Buy 5gm bactroban otc
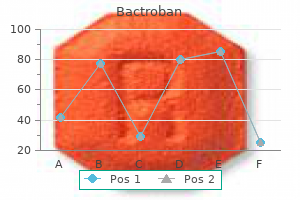
The differentiation of focal lesions in the kidney and perinephric space is discussed in Tables 27 acne x out purchase discount bactroban online. The long renal axis is medially oriented, and renal pelvises and ureters are situated anteriorly. Comments In longitudinal ectopy, the kidney is malpositioned in any location from the thorax to the sacrum. Pelvic kidney is the most common location and frequently associated with vesicoureteral reflux, hydronephrosis, hypospadia, and contralateral renal agenesis. In crossed ectopy, the malpositioned kidney is commonly fused with the contralateral kidney. A large kidney with usual outline and two collecting systems on one side and an absent kidney on the contralateral side are diagnostic. In renal fusion, the fused kidneys are located in the midline and may assume the shape of a horseshoe, disk, or pancake. Differential diagnosis: A malpositioned kidney may also be caused by a large adjacent mass. In complete renal and ureteral duplication, the ureter draining the upper system inserts ectopically medial and below the orthotopic ureter in to the bladder trigonum or urethra and may be associated with an ectopic ureterocele. Other congenital renal anomalies are partial duplication, supernumerary kidney, and renal hypoplasia or agenesis. Upper pole moiety is subject to obstruction and may simulate an upper pole mass on excretory urography when completely obstructed. The lower poles of both kidneys are fused by a parenchymal isthmus, with the renal pelves and ureters being situated anteriorly. Axial (a) and coronal (b) views showing a malpositioned left kidney located on the right side that is partially fused with the right kidney. Differential diagnosis: renal duplication where either the upper or lower pole moiety is malfunctioning. It may result in concentric encroachment of the renal collecting system (trumpetlike pelvocaliceal system on urography), but without obstruction. Dilated collecting system evident as water-density structure within normal or enlarged kidney on nonenhanced images. After enhancement, a persistent nephrogram and delayed and decreased contrast medium excretion are characteristic. In long-standing obstruction, the kidney appears as a fluid-filled cyst with a thin rim of solid renal tissue draped around it. Comments Etiology: (1) normal increase of sinus fat with aging and in obesity; (2) vicarious proliferation of sinus fat with renal atrophy of any cause; (3) fibrolipomatosis induced by extravasation of urine in to the renal sinus. Early hydronephrosis can be differentiated from an extrarenal pelvis and postobstructive uropathy by the persistent nephrogram and delayed urinary contrast material excretion after contrast enhancement. Freely mobile filling defects in the collecting system other than renal calculi include blood clots and fungus balls. Higher than water attenuation values in a renal cyst are found with hemorrhage in to the cyst, contrast material leakage in to the cyst (caused by either communication with the collecting system or diffusion), calcification of the cyst wall or the cyst content (milk of calcium or calcium carbonate), high protein content of cyst fluid, and infection. Occurs frequently in the fifth and sixth decade of life and is almost always asymptomatic. Very rare complications may include obstructive caliectasis and renal vascular hypertension due to compression of renal arteries. Progressive renal failure and hypertension are usually evident in the fourth decade but occasionally as early as childhood or young adulthood. Parapelvic cyst (renal sinus cyst) Features of a benign renal cyst, but located adjacent to the renal sinus. Multiple cysts of different sizes cause splaying and distorting of the collecting system and may demonstrate varying densities due to blood products of different ages. They represent abnormally proliferated and dilated collecting tubules and do not produce calyceal or renal pelvis distortion. Note tiny punctate calcifications bilaterally in the area of the renal papillae due to hyperparathyroidism. A dilated collecting system (arrow) of the left kidney with persistent dense nephrogram and delayed contrast excretion is characteristic (b). The hydronephrosis is caused by a large and partially thrombosed abdominal aortic aneurysm projecting anterior to the lumbar vertebra. A hydronephrosis (arrow) is seen on the right side of a horseshoe kidney evident by the medially oriented long renal axis and the anteriorly located renal pelvis. A renal cyst (arrow) with a precontrast density similar to the adjacent renal parenchyma is seen. A sharply delineated, homogeneous lesion of near-water density is seen within the left kidney following intravenous contrast material administration. A large right renal cyst with poor definition on its superolateral border and obliteration of the adipose tissue in the adjacent perirenal space is seen. No functional renal parenchyma is detectable after contrast administration (unlike multilocular cystic nephroma and unilateral polycystic kidney disease). Comments Frequent cause of palpable abdominal mass in an otherwise healthy infant or child resulting from failed fusion of the metanephros and ureteric bud. Compensatory hypertrophy of the contralateral kidney is usually present, often with an element of ureteropelvic obstruction. Occurs in children younger than 5 y (M:F 3:1) and in 40- to 70-y-old adults with strong female predominance. On ultrasound, multiple cystic masses separated by highly echogenic septa are evident. Nodular thickening of the cyst wall and/or septa may be the clue for a malignancy. Rare, in the majority of cases inherited, disorder manifesting itself in adolescents and young adults with progressive renal failure. Inherited (autosomal dominant) neurocutaneous dysplasia complex with onset in the second to third decade. Retinal angiomatosis, cerebellar and spinal hemangioblastomas, pheochromocytomas, pancreatic tumors and cysts, hepatic adenomas, and hemangiomas may be associated. Cysts are often separated by thick septa and sharply demarcated from the normal renal parenchyma. Peripheral and central calcifications of circular, stellate, flocculent, or granular nature in up to 50% of cases. In approximately half of the cases, small calculi measuring up to 5 mm are clustered in the ectatic tubules of the papilla. Complications include hemorrhage and development of renal adenomas and carcinomas. Combination of multiple renal cysts and solid tumors (carcinomas, adenomas, and hemangiomas) characteristic. Renal carcinomas are often small, 2 cm in size, and may occur within the cysts themselves. A multiloculated cystic mass without functional renal parenchyma is apparent in the pelvis. Large septated cystic mass originating from the right kidney (arrow) occupies over half of the abdominal cavity at this level. Bilateral small kidneys with tiny cysts and a small renal cell carcinoma (arrow) in the posterior aspect of the right kidney are evident. Multiple bilateral cystic and solid mass lesions in slightly enlarged bilateral kidneys are seen in both patients. Comments these anomalies include: Fetal lobulations: cortical bulges centered over corresponding calyces Dromedary hump: in the midportion of the left kidney due to prolonged pressure by the spleen during fetal development Column of Bertin: focal hypertrophy of the septal cortex in the midportion of the kidney causing deformation of the adjacent calyces and infundibula Hilar lip: supra- and infrahilar cortical bulge above and below the renal sinus Nodular compensatory hypertrophy: hypertrophied normal renal tissue secondary to focal renal scarring Most common cortical lesion at autopsy. Metanephric adenoma typically presents as a slightly hypoattenuating mass with little enhancement and occasionally small calcifications.
Syndromes
- Tanning or darkening of the skin
- Use of certain medications such as lithium, tamoxifen, and thiazides
- Croup-like (barking) cough
- Side effect of a drug such as Dilantin or phenobarbital
- Allergic reaction to the contrast dye
- Dementia
- Properly put weight on your residual limb. You will be told how much weight to put on your residual limb. You may not be allowed to put weight on your residual limb until it is fully healed.
- At the end of the procedure, your portal vein pressure will be measured to make sure it has gone down.
