Purchase zyloprim australia
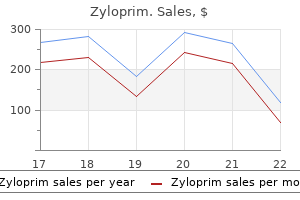
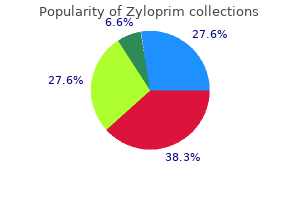
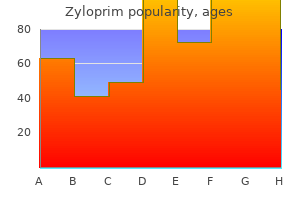
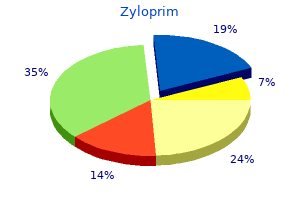
Effective pulmonary flow is decreased and the left ventricle is exposed to conditions similar to a large arteriovenous fistula treatment west nile virus buy generic zyloprim 100 mg on line. Myocardial oxygen demand is increased, diastolic aortic pressure is borderline and the patient is cyanotic; all of which contribute to progressively worsening myocardial performance. Still consideration may be given to stenting the ductus concurrent with valve perforation in selected cases (104). It seems that the best outcomes are clearly achieved with an individualized cooperative creative transcatheter surgical approach including the so-called hybrid interventions (106,107,108,109). The role of transcatheter techniques in the management of these patients is in evolution, however, in at least one series it compared favorably to surgical outflow tract reconstruction (81). It is important to recognize that the postintervention period is characterized by a changing physiology that may include adjustment to postnatal life, right-to-left shunting at the atrial level, systolic myocardial dysfunction, potentially ineffective circulatory flow, restrictive right ventricular physiology, pulmonary stenosis and insufficiency and tricuspid insufficiency represents a tremendous challenge to postintervention management with few, if any, cardiac conditions being more complex to the intensive care unit. One cannot underestimate the influence of expertise in managing this challenging state when evaluating the influence of experience on outcome. With a relatively small number of patients affected by this condition, there is much to be learned from a multicentered approach to collecting a longitudinal experience in a combined transcatheter and surgical approach to a challenging clinical problem. Whereas a percutaneous approach may avoid or delay the use of cardiopulmonary bypass in the newborn period, it remains to be seen whether it results in a decrease of long-term morbidity or mortality. Treatment of the Adult It should be clear from the preceding discussions that there is great anatomic and physiologic diversity of patients surviving to adulthood with pulmonary atresia and intact ventricular septum. Patients may have achieved a biventricular circulation, a univentricular circulation in the form of a total cavopulmonary circulation or a permanently palliated shunted state. Outcome data for the adult population are few and reported results may even be counter intuitive. For instance, it is unclear whether a biventricular circulation holds advantage over a univentricular circulation in the assessment of exercise capacity and indeed may be more influenced by pulmonary than cardiac issues, as aerobic capacity appears decreased in both groups (70,110). Further, restrictive physiology associated with right ventricular pathology appears to play an important role (69). Myocardial perfusion abnormalities persist well beyond definitive repair (palliation) (111). In the adult with a biventricular repair right ventricular restriction may favor better physiologic status, although many patients will go on to require a pulmonary valve replacement to restore competency of the right ventricular outflow tract (69,112). In a recent study (113) of 20 survivors into adulthood (19 to 39 years old) with Fontan (n = 7), biventricular (n = 8), and palliated shunts (n = 5) there were five deaths at a mean of 32 years old. Atrial arrhythmias occurred frequently (80%) but ventricular arrhythmias were not uncommon (15%). Although the literature is sparse it is clear that all of these patients will require continued specialized tertiary and quaternary follow-up, specialized intervention, arrhythmia management, and ancillary support as they reach adulthood. The value of registry data to guide the care of the growing population of adults with congenital heart disease cannot be overstated. Summary Congenitally malformed hearts with pulmonary atresia with intact ventricular septum demonstrate clinically important heterogeneity of the right-sided cardiac structures, the coronary circulation, and the myocardium. Fetal recognition of this condition will affect postnatal epidemiology due to the influence of elective termination of pregnancy (8,114,115). Rarely survival beyond the neonatal period has been documented due to persistent patency of the arterial duct or more rarely by associated conditions that preserve pulmonary blood flow such as an aortopulmonary window or coronary to pulmonary artery connections. An intermediate form of palliation exists in the form of the so-called one-and-a-half ventricle repair where the right ventricle with a patent outflow tract is effectively unloaded with a bidirectional cavopulmonary connection although the long-term advantage of this circulation remains to be seen (72,116,117,118,119). Where some have questioned whether it is possible to improve outcomes, the literature supports cautious optimism by demonstrating improved survival with era of intervention. Understanding the nature of the coronary arterial circulation, the application of a one-ventricle or one-and-a-half ventricle repair, and the application of radiofrequency catheter perforation of the imperforate pulmonary valve all have contributed to increased salvage of these infants, although there is still much to be achieved. Intrinsic, indeed congenital, abnormalities in the vascular supply and myocardial architecture may ultimately argue for a poor outcome in at least some of these patients. Sudden coronary death remains a worrisome long-term concern but establishing risk is unclear (120). It is clear that the anatomic and physiologic diversity of this patient population represented by the neonate will continue to challenge treatment strategies into adulthood. Pulmonary atresia/critical stenosis with intact ventricular septum: prediction of outcome in the second trimester of pregnancy. Echocardiographic predictors of outcome in fetuses with pulmonary atresia with intact ventricular septum. Determinants of outcome in fetal pulmonary valve stenosis or atresia with intact ventricular septum. Pulmonary atresia, "intact ventricular septum", and aortopulmonary collateral arteries. Pulmonary atresia with and without ventricular septal defect: a different etiology and pathogenesis for the atresia in the 2 types Pulmonary atresia/intact ventricular septum: influence of coronary anatomy on single-ventricle outcome. Muscular infundibular atresia is associated with coronary ostial atresia in pulmonary atresia with intact ventricular septum. Angio-pathological appearances of pulmonary valve in pulmonary atresia with intact ventricular septum. Pulmonary atresia with intact ventricular septum: range of morphology in a population-based study. Some thoughts about the underdeveloped right ventricle in pulmonary atresia and intact ventricular septum. Influence of right heart size on outcome in pulmonary atresia with intact ventricular septum. Right ventricular growth potential in neonates with pulmonary atresia and intact ventricular septum. Right ventricular volume determinations in 18 patients with pulmonary atresia and intact ventricular septum. The recognition, identification of morphologic substrate, and treatment of subaortic stenosis after a Fontan operation. Pulmonary atresia, intact ventricular septum, and major aortopulmonary collaterals: morphogenetic and surgical implications. Ductus arteriosus in pulmonary atresia with and without ventricular septal defect. Initial results and medium-term followup of stent implantation of patent ductus arteriosus in duct-dependent pulmonary circulation. Myocardial ischemia in patients with pulmonary atresia and intact ventricular septum. Right ventricular infarction with cardiac rupture in an infant with pulmonary valve atresia with intact ventricular septum. Capillary distribution in the ventricles of hearts with pulmonary atresia and intact ventricular septum. Development of the coronary vasculature and its implications for coronary abnormalities in general and specifically in pulmonary atresia without ventricular septal defect. Competition of coronary arteries and ventriculo-coronary arterial communications in pulmonary atresia with intact ventricular septum. Pulmonary atresia with intact ventricular septum and hypoplastic right heart in sibs: a single gene disorder Usefulness of Doppler echocardiography in diagnosing right ventricular coronary arterial communications in patients with pulmonary atresia and intact ventricular septum and comparison with angiography. Complete atresia of coronary ostia in pulmonary atresia and intact ventricular septum. Echocardiographic determinants of successful balloon dilation in pulmonary atresia with intact ventricular septum. Changing trends in the management of pulmonary atresia with intact ventricular septum: the Melbourne experience. Long-term functional health status and exercise test variables for patients with pulmonary atresia with intact ventricular septum: a Congenital Heart Surgeons Society study. Outcomes and predictors of reintervention in patients with pulmonary atresia and intact ventricular septum treated with radiofrequency perforation and balloon pulmonary valvuloplasty. Pulmonary atresia with intact ventricular septum: long-term results of "one and a half ventricular repair". The Fontan procedure for pulmonary atresia with intact ventricular septum: operative and late results. Pulmonary atresia with intact ventricular septum: results of the Fontan procedure.
