Generic glimepiride 4 mg on-line
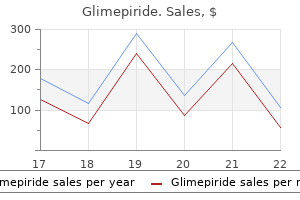
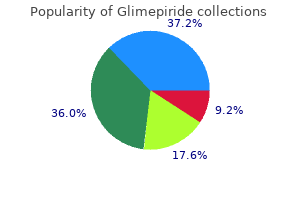
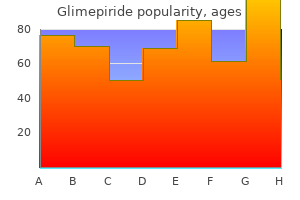
In some cultures (eg in Japan) diabetes type 2 ed buy glimepiride 1mg with amex, chief responsibility for perioperative care lies with the surgeon. It is experi- Patient factors: enced by ~25% of patients (up to 80% if high Female (3 risk) risk). Anaesthesia Ensure that the anaesthetized area is positioned and protected sufficiently both intra- and postoperatively to avoid injury. Extradural (epidural) anaesthesia58 this is anaesthetic into the extradural space. If there has been inadvertent intrathecal placement this will result in spinal anaesthesia. If injecting is difficult (there should be no resistance), or swelling occurs, the needle is in the wrong place-so stop! However, in day-case surgery, neuraxial techniques may be associated with a prolonged stay. Relative contraindications to all neuraxial anaesthesia: Neurological disease-procedure may be blamed for change in state. Pain relief also aids physiotherapy (allowing coughing and mobility), preventing pneumonia. Chronic pain Some anaethesists dedicate significant amounts of their workload to the management of chronic pain, it is an extremely important topic which is only briefly touched upon here. Treatment may be broadly categorized into three categories-pharmacological, physical, and psychological. However, organ retrieval is never straightforward, and so the Maastricht criteria exist for the categorization of non-heart-beating organ donors: 1 Dead on arrival at hospital; 2 Unsuccessful resuscitation; 3 Awaiting cardiac arrest (eg after withdrawal of treatment); 4 Cardiac arrest after confirmation of brainstem death. But they lack signs of awareness-there is no evidence they can perceive the environment or their own body. However, the problem is that these tests not only have to be 100% specific (an impossibility) but they also need to be able to predict return of cognitive function, and not just its presence. To make matters even more complicated, pharmacological and metabolic changes can also interfere with the accuracy of such tests. One review has quoted that with the absence of somatosensory evoked potentials in patients with hypoxic ischaemic encephalopathy, the chances of waking are less than 1%. Management While waiting for any recovery, aim to provide vigorous nursing care to maintain nutrition, and to prevent pressure sores, and tracheostomy and muscle contracture complications. Once it is agreed that there will be no recovery (the difficult issue), discussions on withdrawing active treatment and nutrition raise big ethical questions-which are only partly mitigated if the patient has an advance directive (an unlikely event). Ethicists, medical specialists, nurses, physiotherapists, judges, and the family must all be allowed to have their say. When the Buddha was ailing, he was at first mispronounced dead by Ananda, his attendant for 25 years. What better way to achieve immortality and recognition than have your name live on-even if no one remembers anything about you other than what you discovered. Whilst the golden age of eponyms may be behind us, we hope those that remain-like the spiral-will carry on forever. Features: Visual loss, seizures, loss of motor and cognitive function and early death. Medical eponyms are pickled in something almost as intoxicating: the hidden recesses of our own minds. But as the years go by we may wonder more and more about the people behind the eponyms. We might read about these quacks and geniuses-yet it is always rather unsatisfying. Capgras syndrome A delusional misidentification where the patient believes a person has been replaced by an exact clone, who is an impostor. Men with Capgras syndrome get very destabilized by not knowing who they are talking to-the genuine, or the fake wife. Distal girdle muscles are affected late; selective wasting causes calf pseudohypertrophy. Cyanosis, dyspnoea, faints, clubbing, thrills, harsh systolic murmur at left sternal base. Look for piezogenic papules (easily compressible outpouchings of fat through defects in the dermis on the sides of the feet). It occurs Hepatosplenomegaly in children and adults, eg starting with a polyp Lymphadenopathy at the external auditory meatus. Early findings: auditory & visual reaction times, then mild chorea (flitting, jerky movements), odd extraocular movements, reflexes, rapid alternating movements. Clearance of mucus & bacteria is poor, hence chronic sinusitis and bronchiectasis. Incomplete forms exist, so get expert help today while wrestling with this difficult, important diagnosis. Once the repeat exceeds a threshold length (>200), no fragile X protein is made, and disease results. Type B: Traditionally non-neuronopathic, milder, with later onset and variable severity (often detected by hepatosplenomegaly or lung symptoms). Othello syndrome (delusional jealousy) A lover has a fixed belief that their partner is being sexually unfaithful. Associations: Alcohol, schizophrenia, depression, frontal lobe dysfunction, dementia. Signs: Before cognitive loss, look for: personality change, social disinhibition, emotional blunting, impaired insight, dietary changes, perseverative behaviours (eg drinking from an empty cup).
Glimepiride 4mg
Actually diabetes prevention program colorado discount 4 mg glimepiride with visa, the time of circulatory arrest is shorter for most patients with the step-up method because the charge times are much shorter with lower energy, but longer for the few patients with high energy requirements. A third method of estimating defibrillation efficacy has been validated, in which test shocks are delivered to the vulnerable period of the cardiac cycle, near the peak of the surface T wave. Other parameters include lead/body impedance, waveform tilt, truncation, pulse duration, and positive and negative-phase peak voltage; these can all affect defibrillation success and are usually device- or lead-specific. For example, a waveform whose amplitude is reduced to half the initial value has a 50% tilt. In the examples given, curves A and B represent waveforms A and B with different defibrillation efficacy. This waveform consists of the capacitor discharge divided into two phases of opposite polarity. The first phase is identical to a monophasic waveform (although usually of a shorter duration) before the capacitor discharge is truncated. The basic physiology of defibrillation and its relationship to best or optimized biphasic waveform is well studied. Biphasic waveform characteristics in animals identified two factors that appear to maximize defibrillation efficacy as follows: (1) the first phase should be longer than the second phase; and (2) the polarity of the first phase appears to be important only at phase 1 durations greater than 10 ms or when the second phase duration is greater than the first phase. Additional studies have examined the effectiveness of other phase characteristics. The biphasic waveform currently used in all current implantable defibrillators is composed of a capacitor discharge divided into two phases of oppositepolarity. Summary of biphasic Waveform Characteristics in Currently Available Commercial Implantable Cardioverter Defibrillators Manufacturer boston Scientific, St. In models in which phase parameters are programmable, the value given is the default value programmed in the factory. When a range of values is given, it refers to different models offered by the same manufacturer. Applies only to the atrial shock tilt, the ventricular shocks are not tilt programmable. Multiple recent studies have reported improved defibrillation thresholds with modification of the tilt percentages. The results of these studies were then used to modify the preset tilts in the current available devices. Some devices also have the capacity to specify the duration of the first and second phase of the biphasic shock, which determines the tilt. Although this specificity can make a difference in a few patients, in general it is not required. System integrity is challenged by several factors, including high temperature, high osmolarity, high salt environment, and continuous mechanical stress from the beating heart and body movement. Despite these challenges, the "failure prediction" is small-less than 1% over 5 years. System failure could occur in the device battery, device electronics, or lead design and interact