Cheap cardura 4 mg online
Hackenbruch Y excel blood pressure chart purchase genuine cardura online, Meerhoff E, Besio R, Cardoso H: Familial bilateral optic nerve hypoplasia. Creel D, Spekreijse H, Reits D: Evoked potentials in albinos: efficacy of pattern stimuli in detecting misrouted optic fibers. Richmond B, Huizing M, Knapp J, et al: Melanocytes derived from patients with Hermansky-Pudlak Syndrome types 1, 2, and 3 have distinct defects in cargo trafficking. Summit on cerebral/ cortical visual impairment: education, family and medical perspectives. Cioni G, Bertuccelli B, Boldrini A, et al: Correlation between visual function, neurodevelopmental outcome, and magnetic resonance imaging findings in infants with periventricular leucomalacia. Mercuri E, Anker S, Guzzetta A, et al: Visual function at school age in children with neonatal encephalopathy and low Apgar scores. Ruberto G, Salati R, Milano G, et al: Changes in the optic disc excavation of children affected by cerebral visual impairment: a tomographic analysis. Stiers P, Vanderkelen R, Vandenbussche E: Optotype and grating visual acuity in patients with ocular and cerebral visual impairment. Tank A, Taylor D: Worldwise resources for parents of a visually handicapped child. Warden and Shizuo Mukai this article describes retinal diseases presenting in childhood. Emphasis is placed on key characteristics of each entity that are useful for the pediatric ophthalmologist. Categories include tumors, retinal vascular disease, macular lesions, and congenital abnormalities. Two of the more common causes of infectious chorioretinopathies in children, toxoplasmosis and toxocariasis, are also reviewed. Retinoblastoma and retinopathy of prematurity are more fully discussed in Chapters 369, 309, and 136. More rarely, other presenting signs include exudative retinal detachment, intraocular inflammation, hyphema, preseptal or orbital cellulitis, iris neovascularization, and glaucoma. Retinoblastoma is usually diagnosed before the age of 1 year in hereditary (familial or bilateral) cases, and between ages 1 and 3 years in sporadic unilateral cases. Intraocular retinoblastoma can demonstrate endophytic or exophytic growth patterns. With endophytic growth, a creamcolored mass breaks through the internal limiting membrane and seeds into the vitreous. Exophytic tumors are yellow-white and appear deep to the retina and can be associated with a serous retinal detachment. A few general techniques are helpful in minimizing agitation and improving the examination. More panoramic fundus views can be obtained using a 28 or 30 D lens rather than the more standard 20 D lens for indirect ophthalmoscopy. Reasonable views of the posterior pole can also be obtained using a 20 D lens with a Finoff transilluminator as the light source. Ultrasonography in the office is a useful adjunct to indirect ophthalmoscopy in suitable patients. Retinal detachments, foreign bodies, tumors, and calcifications can be identified even in the setting of media opacities. In patients where intravenous fluorescein angiography is not possible, administering it orally is generally better tolerated and still affords useful angiograms especially with digital enhancement of the images. The physician can also use the blue filter in the indirect ophthalmoscope to visualize the transit of fluorescein in the fundus. A better prognosis in many pediatric ophthalmic disorders directly stems from early detection and management. Astrocytic hamartomas often do not affect vision and usually do not require treatment. Though they are more commonly seen in patients with tuberous sclerosis, they also can be found in patients with neurofibromatosis and rarely in the normal population. Choroidal osteomas are relatively flat lesions that can be solitary or less commonly multifocal, and typically are located in the macula or peripapillary region. Distinctive tufts of numerous small vessels resembling spiders may be seen on the osteoma surface. Calcification can be documented by computed tomography (as well as by ultrasonography). Subretinal fluid and hemorrhage may also be present, and chorodial neovascularization occurs in ~1/3 of patients. However, choroidal osteomas may first be noted in infants as they are considered congenital lesions. They are rarely seen in the posterior pole, and are more commonly seen in superotemporal quadrant. Multiple tumors can be seen with both unilateral and bilateral ocular involvement. Vitreous hemorrhage and tractional and rhegmatogenous retinal detachments can also occur. The features of combined hamartomas include preretinal membrane, retinal vessel tortuosity, and hyperpigmentation under the retina. They are usually located near the optic nerve, but also can be found in the peripheral fundus. Combined hamartomas are typically unilateral and not associated with other disorders. Retinal neovascularization is typically not seen, despite the presence of capillary nonperfusion. The most common presenting signs are strabismus and leukocoria, detected on routine screening. Neovascularization of the peripheral retina, dragged vessels and macula, exudation, and exudative retinal detachments can develop. Vitreoretinal traction involving ischemic and atrophic peripheral retina predisposes to retinal tears and rhegmatogenous retinal detachments. The pattern of inheritance is autosomal dominant or X-linked recessive, and family members should therefore be examined. However, lack of a family history does not rule out the diagnosis, as one study found no family history in 55% of the cases. Further complications can include choroidal neovascularization, vitreous hemorrhage, and macular holes. It affects preterm infants with low birth weight and exposure to high oxygen supplementation. In a child, this is seen well with a direct ophthalmoscope using the red-free filter (green light) and the fixation aperture. Affected males have decreased central vision generally ranging from 20/60 to 20/120, and rarely have normal visual acuity. The pisciform lesions are seen at the level of the retinal pigment epithelium and the foveal changes often have a beaten-bronze appearance. Presentation often is in the first two decades of life with progressive bilateral central visual loss, though symptoms and findings can also occur in adulthood. The dark choroid may be the only visible feature of this condition in children, who may present with vision loss before other retinal changes develop. Different stages, which may not occur in all patients, can be seen as the vitelliform lesion evolves over time. The visual prognosis in Best disease is variable, but 76% of patients under the age of 40 maintain 20/40 vision in one eye. Patients with Best disease have the unique finding of an abnormal electrooculogram reading in the setting of a normal electroretinogram. The myelination can obscure underlining retinal blood vessels and be associated with a scotoma. Cotton wool spots can have a similar appearance as myelinated nerve fiber layers, yet are transient in nature.
