Buy generic augmentin 1000mg online
Other mechanisms involved in vascular damage include: anticellular endothelial and antilysosomal antibodies and the creation of a cellular type of immune response with the formation of granulomas antibiotics for uti leukocytes buy generic augmentin canada. Pulsed methyprednisolone therapy may be initiated; when there is no favourable clinical response, treatment with intravenous cyclophosphamide can be initiated. In Kawasaki disease, intravenous administration of standard human gamma globulin has been widely accepted, in a single dose of 3 g/kg within the first 10 to 12 days of onset of the illness. In systemic vasculitis a certain degree of effectiveness with biological drugs, such as etanercept, inflixomab and rituximab recently been reported. The therapeutic use of antithrombotics is controversial, although certain groups use aspirin in patients at risk of thromboembolic phenomena. Drugs represent the most frequent etiologic factor and are the cause of the neuroleptic malignant syndrome and serotoninergic syndrome. Movement disorders requiring emergency care comprise neurological diseases with an acute or subacute onset in which the predominant clinical presentation is movement disorder, and in which an error in diagnosis or treatment can lead to significant morbidity and even mortality [1,2]. They account for a small percentage of urgent neurological consultations and may have very different etiologies (Table 91. They can be classified according to the presenting signs and symptoms: rigidity, parkinsonism, dystonia, chorea or ballism and myoclonus. Other diseases can also manifest with rigidity, including infectious diseases such as tetanus or rabies, strychnine poisoning, hypocalcemia, and inherited diseases such as hyperekplexia. Its occurrence may be favored by the co-administration of lithium to any of the listed drugs. It is more common in young men using slow-release preparations and is favoured by dehydration. This is an idiosyncratic reaction that occurs within a few weeks after the start of the treatment or after an increase in the dosage; it is characterized by severe 1630 Management of Acute Movement Disorders Process Medication Serotonin syndrome Serotoninergic drugs <12 h Hypertension, tachycardia, tachypnoea, hyperthermia (>41. There are two pathophysiological hypotheses: a central mechanism that blocks dopamine in the striatum (stiffness) and hypothalamus (dysautonomia), and a peripheral mechanism that alters muscle fibre contractility due to alterations of the membrane of the sarcoplasmic reticulum. Subcutaneous apomorphine or transdermal rotigotine patches may also be administered. Dantrolene at a starting dose of 25 mg/24 h with further increases to 25 mg/12 h or 1-10 mg/kg intravenously may be used in severe disease. If untreated, the mortality rate is estimated to reach 20% and the causes of death are pulmonary embolism, aspiration pneumonia and renal failure. In some cases, discontinuation of the offending medication or medications, and offering supportive measures are sufficient to resolve symptoms within 24 hours. In other cases, other measures, such as benzodiazepine administration, should be added. Physical restraint should be avoided because it can cause rapid clinical deterioration. Antipyretics have no role in the management of hyperthermia since it is not the hypothalamus that is involved but rather the muscle activity. Succinylcholine should be avoided because of the risk of arrhythmia, together with the hypercalcemia that occurs with rhabdomyolysis. Mutations of this receptor cause an alteration in calcium homeostasis, with an increase in muscular calcium and sustained muscle contraction which, in turn, leads to a state of hypermetabolism with lactic acidosis, hypercapnia and hyperthermia. It is triggered by inhaled halogenated anesthetics and depolarizing muscle relaxants. The most common early sign is tachycardia, followed by muscle rigidity, masseter spasm, and tachypnoea. Elevated temperature is a late sign, together with arrhythmias, cyanosis, hypotension, hyperkalemia and rhabdomyolysis. It has been speculated that its physiopathology is related to an involvement of dopaminergic transmission. Treatment consists of life support with intravenous lorazepam; electroconvulsive therapy is the treatment of choice(Table 91. Contractures can occur spontaneously or after auditory or sensory triggers and disappears during sleep. Neurophysiological studies suggest that it is a central continuous motor activity. Other clinical manifestations that may occur spontaneously are stiffness, decreased level of consciousness (from light drowsiness to coma), autonomic alteration with tachycardia, fluctuating blood pressure, lack of perspiration, ileus, or vocal cord paralysis. In addition to levodopa dose reduction, other triggers may be the change in one agonist for another, infection, elevated environmental temperature (heat stroke) causing dehydration, or changes in the distribution of levodopa due to changes in nutrition. Sometimes a sudden decline occurs as a consequence of antiparkinsonian treatment suspension (the so called "superoff effect"). Underlying the pathophysiology may be acute dopaminergic hypotransmission in the hypothalamus, nigrostriatal system and mesocortical dopamine system. Treatment consists in its early detection and the administration of fluids (2500-3000 ml/24 h) with electrolytes and glucose, vitamin B1, physical and pharmacological measures against hyperthermia, treating infection if diagnosed, and antiparkinsonian treatment reinstated as soon as possible by nasogastric tube if there are problems with swallowing (Table 4). If the stiffness is severe, it may be necessary to use dantrolene at doses of 80 mg/day intravenously. Hallucinations and delirium can be accompanied by intense agitation, confusion and sleep disturbances which alter the quality of life of patients and their caregivers. Psychosis is related to antiparkinsonian treat- 1634 Management of Acute Movement Disorders ment. Its onset is not only due to dopaminergic dysfunction but also other neurochemical changes. It has been suggested that hallucinations are due to early mesolimbocortical receptor hypersensitivity not purely related to the degeneration of serotonergic or cholinergic mechanisms [9]. When acute psychosis is suspected, triggers such as infections and metabolic or structural brain processes should be investigated. If, despite these changes, the symptoms persist, it may be necessary to reduce levodopa, and, if this is not enough, atypical neuroleptics such as clozapine, quetiapine, or aripiprazole should be administered. This treatment may cause complications leading to emergency complications that the general neurologist should be familiar with; however, the patient should be referred to a specialized centre in these circumstances [10]. Among the surgical delayed complications we can list deep vein thrombosis and pulmonary thromboembolism, together with any surgical procedure involving prolonged bed rest. In addition, local infections can occur because of: accumulation of serous fluid in the surgical bag housing the stimulator; problems with the implanted material such as electrode displacement or breakage, or cable infection or necrosis in the subcutaneous track. Additionally, the generator may be disconnected because of inadvertent contact with a strong magnetic field, thus producing a sudden worsening of parkinsonian symptoms. This can also happen if the neurostimulator batteries are depleted (they typically last about 5 years). In both cases, in which a negative effect induced by a recent change in the parameters of the neurostimulator is suspected, consultation with neurologists expert in the management of its programming system will be necessary. Complications consequent to brain stimulation are the appearance of choreic or ballistic movement disorders due to stimulation of the subthalamic nucleus. Psychiatric disorders may also occur, such as apathy or cognitive impairment, anhedonia, euphoria or hypomania, which have been associated with stimulation of the medial and ventral areas of the subthalamic nucleus. The stimulation of neighbouring fibres of the internal capsule can produce pseudobulbar symptoms, such as dysphagia, dysarthria and inappropriate crying. These effects should be considered when a patient with a neurostimulator enters the emergency room for other medical problems. It may be caused by infectious agents such as mycoplasma or drugs such as amphotericin B. Metabolic disorders such as central pontine or extrapontine myelinolysis can produce acute parkinsonism. This dis1635 Intensive Care in Neurology and Neurosurgery ease occurs as a result of osmotic alterations. There is a rare hereditary disease with linkage in a region of chromosome 19, called dystonia-parkinsonism, in which symptoms may occur acuteTable 91. The onset of parkinsonism by accidental consumption or addiction to various drugs is documented in the literature (Table 91.
