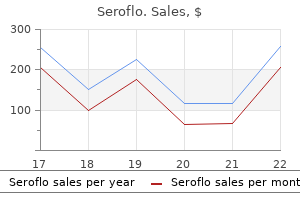
Discount seroflo 250mcg on-line
Florid cutaneous and mucosal papillomatosis with acanthosis nigricans revealing a primary lung cancer allergy symptoms child buy cheap seroflo online. Acanthosis nigricans associated with transitional cell carcinoma of the urinary bladder. The site and histology of the cancer associated with malignant acanthosis nigricans. Florid cutaneous papillomatosis with acanthosis nigricans in a patient with carcinomas of the lung and prostate. Improved acanthosis nigricans with lipodystrophic diabetes during dietary fish oil supplementation. The syndromes of insulin resistance and acanthosis nigricans: Insulin-receptor disorders in man. Acanthosis nigricans with severe obesity, insulin resistance and hypothyroidism: Improvement by diet control. Clinical, biochemical, and ovarian morphologic features in women with acanthosis nigricans and masculinization. Association of acanthosis nigricans with insulin resistance in patients with polycystic ovary syndrome. Acanthosis nigricans in a plaque of scleredema on the back of a diabetic patient: A case report. A case of acanthosis nigricans in obese siblings with a pedigree of familial polyposis coli. Seborrheoeic keratoses and acanthosis nigricans in a long-term survivor of thanatophoric dysplasia. Resolution of nicotinic acid-induced acanthosis, nigricans by substitution of an analogue (acipimox) in a patient with type V hyperlipidaemia. Acanthosis nigricans as an adverse effect of highly active antiretroviral therapy in an adolescent girl with human immunodeficiency virus infection. The involvement of insulin receptor genotypes in pre- and co-obese acanthosis nigricans children and adolescent. Keratin pattern of acanthosis nigricans in syndromelike association with polythelia, polycystic kidneys, and syndactyly. Confluent and reticulated papillomatosis of Gougerot and Carteaud: Its relation to other papillomatoses. Confluent and reticulate papillomatosis of Gougerot and Carteaud clearing with minocycline. Confluent and reticulated papillomatosis:, Response to high-dose oral isotretinoin therapy and reassessment of epidemiologic data. Pruritic eruption with reticular pigmentation: Confluent and reticulate papillomatosis. Confluent and reticulated papillomatosis associated with tinea versicolor in three siblings. Dietzia strain X: A newly described Actinomycete isolated from confluent and reticulated papillomatosis. Confluent and reticulated papillomatosis and, acanthosis nigricans in an obese girl: Two distinct pathologies with a common pathogenetic pathway or a unique entity dependent on insulin resistance Two patients with confluent and reticulated papillomatosis: Response to oral isotretinoin and 10% lactic acid lotion. Six cases of confluent and reticulated papillomatosis alleviated by various antibiotics. Confluent and reticulated papillomatosis: Failure of response to calcipotriol and coincidental association and vascular mottling. Successful treatment of confluent and reticulated papillomatosis with topical mupirocin. Confluent and reticulated papillomatosis: Clinical, light and electron microscopic studies. Is confluent and reticulated papillomatosis without papillomatosis early or late stage of confluent and reticulated papillomatosis Clinical pathologic challenge: Confluent and reticulate papillomatosis of Gougerot and Carteaud. Acrokeratosis paraneoplastica associated with recurrent metastatic thymic carcinoma. Coexistence of papuloerythroderma of Ofuji and acrokeratosis paraneoplastica (Bazex syndrome) preceding the diagnosis of primary hepatocellular carcinoma. Acrokeratosis paraneoplastica (Bazex syndrome) preceding the diagnosis of metastatic squamous cell carcinoma of the esophagus. Bullous lesions in Bazex syndrome and successful treatment, with oral psoralen phototherapy. Bazex syndrome (acrokeratosis paraneoplastica) diagnosed in a patient with oral persistent ulcerations. Acrokeratosis paraneoplastica (Bazex syndrome): Report of a case associated with small cell lung carcinoma and review of the literature. The incidence of erythroderma: A survey among all dermatologists in the Netherlands. Exfoliative erythroderma, recurrent infections, generalized lymphadenopathy and hepatosplenomegaly in a newborn: Omenn syndrome. Erythroderma/generalized exfoliative dermatitis in pediatric practice: An overview. Erythrodermic psoriasis: Precipitating factors, course, and prognosis in 50 patients. Dramatic improvement of psoriatic erythroderma after acute hepatitis: Analysis of cytokine synthesis capability in peripheral blood T cells. Erythroderma: A clinical and follow-up study of 102 patients, with special emphasis on survival. Generalized exfoliative dermatitis from ethylenediamine: Sensitization and induction. Drug eruption induced by cyanamide (carbimide): A clinical and histopathologic study of 7 patients. Photoallergic erythroderma due to , doxycycline therapy of erythema chronicum migrans. Erythroderma after autologous bone marrow transplantation modified by administration of cyclosporine and interferon gamma for breast cancer. Paraneoplastic erythroderma: An unusual manifestation of diffuse large B-cell lymphoma. Histopathology in erythroderma: Review of a series of cases by multiple observers. Heteroduplex analysis of T-cell receptor gene rearrangement as an adjuvant diagnostic tool in skin biopsies for erythroderma. Benign and malignant forms of erythroderma: Cutaneous and immunophenotypic characteristics. Lichenoid histopathologic changes in patients with clinical diagnoses of exfoliative dermatitis. Histopathologic diagnosis of lymphomatous versus inflammatory erythroderma: A morphologic and phenotypic study on 47 skin biopsies.
