Purchase 100mg mycelex-g
Bruising at the port site on transillumination can help to identify suspected trauma fungus under armpits purchase mycelex-g online. Operating near large vessels Lymphadenectomy, presacral neurectomy, and surgery for deep endometriosis all carry a high risk of trauma to large vessels, especially in the presence of anatomical distortion. In adnexal surgery the surgeon must be aware of the course of the internal iliac vessel along the pelvic sidewall and resist the temptation to rest adnexal tissue on this area during dissection; instead, adnexal tissues should be lifted away from the sidewall. The same error occurs if the Trendelenburg position is erroneously assumed before trocar entry. Choice of mode of access There is no difference in the rate of vascular complications when comparing various entry techniques, including Veress needle insufflation before trocar entry, open (Hasson) entry, or optical trocar entry [6]. I prefer an optical trocar for the primary port, but this is only useful if the camera head is properly oriented during trocar insertion and the trocar movement is controlled. If a laparoscope is in place, efforts should be made to maintain visualization by placing the distal lens outside the angle of the spurting blood vessel. If the trauma has occurred during Veress needle placement (as indicated by the aspiration of blood in the case history), the needle should be left in place so that the puncture can be identified easily at further exploratory surgery. The operative team needs to prepare for a midline laparotomy, which will be necessary in almost all cases. Until the vascular surgeon arrives, direct pressure ought to be applied to the traumatized vessel. In some situations, as judged by the vascular surgeon, large veins may be ligated, but large arteries always require repair. Repair can be undertaken with clips, fine sutures such as 50 Prolene, reanastomosis, or by using grafts. Only very accomplished laparoscopic surgeons should attempt laparoscopic vessel repair. Other techniques include the laparoscopic application of clips or oversuturing while the leak is compressed with a nontraumatic grasper. If there is bleeding at trocar removal, bipolar electrosurgery should be attempted. Failing this, a suture can be placed across the lesion and tied extracorporeally below the skin surface within the incision. This is best achieved under laparoscopic vision with an Endoclose system or a Jneedle. While waiting for the vascular surgeon, the vascular puncture should be compressed. The lesion is then repaired by occlusion (ligation or bipolar desiccation) for some veins, or repair (clips, fine sutures) for veins and all arteries. Adnexal structures should always be pulled away from the sidewall vessels for dissection. The relationship of the umbilicus to the aortic bifurcation: implications for laparoscopic technique. An ultrasound scan shows a 20-cm anechoic adnexal cyst thought to be of ovarian origin. Case history 2: A 25-year-old woman is referred with a 2-year history of intermittent pelvic pain. A transvaginal ultrasound scan shows a 12-cm left ovarian mass consistent with a benign dermoid cyst. Background In premenopausal women almost all ovarian masses and cysts are benign [1]. While many ovarian masses in premenopausal women can be managed conservatively given their generally benign nature and the high likelihood of spontaneous resolution, surgical intervention is indicated in both case histories presented. This is because spontaneous resolution is unlikely in cysts over 10 cm in size and both women are symptomatic [2]. At any point where borderline or frank malignancy is suspected, the involvement of a gynecologic oncologist should be sought and laparoscopic management may be contraindicated, although interestingly there are no differences in rates of intraoperative cyst rupture between laparotomy and laparoscopy [1]. The large, benign, ovarian mass presents surgical challenges for the laparoscopic surgeon. Once the decision for laparoscopy has been made, it is important to warn the patient that a laparotomy may become necessary if laparoscopic approach is technically unfeasible or complications arise at laparoscopy. Patients should also be aware that oophorectomy is a possibility if no normal ovarian tissue is identified, to stem bleeding, or where malignancy is suspected. A decision should be made on whether removal of the intact cyst is desired, and the method of cyst extraction from the peritoneal cavity should be devised. Management In Case history 1, the presence of the large mass is causing the abdominal distension and while the origin of the cyst is uncertain, it is likely to be ovarian or tubal. In Case history 2, while the intermittent pain may be arising from the presence of the mass. However, in light of its size and complex ultrasonic appearance, albeit in keeping with a commonly encountered benign teratoma (and reassuringly normal serum tumor markers), surgical removal is necessary to obtain histology, treat symptoms, and prevent ovarian cystic accidents. Management of a simple cyst In Case history 1, the appearances are in keeping with a benign, mobile, simple cyst and the patient is slim so laparoscopic surgery should be feasible. The mass should be inspected carefully to determine its origin, mobility, and nature. The contralateral ovary should be identified and inspected to confirm normality should oophorectomy rather than cystectomy become necessary. The rest of the abdominal cavity including the liver, omentum and peritoneum will need inspection and any free fluid should be aspirated and sent for cytologic evaluation. The cyst should be incised to allow decompression, with all fluid contents removed via suction and sent for cytology. Ovarian cystectomy should then be undertaken using standard laparoscopic techniques. Despite the simple nature of the collapsed cyst, its sheer size is likely to make extraction of the material from the abdomen difficult. Options include the use of a standard retrieval bag though an enlarged port site with or without further decompression or debulking, a mini-laparotomy, Gynecologic and Obstetric Surgery: Challenges and Management Options, First Edition. Management of a dermoid cyst the surgical approach for Case history 2 is more challenging because intraperitoneal spillage of the dermoid cyst contents can potentially result in chemical peritonitis. Indeed, in one published series of 600 dermoid cystectomies, spillage occurred in 65% of cases although chronic granulomatous peritonitis developed in only one patient [4]. Three different surgical approaches for cystectomy or oophorectomy are justifiable: (i) laparotomy, (ii) laparoscopy with mini-laparotomy for exteriorization of the ovary, or (iii) laparoscopy alone. In light of the potential sequelae of rupturing a dermoid cyst, a laparotomy may not be unreasonable. However, a careful laparoscopic approach to mobilize, dissect and enucleate the cyst, the use of additional ports as required, and the judicious use of an endoscopic bag during surgery can avoid or reduce any leakage of cyst material into the peritoneal cavity [3,4]. In contrast to many "functional" ovarian cysts, the cyst wall of a benign teratoma is fairly robust and the avoidance of cyst rupture during enucleation is feasible in most cases. The intact cyst can then be removed from the abdominal cavity by puncturing and evacuating the cyst within a retrieval bag. However, laparoscopic pelvic access is restricted with larger cysts and the bag apertures often of insufficient dimension to accommodate such a cyst. Placement of an open retrieval bag under the dermoid cyst during dissection, with the aim of minimizing the risk of abdominal spillage of intracystic material, has been advocated along with preliminary cystic puncture prior to intraperitoneal cystectomy or oophorectomy depending on the size of the cyst and the preference of the surgeon [4]. At the end of the procedure, in addition to the usual checks for adequate hemostasis, a thorough washout of the abdominal cavity is indicated, especially where intraperitoneal spillage of cystic contents has occurred. All specimens should be sent for histologic assessment and most patients can be discharged within 24 hours of surgery. Laparoscopic management of ovarian dermoid cysts: potential fear of dermoid spill, myths and facts. Does prevention of intraperitoneal spillage when removing a dermoid cyst prevent granulomatous peritonitis Her dating scan confirms her gestation and detects a 12-cm anechoic simple-looking left-sided ovarian cyst.