Buy generic augmentin canada
Facilitate restructuring of core schemes by challenging maladaptive beliefs with newly accessed primary adaptive needs/ goals and resources antimicrobial countertops buy augmentin 625mg amex. Support mobilization of resources, self-soothing capacities, improved affect regulation, and self-empathy. Construct a new narrative and new metaphors to capture new meanings (Greenberg & Paivio, 1997). Complicating Factors in Negotiating a Good Working Alliance There are several factors that can complicate the construction of alliance. Poor self-awareness due to frontal, subcortical, or right hemisphere lesions will have to be worked with as the first goal when resistance in the recovery process occurs. The authors conclude that construction of self-knowledge may occur in rehabilitation through a bidirectional feedback process between the client and the therapist, rather than one-way feedback to the client about the deficits from the clinician. This emphasis of a collaborative approach includes a specific focus on identity by linking meaning, goals, and tasks. Premorbid personality traits, core beliefs, and schemas, as well as basic assumptions about life, can also cause impasses, if not recognized. Interindividual differences form a challenge to individually tailored programs, as well as group interventions. Metacognition-A Link to Awareness How to create awareness after brain injury is not an easy task, even though necessary for treatment efficacy. Components of metacognitive reflection have been described and defined by Cornoldi (1998). Metacognitive conceptualization of a task (metacognitive reflection present at the moment of starting a task and during execution); 4. Specific metacognitive knowledge (knowledge concerning specific aspects or cognitive functioning). It may be also tacit and covert, when the patient is periodically unaware of the changes due to injury. However, it can be worked with in the intervention procedure using a strategic method. Structured but relaxed discussions of the nature of cognitive functions, disturbances, and the meaning of intentional collaboration, as well as therapeutic exercises for recovery, can create new insights and motivation. The psychotherapeutic approach and methods are dependent on the theoretical framework of the therapist and the methods he or she is able to master. Most of the psychotherapy techniques introduced in this chapter have been adopted from cognitive psychotherapies. However, the creative and experimental strategies also originate from other sources. Answers for the meaning of creative writings, particularly metaphors and poems, have been studied and described by Teasdale and Barnard (1993). They state that metaphors and poems are more closely integrated with emotions than is common dialogue. This implicational speech also captures emotional change better than factbased knowledge alone. Preference of music chosen is influenced by previous experiences the person has had. Mindfulness-based therapeutic methodologies provide potentially useful theoretical and therapeutic windows in to a range of affective disorders (Segal, Williams, & Teasdale, 2002). Mindfulness methodology has united Eastern meditative practices and Western epistemologies and practices, according to the aforementioned authors. This provides a Summary of Applications of Psychotherapeutic Methods 223 potential use for sufferers of brain injury in individual cases needing experiential contact with themselves: awareness of thoughts, feelings, and bodily sensations. Scientific studies on the effects of brain function are beginning to appear, so this could prove to be a useful tool in the future. All of these methods have been used by neuropsychotherapists in the finish training tradition. Psychoeducation In neuropsychological intervention, psychoeducation is necessarily multidisciplinary-drawing from neuroscientific, psychosocial, and psychotherapeutic knowledge. We therapists communicate to our clients something that they most likely never knew about themselves. This may require time and effort, but it can be a concrete way of working towards awareness through the neuropsychotherapy process. This can also be said of neuropsychological rehabilitation 224 Introduction to Neuropsychotherapy with psychotherapeutic orientation. With psychoeducation, we can show appreciation and professionalism, and we can convey new knowledge to the patient. Dialogue Forms of dialogue discussed in this context have been adopted from cognitive therapy. Freeman, Pretzer, Fleming, and Simon (1990) have listed ways of carrying dialogue that can also be useful with neurological and neuropsychiatric patents or clients. This is particularly relevant when the therapist finds it difficult to understand and follow the basic meanings in the dialogue. The effective way to challenge a dysfunctional thinking process is to examine the supporting existence for the ideas. Together with validation, this could be used for sufferers of poor self-awareness. However, if the client is Summary of Applications of Psychotherapeutic Methods 225 blaming himself or others, and feelings of guilt and anger are overwhelming, it is helpful to try to proceed towards change in thinking to find a broader view, and even something positive in "disaster. They may have been spontaneous ways of coping with ideation of altered self, as in case of Maria below. Systematic art therapy programs, such as the Sarie Mai method, will be described later in this chapter. Cognitive rehearsal is integrated in to the treatment process according to the necessity of treating cognition. It is not within the scope of this chapter to deal with cognitive exercises or treatment programs, but of course it is to be borne in mind that they form part of the procedure (see Chapter 1). Case Study: Maria Creativeness in the form of poetic writing can be a helpful coping strategy for experiencing strangeness when compared with peers. The feeling that something is missing in the inner world and self, of not being a whole integrated personality, is well described by Maria. Maria was 12 years old when she was hit by a motorcycle while crossing the street. At the acute phase, Maria had fractures in the left leg, which also remained shorter than the right. She experienced amnesia of the accident for at least a few hours, but no loss of consciousness was reported. The poems are authentic experiences 226 Introduction to Neuropsychotherapy and were translated in to English from Finnish for this book by Maria herself. However, in neuropsychological treatment procedures, the use has not been as common. In neuropsychological rehabilitation, the neuropsychologist can use many methods to cope with these symptoms. Neuropsychotherapy often continues after the active phase of neuropsychological rehabilitation. Art therapy offers the opportunity to activate the neural integration and ultimately higher cortical functions that come from mentalizing personal idiosyncratic epistemologies (how we know who we are; Hass-Cohen & Carr, 2008). In neuropsychotherapy, there are also many possibilities to use methods from art therapy in dealing with still-existing neuropsychological problems.
Augmentin 625mg overnight delivery
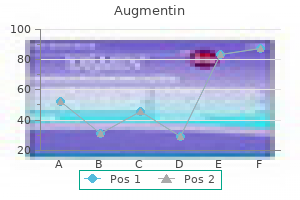
For this reason infection jaw bone 625mg augmentin overnight delivery, adequate pain treatment is essential in the management of critically ill patients. The neurocritical patient feels pain not only because of the underlying disease but also because of the routine procedures received, for example, changes in decubitus, aspiration of secretions, blood sampling, wound healing, and catheter implantation. For sedated patients, in which analgesia tends to be underutilized, it is important to evaluate the physiological equivalent of somatic pain, for example: facial expression, movement and posture can be clear indicators of pain. Among physiological signs, tachycardia, hypertension, or tachypnoea require adjustment of analgesic dose or its utilization, if not being administered. Continuous infusion of analgesic drugs or regularly administered doses (extra dose or "bailout" when required) are more effective than bolus doses "as needed", which can lead to time intervals without coverage. Intravenous administration allows faster, more accurate titration according to the needs of the patient. We must remember the side effects of opioids: respiratory depression, constipation, gastroparesis, hypotension, and hallucinations. Furthermore, the fact that a patient cannot speak does not mean that he or she does not have pain. The intent of both strategies is to individualize and optimize the management of sedation (adjust the level of sedation to an individual target), minimize oversedation and its complications by preventing the accumulation of analgesics and sedatives (tachyphylaxis). The daily interruption strategy has additional advan1679 Intensive Care in Neurology and Neurosurgery Score +4 +3 +2 +1 0 -1 -2 -3 -4 Designation Combative Very agitated Agitated Restless Alert and calm Somnolent Mild sedation Moderate sedation Deep sedation Description Combative, violent, immediate danger to staff Aggressive attempts to withdraw tubes and catheters Frequent and purposeless movements, "struggle" with the fan Anxious but not aggressive or vigorous movements Not fully alert but remains (10 seconds) awake (eyes open and track) to the call Wakes up briefly (<10 seconds) to the call with eye tracking Movement or eye opening to the call (but with eye tracking) No response to the call, but movement or eye opening to physical stimulation No response to voice or physical stimuli Exploration Observe the patient Call the patient by name and say "open your eyes and look at me" Encourage the patient by shaking his shoulder or rubbing over the sternal region -5 Unanswered Table 93. If the patient cannot be ventilated and is receiving the maximum dose of analgesia and sedation, he or she can be assessed with the use of muscle relaxants. Neuromuscular blockade should be used only when strictly necessary and for the shortest time possible. Objective assessment of sedoanalgesia with a validated measurement scale is recommended. Sedation levels will differ for each patient and should be adapted to their condition and time of evolution. Sequential compression devices should be used when heparin is contraindicated [10] or as an adjuvant. We recommend graduated compression stockings or intermittent pneumatic compression stockings, unless a lower extremity injury prevents their use. Those that have demonstrated an advantage, albeit with low levels of prevention, are known as graduated compression stockings which compress more in the calf region and less towards the root of the thigh. Despite available evidence and recommendations, this simple strategy does not have the expected response of the critical care team although it is an inexpensive measure. It is important to remember that we are talking here about the semi-sitting position and not only maintaining the head raised. To reduce the likelihood of gastro-oesophageal reflux, staff must ensure that the entire trunk is inclined. This requires continuous postural corrections because even sedated patients tend to slide toward the foot of the bed. The semi-sitting position should be maintained in all patients unless there are express contraindications (for example, neurocritically ill patients with postoperative subacute or chronic subdural hematoma should be positioned flat in bed). They should be used until you can start a good nutrition enteral caloric intake, then should be discontinued. Prevention of stress ulceration is especially important in patients with respiratory failure, clotting abnormalities, under steroid therapy, or with a history of peptic ulcer because of increased risk of developing gastrointestinal bleeding related to stress. All guidelines recommend early enteral nutrition as a cornerstone in the prevention of stress ulceration. This point has also been demonstrated in several acute neurological diseases such as stroke and head injury. If the patient cannot expel secretions from the throat and mouth by coughing, a Valsalva manoeuvre will be performed. Whenever possible, talk with nurses, family, doctors, and other people outside the room. If we lower serum glucose levels, we will restrict the availability of this fuel just when the injured brain needs it most [14]. Although the optimal blood glucose range has not yet been determined, extreme oscillations should be avoided. Subcutaneous insulin administration has proved to be unpredictable and less effective than intravenous administration in critically ill patients. One aspect to consider in subcutaneous administration is the low predictability of absorption, even more so in patients with edema, compromised peripheral perfusion or state of shock. The role of insulin infusion in patients with acute brain injury continues to be investigated. Several protocols have shown satisfactory nurse-led blood glucose control in critical care units. Since patients with hypoglycemia may have symptoms that mimic an acute stroke, manifesting focal signs, speech disturbances, and cognitive changes, capillary blood glucose monitoring should be a routine practice in patients with impaired awareness. Some additional considerations and procedures may be performed to prevent increased intracranial pressure (Table 93. The most common causes of hypoxia are partial airway obstruction, hypoventilation, aspiration pneumonia, bronchial secretions, and atelectasis. Patients with decreased level of consciousness or signs of brainstem dysfunction are at increased risk of airway compromise because oropharyngeal motility is impaired and there is loss of protective reflexes [15]. Endotracheal intubation should be performed rapidly with manual immobilization of the cervical spine [16]. However, the ability to swallow or remove oral secretions (effective cough mechanism) could be a more reliable parameter. In general, if the patient is able to tolerate placement of an accessory to the airway. The airway also needs to be maintained permeable due to the risk of obstruction from the inability to manage copious secretions or anatomic obstruction due to airway ede1683 Intensive Care in Neurology and Neurosurgery ma or traumatic injury. While it is assumed that the protective reflexes of the airway are nausea and coughing, many authors argue that the gag reflex is also important. The principal cause of obstruction in patients with sensory impairment is relaxation of the muscles at the base of the tongue which can drop in to the hypopharynx. Also, it is important to assess signs of increased breathing effort such as noisy breathing, or snoring, or accessory muscle utilization. Coma does not represent a loss of response to noxious stimuli; however, loss of this response may precipitate intracranial hypertension and herniation. Therefore, sedoanalgesia should be given properly during airway manipulation whenever possible. The tracheal tube should be placed in the middle of the oral cavity, perpendicular to the plane of the face, and properly set to prevent movement. It is recommended to mark the tracheal tube at the time of placement in order to know its depth, taking the dental arch as a landmark reference. In this regard, it must be remembered that changes in decubitus can displace a tracheal tube up to 2-3 cm. It is recommended that tapes are not wound around the entire neck but are applied only to the face or loose enough to pass a finger between the tape and the face. Patients without teeth and with the mouth kept wide open pose a greater challenge in this regard. Migration of the distal end of the tracheal tube in to a main bronchus, inadvertent extubation, inadequate ventilation, oxygenation and suctioning, and physical airway injury are some of the consequences of failure to properly stabilize a tracheal tube. The tracheal tube should be anchored whenever necessary to prevent inadvertent extubation and excessive movement. Monitoring the tracheal tube should ensure that the cuff pressure remains <20 mmHg while allowing a safety margin below the tracheal capillary perfusion pressure (25-35 mmHg). It is generally assumed that 25 mmHg is the maximum acceptable value for lateral pressure by the inflated balloon on the tracheal wall. If the patient shows signs of poor perfusion and/or high airway pressures during mechanical ventilation, the pressure value must be reduced.
