Esidrix 12.5mg fast delivery
Infection symptoms 7dpo discount esidrix generic, Inflammation, and Demyelinating Diseases 412 (13-68) Listeriosis shows classic findings of midbrain abscess. They tend to be located in the same hemisphere and appear distributed along the white matter fiber tracts of the brain. This distinct pattern may allow for earlier diagnosis and possibly improve patient outcome. During the 2015 Ebola epidemic in West Africa, it became apparent that many patients likely died from acute fulminant meningoencephalitis, which was not initially recognized because of multiorgan involvement. The full range of neurologic sequelae in survivors is still being characterized in ongoing studies. The flaviviruses-primarily dengue and Zika virus-are some of the most important emerging viral infections with high global disease incidence and the potential for rapid spread beyond nonendemic regions. The clinical spectrum of dengue ranges from asymptomatic infection to life-threatening dengue hemorrhagic fever and dengue shock syndrome. Approximately 10% of patients with serologically confirmed dengue infection develop neurologic complications. In endemic areas, dengue has become the most frequent cause of encephalitis, surpassing even Herpes simplex virus. Currently, there are no licensed vaccines or therapeutics to counter human Filovirus infections. Tuberculosis and Fungal, Parasitic, and Other Infections spreading across the Americas. Autopsy studies demonstrate pituitary hemorrhage in 37%, pituitary necrosis in 5%, and brainstem hemorrhage in nearly 70%. Women now account for almost 52% of adult cases globally, and adolescent girls and young women in sub-Saharan Africa are being infected at twice the rate as that of boys and men of the same age. The same disease can have vastly different consequences-and therefore imaging appearances-in different parts of the world. New infection rates have been relatively stable since 2006 but are disproportionately higher in African American men compared with African American women, as well as higher in white men compared with white women. Opportunistic infections are absent early although coinfections or multiple infections are common later in the disease course. Although many patients remain asymptomatic for variable periods, brain infection is the initial presenting symptomatology in 5-10% of cases. Symmetric confluent hyperintensities have developed in the cerebral white matter and corpus callosum splenium. A burst of viremia develops within days and leads to widespread tissue dissemination. The activated cells also release neurotoxic factors such as excitatory amino acids and inflammatory mediators, resulting in neuronal dysfunction and cell death. The slight hyperintensity in the hemispheric white matter is not true diffusion restriction; rather, it is secondary to T2 "shinethrough. The multinucleated giant cells contain viral antigens and are immunoreactive for the envelope protein gp120. Disseminated patchy foci of white and gray matter damage with myelin pallor and diffuse myelin loss are prominent features. Lesions are most prominent in the deep periventricular white matter and corona radiata. Slowly progressive impairment of fine motor control, verbal fluency, and short-term memory is characteristic. Cortical thinning and bilateral white matter lesions are the most common parenchymal abnormalities. Mild to moderate atrophy with patchy or confluent white matter hypodensity develops as the disease progresses (142). With time, confluent "hazy," illdefined hyperintensity in the subcortical and deep cerebral white matter develops, and volume loss ensues (14-3). In fulminant cases, perivenular enhancement may indicate acute demyelination (14-5). Radial diffusivity is affected to a much greater extent than axial diffusivity, suggesting that demyelination is the prominent disease process in white matter. Large vessel disease is most common in immunocompetent individuals, whereas small vessel disease usually develops in immunocompromised patients. Overt neurologic disease often occurs months after zoster and sometimes presents without any history of zoster rash. Pathologic processes alter the composition of bone marrow, causing a relative increase in cellular hematopoietic tissue and a corresponding replacement of adipose tissue. Extracellular hemosiderin, hypercellularity, and increased numbers of monocytes and macrophages all contribute significantly to marrow hypercellularity. The cranium and mandible alone account for approximately 13% of active (red) marrow in adult humans. The prolonged T1 relaxation times alter signal intensity of hematopoietic bone marrow. However, they differ greatly regarding their etiology, clinical presentation, and management. Most lesions represent either benign nonneoplastic lymphoepithelial cysts or reactive lymphoid hyperplasia. Note the hyperplastic tonsils and multiple cysts in the superficial and deep lobes of both parotid glands. Affected patients can be asymptomatic or present with a nasopharyngeal mass, nasal stuffiness or bleeding, hearing loss, or cervical lymphadenopathy. Terminology and Etiology Toxo is caused by the ubiquitous intracellular parasite Toxoplasma gondii. Although any mammal can be a carrier and act as an intermediate host, cats are the definitive host. Although large lesions do occur, most lesions are small and average between 2-3 cm in diameter. Several small hyperintensities are also present in the right basal ganglia and thalamus. A large "tumefactive" lesion with a hypointense rim, hyperintense center, and striking peripheral edema is present. As a toxo abscess organizes, intensity diminishes, and eventually the lesion becomes isointense relative to white matter. A ring-shaped zone of peripheral enhancement with a small eccentric mural nodule represents the "eccentric target" sign (14-15D). The enhancing nodule is a collection of concentrically thickened vessels, whereas the rim enhancement is caused by an inflamed vascular zone that borders the necrotic abscess cavity. Disseminated toxoplasmosis encephalitis, also called microglial nodule encephalitis, produces multifocal T2 hyperintensities in the basal ganglia and subcortical white matter. Etiology and Epidemiology Crypto is excreted in mammal and bird feces and is found in soil and dust. Multiple gelatinous pseudocysts occur in the basal ganglia, midbrain, dentate nuclei, and subcortical white matter. Toxo usually has multifocal ring- or "target"-like enhancing lesions with significant surrounding edema. Lack of enhancement on T1 C+ is typical although mild pial enhancement is sometimes observed. Asymptomatic infection is probably acquired in childhood or adolescence and remains latent until the virus is reactivated. In the second phase, the virus persists as a latent peripheral infection, primarily in the kidneys, bone marrow, and lymphoid tissue. As the disease progresses, small foci coalesce into confluent lesions that can occupy large volumes of white matter. Early lesions appear as small yellow-tan round to ovoid foci at the gray-white matter junction. With lesion coalescence, large spongyappearing depressions in the cerebral and cerebellar white matter appear (14-23). Pale-staining demyelinating foci are bordered by large infected oligodendrocytes with violaceous nuclear inclusions (14-24). Drug withdrawal and plasma exchange therapy have been used with some success to increase survival in these patients. Note faint hyperintensity along the margins of the more anterior cerebellar lesions.
