Order motilium 10mg without a prescription
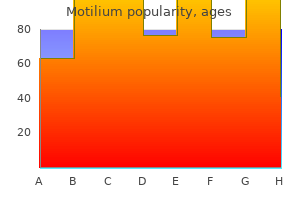
After its publication gastritis diet �������� buy motilium us, doctors from different regions of the country started to apply this method clinically. The major pattern in the practice of anesthesia was complete dependence on foreign surgeons, who could administer anesthetics, and on local and foreign nurses or nonanesthesiologists and technicians, who administered ether or chloroform. This period also witnessed the foundation of faculties of medicine in some countries of the Middle East (Syria, Sudan, and Iraq). An influx of newly trained surgeons increased the demand for qualified anesthesiologists, thus prompting anesthesia residencies. In addition, in response to a manpower shortage in many countries in the Middle East, nurse and technician training began as well, although this was gradually phased out as locally and internationally trained and certified anesthesiologists began arriving in many countries of the Middle East. During the second half of the twentieth century, all countries of the Middle East were striving to attain stateof-the-art anesthesia. Raising the Professional Profile of Anesthesia As in many other places in the world, the status of anesthesia in the Middle East depends partly on the establishment of fully independent departments of anesthesia that have their own structure, staff, residency training, research, and certification by international academic institutions and that offer fellowships in cardiovascular, obstetric, and pediatric anesthesia, as well as pain management. Its main objectives are to act as a forum for education and exchange of opinions and to promote research and publication of Middle Eastern medicine and anesthesia. In addition, in the 1960s and 1970s, many Middle Eastern countries founded their own national societies of anesthesia, which promoted the practice and image of the specialty. Every 2 years, the Pan Arab Society holds the Pan Arab Congress of Anesthesia and Intensive Care in one of the member countries. Chapter 2: International Scope, Practice, and Legal Aspects of Anesthesia 21 As all these developments grew into complex surgical procedures and as the use of neuromuscular blocking drugs spread, it became necessary in Russia to develop a new kind of subspecialty in medicine: anesthesiology. This would require extensive and detailed knowledge of many disciplines, including physiology, biochemistry, surgery, medicine, neurology, pharmacology, traditional anesthesia, and critical care. The first Department of Anesthesiology in Russia was formed in 1958 at the Military Medical Academy in Leningrad. The first postgraduate courses for physicians to become anesthesiologists lasted 4 months. Later, more courses of anesthesiology were incorporated, requiring additional months of training and including the basics of intensive care. The broad variety of topics covered and the complexity of the potential patient care issues meant that the new specialists needed more time to prepare properly for their careers. These careers were in demand as newly formed anesthesiology and intensive care departments required more anesthesiologists to teach and take care of patients. In 1966, the Ministry of Health of the Soviet Union released the "Order of improvement of anesthesiologic and reanimatologic (intensive care) services in the country. Along with the legalization of anesthesiology came the definition of functions and organizational structure. Most hospitals deployed units of anesthesiology, whereas institutions and universities formed departments of anesthesiology. Since 1969, anesthesiology and intensive care have been merging into a single specialty called anesthesiology-reanimatology. An electrocardiogram, noninvasive blood pressure meter, and a pulse oximeter are the minimal monitors for any kind of anesthesia. Pediatric and cardiovascular anesthesia is generally performed by physicians with subspecialty training in these areas. Pain management and critical care reflect important areas in which the influence of the anesthesiologist has been important. Another area of interest is the choice that many physicians, including anesthesiologists, must make between public and private hospitals. The development of private practices in small clinics and in other institutions attracted many practitioners, who then reduced their work in public hospitals to part-time in the mornings. Currently, anesthesiologists work solely in one hospital, either public or private, with strict professional duties and cost containment as a major responsibility. Most of the private clinics are run by private economic groups that operate under stringent financial criteria. In these institutions, the activities of anesthesiologists and other specialists are restricted, and only a few colleagues dedicate their time to administrative duties. Although the resources to public hospitals are increasing, the benefit of these resources is less than one might have expected, probably because of their centralized administration, which is not run by practitioners. Thus, economic restraints and inadequate conditions for anesthesiologists make positions in public practice unlikely to be filled completely, because private work is a more attractive option. Today, all anesthesiologists, no matter where they practice in the world, can gain access to the information necessary to deliver safe anesthesia. However, there are still places in the world that do not have access to the equipment or supplies needed to implement that knowledge. This section details the essentials: the roles and responsibilities, the facilities and equipment available, the education and accreditation, the professional societies, the research conducted by anesthesiologists around the world, and the safety and medicolegal initiatives that have developed in these countries. China (Yuguang Huang) In the last decade, the overall professional level and social status of Chinese anesthesiologists have gained prominence, as has medical education in the field. Each year, large numbers of outstanding medical graduates enter the anesthesiology resident training program, adding greatly to the activities of existing teams. The development of anesthesiology has also encouraged the continuing growth of other surgical departments. The specialty of anesthesiology in China is mainly composed of clinical anesthesia, pain management, emergency resuscitation, and extracorporeal circulation. These clinicians are capable of performing intraoperative ultrasound examinations independent of assistance from ultrasound physicians. Aside from clinical practice in the operating theaters, anesthesiologists are also becoming involved in such clinical diagnostic and therapeutic procedures as endoscopy, fetus reduction at the fertility center, and provision of comfortable alternative solutions to patients undergoing mini-invasive procedures outside the operating theater. Anesthesiologists are earning more respect and recognition from physicians of other specialties and patients in China. Anesthesiology has also evolved to be the perioperative medicine in multiple aspects. Patient blood management and perioperative blood conservation techniques are an internationally acknowledged issue. Currently, national guideline and blood management standards have been adopted in a majority of provinces, greatly alleviating the pressures exerted by limited blood supply and avoiding transfusion-related complications to a large extent. In addition, a number of hospitals have pain clinics providing good pain management for inhospital patients. Anesthesiology has evolved as a crucial medical specialty that enjoys rising status in general hospitals, with department chiefs being involved in the leadership of hospital management. In addition, anesthesiologists have become integral to multidisciplinary collaborations, reflecting the growing status and recognition of anesthesiologists by their peers. This project has received great acclaim and recognition from physicians and local hospital leaders, reflecting the execution skills, unified collaboration, and leadership capabilities of Chinese anesthesiologists. Eriksson and Jannicke Mellin-Olsen) the main activities in European anesthesia departments are to provide operating room anesthesia, postoperative care, critical care medicine, pain medicine, and critical emergency medicine. The concept of anesthesiologists as perioperative physicians is a hallmark and well developed in many European countries. A considerable proportion of health care leaders are anesthesiologists who have a good overview of hospitals in general. In addition, in recent years anesthesiologists have taken more responsibility in leading patient safety initiatives. In some countries, such as the Czech Republic, Germany, Italy, Moldova, Norway, and the United Kingdom, more than 30% of the activity of anesthesiologists is devoted to critical care medicine. Even in those countries where critical care is recognized as a separate primary specialty, as in Spain and Switzerland, anesthesiologists are involved in the care of the critically ill. Some physician groups want to introduce more specialties on a European level, such as in critical care medicine. Thus far, anesthesiologists have opposed such initiatives as counterproductive and assert that it is more desirable to define and develop competencies and particular qualifications to develop critical care medicine further. Emergency medicine is currently a separate specialty in Europe, but anesthesiologists regard critical emergency medicine a part of the professional domain. In some countries, a large proportion of anesthesiologists are also active in acute and chronic pain medicine. In most European countries, nurses are involved, but with varying tasks and responsibilities. One model is the nurse anesthetist who is allowed to provide anesthesia without the presence of the in-charge physician in the room.

