Purchase 400 mg skelaxin otc
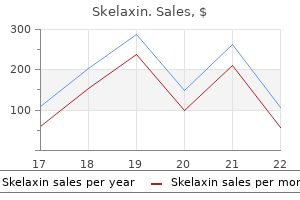
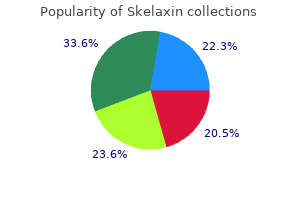
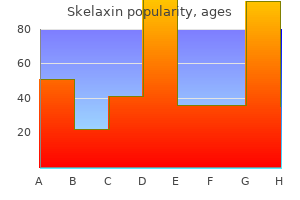
The influx of water into the middle ear may cause extreme vertigo and lead to a diving disaster muscle relaxant ibuprofen discount skelaxin 400mg on line. Associated barotraumatic injuries should be considered when the diagnosis of barotitis media is made. Management and Disposition Treatment includes decongestants and appropriate analgesia. If a diver descends without equalizing pressure by exhaling through the nose, significant negative air pressure will exist inside the mask. The net result may include rupture of capillary beds, leading to conjunctival hemorrhage and skin ecchymosis. A thorough eye examination should be performed and ophthalmologic consultation considered if warranted. Special consideration should be given to patients with anticoagulant use or recent keratotomy, as corneal incisions heal relatively slowly. Management and Disposition Treatment consists of ascent and essentially supportive care. Stingrays are not typically aggressive and the majority of envenomations are defensive in nature. Injuries typically involve the lower extremity if the animal is stepped upon or upper extremity if the animal is handled. Fatal injuries have been reported from chest trauma, which may result in perforation of the myocardium. Stingray envenomation occurs when a reflexive and forceful forward thrust of the caudal spine or spines of the animal impacts the victim, producing a puncture wound or laceration. The force of injection causes the integumentary sheath covering the spine to be driven into the wound, fragmenting and potentially releasing venom, mucus, pieces of the sheath, and spine fragments deep within the wound. The initially dusky or cyanotic wound may progress to erythema, with rapid fat and muscle hemorrhage. Systemic symptoms may include nausea, vomiting, diarrhea, diaphoresis, muscle cramps, fasciculations, weakness, headache, vertigo, paralysis, seizures, hypotension, and syncope. Management and Disposition the wound should be irrigated immediately and primary exploration accomplished to remove any visible debris. After soaking, wounds should be formally explored, debrided, and dressed for delayed primary closure or primary closure with drainage. Stingrays often dwell on the ocean floor and may burrow into the sand, leading to envenomation by accidentally stepping on the animal. The coloring of the stingray tends to blend with the ocean floor, leading to injury from inadvertent stepping on the stingray. A radiograph should be obtained after debridment to rule out retained foreign body. Patients can usually be discharged home after a 3- to 4-hour observation period if no systemic symptoms arise. Aggressive debridement is of primary importance in managing stingray wounds, as retained foreign bodies are a common problem. Antibiotics chosen should include coverage of staphylococci, streptococci, and Vibrio species. Stingrays like to burrow into the sand on the ocean floor, making them very difficult to see and easy to inadvertently step on. This envenomation occurred after the fisherman inadvertently caught a stingray and was envenonmated taking the animal off the hook. Long, brittle, venom-filled spines or specialized jaw-like appendages (pedicellariae) are responsible for the injury. Other echinoderms, notably the crown of thorns starfish, may also cause injury via similar mechanisms. The spines frequently break and pedicellariae can remain attached and active for several hours. They may advance into muscle or joint spaces and cause infection or injury from the venom itself. Multiple envenomations may produce systemic symptoms including nausea, vomiting, abdominal pain, paresthesias, numbness, paralysis, hypotension, syncope, or respiratory distress. While the envenomation causes a reaction that may be quite painful, deaths, though reported, are exceedingly rare. Retained spines often dissolve spontaneously; however, granulomas may form, producing locally destructive inflammation. Antibiotics may be useful in certain cases, and tetanus prophylaxis should be addressed. The majority of urchins are nonvenomous and only cause injury from puncture wounds. Their spines may break off in the victim, resulting in a high likelihood of infection. This x-ray is of a patient who was reaching into a rock crevasse in the ocean and experienced sudden sharp pain. Note the retained sea urchin spine in the fifth digit adjacent to the proximal phalanx. Note the multiple puncture wounds on the foot of a patient who accidentally stepped on a sea urchin in shallow water. Some species of sea urchin contain dye, which may give the false impression of a retained spine. Sea urchins known to be hazardous to humans are generally found in the Indian Ocean, Pacific Ocean, and Red Sea. Envenomations from fire urchins, while extremely painful, are seldom if ever fatal. This diverse group includes hydrozoans (eg, Portuguese man-of-war, stinging hydrozoans, and fire coral), scyphozoans (ie, "true" jellyfish), and anthozoans (ie, soft corals, stony corals, and anemones). The important species involved in human injuries have stinging cells called nematocysts. Nematocysts are enclosed in venom sacs and are present in tentacles that hang from air-filled structures. After external contact, the nematocysts are discharged from their sacs, often penetrating the skin, and release their venom. Nematocyst venom is an extremely complex substance containing numerous proteins and enzymes. Clinical presentation following envenomation ranges from the mild dermatitis to cardiovascular and pulmonary collapse. Mild envenomations usually result in a self-limited papular inflammatory eruption associated with burning and limited to areas of contact. Moderate to severe envenomations produce a spectrum of neurologic, cardiovascular, respiratory, and gastrointestinal symptoms. Anaphylactoid reactions-including hypotension, dysrhythmias, bronchospasm, and cardiovascular collapse- may occur, resulting in unexplained drownings. Similar to fire coral, contact with stinging hydrozoan results in local burning pain followed by erythematous papules or urticarial eruptions and blisters. After contact, fire coral most commonly causes immediate local burning pain, followed by erythematous papules or urticarial eruptions. The hypotonic nature of fresh water, as well as isopropyl alcohol, may cause additional nematocysts to fire and should be avoided. A 5% solution of acetic acid (vinegar) applied for at least 30 minutes is the most widely accepted mechanism for inactivating nematocysts. It has been suggested to remove tentacles with the application of shaving cream, followed in 5 minutes by a careful scraping with a firm, dull object (eg, tongue blade, credit card). Any victim with systemic symptoms requires at least 6 to 8 hours of observation because rebound phenomena are common. The box jellyfish (Chironex fleckeri) is generally considered the most deadly of marine animals and is most predominant in Australian and Southeast Asian waters. The detached tentacles of some species may contain active nematocysts for months, even when fragmented on the beach or floating in water.
