25mg phenergan sale
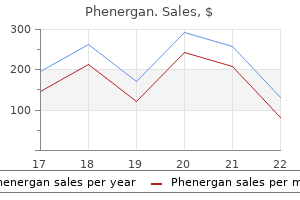
To avoid the surgical morbidity associated with a full axillary lymph node dissection anxiety symptoms night sweats order phenergan with paypal, biopsy of sentinel nodes is often used to assess the presence or absence of metastatic lesions. A sentinel lymph node is defined as "the first node in a regional lymphatic basin that receives lymph flow from the primary tumor. Sentinel node examination has also been used to assess the spread of melanomas, colon cancers, and other tumors. In many cases the regional nodes serve as effective barriers against further dissemination of the tumor, at least for a while. Conceivably, after arrest within the node the cells may be destroyed by a tumor-specific immune response. The immune response to tumor cells or antigens in draining lymph nodes may lead to enlargement (hyperplasia) of the nodes. Thus, enlarged lymph nodes do not always harbor metastases, which can be assessed definitively only by microscopic examination. Note the aggregates of tumor cells within the substance of the node and the dilated lymphatic channel. Tumors do not contain functional lymphatic vessels, but lymphatic vessels located at the margins of invading cancers are apparently sufficient for the lymphatic spread of tumor cells. For example, because carcinomas of the breast usually arise in the upper outer quadrants, they generally disseminate first to the axillary lymph nodes and then to infraclavicular and supraclavicular lymph nodes. Carcinomas of the lung arising in the major respiratory passages metastasize first to perihilar tracheobronchial and mediastinal lymph nodes. Local lymph nodes, however, may be bypassed-so-called skip metastasis- possibly because microscopic metastases are missed or Lymphatic Spread. In general, histologic evidence of penetration of small vessels at the site of the primary neoplasm is an ominous feature associated with hematogenous metastasis. The involved vessels are usually small veins, as arteries, with their thicker walls, are more resistant to penetration. Arterial spread may occur, however, when tumor cells pass through pulmonary capillary beds or pulmonary arteriovenous shunts or when cancers in the lung (primary or metastatic) give rise to tumor emboli. With venous invasion, the blood-borne tumor cells often come to rest in the first capillary bed they encounter. Cancers arising in close proximity to the vertebral column often embolize through the paravertebral plexus; this pathway produces frequent vertebral metastases from carcinomas of the thyroid and prostate. Nonetheless, many observations suggest that the location of the primary tumor and its natural pathways of venous drainage do not wholly explain the observed patterns of metastatic spread, which are often cancer-specific. Renal cell carcinoma often invades the branches of the renal vein and then the renal vein itself, growing in a snakelike fashion up the inferior vena cava until it sometimes reaches the right side of the heart. Similarly, hepatocellular carcinomas often penetrate portal and hepatic radicles and then grow into the main venous channels. Remarkably, such intravenous growth may not be accompanied by widespread metastasis. The distinguishing features of benign and malignant tumors are summarized in Table 7. Having completed our overview of the morphology and behavior of neoplasms, we now discuss the pathogenesis of neoplasia, starting with clues gleaned from studies of the epidemiology of cancer. Carcinomas tend to spread via lymphatics, whereas sarcomas prefer the hematogenous route. Epidemiologic studies have established the causative link between smoking and lung cancer, and comparison of diet and cancer rates in different regions of the world has linked diets high in fat and low in fiber to colon cancer. It is hoped that additional insights into the causes of cancer will be obtained by studies that relate particular environmental, racial (possibly hereditary), and cultural influences to specific neoplasms. The strong association of certain inflammatory and other diseases with cancer also provides clues to its pathogenesis. In the following sections, we discuss the overall incidence of cancer and then review environmental and host factors that influence the predisposition to cancer. Moreover, due to increasing population size and age, cancer cases and cancer-related deaths worldwide are projected to increase to 21. The major organ sites affected and the estimated frequency of cancer deaths in the United States are shown in. Cancers of the lung, female breast, prostate, and colon/rectum constitute more than 50% of cancer diagnoses and cancer deaths in the United States. Most longitudinal data pertaining to cancer incidence come from higher income countries, where age-adjusted death rates (deaths per 100,000 population) for many cancers have changed significantly over the years. In the last 50 years of the 20th century, the age-adjusted cancer death rate increased significantly in both men and women. However, since 1995 the cancer incidence rate in men has been stable, and since 1990 the cancer death rate has decreased by approximately 20%. Similarly, the cancer incidence rate also stabilized in women in 1995, and the cancer death rate has fallen by approximately 10% since 1991. Among men, nearly 80% of the decrease is accounted for by lower death rates from lung, prostate, and colorectal cancers; among women, nearly 60% of the decrease is due to reductions in death rates from breast and colorectal cancers. Decreased use of tobacco products is responsible for the reduction in lung cancer deaths, while improved detection and treatment are responsible for the decrease in death rates for colorectal, female breast, and prostate cancer. The last half-century has also seen a sharp decline in deaths caused by cervical cancer in the United States. This decrease is largely attributable to the Papanicolaou (Pap) smear test, which enables detection of "precursor lesions" (discussed later) and early, curable cancers. Excludes basal cell and squamous cell skin cancers and in situ carcinomas except urinary bladder. Alcohol abuse increases the risk of carcinoma of the oropharynx (excluding lip), larynx, and esophagus and, by the development of alcoholic cirrhosis, hepatocellular carcinoma. Moreover, the risk of cancers in the upper airways and digestive tract imposed by alcohol is increased synergistically when combined with tobacco use. Although the precise dietary factors that affect cancer risk remain a matter of debate, wide geographic variation in the incidences of colorectal carcinoma, prostate carcinoma, and breast carcinoma has been ascribed to differences in diet. Given that the obesity epidemic in the United States is spreading to other parts of the world (Chapter 9), it is concerning that obesity is associated with increased cancer risk. Lifelong cumulative exposure to estrogen stimulation, particularly if unopposed by progesterone, increases the risk of cancers of the breast and endometrium, tissues that are responsive to these hormones. It is likely that some of the geographic variation in breast cancer incidence is related to differing cultural mores that influence the timing and number of pregnancies a woman has during her lifetime. There is no paucity of wellcharacterized environmental carcinogens: they lurk in the ambient environment, in the workplace (Table 7. It appears that almost everything one does to earn a livelihood or for pleasure is fattening, immoral, illegal, or, even worse, carcinogenic! Race is not a discrete biologic variable, but it can define groups at risk for certain cancers. The disparity in cancer mortality rates between Americans who are Caucasian or of African descent persists, but African Americans had the largest decline in cancer mortality during the past decade. People identifying as Hispanic living in the United States have a lower frequency of the most common cancers affecting the Caucasian non-Hispanic population and a higher incidence of cancers of the stomach, liver, uterine cervix, and gallbladder as well as certain leukemias. Environmental Factors Although both genetic and environmental factors contribute, environmental influences are the dominant risk factors for most cancers. One line of evidence supporting this idea comes from longitudinal changes in cancer incidence in the United States. Other evidence is found in the wide geographic variation that exists in the incidence of specific cancers. For example, the most common cancer of men in the United States and in most other higher income countries is prostate cancer, but in other countries or regions, cancers of the liver, stomach, esophagus, bladder, lung, oropharynx, and the immune system rise to the top of the list. Similarly, the incidence of breast cancer is generally much higher in women living in higher income countries than in lower income countries. Although racial predisposition may factor in, it is believed that environmental influences-some known, some not-underlie most of these differences in cancer incidence. Among the best-established environmental factors affecting cancer risk are the following. About 15% of all cancers worldwide are caused directly or indirectly by infectious agents, with the burden of cancers linked to infections being roughly three times higher in the developing world than in the developed world. Specific infectious agents and their associated cancers are discussed later in this chapter. Cigarette smoking is the single most important environmental factor contributing to premature death in the United States. Smoking, particularly of cigarettes, is implicated in cancer of the mouth, pharynx, larynx, esophagus, pancreas, and bladder and, most significantly, in about 90% of lung cancers (Chapter 9).
Syndromes
- What medicines do you take?