Discount bactroban 5 gm fast delivery
The posterior aspect of the sublingual space is divided by the hypoglossal muscle in to medial and lateral compartments acne before and after buy cheap bactroban 5gm on line. The lateral compartment contains the hypoglossal and lingual nerve, combined with the chorda tympani branch of the facial nerve, sublingual glands and ducts, deep portion of the submandibular gland, and submandibular duct. Normal occupants of the medial compartment are the glossopharyngeal nerve and lingual artery and vein. A mass is confined to the sublingual space when the center of the lesion is superomedial to the mylohyoid muscle and lateral to the genioglossus muscle. Lesions may escape the sublingual space in to the submandibular space at the posterior margin of the mylohyoid muscle or through a cleft of the mylohyoid muscle between its anterior one third and posterior two thirds. Larger lesions of the sublingual space may cross the anterior midline under the frenulum of the tongue and become bilobular. The most common lesions of the sublingual space include squamous cell carcinoma arising from the epithelial lining of the sublingual space, abscess formation from odontogenic infection, a variety of congenital/developmental lesions, ranula, and an obstructed submandibular duct. It is a horseshoe-shaped, fascial-lined space located inferolaterally to the mylohyoid muscle sling and deep to the platysma muscle, below the mandible and superiorly to the hyoid bone. The superficial layer of the deep cervical fascia splits to encircle the submandibular space, with the deeper slip of fascia running along the external surface of the mylohyoid muscle and a more shallow slip paralleling the deep margin of the platysma. The principal contents of the submandibular space are the superficial portion of the submandibular gland, the submandibular and submental lymph nodes, the anterior belly of the digastric muscle, the facial vein and artery, and the inferior loop of the hypoglossal nerve and fat. A mass is primary to the submandibular space when its center is within the submandibular space inferolateral to the mylohyoid muscle. With rare exceptions, lesions of the submandibular space do not decompress in to the sublingual space (in contrast to the tendency of large masses of the sublingual space to work their way in to the submandibular space). Most lesions of the submandibular space are from either the submandibular gland or nodes. In adults, the most common pathology of the submandibular space is metastatic lymph nodes from squamous cell carcinoma of the oral cavity. There are few diseases that do not follow the spatial anatomical confinement or involve multiple spaces, either contiguously or noncontiguously. The term transspatial is applied to disease processes that involve multiple contiguous spaces of the neck. Transspatial diseases can be divided in to three broad categories: developmental lesions, infections, and tumors. Transspatial developmental lesions include thyroglossal duct cysts, branchial cleft cysts, infantile hemangioma, vascular malformations, and macrocystic lymphatic malformations. Transspatial infectious diseases include cellulitis and abscesses, as well as diving ranulas. Transspatial benign tumors include lipomas, schwannomas, neurofibromas, juvenile angiofibromas, and aggressive fibromatosis. The term multispatial is applied to disease processes that involve multiple noncontiguous spaces of the neck. Multispatial nodal diseases include malignant adenopathy (lymph node metastases and lymphoma) and nonmalignant inflammatory adenopathy (any upper respiratory infection, either viral or bacterial, with reactive adenopathy; less frequently, mononucleosis, tularemia, tuberculosis, cat scratch fever, sarcoidosis, human immunodeficiency virus, Castleman disease, and Kimura disease). Level I includes all the nodes above the hyoid bone, below the mylohyoid muscles, and anterior to a transverse line drawn on each axial image through the posterior edge of the submandibular gland. They lie anterior to a transverse line drawn on each axial image through the posterior edge of the sternocleidomastoid muscle and posterior to a transverse line through the posterior edge of the submandibular gland. Retropharyngeal nodes, only present in suprahyoid neck, lie medial to the internal carotid artery. These nodes lie anterior to a transverse line drawn on each axial image through the posterior edge of the sternocleidomastoid muscle and lateral to the carotid arteries. These nodes lie anterior and medial to an oblique line drawn through the posterior edge of the sternocleidomastoid muscle and the posterolateral margin of the anterior scalene muscle. Level V (posterior triangle) nodes extend from the skull base to the level of the clavicle. Level V nodes all lie anterior to a transverse line drawn through the anterior edge of the trapezius muscle. Suprahyoid Neck 301 bone, superior to the top of the manubrium, and between the left and right carotid arteries. Supraclavicular, retropharyngeal, parotid, facial, occipital, and postauricular nodal groups will still be referred to by their anatomical names. The maximal diameter of a normal cervical lymph node varies from 3 to 11 mm; the greatest nodes are located in the submandibular and jugular digastric region. Fatty hilar metaplasia occurs almost exclusively at the periphery of the node as an area of low density. In a child, metastatic neuroblastoma is the most common cause of calcified cervical lymph nodes. In adults, the most common cause of a calcified cervical lymph node is metastatic papillary thyroid carcinoma and scrofula. Within 2 cm of the skull base, any node medial to this line is classified as a retropharyngeal node. Eggshell-type calcifications can occur in silicosis, sarcoidosis, tuberculosis, scleroderma, amyloidosis, sinus histiocytosis, and massive lymphadenopathy treated with interferon. Cystic nodes are seen in metastatic papillary thyroid carcinoma and in squamous cell cancer of the head and neck (base of the tongue and tonsil). Maintenance of soft tissue planes in the adjacent parapharyngeal and retropharyngeal spaces strongly argues against a true mass lesion. A collapsed lateral pharyngeal recess can frequently be distended with the Valsalva maneuver, a modified Valsalva maneuver, or opening of the mouth widely. Although usually asymptomatic, these cysts may become infected, giving rise to pain, halitosis, nasal discharge, and prevertebral muscle spasm. Differential diagnosis: Rathke pouch, a small epithelial cyst in the sphenoid body anterocephalad to Tornwaldt cyst. Uncommon and rare congenital cysts of the nasopharynx include transsphenoidal meningoencephalocele, neurenteric cyst, dermoid cyst, epidermoid cyst, cystic hamartoma, cystic teratoma, and extension of a second branchial cleft cyst or of a thymic cyst to the lateral pharyngeal wall. Inflammatory/infectious conditions Adenoidal and tonsillar hyperplasia Symmetric involvement of the lymphatic tissue in the nasopharynx and oropharynx with attenuation similar to that of muscle, usually associated with hypertrophic faucial tonsils and reactive retropharyngeal and cervical adenopathy. Tonsillitis presents as nonspecific, uni- or bilaterally tonsillar enlargement, with heterogeneous contrast enhancement, consistent with early infection and edema, bulging in to the airway. Inflammatory changes may extend in to the soft palate, parapharyngeal space, and masticator space. Immunobiological overactivity results in hypertrophy of the lymphoepithelial tissue in the pharynx, most commonly the adenoid component, less commonly the faucial and lingual tonsils. Beta-hemolytic Streptococcus, Staphylococcus, Pneumococcus, Haemophilus, and Fusobacterium are the most common organisms. When bilateral, tonsils may abut medially ("kissing tonsils"), obstructing the oropharyngeal airway. The abscess pocket is confined by the superior constrictor pharyngeal muscle to the pharyngeal mucosa space. Peritonsillar abscess shows a pocket of fluidlike central areas of low attenuation within the enhancing cellulitic soft tissues of the peritonsillar area near the superior pole of the tonsil. Most feared complication is extension of infection in to the carotid space with septic thrombosis of the internal jugular vein or septic aneurysm of the carotid artery. Comments Usually occurs in children or young adults with sore throat and fever, followed by rapidly increasing painful swallowing, ear pain, and trismus. The disease is usually self-limited, but when it is severe, infection undergoes internal cavitations and suppuration, creating tonsillar or peritonsillar abscess. Peritonsillar abscess is the most common deep infection of the neck and chiefly involves patients between the ages of 10 and 40 y. Well-defined, ovoid or pear-shaped, nonenhancing lesion of low (cystic) density in the nasopharynx, oropharynx, or vallecula, 1 to 2 cm, with no deep extension. Large cyst in the lateral pharyngeal recess may obstruct the eustachian tube, with resulting mastoid fluid. Postinflammatory dystrophic calcifications within the tonsils exist in as much as 10% of the population (men women, mean age 55 y).
