Buy haldol on line
Molecular dissection of the intrinsic factor-vitamin B12 receptor medicine 834 purchase 5 mg haldol free shipping, cubilin, discloses regions important for membrane association and ligand binding. Amnionless, essential for mouse gastrulation, is mutated in recessive hereditary megaloblastic anemia. Cubilin and megalin expression and their interaction in the rat intestine: Effect of thyroidectomy. Imerslund-Grasbeck syndrome (selective vitamin B(12) malabsorption with proteinuria). Long term treatment with metformin in patients with type 2 diabetes and risk of vitamin B-12 deficiency: Randomized placebo controlled trial. Malabsorption of vitamin B12 and intrinsic factor secretion during biguanide therapy. Metformin induces reductions in plasma cobalamin and haptocorrin bound cobalamin levels in elderly diabetic patients. Pteroylpolyglutamate hydrolase from human jejunal brush borders: Purification and characterization. Intracellular pteroylpolyglutamate hydrolase from human jejunal mucosa: Isolation and characterization. Adaptive regulation of intestinal folate uptake: Effect of dietary folate deficiency. Bacterially synthesized folate in rat large intestine incorporated into host tissue folylpolyglutamates. Use of deoxyuridine suppression test to evaluate localized folate deficiency in rat colonic epithelium. The effect of folate supplementation on the incidence of dysplasia and cancer in chronic ulcerative colitis: A case control study. The human reduced folate carrier gene is ubiquitously and differentially expressed in normal human tissues: Identification of seven non-coding exons and characterization of novel promoter. Distribution of the folate receptor in normal in normal and malignant cell lines and tissues. Structure and function of the reduced folate carrier a paradigm of a major facilitator superfamily mammalian nutrient transporter. Localization of the murine reduced folate carrier as assessed by immunohistochemical analysis. Apical membrane targeting and trafficking of the human proton-coupled folate transporter in polarized epithelia. Restoration of high-level transport activity by human reduced folate carrier ThTr1 thiamine transporter chimaeras: Role of the transmembrane domain 6/7 linker region in reduced folate carrier function. Intracellular trafficking and membrane targeting mechanisms of the human reduced folate carrier in mammalian epithelial cells. Identification of dynein light chain road block-1 as a novel interaction partner with the human reduced folate carrier. Folate uptake in the human intestine: Promoter activity and effect of folate deficiency. Functional elements in the minimal promoter of the human proton-coupled folate transporter. Differentiationdependent regulation of the intestinal folate uptake process: Studies with Caco-2 cells and native mouse intestine. Effect of folate oversupplementation on folate uptake by human intestinal and renal epithelial cells. Reduced folate carrier: Tissue distribution and effects of chronic ethanol intake in the micropig. Down-regulation of reduced folate carrier may result in folate malabsorption across intestinal brush border membrane during experimental alcoholism. Low folate transport across intestinal basolateral surface is associated with down-regulation of reduced folate carrier in in vivo model of folate malabsorption. Availability of monoglutamyl and polyglutamyl folates in normal subjects and in patients with celiac sprue. Sulfasalazine is a potent inhibitor of the reduced folate carrier: Implications for combination therapies with methotrexate in rheumatoid arthritis. Impaired folic acid absorption in inflammatory bowel disease: Effects of salicylazosulfapyridine (azulfidine). Hydrolysis and absorption of pantothenate and its coenzymes in the rat small intestine. Transport and metabolism of pyridoxamine and pyridoxamine phosphate in the small intestine. Pyridoxine uptake by colonocytes: A specific and regulated carrier-mediate process. Brown-Vialetto-van Laere syndrome, a ponto-bulbar palsy with deafness, is caused by mutations in C20orf54. Uptake of riboflavin across the brush border membrane of rat intestine: Regulation by dietary vitamin levels. Regulation of riboflavin intestinal uptake by protein kinase A: Studies with Caco-2 cells. Transport functions of riboflavin carrier in the rat small intestine and colon: Site difference and effects of tricyclic-type drugs. Mechanism of transport of riboflavin in rabbit intestinal brush border membrane vesicles. Oxidative stress is associated with region-specific neuronal death during thiamin deficiency. Blood serum thiamin and thiamin phosphate esters concentrations in patients with alcohol dependence syndrome before and after thiamin treatment. Thiamin and thiamin phosphate ester deficiency assessed by high performance liquid chromatography in four clinical cases of Wernicke encephalopathy. Further studies on erythrocytes thiamin transport and phosphorylation in seven patients with thiamin-responsive megaloblastic anaemia. Mutations in a new gene encoding a thiamin transporter cause thiaminresponsive megaloblastic anaemia syndrome. Cloning of the human thiamin transporter, a member of the folate transporter family. Evidence for carriermediated mechanism for thiamin transport to human jejunal basolateral membrane vesicles. In situ localization of enzymes and mucin in normal rat colon embedded in plastic. The distribution of certain enzyme systems in the normal human gastrointestinal tract. Enteropathogenic Escherichia coli inhibits intestinal vitamin B1 (thiamin) uptake: Studies with human-derived intestinal epithelial Caco-2 cells. Impaired intestinal vitamin B1 (thiamin) uptake in thiamin transporter-2-deficient mice. Thiaminresponsive megaloblastic anemia syndrome: A disorder of high-affinity thiamin transport. Targeting and trafficking of the human thiamine transporter-2 in epithelial cells. Tspan-1 interacts with thiamine transporter-1 in human intestinal epithelial cells and modulates its stability. Identification of a mouse thiamin transporter gene as a direct transcriptional target for p53. Differentiationdependent up-regulation of intestinal thiamin uptake: Cellular and molecular mechanisms. Thiamin uptake in human intestinal biopsy specimens, including observations from a patient with acute thiamin deficiency. Adaptive regulation of intestinal thiamin uptake: Molecular mechanisms in wild-type and transgenic mice. Transport of thiamin in the human intestine: Mechanism and regulation in intestinal epithelial cell model Caco-2. Pancreatic beta cells and islets take up thiamin by a regulated carrier-mediated process: Studies using mice and human pancreatic preparations. Chronic alcohol consumption and intestinal thiamin absorption: Effects on physiological and molecular parameters of the uptake process.