Buy augmentin 1000mg on-line
This is contraindicated in case of paralysis infection from cut purchase augmentin with amex, obstruction or perforation of the ileus or in comatose patients without airway protection. Once the toxic agent is adsorbed, its passage through the digestive tract should be accelerated by the administration of purgatives. The dosage is 13-30 ml in children and 60 ml in adults every 4 hours, until the colour of coal deposition. Other cathartics used are sodium sulphate or magnesium: 30 g in 250 ml of water for adults, with a maximum of three doses, and 70%sorbitol solution, 50-70 ml every 4 hours. Oleose purgatives, solbitol and salite solutions are not recommended for pediatric use because of the risk of causing severe electrolyte alterations. The administration of cathartics is contraindicated in patients <1 year of age or in patients with diarrhoea, evidence of intestinal obstruction, bleeding, perforated viscus or peritonitis, electrolyte alterations, dietary sodium restriction, and renal failure for magnesium sulphate. Forced diuresis promotes the elimination a copious flow of urine (5-10 ml/min or 500 ml/h) through the provision of sufficient fluids intravenously, and, depending on the pKa of the toxic agent, at changing urinary pH by the administration of alkalizing substances such as sodium bicarbonate (1-2 mEq kg in dextrose solution 5%) in order to raise the urinary pH to 7. Other methods that can be used in specific cases include: peritoneal dialysis, hemodialysis, hemoperfusion, exchange transfusion, and plasmapheresis. Its use is recommended in cases of coma and respiratory depression secondary to the use of benzodiazepines. Flumazenil administration may involve risks for patients with hypotension, arrhythmias or hemodynamic instability; furthermore, it can cause seizures in patients with a history of epilepsy, increased intracranial pressure, concomitant ingestion of tricyclic antidepressants, anticonvulsants or cocaine, and benzodiazepine withdrawal syndrome in addicted patients. The use of flumazenil is unnecessary in most cases and can be associated with high risks, so it should be restricted to selected cases. Its effect begins within 1-2 minutes after the first dose and persists for 1-5 hours, depending on dose and type of benzodiazepine involved. Closely monitor the state of ileus, because of the anticholinergic effects of the drug. The cathartic should be administered after the first dose of charcoal and repeated at the same dose if no bowel movement is observed within 4 h, taking care not to repeat the activated carbon until an effective catharsis is obtained. Do not administer drugs such as phenytoin or antipsychotics such as haloperidol and group I antiarrhythmics, which increase the risk of cardiac toxicity and decrease the threshold of seizure. If sensory depression exists, endotracheal intubation prior to gastric lavage should be done, considering that aspiration is a cause of high mortality. If mannitol is not available, magnesium sulphate should be administered (30 g in adults and 250 mg/kg in children). If in the following 4 h the effect is not obtained, an additional dose of cathartic should be administered. Keep in mind that these drugs have enterohepatic circulation, so carbon administration must be repeated serially for 24 and 48 h. The use of antipsychotics such as haloperidol is associated with an increased risk of cardiac toxicity and reduced seizure threshold. In such cases, the patient should be hospitalized or referred to a higher level of care. In patients with hepatic encephalopathy, lactulose 30 ml per os should be administered. It affects the small, medium and large vessels, as well as a number of organs, which results in the diversity of its clinical manifestations. Thickening is often observed with signs of pain and tumefaction of the temporal artery. It usually affects patients older than 50 years and is frequently associated with rheumatic polymyalgia. Anemia, increased erythrosedimentation rate and alkaline phosphatase are frequent in the laboratory Granulomatous inflammation of the aorta and its branches. The clinical picture depends on the involved branches of the aorta, which may present with hemispheric ischemic symptoms, subclavian steal syndrome, lower limb claudication, renal or mesenteric ischemia Arteritis affecting the small, medium and large vessels associated with mucocutaneous lymph node syndrome. This disease was described only in patients up to 20 years old Granulomatous inflammation affecting the respiratory tract and necrotizing vasculitis of the small, medium and large vessels. It is often accompanied by necrotizing glomerulonephritis Granulomatous inflammation with abundant eosinophils affecting the respiratory tract and necrotizing vasculitis of the small and medium vessels. Neurological manifestations include: headache, convulsions, signs of focal compromise, cognitive deterioration, altered state of consciousness, involuntary movements, and cranial nerve deficits. A complementary serum study Anti Sm Systemic lupus erythematosus may provide information concerning the Anti P Systemic lupus erythematosus pathogenesis of the disease. Vascular lesions in these patients tend to be multiple and with a hemorrhagic component. Magnetic resonance imaging with multiple lesions hyperintensitive in diffusionweighted, sequences. Two different patterns of vasculitis: necrotizing granulomatsis in large vessels and nongranulomatosis lymphocitic vasculitis of the small vessels. The most common is caused by the formation of immune complexes, as in serum disease. Attachment of immunocomplexes to the vascular wall induces adherence and activation of the complement cascade, with immune amplification through the release of cytokines, the consequent expression of adhesion molecules in their membranes, and the release of their lysosomal products, with damage to the endothelium and other components of the vascular wall. Lethargic encephalitis occurred in epidemics in the early 20th century as encephalitis with involvement of the basal ganglia, mainly producing parkinsonism and psychiatric and sleep disorders. In recent decades, there have also been reports of encephalitis whose pathophysiology is poorly understood. There is no clear evidence of infectious agents invading the nervous system, although lymphocytosis is found in the oligoclonal bands of cerebrospinal fluid. In recent cases, steroids have been used with good clinical response, with complete recovery of the patients in many cases [2]. Other drugs such as rivastigmine or interferon alfa-2b may occasionally cause acute dystonic reactions. The clinical manifestations usually consist of focal craniocervical dystonia, which often occurs in the form of torticollis, but can be as trismus, lingual protrusion, oculogyric crises, pharyngeal or laryngeal dystonia, blepharospasm and even axial and limb dystonia. It occurs in 30-40% of young psychotics who started treatment with antipsychotics. In such patients, dystonic reactions have been reported after treatment with other drugs such as intravenous immunoglobulins. This rare entity is confirmed by fibroscopy and treatment involves the injection of botulinum toxin in to the thyroarytenoid muscle [2]. Patients with multiple system atrophy may also present with stridor caused by altered abduction of the vocal cords due to dystonic spasms of the thyroarytenoid muscles (adductors), abductor muscle weakness and neurogenic posterior cricoarytenoid muscle atrophy. The symptom is the appearance of severe dystonic spasms involving painful generalized hyperthermia, rhabdomyolysis with the risk of acute renal failure, anarthria, respiratory failure and dysphagia with the risk of pneumonia by bronchoaspiration. Precipitating factors may be the same for both: trauma, surgery, infection, fever and rapid introduction or withdrawal of a drug. Only in rare cases are oral medications (haloperidol, tetrabenazine and pimozide) effective. Midazolam and short-acting and short half-life benzodiazepines can be used as first-line therapy (30-100 mg/kg/h). As in status epilepticus, general anesthesia is sometimes necessary, and neuromuscular blockade by curaring agents. Oro-lingual-facial dyskinesias are the most characteristic abnormal movements but other types might occur simultaneously or alternate with limb and trunk choreoathetosis, oculogyric crisis, dystonia, rigidity and even opisthotonic postures. Autonomic manifestations include hyperthermia, tachycardia or bradycardia, hypertension or hypotension, hypersalivation, urinary incontinence and erectile dysfunction. Seizures develop at early stages of the disease that may overlap with abnormal movements. This disorder predominantly affects children and young adults and it can occur associated or not to a tumour (usually an ovarian teratoma). Treatment consists of tumour resection, if it is present, and immunotherapy (corticosteroids, intravenous immunoglobulinor plasma exchange). Sometimes a second line treatment with cyclophosphamide or rituximab is necessary. Among these emergencies, we may include psychogenic movement disorders that usually consist of motley and flowery movements that have an acute onset. It is important to consider this diagnosis to avoid unnecessary examinations, but the differential diagnosis can sometimes be difficult and the patient should be kept under observation.
