Order online zovirax
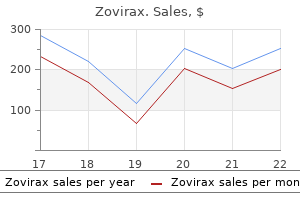
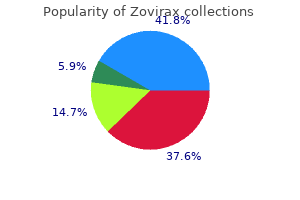
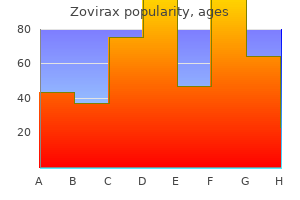
Newer fiber-packing techniques and advanced camera systems have led to further improvement anti viral tissues kleenex buy 800 mg zovirax with mastercard. Fiberoptic systems now provide light and image transmission through most current semi-rigid ureteroscopes. As discussed earlier, offset eyepieces became necessary when rigid ultrasound probes were developed for ureteroscopic lithotripsy. These probes, as well as larger more rigid working instruments, required a straight working channel for passage through the scope. Instrument manufacturers have made attempts to reduce the trauma of insertion by modifying shaft design and manufacture. The miniureteroscope shaft has a graduated stepless design, starting with a distal tip diameter as small as 6. This ensures maximal proximal strength of the scope whilst providing a gradual dilation of the ureter as the scope is advanced. The continued reduction in ureteroscope diameter has led to a reduction in the number of ureteral strictures seen and an increased success rate for the procedure [17]. Most of the currently available miniureteroscopes are beveled for easier advancement and have a round or oval tip design; however, scopes with smooth triangular tips have recently become available. A "short" ureteroscope of just over 30 cm can be used to access up to the level of the mid ureter in males and renal pelvis in females. To reach the renal pelvis in a male requires a "long" ureteroscope of 40 cm or more. A larger single channel permits the use of larger instruments and possible removal of small stone fragments or biopsy specimens through the sheath, and dual instrumentation depending on the limits of each channel port. Two separate channels allow the operator to work through one channel without impeding irrigation flow through the other. The channels are either triangular or oval in cross-section, which allows irrigation to continue around the sides despite the placement of an accessory instrument. These facilitate both easy insertion under direct vision with the (A) standard design, as well as the ability to use the straight rigid accessories in comfort with the (B) lateral and (C) oblique offset designs (courtesy of Richard Wolf). The introduction of holmium laser lithotripsy for the treatment of upper urinary tract stone disease in 1996 [18] was a huge step forward in endoscopic stone treatment, and is now the bedrock of contact lithotripsy in most departments. With fiber diameter measuring only 200 and 365 m, this has virtually abolished the requirement for anything larger than a 3. The narrow lasers also allow them to be used simultaneously with another accessory down a working channel, while still maintaining some flow. Camera and video systems Image transmission has evolved in line with changes seen with the semi-rigid ureteroscopes. The video camera and monitor-based endoscopes allows binocular vision that is projected on to a large television monitor; this is ergonomically easier for the urologist and also can be enjoyed by the theater team. The high-resolution image output has also reduced the discrepancy between the better images obtained with the larger endoscopes compared with those previously seen with the ureteroscope. Analog images produced by transmission down fiberoptic bundles continue to be the main pathway to deliver views of the subject matter to the camera in the majority of semi-rigid ureteroscopes. The drive to engineer semi-rigid ureteroscopes with digital distal sensor 372 Section 3 Ureteroscopy: General Principles exist which require no input from the endoscopist. Current ureteroscopes Rigid ureteroscopes are available in many of the designs previously described. The characteristics of the latest designs of currently available semi-rigid ureteroscopes are given in Table 34. Care, maintenance, and technical failure An important consideration when weighing up the purchase of a new ureteroscope is its longevity and often a balance is sought between optimal duration of scope life and its efficacy. Although less of a problem with the semi-rigid ureteroscope in comparison with its flexible counterpart, applying excessive torque causing deflections over 5 cm can lead to significant image distortion and scope failure. The majority of ureteroscopic failures are attributed to iatrogenic causes, including improper handling at the time of instrumentation and problems during the sterilizing process [21]. Regardless of the type and make of ureteroscope, the frequency of repair increases with decreasing ureteroscope diameter and increasing length of instrument [22]. Previously, with stepped shaft design of the rigid ureteroscope, bend stress was concentrated at solder points. Newer tapered shafts were produced to reduce this problem, making them more durable and less traumatic. Other notable risk factors for predicting the number of uses expected from a ureteroscope are its age and whether the ureteroscope has undergone comprehensive repair as a result of prior damage [21]. For optimal scope life, it is important that optimal care is taken in looking after the instrument and cleaning procedures are carried out with strict adherence to company instructions. This is partly due to the high density of fiberoptic bundles that can be incorporated in to the semi-rigid ureteroscope, which are more resistant to image degradation when compared to those found in the flexible ureterorenoscope. Irrigation An effective irrigation system is important to optimize the chance of access in to the ureteric orifice and provide good visibility during either rigid or flexible ureteroscopy. The simplest arrangement involves gravity irrigation, which has to contend with the small diameter and long length of the ureteroscope causing a reduction in flow. Other configurations are available that generate a greater pressure and therefore flow, with the pneumatic sleeve applied around the bag of fluid being the most common semi-automated set-up. Devices requiring operator/assistant input to supply increased flow on demand include attaching two 60 mL syringes via a Y-connector to inject irrigation as needed, and the Peditrol irrigation device that delivers a bolus via a foot pedal [19]. Automated infusion systems offering continuous saline irrigation, such as the Ureteromat, also Flexible ureteroscopes Flexible ureteroscope versus rigid ureteroscope Flexible ureterorenoscopy has developed rapidly over the past 30 years as technologic improvements have been made in both instrument size and design. Advances in fiberoptic technology, improved deflecting mechanisms, and a greater diversity of working instruments, have all increased the utility of the flexible ureterorenoscope in the diagnosis of upper tract disorders. This has led to ever-increasing indications for minimally invasive diagnostic and therapeutic interventions. Over the same time frame, the number of ureteric complications Chapter 34 Rigid and Flexible Ureteroscopes: Technical Features 373 Table 34. Although differing significantly in cost and complexity, the flexible ureterorenoscope should not be considered as a separate entity from the semi-rigid ureteroscope. Both types of ureteroscope are in fact used in a complementary fashion to access, inspect, and treat pathology in the entire upper urinary tract collecting system [25]. So complementary, in fact, that it is common practice to first use the semi-rigid ureteroscope with its graduated increase in diameter to optically dilate the ureteral orifice and lower ureter, both to ease passage of the flexible scope and increase the longevity of the delicate smaller caliber flexible ureterorenoscope. The rigid ureteroscope is therefore ideal for managing pathology in the lower aspects of the urinary tract, whereas the flexible ureteroscope is better suited to the upper ureter, renal pelvis, and calyces. Using active tip deflection, the flexible ureterorenoscope is able to negotiate the angulations of the ureter and pass safely beyond the iliac vessels before being advanced all the way up to the intrarenal collecting system under direct visual control. Subsequent improvements in fiberoptic technology have allowed the bundling together of greater numbers of fibers, along with a second layer of glass cladding that has a different refractive index from the core of glass. The interface between these two different glasses produces the internal reflection [6, 28], resulting in the production of a sharper image with better illumination. The advances in fiberoptics have not only produced superior images, but have also enabled a reduction in instrument size, allowing for both larger working channels and a smaller outer shaft diameter. Further modifications to the endoscope have allowed its tip to be actively manipulated by the endoscopist along with the development of instrument channels. Digital endoscope the image quality with the fiberoptic endoscope is limited by the finite diameter of the image-carrying glass fibers, leading to the pixelated "chicken wire" Flexible endoscope development Fiberoptic endoscope the existence of the flexible endoscope owes a great deal to the development of fiberoptic technology, the principles of which were developed over a century ago by John Tyndall (Table 34. Based on the physical properties of light [6], small-diameter transparent glass fibers when bundled randomly will uniformly transmit light from one end to the other (even when bent), but no image. The use of glass fibers in a "noncoherent" arrangement to provide illumination was soon followed by the introduction of fibers bundled together coherently and with identical orientation at either end. The view seen is therefore made up of thousands of images from each individual fiber to produce a composite matrix image. In the 1950s, Harold Hopkins designed the "fiberscope," a coherent bundle of fibers with the ability to transmit images [27]. It was not however until 1957 that the South African physician Basil Hirschowiz created a diagnostic flexible endoscope that was fit for clinical practice. Using superior glass fiber technology, the potential of his invention was soon realized by several medical specialities, and Table 34. Year 1854 1950s 1957 X1960 X1962 1971 X1970 1983 1994 2005 2006 Pioneer John Tyndall Harold Hopkins Basil Hirschowiz Marshall McGovern and Walzak Takagi et al.