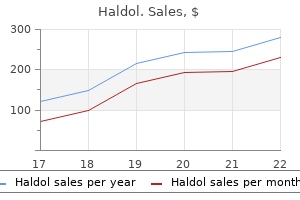
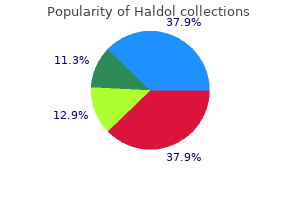
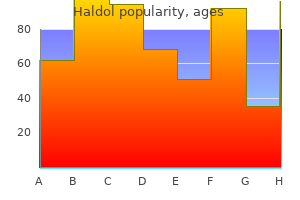
Buy haldol cheap
Bile acids recycle 20 to 30 times per day via the enterohepatic circulation and use specific transmembrane transporters at apical and basolateral domains of hepatocyte plasma membrane medicine lake california order 5mg haldol otc, as well as intracellular binding proteins. Fatty acids may be taken up by hepatocytes by passive diffusion or via fatty acid transport proteins in the sinusoidal domain of the cell membrane. It binds ligands at the cell surface, after which the ligand-receptor complex is internalized via the classic endocytotic pathway. Subsequently, the ligand is delivered to lysosomes for degradation and the receptor returns to the surface. Chylomicron remnants are removed from the circulation exclusively by the liver, probably because these large complexes can penetrate the unique sinusoidal vascular space. Mechanisms and functional features of polarized membrane traffic in epithelial and hepatic cells. Role of differentiation of liver sinusoidal endothelial cells in progression and regression of hepatic fibrosis in rats. Derangement of Lipid Metabolism in Liver Disease the most common lipid abnormality in patients with chronic liver disease is hypertriglyceridemia (plasma levels of 250 to 500 mg/dL), which is found in patients with alcoholic or viral liver disease and tends to resolve when the liver disease improves. The serum cholesterol level may be a useful prognostic marker in patients with noncholestatic liver diseases. The hepatocyte plasma membrane: Organization, differentiation, biogenesis and turnover. Three-dimensional organization of rat hepatocyte cytoskeleton: Relation to the asialoglycoprotein endocytosis pathway. Control by signaling modulators of the sorting of canalicular transporters in rat hepatocyte couplets: Role of the cytoskeleton. The catalog of human cytokeratins: Patterns of expression in normal epithelia, tumors and cultured cells. The role of actin filaments and microtubules in hepatocyte spheroid self-assembly. Mr 46,000 mannose 6-phosphate specific receptor: Its role in targeting of lysosomal enzymes. Sorting of membrane components from endosomes and subsequent recycling to the cell surface occurs by a bulk flow process. Delivery of ligands from sorting endosomes to late endosomes occurs by maturation of sorting endosomes. Structure and function of submitochondrial particles completely resolved with respect to coupling factor. Energy transduction by coupling of proton translocation to electron transfer by the cytochrome bc1 complex. Membrane and secretory proteins are transported from the Golgi complex to the sinusoidal plasmalemma of hepatocytes by distinct vesicular carriers. The transcytotic pathway of an apical plasma membrane protein (B10) in hepatocytes is similar to that of IgA and occurs via a tubular pericentriolar compartment. Cellular adhesion molecules: Regulation and functional significance in the pathogenesis of liver diseases. The mitochondrial permeability transition in cell death: A common mechanism in necrosis, apoptosis and autophagy. Autophagy as a stress-response and quality-control mechanism: Implications for cell injury and human disease. Secretory versus degradative autophagy: Unconventional secretion of inflammatory mediators. Autophagy induction favours the generation and maturation of the Coxiella replicative vacuoles. Autophagy releases lipid that promotes fibrogenesis by activated hepatic stellate cells in mice and in human tissues. Loss of macroautophagy promotes or prevents fibroblast apoptosis depending on the death stimulus. Muscle protein breakdown and the critical role of the ubiquitin-proteasome pathway in normal and disease states. The ubiquitin pathway of protein degradation and proteolysis of ubiquitin-protein conjugates. Upper intestinal lipids trigger a gut-brain-liver axis to regulate glucose production. Free fatty acidinduced beta-cell defects are dependent on uncoupling protein 2 expression. Mammalian facilitative glucose transporter family: Structure and molecular regulation. Glucokinase as glucose sensor and metabolic signal generator in pancreatic beta-cells and hepatocytes. Role of ApoCs in lipoprotein metabolism: Functional differences between ApoC1, ApoC2, and ApoC3. Remnant lipoprotein metabolism: Key pathways involving cell-surface heparan sulfate proteoglycans and apolipoprotein E. Plasma lipid transfer proteins, high-density lipoproteins, and reverse cholesterol transport. Molecular mechanisms of hepatic bile salt transport from sinusoidal blood into bile. Cell and molecular biology of the assembly and secretion of apolipoprotein B-containing lipoproteins by the liver. The low-density lipoprotein receptor gene family: multiple roles in lipid metabolism. Serum lipid and lipoprotein patterns in patients with liver cirrhosis and chronic active hepatitis. When appropriately ordered and interpreted, serum biochemical tests, the so-called "liver function tests" or "liver chemistries," can be useful in the evaluation and management of patients with liver disorders. The term liver biochemical tests is preferable to liver function tests because the most commonly used tests-the aminotransferases and alkaline phosphatase- do not measure a known function of the liver. These tests have the potential to identify liver disease, distinguish among types of liver disorders, gauge the severity and progression of liver dysfunction, and monitor response to therapy. Furthermore, considered individually, these tests lack sensitivity and specificity for liver injury; a battery of tests must be used to evaluate the liver. Interpretation of these results in concert with careful history taking and a physical examination may suggest a specific type of liver injury, thereby allowing a directed evaluation, risk assessment for surgical procedures, and estimation of prognosis. Other more specialized tests include quantitative tests of liver function and a growing number of options to assess the degree of hepatic fibrosis. About 4 mg/kg body weight of bilirubin is produced each day, nearly 80% from the breakdown of hemoglobin in senescent red blood cells and prematurely destroyed erythroid cells in the bone marrow and the remainder from the turnover of hemoproteins such as myoglobin and cytochromes distributed throughout the body. Biliverdin is then converted to bilirubin by the cytosolic enzyme biliverdin reductase. Bilirubin formed in the reticuloendothelium is lipid soluble and virtually insoluble in water. The process is initiated by reversible, noncovalent binding to albumin, which has both high-affinity and lower-affinity binding sites for unconjugated bilirubin. The unconjugated bilirubinalbumin complex passes readily through the fenestrations in the endothelium lining the hepatic sinusoids into the space of Disse, where the bilirubin dissociates from albumin and is taken up by hepatocytes via a protein-mediated, facilitated process, possibly mediated by a liver-specific organic anion transport protein. After entering the hepatocyte, unconjugated bilirubin is bound in the cytosol to a number of proteins, including proteins in the glutathione S-transferase superfamily. Once in the bile, conjugated bilirubin passes undisturbed until it reaches the distal ileum and colon, where bacteria containing -glucuronidases hydrolyze conjugated bilirubin to unconjugated bilirubin, which is further reduced by bacteria to colorless urobilinogen. Unconjugated bilirubin is never found in urine because in the serum it is bound to albumin and not filtered by the glomerulus. The presence of bilirubin in urine indicates conjugated hyperbilirubinemia and hepatobiliary disease. The magnitude and duration of hyperbilirubinemia have not been critically assessed as prognostic markers.