Generic 1000mg augmentin overnight delivery
Monitor for changes in the therapeutic and adverse effects of warfarin if methimazole is initiated antibiotic nclex questions buy augmentin 1000 mg free shipping, discontinued or dose changed Methohexital may decrease the serum concentration of warfarin by increasing its metabolism. Monitor for changes in the therapeutic and adverse effects of warfarin if methohexital is initiated, discontinued or dose changed Metronidazole may increase the serum concentration of warfarin by decreasing its metabolism. Consider alternate therapy or monitor for changes in the therapeutic and adverse effects of warfarin if miconazole is initiated, discontinued or dose changed the tetracycline, minocycline, may increase the anticoagulant effect of warfarin 1209 Medroxyprogesterone Mefenamic acid Mefloquine Meloxicam Mercaptopurine Mestranol Methimazole Methohexital Metronidazole Miconazole Minocycline Intensive Care in Neurology and Neurosurgery Mitotane Moxifloxacin Nabumetone Mitotane may decrease the anticoagulant effect of warfarin the quinolone antibiotic, moxifloxacin, may increase the anticoagulant effect of warfarin the antiplatelet effects of nabumetone may increase the bleed risk associated with warfarin. Consider alternate therapy or monitor for signs and symptoms of bleeding during concomitant therapy Nafcillin may increase the anticoagulant effect of warfarin increasing the risk of bleeding. Consider alternate therapy or monitor for changes in the therapeutic and adverse effects of warfarin if nafcillin is initiated, discontinued or dose changed the quinolone antibiotic, nalidixic acid, may increase the anticoagulant effect of warfarin Nandrolone may increase the serum concentration and anticoagulant effect of warfarin. Monitor for changes in prothrombin time and therapeutic effects of warfarin if nandrolone is initiated, discontinued or dose changed Nandrolone may increase the serum concentration and anticoagulant effect of warfarin. Monitor for changes in prothrombin time and therapeutic effects of warfarin if nandrolone is initiated, discontinued or dose changed the antiplatelet effects of naproxen may increase the bleed risk associated with warfarin. Consider alternate therapy or monitor for changes in the therapeutic and adverse effects of warfarin if nicardipine is initiated, discontinued or dose changed Norethindrone may alter the anticoagulant effect of warfarin. Monitor for changes in coagulation status if norethindrone is initiated, discontinued or dose changed the quinolone antibiotic, norfloxacin, may increase the anticoagulant effect of warfarin Norgestimate may alter the anticoagulant effect of warfarin. Monitor for changes in coagulation status if norgestimate is initiated, discontinued or dose changed the quinolone antibiotic, ofloxacin, may increase the anticoagulant effect of warfarin Orlistat may increase the anticoagulant effect of warfarin Nafcillin Nalidixic acid Nandrolone decanoate Nandrolone phenpropionate Naproxen Nelfinavir Nevirapine Nicardipine Norethindrone Norfloxacin Norgestimate Ofloxacin Orlistat 1210 Antithrombotic Therapy for Secondary Stroke Prevention Oxandrolone Oxandrolone may increase the serum concentration and anticoagulant effect of warfarin. Monitor for changes in prothrombin time and therapeutic effects of warfarin if oxandrolone is initiated, discontinued or dose changed the antiplatelet effects of oxaprozin may increase the bleed risk associated with warfarin. Consider alternate therapy or monitor for signs and symptoms of bleeding during concomitant therapy Oxymetholone may increase the serum concentration and anticoagulant effect of warfarin. Monitor for changes in the therapeutic and adverse effects of warfarin if pentobarbital is initiated, discontinued or dose changed Pentoxifylline may increase the anticoagulant effect of warfarin Phenobarbital may decrease the serum concentration of warfarin by increasing its metabolism. Monitor phenytoin levels, prothrombin time, and therapeutic and adverse effects of both agents during concomitant therapy Phytonadione (vitamin K) may antagonize the anticoagulant effects of warfarin. The antiplatelet effect of piroxicam may also increase the bleed risk associated with warfarin. Consider alternate therapy or monitor for changes in the therapeutic and adverse effects of warfarin if piroxicam is initiated, discontinued or dose changed the corticosteroid, prednisolone, alters the anticoagulant effect of warfarin 1211 Oxaprozin Oxymetholone Oxyphenbutazone Paroxetine Pentobarbital Pentoxifylline Phenobarbital Phenylbutazone Phenytoin Phytonadione Piroxicam Prednisolone Intensive Care in Neurology and Neurosurgery Prednisone Primidone Propafenone Propoxyphene Propylthiouracil the corticosteroid, prednisone, alters the anticoagulant effect of warfarin the barbiturate, primidone, decreases the anticoagulant effect of warfarin Propafenone may increase the anticoagulant effect of warfarin Propoxyphene may increase the anticoagulant effect of warfarin Propylthiouracil may decrease the anticoagulant effect of warfarin. Rifampin may decrease the anticoagulant effect of warfarin by increasing its metabolism Additive anticoagulant effects increase the risk of bleeding. Concomitant therapy should be avoided the antiplatelet effects of sodium salicylate may increase the bleed risk associated with warfarin Secobarbital may decrease the serum concentration of warfarin by increasing its metabolism. Monitor for changes in the therapeutic and adverse effects of warfarin if sitaxentan is initiated, discontinued or dose changed St. Warfarin should be administered at least 2 hours before or 6 hours after sucralfate administration. Monitor for changes in prothrombin time if sucralfate is initiated, discontinued or dose changed Quinidine Quinine Ranitidine Rifabutin Rifampin S-adenosylmethionine Salicylate-sodium Secobarbital Sitaxentan St. Consider alternate therapy or monitor for changes in the therapeutic and adverse effects of warfarin if sulfadiazine is initiated, discontinued or dose changed Sulfamethoxazole may increase the anticoagulant effect of warfarin by decreasing its metabolism. Consider alternate therapy or monitor for changes in the therapeutic and adverse effects of warfarin if sulfisoxazole is initiated, discontinued or dose changed the antiplatelet effects of sulindac may increase the bleed risk associated with warfarin. Concomitant therapy is contraindicated due to significant increase in bleed risk Telithromycin may increase the anticoagulant effect of warfarin. Monitor for changes in prothrombin time and therapeutic effects of warfarin if testolactone is initiated, discontinued or dose changed Testosterone may increase the serum concentration and anticoagulant effect of warfarin. Monitor for changes in prothrombin time and therapeutic effects of warfarin if testosterone is initiated, discontinued or dose changed the androgen, testosterone, may incrase the anticoagulant effect of the Vitamin K antagonist, warfarin. Monitor for changes in the therapeutic effect of warfarin if testosterone is initiated, discontinued or dose changed Tetracycline may increase the anticoagulant effect of warfarin Thiopental may decrease the serum concentration of warfarin by increasing its metabolism. Monitor for changes in the therapeutic and adverse effects of warfarin if thiopental is initiated, discontinued or dose changed 1213 Sulfamethoxazole Sulfinpyrazone Sulfisoxazole Sulindac Tamoxifen Telithromycin Tenoxicam Testolactone Testosterone Testosterone Propionate Tetracycline Thiopental Intensive Care in Neurology and Neurosurgery Tiaprofenic acid the antiplatelet effects of tiaprofenic acid may increase the bleed risk associated with warfarin. Consider alternate therapy or monitor for signs and symptoms of bleeding during concomitant therapy Increased bleeding risk. Consider alternate therapy or monitor for changes in the therapeutic and adverse effects of warfarin if tolbutamide is initiated, discontinued or dose changed the antiplatelet effects of tolmetin may increase the bleed risk associated with warfarin. Consider alternate therapy or monitor for signs and symptoms of bleeding during concomitant therapy the androgen, Testosterone, may incrase the anticoagulant effect of the vitamin K antagonist, and warfarin. Monitor for changes in the therapeutic effect of warfarin if testosterone is initiated, discontinued or dose changed the prostacyclin analogue, treprostinil, increases the risk of bleeding when combined with the anticoagulant, Warfarin. A dosage reduction may be required if used in combination the anticoagulant effect of Warfarin, a Vitamin K antagonist, may be altered by antineoplastics such as Trimetrexate. However, adverse effects can arise while finding the appropriate maintenance dose, which can vary by a factor of ten among patients. An algorithm for estimating the appropriate warfarin dose that is based on clinical and genetic data has been developed and validated, and provided significantly better predictions of appropriate dose of warfarin than either the clinical algorithm or a fixed-dose approach [153]. Compared to warfarin, dabigatran (Pradaxa) 150 mg twice daily further reduces risk for stroke with similar bleeding risk (Level 1 [likely reliable] evidence) and possibly higher incidence of myocardial infarction (Level 2 [mid-level] evidence). Rivaroxaban (Xarelto) may be as effective as warfarin for preventing stroke or systemic embolism in patients with nonvalvular atrial fibrillation (Level 2 [mid-level] evidence). Apixaban (Eliquis) associated with reduced risk of stroke and major bleeding and might reduce risk of mortality compared to warfarin (Level 2 [mid-level] evidence). Use of aspirin as bridging