Purchase 3 mg risperidone visa
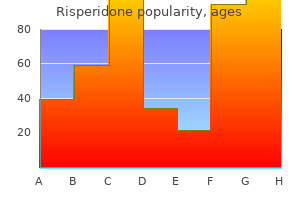
Although 27 patients had inadequate margins treatment atrial fibrillation order risperidone now, only three developed local recurrence, all within the first 2 years after diagnosis. The most common anatomic site for inadequate margins was the popliteal region near the vascular and neural structures, where 20 of 140 patients were found to have inadequate margins (either marginal or intralesional). Locally persistent disease developed in only 3 of 15 patients with inadequate margins associated with lesions around major joints locally persistent disease. The intramedullary canal was the site of inadequate margins in 20 of 237 patients, and local recurrence developed in 6 patients. It is of interest that 7 of the 11 patients with intralesional surgical margins and 16 of the 21 with contaminated margins did not have local recurrence. These findings could not be explained on the basis of poor survival or early death. The observation is believed to be related to the effectiveness of preoperative chemotherapy at producing tumor necrosis and the development of a "mature" capsule surrounding the tumor where satellite tumor nodule formation had been suppressed. Limb-sparing procedures were performed in 136 patients (83%), 18 patients (11%) had amputation, and 10 (6%) had rotationplasty. In amputations, 18 margins were wide or greater; in rotationplasty, nine were wide and one was intralesional. In the limb salvage procedures, 110 patients had wide margins, 12 were marginal, seven had intralesional margins, and seven had wide contaminated margins. Although 27 patients had inadequate margins, only three experienced local recurrence, all within the first 2 years after diagnosis. It may also relate to the ability of the surgeon in conjunction with the pathologist to accurately determine whether margins are truly wide because the soft tissues around the tumor move about during the operation and after the specimen has been removed, making it difficult to accurately determine whether a margin is wide, marginal, or intralesional even when the specimen is inked. Adequate surgical resection is certainly a worthwhile goal, but the causes of local recurrences are probably more complex than adequacy of margin. Surgical Treatment the goal of surgical management is complete resection of the tumor with a cuff of normal tissue surrounding the tumor (wide resection). This can be accomplished with either amputation or local resection as long as this goal is achieved. What is known comes from retrospective analyses of tumor specimens and from outcomes of patients treated in clinical trials. To identify the potential risks of delaying resection to prepare for limb-sparing surgery versus immediate amputation, the results of data on 279 patients treated at Memorial Sloan-Kettering between 1975 and 1984 were reviewed retrospectively. Sixty-three patients who completed primary local control surgery (amputation primarily, although this is not clear in the report) and adjuvant chemotherapy were compared with patients who had primary preoperative chemotherapy followed by local control surgery and adjuvant chemotherapy. The Kaplan-Meier estimates for the three surgical groups revealed no significant difference in continuous disease-free and ultimate survival rates for each group (Mantel-Cox test, P =. The continuous disease-free survival rate for the entire group was 42%, with an overall survival rate of 55% at 5 years. Outcome results showed that one-third of patients with limb-sparing procedures required at least one additional surgical procedure, and one-fourth eventually required amputation. Seventy-three patients had limbpreserving procedures, 115 had above-knee amputations, and 39 had hip disarticulations. The Kaplan-Meier estimate of the disease-free survival rate for all patients at 10 years was 41%. Fourteen of the original 17 patients experiencing a local recurrence in the first study did so within the first 2 years after the index procedure, and only one of the original 17 patients survived. There were nine local recurrences after above-knee amputations and eight after limb-sparing procedures. No patient who had a hip disarticulation (radical margin) experienced a local recurrence. Although the function of patients with limb-sparing procedures was superior to that of both the amputation and disarticulation groups, no differences could be identified regarding patient acceptance or psychosocial outcome (quality of life [QoL]) among the three operative groups. Advances in chemotherapy, imaging technology, implant design and materials, and subspecialization in orthopedic oncology have reversed the trends of previous decades. Limb preservation, however, has not altered disease-free survival rates when compared with ablative procedures. Although limb-sparing surgery in appropriately selected patients appears to be safe from an oncologic viewpoint, it is not clear that functional outcome and QoL are superior in limb salvage patients compared with those who have undergone amputation. Most patients prefer to keep their limbs, however, and limb-sparing procedures are now routinely offered. Problems associated with limb sparing include an increased early complication rate of 25% to 35%. Lindner and associates,180 from the University of Muenster, reported the results of their study with 133 patients who had high-grade osteosarcoma of the extremities treated with intravenous neoadjuvant chemotherapy and surgery between 1978 and 1994. Seventy-nine patients had limb-preserving procedures, including 32 with endoprosthesis, 39 with allograft replacement, six with autograft reconstruction, and two with shortening procedures. Twenty of the 39 patients with allografts experienced a major complication, and 6 of the 20 patients required removal as well. Ten of the 21 patients with rotationplasty also experienced major complications, but none required revision to amputation. Eight of the 33 patients who were treated with transmedullary amputation experienced a major complication, and three of the eight required a more proximal reamputation. Lindner and associates concluded that the extent of preoperative primary tumor necrosis, surgical margins, and tumor volume were the most important oncologic prognostic factors and that functional outcome after rotationplasty was superior to that of amputation and other limb-preserving techniques. A minimum of a "wide" margin should be achieved for adequate local control of high-grade primary sarcomas of bone. If there is invasion of a major peripheral nerve from lesions arising around the knee, then the equivalent of a wide amputation should be performed, but this is a rare occurrence. If the nerve is spared, then consideration may be given to limb-sparing resection. In the early days of limb salvage, most surgeons desired 1 cm or more of soft tissue and 7 to 10 cm of uninvolved bone marrow when performing resections or amputations. As more experience has been gained and neoadjuvant chemotherapy has come into common use, the "acceptable" thickness of the margins has decreased for most surgeons, but it is unclear how close is too close to the tumor before risk of local recurrence increases. Most surgeons now are accepting 1- to 3-cm bone marrow margins and soft tissue margins in the millimeter range (avoiding "ink on tumor"), especially if the histologic response is good. One problem is that the response is not known predictably until the resection has been carried out. Suffice it to say that this issue has not been resolved, and the margins that are accepted vary depending on the experience and judgment of the surgeon and treatment team on any given case. It is clear that intralesional margins are likely to lead to local recurrence, especially if there has been a poor response, but some osteosarcomas recur despite wide margins and good histologic response, suggesting that the aggressiveness of the tumor may play an important but at this point undefined role. Once the decision whether to perform amputation or limb salvage has been made, it is necessary to decide on the type of reconstruction. This requires lengthy discussion with the patient and, in the case of pediatric patients, the parents. The type of reconstruction varies with the location and extent of the tumor, the age of the patient, the experience of the surgeon, and the desires of the patient. In general, patients who desire unrestricted athletic activities are encouraged to have amputations or rotationplasty in the lower extremity because they are more durable options and not subject to mechanical failure, loosening, or fracture. Patients who are more concerned with preserving the limb must first undergo careful imaging to ensure resectability and must understand the various reconstruction options. The surgeon and radiologist must critically assess these studies to determine whether the major neurovascular structures are free of the tumor and the extent of tumor in the medullary cavity and in the soft tissues. If sufficient muscle cannot be preserved, soft tissue healing may be problematic, and the muscle power of the limb will be compromised. The presence or absence of tumor extending into the adjacent joint will determine whether an intraarticular resection or extraarticular resection can be carried out, and this will affect the type of reconstruction. Intraarticular resections that preserve the joint muscles and adjacent bone are reconstructed with tumor prostheses, osteoarticular allografts, or allograft-prosthetic composites. Resection arthrodesis was used exclusively by some surgeons in the past, but is less commonly performed today for lesions around the knee or shoulder. Extraarticular resections around the knee that include the patella and quadriceps mechanism can be treated with allograft-prosthetic composites that use a tibial graft with a patella and quadriceps that can be repaired to the host quadriceps tendon as an alternative to arthrodesis, amputation, or rotationplasty. The age of the patient has a major influence of the type of reconstruction that is chosen.