Cheap esidrix 25mg otc
A lesion proximal to the geniculate ganglion will cause facial paralysis and affect all three special functions treatment gonorrhea cheap 12.5mg esidrix mastercard. Cochlear nerve/modiolus, inferior /superior vestibular nerves, nuclei in medulla, tracts in inferior cerebellar peduncle. Ask if upper or lower motor neuron Parotid malignancies "creep up" facial nerve Special functions affected (taste, hyperacusis, lacrimation) It is the afferent sensory nerve responsible for hearing and the sense of balance. The cochlear nerve arises from the spiral ganglion in the modiolus of the cochlea. Its fibers coalesce to form the superior and inferior vestibular nerves, which are separated by a bony bar called the falciform (transverse) crest. The cochlear nuclei are found in the restiform body at the lateral surface of the inferior cerebellar peduncle. At least 90-95% of all lesions that cause unilateral sensorineural hearing loss-and are detected on imaging-are vestibulocochlear schwannomas. It is a special sensory nerve (responsible for taste in the posterior third of the tongue) as well as a regular sensory nerve (innervating middle ear, pharynx). It carries parasympathetic fibers to the parotid gland and is the motor supply to the stylopharyngeus muscle. All are in the upper and middle medulla, anterolateral to the inferior fourth ventricle. The tracts course anterolaterally from the nuclei to exit or enter the medulla in the postolivary sulcus. The cisternal segment travels toward the jugular foramen, coursing just above the vagus nerve. The glossopharyngeal nerve exits the skull by passing into the anterior aspect (pars nervosa) of the jugular foramen (23-7) (2335). In its skull base segment, the glossopharyngeal nerve lies adjacent to the inferior petrosal sinus. In the coronal plane, the jugular tubercles and basiocciput form a construct that resembles the head, beak, and body of an eagle. The vagus nerve is also a mixed nerve with sensory (ear, larynx, viscera), special (taste from epiglottis), motor (most of soft palate, superior and recurrent laryngeal nerves), and parasympathetic (regions of head/neck, thorax, abdominal viscera) functions. It descends, passing under the aortic arch on the left and the subclavian artery on the right. The recurrent laryngeal nerves on both sides then turn cephalad to course superiorly in the tracheoesophageal groove. Proximal vagal neuropathy requires imaging from the medulla to the level of the hyoid. Distal vagal neuropathy is usually isolated and manifests as laryngeal dysfunction (look for a paramedian vocal cord). It requires imaging from the level of the hyoid all the way to the carina/aortopulmonary window on the left and the subclavian artery on the right. The spinal accessory nerve is a pure motor nerve that innervates the sternomastoid and trapezius muscles. Spinal fibers originate from the spinal nucleus, a column of cells along the anterior horn extending from C1-C5 (23-39). The spinal fibers emerge from the lateral aspect of the cervical spinal cord and course superiorly (23-41). The extracranial segment begins as the glossopharyngeal nerve exits the jugular foramen into the carotid space. Look for trapezius atrophy and compensatory hypertrophy of the ipsilateral levator scapulae. The hypoglossal nerve is a pure motor nerve that innervates both the intrinsic and most of the extrinsic (styloglossus, hyoglossus, genioglossus) tongue muscles. The only exception is the geniohyoid muscle, which is innervated by the C1 spinal nerve. The hypoglossal nucleus lies just under the hypoglossal eminence of the inferior fourth ventricle. Fibers course anteriorly across the medulla and exit at the preolivary (ventrolateral) sulcus to enter the medullary (basal) cistern. The cisternal segment extends from its exit at the medulla through the basal cistern to the entrance of the hypoglossal canal (23-41). The extracranial segment of the hypoglossal nerve descends in the posterior aspect of the carotid space. It exits the carotid space between the carotid artery and the internal jugular vein, then runs anteroinferiorly toward the hyoid bone to provide motor innervation to the tongue muscles. Neoplasms, Cysts, and Tumor-Like Lesions 708 forms the medial wall of the short, obliquely oriented hypoglossal canal (2342). In the coronal plane, the jugular tubercle and occipital condyle form a visual construct that resembles the head, beak, and body of an eagle. The hypoglossal canal and nerve are located between its "head" and "beak" (2337) (23-43). Schwannomas Neuropathologists now recognize four histologic subtypes of schwannoma: conventional, cellular, plexiform, and melanocytic. The vast majority of schwannomas that involve cranial nerves are the conventional type. With the exception of melanotic schwannoma, imaging findings do not distinguish between histologic subtypes. Rather, conventional intracranial schwannomas are distinguished-and discussed here-according to their cranial nerve of origin. Because the pathology of intracranial schwannomas is similar, we discuss it and other shared features before delving into specific schwannomas. Schwannoma Overview Terminology Schwannomas are benign slow-growing encapsulated tumors that are composed entirely of well-differentiated Schwann cells. Schwannomas originate from Schwann cells, which are derived from precursor cells in the embryonic neural crest. The rare reported cases of "olfactory groove schwannomas" are probably tumors that arise from olfactory ensheathing cells. The exceptionally rare intraparenchymal schwannoma is thought to arise from neural crest remnants that later express aberrant Schwann cell differentiation. Intramedullary (spinal cord) schwannomas are more common than intraparenchymal brain schwannomas. Both sporadic and familial forms of schwannomatosis occur and can be associated with both nonvestibular intracranial and spinal schwannomas. Patients with schwannomatosis tend to be younger than those who present with solitary schwannomas. Plexiform schwannoma, also known as multinodular schwannoma, is a Schwann cell tumor in which multiple (2-50) circumscribed lesions occur along an affected nerve fascicle. The distance from the brain to the interface where the glial covering terminates and Schwann cell ensheathing begins varies with each cranial nerve. Sensory nerves are much more commonly affected by schwannomas compared with pure motor cranial nerves. The vestibulocochlear nerve is by far the most common Neoplasms, Cysts, and Tumor-Like Lesions 710 (23-45) Axial (L) and sagittal (R) graphics show a schwannoma arising within a unifascicular nerve. Intraparenchymal and intraventricular schwannomas occur but are extremely uncommon. Most intracranial schwannomas are small, especially those that arise from motor nerves. Some, especially trigeminal schwannomas, can attain huge size and involve both intra- and extracranial compartments. Most schwannomas occur singly in otherwise healthy individuals and are termed "sporadic" or "solitary" schwannomas. The presence of multiple schwannomas in the same individual suggests an underlying tumor predisposition syndrome. Schwannomas arise eccentrically from their parent nerves and are smooth or nodular well-encapsulated lesions (23-45) (23-46). The "Antoni A" pattern consists of compact fascicles of elongated spindle cells that demonstrate occasional nuclear palisading (Verocay bodies). A less cellular, loosely textured, more haphazard arrangement with clusters of lipid-laden cells is called the "Antoni B" pattern (23-48). Immunohistochemistry is characterized by strong diffuse positivity for S100 protein.
