal lymphoid tissue. Enlarged adenoids may cause partial or complete obstruction of the eustachian tube, leading to otitis media. The tumor infiltrate is characteristically polymorphic and surrounds small- to medium-sized blood vessels (angiocentric), infiltrates through vascular walls (angioinvasive) and often occludes vessel lumina like a thrombus, causing necrosis in adjacent tissues (ischemictype). Ulcers are covered by a black crust, under which lesions progress to erode cartilage and bone, causing defects in the nasal septum, hard palate and nasopharynx. Death is due to secondary bacterial infection, aspiration pneumonia or hemorrhage from eroded large blood vessels. These tumors most commonly arise in adolescent males but are not restricted to that age group. Nasopharyngeal inflammation occurs mainly in children, although it is also common in adolescents and young adults. Viral or bacterial infections may be limited to the palatine tonsils, but nasopharyngeal tonsils or adjacent pharyngeal mucosa may also be involved, often as part of a general upper respiratory tract infection. In the latter case, initial infecting agents are most often viruses spread by droplets or by direct contact. These include influenza, parainfluenza, adenovirus, respiratory syncytial virus and rhinovirus. They typically arise submucosally in the posterolateral nasal wall, posterior to the sphenopalatine foramen, and tend to expand into adjacent structures, causing local mass effects. Angiofibromas may grow into fissures and foramina of the skull or destroy bone and spread into adjacent structures.

Purchase lopressor 50 mg with visa
Common mechanism of injury is excessive flexion of hip in lithotomy position Foot drop arteria tibialis posterior buy cheap lopressor, foot eversion weakness compared with inversion and sensory loss over the dorsum of foot and lateral aspect of shin. Can be precipitated by prolonged squatting or stirrups Weakness of hip adduction and sensory loss medial aspect of thigh. Usually precipitated during assisted delivery Short course prednisolone treatment, eye protection, and artificial tears Overnight wrist splints. Some require local steroid injections or even decompression Usually improves spontaneously but treatment options can include lidocaine patch or capsaicin cream Conservative management with physiotherapy and analgesia Recovery usually within three to four months See treatment of femoral neuropathy Common peroneal nerve Obturator nerve See treatment of femoral neuropathy Arteriovenous malformations Intracranial arteriovenous malformations are relatively uncommon but a recognized cause of catastrophic intracerebral haemorrhages. Furthermore, there are identified predictors of haemorrhage, such as age, location, and deep venous drainage, and these can be useful for evaluating risk. Treatment of unruptured arteriovenous malformations should largely be restricted to outside of pregnancy. Treatment options include endovascular embolization, surgery, or stereotactic radiotherapy. In terms of the issues surrounding labour, these are similar to those mentioned in the management of cerebral aneurysms, and decisions should be made on an individual patient basis. Reversible cerebral vasoconstriction syndrome: a rare cause of postpartum headaches. Peripheral nerve disorders the most frequent examples of peripheral nerve disorders encountered during pregnancy, labour, and the post-partum period are listed in Table 14. It is particularly important to recognize these as they may have serious health implications for mother and child. Intrahepatic cholestasis of pregnancy-occurs in 1/40 to 1/500 pregnancies and is the most serious cause of itch in pregnancy, with potentially substantial effects on mother and fetus. Atopic eruption of pregnancy-affects 1/300 pregnancies, typically with an eczematous eruption over abdomen and limbs. Polymorphic eruption of pregnancy- affects about 1/ 240 pregnancies, usually beginning with red papules and plaques on the abdomen and thighs before spreading more widely. Treatment is with reassurance and emollients, with topical steroids if neccessary. Pemphigoid gestationis-occurs in 1/50 000 pregnancies and is due to circulating antibodies against the skin basement membrane zone. The eruption often begins around the umbilicus and spreads to the whole trunk, limbs, hands, and feet. Common skin changes in pregnancy Vascular changes and lesions There is increased skin blood flow during pregnancy, possibly resulting in oedema Spider naevi and palmar erythema are common, and there maybe erythema of the gums (with gingivitis) and the vulvovaginal area. Swollen skin around the ankles may be a first sign, worsening during the day and improving over night when lying down. Supportive stockings or flight socks should be worn: special pregnancy types are available. If there is a family or personal history of the development of varicose veins or thrombophlebitis/phlebothombosis, further risk assessment for venous thromboembolism is required. Pyogenic granuloma, a benign tumour with a tendency to ulcerate and bleed, may develop on the skin or oral cavity, where they are known as pregnancy tumours. They are Introduction the skin undergoes profound alterations during pregnancy as a result of endocrine, metabolic, and physiological