Buy genuine motilium on line
Van Gessel E gastritis and chest pain generic motilium 10mg without a prescription, Goldik Z, Mellin-Olsen J: Education, Training Standing Committee of the European Board of Anaesthesiology, Reanimation, Intensive Care. Postgraduate training in anaesthesiology, resuscitation and intensive care: state-of-the-art for trainee evaluation and assessment in Europe, Eur J Anaesthesiol 27(8):673-675, 2010. Walker I, Wilson I, Bogod D: Anaesthesia in developing countires, Anaesthesia 62:2-3, 2007. Bainbridge D, Martin J, Arango M, et al: Perioperative and anaesthetic-related mortality in developed and developing countries: a systematic review and meta-analysis, Lancet 380:1075-1081, 2012. Pollach G: Anaesthetic-related mortality in sub-Saharan Africa, Lancet 381:199, 2013. Landoni G, Bignami E, Nicolotti D, et al: Publication trends in the journal of cardiothoracic and vascular anesthesia: A 10 year analysis, J Cardiothorac Vasc Anesth 24:969-973, 2010. Baraka A: the Influence of carbon dioxide on the neuromuscular block caused by tubocurarine chloride in the human subject, Br J Anaesth 36:272, 1964. Baraka A, Noueihid R, Hajj S: Intrathecal injection of morphine for obstetric analgesia, Anesthesiology 54:136-140, 1981. Naughton P, Mossad E: Retraining the left ventricle after arterial switch operation: Emerging uses for the left ventricular assist device in pediatric cardiac surgery, J Cardiothorac Vasc Anesth 14:454-456, 2000. Indian Medical Council (Professional conduct, Etiquette and Ethics) Regulations, 2002. Concurrently, anesthesia has evolved to include acute and chronic pain management, critical care medicine, palliative care, and sleep medicine. In response to the increasing costs and emphasis on quality and patient safety, payers are modifying payment methodologies to better align goals of care. Clarifying roles and responsibilities of the surgeon, anesthesiologist, and other providers is critical to delivering high-quality cost-effective care. Although nonanesthesiologists, including hospitalists, can be very helpful in addressing some clinical needs for the surgical patients, anesthesiologists are well positioned to take a more prominent role in overall perioperative management, benefiting patients, optimizing quality and outcomes of care, and improving efficiency during and after surgical procedures. These goals also depend on accessibility to clinical and financial data and personnel with the skills to analyze the information for delivery of optimal care while improving efficiencies. Fifty years ago, anesthesia care was dominated by intraoperative management, and most clinical income came from services related to surgical care. Gradually, the scope of anesthesia broadened beyond the intraoperative period to include preoperative evaluation, intraoperative management, and postoperative assessment to determine whether the patient suffered any consequences of anesthesia care. Although this model of care-and the associated payment methodology-was an appropriate model of anesthesia care in the past, today the changing needs of the patient, complexity of care, and the role of the various health care providers mandate that we define alternative models for perioperative management to optimize clinical outcomes. Management of clinical care throughout the perioperative period includes preoperative assessment and management to optimize outcomes after procedures, intraoperative care, and postoperative strategies. Thus, the anesthesiologist has an expanded scope of practice and participates more broadly in all aspects of care, with the overall result of improving outcomes and reducing costs. The impetus for expansion of the scope of anesthesia practice comes from multiple perspectives. First and foremost is the commitment to provide patients with high-quality and safe care that fulfills their goals. To do so requires a broader focus on the overall perioperative course rather than a scope of care that is limited to the intraoperative and immediate postoperative care periods. A second and equally important goal toward which the anesthesiologist plays an integral role is the increasing emphasis on evidence-based practice, limiting unnecessary or redundant services, and providing more efficient care, particularly in the immediate perioperative period. There is no question that the high costs of inpatient services, particularly for patients with underlying comorbidities who undergo complex surgical procedures, contribute to escalating overall health care expenditures. At the same time, the evolution and expansion of anesthesia practice have created many new opportunities for anesthesiologists to participate in perioperative care beyond the immediate postoperative period-and to define standards of care for selected patient populations. Some anesthesiologists are integral members of teams of providers who care for selected surgical patient populations, and they collaborate with surgeons to develop clinical pathways and identify ways to improve preoperative care as well as intraoperative and postoperative management strategies that enhance outcomes. For example, transplant anesthesiologists (also see Chapter 74) are often involved in discussions about patient selection, preoperative management, and transitions of care from the operating room to postoperative period. In each of these examples, collaboration among the surgeons, anesthesiologists, and the overall team of providers both within and beyond the operating room environment is critical to realizing improved outcomes and reduced costs of care. The role of the anesthesiologist in perioperative management also includes the subspecialties of pain medicine and critical care. Pain management strategies have significant positive impact on the care of patients with both acute and chronic pain (also see Chapters 64, 96, and 98). More rational approaches to perioperative pain management, particularly for patients with longstanding chronic pain, have had positive impact on perioperative outcomes and, in many cases, reduced lengths of stay in hospitals and improved patient satisfaction. Although not frequently addressed by anesthesiologists, postdischarge care needs are often related to perioperative management; anesthesiologists can have a meaningful role in addressing some of these significant costs of care and the related issues that lead to dissatisfied patients and providers. A third area of concern that has taken on greater importance over the past decade is the rising cost of health care in general and perioperative care in particular. Advances in technology for both anesthesiologists and surgeons have made it possible for patients who previously were denied surgery because of underlying chronic medical conditions, anesthesia risk, or limited surgical options to undergo often complex and costly procedures that may require prolonged postoperative and rehabilitative care. In addition to surgery costs, additional costs (often significant) are associated with complications of care, postdischarge care, and readmissions. For example, in the United States, both government and private payers have raised concerns about the costs associated with managing complications of care, some of which are relevant to anesthetic management. These payers have been reducing payment for costs associated with complications and denying payment for costs associated with readmissions. For example, central line infections, ventilator-associated pneumonia, decubitus ulcers, and renal failure may be either directly or indirectly related to perioperative (anesthetic) management. Implementing strategies to reduce these complications has been very successful; a more coordinated approach to perioperative management by the anesthesiologists can have significant positive impact on both clinical care and costs. Under this payment methodology, each provider receives compensation for the specific services provided to the patient. Payment is encounter based and does not encourage collaboration or coordination of care. Many of these payment methodologies have significant impact on anesthesiologists and the roles they play in perioperative management. Although issues related to payment methodologies differ greatly from one country to another and are beyond the scope of this chapter, the goals and implications of these newer payment methodologies have major effects on the practice of anesthesia. Also, these various models provide potential opportunities for expanding the role of the anesthesiologist or other providers in perioperative management. Finally, although the expanded roles of anesthesiologists in perioperative management have had a positive impact and, in some cases, resulted in more cost-effective and efficient care, the subspecialization of anesthesia care has, in some ways, fragmented care and detracted from a coordinated approach to perioperative management. Under current models of care delivery, perioperative care is rarely provided by a single anesthesia provider. More often, the care is provided by multiple providers, each with a specific role and responsibility. Preoperative care is now often provided in a dedicated preoperative evaluation clinic, which is physically separate from the operating room or other clinical sites. Operating room care is provided by an anesthesiologist either individually or as part of the anesthesia care team model. New models of care that more effectively integrate the diverse roles of anesthesiologists are required to effectively fulfill the goals outlined here. For example, Chapter 38 emphasizes the changing role of the anesthesiologist in preoperative assessment and management. Formal preoperative assessment of an otherwise healthy patient may not be needed in all cases14,15; however, advances in surgery and anesthesia have made it possible to identify patients who require more comprehensive evaluation that includes extensive testing and management of underlying conditions in order to prepare them for surgery and the postoperative course. However, in many cases, the management strategies required to optimize the patient before surgery are best determined by the anesthesiologist, who is most knowledgeable about the impact of chronic conditions on perioperative care needs and the implications of anesthesia on underlying physiology. The anesthesiologist is the provider who can most appropriately coordinate the preoperative assessment and management of the patient to confirm that the evaluation and interventions are necessary to optimize the patient for surgery and anesthesia and to minimize unnecessary assessment and care that will not affect the perioperative course. Similarly, the anesthesiologist, whether individually or as part of the care team model, provides intraoperative care (although in some cases nurse anesthetists have obtained independent practice). In situations in which the anesthesiologist is personally providing or medically directing care, the anesthesiologist can and should ensure a coordinated approach to the transitions from preoperative to intraoperative care, as well as the collaboration required for optimal postoperative management. As important, the anesthesiologist-in conjunction with the surgeon, operating room nurses, and other staff-must communicate effectively to ensure that the correct procedure is being performed on the correct patient, to ensure that all supplies and equipment are available, to facilitate the timely turnover of operating rooms, and to optimize coordination of care from the preoperative to the postoperative period. A number of initiatives have been implemented in hospitals throughout the world to improve intraoperative management, minimize complications, and reduce costs. The implementation of checklists has been demonstrated to improve patient safety in the operating room17-19 (also see Chapters 4 and 6). This process has reduced errors and facilitated the transition from the operating room after a surgical procedure.