Order zyloprim 100mg without a prescription
Cardiopulmonary bypass induces significant platelet activation in children undergoing open-heart surgery medicine omeprazole buy cheap zyloprim on line. Thrombosis in children with cardiac pathology: analysis of acquired and inherited risk factors. Interaction of fibrinolysis and prothrombotic risk factors in neonates, infants and children with and without thromboembolism and underlying cardiac disease. Coagulation factor abnormalities in patients with single-ventricle physiology immediately prior to the Fontan procedure. Abnormalities in liver function and coagulation profile following the Fontan procedure. Hemostatic parameters and platelet activation marker expression in cyanotic and acyanotic pediatric patients undergoing cardiac surgery in the presence of tranexamic acid. In vivo tracking of platelets: circulating degranulated platelets rapidly lose surface P-selectin but continue to circulate and function. Early systemic-to-pulmonary artery shunt intervention in neonates with congenital heart disease. Benefit of heparin in peripheral venous and arterial catheters: systematic review and metaanalysis of randomised controlled trials. Association between thrombosis and bloodstream infection in neonates with peripherally inserted catheters. Risk, clinical features, and outcomes of thrombosis associated with pediatric cardiac surgery. Thrombotic complications in a pediatric cardiovascular surgery population: a nine-year experience. Three-dimensional echocardiographic evaluation of the Fontan conduit for thrombus. Diagnosis and management of deep venous thrombosis and pulmonary embolism in neonates and children. Clinical outcomes of palliative surgery including a systemic-to-pulmonary artery shunt in infants with cyanotic congenital heart disease: does aspirin make a difference Aspirin unresponsiveness predicts thrombosis in high-risk pediatric patients after cardiac surgery. Endovascular stents for relief of cyanosis in single-ventricle patients with shunt or conduitdependent pulmonary blood flow. Obstruction in modified Blalock shunts: a quantitative analysis with clinical correlation. Risk factors for cerebrovascular events following fontan palliation in patients with a functional single ventricle. Factors associated with thrombotic complications after the Fontan procedure: a secondary analysis of a multicenter, randomized trial of primary thromboprophylaxis for 2 years after the Fontan procedure. Aortic valve replacement in children under 16 years of age with congenital or rheumatic valvular disease. Mechanical valve in aortic position is a valid option in children and adolescents. The long-term risk of warfarin sodium therapy and the incidence of thromboembolism in children after prosthetic cardiac valve replacement. Melody transcatheter valve: histopathology and clinical implications of nine explanted devices. Thrombotic obstruction of a melody valve-in-valve used for prosthetic tricuspid stenosis. A prospective trial showing the safety of adjusted-dose enoxaparin for thromboprophylaxis of pregnant women with mechanical prosthetic heart valves. Thrombolysis of prosthetic tricuspid valve thrombosis with human recombinant tissue plasminogen activator in an adolescent. Assessing the outcome of systemic tissue plasminogen activator for the management of venous and arterial thrombosis in pediatrics. Bleeding and thrombotic emergencies in pediatric cardiac intensive care: unchecked balances. Intracardiac thrombosis diagnosed by echocardiography in childhood: predisposing and etiological factors. Surgical thrombectomy of two left ventricular thrombi in a child with acute myocarditis. Perioperative management of antithrombotic therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. The role of tissue plasminogen activator in the successful treatment of infected cardiac thrombus in children. Early intracardiac thrombosis in preterm infants and thrombolysis with recombinant tissue type plasminogen activator. Management of preterm infants with intracardiac thrombi: use of thrombolytic agents. Successful thrombolytic therapy for acute massive pulmonary thrombosis after total cavopulmonary shunt. Successful treatment of infective endocarditis with recombinant tissue plasminogen activator. Successful thrombolysis of acute left atrial thrombi in two pediatric patients following interventional cardiac catheterization. Management of a large organized intraatrial catheter-tip thrombus in a child with acquired immunodeficiency syndrome using escalating tissue plasminogen activator infusions. Use of tissue plasminogen activator for femoral artery thrombosis following transcatheter coil occlusion of patent ductus arteriosus. Treatment of infective endocarditis with recombinant tissue plasminogen activator. Therapeutic application of intrapericardial tissue plasminogen activator in a 4-month-old child with complex fibropurulent pericarditis. Thrombosis of an extracardiac Fontan tunnel: combined treatment of thrombolysis and stenting. The use of recombinant tissue plasminogen activator in the management of infective intracardiac thrombi in pre-term infants with thrombocytopaenia. Successful treatment of a thrombus in the left aortic coronary sinus in a child with systemic lupus erythematosus. Clinical experience with alteplase in the management of intracardiac and major cardiac vessels thrombosis in pediatrics: a case series. An institutional approach to interventional strategies for complete vascular occlusions. The use of recombinant tissue-type plasminogen activator in a newborn with an intracardiac thrombus developed during extracorporeal membrane oxygenation. Cardiac findings and long-term thromboembolic outcomes following pulmonary embolism in children: a combined retrospective-prospective inception cohort study. Clinical experience with recombinant tissue plasminogen activator in the management of intracardiac and arterial thrombosis in children. Intracardiac thrombus in children: the fine equilibrium between the risk and the benefit. Successful thrombolysis following enoxaparin therapy in two pediatric patients with congenital heart disease presenting with intracardiac and cerebral thrombosis. Risk factors supported by focused retrospective observational studies include atriopulmonary type of Fontan connection, bilateral bidirectional cavopulmonary anastomoses, hypoplastic cardiac chambers with flow stasis, presence of a blind-ended pulmonary artery stump, and a history of previous thrombosis. Additional potential factors supported by general retrospective observational studies or expert opinion include protein-losing enteropathy, prolonged pleural effusions, prolonged immobilization, ventricular dysfunction, arrhythmia, presence of thrombogenic foreign material, atrial-level fenestration, Kawashima connection, and an abnormal thrombophilia profile. Considering the role of the heart as the engine of circulatory propulsion, cardiac structural aberrations may impact capacity for blood flow delivery, with important downstream consequences affecting end-organ functionality. Organs not receiving adequate blood flow with decreased oxygen delivery may malfunction, or develop poorly, leading to long-term complications. There can also be consequences following treatment of heart disease in the developing, immature human infant or child while organs are in a vulnerable, at risk state. Even in cases that are deemed successfully treated by current standards, residual hemodynamic disturbances may persist which can exert either acute, overt changes or indolent, subclinical alterations in end-organ performance. Chromosomal or genetic anomalies influence multiple developing cell lines and often result in abnormalities of both the cardiac and noncardiac systems. The most commonly associated major noncardiac anomalies were musculoskeletal (24%), anomalies of the urinary tract (14%), gastrointestinal system (11%), and central nervous system (11%) (4). Such a child would also be at risk for a multitude of additional noncardiac consequences, including dysmorphology, neurodevelopmental delay, musculoskeletal abnormalities, and a host of other organ system abnormalities. These findings have their origin in the nondisjunction of chromosome 21, resulting in the constellation of findings recognized as Down syndrome. Patterns of phenotypic findings may recur in various patients suggesting an association, although a genetic explanation may not be all that clear.
