Purchase quibron-t no prescription
Talcum powder has been associated with asbestos contamination allergy testing vancouver bc purchase quibron-t on line, and its use on the perineum has been studied for a potential link to ovarian cancer, with conflicting results. Clinical Presentation Ovarian cancer is often called the cancer that "whispers" because symptoms are subtle and nonspecific. Bloating, abdominal pain, gastrointestinal disturbance, and bladder symptoms may present once diffuse carcinomatosis develops with nodules of cancer and ascites throughout the abdomen and pelvis. Common sites of metastasis include the omentum, peritoneal surfaces, lymph nodes in the pelvis and abdomen, and pleural effusions. Advanced ovarian cancer is suspected on imaging with the presence of an adnexal mass accompanied by ascites, peritoneal carcinomatosis or enlarged pelvic and para-aortic lymph nodes. Patients with an enlarged complex ovarian mass and no evidence of metastatic disease should have surgery for resection of the mass with effort made to avoid disrupting the integrity of the neoplasm, because rupture may spread cancer if present. If widespread disease is seen on imaging, a clinician may recommend an image-guided biopsy of solid tumor, drainage of ascites or surgical resection to obtain tumor for tissue diagnosis. Ovarian cancer stage is assigned by review of clinical, pathologic, and radiologic evaluation. Pathology Ovarian carcinoma refers to a family of tumors arising from the epithelial lining of the ovary, fallopian tube, and peritoneum. Borderline ovarian neoplasms are an unusual category of ovarian neoplasm with a favorable prognosis that can spread and recur but do not exhibit invasion of tissue. Nonepithelial ovarian cancers account for less than 5% of ovarian cancers and originate from sex-cord cells, stromal cells, and germ cells of the ovary. These rare tumors often occur in adolescent Treatment the treatment for presumed early stage ovarian carcinoma is surgical resection and staging to evaluate for metastatic disease. High-grade cancers isolated to the ovary, or cancer with any sign of spread beyond the ovary, is treated with adjuvant chemotherapy. The standard of care calls for the administration of intravenous carboplatin and paclitaxel every 3 weeks. We continue to recommend six cycles for women with early stage ovarian cancer, though have a lower threshold to discontinue treatment after three cycles for women with nonserous cancers, if they opt to stop or if side effects intervene. Debulking is favored when imaging suggests all visible tumor may be resected at the time of surgery. In either case, adjuvant therapy is indicated, and we suggest patients receive up to three cycles following surgery to complete at least six cycles total of chemotherapy. Recurrent ovarian cancer can be treated with additional chemotherapy and surgery can be considered if there are resectable sites of limited disease. If the recurrence occurs more than 6 months after completing primary platinum-based treatment, the tumor is considered "platinum sensitive" and retreatment with a platinum combination is preferred. When recurrence occurs in less than 6 months, the cancer is considered "platinum resistant," and an alternative agent is chosen. Patients with recurrent ovarian cancer do not have curable disease; therefore, clinical trials should be offered whenever possible. Unfortunately, patients with advanced stage disease usually recur and develop treatment resistance. Bowel obstruction from massive carcinomatosis is a common terminal event for women with ovarian cancer. Worldwide, it is the sixth most common malignancy affecting women, and it ranks as the fourteenth cause of cancer death. Increased circulating estrogen without progesterone to balance stimulation of the endometrial lining is associated with endometrial cancer development. Obesity is a strong risk factor due to high levels of circulating estrogen via conversion of androgens to estrogen by aromatase within adipose cells. Other increased estrogen-related risk factors include anovulatory menstrual cycles, nulliparity, early menarche, late menopause, estrogen producing ovarian neoplasms (benign thecomas and malignant dysgerminomas), and estrogen replacement without the use of protective progesterone. Breast cancer treatment with tamoxifen blocks estrogen action in the breast but has pro-estrogen effects on the endometrium resulting in a 2- to 5-fold increased risk of endometrial cancer after 5 years of use. Women with hereditary Lynch syndrome (see section on epidemiology of ovarian cancer) have a 60% lifetime risk of developing endometrial cancer and require screening with annual endometrial biopsy, and when childbearing is complete, a hysterectomy with bilateral salpingo-oophorectomy is recommended. Diabetes and hypertension are associated with increased risk of endometrial cancer. These low-grade endometrioid type cancers are usually limited to the uterus and have a good prognosis. Type 2 endometrial cancer is the more aggressive form of cancer, more likely to metastasize, and carries a worse prognosis. Type 2 histologies include high-grade endometrioid, serous, clear cell, and carcinosarcoma. Mesenchymal cancers of the uterus are rare and include cancers, such as sarcoma, arising from the myometrial wall of the uterus and cancers arising from the endometrial stromal cells. Radical hysterectomy extends the surgical margin with removal of surrounding parametrial tissue and upper vagina. Clinical Presentation Studies show that 70% to 90% of women with endometrial cancer present with postmenopausal bleeding. In premenopausal women, irregular or heavy vaginal bleeding is the most common symptom. An abnormal Papanicolaou (Pap) smear, or abnormal imaging of the uterus, may also lead to a diagnosis of endometrial cancer. Diagnosis and Staging Postmenopausal women with any uterine bleeding, even spotting, should be evaluated for endometrial cancer. The work-up includes a full gynecologic exam with endometrial sampling and imaging to evaluate the appearance of the endometrium (normal endometrial thickness measures 4 mm after menopause). Endometrial biopsy may be performed as an office procedure and has a high sensitivity when the endometrial lining measures 11 mm or less. A thicker lining may require further evaluation with a dilatation and curettage of the uterus to definitively rule out malignancy. Premenopausal women with persistent bleeding between menses should also be evaluated with endometrial sampling and radiographic imaging, especially those presenting with known risk factors for endometrial cancer. If the uterus is small, this procedure may be performed with a laparoscopic or robot-assisted laparoscopic technique. Laparotomy may be indicated for a large uterus that cannot be extracted vaginally. Sentinel nodal evaluation has largely replaced complete pelvic and para-aortic lymphadenectomy. This procedure involves injecting the cervix with dye and removing lymph nodes that collect the dye. The advantages of sentinel node dissection include a limited, more targeted surgery, with less risk of surgical complications including lower extremity lymphedema. Early stage endometrial cancer with low grade histology that invades less than 50% of the myometrium has an excellent prognosis for cure with surgery alone. The protocols for administering adjuvant therapy for endometrial cancer after surgical staging are complex. Recommendations may include vaginal cuff brachytherapy, pelvic radiation, and/or chemotherapy. Stage 1 tumors that invade more than 50% of the myometrium are typically treated with vaginal radiation to prevent local recurrence of cancer. Tumors with cervical stromal involvement are treated with additional whole pelvic radiation. If lymph node metastases or other disease beyond the uterus is identified, then chemotherapy with intravenous carboplatin and paclitaxel with or without radiation is typically recommended. Some patients with high grade cancer such as the serous subtype may also benefit from chemotherapy even if cancer is isolated to the uterus. Distant recurrences often require platinum-based chemotherapy; however, a low-grade metastatic endometrial cancer may respond to antiestrogen hormonal therapy alone. For those who progress on first-line chemotherapy, clinical trials should be pursued. A subset of women with early endometrial cancer may opt to forego standard hysterectomy.