Buy 4 mg risperidone visa
Further delays may lead to increased radiation-induced fibrosis treatment zit purchase 3mg risperidone with visa, more challenging operations, longer operating times, and increased lengths of stay. Surgery is often followed with an additional 2 to 3 cycles of adjuvant chemotherapy but may vary based on the final pathologic features and regimens received previously. Foremost, neoadjuvant therapy allows the early administration of systemic therapy to address potential micrometastatic disease that is not appreciated on initial staging studies. Additionally, it serves as a tool for patient selection, sparing the morbidity of surgical resection for patients whose initially subclinical metastatic disease becomes apparent on subsequent restaging scans. It does have the advantage of downstaging borderline resectable patients who achieve a partial response with therapy, allowing them to undergo surgery with a higher likelihood of an R0 resection. In patients with limited performance status or significant comorbidities single-agent treatment can provide clinical benefit. Data from randomized trials or metaanalysis suggest that systemic chemotherapy provides a significant survival benefit over best supportive care alone, both for first-line and second-line treatment. The best regimen to use for neoadjuvant therapy in this setting is not established, but most centers use similar regimens as for locally advanced or unresectable disease. Grade 3 or 4 adverse events that were seen more often with combined therapy included neutropenia (38% versus 27%), febrile neutropenia (3% versus 1%), fatigue (17% versus 7%), diarrhea (6% versus 1%), and neuropathy (17% versus 1%). Longer follow-up identified some long-term (>3 years) survivors in the nab-paclitaxel/ gemcitabine arm. Gemcitabine and capecitabine: Standard-dose gemcitabine has also been compared with gemcitabine plus twice-a-day capecitabine at various doses. Single-agent capecitabine (1250 mg/m2 orally, twice daily for 14 of every 21 days) provides clinical benefit response and could be considered as an alternative to single-agent gemcitabine in patients with moderate performance status. In the United States, the doses have been reduced and adjusted due to concerns of greater toxicity seen here. A variety of cytotoxic agents, either alone or in combination, have been evaluated, although primarily in the context of small single-arm or retrospective studies. Single-agent capecitabine is well tolerated and can be considered in patients with moderate performance status. If the disease relapse is locoregional only, chemoradiation can be performed as detailed later if no prior radiation was given. Regarding chemotherapy, if relapse occurs more than 6 months after completion of adjuvant therapy, the same regimen can be considered. Although resection of liver metastases have shown mixed results in terms of improving survival compared with a palliative procedure only,306,307 pulmonary,127,308 liver309 and brain310 metastasectomy have improved survival in a carefully selected group of patients with limited disease burden. Recurrence after adjuvant chemotherapy Radiation for Locally Advanced Disease the role of chemoradiation in patients with locally advanced disease is unclear. Chemoradiation can be considered for patients with locally advanced disease with adequate performance status to provide consolidative local therapy and potentially downstage approximately 10% to 15% of patients to allow them to undergo surgical resection. However, chemoradiation may be preferred to be given first if patients are having pain or obstructive symptoms from the tumor. Regardless of the order, a total of at least 6 cycles of systemic chemotherapy are typically given either before or after chemoradiation. In some cases, patients will continue chemotherapy until progression or treatment-related toxicity becomes prohibitive. Gemcitabine can be given at full dose (1000 mg/m2 weekly) safely during the radiation. Patients were then given gemcitabine with or without erlotinib after completing chemoradiation. However, it is delivered over one to five treatments as opposed to 25 to 30 treatments and uses a smaller margin around the tumor to limit dose to normal tissues. The dose of radiation per day is also higher (5 to 25 Gy) as opposed to standard therapy (1. Metal stents are recommended because they have a larger diameter, lower occlusion rates, and lower complication rates than plastic stents, but they can become embedded in the bile duct and be more difficult to replace. This is more uncommon today because higher quality imaging can better predict resectability. Both surgery and endoscopy have similar success rates for palliating jaundice; however, surgical intervention has a longer hospital stay and a higher complication rate and is typically reserved for patients who are already in surgery or in whom endoscopic maneuvers fail. Similar to the above, surgical decompression can be done when patients are found to be unresectable during surgery and can prevent future gastric outlet obstructions. Surgical bypass may also be considered in patients with longer life expectancies because it has a lower failure rate than stents and better long-term outcomes, but it is more expensive, prolongs the hospital stay, has a higher complication rate, and has a longer time to resumption or oral intake. It is clear that planned palliative resections lead to increased morbidity and mortality rates and worse QoL compared with surgical bypass alone; therefore resections should not be attempted when gross tumor will be left behind. Management with oral opioids is the first step; however, onethird of patients cannot obtain reasonable pain control with oral medications alone. The celiac plexus is a dense network of nerves that innervates the upper abdominal organs. Pain may be relieved by inhibiting synaptic pathways within the plexus without nerve destruction. It is a common symptom affecting 64% to 100% of patients with pancreatic cancer, even those who have not had surgery. If reaccumulation requires more than once-weekly paracentesis, placement of a long-term drainage catheter is a suitable option and commonly done in many centers. Assessing the serum-to-ascites albumin gradient is helpful in confirming the cause and guiding treatment approaches. Emerging data from genome-wide association studies suggest that inherited single-nucleotide polymorphisms that affect expression of certain genes. One patient developed a partial response, and three patients developed disease stability. Vascular invasion in pancreatic cancer: Imaging modalities, preoperative diagnosis and surgical management. Preoperative/neoadjuvant therapy in pancreatic cancer: a systematic review and meta-analysis of response and resection percentages. Preoperative capecitabine and concurrent radiation for borderline resectable pancreatic cancer. Epidemiology and potential mechanisms of tobacco smoking and heavy alcohol consumption in pancreatic cancer. Major molecular markers in pancreatic ductal adenocarcinoma and their roles in screening, diagnosis, prognosis, and treatment. Pancreatic intraepithelial neoplasia: a new nomenclature and classification system for pancreatic duct lesions. Five years of prospective screening of high-risk individuals from families with familial pancreatic cancer. Phase 2 multi-institutional trial evaluating gemcitabine and stereotactic body radiotherapy for patients with locally advanced unresectable pancreatic adenocarcinoma. Palliative care and the aggressiveness of end-of-life care in patients with advanced pancreatic cancer. Vascular invasion in pancreatic cancer: imaging modalities, preoperative diagnosis and surgical management. Clinical calculator of conditional survival estimates for resected and unresected survivors of pancreatic cancer. Neoadjuvant chemoradiotherapy for adenocarcinoma of the pancreas: treatment variables and survival duration. Preoperative gemcitabine-based chemoradiation for patients with resectable adenocarcinoma of the pancreatic head. Neoadjuvant therapy may lead to successful surgical resection and improved survival in patients with borderline resectable pancreatic cancer. Adjuvant chemotherapy with gemcitabine vs observation in patients undergoing curative-intent resection of pancreatic cancer: a randomized controlled trial. Fluorouracil-based chemoradiation with either gemcitabine or fluorouracil chemotherapy after resection of pancreatic adenocarcinoma: 5-year analysis of the U. Adjuvant chemoradiation for pancreatic adenocarcinoma: the Johns Hopkins Hospital-Mayo Clinic collaborative study.