Diseases
- Facioscapulohumeral muscular dystrophy
- Charcot Marie Tooth disease type 2B1
- Heart attack
- Ectrodactyly ectodermal dysplasia cleft syndrome
- Angiotensin renin aldosterone hypertension
- Hirschsprung disease ganglioneuroblastoma
- Giardiasis
- Pericardium congenital anomaly
- Epilepsy mental deterioration Finnish type
Cheap motilium
The pipeline failure was quickly detected (19 seconds) gastritis diet for children buy generic motilium 10mg online, but the responses to it were extremely variable and showed a variety of problems. Five of 18 anesthesia professionals closed the anesthesia circuit (which preserves the existing oxygen in the circuit), but all 5 subsequently switched to ventilation with a self-inflating bag using room air or to mouth-to-tube ventilation. Five of 18 could not open the reserve oxygen cylinder because they could not locate the tank wrench attached to the machine (it tended to rest between two gas cylinders). Several teams had trouble mounting a new oxygen tank on the anesthesia machine; problems with the gasket disk were frequent. A study by Byrne and Jones looked at differences in the performance of experienced and less experienced anesthesia professionals. The results showed significant differences only between the first and second year. These studies underscore the importance of recurrent training for experienced anesthesia professionals and the truism that experience is not a substitute for excellence. The reader is referred to Chapter 8 for discussion of newer studies with the use of patient simulators and performance assessment as such. Cooperative work, team interaction, and communications issues were problems in several cases. These stemmed from both individual and organizational failures to coordinate information and efforts from different organizational components. Indirect Observation of Anesthesia Professionals Involved in Difficult Cases An unusual approach involving indirect observation of actual cases was used by Cook and colleagues at the Ohio State University in Columbus. These investigators argued that this approach allowed them to apply a "neutral observer criterion" to the behavior of the anesthesia professional. The investigators acknowledged the risks of hindsight bias and selection bias with this methodology, but they suggested that their technique provided a unique window on human performance issues. Fifty-seven cases were analyzed, 21 of which had a full cognitive analysis in the final report. From the presentation and discussion of a case, the investigators classified evolution of the events into 1 of 5 categories: acute incident, going-sour incident, inevitable outcome incident, difficult-airway incident, and no-incident incident. Cook and colleagues called attention to several issues that surfaced in their cognitive analysis of these cases, including the following295: 1. Many cases involved several lines of concern simultaneously, each of which could have interacted with another. Adaptive planning (as described in the section on abstract task analysis) was sometimes required. The greatest expertise was seen with infrequent or unusual situations rather than with typical situations. Allocation of attention to relevant stimuli or to the most important "theme" was an important issue. The attentional shifts were not always well supported by existing alarm and display technologies. Anesthesia professionals attempted to reduce their cognitive workload whenever possible. Meanwhile, a few groups around the world have started to use video for task analysis and assessment of performance for research and training, which are not detailed here. Several of the previously mentioned groups are working on methodologies for evaluating technical and behavioral aspects of performance. Pierre M, et al: Crisis management in acute care setting: human factors and team work in a high stakes environment. Buerschaper C, et al: Forum Qualitative Sozialforschung [Forum: Qualitative Social Research; online journal] 4, 2003 122. Rall M, et al: Bull R Coll Anaesth, [special human factors issue] 2614-2616, 2008. DeKeyser V, et al: Fixation errors: failures to revise situation assessment in dynamic and risky systems. Xiao Y, et al: Incident evolution and task demands: an analysis and a field study of "going sour" incidents [abstract]. Presented at the 36th annual meeting of the Human Factors Society, Atlanta, 1992, p 1279. Presented at symposium of the American Medical Informatics Association, 2001, p 756. Columbus, Ohio, 1991, Cognitive Systems Engineering Laboratory, Department of Industrial and Systems Engineering, Ohio State University. In Ennker J, Pietrowski D, Kleine P, editors: Risikomanagement in der operativen Medizin. McNeese M, et al: New trends in cooperative activities: understanding system dynamics in complex environments. Stuttgart, Germany, 1998, Institut fuer Arbeits-und Organisation Psychologie, p 130. Beatty J, et al: Sleep deprivation and the vigilance of anesthesiologists during simulated surgery. Rall M, et al: Mobile "in-situ" crisis resource management training: simulator courses with video-assisted debriefing where participants work. In Proceedings of enhancing patient safety and reducing errors in health care, Rancho Mirage, Calif, 1999, National Patient Safety Foundation, p306. These studies and others show that fatigue increases the risk of adverse events, compromises patient safety, and increases risk to personal safety and well-being. An article in the November 2007 Joint Commission Journal on Quality and Patient Safety concluded that evidence strongly suggests that extended-duration work shifts significantly increase fatigue and impair performance and safety. The author of several research studies exploring the effects of provider sleep deprivation on patient and provider safety, Dr. Landrigan stresses the importance of reduced work hours for all health care workers and the need for widespread education of health care providers to recognize their limits. This includes an assessment of off-shift hours and consecutive shift work and a review of staffing and other relevant policies to ensure they address extended work shifts and hours. Invite staff input into designing work schedules to minimize the potential for fatigue. Findings from a groundbreaking 2004 study of 393 nurses over more than 5300 shifts-the first in a series of studies of nurse fatigue and patient safety-showed that nurses who work shifts of 12. Published for Joint Commission accredited organizations and interested health care professionals, Sentinel Event Alert identifies specific types of sentinel events, describes their common underlying causes, and suggests steps to prevent occurrences in the future. Accredited organizations should consider information in an Alert when designing or redesigning relevant processes and consider implementing relevant suggestions contained in the Alert or reasonable alternatives. Sentinel Event Alert may be reproduced only in its entirety and credited to the Joint Commission. The Patient Safety Advisory Group informs the Joint Commission on patient safety issues and, with other sources, advises on topics and content for Sentinel Event Alert. Create and implement a fatigue management plan that includes scientific strategies for fighting fatigue. Sleep hygiene includes getting enough sleep and taking naps, practicing good sleep habits (for example, engaging in a relaxing presleep routine, such as yoga or reading), and avoiding food, alcohol, or stimulants (such as caffeine) that can impact sleep. Support staff when appropriate concerns about fatigue are raised, and take action to address those concerns. Encourage teamwork as a strategy to support staff members who work extended work shifts or hours and to protect patients from potential harm. Consider fatigue as a potentially contributing factor when reviewing all adverse events. For organizations with a current policy that allows for sleep breaks for staff defined as essential by the organization: 9. Assess the environment provided for sleep breaks to ensure that it fully protects sleep. Fully protecting sleep requires the provision of basic measures to ensure good quality sleep, including providing uninterrupted coverage of all responsibilities (including carrying pagers and phones, and coverage of both admissions and all continuing care by another provider) and providing a cool, dark, quiet, comfortable room and, if necessary, use of eye mask and ear plugs.

Buy generic motilium 10mg on line
It is not recommended for use in patients with longstanding or uncontrolled diabetes gastritis que es bueno buy generic motilium 10mg line, especially those with vascular complications (renal and ophthalmologic involvement). Other absolute contraindications include: history of cerebrovascular accident, breast or endometrial cancer, suspected or current pregnancy, and severe hypercholesterolemia or hypertriglyceridemia. Vignette 3 Question 2 Answer A: the Ortho Evra patch is a combination contraception patch, and contains both estrogen and progesterone (ethinyl estradiol and norelgestromin). A patch is placed on the skin for 3 weeks, then removed for 1 week at which time a withdrawal bleed should occur. It carries the same risks as oral contraceptives, and should not be given to women who are smokers over the age of 35 years, as well as the other absolute contraindications listed in Vignette 3 Question 1. There is a negligible risk of thromboembolism with these methods, and they are often used for those patients who are not candidates for estrogen use. It should not be used in women with a history of menorrhagia or unexplained abnormal bleeding. Vignette 3 Question 3 Answer E: Nausea is present in approximately 50% and vomiting in 20% of patients who take Plan B. These are slightly less severe in those taking Plan B (progestin-only, single dose) versus prior combination methods (Yuzpe method) containing estrogen. Often providers prescribe antiemetics at the same time as emergency contraception. Headaches, dizziness, and breast tenderness are also side effects, however, not the most common. There are no significant reports of fever or diarrhea when using emergency contraception. Vignette 4 Question 1 Answer E: Oral contraceptives have multiple mechanisms of action. Their primary effect is to suppress the mid-cycle surge by interfering Chapter 25 elective termination of Pregnancy There are several surgical and medical procedures by which pregnancy termination can be achieved. Evacuation of the uterus is an important technique in the field of obstetrics and gynecology. Not only is it used for elective termination of pregnancy, but it is also an integral part of managing spontaneous abortion, missed abortion, intrauterine fetal demise, retained products of conception, and gestational trophoblastic neoplasia. Approximately 88% of induced abortions are performed in the first trimester of pregnancy (75% prior to 9 weeks), utilizing a surgical evacuation of the uterus (D&C). The options for first trimester abortion include suction curettage, manual vacuum aspiration, and nonsurgical "medical" abortion using either mifepristone or methotrexate. Second trimester options include surgical evacuation of the uterus and medical induction of labor. In general, the technique used for termination is determined by the duration of the pregnancy, provider experience, and patient preference. Table 25-1 outlines the various options available during the first and second trimesters. After week 24, abortions are generally only performed when necessary for the preservation of maternal life. Though second trimester abortions are rare, access to providers is often reported as a barrier that pushes women into having procedures beyond the first trimester. In 2000, 87% of counties in the United States had no access to an abortion provider. In the United States, nearly 50% of all pregnancies are unintended and 40% of these end in elective abortion. As such, the availability of safe and effective means of elective pregnancy termination is an important component of family planning and an integral part of obstetrics and gynecologic care. Abortion is a common procedure in the United States, with 3 in 10 women having the procedure done by the age of 45 years. Over 60% of women undergoing abortions have one or more children and 80% are unmarried. Caucasian women account for 36% of procedures; Black women for 30%; and Hispanic women for 25%. The most common reasons women give for choosing to have an abortion include financial burden, familial obligations, interference with work or school, and desire to