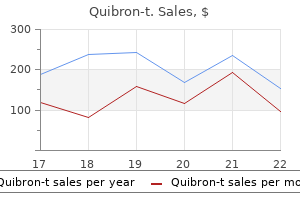
Buy cheap quibron-t 400 mg on line
For both men and women allergy testing guidelines cheap quibron-t 400 mg fast delivery, fertility treatment requires the use of gonadotropin therapy. Nonfunctioning pituitary adenomas are the second most common pituitary adenoma after prolactinomas. Gonadotropin-secreting pituitary tumors typically manifest with signs and symptoms of mass effect. Immunoperoxidase staining on tumor tissue is also needed to establish the diagnosis, especially as seen in postmenopausal women when gonadotropins are appropriately elevated. Primary treatment is transsphenoidal surgical removal, which is generally successful. Patients with primary polydipsia concentrate their urine without the need for synthetic vasopressin. It can also be acquired secondary to intrasellar and suprasellar tumors, infiltration of the hypothalamus and posteTreatment rior pituitary, infection, trauma or surgery, or as part of an autoimmune condition. Swearingen B, Biller B: Diagnosis and management of pituitary disorders, New York, 2008, Humana Press. Microscopically, the thyroid is composed of several follicles that contain colloid surrounded by a single layer of thyroid epithelium. Biosynthesis of T4 and T3 occurs by iodination of tyrosine molecules in thyroglobulin. Physiologic Effects of Thyroid Hormones Thyroid hormones increase the basal metabolic rate by increasing oxygen consumption and heat production in several body tissues. These effects are exaggerated in hyperthyroidism and reduced in hypothyroidism, accounting for the well-recognized signs and symptoms of these two disorders. Iodine, after conversion to iodide in the stomach, is rapidly absorbed from the gastrointestinal tract. After active transport from the bloodstream across the follicular cell basement membrane, iodide is enzymatically oxidized by thyroid peroxidase, which also mediates the iodination of the tyrosine residues in thyroglobulin, to form monoiodotyrosine and diiodotyrosine. The iodotyrosine molecules couple to form T4 (3,5,3,5-tetraiodothyronine) or T3 (3,5,3-triiodothyronine). Once iodinated, thyroglobulin containing newly formed T4 and T3 is stored in the follicles. Tests of Serum Thyroid Hormone Levels Measurements of total serum T4 and total T3 indicate the total amount of hormone bound to thyroid-binding proteins by radioimmunoassay. The unbound or free fractions are the biologically active fractions; they represent only 0. Most of the circulating T3 is derived from deiodination of circulating T4 in the peripheral tissues. Deiodination of T4 can occur at the outer ring (5-deiodination), producing T3 (3,5,3-triiodothyronine), or at the inner ring (5-deiodination), producing reverse T3 (3,3,5-triiodothyronine). The use of thyroid ultrasounds in patients with thyroid nodules is discussed later. Similarly, total T4 and T3 are low despite euthyroidism in conditions associated with low levels of thyroid-binding proteins. Therefore, further tests to assess the free hormone levels, which reflect biologic activity, must be performed. Free T4 and free T3 levels can be measured directly or by dialysis or ultrafiltration and have, at most institutions, replaced measuring total T4 and T3 levels. In hyperthyroidism, the free T3 may be elevated in the presence of a normal free T4. Serum thyroglobulin measurements are useful in the follow-up of patients with papillary or follicular carcinoma. After thyroidectomy and iodine-131 (131I) ablation therapy, thyroglobulin levels should be less than 0. Levels in excess of this value indicate the possibility of persistent or metastatic disease. Calcitonin is produced by the C cells of the thyroid and has a minor role in calcium homeostasis. Calcitonin measurements are invaluable in the diagnosis of medullary carcinoma of the thyroid and for monitoring the effects of therapy for this entity. Clinical manifestations of thyrotoxicosis result from the direct physiologic effects of the thyroid hormones as well as the increased sensitivity to catecholamines. Tachycardia, tremor, stare, sweating, and lid lag are all caused by catecholamine hypersensitivity. Thyroid Imaging Technetium-99m (99mTc) pertechnetate is concentrated in the thyroid gland and can be scanned with a gamma camera, yielding information about the size and shape of the gland and the location of the functional activity in the gland (thyroid scan). The thyroid scan is often performed in conjunction with a quantitative assessment of radioactive iodine (123I) uptake by the thyroid. Functioning thyroid nodules are called warm or hot nodules; cold nodules are nonfunctioning. Thyrotoxic crisis, or thyroid storm, is a life-threatening complication of hyperthyroidism that can be precipitated by surgery, radioactive iodine therapy, or severe stress. Patients develop fever, flushing, sweating, significant tachycardia, atrial fibrillation, and cardiac failure. Hyperpyrexia out of proportion to other clinical findings is the hallmark of thyroid storm. However, it may be the result of excessive ingestion of thyroid hormone or, rarely, thyroid hormone production from an ectopic site (as in struma ovarii). One or more of the following features are present: (1) goiter; (2) thyrotoxicosis; (3) eye disease ranging from tearing to proptosis, extraocular muscle paralysis, and loss of sight as a result of optic nerve involvement; and (4) thyroid dermopathy, usually observed as significant skin thickening without pitting in a pretibial distribution (pretibial myxedema). These thyroid-stimulating immunoglobulins increase thyroid cell growth and thyroid hormone secretion. Ophthalmopathy results from inflammatory infiltration of the extraocular eye muscles by lymphocytes with mucopolysaccharide deposition. Older patients often do not have the florid clinical features of thyrotoxicosis, and the condition termed apathetic hyperthyroidism is exhibited as flat affect, emotional lability, weight loss, muscle weakness, congestive heart failure, and atrial fibrillation resistant to standard therapy. Magnetic resonance imaging or ultrasonography of the orbit usually shows orbital muscle enlargement, whether or not clinical signs of ophthalmopathy are observed. In Europe, Latin America, and Japan, antithyroid drugs are the favored therapy while in the United States, radioactive iodine is the main therapy. Conjunctival chemosis (edema) and erythema with bilateral edema of the caruncles and prolapse of the right caruncle are evident. She also had evidence, on slit lamp examination, of moderate superior limbic keratoconjunctivitis. Medical therapy is usually administered for a prolonged period (1 to 3 years), with the dose gradually reduced until spontaneous remission occurs. Many patients can remain on low doses of thiocarbamide drugs for long periods of time without significant side effects. One approach is to gradually decrease the dose while maintaining T4 and T3 in the normal range, leaving patients on low doses of thiocarbamide drugs if T4 and T3 remain high after a gradual taper. Those who experience relapse can either resume therapy with thiocarbamide drugs or undergo definitive surgery or radioactive iodine treatment. Side effects of the thiocarbamide regimen include pruritus and rash (in about 5% of patients), elevated liver function enzymes, cholestatic jaundice, acute arthralgias, and, rarely, agranulocytosis (<0. Methimazole was found to be more effective at normalizing thyroid hormone levels and led to a lower rate of transaminase elevation and leukopenia than propylthiouracil; it has now become the preferred medical treatment for hyperthyroidism. At the onset of treatment during the acute phase of thyrotoxicosis, -adrenergic receptor blockers can be used to help alleviate tachycardia, hypertension, and atrial fibrillation in symptomatic patients. As the thyroid hormone levels return to normal, the treatment with -blockers is tapered off. However, 80% to 90% of patients become hypothyroid after radiotherapy and require lifelong thyroid hormone replacement. Patients with severe thyrotoxicosis, very large glands, or underlying heart disease should be rendered euthyroid with antithyroid medication before receiving radioactive iodine, because 131I treatment can cause a release of preformed thyroid hormone from the thyroid gland that could precipitate cardiac arrhythmias and exacerbate symptoms of thyrotoxicosis.
Diseases
- Hutchinson incisors
- Rapadilino syndrome
- Atypical lipodystrophy
- Cataract skeletal anomalies
- Pulmonar arterioveinous aneurysm
- Asphyxia neonatorum
- Hereditary type 1 neuropathy
- Hypocalcemia
- Occupational asthma - chemicals and materials
Purchase generic quibron-t
However allergy united discount quibron-t online, emerging data suggest that standard iron dosing may be counterproductive. A recent study Macrocytic Anemias Two categories of hypoproductive macrocytic anemias exist: megaloblastic anemias and nonmegaloblastic macrocytic anemias. Nonmegaloblastic macrocytic anemias usually reflect membrane abnormalities resulting from defects in cholesterol metabolism and are most commonly found in patients with advanced liver disease or severe hypothyroidism. Cells take on a bizarre appearance, with large immature nuclei surrounded by more mature-appearing cytoplasm. In women, megaloblastic changes of the cervical mucosa occur and may cause abnormal results on Papanicolaou smears. The process of cobalamin absorption and metabolism is complex because cobalamin is always bound to other proteins. In the stomach, protein-bound vitamins are released by digestion with pepsin and are bound to haptocorrin (transcobalamin I). The cytoplasmic enzyme homocysteine-methionine methyltransferase is necessary for the transfer of methyl groups from N-methyltetrahydrofolate to homocysteine to form methionine. Demethylated tetrahydrofolate is necessary as a carbon donor in the conversion of deoxyuridine to deoxythymidine. The megaloblastic changes induced by cobalamin deficiency are mediated through this functional folate deficiency, which explains the similarity in the hematologic abnormalities induced by cobalamin and folate deficiency. Many other lesions in the gastrointestinal tract can interfere with absorption of cobalamin (Table 48. Because the body stores of cobalamin are large and daily loss of cobalamin is low, the stores of cobalamin are adequate for 3 to 4 years if intake stops abruptly; signs of cobalamin deficiency do not develop until defective absorption has occurred for several years. Nutritional cobalamin deficiency is rare and is seen only in individuals who have been on strict vegan diets that exclude all animal products for many years. Infants born to vegan mothers who are breastfed are also at risk for development of cobalamin deficiency. Folate is widely present in foods such as leafy vegetables, fruits, and animal protein. However, because it is destroyed by prolonged cooking, fresh fruits and vegetables are the most reliable sources of folate. Consequently, nutritional folate deficiency is common in malnourished individuals who eat very little fresh fruits and vegetables. Folate deficiency can also be caused by increased demand, as occurs with pregnancy, hemolysis, or exfoliative dermatitis, and by increased losses, which occur with dialysis (Table 48. Folate is absorbed in the proximal small intestine, and malabsorption of folate can also lead to folate deficiency. Some drugs, such as methotrexate and sulfa drugs, act as direct folate antagonists and mimic folate deficiency. Alcohol interferes with folate metabolism, increasing the effect of frequent concomitant nutritional folate deficiency. Myelodysplastic syndrome commonly appears as a macrocytic anemia, with megaloblastic changes primarily in the erythroid series. The development of megaloblastic anemia is usually gradual, allowing adequate time for concomitant plasma expansion to prevent hypovolemia. They may have yellowish skin as the result of a combination of pallor from reduced red cell mass and jaundice from ineffective erythropoiesis and intramedullary hemolysis. Anemia and other cytopenias should respond completely within 1 to 2 months, but the neurologic manifestations of cobalamin deficiency improve slowly and may be irreversible. A peripheral blood smear demonstrates large, oval cells (macro-ovalocytes), hypersegmented neutrophils, and large platelets. The bone marrow is hypercellular, with megaloblastic changes and abnormally large erythroid series precursors. In addition, intramedullary destruction of erythrocytes (ineffective hematopoiesis) causes elevated concentrations of bilirubin (hence the jaundice described earlier) and lactate dehydrogenase. Cobalamin deficiency is associated with neurologic abnormalities that are not seen with other causes of megaloblastic anemia. The neurologic signs may range widely, from a subtle loss of vibratory sensation and position sense caused by demyelination of the dorsal columns to frank dementia and neuropsychiatric disease. The neurologic changes may be present without anemia, especially if a patient with cobalamin deficiency is treated with folate, which may correct the hematologic manifestations of megaloblastic anemia but does not treat the neurologic abnormalities. The neurologic manifestations of cobalamin deficiency are thought to be secondary to loss of function of the mitochondrial enzyme methylmalonyl-CoA mutase. One proposed explanation is that the failure