Discount haldol 10 mg with mastercard
This nutrient-focused assessment of small intestinal function can be combined with the H2 lactulose breath test to measure orocecal transit time as well symptoms gallstones buy haldol 1.5 mg fast delivery. The more familiar visual and anatomic scintigraphic measurement of small intestinal transit is also widely available. The major difficulty with these studies is the lack of a reliable anatomic landmark for the cecum. Either the cecum is defined arbitrarily as the right iliac fossa and a skin marker is used, or it is considered retrospectively as the area in which radioisotope accumulates. Two approaches are used to report the scintigraphic orocecal transit time: in the simpler approach, the time of first appearance of isotope in the cecum is given; in the other, the initial activity of the radiolabeled meal is quantified in the stomach, and the orocecal transit time is reported as the time taken for 50% of this initial gastric activity to reach the cecum. Values obtained vary depending on which of these methods is used, and each laboratory should set its own normal range. Manometry allows recognition of some abnormal patterns of pressure over time at individual recording points, but no studies have yet performed a critical evaluation of the best spacing of pressure recording points and of diagnostic criteria for abnormal pressure patterns to distinguish between health and disease. This lack of specific criteria reflects the limited understanding of the relationship between small intestinal intraluminal time-space pressure patterning and the achievement of mixing and propulsion within the small intestine. Because of practical limitations, one must choose between high spatial resolution over a short segment and lower spatial resolution over a longer segment of intestine. Both approaches are likely to be necessary in achieving an accurate understanding of small intestinal motor physiology, perhaps in conjunction with a technique to assess wall motion or intraluminal flow. Multiple Intraluminal Impedance Recording assemblies can be used to measure impedance in humans in much the same fashion as manometry. Because the small intestine is not all within 1 plane, however, it cannot at present be viewed routinely all at once. Because it is also an anatomic imaging technique, it has a substantial advantage over other techniques of being able to offer additional information in the assessment of patients with suspected small intestinal motility problems. Wall thickening, fibrosis, inflammatory changes, and stenoses all can be revealed, and this information can help with directing diagnosis and even therapy. Fluoroscopy is insensitive for detecting abnormal nutrient absorption and measuring transit time. Clinical fluoroscopy is limited by the necessarily short observation times because of concern with radiation exposure; therefore, only gross disturbances of motor activity may be detected. Once a substantial amount of contrast has entered the small intestine, the usefulness of fluoroscopy is reduced further because overlying loops of bowel hinder interpretation of the movement of contrast. Manometry Manometry of the small intestine gives direct measurement of the forces that are applied to luminal contents as a result of motor function. Manometry can be performed over hours or even days and over long or short segments; it is capable of excellent spatial resolution, although it has major practical limitations. Because not every slow wave leads to a contraction, however, contractions do not always travel at this maximal rate. From animal data and some human studies at high spatial resolution, it is known that a large portion of contractions travel along the small intestine rather than remaining static, although most contractions are limited to only a few centimeters in extent. Schematic representation of the relationship among slow waves, spike bursts, and muscle contraction. Top tracing is from an intracellular electrode in the muscle; middle tracing is from an extracellular electrode; and bottom tracing shows muscle tension. The cyclical fluctuation in membrane potential in the top tracing is the slow wave. When spike bursts are superimposed on the peak of the slow wave, the muscle depolarizes, and contraction occurs. Ascending excitation refers to the contraction that occurs proximal (orad) to a stimulus, and descending inhibition refers to the inhibition of motor activity that occurs distal to a stimulus. These 2 patterns are thought to be responsible for peristalsis and retroperistalsis when they travel in a coordinated fashion along the intestine. Recordings of human small intestinal motility show isolated (stationary) phasic contractions, but often, spatial patterns are more complex. The limited spatial resolution of many recording techniques can lead to over-reporting of the fraction of stationary contractions. The motor pattern is determined by the presence or absence of a significant amount of nutrient within the small intestine. Despite a large number of studies on fasting motility, few studies have been performed on human postprandial small intestinal motility; this paucity probably exists because of the difficulty in knowing which aspects of postprandial motility to study, in contrast to fasting motility, which has an easily recognized cyclic pattern and thus easily studied parameters. The fed motor pattern ensures transit of small intestinal contents at a rate consistent with normal digestion and absorption. The fasting motor pattern is less involved with orderly luminal transport and is thought to serve important roles in clearing the upper intestine of solid residues, which otherwise can accumulate and form bezoars; in maintaining relative sterility of the small intestine by keeping it empty; and in preventing net orad migration of colonic bacteria. Smooth muscle contractions can be tonic or phasic, but common usage has labeled tonic contractions as tone and phasic motor events as contractions. Small intestinal electrical recordings reveal continuous cyclical oscillations in electrical potential, referred to as the slow wave, basic electrical rhythm, or pacesetter potential. In humans, the slow-wave frequency decreases from a peak of 12 per minute in the duodenum to approximately 7 per minute in the distal ileum. The region-specific frequency of the slow wave thus controls small intestinal rhythmicity by determining the timing and maximal frequency of contractions. The rapid increases in free intracellular calcium, or calcium transients, that underlie smooth muscle contraction can be visualized with fluorescence techniques and appear to spread in a coordinated fashion over an area of smooth muscle and to extend over variable distances of the bowel wall. These calcium transients are extinguished by collision with each other or by encountering locally refractory regions. When a slow wave results in contraction, the propagation of the slow wave along the small intestine also leads to the contraction propagating along the small intestine. Hyperosmolar contents and pH changes probably are sensed by receptors in the mucosa, whereas distention is signaled by receptors in the muscle. In the normal course of events, these stimuli occur concurrently with the presence of nutrients, and the significance of their isolated effects in healthy subjects is unclear. The small intestine also exerts negative feedback control on the rate of gastric emptying through neural and humoral means. This negative feedback is achieved by the release of neural signals and intestinal hormones that suppress phasic gastric motor activity, relax the gastric fundus, and increase tonic and phasic pyloric pressures subsequent to mucosal sensing of small intestinal nutrients. The small intestine, in particular the duodenum, is also thought to offer direct mechanical resistance to gastric emptying by acting as a capacitance resistor68 and by re-augmenting gastric contents as a result of duodenogastric reflux. Walter Cannon61,70 observed both localized contractions over short segments of intestine in association with to-and-fro movement of contents and intermittent episodes of propulsion of contents over greater distances caused by aborally traveling waves of peristalsis. In the fed state, the most common pattern of wall motion consisted of localized circular contractions that recurrently divided and formed short columns of chyme into new aliquots by temporary local occlusion of the lumen over distances of less than 1 to 2 cm, this pattern being labeled rhythmic segmentation. During small intestinal nutrient loading, peristalsis was noted to have 2 forms: 1 was a slow advance of chyme over short distances in association with segmentation, and the other was a rapid transit of chyme over longer distances, sometimes several loops, of the small intestine. Manometric tracings that demonstrate small intestinal motility in fasting (top) and fed (bottom) state. Moreover, the sensing of intraluminal nutrients is relatively complex because different types of nutrients, or variable amounts of the same nutrient, generate recognizably different motor responses. In the absence of sufficient proximal small intestinal nutrient stimulation, the fasting motor pattern re-emerges 4 to 6 hours after a meal. Transit Time Observations the small intestinal transit time for a meal varies greatly according to the amount and nature of what is consumed, because both caloric content and physical form of a meal determine the gastric emptying rate and the rate of transport along the intestine. As assessed by lactulose breath testing, however, orocecal transit time can be as rapid as about 70 minutes with low nutrient loads. A systematic evaluation of the optimal conditions for nutrient loading is much needed to reveal abnormal small intestinal motor function, using transit studies. Most small intestinal motility data are quite limited in spatial resolution because of the length of the small intestine. Nevertheless, most phasic pressures (pressure wave sequences) are thought to travel only a short distance49,50 and probably represent the mixing and segmenting contractions noted in earlier radiologic studies. This absence is associated clinically with stasis of small intestinal contents, malabsorption, and small intestinal bacterial overgrowth. Fortunately, like other organs, the small intestine has a substantial reserve capacity and copes with many insults, including infection, resection, inflammation, and denervation, before clinical problems become manifest. The most important diseases and clinical settings associated with abnormal small intestinal motility are listed in Table 99-1. Because these disorders are covered elsewhere in this book, they are mentioned here only with regard to their associated small intestinal motor disturbances.