with the implantation techniques and patient characteristics. More often, battery depletion is caused by excessive power drain from pacing, capacitor charge, and electrogram storage. High pacing thresholds and lead insulation failure are additional causes of excessive current drain. On the other hand, repetitive capacitor charges owing to nonsustained ventricular tachycardia or temporary ventricular oversensing can cause important reductions in battery longevity. Usually these high-current drain issues can be managed with increased frequency of battery assessments. Patientrelated factors include thoracic inlet syndrome, Twiddler syndrome, and certain activities like bench pressing. Operator methods that have contributed to lead failure include subclavian or second rib approach, venous access, poorly applied suture sleeves, excessively tight lead coiling within the pocket, overtorquing of the lead, and iatrogenic damage to the leads during implantation. Lead-related factors that can contribute to lead failure include lead engineering and suture design flaws. There was also evidence of increased risk of high-voltage conductor fracture if a pace-sense conductor fracture has previously occurred; therefore, it is recommended to implant a new high-voltage lead instead of a pace/sense lead if a lead fracture of any type has occurred. Use of a lead integrity algorithm is recommended: extending arrhythmia detection, activating audible alarms, and using quick alert notification to monitor fully functional leads. A lead integrity algorithm could provide most patients with a 3-day warning before inappropriate shocks. The latter often occur close to the pocket and are often the result of lead contact with another part of the lead or the pulse generator. Although inside-out externalizations of the inner cables are not uncommon and can be visualized easily using fluoroscopy, they do not seem to place patients at significant risk of electrical dysfunction. However, outside-in abrasions are difficult to be identified using fluoroscopy and can result in shorting of the high voltage; this is not unique to the Riata lead family, nor is it a new failure mechanism. Additional studies are needed to evaluate whether monitoring will result in improvements in outcomes or reduction in heath care expendature. This bandwidth does not need any licensing and is shared by different manufacturers (currently Medtronic, St. Each manufacturer has applied mechanisms to avoid interference and cross communication with other devices. There is another frequency spectrum in use for long-range telemetry by Boston Scientific (St. InvestigationalShockWaveform Multiple triphasic waveform patterns were tested in animals and failed to improve shock efficacy in terminating ventricular fibrillation over biphasic waves. Cardiac signal sensing is automatically selected from the three available sensing vectors (distal-proximal electrodes, distal electrode-can, and proximal electrode-can) based on the analysis of the signal amplitude and signal-to-noise ratio. Extraction of this system should also be safer because of the subcutaneous location of the lead. It is not indicated in patients who require bradycardia therapy or biventricular pacing. In addition, its role could be limited in patients who require frequent therapies for ventricular tachycardias that are amenable to antitachycardia pacing. The undesirable interactions seen with the reed switch were avoided by replacing it with a Hall sensor. Finally, the lead design was modified to decrease polarization, improve evoked response sensing, and improve heat dispersion, thus preventing lead tip heating. Variation of intrathoracic impedance, measured by the subthreshold electrical impulse between the can and the right ventricular coil with or without a left ventricle lead, correlates with changes in pulmonary fluid accumulation. Because fluid is a good conductor, decompensated heart failure often leads to a decrease in intrathoracic impedance. However, decreases in impedance are also seen in other clinical scenarios, such as pleural or pericardiac effusion, pneumonia, and increased intraabdominal pressure, shortly after device implantation. Studies are currently underway to evaluate the effects on heart failure mortality and hospitalization. The hope is to prevent acute heart failure decompensation with pulmonary edema or complications related to overtreatment. This limited study showed low sensitivity and specificity in detecting coronary events. Because of the increased risk of infection with device changes, there has been significant work to produce batteries with longer longevity including biothermal batteries. If proven effective, these batteries can extend the life of the device by more than 15 to 20 years. Janardhan A, Li W, Gutbrod S, et al: Low-energy three-stage electrotherapy delivered through implantable leads significantly reduces the cardioversion threshold in a canine model of persistent atrial fibrillation. Davis R, Malkin R: Simultaneous comparison of many triphasic defibrillation waveforms. This combination of dynamic adjustment of sensitivity and short blanking periods may cause oversensing, so marker channels should be inspected in both sinus and paced rhythms for oversensing P, R, and T waves (see the section on oversensing later in this chapter). The atrial lead should be positioned to minimize oversensing of far-field R waves. It is independent of baseline R wave amplitude over the clinically relevant range (3-20 mV).
Generic 1mg glimepiride with amex
Women present with a diffuse reduction in hair density over the frontal and vertex areas diabetes type 1 and weight loss 1mg glimepiride fast delivery, but parietal and occipital regions may also be involved. Histopathologically, androgenetic alopecia is characterized by progressive diminution of follicular size. Hirsutism (increase in androgen-dependent terminal hair) occurs on the extremities, the anterior chest, the abdomen, the lower back, and in the beard area. There was a report of three women with plaque-type psoriasis, in which the increase in severity and extent of the skin disease correlated with the development of a prolactin-secretory pituitary gland microadenoma (Regana and Millet 2000). Prolactinoma In women, prolactinoma is detected fairly early because of consequent amenorrhea, infertility, and often galactorrhea. In men, the changes are more subtle, but include impotence, infertility, gynecomastia, and galactorrhea. Thyroid Gland Thyroid hormones potentiate both alpha- and beta-adrenergic receptors in multiple tissues throughout the body with consequent clinical responses including increased body temperature, hyperhidrosis, and warm moist skin (Safer 2011). Congenital Hypothyroidism Congenital hypothyroidism, a condition caused by thyroid hormone deficiency in fetal life, commonly manifests as intellectual disability. In addition, these individuals may develop myxedema, orbital hypertelorism, protruding abdomen with associated umbilical hernia, acral swelling, a clavicular fat pad, and slow-growing nails. The skin tends to be pale both because of the dermal mucopolysaccharides and dermal water content. The diffuse puffiness is secondary to increased deposits of mucin in the skin, known as myxedema. Myxedema is a consequence of the storage of large amounts of proteoglycans, which are also responsible for the yellowish color of the skin. The affliction most commonly affects palms, soles, and nasolabial folds; a lack of scleral involvement can differentiate the clinical manifestations of carotenemia from jaundice (Krause 2006). After substitution of the thyroid hormones, the pathologic proteoglycan deposits are quickly mobilized again. In addition, excess carotene, due to reduced hepatic conversion of beta-carotene to vitamin A, can deposit in the stratum corneum and manifest as a yellowing of the skin. In addition, patients often have rough and brittle hair at least partly due to reduced sebum secretion; diffuse, partial alopecia, often including genital and beard hair and loss of the lateral third of the eyebrow (madarosis), has been described in up to 50% of patients. Asteatotic eczema, acquired ichthyosis, and palmoplantar keratoderma are also observed. Lastly, autoimmune conditions can be observed, such as dermatitis herpetiformis, alopecia areata. Common cutaneous manifestations include flushing of the face, often with striking erythema and hyperhidrosis of the palms and