therapy suggested until anticoagulation reaches therapeutic level. Consider dose reduction of new anticoagulant, especially dabigatran, in patients>75 years old. It derives from a binding between a N-naphthylsulphonylglycyl-4-amidino-phenylalanine-piperidine compound to a benzamidine which leads to antithrombotic activity (Table 64. Dabigatran reversibly binds to active site of thrombin both when free and when clotbound. Dabigatran is administered as pro-drug (dabigatran etexilate); non specific enzymes convert the pro-drug to the active molecule (dabigatran). This is of utmost importance because high polarity of dabigatran proves the impossibility of gastro-intestinal absorption [170-172]. Dabigatran has a quick onset of action when orally administrated and a predictable anticoagulant effect. Metabolism starts in gastro-intestinal tract and end in liver, but it is not mediated by cytochrome P450. Contemporary adiministration of protonic pump inhibitors reduces the max concentration of 20-25% whereas food decreases the plasma peak of two hours. Halflife of dabigatran is near 8 hours after the first dose and 6 hours after multiple doses; after 4-6 hours max concentration is reduced for 30%. Dabigatran is excreted for 80% from kidneys, therefore renal failure could prove a reduced excrection. Dabigatran is contraindicated in patients with severe renal failure (creatinine clearance, ClCr, <30 ml/min). However, the potential benefits of dabigatran compared with warfarin may be reduced in poorly compliant patients (because the longer half-life of warfarin could provide them with a more consistent anticoagulant effect) and in patients taking potent P-glycoprotein inhibitors, which can increase serum concentrations of dabigatran (Table 64. Dabigatran, the main active principle in plasma, is a rapid-acting competitive and reversible direct inhibitor of thrombin. Thrombin, a serine protease, is responsible for the conversion of fibrinogen to fibrin during the coagulation cascade. Dabigatran inhibits free thrombin, fibrin-bound thrombin and thrombin-induced platelet aggregation. Esterase-catalysed hydrolysis of dabigatran etexilate in the plasma and liver yields the active form, dabigatran. Dabigatran competitively and reversibly binds to thrombin thereby inhibiting its ability to convert fibrinogen to fibrin during the coagulation cascade Mechanism of action 1224 Antithrombotic Therapy for Secondary Stroke Prevention Absorption Volume of distribution Protein binding Metabolism Route of elimination Half life Clearance Toxicity Drug interactions Peak plasma concentrations were achieved in 6 hours in post surgical patients. The absolute bioavailability of dabigatran in the body after administration of dabigatran etexilate was 6. Food does not affect the bioavailability of dabigatran etexilate, but it delays the time to peak plasma concentrations by 2 hours. Therefore, capsules should not be opened and pellets taken alone Moderate tissue distribution with Vd of 60-70 l Relatively low binding (34-35%) to plasma proteins Dabigatran is typically metabolised by esterases and microsomal carboxylesterases.
Generic 375 mg augmentin free shipping
Since inflammatory myopathies are mostly chronic antibiotics simplified pdf order augmentin mastercard, initial complaints are myalgia, fatigue and proximal, symmetric muscle weakness. Patients will report difficulty with repetitive movements such as climbing stairs or raising their arms. Rarely, patients will experience an acutely malignant acceleration of weakness involving the pharyngeal muscles, increasing the risk for aspiration; and, ultimately, if the diaphragm is involved, respiratory compromise will occur. In addition to typical upper respiratory complaints, myalgias are often only initially present. With time, a focal, intense myositis affecting the calf muscles appears, which is a hallmark of influenza infection. Endocrine myopathies can be caused by pituitary, thyroid, parathyroid or adrenal dysfunction. In reality, these endocrine organs are interconnected physiologically and therefore a lack of function in one area may lead to a loss of function downstream. For example, loss of proper hypothalamic function often leads to secondary pituitary and adrenal dysfunction. If endocrine dysfunction is suspected, the clinical examination should reflect the underlying endocrine loss or gain of normal activity. Periodic paralysis is an episodic weakness due to channelopathies at the muscle membrane. Hyperexcitable muscle clinically presents as either myotonia (delayed relaxation after voluntary muscle contraction) or paramyotonia (myotonia that worsens with exercise), whereas hypoexcitation of the muscle membrane leads to periodic paralysis. The most common channels found to cause myopathies include sodium, calcium and potassium. These episodes of periodic paralysis can be precipitated by large carbohydrate meals, electrolyte disturbances and thyrotoxic states. Diagnosis of myopathic disease should include serologic markers of muscle disease. These initial studies help with diagnosis and also serve as a baseline to follow once treatment is started. Electrodiagnostic studies in acute weakness, both electromyography and nerve conduction studies, are crucial to categorizing neuropathic versus myopathic weakness as well. Every encounter should begin with a history of present illness that inquires about recent illness, transient neurologic symptoms, and focuses the symptoms tempo, localization and progression. Neuromuscular disease can be localized to the central nervous system or the peripheral nervous system; therefore, a complete neurologic examination is crucial to guide what the next step should be. On the other hand, patients presenting with a progressive weakness should be monitored for respiratory compromise because their symptoms may yet plateau. Corticosteroid therapy has been used in many clinical settings, but recent advancements in immune therapy provide us with a more effective means to treat patients with a wide variety of neuromuscular disease. Weakness leading to respiratory compromise is one of the most important complications to avoid, which is why early aggressive intervention can often prevent this from occurring. Idiopathic transverse myelitis: corticosteroids, plasma exchange, or cyclophosphamide. Godoy 2, Pablo Correa 1 1 2 Neurosurgical Department, Sanatorio Pasteur, Catamarca, Argentina Neurointensive Care Unit, Sanatorio Pasteur. The second section provides the reader with basic information about the distinct etiologies. We will use here the term "paraplegia" which embraces possible cases of quadriplegia. Intense pain in a well-defined segment of the vertebral column can be an indicator of a medullary compression syndrome. The presence of a severe oncologic or rheumatologic disease can be an indicator of extrinsic medullary compression. Flaccid paraplegia of medullary origin results from injuries to the motor neurons of the anterior horns of the spinal cord as well as their intramedullar axis-cylinder prolongations. Initially, there can be bladder retention (balloon) and intestinal paralysis (abdominal strain) prior to incontinence. Spastic paraplegias ensue from bilateral injuries of the pyramidal tract; they are characterized by paralysis with spasticity and evident hypertonicity. Initially, they can go through a more or less brief phase of flaccid paralysis or gradual simultaneous paralysis and spasticity. The lower limbs are usually extended with tight thighs and knees as well as cauda equina. According to the level of damage, the cutaneous abdominal reflexes can be missing or can also be missing earlier in multiple sclerosis. The reflexes of medullary automatism are usually exaggerated, sphincter function is also compromised and walking becomes difficult or impossible. Less frequently, spastic paraplegias are of the flexion type instead of the extension type. In general, they are the result of medullary compression processes, though some other causes such as multiple sclerosis, syringomyelia or other inflammatory processes (syphilis, tuberculosis, etc. Flaccid paraplegias of non-medullary origin can have radicular and neuritic causes. In this case, neither the Babinski sign nor sphincter function is affected and sensitive function is also preserved. This kind intradural extramedullary of evolution could indicate the possibilitumours, etc. Numbering among acute or subacute medullary injuries are extrinsic compressive injuries (secondary tumour metastases to the spine, epidural or subdural abscesses, etc. If a primary medullary injury is suspected (intramedullary tumour, syringomyelia, demyelination disease, etc. It can be a pre-existing cancer or one whose onset becomes evident from the metastasis that causes the compression. It must be taken in to account that cancer is not the only cause of medullary compression. There are other less frequent causes such as epidural abscesses, epidural hematoma, lipomatosis, etc. It is estimated that at some point between 5% and 10% of all cancers develop metastases in the spine. The most frequent ones are lung cancer, breast cancer, melanoma, lymphoma, prostate and colon cancer. In almost one third of cases, multiple spinal metastases are found and in 70% of cases they are located in the dorsal spine. The spinal cord edema can generally be improved with the use of corticoids at a first stage. When percussion of the spinous process causes precisely located pain, this can lead us to suspect mechanical spinal cord compression. In general it will be a case of acute or subacute paraparesis that will develop pyramidal signs. Motor difficulty can result from impairment of the spinocerebellar tracts, and the symptoms will be clumsiness and ataxia.