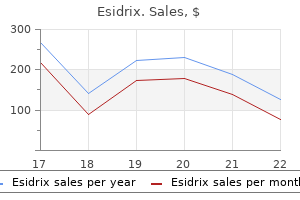
Buy esidrix
Late delayed radiation necrosis is initially expansile and mass-like medications definitions buy genuine esidrix on line, with necrosis largely confined to white matter. Later, volume loss, white matter spongiosis with confluent hyperintensity, and calcifications can be seen (30-46). Mineralizing microangiopathy generally does not appear until at least 2 years following treatment; it is then seen as calcifications in the basal ganglia and subcortical white matter (3048). Approximately 70% are meningiomas, 20% malignant astrocytomas or medulloblastomas, and 10% sarcomas. Meningiomas occur an average of 17-20 years after treatment, whereas gliomas occur at a mean of 9 years. The two most frequent abnormalities are posterior reversible encephalopathy syndrome and treatment-induced leukoencephalopathy. The occipital lobes are frequently spared whereas the cerebellum, brainstem, and basal ganglia are frequently involved. Acute neurotoxicity occurs in 5-18% of children treated for acute lymphoblastic leukemia. Effects of Surgery Interpreting imaging findings in the postoperative brain can be challenging. We focus on just two abnormalities that are important to recognize on imaging studies: retained surgical material ("textiloma") and sinking skin flap syndrome. Textiloma Textiloma-also known as muslinoma or gauzoma-is a foreign body reaction to retained surgical elements. Both resorbable and nonresorbable hemostatic agents may be placed in the surgical bed to provide persistent hemostasis after closure. When they occur, textilomas can be mistaken for recurrent tumor or abscesses on imaging studies. It typically presents weeks to months after craniectomy but most commonly occurs during the second postoperative month. Presenting signs and symptoms vary, but the overwhelming majority of patients exhibit a visibly sunken skin flap. Imaging shows skin flap depression below the level of the calvarium, often with an S-shaped configuration. Mass effect on the cortex, evidenced by sulcal effacement and buckling of the gray-white matter interface under the skin flap, is seen in nearly all cases. Paradoxical deviation of midline structures away from the craniectomy site is typical. Midline shift of the interhemispheric fissure and/or septi pellucidi away from the sunken skin flap is seen in 75% of cases (30-53). Symptoms vary among the various disorders and within the degree of severity in patients with the same disorder. Our focus here will be on disorders most often presenting in the newborn, infant, and child. In utero, the placenta serves the function of an effective dialysis unit, removing toxic metabolites. Therefore, the newborn and young infant with some inherited metabolic disorders may initially appear clinically sound. The specific metabolic disorder will dictate, in large part, the pace of clinical presentation. The expression of this dysfunction may range between sudden neonatal death in the first few weeks of life to gradual deterioration after a symptom-free intmoyaerval of months to years. The neonatal and young infant repertoire of physiologic responses to severe illness is limited. Older affected children and adolescents may exhibit seizures, movement disorders, hypotonia, ataxia, autism, or delayed achievement of developmental milestones. Additional information such as the presence of cysts, calcifications, diffusion restriction, and pathologic enhancement aids in crystallizing the imaging differential diagnosis. We therefore begin this chapter with a review of how normal myelination progresses from birth through 2 years of life. A discussion of classification systems is a recommended and practical approach to analyzing imaging. Selected discussion of the leukodystrophies and nonleukodystrophic white matter disorders focuses on abnormal myelin development, myelin degeneration, and hypomyelination. T1 shortening is related to water molecules within the myelin sheath that are tightly bound to macromolecules and the high myelin content of cholesterol and galactocerebroside. The normal progressive T2 shortening (hypointensity) that occurs in the first 2 years of life is due mainly to decreasing proton density within maturing myelin. In aggregate, during the normal myelin maturational period, the increasingly complex intracellular and extracellular structures that transiently bind water molecules exhibit dynamic T1/T2 relaxivity and diffusivity characteristics that affect T1 and T2 prolongation. During the first 6-8 months of life, T1 shortening occurs earlier and is more conspicuous than T2 shortening. Partially myelinated structures will have high signal on T1 and T2 sequences (T1 and T2 shortening). In the clinical neuroimaging arena, at a minimum, accurate evaluation of myelination status requires both T1 and T2 sequences with orthogonal planes advised. More advanced Normal Myelination and White Matter Development General Considerations Myelination Myelination is an orderly, highly regulated, multistep process that begins during the fifth fetal month and is largely complete by 18-24 postnatal months. The myelin sheath consists of multiple double membranes wrapped radially around axons. Importantly, because white matter abnormalities form a constant part of many if not most inborn metabolic diseases, it is imperative that the radiologist have a firm grasp on normal patterns of myelination. Brain myelination is an event involving more than oligodendrocytes; it is an interaction between oligodendrocytes, axons, astrocytes, and many soluble factors. Normal myelination follows a typical topographical pattern, progressing from inferior to superior, central to peripheral, and posterior to anterior. The lateral cerebral (sylvian) fissures may be slightly prominent but generally resemble those seen in older children. The frontal subarachnoid spaces and basal cisterns often appear prominent up to 1 year of age. The anterior limbs are beginning to myelinate and are not well seen between the hypointensity of the caudate and putamen. Note the normal prominence of the frontal and interhemispheric subarachnoid spaces. Certain diffusion patterns are strongly suggestive of specific inborn errors of metabolism [e. The dentate nuclei of the cerebellum consist of gray matter and thus also appear hypointense. Normal T2 hypointensity is seen at birth within the brainstem cranial nerve nuclei and within the inferior and superior cerebellar peduncles. At birth, the rolandic and perirolandic gyri of the cortex appear quite hypointense. The last normal regions of T2 hypointensity are the orbital region of the frontal lobes and the most anterior temporal lobes. This normal progression of T2 hypointensity may not be complete until 28-30 months. Potential diagnostic pitfall: normal tiny foci of T2 hypointensity may be seen immediately anterior to the frontal horn tips in preterm and term newborns. These represent small aggregates of germinal matrix and typically vanish by 44 postconceptual weeks. Imaging of Normal Myelination Selected major milestones of normal myelination on T1- and T2-weighted images are summarized earlier in the chapter (Table 31-1) and discussed in greater detail here. Although a nonspecific finding, disordered myelination is common among many inborn metabolic errors or inborn errors of metabolism. Compared with the timing of neuronal migration and sulcation, normal myelination lags in the fetus. However, during the early third trimester, the dorsal brainstem myelination is advancing. In the newborn posterior fossa, look for T1 hyperintensity within the brachium of the inferior colliculus and within the inferior and superior cerebellar peduncles.
