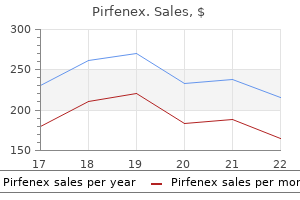
Order pirfenex 200 mg with mastercard
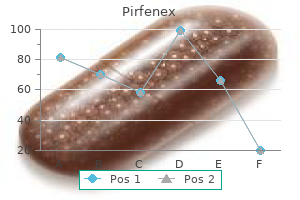
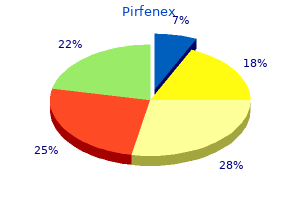
If the patient is otherwise stable symptoms you may be pregnant cheap pirfenex 200mg on-line, two units of red cells should be transfused in adults (or the equivalent in children according to size) and then the clinical situation and haemoglobin concentration should be reassessed. The correct strategy for transfusion of patients with haemoglobin concentrations between 7 and 10 g/dL is less clear. Clinicians often transfuse red cells, although the available evidence suggests this is not often justified. A study in the United States concluded that transfusion is no longer necessary during routine bimaxillary orthognathic surgery4 and another study found that using hypotensive anaesthesia and consistent surgical techniques, 0. Conditional use of fresh frozen plasma In cases of massive transfusion (45 L in 24 hours), dilution of clotting factors may occur. Subsequent therapy should be based on repeat coagulation tests and with the guidance of haematological colleagues. Vitamin K deficiency Patients who present to surgical teams with biliary obstruction may have impaired absorption of the fat soluble vitamin K and therefore have a deficiency of vitamin K-dependent coagulation factors. Chapter 21 Blood groups, blood components and alternatives to transfusion Table 21. Withdraw warfarin for 1 or 2 days then review Investigate possibility of underlying cause such as unsuspected renal or alimentary tract disease nutritional support/protein loss states; plasma exchange procedures, unless there is an underlying coagulopathy. Platelet concentrates have made a major contribution to modern clinical practice, in particular in allowing the development of intensive treatment regimes for haematological and other malignancies. Platelet collection and storage Platelet concentrates are produced either by pooling platelets derived from four separate donations of whole blood or as single donor platelets which are obtained by apheresis. However, the shelf-life is limited to five days because of the risk of bacterial proliferation at this storage temperature. Sepsis secondary to platelet transfusion is more common than red cell infusion and therefore platelets should only be used when necessary. Indications for platelet transfusion the cause of thrombocytopenia should be established as soon as possible so that the most appropriate treatment can be given and so that platelets are not given in conditions where they could cause harm. Prior to a procedure, it is essential to repeat the platelet count after platelets have been transfused to ensure an adequate increment has been achieved. In such cases, platelet transfusion has been associated with acute arterial thrombosis. Therefore, all platelets in particular, should be checked at all stages, including at the bedside, for any possible leak or damage to the bag. Any change of colour or turbidity must be regarded as suspicious of contamination and discussed with the transfusion laboratory. Additionally, prion proteins have been located on the membranes of lymphocytes and platelets and in lymphoreticular tissue. Blood donation is voluntary so that there are no incentives for donors to withhold information about their health and put patients or themselves at risk. The avoidance of the transmission of infection to the recipient of blood products is of paramount importance in transfusion medicine. Clinically, the patient experiences headache, lumbar back pain, chest tightness, nausea or facial flushing. They often result in mild urticarial reactions and are usually treated with an antihistamine with or without hydrocortisone. These may be seen in patients who are deficient in IgA, who may make anti-IgA antibodies, which can react with IgA normally present in blood components, causing anaphylaxis. In known IgAdeficient patients undergoing surgery, it is important that the haematology department is told well in advance of any elective procedure as it requires planning in order to have an IgA-deficient donor or washed products on standby. Management of the patient is again by resuscitation and plain fluids and treatment of any renal failure. This is thought to be due to release of cytokines during storage, but has not been prevented totally by leukodepletion. Hypocalcaemia, due to citrate anti-coagulant in stored blood, does not usually require treatment. Such reactions usually occur between seven and ten days post-transfusion and may manifest as a mild anaemia, a rise in serum bilirubin level and often an accompanying fever. The drop in haemoglobin is proportional to the quantity of red cells transfused, i. Any patient with a haemoglobinopathy, who is due to undergo surgery, should be discussed jointly with both the haematologist and anaesthetist well in advance of any procedure. Such technologies may be useful for individual patients who decline transfusion on the grounds of religious teachings and beliefs. This section will concentrate primarily on alternatives to allogeneic red cell transfusion. The resulting platelet destruction occurs in both autologous and transfused platelets due to cross-reaction or by the formation of immune complexes. Platelet transfusion is unhelpful and not warranted unless life-threatening bleeding occurs. The differential diagnosis postoperatively often includes heparin-induced thrombocytopenia. Patients who are fit enough to donate blood, can take oral iron supplements and donate one unit (450 mL) of blood at weekly intervals in the four weeks leading up to surgery, provided their haemoglobin recovers adequately between weekly donations. These donations are then subject to the same storage and handling procedures as for other donated units but kept solely for the use of the donor at a subsequent time. Such a procedure requires considerable planning and liaison between surgical firms and the local blood service. The other pitfall of autologous donation in clinical practice, is that as the amount of blood that can be used from autologous donation is limited, complications at the time of the planned procedure may mean that allogeneic transfusion may be needed in addition. Autologous transfusion in clinical practice is also limited by the five-week shelf-life of red cells so that if surgery is postponed, the blood expires. Such products are interesting prospects in that they would remove the risk of bacterial, viral and prion transfusion. Unfortunately, at the present time, such preparations are of limited clinical use in areas of acute trauma resuscitation mainly became of their relatively short half-life of around 24 hours. Such preparations are only currently on limited licences in the United States and South Africa. Blood lost can be salvaged either (1) during surgery: intraoperative cell salvage, which requires expensive equipment to suction, anticoagulate, wash, centrifuge and filter the blood or (2) after surgery: postoperative cell salvage, which requires just a modified drain, in which blood is collected for six hours then simply filtered and reinfused. These techniques can be used in a variety of surgical operations, but generally, intraoperative cell salvage is used only where 41 L blood loss is likely and neither is appropriate where the surgical field is bacterially contaminated. Therefore, their application in the clinical arena is limited to situations such as intensive therapy where patients can be highly monitored. Overall, there is a range of measures that can be taken to avoid the use of allogeneic blood where required, but many require planning ahead and liaison in advance with haematologists is advisable. It can be used in the weeks prior to surgery in patients in whom transfusion with allogeneic blood would be a problem. Other alternative treatments to avoid the use of allogeneic blood are directed at reducing blood loss. In an emergency, indicate how long until blood is needed at the bedside, so that the laboratory staff can curtail testing if the clinical balance of risks warrants it Preoperative assessment and correction of anaemia can reduce perioperative transfusion. One syringe containing calcium and human thrombin and another containing human fibrinogen are mixed directly when injected simultaneously at the point of bleeding. Indication, incidence and management of blood transfusion during sinus surgery: a review over 12 years. Average blood loss and the risk of requiring perioperative blood transfusion in 506 orthognathic surgical procedures. There is a lack of, and a need for, good clinical trials to understand when transfusion will be effective. These could then facilitate a balanced approach to risk reduction which could be understood and accepted by a well-informed public. Many diseases affecting the ear, nose and throat or their treatments may have significant haematological effects.