Buy generic seroflo on line
Safety of oral terbinafine: Results of a postmarketing allergy shots gluten purchase discount seroflo line, surveillance study in 25884 patients. Drug interactions with itraconazole, fluconazole, and terbinafine and their management. Drug eruption secondary to aciclovir with recall phenomenon in a dermatome previously affected by herpes zoster. An expanded profile of cutaneous reactions to nonsteroidal anti-inflammatory drugs. Fixed drug eruption related to ibuprofen presenting as giant bullae on the posterior thigh. Acute generalized exanthematous pustulosis-like, folliculitic drug reaction pattern caused by celecoxib. Lamotrigine and phenobarbitone-associated hypersensitivity syndrome: Resolution without corticosteroids. Interferon- production in the peripheral lymphocytes of a patient with carbamazepine hypersensitivity syndrome. Generalized pustulation as a manifestation of the anticonvulsant hypersensitivity syndrome. Generalized pustulosis and severe tubulointerstitial nephropathy as manifestations of cabamazepine hypersensitivity syndrome. Cutaneous necrosis and multinucleate epidermal cells associated with intravenous phenytoin. A rosacea-like granulomatous eruption in a patient using tacrolimus ointment for atopic dermatitis. Review of the potential photo-cocarcinogenicity of topical calcineurin inhibitors: Position statement of the European Dermatology Forum. The safety of tacrolimus ointment for the treatment of atopic dermatitis: A review. Short-contact topical tretinoin therapy to stimulate granulation tissue in chronic wounds. All-trans-retinoic acid-induced scrotal ulcerations in a patient with acute promyelocytic leukemia. Scrotal ulceration induced by all-trans retinoic acid in a patient with acute promyelocytic leukemia. Role of drugs in cutaneous eruptions after chemotherapy for acute myelogenous leukemia. Gemcitabine-induced erysipeloid skin lesions in a patient with malignant mesothelioma. A characteristic eruption associated with ifosfamide, carboplatin, and etoposide chemotherapy after pretreatment with recombinant interleukin-1. Cutaneous effects of thiotepa in pediatric patients receiving high-dose chemotherapy with autologous stem cell transplantation. Chemotherapy-induced toxic erythema under treatment with pegylated liposomal doxorubicin: No restriction to palms and soles. Histologic patterns of polyethelene glycolliposomal doxorubicin-related cutaneous eruptions. Pleomorphic presentation of cutaneous lesions associated with the proteasome inhibitor bortezomib in patients with multiple myeloma. Chemotherapy-induced acral erythema: Report of a case and immunohistochemical findings. A case of cutaneous reaction to chemotherapeutic agents showing epidermal dysmaturation. Syringomatous hyperplasia and eccrine squamous syringometaplasia associated with benoxaprofen therapy. Intradermal bleomycin injections into normal human skin: A histopathologic and immunopathologic study. Persistent supravenous erythematous eruption: A rare local complication of intravenous 5-fluorouracil therapy. Persistent serpentine supravenous hyperpigmented eruption associated with docetaxel. Serpentine supravenous pigmentation: A rare vasculo-cutaneous effect induced by systemic 5-fluorouracil. Onycholysis and subungual haemorrhages secondary to systemic chemotherapy (paclitaxel). Exudative hyponychial dermatitis associated with capecitabine and docetaxel combination chemotherapy for metastatic breast carcinoma: Report of three cases. Methotrexate-associated lymphoproliferative disorder in a patient with rheumatoid arthritis presenting in the skin. The appearance of inflammatory papules in the skin surrounding areas treated with imiquimod cream for basal cell carcinoma. Lupus erythematosus-like reaction in imiquimod-treated skin:, A report of 2 cases. Psoriasiform eruption and oral ulcerations as adverse effects of topical 5% imiquimod treatment in children: A report of four cases. Injection site reaction after subcutaneous administration of bortezomib in Japanese patients with multiple myeloma. Neutrophil-dependent cutaneous side effects of leucocyte colony-stimulating factors: Manifestations of a neutrophil recovery syndrome A generalized cutaneous reaction induced by granulocyte colony-stimulating factor. Histopathology of cutaneous reaction to granulocyte colony-stimulating factor: Another pseudomalignancy. Cutaneous reactions to recombinant human interferon beta-1b: the clinical and histologic spectrum. Local reactions associated with subcutaneous injections of both -interferon 1a and 1b. Dermal fibrosis and cutaneous necrosis after recombinant interferon-1a injection in a multiple sclerosis patient. Abdominal wall ulceration and mucinosis secondary to recombinant human interferon-1b. Skin necrosis with subsequent formation of squamous cell carcinoma after subcutaneous interferon beta injection. Diffuse cutaneous eruption due to interferon alfa and ribavirin treatment of chronic hepatitis C. Granulomatous and suppurative dermatitis at interferon alfa injection sites: Report of 2 cases. Cutaneous necrosis after injection of polyethylene glycol-modified interferon alfa. Adverse cutaneous reactions to anakinra in patients with rheumatoid arthritis: Clinicopathological study of five patients. The role of interleukin 10 in the pathogenesis and potential treatment of skin diseases. Clinical, histological, and immunophenotypic characteristics of injection site reactions associated with etanercept. Immediate type I hypersensitivity response implicated in worsening injection site reactions to adalimumab. Recall injectionsite reactions associated with etanercept therapy: Report of two new cases with immunohistochemical analysis. Etanercept-induced injection site reactions: Mechanistic insights, from clinical findings and immunohistochemistry.