Diseases
- Anemia, hypoplastic, congenital
- Osteodysplasia familial Anderson type
- Hydrops fetalis
- Procarcinoma
- Warburg Sjo Fledelius syndrome
- Reductional transverse limb defects
- Oral facial digital syndrome
- X-linked mental retardation Hamel type
Buy discount risperidone 3mg online
Magnetic resonance imaging combined with artificial erection for local staging of penile cancer medicine 666 discount 4 mg risperidone otc. Risk stratification in penile carcinoma: 25-year experience with surgical inguinal lymph node staging. The role of ultrasound-guided cytology of groin lymph nodes in the management of squamous cell carcinoma of the vulva: 5-year experience in 44 patients. Ultrasonography-guided fineneedle aspiration cytology before sentinel node biopsy in patients with penile carcinoma. Squamous cell carcinoma of the penis: accuracy of tumor, nodes and metastasis classification system, and role of lymphangiography, computerized tomography scan and fine needle aspiration cytology. Nieweg, Simon, horenblas, reliability and safety of current dynamic sentinel node biopsy for penile carcinoma. Regional lymph node staging using lymphotropic nanoparticle enhanced magnetic resonance imaging with ferumoxtran-10 in patients with penile cancer. Regional lymph node staging using lymphotropic nanoparticle enhanced magnetic resonance imaging with ferumoxtran-10 in patients with penile cancer-comment. What surgical resection margins are required to achieve oncological control in men with primary penile cancer The histological extent of the local spread of carcinoma of the penis and its therapeutic implications. Intra-arterial chemotherapy in locally advanced or recurrent carcinomas of the penis and anal canal: an active treatment modality with curative potential. The rosebud technique for creation of a neomeatus after partial or total penectomy. Correlation between the extent of nodal involvement and survival following groin dissection for carcinoma of the penis. Extensive inguinal lymphadenectomy improves overall 5-year survival in penile cancer patients: results from the surveillance, Epidemiology, and end results program. Prophylactic bilateral groin node dissection versus prophylactic radiotherapy and surveillance in patients with n0 and n1-2a carcinoma of the penis. Neoadjuvant taxanebased combination chemotherapy in patients with advanced penile cancer. Extra-anatomic lateral bypass combined with embolization of the femoral stump for management of groin infection and bleeding due to metastatic carcinoma of the penis. Intra-arterial infusion chemotherapy for penile carcinoma with deep inguinal lymph node metastasis. Cisplatin, methotrexate and bleomycin for the treatment of carcinoma of the penis: a southwest oncology group study. Chemotherapy with cisplatin and 5-fluorouracil for penile and urethral squamous cell carcinomas. Combination chemotherapy with methotrexate, bleomycin and cisplatin for advanced squamous cell carcinoma of the male genital tract. Prognostic factors influencing survival from regionally advanced squamous cell carcinoma of the penis after preoperative chemotherapy. A combination of cisplatin and 5-fluorouracil with a taxane in patients who underwent lymph node dissection for nodal metastases from squamous cell carcinoma of the penis: treatment outcome and survival analyses in neoadjuvant and adjuvant settings. Bothadjuvant chemotherapyandadjuvant low-doseradiotherapyto retroperitoneallymphnodescan reducetheriskofrelapse,although inthemajorityofpatients surveillancewithoutadjuvant treatmentisreasonable. Because of their young age, patients who have been cured are at risk of long-term, treatment-induced toxicity. An understanding of staging and risk assessment is crucial if (1) patients with good risk features are not to be overtreated and exposed to undue toxic risks and (2) patients with poor risk features are to receive adequate (curative) therapy. There is also growing support for the concept of transplacental damage to the fetal gonad by maternal estrogen levels as a contributing causative agent of germ cell cancer. This cytogenetic abnormality has been reported in carcinoma in situ tissue, suggesting that it is an early marker, if not a cause, of germ cell tumorigenesis. Similarly, i(12p) is found in malignant tissue of diverse histologic types that has developed from the malignant transformation of teratoma, which is a component of nonseminomatous germ cell cancers. It has an important role in cellular proliferation, and its expression is tightly regulated throughout the cell cycle. The risk is highest (at approximately 5%) when a cryptorchid testis is retained intraabdominally, falls to 1% if retained in the inguinal canal, and appears to fall further if the undescended testis is surgically placed in the scrotum (orchiopexy) before 6 years of age. In phenotypically female but genotypically male patients, this syndrome may be mistaken for ovarian cancer. Brothers or sons of affected patients have a 6- to 10-fold increased risk of developing the disease in their lifetime. This leads to activation of a cascade of biochemical and physiologic responses that are involved in the mitogenic signal transduction of normal and malignant cells. Testicular cancers that are of nongerminal origin include specialized gonadal stromal neoplasms and sarcomas. These, in addition to adenocarcinoma (of the rete testis) and secondary (nonprimary) malignancies such as acute leukemia, lymphoma, other carcinomas, and melanoma, comprise less than 5% of testicular neoplasms. The frequency and natural history of specific histologic subtypes are discussed in subsequent sections and summarized in Table 83. Pure choriocarcinoma is an exception, characterized by early hematogenous dissemination to lungs, brain, and viscera. It is extremely unusual for seminomas to present with hepatic or pulmonary metastases; when they do, it is virtually always in the setting of retroperitoneal nodal involvement. A right-sided testicular primary is most frequently found to have interaortocaval nodal metastases, followed (in order of decreasing frequency) by the precaval and preaortic nodes. In this model, the normal embryonic development counterpart of seminoma is the spermatocyte, whereas pluripotential early cleavage stage tissues are the counterpart of embryonal cell carcinoma. More differentiated malignancies find their normal tissue counterparts in tissues derived from the developing embryo, such as the embryo itself (teratoma), the yolk sac (yolk sac tumors), and the placenta (choriocarcinoma). A commonly used histologic classification of testicular neoplasms is derived from the Armed Forces Institute of Pathology classification schema of Dixon and Moore,35 which recognizes pure seminoma and four other categories, each of which may occur with or without seminoma elements: (1) embryonal carcinoma, (2) teratoma, (3) teratoma with foci of embryonal carcinoma and choriocarcinoma (also termed teratocarcinoma), and (4) choriocarcinoma with and without embryonal elements. Clinically, the most important distinction is between pure seminomas and all other cancers with nonseminomatous components. Distinguished histologically from classic seminoma by relative lack of fibrovascular septa and lymphoid infiltrate, and by marked variation of cell size, but not shape. Compared with seminoma (A), note cellular and nuclear pleomorphism and syncytial pattern (loss of cellular borders). Note fibrovascular septa with lymphoid infiltrate characteristic of seminoma and islands of embryonal carcinoma. Syncytiotrophoblastic cells (giant cells with hyperchromatic nuclei and abundant eosinophilic cytoplasm) are visible in the upper right quadrant. Cytotrophoblasts (sheets of cells with single nuclei and abundant clear cytoplasm) comprise the midportion of this photomicrograph. Hemorrhagic infiltrate at the bottom of the photomicrograph is common in choriocarcinoma. Left testis tumors most frequently have nodal spread to the left paraaortic, preaortic, and interaortocaval nodes, in that order. Suprahilar nodal involvement does not occur in patients with microscopic or low-burden infrahilar disease (stage B1; see later), whereas 25% of patients with gross infrahilar disease have been found to have positive suprahilar nodes. More than 75% of nonseminomas have been reported to have variable amounts of teratomatous elements, so that "pure" teratomas must be sampled carefully to exclude undifferentiated foci. The term teratocarcinoma refers to teratomas in combination with other elements, although some pathologists reserve the term for the combination of teratoma and embryonal carcinoma. When a teratoma has cellular and active stroma with mitotic figures, it is referred to as immature teratoma. Teratomas and teratocarcinomas are composed of solid and cystic spaces on cut surface, with areas of hemorrhage and necrosis. A histologic mix of fully differentiated cartilage, muscle, or epithelial tissue and malignant embryonal elements is seen. Predominant teratomatous features account for one-third of teratocarcinomas, whereas approximately two-thirds of teratocarcinomas are mostly composed of nonteratomatous elements.
