Buy eulexin 250mg with mastercard
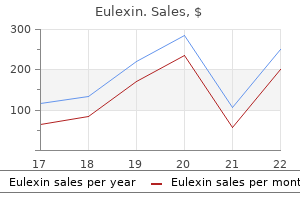
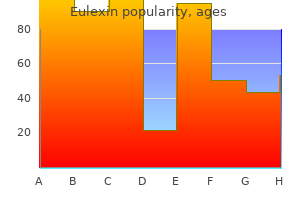
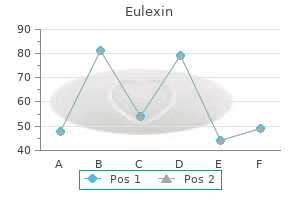
The underlying lamina propria is heavily infiltrated with lymphocytes and plasma cells prostate cancer incontinence purchase eulexin 250mg. For comparison, in the panel on the right is the tip of a villus from the biopsy sample shown in lower panel of Plate 23 from a normal individual. Endoscopic view of a diminutive adenomatous polyp before cold snare excision (narrow-band imaging mode). Sessile adenomatous polyp undergoing hot snare polypectomy without mucosal injection. Hemostatic clips applied after polypectomy for hemostasis and suspected perforation. Snare polypectomy for a large pedunculated polyp, with endoloop in place prior to snare resection. Endoscopic mucosal resection: cap method with transparent cap positioned over irregular nodule in Barrett mucosa. Giant duodenal ulcer occupying the entire duodenal bulb, with a nonbleeding visible vessel at bottom right (arrow). Endoscopic view of bleeding from the minor papilla in a patient with pancreatic cancer (arrow). A B Intentionally swallowed razor blades are seen on abdominal x-ray (A, arrow) and on colonoscopic view in the cecum (B). These were retrieved successfully with use of a Roth net and overtube to protect the tortuous sigmoid colon. After retrieval, with difficulty the object was unfolded and discovered to be a vulcanized latex glove (B). A large bile duct (arrow) shows lymphocytic inflammation and periductal ("onion-skin") fibrosis. It is also possible to have a perforation (Boerhaave syndrome) either spontaneously, due to repeated vomiting, or after endoscopic therapy leading to mediastinitis. Although in most patients the tears resolve spontaneously, massive bleeding can occur from Mallory-Weiss tears in patients who have portal hypertension, especially if esophageal varices are present. Combination therapy with injection initially to slow or stop the bleeding followed by cautery is effective in most patients. However, because the injury is a tear of the lining (and the esophagus lacks a serosa), overinjection and overcauterization should be avoided. Hemoclips have been used for this indication, are effective, and should not cause additional damage to the tissue. In cases of associated portal hypertension or esophageal varices, endoscopic therapy must be cautiously performed and cautery therapy should be avoided. These patients can be treated with sclerotherapy, band ligation, or hemoclip placement. Medical therapy should be initiated in patients with Mallory-Weiss tears, but has not been shown to alter the natural history of the acute bleeding. Surgical intervention, with oversewing of a vessel, is rarely needed in patients with Mallory-Weiss tears. If there are other systemic signs, such as fever, chest pain, and shortness of breath, the Boerhaave syndrome (esophageal perforation) should be considered. Laboratory Findings the laboratory findings for a Mallory-Weiss tear are nonspecific and are similar to those for peptic ulcer disease. Imaging Studies Upper endoscopy, performed promptly, is the diagnostic (and therapeutic procedure) of choice. The tears can be seen as single or multiple longitudinal disruptions of the mucosa of the distal esophagus, at the gastroesophageal junction, within a hiatal hernia, or in the stomach just below the gastroesophageal junction with associated bleeding (Plate 58). A prospective, randomized trial of endoscopic band ligation vs epinephrine injection for actively bleeding Mallory-Weiss syndrome. Mallory-Weiss tears are focal lesions within an otherwise normal-appearing region of mucosa, which distinguishes them from reflux or infectious esophagitis. Patients with pill-induced esophagitis often have injury higher up the esophagus, and this etiology may be suspected by history. A Dieulafoy lesion is associated with normal-appearing adjacent mucosa and the presence of a protuberant artery several centimeters below the gastroesophageal junction. Although originally described in 1884 by Gallard, the French surgeon Georges Dieulafoy 14 years later designated the lesion "exulceratio simplex. The typical location is in the upper stomach along the high lesser curvature, within 6 cm of the gastroesophageal junction. The cause of a Dieulafoy lesion is unknown, although the lesion may be congenital. The typical patient with a Dieulafoy lesion is a man, with multiple comorbidities, already hospitalized for other problems. It may be helpful to tattoo the area with ink or place a hemoclip at or near the site to help localize the area for subsequent endoscopic therapy or future operative treatment. In patients with recurrent bleeding, an attempt to repeat endoscopic therapy is reasonable; however, surgical therapy may be necessary. Surgical treatment of a Dieulafoy lesion is typically a wedge resection, as simple oversewing has a high rebleeding rate. However, the bleeding may be self-limited in nature or follow a stuttering course. In active bleeding, the diagnosis is confirmed by finding a visible vessel with active arterial pumping, without an associated ulcer or mass. The diagnosis can be difficult, as the lesion is without a surrounding ulcer, the location may be dependent within the stomach during endoscopy and as bleeding is often so massive that the area may be covered with blood, and thus the source may not be visualized. In the absence of active bleeding, the lesion is even more difficult to see, as it may appear as a small and subtle raised area, such as a nipple or visible vessel without an associated ulcer. Although not widely utilized, the use of a Doppler probe can provide the correct diagnosis of a visible vessel in this situation. In patients with massive bleeding and no obvious cause, the lesser curvature within 6 cm of the gastroesophageal junction should be carefully inspected for evidence of a Dieulafoy lesion. Imaging Studies Upper endoscopy is the primary modality to detect a Dieulafoy lesion. If bleeding has stopped and there is doubt about the nature of the lesion, the use of a Doppler probe if available or endoscopic ultrasound with Doppler flow may be helpful to confirm the diagnosis. The spectrum of vascular malformations includes Dieulafoy lesions, as previously discussed, watermelon stomach (gastric antral vascular ectasia), Osler-Weber-Rendu syndrome (hereditary hemorrhagic telangiectasia), blue rubber bleb nevus syndrome, and radiation-induced telangiectasias. Combination therapy with injections of epinephrine followed by cautery may be used, or hemoclips may be placed. There are also reports of band ligation or use of an over-the-scope clip over a Dieulafoy lesion. These also can be detected by angiography, with findings including an early filling vein, a vascular tuft, and a late draining vein. Although the diagnosis is made by the characteristic endoscopic appearance, it can be confirmed by histology from endoscopic biopsy. Biopsies of watermelon stomach show areas of vascular ectasia associated with spindle cell proliferation and fibrohyalinosis. The bleeding that occurs is typically chronic and low grade, often associated with iron deficiency anemia and occult bleeding. Endoscopic therapy with thermal coagulation is the treatment of choice, with cautery applied initially to the periphery and then at the center of the lesion. There should be whitening of the mucosa and ablation of all visible vascular tissue. It is important to avoid overdistention (by the argon gas) of the stomach or small intestine during therapy, as well as to avoid contact with tissue when using argon plasma coagulation therapy. Repeated therapy should not be applied to the same location due to the risk of transmural injury and perforation, especially in the small bowel. Angiography and surgery can be offered for failures of endoscopic and medical therapy, but are rarely necessary. Several courses of treatment are required to obliterate the vascular ectasias and decrease or stop bleeding. In refractory patients with watermelon stomach, radiofrequency ablation and cryotherapy have been used with success.
