Purchase viagra vigour us
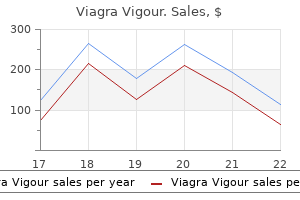
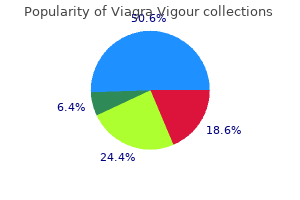
Further erectile dysfunction effects on relationship purchase cheap viagra vigour line, long-term risk factor management involves smoking cessation, hypertension control, and considerations for statin therapy. If there is gross contamination of the abdominal cavity and an autogenous conduit is not available, endarterectomy allows for revascularization without the use of a conduit. New York: respond well to endovascular methods but can be well treated with endarterectomy. Lastly, when disease of both the supraceliac aorta and infrarenal aorta prevents using these two segments for inflow and surgical bypass, endarterectomy is an excellent tool. Right-angled aortic clamps are helpful in optimizing the utilization of exposed space. In these cases, plaque should be everted and divided well into the vessel and the aortic endarterectomy closed. Endovascular therapy formerly was reserved for chronically debilitated patients who were unable to tolerate general anesthesia and open revascularization. Chronic mesenteric venous thrombosis: evaluation and determinants of survival during long-term follow-up. Usefulness of computed tomography in differentiating transmural infarction from nontransmural ischemia of the small intestine in patients with acute mesenteric venous thrombosis. Endovascular thrombolysis in acute mesenteric vein thrombosis: a 3-year follow-up with the rate of short and long-term sequaelae in 32 patients. Multidisciplinary stepwise management strategy for acute superior mesenteric venous thrombosis: an intestinal stroke center experience. Transcatheter thrombolytic therapy for acute mesenteric and portal vein thrombosis. Open and endovascular revascularization for chronic mesenteric ischemia: risk stratification outcomes. Durability of antegrade synthetic aortomesenteric bypass for chronic mesenteric ischemia. Endovascular treatment of stenotic and occluded visceral arteries for chronic mesenteric ischemia. Clinical outcomes of mesenteric artery stenting versus surgical revascularization in chronic mesenteric ischemia. Intraoperative duplex ultrasound of visceral revascularizations: optimizing technical success and outcome. Antegrade visceral revascularization via a throracoabdominal approach for chronic mesenteric ischemia. Comparison of superficial femoral and saphenous vein as conduits for mesenteric arterial bypass. Though less physiologically upsetting for the patient, revascularization by endovascular means may be made more challenging by severe calcifications, occlusions, long lesions, small vessel diameter, and multiple tandem lesions. While most of these interventions are performed using a femoral approach, a left brachial approach may be required in some patients. If a larger than 6-french sheath is needed, an open exposure of the brachial or axillary arteries is another option. If the lesions are amenable to endovascular treatment, heparin is administered and the lesion is crossed using a series of preshaped catheters and hydrophilic wires. After crossing the lesion with the wire, the catheter should be advanced past the lesion and luminal position confirmed. Stiffer wires can be substituted at this point for better tracking of a balloon or stent. Because of the high restenosis rate, routine duplex surveillance is recommended particularly in the first year. However, duplex evidence of restenosis may or may not correlate with symptom development, and the clinical symptomatology should guide further decisions about surveillance and therapy. Mesenteric ischemia: pathogenesis and challenging diagnostic and therapeutic modalities. Operative relief of gangrene of the intestine due to occlusion of the mesenteric vessels. Revascularization of acute mesenteric ischemia after creation of a dedicated multidisciplinary center. Systematic review of survival after acute mesenteric ischaemia according to disease aetiology. The diagnosis of acute mesenteric ischemia: a systematic review and meta-analysis. Debate: whether an endovascular-first strategy is the optimal approach for treating acute mesenteric ischemia. Current results of open revascularization for chronic mesenteric ischemia: a standard for comparison. Perioperative and late clinical outcomes of percutaneous transluminal stentings of the celiac and superior mesenteric arteries over the past decade. Stenting of stenotic mesenteric arteries for symptomatic chronic mesenteric ischemia. Comparison of covered stents versus bare metal stents for treatment of chronic atherosclerotic mesenteric arterial disease. Open surgical treatment for chronic mesenteric ischemia in the endovascular era: when is it necessary and what is the preferred technique Endovascular repair of chronic mesenteric occlusive disease: the role of duplex surveillance. Type 1, or graft-enteric fistula, occurs as the result of an erosion of the proximal aortic suture, with or without the presence of a pseudoaneurysm, into the adjacent bowel. Failure to close the aneurysm sac and retroperitoneum will also leave the suture line in direct contact with the duodenum, increasing the odds of erosion of the suture line into the bowel. Foreign-body ingestion, carcinoma, or infections such as diverticulitis can lead to adhesions that bring the bowel in closer proximity to the aorta. The mechanical pulsations cause thinning of the bowel wall with eventual translocation of enteric organisms into the suture line. The higher likelihood of a fistula forming between the aorta and duodenum is attributed to their proximity to one another, as the duodenum directly overlies the aorta within the retroperitoneum. The diagnosis is often delayed because of the rarity of the disease and the wide differential that accompanies the initial mild symptoms. Patients with this diagnosis have a grim prognosis, and surgery is the only truly definitive management option. However, this triad is found in only 11% of patients6 and thus is not a useful diagnostic marker. Intermittent herald bleeds in the form of hematochezia, melena, or hematemesis are common occurrences, being present in 94% of cases. Laboratory Studies Laboratory studies may demonstrate abnormalities, such as an increased white blood cell count and decreased hematocrit. In the presence of fever, aerobic and anaerobic blood cultures should be obtained. Advanced sepsis confirmed by positive preoperative blood cultures is a predictor of poor outcome. The most common organisms isolated from the fistula site include Staphylococcus aureus (including methicillin-resistant S. A hemodynamically unstable patient should undergo resuscitation while being prepped for an emergency exploratory laparotomy. Indeed, the exploratory laparotomy is the gold standard, with 100% sensitivity and specificity. If the patient is stable, further diagnostic tests should be obtained without delay. Periaortic gas, fluid, and soft tissue edema also may be observed with graft infections and are normal findings immediately after the operation. Computed tomography scan reveals aortoenteric fistula between the aortic graft and the third portion of the duodenum. Increased signal intensity in T1- and T2-weighted images indicates localized inflammation, and perigraft fluid seen after the initial postoperative period may signal a graft infection. In patients who do not have overt signs of graft infection, radiolabeled white blood cell scans show promising results, with 100% sensitivity and 94% specificity.