Purchase genuine risperidone on-line
Clearly treatment zone tonbridge order generic risperidone from india, resecting a growth center has growth consequences similar to those of irradiating one and, depending on the age of the child, has to be addressed with contralateral epiphysiodesis or an expandable prosthesis. The complications of surgical limb salvage were discussed in the section on osteosarcoma. Secondary Malignancies In 1979, Chan and coauthors408 reported that among 24 patients with primary Ewing sarcoma of the pelvis who had survived for 5 years, four patients experienced secondary malignancies within the irradiated fields and died. Also, Strong and associates409 reported an increased hazard of developing secondary malignancy in patients who were treated with radiation therapy, with a cumulative cancer risk of 35% over 10 years. The administration of intensive chemotherapy in five or more courses appeared to exert an enhancing effect, increasing the rate of development of new tumors. Li410 also reported a 12% risk of developing a new cancer in 15 of 410 patients who survived childhood cancers. Tucker and coworkers411 estimated the subsequent risk for bone cancer in 9170 patients who survived 2 or more years. Data on treatment were evaluated on 64 patients in whom bone cancer developed after childhood cancer. The dose-response appeared to reach a 40-fold risk after doses to bone of more than 60 Gy. Similar numbers of patients were treated with orthovoltage and megavoltage, and the patterns of risk among categories of doses did not differ according to the type of voltage. Also, after adjustment for radiation therapy, treatment with alkylating agents appeared to increase the subsequent risk of bone cancer. Coleman412,413 reported that an average latent period for development of treatment-induced solid tumors was 10 to 15 years, with a 10% actuarial risk at 10 years for pediatric patients. The actuarial risk for a second malignancy at 5 years was 8%, with a 4% risk for a secondary bone sarcoma. A study of secondary malignancy in 397 patients who were treated for Ewing sarcoma at the Mayo Clinic over a 25-year period showed that 26 patients (6. The mean age of the patients was 16 years, and the interval from the diagnosis of the Ewing sarcoma to the development of the secondary malignancy averaged 9. The secondary malignancies included eight hematopoietic cancers, 12 sarcomas, and nine carcinomas. It was observed that the carcinomas most likely represented the general risk for cancer in the healthy population but that the sarcomas were caused by radiation therapy, and the hematopoietic tumors were caused by chemotherapy. Future Possibilities and Clinical Trials With evolving and intensified induction and maintenance chemotherapy and improved imaging and patient selection techniques. If the margins are not adequate for local control, postoperative radiation therapy can be administered without significantly altering the result in constructs that do not require bone graft healing and incorporation. The use of intraoperative radiation therapy, proton beam irradiation, and other advances in radiotherapy and improvements in limb salvage surgery in all sarcomas have improved our ability to achieve local control of the primary. The increasing role of surgical therapy in the local management of patients with Ewing sarcoma appears to be beneficial with respect to overall disease-free survival and reduction of treatment-related late effects. Current efforts are being directed at finding newer chemotherapeutic agents and intensifying therapy to improve outcomes further. The goal is to optimize therapy wherever possible to provide the patient with the best overall clinical and functional results. Regardless of the primary or secondary classification, the overwhelming majority of these lesions are high-grade malignancies. Histologically, the tumor is composed of fibroblasts in a storiform (whorling or cartwheel) pattern with multinucleated giant cells, inflammatory cells, and histiocytes with numerous foamy mononuclear or multinucleated giant cells (xanthomatous variant). Ultrastructurally, the lesions seem to derive from a primitive mesenchymal stem cell that might be shared with the common progenitor cell of osteosarcoma. After diagnostic biopsy, neoadjuvant chemotherapy can be administered, and the primary tumor response can be monitored according to clinical and radiographic parameters. A combination of doxorubicin, ifosfamide, and methotrexate is often used, but currently there is no agreed-on regimen. The majority of tumors respond clinically with relief of pain, resolution of the associated joint contracture, diminished local edema, and reduction in the size of the soft tissue component. Preoperative or neoadjuvant chemotherapy is not a requirement, and an immediate surgical resection is recommended if the patient is at risk of sustaining a pathologic fracture. Whether or not the patient receives preoperative chemotherapy, a wide surgical margin is recommended. It is classified into primary and secondary categories, which are related to the absence or presence of a known predisposing and underlying pathologic entity, such as bone infarction, fibrous dysplasia, or Paget disease of bone. Some tumors also appear to be associated with orthopedic implants and could be metal induced in rare cases. The primary variety tends to affect younger patients, whereas the secondary neoplasms are seen predominantly in the sixth and seventh decades of life. First described by Dockerty and Myerding and later refined by Cohn and colleagues423 from the Mayo Clinic in 1962, this rare, low-grade malignant lesion arises predominantly in the tibia (90%), the next most common site being the fibula. The most common symptom is pain and, later, a mass, most often in the midshaft of the tibia (70%). Adamantinoma is associated with osteofibrous dysplasia, and they often occur together. Clinical Manifestations Pronounced loss of normal trabeculation associated with permeative cortical destruction is the characteristic radiographic appearance. Invasion into adjacent soft tissue with the development of a soft tissue mass is not uncommon. The proximal tibia and distal femoral metaphyses are most frequently affected, followed by the pelvis, proximal humeral metaphysis, and scapula. There appears to be a clear association with bone infarction as a preexisting condition. The patient completed three courses of multiagent systemic chemotherapy before consideration of a surgical resection. The lesion was resected with a minimum of a 2-cm proximal bone margin and was reconstructed with use of a modular distal femoral prosthesis. In general, this tumor is managed in a fashion similar to that of conventional osteosarcoma of bone. The lateral digital film demonstrates an expansile intramedullary midshaft tibia mass with cortical thinning and destruction. This intraoperative view demonstrates the intended surgical procedure, resection of 14 cm of the diaphysis of the tibia and reconstruction of the skeletal defect with a free avascular left fibula graft supplemented with autologous iliac crest bone graft. The proximal and distal host/graft osteotomy sites were supplemented with autologous iliac crest bone graft. Left Soft tissue 5 6 7 Right Vertebral body 8 Clinical Manifestations, Patient Evaluation, and Staging Back pain is the most common presenting symptom of a tumor of the spine. Less commonly, some patients have onset of spinal cord compression without any antecedent history of pain. The age of the patient is important in evaluating a suspected lesion involving the vertebral column. Patients younger than 18 years are 80% more likely to have a benign lesion than are those older than 18 years. Boriani and coworkers433 proposed a surgical staging system for tumors of the spine that resembles a 12-sector clock face as viewed from cephalad to caudad, in which 1 and 12 represent the left and right sides of the spinous process, respectively. For those primary bone tumors that have all the characteristics of a benign tumor, observation without biopsy is acceptable when the tumor does not need removal. An open biopsy with frozen section analysis is appropriate when the benign tumor needs surgical removal. An osteoblastoma is an example of a benign bone tumor that should be surgical removed. Fine-needle aspirate biopsy or core needle biopsy is usually preferred for tumors that are suspected to be malignant. The system does not recognize grade (G) or longitudinal compartmental margins (T). Therefore patients are treated with preoperative chemotherapy, and then a surgical resection is performed with as wide a margin as possible. Although there is limited experience, adjuvant irradiation is often recommended, especially for patients with less than 90% necrosis and close or positive margins. Vertebral lesions are most often associated with ill-defined symptoms, usually occurring in younger middle-aged patients. The pain and discomfort are characteristically associated with either radicular pain or a disturbance of balance or gait.
Effective risperidone 2 mg
Accuracy of revised Bethesda guidelines symptoms ebola generic 4 mg risperidone mastercard, microsatellite instability, and immunohistochemistry for the identification of patients with hereditary nonpolyposis colorectal cancer. The cost-effectiveness of routine testing for Lynch syndrome in newly diagnosed patients with colorectal cancer in the United States: corrected estimates. Integrated genetic and epigenetic analysis identifies three different subclasses of colon cancer. Colorectal cancer intrinsic subtypes, predict chemotherapy benefit, deficient mismatch repair and epithelial-to-mesenchymal transition. Gene expression patterns unveil a new level of molecular heterogeneity in colorectal cancer. Subtypes of primary colorectal tumors correlate with response to targeted treatment in colorectal cell lines. A colorectal cancer classification system that associates cellular phenotype and responses to therapy. Poor-prognosis colon cancer is defined by a molecularly distinct subtype and develops from serrated precursor lesions. Gene expression classification of colon cancer into molecular subtypes: characterization, validation and prognostic value. Challenging the cancer molecular stratification dogma: intratumoral heterogeneity undermines consensus molecular subtypes and potential diagnostic value in colorectal cancer. Cancercell intrinsic gene expression signatures overcome intratumoural heterogeneity bias in colorectal cancer patient classification. Changing the paradigm- multistage multiarm randomized trials and stratified cancer medicine. Extended lymphadenectomy versus conventional surgery for rectal cancer: a meta-analysis. Enhanced recovery after surgery: a consensus review of clinical care for patients undergoing colonic resection. Determinants of outcome after colorectal resection within an enhanced recovery programme. Patient readmission and mortality after colorectal surgery for colon cancer: impact of length of stay relative to other clinical factors. Variability in length of stay after colorectal surgery: assessment of 182 hospitals in the national surgical quality improvement program. Enhanced recovery after surgery programs versus traditional care for colorectal surgery: a meta-analysis of randomized controlled trials. Randomized clinical trial on epidural versus patient-controlled analgesia for laparoscopic colorectal surgery within an enhanced recovery pathway. Modulation of post-operative insulin resistance by pre-operative carbohydrate loading. Postoperative gastrointestinal tract dysfunction: an overview of causes and management strategies. Results of the American Society of Colon and Rectal Surgeons Laparoscopic Registry. Laparoscopic-assisted and minilaparotomy approaches to colorectal diseases are similar in early outcome. Laparoscopic surgery versus open surgery for colon cancer: short term outcomes of a randomized trial. Long-term outcome of laparoscopic surgery for colorectal cancer: a Cochrane systematic review of randomised controlled trials. Prospective randomized study of laparoscopic versus open colonic resection for adenocarcinoma. Postoperative pain and fatigue after laparoscopic or conventional colorectal resections: a prospective randomized trial. A prospective, randomized trial comparing laparoscopic versus conventional techniques in colorectal cancer surgery: a preliminary report. Quality of life after laparoscopic