Diseases
- Hereditary hemorrhagic telangiectasia
- Dysfibrinogenemia, familial
- Myhre syndrome
- Tuberculous meningitis
- Usher syndrome, type IB
- Circumscribed disseminated keratosis Jadassohn Lew type
- Kousseff Nichols syndrome
Purchase augmentin canada
Halting sedative infusions and allowing patients to "wake up" on a daily basis reduces the risks of accumulation of longer acting agents antimicrobial cleaner purchase generic augmentin, duration of mechanical ventilation and length of stay. Nevertheless, daily sedation holds are not appropriate in all patients and are not a substitute, but an adjunct to appropriate sedation monitoring and sedative dose titration. Sedative drug choice is also important; for instance, a comparison of patients sedated with dexmedetomidine versus lorazepam demonstrated an increase in coma-free days and trend towards delirium-free days in the dexmedetomidine group. The effect of these methods of sedation on delirium is the subject of ongoing investigations. Managing the disruptive behaviours is often demanding of time and attention and has been highlighted as a cause of stopping or abbreviating care delivery to another patient. Under these circumstances, the newcomer physician may feel urged to quickly end the agitation episode. However, medications only become necessary when other interventions are ineffective in controlling agitation, or to prevent patients endangering themselves or others. Whenever possible, an accurate and fast diagnosis of the cause of agitation should be performed before implementing any pharmacological treatment ("look around" before searching for a syringe). The behavior of an agitated patient is impossible to predict, therefore, there are not rigid guidelines for the management of these cases. Verbal containment, if possible, should precede the use of any other therapeutic procedure. In this phase, the first line of intervention is to develop dialogue with the patient, a companion or family members may also contribute. The attitude toward the agitated patient should be reassuring, and nonjudgmental, they should be approached with a soft and calm voice, while showing interest in their problems and making it clear that the intentions are to help them. Once this point has been reached, we should explain that restriction is not a punishment, but a procedure for his safety, because he is unable to control his behavior. Thus, drug treatment should be reserved for 1) patients whose symptoms of delirium would threaten their own safety or the safety of others, 2) to relieve distress in a highly agitated or hallucinating patient, or 3) in order to carry out essential medical treatment or investigations. It has been proven to be useful in the treatment of both hyperactive or hypoactive subtypes. Once the agitation subsides, scheduled doses (every 4 to 6 hours) should be continued for a few days, followed by tapered doses for several days (up to 7 or 10 days upon symptoms fully resolve). It is important to bear in mind that, usually, the elderly population needs lower doses. Generally, intravenous use of haloperidol is associated with lower incidence of extrapiramydal adverse effects but a higher risk of developing Torsades de pointes. The use of haloperidol should also be avoided in case of hepatic failure, anticholinergic toxicity, and patients with Lewy body dementia. The administration of haloperidol in delirium tremens is somewhat controversial since it reduces the threshold to seizures. However, some clinicians use it as adjunctive therapy with benzodiazepines to control psychiatric symptoms associated with this delirium such as anxiousness, hallucinations, and combativeness. Droperidol, chlorpromazine, levomepromazine and pimozide have all been used in the treatment of hyperactive delirium. Levomepromazine and chlorpromazine have been used for very agitated delirious patients, largely because these drugs are more sedative compared to haloperidol, however, these two drugs are not recommended in hypoactive delirium because they cause excessive sedation; on the other hand, chlorpromazine causes local irritation, an effect to take in to consideration at the time of peripheral intravenous administration. Benzodiazepines are the treatment of choice for delirium tremens and alcohol withdrawal. So far, there is no evidence to support the use of benzodiazepines in the treatment of non-alcohol withdrawal related delirium among hospitalized patients, conversely, when benzodiazepines are used to treat agitation associated with delirium from other causes, they often make it worse, particularly in patients with dementia. There are not studies showing one benzodiazepine to be more effective than another in treating delirium tremens. Selection of a benzodiazepines is dependent on several factors including route of administration, onset and duration of action, hepatic and renal function; lorazepam, for instance, does not have active metabolites, making it an attractive choice for patients with decreased hepatic or renal function. Doses of benzodiazepines used during delirium tremens may exceed that which is considered to be normal; genetic differences in patients may contribute to the variable response seen with these drugs. Clonidine (an -2 receptor agonist) does not stop the delirium or seizures associated with the withdrawal process, however, it is a good adjunctive therapy to treat the symptoms of autonomic hyperactivity. Comparative studies of haloperidol and atypical antipsychotics have failed to identify evidence of any advantage in terms of clinical efficacy. It has also been suggested that, few of these new anti-psychotic drugs have a faster onset of action than haloperidol. Unfortunately, many of these new anti-psychotics are only available as oral formulations. Defining delirium for the International Classification of Diseases, 11th Revision. Different effects of spinally applied Cox-1, Cox-2, and nonselective cyclooxygenase inhibitors on inflammation-evoked spinal hyperexcitability. Spinal antinociceptive effects of cyclooxygenase inhibition during inflammation: Involvement of prostaglandins and endocannabinoids. Swiss Med Wkly 2004; 134: 333-46 1341 68 Acute Hypertensive Response and Stroke Alber to Maud 1, Mustapha A. There is a direct and indirect association between chronic arterial hypertension and ischemic stroke. Hypertension is the most common risk factor for small subcortical infarct associated with small vessel disease in the brain [2]. Moreover, hypertension is a known risk factor that predispose for atherosclerosis in the large cervical and intracranial vessels, which constitute the most common etiology of acute ischemic stroke [3]. On the other hand, hypertension is the most important risk factor for spontaneous intracerebral hemorrhage and it has been associated with about 50% of all the intracerebral hemorrhages [4]. Elevated blood pressure is quite common in acute phase of ischemic or hemorrhagic stroke. Management of acute hypertensive response in acute stroke involves physicians from different disciplines including but not limited to emergency physicians, intensivists, primary care physicians, neurologists, neurosurgeons, and cardiologists. In this chapter we will emphasize the importance of the elevation in blood pressure after ischemic and hemorrhagic stroke and we will discuss its epidemiology, pathophysiology, and current evidence of blood pressure management. This definition of hypertension is a threshold for the use of long-term antihypertensive treatment that is supported by evidence derived from randomized trials and clinic population-based data that demonstrate reduction in cardiovascular events with this threshold for treatment. The same definition cannot be applied in the case of acute hypertensive response, because the above-mentioned ascertainment criteria and rationale are not valid. With approximately 15 million patients experiencing stroke worldwide each year, the acute hypertensive response may be expected in approximately 10 million patients per year [10]. In a systematic review of 18 studies, 52% of patients with stroke were reported to have high blood pressure at the time of the admission. In the same study, the subgroup analysis showed that 67% of the patients with ischemic stroke presented with elevated blood pressure compared to 75% and 100% of the patients with intracranial hemorrhage and subarachnoid hemorrhage, respectively. It has been reported that up to one third of the patients presenting with acute stroke have elevated blood pressure and there is tendency to normalization within ten days with spontaneous reduction without any antihypertensive treatment [12]. In the same study the marked elevated blood pressure (systolic blood pressure >145 mmHg) during the admission and persistent inadequate blood pressure control were both associated with poor clinical outcome [11]. In chronic arterial hypertension, the lower end of the autoregulation curve is shifted toward high pressure, presumably because vessel wall thickening and luminal narrowing limit the capacity of the resistance vessels for dilation [18]. Other conditions, such as cerebral vasospasm in subarachnoid hemorrhage, also cause arteriolar constriction, which shifts the autoregulatory range toward higher values [21]. In these circumstances (chronic hypertension and vasospasm) there is a clear shift of the autoregulatory curve towards the right. Thus, there is a potential risk of ischemic brain injury with sudden decrease in the cerebral perfusion pressure below the lower limit of the autoregulation [22]. In absence of a more sensitive method to evaluate the peristroke perfusion changes, the measure of the global perfusion pressure remains still useful. The underlying reason for high blood pressure in the setting of acute stroke is not known. In part, could be just the reflection of inadequately treated or undetected chronic hypertension [24]. However, the tendency to spontaneous reduction in the subacute phase of the stroke supports the role of other transient and stroke-specific related mechanisms [25]. The parasympathetic and sympathetic nervous systems are lateralized to the left and right cerebral hemispheres, respectively [26]. Prefrontal and insular cortices provide inhibitory and excitatory input, respectively, through pathways that connect to the nuclei in the brainstem, particularly in nucleus tractus solitarius and ventrolateral medulla [27,28].