Cheap skelaxin american express
For example spasms prostate discount skelaxin 400 mg, the excision of skin snips for the diagnosis of onchocerciasis, the collection of rectal snips for the diagnosis of schistosomiasis, and punch biopsy of skin lesions for the identification and culture of cutaneous and mucocutaneous species of Leishmania are simple procedures, but the diagnosis can be missed if the specimens are improperly obtained or processed. Intestinal helminths provoke eosinophilia only during pulmonary migration of the larval stages. Eosinophilia is not a manifestation of protozoal infections, with the possible exceptions of those due to Isospora and Dientamoeba fragilis. Like the hypochromic, microcytic anemia of heavy hookworm infections, other nonspecific laboratory abnormalities may suggest parasitic infection in patients with appropriate geographic and/or environmental exposures. Biochemical evidence of cirrhosis or an abnormal urine sediment in an African immigrant certainly raises the possibility of schistosomiasis, and anemia and thrombocytopenia in a febrile traveler or immigrant are among the hallmarks of malaria. Commercial kits for the detection of antigen by enzyme-linked immunosorbent assay or of whole organisms by fluorescent antibody assay are now available for several protozoan parasites (Table 112-8). Despite these specific limitations, the restricted geographic distribution of many tropical parasites increases the diagnostic usefulness of both the presence and the absence of antibody in travelers from industrialized countries. Despite major efforts at vaccine development and vector control, chemotherapy remains the single most effective means of controlling parasitic infections. However, efforts to combat the spread of some diseases are hindered by the development and spread of drug resistance, the limited introduction of new antiparasitic agents, and the proliferation of counterfeit medications. This chapter deals exclusively with the agents used to treat infections due to parasites. Specific treatment recommendations for the parasitic diseases of humans are listed in subsequent chapters. The pharmacology of the antiparasitic agents is discussed in great detail in Chap. Table 113-1 presents a brief overview of each agent (including some drugs that are covered in other chapters), along with its major toxicities, spectrum of activity, and safety for use during pregnancy and lactation. Food and Drug Administration but are considered investigational for the treatment of certain infections; these drugs are marked accordingly in the table. Rare: hepatitis, seizures, angioneurotic edema, StevensJohnson syndrome, tinnitus Occasional: abdominal cramps, diarrhea, biliary colic, transient headache Frequent: rash, pruritus, nausea, leukopenia, paresthesias Diarrhea, abdominal cramps (usually mild and transient) Occasional: pseudomembranous colitis, abdominal pain, diarrhea, nausea/vomiting. Rare: rash, seizures, severe skin reactions (toxic epidermal necrolysis, erythema multiforme, StevensJohnson syndrome) Occasional: urticaria. Occasional: hemolysis, methemoglobinemia, neuropathy, allergic dermatitis, anorexia, nausea, vomiting, tachycardia, headache, insomnia, psychosis, hepatitis. Rare: agranulocytosis Rare: neutropenia, thrombocytopenia Frequent: nausea/ vomiting, brown urine. Rare: optic neuritis, peripheral neuropathy, seizures, encephalopathy Occasional: fever, pruritus, headache, myalgias. Rare: agranulocytosis, peripheral neuropathy Occasional: nausea, vomiting, diarrhea, abdominal pain. Rare: psychosis, convulsions, hypotension Frequent: myocardial injury, encephalopathy, peripheral neuropathy, hypertension. Rare: seizures (all are reversible and dose-related) Occasional: abdominal pain, diarrhea. Rare: anaphylaxis Warfarin: effect enhanced by metronidazole Disulfiram: psychotic reaction Phenobarbital, phenytoin: accelerate elimination of metronidazole Lithium: serum levels elevated by metronidazole Cimetidine: prolonged halflife of metronidazole See metronidazole B Yes C Yes No major interactions C No information Paromomycin Amebiasis,b D. Rare: fever, chills, arthralgias, headaches Frequent: abdominal pain, diarrhea, dizziness, headache, malaise. Occasional: yellow-orange discoloration of skin, sclerae, urine; begins after 1 week of treatment and lasts up to 4 months after drug discontinuation. Moore this chapter deals exclusively with the pharmacologic properties of the agents used to treat infections due to parasites. Specific treatment recommendations for the parasitic diseases of humans are listed in the chapters on those diseases. Single-dose albendazole therapy in humans is largely without side effects (overall frequency, 1%). Thus, when prolonged use is anticipated, the drug should be administered in treatment cycles of 28 days interrupted by 14 days off therapy. Although rapidly absorbed, amodiaquine behaves as a prodrug after oral administration, with the principal plasma metabolite monodesethylamodiaquine as the predominant antimalarial agent. Severe adverse events can occur, albeit rarely (1 case in 2000 treatment courses), with amodiaquine administration. Agranulocytosis and hepatotoxicity can develop with repeated use; therefore, this drug should not be used for prophylaxis. While highly injurious to nematodes, this fundamental disruption of cellular metabolism also offers treatment for a wide range of parasitic diseases. Poor absorption may be advantageous for the treatment of intestinal helminths, but successful treatment of tissue helminth infections. Although they have been used for almost 100 years, their mechanism of action against Leishmania spp. This form inhibits trypanothione reductase, a critical enzyme involved in the oxidative stress management of Leishmania spp. The drugs are taken up by the reticuloendothelial system, and their activity against Leishmania spp. Sodium stibogluconate is the only pentavalent antimonial available in the United States; meglumine antimonate is principally used in francophone countries. Although low-level unresponsiveness to Sbv was identified in India in the 1970s, incremental increases in both the recommended daily dosage (to 20 mg/kg) and the duration of treatment (to 28 days) satisfactorily compensated for the growing resistance until around 1990. There has since been a steady erosion in the capacity of Sbv to induce long-term cure in patients with kala-azar who live in eastern India. Foremost among the many factors that have probably contributed to this failure is the provision of suboptimal treatment for years, which led to the development of drug resistance among parasites. Sodium stibogluconate is available in aqueous solution and is administered parenterally. This slower phase may be due to conversion of pentavalent antimony to a trivalent form that is the likely cause of the side effects often seen with prolonged therapy. A combined formulation of artemether and lumefantrine has been developed for the treatment of acute uncomplicated falciparum malaria in areas where Plasmodium falciparum is resistant to chloroquine and antifolates. This agent exhibits potent activity against toxoplasmosis and babesiosis when used with pyrimethamine and azithromycin, respectively. The drug is active against both the erythrocytic and the exoerythrocytic stages of Plasmodium spp. Malarone is a fixed-dose combination of atovaquone and proguanil used for malaria prophylaxis as well as for the treatment of acute, uncomplicated P falciparum malaria. Malarone has been shown to be effective in regions with multidrug-resistant P falciparum. Absorption after a single oral dose is slow, increases twoto threefold with a fatty meal, and is dose-limited above 750 mg. Because of the potential for drug accumulation, the use of atovaquone is contraindicated in persons with severe renal impairment (creatinine clearance rate <30 mL/min). No dosage adjustments are needed in patients with mild to moderate renal impairment. These agents are at least 10-fold more potent in vivo than other antimalarial drugs and presently show no cross-resistance with known antimalarial drugs; thus, they have become first-line agents for the treatment of severe falciparum malaria in some areas where multidrug resistance is a major problem. Artemether appears to be effective for the treatment of schistosomiasis and is being evaluated for communitybased treatment programs. The artemisinin compounds are rapidly effective against the asexual blood forms of Plasmodium spp. The drug is extensively metabolized; only 5% of the dose is excreted unchanged in the urine. Fasciola hepatica uses fumarate reduction coupled to rhodoquinone for anaerobic energy metabolism. Bithionol competitively inhibits electron transfer to fumarate by rhodoquinone; the result is impaired anaerobic energy metabolism and trematode death. Bithionol is parasite specific for two reasons: (1) Fumarate reductase catalyzes the reverse of the reaction of mammalian succinic dehydrogenase in the Krebs cycle. However, because it exhibits extensive tissue binding, a loading dose is required to yield effective plasma concentrations. The mean half-life of chloroquine is 4 days, but the rate of excretion decreases as plasma levels decline, making once-weekly administration possible for prophylaxis in areas with sensitive strains. About half of the parent drug is excreted in urine, but the dose should not be reduced for persons with acute malaria and renal insufficiency.