Zovirax 800mg low cost
The short rise time associated with the shock will lead to nonuniform straining of the tissue anti viral echinamide order zovirax 800mg with amex, resulting in shear forces. It is generally recognized that tissue structures are sensitive to shear stress and the distortion of the tissue by the shock wave could induce enough shear to cause damage [109, 110]. Cumulative shear As mentioned above, the positive phase of the shock wave can induce a displacement in tissue of tens of microns. However, there can be a small net displacement remaining in the tissue after the passage of the shock wave. However, for kidney tissue it has been estimated that this time scale may be of the order of 1 s [111]. Over thousands of shock waves the net displacement could build up to sufficient levels to result in tearing of the tissue: a process referred to as cumulative shear [111]. Shear induced by inhomogeneities Tissue is an inhomogeneous medium at multiple length scales. Spatial variation in the sound speed on the millimeter length scale can have a dramatic effect on the focusing of ultrasonic pulses in tissue [112]. As the shock wave focuses, parts of the wavefront that passed through tissue with high sound speed will be advanced and the parts that passed though low sound speed tissue will fall back. This distortion in the wavefront will lead directly to shear stresses in the tissue. Again, these shear stresses could be strong enough to induce mechanical damage of the tissue [109]. Measurements using passive cavitation detection in both humans and pigs have detected the Chapter 49 Physics of Shock-Wave Lithotripsy 551 Cavitation progression Once blood vessels have been ruptured, either by mechanical stresses or cavitation bubbles inside intact vessel, blood will collect in pools. Also, existing bubbles, which can act as nuclei for subsequent cavitation events, will not be swept away by blood flow, but will remain in the pooled region. The ensuing violent cavitation could result in liquefaction of the tissue and the spread of a wave of cavitation-induced damage through the kidney [127]. Further, there are few experimental systems that can be used to test and validate different hypotheses. Although the general consensus among researchers is that cavitation is the primary mechanism for tissue injury, this field still requires much study. The first lithotripters were electrohydraulic devices in which the shock wave was generated by underwater spark discharge and shock-wave coupling was achieved by immersion of the patient in a water bath. It used an open water bath to couple shock waves to the body; treatment was painful, necessitating that the patient be sedated or even anesthetized; the shock wave firing had to be gated to the cardiac cycle ( to reduce risk of arrythmias), which slowed the treatment; and the lithotripter was a large, stationary piece of equipment that required a dedicated water treatment plant. What physicians (and patients) really wanted was lithotripsy that was painless, fast, and convenient with minimal to no anesthesia; a fully ambulatory walk-in-walk-out therapy. Problems related to the overall physical design of the lithotripter were challenging but solvable. For example, the issue of the open water bath was addressed by enclosing the shock head and by using a rubber membrane to couple the shock wave to the body. However, elimination of the water bath meant that medical staff had much easier access to the patient, the lithotripter did not necessarily have to be tied down to a dedicated facility, and lithotripters could be designed as modular systems. Many modern lithotripters have been designed to be portable and are used in mobile lithotripsy units. The cardiac gating was found to be unnecessary for most patients and so most lithotripters run in "ungated" mode in which the urologist can chose the rate at which shock waves are delivered. Commonly, this will be at a rate of 2 Hz or 120 shock waves/min, which results in a much quicker treatment time. However, in vitro studies indicated that firing at higher rates resulted in worse stone fragmentation [131]. The likely explanation for this effect is that bubbles from a previous shock wave can last for many seconds [91] and that these bubbles can end up shielding the stone from the next shock wave [132]. The in vitro studies were followed up by animal studies which confirmed better stone comminution at Evolution of the lithotripter It is more than 30 years since the introduction of lithotripsy to clinical practice and there have been a number of noteworthy changes in equipment design, but none that has involved a fundamental change in the acoustics of the lithotripter. That is, lithotripters have changed (they are now compact, modular, use dry shock heads, have improved imaging), but the acoustic signature of the lithotripter pressure pulse remains the same. Indeed, there has been a very active effort on the part of manufacturers to produce machines that are easier and more practical to use. One refinement was to develop lithotripters that produced a tight focal zone of high peak positive pressure. However, as discussed above, data suggest that this led to decreased efficiency of stone breakage and to an increase in collateral damage. This is an example of progress in lithotripsy which comes at the 552 Section 4 Shock-Wave Lithotripsy positive experimental results, targeting ways to improve stone breakage and reduce tissue injury. One approach is a response to the recent trend toward tight focal zone, high acoustic pressure machines. This machine was developed to test the hypothesis that a very broad focal zone could be used to enhance stone breakage by circumferential squeezing [82]. It has been reported in an early trial that this machine delivers a high stone-free rate (86%) and can be used anesthesia free [128]. Studies have shown that cavitation bubbles generated by one lithotripter pulse can be manipulated by a second pulse [136, 137]. If the second pulse arrives while bubbles are in their early growth phase, further expansion is stopped and the bubbles collapse with minimal damage. If, however, the second pulse arrives later in the cycle, bubble collapse is accelerated and damage is enhanced. Bailey originated dual-pulse lithotripsy and in his studies used twin shock sources oriented coaxially facing one another [138]. The concept holds promise, as this may be a means to tailor acoustic forces within the focal zone for better breakage of stones, hopefully with reduced collateral damage [144, 145]. Shock waves cause trauma and any strategy that lowers the dose of shock waves needed to treat a patient should be welcomed. One way to reduce unnecessary shock wave impact on tissue is to track the stone during treatment and to only fire when the shock wave will hit the stone. A device has also been proposed to exploit acoustic timereversal to dynamically change the focus of the lithotripter and so hit the stone even as it moves [151, 152]. Such concepts have the potential to dramatically reduce the number of shock waves required to break a stone. A number of clinical trials have reported data on the effect of rate and a meta-analysis of those studies indicates that firing at a lower rate does result in improved stone comminution [133]. Further data in the pig model indicate that delivering shock waves more slowly results in less tissue damage [64]. It may also be that at slower rates the cavitation bubbles from the previous shock have more time to dissipate and in addition cumulative shear should produce less damage [111]. The attempt to design a lithotripter so that it can be operated "anesthesia free," on the other hand, has proven to be a much more difficult problem. Discomfort during shock-wave treatment is due primarily to the sensation of cutaneous pain over the area of shock-wave entry at the surface of the body. One attempted solution was to widen the aperture at the shock source in order to spread the energy over a broader area. A wider aperture broadens the acoustic field along the shock-wave axis, but it narrows the focal zone of the pressure pulse. Many current lithotripters have a very narrow focal zone, of the order of 5 mm or less.