to metabolize odd-chain fatty acids, which results in their improper incorporation into myelin, causes the neurologic dysfunction. This explains why these findings are uniquely seen in patients with cobalamin deficiency and are not seen in those with the megaloblastic anemias caused by abnormalities in the folate pathway. Serum levels of both cobalamin and folate should be measured in patients with megaloblastic anemia because megaloblastic changes in the gut mucosa can cause concomitant malabsorption of folate in the presence of cobalamin deficiency and vice versa. Recent studies have shown, however, that many patients with pernicious anemia may have normal serum cobalamin levels. Homocysteine levels are elevated in cobalamin and folate deficiency, and methylmalonic acid levels are elevated in cobalamin deficiency. These levels should be measured if cobalamin deficiency is suggested but serum cobalamin levels are in the normal range. For patients with cobalamin deficiency, both high-dose oral and parenteral cobalamin administration have been shown to be effective. Patients with neurologic abnormalities or medication noncompliance and those who have not responded to oral therapy should receive parenteral therapy with 1000 g subcutaneously or intramuscularly several times per week for four to eight doses. Patients with folate deficiency should receive replacement with 1 to 5 mg per day of oral folate. As previously stated, it is critical to be certain that patients are not cobalamin deficient: Replacement of folate may correct the hematologic parameters in patients with cobalamin deficiency, but it will not improve the neurologic sequelae. Reticulocytosis is seen as early as 2 days after therapy and peaks within 7 to 10 days. Despite rapid resolution of neutropenia, hypersegmentation of neutrophils may persist for several days. During this period, rapid cellular proliferation and turnover occur, which may precipitate hypokalemia, hyperuricemia, or hypophosphatemia. Patients Normocytic Anemias the differential diagnosis of a normocytic hypoproductive anemia is extensive. Most nutritional anemias that cause microcytosis or macrocytosis begin as a normocytic anemia. In patients for whom the diagnosis is not clear after routine nutritional and endocrine studies, a bone marrow examination is indicated to rule out primary pathologic conditions of the marrow. Anemia of Inflammation the anemia of inflammation (previously called anemia of chronic disease) occurs in patients with chronic inflammatory, infectious, malignant, or autoimmune disorders. Patients have low-serum iron levels, but in contrast to the iron indices in iron deficiency anemia, the iron-binding capacity is also reduced, and the transferrin saturation is usually greater than 10%. Ferritin levels are often elevated, both as an acute phase reactant and as a reflection of decreased iron incorporation. These patients have inappropriately high levels of hepcidin, an acute phase reactant that facilitates the metabolism of ferroportin and reduces both intestinal iron absorption and iron mobilization from macrophages. The mainstay of therapy for the anemia of chronic inflammation is treatment of the underlying condition and correction of nutritional deficiencies. Iron supplementation should be offered to all patients with a ferritin level lower than 100 ng/mL. However, randomized studies and meta-analyses have shown that their use is associated with an increased incidence of arterial and venous thromboembolic events, an increased risk of mortality from cancer, and a reduced survival time. Morphologic examination of the erythrocytes is helpful in distinguishing immune hemolysis from microangiopathic hemolytic anemia. Immune Hemolytic Anemia Immune-mediated hemolysis results from coating of the erythrocyte membrane with antibodies or complement, or both. It may be mediated by immunoglobulin G (IgG) antibodies (warm antibody) or by IgM antibodies (cold antibody). The designations warm and cold denote the temperature at which maximal antibody binding takes place and the clinical syndromes caused by the two types of antibodies are distinct. The diagnosis of hemolytic anemia is based on the direct and indirect antiglobulin (Coombs) tests. Warm type hemolysis may be primary (idiopathic) or associated with autoimmune disease, lymphoproliferative disorders, or drugs. Laboratory analysis confirms the presence of IgG on the erythrocyte membrane, as demonstrated by a positive Coombs test; in some patients, the erythrocytes are also coated with complement.
Generic quibron-t 400mg on line
Occasionally allergy testing joplin mo 400mg quibron-t sale, patients with Hashimoto thyroiditis have transient hyperthyroidism with low radioactive iodine uptake owing to the release of T4 and T3 into the circulation. Chronic thyroiditis can be differentiated from subacute thyroiditis in that in the former, the gland is nontender to palpation and antithyroid antibodies are present in high titer. Hypothyroidism and significant glandular enlargement (goiter) are indications for levothyroxine therapy. Recent evidence that symptoms of profound fatigue, poor sleep quality, and muscle joint pain persist despite levothyroxine supplementation leading to euthyroidism suggests that symptoms may be related to the autoimmune disease per se rather than hypothyroidism. Rare Causes of Thyrotoxicosis Struma ovarii occurs when an ovarian teratoma contains thyroid tissue that secretes thyroid hormone. A body scan confirms the diagnosis by demonstrating uptake of radioactive iodine in the pelvis. Early symptoms that are often overlooked include menstrual irregularities (usually menorrhagia), arthralgias, and myalgias. Anemia is usually normocytic and normochromic but may be macrocytic (with vitamin B12 deficiency resulting from associated pernicious anemia) or microcytic (caused by nutritional deficiencies or menstrual blood loss in women). Infants with congenital hypothyroidism (also called cretinism) may exhibit feeding problems, hypotonia, inactivity, an open posterior fontanelle, and edematous face and hands. Mental retardation, short stature, and delayed puberty occur if treatment is delayed. Patients often complain of fatigue, lethargy, and gradual weight gain for years before the diagnosis is established. A delayed relaxation phase of deep tendon reflexes (hung-up reflexes) is a valuable clinical sign that is characteristic of severe hypothyroidism. Subcutaneous infiltration by mucopolysaccharides, which bind water, causes the edema; this condition, termed myxedema, is responsible for the thickened features and puffy appearance of patients with severe hypothyroidism. Severe untreated hypothyroidism can result in myxedema coma, which is characterized by hypothermia, extreme weakness, stupor, hypoventilation, hypoglycemia, and hyponatremia and is often precipitated by cold exposure, infection, or psychoactive drugs. Administration of levothyroxine results in physiologic levels of bioavailable T3 and T4. Levothyroxine has a half-life of 8 days; consequently, it needs to be given only once a day. In some older patients and patients with cardiac disease, levothyroxine should be increased gradually, starting at 25 g/day and increasing the dose by 25 g every 2 weeks; however, most patients can safely be started on a full replacement dose. This reflects the inadequacy of peripheral deiodination to compensate for the absent T3 secretion. Because of these studies, there is renewed interest (accompanied by a large amount of controversy) in treating hypothyroid patients who have not had an adequate clinical response to levothyroxine replacement with a combination of levothyroxine and liothyronine (a manufactured form of T3) or with desiccated thyroid preparations that contain levothyroxine and liothyronine. Respiratory assistance and treatment of hypothermia with warming blankets may be required. Although myxedema coma carries a high mortality rate despite appropriate treatment, many patients improve in 1 to 3 days. Diagnosis Because the initial manifestations of hypothyroidism are subtle, early diagnosis demands a high index of suspicion in patients with one or more of the signs and symptoms (see Table 65. Thyroid enlargement (often focal) may also be the result of a thyroid adenoma or carcinoma. Iodine deficiency (endemic goiter) was once the most common cause of nontoxic goiter. Since the widespread availability of iodized salt, endemic goiter is less common in North America. Goitrogens are agents that can cause a goiter, and iodine and lithium are the two chemicals or drugs that frequently cause a goiter. Natural goitrogens include thioglucosides found in vegetables such as cabbage, broccoli, Brussels sprouts, turnips, cauliflower, kale, and other greens. Other foods that are goitrogens include soybeans and soybean products, peanuts, spinach, sweet potatoes, and some fruits. Thyroid hormone biosynthetic defects can cause goiter associated with hypothyroidism (or, with adequate compensation, euthyroidism). A careful thyroid examination coupled with thyroid hormone tests can reveal the cause of the goiter. A nodular thyroid gland with hypothyroidism and positive antithyroid antibodies is consistent with Hashimoto thyroiditis. A diffuse, smooth goiter with hypothyroidism and negative antithyroid antibodies may be indicative of iodine deficiency or a biosynthetic defect. Goiters can become very large, extending substernally and causing dysphagia, respiratory distress, or hoarseness. Previously, euthyroid goiters were treated with levothyroxine therapy; however, regression with levothyroxine therapy is unlikely and is no longer recommended. Surgery is indicated for nontoxic goiter only if obstructive symptoms develop or substantial substernal extension is present. The major etiologic factor for thyroid cancer is childhood or adolescent exposure to head and neck radiation. Previously, radiation was used to treat an enlarged thymus, tonsillar disease, hemangioma, or acne. Patients with a history of irradiation should have a baseline thyroid ultrasound study, then a repeat study every 5 years. All patients with a thyroid nodule noticed by the patient or during physical examination by a clinician should undergo a thyroid ultrasound. Patients who are found to have asymptomatic, incidental, nonsuspicious thyroid nodules on imaging performed for other reasons should be referred for diagnostic thyroid ultrasound only if they meet the following criteria: (1) younger than 35 years of age with normal life expectancy and nodule 1 cm or greater, or (2) 35 years of age or older with normal life expectancy and nodule 1. Although in the past benign thyroid nodules were treated with levothyroxine suppression, this is no longer recommended because it is uncommon for thyroid nodules to shrink substantially with levothyroxine. Indicators of poor prognosis include thyroid capsule invasion, size greater than 2. Follicular carcinoma is slightly more aggressive than papillary carcinoma and can spread by local invasion of lymph nodes or hematogenously to bone, brain, or lung. Anaplastic carcinoma tends to occur in older individuals, is very aggressive, and rapidly causes pain, dysphagia, and hoarseness. Medullary thyroid carcinoma is derived from calcitonin-producing parafollicular cells and is more malignant than papillary or follicular carcinoma. They can be detected clinically in about 4% of the population and are found in about 50% of the population at autopsy. Benign thyroid nodules are usually follicular adenomas, colloid nodules, benign cysts, or nodular thyroiditis. Patients may have one prominent nodule on clinical examination, but thyroid ultrasound evaluation may reveal multiple nodules. However, higher risk patients with larger tumors (>3 cm) and/or positive lymph nodes should have a total thyroidectomy. Routine central neck dissection is not needed unless lymph nodes are seen on preoperative imaging or if the surgeon discovers nodes during examination during surgery. They should have thyroglobulin measured and a thyroid ultrasound every 6 months for the first 2 years and then yearly. A thyroglobulin greater than 30 ng/mL and/or enlarging nodule on the contralateral lobe or lymph nodes draw concern for recurrent disease and should be evaluated for completion of the thyroidectomy. The most common malignancies of the Nodules with papillary carcinoma less thyroid are well-differentiated maligthan 1 cm may not need to be removed nancies with a favorable prognosis. Of and the option of serial ultrasounds (every these, the most common is papillary 6-12 months) should be discussed with thyroid carcinoma. If the patient feels more include medullary thyroid carcinoma, comfortable with surgery, that can also be poorly differentiated thyroid carcian option. The 5-year survival rate for invasive medullary carcinoma is 50%, whereas the mean survival time for anaplastic carcinoma is 6 months. For a deeper discussion on this topic, please see Chapter 213, "Thyroid," in Goldman-Cecil Medicine, 26th Edition. A rise in serum thyroglobulin levels suggests recurrence of thyroid cancer and should prompt testing for recurrence and/or metastases. Local or metastatic lesions that take up 131I on whole body scanning can be treated with radioactive iodine after the patient has stopped thyroid hormone replacement, whereas those that do not take up 131I can be treated with surgical excision or local radiograph therapy.