avoid single parenting. The abortion procedures used legally in the United States are both safe and effective. Since the legalization of abortion in 1973, the risk of death from abortion has declined by 85%. The most recent maternal mortality rate for induced abortion in the United States is 0. The major causes of abortion mortality are complications of hemorrhage and infection, followed by thromboembolism and anesthetic complications. Clinical, laboratory, or imaging studies should be used as needed to confirm completion of the abortion, and any complications should be treated. Suction curettage (D&C), manual vacuum aspiration, and nonsurgical medical abortions are all methods of inducing abortion in the first trimester. Most first trimester terminations in the United States are achieved using the suction curettage (D&C) procedure. In general, the risk of complications after suction curettage is small and directly proportional to the gestational age. D&C typically involves mechanical dilation of the cervix and removal of the products of conception using a suction cannula. A sharp curettage may then be performed to ensure the uterus is completely evacuated. Antibiotic prophylaxis (doxycycline, ofloxacin, ceftriaxone, or metronidazole) is recommended to avoid the risk of postabortal upper genital Prior to termination, gestational age should be confirmed by last menstrual period, bimanual examination, and ultrasound evaluation. Women should be counseled on reliable forms of contraception with initiation of chosen method, if appropriate. Maternal complications are rare with suction curettage and the maternal mortality rate is 0. For early pregnancies up to 10 weeks of gestation, manual vacuum aspiration can be performed. The uterine contents are then manually extracted using a 50- or 60mL self-locking vacuum syringe instead of a suction machine. Evacuation is achieved by a gentle in and out motion while also rotating the unit to ensure clearance of all products of conception. Since that time, medication abortion has become increasingly utilized and now accounts for 25% of terminations prior to 9 weeks of gestation. Mifepristone thereby disrupts the pregnancy by making the endometrial lining unsuitable to sustain the pregnancy. Although it can be used alone, the success rate of completed pregnancy is greatly improved when used in combination with a prostaglandin analog such as misoprostol. Effectiveness When performed by a trained physician, the success rate for suction curettage is 98% to 99%. In these early pregnancies, an effort should also be made to identify villi after the procedure by floating the evacuated tissue in saline. Complications First trimester termination using suction curettage (D&C) is the safest of all surgical termination methods. Complications of suction curettage are rare and include infection (1% to 5%), excessive bleeding (2%), uterine perforation (1%), and incomplete abortion (1%). Limited data suggest that women who have three or more cervical dilation procedures (for termination, hysteroscopy, D&Cs, etc. Because methotrexate has been approved for use for a variety of medical conditions including ectopic pregnancy, it has been used by clinicians on an off-label basis as an abortifacient. When a second trimester termination is necessary, D&E is the most common and safest method of termination of pregnancy. D&E has a lower maternal mortality and morbidity compared to second trimester induction of labor. Methotrexate is contraindicated for patients with immunodeficiency and those with hepatic or renal disease. Effectiveness When used alone, the efficacy rate of mifepristone is approximately 65% to 85%.
Buy generic motilium 10 mg line
Psychologists studying judgment in aviators have identified five types of attitude as being particularly hazardous gastritis diet of worms cheap 10mg motilium overnight delivery, and they have developed specific antidote thoughts for each hazardous attitude. Aviation psychologists instruct pilots to verbalize the antidote thought whenever they find themselves thinking in a hazardous way. The invulnerable and macho attitudes are particularly hazardous for anesthesia professionals. They are compounded by production pressures to handle more cases in less time with fewer cancellations and less opportunity for preoperative evaluation. The feeling that a catastrophe "cannot happen to me" and that perfect performance can always be called on to avert a disaster can lead to cavalier behavior and poor planning. The individual anesthesia professional rarely, on average, will be responsible for a serious iatrogenic complication. However, planning to avoid catastrophe is likely to be more successful than battling to avert it. Alternatively, one can observe what skilled practitioners actually do in their work and classify these actions into task elements. The two distinct phases of anesthetic care are as follows: (1) preoperative evaluation, planning, and preparation; and (2) conduct of the anesthetic regimen and immediate postoperative care. The performance of anesthesia professionals in selecting appropriate laboratory tests has been found to be relatively poor. Roizen and associates stated the following: Even when physicians agree to reduce testing by using specific, agreed upon criteria for selectively ordering tests based on history and physical examination, they still make a surprising number of mistakes when ordering tests. Whether these devices, in combination with human follow-up for patients with medical problems, will improve the efficiency and accuracy of preoperative evaluation remains to be determined. The extent to which this factor influences the design of anesthetic plans or patient outcomes is unknown. Routine anesthetic plans can be modified or combined to produce a compromise plan that best fits the goals and constraints of the situation. Most of the existing literature on preoperative planning concentrates only on narrow medical and physiologic aspects of underlying diseases and their anesthetic ramifications. No systematic research has been conducted on how various tradeoffs are made or on how normal anesthetic processes are adapted to suit the needs of specific situations. This involves obtaining the necessary equipment and supplies, assembling infusions, preparing syringes of needed drugs, and conducting pre-use checkouts of life-support equipment (see Chapter 44). Buffington and co-workers demonstrated that only 3% of anesthesia professionals examining an anesthesia machine could identify all five faults with which it had been rigged; most practitioners found only two of the five. However, it was found that use of the checkout procedure was minimal and that the extent of pre-use checkout by practitioners was extremely variable. Interestingly, 34% of the faults that were not detected were missed by practitioners who had in fact correctly answered three out of three written test questions concerning that fault. For example, the plan for general anesthesia includes choices for the means of inducing anesthesia, securing the airway and ensuring proper ventilation, maintaining anesthesia, conducting emergence from anesthesia, and controlling postoperative pain. If a significant feature of the situation is missed in formulating the plan, it can leave the patient vulnerable, regardless of how adeptly the plan is implemented. Another approach consists of the readiness and ability to use emergency cognitive aids, particularly emergency checklists or emergency manuals (also known by similar terms, including emergency response protocols, critical event algorithms, and so on). Despite many advances, the use of such cognitive aids is still not a regular part of the culture of medical work in many locales. To reduce cost, the manual is printed on sealed paper; only the front and back pages are laminated. On the front page, it shows the emergency events, thus making it easy to jump to the right page. Experience shows that clinicians must be familiarized with the manual in advance for optimal use. B and C, Two pages of the Emergency Manual checklist for "Anaphylaxis": the content and the layout have been optimized through graphic layout and careful choice of words for easy and ergonomic use in actual operating room emergencies. Users are able to choose to print out the Emergency Manual locally, and instructions are given on choices of printing paper. An Emergency Manual Implementation Collaborative has been started bringing together several leading centers in this arena to facilitate the development, testing, dissemination, adoption, and use of these resources. The anesthesia professional must monitor the plan as it is executed and must adapt it in response to dynamically changing events. The key features of this task are (1) checking for the achievement of milestones and (2) reactive plan adaptation. At various points of a procedure, critical milestones must be achieved to keep the original plan unaltered. If a milestone is not achieved, the anesthesia professional must decide whether to delay the next action in the sequence, modify the plan, or suspend or abort the procedure. On some occasions, the milestones are explicitly identified in advance, whereas in others the milestones are implicit. As plans are changed, actions may be taken that invalidate other aspects of the previous plan, thereby Executing main plan Adapting main plan in response to failure to achieve a milestone Adapting main plan in response to an event Mechanical ventilation, etc. Throughout the procedure, the anesthetist is vigilant for the occurrence of new problems ("police cars"). If a problem is detected, a process of reactive problem solving takes place that may result in new adaptations to the plan (in this case, treatment of bronchospasm). In some cases, even the original goals of the anesthetic plan may need to be adapted. In the Multicenter Study of General Anesthesia,344 86% of patients had at least one undesirable outcome. Although most events were minor and caused no injury to the patient, more than 5% of patients had one or more severe events requiring "significant therapy, with or without full recovery. The investigators did not compute the frequency of severe events, but overall, these data appear to be consistent with those from earlier studies. This sequence can be prevented by prophylactic measures such as preoperative evaluation and treatment of patient diseases or pre-use checkout of life-support equipment. Once a problem occurs, it may remain self-limited or evolve further down the accident chain. Using dynamic decision making, the anesthetist must detect and correct the problems that do occur at the earliest possible point in the chain of evolution. Interruption of the accident chain is made more difficult when tight coupling exists within the system, when multiple interacting problems are present, or when problems disrupt recovery processes. Efficient use of incident analysis may make it easier in the future to prevent or interrupt problem evolution. Multiple small problems combine to trigger a problem that can evolve into an adverse outcome; the original problems by themselves would not have evolved further. An evolving problem should be able to be stopped, but the recovery pathway is faulty. Attention focused on one (minor) problem distracts attention from the (serious) evolution of another. The system has a variety of interruption points at which the occurrence of problems can be prevented (preoperative evaluation of patients and pre-use checkout of equipment). Moreover, although anesthesiology is far more dynamic than many medical domains, it is relatively slow in comparison with many human activities such as sports, driving, and combat flying. Thus, events often evolve slowly enough that the process of accident evolution can be thwarted before an adverse patient outcome actually occurs. In the prospective studies of intraoperative events cited earlier, the incidence of undesirable situations was surprisingly high, whereas the rate of actual patient harm was quite low. This is a markedly different picture from that in commercial aviation, although the accident rate in aviation is very low. Approximately 30,000 airline flights take place each day in the United States, and very few serious incidents or accidents occur, although the exact number is unknown. The total accident rate from all causes (not including terrorist acts) for scheduled airline flights from 2002 through 2011 was 0. In fact, according to the National Transportation Safety Board, in the years 2007 to 2011 there was only a single fatal airline accident.