Bactroban 5gm without prescription
Metastatic adenocarcinomas with signet cells skin care 77054 purchase bactroban 5 gm fast delivery, first described from the stomach, are termed Krukenberg tumor. The ovaries reside on either side of the uterus and are attached to the broad ligament posterior superiorly. There is a third lymphatic drainage along the round ligament to the inguinal nodes. The ovary, covered by epithelium, has its lateral border facing the peritoneal cavity. Lymphatic drainage from the subphrenic recess is through the diaphragm to the diaphragmatic nodes. Visceral peritoneal disease seldom invades the intestinal lumen but coalesces loops of bowel, which can lead to a functional obstruction. Nodes greater than 5 mm are considered positive, are seen in approximately 15% of patients, and have a poor prognosis. Unusual sites of recurrence are becoming more frequent as patient survival is increasing. These include cerebral metastases, mediastinal adenopathy, bone, and solid organs of the abdomen, i. Krukenberg tumors of the ovaries are likely secondary by intraperitoneal spread from gastric or colon mucinous adenocarcinoma. Pelvic Inflammatory Disease Pelvic inflammatory disease implies infection and inflammation of the upper genital tract. It is commonly caused by the sexual transmission of Neisseria gonorrhea and Chlamydia trachomatis. Continuity of subperitoneal spread from the right adnexa to the mesentery of the small bowel. Arrows indicate the cleft between tumor in the broad ligament and the lateral pelvic wall. A tuboovarian complex secondary to adhesions and necrosis results in a tuboovarian abscess. Delgado G, Bundy B, Zasno K: Prospective surgical-pathological study of disease free interval in patients with stage 1B squamous cell carcinoma of the cervix. These are most common in the pelvic recesses adjacent to the adnexa and in the cul-de-sac but can occur anywhere in the abdomen. Morisawa N, Koyama T, Togashi K: Metastatic lymph nodes in urogenital cancers: Contribution of imaging findings. Patterns of Extraabdominal and Extrapelvic Spread 16 Introduction this chapter describes how abdominal and pelvic disease spreads from the coelomic cavity in to the chest, the abdominal and pelvic wall, and to the thigh. A few minor openings also exist to transmit the greater and lesser splanchnic nerves at the crura of the diaphragm and apertures for small veins at the central tendon. A Bochdalek hernia, one of the most common diaphragmatic hernias, is located posterolaterally and commonly contains the kidney and extraperitoneal fat on the left. The left phrenic nerve follows the pericardiophrenic vessels in the mediastinum along the left cardiac border. The diaphragm has a rich lymphatic drainage to absorb peritoneal and pleural fluids that provide lubrication for organs in the chest and abdomen and have a high daily turnover rate. The middle diaphragmatic nodes are around the inferior vena cava and near the phrenic nerve. Below the diaphragm, lymph drains in to the nodes along the inferior phrenic vessels near the diaphragmatic crura and to the cisterna chyli and thoracic duct on the right side of the aorta. This mode also refers to spread of tumors that originate from the organs or structures passing through these apertures such as tumors at the esophagogastric junction, neurogenic tumors, lipomatous tumors, and lymphangioma. In addition, invasive tumors such as lymphoma or metastatic tumors below the diaphragm may penetrate directly through the diaphragm in to the chest cavity and the mediastinum, but it is uncommon. Knowing these pathways is important for identification of potential sites of recurrent disease after curative resection. Transvenous Spread Venous tumor thrombus is a common manifestation of tumors such as hepatocellular carcinoma and renal cell carcinoma. Note the left inferior phrenic artery (arrowhead) and the crura of the diaphragm (curved arrows). The muscles of the abdominal wall derive the blood supply from the rectus abdominis: a long, elliptical-shaped muscle attaching to the lower anterior ribs superiorly and extending to the pubic symphysis and anterior pubic rami inferiorly. The three layers of flat-shaped muscle: the most superficial ``external oblique,' the middle ``internal oblique,' and the deepest ``transversus abdominis. Hepatic metastases from colorectal cancer with metastases to the anterior diaphragmatic and middle diaphragmatic nodes. Metastasis to the right axillary lymph node 18 months after a right liver resection for metastatic colon cancer. Patterns of Disease Spread from the Abdominal Cavity to the Anterior Abdominal Wall Among the various types of spread described in this book, direct contiguous invasion and intraperitoneal spread are the most likely methods to involve the anterior abdominal wall and extend outside the abdominal cavity. The spread can be facilitated through the natural or acquired defects of the abdominal wall, particularly from a surgical incision and at the site of ileostomy or colostomy. For example, a fistula along the incision that causes wound dehiscence may originate from a postoperative anastomotic leak in the abdomen; hematoma or abdominal ascites may extend in to the hernial sac. Carcinoma of the cecum with inflammatory mass involving the bladder and extending behind the inguinal ligament in to the inguinal canal. Varices (arrow) around the stoma (arrowhead) of a colostomy in a patient who developed portal hypertension secondary to chemotherapy for metastatic colon cancer. Recurrent tumor in the abdominal wall after laparoscopic cholecystectomy for carcinoma of the gallbladder. The lesser sciatic foramen is bordered by the sacrospinous ligament superiorly, the sacrotuberous ligament medially and inferiorly, and the medial edge of the obturator internus and the lesser sciatic notch of the ilium. The obturator foramen is covered by the obturator internus muscle and fascia except for a small opening anteriorly that transmits the obturator vessels and nerve. The deep inguinal ring is the opening from the abdominal cavity and the superficial inguinal ring opens in to the scrotum. The pyriformis muscle attaches to the sacrum and the posterior gluteal surface of the ilium covering the posterolateral wall of the pelvic cavity. The obturator internus muscle forms the anterolateral wall; it attaches to the ischial ramus and inferior ramus of the pubic bone. They transmit the organs, vessels, and nerves outside the pelvic cavity and they are potential sites for hernia: the greater sciatic foramen is defined by the greater sciatic notch of the ilium, the lateral border of the sacrum, and the sacrospinous ligament. Its superior opening between the ilium and the superior border of the pyriformis allows the passage of the superior gluteal artery to supply the gluteus muscle. The greater sciatic and lesser sciatic foramen are separated from the parietal peritoneum by connective tissue, extraperitoneal fat, and muscle and its fascia, while the obturator foramen, the deep inguinal ring of the inguinal canal, and the femoral ring are closely in contact with the parietal peritoneum and may be divided only by loose areolar tissues. Weakness of the fascia covering these openings due to excessive stretching, injury, or surgical incision coupled with an increase in intraperitoneal pressure may allow the abdominal organs or structures to transmit through these foramina, resulting in an inguinal hernia, femoral hernia, obturator hernia, or sciatic hernia. Direct Contiguous Spread the extraperitoneal space of the pelvis is largely occupied by the bladder, rectum, and male or female genital organs, and they are enclosed by several groups of muscle that form the pelvic wall, fascia, extraperitoneal fat, and the vessels and nerves. Large ascites (A) is present in the pelvic peritoneal cavity with herniation (white arrow) through the obturator foramen (black arrow) along the obturator vessel (arrowhead). On rare occasion, they may extend anteriorly along the urachus to the umbilicus and anterior abdominal wall. Inflammatory processes and invasive tumors may grow along the anorectum, the urethra, or the vagina through the perineal opening of the levator ani. Pelvic hemangiopericytoma growing outside the pelvis shown on axial, coronal, and sagittal planes. Extraperitoneal hemorrhage from anticoagulation therapy extending along the iliopsoas muscle to the left groin. Diffuse B-cell lymphoma (T) of the bladder (B) and rectum infiltrates the urachus in to the anterior abdominal wall around the umbilicus (arrow) and to the perineum (arrowheads).
Buy cheap bactroban 5 gm line
Symmetric bilateral segmental atelectasis with air bronchograms and discrete ground-glass opacities acne nodule order 5gm bactroban mastercard. Diagnostic pearls: Thickened interlobular septa and centrilobular micronodules, usually involving lung periphery, and diffuse ground-glass opacities (less prominent than in pneumocystic pneumonia). Diagnostic pearls: Patchy, homogeneous, poorly defined peribronchial ground-glass opacities with or without centrilobular nodular pattern. Comments Particularly affects neonates and immunocompromised patients (especially organ transplant recipients). Disseminated disease is an early appearance of acute fungal sepsis and is found particularly in immunocompromised patients. Focal consolidations and cavitations are much more typical for fungal infections but are typically observed only in subsequent stages. Diagnostic pearls: Bilateral ground-glass opacities with sparing of the subpleural space are the dominant finding. Also characteristic are superimposed intra- and interlobular septal thickening leading to crazy paving, lack of tree-in-bud sign, often mosaic pattern caused by alternating involvement and sparing of subsegmental areas. Thin-walled cysts are frequently associated, especially in the upper lobes, and may lead to spontaneous pneumothorax. Diagnostic pearls: Ground-glass opacities (interstitial and alveolar edema and hemorrhagic fluid) and dense parenchymal consolidations (atelectasis) in the dependent lung in combination with normally aerated lung. Can be differentiated from cardiogenic pulmonary edema by a normal heart size, more diffuse lung involvement, extensive and conspicuous air bronchograms, a cystic or "bubbly" appearance of the parenchymal involvement after 7 days, and the absence of significant pleural effusion. Clearly demarcated cavities in the centrilobular portion of the secondary pulmonary lobule. Diagnostic pearls: Primarily affects upper portions of lung zones (apex, apica segment of lower lobules). In premature infants, a "spongy" lung pattern is associated with bronchopulmonary dysplasia due to prolonged high oxygen therapy. Strongly associated with nicotine abuse; also observed after inhalation of industrial dust. More severe cases require medical therapy (bronchodilators) or surgery (lung volume reduction/lung transplantation). Histologically, destruction of alveolar tissue with abnormal enlargement of all parts of the acinus. No therapy may be necessary, but severe cases may require surgical lung volume reduction or even lung transplantation. Diagnostic pearls: Homogeneously distributed diminishment of the interstitium due to acinar enlargement without zonal preference. Thickened interlobular septa and centrilobular micronodules, particularly involving the lung periphery. Acute stage showing bilateral ground-glass opacities with sparing of the subpleural space (a). A 4-month follow-up examination in the same patient without treatment shows progression in to asymmetric reticular consolidations (b). Clearly demarcated pulmonary cavities surrounded by normal lung parenchyma (a), which primarily affects the upper portions of lung zones (b). Homogeneously