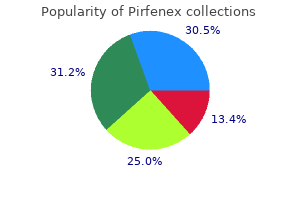
Order 200 mg pirfenex mastercard
In patients with a history of a seizure disorder as well as those with preeclampsia treatment yeast infection home remedies purchase pirfenex uk, careful observation for particular seizure precursors is maintained. However, many patients who seize on labor and delivery have no history and may be normotensive. One of the key ways to differentiate between the two is the presence of a postictal period after the event. Current tocolytics are only marginally effective, but may buy time for a course of betamethasone to accelerate fetal lung maturity. Breech presentations may be managed by external version to vertex, cesarean delivery, and less frequently a trial of labor. The complications of labor and delivery of breech presentation include cord prolapse and entrapment of the fetal head. Prolonged fetal heart rate decelerations may have a variety of etiologies and can be thought of as preuterine, uteroplacental, and postplacental. A quick examination and verification of vital signs will often determine the etiology of a prolonged deceleration. Risk factors for shoulder dystocia include fetal macrosomia, diabetes, previous dystocia, maternal obesity, postterm deliveries, and prolonged stage 2 of labor. Uterine rupture is uncommon in patients with no prior uterine scar; it is seen in 0. Repeat examination after 1 hour shows dilation of 1 cm, 50% effacement, and 22 station. The team decides to start her on magnesium sulfate for tocolysis and administers the first dose of betamethasone. Which of the following is the mechanism of action of magnesium sulfate on cellular calcium What side effects or complications should you counsel your patient that she might experience from magnesium sulfate Magnesium sulfate has potential for serious complications such as respiratory depression, hypoxia, cardiac arrest, and even death. Which of the following clinical tests is most useful to monitor patients who are receiving magnesium sulfate infusions Vignette 2 A 35-year-old G2P1001 woman at 40 weeks 6 days presents to labor and delivery triage with a 5-hour history of painful contractions. Monitoring reveals contractions every 3 minutes and cervical examination on arrival is 3 cm dilated, 50% effaced, and 22 station. Her labor progressed slowly with dilation of 1 cm every 3 hours until labor arrested at 7 cm. A healthy baby girl weighing 4,200 g was delivered by cesarean section after arrest at 7 cm for 4 hours. You recheck her cervix 2 hours later and find that it is 4 cm dilated, 90% effaced, and 21 station. Which of the following factors was least likely to result in her prior failure to progress Which of the following factors places the patient at greatest risk for shoulder dystocia Prior failure to progress 45 lb weight gain in pregnancy Suspected fetal macrosomia Prior fetus weighing 4,200 g c. Which of the following is not associated with increased risk for breech presentation Clavicle fracture Vignette 4 You are working in the emergency department when an 18-year-old Caucasian woman arrives via ambulance. She had no family or friends with her, but police have contacted family who are on the way to the emergency department. Postpartum period between 48 hours and 4 weeks Vignette 3 A 32-year-old G3P2002 woman presents for routine prenatal care at 37 weeks. During your examination you measure the fundal height at an appropriate 37 cm, and find fetal heart tones located in the upper aspect of the uterus. Prior to discharging the patient from labor and delivery triage after her successful external cephalic version, which of the following should you do first Which of the following findings would deter you from offering this patient a trial of breech delivery Fetal ultrasound, if not performed in the previous 4 weeks, can provide additional information on the well-being of the fetus. The fetal heart tracing shows a baseline of 135 bpm with moderate variability and accelerations. Vignette 1 Question 5 Answer C: this scenario describes the development of placental abruption. The description of the fetal monitoring and maternal status tells us that the situation is not emergent and trial of vaginal delivery can continue. However, it is important to be prepared for worsening vaginal bleeding or need for emergent delivery should the fetal status or maternal status deteriorate. You could discuss blood transfusion at this time, but it is not the best answer choice. Vignette 2 Question 1 Answer A: Failure to progress is commonly associated with the 3 Ps-power, passenger, and pelvis. Montevideo units are a measure of average uterine strength of contractions in millimeters of mercury multiplied by the number of contractions in 10 minutes, and 200 to 250 Montevideo units define adequate labor in the active phase of labor. Optimal uterine contractions are believed to be necessary for vaginal birth and are also measured by cervical dilation and effacement. The second P, the passenger or fetus, can be too large to deliver or be malpositioned for delivery. Lastly, the pelvic outlet may not be the right shape or size, in combination with the fetal position, to allow delivery. Magnesium decreases uterine tone and contractions by acting as a calcium antagonist and a membrane stabilizer. Calcium channel blockers decrease intracellular calcium, which reduces uterine contractility. Indomethacin blocks the enzyme cyclooxygenase and decreases the level of prostaglandins, which decreases intracellular levels of calcium and therefore decreases myometrial contractions. Vignette 1 Question 2 Answer A: Flushing, diplopia, and headache are common side effects of magnesium sulfate. Calcium channel blockers such as nifedipine can cause headache, flushing, and dizziness. Lastly, indomethacin has been associated with the premature closure of the ductus arteriosis in the neonate. This injury is due to traction on the anterior shoulder, as it is trapped behind the pubic symphysis. It is important that the mother does not push while the shoulder is impacted, as this can worsen risk for injury. Brachial plexus injuries can occur without shoulder dystocia and are thought to be due to uterine forces on the fetus while delivering. This risk increases after 3 minutes but is highly variable, and depends on the reserve of the fetus prior to the shoulder dystocia. This is the rarest of complications from shoulder dystocia