Order generic seroflo pills
Desmoplastic malignant melanoma: A light and electron microscopic study of two cases allergy testing kit for dogs order seroflo overnight. Gene copy number analysis by fluorescence in situ hybridization and comparative genomic hybridization. Chomosomal gains and losses in primary cutaneous melanomas detected by comparative genomic hybridization. Correlating array comparative melanocytic nevi: Differences between nodular proliferations and melanomas. Genetic changes in neoplasms arising in congenital melanocytic nevi: Differences between nodular proliferations and melanomas. Fluorescence in situ hybridization, a diagnostic aid in ambiguous melanocytic tumors: European study of 113 cases. Distinction of conjunctival melanocytic nevi from melanomas by fluorescence in situ hybridization. Fluorescence in situ hybridization for distinguishing, nevoid melanomas from mitotically active nevi. Diagnosis of cutaneous melanocytic tumours by four-colour fluorescence in situ hybridisation. Fluorescence in situ hybridization as an ancillary, method for the distinction of desmoplastic melanomas from sclerosing melanocytic nevi. Gerami P Discussion on relative significance of specific chromosomal abnormalities in. Distribution and significance of occult, intraepidermal tumor cells surrounding primary melanoma. Fluorescence in situ hybridization as a tool for microstaging in malignant melanoma. Topoisomerase I amplification in melanoma is associated with more advanced tumours and poor prognosis. Copy number gains in 11q13 and 8q24, [corrected] are highly linked to prognosis in cutaneous malignant melanoma. Interobserver reproducibility of histopathologic prognostic variables in primary cutaneous melanomas. Interobserver reproducibility of histological features in cutaneous malignant melanoma. Interobserver reproducibility of ulceration assessment in primary cutaneous melanomas. Prognosis for patients with thin cutaneous melanoma: Long-term survival data from the New South Wales Central Cancer Registry and the Sydney Melanoma Unit. A rational approach to melanoma follow-up in patients with primary cutaneous melanoma: Scottish Melanoma Group. Occult tumor cells in the lymph nodes of patients with pathological stage I malignant melanoma: An immunohistological study. Melanoma patient staging: Histopathological versus molecular evaluation of the sentinel node. Prognostic significance of molecular upstaging of paraffin-embedded sentinel lymph nodes in melanoma patients. Sentinel lymph node molecular ultrastaging in, patients with melanoma: A systematic review and meta-analysis of prognosis. Polymerase chain reaction detection of circulating melanocytes as a prognostic marker in patients with melanoma. Prognostic factors for patients with clinical stage I melanoma of intermediate thickness (1. The frequency of local recurrence and microsatellites as a guide to reexcision margins for cutaneous malignant melanoma. The prognostic implications of microscopic, satellites in patients with clinical stage 1 melanoma. Prognostic factors in localized invasive cutaneous melanoma: High value of mitotic rate, vascular invasion and microscopic satellitosis. Thickness, cross-sectional area and depth of invasion in the prognosis of cutaneous melanoma. Stage I melanoma of the skin: Evaluation of, prognosis according to histologic characteristics. Predicting five-year outcome for patients with cutaneous melanoma in a population-based study. Evaluating invasive cutaneous melanoma: Is the initial biopsy representative of the final depth An evidence base for reconsidering current follow-up guidelines for patients with cutaneous melanoma less than 0. Using a continuous transformation of the Breslow thickness for prognosis in cutaneous melanoma. Rate of growth in melanomas: Characteristics and, associations of rapidly growing melanomas. The relationship between melanoma thickness and time to diagnosis in a large population-based study. Increasing ratio of thin to thick melanoma lesions: Pathogenesis and early detection of this cancer. The use of sequential serial sectioning of thin melanomas in determining maximum Breslow depth. Volume of malignant melanoma is superior to thickness as a prognostic indicator: Preliminary observation. Primary cutaneous malignant melanoma: An analysis of the prognostic value of histologic characteristics. The importance of mitotic rate as a prognostic factor for localized cutaneous melanoma. The importance of mitotic rate as a prognostic factor for localized primary cutaneous melanoma. Tumor mitotic rate is a more powerful prognostic indicator than ulceration in patients with primary cutaneous melanoma: An analysis of 3661 patients from a single center. Histological type and biological behavior of primary cutaneous malignant melanoma: 2. An analysis of 86 cases located on so-called acral regions as plantar, palmar, and sub-/parungual areas. Primary cutaneous melanoma: Identification of, prognostic groups and estimation of individual prognosis for 5093 patients. Immunohistological characterisation of tumour infiltrating lymphocytes in melanocytic skin lesions. Melanophages reside in hypermelanotic, aberrantly glycosylated tumor areas and predict improved outcome in primary cutaneous malignant melanoma. Histologic classification of tumorinfiltrating lymphocytes in primary cutaneous malignant melanoma: A study of interobserver agreement. Favorable prognosis for malignant melanomas associated with acquired melanocytic nevi. Cytomorphometric parameters and the metastatic potential of cutaneous and uveal melanoma: A comparison with prognostic factors. Prediction of lymph node metastases from the histologic features of primary cutaneous malignant melanomas. Plasma cells within the infiltrate of primary cutaneous malignant melanoma of the skin: A confirmation of its histoprognostic value. Paratumoral epidermal hyperplasia: A novel prognostic factor in thick primary melanoma of the skin Thick malignant melanomas (>3 mm Breslow) with good clinical outcome: A histological study and survival analysis. Survival and prognostic factors of patients with skin melanoma: A regression-model analysis based on nationwide cancer registry data. Survival superiority of females with melanoma: A multivariate analysis of 6383 patients exploring the significance of gender in prognostic outcome.