changes. Some of these are trivial and chiefly cosmetic, producing no or minor symptoms; some will improve during or after pregnancy and others can be distressing and/or of major medical importance. Pregnancy will profoundly modify expression of preexisting skin disease, and there are dermatoses that are specific to pregnancy. Hirsutism may begin or worsen in pregnancy, driven by an increase in androgens and usually resolving a few months after delivery. Pilosebaceous changes/acne the development of acne during pregnancy is unpredictable. The increase in oestrogens usually improves acne, but there may be worsening of acne in some unfortunate patients. Acne treatment in pregnancy may be tricky as topical and oral vitamin A derivatives must be avoided because they are teratogenic. Topical treatment with benzoyl peroxide and clindamycin for limited areas (most commonly the face) are the treatments of choice in pregnancy. Striae gravidarum Striae gravidarum (stretch marks) are common in pregnancy, affecting about 50% of women. They are more frequently seen in young women, in women with a raised body mass index, and those who have large babies. They are familial in about 50% of cases and are more likely if a woman has had them previously. The breasts and sides and lower areas of the abdomen are the typical sites, but thighs and arms can be affected. They start as linear depressed purple lines and fade to pale, atrophic, scar-like lesions. Olive oil massage, castor oil, cocoa butter, glycolic or fruit acids, homeopathic creams and/or oils are used, but the benefit of these is not proven. Pruritus Itching occurs in about 20% of pregnancies, frequently in association with an inflammatory dermatosis such as atopic eczema, polymorphic eruption of pregnancy, allergic reactions, or infectious diseases. Oral antihistamines such as loratadine are safe to be used in pregnancy and can be used for symptomatic relief (see Table 14. The most serious cause is intrahepatic cholostasis of pregnancy, which is diagnosed in about 3% of itchy pregnant women (see below and Chapter 14. Pigmentary changes and pigmented lesions Increased skin pigmentation is common, particularly in darkskinned women, up to 90% of whom may be affected. Melasma often disappears spontaneously after delivery, but treatment with topical vitamin A derivatives and hydrochinon may be indicated after pregnancy in some women. Pigmented naevi can increase in size, in particular around the abdomen due to the increased body circumference, and pigmentation during pregnancy. Melanoma may occur and is not associated with a poorer prognosis in pregnant women. Any rapidly changing, irregularly shaped, or irregularly pigmented lesion larger than 6 mm in diameter should be excised under local anaesthesia to exclude a dysplastic naevus or melanoma. Risk factors for developing a melanoma are fair skin, high density of freckles, red hair, more than 50 moles, the presence of more than five atypical moles (irregular shape and colour), a history of severe sunburns during childhood, especially with blistering, and a family history of melanoma. Urticaria Urticaria (hives) and dermographism (wealing in response to pressure, Urticaria has been attributed by some authors to physiological changes in vascular reactivity. Particular drugs or foods may be the cause in some patients and must be avoided in such cases. Treatment with a nonsedating antihistamine such as loratidine, cetirizine or sedating chlopheniramine is safe. Cutaneous infections Candida of the vulva as well as the vagina is common and occurs in about 15% of pregnant women, causing itching, burning, and discharge. During pregnancy, treatment with miconazole or clotrimoxazole cream or vaginal pessaries is preferred and may need to be repeated several times or preventative treatment may be necessary. Oral antiyeast treatments must not be used for vulvo-vaginal yeast infection during pregnancy. Dermatophyte infections (tinea/ringworm) are common and may affect pregnant women. In uncomplicated cases tinea is usually treated with topical antifungals; in pregnancy, clotrimazole and miconazole are preferred. Oral antifungals must be avoided in pregnancy and treatment for onychomycosis postponed until after delivery. Cutaneous and genital warts thrive in pregnancy, often commencing, proliferating, or enlarging. However, in the last eight weeks of pregnancy methods that destroy the warts and harm the skin over large areas should be avoided so there is no damage to the skin before delivery. The choice of the therapy is dependent on the type, the extent, and the location of the warts. Imiquimod has been used in pregnancy without observed adverse effects, but it is not licensed for use in pregnancy. The baby can catch the virus by transmission from the mother via the placenta or during delivery. If the baby is infected before delivery it is at risk of abnormalities, mainly of the brain and the eyes, but herpes virus transmission predominantly occurs during delivery and not during pregnancy. If the baby is infected by the virus during delivery or as a newborn the infection may be restricted to the skin, mucosa, and/or the eyes (45%), the infection may involve the brain (30%), or the infection may be wide spread involving many organs including lungs, liver, and the brain (25%).