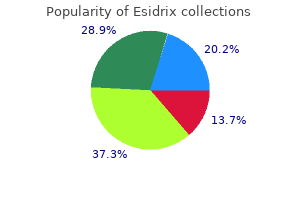
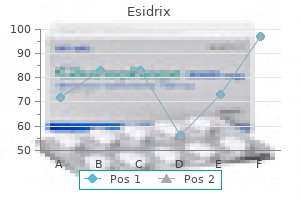
| Comparative prices of Esidrix | ||
| # | Retailer | Average price |
| 1 | Nordstrom | 788 |
| 2 | OSI Restaurant Partners | 643 |
| 3 | DineEquity | 747 |
| 4 | Save Mart | 984 |
| 5 | HSN | 141 |
| 6 | Safeway | 514 |
Order esidrix visa
At least one study suggests that chronic sinusitis is a risk actor or paranasal sinus cancer with a 2 treatment sinus infection purchase esidrix with mastercard. One exception to this is tumors o the maxillary sinus (tumors in erior to Ohngren line). Hutchinson rule: Herpes zoster involvement o the nasal tip is associated with a high incidence o herpes zoster ophthalmicus due to retrograde spread via the nasociliary nerve. Septal deviation, septal hematoma, turbinate hypertrophy, nasal narrowing, nasal valve collapse, tip ptosis, choanal atresia, nasopharyngeal obstruction/mass, trauma ii. In ammatory etiologies include Wegener granulomatosis, sarcoidosis, lupus, and other collagen vascular disease vii. Epithelial tumors derived rom the Rathke cle (embryonal precursor to the adenohypophysis) a. Craniopharyngeal duct is the structure along which the eventual adenohypophysis and in undibulum migrate. Conservative excision Immunosuppression (acquired/iatrogenic) results in an increase in lymphoproli erative disorders and should be kept in mind when evaluating lesions o Waldeyer ring, salivary glands, or cervical nodes. Nodular lesions o tongue, lip, and oral mucosa (oral lesions much more common than in Blastomyces and Coccidioides) 8. Vitamin B2 (ribo avin)-atrophic glossitis, angular cheilitis, gingivostomatitis ii. Vitamin B12-pernicious anemia, tongue with lobulations and possible shiny, smooth, and red appearance iv. Hypopnea in which air ow decreases by 50% or 10 seconds or decreases by 30% i there is an associated decrease in the oxygen saturation or an arousal rom sleep iii. Nasal airways, nasal valve supports, tongue-advancement devices, and bite prostheses to maintain an open bite. Uvulopalatopharyngoplasty-When excising any portion o the so palate, remember that the middle one-third o the palate is the most important rom a unctional standpoint. Papillomas o the oral cavity are most requently seen on the tonsillar pillars and so palate. In those with oral cavity involvement, about hal subsequently develop skin lesions. Subepidermal bullae are present and tend to be smaller than pemphigus and more tense. Develops in the midline as the notochord ascends through the clivus to create the neural plate S. Salivary duct-acinus (surrounded by myoepithelial cells) intercalated duct striated duct excretory duct B. Parotid secretions are watery (due to increased serous cells), low in mucin, and high in enzymes iv. Submandibular and sublingual secretions are thicker due to increased levels o mucin v. Sixty- ve percent o parotid sialoliths are radiolucent and 65% o submandibular sialoliths are radiopaque 3. Eighty percent o tumors occur in parotid and 75% to 80% o these are benign 1090 Pa rt 9: Review 3. Fi een percent o tumors occur in submandibular gland and 50% to 60% o these are malignant 4. Mucosal wave produces a undamental tone accompanied by several nonharmonic overtones. Sound is modi ed by the volume o air ow, movements o the vocal tract, and the degree o vocal cord tension. Lined with ciliated pseudostrati ed columnar (respiratory) epithelium, columnar epithelium, squamous epithelium, or a combination o all three c. Ductal cysts (75%): develop rom an obstructed mucous duct, which subsequently leads to cystic dilation o the mucous gland 2. T yroid cartilage oraminal cysts are extremely rare, herniation o subglottic mucosa through a persistent thyroid ala oramen Gastroesophageal re ux a. Also ound on the tongue, skin, breast, subcutaneous tissues, and respiratory tract c. Bilateral white lesions o en ound at the junction o the anterior one-third and posterior two-thirds o the vocal old c. Unilateral, pedunculated lesion commonly ound between anterior one-third and posterior two-thirds o the vocal old c. Avoid jet ventilation, since this can potentially seed lower respiratory airways x. Most commonly seen in the interarytenoid area and the laryngeal sur ace o the epiglottis. Supraglottic laryngectomy-voice-preserving approach or 1, 2, or 3 (preepiglottic space involvement only) supraglottic lesions without anterior commissure involvement, tongue involvement past the circumvallate papillae, or apical involvement o the pyri orm sinus. Supracricoid laryngectomy-voice-preserving approach or tumors o the anterior glottis. Injection laryngoplasty with e on or autologous collagen/ at, requires injection lateral to vocalis muscle b. Incision o the annular ligaments on one side o the trachea proximal to the anastomosis and on the opposite side distally (1. In the normal individual, lateral pressure over the thyroid cartilage causes an increased voice pitch, whereas anterior pressure causes a decrease. Passy-Muir valve aids in swallowing and helps prevent aspiration by increasing subglottic pressure. Used in pediatric endoscopic procedures, excision o laryngeal papillomata, and endolaryngeal laser procedures. Complications o this technique include hypoventilation, pneumothorax, pneumomediastinum, subcutaneous emphysema, abdominal distention, mucosal dehydration, and distal seeding o malignant cells or papillomavirus particles. Progressive, rapidly spreading, in ammatory in ection located in the deep ascia, with secondary necrosis o the subcutaneous tissues. S pyogenes (group A hemolytic streptococci) and S aureus are the most common inciting bacteria b. Clinical examination reveals rapidly spreading, erythematous skin changes with skin discoloration and subcutaneous emphysema. Carotid paraganglia-located in the adventitia o the posteromedial aspect o the bi urcation o the common carotid artery b. Chie cells (amine precursor and uptake decarboxylase cells) and sustentacular cells (modi ed Schwann cells) organized in clusters known as Zellballen ypes a. Arteriography reveals characteristic splaying o the internal and external carotid arteries (Lyre sign) 6. May present with pulsatile tinnitus, aural ullness, hearing loss, and cranial neuropathies. Examination may show vascular middle ear mass, which exhibits Brown sign (blanching o mass with positive pneumatoscopic pressure). O en present with a painless neck mass with tongue weakness, hoarseness, dysphagia, and a Horner syndrome 5. Radiography reveals vascular lesion that displaces the internal carotid artery anteromedially iii. Ninety percent o primaries eventually ound with repeated examination, biopsies, and scanning iv. Paramedian orehead-supratrochlear artery Cha pter 54: Highlights and Pearls 1099 c.