distributed diminishment of the interstitium (a), resulting in bullous emphysema (b). Diagnostic pearls: Bilateral ill-defined noduli and coarse reticulonodular opacities with basilar preference, as well as thickening of the bronchovascular bundle with ill-defined perihilar consolidations. Diagnostic pearls: Uni- to bilateral focal or multifocal air-space opacities; increased volume of affected lobe (no atelectasis); ill-defined lobulated and/or spiculated peripheral nodules; ground-glass-opacities with or without reticulonodular pattern (crazy paving). Diagnostic pearls: Typically ill-defined consolidations with air bronchograms (nodules ranging from diffuse miliary pattern to only a few large lesions); coarse perihilar reticulonodular pattern (caused by direct extension from hilar lymph nodes); and peripheral interstitial disease with irregular thickened subpleural lines, interlobular septa, and lymphatic nodular distribution pattern (centrilobular nodules involving the subpleural space) (see also. Arterial feeders entering single lesions are common but not specific (differential diagnosis: septic emboli and other hematogenous infections). Diagnostic pearls: Usually asymmetric nodular septal thickening confined to one lung/lobe (may also involve both lungs; may resemble edema: Kerley B lines on radiographs); centrilobular micronodules involving the subpleural space (lymphatic distribution pattern); nonspecific patchy ground-glass opacities with or without septal thickening (crazy paving). Abnormal endothelial vascular channels embedded within spindle-shaped stromal cells. Cancer cells typically spread bronchogenically via the tracheobronchial tree (cancer pneumonia). Diffuse form presenting as bilateral chronic consolidations with air bronchograms is rare. Lung infection in patients with lymphoma is more often due to drug reactions, concomitant pneumonia, or hemorrhage rather than the underlying disease itself. Pulmonary manifestation of lymphoma is usually associated with or subsequent to hilar and mediastinal lymph node involvement. Nodular pulmonary metastases are commonly associated with neoplasms of the lung, kidney, colon, gonads, uterus, bone, head, and neck (including thyroid), melanomas, and soft tissue sarcomas. An important differential diagnosis is pulmonary septicemia, which may not be discernible from hematogenous spread of metastases on imaging findings alone. Bilateral ill-defined noduli and coarse reticulonodular opacities with basilar preference (a). Another patient with thickening of the bronchovascular bundle and ill-defined perihilar consolidations (b). Examples of unilateral growth with a predominantly reticulonodular pattern (a) and multifocal growth with ground-glass opacities (b). Unilateral asymmetric nodular septal thickening (a), with centrilobular micronodules involving the subpleural space, patchy ground-glass opacities, and discrete pleural effusion on the right. Diagnostic pearls: Solitary (two thirds) or multiple (one third) round to oval nodules 1 to 5 mm in size. Vascular occlusion due to a thromboembolic disease often associated with an underlying cardiopulmonary disease. Diagnostic pearls: Wedge-shaped, initially ill-defined, pleura-based consolidation with apex pointing toward the hilum (Hampton hump). Diagnostic pearls: Well-defined, round or lobulated mass in close proximity to the left atrium, as well as contrast enhancement simultaneous with the left atrium. Inflammation Amyloidosis A variety of conditions in which amyloid proteins are abnormally deposited in the lung. Diagnostic pearls: Tracheobronchial type: Endobronchial nodules with obstructive airway disease. Nodular type: Solitary or multiple nodules, partly with cavitation and/or calcification. Diffuse parenchymal type: Diffuse interstitial disease of miliary or reticulonodular nature. Conglomerate masses ranging in the middle and upper lung zones and associated with a variety of pneumoconiosis. Mass appears spindle-shaped, with a shorter anteroposterior and a longer mediolateral diameter. Histologically, deposition of fibrils of light-chain immunoglobulins in perivascular distribution. Primary amyloidosis (amyloid L) associated either with no disease or with multiple myeloma. However, in sarcoidosis, massive fibrosis may also present as a central homogeneous mass or large nodular lesions with irregular margins. A slightly lobulated subpleural mass is seen on the left side with a feeding vessel. Wedge-shaped pleura-based consolidation dorsally in the right lower lobe (a) with corresponding pulmonary artery embolus (b). Diagnostic pearls: Multiple, usually sharply defined, bilateral nodules ranging from 1 to 10 cm and commonly found in the lower lung zones; presence of "feeding" vessels entering the nodules; often thick-walled and nonregular cavitation that may progress in to thin-walled cavities. Diagnostic pearls: Solitary or multiple, wellcircumscribed, peripheral nodules measuring from 5 mm to 5 cm in diameter. Solitary or multiple cystic lesions due to obstructive overinflation associated with acute pneumonia. The lymphomatoid variant of Wegener granulomatosis typically spares the paranasal sinuses.
Generic 5 gm bactroban mastercard
Blood Supply Hypogastric artery (anastomotic network): Vaginal branch of the uterine artery is the primary supply to the vagina acne breakout bactroban 5 gm otc. Middle rectal and inferior vaginal branches of the hypogastric artery (internal iliac artery) are secondary blood supplies. It is the specialized narrow inferior portion of the uterus that is at the apex of the vagina. Components the cervix can be further subdivided into: Portio vaginalis: Portion of the cervix projecting in to the vagina. Answer: the transformation zone should be completely excised because that is where the majority of cervical cancers arise. The transformation zone is the area of metaplasia where columnar epithelium changes to squamous epithelium. It is the most important cytologic and colposcopic landmark, as this is where over 90% of lower genital tract neoplasias arise. Blood Supply Cervical and vaginal branch of the uterine artery, which arises from the internal iliac artery. In pregnancy, the uterus enlarges with the growth of the fetus and progressively becomes an abdominal as well as a pelvic organ. Supracervical hysterectomy = Uterus removed, cervix retained (ovarian status unknown). Inner longitudinal Endometrium: the mucosal layer of the uterus, made up of columnar epithelium. Anatomic Sections, from Lateral to Medial the tubes are occluded at the isthmus for permanent sterilization via laparoscopy. No peritoneum around ovaries leads to fast dissemination of ovarian cancer in the abdomen. They are attached to the broad ligament by the mesovarium and are not covered by peritoneum. Veins drain in to the inferior vena cava on the right side and the renal vein on the left. Histology Reproductive Anatomy the ovaries are covered by tunica albuginea, a fibrous capsule. Patient denies loss of fluid, vaginal bleeding, fever, trauma, sick contacts, and travel. Some ligaments of the pelvis act only as support structures, but others also carry the blood supply for essential organs. Broad ligament: Peritoneal fold extends from the lateral pelvic wall to the uterus and adnexa. Round ligament: the remains of the gubernaculum; extends from the corpus of the uterus down and laterally through the inguinal canal and terminates in the labia majora. Cardinal ligament (Mackenrodt ligament): Extends from the cervix (near the level of the internal cervical os) and lateral vagina to the pelvic side wall; most important support structure of the uterus. Uterosacral ligaments: Each ligament extends from an attachment posterolaterally to the supravaginal portion of the cervix and inserts in to the fascia over the sacrum. Pelvic diaphragm forms a broad sling in the pelvis to support the internal organs. It is composed of the levator ani complex (iliococcygeus, puborectalis, pubococcygeus muscles) and the coccygeus muscles. Urogenital diaphragm is external to the pelvic diaphragm and is composed of the deep transverse perineal muscles, the constrictor of the urethra, and the internal and external fascial coverings. Perineal body is the central tendon of the perineum, which provides much of the support. Bulbocavernosus, superficial transverse perineal, and external anal sphincter muscles converge at the central tendon. Nerve Supply Pudendal nerve, which originates from S2, S3, S4 levels of the spinal cord. The adult pelvis is composed of four bones: the sacrum, the coccyx, and two innominate bones. Sacrum: Consists of five vertebrae fused together to form a single wedge-shaped bone. The sacral promontory is the first sacral vertebrae, and it can be palpated during a vaginal exam. Coccyx: Composed of four vertebrae fused together to form a small triangular bone that articulates with the base of the sacrum. Pelvic Shapes Reproductive Anatomy the ischial spines serve as landmarks in determining the station of the fetus. Gynecoid is the ideal shape for vaginal delivery, having a round to slightly oval pelvic inlet. Prior to this, she reports regular menses every 28 days, lasting for 4 days each month since menarche. Pregnancy must be considered in any woman of reproductive age with complaints of amenorrhea or irregular menses and abdominal pain even if she is using contraception. Including or excluding pregnancy will significantly narrow the list of differential diagnoses. It is important to differentiate the physiological changes of pregnancy from other pathological conditions. Cessation of menses: Pregnancy is highly likely if 10 or more days have passed from the time of expected menses in a woman who previously had regular cycles. Skin changes: Striae gravidarum (aka stretch marks): Reddish, slightly depressed streaks on the abdomen, breast, and thighs. Chloasma or melasma gravidarum (aka mask of pregnancy): Irregular brown patches of varying size on the face and neck. Angiomas: Red elevation at a central point with branching vasculature present on the face, neck, chest, and arms due to estrogens. The uterus in size throughout the pregnancy (its size correlates to gestational age). By week 12, it is about the size of a grapefruit and the fundus of the uterus becomes palpable above the pubic symphysis (see Table 2-1). Changes in cervical mucus: Cervical mucus can be dried on a slide and evaluated via microscope. Vaginal mucosa discoloration: With pregnancy and blood flow, the vagina appears dark bluish or purplish-red. Perception of fetal movement: A primigravida may report fetal movement at approximately 20 weeks gestation, and a multiparous at 18 weeks gestation. Hyperemesis gravidarum is persistent vomiting that typically occurs early in pregnancy. Urologic changes: pressure from the enlarging uterus result in urinary frequency, nocturia, and bladder irritability. A 25-year-old female presents with vaginal spotting and right lower quadrant pain. There is minimal dark blood in the vaginal vault, and her cervix is closed and thick. If the pregnancy is not in the uterus, then an investigation must be carried out for an ectopic pregnancy. This section discusses the various aspects of the hormone, as well as how it is used in the diagnosis of abnormal pregnancies. After the first 7 weeks, the placenta makes its own hormones to sustain the pregnancy. False negatives may occur if: the test is performed too early (ie, before the first missed period). Electronic Doppler device can detect fetal heart tones as early as 10 weeks gestation. The body prepares not only for the development and growth of a fetus, but also for delivery. As a result of these alterations, the mother is at risk for developing complications, which can be serious in pregnancy.