Discount quibron-t online master card
The "window period" from disease acquisition to test positivity has greatly reduced as compared with earlier generations of the test; fourth-generation testing is usually positive within 18 to 45 days allergy testing greenville nc buy quibron-t 400mg otc. Communication of a new diagnosis, and any subsequent discussion of treatment, prognosis, transmission, or other aspects of care, must be performed in a confidential setting. The symptoms may include fever, sore throat, gastrointestinal symptoms, diffuse lymph node enlargement, rash, arthralgias, and headache that usually persist for several days to 3 weeks (Table 103. The rash is typically maculopapular and short-lived and usually affects the trunk or face. Rarely, patients may present with opportunistic infections during this period, most commonly thrush (Candida pharyngitis). The acute retroviral syndrome is often sufficiently severe that the patient seeks medical attention, though it is uncommon to require hospitalization. Primary human immunodeficiency virus type 1 infection: review of pathogenesis and early treatment intervention in human and animal retrovirus infections. These functional impairments are manifested clinically by a 3-fold to 4-fold increase in the incidence of bacteremic pneumonias caused by common pulmonary pathogens (especially Streptococcus pneumoniae and Haemophilus influenzae) and by a marked increase in incidence of active pulmonary tuberculosis in endemic areas (Table 103. Both men and women may show similarly increased rates of dysplasia or neoplasia on anal Pap smear. They respond adequately to specific therapy only if it is accompanied by effective control of viral replication. Typically, but not exclusively, caused by Candida albicans, oropharyngeal candidiasis may manifest as painless, creamy white, plaque-like lesions on the buccal surface, classically on an erythematous base. Esophageal disease is often symptomatic, usually presenting with odynophagia and/or retrosternal burning pain. Treatment with oral fluconazole is as effective as or superior to localized topical therapy and is generally better tolerated and therefore preferred. Primary and secondary prophylaxis against Candida infection is generally not recommended unless patients have severe or frequent recurrences because therapy for acute disease is rapidly effective, mortality is extremely low, therapy is costly, and potential for development of resistance is of concern. The typical presentation is subacute, with progressive fever, shortness of breath, and weight loss over weeks. Profound desaturation with exertion is a common clinical sign, as is a substernal catch on inspiration. Radiographic findings are classically described as diffuse, bilateral, symmetrical "ground-glass" interstitial infiltrates emanating from the hila in a "butterfly" pattern. However, it is important to remember that 10% of patients will have a normal radiograph, and 30% will have nonspecific findings. Atypical findings such as nodules, blebs, or cysts, can occur, as can spontaneous pneumothorax. Early initiation of treatment is crucial, and treatment should not be delayed while waiting for diagnostic results in patients with a high index of suspicion. First-line therapy is trimethoprim-sulfamethoxazole 15 to 20 mg/kg/day in divided doses over a 21-day course. Alternative treatments for mild-to-moderate disease include primaquine with clindamycin, dapsone with trimethoprim, or atovaquone. Alternative treatments for moderate-to-severe disease include primaquine with clindamycin or intravenous pentamidine. Cryptococcal Disease Cryptococcus neoformans is a yeast that generally affects immunocompromised individuals. It enters the body through the lungs, though pulmonary disease is often asymptomatic. Meningitis is the most common clinical presentation of cryptococcal disease, but cutaneous manifestations, classically presenting as umbilicated papules, may be present in 10% of patients. Cryptococcal meningitis occurs in about 1 million cases per year worldwide, with an estimated 600,000 deaths annually. Classic meningeal symptoms occur in only 25% of patients; more commonly, patients present with progressive headache, lethargy progressive to encephalopathy, personality changes, memory loss, coma, and death. Therapy is generally divided into three phases: induction, consolidation, and maintenance. Maintenance therapy is with oral fluconazole 200 mg daily for a minimum of 1 year. Primary infection occurs from eating undercooked meat containing tissue cysts or ingesting oocysts that have been shed in cat feces and sporulated into the environment. Patients present with a focal encephalitis with headache, confusion, motor weakness, and fever. In the absence of treatment, disease will progress to seizures, stupor, coma, and death. Because disease is usually due to reactivation of latent disease, patients may have a positive serum anti-toxoplasma IgG. Treatment is initiated based on high clinical suspicion rather than definitive diagnosis. If repeat imaging in 1 to 3 weeks does not show response to treatment in all visualized lesions, brain biopsy may be necessary. Treatment consists of pyrimethamine and sulfadiazine with leucovorin to reduce hematologic toxicity. Laboratory testing is often initially nonspecific, though anemia and an increased alkaline phosphatase are common. Cultures can be sent from blood, lymph node biopsy, bone marrow, or other tissues or fluids felt to be infected. Treatment is with two or more drugs, usually clarithromycin or azithromycin with ethambutol. Initiation of antiretroviral therapy is the cornerstone of treatment; over 50% of patients will experience remission, though some neurologic deficits often persist. The greatest risk in people living in the United States is birth or residence outside the United States because global rates of tuberculosis are much higher than in the United States itself. Clinical manifestations can be protean, but classic symptoms of fever, cachexia, and night sweats remain common. Chest radiographs in patients may show features of primary tuberculosis, including hilar adenopathy, lower or middle lobe infiltrates, miliary pattern, or pleural effusions, as well as classic patterns of reactivation with upper lobe disease. This may be asymptomatic or present with floaters, scotomata, or visual field deficits. Ophthalmologic exam is generally diagnostic, with fluffy, yellow-white retinal lesions with or without intraretinal hemorrhage, and absent or minimal vitreous inflammation. Thirty percent will also have oral lesions and 40% will have gastrointestinal disease. Radiotherapy and intralesional chemotherapy may be used for skin disease, and chemotherapy, usually with liposomal doxorubicin, is used for widespread disease. Varicella-Zoster Disease Varicella-zoster is a ubiquitous virus known to have infected over 95% of adults in the United States. Herpes zoster, or reactivation varicella virus, manifests as a painful vesicular eruption on the skin in a dermatomal distribution; 50% are in thoracic dermatomes, but cranial nerves and cervical nerves are also common, and any nerve distribution can be involved. Intravenous acyclovir is recommended for treatment of severe or complicated varicella disease. Current recommendations regarding primary vaccination (in patients with no reported history of childhood illness or vaccination) and to prevent reactivation disease are addressed in Table 103. These infections include bacterial and parasitic intestinal infections (including Cryptosporidium, Cystoisospora, and Microsporidia spp). Systemic fungal infections, including endemic fungi such as Coccidioides, Histoplasma, and Talaromyces infections, occur regionally. Future efforts will need to focus on appropriate screening and treatment for this increasingly common and lethal malignancy, particularly as the population ages. Unfortunately, cancer-related mortality is predicted to increase along with increased rates. Steroid treatment is often prolonged, generally for 4 weeks or more, with gradual tapering as symptom management tolerates. Patients may have memory deficits, decreased executive function, and flattened affect, all of which may markedly affect quality of life. Some of the more frequent or treatable problems are discussed here and in the next section. Their sensorium is generally intact, and findings on neurologic examination are normal. Distressing pain, hyperesthesia, or hypesthesia, occurring most commonly in the lower extremities and worse at night, were previously common and were difficult to treat.