Zyloprim 100mg with mastercard
Situs ambiguus describes an uncertain or indeterminate visceral or atrial position medicine vs nursing discount 300 mg zyloprim visa, usually because the structures have taken on a symmetrical or indeterminate anatomic form bilaterally. A common example of this symmetry is seen in patients with abdominal situs ambiguus. These individuals will have a liver that is "bilateral" (equally occupying both the right and left upper quadrants) and is in a midline position. Both lobes of these bilaterally symmetrical livers will resemble a "normal" right lobe and these patients commonly will have absence of the spleen (asplenia). Heterotaxia is the term used to describe a constellation of anomalous viscera situs and related groups of complex cardiovascular malformations. Variations from the normal (situs solitus) in heterotaxy are expressed as randomization (situs ambiguus), bilateral symmetry (mirror images), or as complete reversal of visceral position (situs inversus). They further reported that familial heterotaxy occurs with autosomal dominant, recessive, P. Both situs ambiguus and situs inversus can appear in some families with heterotaxy. A and D are examples of dextrocardia; B and E, mesocardia; and C and F, levocardia. Note that in hearts with mesocardia and two well-developed ventricles, there are two relatively well-defined ventricular apices (B) (usually straddling the midline), but the major axis of the heart is directed inferiorly, and the apex of the ventricular septum lies in the midline. Images are similar to echocardiographic short-axis scans of the abdomen from a subcostal transducer position. The basic types of visceral atrial situs are demonstrated: situs solitus (A), situs inversus (B), and situs ambiguus with asplenia (C) and polysplenia (D). However, these vessels lie on the same side of the vertebral column in situs ambiguus with asplenia (C). Sequential Segmental Approach to Cardiac Diagnosis A segmental approach implies a systematic and therefore sequential review of all structures involved in the congenital cardiovascular anomalies. Therefore, a more practical clinical and pathologic segmental analysis begins with definition of major organ positions (visceral situs, atrial situs, and cardiac position/orientation), followed by a detailed description of four segments and the three connections between them. This approach should be applied regardless of the method of examination being used (any clinical imaging technique or a pathologic examination). The pancreas and spleen are generally located on the same side of the vertebral column as the stomach. Atrial and visceral situs often are considered together because they are usually concordant (the atrial and visceral situs are the same). Situs ambiguus may be best defined as an uncertain or indeterminate situs (organ positions do not fit into any standard category). In visceral situs ambiguus with right isomerism (bilateral right sidedness), the spleen is usually absent (asplenia) and the liver is centrally located, symmetrically straddling the midline. Situs ambiguus with polysplenia has been described as bilateral left sidedness or left isomerism (5,6,7,8,9,10,11,12). However, the degree of right/left symmetry is less pronounced in these patients, compared to that seen in asplenia and bilateral right sidedness. In fact, the most common arrangement of the abdominal viscera in polysplenic patients is situs inversus. As a teaching tool, the concept of isomerism (mirror-image sidedness) is an attempt to simplify the typical features of complex anomalies in which multiple abnormalities tend to occur together. Thus, the asplenia syndrome (Ivemark syndrome) appears as a pathologic grouping of features emphasizing right sidedness, such as bilateral right bronchi and bilateral right (trilobed) lungs, bilateral right atria, and a symmetrical liver. The frequencies represent a compilation of cases reported by multiple investigators (13,14,15,16). As a result, in the case of bilateral right-sided symmetry, the spleen would not be expected to develop -hence the association of right isomerism with asplenia. In contrast, left isomerism is frequently associated with polysplenia, although multiple spleens are usually found on only one side of the vertebral column (along the dorsal aspect of the stomach). Cardiac Atria Clinically, the identification of the morphologic right atrium is important for establishing atrial situs. As a result, its walls are relatively smooth and lack distinctive features for identification by clinical imaging modalities. In contrast to a left atrium, a morphologic right atrium will have a large pyramidal appendage, a crista terminalis, and pectinate muscles (14). In situs ambiguus and other complex cases, the atrial septum can essentially be absent, resulting in a common atrium. In these cases, assignment of atrial "identity" can be challenging and often must rely on secondary, associated features. Anatomic determinants of the other cardiac segments also have been described and are summarized in Table 51. Even more rarely, in polysplenia syndrome with left atrial isomerism, both atrial appendages and free walls may resemble a left atrial appendage. However, in most cases with asplenia or polysplenia, the atrial anatomy is poorly defined, with a large common atrium, a thin rudimentary remnant of atrial septum, anomalies of systemic and pulmonary venous connections, and abnormal, but similarly shaped bilateral appendages. Pathologic specimen illustrating the anatomic features of the morphologic right and left atrial appendages with left juxtaposition. With incorporation of the sinus venosus, the coronary sinus also can be recognized as a reliable marker for the morphologic right atrium. This approach allows clinical assignment of atrial situs in most cases, although the most important clinical issues are often related to the position and spatial arrangement of the venoatrial connections rather than the morphologic identities of the atria themselves. The Lungs Pulmonary situs is determined by the sidedness of the morphologic right and left lungs. In contrast, a morphologic left lung is characterized by a pulmonary artery that courses over the main bronchus and posterior to the upper lobe bronchus. In the setting of pulmonary isomerism (both lungs having the same morphology), however, the ratio approaches unity, because the lengths of the two main bronchi are similar. Pathologic specimen (A) and drawing (B) illustrate normal tracheobronchial branching pattern as observed anteriorly. This anatomic feature predicts pulmonary visceral situs based on measurements of the bronchial length. For example, atria and ventricles should be described both by their morphology and their right or left sidedness. Mesocardia is characterized by a vertical midline septum with side-by-side ventricles. After the morphology and position of the cardiac segments are determined, the manner in which they connect to one another is evaluated. The difficulties encountered in the accurate definition of atrial situs based on atrial anatomy alone emphasize the importance of accurate determination of systemic and pulmonary venous connections, as described in Tables 51. This determination is particularly important for surgical management and should be a routine part of any imaging study. As covered elsewhere in this chapter, an evaluation of this segment should incorporate descriptions of the ventricular locations, relationships, function, and morphology, as well as the anatomy of the ventricular septum and any septal defects. Great Artery Relations the great arterial connections, the spatial relationships between the arteries and their subsequent distribution/branching patterns, must be determined as described in Table 51. Eight basic types of great artery relationship are possible based on the aortic and pulmonary valve positions at the level of the semilunar valves. Directly posterior aorta this type of segmental approach to complex cardiovascular malformations allows prediction of all possible cardiac conditions that could be encountered.