Buy generic zovirax 400mg
It is detected 362 Section 3 Ureteroscopy: General Principles Ureteroneocystostomy can be divided in to two broad categories: (1) that with relative preservation of the ureteral anatomy hiv infection rates lesotho purchase zovirax uk. The Cohen technique is associated with relocating the ureteral orifice to the contralateral side of the trigone in a submucosal tunnel [35]. Possible maneuvers to overcome this problem include antegrade ureteroscopy [33]; antegrade percutaneous placement of an internal ureteral stent followed by retrograde urethral ureteroscopy [36]; percutaneous, needle-guided, transvesical trocar placement in direct alignment with the reimplanted ureter followed by transvesical retrograde ureteroscopy [37, 38]; and application of a 5F cobra-head catheter with the advancement of either a straight or angled-tip glidewire [39, 40]. This maneuver further aids in overcoming "unusual angles" to better delineate the anatomy during retrograde ureteroscopic access [28, 30, 31]. Feces has been noted to reflux in to the collecting system during ureteroscopy; however, as long as proper drainage is maintained, this event should not lead to infectious complications. In addition to a nephrostomy tube, the preferred method of drainage is with a single-J biliary stent, which has multiple large side holes along its distal part, hence optimizing the drainage of both urine and feces [28]. Neobladders Unique challenges have been identified with this type of urinary diversion. Often a retrograde approach to the implanted ureteral orifice is fraught with difficulty. Nonuniformity of the orifice location combined with mucosal folds often make identification of the ureteral orifices time-consuming, if not impossible. In a Kock pouch diversion, the use of a flexible ureteroscope is strongly recommended, as the excessive torque required for a rigid endoscope to reach through an afferent nipple has the potential to injure the sphincter [31]. With a right colon pouch diversion, the delicate continence mechanism may be compromised using a standard cystoscope to identify the ureteral orifice. In many orthotopic neobladder techniques, either one or both ureters are implanted in to an afferent limb of bowel that extends from the reservoir. In such cases, identification of both the limb and associated ureters is crucial [32]. Direct visualization of the ureteral orifice requires flexible cystoscopy as access usually requires a "retroflexion maneuver. Again, the key point in all these cases is placement of an antegrade guidewire through the collecting system down in to the reservoir; it serves as a safety wire and a landmark when performing retrograde ureteroscopy. Renal transplantation Ureteral reimplantation during renal transplant results in an ectopic and anterior ureteral orifice, making its identification difficult [20]. Nevertheless, retrograde ureteroscopy of a transplanted ureter can be successful with technique modifications [41, 42]. In addition, a flexible cystoscope as well as angled catheters (Kumpe or cobra) and angled hydrophilic glidewires may be useful for negotiating both the acutely angled transplanted ureteral orifice, as well as the frequently tortuous and redundant transplanted ureter [20]. Summary and conclusions Whether the ureter has a classical or an unusual appearance, one should be familiar with both the normal and potential abnormal anatomy, as a result of congenital anomalies or previous surgical procedures. The anatomy of the ureter should never be overlooked when considering any type of endoscopic manipulation. Appropriate preoperative evaluation and intraoperative endourologic techniques should ensure proper, smooth, and usually successful endoscopic procedures. Reports of ureteroscopy performed on a reimplanted ureter have started to emerge as this pediatric population has entered adulthood, with an increased incidence of urolithiasis. Crossing vessels at the ureteropelvic junction: do they influence endopyelotomy outcome Holmium laser ureteroscopic treatment of various pathologic features in pediatrics. Successful management of lower-pole moiety ureteropelvic junction obstruction in a partially duplicated collecting system using minimally invasive retrograde endoscopic techniques. Endourological management of a large distal ureteral calculus in a patient with ureterosigmoidostomy diversion. Combined antegrade and retrograde endoscopic approach for the management of urinary diversion-associated pathology. Management of nephrolithiasis after Cohen cross-trigonal and Glenn-Anderson advancement ureteroneocystostomy. Percutaneous transvesical ureteroscopy for removal of distal ureteral stone in reimplanted ureter. Strategies for ureteral catheterization after antireflux surgery by the Cohen technique of transverse advancement. From the humble beginnings where Young performed the first recorded ureteroscopy in 1912 using a 9. The introduction of fiberoptics paralleled by the progression of instrument technology has led to smaller, more maneuverable scopes with more acceptable ergonomic layouts. The latest generation of ureteroscopes now provides high-definition digital images of the ureter and intrarenal collecting system, allowing procedures to be carried out safely, with high success rates and minimal morbidity in adults and children. To appreciate how ureteroscopes have evolved in to their present day guise, this chapter begins with a summary of key technical developments, starting with the first acknowledgment of the endoscope, the effect of changes in instrumentation, and progressing through to the latest digital technology. A breakdown of key features of ureteroscopes is then given, discussing their similarities and differences before moving on to consider ureteroscopes currently available and potential future trends for their further development. The traditional components required to carry out a rigid endoscopic procedure are the telescope with working channels for irrigation and instrumentation, a light source, optics to convey the image, and a camera system to capture the image. The digital era is here and will eventually condemn the fiberoptic arrangement to the historical archives. The forerunner of the endoscope can be traced back to 1806 with the construction of the light-guiding instrument or "Lichtleiter" by Phillip Bozzini for direct inspection of internal organs [5]. This scope was basic in design, consisting of a direct-vision hollow tube through which candlelight was transmitted by a mirror. The NitzeLeiter cystoscope, a rudimentary version of the modern cystoscope, was constructed in 1879, incorporating a simple lens system in to the viewing tube [5]. The introduction of fiberoptic lighting in the 1960s replaced the incandescent bulb, revolutionizing the manufacture of rigid endoscopes. The design was based on the principle of total internal reflection; when light travels in a transparent medium such as glass, internal reflection of the light occurs at the interface between the medium and its surroundings, as demonstrated by John Tyndall in 1854 [6]. This physical property of internal reflection allows the "bending" of light within flexible glass. Thus, light travelling inside a small-diameter flexible glass fiber surrounded by cladding of lower refractory index can be transmitted over a long distance with minimal degradation. The benefit of modern fiberoptic lighting is greater illumination by cooler light, ultimately making it safer. An additional benefit is that the scopes can be made with a smaller-profile shaft, allowing more room within the shaft for the addition of an irrigation and instrument channel. The fiberoptic cable is often attached via a light post to the endoscope, but may alternatively be built in to the design of the scope. Until then, the shaft of the scope consisted of a hollow tube with a series of thin relay lenses separated by long air spaces. The relay lenses had to remain in precise alignment and any displacement of the lens resulted in a significant loss of image transmission. Hopkins replaced the thin relay lenses within the shaft of the endoscope with long, contoured glass rods acting as the transmission medium, whilst the thin pockets interspersed between the glass rods acted as lenses. With the telescope primarily being Chapter 34 Rigid and Flexible Ureteroscopes: Technical Features 367 made of glass, which has a higher refractive index than air, light transmission could be increased ninefold over previous lens systems, with the additional benefit of reduced image distortion and a wider viewing angle. The outer diameter of the endoscope shaft could also be reduced, paving the way for the development of the rigid ureteroscope and the introduction of working channels. The problem manifests itself as a halfmoon or crescent-shaped defect when viewing through the scope eyepiece.