25mg esidrix overnight delivery
It is associated with pharyngitis medicine 7 years nigeria purchase 12.5 mg esidrix otc, nasopharyngitis, adenotonsillitis, tonsillar abscess, parotitis, cervical abscess, and otitis media. Proposals or etiology include overdistention o the atlantoaxial joint ligaments by e usion, rupture o the transverse ligament, excessive passive rotation during general anesthesia, uncoordinated re ex action o the deep cervical muscles, spasm o the prevertebral muscles, ligamentous relaxation rom decalci cation o the vertebrae, and weak lateral ligaments. Clinical eatures include spontaneous torticollis in a child, a exed and rotated head with limited range o motion, at ace, 16 Pa rt 1: General Otolaryngology and Sudeck sign (displacement o the spine o the axis to the same side as the head is turned). Hallermann-Strei Syndrome Hallermann-Strei syndrome consists o dyscephaly, parrot nose, mandibular hypoplasia, proportionate nanism; hypotrichosis o scalp, brows, and cilia; and bilateral congenital cataracts. Hanhart Syndrome A orm o acial dysmorphia, Hanhart syndrome is characterized by (1) bird-like pro le o ace caused by micrognathia, (2) opisthodontia, (3) peromelia, (4) small growth, (5) normal intelligence, (6) branchial arch de ormity resulting in conductive hearing loss, (7) tongue de ormities and o en a small jaw, and (8) possibly some limb de ects as well. Ear surgery should be care ully considered because o the abnormal course o the acial nerve due to this syndrome. Heer ordt Syndrome or Disease In Heer ordt syndrome, the patient develops uveoparotid ever. Hick Syndrome Hick syndrome is a rare condition characterized by a sensory disorder o the lower extremities, resulting in per orating eet and by ulcers that are associated with progressive dea ness due to atrophy o the cochlear and vestibular ganglia. Hippel-Lindau Disease Hippel-Lindau disease consists o angioma o the cerebellum, usually cystic, associated with angioma o the retina and polycystic kidneys. Homocystinuria Homocystinuria is a recessive hereditary syndrome secondary to a de ect in methionine metabolism with resultant homocystinemia, mental retardation, and sensorineural hearing loss. Horner Syndrome The presenting symptoms o Horner syndrome are ptosis, miosis, anhidrosis, and enophthalmos due to paralysis o the cervical sympathetic nerves. Cha pter 1: Syndromes and Eponyms 17 Horton Neuralgia Patients have unilateral headaches centered behind or close to the eye accompanied or preceded by ipsilateral nasal congestion, su usion o the eye, increased lacrimation and acial redness, and swelling. Cerebellar tumor, an intention tremor that begins in one extremity gradually increasing in intensity and subsequently involving other parts o the body B. Facial paralysis, otalgia, and aural herpes due to disease o both motor and sensory bers o the seventh nerve C. A orm o juvenile paralysis agitans associated with primary atrophy o the pallidal system Hunter Syndrome A hereditary and sex-linked disorder, this incurable syndrome involves multiple organ systems through mucopolysaccharide in ltration. Death, usually by the second decade o li e, is o en caused by an in ltrative cardiomyopathy and valvular disease leading to heart ailure. Chondroitin sul ate B and heparitin in urine, mental retardation, beta-galactoside de ciency, and hepatosplenomegaly are also eatures o this syndrome. Abdominal abnormalities, respiratory in ections, and cardiovascular troubles plague the patient. Immotile Cilia Syndrome this syndrome appears to be a congenital de ect in the ultrastructure o cilia that renders them incapable o movement. The clinical picture includes bronchiectasis, sinusitis, male sterility, situs inversus, and otitis media. Histologically, there is a complete or partial absence o dynein arms, which are believed to be essential or cilia movement and sperm tail movement. Also no cilia movements were observed in the mucosa o the middle ear and the nasopharynx. Inversed Jaw-Winking Syndrome When there are supranuclear lesions o the h nerve, touching the cornea may produce a brisk movement o the mandible to the opposite side. There is ipsilateral accid paralysis o the so palate, pharynx, and larynx with weakness and atrophy o the sternocleidomastoid and trapezius muscles and muscles o the tongue. Jacod Syndrome Jacod syndrome consists o total ophthalmoplegia, optic tract lesions with unilateral amaurosis, and trigeminal neuralgia. It is caused by a middle cranial ossa tumor involving the second through sixth cranial nerves. The clinical picture includes air skin, red hair, recurrent staphylococcal skin abscesses with concurrent other bacterial in ections and skin lesions, as well as chronic purulent pulmonary in ections and in ected eczematoid skin lesions. This syndrome obtained its name rom the Biblical passage re erring to Job being smitten with boils. This syndrome is most o en caused by lymphadenopathy o the nodes o Krause in the oramen. T rombophlebitis, tumors o the jugular bulb, and basal skull racture can cause the syndrome. The glomus jugulare usually gives a hazy margin o involvement, whereas neurinoma gives a smooth, sclerotic margin o enlargement. The jugular oramen is bound medially by the occipital bone and laterally by the temporal bone. The oramen is divided into anteromedial (pars nervosa) and posterolateral (pars vascularis) areas by a brous or bony septum. The posterior compartment transmits the internal jugular vein and the posterior meningeal artery. Kallmann Syndrome Kallmann syndrome consists o congenital hypogonadotropic eunuchoidism with anosmia. Kaposi Sarcoma Patients have multiple idiopathic, hemorrhagic sarcomatosis particularly o the skin and viscera. Kartagener Syndrome The symptoms are complete situs inversus associated with chronic sinusitis and bronchiectasis. I these people live to 65 years o age, 50% to 75% o them develop carcinoma o the esophagus. Kimura Disease Kimura disease was rst described by Kimura et al in 1949 as a chronic in ammatory condition occurring in subcutaneous tissues, salivary glands, and lymph nodes. Histologically, there is dense brosis, lymphoid in ltration, vascular proli eration, and eosinophils. Kline elter Syndrome Kline elter syndrome is a sex chromosome de ect characterized by eunuchoidism, azoospermia, gynecomastia, mental de ciency, small testes with atrophy, and hyalinization o semini erous tubules. Klinkert Syndrome Paralysis o the recurrent and phrenic nerves due to a neoplastic process in the root o the neck or upper mediastinum is evidenced. Lacrimoauriculodentodigital Syndrome Autosomal dominant, occasional middle ear ossicular anomaly with cup-shaped ears, abnormal or absent thumbs, skeletal orearm de ormities, sensorineural hearing loss, and nasolacrimal duct obstruction are the characteristics o lacrimoauriculodentodigital syndrome. Large Vestibular Aqueduct Syndrome The large vestibular aqueduct as an isolated anomaly o the temporal bone is associated with sensorineural hearing loss. A vestibular aqueduct is considered enlarged i its anteroposterior diameter on computed tomography (C) scan is greater than 1. Larsen Syndrome Larsen syndrome is characterized by widely spaced eyes, prominent orehead, at nasal bridge, midline cle o the secondary palate, bilateral dislocation o the knees and elbows, de ormities o the hands and eet, and spatula-type thumbs; sometimes tracheomalacia, stridor, laryngomalacia, and respiratory di culty are present. Usually in young adults rst presenting with oropharynx in ection, progress to neck and parapharyngeal abscess, leading to internal jugular and sigmoid sinus thrombosis leading to septic embolism causing septic arthritis, liver and splenic abscess, sigmoid sinus thrombosis ndings include headache, otalgia, vertigo, vomiting, otorrhea and rigors, proptosis retrobulbar pain, papilledema, and ophthalmoplegia. It was rst described by Lermoyez in 1921 as dea ness and tinnitus ollowed by a vertiginous attack that relieved the tinnitus and improved the hearing. High-dose local radiation totaling 5000 rad is the treatment o choice or localized cases. Chemotherapy involving an alkylating agent (cyclophosphamide) is recommended or disseminated cases. A triad o symptoms is present that improves temporarily with middle ear in ation: auditory acuity, distortion o sound, and speech discrimination. Louis-Bar Syndrome this autosomal recessive disease presents as ataxia, oculocutaneous telangiectasia, and sinopulmonary in ection. It involves progressive truncal ataxia, slurred speech, xation nystagmus, mental de ciency, cerebellar atrophy, de cient immunoglobulin, and marked requency o lymphoreticular malignancies. Ma ucci Syndrome Ma ucci syndrome is characterized by multiple cutaneous hemangiomas with dyschondroplasia and o en enchondroma. The dyschondroplasia may cause sharp bowing or an uneven growth o the extremities as well as give rise to requent ractures. Five to 10% o Ma ucci syndrome patients have head and neck involvement giving rise to cranial nerve dys unction and hemangiomas in the head and neck area. The hemangiomas in the nasopharynx and larynx could cause airway compromise as well as Cha pter 1: Syndromes and Eponyms 21 deglutition problems. Fi een to 20% o these patients later undergo sarcomatous degeneration in one or more o the enchondromas.