Cheap cardura 2mg without a prescription
Braue A hypertension 3rd class medical purchase generic cardura online, Ross G, Varigos G, Kelly H: Epidemiology and impact of childhood molluscum contagiosum: a case series and critical review of the literature. Ann Pitsios C, Papadopoulos D, Kompoti E, et al: Efficacy and safety of mometasone furoate vs nedocromil sodium as prophylactic treatment for moderate/severe seasonal allergic rhinitis. Segura S, Romero D, Carrera C, et al: Eczema herpeticum during treatment of atopic dermatitis with 1% pimecrolimus cream. Robb Due to the anatomic organization of chapters in this book, some congenital anomalies of the eye, orbit, and ocular adnexa, including congenital cataract, craniofacial anomalies, ptosis, orbital fibrosis, and optic nerve anomalies are discussed elsewhere. This article will discuss several developmental ocular, orbital, and adnexal anomalies that may affect vision in children, including infantile hemangiomas, orbital venolymphatic anomalies, and abnormalities of the whole eye development including microphthalmia and anophthalmia. Histopathologically, these tumors contain abnormal capillaries and venous channels. The clinical appearance of hemangiomas varies with location, size, and lesion growth. At birth, hemangiomas may be clinically inapparent and typically enlarge in the first 12 months of life (proliferative phase). In the proliferative phase, the superficial skin of the hemangioma may necrose due to ischemia. Subsequent involution occurs over the ensuing years with typical resolution within the first decade. Complete resolution of the lesion is typical, although overlying skin-thinning and prominent vascular channels may persist. Imaging is useful in establishing a diagnosis and differentiating hemangiomas from other vascular malformations, particularly for deep subcutaneous lesions. Infantile hemangiomas occur with a frequency of 40% in the head and neck region, 40% in the extremities, and 20% on the trunk. Amblyopia may occur due to occlusion of the visual axis, or from pressure on the globe and adnexa that may cause an astigmatic refractive error with an axis that is usually oriented toward the location of the lesion. Correction of refractive error and amblyopia therapy are frequently necessary if the lesion involves the eyelids or orbit. Treatment options that have been used to decrease the size of the hemangioma include steroids (topical, oral, and intralesional), systemic alpha-interferon, laser therapy, radiotherapy, and surgical debulking. It is often helpful to have a pediatrician also monitor the child for any steroid-related side effects as infants may be more prone to them. Fundus examination during the intralesional injection is recommended to detect the potential complication of retinal artery embolization. Low-pressure injection and small-gauge needles may reduce the risk of intravascular injection. Steroid treatment, either systemic or local, may cause rapid involution of the lesion with local skin necrosis and ulceration. Local dermal changes such as depigmentation and subcutaneous fat atrophy may also be noted adjacent to the intralesional injection site. Eyeglasses may be necessary to treat induced refractive errors, and occlusion therapy of the fellow eye may be required to reverse the associated refractive or deprivational amblyopia. It is important to offer reassurance to the parents regarding the expected spontaneous resolution of hemangiomas. Histopathological studies have revealed that these lesions are most likely distinct hamartomas. With the advent of surgical navigation systems, there has been use of percutaneous sclerotherapy in the orbit. Orbital venolymphatic malformations frequently become symptomatic with acute intralesional hemorrhage, either spontaneously or with trauma or viral infection. Patients, typically in their first or second decade, develop sudden severe proptosis with motility disturbance, and may have acute glaucoma and optic nerve compression due to the severity of the proptosis. Urgent management with orbital compartment release with canthotomy and cantholysis, or surgical decompression and drainage, may be necessary. In general, the lesions are diffuse and infiltrate the normal tissues of the orbit, so complete surgical excision is impossible and regrowth and recurrent intralesional hemorrhage is common. Clinically, these lesions may appear similar to hemangiomas, and consequently, imaging is essential in establishing a correct diagnosis. Unlike hemangiomas, veno- Congenital dermoids are choristomas, denoting masses of normal tissue found in an abnormal location. Dermoids may occur on the ocular surface (ocular or epibulbar dermoid) or in the orbit or periorbital tissues (orbital dermoid cysts). Orbital dermoid cysts, frequently found at the upper orbital margin or brow, are discussed elsewhere in the book. Epibulbar dermoid at the inferotemporal limbus, at which 76%18 of such lesions occur. Anophthalmia is attributed to a failure of the optic vesicle to form during embryogenesis. They occur sporadically, whether or not they are associated with other facial malformations, and have been linked to mutations at 14q32. If the lesions are relatively inconspicuous, surgery may not be indicated because of the potential scarring and possible effect on ocular motility that may ensue from any extensive dissection in the area. Unfortunately, the associated astigmatism is not reliably improved by this surgery,25 and even with astigmatic spectacle correction, the patient may be left with refractive amblyopia requiring further treatment. In cases with potential for visual rehabilitation, particularly if both eyes are abnormal, treatment should optimize visual potential by cataract surgery and refractive treatment. Treatment of amblyopia, particularly with unilateral severe microphthalmia, however, is difficult and may not be indicated if visual potential is low relative to the contralateral eye. The management of orbital and adnexal deformity associated with microphthalmia should begin as soon as possible with early socket expansion to allow more normal orbital and adnexal growth. The use of orbital expanders is reserved for more severe cases of microphthalmia or anophthalmia. Obtaining a family history or actually examining the parents may be helpful in recognizing inherited cases. Variable expressivity and incomplete penetrance have been observed, and thus individuals with minimal or no findings may carry the mutant gene. Severe microphthalmos with coloboma may also occur with multisystem involvement in many single-gene disorders,34 chromosomal syndromes,35 or nonrandom grouping of malformations (Table 302. Typical colobomas result from failure of the embryonic fissure to close along the inferonasal aspect of the 14q32 Xp11. There is evidence to support the possibility that optic nerve pits, the morning glory syndrome, and the congenital tilted-disk syndrome are all variant products of the process that produces typical colobomas. The prognosis for vision depends on the amount of ocular malformation and the degree of microphthalmia. Coloboma of the optic nerve is usually associated with some decrease in visual acuity, even if the fovea is spared. Secondary retinal detachments caused by a hole at the edge of the coloboma may also cause a reduction in vision. White sclera is visible at the point at which the retinal pigment epithelium and choroid have failed to develop. On the basis of limited data, the recurrence rate for the subsequent child of healthy unrelated parents has been estimated at 9%; for the children of an affected person, this figure is as high as 46%. Persistent fetal vasculature is a distinctive anomaly that occurs sporadically and, for the most part, unilaterally in fullterm normal infants. The lens is often clear at first, but it develops a posterior opacity and swells, causing further shallowing of the anterior chamber and angle-closure glaucoma. Retrolenticular membrane and posterior lens opacity in a patient with persistent fetal vasculature. A hyaloid stalk extends back from the retrolenticular membrane in this enucleated eye with persistent hyperplastic primary vitreous. Persistent fetal vasculature can usually be distinguished from an uncomplicated unilateral congenital cataract by the presence of a shallow anterior chamber and the retrolenticular membrane. It is distinguished from retinopathy of prematurity by its unilaterality and occurrence in full-term infants, and from retinoblastoma by its association with microphthalmos and the lack of intraocular calcification by computed tomography. Rarely, these guides for differential diagnosis are insufficient, and a proper diagnosis can be made only by pathologic examination of an enucleated eye. Retinal detachment and glaucoma have sometimes followed cataract and membrane removal in patients with persistent hyperplastic primary vitreous,57 so a guarded prognosis should be given at the outset of treatment. Forbes G, Earnest F 4th, Waller R: Computed tomography of orbital tumors, including late-generation scanning techniques.