soles. Clinically, the hair in thyrotoxicosis is often fine and soft with a downy texture; a diffuse alopecia areata may also be observed, clinically characterized by sudden onset of patches of hair loss. It may undergo spontaneous remission or exacerbations, sometimes evolving into hair loss of the entire scalp (alopecia totalis) and body hair (alopecia universalis) (Demirkesen 2015). Onycholysis (the separation of the distal nail plate from the bed) is a common occurrence. Less common cutaneous manifestations include generalized pruritus, eczematous dermatitis, chronic urticaria, and dermographism (Jabbour 2003). The phenomenon occurs in 4% of individuals; the hands, face, and pretibial and periorbital areas are most commonly affected resulting in a non-pitting edema. The skin is dry, cool, and atrophic as a consequence of decreased vascular flow and decreased reaction to heat. The eyes can appear puffy or swollen, the outer third of the eyebrow can be lost, and ptosis can occur due to decreased sympathetic stimulation. Additional features of myxedema include broadening of the nose, thickening of the lips, and macroglossia. Rarely, immunobullous disorders have been reported (Leonhardt and Heymann 2002), such as pemphigus foliaceus, pemphigus vulgaris, bullous pemphigoid, herpes gestationis, and dermatitis herpetiformis. Prevention is by efficient and timely management of thyroid dysfunction, and avoidance of trauma, tobacco use, and factors causing stasis in the lower extremity such as obesity. The standard management of dermopathy includes local or intralesional corticosteroids (Lan et al. Nails are brittle and ridged, with cracking at the free margin, or crumbling of the distal nail plate. Chronic mucocutaneous candidiasis, especially of the nails and oral mucosa, may occur in conjunction with hypoparathyroidism, but it is not a feature of postthyroidectomy iatrogenic hypoparathyroidism. Correction of the hypocalcemia usually results in clearing of the skin manifestations. Extensive calcification of the skin and subcutaneous tissue has been reported in a neonate with congenital hypoparathyroidism. Hyperparathyroidism Skin changes are not a particular feature of hyperparathyroidism, although subcutaneous calcification may occur (especially in hyperparathyroidism secondary to renal failure) (Marx 2000). Calcinosis cutis arises in the setting of abnormal calcium or phosphate metabolism and has been observed in primary or secondary hyperparathyroidism, paraneoplastic hypercalcemia, and hypervitaminosis D. Calcinosis cutis presents with firm, white dermal papules, nodules, plaques, or subcutaneous nodules typically at periarticular sites (Oh et al. Lesions tend to resolve spontaneously when calcium and phosphate levels normalize. Calciphylaxis is usually associated with secondary or tertiary hyperparathyroidism. Clinically, it begins as violaceous, mottled patches and plaques that resemble livedo reticularis. Lesions progress to painful, necrotic, indurated plaques and nodules that evolve to nonhealing ulcers covered with thick black eschars. Lesions most often involve the lower extremities and, less commonly, the upper extremities and trunk. Another sign that can be found in hyperparathyroidism is "Jellinek sign" that refers to darkening of the eyelids. Systemically applied corticosteroids at a dose above the daily production of endogenous cortisol (more than 20 mg) usually lead to a clinical picture identical to that of endogenous hypersecretion. Following long-term application of topical glucocorticosteroids leads to striae distensae, thinning of the skin, telangiectasias, and a rosacea-like dermatitis of the face. These side effects are more pronounced on the face, since the glucocorticoids increase the degradation of collagen and elastic fibers induced by sunlight: the aging skin is thus at higher risk than young skin. Novel steroids such as budesonide, mometasone furoate, prednicarbate, 17,21-hydrocortisone-aceponate and 14 Impact of Endocrine Disorders on Skin Disorders 409 hydrocortisone 17-butyrate-21-propionate, methylprednisolone aceponate, and fluticasone propionate all have a good anti-inflammatory effect and lesser side effects (Brazzini and Pimpinelli 2002). The cutaneous manifestations are quite similar whether caused by endogenous or iatrogenic hypercorticism, although there are additional effects mediated by androgens in patients with adrenal disease. A fine "cigarette paper" wrinkling is found on the dorsum of the hand and the elbow due to skin atrophy. They differ from the commonly found striae of adolescence, pregnancy, and obesity with respect to their inordinate depth and breadth and intense color (Hanley et al. Acne) and hirsutism are attributed to increased adrenal androgen and/or cortisol secretion (Stratakis 2016). Erythematous, monomorphic papules or small pustules distributed along the upper trunk, proximal upper extremities, neck, and face may be observed. Acanthosis nigricans) manifests with velvety, hyperpigmented, and thickened plaques occurring most often at the nape of the neck and the axilla, often associated with insulin resistance. Patients are predisposed to fungal overgrowth with pityrosporum yeast resulting in pityriasis versicolor. Pityriasis versicolor) and folliculitis as well as dermatophyte infections of the body, hands, feet, and nails due to cortisol-induced immune suppression and glucose intolerance (Leventhal and Braverman 2016). Other nonspecific cutaneous conditions, such as virilism and dyspigmentation, may be observed. Deposition of adipose tissue in characteristic locations contributes to the Cushingoid appearance: cheeks ("moon facies"), dorsocervical fat pad ("buffalo hump"), supraclavicular fat pad (thick, short neck), and behind the orbit (exophthalmos). Furthermore, loss of subcutaneous tissue can cause easy bruising and delayed wound healing. Other than striae, the majority of dermatologic manifestations resolve after therapy targeted at excess cortisol production. Although management of striae generally yields unsatisfactory results, in many cases, they become less noticeable over time.
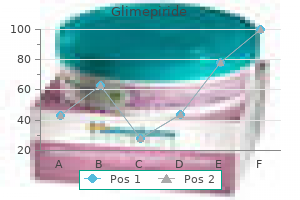
| Comparative prices of Glimepiride | ||
| # | Retailer | Average price |
| 1 | IKEA North America | 534 |
| 2 | Publix | 519 |
| 3 | ShopKo Stores | 738 |
| 4 | Dollar Tree | 984 |
| 5 | SUPERVALU | 680 |
| 6 | BJ'S Wholesale Club | 964 |
Purchase glimepiride 3 mg visa
Postural hypotension or alternating episodes of high or low blood pressures may also present managing diabetes without medicine order 3 mg glimepiride fast delivery. Other common nonspecific complaints are anxiety, panic attacks, trembling, nausea, fatigue, dyspnea, weight loss, visual problems, and polyuria. Paroxysms of symptoms may occur monthly, weekly, or several times daily, lasting from an hour to several days. The desensitization of locally expressed cardiovascular receptors by the chronic exposure of catecholamines may provoke specific wall motion abnormalities leading to Takotsubo cardiomyopathy (Gravina et al. Arrhythmias are present in around 20% of patients, which include sinus tachycardia, supraventricular and ventricular tachycardia, and sick sinus syndrome. Exposure to high levels of circulating catecholamines during surgery may cause hypertensive crises and arrhythmias. In case of persisting tachycardia, treatment with a beta1selective agent such as atenolol is mandatory. A calcium channel blocker should be considered if the hypertension persists without signs of heart failure. In contrast, if heart failure occurs, renin angiotensin aldosterone inhibitors should be preferred. Invasive treatment for advanced heart failure should be considered as a bridge to recovery from surgical excision of the tumor. Radiotherapy could be considered as additional treatment option, especially in metastasized disease. The unborn child is protected from maternal catecholamine outbursts, as the placenta contains enzymes breaking those down. The dissection originates either by a tear in the intima growing further by the inflow of coronary blood or by rupture of the vasa vasorum in the tunica media creating intramural hematoma. Subsequently, a false lumen develops with compression of the true lumen leading to myocardial ischemia. Several triggers have been identified that could be categorized in emotional and physical stress. In particular, estrogen is known to have a softening effect on tissue and may weaken the coronary