- Slurred, irregular speech
- Diabetes
- Infliximab (Remicade)
- Feeling tired
- Bleeding
- Fainting or feeling light-headed
- Urine and fecal urobilinogen
- Feeding problems
Phenergan 25mg on-line
Moreover anxiety symptoms eyesight buy cheap phenergan on-line, cavernous hemangiomas detected by imaging studies may be difficult to distinguish from their malignant counterparts. On histologic examination, the mass is sharply delineated but unencapsulated and composed of large, cavernous blood-filled vascular spaces, separated by connective tissue stroma. They can be locally destructive, but more often are of little clinical significance outside of a cosmetic disfigurement or their vulnerability to traumatic ulceration and bleeding. Brain hemangiomas are problematic, as they can cause symptoms related to compression of adjacent tissue or rupture. Cavernous hemangiomas are one component of von Hippel-Lindau disease (Chapter 28), in which vascular lesions are commonly found in the cerebellum, brain stem, retina, pancreas, and liver. Roughly a quarter of lesions develop after trauma, reaching a size of 1 to 2 cm within a few weeks. Pregnancy tumor (granuloma gravidarum) is a pyogenic granuloma that occurs infrequently (1% of patients) in the gingiva of pregnant women. These lesions may spontaneously regress (especially after pregnancy) or undergo fibrosis, but occasionally require surgical excision. Histologically, lymphangiomas exhibit networks of endothelium-lined spaces that can be distinguished from capillary channels by lymphatic endothelial markers. Cavernous lymphangiomas can occasionally be enormous (up to 15 cm), filling the axilla or producing gross deformities about the neck; cavernous lymphangiomas of the neck are common in Turner syndrome. They are most commonly found in the distal portion of the digits, especially under the fingernails. Although persistent, the tumors are typically asymptomatic and remain localized to the skin and subcutaneous tissue. Inset, Modified silver (Warthin-Starry) stain demonstrates clusters of tangled bacilli (black). A particularly severe form, with prominent lymph node and visceral involvement, occurs in prepubertal children; the prognosis is poor, with almost 100% mortality within 3 years. Lesions can regress as immunosuppression is reduced, but at the risk of organ rejection. Scattered between the vascular channels are extravasated erythrocytes, hemosiderin-laden macrophages, and other mononuclear inflammatory cells. These lesions are composed of sheets of plump, proliferating spindle cells, mostly in the dermis or subcutaneous tissues. Marked hemorrhage, hemosiderin pigment, and mononuclear inflammation are present; mitotic figures are common, as are round, pink, cytoplasmic globules representing degenerating erythrocytes within phagolysosomes. Acquired somatic mutations in the cells of origin also contribute to tumor development and progression. All of these agents have long latencies between initial exposure and eventual tumor development. Angiosarcomas are locally invasive and can readily metastasize, with 5-year survival rates of approximately 30%. Hemangioendotheliomas comprise a spectrum of borderline vascular neoplasms with clinical behaviors intermediate between benign, welldifferentiated hemangiomas and frankly anaplastic angiosarcomas. Epithelioid hemangioendothelioma is a tumor of adults occurring around medium- and large-sized veins. Welldefined vascular channels are inconspicuous, and neoplastic cells are plump and often cuboidal (resembling epithelial cells). The clinical behavior is extremely variable; most are cured by excision, but up to 40% recur, 20% to 30% eventually metastasize, and 15% of patients will die of their tumor. More advanced lesions are large, fleshy masses of red-tan to gray-white tissue with margins blurring imperceptibly into surrounding structures. Older adults, males and females, are more commonly affected; angiosarcomas occur at any site, but most often involve skin, soft tissue, breast, and liver. Angiosarcomas can also arise in the setting of lymphedema, classically in the ipsilateral upper extremity several years after radical mastectomy for breast cancer. Angiosarcomas have also been induced by radiation and are rarely associated with prolonged insertion of foreign material. Hepatic angiosarcomas are associated with a variety of carcinogenic exposures including arsenic. Malignant tumors are more often solid and cellular, exhibit cytologic atypia, and lack well-defined vessels. Endovascular Stenting Arterial stenoses (especially those in coronary arteries) can be dilated by transiently inflating a balloon catheter to pressures sufficient to rupture the occluding plaque (balloon angioplasty). Although most patients improve symptomatically following angioplasty alone, abrupt reclosure frequently occurs due to luminal compression caused by angioplastyinduced vascular dissection, by vessel wall spasm, or by thrombosis. Thus more than 95% of endovascular coronary procedures now involve both angioplasty and concurrent coronary stent placement. They provide a larger and more regular lumen, "tack down" the intimal flaps and dissections that occur during angioplasty, and mechanically limit vascular spasm. Nevertheless, due to endothelial injury, thrombosis is an important immediate post-stenting complication, and patients must receive potent antithrombotic agents (primarily platelet antagonists) to prevent acute catastrophic thrombotic occlusions. The long-term success of angioplasty is limited by the development of proliferative in-stent restenosis. The newest generation of drug-eluting stents is designed to avoid this complication by leaching antiproliferative drugs. Although the duration of drug elution is short (on the order of days to weeks), these drug-eluting stents nevertheless reduce the incidence of restenosis at 1 year by 50% to 80%. However, because of the antiproliferative effect of the drug-eluting stents, the time to reendothelialization is prolonged, and patients require extended courses of anticoagulation to prevent stent thrombosis. Vascular Replacement Synthetic or autologous vascular grafts can be used to replace damaged vessels or bypass diseased arteries. Large-bore (12- to 18-mm) synthetic conduits function well in high-flow locations such as the aorta; unfortunately, small-diameter artificial grafts (8 mm in diameter) generally fail as a result of early thrombosis or late intimal hyperplasia, the latter at the junction of the graft with the native vasculature. The long-term patency of saphenous vein grafts averages only 50% at 10 years; grafts occlude due to thrombosis (typically early), intimal thickening (months to years postoperatively), and vein graft atherosclerosis- sometimes with superimposed plaque rupture, thrombosis, or aneurysms. By contrast, more than 90% of internal mammary artery grafts, which can be used only to bypass the left anterior descending artery, are patent at 10 years. In A Brief History of Blood and Lymphatic Vessels, Cham, Switzerland, 2017, Springer. Jinnouchi H, Guo L, Sakamoto A et al: Diversity of macrophage phenotypes and responses in atherosclerosis, Cell Mol Life Sci 2019. Jaiswal S et al: Clonal hematopoiesis and risk of atherosclerotic cardiovascular disease, N Engl J Med 377:111, 2017. Ridker P: From C-reactive protein to interleukin-6 to interleukin-1: moving upstream to identify novel targets for atheroprotection, Circ Res 118:145, 2016. Pathology of Vascular Intervention Vasculitis Jennette J, Falk R: Nosology of primary vasculitis, Curr Opin Rheumatol 19:10, 2007. In utero, the heart and vasculature are the first fully functional organ system (at roughly 8 weeks of gestation). Without a vascular supply and a beating heart, further development cannot occur and fetal demise is inevitable. In the United States alone, cardiovascular disease accounts for roughly 1 in 4 of all deaths, totaling about 610,000 individuals each year-greater than the number of deaths caused by all forms of cancer combined. This chapter begins with a brief review of the normal heart because most cardiac diseases manifest as structural and/or functional changes in one or more cardiac components. The chapter concludes with a few comments about pericardial diseases and cardiac neoplasms, as well as cardiac transplantation and devices. Increased heart weight or ventricular thickness indicates hypertrophy, and an enlarged chamber size implies dilation; both reflect compensatory changes in response to volume and/or pressure overloads (see later). Increased cardiac weight or size (or both)-resulting from hypertrophy and/or dilation-is called cardiomegaly. Because they are thin enough to be nourished by diffusion from the blood, normal leaflets and cusps have only scant blood vessels limited to the proximal portion of the valve. Conduction System Coordinated contraction of the cardiac muscle depends on the initiation and rapid propagation of electrical impulses- accomplished through specialized myocytes in the conduction system. However, if nodal tissues become dysfunctional, other cells in the conduction system can take over, generating, for example, a junctional escape rhythm (usually at a much slower rhythm).