Purchase haldol in united states online
The presence of amino acids in the lumen inhibits peptide hydrolysis (product inhibition) medications used to treat bipolar haldol 1.5 mg cheap, whereas luminal glucose and luminal acidification each inhibit amino acid and peptide absorption. The 1762 Section X SmallandLargeIntestine tripeptide transporter is more specific for the d-isomer acidic or basic amino acids and for short side chains. Affinity is also greater for dipeptides than for tripeptides, at least in peptides that contain glycine. The transporter for peptides is not dependent on sodium, but co-transport with protons instead. In humans it is expressed in the duodenum, jejunum, and ileum but not in the esophagus, stomach, or colon. The human protein consists of 708 amino acids, with a predicted core molecular size of 79 kd that contains 12 transmembrane domains. It recognizes a variety of neutral, anionic, and cationic dipeptides as substrates, which explains the broad substrate specificity of the intestinal peptide transport system. These enzymes convert most of the absorbed oligopeptides to amino acids that are either used by the absorbing cells or are released into the portal circulation via the amino acid transporters located on the basolateral membrane of these cells. The apparent change in protein expression appears to be increased trafficking from a preformed cytoplasmic pool to the apical membrane. The transport process uses a transmembrane H+ gradient rather than a transmembrane electrochemical Na+ gradient as the driving force. The mechanism of the transport process is a simultaneous translocation of H+ and peptide substrate involving a single H+ binding site on the protein. In adults, these are situated on villus enterocytes and involve carrier-mediated active transport or facilitated diffusion processes, which are typically dependent on the Na+ gradient as the driving force; a small proportion may be absorbed by simple diffusion, independent of any ion gradient. In addition to their stereospecificity (l-amino acids are preferentially transported), amino acid transporters exhibit broad/overlapping substrate specificity; consequently there has been some difficulty in defining the number and types of transporters. Several amino acids utilize a number of different transport systems (Table 102-6). On the basis of kinetic studies, at least 4 active processes for transport of neutral amino acids across the apical cell membrane have been identified. Separate sodium-dependent, active transport processes for basic and acidic amino acids also have been demonstrated, and there is some evidence to suggest that facilitated diffusion of these types of amino acids also occurs, although this is likely to be a minor pathway. Genomic advances have allowed most mammalian amino acid transport functions to be attributed to specific gene products: at least 52 amino acid transporter-related gene products are grouped within 12 solute carrier families, with their own new nomenclature. This high-capacity imino acid carrier has been localized to the small intestinal luminal membrane and transports imino and amino acids (glycine, praline, alanine, taurine). This transporter is defective in the inherited amino acid transport defect known as dicarboxylic aciduria. The acid microenvironment generated by the Na+/H+ exchanger provides an electrochemical proton gradient that drives amino acids to the cytosol. The B0,+ is a Na+-independent transport system that recognizes neutral and cationic amino acids in addition to the disulfide amino acid cystine. It is a heterodimer consisting of a light and heavy chain, with the genes responsible for each chain found on chromosomes 2 and 19, respectively; this transporter is defective in cystinuria. Villus enterocytes normally receive the amino acids necessary for production of their own protein from luminal nutrients; crypt cells obtain their supply from the portal circulation. Of all the amino acids, glutamine appears to be a unique and major source of energy for enterocytes; ammonia is an important metabolic by-product of this process. Active uptake of glutamine at the basolateral membrane, as well as via apical membrane processes, is therefore of particular importance. The amino acid transport systems in the basolateral membrane function to export amino acids from the enterocytes into the portal circulation during feeding. They also participate in the import of amino acids from the portal circulation into the enterocyte for cellular metabolism when amino acids are not available from the intestinal lumen, such as between meals. System y+L is the amino acid exchanger that permits Na+-independent efflux of cationic amino acids from intestinal cells into the blood, coupled to the Na+-dependent influx of neutral amino acids from the blood into intestinal cells. System A is a Na+coupled transport system for neutral amino acids, including glutamine, that plays a role in the entry of amino acids from the blood into intestinal cells for cellular metabolism. A somewhat surprising finding is that digestion of protein continues into the ileum, with about 40% of ingested protein undergoing transport in this segment of small intestine. Oro-sensory perception of dietary lipids: New insights into the fat taste transduction. Dietary fructose: Implications for dysregulation of energy homeostasis and lipid/carbohydrate metabolism. Plasma triglyceride increase after oral fat load in malabsorption during early childhood. Lipase and pepsin activity in the gastric mucosa of infants, children, and adults. Secretion and contribution to lipolysis of gastric and pancreatic lipases during a test meal in humans. Effect of infusion of nutrient solutions into the ileum on gastrointestinal transit and plasma levels of neurotensin and enteroglucagon. Neuroendocrinology of the pancreas; role of brain-gut axis in pancreatic secretion. Relationship to bile acid pool size and cholesterol saturation of bile in gallstone and control subjects. Sugar-sweetened beverages, obesity, type 2 diabetes mellitus, and cardiovascular disease risk. Taste, olfactory and food texture reward processing in the brain and the control of appetite. Genetic influences on oral fat perception and preference: Presented at the symposium "The Taste for Fat: New Discoveries on the Role of Fat in Sensory Perception, Metabolism, Sensory Pleasure and Beyond" held at the Institute of Food Technologists 2011 Annual Meeting, New Orleans, La. Recent fat intake modulates fat taste sensitivity in lean and overweight subjects. Length and site of the small intestine exposed to fat influences hunger and food intake. A possible physiological function of pancreatic pro-colipase activation peptide in appetite regulation. The Arg92Cys colipase polymorphism impairs function and secretion by increasing protein misfolding. The intraluminal phase of fat digestion in man: the lipid content of the micellar and oil phases of intestinal content obtained during fat digestion and absorption. Visualization by freeze fracture, in vitro and in vivo, of the products of fat digestion. Mechanism of intestinal fatty acid uptake in the rat: the role of an acidic microclimate. The mechanism whereby bile acid micelles increase the rate of fatty acid and cholesterol uptake into the intestinal mucosal cell. Mechanism of cellular uptake of long-chain fatty acids: Do we need cellular proteins Uptake of micellar long-chain fatty acid and sn-2-monoacylglycerol into human intestinal Caco-2 cells exhibits characteristics of protein-mediated transport. Membrane fatty acid transporters as regulators of lipid metabolism: Implications for metabolic disease. Keratinocyte-specific expression of fatty acid transport protein 4 rescues the wrinkle-free phenotype in Slc27a4/Fatp4 mutant mice. Caveolin targeting to late endosome/lysosomal membranes is induced by perturbations of lysosomal pH and cholesterol content. Molecular cloning and developmental expression of the caveolin gene family in the amphibian Xenopus laevis. Altered mitochondrial function and metabolic inflexibility associated with loss of caveolin-1. Metabolism of apical versus basolateral sn-2-monoacylglycerol and fatty acids in rodent small intestine. Flotillins play an essential role in Niemann-Pick C1-like 1-mediated cholesterol uptake. Evidence for multiple complementary pathways for efficient cholesterol absorption in mice.