Generic zyloprim 300 mg mastercard
As opposed to other conotruncal abnormalities symptoms underactive thyroid purchase zyloprim 100mg without a prescription, transposition of the great arteries is rarely associated with chromosomal abnormalities (9), although infrequent reports of associations with chromosomal genetic syndromes exist (10). Moreover, unlike other conotruncal abnormalities, extracardiac associations are less frequent (10%) than with other conotruncal outflow tract abnormalities (33%) (11). It is however, associated with dextrocardia (10) and lateralization defects, for example, heterotaxy syndrome, particularly asplenia or right isomerism (10,12). Familial recurrence was previously not felt to occur in patients with transposition of the great arteries. However, in a multicenter study from Italy, the recurrence rate was found to be 1. Noninherited and Environmental Risk Factors Diabetes and Vitamin A have been the most studied modifiable maternal risk factors contributing to transposition of the great arteries. Pregestational diabetes is positively associated with transposition of the great arteries (17,18,19,20). Hyperglycemia has been found to be a major teratogen with regard to transposition of the great arteries (21), and some of these effects can be reversed with treatment with Vitamin E (21,22). High maternal intake of supplemental Vitamin A may significantly increase the risk of having offspring with transposition of the great arteries (23). Maternal exposure to ibuprofen (20), influenza (20), organic solvents (20), and pesticides (24) have all been reported to increase the risk specifically for transposition of the great arteries, in addition to other congenial heart defects. Morphogenesis the embryologic basis of transposition of the great arteries is less well understood than other conotruncal abnormalities. Unlike other conotruncal abnormalities, neural crest ablation does not result in transposition of the great arteries (25). In embryonic development, normally, the aorticopulmonary septum develops a spiral-like configuration resulting in the pulmonary trunk twisting around the ascending aorta. There are two main proposed theories for the embryologic basis for transposition of the great arteries. One theory, the "straight conal septal" theory (26) proposes that there is lack of spiral rotation of the aorticopulmonary septum. The other theory, first proposed by Goor and Edwards (27) and substantiated by Anderson et al. Normally in embryonic development, the subpulmonary conus grows while the subaortic conus undergoes resorption. In embryos that develop transposition of the great arteries, the subaortic conus enlarges, while the subpulmonary conus is resorbed (27,28,29). The aorta is thus positioned anterior and rightward with the pulmonary artery being posterior and leftward. High-dose retinoic acid, by inducing hypoplasia of the conus swellings, may be a primary event with resultant lack of counterclockwise rotation of the distal outflow tract, that leads to transposition of the great arteries (30,31,32). Perlecan-deficient embryos have been shown to exhibit transposition of the great arteries and it is hypothesized that this is due to hyperplastic conotruncal endocardial cushions from excess mesenchymal cells causing disorganized spiral endocardial ridges (33). Morphology Pathologic Anatomy, Variants and Conduction Anatomy the morphology in transposition of the great arteries can be most aptly described as an abnormality of ventriculoarterial connection. The fundamental abnormality involves the presence of a discordant ventriculoarterial connection. As such, the arterial trunks arise from the morphologically inappropriate ventricle, that is, the right ventricle is predominantly aligned with the aorta, while the left ventricle is predominantly aligned with the pulmonary artery. While this arrangement most typically results in the aorta being anterior and rightward, while the pulmonary artery is posterior and leftward, it is important to note that it is not the arrangement of the great arteries in space that defines transposition of the great arteries, but rather the connection of the great arteries to their respective ventricles. Historically, the term transposition had been loosely applied to a wide variety of congenital anomalies in which the great artery arrangement in space was abnormal regardless of connection to the ventricular mass (34). In addition, rare forms of transposition of the great arteries can have a great artery arrangement that resembles the normal arrangement in space. It is also important to note that the term transposition of the great arteries should not be applied to patients with additional abnormalities of atrioventricular connection. It is worthy of mention that the same fundamental abnormality of discordant ventriculoarterial connection can be encountered in the mirror image arrangement of normal, that is, with situs inversus. The conduction system in "simple" transposition of the great arteries discussed in this chapter is generally normal. In transposition of the great arteries with a ventricular septal defect with fibrous continuity between the tricuspid and pulmonary valves leaflets, the conduction system is posterior and inferior to the defect (35). The conduction system is posterior and lateral to the tricuspid valve orifice if straddling or overriding of the tricuspid valve is present (35). Associated Lesions the most common associated lesions in transposition of the great arteries are the presence of a ventricular septal defect, with or without additional presence of left ventricular outflow tract obstruction. In the newborn, the presence of a foramen ovale and ductus arteriosus is expected, and as such these two are not considered associated lesions. A common type of ventricular septal defect encountered in transposition of the great arteries includes direct fibrous continuity between the tricuspid and pulmonary valve, that is, a perimembranous ventricular septal defect. In the setting of transposition of the great arteries, this type of ventricular septal defect is often also referred to as conoventricular. Another common type of ventricular septal defect encountered in transposition of the great arteries is the so-called malalignment type of ventricular septal defect, characterized by the malalignment between the outlet septum and the remainder of the muscular ventricular septum. Malalignment of the outlet septum can occur posteriorly toward the pulmonary outflow tract, and in this manner is responsible for one of the common mechanisms of left ventricular outflow tract obstruction. However, anterior deviation of the outlet septum can also occur, resulting in some degree of override of the pulmonary valve over the right ventricle. A less common type of ventricular septal defect in transposition of the great arteries is the muscular defect, which can be located in the inlet, outlet, apical, or mid-muscular septum, and can sometimes be multiple. Less common types still include those so-called "canal type" of inlet ventricular septal defects included within the spectrum of atrioventricular septal defects with the associated abnormalities of the atrioventricular junction and atrioventricular valves, and sometimes associated with straddling of the tricuspid valve in transposition of the great arteries. The least common type is the so-called doubly committed subarterial ventricular septal defect, in which both semilunar valves are in direct fibrous continuity with each other, and characterized by the absence of muscular outlet septum in this area. Of the types of ventricular septal defects encountered in transposition of the great arteries, only muscular ventricular septal defects and perimembranous ventricular septal defects have the potential for becoming smaller over time or even spontaneously closing. The mechanisms responsible for left ventricular outflow tract obstruction in transposition of the great arteries are numerous, and include obstruction at the level of the pulmonary valve itself, as well as several causes of obstruction at the subpulmonary region, which include posterior malalignment of the outlet septum, tissue tags, muscular ridges, and anomalous insertion of the mitral valve apparatus (35). Precise characterization of the mechanism responsible for subpulmonary obstruction is paramount, because the ability to resect the cause of obstruction is central to the ability to perform an arterial switch operation. Type A, the most common coronary distribution, with the left circumflex coronary artery and left anterior descending coronary artery from the left posterior facing sinus and the right coronary artery from the right posterior facing sinus. Type C, separate close origins of the left and right coronary arteries from the posterior facing sinuses (often with intramural courses). Type E, circumflex coronary artery from right posterior sinus and left anterior descending and right coronary artery from the left posterior facing sinus. The frequency of these variants occurs in that order, with transposition of the great arteries with intact ventricular septum by far the most common, comprising more than 50% of these combinations (36). One rare associated abnormality that deserves special mention is juxtaposition of the atrial appendages, which in transposition of the great arteries most often consists of left juxtaposition of the right atrial appendage (37). Although this anomaly, in and of itself, is inconsequential to the physiology of transposition of the great arteries and does not impact directly on the surgical repair options (although it may affect a Senning operation), it is important that this anomaly be recognized using echocardiography (see "Echocardiography" section) at the time of diagnosis of transposition of the great arteries and may have implications when performing a balloon atrial septostomy (see "Balloon Atrial Septostomy" section). Lastly, coronary anomalies are so common in transposition of the great arteries that they may not typically be considered to constitute associated lesions as such. The highly variable origins of the coronary arteries as well as their variable epicardial course is the subject of much study. Various classifications of coronary branching patterns have been described, of which the Leiden convention (38) and Yacoub and Radley-Smith classification. The "type A" or normal coronary distribution is the most common branching pattern, but abnormal coronary branching patterns can be seen in up to one-third of patients (40). The essence of the circulatory derangement in transposition of the great arteries is that the systemic and pulmonary circulations are arranged in parallel rather than in series. The left ventricle, which receives fully oxygenated blood from the pulmonary veins, pumps this oxygenated blood through the pulmonary valve into the lungs, where it cannot possibly pick up any more oxygen. Similarly, the right ventricle, which receives deoxygenated blood from the systemic veins, pumps this deoxygenated blood across the aortic valve back to the body, where it cannot deliver much oxygen to the body.