and open colorectal surgery: a systematic review. Early bursting strength of human colon anastomosis: an in vitro study comparing current anastomosis techniques. Updated protocol for the examination of specimens from patients with carcinoma of the colon and rectum excluding carcinoid tumours, lymphomas, sarcomas and tumours of the vermiform appendix: a basis for checklists. Lymph node recovery from colorectal resection specimens removed for adenocarcinoma. Trends over time and a recommendation for a minimum number of lymph nodes to be recovered. Colon cancer survival is associated with increasing number of lymph nodes analyzed: a secondary survey of Intergroup Trial Int-0089. Identifying patients with T3-T4 node-negative colon cancer at high risk of recurrence. Impact of the number of negative nodes on disease-free survival in colorectal cancer. The prognosis of T3N0 colon cancer is dependent upon the number of lymph nodes examined. Accuracy of determining nodal negativity in colorectal cancer on the basis of the number of nodes retrieved on resection. Prognostic evaluation of stage B colon cancer patients is improved by an adequate lymphadenectomy: results of a secondary analysis of a large scale adjuvant. Documenting the process in improving the staging of node-negative colorectal cancer. A national study on lymph node retrieval in resectional surgery for colorectal cancer. Analysis of micrometastatic disease in sentinel lymph nodes from resectable colon cancer: results of cancer and leukemia group B Trial 80001. Conventional and laparoscopic reversal of the Hartmann procedure: a review of literature. Intraoperative colonic lavage and primary anastomosis- an alternative to Hartmann procedure in emergency surgery of the left colon. Subtotal colectomy vs intraoperative colonic irrigation in the management of obstructed left colon carcinoma. Single-stage treatment for malignant left-sided colonic obstruction; a prospective randomized trial comparing subtotal colectomy with segmental resection following intraoperative irrigation. Systematic review and meta-analysis of randomized clinical trials of self-expanding metal stents as a bridge to surgery versus emergency surgery for malignant left-sided large bowel obstruction. Management of obstructive colorectal cancer with endoscopic stenting followed by single stage surgery: open or laparoscopic resection The Association of Coloproctology of Great Britain and Ireland study of large bowel obstruction caused by colorectal cancer. Surgical management of the urinary tract in patients with locally advanced colorectal cancer. Impact of primary resection on the outcome of patients with perforated diverticulitis. Endoscopically removed malignant colorectal polyps: clinicopathologic correlations. Comparison of transanal endoscopic microsurgery and total mesorectal excision in the treatment of T1 rectal cancer: a meta-analysis. Evaluation of long-term survival after hepatic resection for metastatic colorectal cancer: a multifactorial model of 929 patients. Survival after hepatic resection in metastatic colorectal cancer: a population-based study. Is hepatic resection justified after chemotherapy in patients with colorectal liver metastases and lymph node involvement Conversion to resectability using hepatic artery infusion plus systemic chemotherapy for the treatment of unresectable liver metastases from colorectal carcinoma. Prolonged survival of initially unresectable hepatic colorectal cancer patients treated with hepatic arterial infusion of oxaliplatin followed by radical surgery of metastases. Adjuvant chemotherapy after resection of colorectal liver metastases in patients at high risk of hepatic recurrence: a comparative study between hepatic arterial infusion of oxaliplatin and modern systemic chemotherapy. American Society of Clinical Oncology 2009 clinical evidence review on radiofrequency ablation of hepatic metastases from colorectal cancer.
Cheap risperidone 4mg
The main symptoms of recurrence that demand palliation are pruritus and cholangitis associated with jaundice medications that cause high blood pressure buy risperidone 2 mg cheap. For limited recurrences, intraluminal brachytherapy or external beam radiotherapy499 may improve palliation and, potentially, survival. Routine follow-up evaluation consists of office visits every 3 to 6 months with physical examination, laboratory tests including liver function tests, and cross-sectional imaging of the chest, abdomen, and pelvis. Although a rising alkaline phosphatase level is a good indicator of evolving biliary obstruction, patients recovering from liver resection and biliary obstruction may have persistent elevations of alkaline phosphatase. In up to 10% of patients with biliary surgical reconstruction, however, a benign anastomotic stricture may develop. Most patients with recurrence or a benign stricture will have jaundice or cholangitis. Follow-up with imaging is also recommended because there are options for effective palliative chemotherapy. The largest benefit was seen in patients with node-positive disease, or those who underwent an R1 resection. Capecitabine is now used as a standard of care in the adjuvant therapy of resected biliary cancers. Several large prospective trials in the United States and Europe evaluated the use of adjuvant gemcitabine-based chemotherapy and chemoradiation in this population, as detailed in the gallbladder section. Isolated locoregional recurrence rates are as high as 60% after curative resection of hilar cholangiocarcinoma. Although it remains controversial, postoperative chemoradiation to patients with positive margins could be recommended. The role of radiation therapy in liver transplantation for unresectable hilar cholangiocarcinoma is under active investigation. These results compare favorably with those of another group of patients who underwent resection alone, whose 3- and 5-year survival rates were 48% and 21%, respectively. Treatment of Metastatic Disease the majority of studies evaluating systemic therapies have included patients with both gallbladder and bile duct cancers, which were discussed at length in the gallbladder section (see Gallbladder Cancer). It is anticipated that as a more sophisticated understanding of the genetic alterations driving these clinically distinct malignancies emerges, systemic therapy may be better targeted to a specific disease. Intraarterial Chemotherapy Chemotherapy delivered by intraarterial administration for cholangiocarcinoma is an attractive concept because of the predilection of cholangiocarcinoma for locoregional relapse. The major disadvantage is the need for a port or pump, which requires a laparotomy for placement. Several small trials have demonstrated promising response rates, with acceptable toxicity, in selected patient populations. Bilirubin elevation (>2 mg/dL) was seen in 24% of patients, and biliary stents were placed in 13. Patients who received an inadequate radiation dose died from tumor-related liver failure. Similar long-term outcomes were reported in a prospective trial using proton therapy. Randomized trials are needed in order to define the role of intrahepatic chemotherapy in biliary tumors. Locally Advanced Disease and Palliation Biliary obstruction is a common clinical problem in patients with cholangiocarcinoma. In the setting of low bile duct obstruction, the entire biliary tree can be drained by a single well-placed catheter or stent. When the obstruction is at or above the hilum, there is often isolation of the right and left hepatic ducts, and tumor may also extend to block the secondary ducts. Relief of biliary obstruction in patients with extrahepatic cholangiocarcinoma is an important component of care. The cause of death in most patients with unresectable extrahepatic cholangiocarcinoma is related to biliary obstruction, either due to cholestatic liver failure or cholangitis. Obstructive jaundice may also result in alteration in taste of food or frank anorexia that is improved with reestablishment of the normal enterohepatic circulation of bile. Drainage of as little as 30% of the liver will effectively palliate pruritus in most patients. In patients with biliary duct isolation, it is critical to evaluate which duct(s) have been instrumented in the past, because the overwhelming likelihood is that the duct(s) that has been previously colonized is the source of infection. Lowering serum bilirubin is one of the more challenging indications for biliary drainage in high bile duct isolation. The likelihood of lowering the bilirubin to an acceptable value, typically 2 mg/dL, is directly related to the volume of functional liver that can be drained. Successfully lowering bilirubin is more likely when the predrainage total bilirubin is less than 9 mg/dL and the international normalized ratio is normal. In patients with extrahepatic cholangiocarcinoma, biliary drainage can be accomplished by surgical bypass, endoscopic stent, or percutaneous biliary drainage and/or stenting. The tumor is obstructing the duct to the level of the common bile duct at the insertion of the cystic duct. In the absence of biliary ductal isolation, endoscopy is preferred over percutaneous stenting because of the lower risk of complications and lack of an external catheter. In addition, to prevent cholangitis, plastic stents require routine exchange every 3 months. When possible, we advocate placement of a primary stent above the papilla to preserve the integrity of the sphincter of Oddi, thereby preventing reflux of enteric contents into the biliary tree. In patients who have acute cholangitis, less manipulation is required for placement of a drainage catheter, and the catheter also provides access to see how much bile is draining and its character over time. In some cases, placement of a drainage catheter may be indicated to facilitate adjuvant therapy including brachytherapy or photodynamic therapy. These clinical observations are supported by recent efforts to compare the molecular characteristics of biliary tract malignancy arising from different anatomic sites. Furthermore, the distribution and frequency of these genetic alterations differ even between intrahepatic and extrahepatic disease. Attesting to the difficult management of patients with hilar cholangiocarcinoma, the postoperative complication rate is as high as 60%. In many series, treatment of hilar cholangiocarcinoma with aggressive resection results in a perioperative mortality rate of 5% to 10%. The overall complication rate is approximately 20% to 30%, with a mortality rate of less than 3%. Such advances probably will require elucidation of the molecular changes associated with the different biliary tumors. Other improvements in screening programs in high-risk areas, potentially resulting in prophylactic cholecystectomy, may be beneficial. Continued assessment of new drugs, novel radiosensitizers, and biological agents is warranted. A better understanding of the molecular pathogenesis and genetics of bile duct cancers may lead to new therapeutic and ultimately preventive strategies for high-risk populations. Controversies, Problems, and Challenges In determining optimal adjuvant treatment strategies for biliary tract cancers, the differing biology of tumors occurring at various locations in the biliary tree should be considered, particularly when considering the incorporation of locoregional therapies. Although the majority of resected extrahepatic cholangiocarcinomas relapse with isolated locoregional disease at the initial site of recurrence, gallbladder carcinoma most frequently recurs with distant metastases. Furthermore, gallbladder cancer is associated with both decreased time to recurrence and decreased survival after relapse when compared with extrahepatic cholangiocarcinoma, reflecting the differing biology of these clinically distinct diseases. Screening for liver cancer: results of a randomised controlled trial in Qidong, China. Clinicopathologic characteristics and survival outcomes of patients with fibrolamellar carcinoma: data from the fibrolamellar carcinoma consortium. Long-term survival and pattern of recurrence after resection of small hepatocellular carcinoma in patients with preserved liver function: implications for a strategy of salvage transplantation. Radioembolization for hepatocellular carcinoma using yttrium-90 microspheres: a comprehensive report of long-term outcomes. Dose-escalation study of single-fraction stereotactic body radiotherapy for liver malignancies.