Senegalia senegal (Acacia). Bactroban.
- Are there any interactions with medications?
- What is Acacia?
- Lowering cholesterol levels.
- Dosing considerations for Acacia.
- How does Acacia work?
- Are there safety concerns?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96291
Cheap 5gm bactroban fast delivery
Hemangiopericytoma Uncommon vascular tumor that can arise wherever capillaries are present skin care 77054 order bactroban 5gm with amex. Hemangiopericytomas may originate in the orbit or from the sinonasal cavities and then invade the orbit. They are aggressive lesions that can infiltrate the orbit in a multicompartmental fashion. Hemangiopericytomas may be difficult to differentiate from other rare vasculogenic tumors, such as angioleiomyoma, malignant hemangioendothelioma, and fibrous histiocytoma. Plexiform neurofibromas present as elongated cords and nodules, poorly defined, irregular, and infiltrating, sometimes suggesting the image of a "bag of worms. Well-circumscribed, ovoid or fusiform, intraconal, heterogeneous mass with density similar to brain that enhances well with contrast. Low-density areas may represent cystic, necrotic, or hemorrhagic degeneration, regions of Antoni B cells or Antoni A cells intermixed with lipid-rich Schwann cells. The optic nerve may be compressed in lesions arising in the orbital apex, or it may be engulfed by the tumor. Comments Localized neurofibromas, unrelated to any syndrome, are seen in middle-aged patients and present as a painless mass leading to nonaxial proptosis. Involvement of the eyelid is considered to be virtually pathognomonic for von Recklinghausen disease. Neurofibromatosis type 1 can also be found in patients with multiple neurofibromas. Arise from the Schwann cells of the various nerve sheaths and constitute 1% to 8% of all orbital tumors. The optic nerve is never the site of origin because it does not have Schwann cells. Usually an isolated lesion, 1% to 18% may be associated with neurofibromatosis type 2. Patients present with slowly progressive, painless proptosis, diplopia, and strabismus. Papilledema and optic atrophy with visual loss may be present with optic nerve compression. The site of origin is thought to be the ciliary nerve, ciliary ganglion, or orbital neural tissue. Present at any age, especially over age 50 y, without any gender bias, with progressive proptosis, eye motility restriction, conjunctival congestion, diplopia, papilledema, pain, and decreased vision. Five to 10% of all paragangliomas are malignant with local invasion and metastases. Sinus histiocytosis with massive lymphadenopathy is a rare benign, idiopathic, proliferative disease of phagocytic histiocytes. Predominantly, it affects children and young adults, with slight male predominance. Most patients have painless bilateral cervical, axillary, and inguinal lymphadenopathy. Extranodal involvement includes the respiratory tract, skin, nasal cavity, intracranium, and skeletal system. Orbital involvement with proptosis, limited eye movement, eyelid edema, epiphora, and decreased visual acuity is usually unilateral. Some cases have eyelid, lacrimal gland, and orbital involvement with extensive pre- and postseptal masses, but lesions can be purely retrobulbar with flattening of the globe. Sclerotic bone changes of the orbital wall are seen with sinonasal and intracranial extension. Coronal reformatted section shows a well-circumscribed, oval homogeneous mass (joystick point) with density similar to brain in the superior quadrants causing nonaxial proptosis of the left globe. Invasion of the eyelid, sinuses, and base of the skull with associated bone destruction or remodeling is common. In retrobulbar involvement the lymphoid tumor infiltrates and replaces the orbital fat by perineural and perivascular spread. The involvement may be diffuse and poorly defined but may produce an isolated, well-circumscribed and lobulated mass with irregular margins, isodense to extraocular muscles with moderate homogeneous enhancement that typically molds around existing orbital structures, such as the globe. Lymphoma may encase the optic nerve, occasionally simulating meningioma or orbital pseudotumor. Extraconal subperiosteal involvement is the result of direct infiltration of orbital bone or soft tissue by leukemic cells. Intraconal metastatic lesions appear as a discrete infiltrating mass or diffuse lesion isodense to extraocular muscles and vascular structures. Metastatic scirrhous carcinoma of the breast may produce diffuse intraconal involvement with enophthalmos. Metastatic disease of the extraocular muscles may produce an asymmetric nodular configuration of the involved muscle or a diffuse muscle enlargement. Most common primary orbital malignancy in children and most common soft tissue malignancy of childhood, arising from pluripotential mesenchymal elements in the orbit or extraocular muscles. The characteristic clinical presentation is the rapid development of a painless unilateral proptosis in a child. The presenting complaints are subacute development and progression of painless swelling, proptosis, and diplopia. It is not uncommon for orbital involvement to be the initial site of clinical presentation of lymphoma. In children with acute myelogenous leukemia, the orbital infiltration may form a mass lesion, referred to as granulocytic sarcoma or chloroma. Nearly all systematic malignancies have been reported to metastasize to the orbit (the most common source is, in descending order of frequency, breast and lung cancer, unknown primary, prostate, and melanoma; childhood tumors reported to metastasize to the orbit include neuroblastoma, Ewing sarcoma, Wilms tumor, and medulloblastoma). Metastases to fat and bone occur twice as frequently as that of extraocular muscles. Patients with orbital metastases frequently complain of diplopia, ptosis, proptosis, eyelid swelling, pain, and vision loss. Cephaloceles are extracranial herniations of intracranial contents due to partial failure of rostral neural tube closure. In naso-orbital cephaloceles, the defect occurs between the ethmoid and frontal processes of the maxilla and may pass in to the orbit, appearing as a medial orbital mass. The orbital ectodermal inclusion cysts are the most common congenital lesions of the orbit. Dermoids consist of epithelial elements plus dermal substructures including dermal appendages. They most commonly present as superficial periorbital lesions in early childhood with proptosis. Most frequently presents in childhood and teenage years with painless subcutaneous mass, fixed to underlying bone, and slowly progressing, eccentric proptosis or progressive upper lid swelling. If ruptured, sudden growth, irregular margins, and inflammatory reactions may be present. Epidermoids are less common and can be differentiated from dermoids by features similar to fluid and more homogeneous appearance. The deep (complicated, endophytic) subtype of adults may extend in to sinuses, high deep masticator space, or intracranially, and cause a dumbbell-shaped dermoid. Ruptured orbital dermoid may be associated with irregular margins and reactive inflammatory changes indistinguishable from cellulitis. There is an additional lateral extraconal mass involving the left lacrimal gland (G). Layering hyperdense fluid-fluid levels correspond to blood products from spontaneous hemorrhage. Comments Congenital hamartomatous lymphatic and venous vascular malformation; orbital lymphangiomas tend to populate the extraconal space but are often transspatial. Lymphangiomas gradually and progresssively enlarge during the growing years (do not involute). Orbital lymphatic-venous malformations occur in children and young adults, with slight female predominance. Most common clinical sign is progressive, painless proptosis with intermittent worsening. Rarely, one may see a rim enhancement in this location or a small collection of gas.