arterial wall as well. Autopsy studies suggest that inflammation with eosinophilic infiltration in the adventitia is involved in the process of periarteritis and dissection. The first presentation may also be more disastrous with life-threatening ventricular arrhythmias (around 5%). Most often, the middle/distal part of the left anterior descending coronary artery is affected. In case of a small myocardial area at risk, one can decide to not intervene invasively and wait for spontaneous healing. The longterm outcome with drug eluting stent is better than with bare metal stent. Balloon angioplasty without stenting or the use of bioabsorbable stents, although not proven, may have some benefits. Beta-blockers might be beneficial to suppress arrhythmias or in case of heart failure. The standard use of statins in the absence of coronary plaques is controversial but may have an effect on the stabilization of the endothelium and prevention of future atherosclerosis. The left ventricle wall motion abnormalities are not consistent with the anatomical coronary artery blood supply and often recover completely within hours, days, or weeks. The pathophysiology is not fully elucidated but catecholamine excess, coronary artery spasm, and microvascular dysfunction may play a key 88 a b M. Normal heart Aorta 120 mmHg Left atrium Open coronary artery Takotsubo heart Aorta 200+ mmHg surge Coronary artery in spasm 120 mmHg 1 2 200+ mmHg surge Left ventricle Catecholamines Nature Reviews Cardiology. It is believed that the over-activation of sympathetic nervous system plays a crucial role. In addition, similar reversible cardiomyopathy with global or focal dysfunction in patients with pheochromocytoma and in the setting of acute brain injury has been described. Endomyocardial biopsy data are consistent with histologic signs of catecholamine toxicity with, in particular, contraction band necrosis (Karch and Billingham 1986). On the coronary, in angiogram or intra-coronary imaging, there are no signs of plaque rupture or obstructive coronary artery disease. Dual antiplatelet therapy is not indicated and 3 Impact of Endocrine Disorders on the Heart 89. Magnetic resonance imaging 4 days after ventriculography shows complete normalization of the left ventricle function (c diastole and d systole) (Hassan and Tornvall 2018) aspirin alone may be considered. In severe heart failure, catecholamine-based inotropes should be avoided and temporary mechanical circulatory support may be helpful. Summary It is magnificent to acknowledge that today there is much more awareness and insight in infrequent occurring cardiac diseases originating from endocrine disorders. Unraveling the role of prolactin in peripartum cardiomyopathy is an excellent 90 M. International and multidisciplinary collaboration is prerequisite for the management of these diseases. The challenge is to disseminate the obtained knowledge between all involved specialties in order to timely recognize and to manage the underlying endocrine-associated cardiac disease. The interaction between the thyroid and the heart has profound implications for contemporary management of patients with cardiovascular disease. Thyroid physiology plays a central role in modulating risk of cardiovascular disease in the area of arrhythmia, heart failure, and accelerating atherothrombosis. Carcinoid heart disease refers to the cardiac manifestations of neuroendocrine tumors. The clinical course is frequently characterized by right-sided valvular disease provoking cardiac decompensation with significant mortality and morbidity. Although medical therapy may relieve symptoms, surgical intervention is the only curative option for carcinoid heart disease. The prognosis of carcinoid heart disease has significantly been improved over the last years with novel medical and surgical interventions. Diabetes triggers a cascade of mechanisms that lead to a significantly higher risk of cardiovascular morbidity and mortality. In order to prevent such events, a multifactorial approach is required that includes lifestyle and glucose-level improvements, as well as antihypertensive, lipid-lowering, antiplatelet drugs, and timely coronary revascularization. Efficacy of individualized therapy based on factors such as gender and atherosclerotic burden is currently under investigation and may yield important improvements. Cross-References Impact of Endocrine Disorders on Typical and Atypical Cardiovascular Risk Factors Impact of Endocrine Disorders on Blood Pressure Impact of Endocrine Disorders on Vasculature References Addison T. Echocardiogram changes following parathyroidectomy for primary hyperparathyroidism: a systematic review and meta-analysis. Thyroid function and sudden cardiac death: a prospective population-based cohort study. Effect of valvular surgery in carcinoid heart disease: an observational cohort study. Pregnancyassociated acute myocardial infarction: a review of contemporary experience in 150 cases between 2006 and 2011. Pheochromocytoma is characterized by catecholamine-mediated myocarditis, focal and diffuse myocardial fibrosis, and myocardial dysfunction. Glucocorticoid receptor-9beta polymorphism is associated with systolic blood pressure and heart growth during early childhood. Outcome of patients with diabetes mellitus and acute myocardial infarction treated with 92 M. Pheochromocytoma mimicking Takotsubo cardiomyopathy and hypertrophic cardiomyopathy: a cardiac magnetic resonance study. Carcinoid heart disease: a guide for screening and timing of surgical intervention. Bromocriptine for the treatment of peripartum cardiomyopathy: a multicentre randomized study. Coronary artery bypass surgery compared with percutaneous coronary interventions for multivessel disease: a collaborative analysis of individual patient data from ten randomised trials. Excess risk of fatal coronary heart disease associated with diabetes in men and women: meta-analysis of 37 prospective cohort studies.
Order discount glimepiride line
Association between use of sodium-glucose cotransporter 2 inhibitors blood sugar log buy glimepiride 4 mg with mastercard, glucagon-like peptide 1 agonists, and dipeptidyl peptidase 4 inhibitors with all-cause mortality in patients with type 2 diabetes: a systematic review and meta-analysis. Impact of Endocrine Disorders on the Liver Agostino Di Ciaula, Grigorios Christidis, Marcin Krawczyk, Frank Lammert, and Piero Portincasa 6 Contents Introduction. Abstract the key role of the liver in systemic homeostatic processes and metabolic functions make unavoidable that this vital organ is a privileged target for a number of endocrine disorders. This is true also considering the wide panel of functional relationships with multiple endocrine organs. Impaired liver functions, on the other hand, pave the way to disrupted hormonal activity. Thyroid hormones have a role in regulating metabolic processes in the liver, and, on the other hand, thyroxine and triiodothyronine undergo liver metabolization, and the liver has a key role in regulating the systemic effects of these hormones. Similarly, complex pathways regulate the relationships between the adrenal gland and the liver, and dysfunctions in these two organs are frequently strongly interrelated. Hypopituitarism generates a phenotype similar to metabolic syndrome, with an increased risk of fatty liver. On the other hand, a compromised liver function (as that observed in liver cirrhosis) can stimulate the secretion of pituitary hormones. Finally, strong correlations exist between metabolic function in the liver and sex hormones in males and females, and both estrogens and androgens, if unbalanced, are able to alter liver function and to generate liver damage. In turn, chronic liver diseases strongly affect the correct function of the hypothalamic-pituitary-gonadal axis. A better knowledge of molecular mechanisms linking liver function and multiple hormonal axes could provide, in the next future, useful therapeutic tools to prevent or limit liver damage secondary to hormonal dysfunction or, conversely, to manage the altered hormonal homeostasis in patients with chronic liver diseases. The adequate homeostasis of the endocrine system requires an efficient metabolic function of the liver, which acts as a secondary endocrine organ. Indeed, the liver plays a major role in endocrine signaling and is at the crossroad between endocrine organs and between endocrine organs and their target organs. The liver also influences