Buy 250 mg eulexin with mastercard
Stenosis and complete occlusion of the shunt occur in 5% to 15% of the cases man health product generic 250mg eulexin otc, requiring revision. The various forms of surgical shunts include portacaval shunts, distal splenorenal shunts, and partial shunts. Revascularization of the esophagus is another surgical option for the treatment of variceal bleeding. Other risk factors such as shock, sepsis, renal failure, liver failure, and glucocorticoids were identified, but the association with bleeding was not statistically significant. However, they reveal the importance of significant bleeding as a sign of the degree of severity of the primary illness. The terms stress ulcer, stress gastritis, stress erosions, and stress lesions are used interchangeably in the literature. However, most of these lesions are of little significance because healing occurs rapidly. Clinically important bleeding, however, is defined as overt bleeding associated with one of the following within 24 hours of the onset of the bleeding: a drop in systolic blood pressure of greater than 20 mm Hg, an increase in the pulse rate of more than 20 beats/min and a 10-mm Hg drop in systolic blood pressure, or a decrease in hemoglobin of greater than 2 g/dL requiring blood transfusion and failure of hemoglobin to increase by the number of units transfused minus 2 g/dL. The role of the microcirculation is to provide nutrients and eliminate toxic oxygen-derived free radicals. Sucralfate works by coating the gastric mucosa and forming a thin protective layer between the mucosa and the gastric acid in the lumen without affecting acid secretion and intragastric pH. Conflicting results were reported regarding this issue, but a large trial by Cook and colleagues in which ranitidine and sucralfate were compared showed no significant difference in the development of nosocomial pneumonia. These concerns should alert providers to the importance of discontinuation of acid suppression in the absence of proper indication. Surgery is reserved for patients with uncontrolled hemorrhage and usually involves vagotomy, oversewing of bleeding sites, and in rare cases, subtotal or total gastrectomy. It is caused by a diverse range of bleeding sources and can range from trivial to lifethreatening bleeding. Totals Studies cited in this table may be found in the complete list of references for this chapter provided online. Most patients stop bleeding spontaneously, but the bleeding can recur in 10% to 40% of cases. As opposed to acute mesenteric ischemia, this reduction is transient and reversible. The typical regions affected are the "watershed" areas of the colon: the splenic flexure, the rectosigmoid junction, and the right colon. Clinically, patients have a sudden onset of abdominal pain, followed by hematochezia within 24 hours. Rare cases require surgery (if peritoneal signs are present) or develop chronic ischemic colitis with stricture formation. Overt bleeding from angiodysplasia is usually brisk and painless and cannot be distinguished from diverticular bleeding. Endoscopic treatment is highly effective and safe and prevents bleeding episodes from recurring. Other Sources of Lower Gastrointestinal Bleeding Acute significant bleeding from colonic neoplasia and polyps is uncommon despite reports in which it accounts for up to 36% of cases. Postpolypectomy bleeding occurs in 1% to 6% of patients undergoing colonoscopic polypectomy. Risk factors for postpolypectomy bleeding include large size, sessile morphologic appearance, and right colonic location. Hemorrhoids can cause significant bleeding and may sometimes require endoscopic or surgical intervention. Bleeding from rectal ulcers is common in elderly bedridden patients and in critically ill patients. Colonoscopy is an attractive choice in this setting because it offers the best opportunity for early diagnosis and subsequent management. Another randomized trial compared urgent colonoscopy with a standard care algorithm in which radionuclide scanning, followed, if positive, by angiography, was used in patients with suspected active bleeding versus expectant colonoscopy in those without active bleeding. This trial showed that a definite source of bleeding was found more often in urgent colonoscopy patients. However, no difference in mortality rate, surgery, and rebleeding was found in the two groups. A major limitation of this trial was that the study was terminated before reaching the prespecified sample size. Concern about poor visibility, the potential for complications, and the adverse effects of bowel preparation in the setting of bleeding is behind the reluctance in performing "urgent" colonoscopy. Several reports have shown that early (or urgent) colonoscopy is safe and has high diagnostic yield in patients with hematochezia. Polyethylene glycol lavage solution by mouth or through a nasogastric tube is commonly used in these cases. It has been used for several decades as a method for localization of the bleeding source. On the other hand, this diagnostic modality lacks therapeutic capability, has variable accuracy, and may delay other diagnostic and therapeutic procedures. The problem with this approach is the inconsistent and widely variable accuracy and the high rate of false-positive results in different reports. In addition to its role in accurate localization of bleeding lesions, angiography offers therapeutic possibilities. As with radionuclide scanning, the ability of angiography to detect the bleeding source varies widely among studies, from 20% to 70%. This sequence in management was the standard approach to ongoing bleeding until recently, when colonoscopy started gaining interest in the setting of acute bleeding (as opposed to expectant elective colonoscopy). When angiographic therapy fails or is not available after localization of the bleeding, the findings are used to guide surgical resection. Angiography can cause serious complications, such as contrast reactions, arterial thrombosis and dissection, and catheter site infection and bleeding. Unfortunately, the accuracy of radionuclide scanning in localization of the bleeding is variable, and hence it should not be used as a guide for surgery. Colonoscopy and angiography may be used as a guide for surgery in cases in which bleeding is initially identified and possibly treated through these modalities, and then recurs and requires surgery. It enables the accurate acquisition of arterial images, which can show contrast extravasation in areas of active bleeding. Obscure bleeding can be occult (positive fecal occult blood testing without frank recognizable blood loss) or overt (clinically evident). Obscure bleeding can be very challenging to the physician and, in cases of overt massive bleeding, life-threatening to the patient. Differential Diagnosis Missed lesions on upper and lower endoscopy should be considered first in the workup of obscure bleeding. Causes difficult to identify on routine endoscopy include hemosuccus pancreaticus, hemobilia, aortoenteric fistula, Dieulafoy ulcer, and extraesophageal varices. However, the experience from published series suggests that this form of therapy is likely to be beneficial. Infusion of vasopressin can control bleeding in up to 91% of cases,141 but complications develop in 10% to 20% and include arrhythmia, pulmonary edema, and ischemia. Review of several studies using superselective techniques showed that immediate hemostasis was achieved in 96% of cases and rebleeding within 30 days occurred in 22%. Surgical Therapy Surgery is indicated in cases of recurrent bleeding (especially diverticular) and massive ongoing bleeding with high transfusion Diagnostic Evaluation Repeat upper and lower endoscopy is usually warranted at least once after the index endoscopy, with the uncommon and subtle lesions just listed kept in mind. When the patient has active ongoing bleeding, radionuclide scanning and angiography should be considered. If results of all these tests are negative, the focus should shift to evaluation of the small bowel. Radiographic imaging of the small bowel may help when Crohn disease or malignancy is suspected. These modalities have lost favor with the advent of capsule endoscopy and device-assisted enteroscopy (except in cases in which there may be narrowing of the small bowel). Small bowel push enteroscopy can be very helpful in identifying and, in some cases, treating lesions in the small bowel that are responsible for obscure bleeding. It consists of swallowing a pillsized camera with sufficient battery life to image the entire small bowel. In patients who can tolerate an invasive procedure, device-assisted enteroscopy can be used when available and has the advantage of therapeutic ability.