Buy discount esidrix on line
Melanocytomas are solitary symptoms viral infection best esidrix 25mg, darkly pigmented, low-grade tumors that do not invade adjacent brain. Preferred sites are the posterior fossa (skull base, cerebellopontine angle), temporal lobe, Meckel cave (with nevus of Ota), and spinal cord/nerve roots. Prognosis is variable for melanocytic tumors of intermediate differentiation and poor for melanoma. The major differential diagnosis for primary melanocytic lesions of the brain is metastatic malignant melanoma. Diffuse melanocytic lesions appear as dense, thick, black confluent aggregates that fill the subarachnoid spaces and coat the pia. They are generally considered benign but can grow rapidly and be locally aggressive with intracranial extension, mimicking solitary fibrous tumor/hemangiopericytoma or sarcoma (2250). Another focus of melanotic deposition with T1 shortening is seen along the midbrain. Hemangiomas vary in size from tiny to large, especially when associated with a cyst. The common appearance is that of a beefy red, vascular-appearing nodule that abuts a pial surface (2252). It is the second most common infratentorial parenchymal mass in adults (after metastasis). Imaging progression alone is not an indication for treatment although tumor/cyst growth rates can be used to predict symptom formation and future need for treatment. A nonneoplastic peritumoral cyst with solid nodule is the most common pattern, seen in 50-65% of cases. The most common appearance is a welldelineated iso- to slightly hyperdense nodule associated with a hypodense cyst. Tumors of the Meninges Intense enhancement of the nodule-but not the cyst itself-is typical (22-53D). Cyst wall enhancement should raise the possibility of tumor involvement, as compressed, nonneoplastic brain does not enhance. The most common appearance is that of an intensely vascular tumor nodule that shows a prolonged vascular "blush" (22-55). If a tumor-associated cyst is present, vessels appear displaced and "draped" around an avascular mass. Note vascular tumor mass supplied primarily by enlarged branches of the anterior and posterior inferior cerebellar arteries. Lyon, France: International Agency for Research on Cancer, 2016, pp 232-245 Yuzawa S et al: Genetic landscape of meningioma. Lyon, France: International Agency for Research on Cancer, 2016, pp 248-254 Reinshagen C et al: Intracranial dural based chondroma. The four basic categories of schwannoma, neurofibroma, perineurioma, and malignant peripheral nerve sheath tumor were retained. A new category, hybrid nerve sheath tumor, was added, as such histologically combined tumors are increasingly recognized by neuropathologists. Because melanotic schwannoma is both clinically and genetically distinct from "conventional" schwannoma, it is also now classified as a distinct entity rather than a variant. With the exception of vestibular schwannoma, all intracranial nerve sheath tumors are rare. They occur ether sporadically or as part of tumor-associated familial tumor syndromes such as neurofibromatosis types 1 and 2. The two major tumor types that are found intracranially and at or near the skull base are schwannomas and neurofibromas. The third type of benign tumor, perineurioma, is primarily a tumor of peripheral nerves and soft tissues, although rare cases involving cranial nerves have been reported. More than 99% of intracranial nerve sheath tumors are associated with a cranial nerve. Because characteristic imaging findings of these tumors are location specific rather than generic, we begin this chapter with a review of normal cranial nerve anatomy. The function, anatomy, and key clinical/imaging points are delineated for the individual cranial nerves. When imaging cranial neuropathies, it is critically important to image-and Neoplasms, Cysts, and Tumor-Like Lesions 696 carefully evaluate-each segment, following the affected nerve all the way from its origin to its "functional endplate. The olfactory nerve is a special visceral afferent involved with the sense of smell. Unmyelinated fibers from bipolar receptor cells high in the nasal vault gather into fascicles, pierce the cribriform plate of the ethmoid bone, and then synapse in the olfactory bulb (23-1) (23-5). Olfactory stria from the trigone pass into the brain with the largest tract, the lateral olfactory stria, terminating in the temporal lobe. Cranial Nerves and Nerve Sheath Tumors astrocytomas, not schwannomas, and were discussed in Chapter 17. The visual pathway consists of the globe/retina, optic nerve, optic chiasm, and retrochiasmal structures. It is covered by the same three meningeal layers as the brain (dura, arachnoid, pia) (23-9). The intracanalicular segment of the optic nerve passes through the optic canal (23-5) (23-8). The intracranial (cisternal) segment extends from the optic canal to the optic chiasm. The optic chiasm is an X-shaped structure that lies in the upper suprasellar cistern. Nerve fibers from the medial half of both retinas cross here, running posterolaterally to the opposite side (23-11) (23-12). The optic tracts are posterior extensions of the optic chiasm that curve around the cerebral peduncles. The optic radiations fan out as they pass posteriorly to terminate in the calcarine cortex (primary visual cortex) along the medial occipital lobes. Intrinsic or extrinsic lesions of the optic chiasm cause bitemporal heteronymous hemianopsia, i. A left-sided lesion causes right homonymous hemianopsia, whereas a right-sided lesion causes left homonymous hemianopsia. The section is through the most cephalad aspect of the superior orbital fissures, which are barely visible. On imaging studies with moderate to severe papilledema, the posterior sclerae become flattened, and the optic nerve head may appear elevated. It innervates all the extraocular muscles except the lateral rectus and superior oblique muscles. Its parasympathetic fibers control pupillary sphincter function and accommodation. The two extraocular muscles just under the orbital roof are the levator palpebrae and superior rectus. Cranial Nerves and Nerve Sheath Tumors the cisternal segment courses anteriorly toward the cavernous sinus, passing between the posterior cerebral and superior cerebellar arteries. The oculomotor nerve exits the cavernous sinus through the superior orbital fissure (23-5). Its extracranial segment passes through the tendinous annulus and then divides into superior and inferior branches. Preganglionic parasympathetic fibers follow the inferior branch to the ciliary ganglion. Pupil-sparing third nerve palsy is commonly caused by microvascular infarction of the core of the nerve with relative sparing of its peripheral fibers. The trochlear nerve is a pure motor nerve that innervates the superior oblique muscle. Its intraaxial segment is also in the midbrain, anterior to the periaqueductal gray matter lying just below the oculomotor nerve nuclei. Its fascicles then course posteroinferiorly around the cerebral aqueduct and decussate within the superior medullary velum. The trochlear nerve exits the dorsal midbrain just below the inferior colliculi (23-14).