Buy haldol toronto
Impaired endothelial nitric oxide synthase activity associated with enhanced caveolin binding in experimental liver cirrhosis medications jamaica 1.5mg haldol free shipping. Sinusoidal remodeling and angiogenesis: A new function for the liver-specific pericyte Platelet-derived growth factor signaling through ephrin-b2 regulates hepatic vascular structure and function. Nitrovasodilators inhibit platelet-derived growth factor-induced proliferation and migration of activated human hepatic stellate cells. Low doses of isosorbide mononitrate attenuate the postprandial increase in portal pressure in patients with cirrhosis. A liverspecific nitric oxide donor improves the intra-hepatic vascular response to both portal blood flow increase and methoxamine in cirrhotic rats. Bioactivation of nitroglycerin and vasomotor response to nitric oxide are impaired in cirrhotic rat livers. Endothelin induced contractility of stellate cells from normal and cirrhotic rat liver: Implications for regulation of portal pressure and resistance. Endothelin 1 is overexpressed in human cirrhotic liver and exerts multiple effects on activated hepatic stellate cells. Endothelin-1 modulates intrahepatic resistance in a rat model of noncirrhotic portal hypertension. Cellular localization of endothelin-1 and increased production in liver injury in the rat: Potential for autocrine and paracrine effects on stellate cells. Hepatic tissue endothelin-1 levels in chronic liver disease correlate with disease severity and ascites. The therapeutic potential of endothelin-1 receptor antagonists and endothelin-converting enzyme inhibitors on the cardiovascular system. Somatostatin suppresses endothelin-1 induced rat hepatic stellate cell contraction via somatostatin receptor subtype 1. Hemodynamic studies in longand short-term portal hypertensive rats: the relation to systemic glucagon levels. Role of endothelium in the abnormal response of mesenteric vessels in rats with portal hypertension and liver cirrhosis. Nitric oxide mediates hyporeactivity to vasopressors in mesenteric vessels of portal hypertensive rats. In vitro hyporeactivity to methoxamine in portal hypertensive rats: Reversal by nitric oxide blockade. Role of nitric oxide in the in vitro splanchnic vascular hyporeactivity in ascitic cirrhotic rats. Increased endothelial nitric oxide synthase activity in the hyperemic vessels of portal hypertensive rats. Hsp90 regulation of endothelial nitric oxide synthase contributes to vascular control in portal hypertension. Increased nitric oxide synthase expression in arterial vessels of cirrhotic rats with ascites. A randomized, double-blinded, placebo-controlled multicenter trial of etanercept in the treatment of alcoholic hepatitis. The effect of selective intestinal decontamination on the hyperdynamic circulatory state in cirrhosis. Hemodynamic, renal, and endocrine effects of acute inhibition of nitric oxide synthase in compensated cirrhosis. Gastric antral ectasia in cirrhotic patients: Absence of relation with portal hypertension. Endogenous cannabinoids: A new system involved in the homeostasis of arterial pressure in experimental cirrhosis in the rat. Increased heme oxygenase activity in splanchnic organs from portal hypertensive rats: Role in modulating mesenteric vascular reactivity. Enhanced cyclooxygenase-1 expression within the superior mesenteric artery of portal hypertensive rats: Role in the hyperdynamic circulation. Vasodilator responses to nitric oxide are enhanced in mesenteric arteries of portal hypertensive rats. Nitric oxidedependent and -independent vascular hyporeactivity in mesenteric arteries of portal hypertensive rats. Changes in protein kinase C isoforms in association with vascular hyporeactivity in cirrhotic rat aortas. Desensitization to the effects of intravenous octreotide in cirrhotic patients with portal hypertension. Randomized controlled trial of carvedilol versus variceal band ligation for the prevention of the first variceal bleed. A study in 230 patients with esophageal and/or gastric varices using portal vein catheterization. Spontaneous (natural) splenoadrenorenal shunts in extrahepatic portal venous obstruction: A series of 20 cases. Nitric oxide synthase 3-dependent vascular remodeling and circulatory dysfunction in cirrhosis. In vivo angiogenesis in normal and portal hypertensive rats: Role of basic fibroblast growth factor and nitric oxide. Administration of N-omega-nitro-L-arginine ameliorates portal-systemic shunting in portal-hypertensive rats. Pharmacology of portal-systemic collaterals in portal hypertensive rats: Role of endothelium. Effects of vasopressin on portal-systemic collaterals in portal hypertensive rats: Role of nitric oxide and prostaglandin. Effects of somatostatin and octreotide on portal-systemic collaterals in portal hypertensive rats. Chronic inhibition of nitric oxide increases the collateral vascular responsiveness to vasopressin in portal hypertensive rats. Octreotide ameliorates the increase in collateral blood flow during postprandial hyperemia in portal hypertensive rats. Endothelin-1 induces vasoconstriction on portal-systemic collaterals of portal hypertensive rats. Increased intraabdominal pressure increases pressure, volume, and wall tension in esophageal varices. An estimation of portal venous pressure by occlusive catheterization of a hepatic venule. Portal hypertension and primary biliary cirrhosis: Effect of long-term ursodeoxycholic acid treatment. Right atrial pressure is not adequate to calculate portal pressure gradient in cirrhosis: A clinical-hemodynamic correlation study. Summary of an American Association for the Study of Liver Diseases and European Association for the Study of the Liver singletopic conference. Predictive value of the variceal pressure response to continued pharmacological therapy in patients with cirrhosis and portal hypertension. Endoscopic measurement of variceal pressure in cirrhosis: Correlation of portal pressure and variceal hemorrhage. Endoscopic measurement of variceal pressure during hemorrhage from esophageal varices. Platelet count is not a predictor of the presence or development of gastroesophageal varices in cirrhosis. Esophageal capsule endoscopy for screening and surveillance of esophageal varices in patients with portal hypertension. Prediction of the first variceal hemorrhage in patients with cirrhosis of the liver and esophageal varices. Predictive value of ultrasonography in the screening of non-ascitic cirrhotic patients with large varices. Which patients with cirrhosis should undergo endoscopic screening for esophageal varices detection Transient elastography for diagnosis of portal hypertension in liver cirrhosis: Is there still a role for hepatic venous pressure gradient measurement Elastography, spleen size, and platelet count identify portal hypertension in patients with compensated cirrhosis. Daily variation of azygos and portal blood flow and the effect of propranolol administration once an evening in cirrhotics. Endoscopic assessment of variceal volume and wall tension in cirrhotic patients: Effects of pharmacological therapy.