Ferrous Sulfate (Iron). Risperidone.
- Anemia from low levels of iron in the blood (iron deficiency anemia).
- What is Iron?
- Are there safety concerns?
- Improving thinking, learning, and memory in iron-deficient children.
- How does Iron work?
- Are there any interactions with medications?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96878
Generic risperidone 2 mg with amex
By contrast medications via ng tube 4 mg risperidone free shipping, some abnormal peptides produced by islet cell tumors have no known clinical hormonal effects. This is thought to be a result of tumor cell regulation by somatostatin and its predominant tumor cell receptor somatostatin receptor subtype 2. The first group consists of those patients who experienced their tumors stochastically, in the absence of significant personal or family history of endocrine disorders. The second group includes those with clear evidence of an inherited predisposition to multiple neoplasias of the endocrine system in an autosomal dominant pattern. The latter patients tend to have a more indolent course than those with sporadic tumors. Where possible, tissue confirmation with biopsy demonstrating characteristic neuroendocrine staining (discussed earlier) is critical. This constellation of imaging findings has a sensitivity of 94% for intrapancreatic lesions. In addition, measurement of -hydroxybutyrate is helpful in diagnosing insulinomas owing to the antiketogenic effect of insulin. Sporadic insulinomas usually are single, smaller than 2 cm, and benign; approximately 10% are malignant with metastatic distribution into lymph node, liver, and bone. In patients with malignant disease, proinsulin may be increased in plasma or circulating human chorionic gonadotropin. Occult lesions can be identified with techniques such as endoscopic ultrasound and selective arteriography and portal venous sampling. Surgical resection usually is curative because of the small size and low metastatic potential of insulinomas. The type of resection indicated depends on the size and anatomic relationship of the tumor to the surrounding vasculature. Laparoscopic surgery can be done for small, solitary tumors that have been localized preoperatively. Frequent feedings between meals and at bedtime are administered with sufficient glucose to control symptoms. Adjustments in the carbohydrate content of the diet may be required, depending on the reactivity of the individual tumor, because the stimulus of a large glucose load may lead to an exaggerated release of insulin. Furthermore, glucagon stimulates pancreatic insulin secretion and may cause paradoxical exacerbation of a hypoglycemic episode. It also may have an extrapancreatic hyperglycemic effect and cause marked edema and hirsutism. Diazoxide is administered orally in divided doses, ranging from 100 to 1000 mg/day. Although the plasma insulin level often can be reduced to a level that causes no symptoms, the tumor will continue to grow and metastasize if malignant, because diazoxide lacks anticancer activity. Insulinomas have excellent long-term outcomes; 20-year survival has been reported in 90% of patients with metastatic insulinomas. Unregulated secretion of glucagon by -cell tumors produces a distinctive clinical syndrome. Glucagon inhibits intestinal motility, and the glucagonoma syndrome often includes ileus and constipation. Because symptoms commonly are mild and nonspecific, the tumor often is recognized late, when metastases are present. In patients with glucagonoma, the plasma hormone level typically is markedly elevated and often is greater than 1000 pg/mL. The diagnosis is further suggested by failure of glucose to suppress glucagon, by an abnormal rise in plasma glucagon following infusion of arginine, by the presence of hypoaminoacidemia, and, if tumor is available, immunoperoxidase staining for glucagon. Reviews have suggested that the tumor is more common in women and typically manifests in the fifth and sixth decades. The primary tumor is in the tail or body of the pancreas in 50% of patients and in the head of the pancreas in 8% of patients; the remaining 42% of patients have diffuse involvement. The tyrosine kinase inhibitor sunitinib has shown good efficacy in one clinical trial, with prolongation of survival for up to 11. Somatostatin may serve as a paracrine regulator of other pancreatic islet cell hormones. Inhibition of secretion of those hormones may account for some of the signs of somatostatinoma, such as diabetes, diarrhea, or gallbladder disorders. However, somatostatin analogues are considered the first line of treatment of unresectable tumors. Gastrinoma Gastrin, the polypeptide hormone normally secreted by the G cell of the gastric antrum, stimulates gastric acid secretion. Tumors of the pancreatic or duodenal wall G cells are responsible for the signs and symptoms of Zollinger-Ellison syndrome, a disorder characterized by hypersecretion of gastrin. First described in 1955, this syndrome is characterized by hypersecretion of gastric acid, severe peptic ulcer disease, and an islet cell tumor of the pancreas. Intermittent diarrhea, often with steatorrhea, may be present as a result of digestive enzyme inactivation in the small intestine by unbuffered gastric acid. All manifestations of the Zollinger-Ellison syndrome are secondary to hypersecretion of gastric acid. Gastric rugal hypertrophy, multiple ulcers, or ulceration of the small bowel on radiographic studies suggests gastrinoma. Extrapancreatic locations include the duodenum, predominantly the first part of the duodenum, and the stomach, retroperitoneal lymph nodes, liver, and bile duct. Although the original case reports stressed the appearance of extensive and multiple gastric ulcers, a heightened index of suspicion and early detection have altered this pattern of disease presentation. Suspicion should be raised in any patient with peptic ulcer disease refractory to Helicobacter pylori eradication. The first step is to identify fasting hypergastrinemia in association with a basal acid output greater than 15 mEq/h. Less-convincing elevations in fasting serum gastrin can be further evaluated with the secretin test, in which a peak level of serum gastrin higher than 200 pg/mL over the baseline after administration of secretin is considered diagnostic. Approximately 75% of patients with Zollinger-Ellison syndrome have solitary ulcers smaller than 1 cm in the first part of the duodenum, 14% in the distal part, and 11% in the jejunum. If no metastatic disease is identified, potentially curable operative intervention is indicated. Before the introduction of histamine receptor antagonists, the only practical way to treat recurrent duodenal and jejunal ulcers was total gastrectomy. Surgical resection of sporadic gastrinomas with no evidence of metastatic disease is associated with a 50% to 97% long-term survival rate. Swedish investigators reported on 22 patients treated with human leukocyte interferon, with an objective response rate of 77% and a median duration of response of 8. Clinical trials still investigate the use of interferon, particularly in pegylated form, but its use outside of clinical trials is not recommended. As with carcinoid tumors and other islet cell tumors, however, in patients with locally unresectable disease or those with hepatic metastases, surgical cytoreduction or regional therapy may improve symptom control. These tumors are exceedingly rare and are associated with metastases in the chest or retroperitoneum. Chemotherapy usually is attempted in patients with symptoms caused by tumor bulk that may not be palliated by cytoreductive surgery or in patients with uncontrolled syndromes of hormone excess. This drug has a diabetogenic action in some animals that is correlated with selective uptake of the drug by pancreatic -cells. These responses generally were of long duration and yielded meaningful improvements in performance status and symptoms, but were not reproduced in later studies in which more standardized radiographic response criteria were used. Therapy Radiation Therapy Radiotherapy has similar indications as carcinoid tumors for symptomatic lesions, particularly in the late and rare complication of bony metastatic disease. Among patients who are not candidates for surgical resection, some data from case reports and small case series indicate that radiation therapy can produce symptomatic improvement and freedom from local progression. For that reason, resection of hepatic metastases is warranted in selected patients. Endocrine and tumor response to hepatic arterial occlusion, with or without chemotherapy, can be impressive. The Mayo Clinic experience documented 46 patients with islet cell tumor regression rates of 43% with hepatic artery occlusion alone versus 78. This result was achieved with the modest radiographic response rate of 5% (2% for placebo). Similarly, the objective response rate was low (9%), and overall survival data may be confounded because of early stoppage of the trial.