Discount 12.5 mg esidrix free shipping
Lesions in Susac syndrome preferentially involve the middle of the corpus callosum medications 1800 purchase esidrix 12.5 mg with mastercard, not the callososeptal interface. Rim enhancement-often the incomplete or "open ring" pattern-is seen during the acute inflammatory stage. Signs of increased intracranial pressure, aphasia, and behavioral symptoms are typical. Large plaques with alternating rims of demyelination and myelin preservation give the lesion its characteristic appearance (15-23). The F:M ratio is approximately 2:1 and is most common in patients of east Asian origin. Infection, Inflammation, and Demyelinating Diseases 464 demyelinating layers enhance on T1 C+ sequences (15-24A). White matter lesions usually predominate, but basal ganglia Demyelinating and Inflammatory Diseases involvement is seen in nearly half of all cases. Viral and streptococcal infections have been implicated and cause enlarged hyperintense basal ganglia, caudate nuclei, and internal/external capsules. Large "tumefactive" lesions cause a gray-pink white matter discoloration and often extend all the way to the cortex-white matter junction (15-25). However, the disease sometimes follows an atypical course, waxing and waning over a period of several months. More than half of all patients recover completely within 1 or 2 months after onset, whereas approximately 20% experience some residual functional impairment. Biopsy disclosed acute demyelinating disease without evidence of neoplasm or infection. The typical gross appearance is that of marked brain swelling with diffuse confluent and/or petechial hemorrhages (15-31A). Hemorrhages are typically present in the leptomeninges, cerebral hemispheres (predominately the white matter), and cerebellum. The large arteries are normal without evidence for aneurysm or subarachnoid bleeding. History of a viral prodrome or flu-like illness is common but not invariably present. Cross reactivity between myelin basic protein moieties and various infectious agent antigens probably causes an acute autoimmune-mediated demyelination. Fever and lethargy with increasing somnolence, decreased mental status, impaired consciousness, and longtract signs are the most common clinical symptoms. Rapid clinical deterioration and death usually occur within days to a week Pathology Location. Basal ganglia involvement is common, but the cortical gray matter is generally (but not invariably) spared. Aggressive treatment with intravenous high-dose corticosteroids, immunoglobulin, cyclophosphamide, and plasmapheresis has been used with some success in a few cases. Multifocal scattered or confluent hyperintensities as well as bilateral confluent hyperintensity of the cerebral white matter are typical but nonspecific findings (15-32). Although large lobar confluent hemorrhages are easily identified on most standard sequences (15-33) (15-34), T2* scans are the key to diagnosis. Multifocal punctate and linear "blooming" hypointensities in the corpus callosum that extend through the full thickness of the hemispheric white matter to the subcortical U-fibers are typical findings on T2*. Additional lesions are frequently present in the basal ganglia, midbrain, pons, and cerebellum. Petechial microhemorrhages are generally invisible, but white matter edema with diffuse, relatively asymmetric hypodensity in one or both hemispheres may be present. Demyelinating and Inflammatory Diseases 471 (15-33) Autopsy case shows two areas of gross hemorrhagic necrosis. Infection, Inflammation, and Demyelinating Diseases 472 Autoimmune Encephalitis the autoimmune encephalitides are an important, newly recognized disease "family" with a spectrum of related disorders that share overlapping clinical features and imaging findings. Most-but not all-are characterized by limbic dysfunction and varying involvement of the temporal lobes and neocortex. The autoimmune encephalitides are differentiated by specific antibody subtypes and can be paraneoplastic or nonparaneoplastic. Paraneoplastic-associated disorders such as anti-Hu and anti-Ma encephalitis are discussed in Chapter 27. Autoimmune Encephalitis In addition to paraneoplastic and non-tumor-associated disorders, the autoimmune encephalitides are further subdivided according to the cellular location of their neuronal antigens. Demyelinating and Inflammatory Diseases Etiology the major antigens responsible for inciting autoimmune encephalitis are an ever-expanding group of antibodies that is shown in the box below. Pathology Regardless of the etiology and antibody profile, the autoimmune encephalitides have a distinct predilection for the limbic system. Clinical Issues Antigenic specificities appear to determine the associated clinical syndromes. The most common presentation is subacute cognitive dysfunction and altered mental status. Less common presentations include stiff leg or stiff person syndromes and cerebellar ataxia. Extralimbic involvement with structures such as the cortex, striatum, and diencephalon varies. Infection, Inflammation, and Demyelinating Diseases 474 (15-37A) T1 C+ in a patient with ataxia, limb weakness, and ophthalmoplegia demonstrates that both oculomotor nerves enhance. Enhancement on T1 C+ occurs in approximately 25% of cases (15-36) and is frequently associated with subsequent development of mesial temporal sclerosis. A subset of patients will have no neuroimaging findings despite severe neuropsychiatric dysfunction. The revised criteria (see below) allow other symptoms such as postrema syndrome (intractable hiccups or nausea and vomiting) and brainstem syndromes (double vision or ataxia) to be included. Clinical features vary with subtype, but progressive limb weakness and diplopia are Demyelinating and Inflammatory Diseases 475 (15-38A) Luxol fast blue stain of a section through the optic chiasm shows classic demyelinating foci characteristic of neuromyelitis optica. The cervical cord is most commonly affected, and lesions typically extend over three or more consecutive segments. Brain lesions are not uncommon and tend to cluster around the third and fourth ventricles and the dorsal midbrain/aqueduct of Sylvius. Infection, Inflammation, and Demyelinating Diseases 478 (15-42) Funduscopic examination demonstrates multiple retinal artery branch occlusions and irregularities. Waxing and waning changes in mental status with memory impairment, confusion, and behavioral and psychiatric disturbances are common, often dominant features. Hearing loss is typically low to medium frequency and can be uni- or bilateral, symmetric or asymmetric. Inflamed retinal arterioles with branch retinal artery occlusions are typically present at fluorescein angiography. Some patients have a relapsing-remitting course, whereas others experience permanent neurologic deficits (most commonly deafness and impaired vision). The infarcts can be acute or subacute and involve either the cortex or white matter or both. Demyelinating and Inflammatory Diseases globulin or cyclophosphamide in refractory cases have produced a good response in many patients. Almost 80% show corpus callosal involvement with lesions that typically involve the middle of the corpus callosum and spare the undersurface (15-45). Basal ganglia lesions occur in 70% of cases and brainstem lesions in nearly one-third (15-44). Imaging findings plus clinical history are virtually diagnostic of Susac syndrome. There are also confluent deep white matter lesions of lesser hyperintensity in both parietal lobes. Lateral ventricle is rather enlarged compared to the comparable scan from 18 months prior. Patients typically present with subacute brainstem symptoms such as gait ataxia, diplopia, facial paresthesias, and nystagmus. Infection, Inflammation, and Demyelinating Diseases 482 (15-47) Graphic illustrates common neurosarcoid locations: (1) infundibulum, extending into the pituitary, (2) plaque-like dura-arachnoid thickening, and (3) synchronous lesions of the superior vermis and fourth ventricle choroid plexus.