Purchase 1.5mg haldol free shipping
In the latent and chronic phases medicine over the counter generic haldol 5mg on-line, a definitive diagnosis is based on the detection of eggs in stool, duodenal aspirate specimens, or bile. Hepatic histologic findings include necrosis and granulomas with eosinophilic infiltrates and Charcot-Leyden crystals. Eosinophilic abscesses, epithelial hyperplasia of the bile ducts, and periportal fibrosis may be seen. Other medications that are potentially efficacious are bithionol and nitazoxanide. Cholangiocarcinoma should be suspected in infected persons with weight loss, jaundice, epigastric pain, or an abdominal mass (see Chapter 69). The diagnosis of clonorchiasis or opisthorchiasis is made by detection of characteristic fluke eggs in the stool, except late in the disease when biliary obstruction has supervened. Endoscopic or intraoperative cholangiography reveals slender, uniform filling defects within intrahepatic ducts that are alternately dilated and strictured, mimicking sclerosing cholangitis. Serologic methods of diagnosis cannot distinguish between past or current infection. All patients with clonorchiasis or opisthorchiasis should receive praziquantel, which is uniformly effective in a dose of 75 mg/kg in 3 divided doses over 1 day. When the burden of infecting organisms is high, the dead flukes and surrounding debris or stones may cause biliary obstruction, necessitating endoscopic or surgical drainage. Echinococcus multilocularis is distributed in northern North America and Eurasia, whereas Echinococcus vogeli is found in scattered areas of Central and Latin America. Infection occurs when humans eat vegetables contaminated by dog feces that contain embryonated eggs. The eggs hatch in the small intestine and liberate oncospheres that penetrate the mucosa and migrate via vessels or lymphatics to distant sites. The liver is the most common destination (70%), followed by the lungs (20%), kidney, spleen, brain, and bone. In these organs, a hydatid Clonorchiasis and Opisthorchiasis Clonorchis sinensis, Opisthorchis viverrini, and Opisthorchis felineus are trematodes of the family Opisthorchiidae. Eggs are passed in the feces into fresh water, consumed by snails, and hatch as free-swimming cercariae, which seek and penetrate fish or crayfish and encyst in skin or muscle as metacercariae. The metacercariae excyst in the small intestine and migrate into the ampulla of Vater and bile ducts, where they mature into adult flukes. If the worm burden in the bile ducts is heavy, chronic or intermittent biliary obstruction can ensue, with frequent cholelithiasis, cholecystitis, jaundice, and, ultimately, recurrent pyogenic cholangitis (see Chapter 68). Liver biochemical test results, especially serum alkaline phosphatase and bilirubin levels, are elevated. The cyst wall contains 3 layers: an outer adventitial layer, which is host-derived and can calcify, and intermediate acellular and inner germinal layers, which are worm-derived. A protoscolex is produced asexually within small secondary cysts that develop from the inner layer. Rupture of the hydatid cyst releases the viable protoscolices, which set up daughter cysts in secondary sites. The adult Echinococcus tapeworm consists of a scolex, which contains a rostellum with 20 to 50 hooklets and 4 suckers, a neck, and an immature, mature, and gravid proglottid. Dogs acquire the infection by consuming organs of sheep, cattle, or other livestock bearing the hydatid cyst. If the cysts grow large enough, they may rupture spontaneously or after trauma into the lungs, thereby leading to dyspnea and hemoptysis. More extensive rupture into the peritoneum or lungs may lead to a lifethreatening anaphylactic reaction to the cyst contents. Rupture into the biliary tract can cause cholangitis and obstruction; marked eosinophilia may be present. Superinfection of the hepatic cysts can lead to pyogenic liver abscesses in up to 20% of patients with hepatic disease. Rare complications of hydatid cysts or cyst rupture include pancreatitis, portal hypertension, Budd-Chiari syndrome, and rupture into the pericardial sac. Alveolar hydatid disease is the term applied to hepatic nodules that appear on microscopy as alveoli-like microvesicles. Infection of bile ducts and vessels and necrosis of parenchyma may result in cholangitis, liver abscess, sepsis, portal hypertension, hepatic vein occlusion, and biliary cirrhosis. Unfortunately, infection generally is not diagnosed until the lesions are inoperable because of extensive invasion or distant metastatic disease, and mortality rates are high, approaching 90%. A history of exposure in a patient with hepatomegaly and an abdominal mass is highly suggestive of hepatic echinococcosis, but the most important diagnostic tools are imaging and serology. Ring-like calcifications in up to one fourth of hepatic cysts are visible on plain abdominal films in patients infected with E. Percutaneous aspiration of the cyst had traditionally been discouraged because of concern about anaphylactic reactions. Encouraging reports, however, suggest that under carefully controlled conditions, with use of thin needles and concomitant antihelminthic therapy, percutaneous aspiration for diagnosis and therapy may be safe. In the past, accessible cysts in younger persons were always treated surgically, and surgery is still considered the preferred treatment in many cases. Successful approaches have included cystectomy, endocystectomy, omentoplasty, and marsupialization. Promising data indicate that careful percutaneous drainage is a safe and effective alternative to surgery for the treatment of complicated cysts. The decision between surgical and nonsurgical techniques depends on the extent and type of lesions. In such cases, palliative drainage procedures or long-term treatment with albendazole or other benzimidazole carbamates may prolong survival. Most disseminated infections occur in leukemic patients undergoing high-dose chemotherapy and become clinically evident during the period of recovery from severe neutropenia. In several series, hepatic candidiasis was present in 51% to 91% of predominantly leukemic patients with disseminated candidiasis. In either focal or disseminated candidiasis involving the liver, clinical features include fever, abdominal pain and distention, nausea, vomiting, diarrhea, and tender hepatomegaly. The serum alkaline phosphatase level is almost invariably elevated, with varying elevations in serum aminotransferase and bilirubin levels. The liver can be invaded in both acute and chronic progressive disseminated histoplasmosis. Fever, oropharyngeal ulcers, hepatomegaly, and splenomegaly may be present in patients with chronic disease. Yeast forms can be identified in liver biopsy specimens with standard H&E staining. The silver methenamine method is superior for detecting yeast forms in areas of caseating necrosis or in granulomas. The organism is difficult to culture and almost never grows from biopsy specimens. Serologic testing for complement-fixing antibodies is therefore helpful in confirming the diagnosis. In immunocompromised persons who may not be capable of mounting an antibody response, detection of H. This presentation is uncommon today as a result of earlier diagnosis and effective antibiotic therapy. Most cases now are cryptogenic or occur in older men with underlying biliary tract disease. Infection may spread to the liver from the bile duct, along a penetrating vessel, or from an adjacent septic focus (including pylephlebitis). Pyogenic liver abscess may arise as a late complication of endoscopic sphincterotomy for bile duct stones or within 3 to 6 weeks of a surgical biliary-intestinal anastomosis. The risk of liver abscess may be increased in patients with underlying diabetes mellitus or cirrhosis. Oral flora have been proposed to be a potential source in such cases, particularly in patients (often alcoholics) with severe periodontal disease. After the introduction of antibiotics, the presentation of pyogenic liver abscess became less acute. Multiple abscesses are typical when biliary disease is the source and are associated with a more acute systemic presentation, often with sepsis and shock, than is the case with solitary abscesses.