Buy skelaxin 400mg otc
Although the incidence has declined spasms right side under ribs buy skelaxin 400 mg free shipping, acute iron poisoning remains a significant cause of pediatric morbidity and mortality. The toxic dose depends upon the quantity of elemental iron in the preparation, which in turn depends upon the iron formulation. While the minimum toxic dose remains controversial, ingestion of more than 40 mg/kg elemental iron may result in toxicity, while ingestion of more than 60 mg/kg elemental iron is associated with severe morbidity and possible mortality. Whole-bowel irrigation has been advocated for substantial ingestions and for patients with evidence of iron tablets on abdominal radiographs. Levels obtained more than 6 hours after ingestion are unreliable due to tissue redistribution. Patients with evidence of iron toxicity (eg, persistent vomiting, acidosis, altered mental status, and hypotension) or a 4- to 6-hour postingestion serum level more than 500 mcg/dL should receive chelation with deferoxamine. Acute iron ingestion and the risk for toxicity must be assessed based upon the quantity of elemental iron ingested, not the total amount ingested. The absence of radiopaque materials on abdominal radiographs is not a reliable indicator to exclude potential iron toxicity; liquid and pediatric (chewable) formulations are not typically radiopaque. Despite the potential for anaphylactoid reactions and hypotension, patients requiring chelation therapy should receive deferoxamine via the intravenous route. A rare example of the progression of coloration of vin rose urine (from the excreted ferrioxamine complex) over 15 hours of chelation with deferoxamine is shown. Other possible exposures may occur from occupational exposures, retained lead bullets in synovial fluid, jewelry, lead-painted toys, fishing weights, ceramic glazes, and cosmetics. Severe lead poisoning in adults has also been associated with ingestion of contaminated moonshine. Neurotoxicity may range from subtle personality changes to encephalopathy and cerebral edema. At the societal level, even small lead burdens are associated with statistically significant decreases in intelligence quotient. Motor neuropathy such as foot drop and wrist drop may be seen in adult patients, especially after occupational exposure. Microcytic anemia may occur and basophilic stippling of the red cells may be seen. Abdominal pain may be described by patients but, unlike other heavy metal poisonings, constipation is more likely than diarrhea. Radiographic "lead lines," bands of increased density on long bones metaphyses, may be seen in young children. These densities are not due to deposition of lead but rather increased calcium deposition. Management and Disposition Whole-blood lead level is the primary measure of lead exposure, but is not usually available in real time. Radiographic studies may demonstrate radiopaque substances from ingested jewelry or paint chips in children. Chelation with oral succimer is currently recommended in asymptomatic children with levels between 45 and 70 mcg/dL. Reducing the exposure in children is paramount to treatment and the source of the lead may be elusive. Workers in a lead dust environment will bring home the lead dust on their clothes and shoes. Imported eye cosmetics with lead have been a source of pediatric exposures in certain ethnic groups. Azarcon and greta are lead-based remedies that are used to treat diarrheal illnesses. Adults usually require much higher blood lead levels than children before encephalopathy occurs. This patient presented with acute encephalopathy after ingesting lead-based, tangerinescented gloss glaze used for making pottery. Basophilic stippling along with a microcytic anemia may be seen in patients with chronic lead poisoning. The increased radiographic densities on the metaphyseal growth plates demonstrate radiological growth retardation and increased calcium deposition. Elemental mercury poisoning is associated with inhalation of volatilized mercurial ions, which may occur after vacuuming or heating. Acute interstitial pneumonitis may occur and may progress to severe lung injury and death. Inorganic mercury poisoning usually occurs from the ingestion of the mercurial salts. Organic mercury poisoning occurs from ingestion of short-chain alkyl mercurial compounds. Methylmercury distributes into brain tissue and causes neurologic disease such as ataxia, paresthesias, visual difficulties, movement disorders, and speech difficulties. If elemental mercury was injected intravenously, mercurial emboli may be seen in the lungs. Local injection in the skin may demonstrate mercury deposition in the soft tissues. For inhalational injury due to elemental mercury, respiratory support may be required. Ingestion of inorganic mercury may lead to early cardiovascular collapse as a result of the severe volume depletion. Elemental mercury toxicity has occurred when it is heated and used to extract gold from jewelry. Though this may be seen from intentional intravenous mercury injection, this patient absorbed the mercury intravenously following an accident involving multiple shattered thermometers. Organic mercury is eliminated via the fecal route, so urine samples for methylmercury will not be reflective of the body burden. Although faded with age, the coffin-shaped tablets contain the word "poison" on one side and the "skull-andcrossbones" on the other. While many species of mushrooms can cause toxicity when ingested, only a few contain amatoxins and account for most fatalities attributed to mushroom ingestion. Examples include Amanita phalloides (the "death cap") and Amanita ocreata (the "destroying angel") species. Amatoxin poisoning results in severe symptoms of gastroenteritis at least 6 to 24 hours after ingestion. Ingestions result in an acute nausea, vomiting, and diarrhea that occurs within 2 hours of ingestion (eg, <6 hours of ingestion). Examples of mushrooms include the Chlorophyllum molybdites which looks like a toasted marshmallow in the grass. Other types of mushroom poisonings include gyromitrin-containing mushrooms that are misidentified for the popular morels. Gyromitrin mushrooms cause status epilepticus that is responsive to high-dose pyridoxine. Coprine-containing mushrooms only cause toxicity when ethanol is co-ingested as they cause a disulfiram reaction. Be wary of using the "6-hour rule" with mushroom scavengers who may have ingested multiple species of mushrooms. The "death cap" produces amatoxins and accounts for most of the fatalities due to mushroom ingestion. For the amatoxin containing mushroom, administration of activated charcoal may be recommended depending on the time since ingestion. These mushrooms were samples of Amanita ocreata provided by a family who had ingested them and subsequently developed significant hepatotoxicity. Coprinus mushroom cause toxicity when ethanol is co-ingested, resulting in a disulfiram-like reaction. Morels are considered a delicacy; however, inexperienced mushroom hunters may collect a "false morel" which contains gyromitrin. Ingestion of gyromitrin results in status epilepticus that is responsive to intravenous pyridoxine. The patient typically presents with acute nausea vomiting less than 2 hours after ingestion. Nausea, vomiting, abdominal pain, confusion, depression, and fatigue may be present. Headaches, paresthesias, weakness, scotomas, and visual color disturbances (yellow halos around lights) may also be seen. Ventricular tachydysrhythmias have been treated with phenytoin or lidocaine when digoxin-specific Fab fragments are not available.