the metabolism of several hormones (in particular thyroid, adrenal, sex, and growth hormones). Consequently, a disrupted metabolic function in the liver generates marked consequences in terms of altered circulating hormones and disturbed hormonal signaling. Several diseases involving the primary endocrine organs frequently promote hepatic damage with a number of disorders ranging from lipid accumulation to cholestatic injury, hepatitis, fibrosis, cirrhosis, and cancer. Changes occur within the scenario of increased insulin resistance and systemic low-grade "metabolic" inflammation due to expansion of visceral adiposity and release of several pro-inflammatory adipocytokines (Grattagliano et al. Of note, fat accumulation in the liver has a key role in the development of insulin resistance at a systemic level and in other district, such as skeletal muscle. The liver is the organ producing several proteins, which can appear into the circulation (up to 25%). An example is the synthesis and secretion of albumin, C-reactive protein and fibronectin, proteins involved in the regulation of hemostasis and fibrinolysis, and apolipoproteins acting as carriers. Other proteins regulate metabolic pathways and act as hepatokines and pro-inflammatory agents, i. Changes lead to perturbation of metabolic/glycol-lipid function and insulin resistance in extrahepatic tissues (Kaur et al. The aim of this chapter is to provide an overview of the complex relationships linking endocrine and liver functions and of the reciprocal effects of diseases both involving the primary endocrine organs and the hepatocytes. Thyroid hormones on one side regulate and coordinate the liver metabolism at the cellular level, and on the other side, the liver is involved in the degradation of the thyroid hormones, acting in that way as a regulator in the feedback loop of the hypothalamic-pituitary-thyroid axis (Malik and Hodgson 2002). In the liver, thyroid hormones regulate central pathways for the synthesis and metabolism of triglycerides and cholesterol. Of note, thyroid hormones induce not only fatty acid uptake and lipogenesis but also their degradation via -oxidation. This explains the total reduction of hepatic triglycerides during an uncontrolled hyperthyrotic state. The biosynthesis and clearance of cholesterol, as well as more complex metabolic pathways of lipids (lipophagy, peroxisomal, and mitochondrial fat oxidation), are subject to the control by thyroid hormones as well. The major part of the activation and inactivation of thyroid hormones occurs in the liver through the catalytic action of the deiodinase systems (Bianco et al. Although this system can also inactivate T3 and T4, the seleno-deiodinase enzyme system type 3 (found in the liver, skin, and central nervous system) represents the main inactivator, converting via inner ring deiodination T4 to reverse T3 (rT3), T3 to T2, and rT3 to rT2, all of which represent inactive metabolites. In this regard, it is interesting to underscore that the latter system is barely detected in the liver of healthy individuals but induced in regenerating the liver and hepatic tumors and in serum and liver tissue of critically ill patients. Findings point to a possible response to inflammation or injury via increased hepatic inactivation of thyroid hormones. In addition, the liver synthesizes numerous proteins such as thyroxin-binding globulin, thyroxin-binding prealbumin, and albumin, which can bind circulating thyroid hormones and thereby affect their biologically active amounts. There are furthermore data indicating that bile acids, which are synthesized in the liver, do not only contribute to the absorption and metabolism of lipids but act as signaling molecules, activating pathways inducing the production of the type 2 deiodinase enzyme and in this way the local conversion of T4 to T3 (Watanabe et al. This could comprise a local mechanism preventing fat accumulation, obesity, or insulin resistance and pose a pharmacological target for the future. The abnormalities of thyroid function in individuals with liver diseases have to be interpreted in the context of the "sick euthyroid syndrome," meaning the reduction of total and free T3 and the elevation of T4 and rT3 secondary to changes of selenodeiodinases, plasma concentrations of thyroid-binding proteins and lipids, and the consequences of acute stress on the hypothalamus-pituitary-thyroid axis. The thyroid-binding globulin represents an acute phase protein, thus reducing the bioactive amount of thyroid hormones, and this has been shown to be clinically relevant in the setting of 6 Impact of Endocrine Disorders on the Liver 163 acute hepatitis irrespective of its etiology. Many autoimmune hepatic diseases coexist with or predict concomitant thyroidal autoimmunity (Kus et al. In severe cases of liver failure, available data are scarce and inconsistent to indicate causative links or clinical benefits through pharmacological modification. Severe hypothyroidism can manifest with overt symptoms and signs mimicking acute liver disease, such as ascites in patients with myxedema or cholestatic jaundice caused by impaired bile secretion, concomitant hypercholesterolemia, and decreased motility of the gallbladder. It was also postulated that the hepatic signs of hypothyroidism might be secondary to primary affection of another target organ, such as right heart failure leading to congestion of hepatic veins, portal hypertension, and ascites development. Hyperthyroidism, and in particular thyrotoxicosis, is associated with elevated aminotransferase activities in up to 40% of cases, at least in part resulting from hypoxic stress due to elevated oxygen demand and inflammatory infiltrates. Especially in the most severe cases, it is difficult to distinguish the primary liver damage from the secondary manifestations due to congestive heart failure, catabolic state, or complications from cardiopulmonary instability. Systemic diseases, such as amyloidosis or hereditary hemochromatosis, may affect both organs, causing non-specific symptoms in the initial stages, which may result in late diagnosis. Intake from amiodarone is the most notable example, predisposing to hypo- or hyperthyroidism and liver fibrosis. Thionamides have been used since many years for the treatment of hyperthyroidism, and it is well established that they can cause acute liver injury, ranging from elevated liver enzymes to fulminant liver failure. Typically, metamizole and carbimazole cause a cholestatic pattern of liver injury, whereas propylthiouracil is associated with a hepatocellular pattern of liver injury. Therefore, monitoring of liver enzymes is essential after the initiation of treatment. A previous medical history of liver diseases or drug-induced liver injury has to be evaluated appropriately. Adrenal Glands and the Liver Adrenal Insufficiency Liver enzymes can increase in patients with adrenal insufficiency (Kalambokis and Milionis 2009). These findings can develop in combination with multi-organ autoimmune disorder (such as autoimmune polyendocrine syndrome type 1) involving autoimmune hepatitis (Meloni et al. Adrenocortical dysfunction (mainly adrenal insufficiency) is common in patients with stable, decompensated or complicated cirrhosis, possibly due to multiple factors including decreased cholesterol concentrations (and, in turn, reduced steroid synthesis in adrenal glands linked to decreased availability of this essential precursor), and increased blood levels of endotoxin and proinflammatory cytokines, leading to impaired hypothalamus-pituitary-adrenal axis (Fede et al. In this case, treatment with steroids could decrease short-term mortality (Kumar et al. In these patients, in particular, increased glucocorticoid levels are paralleled by increased lipogenesis and increased circulating free fatty acids. The latter two abnormalities derive from increased lipolysis reduced fatty liver oxidation in the liver and visceral obesity, altered secretions of adipokines, and, finally, increased lipid accumulation in the hepatocytes (Ferrau and Korbonits 2018) ranging from liver steatosis to steatohepatitis, fibrosis, cirrhosis, and increased risk of hepatocellular cancer (Woods et al. Thus, aldosterone is able to stimulate hepatic gluconeogenesis but also to promote adipogenic effects and metabolic alterations, including insulin resistance, altered lipid metabolism, impaired glucose homeostasis, and the development of fatty liver (Bothou et al.