Generic 4 mg cardura with amex
Parents and child must be fully informed of the pros and cons of these new lenses heart attack warnings buy discount cardura line. Irregular astigmatism may be the result of corneal dermoid removal, penetrating keratoplasty, repair of corneal lacerations, among others. The diagnosis is made by excessive scissoring on retinoscopy, difficulty obtaining a crisp endpoint, irregular mires on keratometry, and in severe cases, inability to obtain keratometry readings. The treatment is a hard contact lens, which in effect creates a new, smooth optical surface over the irregular one, or corneal transplant. Down syndrome and Ehlers Danlos syndrome have an association with astigmatism and keratoconus. Isolated capillary hemangiomas of the lid also cause anisometropia, usually inducing myopia on the ipsilateral side. The input that this last group, and their parents, get from the ophthalmologist can be crucial. In general, sympathizing, then asking about friends or peers who wear glasses, can soften the blow. It is often helpful to ask what activities the child enjoys, then point out how much easier they will be, how much more successful the child will be at performing them, when their vision is crystal clear. Discussing that children often ask about new things because they are curious, not cruel, can help prepare families for questions. Having the child rehearse a few responses to comments he/she thinks might be made often helps prepare them. Because of the social issues involving glasses, finding a style that the child likes and is comfortable in is vitally important in having the child comply with treatment. If a child returns with glasses that are obviously ill-fitting or that the child dislikes, this should be addressed. Prematurity increases the risk of myopia, whether or not retinopathy of prematurity occurred. It is important to remember that internal ophthalmoplegia can also occur, causing lack of accommodation. Children with third nerve palsy should have a cycloplegic refraction and a manifest refraction if possible, to determine whether prescribing the hyperopic correction, even if small, improves vision. Herpes zoster infections have been noted to cause third nerve palsies, at times with loss of accommodation. At times closed head trauma without signs of third nerve palsy may result in loss of accommodation and/or convergence which can be treated with a reading add with prism. A child has presented with 20/200 vision, and the cause is found to be myopia, easily treatable with spectacles now and with a variety of other means when the child grows older. For the ophthalmologist, whose differential diagnosis suddenly went from retinal dystrophy, brain tumor, cataracts, etc, to myopia, it is very good news. They may also harbor the belief, widely held, that wearing glasses will make the eyes weaker. Conversely, some parents assume that wearing glasses is curative and believe that if they are worn constantly for a period of time the refractive error will resolve. The news that a child will receive a glasses prescription should therefore be delivered with sensitivity and a large dose of education about what this does and does not mean, as well as specifics about the expected course of the specific refractive error. It is often helpful to begin by stating plainly that the child needs glasses to see clearly and that you will be giving them a prescription. Many parents do not realize that things like antireflective coating, high index plastic for large prescriptions, lenses that become dark when going into sunlight, etc, are optional and at their discretion. It is often helpful to write specifications on the prescription for these options if they are important, and to tell the parents they are optional if not. They may also be more expensive, so parents should be instructed ahead of time about the advantages. Spectacles are a wonderful,effective, but very ancient treatment for disorders of refraction. Genetic predisposition to disordered emmetropization will be assayed, and if a predisposition exists, environmental as well as pharmacologic prophylaxis may be instituted. Growth factors may be available topically to increase the growth of hyperopic or microphthalmic eyes. Gene therapy may be available if genetic assay shows that the genes responsible for ocular growth are abnormal. Pharmaceuticals to stop the progression of myopia could be prescribed as soon as myopia, or lack of appropriate hyperopia, is detected. Precise laser refractive surgery for residual refractive errors could be performed once final ocular growth was complete, and medications would help the results to remain stable. Until these future treatments are reality, for most refractive errors, a combination of current treatment modalities can achieve good vision safely and effectively for children. The bigger challenge is timely diagnosis, which in the future may be improved with universal screening programs, and compliance with prescribed treatment. Sorsby A, Benjamin B, Sheridan M: Refraction and its components during the growth of the eye from the age of 3 years. Abrahamsson M, Fabian G, Sjostrand J: A longitudinal study of a population based sample of astigmatic children. American Association for Pediatric Ophthalmology and Strabismus 32nd Annual Meeting. American Academy of Ophthalmology Pediatric Ophthalmology Panel: Preferred practice pattern: pediatric eye evaluations. Jensen H: Myopia progression in young school children: a prospective study of myopia progression and the effect of a trial with bifocal lenses and beta clocker eye drops. Posters presented at Association for Research in Vision and Ophthalmology and American Association for Pediatric Ophthalmology and Strabismus Annual Meetings, 1995. He M, Zen J, Liu Y, et al: Refractive error and visual impairment in urban children in southern China. Young T, Paluru P, Heon E, et al: A new locus for autosomal dominant high myopia maps to chromosome 17q21-23. Naiglin L, Gazagne C, Dallongeville F, et al: A genome wide scan for familial high myopia suggests a novel locus on chromosome 7q36. Zylberman R, Landau D, Berson D: the influence of study habits on myopia in Jewish teenagers. Framingham Offspring Eye Study Group: Familial aggregation and prevalence of myopia in the Framinham Offspring Eye Study. Fulton Amblyopia, literally dull sight, is a disorder of vision that originates in infants and young children and demands diagnosis and treatment within the first decade. Most often amblyopia is defined as reduced visual acuity in the presence of optimal refractive correction and absence of eye and visual system abnormalities. Usually the visual deficit is monocular and relative visual function clinically distinguishes the amblyopic from nonamblyopic eye in the patient. Clinicians identify the anomalous inputs by the company that they keep: strabismus, refractive error especially if asymmetric, and deprivation of good retinal image such as that caused by cataract. Asymmetry between inputs from the right and left eye become the basis for binocular competition1,2 and places the child at risk for anomalous visual experience and amblyopia. While visual acuity is the most commonly used indicator of amblyopia, other aspects of spatial vision, including contrast sensitivity and vernier acuity, as well as binocular visual functions are affected in amblyopia. Monocular lid suture, induced strabismus or anisometropia create models of amblyopia in young animals born with normal eyes and visual pathways; studies of animals with naturally occurring strabismus also contribute to the understanding of amblyopia. Changes in the binocular properties of neurons in the primary visual cortex, the site where inputs from right and left eye are combined, are produced and result in neurons being driven by the dominant eye. Binocular function is lost as the balance between excitatory and inhibitory connections shift to the dominant eye. The plasticity, or responsiveness, of the immature visual system to extrinsic factors such as lid suture, ocular misalignment, or optical defocus, decreases as the development of the visual system progresses. The sensitive, or critical, period coincides with the period of normal visual development. Interestingly, the developmental segregation of the columns in the visual cortex19 correspond with the onset of stereopsis. These studies underscore the fact that the visual deficit of amblyopia cannot be captured by a single measure of acuity.