Purchase phenergan 25 mg overnight delivery
The clinical significance is similar to that of fibrinous or suppurative pericarditis anxiety emoji phenergan 25 mg mastercard. In other cases, fibrosis in the form of meshlike stringy adhesions can largely obliterate the virtual space in the pericardial sac (adhesive pericarditis); in most instances, this has no effect on cardiac function. The pericardial sac is obliterated, and adherence of the external aspect of the parietal layer to surrounding structures strains cardiac function. With each systolic contraction, the heart pulls not only against the parietal pericardium but also against the attached surrounding structures. Systolic retraction of the rib cage and diaphragm and pulsus paradoxus may be observed. The increased workload occasionally causes significant cardiac hypertrophy and dilation. The fibrous scar can be up to 1 centimeter in thickness, obliterating the pericardial space and sometimes calcifying; in extreme cases, it can resemble a plaster mold (concretio cordis). Because of the dense enclosing scar, cardiac hypertrophy and dilation Tumors of the heart cannot occur. Cardiac output may be reduced at rest, but more importantly the heart has little if any capacity to increase its output in response to increased systemic demands. Signs of constrictive pericarditis include distant or muffled heart sounds, elevated jugular venous pressure, and peripheral edema. Treatment consists of surgical resection of the shell of constricting fibrous tissue (pericardiectomy). Myxomas range from small (<1 cm) to large (10 cm) and can be sessile or pedunculated lesions. They vary from globular hard masses mottled with hemorrhage to soft, translucent, papillary, or villous lesions having a gelatinous appearance. The pedunculated form is often sufficiently mobile to move during systole into the atrioventricular valve opening, causing intermittent obstruction that may be position-dependent. Histologically, myxomas are composed of stellate or globular myxoma cells embedded within an abundant acid mucopolysaccharide ground substance. The five most common tumors have no malignant potential and account for almost 90% of all primary heart tumors. In descending order of frequency (combined pediatric and adult populations), these are myxomas, fibromas, lipomas, papillary fibroelastomas, and rhabdomyomas. These and other sarcomas of the heart are not clinically or morphologically distinctive from sarcomas arising in other locations. Fibromas and lipomas resemble their counterparts elsewhere; only the myxomas, papillary fibroelastomas, and rhabdomyomas merit further mention here. About 90% of myxomas arise in the atria, with a left-to-right ratio of approximately 4:1. The major clinical manifestations are due to valvular "ball-valve" obstruction, embolization, or a syndrome of constitutional symptoms, such as fever and malaise. Sometimes fragmentation and systemic embolization calls attention to these lesions. Constitutional symptoms are probably due to the elaboration by some myxomas of the cytokine interleukin-6, a major mediator of the acute-phase response. Surgical removal is usually curative; rarely, presumably with incomplete excision, the neoplasm can recur months to years later. Clonal cytogenetic abnormalities have been reported, suggesting that fibroelastomas are benign neoplasms. They resemble the much smaller, usually trivial, Lambl excrescences that project from sites of valve apposition. Each lesion, typically 1 to 2 cm in diameter, consists of a distinctive cluster of hairlike projections up to 1 cm in length. Histologically, the projections are covered by a surface endothelium surrounding a core of myxoid connective tissue with abundant mucopolysaccharide matrix and elastic fibers. Rhabdomyomas are the most frequent primary tumor of the pediatric heart; they are commonly discovered in the first years of life during an evaluation for a valve or other flow obstruction. Because rhabdomyomas often regress spontaneously, they may be considered as hamartomas rather than true neoplasms. These donor-specific antibodies cause allograft compromise by inducing endothelial cell injury leading to microvascular damage with thrombosis. Antibodymediated rejection shows mild perivascular edema and scattered adherent intravascular inflammatory cells; it is often confirmed by immunohistochemical staining for complement fragment C4d, a long-lived catabolite that is released during complement cascade activation. Allograft vasculopathy is the single most important long-term limitation for cardiac transplantation. It is a late, progressive, diffusely stenosing intimal proliferation in allograft blood vessels, predominantly in the coronary arteries. Within 5 years of transplantation, 50% of patients develop significant allograft vasculopathy, and virtually all patients have lesions within 10 years. Despite these problems, the overall outlook is reasonably promising; the 1-year survival is 90%, and 5-year survival is greater than 70%. They are usually multiple and involve the ventricles preferentially, protruding into the lumen. Microscopically, they are composed of bizarre, markedly enlarged myocytes with large collections of glycogen. Routine histologic processing removes the glycogen and artifactually reduces the abundant cytoplasm to thin strands that stretch from the nucleus to the surface membrane, an appearance referred to as "spider" cells. Metastatic Neoplasms Metastatic tumors to the heart occur in roughly 5% of patients dying of cancer; the most frequent are lung and breast carcinomas, melanomas, leukemias, and lymphomas. Metastases can reach the heart and pericardium by retrograde lymphatic extension from the mediastinum (mostly carcinomas), by hematogenous seeding (many tumors), by direct contiguous extension (of intrathoracic tumors), or by venous extension (tumors of the kidney or liver). Clinical symptoms are most often associated with pericardial spread, which can cause symptomatic pericardial effusions or a mass-effect that is sufficient to restrict cardiac filling. Myocardial metastases are usually clinically silent or have nonspecific features, such as a generalized defect in ventricular contractility or compliance; occasionally they may cause arrhythmias. Bronchogenic carcinoma or malignant lymphoma can infiltrate the mediastinum extensively, causing encasement, compression, or invasion of the superior vena cava with resultant obstruction to blood coming from the head and upper extremities (superior vena cava syndrome). Renal cell carcinoma often invades the renal vein and can grow as a continuous column of tumor up the inferior vena cava lumen and into the right atrium, blocking venous return to the heart. Of the major complications, allograft rejection is the primary problem requiring surveillance; routine endomyocardial biopsy is the only reliable means of diagnosing acute cardiac rejection before substantial myocardial damage has occurred and at a stage that is reversible in the majority of instances. Classic cellular rejection is characterized by interstitial lymphocytic inflammation with associated myocyte damage; the histology resembles myocarditis. Thus, stents are now routinely deployed to maintain vascular patency (especially in the coronary arteries; Chapter 11), and endovascular conduit repairs are common approaches for treating abdominal aortic aneurysms. Implantable pacemakers and cardioverter defibrillators are indispensable for patients with cardiac rhythm disorders, and transcatheter aortic valve replacement (discussed earlier) has broadened the population that can benefit from valve replacement. Although impressive, these various devices are not without (somewhat predictable) risk. Mechanical failure can occur with any device, including strut fracture in stents, or lead fracture in pacing devices. The internal elastic lamina (arrow) and media are intact (Movat pentachrome stain, elastin black). Cui M, Wang Z, Bassel-Duby R et al: Genetic and epigenetic regulation of cardiomyocytes in development, regeneration and disease, Development 145:24, 2018.
Purchase 25 mg phenergan mastercard
Voluntary adoption introduces a confounding variable into pharmacologic studies which is challenging but essential to account for anxiety symptoms scale generic 25 mg phenergan amex. Global epidemiology of nonalcoholic fatty liver disease: metaanalytic assessment of prevalence, incidence, and outcomes. Biochemical analysis of hepatic lipid in alcoholic and diabetic and control subjects. Prediction of liver disease by alcohol intake, sex and age: a prospective population study. Nonalcoholic fatty liver disease: an assessment of variability in pathological interpretation. Ballooned hepatocytes in steatohepatitis: the value of keratin immunohistochemistry for diagnosis. Nonalcoholic steatohepatitis: a proposal for grading and staging the histologic lesions. The natural history of nonalcoholic steatohepatitis: a follow-up study of forty-two patients for up to 21 years. Prevalence of obesity and diabetes in patients with cryptogenic cirrhosis: a case-control study. Nonalcoholic fatty liver disease: An underrecognized cause of cryptogenic cirrhosis. The spectrum expanded: cryptogenic cirrhosis and the natural history of nonalcoholic fatty liver disease. Cryptogenic liver disease in the United States: further evidence for non-A, non-B, non-C hepatitis. Cryptogenic cirrhosis: clinical-biochemical comparison with alcoholic and viral etiologies. Body composition in nonalcoholic cirrhosis: the effect of disease etiology and severity on nutritional compartments. Evidence that hepatic uptake of gluconeogenic precursors and of free fatty acids depends on effective hepatic flow. Cryptogenic cirrhosis: clinicopathologic findings at and after liver transplantation. Fatty infiltration of the liver: analysis of prevalence, radiological and clinical features and influence on patient management. Portal architecture: a differential guide to fatty infiltration of the liver on computerized tomography. Hepatic subcapsular steatosis in a patient with insulin dependent diabetes receiving dialysis. Independent predictors of liver fibrosis in patients with nonalcoholic steatohepatitis. Predictors of nonalcoholic steatohepatitis and advanced fibrosis in morbidly obese patients. Non-alcoholic fatty liver disease and insulin resistance: importance of risk factors and histological spectrum. The clinical features, diagnosis, and natural history of nonalcoholic fatty liver disease. Visceral and liver fat are independent predictors of metabolic risk factors in men. Nonalcoholic steatohepatitis, insulin resistance and metabolic syndrome: Further evidence for an etiologic association. Cognitive lifetime drinking history in nonalcoholic fatty liver disease: some cases may be alcohol related. Nonalcoholic fatty liver disease: Predictors of nonalcoholic steatohepatitis and liver fibrosis in the severely obese. Effects of moderate alcohol intake on fasting insulin and glucose concentrations and insulin sensitivity in postmenopausal women. Effects of light-to-moderate alcohol consumption on steatosis and steatohepatitis in severely obese patients. Clinicopathological comparison with alcoholic hepatitis in ambulatory and hospitalized patients. The use of protein tyrosine phosphatase 1B and insulin receptor immunostains to differentiate nonalcoholic from alcoholic steatohepatitis in liver biopsy specimens. Insulin resistance in cirrhosis: prolonged reduction of hyperinsulinemia normalizes insulin sensitivity. Reduced mitochondrial adenosine triphosphate synthesis in skeletal muscle in patients with Child-Pugh class B and C cirrhosis. An assessment of the role of liver biopsies in asymptomatic patients with chronic liver test abnormalities. The prevalence and etiology of elevated aminotransferase levels in the United States. Prevalence of and risk factors for nonalcoholic fatty liver disease: the Dionysos nutrition and liver study. Dissociation between intrahepatic triglyceride content and insulin resistance in familial hypobetalipoproteinemia. Body composition, visceral fat, leptin, and insulin resistance in Asian Indian men. The obese without cardiometabolic risk factor clustering and the normal weight with cardiometabolic risk factor clustering. Clinical and metabolic characterization of lean Caucasian subjects with non-alcoholic fatty liver. Association between metabolic syndrome and liver histology among children with nonalcoholic fatty liver disease. Obesity, insulin resistance, and other clinicopathological correlates of pediatric nonalcoholic fatty liver disease. Influence of gender, race, and ethnicity on suspected fatty liver in obese adolescents. Concurrence of histological features of steatohepatitis with other forms of chronic liver disease. Liver microsomal triglyceride transfer protein is involved in hepatitis C liver steatosis. Relationship between steatosis, inflammation, and fibrosis in chronic hepatitis C: a meta-analysis of individual patient data. Factors associated with the presence of nonalcoholic steatohepatitis in patients with chronic hepatitis C. Oxidative stress and steatosis are cofactors of liver injury in primary biliary cirrhosis. Racial and ethnic distribution of nonalcoholic fatty liver in persons with newly diagnosed chronic liver disease. Racial differences in visceral adipose tissue but not anthropometric markers of healthrelated variables. Ninety patients with nonalcoholic steatohepatitis: insulin resistance, familial tendency, and severity of disease. Familial aggregation of insulin resistance in first-degree relatives of patients with nonalcoholic fatty liver disease. Insulin resistance and hypertriglyceridemia in nondiabetic relatives of patients with noninsulindependent diabetes mellitus. Impaired mitochondrial activity in the insulin-resistant offspring of diabetes with type 2 diabetes. The rs2294918 E434K variant modulates patatin-like phospholipase domain-containing 3 expression and liver damage. Transmembrane 6 superfamily member 2 gene variant disentangles nonalcoholic steatohepatitis from cardiovascular disease. Risk of severe liver disease in nonalcoholic fatty liver disease with normal aminotransferase levels: a role for insulin resistance and diabetes.