Syndromes
- Certain types of vascular stents
- Several x-rays of the gallbladder
- Hyperactivity (as seen with "uppers" such as cocaine, methamphetamine)
- Pregnancy (TBG levels are normally increased during pregnancy.)
- Faster than normal heart rate
- Estrogen therapy
- Foods or drinks with caffeine
10mg motilium sale
Peripheral nerve block and continuous epidural anesthesia were introduced on a gradual basis gastritis diet ������� purchase motilium 10mg with visa. From the 1950s to the 1980s, intravenous procaine combined anesthesia and continuous epidural anesthesia were the most common methods in China. When anesthetic drugs and monitoring tools became scarce in the 1960s, Chinese anesthesiologists tried to develop acupuncture anesthesia based on the pain-relieving mechanisms of traditional Chinese acupuncture. In the 1970s, Chinese anesthesiologists investigated the anesthetic effect of Chinese herbal medicine. Tempe) Until approximately 30 years ago, anesthetic equipment in Indian operating rooms often consisted solely of a simple anesthesia machine, a suction unit, and perhaps an electrocardiographic monitor. Even the oxygen supply was mainly via cylinders, with few hospitals having a centralized medical gas supply. B, Participants of the Second National Conference on Anesthesia, Harbin, 1979, during which the Chinese Society of Anesthesiology was founded. During this period of the twentieth century, Indian anesthesiologists also recognized the need for professional societies. Professors Macintosh and Gray were the distinguished guests during the conference. The group has grown from 19 members when it began to nearly 18,500 members in 2012. The Japanese government invited many medical instructors from Germany (Prussia at that time) to teach in Japan, and medical students from Japan studied in Germany. In those days, German physicians promoted local anesthesia rather than general anesthesia. Therefore, surgeons in Japan focused on local anesthesia, whereas general anesthesia dramatically developed in the United States and the United Kingdom. Meyer Saklad came to Japan to participate in the Joint Meeting of American and Japanese Medical Educators. He presented novel information on anesthesiology, including general anesthesia, to Japanese surgeons. Afonin) In the midst of the economic difficulties and political upheaval after the Russian civil war, medical services underwent dramatic reorganization and expansion, and some positive developments ensued, including campaigns against diseases and poor hygiene. They then went all over the country to educate people and treat deadly diseases, often risking their own lives. This experience emphasized the importance of preventive measures, including vaccinations, and Soviet physicians began working on preventive medicine. Vadim Yurevich was the first in the world to begin using citrate for blood conservation. Vladimir Shamov was the first to use cadaveric blood for transfusion in 1928, thus giving birth to a new field of medicine-transplantation. The first Institute of Blood Transfusion, a scientific center for study and development of the science of blood and blood component use and storage, was formed in 1926 in Moscow by Professor A. Physicians of the institute developed and published the first systematic approach to the treatment of shock, including traumatic, hypovolemic, and "burn related. Chechulin constructed and used the first artificial heart machine in the world, the forerunner of what is now known as a cardiopulmonary bypass machine. Surgical procedures were becoming more complex and required more advanced methods of exposure of the abdominal and thoracic organs. Henry Hickman was transformed into many different machines to provide artificial ventilation, including the famous iron lung at Harvard, used first in Boston in 1928. In Moscow in 1936, the Laboratory of Resuscitation of the Academy of Medical Sciences of the U. Negovsky was instrumental in the integration of resuscitation in practical health care. These methods were used successfully on patients requiring complicated cardiothoracic surgeries in Russia. Nurse anesthetists generally have a nursing degree with an additional 1 to 4 years of training, resulting in a diploma that entitles the nurse to administer anesthesia according to a plan defined by the anesthesiologist, including medication administration, tracheal intubation, and monitoring, depending on local protocol and terms and conditions of service. Countries where anesthesiologists work with nurse anesthetists are Scandinavia, the Netherlands, France, the Slovak Republic, and Bulgaria. The other model is the circulation nurse or anesthesia nurse, who can assist anesthesiologists during procedures but are not allowed to perform any direct patient-related roles beyond basic nursing tasks, such as preparing medication and administering intravenous fluid. In Ireland and Malta, even this model is not Chapter 2: International Scope, Practice, and Legal Aspects of Anesthesia 23 allowed, in contrast to Finland, Germany, Italy, Romania, United Kingdom, and other countries. In India, anesthesia can be administered by a qualified anesthesiologist or by a trainee anesthesiologist under the supervision of a qualified anesthesiologist. In some states, such as Delhi, a directive from the government has been issued that states, "Anesthesia must be administered by a qualified anesthesiologist, that is, an anesthesiologist with a postgraduate qualification and who has been actively working. Typically, anesthesiologists in India are involved in the following types of care: (1) preoperative assessment and preparation of patients; (2) perioperative care of patients; (3) pain relief during the perioperative period; (4) management of critically ill patients; (5) management of acute, chronic, and cancer-related pain; (6) management and teaching of resuscitation skills; (7) provision of outpatient anesthesia services; (8) administrative involvement in establishing and managing health care organizations; (9) disaster management coordinator in the hospital; and (10) teaching and training of the medical and paramedical staff. In addition to the duties just listed, both natural and manmade disasters have provided an extra challenge for anesthesiologists. By virtue of their ability to administer emergency life support measures, as well as their perioperative management skills, anesthesiologists were at the forefront during the 2001 Gujrat earthquake and tsunami disasters, and they actively participated in establishing operating theaters on site and providing care to victims. Likewise, during the 2011 Mumbai and Delhi bomb blasts, anesthesiologists played a leading role in performing emergency surgery and perioperative management. A few hospitals have started awareness programs wherein a lecture is delivered (with illustrations) on a monthly basis to patients and their relatives to familiarize them with the anesthetic techniques and procedures that they will undergo. The operating room continues to be the mainstay of anesthetic practice, where the anesthesiologist fulfills his primary responsibility of providing safe anesthesia to patients undergoing surgery. Operating rooms are major consumers of hospital resources and major sources of income for private hospitals; therefore, it is imperative that they be managed in the most efficient manner. However, there is no consensus on an ideal system to ensure efficiency in this area. The anesthesiologist is actively involved in trying to improve efficiency, especially with triage and the scheduling of urgent and emergency cases. In addition, the anesthesiologist is responsible for designing and equipping the operating rooms. The professional risks (especially those related to needlestick injuries) of anesthesiologists, as well as other operating room staff, are well recognized, and preventing such health care hazards has become an important consideration. Where there is a distinction, the decision about where a postsurgical patient belongs is governed by the degree of morbidity. Patients undergoing day surgery (if practiced in a given hospital) are also transferred to the recovery room before discharge. Practice varies by location, and it is generally governed more by the logistics involved in a particular hospital than by any definite norms. It is difficult to provide exact figures in this matter, but in general, the private (corporate) hospitals provide ambulatory care. The number of government hospitals practicing ambulatory care is relatively small, mainly because of logistic reasons. However, that is likely to change with the increasing availability of short-duration anesthetic drugs and modern surgical facilities (tools for minimally invasive surgery). Saving costs to the patient and the hospital and increasing patient turnover have been the major factors influencing interest in ambulatory care. Anesthesia services are also frequently required in several other areas within the hospital but outside the operating room. These areas tend to be less familiar to most anesthesiologists and provide less access to the facilities typically available in an operating room. Their proliferation, however, has increased the demands on the field of anesthesiology. The anesthesiologist should be familiar with these requirements to maintain safety standards. There is a tendency to consider these procedures as minor (by our clinical counterparts), thus undermining the safety requirements. However, the anesthesiologist must ensure that adequate safety standards are maintained in all these areas. Furthermore, managing a critically ill patient was considered an extension of the job that anesthesiologists performed in the operating room.