Diseases
- Xeroderma talipes enamel defects
- Cryroglobulinemia
- Accessory navicular bone
- Schlegelberger Grote syndrome
- NADH cytochrome B5 reductase deficiency
- 6-pyruvoyltetrahydropterin synthase deficiency
- Urticaria-deafness-amyloidosis
- Goitre
- Fetal warfarin syndrome
Cheap eulexin online
In the starved state prostate cancer women order eulexin without prescription, as little as 2% to 5% of calories can be provided as fat, primarily to prevent essential fatty acid deficiency. Complications of excess lipid administration, particularly when given parenterally, include hyperlipemia, immunosuppression, and hypoxemia as a result of both impaired oxygen diffusion and ventilation-perfusion mismatching. In general, a hypermetabolic patient should receive 15% to 40% of calories as fat, not to exceed 1. Protein catabolism in a stressed patient has long been thought to be unresponsive to protein or amino acid administration or glucose infusion,56 and attainment of nitrogen balance is thought to depend largely on the support of stress protein synthesis. Amino acids are redistributed from skeletal muscle to support hepatic protein synthesis, the cellular inflammatory response, and gluconeogenesis and are used as oxidative fuel sources. To meet the protein requirements of the stressed state and at the same time avoid excess calories and the attendant complications, an injured or septic patient may require nutrition support with a nonprotein calorie-to-nitrogen ratio of 80:1 or 100:1, as compared with a patient with starvation metabolism, who may tolerate a nonprotein calorie-to-nitrogen ratio of 150:1 or higher. Antioxidant vitamins (including vitamins E and ascorbic acid) and trace minerals (including zinc, copper, and particularly selenium) may improve outcome in burns, in trauma, and in critically ill patients requiring mechanical ventilation59 and should be provided to all critically ill patients receiving specialized nutrition support. Initial limitation of trace elements should be considered in patients with renal failure. Vitamin K, which is light sensitive, must be added separately in a light-impermeable bag or given by another route once or twice weekly. Excessive doses of vitamin C should be avoided in renal failure because of the accumulation of oxalate. Vitamin A accumulates and should not be supplemented beyond the recommended dietary allowance. The preferred route has been the subject of considerable controversy during the past 40 years. Both routes have advantages and disadvantages, and nitrogen balance can be achieved by either route. Disadvantages of parenteral nutrition include cost, procedure (central venous catheter)-related complications, an increased likelihood of metabolic complications, including hyperglycemia, and an increased risk of infectious complications. Enteral nutrition is much less expensive, is more physiologic, is associated with fewer metabolic complications such as electrolyte abnormalities and hyperglycemia, and stimulates gut function and preserves mucosal integrity and barrier function better than parenteral nutrition does. Disadvantages of enteral nutrition include the requirement for an intact and functioning gastrointestinal tract, procedure (feeding tube placement)-related complications, pulmonary aspiration, malabsorption, feeding intolerance (pain, vomiting, bloating, diarrhea), and as a result, an inability to deliver the entire nutrient prescription. The gastrointestinal tract is a major interface between the host and the environment and not only regulates the ingestion and absorption of nutrients but is also responsible for defending the host against noxious microorganisms and toxins. Typical daily electrolyte requirements include sodium 60 to 100 mEq/day, potassium 60 to 100 mEq/day, magnesium 10 to 20 mEq/day, calcium 10 to 15 mEq/day, chloride 80 to 120 mEq/day, and phosphorus 20 to 30 mmol/day. Particular attention should be paid to the intracellular electrolytes (potassium, phosphorus, and magnesium), which are required for attainment of nitrogen balance58 and serum levels of which can fall precipitously when nutrition support is initiated. These IgA-producing lymphocytes then migrate to distant organs such as lungs, liver, and kidneys, where they form mucosal-associated lymphoid tissue and produce secretory IgA. Several meta-analyses comparing enteral and parenteral nutrition have shown significant reductions in infectious complications with the use of enteral nutrition. Whether this is the primary reason for the increased infection risk associated with parenteral nutrition is less clear. In several of the studies mentioned in previous paragraphs, many of the patients managed with parenteral nutrition received significantly more calories and had a higher incidence of hyperglycemia80 than did their enterally fed counterparts. In a study in which parenterally fed patients had a higher incidence of sepsis, twice as many patients receiving parenteral nutrition had hyperglycemia as enterally fed patients. There was no difference in 30-day mortality, and secondary endpoints were largely similar with the exception of more vomiting in the enterally fed patients. The incidence of infection was lower in the enterally fed group, but this difference was explained by the subset of trials in which the parenterally fed group received more calories and presumably had poor glucose control. Autophagy is an important housekeeping process that is normally activated by cellular stress to remove cellular damage. All patients received early enteral nutrition by protocol and had insulin infused to maintain normoglycemia. Further, patients in the late initiation group had significantly fewer infections, a significant reduction in the proportion of patients requiring more than 2 days of mechanical ventilation, a significant median reduction of 3 days in the duration of renal replacement therapy, and a mean reduction in health care costs of approximately $1600. There was no difference in ventilator-free days between the groups and the fully fed group had more gastrointestinal intolerance. None has been consistently shown to improve outcomes when compared with conventional formulas. Pulmonary failure formulas are designed for patients with acute respiratory failure associated with chronic lung disease. They contain at least 50% of calories as fat and thus reduce carbon dioxide production and decrease the work of breathing relative to highcarbohydrate formulas. Few data suggest a benefit with specific pulmonary formulas, and avoidance of overfeeding is more important in reducing ventilatory demand. They contain high concentrations of branched-chain amino acids and reduced concentrations of aromatic amino acids. Although these solutions have been shown to correct the abnormal amino acid profile characteristic of patients with liver failure,111,112 it is less clear that they actually treat hepatic encephalopathy. Patients with acute renal failure frequently have associated catabolic illness and as a result need more protein rather than less. Current recommendations for critically ill patients with acute renal failure are that standard recommendations for protein and calories should be followed, and that specialty formulas only be used for management of significant electrolyte abnormalities. Electrolytes can usually be added in standard stock concentrations or individually. Vitamins and trace elements are generally added in standard quantities but can be supplemented. Histamine 2 (H2) blockers for stress ulcer prophylaxis and regular insulin can also be added. Enteral formulas are usually premixed with a fixed nonprotein calorie-to-nitrogen ratio, and the needs of a specific patient are generally met by changing the formula. Protein and carbohydrate supplements can be added at the bedside to alter premixed formulas. Enteral formulas can be classified in numerous ways, including the form in which protein is provided. Such solutions contain 45% to 60% of calories as carbohydrate (oligosaccharides), 20% to 35% of calories as longchain fats. Hydrolyzed formulas provide protein as peptides or amino acids, are generally low in fat, and are designed for patients with gut dysfunction or malabsorption. Controlled studies comparing hydrolyzed or elemental formulas with intact formulas have not demonstrated improved tolerance or outcomes. High-protein formulas contain more than 45 g protein per 1000 kcal and are designed for patients with increased protein needs, such as patients with catabolic illness. Calorie-dense formulas are designed for patients in whom fluid restriction is required. They are generally relatively low in protein and not ideal for a stressed patient. Immunomodulating Enteral Formulas Immunomodulating enteral formulas are supplemented with various combinations of specific nutrients, arginine, -3 polyunsaturated fatty acids, nucleotides, glutamine, and antioxidants aimed at improving immune function and reducing inflammation in critically ill patients. Arginine is a nonessential amino acid that has both beneficial and deleterious effects. It is a secretagogue for anabolic hormones, supports T-cell function, detoxifies ammonia, and supports wound healing via metabolism to polyamine and proline. Considered a nonessential amino acid, glutamine may become conditionally essential when skeletal muscle stores and plasma levels become depleted during catabolic illness, thereby resulting in adverse effects on gut barrier and immune function. A meta-analysis of 14 randomized trials in which glutamine-supplemented nutrition was compared with standard nutrition demonstrated reduced infectious morbidity and mortality rates with glutamine supplementation, particularly in parenterally nourished surgical patients. In a 2001 meta-analysis of 22 studies (2419 patients) in which enteral nutrition supplemented with various combinations of arginine, -3 fatty acids, glutamine, and nucleotides was compared with conventional enteral nutrition, the supplemented patients had decreased infectious morbidity but no difference in mortality rates when compared with patients receiving the control diet. In the subsequently published and largest (597 patients) randomized trial to date, immunonutrition had no benefit in terms of infectious morbidity, length of hospital stay, number of ventilator days, or mortality rate. Second, the immunomodulating enteral formulas studied contained varying combinations of arginine, -3 polyunsaturated fatty acids (fish oil), glutamine, and antioxidants.