Purchase on line skelaxin
Third letter-designates pacemaker response to sensed electrical activity: T: triggered-fires even when beat sensed muscle relaxant no drowsiness 400 mg skelaxin amex, I: inhibitory-holds when beat sensed, D: dual-atrial triggered and ventricle inhibited D. The resulting "rumbling" baseline may have large or indiscernibly small amplitude. Thus, ventricles depolarize variably creating varying R-R intervals and an "irregularly irregular" pattern. Most "irregularly irregular" rhythms are due to atrial fibrillation, but other rhythms may produce similar findings. Therapy is geared toward either rate control of the ventricles or rhythm control and cardioversion (chemically or electrically). Synchronized cardioversion may be indicated if a patient is unstable, but the risk of clot embolization must be carefully considered when planning nonemergent electrical cardioversion of atrial fibrillation. The baseline "rumble," representing "F waves," may be very fine or even indiscernible. Flutter waves appear in a rapid sine wave or "sawtooth" pattern, usually in the inferior leads. Atrial activity in lead V1 often appears as rapid P waves at a rate approximating 300 bpm. A ventricular rate of 140 to 160 bpm should prompt consideration of the possibility of atrial flutter with 2:1 block. The flutter waves (arrows marking every other flutter wave) may be mistaken for P and T waves. When irritated by stretching, medications, or certain acute medical conditions, these foci compete in pacing the atria. R-R intervals are regular (double arrows), differentiating this from fine atrial fibrillation. Ventricular rates of 140 to 160 bpm should prompt consideration of atrial flutter with a 2:1 block. The R-R interval is regular, except for one pause, when characteristic atrial flutter waves are apparent (arrowhead). Ventricular flutter is treated as ventricular tachycardia and usually leads to ventricular fibrillation if not promptly corrected with antiarrhythmic medications or electrical cardioversion. Torsades is treated as a ventricular tachycardia, usually requiring defibrillation. The orientation of the heart in the chest cavity is reversed with the predominant electrical activity moving left to right (as opposed to right to left). Normally placed precordial leads in a patient with dextrocardia are actually placed over the thinner right ventricle instead of the left ventricle. No one system is adequately sensitive and specific enough to warrant exclusion of all others. The left atrium depolarizes after the right atrium and therefore has the most effect on the second portion of the P wave. The right atrium depolarizes before the left atrium and therefore has the most effect on the first portion of the P wave. The ventricular myocardium hypertrophies abnormally, either concentrically or focally. This syndrome was first described in individuals who experienced sudden cardiac death with structurally normal hearts, but congenitally abnormal ion channels in myocyte cell membranes have been associated with the disease. Consultation with a cardiologist is recommended for electrophysiological testing and intracardiac defibrillator placement. This may lead to unopposed ventricular stimulation through the accessory tract and may worsen the tachycardia. They may be indirectly caused by systemic circulatory issues such as hypoperfusion. Defibrillation and many medications may be ineffective in the hypothermic patient. Acute treatment for hyperkalemia includes insulin and glucose, sodium bicarbonate, and -agonists in an attempt to drive potassium into the cell. Intravenous calcium may be used to stabilize the myocardium but has no effect on serum potassium levels. These are temporizing measures which must be followed by definitive treatment of the underlying problem, which may include the need for dialysis. With large emboli, increased resistance to pulmonary arterial flow produces right ventricle overload and dilation. Pericardial effusion should be suspected in the setting of a sinus tachycardia and low voltage. A physiologically significant pericardial effusion compresses the heart, and affects the ability of the heart to fill properly. Initial treatment of physiologically significant pericardial effusion is with intravenous fluid bolus to increase preload. Pericardiocentesis should be reserved for hemodynamically threatening effusions due to a high associated morbidity. Electrical alternans is often best seen in the anterior precordial leads V3 and V4. Bradydysrhythmias, various heart blocks, especially with findings consistent with increased automaticity (atrial tachycardia with block, atrial fibrillation with slow ventricular response, accelerated junctional rhythms). An acute overdose of a digoxin is usually associated with hyperkalemia which may increase the height of the T wave. Avoid calcium for treatment of hyperkalemia in the setting of digoxin toxicity as this may potentiate some adverse effects of digoxin. A "reversed" lead I with normal-appearing V leads strongly suggests accidental limb lead reversal as opposed to dextrocardia. The arm leads were indeed reversed, and correction produced a normal-appearing tracing. Longitudinal image of a gallbladder demonstrating gallstone, biliary sludging, and pericholecystic fluid. Basic information-transducer recommendations, scanning protocols, anatomic schematics-is presented within each application to represent both image acquisition and normal and pathological findings. Key Terms Sonographic windows-Anatomical locations on the body where an ultrasound probe is placed in order to view internal organs. Transducer indicator/probe marker/marker dot-Usually a bump or ridge on the ultrasound transducer that corresponds to a symbol on the ultrasound screen. Hypoechoic/anechoic-Used to describe objects on the ultrasound screen that are dark and therefore transmit sound waves. Echotexture-The characteristic appearance of specific organs when viewed using ultrasound. Transducer movements-When performing sonography, specific terms are used to describe characteristic movements of the transducer used to obtain the image desired. Transducers Emergency sonography is performed using a wide variety of transducers. Lower frequency transducers are used to visualize structures deep within the body, while higher frequency transducers allow better image resolution of superficial anatomic structures. The size and shape of transducers are also configured for imaging specific anatomic locations. The goal of this thoracoabdominal survey is to identify or exclude immediate life threats in the trauma or critically ill patient. Ideally, this is done using a single transducer that can image all three of these areas, but may result in some compromise of image quality and require the use of different probes for different components of the examination. It is recommended that all four views are evaluated for a complete exam, but isolated views may be obtained when indicated. It is important to note that these are not static "single" views, but a series of images obtained in each plane as the transducer is moved or "fanned" through the area of interest. Ultrasound transducer and probe marker positions for evaluation of pericardial fluid, hemoperitoneum, or pneumothorax. Pericardial (usually a subcostal/subxiphoid view- alternatively, one may obtain a parasternal long view of the heart if a subxiphoid view is unobtainable) 2. Pivot, sweep, and tilt the transducer as necessary to view all four cardiac chambers and pericardium. Identify the liver (if in view), heart, four cardiac chambers, and surrounding pericardium. The transducer is directed under the xiphoid process toward the left shoulder in a horizontal plane.