Order cheap glimepiride on-line
Slight resistance is felt on traversing the synovial membrane; it should be possible to aspirate fluid diabetes prevention weight loss purchase glimepiride 4 mg free shipping, and injection fluid should flow easily. If injection is used for prepatellar bursitis, give 25mg hydrocortisone acetate into the most tender spot. First carpometacarpal joint of thumb Avoiding radial artery, inject 25mg hydrocortisone acetate at base of first metacarpal at 1cm depth in anatomical snuffbox (aim at base of little finger). When injecting a trigger finger, ask the patient to flex and extend the finger to ensure that the tip of the needle is not in the tendon. Orthopaedics 710 Tendon rupture and injury the main tendons to rupture are the extensor tendons of the fingers, the Achilles tendon (fig 11. Mallet finger Often caused by a sudden blow to an extended finger (eg hit by cricketball on outstretched finger) which leads to rupture of the extensor tendon at the distal phalanx. Achilles (calcaneal) tendon rupture Typified by sudden pain at the back of the ankle during running or jumping as the tendon ruptures. Treatment: Tendon repair (percutaneous or open) is often preferred by young, athletic patients. Conservative treatment may be most suitable for smokers, diabetics, and those >50yrs old. Open surgery significantly reduces the risk of rerupture compared with conservative cast immobilization or functional bracing; however wound breakdown from open intervention can be catastrophic as the tendon then becomes exposed. Injury may be direct (eg blow) or indirect (stumbling causing sudden contraction of the apparatus). After repair, the knee is immobilized for >4 weeks with immediate postoperative weightbearing; then intensive physiotherapy helps regain knee function. A systematic review of the use of platelet-rich plasma in sports medicine as a new treatment for tendon and ligament injuries. Also note the ordering of the flexor tendons posterior to the medial malleolus, from anterior to posterior-this can be remembered with the mnemonic on p657: Tom, Dick and A Very Nervous Harry. Pes cavus Accentuated longitudinal foot arches which do not flatten with weight-bearing. Claw toes may occur, as weight is Cerebral palsy taken on metatarsal heads when walking (hence Polio causing pain). While the central theme is the diagnosis and Cardiovascular disease management of injury arising from participation in and stroke sport, including but not exclusively elite athletes, Diabetes it has an increasingly important public health role: Obesity promoting healthy living and chronic disease man- Osteoporosis Dementia agement through exercise. As in other areas of medicine, a thorough history and understanding of the injury mechanism is paramount, and is complemented by appropriate clinical examination. Concussion and sport-specific protocols Concussion is a minor traumatic brain injury. Emerging evidence has suggested not only immediate concerns of subsequent increased injury risk and second impact syndrome, but a long term potential for chronic neurological impairment. Many sports have implemented specific guidance for the assessment and management for head injuries, including a graduated return to play- protecting players and empower medical teams. Please refer to the 2012 Zurich consensus statement on concussion in sport for more information. In severe cases, specialist review and steroid injection is an option but the risk of tendon rupture must be balanced. Remember careers are often short lived, athletes are competing for their livelihoods-a drive which must not be underestimated or ignored. Appropriate imaging must be arranged urgently but this must not delay the treatment of life-threatening issues. It is based on the unfurling fern frond which eventually points inward to indicate an eventual return to the beginning. Compare placement (in degrees or %) of distal fragment with respect to proximal fragment so when giving a displacement description, this refers to the distal fragment. This was historically named after judicial hangings, yet post-mortem studies showed that only a few hangings actually demonstrated this injury pattern. Just like modern this time was called the Dark Ages, not because medicine, the clues to aetiology lie in noting the surroundings. Ultrasound can also be used in foreign body detection and to guide removal, especially for those that are not radio-opaque (eg splinters). The appropriateness of scanning in an acute trauma must be decided on the balance of risk and benefit to the patient. Ensure that the patient is haemodynamically stable before moving them to the relatively resource-poor radiology department. Always be on the lookout for clinical deterioration requiring prompt intervention. For this reason, you may be paradoxically encouraged to request more imaging (eg including C-spine), given that having to come back for a second scan doubles the risk. Remember to think of patterns of injury: eg rib fractures with bilateral pulmonary contusions have a high coincidence of intra-abdominal injury. Consider their state of distress at being both in pain and a patient; the latter aruguably more painful. As they face the unknown they defend themselves in the best manner possible, arming themselves with familiar terminology. Although jargon is to be approached with caution in this situation, always use appropriate terminoloy when describing X-rays (p715). For example an adult (6), diaphyseal (12) forearm fracture may take 12 Endochondral ossification weeks to heal. Risk factors for poor healing Use the Gustilo classification to describe the Older age soft tissue damage incurred by open fractures. Trauma Smoking and tissue healing-the consequences of a cigarette break Trauma patients need to knit back together well, and they face a number of complications without adding tobacco into the physiological equation. Nicotine increases the time it takes for a fracture to unite and reduces quality of bone healing. Salter R, Harris W, Injuries involving the epiphyseal plate, the Journal of Bone and Joint Surgery, Volume 45, Issue 3, pp. Most physes are in a plane that makes it relatively easy to diagnose the injury (eg distal radius, and to a lesser extent proximal femur), whereas some cross the plane of the x-ray at multiple angles (eg proximal humerus). Conservative management uses splints (see p811), casts, and traction to realign and stabilize displaced fractures. Manipulation under anaesthesia (for analgesia and muscle relaxation) and X-ray screening. Methods of traction Internal and external fixation has removed the need for much traction in adults, but it is still used for children. Traction or fixation helps hold the reduced fracture in place for healing, which takes from 2 weeks (babies) to >12 weeks (p718). Debridement is performed by plastic & orthopaedic surgeons working together within 24 hours of the injury (unless there is contamination). Cover wound in saline-soaked gauze to prevent desiccation; only handle to remove gross contamination and allow photography. Definitive skeletal stabilization and wound cover are achieved within 72 hours and should not exceed 7 days. The trick is then to Intra-articular #s achieve stable internal fixation in order to facilitate Open # Displaced unstable # healing and also reduce serious complications (p722). K-wires are less rigid than plates and screws but can easily be removed after use. External fixation is useful when there are burns, loss of skin and/or bone, or in case of open fractures since external fixation causes less disruption to the fracture site and associated soft tissue. Pins are inserted into the bones directly; either just through the far bone cortex or directly through the opposite side of the limb. Stability of fixation can be increased in a number of ways; use additional or larger dimeter pins, move rods closer to the bone, pins in different planes, etc. The biochemical theory-release of free fatty acids directly damage the penumocytes.