Discount 400mg quibron-t with mastercard
Lifelong recurring bleeding events and a family history of such suggest congenital disease whereas new bleeding despite previous "hemostatic stress tests" such as surgery or dental extraction without bleeding favor an acquired disorder or a medication effect allergy forecast pflugerville buy 400mg quibron-t fast delivery. Disorders of primary hemostasis including causes of thrombocytopenia or platelet dysfunction or diseases of von Willebrand factor lead to mucocutaneous superficial bleeding, but disorders of secondary hemostasis with missing coagulation factors cause deeper bleeding, for example muscle hematomas, hemarthroses, and intracranial hemorrhages. Superficial bleeding can be easy bruising, gum bleeding when brushing teeth, frequent epistaxis, and heavy menstrual bleeding. When uncovering family history, distinguishing between X-linked genetic disease. The X-linked inheritance pattern for hemophilia A and B means that more severe disease manifests in males than in females and subsequently may appear to skip generations. Hemarthroses result in joint swelling, tenderness, and moderate warmth, and multiple joint hemorrhages cause arthritis and deformity. Without imaging or laboratory tests, hemarthrosis can be indistinguishable from septic arthritis or other causes of joint pain. Platelet disorders classically result in petechiae, small subcutaneous hemorrhages that typically appear on the legs, a result of gravity dependence. For example, small ectatic vessels, prone to bleeding, can be seen on oral mucosa in hereditary hemorrhagic telangiectasia. Liver disease can cause bleeding through a decline in production of coagulation factors and a decline in platelet count, due to hypersplenism and decreased thrombopoietin production by the liver. Hallmark features of liver disease can be obvious on examination, such as jaundice and abdominal distension from ascites, but can be overlooked if not searched for. Dyskeratosis congenita, a disease of short telomeres, leads to leukoplakia, nail dystrophy, and hyperpigmented macules. Importantly, the timing of a thorough examination and subsequent laboratory testing must be tempered in order to control rapid bleeding and hemodynamic instability. Life-threatening hemorrhage requires immediate treatment while simultaneously pursuing diagnostic testing. Life-threatening blood loss is not limited to trauma or gastrointestinal sites but also includes small bleeds near the airway or neck and hemorrhages around other vital organs. Other helpful findings on a peripheral blood smear include schistocytes, suggesting microangiopathic hemolytic anemia. Teardrop cells with immature white and red blood cells characterize the myelophthisic blood smear, indicative of marrow replacement by solid tumor, lymphoma, granuloma, or fibrosis. A mixing study can distinguish a factor deficiency resulting from a decline in production from a decline due to inhibition from an autoantibody. Mixing studies combine patient plasma with control plasma so that missing factors are replaced and the abnormal clotting times correct. A positive mixing study does not correct because of the presence of an inhibitor, blocking the factor from the normal control plasma. Mixing studies can also be useful in finding a lupus anticoagulant, which is important for the diagnosis of antiphospholipid syndrome (see Chapter 53), but a lupus anticoagulant does not affect bleeding and should not be in the differential diagnosis of the bleeding patient. The assay is an easy, rapid, and cheap test to run and should be run early in the evaluation of the bleeding patient. Many fibrinogen assays incorporate function into the quantitative measurement, but since this information may not be readily available, thrombin time is able to measure the function of fibrinogen by adding thrombin to plasma and then measuring the conversion of fibrinogen to fibrin. Similarly, platelet function may be helpful if a defect in primary hemostasis is suspected, but platelet count and von Willebrand factor testing are normal. Platelet dysfunction disorders can be induced by many different medications, although they are often not clinically significant and rarely are congenital. Bleeding time, a test measuring the time it takes to stop bleeding after making a small incision in the forearm as a gauge of platelet function, should no longer be performed because numerous studies have shown poor sensitivity, specificity, and reproducibility with significant technician variability. Additional laboratory tests useful in evaluating bleeding include factor Xa activity for measurement of low-molecular-weight heparin effect, heparin neutralization (with heparinase, hexadimethrine bromide [Polybrene], or protamine), and euglobulin clot lysis time as a measure of fibrinolysis, the time to dissolve a fibrin clot. Because vitamin C deficiency (scurvy) can cause bleeding, measuring ascorbic acid can be helpful when nutrient deficiency is suspected. The time it takes for clot formation to block light passage through the specimen is measured and compared with a reference range. Although vascular purpura usually causes bleeding in the setting of normal platelet counts and normal coagulation tests, vasculitis and vessel damage may be severe enough to cause secondary consumption of platelets and coagulation factors. Collagen breakdown and thinning of the subcutaneous tissue that overlies blood vessels is often observed in older patients. The bleeding gums are caused by gingivitis and not by the subcutaneous tissue defect. Edentulous patients with scurvy do not have bleeding gums, and scurvy should not be excluded on this basis. Over time, activated platelets continue to aggregate, closing off the aperture to whole blood flow. The time it takes for aperture closing is measured in seconds and compared with a reference range. Abnormally prolonged closure times can be associated with von Willebrand disease due to the reliance on adhesion in this assay or with a platelet functional defect due to the reliance on aggregation for complete aperture closure. Screening laboratory tests for platelet and factor deficiencies are used to narrow the work-up for bleeding, followed by specific factor and other coagulation studies. Septic vasculitis can be caused by meningococcemia and other bacterial infections and is often accompanied by thrombocytopenia and prolongation of clotting times. This syndrome may occur after a viral prodrome and appears to be caused by an immunoglobulin A (IgA) hypersensitivity reaction, as evidenced by serum IgA immune complexes and renal histopathologic features resembling IgA nephropathy. In congenital disorders, including Ehlers-Danlos syndrome, hereditary hemorrhagic telangiectasia, and pseudoxanthoma elasticum, patients should avoid medications. Systemic administration of estrogen to patients with hereditary hemorrhagic telangiectasia may help to decrease epistaxis by inducing squamous metaplasia of the nasal mucosa, which protects lesions from trauma. In the case of aseptic vasculitis, steroids and immunosuppressive agents are most effective. Since most patients do not bleed from mild thrombocytopenia (50,000 to 150,000/L), treatment is often not required, but thrombocytopenia should be investigated to determine the cause, expected trajectory, and a plan for when treatment is needed. Broadly, thrombocytopenia results from a decline in platelet production, hypersplenism/sequestration, or destruction/consumption. Bone marrow biopsy can help because megakaryocyte hyperplasia implies increased production, a means of compensating for peripheral platelet destruction, whereas megakaryocyte hypoplasia suggests decreased platelet production. Disorders resulting in a decreased circulating platelet number can be classified by four main pathophysiologic mechanisms: hypoproduction, sequestration, peripheral destruction, and hemodilution. The history, physical examination, and bone marrow evaluation usually narrow the range of possible causes. Decreased Marrow Production of Platelets Decreased production of platelets in the bone marrow is characterized by decreased or absent megakaryocytes on the bone marrow aspirate and biopsy. Suppression of normal megakaryopoiesis occurs after marrow damage and destruction of stem cells (such as occurs with cytotoxic chemotherapy); destruction of the normal marrow micro-environment and replacement of normal stem cells by invasive malignant disease, aplasia, infection. Drug-Associated Thrombocytopenia Many drugs cause immune-mediated thrombocytopenia. However, some can have a direct cytotoxic effect on stem cells and megakaryocytes, causing a decline in platelet production. These medications are used to stop malignant cells from dividing, but they have the same effect on nonmalignant proliferating cells such as in the bone marrow. This myelosuppression frequently results in thrombocytopenia as well as neutropenia and anemia. Diagnostic confirmation comes from recovery of platelets after withdrawal of the medication. After repeated injury, stem cells may not recover, resulting in chronic thrombocytopenia. This process results in large erythroid precursors called megaloblasts and mature large red blood cells (macrocytes). Certain medications can have this effect: azathioprine, 5-fluorouracil, methotrexate, and others. Folate and vitamin B12 deficiencies are classic causes of megaloblastic anemia and when severe can cause pancytopenia. These deficiencies are most commonly caused by poor absorption either from autoimmune interference of intrinsic factor (pernicious anemia), other causes of atrophic gastritis, celiac disease, or previous gastrointestinal surgery. Copper deficiency causes leukopenia and anemia before affecting platelet production. It occurs in two settings, first through malabsorption from celiac disease and past bowel surgeries, and second, through copper transport blockage from zinc excess.
Prickly Yellow Wood (Southern Prickly Ash). Quibron-t.
- Are there safety concerns?
- Are there any interactions with medications?
- Dosing considerations for Southern Prickly Ash.
- How does Southern Prickly Ash work?