Generic viagra vigour 800 mg
Treatment of external gastrointestinal fistulas by a combination of total parenteral nutrition and somatostatin treatment of erectile dysfunction using platelet-rich plasma buy viagra vigour visa. Autologous platelet rich fibrin glue for sealing of low-output enterocutaneous fistulas: an observational cohort study. A multivariate model to determine prognostic factors in gastrointestinal fistulas. Decision for surgical management of perforation following endoscopic sphincterotomy. A randomized study comparing laparoscopic versus open repair of perforated peptic ulcer using suture or sutureless technique. Metabolic and nutritional support of the enterocutaneous fistula patient: a three-phase approach. Duodenal stump fistula after gastrectomy for gastric cancer: risk factors, prevention, and management. Endoscopic modalities for upper gastrointestinal leaks, fistulae and perforations. A retrospective, observational study of enteral nutrition in patients with enteroatmospheric fistulas. Classification, prevention and management of entero-atmospheric fistula: a state-of-the-art review. Gastrointestinal fistulas in acute pancreatitis with infected pancreatic or peripancreatic necrosis: a 4-year single-center experience. Gastrointestinal fistula associated with large abdominal wall defects: experience with 43 patients. Systematic literature review on the use of vacuum assisted closure for enterocutaneous fistula. The importance of early diagnosis and treatment of patients with aortoenteric fistulas presenting with herald bleeds. The effect of omentoplasty on the rate of anastomotic leakage after intestinal resection: a randomized controlled trial. Despite these relatively low statistics, it is nevertheless important for the general surgeon to have a firm understanding of small bowel diverticular disease when considering the broad differential diagnoses of abdominal pain and gastrointestinal bleeding. This article discusses each type of diverticulum as it relates to its epidemiology, pathogenesis, clinical presentation, diagnosis, and management. In general, Meckel diverticula are congenital and not associated with other types of diverticula. Most duodenal and jejunoileal diverticula are acquired, with the exception of intraluminal duodenal diverticula. Duodenal and jejunoileal diverticula are false, or pseudodiverticula, and most result from pulsion due to increased intraluminal pressure and intestinal dysmotility. If the apex of the diverticulum does not have an opening and remains closed, neonatal duodenal obstruction will occur. An extraluminal diverticulum, like those most commonly seen in the colon, is acquired. It is a false diverticulum that contains only the mucosa and submucosa that herniated between the muscle at sites of weakness in the bowel wall. These areas of weakness are usually where the blood supply to the bowel creates small structural defects, allowing the mucosa and submucosa to herniate outward. The most commonly reported symptoms are postprandial epigastric pain, bloating, nausea, vomiting, and gastrointestinal bleeding. Because most of these symptoms can be caused by other more common gastrointestinal problems, the diagnosis is often delayed or missed. The incidence of obstruction from an intraluminal diverticulum is much more common given its anatomic location within the lumen of the duodenum. There have even been case reports of duodenal diverticula causing obstruction of the ampulla of Vater that resulted in biliary obstruction and pancreatitis. Extraluminal duodenal diverticula are much more common, second in incidence only to large bowel diverticula. Unlike intraluminal diverticula that develop in utero, the extraluminal type usually develop in the fifth decade of life or later. Radiographic means of diagnosis are less invasive and are considered more appropriate initial methods of evaluation. The classic "wind-sock" sign describes the saclike projection of an intraluminal duodenal diverticulum outlined by oral contrast within the duodenum. Extraluminal duodenal diverticula can be similar in appearance to those seen in the colon as an outpouching. Three types of small bowel diverticula warrant particular consideration: duodenal diverticula, jejunoileal diverticula, and Meckel diverticula. The most frequently encountered diverticula are duodenal (45%), compared to jejunoileal (25%) and Meckel diverticula (25%), and jejunoileal diverticula are most often symptomatic. This article discusses each type of diverticula and its epidemiology, pathogenesis, clinical presentation, diagnosis, and management. The morbidity and mortality are higher for diverticula in close proximity to the ampulla. Once the diverticulum is resected, the duodenum should be closed in two layers transversely to avoid stricture and can be buttressed with an omental or jejunal patch. Biliary and enteric diversions have been described if the diverticulum is very close to or involves the ampulla. Even more invasive means such as pancreaticoduodenectomy have been reported with a relatively low risk of complications, but there is not adequate data at this time to justify its use in all cases. In the setting of perforation where diverticulectomy cannot be safely performed or if the patient is not a surgical candidate, wide drainage and antibiotics can sometimes serve as definitive management. It is estimated that 60% to 70% of patients with jejunoileal diverticula are asymptomatic. Of those patients who develop chronic symptoms or acute complications, only 10% will require surgery. They are considered to be acquired rather than congenital, and while the exact pathogenesis is unknown, it is thought to be a result of smooth muscle dysfunction or a defect in the myenteric plexus. Similar to extraluminal duodenal diverticula, this results in irregular bowel contractions, increased intraluminal pressure, and subsequent pulsion of the mucosa and submucosa at weakened areas where the vasa recta enter the small intestine. Diverticulitis is the most common presentation, accounting for up to 55% of complications. Clinically, patients have localized or diffuse abdominal pain, fever, and leukocytosis. Imaging may reveal an inflammatory mass, abscess, fat stranding, or air within the mesentery. The presentation and imaging may be suspicious for perforated colonic diverticulitis or appendicitis depending on the location of the abscess. The mortality rate for perforated diverticulitis can reach 50% due to the difficulty, and subsequent delay, in diagnosis. Bleeding results from inflammation of a diverticulum near a mesenteric vessel that erodes into the vessel. These patients often present with painless bright red blood per rectum, although they may also present with melena or hematemesis. Due to the location of the diverticula, endoscopic intervention is unsuccessful at controlling the hemorrhage. Colonoscopy and upper endoscopy can be helpful to rule out proximal and distal sources of gastrointestinal hemorrhage. If bleeding has not been identified on endoscopy, a radiolabeled red blood cell scan or angiography may be performed to better delineate the location of bleeding. Surgical management of pancreaticobiliary disease associated with juxtapapillary duodenal diverticula: case series and review of the literature. Strictures and adhesions from prior diverticulitis, an inflammatory mass causing extrinsic compression of the bowel, volvulus of a segment with large diverticula, and pseudoobstruction due to function dysmotility can all lead to symptoms of abdominal distention, nausea, and vomiting. The enterolith can obstruct the bowel lumen when it is dislodged from the diverticulum. If surgical intervention is indicated due to a complete obstruction, the enterolith may be milked into the distal bowel and removed through an enterotomy in a healthy segment of bowel. Alternatively, it can be resected along with the diverticular disease, especially in the setting of associated inflammation. An upper gastrointestinal series with small bowel follow-through and enteroclysis can be both diagnostic and therapeutic.
Diseases
- Tuberculous meningitis
- Primary agammaglobulinemia
- Jejunal atresia
- Myopathy congenital multicore with external ophthalmoplegia
- Cataract congenital dominant non nuclear
- Hydrocephalus craniosynostosis bifid nose
- Granulocytopenia
- Tricho onycho hypohidrotic dysplasia
- Guizar Vasquez Luengas syndrome
- Cholecystitis
Cheap viagra vigour 800 mg visa
These recommendations do not apply to patients who are very elderly (>80 years old) 5 htp impotence discount viagra vigour online american express, frail, or with poor left ventricular function. In fact, the explosion of new agents has opened up a daunting number of possibilities for future research,49 which will take some time to come into focus. Although a comprehensive discussion is beyond the scope of this chapter, the following will provide a current overview for the reader, who is also referred to a number of current reviews on these topics. Cyclophosphamide and fludarabine are also administered as conditioning chemotherapy. Despite this, nine patients remained in ongoing remission at last follow-up, with the longest remission at 23 months from therapy. The conditioning regimen varied depending on the histologic subtype and past treatment history. Management of primary gastrointestinal non-Hodgkin lymphomas: a population-based survival analysis. Enteropathy-type T-cell lymphoma: clinical features and treatment of 31 patients in a single institution. Survival in refractory celiac disease and enteropathy-associated T-cell lymphoma: retrospective evaluation of single-centre experience. Enteropathy-associated T-cell lymphoma: clinical and histological findings from the international peripheral T-cell lymphoma project. Targeting B cell receptor signaling with ibrutinib in diffuse large B cell lymphoma. Idelalisib, a selective inhibitor of phosphatidylinositol 3-kinase-delta, as therapy for previously treated indolent non-Hodgkin lymphoma. Primary gastrointestinal lymphoma: spectrum of imaging findings with pathologic correlation. A revised European-American classification of lymphoid neoplasms: a proposal from the International Lymphoma Study Group. Primary gastrointestinal lymphoma in Japan: a clinicopathologic analysis of 455 patients with special reference to its time trends. Lymphoma/leukemia molecular profiling project: the use of molecular profiling to predict survival after chemotherapy for diffuse large-B-cell lymphoma. Bcl-6 protein expression, and not the germinal centre immunophenotype, predicts favourable prognosis in a series of primary nodal diffuse large B-cell lymphomas: a single centre experience. Survival prediction of diffuse large-B-cell lymphoma based on both clinical and gene expression information. Chromosomal translocation t(11;18)(q21;q21) in gastrointestinal mucosa associated lymphoid tissue lymphoma. Report on a workshop convened to discuss the pathologic and staging classification of gastrointestinal tract lymphoma. The role of surgery in primary gastric lymphoma: results of a controlled clinical trial. Survival of patients with marginal zone lymphoma: analysis of the survival, epidemiology, and end-results database. Congenital lesions, such as rotational anomalies, duodenal or jejunoileal atresia, meconium ileus, omphalomesenteric remnants, and duplication cysts, are more likely to present in infancy, if not prenatally. Although 90% of cases manifest during the first year of life (with 50% to 75% presenting within the first month of life),1 patients may present with midgut volvulus and/or obstruction at any age, making an understanding of the embryology, diagnosis, and treatment of malrotation essential for all abdominal surgeons. At week 10, the midgut returns to the abdomen, rotating another 180 degrees counterclockwise. The right and left colons are anchored to the posterior abdominal wall by mesenteric attachments. In addition, Ladd bands extending from the right paracolic region to the malpositioned cecum may obstruct the duodenum. Congenital diaphragmatic hernias and abdominal wall defects (omphaloceles and gastroschisis) interfere with or abrogate normal rotation before the 10th week of gestation; as such, infants with these conditions are malrotated by definition. Forty to 60% of