Augmentin 375 mg otc
Both Mark and Lise: It was allowed to show every feeling there was the way I wanted or needed to treatment for dogs broken leg purchase 375mg augmentin with amex. Lise: We loved to do things together, we were home a lot, there was something going on all the time. I had to look out for outbursts of rage, and I learned to avoid unnecessary risks. If one does not understand, it is impossible to believe anything the other one says. Mark: I had all the time in the world, and I used it holding pipes in a bag for 15 years. Mark: I think playing would have been allowed, but I dared not; there was nothing we would share. Mark: Now I think again and again how to express myself to avoid hurting my wife anymore. Both Mark and Lise: There is not much humour in our relationship, but some anyhow. I try now to be more sincere, to be myself, to show my feelings, though there is a well-developed and alert controlling unit in the back of my head. Mark: My actions seem nowadays to speak for themselves and whatever they want to say. Lise: There is hardly any intimacy, tenderness, or sex; some tenderness is anyhow on its way back to our lives. Lise: I am used to this situation, and I even have given some responsibility back to him. She also had to give care to all who needed it, but was not able to get any care herself. Lise missed her partner, whom she formally could have trusted in everything, and with whom it was fun to be. Mark was disappointed with himself all the time and could not understand his actions. The most frightening act was the incident of abuse, which was completely against everything Mark had always believed. The total difference of these two situations meant that these spouses had a long bridge to build from the first narrative to a new and possible present one. They both could have avoided the despair they were experiencing when neuropsychotherapy started. Lise was able to choose to stay in the relationship, as she could see both the possibility of leaving and the possibility for change in their relationship. Most importantly, she become again a partner instead of the assistant and caretaker she had been for years. The most important moment in the course of the therapy was when Mark and Lise for the first time in many years looked each other in the eye. After that, they started communicating with each other, often, if not always, without a mediator. The extremely demanding operations caused severe complications: the loss of vision in the right eye and narrowness of vision in the left eye. In addition, the epileptic seizures remained and turned out to be partly resistant to medication. Mild memory impairment and cognitive slowness were the only neuropsychological deficits that were recognized. One 196 Introduction to Neuropsychotherapy year after the insult, Henry returned to his demanding work as an organization welfare consultant. Nine years after the first insult, he had a right hemispheric infarction in the areas of the brain operation. The thematic division is based on our ideas of the emotional regulation in the situation where the old narratives are not usable anymore. Responsibility-sharing and taking: Irene: It seems that our way to share everyday duties has changed enormously. I feel that the responsibilities related to money belong to me, even though I am not at all interested in economical issues. Henry: Previously, I took more responsibility of family matters, but now my wife has been forced to take that role. Within the changes of the equilibrium in the area of responsibilities, the interview revealed a new emotional tone of being related. Part of my experiences might be related to our long history together, I am not sure. Caring-emotional bonding and expression: Irene: the expression of feelings has certainly been allowed in our long marital relationship, both in the past as well as in the present. In one way, this is an issue related to protection and care, but on the other hand, I am not happy with it. Henry: the feelings have been shown earlier, and also nowadays, when the time has moved on from the acute times of falling ill. I feel more safe, and also sense that I am accepted with my weaknesses and the diminished abilities. Challenge to Change in the Family Narrative 197 When the expression of feelings has changed, it inevitably creates challenges in interpreting intimate information as well. Shaded body messages are difficult to code, and thus, the ability to accept physical contact might be compromised. Irene: Physical closeness may not have narrowed, but the sexual intimacy has diminished indeed. I often wonder whether this is related to aging or what, both me and Henry being not so interested in sex. Irene: We have always spent much time together, however, the ways of commonness have changed. Nowadays, we are forced to make more plans, and doing things together is much more time consuming than it used to be. On the contrary, my wife has a lack of time and, therefore, she is sensing the unnecessary feeling of guilt. Communication-receiving and interpreting messages: Irene: I think that communication between us has always been pretty good. I feel that my temper is very quick, and sometimes I have difficulties in waiting for a sign that my messages have been received, and answered as well. Henry: We do communicate, but we cannot always get ourselves expressed as we wished. That leads to emotional overload and exaggeration of angry expressions, or the need to cry weeks after the struggle. On the other hand, we are also able to talk very openly about all our feelings related to us. During a long relationship, humourous nuances and tones of all expressions are merged to form a shared, mutual understanding for both hidden and unhidden contextual meanings. Concluding Remarks From the clinical point of view, the neuropsychotherapeutic approach is a way to combine the past, present, and future in both psychotherapeutic and neurocognitive perspectives in challenging family narratives. If either approach is left out, the core of the human mind, with its connections to the brain, would be missed. Neuropsychotherapeutic insight deepens the understanding that even the slightest change in the integrated areas of the neural network in the brain cause variable outbursts in the level of behaviour. Within these changes, the family system, as well as shared narratives, must be reconfigured. In addition, the neuropsychotherapeutic setting creates a safe and protective surrounding for bridging the old narratives and new experiences. The search for a narrative-Investigating acute psychosis and the need-adapted treatment model from the narrative viewpoint. Patients and their family members are faced with longlasting changes and suffering while attempting to manage with the consequences of the injury. The main external causes are falls, traffic accidents, 199 200 Introduction to Neuropsychotherapy and violence (Langlois et al. According to the modern approaches, patients need to learn to become aware of their difficulties to learn to compensate for them when necessary and to make realistic commitments and healthy choices in their lives (Prigatano, 1999). Psychotherapy is now an approach used within several models of neurorehabilitation (Coetzer, 2007). Therefore, a specific form of psychotherapy, neuropsychotherapy, is needed (Judd, 1999). During the last decades, neurorehabilitation has developed tremendously, resulting in many different treatment programs.
Purchase 1000 mg augmentin with mastercard
Moreover antibiotics ointment for acne purchase augmentin australia, experimental animal studies have shown that besides reducing serum glucose concentrations, insulin has other beneficial pleiotropic neuroprotective effects [10]. In this chapter, we will review the aspects related to the detrimental role of Hyperglycemia on the injured brain, and we will analyze the available evidence on glycemic control in neurocritically ill patients. Although it weighs about 1500 g, accounting for only 2% of body weight, it receives 15% of cardiac output, 20% of the oxygen and 25% of the total glucose consumed by the entire organ1269 Intensive Care in Neurology and Neurosurgery ism. As one might expect of an organ with highly specialized functions, the brain has a significant spare capacity because it only removes slightly over one third (33%) of the available oxygen and only 10% of the glucose. The cerebral metabolic consumption of glucose is 5 mg/100 g of brain parenchyma/min, which is equivalent to 140 grams per day. The range of brain glucose fluctuation is much smaller than that of blood glucose during euglycemia [34]. In rats, an increase of 50 mg/dl in blood glucose level from baseline only caused a 10 mg/dl increase in brain glucose level [35]. The brain microenvironment is isolated from the plasma by the blood brain barrier formed by tight junctions between vascular endothelial cells, where tightness excludes free diffusion of polar, hydrophilic molecules such as glucose resulting in a constant and significant glucose concentration gradient from blood to brain (Barros et al. Because glucose cannot freely enter the brain, it requires a transport system to cross the endothelial cells of the blood-brain barrier and the membranes of neurons and astrocytes. Both carrier proteins are facilitative glucose transporters that allow glucose to enter cells independently of insulin and are activated by cytokines released via inflammatory responses. They are also upregulated during periods of increased brain activity in order to optimize glucose transport according to demand. Unidirectional model of glucose stores available mainly in astrocytes are transport. The central nervous system cells need a sufficient availability of substrate so they can generate energy to develop and maintain their functions. The pathway that glucose must follow in order to produce energy is a multisequential and finely regulated process. Very low glucose concentrations can immediately induce seizures, loss of consciousness, and death, while chronic hyperglycemia induces changes in hippocampal gene expression and function [38]. As mentioned, glucose can originate intermediates such as lactate and pyruvate, metabolites which in certain circumstances can maintain neuronal activity. However, neither molecule crosses the blood-brain barrier freely, and because neither of the two have specific carriers they cannot replace glucose as a cerebral energy substrate in physiological conditions. Numerous studies have investigated molecules that could substitute glucose as an alternative substrate for brain energy metabolism. Among the vast array of molecules tested, mannose is the only one that can sustain normal brain function in the absence of glucose. Mannose crosses the blood-brain barrier and is converted to fructose-6-phosphate, a physiological intermediate of the glycolytic pathway, via enzymatic steps. However, mannose is not normally present in the blood and therefore cannot be considered a physiological substrate for brain energy metabolism. When formed inside the brain parenchyma, however, they are useful metabolic substrates for neural cells [41,42]. In certain pathological conditions such as fasting, malnutrition, diabetes, and ketonic states, acetoacetate and D-3-hydroxybutyrate are markedly elevated because they may be used by the brain as metabolic substrates. As a corollary to these studies, steadystate arterial-venous (A-V) differences provide indirect evidence that a substance can either be used as a substrate by the brain (a positive A-V difference) or produced by the brain (a negative A-V difference) from a particular substrate such as glucose. Thus, in ketotic states, positive A-V differences have been measured for acetoacetate and D-3-hydroxybutyrate, indicating net utilization under these particular conditions. A net release of lactate and pyruvate (a negative A-V difference) is occasionally found in normal individuals and more frequently in aged subjects or during convulsions. This makes it clear that glucose is the brain energy plant and that it participates in various processes fundamental to brain cell activity. Furthermore, an increase in glucose utilization following the activation of pathways subserving specific modalities, such as visual, auditory, olfactory, or somatosensory stimulation, as well as during motor activity, has been found in the pertinent brain structures [43]. Glucose utilization by the gray matter varies between 5 and 15 mg per 100 g of tissue per minute. Another interesting aspect of the two techniques is the simultaneous study of cerebral consumption of glucose and oxygen, together with blood flow, which has enabled and enhanced our understanding of phenomena occurring not only during functional activation but perhaps more importantly during situations of injury, clearly establishing a relationship between functional activity and energy metabolism. Most current information on brain energy metabolism comes from studies of purified cell cultures enriched with astrocytes, neurons and endothelial cells. However, caution is warranted when extrapolating results obtained in vitro to in vivo situations. It is generally accepted, however, that insights may be gained from these cellularly homogeneous preparations. The results have allowed to review classic assumptions which considered neurons as the only metabolically active cell group and to properly reflect on what happens in the whole brain. Although there are anatomical and structural differences between species, the neuronal population contributes up to 50% of the cerebral cortical volume. In addition, there are strong arguments for attributing astrocytes a key role in brain energy metabolism. Structurally speaking, there are 10 astrocytes per neuron, a relationship found in all brain regions studied. Astrocytes are star-shaped cells strategically located around synapses; they possess receptors for a variety of neurotransmitters and reuptake sites mainly for glutamate. Glutamate, the major excitatory amino acid, after exercising its function is taken up by astrocytes in the postsynaptic terminals and converted to glutamine, which is then released and taken up by neurons to maintain the neurotransmitter pool. Recent magnetic resonance spectroscopy studies in humans have shown that for every molecule of glutamate released from active synaptic terminals and captured by astrocytes one glucose molecule can be metabolized to lactate. In summary, during neuronal activation lactate is released in to the perisynaptic space, the astrocyte detects it and stimulates glucose uptake from the bloodstream. Astrocytes have two well-established functions: 1) to maintain extracellular potassium homeostasis; and 2) to ensure neurotransmitter reuptake (mainly glutamate). Their shape and location suggest they play a key role in the transit of glucose from the bloodstream and in the coupling of energy metabolism to synaptic activity. This is accomplished by dif1273 Intensive Care in Neurology and Neurosurgery ferent types of signals: either metabolites such as lactate, adenosine, K+, H+, or neurotransmitters (vasoactive intestinal peptide, noradrenalin, acetylcholine) or nitric oxide. The brain enters a state of energy dysfunction, called a "metabolic crisis" by some authors. Energy dysfunction is characterized by its heterogeneity (not all brain areas are affected in the same way), and a marked decrease in oxidative metabolism and alterations in glucose metabolism. Immediately after primary brain damage, glucose use dramatically increases to ensure the supply of enough energy to meet the increased metabolic demands, thereby maintaining ion gradients and cell membrane function intact. During this phase, secondary events such as seizures, intracranial hypertension, and hypoglycemia increase the demands on a tissue already working at diminished capacity, further compromising the limited energy reserves available to mitigate catastrophe. Importantly, in pathological situations where the energy production is reduced and the cells cannot metabolize lactate aerobically, utilizing glucose acquires enormous significance. The main source of glucose derives from the extracellular space which, in turn, depends on an adequate supply and transport of glucose from the bloodstream. In these conditions, adequate glucose supplies to the brain might only be sustained when the concentration of systemic glucose is sufficient. Glucose can produce metabolic intermediates, such as lactate and pyruvate, which do not necessarily enter the tricarboxylic acid cycle but rather can be released and removed by the circulation. In this context, astrocytes play a role in glucose uptake by neurons by processing glucose through a glycolytic pathway and subsequently releasing lactate as a metabolic neuronal substrate [53]. Glucose metabolism in neurons is directed mainly to the pentose phosphate pathway, leading to the regeneration of reduced glutathione. Furthermore, transport of glucose at the blood-brain barrier and the neuronal plasma membrane may become inadequate to satisfy brain cellular metabolism. The initial phase characterized by compensatory hyperglycemic glycolysis is typically followed by a regionally heterogeneous reduction in energy consumption, with a reduction 1274 Glycemic Control During Acute Cerebral Injury in cerebral metabolic oxidative metabolism and alterations in glucose metabolism [58].