Buy line zovirax
Inherent to the preoperative assessment is a detailed history and targeted physical examination to identify physiologic changes associated with certain disease states hiv infection rates south africa generic zovirax 200 mg on-line. Evaluating the demographics of age, height, weight, and vital signs, to a full list of medications, allergies, and prior medical, surgical, and social factors is necessary. Furthermore, knowledge of previous laboratory values and ancillary studies facilitates anesthetic plan- Complexity of surgical procedure: considerations for the anesthetic With a larger more complicated stone burden that requires a prolonged surgical time, the likelihood of needing general or neuraxial (spinal or epidural) anesthesia increases. For cases involving access, dilation, and stone extraction during the same procedure, a "type and screen" for blood products should be considered in the event of unanticipated significant blood loss. Further, adequate intravenous access should be secured prior to initiation of surgery. Utilizing the "type and cross" method of reserving blood products can lead to extra cost, blood wastage, and transfusing red cells of increased age that have diminished oxygen carrying capacity. The time for most blood banks to convert a "type and screen" to available crossed units is minimal unless the patient has been recently transfused or has rare antibodies. Many centers have described a "maximum surgical blood ordering schedule" to minimize these issues [26]. Conversely, widespread preoperative testing without consideration of actual utility, cost, or effect on management is not beneficial ("screening" tests), and may actually increase physician liability [31]. Testing should be based upon positive physical examination findings and anticipated physiologic disturbances, such as irrigant absorption or blood loss. Results should aid in assessing the degree of medical optimization and in anesthetic planning. The preanesthetic medical history should include a complete list of medications, including over the counter and homeopathic herbal agents, in order to define an appropriate preoperative medication regimen and anticipate potential interactions with anesthetic agents. Examples of some commonly withheld medications prior to surgery are listed in Tables 8. Furthermore, certain medications, including most antihypertensives, beta-blockers, H2 blockers, and proton pump inhibitors should be continued through the morning of surgery. Clonidine, an alpha-agonist, should be continued through surgery to avoid extreme rebound hypertension. This combination of agents has been suggested to maintain balanced coronary blood flow during times of stress and hemodynamic instability [28, 43]. The pleiomorphic (arterial plaque stabilizing) effects of statins may provide this myocardial protection [39, 44]. Ideally, insulin dependent diabetics should be scheduled early on the morning of surgery and maintained on exogenous insulin serving basal requirements (glargine, subcutaneous insulin pumps, etc. Noninsulin dependent diabetics can withhold most medications on the day of surgery. Additionally, certain disease states are of great significance when planning anesthetic management. Patients with significant arrhythmias (high-grade atrioventricular block, symptomatic arrhythmias with underlying heart disease, or supraventricular arrhythmias with uncontrolled ventricular rate and severe valvular disease) have increased risk of com- plications during noncardiac procedures (>5%). Patients presenting with these clinical predictors of cardiovascular disease warrant further evaluation prior to elective procedures, including low-risk procedures. These issues may be stable and medically managed and may not warrant further evaluation [8]. Assessing pulmonary function requires a basic physical examination and screening assessment that includes questions regarding the history of tobacco use dyspnea, cough, wheezing, stridor, snoring, sleep apnea, or symptoms of recent upper respiratory tract infection [47]. Physical examination should assess diminished breath sounds, wheezing, stridor, or rales, as well as respiratory rate, chest excursion, and use of accessory muscles of respiration. The degree of baseline dyspnea should be assessed relative to physical exertion or exercise tolerance. Further tests (spirometry, lung volumes, and/or arterial blood gas) may be useful to anticipate challenges Chapter 8 Special Anesthetic Considerations for Endourology 127 with anesthesia [48, 49]. Such patients may be dependent upon accessory muscles of respiration to maintain adequate ventilation and thus may be prone to needing prolonged intubation and ventilatory support [49, 50]. All of these medical issues must be weighed relative to the risk of surgical procedure, surgical stress response, and potential for hemodynamic fluctuations. It is worth noting that functional capacity or exercise tolerance is another important determinant of patient status that translates to perioperative risk [8]. Selfreported estimate of exercise tolerance in metabolic equivalents or perceived level of daily exertion has been shown to correlate with perioperative complications [52]. They demonstrated that limits in preoperative functional capacity, as defined by an inability to walk four blocks or climb two flights of stairs, independently predicted complications with an odds ratio of 1. This study and others further support the lack of benefit of further testing if a patient reports good exercise tolerance, independent of surgical severity, complexity, or anticipated method of anesthesia [53]. With the information detailed in the preoperative assessment, the anesthesiologist planning the anesthetic for the procedure should be adequately prepared to design an anesthetic that minimizes postoperative risks inherent to specific disease states. If the patient has become unresponsive to pain and other arousal, due to sedative effects, then the anesthetic is defined as "general. Varying degrees of respiratory suppression and cardiovascular depression (mild at sedative doses) can occur, depending on the agents and combinations used. When determining patient "tolerance" of sedation, it must be considered whether the patient has known or suspected obstructive sleep apnea that may be exacerbated during sedation (especially among the morbidly obese). The hypoventilation that occurs with progressive sedation leads to hypercarbia, which is welltolerated by most patients, but can be life-threatening for patients with severe pulmonary hypertension due to the pulmonary vasoconstriction and right heart failure it precipitates. Patients with sickle cell anemia also tolerate hypercapnia and hypoxemia poorly due to the propensity of hemoglobin S to further decrease oxygencarrying capacity under such conditions. With decreasing oxygen levels and the resultant increase in arterial carbon dioxide tension, intracranial pressure could increase to dangerous levels, especially if there is preexisting intracranial pathology. These depend upon the specific anesthetic agents and technique used, as well as the physiology of a specific patient and the details of the procedure. This Physiologic changes from anesthetics Surgeons should be aware of the basic physiologic effects of the anesthetics given during endourologic procedures. This includes patients who have not fasted for 6 or more hours (solids), patients with gastroparesis and delayed gastric emptying, or those who have recently vomited. Although these laryngeal mask devices can be used with neuromuscular blocking drugs, this technique requires positive pressure ventilation through a partially unprotected airway, possibly increasing the likelihood of aspiration as well as loss of ventilatory pressure and volume from the breathing circuit. Few anesthesiologists choose this technique; however, some will use a low positive pressure assist ventilatory technique to achieve higher tidal volumes than with unassisted, anesthetized, spontaneous ventilation. An endotracheal tube allows for positive pressure ventilation with higher airway pressures than manageable with a laryngeal mask device. It is a definitive airway for prone and lateral positioning and is unlikely to be dislodged if secured in place. Alternatively, the airway may be managed with the insertion of a laryngeal mask airway device, which is a cuffed mask that sits above the glottic opening in the posterior hypopharynx, with a tube conduit exiting the oropharynx. Several manufacturers make these devices that connect to the anesthesia breathing circuit to allow delivery of oxygen and anesthetic vapors, either during spontaneous or assisted hand ventilation modes. This device lowers the risk of injury to the larynx or trachea from endotracheal tube placement, and also allows for a lighter anesthetic, due to lack of tracheal or carinal stimulation. Unfortunately, the device does not Normal ventilation Maintaining airway/ hypoventilation Airway obstruction/severe hypoventilation Central apnea Airway management The guidelines also recommend that these patients receive pre- and post-operative interventions to reduce pulmonary complications, such as triple cough exercises, incentive spirometry, and early ambulation postoperatively. Local anesthetic and adjuvants are chosen based on expected duration of the procedure, postoperative disposition of the patient ( to home vs inpatient), and anticipated dermatomal level of surgical stimulation. Baricity and dose of the local anesthetic injected also influence the extent and duration of anesthesia. With this, another parenteral analgesic may be needed to provide a sufficient "bridge" of analgesia until the patient is ready to take oral analgesics. Epidural anesthesia involves injection of larger volumes and doses of local anesthetics as well as adjuvants in to the epidural space which lies just outside the dural sac. Such larger volumes are needed to ensure significant spread of the local anesthetic within the dural area to reach nerve roots. One drawback of epidural anesthesia for endourologic procedures involving the perineum is occasional "sacral sparing" that may occur. This is a deficit of anesthesia in the sacral dermatomes due to the larger size of the L5, S1, and S2 nerve roots [56]. This may be advantageous in that a smaller band of anesthesia may be achieved, if desired, by using smaller doses of local anesthetics. Choice of specific local anesthetic and its dose affect the duration and density of the block, as well as the extent of motor block achieved.