Purchase seroflo 250mcg with mastercard
Nocardia infection unassociated with grain formation should be differentiated from other infections due to filamentous bacteria allergy testing acne discount 250 mcg seroflo mastercard. Compared to Actinomyces, Nocardia organisms are shorter and have a greater tendency to fragment, sometimes even forming bacillary structures. It is also doubtful that methenamine silver stains are truly helpful in distinguishing small bacillary fragments of Nocardia from other acid-fast bacilli, as has been suggested in the past, because both M. Similar lesions can be caused by other actinomycetes, including species of Streptomyces and Actinomadura. One case was successfully treated with a combination of amoxicillin and minocycline. There are often several locules, which are separated by areas of granulation tissue in which foamy macrophages are present. The granules are composed of numerous slender beaded filaments that tend to be crowded at the periphery of the granules. Histopathology There is usually a dense infiltrate of neutrophils in the deep dermis and subcutis, with frank abscess formation. Special stains show them to be fine, branched filaments that are gram positive, usually weakly acid fast, and that stain with the silver methenamine method. Nocardia can form grains and are also filamentous, but the filaments tend to be shorter, and unlike Actinomyces, Nocardia organisms are acidfast (however, see the previous section on nocardiosis). The filaments of other actinomycetomas (including those caused by Actinomadura or Streptomyces species) can have a close resemblance to Actinomyces, but the organisms of eumycetomas. Grossly, inspecting the color of the grains in lesional drainage can sometimes provide clues to the nature of the organism, which can then be supported by microscopic and culture studies. Because the lesions closely mimic clinically and histologically those of mycetoma, botryomycosis is included in this chapter. Antibiotics are used to treat botryomycosis, with the agent used depending on the sensitivity of the causative bacteria and the immune status of the host. However, because the infections caused by fungi within the order Entomophthorales, which is the other major group of Zygomycetes, are clinically quite different from mucormycosis, the two groups of infections are considered separately. These fungi are widespread in nature, particularly in soil and decaying vegetable matter. Primary cutaneous mucormycosis is rare and usually develops in diabetics, in patients with thermal burns, and sometimes in those who are immunocompromised. The new triazole antifungal agents, such as posaconazole, have shown greater efficacy and less toxicity than amphotericin B and may become the treatment of choice. They must be distinguished from other organisms, particularly swollen, degenerated hyphae of Aspergillus. Cross-sectional profiles of zygomycete hyphae could be confused with empty spherules of Coccidioides immitis (discussed previously), but in contrast to Coccidioides, endosporulation is not seen, and other portions of the specimen are likely to show identifiable hyphal forms. There may be a resemblance to superficial granulomatous pyoderma, although the presence of fungal elements assists in making a distinction. They branch at right angles, in contrast to Aspergillus, which usually branches at an acute angle. The most striking feature is the presence of smudgy eosinophilic material surrounding the hyphae. One case of subcutaneous infection due to Cephalotheca foveolata, not previously thought to cause human infection, has been reported. Histopathology There is usually a heavy acute and chronic inflammatory cell infiltrate in the dermis and/or the subcutis. Dermal necrosis may be associated with mycelia invading blood vessels with subsequent thrombosis. The majority of cutaneous lesions are umbilicated papules, resembling molluscum contagiosum. Systemic fusariosis mainly occurs in immunocompromised individuals with hematological malignancies, usually with associated neutropenia. In a series of 35 patients with cancer and Fusarium infection, reported from the M. Anderson Cancer Center in Houston, Texas, 20 had disseminated infection, 6 had primary localized skin infections, 4 had skin lesions associated with sinus infections, and 5 had onychomycosis. There may be red or gray macules, pustules, subcutaneous nodules, ecthyma gangrenosum-like lesions with a black eschar,1116,1117 target lesions, lupus vulgaris-like lesions,1118 vasculitic Histopathology There is a diffuse dermal infiltrate composed mainly of histiocytes and lymphocytes. They have some resemblance to Histoplasma but differ by the lack of surface budding and by the presence of central division with the formation of septa within the organism. Caspofungin, voriconazole, flucytosine, terbinafine, and itraconazole have all been used at different times. Fusarium organisms may be slightly wider than Aspergillus, and the branches arise at right angles and are constricted at the point of connection to the hyphae of origin. Pseudallescheria organisms are somewhat thinner than Aspergillus organisms, with haphazard branching and formation of vesicles and ovoid conidia. Histopathology Depending on the host response, there can be a variety of changes ranging from well-developed granulomas1139 to areas of suppuration and abscess formation1150 or the presence of masses of fungi with a minimal mixed inflammatory cell response. Granulomas tend to occur in localized lesions of aspergillosis in patients who are immunocompetent or who have received antifungal therapy. Thus, as is sometimes true of mucormycosis, aspergillosis can show subcutaneous tissue changes that mimic the ghost cells of pancreatic panniculitis or the radially arranged crystals seen in gouty panniculitis. Differential diagnosis Multiple buds can sometimes be seen around the cells of lobomycosis, which can then be confused with the organisms of paracoccidioidomycosis. Chains of cells as seen in lobomycosis are not observed in North American blastomycosis, and L. Despite the alternative name for this infection (keloidal blastomycosis) and the keloid-like clinical appearance of some lesions, the microscopic features of keloid are not observed. Cutaneous lesions are rare, even in India, Sri Lanka, and South America, where the causative agent, Rhinosporidium seeberi, is endemic. In addition to protothecosis (discussed next), the intake of the blue-green alga Spirulina platensis in a food supplement has produced a presumptive eruption that exhibited features of both bullous pemphigoid and pemphigus foliaceus. Cutaneous lesions are eczematous,1215 pustular,1216 herpetiform,1217 or papules1218 and papulonodules that may coalesce, resulting in the formation of slowly progressive plaques. There is focal necrosis in some lesions, particularly those with subcutaneous involvement. They may also be found in necrotic foci1224 and free in the dermis, but they are difficult to see in H&E-stained preparations. Specific identification can be made with a fluorescein-labeled monoclonal antibody. Rapid detection of fungi in tissues using calcofluor white and fluorescence microscopy. Evaluation of the use of Congo red staining in the differential diagnosis of Candida vs. Molecular determination of dermatophyte fungi using the arbitrarily primed polymerase chain reaction. Identification of common dermatophytes (Trichophyton, Microsporum, Epidermophyton) using polymerase chain reactions. Diagnosis of common dermatophyte infections by a novel multiplex real-time polymerase chain reaction detection/identification scheme.