Cheap cardura online master card
Re-bleeding occurs in ~4% to 10 % of patients with traumatic hyphema hypertension the silent killer buy discount cardura 2mg on line, and occurs most frequently within 5 days after the injury. A high degree of suspicion for projectile injury is appropriate when a puncture wound is seen, and specific questions related to firearms may be helpful. Unprotected hammering of metal or stone objects or use of power tools can also be associated with projectile injury and retained foreign body. An area of subconjunctival hemorrhage, ecchymosis, or small break in the skin of the eyelid may be the only surface manifestation of a scleral perforation by such an object. Distortion of the pupil may also be the only evidence of a small corneal or limbal perforation. The composition of intraocular foreign bodies can help determine ocular toxicity, guide antibiotic prophylaxis, and may be useful in planning extraction with magnet devices. Superficial foreign bodies may simply be irrigated from the eye with saline or removed with a moist cotton tip. Retrieval of deeply imbedded foreign bodies in children should be performed in the operating room, unless they are old enough and cooperative to sit still at a slit lamp. If an abrasion occurs as a result of a foreign body, broad-spectrum antibiotic coverage should be initiated. Ruptured Globe Eye Injuries A Ruptured globe or open globe is a serious injury for any patient. If an open globe is detected the ocular exam should be completed in the operating room. Topical medications, contact tonometry, scleral depression, local anesthesia, and other ocular manipulations should not be done in the emergency room or office because the intraocular injury may be worsened. In the interim, the patients should be kept comfortable and the eye should be shielded from rubbing or re-injury. Surgical repair of open globe injuries is performed with general anesthesia, usually with microscopic magnification. In these serious injuries, all attempts should be made to repair the injury primarily, rather than remove the eye. It is best to attempt to close all corneal and scleral wounds and then reevaluate the extent and severity of intraocular damage after the integrity of the eye has been repaired. Traumatic cataract surgery can be postponed temporarily, unless the lens material is completely disorganized and interferes with wound closure. Usually, the quality of the intraocular visualization, and therefore the ease and safety of the cataract surgery, is best if corneal wounds have been repaired for several weeks. The potential of primary intraocular lens implantation is also improved with planned, sequential lens removal after emergency repair of the corneal and scleral wound. Delays in removing traumatic cataract may postpone visual rehabilitation, but in general a few weeks delay will have a small impact on the risk of amblyopia and ultimate visual outcome. Viscoelastic material may be useful in reforming the anterior chamber and separating iris from cornea and sclera. Corneal wounds are typically closed with 10-0 nylon sutures, with the knots buried in the corneal stroma. The left globe was obliterated and there were extensive injuries to the lids, orbit, and facial bones. Note a remnant of sclera laterally and the displaced puncta of the lower lid centrally. Pressure patching generally works best for very small leaks, while additional sutures or gluing will be required in more severe leaks. Orbital Foreign bodies Items such as pellets deep in the orbit are frequently safer left in place, though vegetative matter and objects irritating orbital tissue should be removed for threat of cellulitis. With a penetrating injury it is important to find the composition of the foreign body. Alkali burns, in contrast, rapidly penetrate the cornea causing damage to the entire anterior segment. The initial and most vital step in management of chemical injuries is copious irrigation to dilute the chemical, followed by meticulous removal of any particulate matter from the conjunctival fornices. For severely caustic chemicals, such as alkali materials and concentrated cleaning agents, the irrigation should continue for at least 30 min. Topical antibiotic and antiinflammatory therapy are appropriate, with daily re-examination until the corneal abrasion and other injuries have resolved. Depth of the laceration is crucial and a full thickness laceration medial to the punctum virtually guarantees canalicular injury. Lid margin lacerations medial to the punctum may be easily overlooked since they often seal in proper anatomic alignment and occur with minimal evulsive force. Consequently, any eyelid laceration that is directed toward the medial canthus should be inspected to exclude a canalicular injury. When detected, a canalicular injury should be carefully repaired and stented with a monocanalicular stent. Full-thickness eyelid lacerations should be repaired typically in the operating room under general anesthesia. Organic solvents or soaps found in household cleaning agents are the most frequent cause of chemical burns in children. The canaliculus and laceration were repaired with a monocanalicular stent and absorbable sutures in the emergency department under conscious sedation. In contrast to the marginal and canalicular eyelid lacerations, deep skin wounds and superficial wounds can be repaired in the emergency room using absorbable sutures in the appropriate patient. Surgical repair of the orbital blowout is typically approached through a transconjuctival approach for the floor or a transcaruncular approach for the medial wall. Once the subperiosteal space is entered, the four sides of the fracture are identified, cleared of herniated or incarcerated tissue and covered with either an alloplastic or autogenous implant. Forced ductions should always be checked at the beginning and end of the case to ensure no tissue is entrapped and restricting motility. In some small trap-door fractures with diplopia, once the incarcerated tissue is released the fracture can be left alone to heal without an implant. Corneal injuries from forceps inadvertently placed across the orbit during delivery may lead to vertical striae with long-term visual implications. Bruising of the eyelids and brow, and acute corneal hydrops may be seen initially at the time of delivery. Fortunately these may recover spontaneously over time, but require attention by the ophthalmologist to correctly diagnose the injury and prevent amblyopia. Children, like adults, may sustain isolated fractures of the orbital bones due to blunt impact in the region of the eye. Blowout fractures are the most common and either involve the floor or medial wall of the orbit. Plain sinus and facial films may miss many orbital fractures, and do not help in the evaluation of possible orbital tissue incarceration. Fractures of the orbital roof are relatively less common, but are seen in children with an impact to the brow region, typically from a fall from a height of only a few feet. Orbital roof injuries may be associated with intracranial injury, and careful neurologic evaluation of the patient and imaging studies should be done. Most are simple linear breaks, which heal uneventfully without intervention and without a persistent disturbance of ocular motility or eyelid function. When a fragment of bone is displaced inferiority or evidence suggests dural tear, neurosurgical repair should be considered because of possibility of brain tissue herniations into the orbit, although this not a common problem. Prophylactic antibiotic coverage in the case of nondisplaced orbital wall fractures is also an area of some debate in the literature and is not usually necessary. Victims of shaken injury are most often under three years of age and usually under 12 months. Clinical findings in affected infants include subdural hemorrhage, subarachnoid bleeding, hypoxic-ischemic brain injury, retinal hemorrhages, skeletal injuries, and cutaneous as well as other injuries. Unlike most other forms of ocular trauma there are usually minimal external ocular signs of injury. Retinal hemorrhages can be few in number, exclusively intraretinal, and confined to the posterior pole though often they are too numerous to count, present at all layers, and extend to the ora serrata.