Trusted 10 mg motilium
The user is encouraged to do a monthly string check to ensure the device has not been expelled gastritis diet ����� cheap 10 mg motilium. ParaGard is also approved for emergency contraception when placed within 72 hours of unprotected intercourse or contraceptive failure. It is also as effective as oral progestins in treating endometriosis, endometrial hyperplasia, and cancer. As a result, this decreases the number of surgeries needed for pain and bleeding (hysterectomies, D&Cs, endometrial ablations). Currently, combined hormonal methods are available in oral, transdermal, and vaginal forms, whereas progesterone-only methods are available in oral, injectable, implantable, and intrauterine forms. This pseudo-pregnancy state suppresses ovulation and prevents pregnancy from occurring. The bleeding that takes place during the hormone-free interval is actually a bleed due to the withdrawal of hormone rather than a menstrual period induced by endogenous hormone fluctuation. Monophasic (Fixed-Dose) Combination Pills Monophasic combination pills contain a fixed dose of estrogen and a fixed dose of progestin in each tablet. Nearly 30 combinations of estrogen and progestins are available in the United States. In general, the selection of a particular pill depends on the individual side effects and risk factors for each patient. The combination pill containing both estrogen and progestin is taken for the first 21 days out of a 28-day monthly cycle. Bleeding should begin within 3 to 5 days of completion of the 21 days of hormones. Newer formulations are now available that give 24 days of hormone (rather than the traditional 21 days) and a 4-day hormone-free interval. These extended or long-cycle regimens provide continued suppression of ovulation and decreased menstrual-related symptoms (such as pain, heavy bleeding, anemia, and headaches) for their users. Seasonale, Seasonique, and their generic equivalents contains 84 consecutive hormonal pills followed by 7 placebo pills, or 7 low-estrogen pills, respectively. These dosing regimens were designed to decrease the number of withdrawal bleeds to four per year, again, with the goal of minimizing menstrualrelated symptoms. Lybrel provides a combination estrogen and progestin pill each day, 365 days of the year. There is more breakthrough bleeding in this regimen, but no formal monthly or quarterly withdrawal bleed. Multiphasic (Dose Varying) Combination Pills Multiphasic oral contraceptives differ from monophasic pills only in that they vary the dosage of estrogen and/or progestin in the active hormone pills in an effort to mimic the menstrual cycle. The advantage of the multiphasic dosing is that it may provide a lower level of estrogen and progestin overall, but is still highly effective at preventing pregnancy. Nausea, breakthrough bleeding, and the necessity of taking the pill every day are often cited as reasons for discontinuing the pill. Several medications are thought to interact with oral contraceptives resulting in reduced effectiveness of the pill. Conversely, oral contraceptives can also reduce the efficacy of many medications (Table 24-3). Oral contraceptives with estrogen doses greater than 50 mg can increase coagulability, leading to higher rates of myocardial infarction, stroke, thromboembolism, and pulmonary embolism, particularly in women who smoke. The progestins in oral contraceptives have been found to raise low-density lipoproteins while lowering high-density lipoproteins in pill users smoking more than one pack per day. For these reasons, oral contraceptives are contraindicated in women over age 35 years who smoke 15 or more cigarettes a day. The advent of new progestins and lower estrogen doses has led to pill formulations that are essentially neutral in terms of cardiovascular effect. However, combination oral contraceptive use is still contraindicated in women over age 35 years who smoke. The effect of long-term oral contraceptive use on breast cancer has been studied extensively over the past decade with no conclusive findings. There is, however, an increased incidence of gall bladder disease and benign hepatic tumors associated with oral contraceptive use. Table 24-5 outlines both the absolute and relative contraindications to oral contraceptive use. Disadvantages include cardiovascular complications, increased gallbladder disease, increased incidence of benign hepatic tumors, and the need to take a medication every day. Control of bleeding in bleeding disorders and anovulation Dysmenorrhea Endometriosis Acne/hirsutism Premenstrual syndrome Transdermal Estrogen and Progestin Hormonal Contraception-Ortho Evra the contraceptive patch. The patch releases 150 mg per day of the progestin, norelgestromin, and 20 mg per day of ethinyl estradiol. There does not appear to be an increased risk of heart attack and stroke in these patients. Women apply one patch each week for 3 weeks followed by 1 week patch-free period during which they will have a withdrawal bleed. Mechanism of Action Effectiveness the patch has been shown to have a 1% pregnancy rate in actual use-similar to other combination hormonal methods. Both contain a combination of estrogen and progesterone, which are released over a period of 1 week and 3 weeks, respectively. Other mechanisms of action include endometrial atrophy and ovulation suppression (50% of cycles). Ortho Evra has been found to have a decreased effectiveness in markedly overweight women (. Effectiveness Vaginal Estrogen and Progestin Hormonal Contraception-NuvaRing the hormone-releasing vaginal ring. The ring is placed in the vagina for 3 weeks (it is likely effective for 4 weeks), and is removed for 1 week to allow for a withdrawal bleed. Again, this hormone-free period can be skipped to allow for continuous dosing, typically for 3 months. Advantages/Disadvantages Effectiveness Clinical studies are ongoing, but the vaginal ring is highly effective (1% to 2% failure rate in actual use), similar to other forms of combined hormonal contraception. Advantages/Disadvantages Because one size of vaginal ring fits all women, the vaginal ring need does not need to be fitted by a clinician. Women place the ring in the vagina themselves for 3 continuous weeks and then remove it for 1 week. Because the ring is left in place continuously, it provides a low, steady release of hormone with lower total hormone exposure compared to other combination hormone methods. And while douching with the NuvaRing in place is discouraged, the use of antifungal agents and spermicides is permitted. Studies have shown that women do not feel the ring inside once placed in the vagina and the ring does not need to be removed for intercourse. If it is removed for intercourse, it should be rinsed in cool to lukewarm water and replaced within 3 hours. Reasons for discontinuation include discomfort, headache, vaginal discharge, and recurrent vaginitis. The disadvantages include irregular menses ranging from amenorrhea to irregular spotting. This formulation carries the benefit of lower progestin levels but the same efficacy rates. Depo-Provera acts by suppressing ovulation, thickening the cervical mucus, making the endometrium unsuitable for implantation, and reducing tubal motility. After an injection, ovulation does not occur for 14 weeks; therefore, patients have a 2-week grace period in their every 12-week dosing. These all function primarily using the same mechanisms: thickening the cervical mucus, inhibiting sperm motility, and thinning the endometrial lining so that it is not suitable for implantation. Typical use failure rates are estimated at 3%, mostly attributed to patients failing to return at scheduled times for follow-up injections. Side Effects the primary side effects experienced by Depo-Provera users include irregular menstrual bleeding, depression, weight gain, hair loss, and headache. Over 70% of patients experience spotting and irregular menses during the first year of use. However, the possibility of amenorrhea makes Depo-Provera a good option for women with bleeding disorders, women on anticoagulation, women in the military, and women who are mentally or physically disabled. The effect of Depo-Provera use on bone mineralization is summarized in Table 24-7. Thus, calcium, vitamin D, weight-bearing exercises, and smoking cessation should be encouraged in all women using Depo-Provera.