and the most severe apart from fetal demise. Vignette 3 Question 1 Answer C: Given her gestational age prior to 39 weeks, it would be best to try an external cephalic version. If unsuccessful, a second trial of version at 39 weeks with epidural or spinal anesthesia should be offered. If the version is successful prior to 39 weeks, the patient is followed expectantly with routine prenatal care. If the version is unsuccessful on second attempt with anesthesia, delivery by cesarean section is recommended. External cephalic versions carry the risk of cord compression and placental abruption. It is critically important to monitor the fetus for a period of time after the procedure. Occasionally, an emergent delivery is indicated by cesarean following a trial of version due to nonreassuring fetal testing. In a select population, trial of vaginal breech delivery can be attempted but requires stringent criteria be met. External cephalic version carries the risk of placental abruption and also the possibility of maternal exposure to fetal blood through disruption in the placental interface. In Rh-negative mothers, this could lead to formation of antibodies against Rh factor if the fetus is Rh positive. In future pregnancy with an Rh-positive fetus, maternal antibodies can cross the placenta and destroy fetal blood cells resulting in anemia and fetal hydrops. Other risk factors of external cephalic version include fetal distress, failed rotation, and need for urgent cesarean section. Induction is generally scheduled at 39 to 40 weeks and abdominal binders are commonly used to prevent the fetus from returning to breech presentation but theses are not the best answers. Lastly, rechecking the fetal position is possible and reasonable especially if the mother describes a large fetal movement, but it is not necessary or the best answer choice.
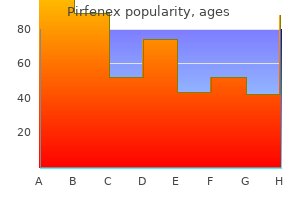
Generic pirfenex 200 mg mastercard
The role of the newer triazole antifungal agents treatment 6 month old cough generic 200 mg pirfenex free shipping, such as itraconazole, voriconazole and posaconazole, is Chapter 18 Fungi] 219 unclear but promising. However, there is some evidence that long-term oral treatment with itraconazole reduces the rate of recurrence [Grade C], or can cure the disease on its own. However, if immunocompromise should occur, then the condition may become invasive and life-threatening. They are sometimes found in the sinus cavities of patients undergoing investigation for chronic sinusitis, nasal obstruction, facial pain or other conditions. Factors associated with a lower survival rate include delayed diagnosis and treatment, hemiparesis or hemiplegia, bilateral sinus involvement, leukaemia, renal disease and treatment with desferroxamine mesilate. Surgical debridement is often mutilating and the conventional formulation of amphotericin B is nephrotoxic. Debridement carries the risk of bleeding in thrombocytopenic patients, as well as the risk of inadvertent damage to the orbit and brain. Furthermore, only 6 percent of patients with intracranial extension were cured by antifungal and surgical treatment, compared with 46 percent of those without intracranial infection. In many cases, however, the content of sinus fungus balls has failed to grow on culture. Affected persons often present with long-standing symptoms of nasal obstruction, purulent nasal discharge, cacosmia (fetid smell) or facial pain. The reported incidence of this disorder ranges from 5 to 10 percent of patients with chronic rhinosinusitis in some studies,27, 28 to a much higher percentage in others. Allergic mucin, containing degenerating eosinophils and their byproducts, was found in 97 (96 percent) of a subset of 101 consecutive patients who underwent surgical treatment; in the four cases in which allergic mucin was absent, eosinophils were also absent. Fungal elements were detected in histopathological specimens from 82 (81 percent) of these 101 cases. Conventional IgE-mediated hypersensitivity to fungi was not a consistent finding in the patients with chronic rhinosinusitis. More recently, an Austrian group31 used the Mayo Clinic procedure and detected fungus in cultures of nasal mucus from 87 percent of patients with chronic rhinosinusitis, as well as from 91. Histopathological investigation should also demonstrate no evidence of allergic mucin in the sinus or granulomatous reaction in the mucosa. There should be no fungal invasion of the mucosa, associated blood vessels or bone. Patients with sphenoid sinus balls are at risk of an intracerebral bleed or infarct as a complication of their surgical treatment. Patients who become immunosuppressed are at risk of developing an invasive fungal sinusitis. More recent series suggest that it is predominantly due to various dematiaceous (brown-pigmented) environmental moulds, including Alternaria, Bipolaris, Cladosporium, Curvularia and Drechslera species. Cases of allergic fungal sinusitis have been described from different parts of the world, but the largest number of reports have come from the warm humid areas of the southern United States where the disorder accounts for about 7 percent of all sinus surgeries. At surgery the dura and periosteum were intact, histologically Aspergillus was present with Charcot Leyden crystals and there was no invasion. Many patients with allergic fungal sinusitis have a history of chronic rhinosinusitis and have undergone multiple operations prior to diagnosis. The nasal polyposis may form an expansive mass that causes bone necrosis of the thin walls of the sinuses. Should the lamina papyracea of the ethmoid bone be traversed it may cause proptosis. In addition, allergic fungal sinusitis may be suspected when a patient with nasal polyposis, having no other known disease, responds only to oral corticosteroids. Adjunctive medical management is also required because it is unlikely that all fungal elements can be removed. In small studies, use of postoperative oral corticosteroids reduced recurrence of disease. The symptoms are often unilateral and include nasal obstruction, purulent discharge and cacosmia. Allergic fungal sinusitis Allergic fungal sinusitis is an important cause of chronic rhinosinusitis. The predominant causes of this condition are dematiaceous (brown-pigmented) moulds. Systemic antifungal treatment is ineffective on its own, but may reduce inflammation and peroperative bleeding