Buy 4mg cardura mastercard
Clinicians reviewing this type of visual-field data must be aware of this potential error heart attack headache discount 2mg cardura. Monocular visual-field testing revealed a full field in the right eye and a left temporal hemianopia in the left eye. Binocular visual-field testing in the functional patient demonstrated retention of the hemianopic defect. While in the nonfunctional (or normal) person, the normal nasal hemifield in the right eye compensated for the deficit temporally in the left eye. The visual field normally expands on increasing the testing distance from 1 to 2 m. In the functional patient, this normal expansion of the visual field is absent and remains contracted despite the increase in the testing distance. In certain cases, particularly with healthcare workers who have easy access to topical ophthalmic solutions, the drug may be purposely administered to feign illness. The clinician faced with a patient with a poorly reactive, dilated pupil must differentiate such pharmacologic mydriasis from that with organic causes such as early oculomotor nerve palsy, tonic pupil, and traumatic mydriasis. Convergence spasm or spasm of the near reflex is characterized by intermittent convergence, accommodation and bilateral miosis. During the spasm, there is limited abduction of the eyes while viewing binocularly. The condition is easily recognized by the presence of bilateral pupillary constriction that takes place when the person attempts to look laterally because the patient has used the convergence mechanism to bring the previously abducted eye medially. Although a functional disorder is the most common cause of convergence spasm, organic conditions like a Chiari malformation, head trauma, cerebellar tumors, and diverse central nervous system inflammatory diseases must be ruled out. The nystagmoid eye movements are actually rapid to-and-fro saccades25 and are often initiated by convergence, which may be accompanied by eyelid fluttering or facial musculature contraction. As creation of the effect requires some effort, it is difficult for patients to sustain the nystagmus for more than a few seconds. The left eye demonstrates diffuse depression sparing the inferotemporal quadrant, demarcated along the horizontal and vertical midlines. Voluntary nystagmus may simulate convergence retraction nystagmus, but the latter may be differentiated by mildly dilated pupils and the larger amplitude, lower-frequency movements associated with attempted up gaze in the dorsal midbrain syndrome. It is unwise to attempt to distinguish malingering from hysteria, as most often this distinction cannot be made with certainty, and wrongly accusing a patient of purposely feigning illness may result in legal action against the physician. If no legal action is involved, for adult cases, the physician should provide reassurance and tell patient that there is no damage to the visual system as determined by the examination. It is also good to emphasize that there was no evidence of brain tumor or degenerative neurologic disease, and was a very positive result of all the testing. As mentioned above, follow-up may be necessary to reveal a previously undocumented organic pathology. Further, a follow up examination may be necessary in some cases as it may reveal an unexpected organic pathology. Psychiatric help is not generally required or recommended unless obvious illness is apparent. The approach to managing a child with nonorganic visual disturbance is somewhat different, although the etiologies and tests may be similar. The situation sometimes needs to be discussed with the child alone in the room or the parents alone in the room. The parents should be told that children often react to stress with physical symptoms, commonly ocular, and recommend that the parents consider any possible home or school stress that might have precipitated the condition. The author has seen children with functional visual loss following a recent parental divorce, failure of performance in school and sibling rivalry/stress at home. The child should not be punished for such behavior, as it is often not a conscious occurrence. One should state that recovery may occur over a period of time, so as not to pressure the child to demonstrate recovery too quickly. Kathol and associates31 reexamined 42 patients with nonorganic visual loss at a mean of 4 years after initial evaluation. They found that 55% continued to demonstrate the original abnormality on clinical examination, although only 19% thought that they had any degree of living incapacity as a result of their condition. Catalano and associates32 indicated a recovery rate in children of greater than 75% within several months. It is important to remember that organic visual loss can occur in conjunction with nonorganic visual loss. Functional visual loss should be diagnosed when no other organic disease is found responsible for the visual loss and confirmatory tests for functional visual loss have been established. Glovinsky Y, et al: Artificially produced quadrantanopsia in computed visual field testing. Hirai T, Sato M, Kachi S: Similar etiologies of functional visual loss observed in children and adults. The section on the pupils is divided into two main portions: (1) the use of the pupillary examination to determine asymmetries in afferent visual input between the eyes and (2) the causes of abnormal integration of the efferent output to the pupils. Efferent defects may result in unequal pupils (anisocoria), pupils that fail to dilate well in darkness, or light-near dissociation (the pupillary contraction to a near stimulus greatly exceeding that to light). The accommodation section provides a framework on which to evaluate abnormalities in accommodative amplitude. The pupillary contraction to light is an important neuronal reflex because it gives information about the integrity of both the afferent visual system and the efferent neuronal outflow to each pupil. The retina, optic nerve, chiasm, and optic tracts are composed of neurons that convey visual and pupillary afferent input, so that damage anywhere along this pathway is likely to affect both the pupillary light reflex and visual function. Because of this, the pupillary light reflex has been used for many years by physicians and investigators as an objective means of detecting damage along the pregeniculate afferent visual pathway. The response to near stimuli, such as blur or image disparity, is usually accompanied by the triad of accommodation, convergence of the eyes, and pupillary contraction. Many factors can influence the integration and expression of this response, including optical properties of the eye, state of the retina, attributes of the accommodative stimulus, age, innervation of the ciliary body, and conscious effort. These neurons give rise to postganglionic parasympathetic axons that travel in the short ciliary nerves to the globe, where they synapse with the iris sphincter muscle. The integration of the pupillary light reflex, including the anatomy of the neurons involved, their receptive field properties, and their response to various attributes of light stimuli, has been reviewed. It consists of retinal input from photoreceptors, bipolar neurons, and ganglion cells. Axons of retinal ganglion cells from each eye provide light input information that is conveyed through synapses with interneurons located in the pretectal olivary nucleus of the midbrain. From here, the neurons send their preganglionic parasympathetic axons along the the neuronal integration of the pupillary light reflex begins in the retina with the photoreceptors, bipolar cells, and ganglion cells. For many years, it was disputed whether rods or cones contributed to the pupillary light reflex and whether these were the same photoreceptors as those contributing to visual perception. Extensive experimental and psychophysical work has shown that the neuronal pathways mediating the pupillary light reflex and visual perception share the same photoreceptors. These modifications include changes in retinal adaptation, wavelength of light, stimulus duration, and stimulus light intensity. In fact, in almost every way measured, the pupillary responses to light parallel those of visual perception. The shift in sensitivity is also the same as the eye is changed from a condition of light adaptation to dark adaptation (the Purkinje shift), providing further evidence that the same photoreceptors are used for both pupil and vision. Patients with various abnormalities of rods and cones can be shown to have the same deficits in color vision or lack of appropriate sensitivity change during dark adaptation when the results of visual threshold are compared with the pupillary threshold to light stimuli. Diagram of the pupillary light reflex pathway consisting of the ganglion cell output of the retina, which synapses with the neurons in the ipsilateral pretectal olivary nucleus. These neurons form the preganglionic parasympathetic nerves that travel within the third nerve to synapse in the orbit at the ciliary ganglion. Postganglionic parasympathetic nerve fibers pass from the ciliary ganglion to the eye through the short ciliary nerves to innervate the iris sphincter.
Green Papaya (Papaya). Cardura.
- What is Papaya?
- How does Papaya work?
- Are there safety concerns?
- Are there any interactions with medications?
- Dosing considerations for Papaya.