100 mg mycelex-g visa
Intubation with an endotracheal tube by an anesthetist is recommended in pregnant patients as there is more risk of aspiration of gastric contents due to decreased gastric motility and reduced lower esophageal sphincter tone antifungal nail gel proven 100 mg mycelex-g. Intubating a pregnant patient can be more difficult because of airway edema and increased breast tissue. The pads may be positioned in anterior and posterior positions on the left side of the chest as it may be difficult to position the apical pad in a left-tilted position [3]. Intervening and treating the patient in response to early signs of demise may prevent deterioration to the point of arrest. Management of cardiac arrest the cardiac arrest team should be called, including an obstetrician and a neonatologist. Good-quality basic life support (chest compressions and ventilation) should continue throughout the arrest. Causes and management the reversible causes of cardiac arrest are denoted by the four "H"s and four "T"s Table 58. In the pregnant patient, causes may be pregnancy-related or a result of conditions unrelated to pregnancy. In pregnancy, the most likely causes of cardiac arrest are cardiac disease, hypovolemia due to sepsis, hemorrhage, or thromboembolism [4]. Other pregnancy-related causes include amniotic fluid embolism, drug overdose, anaphylaxis, intracerebral hemorrhage, and eclampsia [2]. Pregnant patients are more at risk of hypoxic brain injury than non-pregnant patients because of a higher oxygen consumption and lower oxygen store. Delivering the fetus reduces oxygen consumption and improves venous return, thereby improving cardiac output by up to 80% [1]. A perimortem cesarean section should be performed in women at more than 20 weeks of gestation. Perimortem cesarean section should occur at the scene of the resuscitation, and equipment (at least a scalpel and two cord clamps) should be immediately available on the cardiac arrest trolley. A classical incision is used as it provides quicker access to the uterus [1] but a transverse incision may be used if the operator is more familiar with this technique [2]. Releasing the insufflating gas usually restores venous return and thereby improves heart rate. Atropine or glycopyrrolate may be given by the anesthetist to increase heart rate. Less common reasons include amniotic fluid embolism, drug overdose, anaphylaxis, intracerebral hemorrhage, and eclampsia. The patient and her family will also need a debrief, and may require ongoing support. Documentation is important; assigning a scribe during the arrest will aid accurate documentation of events later. Cardiac arrest team should be called, and cardiopulmonary resuscitation must commence immediately. Deficiencies in provision of cardiopulmonary resuscitation during simulated obstetric crises. Case history 2: In preparation for a fibroid resection, the surgeon attempts to dilate the cervical canal to 10 mm, but is unable to advance beyond a size 7 Hegar dilator. In the presence of ongoing difficulty, an alternative approach for accessing the uterine cavity may need to be considered and the strength of the indication for the procedure reviewed. Rather than persevering, the procedure may need to be rescheduled after cervical preparation using mechanical or chemical agents. Background Cervical dilatation to 10 mm and occasionally even up to 12 mm may be necessary for operative procedures such as surgical manage ment of miscarriage, termination of pregnancy, and resection of submucous fibroids or the endometrium. The surgical instruments need to move freely in and out of the uterus; a tight or stenosed cervix will hinder the operation, and may increase the risk of complications. Cervical stenosis may preclude access to the uterine cavity so that the desired operation cannot be performed. Dilatation of the cervix risks traumatizing the genital tract; cervical laceration, "false passage" creation, and uterine perforation can arise leading to substantial bleeding and damage to adjacent structures (Chapter 60). Application of a tenaculum on the anterior lip of the cervix can help to apply gentle traction to straighten the cervicouterine canal and reduce resistance to the insertion of a dilator or minihysteroscope. If the patient is awake, she should be warned in advance about a sharp sensation that often results from application of a tenaculum; very slow application of the tenaculum can minimize the discomfort. Cervical counter-traction Cervical dilatation Semiflexible and graduated "osfinding" probes or graduated rigid cervical dilators can be used to dilate the cervix. However, there is a substantial risk of creation of a false passage or perforation, and therefore the procedure should be carried out under abdominal ultrasound guidance. A good "acoustic window" can be created for the abdominal ultrasound by filling the bladder with 200 mL of sterile water or saline. Fine dilators, including lacrimal duct dilators, can be useful for probing a severely stenosed cervix; however, false passages and perforations are more likely with fine dilators, and a slightly larger dilator can sometimes be easier to pass through the cervical canal because it will ride over the small culdesacs in the endocervical canal [1]. Management Cervical stenosis If cervical stenosis is identified, a number of management steps can be taken. Diagnostic singleflow minihysteroscopy systems are available, typically incorporating a 1. It is important to avoid trauma and bleeding from the endocervical canal as this will impair the views and predispose to false passages and perforations. Slow advancement of the hysteroscope will allow the distension media to open up the canal, thus reducing resistance to the instrument and likelihood of cervical canal injury. As the hysteroscope is advanced, it is important to take note of any turns and twists in the canal, because this knowledge will be informative if blind dilatation is subsequently needed. It may be possible to suture if the bleeding vessel(s) can be seen directly or after splitting the cervix to identify the bleeding vessel(s) [1]. If the bleeding vessel(s) cannot be identified, the uterine artery on the side of the injury can be exposed, as in a vaginal hysterectomy, and sutured [1]. A bleeding cervical or uterine artery branch can also cause a hematoma that can extend into the broad ligament. Intracervical vasopressin A randomized trial found that intracervical injection of 20 mL of dilute vasopressin solution (0. Resolution of the cases Case history 1 A thorough pelvic examination to evaluate the size and the position of the cervix and the uterus is needed. Gentle probing with a small dilator, os finder, or minihysteroscope (with saline flow turned on) can remove flimsy adhesions and identify the external cervical os. A concomitant pelvic ultrasound scan can provide information on the site and axis of the cervical tract to facilitate these measures. Where the external cervical os is obliterated, cutting into the cervix under direct hysteroscopic vision should be undertaken. Deeper cervical excision to identify the cervical canal should rarely, if ever, be required and only by appropriately experienced practitioners after other options described in this chapter have been exhausted. Case history 2 Intracervical injection of dilute vasopressin may aid further dilatation. If dilatation is not possible, then there are two options: (i) use an alternative method to complete the operation. Despite various remedial measures, it may not be possible to dilate beyond a certain diameter in some women. In such situations, modifying the approach to use smaller instruments or an altogether different approach may be necessary. For small submucous fibroids, ablation using bipolar electrodes placed down smaller diameter continuousflow operating systems (typically <6 mm) can be an alternative to resection. If the purpose of the procedure is to obtain an endometrial sample, then ultrasoundguided transvaginal endometrial aspiration is an alternative option [3]. Use of alternative instruments Cervical closure If an external os is not identifiable, this could be because there are flimsy adhesions over it or the cervical canal has closed, often following cervical surgery.