neonatal bilious emesis is attributable to surgical bowel obstructions, of which malrotation is the most common cause. However, it should be noted that volvulized patients may never develop abdominal distention because the point of obstruction may be as proximal as the ligament of Treitz. Malrotation without volvulus may manifest as chronic abdominal pain and/or failure to thrive. It may also be completely asymptomatic and found incidentally during work-up for an unrelated condition. Early diagnosis of malrotation with volvulus is paramount to prevent potentially life-threatening bowel ischemia. Children with suspected midgut volvulus who show signs of bowel ischemia should undergo emergent surgical exploration without radiologic evaluation. There are no plain film findings that are pathognomonic for malrotation with volvulus; x-rays may demonstrate a gasless abdomen, a high-grade bowel obstruction, or an essentially normal bowel gas pattern. However, caution is warranted because false-positive rates of up to 21% are reported with ultrasonographic diagnoses. Acquired pediatric small intestinal diseases include necrotizing enterocolitis and intussusception. This anomaly is the most frequent type of malrotation, and the risk for midgut volvulus is ever present. This abnormality may be manifested clinically as duodenal obstruction secondary to abnormal mesenteric (Ladd) bands from the colon across the anterior duodenum. This abnormality may be manifested clinically as obstruction of the transverse colon. Contrast enema is rarely used in the work-up for malrotation because the presence of a normally located cecum in the right lower quadrant does not exclude duodenojejunal malrotation and infants often have mobile cecum that may result in false-positive results. If ischemic bowel is encountered, its viability should be assessed after a period of observation. Small areas of frankly necrotic bowel should be resected with or without primary anastomosis. Bowel with marginal viability should be left and allowed to declare itself; a second-look procedure should be performed 24 to 36 hours later. If an operation is electively pursued, it may be approached laparoscopically; the steps of the operation are the same. Long-term complications include adhesive small bowel obstruction (10%), recurrent volvulus, and, if significant bowel loss has been sustained, short gut syndrome. It arises from a recanalization error; the gut tube fails to obliterate its lumen in the sixth week of gestation. Eighty-five percent of duodenal atresias are located at the junction of the first and second portions of the duodenum. Commonly, the distal common bile duct traverses the medial septum, to which the ampulla is proximal. Type I duodenal atresias may be incompletely obstructing and therefore remain undetected until solid foods are introduced. In 1936 William Ladd described the surgical procedure for correction of malrotation and midgut volvulus that continues to be used currently. Coils of intestine or ascending colon are wrapped around the root of an incompletely anchored mesentery. The descending duodenum is dilated because of extrinsic pressure from Ladd bands or peritoneal folds that cross it. The small intestines lie on the right side of the abdomen, and the cecum and ascending colon are in the midline or left side of the abdomen. A nasogastric tube has been passed into the jejunum to exclude intrinsic obstruction. Alternatively, duodenojejunostomy or gastrojejunostomy may be performed, although the latter carries the risks of marginal ulceration and blind loop syndrome. A work-up should be undertaken to look for associated anomalies: 28% have Down syndrome, 23% annular pancreas, 23% congenital heart disease, and 20% malrotation. Thin webs may be excised through a longitudinal duodenotomy that is started near the point of obstruction, carried proximally over the web, and later closed transversely. The postnatal presentation is usually that of an infant who develops bilious emesis and progressive abdominal distention. The frequency of the emesis and the degree of distention vary in relation to the location of the atresia; infants with proximal atresias will vomit frequently and display minimal distention, whereas those with distal atresias will exhibit more distention but lateronset emesis. Ten percent of patients present with meconium peritonitis from in utero bowel perforation.
Order viagra vigour now
As the atherosclerotic burden of the mesenteric vessels becomes more pronounced erectile dysfunction treatment pakistan generic viagra vigour 800mg without a prescription, the severity and frequency of symptoms increase. The duration and severity of the pain response depend on the size of the meal as well as the food composition. Foods that are thought to precipitate symptoms are avoided, and unintentional weight loss can result. Without these three elements of the symptom complex, other disease processes should be considered. Other gastrointestinal symptoms including bloating, nausea, vomiting, and diarrhea can accompany the hallmark signs. Many have an extensive smoking history and other risk factors for atherosclerotic disease. Signs of peripheral vascular disease including diminished or absent pulses and scars from prior vascular surgery may be seen. Most patients referred to vascular surgeons have undergone a thorough work-up for gastrointestinal complaints. Radiologic and endoscopic studies are frequently used to evaluate for malignancy during this process. Not uncommonly, lack of symptom improvement following ulcer treatment or cholecystectomy leads the clinicians to investigate less common sources of abdominal pain. In the unfed, unstressed state, the circulatory demands of the resting bowel are easily met and there is no pain. These symptoms develop when fixed mesenteric vascular obstructions limit blood flow to the intestine during the increased metabolic demands of the postprandial state. Flow differences in the resting and postprandial state are significant and necessary for digestion to occur. Blood flow increases two to three times following the consumption of a meal and is necessary for effective digestion. Typical maximal circulatory increases occur within 1 hour following food consumption. The extensive collateral circulation among the mesenteric vessels is usually able to compensate for stenosis in one or two mesenteric arteries. Provided there are no acute-on-chronic events, chronic, progressive vessel stenosis with chronic occlusion of a mesenteric artery is frequently a clinically silent event. Experience of the noninvasive laboratory is extremely important to the routine use of this modality. Alternatively the Dartmouth criteria use end-diastolic velocity to determine the degree of stenosis. Although this study does require both radiation exposure and contrast load, it gives accurate information regarding mesenteric vessel stenosis as well as information regarding perfusion to solid organs and the condition of the bowel. This noninvasive modality has surpassed angiography as the diagnostic modality of choice. Angiography has historically been considered the gold standard for the evaluation of mesenteric occlusive disease. Disadvantages of this imaging modality include not only its invasive nature but also the resources necessary (angiography suite or operating room) to perform the test. Risks of angiography include arterial trauma, dissection, or pseudoaneurysm formation. Prophylactic intervention is seldom performed, as there is minimal risk of ischemia in asymptomatic patients. Over the past two decades, percutaneous and hybrid procedures have provided a less invasive alternative to open therapies. Open Surgery Open surgical techniques for mesenteric revascularization include antegrade or retrograde aorto-mesenteric and/ or celiac bypass grafting, endarterectomy, and mesenteric reimplantation. For patients deemed to be candidates for open surgery, the choice of procedure depends primarily on the presenting anatomy, as indicated by the preoperative imaging and intraoperative findings. Heavily diseased and calcific arterial segments are technically difficult to work with and are typically avoided. The abdomen should be expeditiously explored on entry and the viability of the bowel assessed. Subsequently, the supraceliac aorta should be exposed by division of the left triangular ligament of the liver and retraction of the left lateral lobe. The aorta is then exposed by incising the median arcuate ligament and separating the diaphragmatic crura. During this process, phrenic arteries may be encountered, and these should be ligated. The celiac axis is then exposed by dissecting caudally along the anterior surface of the aorta. Extreme care must be taken, as this tunnel is adjacent to the splenic and portal veins. A Penrose drain or straight aortic clamp can be left in place to assist passage of the bypass limb. If extensive retroperitoneal fibrosis is encountered and tunneling is considered hazardous, a more ventral tunnel over the pancreas through the transverse colon mesentery is acceptable. The proximal anastomosis is performed with clamps, allowing for partial occlusion. If a single artery is to be bypassed, saphenous vein or a 6- to 8-mm prosthetic graft is used. The grafts are tunneled and the distal anastomoses are completed in either end-to-end or end-to-side fashion. Graft patency and technical adequacy can then be assessed by handheld Doppler or intraoperative duplex ultrasound analysis. Most importantly, clamp placement is below the renal arteries and less stressful for the patient. This approach is useful when the patient has had extensive adhesions from upper abdominal surgery or needs simultaneous infrarenal aortic reconstruction, or if one is performing the bypass in an urgent situation, due to a quicker revascularization time from a less extensive exposure. The inflow anastomosis can be completed at the infrarenal aorta or either iliac artery (preferably the right iliac). The selection site should be based on the intraoperative ease of clamp placement in the absence of severe calcification. The retroperitoneum is entered, and the aorta and iliac arteries are dissected free and palpated for appropriate clamp positions. If circumstances are such that the procedure is going well and a second revascularized vessel will not add to the morbidity of the procedure, this should likely be performed. It is not an uncommon observation that several years after multivessel mesenteric revascularization, one limb is occluded and the patient has remained asymptomatic. Similarly, some discussion in the literature exists as to the proper selection of conduit. Similar longterm patencies are noted, with both autogenous and prosthetic conduits. Ease of use without the trauma of vein harvest speaks for the use of prosthetic material. However, in some cases, small-diameter mesenteric vessels and calcified distal targets may demand the use of an autogenous conduit. Open surgical repair provides excellent longterm outcomes with primary intermediate (1- to 3-year) graft patencies reported to be 80% to 100%. Long-term open revascularization is a durable repair with 5-year recurrence-free survival rates of 91%. In general, operative repair is favored in patients who can tolerate surgery, and in those patients where percutaneous revascularization is not feasible. This baseline study can be used for future comparison when and if abdominal complaints occur. In all patients with bulky mesenteric plaque, antiplatelet agents should be considered for life. A clear distinction should be made between the hemodynamically stable patient and one who is actively bleeding and requires an expedient laparotomy. If the patient is hemodynamically unstable, an arterial line and central line should be placed and rapid resuscitation initiated while preparing the patient for an exploratory laparotomy. The patient should be typed and crossmatched and receive empiric intravenous broad-spectrum antibiotics that cover both gram-positive and enteric organisms. In stable patients, a diagnostic work-up may be initiated with a comprehensive operative plan set in place. Because good visualization of the surgical field is essential, the initial should be performed in the operating room, in the event of a catastrophic hemorrhage.