Buy lopressor now
Perforation during diagnostic endoscopy occurs in approximately 1:10 000 blood pressure normal child buy lopressor with visa, and may relate to anterior osteophytes in the region of the cricopharyngeus, a malignant stricture, or an unrecognized pharyngeal or oesophageal pouch (a particularly hazard using the sideviewing duodenoscope). Interventional upper gastrointestinal endoscopy the overall risk of oesophageal perforation following balloon or bougie dilatation of benign strictures is less than 2%, 2 to 5% for achalasia balloon dilatation, and up to 10% for malignant strictures. Management is by putting the patient nil by mouth, giving parenteral antibiotics, and intravenous feeding. There remains, however, a substantial role for radiological imaging in the investigation of the small and large bowel in the diagnosis of abdominal and gastrointestinal disease. Nuclear medicine studies have a role in the examination of the small bowel for the presence of inflammatory conditions, and for demonstration of potential bleeding sources. Colonoscopy has revolutionized imaging approaches to the colon because of its proven diagnostic efficacy and the added facility for biopsy of diffuse mucosal pathology and focal mucosal lesions, but is associated with a small risk of perforation. Furthermore, there have been many technological advances in these imaging techniques in recent years including the development of enteric contrast agents that distend the bowel, multiplanar and three-dimensional imaging, and advanced imaging applications such as motility imaging, and radiation dose reduction techniques. An exception to the trend in the declining use of barium studies is the barium swallow. Eosinophilic gastroenteritis Eosinophilic gastroenteritis is a rare condition with over 50% of cases occurring in patients with atopy. The disease most commonly affects the small bowel and stomach with imaging findings of fold thickening, polyps, mucosal ulcers, stricture formation, ascites, omental thickening, and lymphadenopathy. Vascular diseases of the small bowel Small-bowel ischaemia Small-bowel ischaemia may result from arterial occlusion, venous occlusion, or low-flow states such as cardiac failure or hypovolaemia, with superior mesenteric artery occlusion accounting for over 50% of cases. The imaging manifestations vary according to the degree of vascular insufficiency. Occlusive arterial disease may result in acute transmural infarction with absence of enhancement, mural thinning, and bowel dilatation. Conversely, nonocclusive disease may result in mural thickening and mucosal hyperenhancement related to reactive hyperaemia due to reperfusion injury. Venous occlusion, the least common cause of small-bowel ischaemia, presents with marked mural thickening with hyperenhancement and associated vascular engorgement and mesenteric stranding. This should be suspected in young patients with recurrent symptoms, disease involving atypical sites such as the duodenum, and when additional findings such as aneurysms and solid visceral infarcts are present. Small-bowel bleeding Angiodysplasia is the most common cause of occult gastrointestinal tract bleeding. Furthermore, it may guide interventional management by identifying the bleeding vessel facilitating selective catheterization and embolization. Capsule endoscopy may also be complementary in patients with suspected small-bowel bleeding but is limited by long reporting times. Immune-mediated enteritis Coeliac disease Coeliac disease is a gluten-related, immune-mediated enteropathy occurring in susceptible individuals. The most common imaging finding is moderately dilated fluid-filled loops of small bowel. The classic finding of jejunal fold atrophy with secondary hypertrophy of the ileal folds (jejunoileal fold reversal) is uncommonly encountered. Other imaging features include transient small-bowel intussusceptions and splenic atrophy. The primary role of imaging is the detection of enteropathy-associated T-cell lymphoma, especially in patients with refractory disease. Findings vary from multiple enhancing mural nodules to aneurysmal luminal dilatation due to destruction of the muscle wall and myenteric plexus. Patients with coeliac disease are also