Cheap 100 mg zyloprim
The neonate with critical aortic stenosis is an important class of patients that warrants a separate discussion when considering the surgical options for valvar stenosis symptoms vaginal yeast infection order 300 mg zyloprim amex. The first decision that must be made in cases of critical aortic stenosis in a neonate is whether the left-sided heart structures are adequate for a two-ventricle circulation. This decision can be difficult, and a key point to be stressed is that an assessment of left heart structures in aggregate, as opposed to a focus on any one anatomic feature, is necessary in order to determine the best treatment course. While the equation did not perform quite as well in a follow-up validation study, it was still able to correctly predict outcome in 76% of patients (248). In the validation study, the authors developed a new equation, which included aortic valve annulus z-score, left ventricle to long axis of the heart ratio, and presence of significant endocardial fibroelastosis. Likely more important than the specifics of each equation is the concept that a complex interaction between multiple left-sided structures determines whether a left ventricle will be suitable for a biventricular repair. If a patient is not felt to be a candidate for biventricular repair, stage I single ventricle palliation is indicated (discussed in detail in Chapter 46). If a two-ventricle repair is possible, then balloon valvuloplasty, surgical valvotomy, or less often, primary neonatal Ross procedure are all acceptable options. Both surgical valvotomy and balloon valvuloplasty can achieve good early results with low mortality in the current era (223,249,250). While the need for reintervention may be more common among patients undergoing initial balloon valvuloplasty, the need for eventual valve replacement is comparable between groups with overall freedom from valve replacement just over 50% at 20 years (223). Open valvotomy and balloon valvuloplasty are likely both reasonable options; the crucial decision is whether to pursue a two-ventricle repair at all. Evidence suggests that centers may have a tendency to inappropriately favor two-ventricle repairs in borderline cases with negative consequences on survival (251). Subvalvar Aortic Stenosis the surgical approach to repairing subvalvar aortic stenosis depends greatly on the type of obstruction present. As discussed previously, a discrete fibrous membrane is most common, present in 70% to 80% of cases (36). Repair in these instances involves relatively straightforward membrane resection, a low-risk procedure with early mortality between 1% and 2% (252,253,254). Some evidence suggests that aggressive early repair using a peak gradient of 40 mm Hg as an indication for surgery may spare the aortic valve from injury and development of insufficiency (255), while other studies suggest that early resection does not prevent subsequent valve leakage (256). Risk factors for membrane recurrence include increased peak gradient at the time of diagnosis (51,255,257), early age at diagnosis (255,257), and distance <5 mm between membrane and aortic valve (259). While survival outcomes are still generally excellent despite the increased complexity of these repairs, recurrent obstruction with the need for reoperation is more common, occurring in 15% to 50% of patients (254,257,260). Among all patients with subaortic stenosis, a recent meta-analysis estimated a 20% risk for reoperation at 10 years (36). Supravalvar Aortic Stenosis the initial repairs of supravalvar aortic stenosis utilized a single patch to enlarge the noncoronary sinus and relieve the obstruction (261). While this technique did successfully relieve the stenosis, it also resulted in distortion of the aortic root and valve. Both multiple sinus techniques aimed to avoid distortion of the aortic root and valve, and there is evidence that multiple sinus reconstruction reduces mortality, residual stenosis, occurrence of significant aortic regurgitation, and the need for reoperation when compared to the original single patch technique (16). Overall, survival outcomes are inferior to those of valvar and subvalvar stenosis, with 3% to 9% early mortality, 86% to 96% survival at 10 years, and 77% survival at 20 years (16,17,263). The rate of reoperation is also significant, cited as high as 34% at 20 years (16). If diffuse stenosis is present, additional patching of the ascending and transverse aorta may be necessary (264). The coronary arteries must be carefully assessed both with preoperative imaging P. As discussed previously, aortic valve pathology is common in the setting of supravalvar aortic stenosis, and concomitant repair or replacement of the aortic valve occurs in up to 40% of supravalvar stenosis repairs (16,76,83,263). Finally, concomitant severe central or proximal branch pulmonary artery stenosis is generally patched at the time of aortic stenosis repair, while significant distal branch pulmonary artery stenosis is ideally addressed percutaneously prior to surgery (265). Bicuspid aortic valve: inter-racial difference in frequency and aortic dimensions. Prevalence and associated risk factors for intervention in 313 children with subaortic stenosis. Forty-one years of surgical experience with congenital supravalvular aortic stenosis. Coordinating tissue interactions: Notch signaling in cardiac development and disease. Extracellular matrix remodeling and organization in developing and diseased aortic valves. American College of Cardiology/American Heart Association Task Force on Practice G, Society of Cardiovascular A, Society for Cardiovascular A, et al. Incidence and echocardiographic features of congenital unicuspid aortic valve in an adult population. A clinical and anatomic study of 47 patients with emphasis on its relationship to mitral insufficiency. Paediatric subvalvular aortic stenosis: a systematic review and meta-analysis of natural history and surgical outcome. Rheologic genesis of discrete subvalvular aortic stenosis: a Doppler echocardiographic study. Development of a subaortic membrane after surgical closure of a membranous ventricular septal defect in an infant. Tunnel subaortic stenosis: left ventricular outflow tract obstruction produced by fibromuscular tubular narrowing. Subaortic obstruction after the use of an intracardiac baffle to tunnel the left ventricle to the aorta. Subaortic fibrous ridge and ventricular septal defect: role of septal malalignment. Echocardiographic assessment of subvalvular aortic stenosis before and after operation. Echocardiographic, morphologic, and geometric variations of the left ventricular outflow tract: possible role in the pathogenesis of discrete subaortic stenosis. A developmental complex including supravalvular stenosis of the aorta and pulmonary trunk. Spontaneous intracerebral hemorrhage and multiple infarction in Williams-Beuren syndrome. Pathology of coronary arteries, myocardium, and great arteries in supravalvular aortic stenosis. Surgical management of congenital obstruction of the left main coronary artery with supravalvular aortic stenosis. Sudden death in supravalvular aortic stenosis: fusion of a coronary leaflet to the sinus ridge, dysplasia and stenosis of aortic and pulmonic valves. Atresia of the proximal left coronary artery associated with supravalvular aortic stenosis. Obstruction to left coronary artery blood flow secondary to obliteration of the coronary ostium in supravalvular aortic stenosis. Left ventricular subendocardial ischemia in severe valvar and supravalvar aortic stenosis. Congenital aneurysm of the left ventricle associated with supravalvular aortic stenosis and aneurysm of the left main coronary artery: case report and review of the literature. A case of hypoplastic left heart syndrome and bicuspid aortic valve in monochorionic twins. In a thorough review, Prakash and colleagues provide a summary of the current understanding of the genetic basis of bicuspid aortic valve, as well as a roadmap for future investigation with discussion of potential diagnostic and therapeutic implications. Inheritance analysis of congenital left ventricular outflow tract obstruction malformations: segregation, multiplex relative risk, and heritability. Murine Jagged1/Notch signaling in the second heart field orchestrates Fgf8 expression and tissue-tissue interactions during outflow tract development. Inhibition of calcifying nodule formation in cultured porcine aortic valve cells by nitric oxide donors. Response of the fetal heart to changes in load: from hyperplasia to heart failure. Shear stress regulates endothelial nitric oxide synthase expression through c-Src by divergent signaling pathways.