Order 800mg viagra vigour otc
This sequence of pathophysiologic changes in the hepatic impotence due to alcohol viagra vigour 800 mg for sale, splanchnic, and finally systemic circulation offers an opportunity for pharmacologic manipulation and management of portal hypertension. Prehepatic portal hypertension comprises 5% to 10% of portal hypertension patients in the United States and Europe. Prehepatic portal venous obstruction results from thrombosis, invasion by malignant tumor, or constriction from external surrounding processes. Portal and splenic vein thrombosis is the most common cause of prehepatic portal hypertension. Portal vein thrombosis may be associated with umbilical vein catheterization or other causes of sepsis and dehydration in infancy. Other etiologies include pancreatitis and pancreatic tumors, with the later portending a poor prognosis related to the cancer. Prehepatic portal vein thrombosis is typically associated with few downstream signs of liver injury except in preexisting cirrhosis. Finally, hepatic arteryto-portal venous fistulas, usually secondary to a liver biopsy, can occur and if large can lead to portal hypertension. Fistulas are diagnosed with radiologic imaging and can usually be managed with endoluminal angiographic techniques for their occlusion. One important variant of portal hypertensionis leftsided (sinistral) portal hypertension with isolated splenic vein thrombosis, a normal portal vein, and no intrahepatic block. The most common causes of this are pancreatitis and carcinoma of the body and tail of the pancreas. From a portal hypertension perspective, this is readily handled with splenectomy, but clearly an understanding of the underlying pathology is most important in prognosis. The intrahepatic causes of portal hypertension account for 90% of the cases in the United States and Europe. Most patients with an intrahepatic block have cirrhosis, which has multiple etiologies. These include alcohol, hepatitis B, hepatitis C, the cholestatic liver diseases (primary sclerosing cholangitis and primary biliary cirrhosis), hemochromatosis, and the other metabolic causes of cirrhosis. Although hepatitis C and alcoholic liver disease account for the majority of cirrhosis in adults, nonalcoholic fatty liver disease is an increasing cause of cirrhosis in the developed world. Portal hypertension due to cirrhosis is thought to be primarily a function of increased hepatic vascular resistance in the hepatic sinusoids due to fibrosis, scarring and distortion of the microvasculature, as well as dysregulation of contractile elements, including hepatic myofibroblasts. It is the natural history, activity, and rate of progression of the underlying liver disease that ultimately sets the prognosis. Schistosomiasis is still an important cause of portal hypertension on a worldwide basis. Still seen in the Middle and Far East and in South America, the pathologic block in schistosomiasis is fibrosis of the terminal portal venules. Although it is an intrahepatic disease process, presinusoidal obstruction of the terminal portal venous branches is balanced by an increase in hepatic arterial inflow. Congenital hepatic fibrosis is a relatively rare cause of an intrahepatic block in the United States and Europe, but it is important to recognize because it is usually associated with preserved liver function. However, more recently there have been reports of progression of congenital hepatic fibrosis to end-stage liver disease requiring liver transplantation. A similar entity is seen in India as noncirrhotic portal fibrosis, which is a cause for portal hypertension in that country. It is much more commonly attributed to a broad category of Budd-Chiari syndrome25 and the occasional patient with a constrictive pericarditis. The outflow block leads to an increase in sinusoidal pressure, centrilobular hepatocyte injury, and ultimately fibrosis, scarring, and cirrhosis. These are exceedingly rare syndromes, accounting for 1% to 2% of the cases of portal hypertension. This is largely due to the high prevalence of hepatitis C in cirrhosis but can occur in long-standing liver disease of any etiology, with an annual incidence of 3%. Transplantation should be considered for carefully selected patients who are otherwise not candidates for resection, either due to tumor characteristics or underlying liver disease. Once present, progression of small varices to larger varices and the propensity for those varices to bleed varies widely between studies. One-thirdtohalfofcirrhotic patients will develop varices, and one-third of those patients will develop a clinically significant variceal bleed. Risk of bleeding increases as variceal size increases, and survival is proportional to the severity of underlying liver disease. Despite advances in therapy, mortality from acute variceal hemorrhage is still as high as 15% to 20%. All patients with documented or suspected cirrhosis should have an upper endoscopy to document whether or not they have varices. Due to the natural history of varices and morbidity of variceal hemorrhage, surveillance of esophageal varices is recommended every 2 to 3 years and every 1 to 2 years in patients with small esophageal varices and compensated liver disease. In the presence of decompensated liver disease, upper endoscopy should be performed annually. Medical treatment options have had limited success and transplantation is indicated in these patients, especially in the pediatric population. The diagnostic and prognostic priorities will vary for each patient based on the etiology, presentation, and severity of disease. Radiologic and endoscopic evaluation are the first-line modalities in most circumstances. Endoscopy allows for identification of risk factors for variceal bleeding and provides immediate therapy of at-risk variceal columns. Increased variceal diameter and thin variceal wall thickness indicated by a red color sign are predictive of variceal bleeding due to increased wall tension in these vessels. Grading systems for esophageal varices and portal gastropathy are critical to standardizing prognosis and treatment in these patients. Doppler ultrasonography is used to visualize the size and flow through the portal vein and its tributaries. Due to its appearance along with advanced liver disease, the presence of ascites is associated with renal dysfunction. Recurring encephalopathy due to liver failure, termed hepatic encephalopathy, presents with a spectrum of symptoms ranging from cognitive changes, loss of coordination, and asterixis,tocoma. Morphologic assessment of liver parenchyma as well as liver tumors is easily done through both modalities. Hepatic venous pressures measured via transhepatic or transvenous catheterization of the hepatic veins is the gold standard of diagnosing portal hypertension. In most cases of cirrhotic liver failure, intersinusoidal connections are obliterated and sinusoidal pressure equilibrates with portal pressure. Increasing emphasis is being placed on the value of this measurement in the era of more sophisticated pharmacologic therapies. Patients with suspicion of portal hypertension will require an assessment of liver function via clinical and laboratory evaluation. The important parts in clinical assessment of liver function are the detection of ascites, evaluation for encephalopathy, detection of clinical jaundice, and assessment of muscle wasting. Laboratory data that are important are those that directly assess liver status: bilirubin, albumin, prothrombin time, aspartate aminotransferase, alanine transaminase, and alkaline phosphatase. A platelet count less than 100,000 is indicative of significant portal hypertension. All patients should have checks made of specific liver disease markers, including hepatitis panels, antinuclear antibody, antimitochondrial antibody, and metabolic disease markers for iron, copper, and alpha1-antitrypsin. Calculation of prognostic indices is important when developing a treatment algorithm for patients with portal hypertension. All patients with signs of cirrhosis should be screened for esophageal varices at time of diagnosis and every 2 to 3 years thereafter. After small varices develop or liver disease progresses to Child class B or beyond, the screening frequency should be increased to yearly intervals. Efforts to prevent or delay the first episode of variceal hemorrhage are followed by pharmacologic therapy to reduce the rate of rebleeding. Small varices detected on endoscopic surveillance require no intervention and can be followed up with annual upper endoscopy. Moderate (5 to 10 mm) to large (>10 mm) varices or presence other risk factors. First-line therapy with nonselective -blockers (propranolol, nadolol) has decreased the rate of variceal bleeding from 30% to 14%.