Purchase haldol toronto
Distinguishing the tumor from metastatic adenocarcinoma may be difficult medications an 627 buy haldol overnight, and some experts have advocated assuming that an adenocarcinoma in the liver is cholangiocarcinoma if no primary tumor can be found elsewhere. It occurs almost exclusively in the first 3 years of life; boys are affected twice as often as girls. Sporadic hepatoblastoma is not associated with any known environmental risk factor, and its pathogenesis is unclear. Distant metastases are evident, usually in the lung, in 20% of patients at the initial visit. Liver transplantation plays an increasing role because of technical success with live-donor and splitliver transplantation. Angiosarcoma Epidemiology Although rare, angiosarcoma is the most common malignant mesenchymal tumor of the liver. Pulmonary metastases and, rarely, mottled calcification in the tumor may be seen on plain radiography. In early reports, the tumor became evident approximately 20 years after exposure to thorium dioxide (see Chapter 89). Angiosarcomas have occurred after exposures of 11 to 37 years (or after shorter periods with a heavy initial exposure). Pathology Hepatoblastomas are the malignant derivatives of incompletely differentiated hepatocyte precursors. Their constituents are diverse, reflecting both the multipotentiality of their mesodermal origin and the progressive stages of embryonic and fetal development. Pathologists separate hepatoblastomas into subtypes based on their histopathologic appearance, each with a prognosis that can be risk stratified. The pure fetal type has an excellent prognosis, whereas the aggressive small-cell undifferentiated tumor has the worst prognosis and is usually assigned the most intensive therapeutic interventions. They vary in color, ranging from tan to grayishwhite, and contain foci of hemorrhage, necrosis, and calcification. Epithelial hepatoblastomas are solid, whereas tumors of the mixed variety often are separated into lobules by white bands of collagen tissue. Cells of the second type are embryonal and are less differentiated than the fetal type. Mixed hepatoblastomas contain mesenchymal tissue consisting of areas of a highly cellular primitive type of mesenchyme intimately admixed with epithelial elements. Other frequent complaints are abdominal swelling, rapidly progressing liver failure, malaise, weight loss, poor appetite, and nausea. The duration of symptoms generally ranges from 1 week to 6 months, but a few patients have had symptoms for as long as 2 years before seeking medical attention. Approximately 15% of patients present with acute hemoperitoneum following tumor rupture. If the lesion is solitary and sufficiently localized to be resectable, surgery often is curative, with 5-year survival rates as high as 75%. Encouraging results also have been obtained with liver transplantation in patients with bilobar multifocal tumors without extrahepatic extension. In patients who were exposed to thorium dioxide, radiopaque deposits of the material may be evident in the liver and spleen. The earliest microscopic change is the presence of hypertrophic sinusoidal lining cells with hyperchromatic nuclei in ill-defined loci throughout the liver. With progression of the lesion, sinusoidal dilatation and disruption of hepatic plates occur, and the malignant cells become supported by collagen tissue. Enlarging vascular spaces lined by malignant cells cause the tumor to become cavernous. The malignant endothelial cells usually are multilayered and may project into the cavity in intricate fronds and tufts supported by fibrous tissue. Nuclei are hyperchromatic and vary greatly in size and shape; some cells are multinucleated. Foci of extramedullary hematopoiesis are common, and invasion of the portal and central veins occurs in most cases. Histologically, they are characterized by the presence of dendritic and epithelioid cells that contain vacuoles, representing intracellular lumina. Complications and Prognosis the tumor has low-grade malignant potential and must be distinguished from hemangiosarcoma, because it has a much better prognosis if treated appropriately and aggressively. Epithelioid hemangioendothelioma may metastasize, both within and beyond the liver. Treatment the primary treatment modality for epithelioid hemangioendothelioma is surgical, including resection or liver transplantation. Transplantation appears to be effective for this tumor, even in the presence of advanced or even metastatic disease. Complications and Prognosis Hepatic angiosarcomas grow rapidly, and the prognosis is poor; death ensues within 6 months. Even when surgery is undertaken, the patient commonly survives only 1 to 3 years, although long-term survival may be achieved in the few patients with a solitary tumor. Hepatic Metastases Epidemiology and Etiology the liver is the most frequent target for metastatic spread of tumors. Hepatic metastases occur in 40% to 50% of adult patients with extrahepatic primary malignancies. Outside this distribution, tumors of the lung and breast are the most common origins of hepatic metastases. Epithelioid Hemangioendothelioma Epidemiology Epithelioid hemangioendothelioma is a rare tumor with an estimated incidence of less than 0. Clinical Features Patients typically present with nonspecific symptoms such as abdominal pain and weight loss. Diagnosis Imaging studies show a characteristically highly vascular mass that may infiltrate throughout the liver. Epithelioid hemangioendothelioma should be Clinical Features Symptoms resulting from hepatic metastases often are absent or overshadowed by those of the primary tumor. Occasionally, the symptoms and signs attributable to metastases are the presenting manifestations of an asymptomatic primary tumor. Jaundice, when present, is seldom attributable to replacement of hepatic tissue by metastases. Depending on the extent of the metastatic disease, the liver may be enlarged, sometimes markedly. Its surface may be irregular, and umbilicated nodules may be felt by the examiner. Other invasive methods of destroying metastases, such as ethanol injection, freezing with cryoprobes, and laser vaporization, warrant further study. Radiation therapy and intra-arterial infusion of cytotoxic drugs have limited roles. Cessation of estrogens often leads to regression of an adenoma, adding support to their role in the pathogenesis. In this setting, there is a male predominance, and the diagnosis is usually made during childhood213 (see Chapter 77). It is not clear whether liver adenomatosis is a distinct entity, but it may be more difficult to manage clinically than a single or a few adenomas because of the high number of lesions. Individual metastases may reach a large size, and with multiple metastases, the liver may be greatly enlarged. Metastases commonly are gray-white and may show scattered hemorrhages or central necrosis. The dictum that cirrhotic livers are less likely than noncirrhotic livers to harbor metastatic deposits remains to be verified. Microscopic Appearance the microscopic features, including the degree of stromal growth, of most hepatic metastases duplicate those of the tumor of origin. Metastatic deposits usually are easily delineated from the surrounding liver tissue.