Bactroban 5gm fast delivery
The Bosniak classification is commonly used to assess cystic renal lesions (Table 27 acne zyme purchase bactroban cheap. A renal mass of homogeneous density close to water displacing the left kidney anteriorly is seen on this nonenhanced scan. An isodense anterolateral enlargement of the left kidney containing a tiny calcification (arrow) is seen on this nonenhanced scan. In this position, the tiny calcification (arrow) is moving to the most dependent portion of the kidney. A well-demarcated cyst without enhancement can be differentiated from the enhanced normal renal parenchyma. The tiny intracystic calcification is located at the most dependent portion of the renal cyst. Solid renal mass lesions are usually irregularly shaped with poor demarcation from the normal renal parenchyma. A solid renal mass lesion must be considered malignant until proven otherwise and requires prompt clinical workup, including surgical exploration. The renal mass may be indeterminate for technical reasons, such as breathing artifacts and volume-averaging effects. They correspond to types 3 and 4 in the Bosniak classification of cystic renal lesions and usually require prompt clinical workup, including percutaneous biopsy or surgical exploration. Calcifications in a focal renal lesion occur in both benign and malignant conditions. A poorly defined lesion with less contrast enhancement than the adjacent normal renal parenchyma is seen in the lateral aspect of the kidney. In addition to calcified renal cysts, aneurysms and arteriovenous malformation must be considered. In hydatid (echinococcal) disease, a larger partially calcified cyst with a thin or thick wall containing daughter cysts is diagnostic. Amorphous or punctate calcifications associated with a solid or partially cystic mass are found in a variety of benign. Diffuse renal parenchymal calcifications (nephrocalcinosis) occur most often in the renal medulla, especially in the renal papilla, where the largest urine concentration is attained. Medullary nephrocalcinosis is found with medullary sponge kidney, hyperoxaluria, and conditions associated with hypercalcemia and hypercalcinuria. Cortical nephrocalcinosis is rare and limited to diseases primarily involving the renal cortex. Nonopaque calculi account for approximately 10% of all renal calculi and consist of uric acid, xanthine, or matrix (mucoprotein/mucopolysaccharide). Perinephric fluid collections complicating a renal transplant are caused by lymphocele, urinoma, hematoma, and abscess formation. Lymphoceles are the most common peritransplant fluid collections, characteristically occurring within 2 to 3 weeks after transplantation. A well-demarcated, hypodense lesion mimicking a cyst is apparent in the lateral aspect of the left kidney on this contrast-enhanced scan. A large fluid collection (arrow) is visible in the right hemipelvis after renal transplantation. The density of the lymph in the lymphocele is similar to the urine in the adjacent distended bladder. Urinomas can occur at any time after transplantation and are caused by an anastomotic leak or are secondary to a vascular injury causing a focal necrosis with subsequent leak in the urinary system. Nevertheless, a rapid increase in the size of a failing transplant suggests acute rejection. Histologically, this benign tumor may be mistaken for a welldifferentiated renal cell carcinoma with oncocytic features. A central stellate, nonenhancing scar of lower density secondary to infarction and hemorrhage is characteristic but seen only in larger lesions (33%). After contrast administration, a homogeneous contrast enhancement that is only slightly less dense than the renal parenchyma is common, but occasionally poor tumor enhancement is found. After contrast administration, inhomogeneous tumor enhancement sparing only the fatty tissue and areas of necrosis is characteristic. Renal cell carcinomas may occasionally also contain fatty tissue and calcifications. Hypertrophy of the septal cortex (arrow) simulates an intrarenal mass lesion on urography by causing an extrinsic filling defect on the collecting system. On the precontrast scan, the lesion was isodense with the adjacent renal parenchyma and therefore not appreciated. A large solid mass with less enhancement than the adjacent renal parenchyma is seen originating from the medial aspect of the left kidney. A large, predominantly fatty lesion with mild enhancement of the nonfatty components is seen on the posterolateral aspect of the right kidney. A large, well-defined mass containing fatty foci and scattered calcifications are seen. Spontaneous rupture of an angiomyolipoma is a frequent complication resulting in a large complex renal mass with extension in to the perirenal and pararenal space, as seen here on the left side. Bilaterally enlarged and deformed kidneys containing large inhomogeneous tumor masses (angiomyolipomas) with fatty components are characteristic. Bilateral large and deformed kidneys containing huge angiomyolipomas with considerable fatty components are seen. Calcifications occur in 20% of patients and usually are central and amorphous or peripheral and curvilinear in cystic renal cell carcinomas. After contrast administration, the nonnecrotic parts of the tumor demonstrate an unequivocal increase in density, that is, less than the surrounding normal renal parenchyma, making the tumor more apparent on contrast-enhanced scans. Tumor spread to the perinephric fat, local lymph nodes and vessels, and adjacent organs can also be depicted in more advanced stages. Contrast enhancement may be heterogeneous due to varying amounts of hemorrhage and necrosis. Comments Most common malignant renal tumor, accounting for 80% of all renal primaries. Twice as frequent in men as women and rare in patients younger than 40 y (peak age 55 y). Gross hematuria (60%) and flank pain (50%) are the most common clinical presentation. Presents as large, ill-defined, heterogeneous mass centered in the renal medulla with extension in to the renal sinus and cortex and nonuniform contrast enhancement. Hematuria occasionally associated with flank pain is the most common clinical presentation. Renal calculi are present in 50% of patients, and tumor calcification occurs in 10%. The prognosis is very poor, as the tumor is usually well advanced at the time of diagnosis. Nephrogenic adenoma is an uncommon benign metaplastic response to a urothelial injury or prolonged irritation presenting as a papillary or polypoid filling defect in the renal pelvis. Larger tumors cause hydronephrosis, obliterate the peripelvic fat, and invade the renal parenchyma and vessels, but they do not affect renal contour. An inhomogeneously enhancing mass is seen in the posterolateral aspect of the right kidney (arrow). The tumor extends in to the left renal vein (arrow), which is focally enlarged and depicts filling defects. A welldefined homogeneous lesion with minimal enhancement is seen in the lateral aspect of the left kidney, mimicking a renal cyst. A renal mass (arrows) originating in the renal medulla and isodense to the normal renal parenchyma on this precontrast scan is seen in the left kidney. An enhanced rim of compressed renal parenchyma (pseudocapsule) is frequently present. Rarely, a large cyst with irregularly thickened wall and septa is the dominant feature. In adults, the tumor is virtually indistinguishable from a renal cell carcinoma, except for a large central necrosis, which is more typical for the latter.
Quality bactroban 5 gm
Diagnostic pearls: Omental caking acne gel purchase bactroban 5 gm line, bowel obstruction (subileus), and enlarged mesenteric lymph nodes. Histologically, an intraperitoneal accumulation of gelatinous, mucinous material, which usually derives from the spread of ovarian mucinous cystadenocarcinoma. Contrast media enhances solid components and improves the visibility of the septations. Lymphomas typically encase instead of invade mesenteric vessels, which may result in a "sandwich sign. Peritoneal metastases most commonly derive from ovarian, colonic, or gastric cancer. Calcification and cystic lesions on liver/spleen contour or peritoneal surface suggests ovarian cystadenocarcinoma. Omental fat is involved in 70% and appears normal, permeated with multiple discrete enhancing nodules, or as diffuse caking (omental caking). Mesenteric involvement is present in 60% mainly as diffuse or stellate soft tissue stranding. Carcinomatous type (most common): Diffuse thickening of the peritoneum, multiple mesenteric and peritoneal nodules, and fixation of the small bowel 2. Five histologic subtypes: pleomorphic, round cell, myxoid, sclerosing, and lipomalike. Diagnostic pearls: Stellate peritoneal mass or omental caking, infiltrating vessels and adjacent viscera. Large heterogeneous, solid mass typically with cystic spaces representing necrosis. Findings range from subtle mesenteric soft tissue stranding (a) to a cakelike omental mass (b). The posterior pararenal space extending from the posterior renal fascia to the transversalis fascia. This relatively thin layer of fat continues uninterruptedly as the properitoneal fat of the abdominal wall, external to the lateroconal fascia. Pancreatic, celiac, and superior mesenteric lymph nodes are usually not visible unless they are enlarged. Also, a solitary pelvic or abdominal lymph node 10 mm in diameter or a cluster of multiple small nodes are conspicuous. Appropriate bowel loops opacification with oral contrast medium is important to allow differentiation from adenopathy. Intravenous contrast material helps to distinguish strongly enhancing vascular cross sections from lymph nodes, which usually enhance less strongly. Abnormalities of the aorta and its branches such as aneurysms, atherosclerosis, thrombus formation, or dissection are best evaluated using contrast-enhanced scans acquired during the arterial phase. Optimal vessel opacification is achieved when applying bolus triggering technique (with the monitor scan placed on the aorta at the level of the celiac trunk) and contrast media flow rates of 4 to 5 mL/s. In addition, the iodine concentration of the contrast medium should be at least 350 mg I/mL. The differential diagnosis of various retroperitoneal abnormalities is given in Table 26. The inner and anterior border of the retroperitoneum is formed by the posterior peritoneum. Anterior and posterior renal fasciae fuse behind the colon and form a single lateroconal fascia. The anterior pararenal space extending from the posterior parietal peritoneum to the anterior renal fascia and confined laterally by the lateroconal fascia. It contains the ascending and descending colon, the duodenal loop, and the pancreas. Fluid collections in the anterior pararenal space, unless intrapancreatic, are usually confined to the site of origin but may sometimes extend in to the small-bowel mesentery and the transverse mesocolon, respectively. The two perirenal spaces encompass each one kidney, adrenal gland, and perirenal fat. Both spaces do not communicate across the midline, although the anterior renal fascia below the level of the renal hila occasionally appears