- What is Southern Prickly Ash?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96117
Order quibron-t 400mg amex
Eventually allergy testing pediatrics order generic quibron-t pills, the disease enters the accelerated phase, which is characterized by fever, weight loss, worsening splenomegaly, and bone pain related to rapid marrow cell turnover. The white blood cell count rises with increased numbers of circulating or marrow blasts ranging from 10% to 19%. The increased percentage of peripheral blood basophils (>20%) results in histamine production, with symptoms of pruritus, diarrhea, and flushing. During this phase, patients may develop increasing splenomegaly, persistent thrombocytopenia, or thrombocytosis and leukocytosis, with new clonal cytogenetic abnormalities found in marrow cells. Of note, two thirds of patients develop acute myeloid leukemia, whereas the others develop acute lymphoblastic leukemia, a finding confirming that the initial neoplastic cell is an early stem cell capable of multilineage differentiation. In contrast, the peripheral blood smear in reactive granulocytic hyperplastic states. Initial clinical trials of imatinib in 1998 were notable for a hematologic remission rate of 96% in patients receiving a dose greater than 300 mg per day for 4 weeks. The fact that patients achieving remission could have stable disease for years, even decades, demonstrated conclusively that this agent could effectively alter the natural history of this disease. These scores use patient age, spleen size, platelet number, and percentage of myeloblasts as well as peripheral basophilia and eosinophilia to divide patients into low-, intermediate-, and high-risk disease. However, calculation of these scores has proven useful to guide selection of upfront therapy at initial presentation. They must also be willing to undergo monthly to bimonthly visits for at least 2 years after drug discontinuation for frequent molecular testing. For this reason, it is recommended that patients requiring second-line therapy or beyond undergo testing for identification of mutations as a potential guide to therapy. In a phase 1 trial, almost half (48%) of patients achieved a major molecular response in 12 months, including 8 of 14 patients with prior intolerance or resistance to ponatinib. A major drawback is the need for subcutaneous injections administered twice daily for 7 to 14 days of every 28 days per month and treatment-associated myelosuppression that may warrant dose reduction or interruption. In adults, acute leukemias are relatively uncommon and occur in 8 to 10 of 100,000 people (compared with 42 of 100,000 for prostate cancer and 62 of 100,000 for breast cancer). Transplantation, however, remains the only known curative therapy for these patients. Pathology the pathogenesis of acute leukemia is complex and characterized by a high degree of biologic heterogeneity. Many patients with acute leukemia have detectable characteristic clonal chromosomal abnormalities and mutations that drive malignant transformation of normal hematopoietic stem cells bearing myeloid or lymphoid lineage markers. The resultant unchecked proliferation of these immature cells incapable of further differentiation. Known risk factors for leukemia include high-dose radiation exposure and occupational exposure to chemicals including benzene. Patients with chromosomal instability disorders such as Down syndrome, Bloom syndrome, Fanconi anemia, and ataxia telangiectasia also have an increased incidence of leukemia. Further immunophenotyping of blast cells using cell surface antigens, cytochemistry, and immunohistochemistry confirms cells as having a myeloid or lymphoid origin. Treatment consists of leukapheresis, hydroxyurea, and initiation of induction chemotherapy to inhibit further production of circulating tumor cells. Hydration, urine alkalinization to reduce uric acid crystallization, allopurinol, or rasburicase, or a combination, should be initiated as indicated. Red blood cell transfusions are often contraindicated in patients with high numbers of circulating blast cells because of the risk of further increases in blood viscosity. Severe thrombocytopenia, normocytic anemia, and circulating peripheral blasts are common. Bone marrow aspirate and biopsy typically show a profusion of myeloblasts (20% to 100%) and depressed production of normal mature cells. Clinical Presentation Patients exhibit clinical evidence of bone marrow failure similar to other hematopoietic disorders. Complications of disease include anemia, infection, and bleeding from peripheral cytopenias. Blasts may also invade other organs and lead to peripheral, mediastinal, and abdominal lymphadenopathy, hepatosplenomegaly, skin infiltration, and meningeal involvement. Induction therapy is directed at reducing the number of leukemic blasts to an undetectable level and restoring normal hematopoiesis. At complete remission, however, significant subclinical disease persists, requiring further therapy. Subsequent consolidation therapy involves continuing chemotherapy with the same agents to induce elimination of additional leukemic cells. With development of a wider range of effective agents, intensification therapy has been introduced. Maintenance therapy employs low-dose, intermittent chemotherapy given over a prolonged period to prevent subsequent disease relapse. The goal of therapy is to induce remission (>5% blasts in the bone marrow and recovery of normal peripheral blood counts). In both leukemias, cytogenetic and molecular abnormalities represent the best independent predictors of overall survival (Tables 47. Long-term cure rates (survival >5 years) range from 5% to 60% after chemotherapy alone, with an overall cure rate of 20% to 30%. Clinical Presentation Patients most often have complications related to progressively severe cytopenia, such as infection due to leukopenia, shortness of breath or fatigue due to anemia, or bleeding due to thrombocytopenia. Extramedullary disease includes leukemic involvement in the central nervous system, skin and soft tissues (myeloid or granulocytic sarcoma), and any other organ involvement outside of the bone marrow and peripheral blood. However, recent advances in genomic and Patients who are younger than 60 years and/or fit for intensive chemotherapy. The "traditional" induction regimens administered in the inpatient setting consist of 7 days of cytosine arabinoside. Some cytogenetic aberrations confer poor prognosis and are associated with resistance to and/or early relapse following standard chemotherapy regimens. These "poor-risk" cytogenetics include deletions in chromosome 5 or 7, inv(3q), t(3;3), t(6;9), t(9;22) (also known as the Philadelphia chromosome), monosomal karyotype, and three or more karyotypic abnormalities. These patients have a 30% to 45% long-term survival rate with standard 7+3 chemotherapy (see Table 47. These include substitution of higher-dose intermittent-dosed cytarabine instead of 7-day infusional cytarabine and the addition of other agents (such as cladribine or fludarabine) to cytarabine and anthracycline in attempts to enhance responses. However, the long-term survival rates after autologous transplantation range from 20% to 40% and are at least equivalent to consolidation chemotherapy regimens for these patients. Infectious complications remain the major cause of morbidity and mortality during intensive inpatient chemotherapy despite advances in prophylactic growth factor support, antibiotics, and antifungal agents. The low expected remission rates (30% to 50%) and high mortality and morbidity rates associated with induction are additional reasons for many patients to decline aggressive therapy. Fortunately, multiple therapeutic options are now available specifically for treatment of these older adults who in the recent past would have been offered only supportive therapy with hydroxyurea, transfusion support alone, and hospice. Patients older than 75 years old and/or those unfit for and who choose not to receive intensive therapy now have a panoply of low-dose chemotherapy options. These regimens have been well tolerated, but both are associated with disappointing response rates and median survival duration of less than 6 to 7 months. Adverse events included significant myelosuppression with risk of infection, sepsis, and pneumonia leading to early death in a proportion of patients. Treatment was well tolerated with relatively little myelosuppression or cytopenia. The excellent tolerability of this regimen with relatively little myelosuppression and the ability to treat patients completely in the outpatient setting makes it an option for select individuals. These agents, originally evaluated in the relapsed/refractory setting, result in overall response rates of approximately 40% and are well tolerated without myelosuppression. This serositis-like disorder is attributed to adhesion of differentiating neoplastic cells to the pulmonary vasculature and carries a 5% to 10% mortality rate. Treatment consists of early initiation of corticosteroids and aggressive diuresis.
Purchase discount quibron-t on line
Salads are often contaminated by protozoal cysts; along with street vendor foods allergy shots on nhs purchase quibron-t cheap, they are the most dangerous foods encountered by most travelers. Diphenoxylate (Lomotil) and loperamide (Imodium) may provide symptomatic relief of mild diarrhea. Oral rehydration is recommended in all cases regardless of severity and serves as an adjunct to antibiotics Other Vaccines Some individuals live for prolonged periods in developing countries or are at special risk for contracting certain highly contagious diseases. Consideration should be given to immunization against hepatitis B, cholera, plague (not commercially available in United States), and rabies. Tetanus vaccinations should be up to date: for travel, a tetanus booster within the previous 5 years is recommended. The cholera vaccine became approved in the United States as of 2016 as a single-dose oral vaccine. Given this and limited travel to areas of active cholera transmission, it is not routinely recommended for travelers in the United States, but standard cholera prevention and control measures are emphasized. Malaria Prophylaxis Malaria infection is associated with significant morbidity and mortality, particularly if the causative agent is Plasmodium falciparum. Worldwide, over 200 million cases occur per year, with increasing numbers of cases among travelers. First-line treatment includes fluoroquinolones, although increasing resistance is being seen in South and Southeast Asia, as well as other destinations. Noninfectious causes such as temporary lactose intolerance, irritable bowel syndrome, and, less commonly, inflammatory bowel disease should also be in the differential diagnosis. Special Problems Pregnant Women Although travel is rarely contraindicated during a normal pregnancy, complicated pregnancies require special consideration and may warrant a recommendation that travel be delayed. The risk of obstetric complications is highest during the first and third trimesters. If travel is unavoidable and the risks for yellow fever virus exposure are believed to outweigh the risks of vaccination, a pregnant woman should be vaccinated. Pregnant women should avoid or delay travel to malaria-endemic areas because no prophylactic measures provide complete protection. If travel is unavoidable, pregnant women should take utmost precautions to avoid mosquito bites; for chemoprophylaxis, chloroquine and mefloquine are the drugs of choice for destinations with chloroquine-sensitive and chloroquine-resistant malaria, respectively. Zika virus has been shown to cause congenital brain abnormalities including microcephaly as seen in the 2015-2016 outbreak throughout the Americas and Pacific Islands. If travel is unavoidable, pregnant women should be counseled on mosquito prevention methods to reduce their risk. Zika virus can also be sexually transmitted, and barrier precaution with condoms, or abstinence, should be advised throughout pregnancy. Fever Malaria should be the first diagnosis considered in a febrile traveler who has returned from a malarious area. Detection of the Plasmodium species on Giemsa-stained blood smears by light microscopy is the standard tool for diagnosis of malaria. Rapid diagnostic tests for detection of malaria parasite antigens are becoming increasingly important tools in resource-limited endemic settings because of their accuracy and ease of use. Quinine- and mefloquine-based regimens are more frequently associated with adverse effects, and mefloquine should not be used to treat P. Severe malaria is defined as acute malaria with major signs of organ dysfunction or a high level of parasitemia (>5%) or both. In many parts of the world, intravenous artesunate is used, but it may be associated with high rates of relapse. Other important causes of fever after travel include viral hepatitis (hepatitis A and E), typhoid fever, bacterial enteritis, arboviral infections. Skin Diseases Sunburn, insect bites, skin ulcers, and cutaneous larva migrans are the most common skin conditions affecting travelers after their return home. Persistent skin ulcers should prompt a work-up for cutaneous leishmaniasis, mycobacterial infection, or fungal infection. Careful, complete