and if given postoperatively may reduce the recurrence rate. Postoperative endoscopic follow up is recommended because there is a poor correlation between subjective improvement and the presence of objective regression of disease. Despite surgical debridement and corticosteroid treatment, the condition recurs in up to two-thirds of patients. In addition, corticosteroid use is sometimes associated with limiting side effects. Chronic invasive sinusitis the most common aetiological agents include Aspergillus, Bipolaris and Curvularia species. Chronic granulomatous invasive sinusitis Most cases have been reported from North Africa. Best clinical practice Acute invasive sinusitis [Underlying host disorders must be controlled: correction of acidosis is essential and immunosuppressive drugs should be reduced in dose if possible. Patients who receive amphotericin B should be monitored for signs of renal damage. These opportunistic pathogens can cause acute or chronic deepseated infection, but are more often seen causing mucosal, cutaneous or nail infection. Oropharyngeal candidiasis is a common problem in debilitated or immunocompromised persons. Isolated laryngeal candidiasis can also occur in these individuals, but is much less common. These include previous radiation therapy, broadspectrum antibiotics and corticosteroid use. Although it is not life-threatening, it can be most uncomfortable for the patient, contributing to inadequate oral nutrition and weight loss. Of greater concern, it can predispose patients to develop a more invasive disease, such as oesophageal candidiasis. Candida albicans is present as a commensal in the mouth of up to 40 percent of the normal adult population. The number of organisms in the saliva of carriers increases with tobacco smoking and when dentures are worn. Local factors, such as trauma from unhygienic or ill-fitting dentures and tobacco smoking, are also important. Isolated laryngeal candidiasis has usually been Oral candidiasis can be classified into a number of distinct clinical forms: pseudomembranous, erythematous (or atrophic) and hyperplastic (or hypertrophic) candidiasis. Pseudomembranous candidiasis is an acute infection, but it can recur in patients using steroid inhalers and in immunocompromised individuals. It is also seen in neonates and among terminally ill patients, particularly in association with serious underlying disorders, such as leukaemia and other malignancies. Pseudomembranous candidiasis presents as white raised lesions on the surfaces of the tongue, hard and soft palate, buccal mucosa and tonsils. The lesions are often painless, although mucosal erosion and ulceration may occur. It is important to distinguish this condition from hyperplastic candidiasis (oral leukoplakia). The simplest test is to determine whether the white pseudomembrane can be dislodged.
Cheap pirfenex uk
Initially treatment of scabies 200mg pirfenex for sale, thyroid autoantibodies may be positive but again this is often transient although some retain thyroid autoimmunity for life. Nonsteroidal antiinflammatory drugs such as aspirin and indomethacin are effective analgesics; beta-adrenergic blockers are useful if symptomatic in the thyrotoxic phase. The female preponderance, seasonal incidence, geographical aggregation and raised inflammatory markers have led to a hypothesis of a viral aetiology. Mumps virus, Coxsackie, influenza and adenoviruses have been implicated in the development of the disease although viral role in pathogenesis remains obscure. Silent/painless thyroiditis Painless thyroiditis can occur in the early stages of autoimmune thyroiditis. This may lead to mild biochemical hyperthyroidism and occasionally to symptomatic thyrotoxicosis. The thyrotoxicosis is generally mild and raised markers of inflammation are rarely found in contrast to subacute thyroiditis. The duration of the thyrotoxic phase is around eight weeks and symptomatic treatment with beta-adrenergic blockers may be required. In most, euthyroidism is eventually restored but permanent hypothyroidism is almost certain to develop over time. Radioactive iodine is effective in treating thyrotoxicosis, often at the expense of hypothyroidism. Thyrotoxicosis may complicate pregnancy, and post-partum thyroiditis is relatively common. Subclinical hyperthyroidism predisposes to atrial fibrillation and may contribute to osteoporosis. To treat or not to treat In 1996, the Royal College of Physicians issued a consensus statement indicating that there was little agreement on whether subclinical hyperthyroidism caused morbidity, and thus the benefits of detecting it remain unclear. As these patients are usually elderly, radioiodine is the treatment of choice unless contraindications exist. This may be due to disturbance within the thyroid gland itself (primary hypothyroidism), or within the hypothalamic-pituitarythyroid axis (secondary hypothyroidism). The term myxoedema is not synonomous with hypothyroidism and refers to the accumulation of glycosaminoglycans occurring in severe hypothyroidism. These hydrophilic substances are deposited within the dermis leading to induration of the skin and the characteristic facial features of hypothyroidism. Epidemiology As in other autoimmune conditions, hypothyroidism affects females more commonly than males and its Table 28. The prevalence of hypothyroidism is estimated at around 2 percent of adult women and 0. The symptoms may be nonspecific or falsely ascribed to increasing age, thus a high index of suspicion should exist in this group of patients and some advocate routine screening for hypothyroidism in the elderly. Clinical features of hypothyroidism An insufficiency of thyroid hormone affects almost every organ system in the body and the effects of hypothyroidism can be broadly divided into two: firstly the generalized slowing of all metabolic processes leading to , amongst others, fatigue, cold intolerance and weight gain; secondly, the tissue accumulation of glycosaminoglycans, which leads to characteristic changes such as coarse dry skin, hair loss and doughy peripheral oedema. Manifestations of and laboratory findings in hypothyroidism are listed in Table 28. The onset of symptoms may be insidious and go unrecognized, such that severe myxoedema may result. There may be a slow increase of weight despite a reduction in appetite and constipation is a common feature. Cold intolerance is typical