at an increased risk of developing small-bowel adenocarcinoma. Another entity that has been described in coeliac disease is cavitating mesenteric lymph node syndrome. This consists of enlarged, rim-enhancing, necrotic mesenteric lymph nodes in association with an ulcerative jejunoileitis, predominantly affecting the jejunum. Bowel preparation with dietary restriction and laxatives is recommended in a similar fashion to colonoscopy. A rectal tube is inserted and room air or carbon dioxide is insufflated into the colon under controlled injection until satisfactory colonic distension is achieved. Patients are then scanned in the prone and supine positions with additional imaging being performed as required to ensure complete colonic imaging. Disadvantages of the technique include the prerequisite exposure to ionizing radiation and in the event of a lesion being found, the patient may need a second bowel preparation to undergo colonoscopy to perform biopsy or further treatment. This is then drained and air is administered followed by double-contrast spot films of each colonic segment. Before acquiring a spot image, barium is allowed to pass over the mucosal surface, the patient is turned to displace the barium pool, and air is insufflated. The volume of barium retained by the patient is important as excessive barium will obscure colonic lesions and a paucity of barium will result in poor mucosal coating. Incomplete filling of the right colon may also occur, resulting in the inability to exclude disease of the proximal colon. The technique may be poorly tolerated by some patients due to abdominal cramps despite the use of an antispasmodic agent and/or lax anal sphincter. Glucagon 1 mg or Buscopan 20 mg intravenously may be used to induce colonic hypotonia. The technique combines an aqueous enema with the intravenous administration of a gadolinium-based contrast agent. This discriminates colonic pathology, which appears bright on T1-weighted images post contrast, from the bowel lumen, which is rendered totally dark by the aqueous solution. Residual stool and air bubbles, which may mimic bowel pathology, also remain dark. Approximately 2500 ml of warm tap water is instilled into the colon via a rectal enema tube following which scanning is performed in the prone position to reduce breathing artefacts. Multiplanar reformations are generated from pre- and post-contrast three-dimensional data sets and virtual endoscopic fly-through may be performed on a postprocessing workstation. Both antegrade and retrograde visual fly-through is performed to ensure visualization of both sides of the haustral folds. If the lesion causes a stricture, patients may present with large-bowel obstruction. Extracolonic spread is detected by loss of the fat planes between the colon and surrounding tissue. Tumours may invade the mesentery, abdominal wall, retroperitoneum, or adjacent organs such as the stomach and liver. There are imaging features specific to each disease that may help to distinguish them. In addition, a lowattenuation ring of submucosal fat (halo sign) is more commonly seen in ulcerative colitis. The differential diagnosis for inflammatory bowel disease of the colon includes pseudomembranous colitis, ischaemic colitis, infectious colitis, and radiation colitis. Ischaemic colitis the causes of colonic ischaemia are the same as small-bowel ischaemia. However, there are certain watershed areas that are particularly susceptible to ischaemia from hypovolaemia including the splenic flexure (watershed between the superior and inferior mesenteric arteries) and rectosigmoid (watershed between the inferior mesenteric artery and superior rectal artery). These are regions of poor perfusion at the peripheries of major arterial territories with a poor collateral supply. Ischaemic colitis typically involves the left colon in the elderly patient with hypoperfusion and the right colon in young patients with haemorrhagic shock. Pneumatosis coli is not specific to bowel ischaemia and may be seen in a wide range of nonischaemic conditions such as infection, inflammation, malignancy, respiratory disease, and also following. Thrombus may be identified within the splanchnic vessels in cases of occlusive arterial disease.