non-interrupted. Darkened areas: anterior and posterior pararenal space; white areas: perirenal space. Diagnostic pearls: Vessel tortuosity, intimal calcification, noncalcified atheromatous plaques, and sometimes thrombus formation. Eccentric array of calcifications is an important differentiator to aortic dissection (centrally displaced intima). Crawford classification for staging: Type 1: Aneurysm from left subclavian artery to renal arteries. Type 4: Aneurysm from upper abdominal aorta and all or none of the infrarenal aorta. Surgical/interventional repair required for 1 cm/y diameter growth rate or an aneurysm size 5 cm. Diagnostic pearls: Thickened, often calcified, aortic wall; calcifications found on outer wall of dilated aorta; presence of noncalcified plaques/thrombus. Discontinuity of the aneurysm wall and periaortic hematoma are indicative of rupture. Suprarenal aortic dilation 5 cm with perianeurysmal inflammatory fibrosis and discontinuity of the right laterodorsal aneurysm wall requiring immediate surgery due to high risk of rupture (c). Indicators of the false lumen: Usually the larger lumen with delayed contrast A "beak" sign: An acute angle between the dissected flap and the outer wall Presence of cobwebs: Thin mucosal strands crossing the false lumen Intraluminal thrombus with centrally displaced intima (calcifications). In general, eccentric array of calcifications is an important differentiator to aortic dissection (centrally displaced intima). Characterized by a contrast-filled double channel with an intervening intimal flap. Intraluminal thrombosis, dilation of the aorta with compression of the true lumen, and irregular contour of the contrast-filled part of the aorta are other common findings. Irregular, septated periaortic fluid or gas collection is indicative of an infected graft. Septated periaortic fluid or gas collection is highly suspicious of abscess formation. A blood-equivalent mass lesion with rim enhancement and with or without septations may represent a pseudoaneurysm. Failure to form right subcardinal-hepatic anastomosis, resulting in atrophy of the right subcardinal vein. Comments Histologically, a cystic media necrosis from either atherosclerosis or congenital disorders. Stanford classification of dissections: Type A: Entry of dissection in ascending aorta (70%) Type B: Entry of distal to left subclavian artery (30%) Intimo-intimo intussusception is observed in cases of complete circumferential dissection. Typical complications include occlusion of the aortic side branches and continuation in to the iliac arteries. Ventral collections of perigraft gas and fluid shortly after surgery may be a normal postoperative finding. It is associated in 85% of cases with congenital heart disease; left pulmonary isomerism, polysplenia, dextrocardia, and intracardiac defects. The presence of gas bubbles within the caval filling defect indicates septic thrombosis. Comments May result from bland or septic thrombosis, but is more commonly secondary to direct tumor invasion from the kidney, adrenals, or liver. Stent fully covers the previous aneurysm (a) but shows type I endoleak at the attachment side of the iliac legs (b). Axial scan identifies infiltrating retroperitoneal lymphoma as the underlying cause. Diagnostic pearls: A distinctly enhancing, fibrous sheet/bulky mass extending from the kidneys to the sacrum. Retroperitoneal fibrosis usually displaces the ureters medially, unlike retroperitoneal lymphadenopathy, which tends to displace them laterally.
Order bactroban 5gm with visa
Ill-defined metastases due to hemorrhage are common in Kaposi sarcoma and choriocarcinoma skin care greenville sc generic bactroban 5gm on-line. Endobronchial metastases presenting with airway obstruction occur with bronchogenic, renal, breast, and colon carcinomas and melanomas. Solitary metastases are uncommon and typically originate from carcinomas of the colon (especially rectosigmoid area), kidney, testicles, and breast, sarcomas (especially bone), and melanoma. Primary pulmonary lymphoma is usually non-Hodgkin type; secondary pulmonary lymphoma is more common in patients with recurrent disease. Recurrent or secondary pulmonary involvement may result from direct mediastinal nodal extension, from lymphatic or hematogenous dissemination from distant sites, or from foci of parenchymal lymphoid tissue. Pseudolymphoma presents as localized interstitial or air-space disease with air bronchograms but without lymphadenopathy. Plasmacytoma (primary of the lung) and secondary multiple myeloma manifestations are rare (1%) and similar to lymphoma. A nodule with irregular calcifications is seen in the right lower lobe (chondrosarcoma). In this situation, the noninflated posterior edge of the lower lobe may easily be mistaken for the diaphragm with pleural fluid posteriorly and peritoneal fluid anteriorly. Similarly, inversion of a hemidiaphragm by massive pleural effusion may also simulate intra-abdominal fluid. However, a correct diagnosis usually is possible by analyzing the relationship of both fluid collection and the lower lobe on subsequent transverse images and multiplanar reformations. Both pleural and peritoneal fluid presents as an arcuate or semilunar density displacing liver and spleen inward from the adjacent chest wall. The entity of the fluid collections can be assessed based on a variety of different criteria. Pleural fluid may surround the lung, whereas peritoneal fluid may be surrounded by the lung bases. In the posterior costophrenic angle, pleural fluid is posterior to the diaphragm, causing anterolateral displacement of the crus, whereas peritoneal fluid is anterior to the diaphragm. When scrolling through transverse images in a craniocaudal direction, pleural fluid gradually diminishes, whereas peritoneal fluid increases in size, progressively extending lateral to the liver and spleen. Fluid seen posterior to the liver is within the pleural space, as the peritoneal space does not extend in to this region (the bare area of the liver is not covered by peritoneum). The interface of pleural fluid with the liver or spleen is hazy, whereas with peritoneal fluid, it is sharp. Unilateral or bilateral pleural effusions not associated with any other signs of intrathoracic disease are often tuberculous in younger patients and predominantly neoplastic in the elderly. The latter describes a nonmalignant pleural effusion and ascites in the presence of benign or malignant ovarian tumors, or occasionally a uterine leiomyoma. Starting from the inside, this line represents the visceral and parietal pleura, extrapleural fat, endothoracic fascia, and innermost intercostal muscle. The latter is absent in the paravertebral region, resulting in a distinctly thinner lining. On axial scans, the most posterior ribs are always the lowest in the thoracic cage, with each more anterior rib arising from the level of a vertebral body above. The pleural line may be distinctly thicker in obese patients due to excessive extrapleural fat. This condition can usually be differentiated from pleural disease by its perfect symmetry. Pleural fluid initially collects in the most dependent portion of the pleural space, which is posteromedial and caudal to the lung base in the supine position. Small amounts of fluid usually appear crescent- or lenticularlike, but it may also be impossible to differentiate a discrete pleural effusion from pleural thickening. In these cases, freely mobile fluid can be diagnosed by obtaining an additional set of images in a prone or lateral decubitus position. Furthermore, after intravenous contrast medium administration, a thickened, inflamed, or neoplastic pleura enhances, whereas purely fibrotic pleural thickening and pleural fluid do not. Larger pleural effusions extend toward the lateral chest wall and may enter the major fissure, where the fluid tapers medially, producing a characteristic "beak" sign. A large right tension pneumothorax with shifting of heart and mediastinum to the left. The collapsed right lung still adheres locally to the lateral and posterior chest wall. Right pleural effusion presents as a lowdensity, crescent-shaped lesion posterior to the lung base that has a higher density because of compression atelectasis and edema (a). More caudally, the pleural effusion encircles the posteromedial aspect of the liver, creating a hazy interface (b). Ascites presents as a low-density, crescent-shaped lesion anteromedial to the liver with sharp interface (a). More caudally, the ascites extends to the right side of the liver but spares its posteromedial margin (b). A low-density, lenticular-shaped lesion between high-attenuating thickened layers of parietal and visceral pleura ("split pleura" sign). Regarding collagen vascular diseases, both rheumatoid disease and systemic lupus erythematosus (primary and drug-induced) often present with pleural effusion as the only intrathoracic manifestation. Congestive heart failure is the most common cause of pleural effusion, but it usually is associated with an enlarged cardiac silhouette and other signs of cardiac decompensation. In Dressler syndrome, pericardiac and pleural effusions typically develop 2 to 3 weeks after myocardial infarction or pericardial surgery. However, occasionally they may occur months or even years after the causative episode. Traumatic and postsurgical pleural effusions are common, but both history and associated findings are usually diagnostic. Myxedema, familial Mediterranean fever (familial paroxysmal polyserositis), and primary lymphedema are rare inherited conditions presenting with pleural effusion as the only intrathoracic abnormality. Empyema is a purulent pleural infection usually secondary to a bacterial pneumonia. Other less frequent extrapulmonary sources include bacteremia, subphrenic abscess, spondylitis, thoracotomy, and penetrating chest trauma. An empyema has to be differentiated from a parapneumonic effusion, which is an uninfected (sympathetic) serous exudate in pneumonia that resolves spontaneously. Large empyemas may compress the neighboring lung, resulting in gradual displacement and bowing of the adjacent pulmonary vessels and bronchi. The visceral and parietal pleural layer appears relatively thin, smooth, and of uniform thickness but strongly enhances on postcontrast scans. Nonenhancing pus thus becomes clearly visible between both pleural layers ("split pleura" sign). It is sharply demarcated from lung parenchyma and forms an obtuse angle with the chest wall. In an organizing empyema, the walls may become thickened and eventually even calcified. Demonstration of fluid collections within the thickened pleural peel is highly suspicious of a still ongoing and active infection. An empyema has to be differentiated from a peripheral lung abscess abutting the pleural surface. An empyema (right lung base) is lenticular-shaped and welldefined by smooth, uniform margins (split pleura sign). It creates acute angles with the chest wall, and the outer margin appears ill-defined and irregular. Extensive pleural thickening caused by fibrosis may result in encasement of the lung, resulting in restriction and loss of volume.