with the patient wearing layers of clothes at initial consultation. Myopathy may cause difficulty in walking upstairs or rising from a chair and numbness and paraesthesia in the hands may develop as carpal tunnel syndrome results from peripheral oedema. This is to be distinguished from a myxoedema coma, which is a life-threatening condition often precipitated by infection, trauma or cold and occurring most often in older patients (see Table 28. It is, in many respects, the archetypal Manifestations and laboratory findings in hypothyroidism. Although it is most common in older women, it can occur in infants as young as two years of age and is the major cause of hypothyroidism in children. First recognized in 1912, the pathogenesis of the condition is now relatively well understood. Both cellmediated and humoral factors contribute to the destruction of the thyroid gland. T cell infiltration is pronounced with cellular injury resulting from direct action by cytotoxic T cells. Although patients have high circulating antibodies to thyroid microsomes and to thyroglobulin, these are not thought to have functional activity. Histologically, the gland is infiltrated with lymphocytes and areas of follicular destruction and fibrosis may be evident. Initially, the thyroid hypofunction may be subclinical, but may become overt with a rate of developing hypothyroidism at a rate of around 5 percent per year. A slowly growing goitre may have been found on examination or noted by the patient or a family member. The presence of the goitre may predate the development of overt hypothyroidism and, generally, the goitre remains static or may decrease in size. Occasionally, hypothyroidism can result from overtreatment of hyperthyroidism with antithyroid medication, but with close monitoring this is not common. Thyroidectomy After total thyroidectomy hypothyroidism would be evident without treatment at around two to four weeks postoperatively, thus all patients who have undergone total thyroidectomy commence thyroid hormone replacement before leaving hospital. Hypothyroidism may also result from subtotal thyroidectomy with the majority of patients becoming so within a year of surgery. Radioiodine therapy this can lead to transient hypothyroidism resulting from radiation thyroiditis some four to six weeks after treatment, or permanent hypothyroidism may ensue months or years after therapy. External beam neck irradiation Radiotherapy given to the neck may result in both hypothyroidism and an increased risk of thyroid malignancy, especially in children and adolescents. For patients who have had more than 25 Gy there may be a slow onset dose-dependent development of hypothyroidism. There is a dense interstitial lymphocytic infiltrate, with secondary germinal centre formation, enveloping small colloid-depleted follicles. These are lined with plump cuboidal oxyphil (Askanazy or Hurthle) cells possessing characteristic copious pink granular cytoplasm. Iodine deficiency is the most common cause of hypothyroidism and goitre worldwide. Diets high in goitrogens, such as cassava and some soya beans, can exacerbate the situation. Affecting those living in mountainous areas, it may result in neonatal cretinism, a combination of intellectual impairment, ataxia, coarse facies and deaf mutism. Poor performance and deafness in children can result from marginal iodine deficiency in iodine-deficient regions. Goitres may be present from young adulthood and can enlarge causing obstructive symptoms. Occasionally seen in Europe where less iodine is added to salt, goitre may also be seen in those migrating from areas where iodine intake is low, such as Pakistan and Bangladesh. Those with a pituitary adenoma may have other features of hypopituitarism, such as hypogonadism and hypoadrenalism, obscuring the symptoms of thyroid hormone deficiency. In those with central hypothyroidism, it is imperative that hypoadrenalism be excluded before initiating thyroxine therapy. An adrenal crisis may be precipitated if hypoadrenalism is not treated before thyroxine therapy is commenced. Pregnant women Women need more thyroid hormone during pregnancy and those with pre-existing hypothyroidism cannot increase T4 and T3 secretion as can normal women. Most increases are needed in the second and third trimester when the baby is growing faster. Patients with poor compliance Due to the long half-life of thyroxine, poorly compliant patients may be witnessed taking seven days of thyroxine once a week. Some choose to take T3 in addition to or instead of thyroxine, although due to its rapid absorption and short half-life it must be taken three times a day and fluctuations in thyroid hormone levels exist. At present there is little evidence to suggest advantage over T4 therapy and is probably best avoided. Thyroxine is a prohormone which is deiodinated in peripheral tissues to the active hormone T3.
Generic pirfenex 200 mg line
Preconceptual counseling should be incorporated into the annual well women examination of all reproductive age women medicine 54 357 buy pirfenex pills in toronto, whether they receive care from an obstetrician gynecologist or another primary care provider. Obese patients must be encouraged to lose weight before conception and offered specific programs to help them do so. Once pregnant, these patients should be advised to gain less weight (but never to lose weight) than the average patient, and they should be referred to a nutritionist for assistance in maintaining adequate nutrition, with some control of caloric intake. The risks of this course of action are thought to be an increased rate of cesarean section for failed induction, and potentially neonatal complications of prematurity in a poorly dated pregnancy. Thus, induction should be used primarily when there is either excellent dating or lung maturity as assessed via amniocentesis. For induction in the setting of an unfavorable cervix, prostaglandins and mechanical means should be used to achieve cervical ripening, and this can often take several days to accomplish. Interestingly, prospective studies of the practice of induction for impending macrosomia have not demonstrated an increase in cesarean delivery rates, but do appear to lead to lower rates of macrosomia. Vaginal delivery of the suspected macrosomic infant involves preparing for a shoulder dystocia, and counseling patients on the risks and treatment options. Operative