Buy eulexin visa
Additional variables that complicate the presentation include overall premorbid physical condition man health xchange cheap eulexin 250 mg fast delivery, age, preexisting chronic medical conditions, drug or alcohol intoxication, and timing of presentation to receive medical aid. Finally, other presentations unique to burns include exposure to electricity or an endless variety of chemical compounds. The numerous premorbid conditions, mixed and matched with various types of burn injuries (flame, scald, chemical, electrical) and other burn-related insults (inhalation, trauma from blast), create a vast variety of presentations that make each patient presentation very unique and challenging. Thus an individualized approach is necessary to optimally care for these patients against the backdrop of applying key fundamental critical care principles. Over the past half century, various fluid resuscitation formulas have been proposed and used to guide burn providers. These formulas each estimate the amount each patient may require during the course of a 24- to 48-hour resuscitation postburn period (Box 64. Underresuscitation results in decreased end-organ perfusion, resulting in cell apoptosis, organ failure, and death. On the other hand, overresuscitation is just as morbid, leading to compartment syndromes (extremities, abdomen, and orbits) as well as pulmonary and brain edema. This constellation of complications can be labeled as "resuscitation morbidity" and has been associated with death. These are mere estimates and predict how an ideal resuscitation should be delivered over the first 24 hours. The traditional formulas require a minimum of four computations to derive the fluid rate. This was identified as a potential reason that prehospital providers were not using a formula to initiate burn resuscitation in the field. The compilation of endpoints to assess the adequacy of end-organ perfusion and oxygen delivery is no different than the various endpoints used while resuscitating patients with conditions such as sepsis and hemorrhage. The only difference in patients with burns is the expectation that the pathologic state driving the circulatory and distributive shock will persist up to 48 to 72 hours in most cases. Runaway Resuscitation During the course of resuscitating a patient with severe burns, it is important for providers recognize the point at which resuscitative adjuncts may be necessary to prevent resuscitation-related morbidity. A resuscitation volume greater than 250 mL/kg in a 24-hour period is often used as a benchmark and is otherwise known as the Ivy index. Thus at any point during the first 24 hours of burn resuscitation, if the projected 24-hour volume exceeds the Ivy index, we recommend the addition of adjuncts listed in Box 64. This 24-hour projection is typically done at 8 to 12 hours after the burn injury to determine the need for adjuncts. Colloids: Albumin or Plasma Rescue therapy in the form of colloid infusion with albumin has been described a "colloid rescue. Typically, the 5% albumin infusion rate is continued until the 48-hour mark or until the shock state has clinically resolved. The rate of the combined infusion should be individualized and be geared toward optimizing a compilation of endpoints centered on maintaining urine output. As always, the potential benefit of plasma should be balanced against the known risks of pooled blood product transfusions, which include transfusionassociated lung injury and a variety of infectious complications. Second, that number is multiplied by 10 to derive the initial fluid rate in milliliters per hour. The rule of 10 was recently validated in an in silico analysis of 100,000 simulated "patients" as it calculated a reasonable starting point for a wide range of burn sizes and weights in adults. Once fluid resuscitation is initiated, the crystalloid rate should be titrated up or down on a regular basis. The goal of burn resuscitation is to provide adequate fluid necessary to avoid end-organ failure while avoiding "fluid creep. Physicians order an initial infusion rate of lactated Ringer solution based on Parkland formula calculations and indicate the target maintenance rate. The nursing staff measures hourly urine output and increases or decreases fluids based on this response. If patients develop unexpected changes in vital signs or do not respond appropriately, physicians are contacted. An option for the use of colloid-containing resuscitation is included for patients whose requirements fail to decline. This regimen permits close titration of fluids without requiring hourly physician input. Vitamin C Ascorbic acid, or vitamin C, is an inexpensive, readily available essential nutrient that acts as an antioxidant and reactive oxygen species scavenger. On the other hand, hypertonic saline solution in the form of 3% normal saline solution can be used on a limited, intermittent basis. Army Institute of Surgical Research Joint Trauma System Burn Care Clinical Practice Guidelines. Additionally, vitamin C has been linked with oxalate nephropathy in nonburn populations and has recently been reported in postmortem examinations of burn patients treated with this adjunct. Therapeutic Plasma Exchange and Other Blood Purification Strategies Plasma exchange or plasmapheresis has been described as a therapy initiated in anticipation of difficult burn resuscitations or as a rescue therapy during burn shock. Retrospective studies in this population have demonstrated a decrease in the resuscitative fluid requirement, an increase in mean arterial blood pressure, an increase in urine output, and a decrease in lactate levels. During therapy plasma exchange necessitates replacement of the removed plasma volume with either albumin or plasma. Repeat treatments, which are often needed, place a significant strain on hospital resources over time. The main therapeutic target for such a therapy involves the indiscriminant removal of proinflammatory and antiinflammatory mediators, which are presumed to be profoundly dysregulated. Evidence suggests a potential clinical benefit of high-volume hemofiltration (doses >70 mL/kg per hour) in the treatment of circulatory shock in other clinical conditions. Regardless, it should be noted that this therapy is very difficult to carry out early in burn shock owing to the relative hemoconcentration. Hence, we recommend waiting until sufficient normalization of the hematocrit has occurred in the course of a burn resuscitation (hematocrit 35% to 40%). Resuscitation Morbidity As already discussed, a runaway resuscitation is associated with extreme edema in both burned and unburned tissue. Intensivists must understand the clinical implications and the interplay between this degree of edema against burned tissue and relatively nonexpandable regions of the body. The various types of resuscitation morbidity Hypertonic Saline Solution Hypertonic saline solution preparations have been advocated as an adjunct to avoid volume overload since the 1970s. The most widely reported preparation of hypertonic saline solution is hypertonic lactated saline solution. This preparation has 300 mEq/L of sodium, 88 mEq/L of chloride, and 212 mEq/L of lactate. Oda 1082 Pa rt 7 Physical and Toxic Injury in the Critically Ill Patient typically occur during the first 48 hours after the burn but can be delayed in presentation in some cases. Hence, intensivists must constantly be on guard and look for evidence of these complications, especially if patients are not following the typical trajectory of hemodynamic and end-organ recovery as burn shock is resolving. Airway Edema/Facial Swelling Endotracheal intubation is essential in those with evidence of thermal injury to the oropharynx primarily for airway protection. Edema of the glottis is often maximal at 24 to 48 hours and can persist for a few days. Thus it is very important during this period to assess the need for airway protection separate from the need for the ventilator. This is particularly important in those with isolated facial burns with upper airway injury. A patient may not need ventilator support for gas exchange, but he or she may need airway protection because of the risk of airway obstruction without the endotracheal tube. The decision to extubate must incorporate an assessment of airway edema and patency. In general, a review of the literature supports the use of a cuff leak volume of 110 mL as a standard cutoff to determine adequacy of the cuff leak below which postextubation stridor and reintubation rates are likely to be high. A cuff leak greater than 110 mL is associated with a very low likelihood of extubation failure with a specificity of 99% and negative predictive value of 98%. Treatment with a short course of steroids may be of benefit but has not been well studied in burns. For those in whom total body fluid overload is suspected, a trial of diuresis may be helpful. For those at great risk, extubation over an airway exchange catheter has been advocated, although this is technically challenging.
Order eulexin american express
Low hemoglobin at presentation is suggestive of either anemia that predated the bleed or bleeding that has been present for hours to days prostate cancer meaning cheap eulexin 250mg. Once equilibration has occurred, red cell indices should indicate a normochromic, normocytic anemia. The presence of a hypochromic, microcytic anemia suggests chronic blood loss from another source. Associated medical conditions or drug therapy may lead to an altered platelet count, coagulation parameters, or liver function tests. These conditions, while not responsible for diverticular bleeding, may contribute to its severity. Thus, each diverticulum has an associated arteriole, and mucosa is all that separates the vessel from the bowel lumen. Over time, due to recurrent exposure to injury, eccentric intimal thickening and thinning of the media may develop, leading to segmental weakness, predisposing the artery to rupture along its luminal aspect. This markedly increased propensity for right-sided diverticula to bleed may occur because right-sided diverticula have wider necks and domes, so a longer portion of the vasa recta is exposed to injury. Technetium sulfur colloid has a short half-life and thus can only detect bleeding that occurs within a few minutes of injection. This allows for repeated scanning of patients with intermittent bleeding over 24 hours. The major limitation of radionuclide scanning is that localization is imprecise and can only identify an area of the abdomen where the bleeding is occurring and not an exact site. Blood can move from the site of extravasation due to peristaltic or antiperistaltic motion, which can lead to inaccurate localization. Symptoms and Signs Patients typically present with moderate to large amounts of maroon stool or hematochezia. The bleeding is typically painless, although patients may Diverticular Disease of the colon 285 bleed). Performing a radionuclide scan prior to angiography may decrease the rate of negative examinations, but this may be counterbalanced by an increased rate of negative tests because of the delay introduced by performing the radionuclide scan prior to the angiography. If the initial study result is negative, the angiography catheter can be left in place for a short period to allow for rapid imaging if rebleeding occurs. Complications of angiography, which occur in 9% of patients, include arterial thrombosis, embolization, and renal failure. Plain abdominal films are not helpful in identifying a source of lower gastrointestinal hemorrhage, and barium enemas are contraindicated because the presence of barium interferes with the performance of angiography and colonoscopy. Endoscopy Colonoscopy is the initial examination of choice in the evaluation of lower gastrointestinal bleeding. Colonoscopy can be limited, however, by poor visualization due to retained blood and by the risks of sedation in an actively bleeding patient. Although some physicians will perform a colonoscopy in an unprepared bowel, relying on the cathartic properties of blood to empty the colon, many attempt