Cheap seroflo
Perineal ecthyma gangrenosum in infancy and early childhood: Septicemic and nonsepticemic forms allergy symptoms 1 week after conception buy cheap seroflo on line. Multiple erythematous nodules and ecthyma gangrenosum as a manifestation of Pseudomonas aeruginosa sepsis in a previously healthy infant. Ecthyma gangrenosum: Report of clinical, histopathologic, and bacteriologic aspects of eight cases. Pseudomonas aeruginosa ecthyma gangrenosum, and facial cellulitis complicating carbimazole-induced agranulocytosis. Ecthyma gangrenosum caused by disseminated Exserohilum in a child with leukemia: A case report and review of the literature. Ecthyma gangrenosum and septic shock syndrome secondary to Chromobacterium violaceum. Successful treatment of Fusarium solani ecthyma gangrenosum in a patient affected by leukocyte adhesion deficiency type 1 with granulocytes transfusions. Nonpseudomonal ecthyma gangrenosum associated with methicillin-resistant Staphylococcus aureus infection: A case report and review of the literature. Ecthyma gangrenosum secondary to severe invasive infection caused by Escherichia coli. Ecthyma gangrenosum-like lesions in a healthy child after infection treated with antibiotics. Multiple erythematous nodules as a manifestation of Pseudomonas aeruginosa septicemia. Presentation and outcome of purpura fulminans associated with peripheral gangrene in 12 patients at Mayo Clinic. Bullous cellulitis and myonecrosis secondary to Escherichia coli in a patient with cirrhosis. Painful red nodules of the legs: A manifestation of chronic infection with gram-negative organisms. Persistent infection of the chin with an unusual, skin pathogen (Streptococcus milleri): A sign of intraoral carcinoma. Infectious and toxic cellulitis due to suicide, attempt by subcutaneous injection of ricin. Subcutaneous lesions and bacteraemia due to Stenotrophomonas maltophilia in three leukaemic patients with neutropenia. Cutaneous infections with Stenotrophomonas maltophilia in patients using immunosuppressive medication. Biopsy specimen findings in patients with previous lower extremity cellulitis after saphenous venectomy for coronary artery bypass graft surgery. Manifestation of cellulitis after saphenous venectomy for coronary bypass surgery. Noma-like gangrenous cheilitis in a child with cyclic neutropenia associated with myeloperoxidase deficiency. Rhodococcus equi subcutaneous abscess in a patient with acquired immunodeficiency syndrome. Recurrent Serratia marcescens cutaneous, infection manifesting as painful nodules and ulcers. Cutaneous and soft-tissue manifestations of sepsis due to gram-negative enteric bacilli. Community-acquired methicillin-resistant Staphylococcus aureus skin infections: A review of epidemiology, clinical features, management, and prevention. Bacterial pyoderma in children and therapeutic options including management of community-acquired methicillin resistant Staphylococcus aureus. Community-acquired methicillin-resistant Staphylococcus aureus skin infection: A retrospective analysis of clinical presentation and treatment of a local outbreak. Burden of illness of bacterial cellulitis and erysipelas of the leg in the Netherlands. Recurrence of lymphoedema-associated cellulitis (erysipelas) under prophylactic antibiotherapy: A retrospective cohort study. Streptococcal cause of erysipelas and cellulitis in, adults: A microbiologic study using a direct immunofluorescence technique. Recurrent hemolysis-associated pseudoerysipelas of the lower legs in a patient with congenital spherocytosis. Erysipelas as a sign of subclinical primary lymphoedema: A prospective quantitative scintigraphic study of 40 patients with unilateral erysipelas of the leg. Erysipelas-like erythema of familial Mediterranean, fever syndrome: A case report with emphasis on histopathologic diagnostic clues. Occupational injury in a fishmonger with a macular rash, hepatosplenomegaly and pancytopenia. Cutaneous Erysipelothrix rhusiopathiae (erysipeloid) infection in an immunocompromised child. Staphylococcus aureus-induced blistering distal dactylitis in an adult immunosuppressed patient. Autopsy findings in an outbreak of severe systemic, illness in heroin users following injection site inflammation: An effect of Clostridium novyi exotoxin Community-associated methicillin-resistant Staphylococcus aureus causing orbital cellulitis in Australian children. Orbital cellulitis caused by community-associated methicillin-resistant Staphylococcus aureus in a previously healthy neonate. Vibrio vulnificus septicemia in Korea: Clinical and epidemiologic findings in seventy patients. Clinical, epidemiological, and microbiological features of Vibrio vulnificus biogroup 3 causing outbreaks of wound infection and bacteraemia in Israel. The importance of serum creatine phosphokinase level in the early diagnosis, and as a prognostic factor, of Vibrio vulnificus infection. Cutaneous manifestations of non-01 Vibrio cholerae septicemia with gastroenteritis and meningitis. Life-threatening Escherichia coli cellulitis in patients with haematological malignancies. A rare case of endogenous Streptococcus group C endophthalmitis associated with cellulitis. Necrotizing fasciitis: A clinical, microbiologic, and histopathologic study of 14 patients. Objective criteria may assist in distinguishing necrotizing fasciitis from nonnecrotizing soft tissue infection. Massive infectious soft-tissue injury: Diagnosis and management of necrotizing fasciitis and purpura fulminans. Necrotizing fasciitis in infancy: Report of three cases and review of the literature. Severe necrotizing soft-tissue infections and, nonsteroidal anti-inflammatory drugs. Necrotizing fasciitis: the role of Staphylococcus epidermidis, immune status and intravascular coagulation. Fulminant group A streptococcal necrotizing fasciitis: Clinical and pathologic findings in 7 patients. The importance of serum creatine phosphokinase level in the early diagnosis and microbiological evaluation of necrotizing fasciitis. Chromobacterium violaceum necrotizing fasciitis: A case report and review of the literature. Fulminant necrotizing fasciitis, caused by Serratia marcescens in an immunosuppressed host. Favorable outcome of amphotericin B treatment of zygomycotic necrotizing fascitis (sic) caused by Apophysomyces elegans. Necrotizing pyoderma gangrenosum: An unusual differential diagnosis of necrotizing fasciitis. Necrotizing Sweet syndrome: A new variant of neutrophilic dermatosis mimicking necrotizing fasciitis.