inspection of the skin is important in detecting the rickettsial eschar in a febrile patient or the central breathing hole in a "boil" caused by myiasis. They cause a tremendous burden of disease in the tropics and subtropics as well as more temperate climates. Of all protozoal diseases, malaria causes the most deaths globally, approximately 1 million people each year. The Returning Traveler the most common medical problems encountered by travelers after their return home are diarrhea, fever, respiratory illnesses, and skin lesions. If Giardia tests are Protozoal Infections in the United States Giardiasis Giardiasis is a common cause of nonbloody diarrhea in returning travelers. However, giardiasis is most commonly diagnosed in travelers returning from Latin America, Southeast Asia, or the Middle East. It is usually a self-limited diarrheal illness that lasts 2 to 4 weeks but may persist longer. The diagnosis is made by microscopic examination of stool for cysts or trophozoites or by an antigen detection test. Like Giardia, Entamoeba histolytica is found worldwide, and transmission is by the fecal-oral route. The presentation in those acutely infected includes bloody or watery diarrhea with abdominal cramping lasting up to 4 weeks. In immunocompromised individuals, a severe invasive infection can occur with risk of necrotizing colitis or bowel perforation. The diagnosis can be made by microscopic examination of stool for ova and parasites or by antigen detection tests of stool or serum. Treatment is with metronidazole or tinidazole in symptomatic individuals, followed by paromomycin or iodoquinol. Asymptomatic patients should also be treated with iodoquinol or paromomycin to prevent spread or later disease development. Visceral leishmaniasis can have hepatic, splenic, or bone marrow involvement and is more commonly identified in immigrants from Asia (Leishmania donovani) or South America (Leishmania chagasi). Treatment varies based on severity of presentation and resistance characteristics. Most cutaneous lesions are self-limited, but treatment options include sodium stibogluconate (Pentostam) or paromomycin. For visceral involvement, treatment includes sodium stibogluconate, amphotericin B, or a combination of these two agents. African Trypanosomiasis African trypanosomiasis, or African sleeping sickness, is a protozoal infection caused by Trypanosoma rhodesiense (East Africa) or Trypanosoma gambiense (Central and West Africa), which is transmitted by the tsetse fly. Presenting symptoms include fever, headache, and central nervous system involvement. The disease is rarely reported in travelers returning from sub-Saharan Africa but should be considered in immigrants from these areas. Consultation with an expert in infectious disease or tropical medicine is recommended. Protozoal Infections Common in Travelers and Immigrants Leishmaniasis Leishmaniasis is transmitted by the sandfly and can manifest with cutaneous, mucocutaneous, or visceral involvement. The presentation has an acute phase of 3 months followed by a chronic infection for life. However, most individuals are asymptomatic throughout the infection and are identified only at the time of blood donation. Between 20% and 30% of individuals develop manifestations of chronic infection decades later that can include cardiomegaly and heart failure, megaesophagus, or megacolon. In the chronic phase, various serologic analyses are available to aid in diagnosis. Chronic iron deficiency anemia associated with heavy hookworm infection can be severe and debilitating. Helminth Infections Common in Travelers and Immigrants Strongyloidosis Strongyloides stercoralis is a helminthic parasite that is found worldwide, although more commonly in the tropics. Infection occurs from contact with contaminated soil; the larva penetrates the skin, migrates to the lungs, and is then swallowed by the individual. The infection is usually asymptomatic, but infection can persist into the chronic phase decades later.
Generic quibron-t 400 mg on line
The continuous cycling of hematopoietic cells provides a milieu for the development of clonal genetic abnormalities that supports the multistep model allergy symptoms heart racing purchase quibron-t now. Clonal defects of the hematopoietic stem cell give rise to an array of premalignant and malignant disorders. Primary defects of maturation give rise to the myelodysplastic disorders (see Chapter 46), whereas loss of normal control of proliferation results in myeloproliferative disease encompassing chronic and acute leukemias. This is often accompanied by aberrant cytokine production affecting the marrow microenvironment, a gradual shift in hematopoietic cell production from the bone marrow to extramedullary sites in the liver and spleen, and altered coagulation. Although one half of patients have concurrent leukocytosis or thrombocytosis, erythrocytosis is the hallmark and the cause of the most serious clinical complications of this disease. Typically, patients complain of headache, visual problems, mental clouding, and pruritus after bathing. Occlusive vascular events such as stroke, transient ischemic attacks, myocardial ischemia, and digital pain, paresthesias, or gangrene are common. Paradoxically, patients are also predisposed to hemorrhagic events such as gastrointestinal and mucosal bleeding caused by abnormal platelet function and also ischemic necrosis downstream from vascular occlusion. Physical examination may show retinal vein occlusion, ruddy cyanosis, digital ischemia, and splenomegaly. Diagnosis and Differential Diagnosis When patients are first diagnosed with an elevated hemoglobin concentration per unit volume. Bone marrow biopsy showing hypercellularity for age with trilineage growth (panmyelosis) including prominent erythroid, granulocytic, and megakaryocytic proliferation with pleomorphic, mature megakaryocytes (differences in size) 3. Hypoxia caused by carbon monoxide poisoning, high oxygen affinity hemoglobin, high-altitude residence, chronic pulmonary disease, hypoventilation syndromes such as sleep apnea, right-to-left cardiac shunt, neurologic defects involving the respiratory center 3. Red blood cells in the peripheral blood often appear microcytic, with or without iron deficiency. Bone marrow examination shows a hypercellular marrow with pronounced hyperplasia of erythroid lineage cells. The development of clonal cytogenetic abnormalities heralds transformation in the later stages of disease. Twenty percent of patients show symptoms of arterial and venous thrombosis, and thrombosis remains the most common cause of death. Without treatment, up to one half of patients should focus on whether this increase reflects an enhanced red cell mass. In younger patients, nonsteroidal anti-inflammatory drugs and antiplatelet agents should be used judiciously because of the risk of gastrointestinal hemorrhage. Patients with advanced age (>60 years), prior history of thrombosis, leukocytosis, high hematocrit values, and clinical cardiovascular factors are at high risk for subsequent vascular events. For younger patients with lower cardiovascular risk factors, intermittent phlebotomy and aspirin prophylaxis remain the mainstays of treatment and usually result in iron deficiency anemia, which further reduces the rate of red blood cell production. Cytoreductive therapy is indicated for patients who cannot tolerate and/or fail phlebotomy, older patients with a prior history of and/or coexisting risk factors for cardiovascular events, and those with symptomatic splenomegaly. Choice of therapy is often individualized to the patient to best meet their lifestyle requirements given the chronicity of this disease. As with all myeloproliferative disorders, initiation of cytoreductive therapy may precipitate hyperuricemia that results in secondary gout and uric acid stones, warranting treatment with allopurinol. Reductions in white blood cell and platelet counts following ruxolitinib therapy were also reported. Bone marrow biopsy showing proliferation mainly of the megakaryocyte lineage with increased numbers of enlarged mature megakaryocytes with hyperlobulated nuclei. No significant left-shift of neutrophil granulopoiesis or erythropoiesis and very rarely minor (grade 1) increase in reticulin fibers 3. Vasomotor symptoms include headache, dizziness, visual changes, and erythromelalgia. Serious arterial thrombotic complications such as transient ischemic attacks, strokes, seizures, angina, and myocardial infarctions may occur. Diagnosis and Differential Diagnosis Elevated platelet counts (thrombocytosis) can result as a reactive process arising from other causes. Bone marrow histology typically displays predominant proliferation involving the megakaryocytic lineage and little or no granulocytic or erythroid proliferation or reticulin fibrosis. Although the median age at diagnosis is 60 to 65 years, 10% to 25% of patients are younger than 40 years. However, morbidity from recurrent hemorrhagic and thrombotic complications is high and cannot be reliably predicted from the platelet count or platelet function abnormalities. All patients benefit from aggressive management of cardiovascular risk factors including smoking, hypertension, obesity, and hypercholesterolemia. Although young and pregnant patients are often not treated until they become symptomatic, older patients (>60 years) and those with a history of thrombosis, long disease duration, or significant cardiovascular risk factors are most likely to benefit from the addition of platelet-lowering agents. Hydroxyurea, an oral cytotoxic and myelosuppressive agent, is the most common first-line agent and is usually well tolerated with low long-term leukemogenic risks. Anagrelide, an oral antiplatelet agent that inhibits platelet aggregation and megakaryocyte maturation, is also used, primarily as a second-line agent after hydroxyurea failure. This agent is associated with acute side effects such as fluid retention, palpitations, hemorrhage with concomitant aspirin use, and an increased risk of transformation to myelofibrosis. Chronic myeloproliferative disorders: chronic idiopathic myelofibrosis, chronic myelogenous leukemia, polycythemia vera b. Granulomatous diseases: mycobacterial infections, fungal infections, sarcoidosis b. Other underlying causes of neoplastic and non-neoplastic bone marrow fibrosis (Table 47. Clinical Presentation Although many patients are asymptomatic at diagnosis, most complain over time of progressive fatigue and dyspnea related to anemia or early satiety and left upper quadrant pain associated with splenomegaly and splenic infarction. More than one half of these patients develop massive hepatosplenomegaly due to extramedullary hematopoiesis. Patients with more advanced disease typically have constitutional symptoms such as fever, weight loss, night sweats, cachexia, pruritus, and bone pain, which may be debilitating. As the bone marrow failure evolves, complications of neutropenia, thrombocytopenia, and anemia develop as a result of ineffective hematopoiesis due to fibrotic changes and loss of marrow cellularity. Bleeding from occult disseminated intravascular coagulation is a risk as are infections arising from neutropenia. Etiology An abnormal myeloid precursor is thought to give rise to dysplastic megakaryocytes that produce increased levels of angiogenic and fibroblast growth factors. These cells then migrate and reestablish themselves in other sites, thereby shifting hematopoiesis out of the bone marrow and into other tissues, specifically the spleen and liver. Over time, the disease may progress from a chronic phase to an accelerated phase, with acute leukemic transformation in 8% to 20% of patients. Although low blood counts may occur, overall platelet and red blood cell numbers at diagnosis may be increased or normal depending on the degree of compensatory extramedullary hematopoiesis. Review of the peripheral blood profile commonly reveals leukoerythroblastic changes characterized by teardrop-shaped erythrocytes, giant platelets, and nonleukemic immature myeloid, erythroid, and leukocyte cells. Megakaryocyte proliferation and atypia without reticulin fibrosis > grade 1, accompanied by increased age-adjusted bone marrow cellularity, granulocytic proliferation, and often decreased erythropoiesis 2. Megakaryocyte proliferation and atypia accompanied by either reticulin and/or collagen fibrosis (grade 2 to 3) 2. Presence of one or more of the following, confirmed in two consecutive determinations a. Other causes of nonleukemic death include heart failure, infection, intracranial hemorrhage, and pulmonary embolism. Symptoms caused by excess thrombocytosis and leukocytosis or progressive extramedullary hematopoiesis may be managed with hydroxyurea as a first-line agent or pegylated interferon- in younger or pregnant patients. Enlarging splenomegaly is best managed with medical therapy because open splenectomy is associated with significant operative morbidity and mortality, and splenic irradiation is poorly tolerated except as a palliative approach. Patients receiving ruxolitinib had significantly greater spleen volume reduction and overall symptom improvement in abdominal pain, early satiety, night sweats, and muscle pain, all of which correlated with overall improvement in quality of life.