Generic skelaxin 400 mg mastercard
It may take 48 to 72 hours after the burn to assess correctly the degree of ocular damage spasms right side under ribs cheap skelaxin 400 mg without a prescription. The basis of such an evaluation is the size of the corneal epithelial defect, the degree of corneal opacification and extent of limbal ischaemia. Administration of steroids has been shown to delay stricture formation (in animals) when given within 48 hours of acid ingestion, but the practice is generally not recommended because of increased risk of perforation. In case it is embarked upon, the dosage recommended is 60 to 100 mg/day of prednisolone for the first 4 days, followed by 40 mg/day for the next 4 days, and finally 20 mg/day for the subsequent 7 to 10 days. Prophylactic use is not advisable unless corticosteroid therapy is being undertaken. Since there is often severe pain, powerful analgesics such as morphine may have to be given. The use of flexible fibreoptic endoscopy is now standard practice in the first 24 to 48 hours of ingestion to assess the extent of oesophageal and gastric damage. If there are circumferential 2nd or 3rd degree burns, an exploratory laparotomy should be performed. If the patient recovers, there may be long-term sequelae such as stenosis and stricture formation. Surgical procedures such as dilatation, colonic bypass, and oesophagogastrostomy may have to be undertaken. Some gastroenterologists utilise a "string marker" to keep the lumen open; others employ an intraluminal splint (silastic tubing) as an initial prosthesis. Forensic Issues Accidental poisoning may arise from mistaken identity since sulfuric acid resembles glycerine and castor oil. It is therefore imperative that it is stored in a distinctive bottle, clearly labelled, and kept in a safe place. In addition to routine viscera and body fluids, a portion of corroded skin should be cut out, placed in rectified spirit or absolute alcohol and sent for chemical analysis. Y Though sulfuric acid is commonly used (hence the term vitriolage which is derived from "oil of vitriol"), other acids are also employed. In fact any corrosive which is easy to hand may be used, including organic acids, alkalis, and irritant plant juices. Y Going by newspaper reports, vitriolage is a fairly common crime in India, though it is regarded as a serious offence (grievous hurt), and carries stiff punishment. Nitric acid is formed in photochemical smog from the reaction between nitric oxide and hydrocarbons. Individuals living in heavily polluted areas may receive chronic inhalation exposure to nitric acid. Workers in the following professions may be exposed to nitrogen oxides or nitric acid: glassblowing, engraving and electroplating, underground blasting operations, farming (silage and fertilisers), welding, fire fighting, and industrial chemistry. Therefore exposure to nitric acid potentially involves exposure to oxides of nitrogen, especially nitrogen dioxide. Mode of Action Nitric acid is a powerful oxidising agent and reacts with organic matter to produce trinitrophenol, liberating nitrogen monoxide (xanthoproteic reaction). Clinical Features the general picture is the same as in the case of sulfuric acid, with the following differences: 1. Inhalation of fumes can produce coughing, rhinorrhoea, lacrimation, dyspnoea, and pulmonary oedema. Pungent, dark brown heavy fumes will emanate if nitric acid is present in sufficient concentration. If an open bottle of concentrate ammonia solution is placed near the stomach contents or vomitus, copious white fumes of ammonium chloride will emanate. Though normal stomach contents contain hydrochloric acid, this is usually too dilute (0. Mistaking it for glycerine or castor oil, however is rare because it is a fuming liquid. Hydrofluoric Acid Physical Appearance Hydrofluoric acid is a colourless, fuming liquid. It is a unique acid, in that most of its toxicity is due to the anion, fluoride, and not to the cation, hydrogen. Iodine stains will be decolourised, while those due to nitric acid will deepen in intensity and turn to orange. Mode of Action Hydrofluoric acid burns result in severe progressive tissue and bone destruction, and excruciating pain. Unlike other inorganic acids, hydrofluoric acid rapidly traverses the skin barrier and invades deeper tissue planes. The fluoride ion then proceeds to affect tissue integrity and metabolism in 3 ways: 1. Characteristic features include severe pain and a predilection for the sub-ungual area. A hallmark of dermal exposure to low concentrations of hydrofluoric acid is pain that is out of proportion to the physical examination. Severity and timing of effects depends on the concentration, duration of exposure, and penetrability of the exposed tissue; pain may be delayed. The fluoride ion may cause decalcification and corrosion of bone beneath the area of dermal burn. Inhalation causes severe throat irritation, cough, dyspnoea, cyanosis, lung injury and noncardiogenic pulmonary oedema. Ingestion is associated with severe, burning pain followed by retching and vomiting. Obtain at least hourly serum electrolytes including serial total or ionised calcium, magnesium, and potassium levels. Total calcium may not reflect true hypocalcaemia, but usually has a more rapid turnaround. Several methods have been suggested to deactivate the injurious fluoride ion which is responsible for most of the serious manifestations of hydrofluoric acid poisoning. Options include milk (one-half to one glassful), chewable calcium carbonate tablets, or milk of magnesia. But it may * the ice retards diffusion of fluoride ion, while the magnesium or quaternary ammonium compound interacts with the ion to prevent invasion of deeper tissues. Addition of 10% calcium gluconate to the lavage fluid may provide some free calcium to bind the fluoride. The patient should be subsequently observed for signs of laryngeal oedema, pneumonitis, and pulmonary oedema. Local ophthalmic anaesthetic drops may be instilled to obtain patient compliance for the prolonged irrigation. The pH of the eye fluid should be periodically checked with litmus paper, and irrigation is continued until it is normal. Since this gel is not available in India, it has to be prepared by the physician by mixing 3. Similarly, local infiltration of magnesium sulfate or calcium gluconate are also not recommended today by several clinicians, though there are a few who still advocate their use. If it is decided to be done, a 10% solution should be injected with a 30 gauge needle in amounts no greater than 0. If fingers are involved, the brachial artery is cannulated; if the foot is involved, the femoral artery is cannulated. Therapeutic intervention to prevent development of elevated serum potassium is essential. Quinidine has been shown to be effective in preventing the K+ efflux from cells and preventing cardiotoxicity.
Pegwood (Wahoo). Skelaxin.
- What is Wahoo?
- Are there any interactions with medications?
- Constipation, indigestion, water retention, and other conditions.
- Are there safety concerns?
- How does Wahoo work?