Cheap phenergan online american express
For instance anxiety symptoms jelly legs buy 25mg phenergan overnight delivery, antiretroviral agents can aggravate latent chronic hepatitis C and B by restoring an efficient immune system and by modifying immunotolerance [1,6,7,148]. Extrahepatic diseases Extrahepatic diseases may also contribute to drug hepatotoxicity. Main drugs responsible for liver injury the recent analysis of data collected in Liver Tox indicates that the top 10 drugs are mostly anti-infectious drugs [8]. The most common cause is amoxicillinclavulanate [8], as observed in the European registries [28,31]. Other drugs include isoniazid, nitrofurantoin, trimethoprim-sulfamethoxazole, minocycline, cephalexin, azithromycin, ciprofloxacin, diclofenac, and levofloxacin [8]. The most common drugs are the antimicrobial, agents representing 33% of the drugs. The top five drugs have been determined in three prospective registries [4,28,31]. The relative frequency varies according to country when there is a specifically high prevalence of some diseases. The main drugs reported to cause acute hepatocellular or cholestatic and/or mixed liver injury are listed in Boxes 27. Malignancy and immunosuppression Azathioprine, cisplatin, cytarabine, etoposide, fluorouracil, interleukin 2, 6-mercaptopurine, mitomycin, tamoxifen, 6-thioguanine Cardiovascular diseases Acenocoumarol, amiodarone, captopril, dihydralazine, diltiazem, disopyramide, enalapril, flecaine, mexiletine, nifedipine, papaverine, propafenone, quinidine, rivaroxaban, ticlopidine, verapamil Gastroenterology Cimetidine, mesalazine, penicillamine, ranitidine, sulfasalazine Endocrinology, metabolic diseases Atorvastatin, carbimazole, clofibrate, fenofibrate, fluvastatin, glibenclamide, pravastatin, tamoxifen, troglitazone Infectious and parasitic diseases Abacavir, albendazole, amoxicillin, amoxicillin-clavulanate, cephalexin, cephalosporins, ciprofloxacin, chloramphenicol, clarithromycin, cloxacillin, cotrimoxazole, dapsone, didanosine, erythromycin and its derivatives, ethambutol, itraconazole, josamycin, ketoconazole, metronidazole, minocycline, nitrofurantoin, norfloxacin, ofloxacin, oxacillin, penicillin, rifampin, ritonavir, roxithromycin, stavudine, sulfonamides, terbinafine, tetracycline, thiabendazole, voriconazole, zidovudine Neuropsychiatric disorders Amitriptyline, carbamazepine, chlordiazepoxide, chlorpromazine and other phenothiazines, clomipramine, desipramine, diazepam, dosulepin, haloperidol, imipramine, iproniazid, lamotrigine, mianserin, phenobarbital, phenytoin, tianeptine, trazodone, triazolam, valproic acid, zimelidine Rheumatoid diseases, gout, and pain killers Allopurinol, baclofen, dextropropoxyphene, diclofenac, diflunisal, gold salts, ibuprofen, ketoprofen, naproxen, nimesulide, penicillamine, phenylbutazone, piroxicam, probenecid, sulfasalazine, tiaprofenic acid Dermatology Etretinate, isotretinoin, minoxidil Hormonal steroids Estrogens, oral contraceptives, androgens Box 27. The main drugs reported to cause chronic hepatitis and/or cirrhosis are listed in Box 27. The clinicobiological pattern is usually that of cholestatic or mixed liver injury [88,90,170]. Only histological examination enables the demonstration of small bile duct lesions [88,90,170]. Allopurinol Amiodarone Amoxicillin-clavulanate Aprindine Aspirin Azathioprine Carbamazepine Carbimazole Carbutamide Cephalexin Chlorpromazine Clindamycin Clofibrate Cotrimoxazole Cyclofenil Dapsone Dapsone Diazepam Diclofenac Dicloxacillin Difebarbamate Diflunisal Diltiazem Disopyramide Enflurane Estroprogestatives Feprazone Flucloxacillin Fluconazole Flumequine Glibenclamide Glyburide Gold salts Halothane Hydralazine Isoniazid Ketoconazole Lovastatin Mesalazine Methimazole Methotrexate Methyldopa Minocycline Naproxen Nitrofurantoin Nomifensine Ofloxacin Oxacillin Oxyphenbutazone Papaverine Penicillin Penicillamine Perhexiline Phenazone Phenindione Phenprocoumon Phenylbutazone Phenytoin Piroxicam Procainamide Procarbazine Quinidine Quinine Ranitidine Sulfadiazine Sulfadimethoxine Sulfadoxine Sulfamethoxazole Sulfanilamide Sulfathiazole Sulfasalazine Tacrine Ticlopidine Tocainide Tolbutamide Troglitazone Box 27. The main agents reported to cause vascular lesions of the liver are listed in Box 27. Despite a clinicopathological picture similar to primary biliary cholangitis, the clinical course of drug-induced prolonged cholestasis is overall much better [90,92,93,170]. The main drugs reported to cause acute and chronic cholangitis are listed in Box 27. Benign and malignant tumors There are few drugs that have been established to cause liver tumors. Acepromazine Ajmaline Allopurinol Amitriptyline Amoxicillin-clavulanate Ampicillin Azathioprine Barbiturate Candesartan cilexetil Carbamazepine Carbutamide Cefoperazone Chlorothiazide Chlorpromazine Chlorpropamide Cimetidine Ciprofloxacin Clometacin Cyamemazine Cyproheptadine Dantrolene Diazepam Difetarsone Doxycycline Erythromycin + chlorpropamide Etretinate Fenofibrate Flucloxacillin Glibenclamide Gold salts Haloperidol Hydralazine Imipramine Interleukin-2 Methahexamide Methyltestosterone Norandrostenolone Penicillamine Phenylbutazone Phenytoin Prochlorperazine Propoxyphene (dextropropoxyphene) Ramipril Rosiglitazone Sulindac Tenoxicam Terbinafine Tetracycline Thiabendazole Ticlopidine Tiopronin Tolbutamide Trimethoprim-sulfamethoxazole Troleandomycin Xenylamine Box 27. The increasing attraction of herbal medicines is partly explained by the return to natural products occurring along with the ecological movement in industrialized countries [173]. The enhanced use of herbal medicines may be also related to the limited efficacy or important side effects of conventional treatments for various chronic diseases [173]. Several studies focused on the use of herbal medicines in chronic hepatitis C in occidental countries are particularly demonstrative of this [166,175]. A prospective inquiry carried out in France, based on outpatients seen for chronic liver diseases, has revealed that there was herbal medicine intake for at least one month in 30% of patients with hepatitis C [176]. Patients may find these products in various stores, some of them specializing in herbal products but also in pharmacy stores. Furthermore, herbal medicines may produce interactions with liver drug metabolizing enzymes [177]. In part to avoid these side effects, utilization of "natural medicine" is increasingly being controlled in many countries. Marketing authorization has been given for plants considered efficient and innocuous. Hepatotoxicity of herbal remedies is particularly difficult to demonstrate [23,173]because of the usual difficulties in assessing a relationship between an adverse event and the intake of a drug largely caused by the absence of clinical specificity [173]. There may be additional difficulties because of the frequency ofself-medication and the reputation of safety so that patients often forget to mention herbal medicine ingestion to the physician [173]. In addition, there are specific risks contributing to the hepatotoxicity of herbal remedies [173]: misidentification of the plant, selection of the wrong part of the medicinal plant, inadequate storage modifying the native product, adulteration during processing, and mislabeling of the final product [173]. Another instance is Herbalife hepatotoxicity, reported in Israel and Switzerland in 2007 [179,180]. Interestingly, it seems that the complex composition of the products marketed under this brand name in these two countries was not exactly the same [179,180]. Another difficulty is that the real composition of the herbal preparation may remain unclear [23,173]. A safe herbal product may be contaminated by a toxic compound leading to hepatotoxicity. This may result from adulteration with heavy metals, pesticides, herbicides, microorganisms, and even classical pharmaceutical products [23,173]. A recent illustration is a product marketed in Scandinavian countries under the brand name Fortodol, normally containing Curcuma longa (turmeric) as a gentle pain-killer [181,182]. It turned out that it also contained nimesulide, a nonsteroidal anti-inflammatory compound, well documented as causing acute liver injury [181,182]. The degree of evidence of toxicity is variable, as for classical pharmaceutical agents. Herbal medicines with the highest level of evidence of hepatotoxicity are plants containing pyrrolizidine alkaloids, germander (Teucrium chamaedris), Atractylis gummifera, plants containing pennyroyal oil (Mentha pulegium, Hedeoma pulegioides), greater celandine (Chelidonium majus), kava-kava (Piper methysticum), black cohosh (Actaea racemosa), and several Asian medicinal preparations (Table 27. Pyrrolizidine alkaloids are a remarkable illustration of the difficulties encountered with herbal medicine hepatotoxicity and the particular need to develop biomarkers to identify the problem. The main species implicated are Heliotropium, Senecio, Crotalaria [23,173], and Symphytum (comfrey) and, more recently, Gynura segetum [23,67,184]. Pyrrolizidine poisoning is endemic in areas such as Africa and Jamaica, where toxic alkaloids are ingested as infusions, herbal teas or decoctions, or used as an enema [23,173]. Contamination of flour by plants containing pyrrolizidine alkaloids has also caused epidemic intoxications in India and Afghanistan [173].