Purchase zyloprim american express
Parent- versus child-reported functional health status after the fontan procedure treatment narcissistic personality disorder cheap zyloprim 300 mg with mastercard. Matthew Baillie in 1797 (1), transposition of the great arteries was for decades merely known as a fascinating disease that was universally fatal. Patients who were initially felt to have a fatal disease can now be expected not only to survive, but also to have an excellent quality of life. Indeed, the innovations in therapy over the years for patients with transposition of the great arteries became the basis for many advances in technology in the disciplines of interventional cardiology and cardiac surgery. The left ventricular outflow tract obstruction in (C) is caused by posterior malalignment of the muscular outlet septum, but other causes of left ventricular outflow tract obstruction in this setting can occur (see text). These lesions encompass transposition of the great arteries with intact ventricular septum, transposition of the great arteries with ventricular septal defect, and transposition of the great arteries with ventricular septal defect and left ventricular outflow tract obstruction. Other forms of transposition of the great arteries, for example, congenitally corrected transposition of the great arteries or transposition of the great arteries in association with other lesions, such as double outlet right ventricle, are discussed elsewhere in this text. Early estimates from the Report of the New England Regional Infant Program (5) reported the incidence of transposition of the great arteries to be 218 per million live births. A more recent meta-analysis from 41 studies estimated the incidence to be a median of 303 and mean of 315 per million live births (6). Etiology Genetic Transposition of the great arteries is predominately seen in males (particularly large-term males). After being pumped to the body, the even more deoxygenated blood returns to the right ventricle, and is once again pumped to the body. According to this construct, one can see that within just a few heartbeats, the right ventricle would be pumping blood that is essentially devoid of oxygen, while the left ventricle keeps recirculating fully oxygenated blood to , and from, the lungs. Clearly survival with the systemic and pulmonary circulations arranged in parallel is not possible, and requires some blood to exit the pulmonary circuit in order to enter the systemic circuit, and for blood to similarly exit the systemic circuit in order to enter the pulmonary circuit. Any blood exiting one circuit to enter the other would result in one circulation emptying itself into the other; there must therefore be an equal flow returning blood back to the original circuit. The levels of communication that allow blood to cross from one circuit to the other can occur either centrally at the atrial (atrial septal defect or patent foramen ovale), ventricular (ventricular septal defect), or great artery level (patent ductus arteriosus), or can occur peripherally at the naturally existing shunts at the level of the bronchial circulation and thebesian veins. In order to correctly describe the intricacies of this highly variable physiology, it is important to recall some basic definitions, which will first be illustrated using simpler forms of congenital heart disease, and then be applied to the understanding of transposition of the great arteries. A left-to-right shunt is defined as the flow of blood which has already completed its circulation to the lungs, and yet is being sent to the lungs once again without having seen the systemic circulation, while a right-to-left shunt represents the flow of blood that has already completed its course through the systemic circulation, and yet is being circulated once more to the systemic circulation without seeing the pulmonary circulation. In transposition of the great arteries specifically, the terms "left-to-right shunt" or "right-to-left shunt" can be confusing, and some authors have attempted to avoid confusion by distinguishing the terms "physiologic left-toright shunt" from "anatomic left-to-right shunt. This will become clear as we discuss what precisely constitutes the "shunted" blood in transposition of the great arteries. It is therefore inaccurate in the setting of transposition of the great arteries to describe flow occurring from the left atrium to the right atrium across a foramen ovale as a left-to-right shunt, although some authors might use the term " anatomic left-to-right shunt" because it is occurring from a left-sided anatomical structure to a right-sided anatomical structure (certainly, all would agree that this does not constitute a physiologic left-to-right shunt). In addition, it can be seen that the terminology "anatomic shunt" breaks down when describing a shunt between the aorta and the pulmonary artery: Normally the aorta is considered a left-heart structure and the pulmonary artery a right-heart structure, but in transposition of the great arteries, the aorta is connected to the right ventricle and the remainder of the right heart. Does that make the aorta an anatomic right-heart structure, while the pulmonary artery becomes a left-heart structure This becomes confusing, and it is therefore best to avoid the terms "anatomic left-to-right shunt" and "anatomic right-to-left shunt," in favor of describing the actual chambers or vessels that allow communication between them and the manner in which the flow occurs between these structures. Similarly when interpreting hemodynamic cardiac catheterization data in these patients, it is important to understand the limitations in this situation and to interpret the data in the context of "transposition physiology" discussed in this section. When considering a newborn baby with transposition of the great arteries, the foramen ovale is expected to be available for shunting, as is the ductus arteriosus in the first few minutes or hours of life. Hence, the two parallel circuits consisting of the pulmonary and systemic circulations are expected to have two possible areas of communication between them in almost every newborn with transposition of the great arteries. Hence, immediately after birth the pulmonary vascular resistance is elevated, and accordingly it is possible for the ductus arteriosus to have flow occur bidirectionally, typically from pulmonary artery to aorta in systole, and from aorta to pulmonary artery in diastole. This phenomenon is responsible for the classic "reversed differential cyanosis" seen in newborns with transposition of the great arteries. It is important to note that this phenomenon is a fleeting one, typically lasting only the first few hours of life. The two conditions necessary for the presence of this phenomenon are patency of the ductus arteriosus, and elevation of the pulmonary vascular resistance. The systolic flow of blood from pulmonary artery to aorta brings highly oxygenated blood from the pulmonary artery to the descending aorta to result in relatively higher saturations in the lower extremities compared to the upper extremities. However, within the first few hours of life as the pulmonary vascular resistance drops precipitously, there will cease to be systolic flow from pulmonary artery to aorta across the ductus, and eventually the flow across the ductus will entirely be from aorta to pulmonary artery throughout the cardiac cycle. When this occurs, differential cyanosis disappears, and with it an important bedside clinical clue to the presence of transposition physiology. The increased flow across the ductus arteriosus from aorta to pulmonary artery caused by the drop in pulmonary vascular resistance also results in increased pulmonary venous return to the left atrium. The relative increase in left atrial pressure causes the foramen ovale to flow from the left atrium to right atrium. This physiologic set up is the justification of two of the most important strategies for treatment of newborns with transposition of the great arteries: the institution of a prostaglandin infusion to maintain patency of the ductus, and the performance of a balloon atrial septostomy to enlarge the foramen ovale. It is a common misconception that the ductus and foramen are necessary to improve "mixing" in transposition of the great arteries. In fact, it is not mixing back-andforth across these structures, but rather net flow across these structures (from aortic to pulmonary artery, and from left atrium to right atrium) that is occurring during this physiologic state in transposition of the great arteries (41). After a septostomy has been performed, the systemic arterial saturation typically increases tremendously, such that prostaglandin can frequently be discontinued. In the setting of a closed ductus, the patient then relies essentially on the atrial defect that has been created via balloon atrial septostomy to maintain adequate oxygen saturation. In this physiologic state, the flow of blood across the atrial septal defect occurs bidirectionally, thus it is perfectly accurate to describe the atrial septal defect as being responsible for improving "mixing. Associated lesions such as ventricular septal defects, pulmonary stenosis, or both, add additional complexity to the physiology of transposition of the great arteries. Accordingly, the saturations will generally be higher in patients with transposition of the great arteries with ventricular septal defect. In patients with transposition of the great arteries, ventricular septal defect, and pulmonary stenosis, the pulmonary stenosis, especially if severe, will significantly limit pulmonary blood flow and contribute to lower oxygen saturation. Clinical Features and Investigation Presentation and Symptoms the clinical features of children with transposition of the great arteries depends on the anatomic details of the lesion. In addition, the clinical features depend on the age of presentation, which in most cases is the newborn period, but in developing countries, late presentation can occur. Newborns with transposition of the great arteries and intact ventricular septum present with cyanosis. Inadequate atrial and ductal communications result in profound cyanosis and lethargy. Patients with left ventricular outflow tract obstruction and a ventricular septal defect may present with profound cyanosis and lethargy if severe left ventricular outflow tract obstruction is present, or heart failure symptoms if little obstruction is present. Mild cyanosis with no symptoms may be present in infants with a "well-balanced" degree of left ventricular outflow tract obstruction. However, "reverse" differential cyanosis, for example, oxygen saturation higher in the lower extremities than upper extremities, may be present in newborns with transposition of the great arteries and a patent ductus arteriosus with pulmonary hypertension or coarctation of the aorta/interrupted aortic arch. Compromise in systemic perfusion, manifested by cool extremities and hypotension may be present if little mixing is present. A harsh holosystolic murmur is heard at the left lower sternal border and is more evident as the pulmonary vascular resistance drops, along with a diastolic rumble at the apex. In the presence of left ventricular outflow tract obstruction, a harsh systolic ejection murmur of varying intensity depending on the degree of obstruction is heard at the left sternal border. Biventricular hypertrophy may be seen particularly in cases of left ventricular outflow tract obstruction or significant left ventricular volume overload. Pulmonary vascular markings correlate inversely to the severity of left ventricular outflow tract narrowing in patients with transposition of the great arteries, ventricular septal defect and left ventricular outflow tract obstruction.