Discount 3 mg risperidone with amex
Thus although no benefit from the addition of ifosfamide and etoposide in patients with metastases was demonstrated medications used for migraines purchase risperidone mastercard, substantial improvement in patients with nonmetastatic disease was observed. Four to six cycles of vincristine, doxorubicin, and cyclophosphamide alternating with ifosfamide and etoposide are typically administered before local control, with a total of approximately 48 weeks of this regimen completed after local control. In the experimental arm, patients received their cycles every 2 weeks compared with the standard regimen of every 3 weeks; the total doses of drugs were equal in the two arms. This study demonstrated only modest toxicity with this approach, but further randomized trials are needed to determine efficacy. Now that patients are surviving longer, however, late effects such as growth disturbances in children, fractures of irradiated long bones, local recurrence, and secondary malignancies have caused a rethinking of this modality as the routine method of local control. Developments in surviving patients have led to a reassessment of the role of surgery in providing management of the primary tumor with sustained local control and minimal risk of developing a secondary malignancy. There is a definite local recurrence rate with radiotherapy alone as local control. The outcome of limb salvage surgery has improved, allowing surgeons to achieve functional reconstructions and soft tissue closure without a high complication rate that would delay chemotherapy. Finally, the risk of combined chemotherapy and radiotherapy for development of late secondary malignancies within the radiation portal and tumor bed of surviving patients have led many centers to prefer surgical local control. Several older, noncontrolled studies showed a benefit to surgical resection for local control. The local control rate for the 21 patients who underwent surgical resection with wide margins and an additional 16 patients (total 26%) who required postoperative radiation therapy with inadequate margins was also approximately 80%. Donaldson and colleagues374 reviewed the end results of Pediatric Oncology Group study 8346, evaluating 178 eligible patients, of whom 141 (79%) had only local disease and 37 (21%) had metastatic disease. Thirty-seven patients with localized disease underwent local resection, and 16 (43%) of those required postoperative radiotherapy. The remaining 104 patients with local disease were eligible for random assignment or assignment to receive radiotherapy. The 5-year local control rate for the surgical patients, either with or without postoperative radiotherapy, was 88%, and the rate for the patients who underwent radiotherapy alone was 65%. Patients who had appropriate radiotherapy (treatment of appropriate volumes) had a 5-year local control rate of 80%, whereas those with minor deviations had a 5-year local control rate of 48%, and those with major deviations had a local control rate of only 16%. The local failure was within the irradiated volume in 62% of patients and outside the irradiated volume in 24% of cases. Data reported from the Rizzoli Institute on 124 patients with nonmetastatic Ewing sarcoma also concluded that surgery or surgery plus radiation therapy appeared to have a better overall patient outcome than did radiation therapy alone. For tumors in the extremities and/or other bones, local recurrences were observed in patients who were managed with surgery plus radiation therapy. Recurrence rates for those who received radiation therapy alone were 30% local recurrence in the extremities and 18% in other sites. It has been suggested that this observed benefit of surgical resection is a result of smaller tumor size. It appeared that more patients with smaller tumors were being managed with surgical therapy. The majority of recent clinicopathologic studies have shown improved local control with the addition of surgery. The overall impact of operative treatment on outcome or survival of patients with Ewing sarcoma of the pelvis or sacrum has been debated. Patients with small (<100 mL) extremity tumors were classified as standard-risk patients (n = 52), and patients with tumor volumes of greater than 100 mL (n = 177) and/or central axis tumors (skull, shoulder, chest, spine, pelvic bones; n = 164) were classified as high-risk patients (n = 241). Local therapy was surgery for 68 patients (23%), surgery and radiation for 146 patients (49%), and radiotherapy alone for 82 patients (28%). In multivariate analyses, small tumor volumes of less than 200 mL, good histologic response, and intensive chemotherapy argued for a fair outcome. Bacci and coworkers385 retrospectively reviewed 91 consecutive patients who were treated for Ewing sarcoma of the femur in an attempt to eliminate selection bias toward those treated with surgery with or without radiotherapy and those treated with radiotherapy alone at other locations. The probability of survival without local recurrence was significantly higher (P =. Surgical treatment of patients with Ewing sarcoma arising in pelvic bones has improved, principally because of improved imaging techniques, improved neoadjuvant chemotherapy regimens, and an improved surgical understanding of the disease. Frassica and coauthors386 reviewed 21 patients with nonmetastatic Ewing sarcoma of the pelvis. Thirteen of the 21 received chemotherapy and radiation therapy, and eight received chemotherapy and local operative resection with or without postoperative radiotherapy. The actuarial 5-year overall survival rate for patients who had chemotherapy and radiation therapy without surgical resection was 25%, whereas patients who underwent surgical resection had a 75% survival rate (P <. The actuarial overall 5-year survival rate was 45% for patients who were seen without evidence of metastases. The rate of local failure was 44% for the group that was managed with chemotherapy and radiation therapy alone, compared with 13% for patients with a local resection (P > 0. Shamberger and colleagues387 reported the results of treatment of 98 of 869 patients (11. Ten of 20 (50%) initial resections resulted in negative margins, compared with 41 of 53 (77%) negative margins with delayed resections after chemotherapy (P =. Initial chemotherapy decreased the percentage of patients who needed radiotherapy. In cases of delayed operation, excluding patients who received only radiation therapy for local control, only 25 of 62 patients needed radiotherapy (40. The authors concluded that complete tumor resection with a negative microscopic margin and consequent avoidance of external beam radiation and its potential complications are increased with neoadjuvant chemotherapy and delayed resection of chest wall Ewing sarcoma or primitive neuroectodermal tumor. One criticism is that the large, bulky tumors are treated with radiotherapy and the small ones are treated with surgery. Size alone, however, is not the sole determinant of who is eligible for an operation and who is not. Response to neoadjuvant chemotherapy and the precise location of the tumor are also important, and these factors have not been adequately controlled in the retrospective data that exist today. For instance, a large, bulky tumor of the ilium might be easily resectable after induction chemotherapy with little morbidity, whereas a small periacetabular tumor might be selected for radiation because we do not have good reconstruction options after removing the acetabulum. In the Grier study,364 38% of patients had surgery alone, 39% had radiation alone, and 23% had both. DuBois and colleagues388 reported the clearest data to date on this topic; they used extensive measures to control for these confounding issues. There was a slightly improved rate of local control in patients treated with surgery only compared with patients treated with radiation alone or radiation with surgery, but there was no difference in disease-specific survival. It is unlikely that we will ever have a randomized study to address this issue, but the current practice in most centers is to attempt a resection whenever it is deemed possible to do so with negative margins and a good functional result, mainly to avoid the risk of radiation-induced malignancy. When those goals are not possible, radiation is used, with high rates of local control. Current Guidelines for Surgical Therapy All active multimodality Ewing sarcoma protocols have provisions and recommendations for surgical resection in an effort to avoid the late effects of therapy when possible. The majority of these procedures should not require reconstruction, which is best avoided because of the occasional need for adjuvant radiation therapy to the surgical bed and prolonged intensive adjuvant chemotherapy. Rib primaries are best managed by excision after preoperative chemotherapy to decrease the size of the soft tissue mass and reduce the likelihood of contamination of the pleural cavity. A wide resection of the recommended entire rib and surrounding soft tissue is completed after induction chemotherapy. In most instances, this approach will eliminate the need for radiation or at worst reduce the amount of chest wall and lung that require radiation. Also, tumors that arise in the lower portion of the sacrum and coccyx are amenable to sacral amputation with minimal neurologic sequelae. After a prolonged period of conservative care, the choice was made to proceed with resection and reconstruction with a custom modular titanium prosthesis. The arrows identify the contiguous previous biopsy incision and the humerus to provide an en bloc wide resection. Note the closure of the epiphysis in the humeral head after external beam radiotherapy (arrow in humeral head). This anteroposterior tomogram demonstrated local bone destruction and loss of trabeculation along the entire length of the right clavicle.