Buy seroflo 250 mcg
Chemotherapy-induced inflammation in seborrheic keratoses mimicking disseminated herpes zoster allergy forecast maryland buy seroflo once a day. Spontaneous regression of multiple seborrheic keratoses associated with nasal carcinoma. Florid eruption of seborrheic keratoses associated with elevated insulin-like growth factor, hypoglycemia, and solitary fibrous tumor of the pleura. Eruptive seborrheic keratoses associated with erythrodermic pityriasis rubra pilaris. Seborrheic keratoses: Appearances in course of exfoliative erythroderma and regression associated with histologic mononuclear cell inflammation. Transient eruptive seborrhoeic keratoses associated with erythrodermic pityriasis rubra pilaris. Transient eruptive seborrheic keratoses associated with erythrodermic psoriasis and erythrodermic drug eruption: Report of two cases. Immunohistochemical features of multifocal melanoacanthoma in the hard palate: A case report. Multiple clear cell acanthomas: Case report and delineation of basement membrane zone antigens. Clear cell acanthoma presenting as polypoid papule combined with melanocytic nevus. Clear-cell acanthoma versus acanthosis: A psoriasiform reaction pattern lacking tricholemmal differentiation. Immunohistochemical characterization of keratin expression in clear cell acanthoma. Clear cell acanthoma developing on a psoriatic plaque: Further evidence of an inflammatory aetiology Disseminated eruptive clear cell acanthoma with spontaneous regression: Further evidence of an inflammatory origin Multiple clear-cell acanthoma (Degos):, Histochemical and ultrastructural study of two cases. Value of the Tzanck smear test and dermatoscopy in the diagnosis of clear cell acanthoma. Clear cell papulosis: A unique disorder in early childhood characterized by white macules in milk-line distribution. Clear-cell papulosis: A rare entity that may be misconstrued pathologically as normal skin. A conjunctival lesion with histological features similar to large-cell acanthoma of the skin. Clinocopathologic and immunohistochemical studies of conjunctival large cell acanthoma, epidermoid dysplasia, and squamous papilloma. Large-cell acanthoma of the skin: A study by image analysis cytometry and immunohistochemistry. Multiple disseminated large-cell acanthomas of the skin associated with human papillomavirus type 6. Chemotherapy for disseminated actinic keratoses with 5-fluorouracil and isotretinoin. Destructive procedures are the standard of care for treatment of actinic keratoses. Unusual distribution of punctate dysplastic keratoses and skin cancers in sunbed users: A report of three cases. Sun-related factors, betapapillomavirus, and, actinic keratoses: A prospective study. Solar keratosis: Fallacies in measuring remission rate and conversion rate to squamous cell carcinoma. Patients with solar keratosis, particularly of the trunk or lower extremities, are at high risk for skin cancer development. Actinic keratosis is an early in situ squamous cell carcinoma: A proposal for reclassification. An actinic keratosis is neither malignant nor premalignant: It is an initiated tumor. The prevalence and determinants of solar keratoses at a subtropical latitude (Queensland, Australia). Prevalence of sunless tanning product use and, related behaviors among adults in the United States: Results from a national survey. Increased Fas ligand expression by T cells and tumour cells in the progression of actinic keratosis to squamous cell carcinoma. Expression of E-cadherin and beta-catenin in cutaneous squamous cell carcinoma and its precursors. Cyclin D and retinoblastoma gene product expression in actinic keratosis and cutaneous squamous cell carcinoma in relation to p53 expression. Expression of apoptotic, cell proliferation regulatory, and structural proteins in actinic keratosis and their association with dermal elastosis. Activated ras genes occur in human actinic keratoses, premalignant precursors to squamous cell carcinomas. Microarray analysis of aberrant gene expression in actinic keratosis: Effect of the Toll-like receptor-7 agonist imiquimod. A prospective study of the use of cryosurgery for, the treatment of actinic keratoses. Long-term treatment of photoaged human skin with topical retinoic acid improves epidermal cell atypia and thickens the collagen band in papillary dermis. Clinical recurrence of actinic keratosis following marginal biopsy: A retrospective study. Clinical recognition of actinic keratoses in a high-risk population: How good are we The significance of the Darier-like solar keratosis and acantholytic changes in preneoplastic lesions of the epidermis. Large haematoxylin-stainable keratohyaline granules in solar keratoses: Immunohistochemical comparison using anti-Ted-H-1 antibody and antiloricrin antibody. Inflammation of actinic keratoses and acral erythrodysesthesia during capecitabine treatment. Inflammation of actinic keratoses subsequent to therapy with sorafenib, a multitargeted tyrosine-kinase inhibitor. Inflammation is associated with progression of actinic keratoses to squamous cell carcinomas in humans. Correlation between Bcl-2 and Bax in atrophic and hypertrophic type of actinic keratosis. Distinctive epidermal atypia in immunosuppression-associated cutaneous malignancy. Histopathologic features of actinic keratoses in solid organ transplant recipients and healthy controls. Histologic features of actinic keratoses in solid organ transplant recipients and healthy controls. What is the boundary that separates a thick solar keratosis and a thin squamous cell carcinoma Accurate diagnosis of cutaneous keratinocytic neoplasms: the importance of histological step sections (and other factors). Utility of step sections: Demonstration of additional pathological findings in biopsy samples initially diagnosed as actinic keratosis.