Buy mycelex-g 100mg fast delivery
If the secondary oocyte is penetrated by a the second 18 division forms an 19 and a second 20 fungus define generic mycelex-g 100 mg amex, each with 21 chromosomes. Female Sexual Response Write the words that complete the sentences in the spaces at the right. Sexual stimulation results in enlargement of the 1 and 1) breasts, and erection of the 2 bulbs of the vestibule and 2) nipples due to increased blood flow. Sexual response culminates in 4, which produces rhythmic contractions of the pelvic floor, 5, and 6 tubes plus intense pleasure. Between puberty and 1, a woman experiences one 1) reproductive cycle per month consisting of an ovarian cycle and a 2 cycle. A cycle is started by the secretion of release of 6 5 by the hypothalamus, which activates the and a small amount of 7 by the anterior 2) 3) 4) 5) 6) 7) 8) 9) 10) 11) 12) 13) 14) 15) 16) 17) 18) lobe of the pituitary. Disorders of the Reproductive Systems Write the disorders that match the statements in the spaces provided. Sexually Transmitted Diseases 1) Results from infection with herpes simplex virus type 2. Failure of the testes to descend into the scrotum (cryptorchidism) causes sterility in males. Secondary amenorrhea in female athletes results from strenuous activity, which blocks the hypothalamic regulation of reproduction. Women with amenorrhea produce little, if any, estrogens, which causes osteoporosis (bone loss). A 1 oocyte containing 2 chromosomes is 1) 2) 3) 4) 5) 6) 7) 8) 9) 10) 11) 12) 13) 14) 15) 16) 17) 18) 19) 20) 21) 22) b. After entering a 4 tube, it is slowly carried toward the through peristalsis 6 of the cells lining the tube. The sperm the uterus and on into the usually encounter the secondary oocyte in the 10 portion of a uterine tube. The 12 disperse the of the sperm releases enzymes that 13 cells surrounding the secondary 14 8 5 enters the secondary oocyte, chemical changes in the 15 prevent other sperm from entering. The secondary oocyte immediately completes the 16 meiotic division, forming an 18 17 and another polar body, each containing chromosomes. Fetal Development Write the appropriate numbers indicating the weeks of development that match the statements in the spaces at the right. Hormonal Control of Pregnancy Write the terms that match the statements in the spaces at the right. As the time of birth approaches, the high blood concentration of 1 overrides the inhibitory effect of 2 on uterine contractions so that such contractions are possible. The 3 feedback mechanism controlling labor seems to be started by pressure of the fetus on the 4, which triggers the formation of 5 that are carried to the hypothalamus. The stimulates the posterior lobe of the pituitary to release 7, which stimulates uterine 8. The continued dilation of the 9 increases the frequency of 10 sent to the hypothalamus, which, in turn, stimulates the posterior lobe of the pituitary to release more 11, which increases the strength and frequency of uterine 12. This pattern of positive feedback produces increasingly stronger contractions until the fetus is 13. Shortly after birth, uterine contractions cause the detachment and expulsion of the 14. After the first breath, breathing becomes easier because 18 in the alveoli keeps the 19 open. Write the terms that match the statements relating to fetal circulation in the spaces at the right. Write the words that complete the sentences regarding fetal circulation in the spaces at the right. Oxygenated blood is carried from the placenta by the 2 vein that enters the fetus at the 3. This vessel divides near the liver, allowing about half of the oxygenated blood to pass through the 4, bypassing the liver, and mixing with deoxygenated blood in the inferior 5. When this mixed blood enters the atrium, most of it passes through the 7 into the 8 atrium and then into the 9 ventricle. However, most of it bypasses the lungs by flowing through the 12 into the aortic arch. A small amount of blood is carried by 14 arteries to the nonfunctional lungs and returned to the left 15. Write the terms that match the statements relating to postnatal circulatory changes in the spaces at the right. After birth, the drop in the blood levels of 1 and 2 allows the hypothalamus to secrete which stimulates secretion of 4 1) 3, 2) 3) 4) 5) 6) 7) 8) 9) 10) 11) 12) 13) by the anterior lobe of the pituitary, promoting lactation. Suckling stimulates formation of 9 that are carried to the hypothalamus, causing it to secrete 10, which continues production of prolactin in order to maintain 11. The hypothalamus also stimulates the posterior lobe of the pituitary to release 12, which stimulates 13 through the contraction of specialized epithelial cells within the mammary glands. Disorders of Pregnancy, Prenatal Development, and Postnatal Development Write the terms that match the statements in the spaces at the right. Indicate the possible genotypes of gametes that can be formed by parents with these genotypes. Recessive sex-linked traits appear more frequently in females since they have two X chromosomes. Genetic counseling may be helpful for prospective parents with genetic disease in their family histories. When the sperm count in semen falls below 20 million/ml, male infertility results. Why can monozygotic twins receive blood transfusions from each other without difficulty, whereas dizygotic twins often cannot Mary and Joe have discovered that they are both heterozygous for sickle-cell disease. They want to know what the chance is that their children will inherit sickle-cell disease. Both the prefix and the suffix modify the meaning of a root word, and they may be used with many different root words. Root words often occur at the beginning of a term, but they also may end a term or may be sandwiched between a prefix and a suffix. When determining the meaning of a term, you start with the suffix, then move to the prefix, and finally consider the root word. For example, when linking gastr- and -pathy to form a term meaning disease of the stomach, the vowel o is inserted to form gastropathy. For example, gastr/o/enter/o/col/itis means inflammation of the stomach, intestine, and colon. You can see that once you know the meaning of common prefixes, root words, and suffixes, understanding medical terminology becomes much easier. In the sections that follow, some common prefixes, suffixes, and root words are listed along with examples to help you understand medical terminology. Singular and Plural Endings Most medical terms are derived from Greek and Latin words. A active immunity Immunity derived from activation of B cells and T cells by an invasion of a pathogen. Addison disease An endocrine disorder caused by a hyposecretion of hormones by the adrenal cortex. Alzheimer disease A disorder caused by a loss of cholinergic neurons in the brain and characterized by loss of memory. B B lymphocyte A lymphocyte that develops into an antibody-producing plasma cells; a B cell. Broca area the portion of the frontal lobe of the cerebrum that coordinates muscles involved in speech. C calcitonin A hormone secreted by the thyroid gland that decreases the Ca2+ level of the blood. Glossary 541 cleavage the early divisions of a zygote leading to the formation of a morula.