to cleanse the colon either with enemas or with polyethylene glycol. Metoclopramide (10 mg intravenously) may help to control nausea and to increase gastric emptying. Although visualizing active bleeding is uncommon, a presumptive source can be identified through the visualization of an adherent clot or a mucosal lesion. Forty percent of patients with presumed diverticular bleeds demonstrate stigmata of recent hemorrhage, including a bleeding diverticulum, accumulation of fresh blood after clearing the colon, a nonbleeding visible vessel at the mouth of a diverticulum, or an adherent clot that cannot be dislodged with vigorous irrigation. Tagged red blood cell scan demonstrating bleeding originating in the right upper quadrant (arrow) along with pooling of the tagged red blood cells (arrowhead). For example, bleeding from a redundant sigmoid colon may incorrectly be attributed to the right colon. Although radionuclide scanning does not allow for therapeutic maneuvers, it can aid in directing subsequent angiography. Transvenous angiography has the advantage of being both diagnostic and therapeutic. If a prior study has suggested a possible location for the bleed, angiography starts with the injection of the appropriate feeding vessels. However, if prior localization is not available, sequential injection of the mesenteric arteries is performed, starting with the superior mesenteric artery, because the majority of bleeds arise from the right colon. If results are negative, the inferior mesenteric artery and, finally, the celiac artery are studied. The success rate is influenced by both the timing of the study relative to an episode of active bleeding and by the expertise of the radiologist performing the study. Colon cancer is the most common cause of lower gastrointestinal blood loss, but accounts for less than 10% of lower gastrointestinal hemorrhage. Rectal causes of lower gastrointestinal hemorrhage include ulcers, radiation proctopathy, varices, and Dieulafoy lesions. Rarely, inflammatory bowel disease can result in massive lower gastrointestinal hemorrhage. Although rectal bleeding is more common with ulcerative colitis, massive lower gastrointestinal hemorrhage is more common with Crohn disease. This observation may stem from the fact that Crohn disease is a transmural process and thus may involve larger submucosal vessels. Unlike patients with other causes of lower gastrointestinal hemorrhage, patients with inflammatory bowel disease usually have severe abdominal pain and tenderness. Patients should have large-bore intravenous access, such as a central venous catheter, or two 18-gauge peripheral intravenous lines. Blood transfusions are typically indicated in patients with massive bleeding and hemodynamic instability, since serum hemoglobin levels do not accurately reflect the degree of blood loss. For patients without massive bleeding, a more restrictive approach to transfusion may be appropriate. Ischemic injuries to the heart, brain, or kidneys are the most common manifestations, especially in the elderly. Diverticular Disease of the colon (<7 g/dL) for patients who do not have unstable coronary artery disease is associated with better outcomes. Patients with hemodynamic instability or with underlying cardiopulmonary disease should receive care in an intensive care unit. Endoscopic or angiographic interventions are then employed in an attempt to provide definitive therapy. If a bleeding source is identified endoscopically, therapy with injection of epinephrine (1:10,000 to 1:20,000) followed by thermal coagulation is recommended; if a nonbleeding visible vessel is seen, electrocautery alone can be applied. It is recommended that the multipolar electrocautery probe be applied to the vessel with mild to moderate pressure. If an adherent clot is noted, it is recommended that it be removed after the base is injected with epinephrine. The pedicle of the clot, once visualized, should be treated with electrocautery if active bleeding or a visible vessel is seen. If the bleeding vessel within a diverticulum cannot be identified, blind injection therapy with epinephrine can be carried out, or the mouth of the diverticulum can be closed with hemostatic clips. It is recommended that a tattoo or a hemoclip be placed at the site of the bleed in case there is recurrent hemorrhage requiring either repeat endoscopy or surgery. Patients treated with electrocautery should be monitored for signs of perforation.
Buy eulexin 250 mg low cost
This is true for both the symptom profile and pathophysiology of functional dyspepsia prostate abscess generic eulexin 250mg with mastercard. Although some epidemiologic studies have suggested an association between H pylori infection and functional dyspepsia, others have not. The discrepancy may stem in part from differences in methodology and lack of adequate consideration of confounding factors such as past history of peptic ulcer disease and socioeconomic status. Controlled trials disagree about whether or not H pylori eradication is beneficial in functional dyspepsia, with roughly half of the trials showing improvement and the other half no improvement. Despite the conflicting results, current guidelines by both major gastroenterological societies in the United States recommend H pylori test-and-treat as one of the first-line noninvasive strategies in management of patients with dyspepsia. Psychological Factors Psychosomatic and cognitive factors are important in the evaluation of patients with chronic dyspepsia. The psychiatric hypothesis holds that the symptoms of dyspepsia maybe due to depression, increased anxiety, or a somatization disorder. Epidemiologic studies suggest there is an association between functional dyspepsia and psychological disorders. Symptoms of neurosis, anxiety, hypochondriasis, and depression are more common in patients being evaluated for unexplained gastrointestinal complaints than in healthy controls. In addition, prior studies have demonstrated significant associations between dyspepsia symptoms and a history of abuse in childhood or adulthood. Comparisons of functional and organic dyspepsia have shown that patients with functional dyspepsia are less likely to have decreased stress or anxiety at 1-year follow-up after being reassured of having no serious disease. This suggests that functional dyspepsia symptoms are long-lasting, compared with those of organic dyspepsia, and that the emotional ties are strong. A community-based, controlled study of the epidemiology and pathophysiology of dyspepsia. A prospective 1-year follow-up study in patients with functional or organic dyspepsia: changes in gastrointestinal symptoms, mental distress and fear of serious illness. Gastrointestinal tract symptoms and self-reported abuse: a population-based study. An update of the Cochrane systematic review of Helicobacter pylori eradication therapy in nonulcer dyspepsia: resolving the discrepancy between systematic reviews. Symptoms and Signs the initial clinical evaluation should focus on symptom characteristics, onset, and chronicity. Important history to obtain include comorbidities, surgical history, family history of upper gastrointestinal malignancy, alcohol and tobacco use, dietary changes or allergies, stressful life events, and psychological factors. In most cases, however, the clinical history is of limited use in distinguishing organic causes from functional dyspepsia. A large systematic review of the literature was performed to evaluate the effectiveness of diagnosing organic dyspepsia by clinical opinion versus computer models in patients referred for upper endoscopy. The computer models were based on patient demographics, risk factors, historical items, and symptoms. The study showed that neither clinical impression nor computer models were able to adequately distinguish organic from functional disease. In a recent study, patients with peptic ulcer disease were compared with patients with functional dyspepsia in an ageand sex-matched study. Although the functional dyspepsia group reported more upper abdominal fullness and nausea and overall greater distress and anxiety, almost all the same symptoms were seen in both groups. However, the utility of these features in identifying the presence of upper gastrointestinal malignancy has been debated. Although this finding is nonspecific, several features may shed lights on possible underlying etiologies. A positive Carnett sign, or focal tenderness that increases with abdominal wall contraction and palpation, suggests an etiology involving the abdominal wall musculature. Cutaneous dermatomal distribution of pain may suggest a thoracic polyradiculopathy. A review of gender differences in epidemiology, pathophysiologic mechanism, clinical presentation and management. Diagnostic Evaluation If a careful history and physical examination, along with judicious use of screening laboratory tests, does not lead to the diagnosis, then other studies with specific management strategies are recommended. Special consideration may also be given to patients whose country of origin is a region where stomach cancer is more prevalent (eg, Japan, China, and Chile). A recent study of 2741 dyspeptic patients without alarm features in the United States found a low prevalence of cancer (0. Patients who respond to the H pylori testing and treatment strategy, outlined below, can be managed without further investigation. In younger patients with continued symptoms despite this strategy, endoscopy usually adds little more to the diagnostic workup. Furthermore, the utility of endoscopy in reassuring patients with functional dyspepsia has been studied and deemed questionable as measured by anxiety and depression, which did not change before and after the procedure in these patients. Cost of detecting malignant lesions by endoscopy in 2741 primary care dyspeptic patients without alarm symptoms. Upper gastrointestinal endoscopy does not reassure patients with functional dyspepsia. American Gastroenterological Association medical position statement: evaluation of dyspepsia. Helicobacter pylori testing-For patients younger than 55 years and without alarm features, the clinician should first consider testing for H pylori and treating, if positive. Patients with biliary-type pain with findings of gallstones should be considered for cholecystectomy. A quantitative cholescintigraphy scan with cholecystokinin challenge may suggest chronic cholecystitis as the diagnosis if the ejection fraction is less than 50%. Gastric scintigraphy usually does not add much more information to the diagnostic picture. Limited value of alarm features in the diagnosis of upper gastrointestinal malignancy: systematic review and meta-analysis. The findings from history and physical examination and judicious use of the diagnostic studies outlined in the preceding section can aid in distinguishing the various organic causes of dyspepsia from functional dyspepsia. Cholelithiasis usually is distinguishable from dyspepsia in being more localizable to the right upper quadrant. In a study of 186 functional dyspepsia patients with 24-hour pH monitoring study, 31. Patients with the postprandial distress syndrome subtype and the epigastric pain syndrome subtype have 36. Motility Disorders Upper gastrointestinal motility disorders also overlap with dyspepsia. Nonetheless, there is a preponderance of symptoms of bloating, early satiety, and nausea with vomiting in patients with functional dyspepsia. Causes of motility disturbance may include diabetic gastroparesis, chronic intestinal pseudo-obstruction, scleroderma, or postvagotomy syndromes. Systemic Disorders Dyspepsia may exist in a number of systemic disorders such as diabetes mellitus, coronary artery disease, thyroid disease, hyperparathyroidism, adrenal insufficiency, and collagen vascular diseases. Peptic Ulcer Disease About 15% of patients with dyspeptic symptoms have gastric or duodenal ulcers. Small intestinal bacterial overgrowth is associated with nonspecific symptoms such as bloating, gassiness, and abdominal discomfort that may emulate dyspepsia and is increasingly identified.