Purchase lopressor cheap online
If pregnancy is decided upon prehypertension prevention discount 25 mg lopressor with mastercard, intensive specialist cardiac and obstetric monitoring needed throughout pregnancy, childbirth, and the puerperium Extremely high risk of maternal mortality or severe morbidity; pregnancy contraindicated. Many cardiac drugs are relatively or absolutely contraindicated in pregnancy (see Chapter 14. In general warfarin should be changed to subcutaneous low-molecular-weight heparin (with anti-Xa level monitoring) for the duration of pregnancy, except in the case of mechanical valve replacements discussed later in this chapter. Awaiting spontaneous onset of labour is the norm, with induction indicated for the standard obstetric reasons, maternal cardiac decompensation, or for practical reasons, for example when the mother lives far from the intended site of delivery. Current National Institute for Health and Care Excellence guidelines do not recommend antibiotic prophylaxis for delivery. Invasive blood pressure monitoring is advisable in women with obstructive lesions Observation and monitoring on a high-dependency unit may be required for up to one week post-partum. The left ventricle may not be dilated but the ejection fraction is nearly always reduced below 45%. Risk factors include multiple pregnancy, multiparity, hypertension, increased maternal age, and black ethnicity. The cause of peripartum cardiomyopathy is not known but may involve angiogenic imbalance in the heart due to systemic antiangiogenic signals in late pregnancy combined with inadequate local cardiac proangiogenic defences. It may be that activation of cathepsin D by oxidative stress is involved, leading to proteolytic cleavage of prolactin into a potent antiangiogenic, pro-apoptotic, and pro-inflammatory 16 kDa subfragment. Clinical features are those of left ventricular failure; the diagnosis should be suspected in any peripartum woman with dyspnoea, orthopnoea, paroxysmal nocturnal dyspnoea, or tachycardia. The differential diagnosis in includes pre-existing cardiomyopathy, valve disease or congenital heart disease, pregnancy associated myocardial infarction, pulmonary embolism/amniotic fluid embolism, and myocarditis. There is a high risk of thromboembolism, necessitating the addition of a prophylactic or, in high-risk cases, treatment dose of lowmolecular-weight heparin. There is some evidence to support the use of bromocriptine, an inhibitor of prolactin secretion. Patients with haemodynamic instability despite treatment should undergo urgent delivery. Up to 60% of patients recover normal resting left ventricular function, which is crucial to the outcome of a future pregnancy 14. During labour cardiac filling pressures should be maintained by fluid infusion, especially in the event of post-partum haemorrhage, and any epidural analgesia/anaesthesia should be low dose and slowly titrated to avoid vasodilatation and hypotension. Ischaemic heart disease In the 10 years from 1994, a small decrease in the female prevalence of hypertension and smoking, combined with an increase in diabetes and obesity, resulted in an unchanged prevalence of cardiovascular disease in women. However, the proportion of live births occurring to women in their thirties or older has more than doubled over the last 30 years, such that the prevalence of coronary atheroma in pregnant women is increasing. Known ischaemic heart disease pre-pregnancy is rare and should be assessed as if risk-stratifying for noncardiac surgery. Previous percutaneous coronary intervention or coronary artery bypass grafting is no bar to pregnancy if functional status is good and ventricular function normal. Angina presenting in pregnancy should be managed with standard medical therapy, other than a statin as these are teratogenic. Drug eluting stents should be avoided as their safety is unknown in pregnancy and their use would require prolonged dual antiplatelet therapy. Risk factors include thrombophilia, infection, twin pregnancy, pre-eclampsia, and transfusion in addition to standard coronary risk factors. In 29% of cases, angiography is entirely normal and coronary spasm the presumed diagnosis; this has been reported following administration of the vasoconstrictor ergometrine to prevent post-partum haemorrhage (transfusion, listed here as a risk factor, may be a surrogate marker for this). Immediate angiography is the management of choice as it allows percutaneous intervention and appropriate targeting of secondary coronary prevention. Thrombolysis is not contraindicated, but best avoided two weeks peripartum because of the risk of postpartum haemorrhage. Aspirin is safe, but there is only case report