Discount zyloprim 300mg with mastercard
Laboratory Evaluation Initial evaluation typically involves a broad laboratory investigation in most cases premonitory symptoms discount zyloprim 300mg mastercard. Patients may have elevated white blood cell counts, inflammatory markers, and liver enzymes, none of which are specific to the diagnosis of myocarditis (75). Troponin T and I levels may also be elevated as a marker of cardiac damage, but absence of increased troponin does not rule out myocarditis (79,80). Use of troponin levels have been suggested for differentiation of cardiac and noncardiac causes of pediatric chest pain, with nearly half of patients with elevated troponin levels ultimately diagnosed with cardiac disease, including 27% with myocarditis (81). However, another study found only low yield of identifying cardiac disease with use of screening during initial infectious workup in patients without cardiac symptoms (82). For pediatric patients with cardiac dysfunction of unknown etiology, a cut-off troponin T level of 0. Another study found higher troponin T and I levels in myocarditis patients compared to controls and higher levels were associated with more severe disease and mortality (79), although other studies have failed to find the same association with higher mortality (62,83). In adults, high-sensitivity troponin T was higher in myocarditis patients with positive histology and evidence of viral genome in endomyocardial tissue, but was not predictive of death or transplant (84). Antibodies to cardiac proteins, such as to myosin and beta-adrenergic receptors, have been demonstrated in animal models of myocarditis and antibody levels were found to be elevated in adults with myocarditis (42,43). However, the prognostic use of cardiac antibodies in children is not known and availability of antibody assays remains mainly experimental (87). B: Ventricular tachycardia as the presenting rhythm in a 9 year old with myocarditis. D: Left axis deviation and left bundle branch block in a 16 year old with severely decreased function and dilation due to myocarditis. Conduction abnormalities range from first-degree heart block to complete heart block, requiring permanent pacemaker placement in patients with refractory disease. Other findings include pulmonary edema, pulmonary infiltrate, or pleural effusion (75). However, cardiomegaly may not be seen in myocarditis patients who present with acute coronary-like symptoms (65). Echocardiographic Findings Although there are no specific echocardiographic features of myocarditis, an echocardiogram is usually obtained to assess ventricular function and left ventricular dilation, as each of these P. An echocardiogram may also reveal an associated pericardial effusion or intracavitary thrombi, which have been noted in a number of patients with myocarditis (93). The common echocardiographic findings include ventricular dysfunction, dilation, and changes in wall thickness or wall motion abnormalities. Echocardiographic imaging can assist with distinguishing fulminant myocarditis from acute (nonfulminant) myocarditis (94). Patients with acute myocarditis usually have normal wall thickness, and may have left ventricular dilation. In contrast, those with fulminant myocarditis usually have markedly decreased systolic function, with normal chamber size and may have increased ventricular septal thickness due to myocardial edema (94). Ventricular dysfunction is not uniformly present, but may be global or regional (95). Right ventricular dysfunction has also been noted to be an independent predictor of adverse outcome in patients with biopsy-confirmed myocarditis (97). Diastolic dysfunction, including abnormal tissue velocities and strain, has been reported in children with acute myocarditis, even in the setting of normal systolic function (98). However, the pattern and prominence of diastolic dysfunction in children and adults over long-term follow-up has not been well described. Thus, it provides important information regarding these factors that have prognostic value in myocarditis. Various pulse sequences have been validated to evaluate the characteristic findings in myocarditis. T2-weighted imaging is used to evaluate the presence of myocardial edema (103,104). This sequence is somewhat prone to artifacts that may decrease specificity, although several studies have confirmed its diagnostic merit (103). Areas of myocardium with fibrosis or scar retain gadolinium contrast, thereby revealing areas with increased accumulation of gadolinium as bright regions. In the setting of clinically suspected myocarditis, these criteria specify the quantitative assessment of edema on T2-weighted images. Regional or global myocardial signal intensity is increased in T2-weighted images (indicating myocardial edema) 2. Increased global myocardial early gadolinium enhancement ratio between myocardium and skeletal muscle in gadolinium-enhanced T1-weighted images (indicating hyperemia/capillary leak) 3. Instead, these classifications are based on the clinical course rather than imaging (or biopsy) findings (105). In 1987, the "Dallas criteria" were described and remain the standard histologic criteria for myocarditis, consisting of inflammatory cellular infiltrate and cardiac myocyte necrosis and/or degeneration not typical of coronary artery disease or other etiology (113). Histologic findings are described as (1) acute myocarditis with inflammation and myocyte damage, (2) borderline myocarditis with inflammation but absence of associated cellular damage, and (3) no myocarditis, although evidence of chronic myocarditis with ongoing inflammation and scar tissue formation can also be observed (38). Differences in interobserver expert interpretation of histopathologic samples and apparent lack of correlation P. In light of the available diagnostic tools and associated limitations, Sagar et al. Probable acute myocarditis is associated with cardiovascular symptoms in addition to any of the previous findings in subclinical disease. Treatment Activity Restrictions According to the 2005 Bethesda guidelines, patients with myocarditis should be restricted from all competitive sports for 6 months after diagnosis (118). These recommendations are based largely on the rate of myocarditis found in athletes with sudden death as mentioned above (70,71). Murine models of coxsackie myocarditis have also shown increased mortality with exercise compared to wild-type mice (119), although no comparable human studies have been performed. Medical Management Myocarditis is mainly treated with supportive and symptomatic care. For patients with symptomatic heart failure, treatment should follow standard therapy as outlined by American College of Cardiology and American Heart Association guidelines (120). For patient with severe symptomatic dysfunction, including cardiogenic shock, use of inotropic support or even mechanical circulatory support may be necessary. Another study of 216 pediatric patients diagnosed with myocarditis found milrinone use in 45% and epinephrine in 35% of patients (121). Reported use of mechanical ventilator support has ranged from 37% to 54% in children (76,77,121). Similarly, aldosterone-receptor antagonist use in mice with experimental myocarditis was associated with less fibrosis, especially with earlier initiation of treatment (125). Calcium channel blockers were associated with decrease in inflammatory cytokines (126) and increased survival in mice, possibly through effects on production of nitric oxide (127,128). Whereas carvedilol has been associated with positive anti-inflammatory and antiviral effects in murine models of myocarditis (129,130), metoprolol was associated with a less robust response and worse outcomes in some studies (131,132,133). In a study of adults with suspected myocarditis, lack of beta-blocker therapy was associated with a greater risk for death or transplant (134). Rhythm control of associated atrial and ventricular arrhythmias is important for attaining stability in the acute and chronic phase. However, use of digoxin is not recommended due to prior evidence of worsening viral myocarditis in murine models with increased mortality and inflammatory cytokines in treated mice, especially at higher doses (136). In a review of 40 children with complete heart block secondary to myocarditis, 27% required permanent pacemaker placement for prolonged heart block, but 67% had resolution on an average of 3. A small series of children with fulminant myocarditis found frequent associated arrhythmias during the acute illness, but complete resolution of rhythm abnormalities in survivors at follow-up, including complete heart block (139). Immunomodulators, Immunosuppression, and Antiviral Therapy Antiviral Therapy As a viral infection is thought to be the cause of the majority of myocarditis, antivirals have been proposed as a therapeutic option in patients with an identified causative agent.