Discount viagra vigour 800 mg amex
This test is particularly sensitive to the assay technique erectile dysfunction best treatment buy 800 mg viagra vigour free shipping, and it is advised that serial measurements be performed. In addition, there are many nonneoplastic causes of elevated CgA that should be considered, including impaired renal and hepatic function, hypergastrinemia secondary to proton pump inhibitors or atrophic gastritis, and inflammatory bowel disease. Other pancreatic peptides should be measured as indicated by the clinical picture, including gastrin, vasoactive intestinal peptide, somatostatin, insulin, and glucagon. Other tests that can be helpful in the diagnosis, in rare cases, include pancreatic polypeptide, neuron-specific enolase, pancreastatin, and neurokinin A. It is thought to be the most sensitive imaging modality for detecting metastatic disease. Other imaging modalities to consider include the use of intraoperative or endoscopic ultrasound for difficult-to-locate pancreatic lesions. This category is inclusive of a wide spectrum of disease biology and has four types. Type I gastric carcinoids are defined by their association with chronic hypergastrinemia as a result of chronic atrophic gastritis. These tumors often are small, multiple, well differentiated, and associated with prolonged survival. These sporadic tumors are usually large, singular, and not associated with hypergastrinemia. These tumors produce 5-hydroxytryptophan and can be associated with the development of an atypical carcinoid crisis (flushing, hypotension, lacrimentation, edema, and bronchoconstriction). Incidence Gastric carcinoids have long been considered rare lesions, but with an increasing use of upper endoscopy and the increasing use of proton pump inhibitors, their incidence is increasing. Over a period of 50 years, the proportion of gastric carcinoids among all carcinoid tumors has increased from 2. Furthermore, although still quite uncommon, they are also increasing in frequency relative to other gastric malignancies-from 0. The diagnosis is made at gastroscopy by biopsies, which should be taken of the largest polyps as well as from the antrum (two biopsies) and fundus (four biopsies). The purpose of biopsies is to confirm that the polyps represent carcinoid rather than more benign (inflammatory polyps or hyperplastic polyps) or more malignant pathologies (adenocarcinoma). In addition, the normal mucosa is sampled so that the diagnosis of associated atrophic gastritis can be confirmed. Endoscopic ultrasound and cross-sectional imaging should be considered for tumors larger than 1 cm. The principles of treatment include resection with widely negative margins, formal lymphadenectomy, and assessment of metastatic disease. Those with metastatic disease can be considered for either surgical or percutaneous treatment of hepatic metastases in conjunction with resection of the primary, whereas those with widely metastatic disease should have gastric surgery only as a means of symptom control. The treatment of patients with type I gastric carcinoids is controversial because there are very little data about their natural history and how it is influenced by various treatment strategies. Furthermore, because they are relatively indolent tumors, large numbers of patients would be required, over longer periods of time, to definitively determine the best treatment strategy. Nearly 400 patients undergoing treatment for type I gastric carcinoid have been cumulatively reported by several groups. The overall disease-specific survival in most series was 100%, with a follow-up on the order of 5 years. Furthermore, a mixture of conservative and aggressive strategies was used, making it difficult to sort out natural history from treatment effect. The ideal treatment strategy would of course be able to identify those at highest risk for locoregional disease and treat them accordingly. Unfortunately, at present, this cannot be achieved with precision, so size and depth of the primary tumor are used as surrogates for poor tumor biology. When taken together, it is clear that there is significant confusion about the optimal treatment strategy for these patients. Antrectomy and local resection is advised with lymphadenectomy added only for patients with positive nodes. Although they express agreement with the threshold of 1 cm for surgical therapy, more than half of the patients who underwent resection in their series had tumors less than 1 cm. They specifically disagree that the number of lesions should guide a decision with regard to surgical therapy. As more data accumulate, we will be able to determine which patients would most benefit from surgical intervention, what the proper place of antrectomy is for these patients, and how large the benefit of surgical therapy will be for patients with a relatively indolent disease process. They can present in a protean fashion, with the symptoms most commonly being vague abdominal pain, bloating, diarrhea, weight loss, and intermittent bowel obstruction. This can occur either as a direct consequence of the tumor itself, with either luminal compromise or as a lead point for intussusception. However, it is more often the effect of local tissue change from presumed neurohormonal effectors. This can lead to extensive fibrosis and kinking of the small bowel, with resultant obstruction. Alternatively, mesenteric ischemia can occur and is related to either mechanical compromise of arterial inflow or venous outflow, or alternatively to elastic vascular sclerosis and vasospasm that is potentially related to the effects of tissue levels of serotonin. These tumors are multifocal in 25% of affected patients, particularly in the ileum. Importantly, clonality studies have suggested that multiple tumors are metastases from the primary tumor rather than distinct primaries. Prognostic indicators for carcinoid neuroendocrine tumors of the gastrointestinal tract. At presentation, only 31% of small bowel tumors are localized, 37% are regional, and 27% are distant. The estimates for lymphatic metastases from small bowel tumors less than 1 cm in size range from 11% to 44%. The 5-year survival of the most favorable group of patients with small bowel carcinoids (T1, N0) is only 86%, suggesting that early tumors can still behave aggressively. This often occurs when liver lesions are detected by ultrasound and then further imaging is undertaken. With cross-sectional imaging, the bowel, liver, and peritoneal cavity can all be adequately evaluated. Octreotide scanning is very useful for disease staging and is positive in more than 80% of patients with small bowel carcinoids. Its limitations are for small lesions and those tumors lacking types 2 and 5 somatostatin receptors. Capsule endoscopy should be used only with caution given that, in patients with significant small bowel tethering and luminal disease from carcinoid, it may lead to obstruction. Treatment It is essential in all cases of small bowel carcinoid to consider the possibility of other concomitant malignancies, reported to occur in 12% to 46% of cases. Furthermore, at exploration, a thorough search of the abdominal cavity should always be undertaken. Resection of small bowel carcinoids entails segmental resection with wide mesenteric lymphadenectomy. These patients often have significantly foreshortened mesenteries and extensive fibrotic changes throughout the mesentery that can make this procedure difficult and hazardous. These difficult cases can be approached by mobilizing the right colon and small bowel mesenteries off of the retroperitoneum and isolating the mesenteric vessels as they exit near the pancreatic neck. The vessels can then be dissected from the root out into the mesentery, peeling the nodes carefully away from the vasculature. This technique requires delaying the bowel resection until after the mesenteric dissection is completed to preserve a maximum length of well-perfused bowel. Colonic carcinoids are larger tumors with an average size of 5 cm at diagnosis and are metastatic in 40% of patients at presentation. In contrast, rectal carcinoids are most often detected incidentally or with symptoms of rectal bleeding or pain. Approximately 80% of rectal carcinoids are localized at presentation, and they are most often less than 1 cm in size. In contrast, serum chromogranin is highly sensitive and should be measured routinely. These tumors have a typical appearance, as sessile, submucosal tumors with a discolored, yellowed mucosal covering.
Oat (Oats). Viagra Vigour.
- Preventing cancer in the large intestine (colon cancer) when oat bran is used in the diet.
- Blocking fat from being absorbed from the gut, preventing fat redistribution syndrome in people with HIV disease, preventing gallstones, treating irritable bowel syndrome (IBS), diverticulosis, inflammatory bowel disease, constipation, anxiety, stress, nerve disorders, bladder weakness, joint and tendon disorders, gout, kidney conditions, opium and nicotine withdrawal, skin diseases, and other conditions.
- Lowering high blood pressure.
- What is Oats?
- Reducing blood sugar levels in people with diabetes when oat bran is used in the diet.