Rusmary (Rosemary). Phenergan.
- Causing abortions.
- How does Rosemary work?
- Hair loss, in combination with thyme, lavender, and cedarwood.
- Dosing considerations for Rosemary.
- Gas (flatulence), indigestion, increasing menstrual flow, gout, cough, headache, liver and gallbladder problems, high blood pressure, toothache, eczema, joint or muscle pain, and other conditions.
- What is Rosemary?
- What other names is Rosemary known by?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96191
Safe 25mg phenergan
Antibody levels and protection after hepatitis B vaccination: results of a 15-year followup anxiety symptoms vomiting generic 25 mg phenergan free shipping. Long-term entecavir therapy results in the reversal of fibrosis/cirrhosis and continued histological improvement in patients with chronic hepatitis B. Meta-analysis: Treatment of hepatitis B infection reduces risk of hepatocellular carcinoma. Meta-analysis: the effect of interferon on development of hepatocellular carcinoma in patients with chronic hepatitis B virus infection. Interferon and prevention of hepatocellular carcinoma in viral cirrhosis: an evidencebased approach. Long-term effect of interferon treatment on the progression of chronic hepatitis B: Bayesian metaanalysis and meta-regression. Meta-analysis: the impact of oral anti-viral agents on the incidence of hepatocellular carcinoma in chronic hepatitis B. Incidence of hepatocellular carcinoma in chronic hepatitis B patients receiving nucleos(t)ide therapy: a systematic review. Long-term entecavir treatment reduces hepatocellular carcinoma incidence in patients with hepatitis B virus infection. Universal hepatitis B vaccination in Taiwan and the incidence of hepatocellular carcinoma in children. Long-term efficacy of continuing hepatitis B vaccination in infancy in two Gambian villages. Changes of hepatitis B surface antigen variants in carrier children before and after universal vaccination in Taiwan. Effectiveness of hepatitis b vaccination in babies born to hepatitis b surface antigen-positive mothers in italy. Vaccination of chronic hepatitis B virus carriers with preS2/S envelope protein is not associated with the emergence of envelope escape mutants. Licensed recombinant hepatitis B vaccines protect chimpanzees against infection with the prototype surface gene mutant of hepatitis B virus. Central-nervous-system demyelination after immunisation with recombinant hepatitis B vaccine. Geographic distribution and genetic variability of hepatitis delta virus genotype I. Characterization and phylogenetic analysis of a novel hepatitis D virus strain discovered by restriction fragment length polymorphism analysis. Oral prenylation inhibition with lonafarnib in chronic hepatitis D infection: a proof-of-concept randomised, double-blind, placebo-controlled phase 2A trial. Diagnosis of chronic hepatitis C relies on testing patients with sensitive and specific serologic and virologic assays. Combinations of different classes of direct-acting antiviral agents can cure virtually all patients with chronic hepatitis C. This led to the description of a new disease entity termed "nonA, non-B" hepatitis, now known as "hepatitis C," and prompted a fierce search for a new, previously unrecognized hepatitis virus. The virion is spherical in shape but highly heterogeneous in size, varying from 40 to 100 nm in diameter, with spike-like surface projections. Host-encoded apolipoprotein E (ApoE) and ApoB are intimately associated with the virion, and may partially mask the envelope glycoproteins E1 and E2 on the surface of the particle [9,10]. Genotype 3 represents a substantial proportion of infections in parts of Europe, India, and Pakistan and genotype 4 is most prevalent in Egypt. Structural proteins present in the virion the N-terminus of the polyprotein is proteolytically processed by the host cell signal peptidase to produce a series of structural proteins. Core has been suggested to interact with a wide array of host cell proteins, potentially impacting cell signaling pathways, transcription, apoptosis, lipid metabolism, immunomodulation, oxidative stress, cell cycle regulation, and carcinogenesis. The biological relevance of many of these putative interactions is uncertain, as most have been identified only in protein overexpression studies. The two envelope glycoproteins, E1 and E2, are also processed from the polyprotein by cellular signal peptidase and are displayed on the surface of the virion. They function both in the attachment of virus to host cells in the earliest stages of virus infection, and in the membrane fusion event that comprises virus entry, and are also the primary target of neutralizing antiviral antibodies. The C-terminal domains of E1 and E2 contain endoplasmic reticulum retention signals, while the ectodomains are highly glycosylated; approximately 50% of their mass in the virion comprises N-linked glycans [31]. The glycoproteins are embedded in the viral envelope as noncovalent heterodimers [32]. It is essential for infectivity of the virus in chimpanzees [36] and it plays a crucial role in assembly and release of infectious virions from infected cells by protecting nascent viral particles from an acidic environment [35,37]. It is a membrane-bound protein that is cleaved from the polyprotein at its N-terminus by signal Chapter 25: Hepatitis C 631 peptidase. It has multiple key functions in the virus life cycle, but remains poorly understood and without a fully defined structure even after decades of study. It is a phosphoprotein with its phosphorylation status likely to regulate various aspects of genome replication and virus assembly [53,54]. The molecule is composed of three distinct domains that are separated by segments of the protein that are relatively disordered. High-resolution X-ray crystallography models [56,57] suggest this domain exists as a dimer that associates with lipid bilayers in membranebound replicase complexes. It has a error rate with a strong preference for G: U/U: G mismatches and a mutational bias in favor of transitions vs. However, cell culture isolation of patient-derived viruses remains a technical challenge. The nascent polyprotein is cotranslationally processed by cellular and viral proteases, as described earlier, giving rise to the nonstructural and structural viral proteins described in the preceding section. The membranes of the membranous web are relatively resistant to detergents and enriched in cholesterol and sphingolipids. Viral entry the first step in replication is the entry of virus into hepatocytes [76]. The secretion process involves multiple host cell components [88], and is facilitated by the small viral ion channel protein p7 [35]. This unfavorable genetic polymorphism is found more frequently in African American people than in individuals of European descent, explaining in part racial differences in interferon treatment response. Newer agents, however, are showing increasing potential for pan-genotypic coverage. Host-targeting antivirals represent an alternative approach that potentially avoids resistance and achieves pan-genotypic coverage. Although the substrate-binding cleft of the protease is unusually broad and shallow, compounds that mimic the structure of this peptide sequence have substantial inhibitory activity. Peptidomimetic compounds fall into two general classes: linear peptidomimetics, which were the first to achieve regulatory approval, and macrocyclic compounds that contain links between residue side-chains. As with many smallmolecule antivirals, protease inhibitors generally present a relatively low barrier to resistance, with resistant virus potentially emerging rapidly during monotherapy [135]. Enzymes are always preferred targets for development of smallmolecule antivirals, as it is usually possible to express the enzymatic activities in vitro under highly controlled conditions, and to define the molecular structure of the active site at an atomic level of resolution. This allows for simplified screening of compound libraries as well as structure-guided drug design. Sofosbuvir is a prodrug that undergoes progressive phosphorylation by cellular kinases to mono-, di-, and triphosphate forms following its uptake into hepatocytes. They bind into one of four discrete sites on the surface of the polymerase that are variably distanced from the active site. In contrast, inhibition of virus assembly is immediate and profound resulting in potent reductions in the release of new virus. Most work in humans is done either retrospectively or in incidental patients who present with symptomatic acute infection or with needlestick injuries. Their responses are typically characterized by specific proliferation and/or cytokine production following incubation with recombinant viral proteins or overlapping peptides. Differential cytokine production underpins the specific types of T helper (Th)-induced immune responses. Proinflammatory cytokines have been correlated with severity of liver fibrosis [186,187], implicating both antigenspecific and independent mechanisms of hepatocellular injury.