Cuscuta epithymum (Dodder). Eulexin.
- Are there safety concerns?
- How does Dodder work?
- Bladder, liver, and spleen problems.
- Dosing considerations for Dodder.
- What is Dodder?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96067
Discount eulexin 250mg amex
Imagine having a single type of ventilator; it means one type of spare parts mens health cover model 2013 buy 250mg eulexin fast delivery, one type of accessories, one reservoir of clean machines on standby for use, and one type of training cost. This should not suggest slavish dependence on a single source for essentials, but it does suggest that purchasing in bulk consistently provides unique leverage at many points in the care continuum, which is only partially reflected in the purchase contract price. The third imperative-fiscal responsibility-requires skills that are typically neither taught nor learned until ascent to a leadership position. Nonclinical administrators typically introduce that third imperative into the conversation with allusions of "building value" and "improving performance. Understanding Standardization Standardization-better thought of as removing unnecessary variation-can apply to people, processes, equipment, and supplies. Critical care professionals are trained more to competencies and less to standards. There are neither expectations nor restrictions on specific sequences provided that the key findings are gleaned and reported. Although most practitioners develop a consistent routine, there is no agreed-upon "one best way. The range of processes available to standardize is vast and far exceeds the time and effort available. If the outcome is not critical, will standardization reduce costs or improve satisfaction None of this is easy- witness the difficulty in standardizing a process that should be easy and has great impact on safety-namely, handwashing. Although cash incentives are effective, even small tokens like coffee cards and candy bars are powerful tools to change behaviors. If there are several types of ventilators, spares and repairs and skills must be maintained for all types. Similar to all durable equipment, from beds, to defibrillators, to monitors, to ultrasound machines, the consumables add up as well. A tour through the "clean utility room" often reveals near-identical kits and, worse, items that expire through lack of regular use. Equipment and supplies often represent the first and easiest targets for standardization. Some tasks have "sunsetted" owing to technological advancements, such as the filing of laboratory data and imaging reports into physical charts. Others are candidates for simplification and automation, such as the recording of intravenous fluid administration that can be automated via device integration. We do not mean to suggest a wholesale revision of workflows, but rather a critical examination of the value stream and the assignment of each team member to the specific tasks. Quite the opposite-there should be a leadership team that visibly embodies the behaviors expected of the workforce. At a minimum, this demands a partnership between the nurse unit director and the physician unit director. Set standards high and goals higher; demand the former and incentivize the latter. For example, there should be standards of family visitation, hand hygiene, use of universal precautions, and timely administration of antibiotics when sepsis is suspected. Such general standards do not preclude local additions that are necessarily focused in particular units-for example, adherence to practices regarding extraventricular drains in neurology units and intraaortic balloon pumps in cardiac units. Rather, the mechanisms by which those general standards are communicated, compliance evaluated, and corrected provide a foundation for unit-specific behaviors. Albumin utilization was also decreased over a 2-year intervention with an estimated savings of $2. Interestingly, although the physicians were ineligible for this incentive, their billable time increased from 4. The tasks can be further divided into those that must be performed at the bedside. An alternate division of tasks relates to the profession(s) qualified to complete the task. The aforementioned bladder catheter could be inserted by a physician, an advanced practice provider, a nurse, or a specialized catheter insertion "team. Insertion of peripherally inserted central venous catheter line teams is one example of a task where constant repetition seems to improve outcomes. The process of charting, for example, can be accelerated with voice recognition transcription or use of a scribe. Monitoring of vital signs, laboratory data, and medication interactions can be performed remotely. A list of domains that have formed the bases for recent incentives is included in Table 70. We will neither review nor dwell on "burnout," a construct that is increasingly applied to critical care among the many medical professions. Although most critical care professionals find their work deeply satisfying, they are no different than the general population in being susceptible to depression, fatigue, isolation, and other common threats to mental health. One area in which critical care professionals may differ from the general population is their chronic and repeated professional exposure to emotionally stressful situations. We hasten to add that critical care professionals knowingly choose such exposures when they join the professions, yet only a fraction experience burnout syndrome. Although compensation is important, a sense of teamness and of a "work family" sharing the joys and burdens may play heavily into decisions by an employee to remain or depart. Those who report burnout emphasize isolation, depersonalization, and emotional exhaustion. Thus attention to well-being cannot be a response to crises but rather must be engineered into the fabric of daily work. By 2030, nursing shortage ratios will be largest in the Western portion of the United States, followed by the South, Midwest, and Northeast regions. Ninety-eight percent of nurses believed that the shortage would increase stress on nurses, 93% indicated it would lower quality of care, 93% reported it would cause nurses to leave the profession, and only one-fifth believed that their working conditions would improve or that respect for nurses would increase. We have deployed tele-critical care to leverage our scarce experienced physicians and critical care nurses, thereby enabling guidance on demand. The patient may be enrolled in a protocol related to the primary illness for which critical care is incidental. For example, patients with sepsis might be randomly assigned to receive a placebo or a study drug in addition to standard care. Failure to do so may result in protocol violation, patient injury, and study interruption. This section briefly reviews the convergent training pathways and the role of the administrator in facilitating effective learning toward practice. This section omits consideration of formal training in critical care research, except where such training is needed to prepare bedside professionals to participate in clinical research trials. Pathways to Degrees, Licensure, Certification, and Credentialing Although the professions of critical care are diverse, there are homologies among the paths to competency. For this largest cohort of learners, administrators must ensure that learners are constantly accompanied by teacher/supervisors; that appropriate confidentiality agreements are in place; and that the role of the learner is appropriately restricted (often to observation and unofficial "student" entries into the medical record). In general, licensure is sufficient to qualify for some care privileges, although there are nuances. For example, a newly graduated physician may qualify for limited licensure as a trainee provided he or she is supervised in an accredited postgraduate training program. A newly graduated physician assistant will have one or more supervising physicians. The administrator has three typical tasks associated with mentorship of the newly licensed professional: (1) verifying the existence of a training plan; (2) verifying the assignment of one or more supervising mentors, including clarification of the roles and responsibilities of trainee and mentor; and (3) monitoring completion, including an objective determination from the responsible individuals that training is satisfactory and complete and further an attestation that the trainee can practice independently. Whereas licensing is a regulatory and legal matter, certification by a board representing that profession validates not only that the individual has completed a prescribed course of training but also that certain advanced competencies have been evaluated and found satisfactory, typically by an examination that may be written, oral, simulated, or a combination thereof. Of note, certification by a board occurs not only at different stages across professions but also can occur at different experience levels within a profession. For example, boardcertified internal medicine physicians require 2 to 3 years of postgraduate training to complete critical care medicine training and enter the examination process, whereas board-certified surgeons and anesthesiologists require a single additional year of critical care medicine training.