| Comparative prices of Mycelex-g | ||
| # | Retailer | Average price |
| 1 | SUPERVALU | 873 |
| 2 | Apple Stores / iTunes | 635 |
| 3 | Meijer | 763 |
| 4 | Giant Eagle | 816 |
| 5 | Big Lots | 433 |
| 6 | YUM! Brands | 491 |
| 7 | Kroger | 185 |
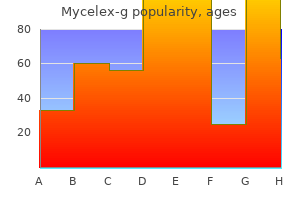
Buy mycelex-g line
Vaginal misoprostol can be administered either by the woman herself or by a clinician fungus gnats in worm bin buy discount mycelex-g 100mg on-line. The majority of abortions in the second trimester will be performed under general anesthesia, although there is increasing evidence that Gynecologic and Obstetric Surgery: Challenges and Management Options, First Edition. Typical regimens include an intravenous opioid (such as fentanyl) plus an intravenous sedative (such as midazolam or propofol). Vacuum aspiration is appropriate up to 14 weeks of gestation, although it may be done up to 16 weeks with the use of specialized instrumentation, namely using a large-bore cannula and tubing or completion of the abortion (to remove larger fetal parts) using a forceps. For gestations of 20 weeks and above, the amount of fetomaternal hemorrhage should be assessed using either the traditional Kleihauer acid elution test or the more accurate flow cytometry. If the test indicates a fetomaternal hemorrhage of over 4 mL, additional anti-D IgG should be administered. Initiation of contraception immediately following induced abortion has several advantages. Sterilization can be safely performed at the time of induced abortion, although the risk of regret should be considered. Routine histopathology assessment and gestational trophoblastic neoplasia screening are not recommended. In general, abortion service providers arrange for fetal material from late medical and surgical abortions to be incinerated. Unlike uterine fibroids, which are located within the peritoneal cavity, cervical fibroids are most commonly retroperitoneal. They may be classified according to their anatomic location; anterior, posterior, lateral, or deep-rooted/ vaginal. In rare circumstances they may be found prolapsing into the vagina and are then considered submucosal or polypoidal. Unlike fibroids originating in the uterine body, cervical fibroids are most often solitary tumors. They may grow rapidly, and because of their retroperitoneal location, may often reach massive sizes before symptoms manifest [2]. Symptoms of cervical fibroids include pressure effects on surrounding pelvic organs such as the bladder, urethra, and rectum. Symptoms can include urinary retention or frequency, constipation with tenesmus, back pain, or dyspareunia. Reproductive sequelae of cervical fibroids include infertility with anatomic blockage of the endocervical canal or uterine cavity, recurrent pregnancy loss, and obstruction of labor with dystocia leading to high rates of cesarean delivery, cesarean hysterectomy, postpartum hemorrhage, and blood transfusion [3]. Preoperative examination of women with cervical fibroids will reveal a fixed mass with little or no mobility. In cases of intracervical and submucosal cervical fibroids, the cervical os is often dilated. In cases of large cervical fibroids, acoustic shadowing may limit the ability of sonography to determine the fibroid location with accuracy. Management Angiographic embolization of the uterine artery for cervical fibroids yields poor results, with incomplete necrosis of the fibroids in 8 of 10 patients (80%) in one series [4]. This is largely thought to be due to the fine plexus of collateral vessels supplying the cervix, which may not even be visualized on standard angiography and are thus not amenable to embolization. Collateral arterial supply is vast and often aberrant, incorporating the cervico-vaginal or descending branch of the uterine artery and branches of the ovarian, vaginal, and middle hemorrhoidal arteries. Reported complications with attempts at embolization of these fibroids include vaginal expulsion of fibroid material and necrosis of the vagina. Surgery for cervical fibroids should only be undertaken in appropriately equipped settings, by expert pelvic surgeons who are skilled in radical dissection of the pelvis, as there are challenges from the large size, retroperitoneal location, and close proximity of Gynecologic and Obstetric Surgery: Challenges and Management Options, First Edition. Impaction and distortion of normal pelvic anatomy increases the risk of operative complications such as urinary tract injury, inadvertent enterotomy, and massive intraoperative hemorrhage. Cervical fibroids are typically fixed in place even after peritoneal flaps and deep attachments are freed. In rare circumstances, vaginal fibroids have been discovered postoperatively and are thought to be due to either incomplete excision of cervical fibroids or possibly inadvertent expulsion of cervical fibroid cells into the adjacent spaces [6]. Fertility-sparing surgery Vaginal myomectomy (Chapter 96) In cases of a prolapsing submucosal or polypoidal cervical fibroid, a vaginal myomectomy can be considered. Care should be taken as these fibroids can grow large enough to completely fill the vaginal vault, limiting safe and easy access from a vaginal approach. In these cases where a stalk or sessile attachment is identified, infiltration of the fibroid with dilute vasopressin aided with careful blunt and sharp dissection should be used to remove the fibroid and its attachment from the cervix [7]. Blindly twisting out the fibroid without a thorough understanding of its origin and attachment may cause damage to the myometrium and hemorrhage. Abdominal myomectomy Abdominal myomectomy, performed either by a laparoscopic or open route, should be the fertility preservation procedure of choice for cervical fibroids that are intracervical or deep-rooted within the cervix. Bilateral uterine artery ligation where they originate as a branch of the internal iliac artery should be considered at the onset of surgery. The origin of the uterine artery is located by placing gentle traction along the obliterated umbilical ligament on the lower anterior surface of the peritoneum, which will place the anterior division of the internal iliac artery under tension. In cases where the fibroid is completely filling the pelvic cavity, access to the retroperitoneal space may not be possible. In such cases the use of angiographic interventional procedures should be contemplated. A transverse incision is made along the prominent portion of the cervical fibroid at the proximal junction of the fibroid and the uterine body, taking care to prevent injury to nearby organs such as the bladder (anterior fibroid), rectum (posterior fibroid), and ureters (lateral or deep-rooted fibroid). If possible, the fibroid is then completely enucleated with the use of a myoma screw placed to provide traction. Because of their large size, there may be a lack of space for application of traction and counter-traction. If the fibroid cannot be enucleated completely due to limited working space in the pelvis, in situ morcellation can be performed [9]. A transverse incision is made at the anterior-most aspect of the fibroid in order to expose the fibroid capsule. After ensuring the rectum, both ureters, and uterine arteries are adequately separated, the fibroid is enucleated or morcellated. An incision is made within the peritoneum overlying the broad portion of the fibroid and the capsule is identified. Morcellation or enucleation proceeds after identification and separation of the ureter and ligation of the uterine vessels. Once the fibroid is pushed in a cephalad manner, it will be accessible within the pelvis, and the fibroid may be approached in a similar manner to subserosal fibroids. In all cases, the base of the capsule should be coagulated to reduce bleeding and the cervix is then closed in multiple layers; consideration should be given to placing a drain within the cul-de-sac as there is likely to be serous oozing from the bed of the tumor that may lead to a pelvic collection and postoperative febrile illness. Cervical fibroids obliterate the vaginal fornices making an anterior or posterior colpotomy difficult, and ligation of the uterine arteries prior to fibroid removal impossible from a vaginal approach. After access to the peritoneal cavity is obtained, a complete retroperitoneal dissection is performed in order to facilitate safe dissection of the anterior, lateral, and posterior aspects of the fibroid from the bladder, ureter, and rectum, respectively. When undertaking a hysterectomy, ligation of arterial blood supply, careful ureterolysis, and maximal debulking of the cervical fibroid are advisable in order to maintain adequate hemostasis, protect the genitourinary tract, and correct anatomic distortions of the uterine cervix prior to proceeding with hysterectomy. If debulking is not undertaken, then a modified radical abdominal or laparoscopic hysterectomy can be undertaken. Ligation of the uterine arteries is then performed at their origin from the anterior branch of the internal iliac artery. In cases of large intracervical fibroids, the walls of the cervix will be severely attenuated.