- Stomach and intestine problems, parasite infections, and other conditions.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96494
Buy cheap cardura 4mg on-line
History Family history (autosomal dominant blood pressure medication starting with b purchase 2mg cardura with mastercard, X-linked) Slit-lamp examination of parents and siblings History of exposures (treatments, trauma) General health, growth, and developmental history 2. Pediatric Physical Examination Consider consultation with geneticist or dysmorphologist 3. Hypocalcemia13,14 and hypoglycemia15 of infancy that is sufficient to cause cataracts are heralded by tetany or seizures in the neonatal period, and without this history, routine testing of serum calcium and blood glucose levels is probably not warranted, though these tests may confirm the diagnosis if the history is questionable. Diabetes is a rare cause of childhood cataracts, and lens opacities are generally not the presenting sign of the disease. Cataracts associated with systemic disease or recognizable syndromes are likely to be evident to an ophthalmologist and a pediatrician working together to arrive at a diagnosis. Additional exams at the early well-child visits should include identification of a bright red reflex, and when there is any concern on the part of the pediatrician, it is the responsibility of the ophthalmologist to examine the child in a reasonably short time. A lamellar cataract with several peripheral spoke opacities can be seen against the fundus reflex as it would be with light from a direct ophthalmoscope. Once identified, the ophthalmologist must determine whether the cataract is visually significant and decide about treatment. Central and posterior opacities that are dense and >3 mm generally cause significant deprivation amblyopia,86 and should be removed early. However, the density of the cataract is as important as the size,87 and good vision may develop with an opacity that is large but has areas of clear lens. Anterior cataracts located in the pupillary space and evident on diffuse external illumination. Retinoscopy is another highly useful technique for assessing the visual significance of a cataract, regardless of its size. Retinoscopy can help the examiner determine when lens irregularities extend beyond the region of visible opacity, and to determine when such irregularities are not present and the annulus of lens surrounding the cataract is healthy and functional. A rule of thumb used by some clinicians is that if it is possible to perform an accurate retinoscopy through the undilated pupil of a patient with a congenital cataract, then it is safe to defer surgery, but that if accurate and consistent retinoscopy is not possible, then surgery is indicated. Evaluation of the cataract with direct ophthalmoscopy and retinoscopy should be employed prior to dilation of the pupil, then repeated after pupillary dilation. The posterior segment should be assessed for abnormalities, and if an adequate view with indirect ophthalmoscopy cannot be obtained, ultrasound examination can provide additional information. Cataracts that are not amblyogenic at birth may progress, so serial examinations should be performed. Assessment of vision is generally possible after the early months of infancy, and fixation behavior that is central, steady, and maintained is a good indication of normal vision. In children with incomplete cataracts, especially bilateral opacities without nystagmus or strabismus, there is no harm in delaying cataract surgery until it can be determined that visual acuity lags significantly behind normal levels for age. Development of myopia or increased axial length with a unilateral cataract may be indicative of the development of deprivational amblyopia. For small but dense central cataracts with a small pupil, dilation with cyclopentolate or atropine may provide a sufficient view around the cataract, though cycloplegia in the presence of high refractive error will require optical correction, including contact lenses in some cases, to assure that the eye is in focus at near (similar to treatment of unilateral aphakia). Part-time patching of the sound eye should be done for patients with a unilateral cataract. These patients should be monitored carefully, and if it is clear that amblyopia is present despite compliance with treatment, cataract surgery should be performed. Amblyopia treatment may be necessary both prior to and after cataract extraction, and treatment of amblyopia may be the major challenge in many cases of pediatric cataracts. The most profound amblyopia in association with pediatric cataracts is the deprivational amblyopia occurring in eyes with unilateral congenital cataracts. Dense congenital cataracts, whether unilateral or bilateral, may produce irreversible amblyopia if surgery is not performed in the early months of life, but partial opacities may not require surgical intervention until years later. While a partial cataract may produce slight blurring of images, lens extraction requires some form of optical correction to establish a clear retinal image, and amblyopia may still result in the setting of uncorrected aphakia or undercorrected pseudophakia. Loss of accommodation after lens extraction must be weighed against visual implications of small lens opacities in young patients. Strabismus is another cause of amblyopia, and is a common feature in children with cataracts. Virtually all patients with visually significant unilateral congenital cataracts have strabismus, and the deviation persists even in patients who have had early cataract surgery and have undergone vigorous efforts to rehabilitate the affected eye. Nystagmus may develop as a sign of irreversible amblyopia when cataracts are detected late, and it has been suggested that early surgery prevents the development of nystagmus. The presence of nystagmus is predictably associated with lower visual acuity measures. Infant with aphakic contact lens on the right eye and occluder contact lens on the left to encourage use of the right eye after cataract surgery. Patching must be instituted as soon as amblyopia is detected, or in the case of dense cataracts, immediately after a clear pupil and optical correction are established. Some patients will develop skin irritation from the patch adhesive, or will remove the patch. The opaqueness of the occluder lens must be sufficient to cause a switch in fixation to the amblyopic eye. In bilateral aphakia with strabismic amblyopia, the contact lens of the preferred eye can be removed for time periods to induce this change in fixation pattern. Since most patients with bilateral aphakia and amblyopia have strabismus, the clinician should look for a switch in fixation preference if removal of an aphakic contact lens is used for amblyopia treatment. Some clinicians suggest patching 50% of waking hours, which corresponds to a smaller amount of time in early infancy, but increasing time as the child is awake a greater proportion of the day. Avoidance of overpatching may also help binocular vision development without negatively affecting visual outcome. Late detection of a cataract may lead to irreversible amblyopia, in which case vision will remain poor despite optical correction and patching treatment, and excessive attempts at amblyopia treatment should not be pursued. The nucleus and cortex of pediatric lenses are relatively soft, and easily aspirated. In the infant eye, creating a continuous curvilinear capsulorrhexis is difficult, and occasionally congenital cataracts contain hard inclusions or fibrous membranes that require cutting. Thus, the vitrectomy handpiece is an ideal instrument for cutting a circular opening in the anterior capsule, aspirating the lens, cutting and aspirating any fibrous or hard lens material, cutting the posterior capsule, and performing anterior vitrectomy. A posterior capsulotomy with anterior vitrectomy should always be performed in infants since the posterior capsule of infants will become opacified in short time. For older children, cataract surgery may be performed either via a clear corneal incision or scleral tunnel. Most children under 5 years old should have a primary posterior capsulotomy and anterior vitrectomy due to the high rate of posterior capsule opacification in this age group. The contact lens may be placed as soon as the incision has healed well enough to allow placement, generally about one week after surgery. Rigid gas permeable lenses are also used, especially for eyes with microphthalmia or steep corneas. These lenses come with a wider power/base curve range, but are approved only for daily wear. The average contact lens correction for a 1 month old infant is +30 D, and the residual hyperopia of the aphakic eye decreases at a fairly predictable rate as the eye grows. Unilateral cataracts should ideally be removed prior to 2 months of age if useful vision is to be obtained. Because of the difficulties associated with amblyopia treatment and compliance in the presence of a sound, normal eye, few patients achieve acuity of 20/40 or better, even with early surgery. A disadvantage is the daily requirement of parents to insert, remove, and/or maintain the contact lens. Aphakic spectacles are a reasonable alternative to contact lenses, especially for infants or young children who have undergone bilateral surgery and cannot successfully wear contact lenses. Bifocal segments can be incorporated into aphakic spectacles at around age 3 years, and bifocal spectacles can be given to patients with contact lenses for improved distance and near focus. Spectacles introduce asymmetric image magnification, which is a disadvantage if binocular vision is present. Most children who have had a unilateral cataract, however, lack binocular vision, so that spectacles may still be a reasonable choice in cases of contact lens noncompliance.