Purchase zovirax mastercard
The rate of proliferation of tubule cells was 10-fold higher than that of interstitial cells antiviral ribavirin buy zovirax 200mg. There was a sharp peak in tubular apoptosis at day 25, whereas interstitial apoptosis peaked at day 75. The apoptotic rate was twofold higher in tubular cells than in interstitial cells. Tubular apoptosis was maximal at day 15, whereas interstitial apoptosis was still increasing at day 45. Thus, the function of several known antifibrotic agents can be explained by effects on apoptosis. We have recently used a tetrapeptide antioxidant, has been studied using immunohistochemistry, and conflicting results have been found. Control renal tissue was obtained from presumed normal sections of kidneys of patients with renal tumors. Compared to control tissue, kidneys from patients with hydronephrosis exhibited increased interstitial volume and collagen deposition. Administration of either 1D11 or enalapril individually significantly decreased all these changes; when 1D11 and enalapril were combined, there was little additive effect, and the combination did not provide full protection against damage [126]. Blunt ended blue lines and green arrow-tipped lines indicate the site/stage of antiapoptotic effect. With the new description of other cell types and other cell transdifferentiations, as well as mediators such as cytokines or reactive oxygen species, there may be new targets which can be developed to improve antifibrotic therapy. Pathophysiology of unilateral ureteral obstruction: studies from Charlottesville to New York. Renal function in chronic hydronephrosis with and without infection and the role of the lymphatics. The absence of a triphasic renovascular response by the multicalyceal kidney of the primate in reaction to acute, complete, unilateral, ureteric obstruction. Hemodynamic changes after complete unilateral ureteral obstruction in the young lamb. On the site of decreased fluid reabsorption after release of ureteral obstruction in the rat. Deep nephron function after release of acute unilateral ureteral obstruction in the young rat. Effect of acute ureteral obstruction on terminal collecting duct function in the weanling rat. Acute effects of brief ureteral stasis on urinary and renal papillary chloride concentration. The influence of volume expansion on renal function after relief of chronic unilateral ureteral obstruction. Effect of prostaglandin E1 on the permeability response of the isolated collecting tubule to vasopressin, adenosine 3, 5-monophosphate, and theophylline. Technetium-99m (99mTc) mercaptoacetyltriglycine: Update on the new 99mTc renal tubular function agent. Well-tempered" diuresis renography: its historical development, physiological and technical pitfalls, and standardized technique protocol. Diuretic-induced urinary flow rates at varying clearances and their relevance to the performance and interpretation of diuresis renography. A comparison of pressure flow studies and renography in equivocal upper urinary tract obstruction. Diuretic enhanced duplex Doppler sonography in 33 children presenting with hydronephrosis: a study of test sensitivity, specificity and precision. Tubular reabsorption of phosphate after release of complete ureteral obstruction in the rat. Comparison of the renal hemodynamic response to unilateral and bilateral ureteral occlusion. Volume expansion enhances the recovery of renal function and prolongs the diuresis and natriuresis after release of bilateral ureteral obstruction: a possible role for atrial natriuretic peptide. Glomerular hemodynamics before and after release of 24-hour bilateral ureteral obstruction. Natriuretic peptides, their receptors, and cyclic guanosine monophosphate-dependent signaling functions. Atrial natriuretic peptide, right atrial pressure, and sodium excretion rate in the rat. Role of atrial peptide in the natriuresis and diuresis that follows relief of obstruction in rat. Renal function after release of ureteral obstruction: Role of endothelin and the renal artery endothelium. Role of platelet-activating factor in renal function in normal rats and rats with bilateral ureteral obstruction. Fluid balance in the urological patient: disturbances in the renal regulation of the excretion of water and sodium salts following decompression of the urinary bladder. Plasma levels and dialysance of atrial natriuretic peptide in terminal renal failure. Effects of acute bilateral ureteral obstruction on deep nephron and terminal collecting duct function in the young rat. Atrial natriuretic factor inhibits vasopressin-stimulated osmotic water permeability in rat inner medullary collecting duct. Dissection of key events in tubular epithelial to myofibroblast transition and its implications in renal interstitial fibrosis. Bone marrow-derived cells do not contribute significantly to collagen I synthesis in a murine model of renal fibrosis. Involvement of renal progenitor tubular cells in epithelial-to-mesenchymal transition in fibrotic rat kidneys. Pericytes and perivascular fibroblasts are the primary source of collagen-producing cells in obstructive fibrosis of the kidney. Metabolic and cellular alterations underlying the exaggerated renal prostaglandin and thromboxane synthesis in ureter obstruction in rabbits. Accelerated fibrosis and collagen deposition develop in the renal interstitium of angiotensin type 2 receptor null mutant mice during ureteral obstruction Rapid Communication. Chronic unilateral ureteral obstruction is associated with interstitial fibrosis and tubular expression of transforming growth factor-. Significance of postglomerular capillaries in the pathogenesis of chronic renal failure. Pathogenesis of chronic renal failure in the primary glomerulopathies, renal vasculopathies, and chronic interstitial nephritides. Significance of tubulointerstitial changes in the renal cortex for the excretory function and concentration ability of the kidney: a morphometric contribution. Number of interstitial capillary crosssections assessed by monoclonal antibodies: relation to interstitial damage. Induction of smooth muscle characteristics in renal interstitial fibroblasts during obstructive nephropathy. Proliferation of renal interstitial cells following injury induced by ureteral obstruction. Transforming growth factor-beta, basement membrane, and epithelial-mesenchymal transdifferentiation: implications for fibrosis in kidney disease. Origin of renal myofibroblasts in the model of unilateral ureter obstruction in the rat. Obstructive uropathy in the mouse: role of osteopontin in interstitial fibrosis and apoptosis. Renal growth factor expression during the early phase of experimental hydronephrosis. Chronic ureteral obstruction in the rat suppresses renal tubular Bcl-2 and stimulates apoptosis.