- Dosing considerations for Wahoo.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96367
Buy skelaxin without a prescription
This plant grows well in India spasms right side order 400mg skelaxin mastercard, but its cultivation is banned except on license obtained from the central government, for growing the plant strictly for the pharmaceutical industry. Such a license is issued only for the states of Rajasthan, Uttar Pradesh, and Maharashtra. India produces 70 to 80% of opium that is used worldwide by pharmaceutical companies to manufacture several vital drugs including morphine, codeine, and pethidine. Unfortunately, a significant quantity of opium is funnelled clandestinely into a global smuggling racket which feeds the illicit drug trade flourishing in Western countries. It is minimally branched with leaves clasping the glabrous stem by their cordate base. Apart from these natural derivatives there are several other drugs used in pharmacotherapeutics which are either semisynthetic or synthetic analogues. Examples of other derivatives include alfentanil hydrochloride, alphaprodine, anileridine hydrochloride, diprenorphine, ethoheptazine, ketobemidone, meptazinol hydrochloride, methylfentanyl, pholcodine, remifentanil hydrochloride, and sufentanil citrate. When referring to these derivatives, there has always been confusion in terminology. While strictly speaking, the term "opiate" refers to natural and semisynthetic derivatives, and the term "opioid" is a more inclusive term applying to all agonists and antagonists with morphine-like activity, for the sake of convenience (and to avoid confusion), the former term will be used in this book as an umbrella-expression to cover all derivatives of opium-natural, semisynthetic, and synthetic. Uses Opiates have tremendous pharmacological importance, and are used for various therapeutic purposes (Table 13. Toxic Principles Opium obtained from the unripe fruit capsule contains a number of alkaloids which fall into two groups- Phenanthrene group: morphine, codeine, and thebaine. Section 5 Classification Partial agonist Agonist-antagonist Agonist - Agonist Agonist Agonist Agonist Agonist Agonist Agonist Agonist Agonist Agonist-antagonist Antagonist Antagonist Antagonist Agonist Agonist Agonist Agonist-antagonist Agonist Agonist Agonist Use Analgesic, pre-anaesthetic medication Analgesic Antitussive Antitussive Antidiarrhoeal Adjunct to anaesthesia - - - Analgesic Antidiarrhoeal Analgesic, treatment of heroin abuse and opiate abstinence syndrome Analgesic Analgesic Treatment of opiate poisoning Treatment of opiate poisoning Treatment of opiate poisoning and alcoholism Analgesic - Analgesic Analgesic Analgesic Analgesic Analgesic Table 13. Most of the clinically used opiates are relatively selective for m receptors reflecting their similarity to morphine. The s (sigma) receptor originally thought to be an opiate receptor is no longer considered to be opioid in nature since it is insensitive to naloxone, which is the most important characteristic of such receptors. However some opiates such as dextromethorphan and pentazocine are s receptor agonists. Stimulation of s receptor produces psychotomimetic effects and movement disorders (both of which have been reported with dextromethorphan and pentazocine). Two more receptors have been postulated to exist, but not demonstrated so far: e (epsilon) and z (zeta). Mu and delta receptors appear to be involved in systems that influence mood, reinforcing effects, respiration, pain, blood pressure, and endocrine and gastrointestinal functions. In human subjects kappa agonists appear to produce dysphoria, rather than euphoria. Respiration, which is controlled mainly through medullary respiratory centres with peripheral input from chemoreceptors and other sources, is affected by opiates which produce inhibition at chemoreceptors via mu opiates receptors and in the medulla via mu and delta receptors. However the effect of an oral dose is usually much less than that obtained on parenteral administratrion due to significant first-pass metabolism in the liver. Extent of protein-binding is variable depending on the exact nature of the opiate, and varies from 7% for codeine to 96% for buprenorphine. The major metabolic pathway of morphine is conjugation with glucuronic acid to produce morphine-6-glucuronide which is also pharmacologically active. Duration of action of opiates varies from 2 hours (pentazocine, pethidine) to 4 hours (morphine, codeine, heroin), to 8 hours (methadone, buprenorphine). Fentanyl, alfentanil, and surfentanil are ultra-shortacting (few minutes to 1 hour). Chapter 13 Somniferous Drugs Adverse Effects Respiratory depression, vomiting, vertigo, dysphoria, miosis, constipation, hypotension, urinary retention, and pruritis are commonly encountered. Pruritus is a common adverse event following the administration of opiates, particularly morphine sulfate. The triad of coma, pinpoint pupils, and respiratory depression is said to be almost pathognomonic for opiate poisoning. Such cases may be due to therapeutic overdose, accidental overdose (in addicts), or deliberate overdose (suicidal). Snoring prior to fatal opiate overdose has been reported and is likely due to a failure to maintain the patency of the upper airway. Non-cardiogenic pulmonary oedema ("heroin-lung") is an infrequent, but severe, complication of heroin overdose and is generally abrupt in onset (immediate-2 hours) following intravenous heroin overdose. Manifestations include rales, pink frothy sputum, significant hypoxia, and bilateral fluffy infiltrates on chest X-ray. Hyperkalaemia may occur following an overdose, especially in the presence of rhabdomyolysis and acute renal failure. If delivery occurs quickly following an opiate dose to the mother, or after adequate time has passed to allow for maternal clearance, it is unlikely that the foetus would be affected. Foetuses demonstrating significant distress and acidosis and whose mothers received opiates 1 to 3 hours prior to delivery, or multiple doses, may be at increased risk for respiratory depression, which would most likely be multifactorial in origin. The American Psychiatric Association has laid out diagnostic criteria for opiate dependence and for categorising the severity of such dependence (Table 13. Severity of Opiate Dependence Mild: few symptoms; mild impairment of social and occupational activities Moderate: intermediate between mild and severe Severe: many symptoms; marked impairment of occupational and social activities Partial remission: during past 6 months there has been some opiate use and some dependence symptoms Full remission: during past 6 months there has been no opiate use and no dependence symptoms Unexplained overspending. Compartment syndrome may occur following abuse of narcotic injections, such as heroin. Neonatal withdrawal may be seen in the infants of addicted mothers 12 to 72 hours after birth. Infants may be dehydrated, irritable, and experience tremors and cry continually and may have diarrhoea. In general the pulmonary artery wedge pressure should be kept relatively low while still maintaining adequate cardiac output, blood pressure and urine output. Activated charcoal is most effective when administered within one hour of ingestion. However, there is controversy regarding such a measure since physostigmine (unlike regular opiate antagonists) is a dangerous antidote with serious adverse effects. Dramatic reversal of the following features is achieved: miosis, respiratory depression, hypotension, coma. Sincetheeffectofa single bolus dose of naloxone is usually short-lived, repeated doses are required. Generally, if no response is observed after 10 mg has been administered, the diagnosis of opiate-induced toxicity should be questioned. Very large doses of naloxone (10 mg or more) may be required to reverse the effects of buprenorphine overdose. Some investigators state that a naloxone infusion is better than repeated injections. Naloxone can be diluted in normal saline or 5% dextrose, but should not be added in alkaline solutions. Caution should be exercised in reversing opiate toxicity in addicts because of the risk of precipitating withdrawal reaction. Naltrexone- Naltrexone is a long-acting opiate antagonist which can be administered orally. Dose: 50 mg/day orally, which may have to be continued for several weeks or months. Nalmefene- Nalmefene is a naltrexone derivative with pure opiate antagonistic effects, and has a longer duration of effect than naloxone in acute opiate poisoning. The use of drugs such as levorphanol and amiphenazole is no more recommended today. Convulsions may be treated with benzodiazepines in the usual manner (5 to 10 mg initially, repeat every 5 to 10 minutes as needed), though this is frequently not necessary if naloxone is available. If hypotension persists, administer dopamine (5 mcg per kg per min, progressing in 5 mcg per kg per min increments as needed), or noradrenaline (0. Prevention of rhabdomyolysis: Early aggressive fluid replacement is the mainstay of therapy and may help prevent renal insufficiency. Substitution therapy with methadone begun at 30 to 40 mg/day and then gradually tapered off. A beta adrenergic blocker like propranolol (80 mg) is said to be quite effective in relieving the anxiety and craving associated with opiate addiction, but has no effect on physical symptoms. Recent reports suggest favourable outcome with gabapentin combined with clonidine and naltrexone.