Buy generic cardura online
Histologic examination demonstrates a severe loss of photoreceptors and outer nuclear layer cells hypertension lungs discount cardura uk, with gliosis of the inner retinal layers as well as diffuse pigment epithelial disorganization, pigment migration into the retina, and atrophy of the choriocapillaris. The disease was originally reported separately by Senior124 and Loken125 and their associates in 1961. Affected children are blind from birth, have flat electroretinograms, and develop retinitis pigmentosa. Definitive diagnosis is made by histologic examination of a renal biopsy specimen. Prenatal diagnosis can be performed by genetic testing when a specific mutation has already been identified in an affected sibling. Patients with the juvenile type often die within the first decade; patients with the adult type progress to end-stage renal disease in the third to fourth decade. Treatment is supportive and aimed at managing the renal disease and its complications. Dialysis and renal transplantation have been used successfully to treat the renal failure. The primary injury is to the renal tubular epithelium and results in a diminished ability to concentrate urine. Patients develop complications associated with progressive renal failure, including renal osteodystrophy, anemia, growth retardation, hypertension, and progressive uremia. Histologically, mild tubular atrophy and dilatation are present early in the disease. As the disease progresses, renal tubules become more atrophic and dilated, with irregular focal thickening of the tubular basement membrane and interstitial fibrosis. Electron microscopy has demonstrated areas of thickened, lamellated, and duplicated tubular basement membrane, as well as regions where it is thinned or absent. Diagnostic Criteria for Fraser Syndrome Major criteria Cryptophthalmos Syndactyly Kidney Systemic Sibling with Fraser syndrome Minor criteria Congenital malformation of nose Congenital malformation of ears Congenital malformation of larynx between the eyelids and anterior segment. Cryptophthalmos can be seen as an isolated condition, but most cases are part of a syndrome with multiple other malformations. The most consistent features are cryptophthalmos, syndactyly, malformations of the larynx, ear, nose and genitourinary tract, craniofacial dysmorphism, mental retardation, and musculoskeletal anomalies. Cryptophthalmos seems to be inherited in an autosomal recessive manner, but the genetics and pathophysiology have not been clearly described. Patients with bilateral renal hypoplasia do poorly, as a result of oligohydramnios and pulmonary hypoplasia. Some attempts have been made to separate the lids from the globe; however, because of the severe anterior segment malformation, this has been unsuccessful in both the complete and incomplete forms. Their explanation for the contradiction between oligohydramnios and voluminous hyperechogenic lungs in the presence of renal agenesis was: overdistended lungs, and the occurrence of nonimmune hydrops fetalis secondary to laryngeal stenosis. Renal Manifestations Renal hypoplasia or even aplasia is a relatively common feature of cryptophthalmos syndrome. Unilateral or bilateral renal hypoplasia occurs in 37% of patients with cryptophthalmos syndrome. Bilateral renal hypoplasia results in oligohydramnios, pulmonary hypoplasia, and early death. In addition to renal malformations, there are often associated genitourinary malformations. Cryptophthalmos is complete when eyelids are totally absent, replaced by skin covering the globe. Cryptophthalmos is incomplete when the eyelids are partially formed and there is a small conjuctival sac, but most of the globe is covered by skin. Clinical features include microcephaly, progressive deterioration of the central nervous system and growth retardation. A prevalent feature of Cockayne syndrome is photosensitivity to ultraviolet light and pigmentary retinal degeneration. Premature aging is the cardinal feature of both types; however, within the first years of life, growth, and development become abnormal. The term cachectic dwarfism is often used to describe the general appearance of these patients. The characteristic physical appearance of cachectic dwarfism with thinning of the skin and hair, sunken eyes, and a stooped standing posture illustrates the aging process. Pathologic studies reveal diffuse and extensive demyelination in the central and peripheral nervous systems. Patients demonstrate pericapillary calcifications in the cortex and basal ganglia at an early age; severe neuronal loss in the cerebral cortex and cerebellum also occurs. Normal gait is impaired by cerebellar ataxia as well as kyphosis and flexion deformities of the hip, knee, and ankles. Histologically, there is a loss of photoreceptors, ganglion cells, and outer nuclear layer cells. Lipofuscin is deposited in the retinal pigment epithelium, and there are pigment-laden cells in the subretinal space. Cataract within the first 3 years of life is predictive of severe disease, with a poor prognosis and early death. The diagnosis can be confirmed by demonstrating an abnormal sensitivity of cultured fibroblasts to ultraviolet light. Ophthalmoscopic findings contribute to the diagnosis and may be predictive of severe disease. Williams R, et al: Epidemiology of diabetic retinopathy and macular oedema: a systematic review. Identification and characterization of the tuberous sclerosis gene on chromosome 16. Bonetta L, et al: Wilms tumor locus on 11p13 defined by multiple CpG island-associated transcripts. Gessler M, et al: Homozygous deletion in Wilms tumours of a zinc-finger gene identified by chromosome jumping. Gronskov K, et al: Population-based risk estimates of Wilms tumor in sporadic aniridia. Sohar E: A heredo-familial syndrome characterized by renal disease, inner ear deafness, and ocular changes. Prognosis for vision is poor because of the retinal degeneration, but cataract extraction may be appropriate in cases in which cataract appears to be symptomatically limiting vision. Colville D, Savige J: Albipunctatus retinopathy in inherited interstitial nephritis. Spada M, et al: High incidence of later-onset fabry disease revealed by newborn screening. Mastropasqua L, et al: Corneal and conjunctival manifestations in Fabry disease: in vivo confocal microscopy study. The Cystinosis Collaborative Research Group: Linkage of the gene for cystinosis to markers on the short arm of chromosome 17. Town M, et al: A novel gene encoding an integral membrane protein is mutated in nephropathic cystinosis. Tsilou E, et al: Ophthalmic manifestations and histopathology of infantile nephropathic cystinosis: report of a case and review of the literature. Knoll T, et al: the influence of oxalate on renal epithelial and interstitial cells.