Order motilium 10 mg fast delivery
External beam radiation gastritis english buy motilium 10mg online, cisplatin-based chemotherapy, and intracavitary radiation. In addition to removing the uterus, a radical hysterectomy also removes the parametria, upper vaginal cuff, uterosacral/cardinal ligament complex, and local vascular and lymphatic supplies. For early disease, both Recurrent Disease When cervical cancer recurs in a patient initially treated with surgery alone, radiation can be used to treat the recurrence. When the cancer recurs in a patient already treated with radiation, surgical treatment with pelvic exenteration can be used if the recurrence is centrally located. Regular pap testing should begin at age 21 regardless of the onset of sexual activity. They can stop routine surveillance at that time or at age 65, whichever comes last. These changes can potentially lead to cancer, but a high number (70%) will regress spontaneously. Complications of cervical conization include bleeding and infection and, much less likely, cervical stenosis or cervical insufficiency. Preinvasive (stage 0) and microinvasive disease (stage Ia-1) can be treated with cone biopsy or simple hysterectomy. She has had Chlamydia and vulvar warts in the past, both of which have been treated and resolved. You perform colposcopy and see a condylomatous acetowhite lesion on her cervix with punctation. After the application of acetic acid, you see a large, dense, white area with mosaic vessels encompassing the entire anterior cervix and extending into the endocervical canal. She has seen a lot of information about abnormal Pap smears and cervical cancer in school and in the community, and she wants to know how she can decrease her own risk. You inform her there are no interventions that will decrease her risk active in 10 years. She wants to know how the vaccine will change her recommended Pap smear screening. Vignette 4 A 62-year-old woman presents to the office complaining of watery vaginal discharge and bleeding for the past 2 months. She states she had a mildly abnormal pap in her 30s, but that was treated with cryotherapy. She states she went through menopause at age 50 and has never been on hormone replacement therapy. Vignette 3 Question 1 Answer D: the current recommendation for screening for cervical dysplasia and cancer should begin at age 21 regardless of the onset of sexual activity. The appropriate screening for women from age 21 to 29 is to have a Pap smear every 3 years. These are recommended for girls aged 11 to 12 (but may be given as early age 9) up through women aged 26. It also lowers the risk of vaginal and vulvar dysplasia as well as some cancers of the head and neck. Vignette 3 Question 4 Answer B: the current recommendation for screening for cervical dysplasia and cancer for women aged 21 through 29 is for Pap smear screening every 3 years. Vignette 4 Question 1 Answer D: Cervical cancer is clinically staged as opposed to surgically staged. Other imaging studies, laboratory tests, and surgical procedures are often used to assess for lymph node involvement and metastases. Treatment with cold knife cone is an acceptable option, but due to her age and the likelihood of future childbearing, observation is an appropriate plan. Screening recommendations for women aged 21 to 29 is to have Pap testing every 3 years. Vignette 2 Question 3 Answer A: Complications of cervical excision procedures are cervical stenosis, cervical insufficiency, infection, and bleeding. Vignette 4 Question 3 Answer D: When cervical cancer recurs in a patient initially treated with surgery alone, radiation can be used to treat the recurrence. When the cancer recurs in a patient who has already been treated with radiation, surgical treatment with pelvic exenteration can be used if the recurrence is centrally located (vaginal apex or pelvis without pelvic sidewall involvement) and there is no metastatic disease. Exenteration involves removal of the pelvic organs, including the uterus, tubes, ovaries, vagina, bladder, rectum, sigmoid colon, and muscle and support structures of the pelvic wall. The 5-year survival rate after pelvic exenteration for recurrent cervical cancer is about 50%. Young patients are often treated with surgery to maintain ovarian function that would be diminished or eliminated by radiation. This typically involves the use of both external beam radiation and Chapter 29 Endometrial Cancer Endometrial carcinoma is the fourth most common cancer in American women, exceeded only by cancer of the breast, bowel, and lung. Over 43,000 women are diagnosed with this disease each year in the United States alone, accounting for 6% of all cancers in women. Although endometrial cancer is the most commonly encountered gynecologic malignancy in the United States, it is associated with a favorable survival profile because the majority of disease is diagnosed early. Factors such as obesity, chronic anovulation, nulliparity, late menopause, unopposed estrogen use. These tumors usually start as atypical endometrial hyperplasia and progress to carcinomas. The tumors tend to be well differentiated (endometrioid type) with lower grade nuclei and usually have a more favorable prognosis. These cancers often have high-grade nuclear atypia with serous or clear cell histology. Grossly, endometrial cancer itself may appear as a single mass within the endometrium, or it may be spread diffusely throughout the endometrium. Depth of myometrial invasion is an important component in the staging and prognosis of endometrial cancer. The prognosis is dramatically worsened when the cancer has invaded more than one-half of the thickness of the myometrium. The most common route is direct extension of the tumor downward to the cervix or outward through the myometrium and serosa. When there is significant myometrial penetration, cells may spread through the lymphatic system to the pelvic and para-aortic lymph nodes. Exfoliated cells may also be shed transtubally through the fallopian tubes to the ovaries, parietal peritoneum, and omentum. Hematogenous spread occurs less frequently, but can result in metastasis to the liver, lungs, and/or bone. The most common type of endometrial cancer is endometrioid adenocarcinoma (75% to 80%). Other nonendometrioid tumor types include mucinous carcinomas (5%), clear cell carcinomas (5%), papillary serous carcinomas (4%), and squamous carcinomas (1%). Invasive adenocarcinoma usually results from proliferation of the glandular cells of the endometrium in a back-to-back fashion without intervening stroma. Histologic grade is the most important prognostic factor for endometrial carcinoma (Table 29-1). Poorly differentiated tumors have a higher grade and a higher percentage of solid (nonglandular) growth. High-grade tumors have a much poorer prognosis due to the likelihood of spread outside of the uterus. Five percent to 10% of those with premenopausal diagnoses are less than 40 years of age. The average age of diagnosis is 61; the largest affected group is between age 50 and 59. Most tumors are caught early when they are of low grade and low stage (Table 29-3); therefore, the overall prognosis for the disease is good and overall mortality rates are declining. These include a history of unopposed estrogen exposure, obesity, nulliparity, late menopause, chronic anovulation, and tamoxifen use (Table 29-4). Other risk factors include diabetes mellitus; hypertension; cancer of the breast, ovary, or colon; and a family history of endometrial cancer.

Buy motilium online
Knowing when and how to verify data is a good illustration of strategic knowledge (metacognition) gastritis symptoms bupa safe 10mg motilium. For example, the anesthesia professional must decide under what conditions it is useful to invest time, attention, and energy in establishing a new information source. If a problem is found, a decision must be made regarding its identity and its importance. This process of problem recognition (also known as situation assessment) is a central feature of several theories of cognition in complex, dynamic worlds. Given the high uncertainty seen in anesthesia, the available information sources cannot always disclose the existence of a problem, and even if they do, they may not specify its identity or origin. The experiment by Westenskow and colleagues with the intelligent alarm system mainly probed these parts of problem recognition. In 11 cases, the fault could not be identified, but compensation for the fault was successful, as described in the next paragraphs. The supervisory control level mediates the decision when a clear-cut match or "diagnosis" cannot be made. Anesthesia professionals and other dynamic decision makers use approximation strategies to handle these ambiguous situations; psychologists term such strategies heuristics. Another is to gamble on a single diagnosis (frequency gambling279) by initially choosing the single most frequent candidate event. During preoperative planning, the anesthesia professional may adjust a mental "index of suspicion" for recognizing certain specific problems anticipated for that particular patient or surgical procedure. The anesthesia professional must also decide whether a single underlying diagnosis explains all the data or whether these data could have multiple causes. This decision is important because excessive attempts to refine the diagnosis can be very costly in terms of allocation of attention. The use of heuristics is typical of expert anesthesia professionals and often results in considerable time savings in dealing with problems. Trends of physiologic parameters almost always follow curves, not steps An existing redundant channel is checked. This also adds another parameter for the method of "correlating" the quality and reliability of a measurement are checked, and its function is tested. Observation of redundant channels can also help verify a value (see above) If doubt exists about the function of a device, an entirely new instrument or an alternative backup device may be installed If the decision on the values remains unclear, help should be sought early to obtain a second opinion from other trained personnel 141 Checking trend information nonlinear fashion. Under such circumstances, which are not uncommon for natural systems such as the human body, the rate of change is almost invariably underestimated, and people are surprised at the outcome. If the weak signs of the developing problem were not detected, the ensuing catastrophe may seem to have occurred "suddenly. The classic paradigm of decision making posits a careful comparison of the evidence with various causal hypotheses that can explain them. This approach, although powerful, is relatively slow and does not work well with ambiguous or scant evidence. In complex, dynamic domains such as anesthesia, many problems require "decisions under uncertainty,"273,296 with quick action to prevent a rapid cascade to a catastrophic adverse outcome. For these problems, deriving a solution through formal deductive reasoning from "first principles" is too slow. Observing a redundant channel Correlating Activating a new monitoring device Recalibrating an instrument or testing its function Precompiled Responses and Abstract Reasoning In complex, dynamic domains, the initial responses of experts to the majority of events stem from precompiled rules or response plans for dealing with a recognized event. In the anesthesia domain, these responses are usually acquired through personal experience alone, although there is a growing realization that critical response protocols must be codified explicitly and taught systematically. When the exact nature of the problem is not apparent, a set of generic responses appropriate to the overall situation may be invoked. For example, if a problem with ventilation is detected, the