vaginal delivery with forceps or vacuum is generally not advised in the setting of known macrosomia because of the increased risk of shoulder dystocia; however, this decision is one to be made in a setting of shared decision making with the patient. Etiology the most classically associated risk factor for fetal macrosomia is preexisting or gestational diabetes mellitus. This association is seemingly independent of maternal stature and gestational diabetes. Multiparity and advanced maternal age are also risk factors (Table 7-2), but these are mostly secondary to the increased prevalence of diabetes and obesity. Ultrasound uses the biparietal diameter, femur length, and abdominal circumference to estimate fetal weight. These estimates are usually accurate to within 10% to 15%; however, with estimates beyond the 90th percentile, the positive predictive value of the weight being greater than or equal to that predicted is less than 50%. This volume is maintained until close to term when it begins to fall to about 500 mL at week 40. The balance of fluid is maintained by production of the fetal kidneys and lungs and resorption by fetal swallowing and the interface between the membranes and the placenta. A disturbance in any of these functions may lead to a pathologic change in amniotic fluid volume. Traditionally, amnioinfusion has been performed to dilute any meconium present in the amniotic fluid, and therefore decrease the risk of meconium aspiration syndrome. However, in a large, multinational, randomized trial, amnioinfusion in the setting of meconium did not improve neonatal outcomes, and it is decreasingly used for this indication. In the setting of recurrent variable decelerations, there is evidence to suggest that amnioinfusion does decrease the number of variable decelerations caused by cord compression, and it is still used commonly for this indication, despite less clear evidence for neonatal benefit. This is partially because without the amniotic fluid to cushion it, the umbilical cord is more susceptible to compression thus leading to fetal asphyxiation. It is also associated with congenital anomalies, particularly of the genitourinary system, and growth restriction. It is associated with maternal diabetes and malformations such as neural tube defects, obstruction of the fetal alimentary canal, and hydrops. Etiology the cause of oligohydramnios can be thought of as either decreased production or increased withdrawal. It can be resorbed by the placenta, swallowed by the fetus, or leaked out into the vagina. Congenital abnormalities of the genitourinary tract can lead to decreased urine production. These malformations include renal agenesis (Potter syndrome), polycystic kidney disease, or obstruction of the genitourinary system. Even without a history of leaking fluid, the patient should be examined to rule out this possibility. It is also more common in pregnancies complicated by diabetes, hydrops, and multiple gestation. Just as in other diabetic patients, the increased levels of circulating glucose can act as an osmotic diuretic in the fetus leading to polyhydramnios. Hydrops secondary to high output cardiac failure is generally associated with polyhydramnios. Monozygotic multiple gestations can lead to twin-to-twin transfusion syndrome with polyhydramnios around one fetus and oligohydramnios around the other. Some centers use the deepest vertical pocket of amniotic fluid less than 2 cm as diagnostic for oligohydramnios. Once the diagnosis of oligohydramnios is made, the etiology needs to be determined prior to creating a management plan. Diagnosis Polyhydramnios is diagnosed by ultrasound in patients being scanned for size greater than dates, routine screening of diabetic or multiple gestation pregnancies, or as an unsuspected finding on an ultrasound performed for other reasons. Treatment As in oligohydramnios, the particular setting of polyhydramnios dictates the management of the pregnancy. Patients with polyhydramnios are at risk for malpresentation and should be carefully evaluated during labor. Treatment Management of oligohydramnios is entirely dependent on the underlying etiology. A plan for delivery should be made in coordination with the pediatricians and pediatric surgeons. Severely preterm patients with no other etiology are usually managed expectantly with frequent antenatal fetal testing. Commonly, most individuals become sensitized only during pregnancy and blood transfusion. In sensitized patients with Rh-positive fetuses, the antibodies cross the placenta and cause hemolysis leading to disastrous complications in the fetus. The anemia caused by hemolysis leads to increased extramedullary production of fetal red cells. Erythroblastosis fetalis, or fetal hydrops (see Color Plate 1), a syndrome that includes a hyperdynamic state, heart failure, diffuse edema. Fetal hydrops is defined as accumulation of fluid in the extracellular space in at least two body compartments. An antibody screen is performed at the initial visit to detect prior sensitization. If paternity is not in question, blood type can be performed on the father of the baby to determine whether the fetus is at risk. However, because approximately 5% of all pregnancies have unknown or incorrect paternity, the safest course is to treat all pregnancies as if the fetus is at risk. However, if it becomes 1:16 or greater, serial amniocentesis is begun as early as 16 to 20 weeks. While the risk of immediate delivery may be as high as 3%, this risk is preferred to worsening fetal anemia, hydrops, and likely fetal death. Zone 1 is suggestive of a mildly affected fetus, and followup amniocentesis can be performed approximately every 2 to 3 weeks. Zone 2 is suggestive of a moderately affected fetus, and amniocentesis should be repeated every 1 to 2 weeks. When there is no explanation for a fetal demise, it is usually attributed to as "cord accident. After week 20, fetal death is suspected with absence of fetal movement noted by the mother or absence of uterine growth. Given the importance of making an appropriate, accurate diagnosis, the absence of fetal heart motion is usually verified by two clinicians. Early gestations can be evacuated from the uterus by dilation and evacuation or with mifepristone and misoprostol in some cases. After 20 weeks, the pregnancy is usually terminated by induction of labor with prostaglandins or high-dose oxytocin.