Order generic phenergan
Drugs can also inhibit transporters that do not transport bile acids directly anxiety symptoms children order generic phenergan on line, but still play a role in bile acid homeostasis. It mediates the biliary secretion of phosphatidylcholine, which is essential for the formation of phospholipid/bile acid/cholesterol micelles which encase bile acids and prevent their direct contact with cell membranes [22]. Drugs may also impact transporter function by impairing transporter trafficking to the plasma membrane. Phosphatidylserine flipping increases sphingomyelin content in the canalicular membrane which is important for protecting the membrane from detergents such as bile acids. As a result, it has been hypothesized to act as a gatekeeper, preventing hepatic bile acid overload. Another mechanism by which drugs have been shown to alter bile acid homeostasis is by impacting bile canaliculi dynamics. It has been hypothesized that this effect is secondary to effects on bile acid transport, but more recent studies have demonstrated that drugs can directly alter the signal transduction pathways that regulate bile canaliculi dilation and constriction [27,28]. Bile canaliculi structures are highly dynamic in terms of continuous swelling and collapse and this process is essential for bile acid efflux [29]. More recently, a similar phenomenon has been associated with pyrazinamide-induced liver injury [31]. There are multiple different processes involved in the targeting of proteins to both the basolateral and apical membranes. Once on the membrane, transporters can undergo coordinated dynamic recycling on and off of the membrane via recycling endosomes. Polymorphisms in genes that are essential for functional hepatocyte polarity and membrane trafficking have been associated with liver injury. This is likely explained by species differences in animal models and/or physiological differences in cultured human hepatocytes. This species difference appears to relate in part to differences in transporter inhibition kinetics, but also to species differences in the toxicity profile of bile acids [17]. Humans have a higher proportion of the more toxic hydrophobic bile acids while rodents and dogs have a higher percentage of less toxic polar bile acids. And while cultured human hepatocytes may produce a physiologically relevant complement of endogenous bile acids [35], the majority (>95%) of bile acids present in the liver come from the extrahepatic pool. This pool is absent in static 2D cultures, preventing any significant intracellular accumulation due to transport inhibition. However, recent efforts have shown promise for eliciting bile acid-mediated toxicity in vitro by adding physiologically relevant concentrations of human bile acids to the culture media [36,37]. In this case, bile acid-dependent bile flow is only minimally affected although the hepatocyte bile acid concentrations may rise to exceed the threshold of toxicity. Although only hepatocytes are illustrated and subsequently discussed, the principles apply to biliary cells, which could also be the target of an adaptive immune attack. Furthermore, the target antigens should be "neoantigens" that are only formed in response to drug treatment and were not considered as "self" during early immune surveillance. Furthermore, at least two studies have shown a requirement for antigen-presenting cells to be pulsed with parent compound for at least 16 h in order to elicit a T-cell response [45,46]. This delay is consistent with hapten formation and antigen processing prior to neoantigen presentation. The rapid recurrence upon rechallenge is expected because the expanded antigen-specific population of lymphocytes remains in the body. When new peptides are presented, they can be seen as neoantigens by T cells, even though they are not "new" to the cell. This has been shown to be the mechanism underlying abacavir hypersensitivity reactions, predominately impacting skin [47]. Regardless of the mechanism of neoantigen formation, the question remains, what makes these reactions liver specific Liver specificity could reflect a higher concentration of parent drug and/or metabolites in the liver (especially after oral administration). Furthermore, it should not take several months to mount an adaptive response, supporting the requirement of preceding non-immune-mediated events for an adaptive immune attack on the liver. Finally, it is believed that a robust adaptive immune response requires local release of "danger signals" or "alarmins" to stimulate an adaptive immune attack [49,50]. It is believed that release of danger signals results from the direct effect of the drug on the liver. In susceptible individuals, these events lead to the release of danger signals that result in activation of innate immune cells. Activation of macrophages and other antigen-presenting cells is required to stimulate T cells and promote an adaptive immune attack. An adaptive immune attack may result in asymptomatic elevations in serum liver chemistries that typically resolve despite continued drug treatment. If immune tolerance does not promptly occur, progressive and symptomatic liver injury may result. Without prompt adaptation, the stress responses may result in the release of "danger signals" that are necessary to provoke a robust immune response. Danger signals and innate immune response the role of the danger signals is to stimulate innate immune cells and create inflammation. The activation of innate immune cells promotes the release of cytokines and chemokines that act through a variety of mechanisms to enhance the adaptive immune response and target the response to the infected tissues. These molecules upregulate costimulatory factors on professional antigen-presenting cells necessary to activate T cells and promote cytokine and chemokine release which help to target the adaptive immune attack on the liver. However, it is not clear that hepatocyte necrosis is a prerequisite for the release of these danger signals. The ability to trigger an adaptive immune attack on the liver in the absence of hepatocyte death is consistent with infection of the hepatocyte by the hepatitis B virus. The hepatitis B virus is not cytolytic yet it generates a liver-specific adaptive immune attack resulting in hepatocyte necrosis and the clinical disease [58]. However, if the release of danger signals does not require cell death, how does immune activation occur Recent work suggests that the danger signals may travel in hepatocyte-derived exosomes [59]. Exosomes, the smallest class of extracellular vesicles (<150 nm), can be released from the liver and diffuse into circulation due to the porous fenestrations that are unique to the sinusoidal endothelium. Liver-derived exosomes have been detected under basal conditions in biofluids such as plasma, and more recent evidence has demonstrated that the abundance and cargo of exosomes released from hepatocytes changes in response to drug-induced stress, prior to and in the absence of overt necrosis [59]. It also appears that exosomes from hepatocytes treated with subtoxic doses of drugs can stimulate the activation of monocytes (Natalie Holman, personal communication). The adaptive immune response and immune tolerance the culmination of the proposed early events is the targeting of cytotoxic lymphocytes to hepatocytes presenting the target neoantigen(s). Cytotoxic T cells kill the target cells through the secretion of cytolytic molecules including Fas-L, perforin, and granzyme B. This suggests that the initiation of a drug-induced adaptive immune attack on the liver is usually reversible, presumably through immune tolerance mechanisms. An important development in the understanding of the role of immune tolerance comes from recent reports of a mouse Chapter 28: Mechanisms of Drug-induced Liver Injury 785 model that recapitulates some of the clinical characteristics of idiosyncrasy including delayed onset and involvement of the innate and adaptive immune responses [61]. It was postulated that the latency observed in the clinic was due to the progression of kidney dysfunction and/or liver cysts that might occur slowly over time and thereby lower threshold for toxicity. Risk factors for drug-induced liver injury Even within a therapeutic class, there are sometimes marked differences in hepatic safety liability. Drug-specific drivers of toxicity include dose and intrinsic chemical properties such as lipophilicity and metabolism. Individual factors that enhance susceptibility can be categorized as nongenetic (physiological and environmental) and genetic. The outcome is related to some threshold concurrence of these independent factors, which are discussed in more detail in the subsequent sections. This has prompted recommendations that drug developers should focus on developing compounds that are administered at doses <50 mg/day [69].

Order cheapest phenergan
Patients with a prolonged stable course could be differentiated from those with a rapidly progressive course on the basis of overall life functioning but not on the basis of other more conventional clinical or biochemical criteria anxiety symptoms light sensitivity buy cheap phenergan 25 mg. Early studies of liver biopsy collections suggested that there was a relation between heterozygosity and the development of liver disease [15]. However, both these studies Chapter 31: Alpha-1 Antitrypsin Deficiency 845 were biased in ascertainment and did not include concurrent prospective controls. The W variant was reported in three consanguineous children homozygous for the allele, two of whom died during infancy of severe liver disease [22]. The patient was 46 years old and had a 10-year history of elevated serum transaminases but there was no further characterization of liver involvement and no indication as to whether the patient had been evaluated for other causes of liver disease. Furthermore, intrahepatocytic inclusions were not detected by immunohistochemical analysis in a liver biopsy specimen. Reports of individual cases can be difficult to interpret unless other causes of liver disease have been investigated, including alcohol consumption, viral hepatitis, and autoimmune disease, particularly in adults. Furthermore, based on what we know from the classical form of the disease, one would predict that only a subgroup affected by the variant will develop clinically significant liver disease and, thus, attribution of liver disease causation is even more challenging. Cigarette smoking markedly accelerates this destructive lung disease, reduces the quality of life, and markedly shortens the longevity of these persons [26]. The usual initial symptoms are shortness of breath, wheezing, cough, sputum production, and frequent chest infections [25]. Liver biopsies were not performed in this study and may be necessary for the accurate determination of the extent of liver injury in these patients. Indeed, we recently found that the PiZ mouse model has marked fibrosis in the lungs as well as the liver [31]. Because there is no evidence that it is expressed, the downstream gene is considered a pseudogene. A mobile reactive center loop rises above a gap in the center of the A sheet [35,36]. For example, the most common normal variant migrates to an intermediate isoelectric point, designated M. With these techniques, in addition to isoelectric focusing, investigators have identified more than 100 allelic variants [38]. Alpha-1 antitrypsin protein structure Alpha-1 antitrypsin is a single-chain, approximately 55 kDa polypeptide with 394 amino acids and three asparagine-linked complex carbohydrate side-chains [35]. There are two major serum isoforms depending on the presence of a biantennary or triantennary configuration of the carbohydrate side-chains. A serpinlike structure is also found in several cellular proteins, trophic factors, and circulating carrier proteins, such as corticosteroid- and thyroid hormone-binding globulin. There are many rare normal allelic variants with allelic frequencies of less than 0. The inheritance of a null allelic variant with another null variant or a deficiency variant is associated with premature development of emphysema. Serum samples from a person with the normal M1M2 variant, from an M2Z heterozygote, and from a person with the normal M1M1 variant were subjected to isoelectric focusing with the anode at top and cathode at bottom. The episodic nature of the illness was attributed to changes in the synthesis of the mutant protein during the host response to acute inflammation and tissue injury, the acute-phase response. Some of these variants are not associated with clinical disease when homozygous, such as the S variant [20,45]. Several evidence for liver injury in persons with null variants who were examined in detail [34]. The most common deficiency variant, the Z variant, is associated with emphysema and liver disease, as discussed later. Alpha-1 antitrypsin function Alpha-1 antitrypsin is an inhibitor of serine proteases in general, but its most important targets are neutrophil elastase, cathepsin G, and proteinase 3, proteases released by activated neutrophils. The reaction between enzyme and inhibitor is essentially of second order, and the resulting complex contains one molecule of each of the reactants. There is also a profound alteration in the structure of the enzyme, including disruption of the catalytic site, such that the enzyme becomes inactive and subject to proteolytic destruction [50]. Carrell and