Purchase zovirax discount
Laparoscopic surgical repair Prior to surgical repair of a ureteral stricture antiviral zoster purchase cheap zovirax, it is important to conduct an evaluation of the nature, location, and length of the involved segment of ureter. This can be accomplished by performing a contrast imaging study: intravenous urogram, antegrade nephrostogram, or retrograde pyelogram, depending on the clinical circumstances. Ancillary studies, such as nuclear renography to assess renal function and ureteroscopy to define tissue viability and to help rule out upper tract carcinoma, should be performed depending on the clinical situation. Intraluminal sonography has an adjunctive role and has been employed to define the nature of a ureteral stricture including submucosal calculi, as well as periureteral structures including directly adjacent vasculature [10, 22]. Based on the results of these investigations, appropriate surgical intervention can then be planned and implemented. Combined retrograde/antegrade approach In rare situations, a ureteral stricture is associated with complete ureteral obstruction through which a guidewire cannot be passed in either a retrograde or antegrade fashion, thereby preventing balloon dilation or ureteroscopic endoureterotomy. A guidewire is then passed through one ureteral end, through-and-through to the other lumen, using a combination of fluoroscopy and direct visual control. If this is unsuccessful, a "cut-to-the-light" technique can be employed, whereby the ureteral segments are aligned as closely as possible using fluoroscopic and endoscopic control. The light source of one of the ureteroscopes is turned off and, using the light source of the other ureteroscope as a guide, an incision is made to restore ureteral continuity. A guidewire is then passed across the area incised to obtain through-and-through access. Endoscopy should be performed at the time of stent removal to re-evaluate the strictured area and determine if further endourologic maneuvers are required. Regular follow-up should be performed using a combination of renal ultrasound, intravenous urography, or nuclear renography to evaluate for stricture recurrence. Laparoscopic ureterolysis Retroperitoneal fibrosis and certain gynecologic lesions. Ureterolysis is effective for correction of ureteral obstruction in 90% of patients with retroperitoneal fibrosis [39]. When open surgical intervention is employed, it may be associated with significant morbidity in up to 60% of cases [39]. With the development of laparoscopic techniques for ureterolysis, the morbidity of the procedure has been reduced. Laparoscopic ureterolysis was associated with less intraoperative blood loss and need for parenteral pain medication, and significantly shorter hospital stay and convalescence than open surgery. Operative time was only marginally longer in the laparoscopy group (255 vs 232 min). Excretory urography and/or renal scan showed improved renal function and relief of obstruction in all patients in this study. Laparoscopic ureterolysis often begins with cystoscopic placement of a ureteral stent. The patient is then placed in the lateral decubitus position, pneumoperitoneum is obtained, and the laparoscopic ports are placed. Postoperative follow-up should include early imaging, at which time the ureteral stent can be removed. Laparoscopic ureteroureterostomy and ureterocalicostomy Ureteroureterostomy is most appropriate for short strictures involving either the upper or mid ureter. Only short defects should be managed by end-to-end ureterostomy, as longer strictured segments may result in tension on the anastomosis with potential recurrence of obstruction. Determination of whether enough ureteral mobility can be achieved to obtain a tension-free ureteroureterostomy anastomosis is often an intraoperative decision. Long-term success with a tension-free, watertight ureteroureterostomy is well over 90% [40]. Ureteroureterostomy has been performed using both an open or laparoscopic approach. The laparoscopic technique, albeit endoscopic, follows the tenets of open surgical repair, creating a tension-free spatulated anastomosis. The obstructed ureteral segment was resected and the ureteroureterostomy was performed laparoscopically over a ureteral stent. In a retrospective review involving eight laparoscopic ureteroureterostomy patients, Nezhat et al. Laparoscopic ureteroureterostomy is also an option for managing mid-ureteral obstruction due to a retrocaval ureter. Laparoscopic management of ureteral injuries employing a primary ureteroureterostomy has also been described, albeit in only a few cases. When a ureteral injury occurs during a laparoscopic procedure, for example, it can be primarily repaired over a stent using intracorporeal laparoscopic suturing without the need for open conversion. The peritoneum is incised along the line of Toldt and extended caudally over the iliac vessels and medial to the medial umbilical ligament. The colon is reflected medially and the entrapped ureter identified with the indwelling stent acting as a guide. Meticulous dissection is performed to mobilize the ureter, freeing it from adjacent structures. Similar to the open surgical technique, a vessel loop can be placed around the ureter to facilitate gentle traction during mobilization. A biopsy of the retroperitoneal fibrotic process can be helpful if clinically indicated. Once the ureter is freed from the retroperitoneal fibrotic process, it is positioned in to the peritoneal cavity by reapproximating the previously incised edges of the posterior peritoneum using standard laparoscopic intracorporeal suturing techniques with 2-0 absorbable suture. Follow-up is based on serial evaluations, identical to the algorithm employed after open surgical repair. Two patients were discharged home within 3 days postoperatively, whereas one patient had a lengthy hospital stay due to Clostridium difficile colitis. Patency of the anastomosis was radiographically demonstrated at 6-month follow-up. The overall clinical experience in laparoscopic ureteroureterostomy is broadening [46]. Ureterocalicostomy is a standard intervention for more proximal ureteral strictures that cannot be repaired with a primary ureteral reconstruction. As with ureteroureterostomy, laparoscopic technique should mirror the open surgical procedure. Resecting a generous portion of lower pole parenchyma and exposing a suitable calyx for anastomosis is key. Viable proximal ureter is spatulated and anastomosis performed with interrupted absorbable suture, commonly over a ureteral stent. Postoperative management and follow-up is identical to that employed with pyeloplasty. Both ureteroureterostomy and ureterocalicostomy reflect excellent minimally invasive interventions for moderate length ureteral strictures or injuries. Conclusions With advances in technique and endoscopic instrumentation, urologists are commonly employing minimally invasive therapies to address various urologic disorders, including ureteral obstruction. As progress continues in the field of endourology and laparoscopy, additional urologic procedures will be performed using a minimally invasive approach, reducing patient morbidity, while maintaining or expanding treatment efficacy. In this era of the endoscopist, minimally invasive treatment of ureteral strictures has not only become standard at teaching centers, but is also commonly employed in community settings worldwide. Laparoscopic Boari flap When the diseased ureteral segment is distal and deemed too long for primary repair or when ureteral mobility is too limited to perform a tension-free ureteroureterostomy or a Psoas hitch ureteroneocystostomy, a Boari flap repair is a useful alternative. Evaluation of bladder function should be performed preoperatively in addition to the aforementioned evaluation of the ureteral stricture. If there is evidence of bladder outlet obstruction or neurogenic dysfunction, this should be evaluated and addressed preoperatively. Additionally, the bladder should be of sufficient capacity to allow for creation of a sufficiently long Boari flap; otherwise alternative options should be considered. A laparoscopic Boari flap has been successfully employed to treat long distal ureteral defects and strictures. Following open surgical principles, the bladder is mobilized from its peritoneal attachments and the most superior contralateral bladder pedicle is divided, allowing greater mobility toward the ipsilateral ureter. The ipsilateral bladder pedicle, including the superior vesical vasculature, is preserved and the affected ureter is carefully mobilized, with care taken to preserve its blood supply.