Buy 250 mcg seroflo mastercard
The term pseudoerysipelas has been given to a recurrent hemolysisassociated erythematous eruption of the lower legs in a patient with hereditary spherocytosis allergy symptoms oregon discount seroflo 250mcg overnight delivery. Rheumatoid disease can be accompanied by cutaneous neutrophilic infiltrates, two examples being rheumatoid neutrophilic dermatosis and interstitial granulomatous dermatitis (the latter is not restricted to rheumatoid disease and can be seen in a wide variety of connective tissue, inflammatory, and infectious processes). The density of neutrophils in rheumatoid neutrophilic dermatosis and the presence of interstitial granulomas in interstitial granulomatous dermatitis would be distinctive. There are some microscopic differences between true erysipelas and the erysipelas-like erythema that accompanies familial Mediterranean fever. In contrast to erysipelas, erysipelas-like erythema has a milder inflammatory infiltrate, is less likely to have an interstitial component to the infiltrate, includes mononuclear cells as well as neutrophils, may or may not demonstrate leukocytoclasis, and shows absent or only mild papillary dermal edema. A recent case of erysipeloid of 1-year duration presented as macrocheilitis; microscopic examination showed noncaseating granulomas. Sometimes there is spongiosis of the epidermis, leading to intraepidermal vesiculation. Organisms are not demonstrable in tissue sections, even with a Gram stain, possibly because they are present in the L form (without a cell wall). Beneath this zone, there is a diffuse and usually heavy infiltrate of neutrophils, but abscesses do not form. Direct immunofluorescence has been used to confirm the streptococcal etiology of most cases of erysipelas. Differential diagnosis Histopathologic evaluation is not always carried out in cases of erysipelas (or cellulitis), and when carried out, it generally provides only supportive rather than independently diagnostic information. The finding of neutrophils in the dermis in the absence of an obvious source, such as ulceration, ruptured follicles or cysts, or leukocytoclastic vasculitis, should always raise the possibility of infection and prompt cultures or other laboratory studies. Uncommonly, the condition follows surgery;250 in one case, it followed mosquito bites. B Differential diagnosis the depth of involvement, as well as the degree of connective tissue degeneration and necrosis, is much greater in necrotizing fasciitis than in erysipelas or traditional forms of cellulitis. Necrosis and connective tissue degeneration are also seen in forms of ischemia, including calciphylaxis and bullae related to coma or barbiturate intoxication, but these conditions lack the neutrophilic infiltration of necrotizing fasciitis, and Gram stains and tissue culture studies are typically negative. The clinical distinction between necrotizing fasciitis and pyoderma gangrenosum can sometimes be difficult. In summary, pyoderma gangrenosum beyond early stages tends to show subepidermal edema and undermining inflammation at the ulcer border. Although there can be extension of inflammation into the subcutis, deep vessel thrombosis is not a characteristic feature of pyoderma gangrenosum. The granulomas seen in some examples of pyoderma gangrenosum would also argue against necrotizing fasciitis, as of course would negative blood and tissue culture studies. Edema, purpura, and blisters were among the clinical features, although the patient was not pyrexic, appeared systemically well, and the affected areas in many cases were cooler than adjacent, uninvolved skin. Biopsy showed epidermal necrosis, subepidermal bullae, and dermal edema with hemorrhage and necrosis. Predisposing factors for thrombosis in this patient included heterozygosity for the factor V Leiden mutation (resulting in resistance to activated protein C) and her pregnancy status at the time of presentation. Microscopically, acute inflammation involved the subcutis and fascia, associated with fat necrosis and significant myonecrosis. They include clostridial myonecrosis (gas gangrene), progressive bacterial synergistic gangrene, and erosive pustular dermatosis of the scalp, legs, and other sites. Clostridialmyonecrosis(gasgangrene) Clostridial myonecrosis (gas gangrene) is associated with muscle and soft tissue necrosis. The usual causative organisms in gas gangrene are clostridial species; nonclostridial cases are infrequently reported. Hyperbaric oxygen therapy is also effective, but it should not delay the other measures already mentioned. Topical tacrolimus ointment and calcipotriol (calcipotriene) cream can also be used. Intact pustules are rarely seen; in one case, the pustule was subcorneal, with focal spongiform pustulation. Erythematous papules have shown perifollicular neutrophilic and eosinophilic infiltrates. Local ablative measures such as curettage and cautery, carbon dioxide laser, or cryotherapy may be used if surgical excision is unsuitable. It presents with widespread erosions and crusted sterile pustules, leading to scarring alopecia. The condition has a female predominance, and most affected individuals are older than age 65 years; it has also been reported in a 15-year-old boy290 and in infants. Trauma, previous herpes zoster infection, recent cryotherapy, 5-fluorouracil application, topical imiquimod treatment for actinic keratoses,294 topical minoxidil solution,295 radiation therapy, and surgery have all been implicated as predisposing factors. There is prominent pseudoepitheliomatous hyperplasia, which in some areas appears to result from hypertrophy of the follicular infundibulum. Intraepidermal microabscesses are present, and these probably represent the attempted transepidermal elimination of the dermal inflammatory process. Systemic effects, from the absorption of exotoxin, and severe lymphadenitis may develop. The treatment of diphtheria requires the administration of a specific antitoxin as soon as the diagnosis is made and also the use of penicillin or erythromycin. A Histopathology There is necrosis of the epidermis and varying depths of the dermis. The base of the ulcer is composed of necrotic debris, fibrin, and a mixed inflammatory infiltrate. Electronmicroscopy Electron microscopy has confirmed the bacterial nature of erythrasma. It has also shown decreased electron density in keratinized cells, with dissolution of normal keratin fibrils at sites of proliferation of organisms. If there is a heavy growth of organisms on the hairs, clipping followed by the application of a topical antibacterial agent will hasten resolution. As with erythrasma, the topical application of one of the imidazole antifungal agents is usually effective. A Histopathology361,369 Microscopically, the pits appear as multiple crateriform defects in the stratum corneum. In the base and margins of the pits, there are fine filamentous and coccoid organisms that are gram positive and argyrophilic with the methenamine silver stain. It has been suggested that two types of pitted keratolysis can be distinguished histologically. The causative organism was originally designated as Corynebacterium tenuis, but it now seems that at least three species are involved. However, cutaneous lesions do occur quite commonly in meningococcal and gonococcal septicemia; they take the form of a vasculitis (see Chapter 8, p. There are neutrophils in and around the vessels, but the infiltrate is not as heavy as it is in hypersensitivity vasculitis. In pustular lesions of chronic meningococcemia, there are intraepidermal and subepidermal collections of neutrophils. The macrolide antibiotics appear to be more effective than tetracyclines in this group of infections. There is a complex interaction between the organism, the environment, and the host. Patients with hypomorphic mutations of the nuclear factor B essential modulator gene may also have increased susceptibility to mycobacterial disease. Gram-negative intracellular diplococci can usually be found in tissue sections, but they are more easily found in smears made from the purulent exudate on the surface of the lesion. Within these three categories, there are clinicopathological variants that are sometimes given the status of distinct entities; for example, infections by Mycobacterium ulcerans and M. This traditional classification has been disparaged somewhat, and a classification based on the presumed route of infection has been proposed. The last of these three categories can be further subdivided into lupus vulgaris, acute disseminated tuberculosis, and the formation of cutaneous nodules or abscesses. This relatively new system of classification has the advantage of applying to infections with atypical mycobacteria as well as those caused by M.