anesthesia professional may switch to manual ventilation at a higher fraction of inspired oxygen (FiO2) while considering further diagnostic actions. However, experiments involving screen-only298 and realistic161,299-301 simulations have demonstrated that even experienced anesthesia professionals show great variability in their use of response procedures to critical situations. This finding led these investigators to target simulator-based training in the systematic training of responses to critical events. Prediction of Future States Problems must be assessed in terms of their significance for the future states of the patient. Prediction of future states also influences action planning by defining the timeframe available for required actions. Cook and colleagues described "going sour" incidents in which the future state of the patient was not adequately taken into account when early manifestations of problems were apparent. Abstract reasoning about the problem through the use of fundamental medical knowledge still takes place in parallel with precompiled responses, even when quick action must be taken. This seems to involve a search for high-level analogies279 or true deductive reasoning using deep medical and technical knowledge and a thorough analysis of all possible solutions. Anesthesia professionals managing simulated crises have linked their precompiled actions to abstract medical concepts. At this time, the degree to which abstract reasoning is necessary for optimal intraoperative crisis management is unknown. Reevaluation and Situation Awareness To cope with the rapid changes and profound diagnostic and therapeutic uncertainties seen during anesthesia, the core process must include repetitive reevaluation of the situation. The process of continually updating assessment of the situation and monitoring the efficacy of chosen actions is termed situation awareness. Although such direct involvement has many benefits in timeliness and flexibility of action, it also poses risks. This is particularly an issue when other tasks have been interrupted or temporarily suspended. Errors in executing a task are termed slips, as distinguished from errors in deciding what to do, which are termed mistakes. Thus, when critical incident221,305 and quality assurance studies described "technical errors" in using equipment, they were referring to slips, whereas "judgment errors" referred to mistakes. One particular type of execution error, termed a mode error,278 is becoming more frequent in all domains with the increased use of microprocessor-based instrumentation and devices. An example in anesthesiology is the "bag/ventilator" selector valve in the anesthesia breathing circuit, which selects between two modes of ventilation. Failing to activate the ventilator when in the "ventilator mode" can be catastrophic. Mode errors can also occur with monitoring or drug delivery devices if they assign different functions to the same displays or switches depending on the mode of operation selected. Particularly dangerous slips of execution can be addressed through the use of engineered safety devices that physically prevent incorrect actions. Other interlocks physically prevent the selection of a gas mixture containing less than 21% oxygen. Therefore, the anesthesia professional must strike a balance between acting quickly on every small perturbation (which requires a lot of attention) and adopting a more conservative "wait-and-see" attitude. This balance must be constantly shifted between these extremes as the situation changes. However, during simulated crisis situations, some practitioners showed great reluctance to switch from business as usual to emergency mode even when serious problems were detected. Erring too far in the direction of wait and see is an error that can be particularly catastrophic. Practitioners find false auditory alarms from monitors or other equipment extremely distracting. Expert anesthesia professionals modulate the distractions by eliminating them when the workload is high and allowing them to occur when the workload is low (to improve morale and team building). Active Management of Workload One major aspect of strategic control of attention is the active management of workload. Rather than passively dealing with rising or falling workload, the anesthesia professional actively manages it. Schneider and Detweiler187 and Gopher (position paper, Conference on Human Error in Anesthesia, Asilomar, Calif. Chapter 7: Human Performance and Patient Safety 143 theoretic basis for a variety of strategies of workload management. These strategies were addressed specifically for anesthesiology by several investigators.
Order motilium visa
Differences in the deflation limb of the pressure-volume curves in acute respiratory distress syndrome from pulmonary and extrapulmonary origin gastritis daily diet buy motilium from india. Acute lung injury and the acute respiratory distress syndrome: four decades of inquiry into pathogenesis and rational management. Neutrophil deformability in patients with sepsis, septic shock, and adult respiratory distress syndrome. Endothelium and disordered fibrin turnover in the injured lung: newly recognized pathways. A contributive result of open-lung biopsy improves survival in acute respiratory distress syndrome patients. The fibroproliferative response in acute respiratory distress syndrome: mechanisms and clinical significance. Randomized, placebo-controlled clinical trial of an aerosolized beta(2)-agonist for treatment of acute lung injury. Neuromuscular blocking agents in acute respiratory distress syndrome: a systematic review and meta-analysis of randomized controlled trials. Prone positioning reduces mortality from acute respiratory distress syndrome in the low tidal volume era: a meta-analysis. Chapter 10 Organ Dysfunction in Sepsis: Brain, Neuromuscular, Cardiovascular, and Gastrointestinal Brian J. Mikkelsen Introduction Sepsis-related organ dysfunction is common, complex, and associated with significant morbidity and mortality. Its presence defines sepsis, in addition to sepsis-related hypotension and sepsis-related hypoperfusion [1], and it has utility as a risk stratification tool to identify those at increased risk of death. Organ failure manifests in myriad ways in sepsis, mediated by a complex interplay between preexisting organ function and acute inflammation and endothelial and coagulation dysfunction incited by the infectious insult. Given the pathophysiology of sepsis-associated organ dysfunction, each organ in the body is known to manifest tissue injury in response to sepsis that is clinically apparent to various degrees (Table 10. Given the prevalence and frequent need for life support in the setting of sepsis-related respiratory and renal failure, lung injury and kidney injury are covered in separate chapters. In this chapter, we focus on non-pulmonary, non-renal sepsisassociated organ dysfunction. We begin by examining neurologic complications of sepsis, followed by examination of cardiovascular and gastrointestinal organ dysfunction. In the literature, this clinical manifestation is known as sepsis-associated encephalopathy or septic encephalopathy, in addition to the more general terms of coma or delirium. Acute brain dysfunction, defined as coma and/or delirium during the critical illness state, is common and is associated with short- and long-term morbidity and mortality. Many studies now use coma and delirium as outcomes to describe brain dysfunction in critical illness because they utilize reliable and valid measurements to define these states. At the bedside, an objective evaluation of consciousness is a vital initial step in the neurologic examination. A score of 0 corresponds to an alert and calm state, increasingly negative values correspond to deeper degrees of sedation, and increasingly positive values correspond to an increasingly agitated state [10]. Strategies to measure delirium severity appear promising [53], but require further investigation before implementation in the clinical setting. The incidence of coma and delirium among patients with sepsis is difficult to know with certainty because most studies have enrolled critically ill patients with a variety of diagnoses, and the rates may vary by disease process. However, many studies exclude patients 10 Organ Dysfunction in Sepsis: Brain, Neuromuscular, Cardiovascular. Risk Factors Studies evaluating risk factors for delirium have not exclusively enrolled patients with sepsis but provide some important findings. Observational studies in a variety of critically ill populations have reported that age [40], severity of illness [24, 40, 41, 46, 50], dementia or preexisting cognitive impairment [16, 41, 50], hypertension [45, 46], current smoking [45, 50], alcoholism [46, 50], and the use of restraints [58] are all risk factors for delirium. Based on the inflammatory hypothesis, a number of studies have investigated statins as an intervention that may mitigate the risk of delirium development or severity. Prognosis Acute brain dysfunction during sepsis is associated with worse outcomes. Furthermore, there appears to be a dose-response relationship, with longer duration of delirium. In the largest study to date, which enrolled patients with shock or respiratory failure, 34 % of patients had cognitive impairment at 1 year similar in severity to patients with moderate traumatic brain injury [14]. Prevention and Treatment Several clinical trials in a variety of critically ill populations have evaluated interventions aimed at preventing or treating coma and/or delirium. Interventions have included pharmacological and non-pharmacological interventions, as well as different sedation regimens. The most successful strategies to date have prioritized daily sedation interruption, sedation protocols, and early mobilization. Daily sedation interruption has been 10 Organ Dysfunction in Sepsis: Brain, Neuromuscular, Cardiovascular. Finally, interruption of sedation, paired with early mobilization, has been shown to reduce the duration of delirium [27]. Pharmacological interventions have included the use of antipsychotics, anticholinergics, and different sedation regimens. Antipsychotics may reduce the duration of delirium [48], but additional studies are still ongoing [26]. Rivastigmine, a cholinesterase inhibitor, was associated with longer duration of delirium and higher mortality in one study [25]. Several randomized clinical trials have suggested that dexmedetomidine may be the preferred sedative in treatment of coma and/or delirium [23, 28, 29, 78]. Sedation with dexmedetomidine is associated with lower rates of coma and more coma/delirium-free days when compared to lorazepam [23, 78] and with lower rates of delirium when compared to midazolam [29]. Ultimately, further research is needed to identify preventive and treatment options aimed at reducing rates and duration of acute brain dysfunction in order to potentially improve outcomes. Its development is associated with functional disability that frequently endures and an increased risk of long-term mortality [79]. Diagnosis Neuromuscular dysfunction in critical illness has been variably defined with some studies using clinical parameters such as muscle strength testing, others using electrophysiological testing, and some using a combination of the two. In the literature, the terms used to describe neuromuscular dysfunction are often used interchangeably prompting the proposal for uniform nomenclature and diagnostic criteria [80]. A less commonly used measure of strength is the Function Disability Score [91, 92]. Some more recent studies have evaluated the use of ultrasonography, handgrip strength [83, 90, 93, 94], or portable dynamometry [94] as diagnostic tools or measures of clinical strength but additional studies are necessary.