Purchase 400mg skelaxin with mastercard
The presence of hydronephrosis in the patient with renal colic is presumed to be a direct result of ureteral obstruction muscle relaxant easy on stomach buy cheap skelaxin 400mg on-line. There are no accurate means of determining the degree of obstruction by the presence of hydronephrosis. The coronal view allows the sonographer to visualize the right or left kidney from the superior to inferior poles. However, rather than focusing on the potential spaces of the peritoneum, attention is focused on the bladder and its contents. The transducer is directed as a coronal section through the body in the mid to posterior axillary lines. The liver, right kidney, renal cortex (with pyramids), and central renal sinus are seen. Alternatively, the patient may be placed in a prone position with the probe placed in the midscapular line and the transducer directed toward the abdomen. Identify the bladder (triangular in this view when fully distended), uterus (pear-shaped if present), prostate, seminal vesicles, and rectum. Begin scanning between the 9th and 11th ribs on the right and the 8th and 11th ribs on the left. Identify the liver, right kidney, renal cortex (with pyramids), and central renal sinus. Identify the spleen, left kidney, renal cortex (with pyramids), and central renal sinus. Moderate hydronephrosis is seen as dilatation of the bright renal sinus and secondary calyces by anechoic (black) fluid. Rotate the transducer 90 degrees counterclockwise to visualize the renal parenchyma and central renal sinus in a cross-sectional view. Urinary retention: By calculating the volume of the bladder, one may determine the presence of urinary retention. Identify the bladder (rectangular in this view when fully distended), uterus (oval hyperechoic structure if present), prostate, seminal vesicles, and rectum. Have the patient hold his or her breath in inspiration and move the transducer a rib space higher or lower to visualize the kidney from the superior to the inferior pole. The presence of a ureteral jet confirms the passage of urine into the bladder from a specific side. Findings Hydronephrosis: Dilatation of the bright renal sinus with black, anechoic fluid. Hydronephrosis is graded based on its extension into the secondary calyces and whether there is accompanying cortical thinning. Renal calculi: Bright hyperechoic oval/round structures within the cortex or renal sinus (acoustic shadowing is often present). Mild hydronephrosis does not involve the secondary calyces, moderate does, and severe hydronephrosis is accompanied by cortical thinning. With color flow doppler, uroliths will often demonstrate twinkling artifact deep to their reflective echogenic surface. The presence of a ureteral jet confirms the passage of urine into the bladder from a specific ureter. Ultrasound of pregnant patients is accomplished with two different scanning techniques: transabdominal and transvaginal. Pregnant patients presenting with abdominal pain or vaginal bleeding during the first trimester must be evaluated for the presence of an ectopic pregnancy. Identify the bladder, uterus, rectum, ovaries, and the rectouterine pouches (pouch of Douglas). The patient is supine and preferably in the lithotomy position for transvaginal views. The transducer should be inserted until it rests in the anterior fornix of the vagina. Abnormal Findings Free intraperitoneal fluid: Anechoic (black) bands of fluid located in the rectouterine pouch (pouch of Douglas). Ectopic pregnancy: Most commonly, an ectopic pregnancy is identified as an adnexal mass with an associated empty uterus. At times, an extrauterine gestational sac with or without a fetal pole may be seen. Some of the urinary bladder is seen deep and lateral (right on the image) to the uterus. The transducer is directed toward the anterior fornix in a line through the umbilicus (A); it is placed into the vagina (B). A gestational sac that is within the cornua or cervix of the uterus, although technically within the uterus, is still considered an ectopic pregnancy. A gestational sac within 5 to 7 mm of the border of the myometrium is concerning for interstitial ectopic pregnancy. A full bladder improves visualization of structures posterior to the bladder in the transabdominal approach. The bladder is a good landmark to find initially for orientation to the anatomy when scanning transabdominally. When scanning transvaginally in the sagittal view, identify the endometrial stripe from the fundus of the uterus to the cervix. This is accomplished by tilting the probe (anteriorly to posteriorly) while maintaining a sagittal plane of the uterus. From the sagittal view, the transducer is rotated counterclockwise 90 degrees (A) and directed toward the posterior fornix in a line through the umbilicus (B). Return to the fundus of the uterus in a sagittal view and slowly evaluate the right and then left borders of the uterus in the longitudinal axis. Scan posteriorly to the cervix and then superiorly to the fundus of the uterus to exclude the presence of a bicornuate uterus. If a pregnancy or intrauterine sac is identified with fetal cardiac activity, M-mode, not Doppler, should be used for documentation of fetal heart rate. Evaluate both adnexa/ovaries individually by scanning each side in both coronal and sagittal planes. This is often only a guide to their location, and a methodical approach is often required to visualize both ovaries. A common error is insertion of the transducer too far, thus bypassing the uterus and imaging only bowel. Traditionally, knowledge of common venous anatomy in experienced hands was the standard method of obtaining venous access. Factors such as obesity, prior access, and volume depletion can increase the difficulty of the conventional approach. This increased difficulty not only leads to failure to obtain access, but also increases the risk of complications. Ultrasound-guided vascular access reduces the variables associated with the traditional landmark-based approach for central venous access and has become the standard of care. Additionally, ultrasound is useful for both difficult peripheral venous and arterial access. Short-Axis Approach Indications Need for venous access Obscured landmarks (obesity, trauma, etc) Cardiac arrest Equipment Linear Convex Patient preparation Position and prepare the patient as per convention for access and use a sterile sheath for the transducer. For central venous access, the patient is supine with the access site in a dependent position. In the short-axis approach, maintain your transverse view and position the vein in the center of the image. Continue to advance until a venous flash is seen and the needle has reached the intended depth. Once the vein of interest is identified and centered on the screen, rotate the probe so that the transducer is in the same axis as the vein. Direct the needle along the long axis of the probe careful to keep the needle completely in-line with the probe and ultrasound beam. Continue to advance until a venous flash is seen or the needle has reached the intended depth. If no flash is seen at the appropriate depth in the correct path, slowly withdraw the needle and observe for venous return.