Purchase generic zovirax online
There are many electrohydraulic generators available and probe size is variable from 1 hiv infection rate in botswana purchase cheap zovirax on-line. It is noteworthy that the smaller probes are flexible enough to allow their use with flexible ureteroscopes. The goal of treatment is to create fragments that can either be easily extracted or passed spontaneously. Attempts to create fragments smaller than 2 mm have a higher probability of mucosal injury. Ultrasonic lithotripsy the upper limit of sound audible to the human ear is generally regarded to be 20 kHz. Sound waves with a frequency above this threshold are referred to as ultrasound waves. The first attempted use of ultrasound waves to fragment urinary calculi was reported in 1953 by Mulvaney [14]. Since then the technology has progressed significantly and ultrasonic lithotripsy is now commonplace within clinical endourologic practice. The plate generates vibrational energy in the form of ultrasonic waves at a frequency between 23 and 25 kHz. This energy is transmitted through the hand piece to a solid or hollow probe that is placed in contact with the stone. The vibrations of the probe transmit the energy to the calculus, resulting in a drilling effect. The larger probes incorporate a hollow channel through which suction is applied [the smaller probes (2. The presence of this channel gives these devices a major advantage in that small stone fragments (<2 mm) can be evacuated as lithotripsy is performed. As the mechanism of stone fragmentation in ultrasonic lithotripsy is purely mechanical, direct contact with the stone is necessary. As pressure is used to pin the calculus between the probe and urothelium in most cases, the question of safety and the potential for urothelial perforation is of utmost concern. After histologic examination it was demonstrated that injury was limited to abrasions of the epithelium [8]. The mechanism of stone destruction raises a concern regarding the generation of heat at the site of interaction between the stone and probe. Although there is a potential for thermal injury, it is only of concern if irrigation is interrupted, as it has been demonstrated that at an irrigation rate of 30 mL/min the change in temperature at the probe tip is minimal (1. Despite the intermanufacturer variability in efficiency, ultrasonic lithotripsy has been demonstrated to be an effective and safe means of lithotripsy. As previously stated, a major limitation of the ultrasonic lithotriptor is its inherent rigidity. When used in conjunction with a semi-rigid ureterscope to treat ureteral calculi, a large working channel of at least 5F is needed to accommodate the smallest probe with an incorporated suction channel (4. Given the rigid nature of the ultrasonic probes, which inherently limits the deflection of flexible scopes, ultrasonic lithotripsy of ureteral calculi may have its greatest utility in distal ureteral stones. The first use of ultrasound to treat a staghorn calculus was reported in 1977 [24]. Since then many researchers have demonstrated percutaneous ultrasonic treatment of renal stones to be an effective and safe procedure with success rates of 80. Technically, when ultrasonic lithotripsy is applied, the stone should be trapped between the probe and the urothelium. Pressure is needed to maintain this relationship, but care should be taken to avoid excessive pressure as perforation is possible, especially in the thin-walled renal pelvis or ureter. Multiple shortduration applications of the ultrasonic energy to the stone results in fragmentation. Longer durations of activity provide shorter treatment times but carry the potential to generate a thermal injury and may lead to diminished vision. In addition to the aforementioned advantages of ultrasonic lithotripsy, it is relatively inexpensive. Pneumatic lithotripsy Another example of a direct contact lithotriptor is ballistic lithotripsy. In this model of lithotripsy a projectile is set in motion, culminating in a jackhammer effect. Although any number of driving forces can initiate the movement of the projectile, the most notable and most widely utilized is compressed air. Using this model the Swiss Lithoclast has been found to be a very effective means of intracorporeal lithotripsy. Under close visual guidance, the tip of the metal probe is placed in to direct contact with the calculus and repetitive impacts result in stone fragmentation. Since its first clinical use in 1991 [29], the Swiss Lithoclast has been extensively studied. As in ultrasonic lithotripsy, the mechanism of action in pneumatic lithotripsy raises concern over the potential for collecting system injury, specifically perforation. On histologic examination, the lithoclast resulted in only partial abrasion of the epithelium and edema of deeper layers [8]. Additional animal studies have further documented the safety of the Swiss Lithoclast; notably Santa-Cruz et al. One of the limitations of pneumatic over ultrasonic lithotripsy is the solid design of the probe, and therefore the lack of a suction channel. The development of a suction channel through which pneumatic lithotripsy is commenced and suction is applied alleviated this concern. In addition, the application of suction during pneumatic lithotripsy can counteract another major disadvantage of direct contact lithotripsy, retropulsion of stone fragments [33]. Its 272 Section 2 Percutaneous Renal Surgery: Stone Removal pedal and enables the surgeon to use either of the lithotriptors individually or in combination. Stone fragmentation was successful in all 15 patients with renal and bladder stones. The combination pneumatic/ ultrasonic unit was found to be significantly more efficient in completely fragmenting and clearing the stone model compared to either pneumatic or ultrasonic lithotripsy alone (7. In the largest of these studies, 68 patients were treated for staghorn calculi over a 2-year period. The combination device required significantly less time for complete stone clearance (21. Further studies are required to adequately define the role of the combined ultrasonic and pneumatic lithotriptor amongst the currently available intracorporeal lithotriptors. The rigid nature of the probes also limits the ability to use the Swiss Lithoclast with ureteroscopy. Despite the added ability to use the Lithoclast with a flexible ureteroscope, a significant decrease in tip displacement and velocity, and therefore effectiveness, is noted as the scope is deflected [40]. Technically, the use of pneumatic lithotripsy is facilitated by the use of a nondeflected working channel. Direct vision should always be employed to ensure safety as well as to facilitate adequate fixation of the calculus against the urothelium. When the smaller probe was used, however, a slower rate of impact (6 vs 12 Hz) was found to be more effective [41]. Combined ultrasonic and pneumatic lithotripsy Ultrasonic lithotripsy provides the surgeon with a very effective method for stone removal. The incorporated suction channel functions to decrease the effects of stone retropulsion and further assists with the removal of fragments less than 2 mm in diameter. Unfortunately, ultrasonic lithotripsy has limitations, especially when it comes to the destruction of very dense or hard stone compositions (calcium oxalate monohydrate). Pneumatic lithotripsy has previously been demonstrated to be a very effective endoscopic lithotriptor, especially when treating hard or very large stones [38, 39]. Unfortunately, this device results in the formation of relatively large stone fragments and the lack of a suction channel further interferes with stone removal.