Purchase eulexin 250mg mastercard
Blood culture-Blood cultures should be obtained from patients with high fever prostate lump generic eulexin 250mg line, those with shaking chills, and those who are immunosuppressed. Stool examination for ova and parasites-The yield of positive examinations for ova and parasites is low among patients with acute diarrhea as most parasitic infestations that cause diarrhea cause symptoms lasting several weeks or more. As ova and parasites can be passed intermittently, optimal testing requires prompt examination of each of three specimens collected on separate days. Clostridium difficile toxin-The recently reported rising incidence and increased morbidity and mortality of C difficile colitis (see later discussion) underscores the importance of C difficile toxin testing of the stool for timely diagnosis and implementation of therapy for this important disease. Community-acquired cases even in the absence of known recent antibiotic use are being increasingly recognized. Endoscopy and Biopsy Sigmoidoscopy and biopsy can be very useful in selected patients with acute diarrhea. Sigmoidoscopy can also help exclude ischemic colitis, which may present with abdominal pain and bloody diarrhea. Additionally, sigmoidoscopy can provide rapid diagnosis of amoebiasis if secretions from the edge of ulcers are examined microscopically and the organism is seen. Mucosal biopsy from immunosuppressed patients may detect cytomegalovirus or herpetic proctocolitis. Upper endoscopy is indicated in patients with persistent diarrhea and malabsorption and, through examination of duodenal aspirates and mucosal biopsies, may detect parasitic infections including giardiasis, cryptosporidiosis, Cystoisospora infection, and occasionally strongyloidiasis. Imaging Studies Imaging studies are usually not required in patients with uncomplicated acute diarrhea. An abdominal flat and upright film may be useful if there is worrisome abdominal distention in order to screen for toxic megacolon, which can occur in C difficile colitis and colonic amoebiasis. Some clinicians favor preparations formulated with complex carbohydrates such as rice-based solutions (CeraLyte). Intravenous hydration is often overutilized in developed countries such as the United States. However, if diarrhea is massive and dehydration severe, especially in infants and young children, the elderly, and patients unable to rehydrate orally due to nausea, vomiting, or other comorbidities, intravenous rehydration is indicated. Antidiarrheal Drugs the antimotility agent loperamide can be used with caution to provide symptomatic relief in patients without high fever, colonic distention, or dysenteric stools. Absorption may be increased by prolonging contact time of luminal contents with mucosa, although oral fluid intake should be continued. Fluid may pool in the gut lumen as antimotility agents do not decrease intestinal secretion. Diphenoxylate has also been used but is less desirable as it crosses the bloodbrain barrier and has central opiate actions. Antimotility drugs should generally be avoided in patients with dysentery, and no antimotility drug should ever be used if the possibility of toxic megacolon is a concern. Bismuth subsalicylate reduces stool number, but there is no evidence that fecal fluid losses are decreased significantly. General Principles Some general principles of treatment of acute diarrhea are summarized next. When specific therapy of a defined cause of acute diarrhea is indicated as, for example, for C difficile colitis, such treatment is described later, in the section titled "Acute Diarrheal Disease Caused by Specific Infections. Treatment of Dehydration Oral rehydration therapy will suffice in most patients who develop acute diarrhea. In milder cases, juices, broth, and water along with salted crackers usually suffice. Empiric Antibiotic Therapy Although a controversial topic, antibiotics are overutilized in acute infectious diarrhea. Others produce tissue-damaging cytotoxins while in the lumen and in contact with the epithelium. Still others elaborate enterotoxins that produce profound functional alterations but no detectable histologic lesion. Some adhere to the epithelial surface and induce epithelial damage and mucosal inflammation without invasion. Finally, still others produce toxins in vitro that, when ingested, induce symptomatic gastrointestinal illness. Gastric acid secretion reduces bacterial colonization of the proximal small intestine, and there is evidence that individuals who have had acid-reducing gastric surgery are more susceptible to nontyphoidal salmonellosis and selected other enteric infections. Normal gastric motility is a defense factor; stasis predisposes to intestinal intraluminal bacterial proliferation, and there is evidence that the use of antimotility agents prolongs diarrhea caused by some enteric pathogens. Its alteration by antibiotic therapy predisposes to C difficile colitis and reduces the number of organisms required to produce nontyphoidal salmonellosis. Antibodies secreted into the intestinal lumen by the intestine and via the biliary tract appear to play a protective role in reducing colonization of pathogens in the gut. Their benefit in Yersinia, Campylobacter, and Aeromonas infections is controversial. Quinolones are widely used for empiric treatment; macrolides such as azithromycin or erythromycin and, for travelers, rifaximin are alternatives. Specific Antibiotic Therapy Recommendations regarding antibiotic therapy for specific pathogens that cause acute infections are discussed in the next section. Mechanisms Invasive Examples Rotavirus Campylobacter Salmonella Shigella Clostridium difficile Enterohemorrhagic Escherichia coli Vibrio cholerae Enterotoxigenic E coli Enteropathogenic E coli Giardiasis Bacillus cereus Staphylococcus aureus 1. With advent of effective rotavirus vaccines, norovirus disease is now the most common cause of viral gastroenteritis in children as well as adults. Epidemic outbreaks in hospitals, nursing homes, in schools from catered food, in restaurants, and on cruise ships have been widely publicized, but endemic cases also occur. Transmission is via the fecal-oral route through contaminated food and water, from virus-contaminated environmental surfaces, and direct person-to-person contact. After ingestion, noroviruses bind to histo-blood group antigens on the enterocyte surface. The histo-blood group antigens are a major determinant of host susceptibility; nonsecretors are resistant to infection by a majority of strains of norovirus. Attempts to develop an effective vaccine are ongoing and some early phase 2 studies are encouraging. The prognosis is excellent for this generally self-limited disease, although deaths may occur in association with norovirus gastroenteritis, largely in debilitated, elderly patients with significant comorbidities or in very young children. Rotaviruses Rotaviruses are a major cause of infectious diarrhea worldwide, accounting for an estimated 500,000 or more deaths each year. In the United States, prior to the widespread use of rotavirus vaccines, approximately 2. However, there is increasing evidence that with the introduction of effective vaccines in 2006, the incidence of rotavirus infection has decreased dramatically by over 80%. There are several groups, which, in turn, may contain subgroups and multiple serotypes. Significant enteritis develops, with patchy shortening or even complete loss of villi, crypt hyperplasia, and inflammation of the lamina propria. Symptomatic illness is more common in winter and occurs largely in infants and young children. Watery diarrhea, which can be profuse, and vomiting are the major symptoms, accompanied by fever in 50% or more of cases. Reinfections in older children and adults are usually asymptomatic or mild but can occasionally cause severe symptoms. Dehydration is a hazard-especially in infants, if diarrhea is accompanied by vomiting that precludes adequate oral fluid intake-and is the major cause of morbidity and death.
250 mg eulexin
It comprises 60% of the cytosolic protein in neutrophils and is stable in the stool for 7 days mens health getting abs pdf purchase eulexin 250mg with amex. Both appear to be promising markers for monitoring therapy as well as surrogates for mucosal healing. Future drug trials are incorporating these markers and will hopefully lead to improved coverage. Nine genes involved in Crohn disease have been implicated in dysregulation of adaptive immunity. Thirteen genes have been associated with ulcerative colitis by gene array studies. Imaging studies-Standard abdominal plain films are useful for detecting obstructive disease and megacolon, but otherwise have a limited role in imaging Crohn disease. Small bowel series are useful for imaging small bowel mucosal disease, including strictures, ulcerations, and fistulae. Enteroclysis, although more sensitive, is limited by patient discomfort, increased radiation exposure, and its technically demanding nature. Barium enema remains an option for imaging colonic disease, especially to help delineate obstructive or fistulizing disease. Common abnormalities of the gut include thickening and excessive mesenteric fat proliferation (so-called creeping fat). Other significant advantages include lack of ionizing radiation and, importantly, comprehensive evaluation of the perianal region. Colonoscopy remains a mainstay in the assessment of Crohn disease, as it allows direct visualization of the bowel mucosa and sampling of tissue. Ileal ulceration and skip lesions help distinguish Crohn disease from ulcerative colitis. Endoscopic ultrasound, as previously mentioned, is useful in delineating perianal disease. Capsule ("pill") endoscopy has been revolutionary in terms of allowing direct visualization of the small bowel in Crohn disease. The most common finding is ulceration, ranging from shallow aphthous-type to deep "punched-out" lesions. Strictures may also be encountered, occasionally causing pill retention and subsequent obstruction. Symptoms and signs-As with Crohn disease, the symptoms of ulcerative colitis depend on the extent and severity of inflammation. Overt rectal bleeding and tenesmus are virtually universally present and may be the only symptoms in patients with proctitis alone. When the proximal colon is involved, diarrhea and abdominal pain are more frequent complaints. Signs of ulcerative colitis include mild abdominal tenderness, often most localized in the hypogastrium or left lower quadrant. Laboratory findings-Patients with active disease are generally anemic and often iron deficient. Hypoalbuminemia suggests extensive disease with subsequent colonic protein losses. Stool studies should be sent and found negative for typical bacterial pathogens, C difficile, and ova and parasites. Common positive findings in ulcerative