Purchase 400 mg skelaxin with visa
A more portable version spasms chest buy 400mg skelaxin, suitable for out-ofhospital use, is marketed as the Glidescope Ranger. Little-to-no anterior force is required, and in contrast to standard laryngoscope, levering the blade is recommended to enhance the view. Once the tube is passed through the cords, the proprietary stylet is withdrawn 5 cm to allow further passage of the tube. The steep angle of Glidescope blade and stylet causes the tube to abut the anterior tracheal rings and arrest tube delivery in most patients. Withdrawing the stylet 5 cm and rotating the tube clockwise will allow complete tube delivery to an appropriate depth. Available blades are similar in size and shape to the Mac 2, Mac 3, Mac 4, Miller 0, Miller 1, and a D-blade designed for patients with difficult airway anatomy. The near-standard shape of the blade allows direct laryngoscopy for glottic visualization as well as video laryngoscopy. Technique the blade connected to the power coupling should be handled like a standard laryngoscope blade. It should be inserted just to the right of midline of the tongue with the handle pointing toward the feet. As the tip of the blade advances downward along the tongue base and into vallecula, the tongue is swept slightly to the left to increase the amount of workspace. At anytime, the laryngoscopist can switch from a standard direct laryngoscopy to a video laryngoscopy; however, once changed to video laryngoscopy, it is best not to switch back and forth from video laryngoscopy to direct laryngoscopy. The blade is inserted just to the right of midline of the tongue with the handle pointing toward the feet. When fully inserted into the vallecula, the angle of the handle is now approximately 40 degrees from horizontal with lifting forces directed upward and forward. It has been shown to provide improved ventilation in cardiac arrest and failed airway cases and has a shallow learning curve, promoting its use by relative novices. The shape promotes blind insertion with an endpoint detected as resistance as the leading edge of the cuff just enters and obstructs and the esophageal inlet. The distal "mask" incorporates a small grate to prevent prolapse of the epiglottis within the mask. For a patient who is in a neutral head/neck position, such as a patient in a halo device, the stylet should be configured to about an 80 degree acute angle. If the patient is hyperflexed, a more acute angle is required, approximately 60 degrees. Finally, for patients who are hyperextended, an obtuse angle of 110 or 120 degrees would be appropriate. The technique can be performed with the intubator facing the patient, or with the intubator at the head of the bed behind the patient. With his nondominant hand, the intubator should grasp the tongue with gauze, gently distracting forward. The correctly assembled TrachLight demonstrates the correct alignment of the centimeter markings (inset) on the tube, the correct location of the bend (inset), and the correct engagement of the wire portion of the stylet (inset). Advancement stops when the intubator recognizes an orange glow on the anterior neck tissues or when tube advancement meets resistance. This process is continued repeatedly in an iterative manner until the correct midline glow indicating tracheal position is encountered. At that point, the stiffening wire is withdrawn several centimeters, resulting in a caudad displacement of the glow as the intratracheal stylet "relaxes. The tube is now confirmed to be intratracheal and the tube tip is confirmed to be reliably in the mid-trachea, with no need for confirmatory chest radiograph. Failure to modify the position of the transilluminated glow usually indicates that the stiffening wire has displaced from the locking notch that keeps the wire from rotating in place. The device is placed in the center of the mouth while the left hand is lifting the tongue anteriorly. Technique Digital intubation technique is performed with the intubator facing the patient from the side. He should next "walk" the fingers down the tongue to progressively displace the tongue anteriorly as the fingers are advanced to the epiglottis. As the third finger encounters the epiglottis, the finger traps and holds the epiglottis anteriorly. Index and third finger inserted into the mouth with "C" shaped stylet held in left hand. Digital intubation may be the best airway delivery option in austere conditions or in patient with copious airway secretions or blood. The cuff is then inflated with approximately 20 mL of air or until the pilot balloon is firm. The distal cuff seals the esophagus and the proximal seals the oropharynx and nasopharynx when inflated. The tube is advanced until resistance is met or until the connector base is aligned with the teeth or gums. The tube is advanced until resistance is met or the base of the connector is at the level of the lip or gum. The balloon is inflated with 45 to 90 mL of air depending on the size of the tube. Lidocaine jelly can be used as the lubricant to provide additional topical anesthesia. We favor the use of disposable atomizers to instill 2 mL of a mixture of tetracaine 1%/phenylephrine 0. Pulling on the proximal loop "trigger" causes anterior deflection of the tube tip. To minimize trauma to the nasal turbinates, the bevel of the tube should face the turbinates. This implies that if the left naris is being intubated, the tube can be inserted along the normal curve of the nose-nasopharynx; however, if the right naris is being intubated, the tube should be inserted with the curve of the tube in a cephalad direction until the tube is advanced to the nasopharynx, at which point the tube is rotated to the correct anatomic configuration. As the tube is slowly advanced to the hypopharynx, the intubator listens closely for transmitted breath sounds, rotating the tube right or left to maintain maximal transmission. It takes a more-severe-than-expected rotation externally to generate a small rotation of the supraglottic tube tip. The tube is then rapidly advanced unless resistance is encountered, as would be expected with pyriform sinus tube tip position. Correct intratracheal placement should elicit cough, a reflex deep inspiration, and a loss of phonation. When inserted into the nose, the bevel of the tube should face the turbinates to minimize the trauma to these structures. In addition to amplifying transmitted sounds, this trick also can spare the intubator from a sputum ear wash. Positional feedback can also be enhanced by use of a quantitative waveform capnometer/capnograph. Tube tip position is determined identically to that with orotracheal transillumination, with identical repositioning maneuvers, except that rotational maneuvers are likely to be more extreme as noted above. Blind nasotracheal intubation offers a viable option in the event that oral intubation is rendered impossible in the short term, such as a patient who has a wired jaw or large subglossal hematoma. The endoscope tip is manipulated by a combination of trigger deflection (up/down) and scope rotation (left/right) to keep the lumen in the center of the optical field. As the tube is advanced to the posterior nasopharynx, the scope tip is deflected downward to reveal the epiglottis and laryngeal inlet. The scope is advanced further, with the operator maneuvering the scope tip to keep the glottic opening in the center of the optical field. With the endoscope tip just above the cords, 2 mL of 1% lidocaine should be injected through the injection port of the fiberscope to provide vocal cord anesthesia prior to tube passage. The endoscope advancement continues until the endoscope tip is approximately 3 to 5 cm above the carina. The tube is then gently advanced over the fiberoptic sheath into the naris and to the trachea. If resistance is encountered at 14 to 16 cm, the tube may be Patient Preparation For both methods, the nose is prepared as described above under blind nasotracheal intubation. The endoscope is then guided to the glottic opening and the tube is then advanced over the endoscope. The endoscope is then advanced through the tube and maneuvered to the glottic opening. As discussed previously, this can be corrected by a severe counterclockwise rotation.