Best order for mycelex-g
Modern bipolar resectoscopes can be used with normal saline medium fungus gnats basil buy mycelex-g overnight delivery, reducing the risk of electrolyte imbalance from fluid overload (Chapter 63). As with D&C, hysteroscopic surgery can be combined with hemostatic interventions such as ligation of the cervical branch of the uterine artery [26] and laparoscopic uterine artery ligation [27]. The following criteria have been suggested for determining when to consider the use of hysteroscopic resection after a failed medical treatment [12]. Interventional radiology Interventional radiology should be considered in both the stable and unstable patient. Embolization of the major pelvic arteries has been successfully used in conjunction with medical or surgical treatments. The radiologic procedure can also be used to control acute hemorrhage in association with a laparotomy. Cervical pregnancy treated with systemic methotrexate administration and resectoscopy. Methotrexate in local treatment of cervical heterotopic pregnancy with successful perinatal outcome: case report. Prognostic factors for an unsatisfactory primary methotrexate treatment of cervical pregnancy: a quantitative review. Cervical ectopic pregnancy: diagnosis with endovaginal ultrasound examination and successful treatment with methotrexate. Cervical pregnancy after in vitro fertilization and embryo transfer successfully treated with methotrexate and intracervical injection of vasopressin. Cervico-isthmic pregnancy successfully treated with bipolar resection following methotrexate administration: case report and literature review. Differential diagnosis of suspected cervical pregnancy and conservative treatment with the combination of laparoscopyassisted uterine artery ligation and hysteroscopic endocervical resection. Clinical observations are normal and examination reveals no abdominal masses or tenderness. A transvaginal ultrasound scan detects the presence of a gestation sac containing a fetal pole with cardiac activity consistent with a 7week pregnancy in the anterior part of the uterine isthmus. The uterine cavity and cervical canal are noted to be empty and without any apparent contact with the gestation sac. Thus, in such circumstances, as for other types of ectopic pregnancy, surgical management is an option alongside or in conjunction with expectant and medical approaches. Systemic use of methotrexate and/or local injection of embryocides including methotrexate, potassium chloride, hyperosmolar glucose, and crystalline trichosanthin have been described [4] usually under transvaginal imaging, although hysteroscopy has also been employed. While medical approaches are less invasive compared with surgery, they may simply interrupt the pregnancy, such that trophoblast remains and symptoms continue with heavy bleeding. Furthermore, it can be difficult to exclude scar dehiscence developing during the process of treatment. Surgically, the uterine isthmus is accessible via vaginal, uterine, hysteroscopic, laparoscopic, and laparotomic routes. The apparent increased incidence also mirrors the inexorable rise in cesarean delivery. The gestational age at diagnosis appears to range from 5+0 to 12+4 weeks with a mean of 7. There is a consensus, however, that termination of the ectopic pregnancy in the first Medical treatment combined with surgical sac aspiration Here the contents of the gestation sac are disrupted and aspirated usually under ultrasound guidance after prior medical treatment. The minimal invasiveness of this enhanced "medical" technique needs to be weighed against the probability of incomplete treatment and ongoing symptoms. Various adjuvant hemostatic measures have been described to prevent or control hemorrhage and these include local injection of vasopressin, intrauterine balloon tamponade, placement of a Shirodkar suture, selective bilateral uterine artery embolization, and even bilateral uterine artery ligation [4]. However, rupture of the uterine scar where the chorionic villi of the ectopic pregnancy have implanted remains a major risk that would necessitate immediate laparoscopy or laparotomy to rectify. Advanced hysteroscopic skills are required to visualize and coagulate the blood vessels at the implantation site to prevent severe intraoperative hemorrhage. Adequate distension and visualization of the surgical field at the level of the uterine isthmus may be problematic and uterine rupture, although unreported with this technique, remains a possibility. Bleeding can be minimized by local injection of vasopressin and meticulous hemostasis using bipolar diathermy. Open surgical removal the surgical method is as described using a laparoscopic approach. The open approach is more invasive with prolonged hospital stay compared with vaginal and laparoscopic techniques, but is within the skill set of most practicing gynecologists. A laparotomy may allow a more extensive "wedge" resection of the lesion and complete excision of the old cesarean scar. In the latter circumstance, fertilitysparing hemostatic interventions such as bilateral uterine artery ligation or embolization should be considered prior to removing the uterus. Thus, early detection and therapeutic intervention in the first trimester is of prime importance to minimize subsequent morbidity. Pregnancy following prior Caesarean scar pregnancy rupture: lessons for modern obstetric practice. First trimester diagnosis and management of pregnancies implanted into the lower uterine Caesarean section scar. She described the pain as severe with acute exacerbations coming in waves and associated with nausea and vomiting. An ultrasound scan performed 3 months previously for intermittent abdominal pains had shown an enlarged right ovary (7 cm) containing three dermoid cysts, with no visible left ovary. She had a past gynecologic history of a laparoscopic left ovarian cystectomy for a dermoid cyst. On examination, the abdomen was soft, with tenderness and guarding in the right lower quadrant. Bimanual pelvic examination revealed cervical motion tenderness and a suspected mass in the right adnexa with tenderness on that side. A transvaginal ultrasound was performed the following day that showed a 9-cm right adnexal mass containing echogenic material consistent with dermoid cysts. By the time this was done she had been in pain for over 72 hours and the ovary was congested and appeared friable and necrotic. Only a streak of ovarian tissue was visible on the left side due to her previous ovarian cystectomy. The right ovary was detorsed and the decision made that, on balance, it was worth attempting to preserve the right ovary rather than risk an iatrogenic menopause and infertility. However, at clinical review 12 days later the patient complained of feeling feverish and on scan the ovary appeared non-viable, with no detectable perfusion on Doppler examination. Postoperatively, she did not resume taking her combined contraceptive pill and her periods resumed a couple of months later. A small left ovary was seen on follow-up scan, and the patient conceived naturally after a year. Torsion causes reduced venous return from the ovary and, as a result, is associated with stromal edema and congestive hemorrhage into any underlying ovarian lesion. The clinical presentation is often non-specific with few distinctive clinical signs, commonly resulting in delay in diagnosis and surgical management. The clinical history is typically very similar to that of renal colic and the pain is often associated with nausea and vomiting [2]. Torsion may occur at any age, with an underlying ovarian lesion being more common with increasing age [3]. A quick and confident diagnosis is required to save the adnexal structures from infarction and irreversible tissue necrosis, particularly in women who wish to retain their fertility. Ultrasound (and other imaging modalities) have high positive predictive values for torsion, but relatively poor negative predictive values, and are also highly operator dependent. This means that if the ultrasound scan is suggestive of torsion, then it is very likely to be present, but a negative scan does not exclude torsion [4], so a diagnostic laparoscopy may be necessary. Management preoperative preparation Before embarking on surgery for suspected adnexal torsion, there should be a clear plan. Does he or she have the surgical skills necessary to deal with torsion if it is confirmed There is little to be gained in attempting to preserve the ovary of a woman who is certain that her family is complete or who is over 45 years of age. This will also affect decision-making regarding the urgency and timing of surgery. This is particularly a consideration in a postmenopausal woman as a staging procedure may be the optimum treatment.