Generic zovirax 800 mg free shipping
The advent of smaller-caliber endoscopes [2] antiviral immune response buy zovirax 800mg without a prescription, and development of laparoscopic reconstructive techniques, laser technology, and robotics have diversified the treatment options for this condition. Although the efficacy, and decreased morbidity, hospital stay, and need for analgesia with endopyelotomy have been clearly demonstrated, several issues have still not been completely resolved. In the era of minimally invasive laparoscopy and robotic-assisted surgery, is there still a role for endopyelotomy Open surgical correction was the only mode of treatment for this condition before the introduction of endoscopic and laparoscopic techniques, and has been considered the gold standard of treatment for this condition, with success rates over 90% [3]. However, associated morbidity is not unusual with open surgery; specifically, there is fistula formation in 2. Also, the initial report of ureteral stricture formation because of thermal injury from transmission of the electrocautery current has been eliminated with the use of insulated ureteroresectoscopes and holmium laser fibers [30]. Among the absolute contraindications are patients with active infection and bleeding diathesis. Patients with a relatively long length of obstruction, usually greater than 2 cm, are best managed either with open surgical, laparoscopic, or roboticassisted techniques. Patients with ipsilateral differential renal function of less than 20% and severely decreased parenchymal thickness can be given a trial of drainage and re-evaluation [15] or should be offered a laparoscopic simple nephrectomy for a poorly functioning or nonfunctioning kidney. Patients with massive hydronephrosis should be treated with dismembered pyeloplasty, either open surgical, laparoscopic, or robot assisted, because of the need for trimming and reduction of the redundant renal pelvis. A single-setting, onestage procedure was subsequently described by Soroush and Bagley in 1998 [11]. Currently, a retrograde endopyelotomy can be performed in three ways: (1) using a rigid ureteroscope and a cold-knife, electrocautery, or holmium laser incision; (2) using a flexible ureteroscope and electrocautery or laser incision; and (3) in rare select cases, using a balloon with a cutting wire (Acucise) [15]. Although once considered a contraindication because of poor results, published series report that the type of ureteral insertion has no significant impact on the outcome of endopyelotomy [24], and that patients with crossing vessels had long-term success with retrograde endopyelotomy [14]. Lastly, patients with known intractable stent intolerance should be considered candidates either for an antegrade endopyelotomy or an open pyeloplasty with a nephrostomy tube, and not for ureteroscopic endopyelotomy. Above all, preoperative placement of the stent allows evaluation of any degree of stent intolerance and identifies improvement of renal function after drainage. A B Step-by-step operative technique the required instrumentation is listed in Table 42. After either a general or a spinal anesthesia, the patient is placed in the lithotomy position. Caution is taken so that all pressure points are well cushioned, and antiembolic stockings are used in high-risk patients. A retrograde pyelogram can assess any resolution of hydronephrosis and can be used as a prognostic indicator. The next step varies depending on whether the endopyelotomy is done with electrocautery through a ureteroresectoscope or whether a holmium laser is used through a rigid, semi-rigid, or flexible ureteroscope. A balloon dilator can be passed over the guidewire and the ureteral orifice dilated in case of difficulty advancing the ureteroscope within the ureter. If necessary, another guidewire can be passed through the ureteroscope and the narrow area subsequently balloon dilated. A 365-m holmium laser fiber, when using a rigid or semi-rigid ureteroscope, or a 200-m fiber in the case of a flexible ureteroscope, is passed through the working channel of the ureteroscope. After hemostasis of any venous bleeding is performed, the laser fiber and ureteroscope are removed. An endopyelotomy stent is placed under fluoroscopic control, leaving Ureteroscopic endopyelotomy with electrocautery A 5F open-ended catheter is passed over the super-stiff wire. Short and shallow strokes should be performed and aggressive and deep incisions avoided. The incision is carried down until periureteral fat is seen and the ureteroresectoscope enters the renal pelvis with ease. Postoperative care the vast majority of patients are discharged either the same day or within the first 24 h following the procedure. Success following endopyelotomy is measured by evaluating improvement of the function and drainage of the involved kidney and alleviation of symptoms. Also, the open-ended catheter may serve to continuously drain the renal pelvis of the irrigant used during the procedure, once the wire is removed. The ureteroresectoscope is passed directly alongside the insulated guidewire with the cold knife in place. The electrocautery element is right angled and would impede vision if placed during the insertion of the ureteroresectoscope [1]. If there is difficulty accessing the ureteral orifice or the intramural ureter, a balloon dilator can be passed over the guidewire to dilate the area. If necessary, another guidewire can be passed through the self-dilating ureteroscope and the narrow area is balloon dilated. These patients included seven pediatric patients, four solitary kidneys, two horseshoe kidneys, and one ptotic kidney. Seventy-nine percent of the patients were discharged home on the same day, and 97% of them within 24 h. Of the 139 patients 32 (23%) required subsequent procedures to treat recurrence of obstruction, showing an overall long-term success rate for retrograde ureteroscopic endopyelotomy of 77%. Significant bleeding requiring emergent nephrectomy is another possible complication that justifies the need for vascular or three-dimensional (3D) radiographic studies to identify aberrant vessels. Minor complications of retrograde ureteroscopic endopyelotomy include proximal stent migration, stent intolerance, minor bleeding, and urinary tract infection after manipulation. Most of these complications are alleviated after removal of indwelling ureteral stents. The routine use of antispasmodic and anesthetic drugs after surgery improves tolerance to the stent and decreases complaints from the patient. After analyzing the failures of treatment in this series, two factors were obviously associated with poor results (no improvement of symptoms, drainage, and function after endopyelotomy): (1) a long-standing obstruction with a decrease in ipsilateral renal function of less than 20% of the total renal function; and (2) a severely dilated renal pelvis, which did not improve on drainage with an indwelling ureteral stent. After evaluation of these results, we conclude that patients with patulous redundant renal pelvis and borderline salvageable renal function should be considered candidates for alternative treatment modalities, such as open or laparoscopic/robotic pyeloplasty or nephrectomy, rather than endopyelotomy. Antegrade endopyelotomy requires expertise in percutaneous renal surgery, with detailed knowledge of the intrarenal anatomy and adequate experience in "realtime" 2D fluoroscopic imaging. This is the preferred technique when treating concomitant intrarenal calculi, but it is also associated with a larger potential for complications and morbidity. Antegrade and retrograde endopyelotomy share the potential for hemorrhage from injury to aberrant crossing vessels; however, antegrade access may also be associated with hemorrhage from the percutaneous renal tract and with a higher risk of infection owing to external urinary drainage through the percutaneous nephrostomy tube. Short-term success rates of this procedure have been comparable to those obtained with retrograde ureteroscopic endopyelotomy and range from 66% to 84% [35]. Extreme caution should be exercised when using this technique in the presence of aberrant crossing vessels. Use of this technique has Complications Since its initial description by Young in 1912, retrograde ureteroscopy has come a long way and has gained widespread acceptance as an option for the treatment of multiple pyeloureteric conditions. Further advances in technology have lead to the introduction of smallercaliber ureteroscopes with the capacity to accommodate accessory instruments necessary to perform diagnostic and therapeutic upper urinary tract procedures. As with ureteroscopy, the complications and adverse events associated with retrograde ureteroscopic manipulation of the ureter have decreased dramatically in the past two decades. Smaller-caliber ureteroscopes, the advent of laser technology, improved paraphernalia, and, above all, experience in the procedures should be given credit. Although these advances have decreased the need for open ureteral surgery, iatrogenic injury can still occur with the endoscopic technique. Possible iatrogenic complications of ureteroscopy include ureteral perforation, stricture, false passage, ureteral avulsion, bleeding from the ureteral mucosa or adjacent structures, infection, and sepsis. The reported incidence of pain, fever, false passage, and urinary tract infection are 5. At our institution we use an 8F double-J ureteral stent with postoperative results similar to those obtained with endopyelotomy stents.