- Preventing stomach cancer when oats and oat bran are used in the diet.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96791
Discount viagra vigour master card
Removal of the fibrous remnant between the point of entry of the portal vein branches into the hepatic parenchyma is the goal and is the highest safe point for dissection erectile dysfunction drugs non prescription order 800mg viagra vigour mastercard. Gentle traction on the portal vein branches has been advocated to facilitate this dissection. A Roux-en-Y limb of jejunum is formed by dividing the proximal jejunum approximately 10 cm from the ligament of Treitz. The distal end is passed through the transverse mesocolon to the area of the porta hepatis. The anastomosis of the proximal jejunum is to the side of the distal jejunum approximately 30 cm from the initial point of jejunal division. The portal reconstruction is performed using an anastomosis of the antimesenteric side of the Roux limb of the jejunum close to the blind end to the tissue surrounding the biliary plate. Especially on the inside row a single layer of suture creates the inside back wall of the anastomosis. A running technique for this suture is a useful alternative and avoids the placement of intraluminal knots. The anastomosis should incorporate the entire biliary plate resulting in an area of the biliary plate covered by the Roux that is roughly the shape of an hourglass that is lying on its side. At the completion of the hepaticojejunostomy, the retrocolic tunnel and the mesenteric defects are repaired. A single, closed-suction drain is placed posterior to the anastomosis, exiting through the side of the infant. A needle biopsy of the liver is always obtained at the time of operation to document the degree of hepatic inflammation and fibrosis. Analysis of this tissue may become very helpful in determining the postoperative medical management. Biliary diversion or formation of one-way valves in the Roux limb has not measurably altered the progression of this disease to biliary cirrhosis, although the incidence of cholangitis may be decreased. Placement of the initial incision should be guided by ultrasound location of the porta or palpation of the liver under general anesthesia. Malrotation may also be found associated with the syndrome and may make retrocolic placement of the Roux limb impossible. Abnormalities of hepatic arterial supply and the presence of a preduodenal portal vein should be anticipated and recognized during portal dissection. Placement of the hepaticojejunostomy is guided by identification of the portal vein bifurcation. Reports of a laparoscopic approach to hepatoportoenterostomy are found in the literature with initial favorable results. This clinical situation is usually precipitated by cholangitis with subsequent damage to bile ducts and decreased bile flow due to that damage and the effect of infection on bile production. Most surgeons do not advocate second or even more than two attempts to reopen the hepatoportoenterostomy. That procedure is very challenging and may lead to vascular injury to the portal vein or hepatic artery. Subsequently, the effect of repeated Kasai procedures is deleterious for liver transplantation. That procedure is undertaken just as it would be for an infant who may have biliary atresia. The gallbladder is usually normal or small in caliber and often contains bile, although it may be dilute. Once a catheter is secured in the dome of the gallbladder, injection of the contrast is performed with fluoroscopic visualization of the contrast injection. Contrast is usually seen flowing into the duodenum, but the extrahepatic biliary structures and the intrahepatic ducts are quite small. No further operative treatment is performed, and the incision is closed without a drain after suture closure of the gallbladder with absorbable sutures. Bile flow may be slow at first and not reach normal proportions for several months. A medical regimen of corticosteroids, ursodeoxycholic acid, and prophylactic antibiotics to prevent cholangitis appears to enhance and sustain bile flow. Wide variation is found in choice and length of treatment with antibiotics, steroids, and ursodeoxycholic acid. Systemic antibiotics and increased corticosteroids may result in improved bile flow. At one time, repeat operation was advocated for infants who had drained bile initially and subsequently became jaundiced. This treatment is no longer advocated because it has not had a high rate of success. Infants whose jaundice does not clear or those with recurrent jaundice should be referred for early evaluation for liver transplantation. The average length of survival in those infants whose total bilirubin did not decrease below 5 mg/dL after hepatoportoenterostomy was 18 months. Nutritional requirements for all biliary atresia patients are greater than normal and especially so for those who remain jaundiced. In the syndromatic condition, the search for associated anomalies includes consultation by ophthalmology, cardiology, nephrology, and gastroenterology. The child will require long-term follow-up to assess their progression of liver disease. Most challenging for the child facing liver transplantation is the inadequacy of the donor organ pool. Segmental transplantation from cadaveric or live donors can meet this need but is neither universally practiced nor possible without the cooperation of adult transplant surgeons. Liver transplantation, whether prior to or after hepatoportoenterostomy, is straightforward, although technically challenging. Hepatic artery and portal vein anastomoses are facilitated by operating loupes or microscope. Patient and graft survival rates are excellent; more than 90% of children are alive at 1 year, and of those, most are alive at 10 years. Sequential treatment of biliary atresia with Kasai portoenterotomy and liver transplantation: a review. Biliary atresia: surgical management and treatment options as they relate to outcome. Syndromatic paucity of interlobal bile ducts (Alagille syndrome or arteriohepatic hypoplasia): review of 80 cases. Technical innovation for noninvasive and early diagnosis of biliary atresia: the ultrasonographic "triangular cord" sign. Design and validation of the biliary atresia research consortium histologic assessment for cholestasis in infancy. Biliary atresia and other structural anomalies in congenital polysplenia syndrome. The anatomic pattern of biliary atresia at time of Kasai hepatoportoenterostomy and early postoperative clearance of jaundice are significant predictors of transplant-free survival. Prognostic value of computerized quantification of liver fibrosis in children with biliary atresia. A recent systematic review of native liver survival without transplantation at 10 years ranged between 24% and 52. Almost one-third of patients have only modest or no improvement in the jaundice after hepatoportoenterostomy. Liver transplantation is the next line of therapy for the jaundiced child and for those with the sequelae of progressive liver disease. Transplantation may be required in infancy because of the inability to obtain bile drainage with hepatoportoenterostomy or at the time of initial diagnosis if end-stage liver disease is present. Randomized, double-blind, placebo-controlled trial of corticosteroids after Kasai portoenterostomy for biliary atresia. Should open Kasai portoenterostomy be performed for biliary atresia in the era of laparoscopy Effect of repeat Kasai hepatic portoenterostomy on pediatric live-donor liver graft for biliary atresia. On the other hand, pancreaticobiliary maljunction, which was first noted by Kozumi and Kodama8 in an autopsy case with congenital biliary dilatation in 1916, is a congenital anomaly defined as an abnormal union of the pancreatic and biliary ducts. This initial observation did not attract attention for many years, but the concept has been accepted widely since Babbitt9 reported the anomaly in 1969. Incidence Congenital biliary dilatation has generally been considered a rarity, but recently the number of cases reported in the literature has steadily increased.
Buy discount viagra vigour 800mg on-line
Islets (usually 2 to 5 mL; up to 10-mL tissue pellet) are suspended in 200 to 400 mL solution (transplant media) with heparin and human albumin contained in a plastic infusion bag injections for erectile dysfunction that truly work best purchase for viagra vigour. The procedure starts with portal pressure measurements to ensure absence of portal hypertension. Next, islets are dripped slowly through the intravenous line connecting the harvested islet bag with the portal catheter. Alternatively, it can be done under general anesthesia and in the operating room during a mini-laparotomy with infusion through the mesocolonic vein if percutaneous access via the portal vein fails. Postoperatively, subcutaneous heparin and insulin are administered for at least 2 weeks to promote islet engraftment. Because islets were used in "brittle" type 1 diabetics with preserved kidney function, the main rationale was to improve islet survival and function (thus a steroid-free approach) and protect kidney function (calcineurin inhibitors were minimized). After 5 years of disappointing experience with this approach, many different protocols were developed. Allosensitization Because pancreatic islet allotransplantation usually requires two or three islet infusions from the same number of different donors, there is theoretically an increased risk for allosensitization. With the current technology, we are able to retrieve only 30% to 50% of original islet mass, even from the best cadaveric pancreata. It is also estimated that an additional 50% of islets are being destroyed by the native immunity instant blood-mediated inflammatory response. After 1 to 2 months, after islet engraftment is accomplished, the patient is offered subsequent transplant with a chance of additional benefit-insulin independence (secondary endpoint). If required later, a patient may be offered supplemental islet infusions to maintain insulin independence. Of course, the ultimate goal of the current islet studies is to improve islet isolation and transplantation procedure to achieve insulin independence with only one infusion from a single donor routinely (currently 15% rate in Edmonton). Islet graft function (C-peptide positive) was preserved in 94% of patients with insulin independence rate of 51% at 1-year follow-up. As expected for a new and sophisticated procedure, there have been varied results among centers; therefore the average insulin independence rate might be seen as low. Those few, most experienced centers have reported much higher insulin independence rates, as high as 40% to 50% at 5-year follow-up. The median time to achievement of insulin independence was 6 to 7 months after the first transplant. Insulin independence was superior in groups 1 and 2 compared with groups 3 and 4 at 3 and 5 years post transplant; groups 1 and 2 did not differ statistically from pancreas transplant alone (group 5). Potent induction immunotherapy promotes long-term insulin independence after islet transplantation in type I diabetes. Causes of death were (number of cases): cardiovascular (5), hemorrhage (3), pneumonia (2), diabetic ketoacidosis (1), infection (1), respiratory arrest (1), acute toxicity (1), pneumopathy (1), multiorgan failure of unknown etiology (1), viral meningitis (1), and lung cancer (1). Even low-dose tacrolimus compromied renal function, especially in patients with preexisting renal impairment. Of note, most studies report some degree of kidney dysfunction without distinction of the islet graft function and long-term glucose control, implicating that only toxic effects of immunosuppression are responsible for impairment. Our four patients, who have been insulin free for more than 5 years (5 to 11 years) still present completely normal kidney function (serum creatinine below 1 mg/mL) despite years of immunosuppression including tacrolimus or rapamycin. Younger patients have higher rates of rejection, but those older than 50 years of age have higher postoperative complication rates. The most appropriate type of pancreas transplant depends on patient comorbidity, renal function, and availability of living or cadaveric donor. However, 3% to 30% of those patients will require a kidney transplant in 9 to 10 years because of calcineurin-inhibitor nephrotoxicity, which is an independent risk factor for progression of kidney failure. Islet transplantation provides an advantage of being a minimally invasive procedure, especially to patients with contraindication for major surgery, whereas pancreas transplantation delivers instant and more durable endocrine effects. Nevertheless, medical indications for pancreas and islet transplantation remain the same. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. Allotransplantation of the pancreas and duodenum along with the kidney in diabetic nephropathy. Pancreatic islet transplantation after upper abdominal exenteration and liver replacement. Islet transplantation in seven patients with type 1 diabetes mellitus using a glucocorticoid-free immunosuppressive regimen. Access to pancreas transplantation should not be restricted because of age: invited commentary on Schenker et al. Clinical islet isolation and transplantation outcomes with deceased cardiac death donors are similar to neurological determination of death donors. Improved survival in patients with insulin-dependent diabetes mellitus and end-stage diabetic nephropathy 10 years after combined pancreas and kidney transplantation. Long-term survival following simultaneous kidney-pancreas transplantation versus kidney transplantation alone in patients with type 1 diabetes mellitus and renal failure. The impact of simultaneous pancreas-kidney transplantation on long-term patient survival. Survival after pancreas transplantation in patients with diabetes and preserved kidney function. Islet-after-failed-pancreas and pancreas-after-failed-islet transplantation: two complementary rescue strategies to control diabetes. Lessons learned from more than 1,000 pancreas transplants at a single institution. Progression of diabetic retinopathy after pancreas transplantation for insulin-dependent diabetes mellitus. Islet transplantation at the university of Alberta: status update and review of progress over the last decade. Prevention of bleeding after islet transplantation: lessons learned from a multivariate analysis of 132 cases at a single institution. Portal vein thrombosis is a potentially preventable complication in clinical islet transplantation. Supplemental islet infusions restore insulin independence after graft dysfunction in islet transplant recipients. Outcomes of pancreatic aslet allotransplantation using the Edmonton protocol at the university of Chicago. Pancreas after islets transplantation: a first report of the International Pancreas Transplant Registry. A multi-year analysis of islet transplantation compared with intensive medical therapy on progression of complications in type 1 diabetes. Reduced progression of diabetic microvascular complications with islet cell transplantation compared with intensive medical therapy. The effect of pancreatic islet transplantation on progression of diabetic retinopathy and neuropathy. Positive effects of clinical islet transplantation on diabetic retinopathy over 5 years. Diabetic peripheral neuropathy is stabilized after clinical islet transplantation: 7 year follow-up study. Islet cell transplantation improves diabetic neuropathy compared with intensive medical therapy. What defines success in pancreas and islet transplantation-insulin independence or prevention of hypoglycemia Positron emission tomography and autoradiography of (18)F-Fluorodeoxyglucose labeled islet with or without warm ischemic stress in portal transplanted rats. Eich T, Eriksson O, Lundgren T, Nordic Network for Clinical Islet Transplantation. Visualization of early engraftment in clinical islet transplantation by positron-emission tomography. Optimizing islet engraftment is critical for successful clinical islet transplantation. Restoration of glucose counterregulation by islet transplantation in long-standing type I diabetes.

Purchase generic viagra vigour from india
When completed erectile dysfunction 32 years old buy 800mg viagra vigour fast delivery, this anastomosis invaginates the cut surface of the pancreatic neck into the jejunal lumen for several centimeters. The stomach can also be used to reconnect the pancreas with an invagination method similar to the one described for the jejunum. The biliary anastomosis is performed next with an end-to-side hepaticojejunostomy approximately 5 to 10 cm distal to the pancreaticojejunostomy. This anastomosis is performed with a single layer of interrupted absorbable suture. Finally, the last anastomosis, either a duodenojejunostomy or gastrojejunostomy, is performed depending on whether the pylorus has been preserved. This anastomosis can be performed 10 to 15 cm distal to the hepaticojejunostomy, proximal to the portion of jejunum traversing the defect in the mesocolon. Alternatively, it can be performed in antecolic fashion more distally on the jejunal limb, distal to where it traverses the mesocolic defect. At the end of the operation, closed suction drains are left in place near the pancreatic and biliary anastomoses. Some groups prefer not to drain and accept that if a fluid collection becomes clinically evident postoperatively, percutaneous drainage by interventional radiology may be required. The drains around the pancreatic anastomosis are typically removed once the patient has been on a regular diet without any significant output of amylase-rich or bilious fluid. However, given the technical demands of this operation, it is primarily limited to high-volume centers. The hepatic artery is identified and dissected with the hook cautery to find the takeoff of the gastroduodenal artery, which is a landmark for the portal vein below. At this point, the inferior portion of the pancreas is dissected looking for the superior mesenteric vein. Earlier identification of the portal vein helps with superior mesenteric vein identification. Once found, the tunnel is created under the neck of the pancreas with gentle blunt dissection and encircled with an umbilical tape. Once the tunnel under the pancreas neck is created, the gallbladder is mobilized and used to find the common bile duct, which is encircled with a vessel loop prior to transection. Following the resection of the common bile duct, the Kocher maneuver can be started by mobilizing the duodenum staying close to the bowel. After the extended kocherization is complete, the distal jejunum is identified 30 to 40 cm distal to the ligament of Treitz and transected with a stapler. The stapled ends of the jejunum are sewn to each other with a 25-cm silk stitch with a large gap to facilitate pulling the distal jejunum through the ligament of Treitz for future anastomosis. Next, the colon is lifted and the ligament of Treitz is freed with a hook cautery and the antrum is divided with a stapler. As the specimen is pulled to the right upper quadrant, the previously sewn jejunal limb will be pulled through the ligament of Treitz defect into proper place for pancreatic and biliary anastomosis. Reconstruction of the three anastomoses can now be done with the jejunum already in proper position. These anastomoses are done similar to the open technique requiring intracorporeal stitches. The pancreatic anastomosis can be done from the duct to the mucosa or using the invagination technique. The hepaticojejunostomy is done with interrupted suture with the assistant holding the bowel up to facilitate this step. The final gastroduodenojejunal anastomosis can be done in a two-layered intracorporeal sewn fashion or stapled. Staging laparoscopy is advocated for patients with distal pancreatic cancer because carcinomatosis is a more common finding in patients with cancers of the body and tail. Exposure is provided by a vertical midline incision from the xiphoid process to several centimeters below the umbilicus. The lesser sac is entered by elevating the greater omentum off the transverse colon. The splenic flexure of the colon is then mobilized caudally and away from the spleen by dividing the splenocolic ligament. Splenectomy is usually performed with distal pancreatectomy in patients suspected of having carcinoma to obtain better margins, and to remove the lymph nodes at the tip of the pancreas and the hilum of the spleen. However, for some limited benign pancreatic diseases, the spleen can be preserved. The spleen is mobilized toward the midline by dividing the splenorenal ligament with the electrocautery device. A plane is then developed behind the pancreatic tail and body to also mobilize and control the splenic vein. This dissection is continued until an adequate margin is reached beyond the tumor. The electrocautery device is next used to transect the pancreatic parenchyma distal to this suture line. A row of overlapping "U" stitches of absorbable suture should then be placed to control the transected remnant. If the main pancreatic duct can be identified, it should be suture ligated with an absorbable monofilament suture. A frozen section should be performed on the pancreatic margin to confirm clearance of the lesion prior to completion of the operation. If an operative drain is left in place, it is monitored for signs of a pancreatic leak. Removing the spleen does place the patient theoretically at increased risk for postsplenectomy sepsis, and vaccines are given preoperatively or after recovery for pneumococcus, Neisseria meningitidis, and Haemophilus influenzae. In recent years, the laparoscopic approach has become a standard method to perform a distal pancreatectomy with or without splenectomy. Laparoscopic distal pancreatectomy has been demonstrated to have similar outcomes without any increase in morbidity or mortality when compared to the open approach. However, several postoperative complications continue to be frequent after pancreatic resection. With these interventions, symptoms will typically resolve and the majority of patients are able to tolerate an oral diet. Grade B pancreatic fistulas occur in patients who generally appear well, but may require parenteral nutrition or fistula drainage for the fistula to heal. The most severe form are grade C fistulas, in which patients appear ill and require parenteral nutrition, interventional drainage, and potentially even reoperation for treatment. Conversely, severe hemorrhage involves large-volume blood loss evidenced by a hemoglobin drop of greater than 3 g/dL and requires urgent intervention to treat. Early hemorrhage occurs within 24 hours of surgery, whereas late hemorrhage is defined as occurring on or beyond 5 days after surgery. Late bleeding is usually caused by a pseudoaneurysm formed by a pancreatic fistula or nearby infection, leading to erosion of the vasculature by amylase-rich fluid. Surgical exploration and control is reserved for instances in which the patient is too unstable for interventional radiology or in whom embolization is unsuccessful. In addition, improved 5-year survival is seen for patients with well-differentiated tumors, negative lymph nodes, and negative (or R0) resection margins despite the tumor type. Median and overall survival at 5 years is higher for patients with right-sided lesions in the pancreatic head when compared to left-sided pancreatic cancers. It is estimated that as many as 80% of patients with pancreatic malignancies will present with unresectable or metastatic disease. As a result, a combination of operative and nonoperative management is usually required for symptom management. In the majority of patients, nonoperative palliation is the first choice in treatment, with surgery reserved for patients unable to be adequately managed by these methods. The three main symptoms necessitating palliation are obstructive jaundice, gastric outlet obstruction, and pain. Often, this obstruction will lead to symptoms such as jaundice, abdominal discomfort, pruritus, and nausea. Many patients will require endoscopic or surgical decompression of the biliary tract to relieve obstruction, mitigate symptoms, and improve quality of life. This is accomplished by surgical resection of the primary tumor in patients with early stage, resectable disease.