Cheap mycelex-g online master card
Infraclavicular "blowholes" (bilateral skin incisions under the clavicles) to allow the trapped air to escape have also been described [7] xylecide anti fungal shampoo reviews order 100mg mycelex-g amex. If this is noted, then the patient should be examined, including palpation of the anterior chest and neck for crepitus. Tachycardia, loss of cardiac dullness, decreased Gynecologic and Obstetric Surgery: Challenges and Management Options, First Edition. The operative time should be minimized and the most experienced surgeon should complete the operation. The risk of interstitial insufflation can be minimized by careful placement of the Veress needle and trocar at exactly the base of the umbilicus where all layers of the anterior abdominal wall fuse. Investigations including a chest X-ray and arterial blood gases are needed to understand the extent of the complication. If airway compromise is suspected, ventilation will need to be continued for longer. Massive emphysema can result in severe acidosis, hypercarbia, upper airway obstruction, pneumomediastinum, pneumopericardium, pneumothorax, and gas embolism. If emphysema extends to the upper body, consider termination of the operation or conversion to laparotomy. Subcutaneous carbon dioxide emphysema following endoscopic extraperitoneal hernia repair: possible mechanisms. Risk factors for hypercarbia, subcutaneous emphysema, pneumothorax, and pneumomediastinum during laparoscopy. Massive subcutaneous emphysema and hypercarbia: complications of carbon dioxide absorption during extraperitoneal and intraperitoneal laparoscopic surgery. Subcutaneous carbon dioxide emphysema following laparoscopic salpingo-oophorectomy: a case report. Case history 2: A 30-year-old female is undergoing an elective cesarean section under spinal anesthesia for a breech presentation. Air is the commonest gas entrained; however, embolism from carbon dioxide and nitrous oxide can also occur [2]. Carbon dioxide used for laparoscopic abdominal insufflation is more soluble than other gases, and thus any carbon dioxide gas embolism will dissolve over time [3]. They can be classified as patient-related, anesthesia-related, and surgery-related Table 69. Intravascular gas may travel from its site of entry to the right atrium and subsequently to the right ventricle, where it can produce an "airlock" obstructing outflow to the pulmonary circulation and increasing pulmonary vascular resistance [3]. This presentation is more common following introduction of a large bolus of air (approximately 5 mL/ kg) into the venous circulation [2,5]. If sufficient pressure builds up in the right ventricle, the air trapped in the right ventricle can be pushed through the pulmonary circulation and into the left atrium, producing a paradoxical air embolism [2]. More gradual air entrainment leads to microemboli, which not only obstruct flow but also stimulate neutrophils, fibrin, red blood cells, fat globules, and platelets to bind to the air bubbles [2]. These physical and chemical responses can lead to increased basement membrane permeability and subsequently pulmonary edema [2,6]. Moderate gas entrainment can lead to significant right ventricular outflow obstruction with subsequent reduction in cardiac output, resulting in hypotension and myocardial and cerebral ischemia [5]. Diagnosis Clinical signs and symptoms vary and presentations can range from subclinical suspicion to acute life-threatening events. The awake patient may complain of severe chest pain, breathing difficulties, light-headedness, and a sense of impending doom [2,5]. The classical "millwheel" murmur heard on precordial auscultation is insensitive and is often a late sign. In severe cases cardiovascular instability will require management with inotropes and vasopressors. Rapid intravenous fluid boluses should be administered in an attempt to increase venous pressure. The surgeon should decompress the pneumoperitoneum and flood the pelvis with sterile saline. The Trendelenburg position should be reversed and the patient placed in a partial left lateral decubitus position (Durant maneuver [5]). As this patient is awake it may be reasonable to convert to general anesthesia in order to facilitate delivery of the baby and adequately resuscitate the patient. Key points prevention A thorough preoperative assessment is vital in identifying at-risk patients. Patients should be well hydrated prior to surgery and intravenous fluids prescribed where necessary. The use of nitrous oxide in anesthesia should be avoided (nitrous oxide can dramatically increase the size of an air embolus as it is 35 times more soluble than nitrogen [5]). Where possible the level of the operative site in relation to the heart should be lowered and the time the venous circulation is open to the atmosphere minimized. Specific management is targeted at preventing further gas entrainment, limiting the spread of central progression, and minimizing the systemic cardiovascular effect [3,5]. It is important to ensure that 100% oxygen is administered and the use of any nitrous oxide is discontinued. In laparoscopic procedures, the pneumoperitoneum should be immediately decompressed. The surgical site should be flooded with sterile saline or covered with saline-soaked drapes. Alternatively, placing the patient in the left lateral position with a slight head-down tilt may trap the embolism in the right atrium [8]. Acute pulmonary edema following venous air embolism during a neurosurgical procedure. She underwent extensive lysis of the adhesions and enterolysis with monopolar scissors. In the office, her physical examination demonstrated rebound tenderness and she was admitted to the hospital. This increase in voltage allows an increase in thermal spread and possible adjacent tissue injury. At these frequencies the energy is dissipated, converted into heat by tissue impedance and does not cause tetanic contractions [2]. Background Electrosurgical equipment can cause thermal injury for a number of reasons. A good understanding of the basic principles of electrosurgery can drastically reduce this risk. Unfortunately, many surgeons do not have a good understanding of the electrosurgery instruments they use, and therefore increase their potential for thermal injury. Basics of energy Instead of electrosurgery, the term "electrocautery" is often used in the operating room, but the use is incorrect. Electrocautery involves the use of a direct current to heat up a metal conductor with a high impedance to flow so that the metal becomes hot. Electrosurgery involves manipulating electrons through living tissue by using an alternating current with enough current density to create heat within a cell to destroy the tissue [1]. The standard unit of current is amperes (A), or coulombs per second, while the standard unit of resistance is ohms. The original generators relied on grounding from a wall outlet (ground-referenced generators), which had the potential to allow the energy to follow alternative pathways (as it follows the path of least resistance). These could cause burns, and most of the burns were at the site of the return electrode if part of the electrode was peeled off or was not in full contact with the patient. In this type of system, current in the transformers as well as the return current is insulated from the frame of the generator.