Buy discount haldol 5 mg on line
Incidence is usually defined as the number of new cases of gallstones occurring in a time period divided by the population at risk of forming stones medicine just for cough order haldol 1.5mg with amex. Therefore, the determination of incidence requires that investigation for gallstones be performed at a minimum of two different times-that is, at the beginning and at the end of an interval of time. Although determining the true incidence of gallstones in a given population is not easy, a large study of the incidence of gallstones in the Danish population has been performed. Women have a higher incidence than men at ages 30 and 40, but the difference declines with increasing age. These incidence rates may reflect an interaction between genetic and environmental factors on gallstone formation in the specific populations studied because they are in accordance with estimated prevalence rates reported for Denmark and other populations. Although age, female gender, parity, obesity, and hypertriglyceridemia were associated with gallstones in the cross-sectional prevalence study of Sirmione, multivariate analysis of risk factors for the formation of gallstones in the longitudinal study identified only age and obesity as risk factors. Differences in the incidence of gallstone formation among different populations are striking, suggesting that genetic factors play a crucial role in the pathogenesis of cholesterol gallstones. Pathogenic factors are likely to be multifactorial Women Men and to vary among populations. Most relevant studies have found that the prevalence of gallstones in women ranges from 5% to 20% between the ages of 20 and 55 and from 25% to 30% after the age of 50. The prevalence of gallstones in American Pima Indians was investigated by oral cholecystography. The cross-sectional prevalence rates of gallstones were found to be highest in certain tribes of Native Americans. Other high-risk populations include Native American groups in North and South America and Scandinavians, of whom 50% develop gallstones by age 50. Within a given population, first-degree relatives of index cases of persons with gallstones are 4. Risk Factors Age and Gender Epidemiologic and clinical studies have found that cholesterol gallstones occur infrequently in childhood and adolescence, 65. Cholesterol saturation of bile is significantly higher in older adult Swedes and Chilean women than in younger controls, and age correlates positively with an increased hepatic secretion rate of biliary cholesterol. The difference between women and men begins during puberty and continues through the childbearing years because of the effects of female sex hormones10 and differences between the sexes in metabolism of cholesterol by the liver in response to estrogen. Human and animal studies have shown that estrogen increases the risk of cholesterol gallstones by augmenting hepatic secretion of biliary cholesterol, thereby leading to an increase in cholesterol saturation of bile. In addition, gallbladder motility is impaired, with a resulting increase in gallbladder volume and bile stasis. Because plasma concentrations of sex hormones, especially estrogen, increase linearly with duration of gestation, the risk of gallstone formation is high in the third trimester of pregnancy. Increasing parity is probably a risk factor for gallstones, especially in younger women. Rapid Weight Loss Rapid weight loss is a well-known risk factor for the formation of cholesterol gallstones. Gallstones also develop in 25% of patients who undergo strict dietary restriction. Furthermore, about 40% of these patients display symptoms related to gallstones within the same 6-month period. The mechanisms by which rapid weight loss causes gallstone formation include enhanced hepatic secretion of biliary cholesterol during caloric restriction, increased production of mucin by the gallbladder, and impaired gallbladder motility. The incidence of cholesterol gallstones is significantly higher in North and South American as well as European populations than in Asian and African populations. In addition, the sphincter of Oddi may fail to relax, leading to preferential flow of bile into the gallbladder. Lipid-Lowering Drugs Lipid-lowering drugs may influence the formation of gallstones because they regulate key pathways in cholesterol and bile salt metabolism. Clofibrate induces cholesterol supersaturation in bile and diminishes bile salt concentrations by reducing the activity of cholesterol 7-hydroxylase (the rate-limiting enzyme in bile salt synthesis of classical pathway) (see Chapter 64). Ezetimibe also may act as a potent biliary cholesteroldesaturating agent in patients with gallstones. Biliary Sludge Biliary sludge is a crucial intermediate stage in the pathogenesis of both cholesterol and pigment gallstones because it facilitates crystallization and agglomeration of solid platelike cholesterol monohydrate crystals, as well as precipitation of calcium bilirubinate, and ultimately develops into macroscopic stones. Octreotide the somatostatin analog octreotide increases the prevalence of gallstones when administered to patients as treatment for acromegaly, with some 28% of treated acromegalic patients forming gallstones. Acromegalic patients who are treated with octreotide display dysfunctional gallbladder motility, sluggish intestinal transit, and increased colonic deoxycholic acid formation and absorption,46 all of which facilitate formation of cholesterol gallstones. Drugs Estrogens Most but not all relevant clinical studies have shown that use of oral contraceptive steroids and conjugated estrogens in premenopausal women doubles the prevalence of cholesterol gallstones. In mice, the hepatic estrogen receptor, but not, plays a crucial role in cholesterol gallstone formation in response to estrogen. High levels of estrogen may induce gallbladder hypomotility and consequently bile stasis. Ceftriaxone the third-generation cephalosporin ceftriaxone has a long duration of action, with much of the drug excreted in the urine. Approximately 40% of the drug, however, is secreted in an unmetabolized form into bile, where its concentration reaches 100 to 200 times that of the concentration in plasma and exceeds its saturation level in bile. Once the saturation level of ceftriaxone is exceeded, it complexes with calcium to form insoluble salts, thereby resulting in formation of biliary sludge. Up to 43% of children who receive high doses of ceftriaxone (60 to 100 mg/kg/day) have been reported to form biliary sludge, and about 19% of these patients experience biliary symptoms. As a result, gallbladder bile is more lithogenic in obese than in nonobese persons, and a higher ratio of cholesterol to solubilizing lipids (bile acids and phospholipids) is observed in the former group. These alterations predispose to cholesterol crystallization and gallstone formation. Gallbladder motility is often impaired in obese persons, thereby promoting mucin secretion and accumulation, as well as cholesterol crystallization. The effect of pronucleating and antinucleating factors on cholesterol crystallization and gallstone formation warrants further investigation in gallbladder bile of obese and nonobese subjects. Protective Factors Statins Use of statins has been associated with a decreased risk of gallstone disease in 2 large case-control studies. The first study compared 27,035 patients with gallstone disease requiring cholecystectomy with 106,531 matched controls and showed a benefit to long-term statin use (>20 prescriptions filled and use of statins for >1. Similar results were observed in a population study from Denmark of 32,494 patients with gallstone disease matched with 324,925 controls. Ascorbic Acid the observation that deficiency of ascorbic acid (vitamin C) is associated with development of gallstones in guinea pigs prompted investigation of the relationship between ascorbic acid levels and gallstones in humans. Serum ascorbic acid levels have been correlated with clinical or asymptomatic gallstones in 7042 women and 6088 men who were enrolled in the Third National Health and Nutrition Examination Survey. Diabetes Mellitus Patients with diabetes mellitus have long been considered to be at increased risk of developing gallstones because hypertriglyceridemia and obesity are associated with diabetes mellitus and because gallbladder motility is often impaired in patients with diabetes mellitus. Mice with hepatic insulin resistance induced by liver-specific disruption of the insulin receptor are markedly predisposed to formation of cholesterol gallstones. It also reduces expression of the bile salt synthetic enzymes, particularly oxysterol 7-hydroxylase, thereby resulting in a lithogenic bile salt profile. Coffee In a 10-year follow up of 46,000 male health professionals, subjects who consistently drank 2 to 3 cups of regular coffee per day were approximately 40% less likely to develop symptomatic gallstones. A similar benefit to regular coffee was noted in a cohort study involving 81,000 women. These changes may also lead to formation of pigment gallstones because increased bile salt delivery to the colon enhances solubilization of unconjugated bilirubin, thereby increasing bilirubin concentrations in bile. Cholesterol accounts for up to 95% of the sterols in bile and gallstones; the remaining 5% of the sterols are cholesterol precursors and dietary sterols from plant and shellfish sources. Concentrations of cholesteryl esters are negligible in bile and account for less than 0. The major phospholipids are lecithins (phosphatidylcholines), which account for more than 95% of total phospholipids; the remainder consists of cephalins (phosphatidylethanolamines) and a trace amount of sphingomyelin. Lecithins are insoluble amphiphilic molecules with a hydrophilic zwitterionic phosphocholine head group and hydrophobic tails that include 2 long fatty acyl chains.