Order seroflo from india
Alpha 1-antitrypsin deficiency-associated panniculitis: Case report and review of the literature allergy testing your dog order 250 mcg seroflo visa. Panniculitis secondary to extravasation of clarithromycin in a patient with 1-antitrypsin deficiency (phenotype PiZ). Alpha-1-antitrypsin deficiency, associated with panniculitis treated with plasma exchange therapy. Severe ulcerative panniculitis caused by alpha 1-antitrypsin deficiency: Remission induced and maintained with intravenous alpha 1-antitrypsin. Hemorrhagic diathesis associated with benign histiocytic cytophagic panniculitis and systemic histiocytosis. Cutaneous histopathologic, immunohistochemical, and clinical manifestations in patients with hemophagocytic syndrome. Fatal systemic cytophagic histiocytic panniculitis: A histopathologic and immunohistochemical study of multiple organ sites. Panniculitis associated with cutaneous T-cell, lymphoma and cytophagocytic histiocytosis. Histiocytic cytophagic panniculitis:, Molecular evidence for a clonal T-cell disorder. Histiocytic cytophagic panniculitis: A rare late complication of allogeneic bone marrow transplantation. Aggressive subcutaneous panniculitis-like T-cell lymphoma: Complete remission with fludarabine, mitoxantrone and dexamethasone. Immunophenotypic and molecular features, clinical outcomes, treatments, and prognostic factors associated with subcutaneous panniculitis-like T-cell 555. High-dose chemotherapy with autologous blood stem cell transplantation for aggressive subcutaneous panniculitis-like T-cell lymphoma. Subcutaneous panniculitic T-cell lymphoma in children: Response to combination therapy with cyclosporine and chemotherapy. Subcutaneous panniculitis-like T-cell lymphoma in a 26-month-old child with a review of the literature. A case of subcutaneous panniculitis-like T-cell lymphoma with haemophagocytosis developing secondary to chemotherapy. Cytotoxic / subcutaneous panniculitislike T-cell lymphoma: Report of a case with pulmonary involvement unresponsive to therapy. Rimming of adipocytes by neoplastic, lymphocytes: A histopathologic feature not restricted to subcutaneous T-cell lymphoma. Subcutaneous panniculitis-like T-cell lymphoma with vacuolar interface dermatitis resembling lupus erythematosus panniculitis. Fatal subcutaneous panniculitis-like T-cell lymphoma with interface change and dermal mucin, a dead ringer for lupus erythematosus. Lupus profundus, indeterminate lymphocytic lobular panniculitis and subcutaneous T-cell lymphoma: A spectrum of subcuticular T-cell lymphoid dyscrasia. Atypical lymphocytic lobular panniculitis: A clonal subcutaneous T-cell dyscrasia. Subcutaneous fat necrosis after paracentesis: Report of a case in a patient with acute pancreatitis. A fatal case of pancreatic panniculitis presenting in a young patient with systemic lupus. Panniculitis complicating gallstone pancreatitis with subsequent resolution after therapeutic endoscopic retrograde cholangiopancreatography. Pancreatic panniculitis caused by L-asparaginase induced acute panniculitis in a child with acute lymphoblastic leukemia. Association of islet cell carcinoma of the pancreas with subcutaneous fat necrosis. A case of subcutaneous nodular fat necrosis with lipase-secreting acinar cell carcinoma. Lupus erythematosus panniculitis (profundus): Commentary and report on four more cases. Generalized lupus panniculitis and antiphospholipid syndrome in a patient without complement deficiency. Coexistence of acquired localized hypertrichosis and lipoatrophy after lupus panniculitis. Lupus erythematosus panniculitis: A unique subset within the lupus erythematosus spectrum [Abstract]. Panniculitis mimicking lupus erythematosus profundus: A new histopathologic finding in malignant atrophic papulosis (Degos disease). Lupus erythematosus profundus successfully treated with dapsone: Review of the literature. Lupus erythematosus panniculitis (lupus profundus): Clinical, histopathological, and molecular analysis of nine cases. A light and electron microscopical study of membranocystic lesions in a case of lupus erythematosus profundus. Lipomembranous changes and calcification associated with systemic lupus erythematosus. Systemic lupus erythematosus with cytophagic histiocytic panniculitis successfully treated with high-dose glucocorticoids and cyclosporine A. Extensive fat necrosis with lipomembranous changes and calcification in lupus erythematosus panniculitis is not necessarily associated with systemic lupus erythematosus. The clinical spectrum of lipoatrophic panniculitis encompasses connective tissue panniculitis. The findings do not conform precisely: Fibrosing sarcoidal expressions of panniculitis as example. Incidence and risk factors for corticosteroid-induced lipodystrophy: A prospective study. Of mice and men: the road to understanding the complex nature of adipose tissue and lipoatrophy. Novel subtype of congenital generalized lipodystrophy associated with muscular weakness and cervical spine instability. Acquired generalized lipodystrophy (panniculitis variety) triggered by pulmonary tuberculosis. Partial lipodystrophy associated with a type 3 form of membranoproliferative glomerulonephritis. Acquired partial lipodystrophy with C3 hypocomplementemia and antiphospholipid and anticardiolipin antibodies. Annular and semicircular lipoatrophies: Report of three cases and review of the literature. Semicircular lipoatrophy in a child with systemic lupus erythematosus after subcutaneous injections with methotrexate. Nonregressing lipodystrophia centrifugalis abdominalis with angioblastoma (Nakagawa). Lipodystrophia centrifugalis abdominalis infantilis: A possible sequel to Kawasaki disease. Lipodystrophia centrifugalis abdominalis infantilis in a 4-year-old Caucasian girl: Association with partial IgA deficiency and autoantibodies. Local panatrophy with linear distribution: A clinical, ultrastructural and biochemical study. Post-injection involutional lipoatrophy: Ultrastructural evidence for an activated macrophage phenotype and macrophage related involution of adipocytes. Multifocal disseminated lipoatrophy secondary to intravenous corticosteroid administration in a patient with adrenal insufficiency.