colitis include fecal leukocytes and fecal lactoferrin. However, as previously mentioned, it is also present in Crohn colitis, which limits its ability to distinguish the two conditions. Ulcerative Colitis Unlike Crohn disease, inflammation in ulcerative colitis is limited to the mucosal layer of the colon. The rectum is virtually always involved, with inflammation extending proximally in a confluent fashion. A significant proportion of patients have disease confined to the rectum (ulcerative proctitis). Roughly one-third of patients have proctosigmoiditis, and the majority of patients have gross colitis only distal to the splenic flexure. Approximately one-third of patients have disease that extends proximal to the splenic flexure (extensive colitis), often involving the entire colon (pancolitis or universal colitis). On occasion, a so-called cecal patch of periappendiceal inflammation is encountered. Similarly, limited ileal involvement (backwash ileitis) can be seen in patients with ulcerative colitis who have pancolonic disease. Deep ileal ulcers, long segments of ileal involvement, or stricturing disease are consistent with Crohn disease and not ulcerative colitis. Although confluent disease involving the rectum is the rule in ulcerative colitis, patients on medical therapy, particularly topical therapy, may have apparent skip lesions or rectal sparing. This should be recognized as a treatment effect and not a manifestation of Crohn disease. Unlike Crohn disease, ulcerative colitis is frequently acute or subacute in onset. Like Crohn disease, the subsequent clinical course is one of recurring episodes of symptomatic disease interspersed with episodes of relative (or complete) quiescence. Imaging studies-Plain films of the abdomen are useful predominantly in patients with symptoms of severe or fulminant colitis. So-called thumbprinting or thickening of the colon wall indicates severe colitis with bowel wall edema. Intestinal pneumatosis is a late finding and signals bowel ischemia and infarction. Obstructive findings are less common in ulcerative colitis than in Crohn disease and usually suggest malignancy. Barium enema is less commonly used since the advent of flexible sigmoidoscopy and colonoscopy. Nonetheless, it can be useful for detecting active ulcerative disease, polyps, or masses. Small bowel disease is not present, other than perhaps mild ileal inflammatory changes. Colonoscopy allows assessment of the extent of disease and severity of involvement. Classic findings include confluent inflammation extending proximally from the anal verge, with mucosal erythema, edema, and granularity and loss of normal vasculature. With more severe disease, the mucosa becomes overtly hemorrhagic, with ulcerations and a purulent exudate. So-called backwash ileitis, characterized by mild terminal ileal erythema, is seen in patients who have pancolitis. These are polypoid nondysplastic colonic lesions of hypertrophied tissue, often with surrounding atrophic mucosa. They are thought to represent the sequelae of chronic recurrent inflammation and healing, and harbor no malignant potential. Dysplastic or frankly malignant polyps or mass lesions are also encountered at higher rates in patients with ulcerative colitis. Both pseudopolyps and colitisassociated neoplastic lesions are also seen in patients with Crohn disease. Flexible sigmoidoscopy is a useful tool for disease assessment in the setting of flares of colitis. In this setting, a full colonoscopy is typically overly cumbersome for the patient and may carry an undue risk of perforation in patients with severe colitis. Flexible colonoscopy can assist with assessment of disease severity and help to exclude alternative diagnoses, such as infectious or ischemic colitis. Common enteric bacterial pathogens, such as Campylobacter, Salmonella, Shigella, and Escherichia coli, can cause an infectious colitis characterized by abdominal pain, diarrhea, and hematochezia. The E coli serotype O157:H7 is of particular note due to its propensity to produce a hemorrhagic colitis that may closely mimic fulminant ulcerative colitis. Campylobacter, Salmonella, Shigella, and Yersinia can cause an ileitis, which may mimic the radiographic appearance of Crohn disease. Yersinia is particularly notable for its predilection for the terminal ileum and cecum.
Eulexin 250 mg line
Adrenal insufficiency in patients with cirrhosis and septic shock: effect of treatment with hydrocortisone on survival prostate oncology 77030 cheap eulexin 250 mg fast delivery. Short-term prognosis in critically ill patients with cirrhosis assessed by prognostic scoring systems. Risk factors, sequential organ failure assessment and model for end-stage liver disease scores for predicting short term mortality in cirrhotic patients admitted to intensive care unit. Development and validation of a prognostic score to predict mortality in patients with acute-on-chronic liver failure. Prognostic evaluation of early indicators in fulminant hepatic failure by multivariate analysis. Changing patterns of causation and the use of transplantation in the United Kingdom. Results of a prospective study of acute liver failure at 17 tertiary care centers in the United States. Circulating markers of endothelial activation in acetaminophen induced acute liver failure. Intravenous acetylcysteine in paracetamol induced fulminant hepatic failure: a prospective controlled trial. Persistence of hepatitis A virus in fulminant hepatitis and after liver transplantation. Appearance and persistence of hepatitis A IgM antibody in acute clinical hepatitis A observed in an outbreak. Hepatitis B virus strains with mutations in the core promoter in patients with fulminant hepatitis. Factors associated with fulminant liver failure during an outbreak among injection drug users with acute hepatitis B. Management of severe acute to fulminant hepatitis B: to treat or not to treat or when to treat Prevalence and clinical outcome of hepatitis C infection in children who underwent cardiac surgery before the implementation of blood-donor screening. Current issues and treatment of fulminant hepatic failure including transplantation in Hong Kong and the Far East. A 20-year single-center experience with acute liver failure during pregnancy: is the prognosis really worse Outcomes following liver transplantation for seronegative acute liver failure: experience during a 12-year period with more than 100 patients. Liver autoimmune serology: a consensus statement from the committee for autoimmune serology of the International Autoimmune Hepatitis Group. Indications for referral and assessment in adult liver transplantation: a clinical guideline. Fulminant hepatic failure in pregnant women: acute fatty liver or acute viral hepatitis Outcomes of severe pregnancy-related liver disease: Refining the role of transplantation. Reversible peripartum liver failure: a new perspective on the diagnosis, treatment, and cause of acute fatty liver of pregnancy, based on 28 consecutive cases. Liver transplantation for Budd-Chiari syndrome: a European study on 248 patients from 51 centres. Veno-occlusive disease of the liver and multiorgan failure after bone marrow transplantation: a cohort study of 355 patients. Fulminant liver failure due to severe veno-occlusive disease after haematopoietic cell transplantation: a depressing experience. Acute liver injury and acute liver failure from mushroom poisoning in North America. Neomycin-sorbitol and lactulose in the treatment of acute portal-systemic encephalopathy. Serum phosphate is an early predictor of outcomeinsevereacetaminophen-inducedhepatotoxicity. Blood lactate but not serum phosphate levels can predict patient outcome in fulminant hepatic failure. Staggered overdose pattern and delay to hospital presentation are associated with adverse outcomes following paracetamol-induced hepatotoxicity. Regional cerebral blood flow during mechanical hyperventilation in patients with fulminant hepatic failure. Circulatory, respiratory, cerebral, and renal derangements in acute liver failure: pathophysiology and management. Early death from paracetamol (acetaminophen) induced fulminant hepatic failure without cerebral oedema. Worsening of cerebral hyperemia by the administration of terlipressin in acute liver failure with severe encephalopathy. Comparison of terlipressin and noradrenalin on cerebral perfusion, intracranial pressure and cerebral extracellular concentrations of lactate and pyruvate in patients with acute liver failure in need of inotropic support. Hemodynamics and metabolic studies on septic shock in patients with acute liver failure. The effects of supraphysiological doses of corticosteroids in hypotensive liver failure. Controlled trials of charcoal hemoperfusion and prognostic factors in fulminant hepatic failure. Introduction to the revised American Association for the Study of Liver Diseases Position Paper on acute liver failure 2011. High-volume hemofiltration in the intensive care unit: a blood purification therapy. High-volume continuous veno-venous haemofiltration in hyper-acute liver failure: a pilot study. Clinical review: optimal dose of continuous renal replacement therapy in acute kidney injury. High-dose renal replacement therapy for acute kidney injury: systematic review and meta-analysis. Hyperlactataemia and metabolic acidosis during haemofiltration using lactate-buffered fluids. Blood lactate as an early predictor of outcome in paracetamol-induced acute liver failure: a cohort study. Dialysate and substitution fluids for patients treated by continuous forms of renal replacement therapy. Intracranial pressure monitoring in patients with acute liver failure: a questionable invasive surveillance. Cerebral herniation in patients with acute liver failure is correlated with arterial ammonia concentration. Predictive value of arterial ammonia for complications and outcome in acute liver failure. Electron microscopic evaluation of brain edema in rabbits with galactosamine-induced fulminant hepatic failure: ultrastructure and integrity of the bloodbrain barrier. Electron microscopic study of brain capillaries in cerebral edema from fulminant hepatic failure. Inhibition of brain glutamine accumulation prevents cerebral edema in hyperammonemic rats. Glutamine, myo-inositol, and organic brain osmolytes after portocaval anastomosis in the rat: implications for ammonia-induced brain edema. Cerebral hemodynamic and metabolic profiles in fulminant hepatic failure: relationship to outcome. Liver function, cerebral blood flow autoregulation, and hepatic encephalopathy in fulminant hepatic failure. The effect of indomethacin on intracranial pressure, cerebral perfusion and extracellular lactate and glutamate concentrations in patients with fulminant hepatic failure. Neuroinflammation in acute liver failure: mechanisms and novel therapeutic targets.