Purchase mycelex-g 100 mg with amex
This can be achieved with bipolar diathermy (Chapter 71) and/or suture ligation before transection antifungal creams for yeast infection purchase mycelex-g 100 mg visa. When the uterus is heavy, it is important to avoid excessive traction on the divided pedicles due to the risk of troublesome back-bleeding from the engorged uterus during the procedure. The latter is an excellent tool allowing tactile, precise, and hemostatic dissection of tissues in this situation. Therefore, the surgeon should not assume that "hugging" the body of the uterus will avoid risk of ureteric injury in this situation. Once the ovarian and uterine vessels are safely secured, the prospect of successfully completing the operation laparoscopically is greatly enhanced. On the other hand, failure to access or identify the ureters and the uterine vessels clearly should make the surgeon consider conversion to laparotomy. Colpotomy under laparoscopic visualization Once the uterus is devascularized, it is advantageous to perform colpotomy under laparoscopic visualization so as to avoid a separate vaginal set-up. This can be done by using laparoscopic scissors with monopolar diathermy or preferably by using laparoscopic ultrasonic curved shears because this latter energy modality avoids excessive smoke plume. Using a colpotomy tube, the anterior vaginal fornix may be entered in the midline followed by circumferential incision until the entire cervix is dissected. However, if there is any suspicion of sarcomatous change within a fibroid, especially in women of postmenopausal age, then morcellation should be avoided because of concerns over potential dissemination of disease [4,5]. It is advisable to re-insufflate the abdomen to check for hemostasis and complete removal of all specimens. Because of the size of the uterus, the surgeon needs to give special consideration to higher port positioning and the use of a laparoscope with an offset distal lens to help overcome problems presented by the restricted operative field and limited maneuverability of ancillary instruments. Once the ureters are clearly identified, the uterine vessels may be secured lateral or medial to the ureters depending on individual circumstances with bipolar diathermy, vascular clips, or sutures Chapter 82: Laparoscopic Hysterectomy for a Large Fibroid Uterus 249 Key points Challenge: Problems in laparoscopic removal of a huge fibroid uterus. If there is any suspicion of sarcomatous change within a fibroid, especially in women of postmenopausal age, then morcellation should be avoided because of concerns over potential dissemination of disease. Successful laparoscopically assisted vaginal hysterectomies for large uteri of various sizes. Identifying the indications for laparoscopically assisted vaginal hysterectomy: a prospective, randomised comparison with abdominal hysterectomy in patients with symptomatic uterine fibroids. The surgeon now faces the challenge of removing the large dermoid cyst containing solid components. Background the use of laparoscopic surgery has become accepted as the "standard" approach for removal of benign pathology such as ovarian cysts or fibroids. This is because minimal access surgery, compared with open surgery, is associated with smaller skin incisions, better cosmetic results, less postoperative pain, shorter hospital stay, faster recovery, and earlier return to normal activities [1,2]. Retrieval of tissue specimens by laparoscopic surgery is intrinsically more difficult compared with open surgery, presenting a number of challenges. Firstly, when the surgical specimen cannot be removed via a 5- or 10-mm port, it must be reduced in size either within the abdomen, or placed inside a tissue retrieval bag to be removed in a piecemeal fashion or by morcellation through an extended port-site incision. Secondly, there is a higher risk of specimen rupture or spillage during laparoscopic dissection and specimen removal. Thirdly, the use of endoscopic retrieval bags can minimize the risk of spillage but will add to the procedural costs because of the requirement for these consumables. Fourthly, extension of the incision site may aid retrieval of large specimens but this can increase the risks of port herniation (Chapter 90), hematoma formation, and postoperative pain [3]. The suitability for laparoscopic specimen retrieval is dependent on various factors. The size of the specimen will likely influence the size of the retrieval bag and the degree of difficulty in manipulating the cyst into the bag. Once inside the retrieval bag, the larger specimen is also likely to require aspiration to reduce cyst volume before it can be debulked or morcellated for removal from the peritoneal cavity. In the case of large uterine fibroids or uteri after subtotal hysterectomy, the surgeon needs to select a 15-mm morcellator or remove the specimen via a mini-laparotomy incision. On the other hand, soft friable tissues such as degenerative fibroids may be impossible to grasp, while heavily calcified fibroids may be impossible to morcellate and may require a mini-laparotomy to extract from the peritoneal cavity. Benign specimens can be removed piecemeal but the surgeon should be aware of special circumstances where specimen retrieval may lead to complications if the cyst ruptures or if the tissue comes into contact with the port-site skin incisions during the process of removal from the peritoneal cavity. Examples include the risks associated with tissue spillage and dissemination of malignancy (ovarian carcinoma, uterine leiomyosarcoma), pseudomyxoma peritonei (mucinous cystadenoma), chemical peritonitis (ruptured dermoid cyst), and tissue seedling (endometriosis and fibroids implanting onto distant sites within the peritoneal cavity or port sites). This method is suitable for simple large ovarian cysts, endometriomas, and small dermoid cysts with no solid components. To minimize spillage of the cyst contents, an Endoloop can be used to tie around the punctured cyst opening while grasping the perforation edges with forceps, after initial aspiration. Alternatively, large unruptured cysts, once dissected free, can be placed inside a retrieval bag and decompressed by exteriorizing the bag through the port site. However, the disadvantages include another intervention with associated resource use and inflated costs as well as the lack of direct final inspection and assessment of the pathology before surgical intervention. This maneuver will minimize spillage of the fluid content during suction drainage. The advantages include performing the procedure under direct vision while utilizing the same port incision, albeit larger. This method of tissue retrieval is suitable for firm masses such as uterine fibroids but inappropriate for cystic masses such as ovarian dermoid cysts, degenerative fibroids, and potentially premalignant or malignant cysts. Risks include internal organ injury from uncontrolled or inappropriate use of the morcellator and from repeated introduction and removal of sharp laparoscopic graspers. Risks include vaginal hematoma, vaginal scarring potentially resulting in dyspareunia, pelvic infection, and rectal injury. This method is contraindicated in cases where the pouch of Douglas is obliterated or vaginal access is very limited. Introduction of these bags into the peritoneal cavity requires at least a 10-mm port. A popular method is to introduce the retrieval bag via the 10-mm umbilical port [5] with the guidance of a 5-mm laparoscope inserted via a lateral port. This allows clear visualization of the pelvis and enables the excised tissues to be fed directly into the bag. Exteriorization of the retrieval bag via the 10-mm port allows cyst contents to be decompressed by aspiration with a large-bore needle, or incision into the cyst wall and aspiration using laparoscopic suction. However, transvaginal specimen retrieval using tissue retrieval bags is associated with less pain than removal through a more conventional umbilical port [6]. Solid tissues, such as fibroids, can be manually morcellated and bony calcification within dermoid cysts broken up with a bone crusher within a retrieval bag. However, specimen retrieval bags can be expensive and those made with less durable material may tear during surgical manipulation. A surgeon has to consider certain prerequisites before determining the route of surgery. History, clinical examination, and investigations such as ultrasonography and tumor markers will allow the surgeon to formulate a likely diagnosis. The suitability of laparoscopic surgery will depend on the size, consistency and pathology of the pelvic mass. In addition, any existing patient comorbidities have to be identified preoperatively. The surgeon should have undergone specialized training and possess good technical skills and knowledge. Careful patient selection and understanding the limitations of laparoscopic surgery, such as the difficulties which can be encountered in specimen retrieval, are important.