Lomas [51,52] likened the inhibitory mechanism to a mousetrap: the active inhibitor circulates in the metastable, stressed form and then springs into the stable, relaxed form to lock the complex with its target protease. First, the reactive site methionine may be oxidized and thereby rendered inactive as an elastase inhibitor [52]. Most of the evidence from these studies indicates that this protective effect is due to inhibition of the synthesis and release of platelet-activating factor from neutrophils [62], presumably through the inhibition of neutrophil-derived proteases. The chemotactic response is equivalent to that elicited by formyl-methionyl-leucylphenylalanine. This effect appears to involve inhibition of viral entry and does not require protease inhibitory activity. Its concentration in lavage fluid from the lower respiratory tract is approximately equivalent to that in serum. Site-directed mutagenesis studies have shown that this single amino acid substitution is sufficient to produce the cellular defect [104]. The model predicts that the final step in the folding of the serpin molecule is the incorporation of strand s5a into the central -sheet A. Finally, the unfolding event that leads to domain swapping is predicted to expose a 30-residue helical linker region. Polymerization also appears to occur for other serpins in clinical deficiency states, including antithrombin deficiency [110] and C1 inhibitor deficiency [111]. A striking example of this phenomenon is the familial dementia associated with Collins bodies. However, these studies do not exclude the possibility that there is an abnormality in folding that is distinct from the tendency to polymerize and is also partially corrected by the second, experimentally introduced mutation. Nonetheless, the polymerogenic properties of the Z mutant are still likely to be critical determinants in the pathobiology of liver disease. Before being transported to their final destination, these nascent secretory and membrane polypeptide chains undergo a series of posttranslational modifications, including glycosylation, formation of disulfide bonds, oligomerization, and folding. These observations have therefore led to the concept that modifiers, either genetic or environmental, predispose a subgroup of homozygotes to liver disease and/or protect the remainder of the population from liver disease. Furthermore, the modifiers are likely to be heterogeneous among patients and their families because this would explain the rather remarkable diversity in natural history of liver disease that has been observed. Increased autophagosomes were observed in the liver of PiZ mice and in liver biopsy specimens from patients [130]. It also appears to play a role in homeostasis, cell growth, and cell differentiation. It begins with the formation of a membranous platform around a targeted region of the cell. This platform becomes a double-membrane vesicle as it envelopes cytoplasm together with parts of or entire subcellular organelles. Eventually this autophagosome fuses with the lysosome for degradation of its contents. This Golgi-to-lysosome pathway appears to involve the endosomal protein sorting receptor sortilin and has been demonstrated in mammalian cell systems as well as yeast [136]. Recent experiments have shown that this protein is localized to the Golgi and plays a role in regulation of protein secretion [138]. Furthermore, the study could have led to an entirely different conclusion with a legitimate alternate way of classifying one of the patient groups. Adenoma occurs within 1 year, and invasive hepatocellular carcinoma occurs between 1 and 2 years of age [145]. This study showed that there was increased hepatocellular proliferation in the liver at baseline. This suggested that the globule-containing hepatocytes were producing a regenerative signal or signals. This result suggested that the block in proliferation of globule-containing hepatocytes is relative; that is, that they would proliferate if the stimulus were as powerful as the one generated after partial hepatectomy. This was interpreted to mean that the globule-containing hepatocytes were "sick but not dead.

Purchase phenergan 25mg overnight delivery
The genome architecture of the Collaborative Cross Mouse Genetic Reference Population anxiety symptoms related to menopause purchase phenergan 25mg overnight delivery. Candidate risk factors and mechanisms for tolvaptan-induced liver injury are identified using a Collaborative Cross Approach. Utilization of causal reasoning of hepatic gene expression in rats to identify molecular pathways of idiosyncratic drug-induced liver injury. Oxidative stress/reactive metabolite gene expression signature in rat liver detects idiosyncratic hepatotoxicants. In silico prediction of drug induced liver toxicity using substructure pattern recognition method. Prediction of drug induced liver injury using molecular and biological descriptors. A novel high mobila ity group box 1 neutralizing chimeric antibody attenuates druginduced liver injury and postinjury inflammation in mice. Anti-tumour necrosis factor agent and liver injury: Literature review, recommendations for management. Drug-induced liver injury: advances in mechanistic understanding that will inform risk management. Mechanism of cell death in acute-on-chronic liver failure: a clinico-pathologic-biomarker study. Profiles of serum cytokines in acute drug-induced liver injury and their prognostic significance. The diagnosis of Wilson disease is established by a combination of clinical and biochemical findings or by molecular genetic studies. Biochemical findings include most notably a decrease in levels of circulating ceruloplasmin, and a hepatic copper concentration above 250 mg/g dry weight of liver in most affected individuals. Most patients are compound heterozygotes with two different mutations, but clinical and biochemical evaluation are needed to demonstrate phenotypic expression and to stage the disease. In most symptomatic patients, treatment with copper chelating agents is effective in stabilizing or reversing the disease. In all circumstances, lifelong pharmacologic treatment is required and results in excellent patient survival. Acute liver failure in Wilson disease or hepatic insufficiency unresponsive to medical therapy is best treated with orthotopic liver transplantation, which, by providing the liver with a normal physiologic capacity for copper excretion, is curative. Correctly, he speculated that the brain disease, characterized by extrapyramidal features, was caused by the liver disease. However, his concept of a "morbid toxin" produced by the cirrhotic liver, although strictly correct, could not have anticipated the much later insights into the role of the liver in copper metabolism and the vulnerability of certain areas of the brain to the toxic effects of excessive copper deposition. It was not until 33 years later that Glazebrook [2] detected a marked excess of copper in the basal ganglia of a patient dying of Wilson disease and surmised from the recognized accumulation of copper in the liver that the inability of the liver to excrete copper was the dysfunction responsible for the lenticular degeneration, a pathogenetic association later confirmed by other workers [3,4]. Recognition of the value of a low serum ceruloplasmin concentration in the diagnosis of Wilson disease came from the observations of Scheinberg and Gitlin [10], who first reported this phenomenon in 96% of Wilson disease homozygotes. However, Sternlieb and Scheinberg [11] subsequently recognized that up to 20% of heterozygotes also have low ceruloplasmin concentrations without any other clinical manifestations of Wilson disease. This observation and the presence of a normal ceruloplasmin in a small minority of Wilson disease homozygotes, and the lack of copper accumulation in patients with a defect in ceruloplasmin biosynthesis (aceruloplasminemia), argued against a direct pathogenetic role for ceruloplasmin in the accumulation of copper in tissues in cases of Wilson disease. With the understanding that the clinical features of Wilson disease are the result of copper toxicity in the various affected tissues of the body, the rationale for chelation therapy became apparent. This drug, which is lipophilic and therefore administered intramuscularly, provided the first effective therapy for a previously untreatable disorder. The principle on which its action was based depended on its two sulfydryl groups for the binding and inactivation of arsenic. It was Walshe, while working at the Boston City Hospital, who made the incidental finding of the excretion of dimethylcysteine in the urine following the administration of penicillin that led him to postulate that this breakdown amino acid product of the antibiotic (also known as d-penicillamine) might have copper chelating properties. This led Walshe to test and then introduce the first effective oral chelation therapy in the form of penicillamine where he demonstrated its cupriuretic action and role in the symptomatic improvement of patients with lifethreatening features of Wilson disease [15]. Early studies showed that the d-isomer of dimethylcysteine was the favored treatment for use for Wilson disease, with very promising benefits for both the hepatic and neurologic components of the disease. Sternlieb and Scheinberg [11] subsequently expanded the use of this drug to include the treatment of asymptomatic (or presymptomatic) patients with Wilson disease by showing its effectiveness in preventing disease progression. Walshe [16] proceeded to develop another chelating agent, triethylene tetramine dihydrochloride (trientine), as an alternative agent for the treatment of those patients intolerant of the toxic effects of penicillamine. It had powerful copper chelating ability with clinical benefits comparable to those of penicillamine but with fewer side effects, and was shown capable of treating patients who were intolerant of dpenicillamine. Walshe [17] was also instrumental in the initial human use of tetrathiomolybdate, currently an investigational drug in the United States and Europe. Its mode of action is through tight binding of copper and the ability to form an inert complex with albumin and copper, with the potential for rapidly removing copper from tissues. The possibility of preventing the toxic accumulation of copper in Wilson disease by blocking the intestinal absorption of copper with oral zinc therapy was first considered by Schouwink [18]. Brewer and his colleagues however conducted the first copper balance studies showing that zinc effectively induced a negative copper balance. Subsequent studies have shown that zinc is a valuable alternative to chelation agents for long-term maintenance therapy based on its effectiveness in preventing copper reaccumulation [19,20]. The phenotypic reversion from a diseased to a normal state in transplant recipients demonstrates the central role of the liver in Wilson disease and copper metabolism. The recognition of Wilson disease as an inherited disorder, defined by a complex of signs and symptoms, evolved in less than a century to the point where we are able to define the molecular basis for the pathophysiology of this disorder. Genetics Although Wilson correctly recorded the familial nature of the disease, it was Hall in 1921 [22] who demonstrated its inheritance, later shown to be autosomal recessive [23]. Subsequently, the linkage of Wilson disease to the locus of the red cell esterase-D gene placed the gene for Wilson Chapter 29: Wilson Disease Table 29. The detection of specific mutations unique to individuals with clinical and biochemically proven disease confirmed the identity of the responsible gene [30,31]. Most of the mutations thus far identified are point mutations that result in amino acid substitutions. However, deletions, insertions, missense, and splice site mutations have also been reported. A summary of the mutations and polymorphisms of the gene can be found in the following website. The most frequently observed point mutation, which results in a change from histidine to glutamine (H1069Q), is present in nearly 30% of patients of European descent [31,37]. In only a single population in Austria has the frequency of this mutation been reported to be higher (up to 65%) [38]. Pathophysiology Copper is an essential cofactor for many enzymes and proteins and is important for the mobilization of tissue iron stores. It is subsequently used for cellular metabolic needs, incorporated into the secretory glycoprotein ceruloplasmin, or excreted into bile. Dietary copper is absorbed in the proximal small intestine, whereas nonabsorbed copper or copper bound within shed enterocytes passes into the feces. Absorbed copper is bound mainly to albumin in the portal circulation, from which it is avidly extracted by hepatocytes. Hepatocellular copper is bound to ligands and used for metabolic needs, transferred to endogenous chelators, incorporated into ceruloplasmin, or excreted into bile. Biliary copper does not undergo enterohepatic recycling and is therefore excreted in the feces. In Wilson disease, biliary copper excretion is reduced, and copper accumulates within hepatocytes. The incorporation of copper into ceruloplasmin is also impaired in Wilson disease; as a result, circulating levels of this protein are decreased in most patients. When cellular stores are overloaded or after a hepatocellular injury, the amount of copper released into the circulation is increased.