Safe 400mg quibron-t
Shunt placement is most likely to be effective if normal-pressure hydrocephalus occurs after severe head trauma or subarachnoid hemorrhage allergy shots bc purchase quibron-t 400 mg online. The disease causes spongiform degeneration and gliosis in widespread areas of the cortex. Clinical variants of the disorder are differentiated by the relative predominance of cerebellar symptoms, extrapyramidal hyperkinesias, or visual agnosia and cortical blindness (Heidenhain variant). Patients with all forms of the disease share a relentlessly progressive dementia and disruption of personality over weeks to months. The electroencephalogram shows characteristic abnormalities, including diffuse slowing and periodic sharp waves or spikes. The transmissible agent, a prion protein, is invulnerable to routine modes of antisepsis. Certain infectious agents can cause the subacute or chronic development of subcortical dementia. Human immunodeficiency virus accesses the central nervous system through monocytes and the microglial system and causes associated neuronal cell loss, vacuolization, and lymphocytic infiltration. The dementia associated with this infection is characterized by bradyphrenia and bradykinesia. Patients have executive dysfunction, impaired memory, poor concentration, and apathy. Treatment of the underlying viral infection with effective antiretroviral therapy may slow the progression of the dementia (see Chapter 103). There is increasing recognition of the potential for abnormal production of antibodies misdirected against brain epitopes to cause encephalopathy that can sometimes mimic classical dementia. Waxing and waning mental status rather than insidious progression of cognitive decline should prompt consideration of this category of illness as should cancer comorbidity, a history of autoimmune disease, or seizures in a patient presenting with cognitive changes. Patients with amnesia resulting from lesions of the medial temporal lobes or midline diencephalic structures have deficits of declarative memory. Nondeclarative memory encompasses several distinct and neuroanatomically less clearly localized functions related to the performance of specific learned motor, cognitive, or perceptual tasks. Deficits in nondeclarative memory may involve various areas of association neocortex, depending on the nature of the task. Patients with amnesia resulting from lesions of the medial temporal lobes tend to perform normally on tests of nondeclarative memory. Both types of amnesia usually occur together in brain injury syndromes, although the extent of one type or the other may vary. The degree of anterograde amnesia after head injury correlates with the severity of the injury. Isolated Disorders of Memory Function Memory can be impaired in relative isolation as a consequence of head injury, thiamine deficiency. Head injury typically results in retrograde amnesia in excess of anterograde amnesia, with both forms stretching out over time from the discrete event. As time passes, these disrupted memories gradually return, although rarely to the point at which the events immediately surrounding the trauma are recalled. Korsakoff syndrome is characterized by the near-total inability to establish new memory. Patients often confabulate responses when they are asked to convey the details of their current circumstance or to relay the content of a recently presented story. Deficiency of thiamine and other nutritional deficiencies in the context of chronic alcoholism are the most common underlying causes. Thiamine is a necessary cofactor in the metabolism of glucose, and thiamine must be replenished at the same time glucose is administered whenever a comatose patient is seen in the emergency department. Aging is associated with mild loss of memory, exhibited by difficulty in recalling names and by forgetfulness for dates. Population-based assessments of neuropsychological function have demonstrated that poor performance on delayed-recall tasks is the most sensitive indicator of cognitive change with advancing age. Verbal fluency, in contrast, remains intact with advancing age, and vocabulary may increase with time, even into old age. Transient global amnesia is a dramatic memory disturbance that affects older patients (>50 years). Patients usually have only one episode; occasionally, episodes recur over the course of several years. Patients have complete temporal and spatial disorientation; orientation for person is preserved. Near-total retrograde and anterograde amnesia persists for various periods, typically 6 to 12 hours. Transient global amnesia may be confused with psychogenic amnesia, fugue state, or partial complex status epilepticus. Transient global amnesia is thought to reflect underlying vascular insufficiency to the hippocampus or midline thalamic projections. Most characteristically, patients with psychogenic amnesia tend to express disorientation to person (asking, Who am I Vegetative signs, including changes in appetite, weight, and sleep pattern, are common, whereas signs of cortical impairment, such as aphasia, agnosia, and apraxia, are rare. For a deeper discussion on this topic, please see Chapter 374, "Cognitive Impairment and Dementia," in Goldman-Cecil Medicine, 26th Edition. Many mental disorders are caused by the direct effects of drugs, systemic disease, or neurologic disease on brain physiology. They may be broadly considered as secondary psychiatric disorders, as opposed to the primary or idiopathic psychiatric disorders. The distinguishing feature of neurocognitive disorders is impairment in intellectual functions such as level of consciousness, orientation, attention, or memory; however, these disorders also often include disruption of mood, thoughts, and behaviors similar to that seen in other psychiatric syndromes. The noncognitive secondary syndromes by definition cause psychiatric phenomena similar to their idiopathic counterparts. During the evaluation of any patient with new or worsened psychiatric symptoms, it is essential to conduct a thorough evaluation for other medical causes, including a careful history and physical examination (with a screening neurologic examination) that often are supplemented by laboratory evaluations. Although some conditions are likely to produce certain psychiatric syndromes, many manifest as any of several psychiatric syndromes. Because the cause of primary psychiatric disorders is unknown, approaches to classification depend on reliable empirical observations of phenomena clustered into recognizable syndromes. For example, major depression with psychotic features manifests with a depressive syndrome and a psychotic syndrome. In evaluating a patient with new or worsened psychiatric symptoms, the clinician must construct a differential diagnosis based on syndromes alongside the differential diagnosis based on potential secondary causes. Major depressive disorder is defined by episodes of a least five symptoms, including depressed mood, anhedonia, or loss of interests, that occur almost every day for at least 2 consecutive weeks, sufficient to cause significant distress and affect functional status. Other prominent symptoms may include associated anxiety, somatic worry, or new somatic symptoms, and in the most severe cases, psychotic symptoms, including nihilistic or self-deprecatory. Major depression is common, with a 12-month prevalence of approximately 7% and a lifetime prevalence of up to 10% among men and 20% to 25% in women. First onset may occur at any age but is most common in the third through fifth decades of life. Whereas most episodes of major depression fully remit spontaneously or with treatment, the lifetime risk of recurrence is at least 50% to 70%, and up to 20% of patients may experience chronic symptoms over many years. Major depression is a leading correlate of disability worldwide, is an important determinant of death by suicide, and is associated with increased risk of death from comorbid physical illnesses. Major depression also causes significant economic burden, costing approximately 210. Depressive disorders are heterogeneous, with many potential pathogenic mechanisms. Genetic factors, such as polymorphisms of the serotonin transporter protein, affect vulnerability to depressive episodes in the face of psychosocial stressors. Depression is polygenic and multifactorial, with genetic factors accounting for about 40% of the risk. Alterations in the functioning of brain serotonergic and noradrenergic systems and of the hypothalamic-pituitary-adrenal axis are found in depression. Neuroimaging studies show smaller hippocampal volumes and altered metabolic activity in several regions, including the anterior cingulate cortex. However, the information in these studies is not sufficient for making the clinical diagnosis, which depends on identification of the clinical syndrome.