1000mg augmentin otc
Both have been studied in trials which evaluated them individually and in combination bacteria journal buy 375mg augmentin mastercard. The recommended regimen is 2 g/kg (ideal body weight) divided in to 5 doses given once daily as 0. First, when calculating the dosing, you may land on a dosage that is in between two vial sizes. We recommend simply rounding up to the next highest dose (calculated 32 g per day rounded to a 35 g vial). Subsequently, when ordering baseline serology, also include a serum IgA level to screen for patients with IgA deficiency who may be at risk for anaphylaxis. These antibodies act to ultimately decrease the total number of functional postsynaptic receptors. Population studies demonstrate a prevalence of 20 per 100,000, with a bimodal distribution of both early and late onset. Early-onset women outnumber men during the second and third decades of life, while late-onset men outnumber women during the sixth and seventh decades. Thymectomy is recommended for patients with generalized weakness prior to the age of 50 years. Approximately 15 to 25% of patients with generalized weakness due to a myasthenic exacerbation will evolve in to myasthenic crisis requiring ventilatory support, with a mortality rate of 4 to 13%. When attempting to elicit ptosis, the examiner should fatigue the patient with sustained upgaze for 60-180 seconds, while having the patient sustain gaze in any field for 30 seconds should test cranial nerve weakness. Bulbar weakness can be noted with drooping at the corner of the mouth when smiling, recent history of dysphagia and dysarthria. Dysphagia is often due to soft palate and tongue weakness that may lead to difficulties with swallowing a food bolus. Patients may also note a change in their voice to a more hypophonic/nasal quality due to a combination of facial and tongue weakness. Testing muscle weakness in limb muscles is often facilitated by having the patient repeat functional actions 10 to 20 times in between examinations to check for diminishing strength. Having the patient raise their leg and hold it at 30-40 degrees for 1-2 minutes, or rising from a chair or squatting 10-20 times are simple tests for revealing fatigable weakness. Finally, one of the most feared complication is respiratory weakness, which may be underappreciated in a patient with a chief complaint of generalized weakness. Any combination of weakness with inspiration/expiration and a weak cough in the setting of tachypnea are signs of impending respiratory failure. Recent illness (urinary tract infection, respiratory infection) or a decrease in baseline steroid or immunosuppression can trigger an exacerbation. Many medications are also known to trigger exacerbations such as calcium channel blockers (diltiazem, verapamil), aminoglycosides (gentamicin, clindamycin) and beta blockers. During pregnancy, the immediate post-partum period and during labour, medications such tocolytic agents (terbutaline), as well as magnesium sulphate, can worsen myasthenic symptoms. The diagnosis of myasthenia gravis is based on history and physical findings, then confirmed by serum studies, neurophysiologic testing and/or pharmacologic testing. This test is the classic method for evaluating a patient with observable or subjective weakness; however, it is no longer performed routinely in the United States due to risks to the patient and lack of the medication itself. If the test is being considered, it should be deferred in patients with respiratory insufficiency because it can increase pulmonary secretions. Most pharmacologic confirmation comes from a diagnostic and therapeutic trial of cholinesterase inhibitor and the most commonly prescribed drug is oral pyridostigmine bromide (Mestinon). Patients can sense an onset of the medication effect within 30-45 minutes, which allow for this diagnostic and therapeutic trial to easily occur in an emergency room setting. One indirect method that acts as a local cholinesterase inhibitor is the "ice pack" test. By placing a small bag of ice on the lid of a patient with ptosis, the breakdown of acetylcholine should be slowed temporarily and the ptosis should improve. Repetitive stimulation (2-5 Hz) should cause a decreasing response and lead to failure at the neuromuscular junction. Finally, acetylcholine receptor-blocking antibodies and receptor-modulating antibodies can also be found in a small percentage of patients. Enough emphasis cannot be placed on the importance of both a thorough history and physical exam when an examiner first encounters a patient with neuromuscular weakness. Once a patient is felt to require inpatient admission, a few simultaneous events should occur. During initial clinical assessment, if the patient demonstrates "paradoxical breathing" (movement of chest outward and abdomen inward), shortness of breath (inability to count beyond 20 in one breath) and/or tachypnoea, the physician in charge should anticipate the probable evolution of a myasthenic exacerbation of a myasthenic crisis. Myasthenic crisis can be defined as a patient who develops respiratory insufficiency that may necessitate mechanical ventilation. In addition to bedside spirometry, further data to be collected are arterial blood gases, continuous pulse oximetry, cardiac telemetry and serial mental status assessment. Cardiac telemetry is also important because arrhythmias are a common cause of death in myasthenic crisis. Serial mental status examination is a useful means to monitor the patient for respiratory compromise and decreasing airway protection. Evaluation for early elective mechanical ventilation will avoid emergency intubations and decrease the risk of aspiration pneumonia. The first choice, non-invasive positive pressure ventilation, may be a viable option in patients without hypercapnia and it may afford enough time for medical therapy to take effect. Especially with a change in mental status, the patient will no longer be able to protect their airway by removing the facemask. One final note regarding mechanical ventilation is to not overlook the importance of discussing with the patient and family members the future possibility of ventilatory support prior to its need. Especially in the elderly or those with advance directives, knowing that intubation during a myasthenic crisis often acts as a temporary bridge, helps patients and their families make fully informed decisions. This also allows the clinician to make an educated decision if respiratory failure occurs in the middle of the night and the patient no longer retains a decision making capacity. Initial concomitant introduction of high-dose steroid therapy is not recommended due to the possibility of exacerbating myasthenic symptoms; however, if the patient begins to improve by day 3, one can consider its addition. Patients who evolve in to a myasthenic crisis or present with one require plasma exchange therapy, which provides slightly more robust results in a shorter time period. With any suspicion of pneumonia or other source of infection, treatment of that infection is equally important. Yet, up to one third of patients may have retained reflexes and cranial nerves are often spared. In a patient with previous spontaneous movements and intact sensation, failure to withdraw to painful stimuli applied to a distal extremity should suggest sensory loss. Often, reflexes are normal or slightly decreased and the sensory exam should remain intact. Whenever evaluating a critically ill patient, it is important to assure that the patient is awake, alert, and understands your commands. Selecting where to biopsy should be based on an area that has not undergone extensive disease because results may be non-diagnostic. In addition, aggressive physical rehabilitation provides the best chance to regain function. Poisoning of the neuromuscular junction can be broadly categorized in to pharmacologic, biologic and environmental. Pharmacologic: Persistent Neuromuscular Blockade Residual neuromuscular blockade has recently increased in incidence as the utilization of neuromuscular blockade has moved beyond intubation and the operating room. Agents for neuromuscular blockade are grouped in to two categories: depolarizing (succinylcholine) and non-depolarizing. Depolarizing agents act by binding to the postsynaptic nicotinic acetylcholine receptor, leading to persistent depolarization. The mechanism of action for this group limits its current use beyond rapid sequence intubation. Non-depolarizing agents bind with postsynaptic nicotinic acetylcholine receptors and prevent acetylcholine from reaching its target, thereby preventing depolarization.