Cheap esidrix 12.5 mg without a prescription
Fast image acquisition during contrast administration can often discriminate between the slowly enhancing microadenoma and rapidly enhancing normal gland administering medications 6th edition esidrix 12.5mg low price. Differential Diagnosis the differential diagnosis of pituitary adenoma varies with size and patient demographics. The major differential diagnosis of pituitary macroadenoma is pituitary hyperplasia. The height of the gland is usually at least 10 Sellar Neoplasms and Tumor-Like Lesions mm unless the patient is pregnant or lactating. Less commonly, end-organ failure (such as hypothyroidism) results in compensatory pituitary enlargement. As adenomas are very rare in children, if a prepubescent female patient or young male patient has an "adenoma-looking" pituitary gland, endocrine work-up is mandatory! Tumors that can resemble pituitary adenoma include meningioma, metastasis, and craniopharyngioma. Meningioma of the diaphragma sellae can usually be identified as clearly separate from the pituitary gland below. Metastasis to the stalk and/or pituitary gland from an extracranial primary neoplasm is uncommon. Most pituitary metastases are secondary to spread from adjacent bone or the cavernous sinus, generally occurring as a late manifestation of known systemic tumor. Craniopharyngioma is the most common suprasellar tumor of childhood, whereas pituitary adenomas in children are rare. Craniopharyngiomas in middle-aged adults are typically solid papillary tumors that do not calcify as the adamantinomatous ones do. Often in adults with craniopharyngioma, the pituitary gland can be identified as anatomically separate from the mass. Because of this rarity, even the most aggressive-looking pituitary tumors are statistically far more likely to be adenomas than carcinomas. Nonneoplastic entities that can mimic macroadenoma include aneurysm and hypophysitis. An aneurysm arises eccentrically from the circle of Willis and is usually not in the midline directly above the sella. Hypophysitis is much less common than macroadenoma but can appear virtually identical to an adenoma on imaging studies. Lymphocytic hypophysitis-the most common type-typically occurs in peripartum or postpartum female patients or as an autoimmune hypophysitis in patients treated with immunomodulating therapies. Pituitary microadenoma may be difficult to distinguish from incidental nonneoplastic intrapituitary cysts such as Rathke cleft cyst or pars intermedia cyst. Microadenomas enhance; cysts are seen as nonenhancing foci within the intensely enhancing pituitary gland. Conventional histologic criteria for malignancy (necrosis, nuclear atypia, pleomorphism, mitotic activity) are insufficient for diagnosis. Only documentation of craniospinal metastases or systemic tumor spread can confirm the diagnosis. Pituitary Blastoma Pituitary blastoma is a recently described pituitary tumor in neonates and infants characterized by large glandular structures that resemble Rathke epithelium and adenohypophysial cells. Arrested pituitary development and unchecked proliferation are the likely etiology of this unusual tumor. Histology shows small undifferentiated blastema-like cells interspersed with large pituitary secretory cells. Imaging findings are nonspecific and Neoplasms, Cysts, and Tumor-Like Lesions 796 (25-50A) Coronal graphic depicts a pituitary microadenoma. Incidental asymptomatic microadenomas are common on imaging studies and at autopsy. The mass enhances more slowly than normal gland and appears relatively hypointense. Sellar Neoplasms and Tumor-Like Lesions 797 (25-54) Sagittal T1 C+ image shows a large, heterogeneous invasive pituitary macroadenoma. The T2 low signal, stalk involvement, and infiltrative appearance help differentiate this lymphoma from the more common adenoma. Considerations in this young patient include germinoma and Langerhans cell histiocytosis. Neoplasms, Cysts, and Tumor-Like Lesions 798 (25-58) Sagittal graphic shows a predominantly cystic, partially solid suprasellar mass with focal rim calcifications. The few described cases show a heterogeneously enhancing sellar/suprasellar mass, often invading the cavernous sinus. Germinomas are tumors of young patients with the vast majority presenting in patients in the first two decades. Germinomas of the suprasellar region most commonly present with diabetes insipidus. Less common presenting signs include visual loss and hypothalamic-pituitary dysfunction with decreased growth and precocious puberty. When involving the pituitary axis, a germinoma involves the infundibulum and/or neurohypophysis and often presents in a child with an absent posterior pituitary "bright spot" (25-57). Germinoma A germinoma is the most common intracranial germ cell tumor, representing two-thirds of intracranial germ cell tumors and 1-2% of all primary brain tumors. Germinomas are located in the pineal region most commonly (50-65%) and the suprasellar region in approximately 25-35% of cases. Posteroinferior extension between the clivus and pons down to the foramen magnum can be seen in exceptionally large lesions. The cysts often contain dark, viscous, "machinery oil" fluid rich in cholesterol crystals (25-58). Neoplasms, Cysts, and Tumor-Like Lesions 800 (25-61) Axial autopsy specimen shows a mostly cystic craniopharyngioma in the suprasellar cistern. When a multicystic, bizarre-appearing mass in a child extends into several fossae, craniopharyngioma should be a consideration. Patients most commonly present with visual disturbances, either with or without accompanying headache. Large tumors compress the infundibular stalk ("stalk effect") resulting in abnormal pituitary function (often with mild elevation of prolactin). Endocrine deficiencies including growth failure, delayed puberty, and diabetes insipidus are common. However, the recurrence rate at 10 years approaches 20-30% even in patients with gross total resection. Recurrence is significantly more common with larger and incompletely excised lesions. Approximately half of long-term survivors experience reduced quality of life, mostly due to morbid hypothalamic obesity. A partially calcified, mixed solid and cystic extraaxial suprasellar mass in a child is the classic appearance. A compressed, displaced pituitary gland can sometimes be identified as separate from the mass. Hyperintensity extending along the optic tracts is common and usually represents edema, not tumor invasion (25-66) (25-67A). The cyst walls and solid nodules typically enhance following contrast administration (25-62) (25-67). Hypothalamic/chiasmatic astrocytoma is usually a solid suprasellar mass that is clearly intraparenchymal. Pituicytoma Previously also known as "choristoma" and "infundibuloma," pituicytoma arises from modified glial cells ("pituicytes") that reside in the infundibular stalk and neurohypophysis (25-68). Visual disturbance with or without headache is the most common presenting symptom. Patients with pituicytoma almost never present with diabetes insipidus, galactorrhea, or prolactinemia. They usually arise along the infundibulum or neurohypophysis and enhance homogeneously following contrast enhancement (25-69).