Glimepiride 2mg overnight delivery
The usual surgical procedure is a partial hemilaminectomy with excision of the prolapsed disc diabetes mellitus definition pdf 2013 purchase glimepiride 1 mg with mastercard. Surgical decompression is done if there is leg pain rather than backpain or stenosis is focal. All patients for prevention of G10 should receive calcium, vitamin D and bisphosphonate. Nonsurgical interventional therapies for low back pain: a review of the evidence for an American Pain Society clinical practice guideline. A randomised controlled trial of spinal manipulative therapy in acute low back pain. In addition to accelerated atherosclerosis, these patients often demonstrate endothelial dysfunction secondary to early development of coronary artery disease, impaired nitric oxide release, increased serum levels of free fatty acids, and advanced end products of glycosylation. Hypercoagulability secondary to increased levels of fibrinogen and plasminogen activator inhibitor type I and enhanced platelet aggregation is present. Autonomic nervous system dysfunction may produce increased sympathetic tone at baseline and may contribute to silent myocardial ischemia, impaired heart rate variability, and poor prognosis (Haffner et al. Dopamine agonists, including cabergoline, bromocriptine, and quinagolide, are the primary treatment for prolactinomas. High doses and long duration of therapy 1 Impact of Endocrine Disorders on Typical and Atypical Cardiovascular. This treatment duration raises concern for increased risk of valvulopathy, including tricuspid regurgitation, mitral regurgitation, and aortic regurgitation (Valassi et al. Although most reports do not show an association between the use of dopamine agonists and cardiac valve disease, clinicians are advised to use the lowest possible doses of dopamine agonists. Echocardiographic monitoring should be considered, especially in patients requiring long-term and/or higher-dose therapy, and those with underlying heart or valvular disease. Effects of Sexual Hormone Disturbances on Traditional and Nontraditional Cardiovascular Risk Factors Androgens play a major role in human metabolic health and disease. Effects of androgens on adipose tissue and muscle may largely be governed by circulating serum and tissue-specific concentrations, with a narrow physiological window in both sexes, outside of which disturbances in metabolism and body composition are observed. Androgen Excess in Women and Related Metabolic Consequences Disturbances in androgen metabolism secondary to gonadal, adrenal, or hypothalamic-pituitary disease lead to alterations of circulating androgen concentrations and result in reproductive and metabolic complications. As a consequence of the enzymatic block, precursor steroids are shunted down the pathways of androgen biosynthesis, which is further increased by enhanced hypothalamic-pituitary-adrenal drive due to the loss of the negative feedback by cortisol. Defects in insulin signaling can be found at the level of the insulin receptor or in postreceptor signal transduction. Compensatory hyperinsulinemia may stimulate ovarian androgen biosynthesis by direct effects of insulin on theca and stromal cells, although other peripheral sources of insulin-stimulated androgen generation cannot be discounted. Common symptoms are a reduction of libido and erectile strength, fatigue, reduced physical strength and endurance as well as sometimes impaired cognitive function and mood disturbances (Boehm et al. The overwhelming majority of such cases are caused by tumors of the hypothalamic-pituitary area. Congenital hypogonadotropic hypogonadism may be observed in the context of multiple pituitary hormone deficiencies in conditions such as septo-optic dysplasia but more commonly is associated with isolated gonadotrophin deficiency as observed in Kallmann syndrome, which may be associated with anosmia and craniofacial abnormalities. Surgical or pharmacological androgen deprivation therapy is an established treatment option for both metastatic hormone-naive and castrationresistant prostate cancer. Obesity significantly increases the age-related T decline and is associated with disordered gonadotrophin release. The concept of a hypogonadal-obesity-adipokine cycle is a proposed mechanism behind this association. Obesity has been suggested to lead to enhanced aromatization of androgens to estrogens by aromatase in adipose tissue, thereby reducing the level of active androgens. The Role of Androgens in Metabolic Target Tissues In addition to their central role in the development and maintenance of male and female reproduction and sex drive, androgens exert key effects on metabolic target tissues. These include adipose tissue and skeletal muscle, compartments crucially involved in maintaining systemic glucose and lipid homeostasis. Androgens, Adipose Tissue, and Lipid Metabolism Patterns of body fat distribution show a clear sexual dimorphism, with women showing a higher percentage of body fat than men and, on the contrary, with men having a greater total lean mass. The typical fat distribution in women is in a gynecoid manner, with less visceral but more subcutaneous fat; men have a predominant android fat distribution, with more visceral and less subcutaneous adipose tissue. Adipose tissue expansion is a consequence of both hyperplasia (adipogenesis), which is driven by proliferation of preadipocytes and their differentiation into adipocytes, and hypertrophy, which is driven by accumulation of lipid in differentiated adipocytes; both processes are major determinants of metabolic dysfunction (Demerath et al. Androgens impair adipogenesis by inhibiting proliferation and differentiation of mesenchymal stem cells and preadipocytes. Differential effects of androgens on adipose tissue and skeletal muscle and implications for global metabolism can be summarized as follows: androgens may exert pro-lipogenic effects on adipose tissue, resulting in fat mass expansion; at 1 Impact of Endocrine Disorders on Typical and Atypical Cardiovascular. Mechanisms in endocrinology: the sexually dimorphic role of androgens in human metabolic disease. Eur J Endocrinol 2017;177(3):R125-R143) higher concentrations, as observed in the healthy male range, net anabolic effects on increasing skeletal muscle bulk predominate. A large amount of literature supports the association between low T and increased fat mass compared to eugonadal controls. Although age is associated with decreased androgen levels, negative associations between T and total body fat mass, body fat percentage, waist circumference, and visceral adipose tissue are maintained after adjustment for age (Blouin et al. The initial mechanism hypothesized for this association was the increased visceral adiposity in the context of hypogonadism, but recent studies have pointed out a direct role for androgens on liver metabolism, resulting in an increased malonyl-CoA, a substrate for de novo lipogenesis (Schwingel et al. Moreover, synthetic anabolic steroid use has also been linked hepatic steatosis in men. On the other hand, men with coronary artery disease present with lower T levels, and its severity is negatively correlated with T levels. Perticone the thyroid gland secretes two main iodinated hormones, 3,5,30 -triiodothyronine (T3) and 3,5,30 50 -tetraiodothyronine (T4), also known as thyroxine. The affinity of the thyroid hormone receptor is approximately tenfold higher for T3 than for T4; for this reason T4 must be converted to T3 to produce potent thyroid hormone receptor-mediated effects. Anyway, although T4 is a prohormone for T3, it can directly act through thyroid hormone receptors in a variety of tissues, such as blood vessels, exerting a proangiogenic effect. Thyroid hormones also have a direct inotropic effect on the heart by positively regulating the gene expression of the 1-adrenergic receptor. In addition, thyroid hormones influence cardiac chronotropy through both genomic and nongenomic effects on components of the adrenergic receptor complex and on sodium, potassium, and calcium channels. The effect of thyroid hormones on cardiac chronotropy manifests as tachycardia and increased risk of atrial fibrillation in hyperthyroid states and as bradycardia and reduced cardiac contractility in hypothyroidism. Nongenomic effects of thyroid hormones on cardiomyocytes and the systemic vasculature include activation of sodium, potassium, and calcium membrane ion channels, effects on mitochondria, and involvement in signaling pathways of cardiomyocytes and vascular smooth muscle cells. The decrease in systemic vascular resistance induced by thyroid hormones, together with their direct inotropic effects, leads to an increase in cardiac output. The renin-angiotensin-aldosterone system also has an important role in the hemodynamic effects of thyroid hormones. The initial decrease in systemic vascular resistance induced by thyroid hormones leads to decreased perfusion in the kidneys, which increases renin and aldosterone levels. The activation of the renin-angiotensin-aldosterone axis leads to an increase in cardiac preload, which is another explanation for the increase in cardiac output induced by thyroid hormones. Hyperthyroidism may result from autoimmune disease, thyroid nodule autonomy, or exogenous thyroid hormone ingestion. Normalization of thyroid hormone levels leads to the reversion to normal sinus rhythm in approximately 60% of patients who have atrial fibrillation due to hyperthyroidism. Shortness of breath during minimal exertion is also commonly reported by patients with hyperthyroidism; however, the exact etiology of this symptom has not been clearly defined. If overt hyperthyroidism is left untreated, or in those individuals with severe long-standing hyperthyroidism, this increased cardiac output can lead to symptoms and signs of heart failure as a result of left ventricular hypertrophy, arrhythmias, and an increase in cardiac preload secondary to fluid overload. The prevalence in the general population of endogenous subclinical hyperthyroidism depends on age, sex, and iodine intake, with a reported prevalence of 0.