Buy zyloprim overnight
Schools must be involved by creating an improved environment for both eating and physical activity symptoms liver disease order discount zyloprim. Individual Approach the individual approach is directed at identifying children and adolescents who are at higher risk of future cardiovascular disease and treating them to lower their risk. This approach is probably most important from the standpoint of the pediatrician and the pediatric cardiologist. Identification To initiate the individual high-risk strategy, it is necessary to identify those children who are at higher risk of cardiovascular disease. This approach is directed at identifying children who are likely to have genetic dyslipidemias, who are at highest risk. The use of this score is dependent on all adults having their risk factors including cholesterol measured on a regular basis. To construct a similar risk score for children would require large-scale longitudinal studies with complete follow-up in which risk factor levels are measured in childhood and subjects are followed until the occurrence of cardiovascular end points in adulthood. It is likely that this approach will miss 30% to 60% of pediatric patients with elevated cholesterol (155,156,157). Difficulties with using the family history as a trigger for screening include that the family history may be incomplete or inaccurate. In addition, parents (and sometimes grandparents) of younger children are often too young themselves to have reached the age when they are at greatest risk for a myocardial infarction or a stroke (157). These problems with a targeted approach to screening have led to the recommendation of universal screening of all children at 9 to 11 years of age (158). In addition, children aged 2 years or older should have a lipid profile if they have a family history of premature cardiovascular disease (prior to age 55 in men or age 65 in women) or of dyslipidemia or with other cardiovascular disease risk factors, such as diabetes, hypertension, or obesity (90). This use across a broad age range is recommended despite the fact that there is considerable variation of cholesterol with age during growth and development. However, it has been shown that the proposed single cutpoints work well in practice (161). Dietitians can be helpful both in providing education about the fat and cholesterol content of foods and in providing behavioral strategies that improve the likelihood that the recommended diet will be adopted by the family and the pediatric P. Parents can promote improvement in diet by making healthful foods available in the home and restricting the availability of foods that are high in energy density, fat, saturated fat, cholesterol, and simple sugars (162). Research has supported the concept that children will choose to eat foods that are available (163,164). It is important for children to try new foods multiple times to develop familiarity with and ultimately have a preference for these foods. A minimum of 8 to 10 exposures to new foods may be required before preference for these foods increases and is established (165,166). This involved sessions with the family from 4 to 12 times per year over a 3-year period (169). It is encouraging that a 7-year follow-up showed that the intervention effect was maintained and that growth and development continued to be normal in the intervention group (169). This emphasizes the concept that these changes can be made in practice in a safe and effective manner. Plasma cholesterol reduction of 7% to 15% has been reported using these compounds in a spread (173,174). Simvastatin the long-term safety and efficacy have not been established in children. Unfortunately, adherence with these medications is often limited because they are difficult for children to take. The tablet forms are more palatable, but the tablets are large and difficult for some children to swallow (176,177,178). The safety and efficacy of colesevelam has been evaluated in a clinical trial of pediatric patients with heterozygous familial hypercholesterolemia (179). There were no important adverse effects, and adherence to the medication regimen was good. Inhibitors of Cholesterol Absorption Ezetimibe works by blocking cholesterol absorption in the gastrointestinal tract. In adults, ezetimibe is used primarily in combination with statins to achieve additional cholesterol lowering. This appears to be true of both primary prevention (prevention of an initial myocardial infarction) and secondary prevention (prevention of subsequent myocardial infarctions) (184,185,186). A Cochrane review of the use of statins in primary prevention of cardiovascular disease has been published (187). They evaluated 14 randomized controlled clinical trials including more than 34,000 participants. There is also some concern about the cost-effectiveness of statins for primary prevention of cardiovascular disease. Several studies have been performed to evaluate the safety and efficacy of statins in children and adolescents (175,188,189,190,191,192,193,194). There have also been studies of stains that have evaluated vascular structure and function as endpoints. The side effects of statin agents are an increase in hepatic transaminases and elevation of creatine kinase. Statins have also been associated with myositis, which can progress to rhabdomyolysis. If symptoms of abnormal muscle aches or cramps are present, then creatine kinase should be measured and the medication should be discontinued. A recent meta-analysis of adult patients taking statins has demonstrated a small but measurable increase in risk of type 2 diabetes mellitus in those taking statins, particularly at higher doses (195). Once such pediatric patients are identified, appropriate dietary treatment should be implemented. Hypertension Epidemiology Blood pressure elevation is established as an important risk factor for the development of cardiovascular disease in adults. In the Framingham study, elevated blood pressure is associated with increased incidence of myocardial infarction, cerebrovascular disease, left ventricular hypertrophy, and congestive heart failure (197). A 10-mm Hg increase in systolic blood pressure is associated with a 20% increase in risk of cardiovascular events in adults aged 35 to 64 years (198). In adults, it is estimated that 92% to 95% of cases of hypertension are due to essential hypertension (199). High blood pressure in children and adolescents is based on percentile values as opposed to a single cutpoint, which is used for adults. For pediatric patients, the 95th percentile based on previous large epidemiologic studies is used to define high blood pressure. The prevalence of hypertension has been previously estimated to be 1% to 3% for children and adolescents (202). More recent estimates have placed the prevalence at approximately 5% (203,204,205). It appears that average blood pressure may be increasing across the pediatric population over time. These results emphasize that abnormal weight gain and obesity are pivotal factors in blood pressure elevation in children and adolescents (209). Birth Weight and Blood Pressure Barker (210) has proposed that birth weight is an important determinant of blood pressure elevation later in life. They found that lower birth weight and greater weight gain between age 1 and 5 years were correlated with higher blood pressure at age 22. Tracking In general, there is a continuous rise in blood pressure from infancy through adolescence. This means that those with higher blood pressures at one age would also tend to be higher later in life. Longitudinal studies have shown that blood pressures do tend to track over time for children and adolescents (67,213).