evidence about other antiplatelet drugs. We counsel against subsequent pregnancy in women whose left ventricular function has not recovered and offer termination of unplanned pregnancy. This, however, will not predict cases of recurrence of the original pathological process and hence a further pregnancy will always involve a degree of risk. Women may present with a pre-existing diagnosis or de novo in pregnancy when the haemodynamic load unmasks limited cardiac reserve. Management is largely as discussed for peripartum cardiomyopathy, with the important addition of consideration of termination of pregnancy for women with worsening symptoms or ventricular function prior to fetal viability. Hypertrophic cardiomyopathy Women with hypertrophic cardiomyopathy generally tolerate pregnancy well, with outcome predicted by pre-pregnancy functional status. An asymptomatic woman has a better than 90% chance of remaining so throughout her pregnancy. Pre-pregnancy assessment should include exercise testing, echocardiography, and standard assessment of sudden cardiac death risk. Women with a high outflow tract gradient are at increased risk and those with severe systolic or diastolic dysfunction should be advised against pregnancy. Women with moderate diastolic dysfunction may require Aortopathy Dilated aortic root Aortic root dilatation secondary to cystic medial necrosis occurs in association with Marfan syndrome and related disorders, Turner syndrome, familial thoracic aneurysm, bicuspid aortic valve, and repaired tetralogy of Fallot, but has also been reported in healthy pregnant women. Together with hypertension, atherosclerosis, and infection it confers a risk of type A dissection, most commonly in the third trimester or peripartum-the time of greatest haemodynamic shear stress to the aortic wall. Most of the literature concerns Marfan syndrome, with an overall pregnancy mortality of 1%. Although the number of reported cases is small, the risk in Marfan syndrome appears to increase significantly if the aortic root diameter is greater than 4. The risk of dissection is lower in other conditions, such as bicuspid aortic valve and tetralogy of Fallot, and a pre-pregnancy threshold of 5 cm is used for prophylactic surgery. It is recommended that, regardless of root diameter, all higher risk women are fully blocked throughout pregnancy. If despite these measures the root dilates rapidly or dissects, the management of choice is caesarean delivery of a viable fetus followed by root replacement. If the fetus is nonviable, surgery should proceed, accepting the risk of fetal loss. Low-risk cases should have a normal delivery with consideration of an assisted second stage, but caesarean section should be considered when maximum aortic dimension exceeds 4. Other obstetric complications of Marfan syndrome include recurrent miscarriage, preterm rupture of membranes, and post-partum haemorrhage. Two recent series reported a single death, by type A dissection, in 104 women (20 unrepaired) undergoing 244 pregnancies. The incidence of hypertension is fourfold higher than in the general pregnant population, particularly in those women with a residual or native gradient higher than 20 mm Hg. In the presence of a significant gradient the concerns are dual: maternal hypertension, with risk of aortic dissection and stroke, and hypotension of the fetoplacental unit. Blood pressure should therefore be measured in the right arm and either leg, using -blockers as the first line antihypertensive agent to achieve systolic pressures of less than 140 mm Hg in the arm and more than 70 mm Hg in the leg. Delivery should usually be vaginal, with consideration of assisted second stage in the presence of a significant gradient or hypertension, unless an aneurysm is present. Angioplasty and stenting of coarctation during pregnancy and the puerperium is not recommended because of the increased predisposition to dissection during this period, although there are no series from which to estimate risk. Women who elect to continue should be monitored closely in a specialist centre and advised strongly to reconsider termination should they deteriorate in the first or second trimester. Suggested treatments include bed rest, oxygen, anticoagulation, and targeted pulmonary vascular therapies such as sildenafil, nitric oxide, and prostacyclin analogues, but the evidence is scant. One small series reported an improved maternal mortality with a regimen of oxygen, heparin before delivery, and warfarin after 48 h; 60% of infants were liveborn, with most premature. Early reports of the use of nebulized iloprost, intravenous prostacyclin, and oral sildenafil are optimistic, but numbers are small, and deaths still occur.