3 mg glimepiride
The vestibular portion of the membranous labyrinth is divided into two sections: kinetic labyrinth (formed by the semicircular canals) diabetes symptoms hand pain purchase generic glimepiride on line, and the static labyrinth (formed by the saccule and utricle). Neural activity generated by the canals is transmitted in the vestibular nerve to the vestibular nuclei on the same side of the brainstem. Both are expansions of the membranous labyrinth and contain a macula which consists of hair cells covered by an otolithic membrane (lying on top of the hair cells) and otoconia (composed of calcium carbonate crystals or otoliths) on the surface. Organ of Corti this contains receptor hair cells which lie on supporting tissue arising from the basilar membrane in the cochlea. The hair cell processes are embedded in a thin membrane that bridges across the organ of Corti, known as the tectorial membrane. The pressure wave is transmitted through the perilymph, and leads to vibration of the basilar membrane, depending on the frequency of the sound. Hair cells located in the tip of the cochlea are stimulated by low-frequency tones and those located at the base are stimulated by high-frequency tones. Consequently, vestibular symptoms and signs are almost always present in brainstem disease but are of limited intrinsic localizing value within the brainstem. Conductive hearing loss is due to a dysfunction in transmission of sound to the cochlea (in the external or middle ear). The presence of associated unilateral hearing loss or fullness in the ear suggests ear pathology. Evaluation of the vestibular system includes: Neuro-ophthalmological evaluation to assess for the presence of nystagmus in primary gaze and in all directions of gaze. Using Frenzel goggles to remove ocular fixation is often helpful in assessing nystagmus. In central vertigo, the nystagmus may have a vertical component and the direction of the nystagmus may change. Tip E Peripheral nystagmus usually is horizontal and torsional and the direction of the nystagmus does not change. Differential diagnosis Hearing loss Brainstem (pontomedullary junction): Infarct or hemorrhage. Vestibular dysfunction Peripheral causes of vertigo Peripheral vestibular syndromes usually present with severe vertigo, often associated with tinnitus, hearing loss, and nystagmus. Patients present with severe vertigo that lasts several days, associated with nausea, vomiting, and at times unilateral hearing loss. Anatomy the glossopharyngeal nerve contains sensory, motor, special visceral afferent, and parasympathetic fibers1. Sensory fibers Taste fibers from the posterior third of the tongue and pharynx terminate (via the glossopharyngeal nerve) in the nucleus of the tractus solitarius. Base of skull (jugular foramen) (654) the glossopharyngeal nerve emerges from the posterior lateral sulcus of the medulla in line with the vagus and the bulbar fibers of the spinal accessory nerve, and enters the internal part of the jugular foramen lying on the medial side of the sigmoid sinus. Central causes of vertigo Vertigo of central origin is usually less severe than peripheral vertigo and is usually continuous. It is associated with abnormalities referable to the brainstem or cerebellum and hearing impairment is less frequent. The gag reflex therefore is too gross for accurate clinical diagnosis of a glossopharyngeal lesion. It carries motor, sensory, and parasympathetic fibers that innervate the head, neck, thorax, and abdomen. In the region of the jugular foramen are two vagal ganglia: the jugular ganglion (superior vagal ganglion) and the nodose ganglion (inferior vagal ganglion) (655)1. The right recurrent laryngeal nerve descends anterior to the right subclavian artery and turns posteriorly under the artery to ascend in the tracheoesophageal sulcus, whereas the nerve on the left turns posteriorly around the aortic arch and ascends in the same sulcus on the left. Both recurrent branches then enter the larynx and supply all intrinsic muscles of the larynx except the cricothyroid muscle (supplied by the external branch of the superior laryngeal nerve). The sensory fibers carried in the vagus nerve have their cell bodies in the jugular and nodose ganglia. The vagus nerve supplies parasympathetic innervation to smooth muscle and glands of the pharynx, larynx, and thoracic and abdominal viscera. Etiologies include infarcts, demyelinating lesions, tumors, infectious and inflammatory conditions, syringobulbia, and motor neuron disease. Patients with isolated vagus nerve lesions present with hoarseness as their primary symptom. Lesions of recurrent laryngeal nerve the recurrent laryngeal nerve is longer on the left than the right and is therefore more susceptible to injury23. Etiologies include thoracic malignancies, lymphadenopathy, aneurysms, tumors, and operative injuries. A unilateral recurrent laryngeal lesion results in paralysis of all laryngeal muscles except the cricothyroid (innervated by the superior laryngeal nerve) and manifests as hoarseness. Neuromuscular junction disorders Patients with myasthenia gravis usually present with ocular symptoms or generalized weakness. However, some patients present with fatigable bulbar weakness including hoarseness, dysarthria, and dysphagia. If there is weakness of bilateral sternocleidomastoids, there is impairment of neck flexion. When the trapezius is weak, there is drooping of the shoulder at rest and the scapula is displaced downward and laterally with slight winging of the scapular vertebral border. Proximal spinal accessory nerve lesions result in weakness of the trapezius and sternocleidomastoid. Anatomy the hypoglossal nerve fibers arise from a nuclear column located under the floor of the fourth ventricle that extends the entire length of the medulla (658). Unilateral hypoglossal nerve palsy Wasting, furrowing, fasciculations, and weakness of one side of the tongue (ipsilateral to the lesion), with deviation of the tongue to the side of the paresis. With tongue protrusion, the normal contralateral muscles force the tongue forward and to the opposite side (which is towards the side of the weak muscle). Bilateral hypoglossal nerve palsies Bilateral weakness, atrophy, and fasciculations. With bilateral corticobulbar lesions affecting fibers to the hypoglossal nuclei, the tongue is paretic with slow lateral movements and spastic dysarthria. Nuclear and fascicular lesions the hypoglossal nuclei in the dorsal medulla may be affected by pathologic processes such as demyelinating disease, motor neuron disease, syringobulbia, Chiari malformation, tumor, arteriovenous malformation, hemorrhage, ischemia, inflammatory, and infectious conditions. A unilateral ischemic lesion in the medulla in the territory of the vertebral or anterior spinal artery (medial medullary syndrome) may result in involvement of the hypoglossal nerve fibers coursing ventrally in the medulla (ipsilateral tongue weakness and atrophy), the pyramid (contralateral arm and leg weakness), and the medial lemniscus (contralateral impairment of position and vibration sense). Peripheral lesions the hypoglossal nerve may be involved in lesions of the meninges, posterior fossa, the skull base, retropharyngeal space, or neck. The distal hypoglossal nerve may be involved in the neck resulting in ipsilateral weakness and hemiatrophy of the tongue. Practice parameter: therapies for benign paroxysmal positional vertigo (an evidencebased review). Although the ganglion cell axons that make up the optic nerve project to the lateral geniculate nucleus, the scope of this section will be limited to optic neuropathies anterior to the chiasm. They receive information from the rods and cones that is modified by amacrine, bipolar and horizontal cells in the outer retina (659). The nerve travels within the muscle cone and exits the orbit through the optic canal. The optic nerves pass medially to the internal carotid arteries and above the ophthalmic arteries. Color vision More important in diagnosing optic neuropathies is acquired dyschromatopsia. Congenital color blindness occurs in one in eight men and is symmetric and stable during the course of their lives. In truth there is significant cross over between the two types of acquired dyschromatopsia, such as in patients with glaucoma.