Cheap 200mg pirfenex overnight delivery
One potential advantage of the use of EcochG is the large amplitude of the activity recorded medicine abuse order pirfenex without prescription. The reader who intends to perform this procedure is directed to the comprehensive reviews by Moller31 and Martin and Mishler. There is considerable variability in the methods advocated and clinical trial evidence is not apparent. Second, this variability may account in part for the lack of a strong evidence base for the benefits of auditory monitoring. Direct recordings from the cochlear nerve the need for rapid acquisition of responses may be met by recording directly from the cochlear nerve, the large amplitude of the elicited activity obviating the need for lengthy averaging. Changes in latency, amplitude and morphology should all be reported to the surgical team. A similar dearth of evidence is found when determining the relative efficacy of techniques or combinations of techniques. Only accurate estimation of motorneuron function will give the surgeon a true representation of immediate facial function and hopefully then enable development of a valid predictive technique. The speciality as a whole requires a good evidence base to support the use of intraoperative facial nerve monitoring as the standard for all otological procedures that place the facial nerve at risk. Facial nerve preservation by posterior fossa transmeatal microdissection in total removal of acoustic tumors. Intraoperative monitoring of facial muscle evoked responses obtained by intracranial stimulation of the facial nerve: a more accurate technique for facial nerve dissection. Prediction of facial nerve function following acoustic neuroma resection using intraoperative facial nerve stimulation. There is a good evidence that monitoring facial nerve function improves outcomes of facial function. A consensus has not yet been reached on techniques for monitoring auditory function, but it looks likely that a combination of techniques will be optimal. Best clinical practice [Regarding monitoring of facial nerve function, there is evidence that these techniques offer benefit in improving facial nerve outcomes in surgery that may challenge the facial nerve. Intraoperative facial nerve monitoring in chronic ear surgery: A resident training program. Predictive value of facial nerve electrophysiologic stimulation thresholds in cerebellopontine-angle surgery. Facial nerve function following cerebellopontine angle surgery: Prognostic value of intraoperative thresholds. Value of intraoperative threshold stimulus in predicting postoperative facial nerve function after acoustic tumor resection. Assessment of real-time clinical facial function during vestibular Schwannoma surgery. Quantitative parameters of intraoperative electromyography predict facial nerve outcomes for vestibular schwannoma surgery. Hemifacial spasm: intraoperative electromyographic monitoring as a guide for microvascular decompression. Intraoperative monitoring of auditory evoked potentials and facial nerve electromyography. The feasibility of using oto-acoustic emissions to monitor cochlear function during acoustic neuroma surgery. Intraoperative monitoring during surgery for acoustic neuroma: benefits of an extratympanic intrameatal electrode. Technical developments in intraoperative monitoring for the preservation of cranial motor nerves and hearing in skull base surgery. Intraoperative brainstem auditory evoked potentials: Significant decrease in postoperative morbidity. Acoustic neuroma surgery: Use of cochlear nerve action potential monitoring for hearing preservation. Advances in monitoring of seventh and eighth cranial nerve function during posterior fossa surgery. Levels of evidence are not really applicable to this area, but the human studies that underlie the discussion of optical coherence tomography as applied to otorhinolaryngology are observational or at best non-randomized. In the field of laryngology, light endoscopy currently forms the cornerstone of clinical imaging and biopsy guidance, yet conventional light endoscopic techniques are unable to reveal information concerning subepithelial tissue. Since many laryngeal pathologies originate near the boundary between the epithelium and the underlying mucosa or within the mucosa itself, the inability to image subepithelial tissue represents a serious limitation of conventional light endoscopy. Even as a method for guiding biopsy, conventional light endoscopy gives only a relatively coarse indication of prospective biopsy locations. Frequently, a large number of biopsies are required to achieve high diagnostic accuracy, a situation that is often undesirable or unfeasible. This is particularly true for the vocal folds, which have a specialized and delicate microstructure that is highly intolerant of trauma. These limitations restrict the effectiveness of light endoscopy for the diagnosis, monitoring and treatment of many laryngeal pathologies. Clinical laryngology would thus greatly benefit from a noninvasive imaging technology capable of resolving subepithelial tissue microstructure in the range of conventional biopsy. Imaging can be performed in real time, without the need to process a specimen, as in conventional biopsy, and without the need for a transducing medium, as in ultrasound imaging. In ultrasound, a high frequency acoustic pulse travels into the tissue and is reflected or backscattered from internal structures having different acoustic properties. The magnitude and the delay time of the echoes are electronically detected, and the structural properties of the internal tissues are determined from the measured signals. Unlike in ultrasound, though, the speed of light is very high, rendering electronic measurement of the echo delay time of the reflected light impossible. Within the interferometer, the beam leaving the optical light source is split into two parts, termed the reference and sample beams, at the beam splitter. The reference beam then travels to a mirror, located at a known distance from the detector and subsequently returns to the beam splitter. The sample beam travels to the tissue sample and is reflected back toward the detector by scattering sites within the tissue. Light reflecting from deeper tissue layers has traversed a greater optical pathlength (optical distance) and therefore arrives at the detector at a later time. Light is distinct, however, in that it has an additional vector characteristic known as polarization. The polarization direction is orthogonal to the propagation direction and can be influenced by the medium in which the light propagates. Polarization measurements can be used to provide additional insights into the microscopic structure and integrity of tissues. Chapter 60 Optical coherence tomography] 757 differing strengths of the scattering sites. The reflected portions of the sample beam then return to the beam splitter where they interact with the reflected reference beam and are directed toward the detector. When two waves from the same source recombine in this manner, an interference pattern will result if the optical pathlength travelled by the two waves is identical. The output detector measures the intensity of this interference pattern and thus only measures information contained in the portion of the sample beam that has travelled the same optical distance as the light in the reference arm. Information about the remaining tissue layers can be extracted by moving the mirror in the reference arm, which changes the optical pathlength travelled by the reference beam. Two- or three-dimensional images are produced by scanning the beam across the sample and recording the optical backscattering versus depth at different transverse positions. The resulting data is a two- or three-dimensional representation of the optical backscattering of the sample on a micron scale. Several different layers of the epiglottic tissue are visible, with epithelium, lamina propria and cartilage being clearly demarcated. To illustrate, the human vocal fold lamina propria is generally subdivided into the superficial, intermediate and deep layers, with each layer having a characteristic composition and functionality. The relative thickness and integrity of these various layers appear to have a profound impact on voice. This idea is supported by the fact that the average adult will experience marked thinning of the superficial lamina propria relative to the intermediate and deep layers with increasing age,16 with a concomitant reduction in voice quality.