Purchase cardura 2mg
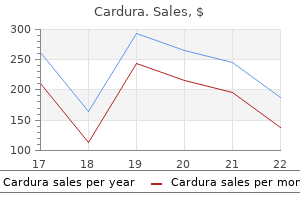
Fundus photographs of the left eye showing disk edema heart attack jeff x ben generic 2 mg cardura, dilated veins, cotton-wool spots, and retinal hemorrhages. Retinopathy was unresponsive to panretinal photocoagulation, and the patient eventually required bilateral vitrectomies during her pregnancy. Pregnancy may cause remission of some forms of chronic noninfectious uveitis, with postpartum flare-ups. Toxoplasmosis transmission to the fetus occurs in primary infection during pregnancy. Pregnancy may reactivate latent toxoplasmosis, but there is little risk to the fetus in reactivated disease. Though pregnancy may stimulate growth of pituitary adenomas, successful pregnancies can occur in patients with pituitary tumors. There was some regression in 57% of those developing nonproliferative diabetic retinopathy. In a study152 of 38 patients without diabetic retinopathy at conception, 10 patients (26%) had mild progression of disease and none progressed to proliferative disease. Increasing background change occurred in 47% and proliferative change developed in 5%. Changes in background disease seemed to follow a waxing and waning 4592 Pregnancy and the Eye course with improvement in the third trimester and postpartum period. Studies of preproliferative disease have concentrated on the presence of soft exudates and cotton-wool spots. In patients with background diabetic retinopathy, the development of new soft exudates during pregnancy was reported to range from 41 to 47. Some degree of regression occurred in 78% of patients post partum, with 33% experiencing total regression. Nevertheless, for patients with only minimal diabetic retinopathy, there appears to be no increased risk to the fetus. Proliferative Diabetic Retinopathy A review of 12 studies involving a total of 122 patients with proliferative diabetic retinopathy at the onset of pregnancy showed that progression of disease occurred in 46%. If proliferative disease totally regressed either spontaneously or with laser treatment before pregnancy, no recurrence developed during pregnancy. Given the risk of progressive disease in pregnancy, some ophthalmologists treat patients approaching high-risk characteristics. Transplacental transmission to the fetus is thought to occur during primary maternal infection. The overall risk of fetal infection from a primary maternal infection appears to be low. In a study of 360 pregnancies in which maternal toxoplasmosis was acquired in the first 8 weeks of gestation, 90% of live born offspring were free of infection. Of the seven infected children, only two manifested peripheral chorioretinal scarring and both children had inactive disease at 70 months. In one study176 of four pregnancy-associated ocular toxoplasmosis recurrences in 18 pregnancies among 10 patients with preexisting toxoplasmosis retinochoroiditis, it was concluded that the most important factor in advising pregnant patients is whether the antibody titer is increasing during pregnancy, rather than the clinical picture or the absolute value of the antibody titer. In another study of 35 pregnancies, reactivation of latent ocular toxoplasmosis occurred in seven pregnancies. Thus, while it might be advisable to measure antibody levels once per trimester, the overall risk of vertical toxoplasmosis transmission to live-born children, in either primary or recurrent maternal infection, appears to be low. Macular Edema Macular edema may develop during pregnancy, although its exact incidence is not known. One study163 found macular edema to be associated with significant proteinuria and mild hypertension. Furthermore, there were significant macular capillary nonperfusion and worsening of the edema as the pregnancy progressed. Although more studies are needed, it may be reasonable to follow patients with macular edema without treatment in certain cases, given the possibility of postpartum recovery. Gestational Diabetes Although previous studies reported no apparent risk of diabetic retinopathy developing in patients with gestational diabetes,165 a case report described a pregnant woman with gestational diabetes who developed severe bilateral proliferative diabetic retinopathy. Several studies have sought to determine whether the severity of diabetic retinopathy correlates with perinatal outcome. In one study,167 retinal hemorrhages and neovascularization were associated with increased infant morbidity. Abnormalities include anterior and posterior uveitis, serous retinal detachment, optic disk edema, cerebrospinal fluid pleocytosis, vitiligo, alopecia, poliosis, tinnitus, vertigo, and deafness. Recurrence is common, and although the disease is responsive to corticosteroids, visual prognosis is poor. In this series, flare-ups occurred in almost 80% of cases within the first 4 months. Similar results were found even after adjusting for flares potentially explainable by early tapering of uveitic medications. The 5-year survival rate of these 16 pregnant women was similar to that reported for nonpregnant women with uveal melanomas. In another series, a greater than expected number of women with malignant uveal melanomas presented during pregnancy, suggesting a hormonal influence on the growth of these tumors. The authors postulated that other hormones or immunologic mechanisms occurring during gestation might play a role. Egan and colleagues189 examined the rate of metastasis from intraocular melanomas and found no increased risk in pregnancy or in patients taking oral contraceptives. In fact, childbearing may be associated with improved survival in choroidal melanoma. In a series of 1818 men and women with choroidal melanoma, overall multivariate-adjusted death rates were 25% higher in nulliparous women and men vs parious women. It has been postulated that the improvement in the disease during pregnancy is due to increased levels of circulating corticosteroids. Induced pregnancies are typically limited to patients without demonstrable pituitary tumors. Nevertheless, small unrecognized tumors may be present and enlarge in patients who become pregnant. Acute neurologic symptoms such as headache, nausea, vomiting, visual disturbances, bitemporal visual-field defects, decreased visual acuity, and occasionally diplopia may develop. Although pregnancy is known to result in pituitary enlargement and appears to stimulate growth of pituitary adenomas, successful pregnancies can occur in patients with pituitary tumors. In one review of pregnancies in patients with previously untreated pituitary tumors, 60% remained asymptomatic, 70% required no radiation or surgical intervention during pregnancy, and 96% had no permanent sequelae of any kind. Progression of signs and symptoms is much more rapid in pregnant, patients, but final outcome does not appear to be different from that of nonpregnant patients. In addition, both radiation and surgical treatments are effective during pregnancy, and although there is an increased rate of prematurity with therapy, there is no increased rate of perinatal mortality. This treatment has been shown to induce regression of prolactinomas that had expanded during pregnancy. If none is detected and the patient desires to conceive, induction of ovulation should be attempted only after the patient understands the risks involved. The patient should be informed of the possibility of harboring an undetectable pituitary tumor that may enlarge during pregnancy, causing various neurologic symptoms and potentially requiring medical AnkylosIng Spondylitis Pregnancy has a variable effect on the course of ankylosing spondylitis. In a study of 87 pregnancies in 50 patients, remission occurred in 21%, exacerbation in 24%, and no change in 55%. Postpartum ante1ior uveitis was seen fairly frequently, arising in 20% of patients. In a study of 76 pregnancies in 51 patients reported by Ostensen et al, the patients with quiescent disease before conception did not experience exacerbations during pregnancy and patients with active inflammation experienced improvement or complete remission in the second half of gestation. Four patients with ongoing uveitis had no change in the severity of their ocular inflammation during pregnancy. Ten patients were treated with enucleation, and the histology of these specimens did not differ significantly in cell type, mitotic activity, or other features 4594 Pregnancy and the Eye or surgical treatment. In pregnant patients with known prolactinomas, monthly measurements of prolactin levels, visualfield examinations, visual acuity tests, and ophthalmoscopic examination of the optic nerve are recommended.