Generic 800 mg viagra vigour with mastercard
Although these tumors may be extremely large and can invade critical vasculature erectile dysfunction studies purchase 800mg viagra vigour amex, most lesions are usually amenable to complete resection. Pancreaticoduodenectomy or distal pancreatectomy can be performed with en bloc resection of involved adjacent organs when indicated. Given the excellent survival rates after surgical resection alone, adjuvant systemic therapy is not routinely used. If metastatic disease occurs, the most common sites include liver, mesentery, and peritoneum. Jaundice has been reported in up to 70% to 80% of patients and is likely due to inflammation and narrowing or stricture of the distal common bile duct. Immunostaining often demonstrates abundant (>10 cells/ high-power field) IgG4-positive cells. Diagnostic criteria rely on a combination of histology, cross-sectional and endoscopic imaging, serologic findings, and a detailed clinical history. The International Consensus Diagnostic Criteria for Autoimmune Pancreatitis recommends a trial of 0. With clinical and radiologic improvement, the prednisone can be tapered by 5 mg/week. Because clinical relapse can occur in up to 30% of patients, some investigators have advocated the administration of low-dose maintenance prednisone. Common presenting symptoms include abdominal pain (67% to 73%), B symptoms such as fever, night sweats, chills, weight loss (38% to 58%), jaundice (33% to 42%), and gastric or duodenal outlet obstruction (2% to 26%). The involved lymph nodes lack central necrosis or calcifications, and the pancreatic duct is rarely dilated despite what appears to be a large pancreatic tumor. Cytopathologic features include large malignant lymphocytic nuclei, prominent nucleoli, abundant karyorrhexis, and a background of necrosis. Note the hypodense appearance of the mass (arrowheads) and the adjacent abutment of the superior mesenteric vein (long arrow) and proximity to the superior mesenteric artery (short arrow). Complete remission can be expected with multidrug therapy in 63% to 77% of patients with large B-cell lymphoma. Note the characteristic enhancement of the metastatic lesion (arrow) on arterial phase imaging, as well as the posterior displacement of the pancreas (arrowheads) due to the absence of the left kidney. The imaging characteristics can be similar to pancreatic neuroendocrine neoplasms, and these lesions should be included in the differential diagnosis. In contrast, the hypervascularity of the tumor is inconsistent with pancreatic ductal adenocarcinoma. Men and women are equally affected, and there are no differences in the laterality of the primary tumor and the location of the metastases within the pancreas. The majority of patients have solitary metastases, which are usually asymptomatic (>50%) and identified incidentally or during follow-up surveillance. Among those who are symptomatic, abdominal pain, weight loss, jaundice, or gastrointestinal hemorrhage may be the presenting complaint. However, a tissue biopsy may be helpful if there is diagnostic concern for a pancreatic neuroendocrine neoplasm or if there is disease outside of the pancreas suggesting multiple sites of recurrence. This is best achieved by a coordinated approach involving a multidisciplinary team of physicians, with particular attention to radiographic and pathologic analysis. Clinical characteristics and outcomes from an institutional series of acinar cell carcinoma of the pancreas and related tumors. Acinar cell carcinoma of the pancreas: an institutional series of resected patients and review of the current literature. Acinar cell carcinoma of the pancreas: clinical and computed tomography manifestations. Cytomorphologic and immunophenotypical features of acinar cell neoplasms of the pancreas. Acinar cell carcinomas of the pancreas: a molecular analysis in a series of 57 cases. Neurogenin 3-directed cre deletion of Tsc1 gene causes pancreatic acinar carcinoma. Acinar cell carcinoma of the pancreas in the United States: prognostic factors and comparison to ductal adenocarcinoma. Acinar cell carcinoma of the pancreas: new genetic and treatment insights into a rare malignancy. Aggressive approach to acinar cell carcinoma of the pancreas: a single-institution experience and a literature review. Pancreatic solid-cystic papillary tumor: clinical features, imaging findings and operative management. Note the solid sheets of tumor cells that are separated into acini by vascular septae. Solid pseudopapillary tumor of the pancreas: a single-institution 20-year series of pediatric patients. Solid pseudopapillary neoplasm of the pancreas: a single institution experience of 14 cases. Solid pseudopapillary tumors of the pancreas: review of 718 patients reported in English literature. Institutional experience with solid pseudopapillary neoplasms: focus on computed tomography, magnetic resonance imaging, conventional ultrasound, endoscopic ultrasound, and predictors of aggressive histology. Solid-pseudopapillary tumor of the pancreas: a typically cystic carcinoma of low malignant potential. Clinical and pathological features of solid pseudopapillary neoplasms of the pancreas at a single institution. Alpha-methylacyl-CoA racemase (P504S) is a useful marker for the differential diagnosis of solid pseudopapillary neoplasm of the pancreas. The prognosis and clinical characteristics of advanced (malignant) solid pseudopapillary neoplasm of the pancreas. Recurrence of solid pseudopapillary neoplasms of the pancreas: results of a nationwide study of risk factors and treatment modalities. A combination of molecular markers and clinical features improve the classification of pancreatic cysts. Solid-pseudopapillary tumors of the pancreas are genetically distinct from pancreatic ductal adenocarcinomas and almost always harbor beta-catenin mutations. Identification of potential biomarkers to differentially diagnose solid pseudopapillary tumors and pancreatic malignancies via a gene regulatory network. Characterization of gene expression and activated signaling pathways in solid-pseudopapillary neoplasm of pancreas. Surgical management of solid-pseudopapillary neoplasms of the pancreas (Franz or Hamoudi tumors): a large single-institutional series. Resection of a solid and papillary epithelial neoplasm of the pancreas following treatment with cis-platinum and 5-fluorouracil: a case report. Preoperative gemcitabine for unresectable, solid pseudopapillary tumour of the pancreas. International Consensus Diagnostic Criteria for Autoimmune Pancreatitis: guidelines of the International Association of Pancreatology. Incidence and characteristics of chronic and lymphoplasmacytic sclerosing pancreatitis in patients scheduled to undergo a pancreatoduodenectomy. Differences in clinical profile and relapse rate of type 1 versus type 2 autoimmune pancreatitis. Autoimmune pancreatitis: differences between the focal and diffuse forms in 87 patients. Histopathologic and clinical subtypes of autoimmune pancreatitis: the Honolulu consensus document. Assessment of the rate of decrease in serum IgG4 level of autoimmune pancreatitis patients in response to initial steroid therapy as a predictor of subsequent relapse. Rituximab therapy leads to rapid decline of serum IgG4 levels and prompt clinical improvement in IgG4-related systemic disease. Cross-classification and survival characteristics of 5,000 cases of cancer of the pancreas. Primary pancreatic lymphoma-pancreatic tumours that are potentially curable without resection, a retrospective review of four cases. Guide to diagnosing primary pancreatic lymphoma, B-cell type: immunocytochemistry improves the diagnostic accuracy of endoscopic ultrasonography-guided fine needle aspiration cytology. Endoscopic ultrasoundguided fine-needle aspiration with or without flow cytometry for the diagnosis of primary pancreatic lymphoma-a case series. Surgical management of metastatic renal cell carcinoma in the era of targeted therapies.