Cheap bactroban 5 gm
Signs of an imminent aortic aneurysm rupture are soft tissue stranding of perianeurysmal fat and local lung atelectasis skin care reddit order bactroban amex. Comments Common conditions associated with aortic aneurysm are atherosclerosis, cystic medial necrosis (including Marfan disease), trauma, and mycotic infection. An aneurysm just distal to the origin of the left subclavian artery is likely due to closed trauma. Crawford classification for staging: Type 1: Aneurysm from left subclavian artery to renal arteries Type 2: Aneurysm from left subclavian artery to aortic bifurcation Type 3: Aneurysm from descending aorta to aortic bifurcation Type 4: Aneurysm from upper abdominal aorta and all or none of the infrarenal aorta Surgical/interventional repair required for 1 cm/y diameter growth rate or diameters 5. Histologically, a cystic media necrosis from either atherosclerosis or congenital disorders. Stanford classification of dissections: Type A: Entry of dissection in ascending aorta (70%) Type B: Entry of distal to left subclavian artery (30%) Intimo-intimo intussusception is observed in case of complete circumferential dissection. Typical complications include occlusion of aortic side branches and continuation in to iliac arteries. Fusiform aneurysm of the ascending aorta (a) without involvement of the aortic arch or supra-aortic vessels (b). Soft tissue stranding of perianeurysmal fat and local lung atelectasis are highly suspicious of an imminent aortic rupture. A contrast-filled double channel spirals down the entire aorta and also involves supra-aortic vessels (Stanford type A) (b). The false lumen is the smaller lumen, recognizable by the beaklike angulation with the aortic wall and presence of intraluminal cobwebs (c). Stanford type B aortic dissection (a) with a partly thrombosed larger false lumen (b). Protocols for aortic imaging should always begin with noncontrast helical images of the chest. On postcontrast scan, hypoattenuating as compared with hyperattenuating aortic lumen ("flip-flop" pattern) is common. Widespread smooth wall thickening and narrowing of the aorta and adjacent major vessels. Diagnostic pearls: Concentric smooth wall thickening and local aortic and arterial stenosis. Dystrophic wall calcifications may occur, also homogeneous involvement of large supra-aortic arteries. Penetrating atherosclerotic ulcer induced by rupture of an intimal atherosclerotic plaque, allowing blood to gain access to the aortic media. Disease of unknown etiology, which is typically observed in Asian countries/populations. Histologically, the inflammation starts with a mononuclear infiltration of the adventitia, followed by granulomatous changes in the media and subsequent fibrosis and thickening of the intima and media. Collateral pathways include the posterior system (azygos-hemiazygos vein/paravertebral veins), the anterolateral system (internal mammary veins/ anterior thoracic veins), and the superior system (anterior jugular venous system/external jugular vein/ transverse arch). Diagnostic pearls: Diagnosed by visualization of underlying cause and the exact level of the occlusion, as well as display of collateral pathways. Tortuous intercostal arteries serve as collaterals and thus lead to marked inferior rib notching. Two aortic arches form a complete vascular ring that can compress the trachea and/or esophagus. Diagnostic pearls: the arches may compress both sides of the trachea, usually more on the right side. Most commonly, there is a larger (dominant) right arch behind and a hypoplastic left aortic arch in front of the trachea/esophagus. The two arches join posteriorly to form the descending aorta which is usually on the left side (but may also be right-sided or in the midline). The right subclavian and common carotid arteries arise from the right arch and the left from the left arch. The right subclavian artery arises as the last branch of the aortic arch and crosses the mediastinum from left to right behind the trachea and the esophagus. Diagnostic pearls: Tubular opacity behind the esophagus in contiguity with the aberrant right subclavian artery, which is seen on the right posterior aspect of the trachea. A rare congenital abnormality but one of the two most common forms of vascular ring, a class of congenital anomalies of the aortic arch system in which the trachea and esophagus are completely encircled by connected segments of the aortic arch and its branches. Although the double aortic arch has various forms, the common defining feature is that both the left and right aortic arches are present. Seventy-five percent occur in the left descending aorta, and the smaller arch is usually (80%) anterior. Double aortic arch Left aortic arch/aberrant right subclavian artery (continues on page 658) Mediastinal Vessels 657 a b c. Penetrating atherosclerotic ulcer of the aorta: hypodense atheroma with central ulceration at the flow of the aortic arch (c). Widespread smooth wall thickening of the aorta, dystrophic wall calcifications in the aortic arch, local stenosis of the distal aorta, and homogeneous involvement of large supra-aortic arteries. Near occlusion of the superior vena cava due to infiltration of central bronchogenic carcinoma with collateral flow through an enlarged azygos vein (visible on the left side, just above the left atrial appendage). Diagnostic pearls: In both types, the aortic arch passes and descends to the right of the trachea. The left common carotid artery is the first branch, whereas the left subclavian artery is the last, taking a retropharyngeal course. The left innominate artery originates as the first branch of the aorta, and there is no visible retroesophageal vessel. Diagnostic pearls: Transversely oriented right aortic arch causes impression of the posterior trachea and descends on the left side. Persistent left anterior and common cardinal vein that drains via the coronary sinus in to the right atrium. Traumatic Mediastinal hemorrhage or hematoma Diffuse mediastinal widening, commonly in upper mediastinum. Diagnostic pearls: Ill-defined mediastinal mass with direct relationship to larger vessels. Hyperdense contrast streaks/pools on postcontrast scans are indicative of an Hb-relevant bleeding. Diagnostic pearls: Anterior mediastinal mass sometimes with presence of phleboliths; well-defined mass with heterogeneous attenuation; small ringlike or round calcifications (phleboliths) in one third of cases; on postcontrast scans, heterogeneous (often delayed) attenuation. Histologically, hemangiomas are endothelial-lined vascular channels with admixed fibrosis and sclerosis. The aortic arch passes and descends to the right of the trachea, aberrant left subclavian, taking a retropharyngeal course. In addition, proper patient preparation and use of bolus triggering or test bolus calculation at the level of the aortic root are critical for sufficient image quality. Motion or reconstruction artifacts and/or vessel calcifications are typical reasons to overcall the degree of coronary artery stenosis. Thus, it is useful to apply near-bone window/level settings for better appreciation of these lesions. Functional assessment is usually done by using short- or long-axis reformations, which are cut perpendicular to each other, the level of atrial valves, and the myocardial septum. Intrathoracic nonvascular calcifications are usually harmless sequelae of bygone processes. They occur in the lung parenchyma, mediastinum, hilar and mediastinal lymph nodes, pleura, and chest wall, or in any combination of these structures. The cause of calcifications may be determined by means of the location and pattern of calcifications, as well as knowledge of associated clinical features. Apart from vascular lesions, the most common cause of thoracic calcifications is a previous infection. Less often they may be due to neoplasms, metabolic disorders, occupational exposure, or previous medical therapy. Usually the plaque is nicely visualized as a hypodense area within hyperdense vessel. Atherosclerotic risk factors (see Framingham risk factors) initiate vascular stress with subsequent local vascular inflammation, progressive intimal thickening, and finally stenosis. Presence of contrast material distal to a total occlusion may be due to collateral flow and not indicative of a remaining lumen.