Purchase pirfenex 200mg with mastercard
Some of the lower glands were situated anteriorly on the lower thyroid lobe (17 percent of cases) medications 1 purchase pirfenex overnight. Other locations of the inferior glands are inferior to the thyroid in close association with the thyrothymic ligament (fibrous tissue connecting the inferior pole of the thyroid to the superior aspect of the thymus) or within the cervical part of the thymus (26 percent of cases). Clearly, in the operation of total parathyroidectomy in cases of renal failure, it would be important in this situation to thoroughly explore the superior mediastinum and expose the thymus. Sternal split is usually only required in cases where there has been previous retrosternal surgery such as in cases of coronary artery grafting, previous exploration for parathyroid glands in this area or a rare occurrence of ectopic parathyroid tissue in the aortopulmonary window. Rarer sites for an inferior parathyroid gland include an area extending from the carotid bifurcation (due to failure of descent embryologically) to the anterior and posterior mediastinum. Inferior glands which fail to descend are located superiorly to the superior parathyroid glands and usually have remnants of thymic tissue surrounding them which facilitates their identification. Normal parathyroid glands in ectopic locations receive their blood supply from local vessels, for example, the thymic or internal thoracic arteries. Usually, the inferior glands are obscured by fatty or vascular tissue, or lie within the fibrous sheath of the thyroid gland, which makes identification difficult. Symmetry in position of the superior glands has been documented in 80 percent of cases, in inferior glands in 70 percent of cases and for all four glands 60 percent of cases. Three glands were located within the thyroid region and a fourth gland from either side was located within the thymus (13 percent of cases); on one side the superior and inferior glands were located above and below the inferior thyroid artery and recurrent laryngeal nerve intersection, respectively, and on the other side both superior and inferior glands were located below (5 percent cases) or above (2 percent cases) the intersection. At this point, it descends on longus colli to the lower border of the thyroid gland. The superior thyroid artery, a branch of the external carotid artery may supply the superior parathyroid gland, but more commonly it receives an independent direct blood supply from the inferior thyroid artery. Injected contrast material into the superior thyroid artery of cadavers demonstrated that it supplied the superior parathyroid gland in 98 percent of cases. A distinct anastomosis between the superior and inferior thyroid arteries was seen in 45 percent of cases. A single artery usually supplies each gland, dividing into several branches before entering the glandular tissue, although sometimes, two or three vessels may supply a gland. The thyroidea ima artery and other accessory vessels may contribute to the blood supply but are of less importance. Ectopic parathyroid tissue receives its blood supply locally, as mentioned earlier. Despite vascular anastomoses existing between the thyroid vessels, injury to the vascular supply to the parathyroid gland can result in infarction and necrosis, an important point to note at operation. There have also been reported cases of spontaneous infarction of the parathyroid glands in patients with hypercalcaemia and subsequent resolution. The superior and middle thyroid veins drain the upper and central parts of the ipsilateral thyroid and parathyroid glands in that region. The superior thyroid veins are relatively constant in position and always drain into the internal jugular veins, but can communicate with the facial venous system superiorly. The inferior thyroid veins are more variable in position and usually drain into the left brachiocephalic vein. Drainage into the right and distal segment of the left brachiocephalic vein was also documented. In some patients the inferior thyroid veins drained the mediastinum, communicating with the thymic Arterial blood supply the principal blood supply to the parathyroid glands is from specific ascending glandular branches from parenchymal, muscular or oesophageal branches of the Chapter 29 the parathyroid glands: anatomy and physiology] 373 vein. Monchik30 performed 32 autopsies and demonstrated that the inferior thyroid veins drained separately into the left brachiocephalic vein (25 percent of cases) or formed a common trunk (47 percent of cases). Occasionally, the inferior thyroid venous trunk drained directly into the internal jugular vein. Each parathyroid gland tends to drain ipsilaterally and inferiorly, but contralateral drainage can occur. This results from anastomoses posteriorly with the vertebral venous plexus and anteriorly with the anterior jugular veins, which drain via the transverse cervical vein into the subclavian vein. Knowledge of the variations in appearance will aid the surgeon to identify normal parathyroid tissue. Tissue located in the region of the parathyroid glands may be mistaken for parathyroid tissue, especially lymph nodes, fat lobules and thyroid nodules. This is variable but it is uncommon for either less than three or more than five glands to be found. Where are the parathyroid glands located and what are the possible locations of an aberrant parathyroid gland Bearing in mind the embryological development and due to the variable extent of their migratory pathways, the surgeon should have a systematic approach to explore the anatomical regions in which the parathyroid glands are likely to be found. The superior parathyroid glands are more constant in their location than the inferior glands. A missing parathyroid gland may be located at an ectopic site more often than the patient having only three glands. Innervation the nerve supply to the human parathyroid glands is principally adrenergic from the sympathetic system. The nerves are vasomotor, but not secretomotor, with gland activity controlled by changes in plasma calcium levels. Microscopic appearance the parathyroid gland has a thin connective tissue capsule and septae which divide it into lobules. Vascular mesenchyme grows into nodules on the dorsal aspect of the pharyngeal pouches to form a rich capillary network in the parathyroid glands. There are three types of chief cells, dependent upon the depth of cytoplasmic staining visible on light microscopy, named light, dark and clear cells. Chief cells in humans can be divided into active and inactive cells, the latter outnumbering the former by three to one. A second cell type, the oxyphil cell, becomes apparent before puberty and increases in number with age. Rare cases of hyperparathyroidism have been documented with only oxyphil cells present in the excised glands. Fifty percent of plasma calcium exists in its free (ionized) form, which is metabolically active and under tight hormonal regulation. The remainder is bound to albumin, and small amounts are bound to pyruvate, citrate and lactate. Essential functions reliant upon tight regulation of serum calcium levels include neural transmission, muscle contraction (and relaxation), exocrine secretion, blood clotting and cellular adhesion. The hormone is cleaved into two major fragments in chief cells and Kuppfer cells of the liver. This calcium-sensing receptor is a typical sevenspanning membrane G protein-coupled receptor. The minimal secretory rate is low but not zero, with the maximal secretory rate representing parathyroid gland reserve. A steady-state occurs lower on the dose-response curve which means the parathyroid gland responds more efficiently to hypocalcaemia than to hypercalcaemia. Parathyroid cells replicate little in adulthood, but can increase dramatically in number secondary to hypocalcaemia, low levels of vitamin D3 and neoplasia. An increased cell number secondary to hypocalcaemia is a slow response, but appears to be irreversible, as after renal transplantation persistent hyperparathyroidism can be problematic. Vitamin D Exposure to ultraviolet irradiation converts the cutaneous precursor of vitamin D, 7-dehydrocholesterol, to vitamin D3. The degree of skin pigmentation regulates the conversion by influencing the penetration of ultraviolet light. An important source of vitamin D, if exposure to sunlight is limited, is from dietary sources. Metabolites of vitamin D are fat-soluble compounds which circulate bound to vitamin D-binding protein, and some to albumin. Probably the most important physiological function is the regulation of intestinal calcium transport. Calcium is absorbed in the intestine by three pathways: transcellular, vesicular and paracellular transport. The role of calcitonin in humans may inhibit osteoclast-mediated bone resorption to increase osteoblast numbers and decrease osteoclasts.