Buy phenergan 25 mg cheap
As might be expected anxiety symptoms 2 order phenergan 25 mg visa, symptoms result from inflammatory destruction of the exocrine glands. The keratoconjunctivitis produces blurring of vision, burning, and itching, and thick secretions accumulate in the conjunctival sac. The xerostomia results in difficulty in swallowing solid foods, a decrease in the ability to taste, cracks and fissures in the mouth, and dryness of the buccal mucosa. Parotid gland enlargement is present in one-half of patients; dryness of the nasal mucosa, epistaxis, recurrent bronchitis, and pneumonitis are other symptoms. Manifestations of extraglandular disease are seen in one-third of patients and include synovitis, diffuse pulmonary fibrosis, and peripheral neuropathy. Defects of tubular function, however, including renal tubular Autoimmune diseases acidosis, uricosuria, and phosphaturia, are often seen and are associated with tubulointerstitial nephritis (Chapter 20). About 60% of patients have another accompanying autoimmune disorder, such as rheumatoid arthritis, and these patients also have the symptoms and signs of that disorder. The combination of lacrimal and salivary gland inflammation was once called Mikulicz disease. The name has now been replaced by Mikulicz syndrome, broadened to include lacrimal and salivary gland enlargement from any cause, including sarcoidosis, IgG4-related disease (described later), lymphoma, and other tumors. In early stages of the disease, this immune infiltrate consists of a mixture of polyclonal T and B cells. However, if the reaction continues unabated, there is a strong tendency over time for individual clones within the population of B cells to gain a growth advantage, presumably because of the acquisition of somatic mutations. Emergence of a dominant B-cell clone is usually indicative of the development of a marginal zone lymphoma, a specific type of B-cell malignancy that often arises in the setting of chronic lymphocytic inflammation. Although the term scleroderma is ingrained in clinical medicine, this disease is better named systemic sclerosis because it is characterized by excessive fibrosis throughout the body. In some patients, the disease seems to remain confined to the skin for many years, but in the majority it progresses to visceral involvement with death from renal failure, cardiac failure, pulmonary insufficiency, or intestinal malabsorption. The clinical heterogeneity of systemic sclerosis has been recognized by classifying the disease into two major categories: diffuse scleroderma, characterized by widespread skin involvement at onset, with rapid progression and early visceral involvement; and limited scleroderma, in which the skin involvement is often confined to fingers, forearms, and face. Visceral involvement occurs late; hence, the clinical course is relatively benign. Several other variants and related conditions, such as eosinophilic fasciitis, occur far less frequently and are not described here. Unknown external stimuli cause vascular abnormalities and immune activation in genetically susceptible individuals, and both contribute to the excessive fibrosis. With progression of the disease, there is increasing fibrosis of the dermis, which becomes tightly bound to the subcutaneous structures. There is marked increase of compact collagen in the dermis, usually with thinning of the epidermis, loss of rete pegs, atrophy of the dermal appendages, and hyaline thickening of the walls of dermal arterioles and capillaries. In advanced stages, the fingers take on a tapered clawlike appearance, joint motion is limited, and the face becomes a drawn mask. Loss of blood supply may lead to cutaneous ulcerations and to atrophic changes in the terminal phalanges. Progressive atrophy and collagenous fibrous replacement of the muscularis may develop at any level of the gut but are most severe in the esophagus. The associated dysfunction of the lower esophageal sphincter gives rise to gastroesophageal reflux and its complications, including Barrett esophagus (Chapter 17) and strictures. The mucosa is thinned and may be ulcerated, and there is excessive collagenization of the lamina propria and submucosa. Loss of villi and microvilli in the small bowel sometimes produces a malabsorption syndrome. Inflammation of the synovium, associated with synovial hypertrophy and hyperplasia, is common in the early stages; fibrosis later ensues. These changes are reminiscent of rheumatoid arthritis, but joint destruction is not common in systemic sclerosis. In a small subset of patients (approximately 10%), inflammatory myositis may develop. Renal abnormalities occur in two-thirds of patients with systemic sclerosis, most prominently vascular lesions. Interlobular arteries show intimal thickening as a result of deposition of mucinous or finely collagenous material, which stains histochemically for glycoprotein and acid mucopolysaccharides. Hypertension, however, does occur in 30% of patients with scleroderma, and in 20% it takes an ominously rapid, downhill course (malignant hypertension). In hypertensive patients, vascular alterations are more pronounced and are often associated with fibrinoid necrosis of arterioles, thrombosis, and infarction. Such patients often die of renal failure, which overall accounts for about 50% of deaths from systemic sclerosis. Pulmonary involvement is seen in more than 50% of individuals with systemic sclerosis and may manifest as interstitial fibrosis and pulmonary hypertension. Pulmonary vasospasm, secondary to pulmonary vascular endothelial dysfunction, is considered important in the pathogenesis of pulmonary hypertension. Pulmonary fibrosis, when present, is indistinguishable from that seen in idiopathic pulmonary fibrosis (Chapter 15). Pericarditis with effusion, myocardial fibrosis, and thickening of intramyocardial arterioles occur in one-third of patients. Microvascular disease is consistently present early in the course of systemic sclerosis and may be the initial lesion. Intimal proliferation is evident in the digital arteries of patients with systemic sclerosis. Nailfold capillary loops are distorted early in the course of disease, and later they disappear. However, what causes the vascular injury is not known; it could be the initiating event or the result of chronic inflammation, with mediators released by inflammatory cells inflicting damage on microvascular endothelium. Repeated cycles of endothelial injury followed by platelet aggregation lead to release of platelet and endothelial factors. Vascular smooth muscle cells also show abnormalities, such as increased expression of adrenergic receptors. Eventually, widespread narrowing of the microvasculature leads to ischemic injury and scarring. The progressive fibrosis characteristic of the disease may be the culmination of multiple abnormalities, including the accumulation of alternatively activated macrophages, actions of fibrogenic cytokines produced by infiltrating leukocytes, hyperresponsiveness of fibroblasts to these cytokines, and scarring following ischemic damage caused by the vascular lesions. There is some evidence that fibroblasts from patients with systemic sclerosis have an intrinsic abnormality that causes them to produce excessive amounts of collagen. This idea is based on studies with cultured fibroblasts, and whether or how this abnormality relates to pathogenesis in vivo is unknown. Prominent changes occur in the skin, alimentary tract, musculoskeletal system, and kidney, and lesions also are often present in the blood vessels, heart, lungs, and peripheral nerves. The majority of patients have diffuse, sclerotic atrophy of the skin, which usually begins in the fingers and distal regions of the upper extremities and extends proximally to involve the upper arms, shoulders, neck, and face. Note the extensive deposition of dense collagen in the dermis with virtual absence of appendages. Raynaud phenomenon, manifested as numbness and tingling of the fingers and toes caused by episodic vasoconstriction of arteries and arterioles, is seen in virtually all patients and precedes other symptoms in 70% of cases. Dysphagia attributable to esophageal fibrosis and its resultant hypomotility are present in more than 50% of patients. Eventually, destruction of the esophageal wall leads to atony and dilation, especially at its lower end.