Discount 100 mg mycelex-g
The number of prior incisions does not have a bearing on the incidence of adhesions antifungal infant buy 100 mg mycelex-g otc. Women with prior gynecologic pelvic procedures have more adhesions compared with those who have undergone a cesarean section. Patients with prior midline incisions for cesarean delivery do not have more adhesions compared to those with the more common low transverse access [4]. Extensive adhesions are frequently encountered in women with a history of generalized peritonitis, bowel resection after intestinal obstruction, oncologic procedure with omentectomy, and previous irradiation or intraperitoneal chemotherapy [2]. The anesthetist should be notified so that he or she can evacuate the stomach with a nasogastric tube before insertion of the insufflation needle. The subumbilical adhesions can then be assessed and divided to allow insertion of an umbilical 10-mm port. Key points Challenge: Failure to enter and insufflate the peritoneal cavity during laparoscopic surgery. If Veress needle insertion is unsuccessful, the surgeon should consider requesting help from a senior colleague, consider an alternative site entry, revert to an open technique, perform a laparotomy, or abandon the procedure altogether. An evaluation of four tests used to ascertain Veres needle placement at closed laparoscopy. Case history 2: Midway through a laparoscopic hysterectomy, the anesthetist notices neck and facial swelling consistent with subcutaneous emphysema. Risk factors for surgical emphysema include advanced age, the use of multiple ports, high-pressure pneumoperitoneum, prolonged surgery, and extraperitoneal laparoscopic procedures [2,3]. Complications of surgical emphysema Mild or marked surgical emphysema normally subsides without any complications. However, massive surgical emphysema can result in potential complications such as severe acidosis, hypercarbia, upper airway obstruction, pneumomediastinum, pneumopericardium, pneumothorax, and gas embolism (Chapter 69). Pneumomediastinum, characterized by impaired cardiovascular and pulmonary functions, can be life-threatening. Anesthetic measures include an increase in minute ventilation and several manual breaths to help with alveolar recruitment. If there is any evidence of pharyngeal compression and airway compromise, or if significant neck swelling is present, then it will be necessary to keep the patient sedated and intubated until the neck swelling and compression settle and hypercarbia is corrected. When extubating the patient, it is necessary to ensure that there is someone with the skills and materials for establishing a surgical airway should this become necessary. In the rare event of critical cardiorespiratory compromise, mediastinotomy may be necessary to relieve tension pneumomediastinum [6]. Unlike groundreferenced systems, these systems will not work if there is a break in the circuit. Another safety feature built into the grounding pads is having two pads that are side by side and which have built-in monitors that can measure contact stability and power density. Several variables can be altered to achieve different tissue effects when using monopolar electrosurgery, such as changing the waveform, the size or shape of the electrode (power density), and the speed at which the instrument is moved. The waveform of the Coag setting is not continuous and is only on 6% of the time; however, it is set to a higher voltage/amplitude. The Cut waveform in comparison is continuous, and because of this the voltage is lower to achieve the same wattage. The Blend waveform is also non-continuous but is on for a longer duration depending on the setting. It is advisable to use the lowest power setting possible to achieve the desired tissue endpoint [2]. The tissue effects of coagulation and cutting can be achieved simply by changing the power density or size of the electrode (surface area) used. If the surgeon uses a smaller surface area, cutting will occur; if a larger surface area is used, coagulation occurs. Burns in other sites can occur where cardiac monitor leads and body jewellery are located; jewellery should be removed if possible or taped down so that the surface area increases, minimizing any current density. If jewellery is located in a direct line from the surgical field to the grounding electrode and it cannot be removed, the grounding pad should be placed in a different position [2]. If a patient has an implanted electronic device, such as a pacemaker, cochlear implants, or an infusion pump, it is safer to avoid monopolar diathermy and use bipolar diathermy instead (Chapter 71). If monopolar diathermy needs to be used, the return electrode should be placed as far from the implanted device and as close to the surgical site as possible. Bowel Insulation failure Trocar Direct coupling prevention preoperative measures the most common complication from monopolar electrosurgery is burns from improper placement of grounding pads. Chapter 70: Laparoscopy: Problems with Monopolar Diathermy 215 Insulation failure Insulation failure presents a danger in electrosurgery because of the introduction of an alternative current pathway. Smaller breaks are more dangerous than larger breaks because the power density is higher. Insulation failure injuries can be reduced by thorough inspection of the instruments, by limiting high-voltage waveforms, and by decreasing unnecessary removal and entry of the instrument through the trocar. Direct coupling When one instrument is active it is important that the surgeon remains vigilant to the location of all instruments and that the appropriate field of view is maintained. When the electrode is activated and a metal accessory instrument is near or touching it, the accessory instrument will become energized as well. This presents a danger because thermal injury can occur to the viscera if the power density is high enough. As with any other thermal injury, the signs of the injury may not be apparent at the time of injury and may present several days following surgery. Injury can occur not only with direct contact to the tissue but also secondary to electrical sparks or arcing. If jewellery is located in a direct line from the surgical field to the grounding electrode and it cannot be removed, the grounding pad should be placed in a different position. Capacitive coupling Capacitive coupling is a known electrical phenomenon where electricity can be capacitated in a secondary conductor when two conductors are separated by an insulator and the primary conductor is charged. This phenomenon occurs in laparoscopic surgery when the electrode in a monopolar device is surrounded by an insulator and introduced through the metal sheath. No insulator is able to completely shield the flow of electrons from the electrode to the surrounding sheath. If the sheath is composed of metal, it may then store energy as a capacitor, and this energy will always be discharged to the abdominal wall. If there is a plastic collar shielding the abdominal wall and isolating the metal sheath, there is a higher capacitive effect, which increases potential for a higher power density since the capacitated electricity is stored in the metal cannula. A possible second scenario would be if electrosurgical scissors were introduced through the channel of the operative scope and the scope introduced through a plastic cannula. The risk of tissue injury from capacitive coupling can be minimized by avoiding open circuit activation and by using the lowest power setting necessary to achieve the desired tissue effect [2]. Any of the mechanisms described in this chapter could be implicated, although in this instance a direct surgical injury is possible given the complexity of the surgery, which involved division of bowel adhesions. The pedicle was grasped with a bipolar electrosurgical device in an attempt to stop the bleeding. It was noted that the pedicle was still bleeding and a larger grasp of the pedicle was taken and desiccated. On postoperative day 6, the patient re-presented complaining of severe back pain on the right. On examination she was found to have tenderness over the right costovertebral angle (loin) and was admitted for further work-up. Bipolar instruments are designed to have two opposing electrodes that can grasp the desired tissue that needs to be coagulated. These instruments work by receiving energy from a generator (the same generator used for monopolar devices). Bipolar electrosurgery therefore does not require a large dispersive return electrode to be attached to the patient as in monopolar electrosurgery, and consequently decreases the possibility of cross-interference with implanted electrical devices such as cardiac pacemakers [1]. Because of this bidirectional circuit in the instrument itself, the risks of direct coupling and capacitive coupling are not present in bipolar electrosurgery [2].