Order risperidone visa
Others prefer to classify the tumor on the basis of growth pattern: lobular treatment quotes cheap risperidone american express, comedocarcinoma, papillary, and mixed. The histologic features include anaplastic cells with varying degrees of differentiation. Special stains, such as oil red O and Sudan black, often are helpful in delineating the atypical sebocytes; however, poorly differentiated tumors may not stain positively for lipids. Mutations in p53 are significantly associated with sebaceous carcinoma and are independent of microsatellite instability, therefore suggesting a divergence in molecular pathogenesis. The unsaturated 8-carbon fatty acid oleic acid has been shown to cause dysplasia in glandular structures. The tumor usually originates from sebaceous glands in the tarsus (meibomian glands) or from sebaceous glands of the eyelash (glands of Zeis). A chest radiograph, complete blood cell count, liver function tests, and electrolytes are recommended. Primary Therapy Management of sebaceous gland carcinoma is primarily surgical, although there are a few reports of tumors managed primarily with radiation. Given the complex issues in dealing with this aggressive tumor, individuals are best served in a tertiary care setting with a multidisciplinary approach. Physical examination, evaluation of the surgical site, and a low threshold for biopsy of suspicious lesions constitute a reasonable approach. Treatment of Locally Advanced and Metastatic Disease Local recurrence usually is the result of inadequate management of the primary tumor. These cells have frequent mitotic figures, apoptotic bodies, scanty cytoplasm, and vesicular nuclei with finely dispersed chromatin and inconspicuous nucleoli, giving a so-called salt-and-pepper appearance. Histologic and immunohistochemical studies are the key to confirmation of the diagnosis. The updated system has better prognostic discrimination and incorporates two major changes (Table 67. However, elderly, poor surgical candidates with micrometastases to lymph nodes may receive radiotherapy alone. In general, patients with larger tumors, macrometastases, or extranodal invasion require combined therapy. For patients with less than optimal margins, especially in the head and neck region, where adjuvant radiotherapy is planned, conservative excision of lymph nodes close to the positive node basin without performance of a radical lymphadenectomy might be considered. Future directions may include stratifying clinical trials by viral status, monitoring disease status with circulating biomarkers, stimulating host immune responses with tumor vaccines, and examining radiotherapy with checkpoint inhibitors. The overlying epidermis usually appears normal, and a tumor-free zone, known as a grenz zone, may be present between tumor and epidermis in early lesions. The peripheral margins may have a deceptively bland appearance resembling normal collagen and making interpretation of tumor margins difficult. In addition, it stains negative for S100, which can be used to distinguish it from nerve tumors and melanoma. The tumors can also be violaceous or red-brown, especially along the margins at an early stage. The nodular component is fixed to the dermis initially, but progressive fixation to the deeper structure can be observed late in the course of the disease. The tumor size at diagnosis typically ranges from 1 to 5 cm, but neglected lesions can be as large as 20 cm in diameter. The test may be especially useful in atypical cases in which diagnosis is uncertain based on histologic findings. Atypical clinical manifestations include sclerotic plaques with a morpheaform appearance. The diagnosis is usually made by means of histologic evaluation of biopsy specimens. Because local or systemic metastases are extremely rare, neither prophylactic lymph node dissection nor extensive laboratory or imaging studies are indicated. The overall rate of distant metastasis is approximately 5% and of regional metastasis is 1%. Particular attention to evaluation of surgical site, regional lymph node palpation, and a complete review of systems is appropriate. This method also allows for maximum conservation of tissue, a crucial factor in certain anatomic areas, such as the head, neck, distal extremities, and genitalia. The technique involves resection of the tumor followed by processing of the specimen with standard permanent fixation and evaluation. This technique allows the use of immunohistochemical stains to help define the tumor margin, because it is often difficult to distinguish the lesion from scar tissue on frozen section. In cases in which local recurrence occurs, the tumors have significant propensity for deeper invasion into fascia, muscle, or bone, which makes complete resection even more difficult. Therefore when surgical margins are positive, repeat surgery is usually recommended, followed by adjuvant radiotherapy. The therapy, however, should not be used as primary treatment or a substitute for inadequate surgical resection. The broad indication allows imatinib to be used as both neoadjuvant and adjuvant therapy as an alternative to radiotherapy. The lungs are more frequently affected than other sites such as the brain and bone. In 1948, Stewart and Treves reported an association between angiosarcoma and post mastectomy lymphedema. Although angiosarcomas are reported in renal transplant recipients, the role of immunosuppression to the pathogenesis of angiosarcoma is uncertain. The vessels are irregular and lined by atypical endothelial cells, which can range from a nearly normal, single endothelial-cell lining to more aggressive, multilayered, papillary projections into irregular vascular lumens. In the solid pattern, poorly differentiated tumors contain the malignant endothelial cells that are arranged in solid sheets or cords, with areas of hemorrhage and necrosis, and invading the dermis and underlying tissue. Those poorly differentiated or anaplastic tumors can resemble carcinoma or amelanotic melanoma. Skin biopsies followed by pathologic and immunohistochemical evaluations are necessary for initial diagnosis. The tumor infiltrates the surrounding structure in a centrifugal and multifocal fashion, which may result in a much larger subclinical extension than the apparent clinical margins, with multiple foci separated by an isthmus of normal-appearing skin. Initial differential diagnoses include cellulitis, nonspecific inflammatory changes, fungal infection, trauma, hemangioma, cutaneous lymphoma, and pseudolymphoma. Patients younger than 50 years with tumors arising in the trunk and localized to the skin have the best prognosis. The role of chemotherapy in the neoadjuvant or adjuvant setting after definitive surgery and radiotherapy is not well established and has not been proven to increase survival. Additional surgery in locally recurrent disease to achieve a pathologic complete resection may improve survival. Radical surgery attempting for complete resection is considered the primary treatment of choice. Wide excision margins of 3 to 6 cm or Challenges and Future Possibilities As aforementioned, antiangiogenic biologic molecules are promising candidates in conjunction with surgery and radiotherapy. Staging for cutaneous squamous cell carcinoma as a predictor of sentinel lymph node biopsy results: meta-analysis of American Joint Committee on Cancer criteria and a proposed alternative system. Multivariate analysis of potential risk factors for lymph node metastasis in patients with cutaneous squamous cell carcinoma of the head and neck. Systemic treatment of locally advanced nonmetastatic cutaneous squamous cell carcinoma: a review of the literature. Solitary keratoacanthoma is a squamous-cell carcinoma: three examples with metastases. Array comparative genomic hybridization of keratoacanthomas and squamous cell carcinomas: different patterns of genetic aberrations suggest two distinct entities. Trends of skin cancer mortality after transplantation in the United States: 1987 to 2013. A clinical scoring system to identify patients with sebaceous neoplasms at risk for the MuirTorre variant of Lynch syndrome.
Purchase risperidone 2 mg amex
A meta-analysis of 21 studies revealed that individuals with a larger waist circumference have a 36% increased risk for developing adenomas treatment carpal tunnel order risperidone toronto, and 46% for colon and rectal cancer. Nearly 35% of all Americans have metabolic syndrome, and obesity is the number one cause. A meta-analysis of 17 studies revealed that the risk of colorectal cancer is 33% to 41% higher in individuals with metabolic syndrome. Twentyfour prospective studies found that former and current smokers have a 17% to 25% increased risk of colorectal cancer compared with never-smokers. Other purported protectants found in whole grains include folate, vitamins, antioxidants, phenolic acids, lignans, phytoestrogens, and trace minerals. Nonsupplemental dietary intake of certain vitamins (-carotene; vitamins C, D, E) and minerals (zinc) has been shown to decrease the risk of colorectal cancer by 20% to 40%. Folate is found in numerous sources, with the highest levels noted in beans, lentils, green leafy vegetables, avocado, asparagus, and fruits. Epidemiologic studies have indicated that increased dietary folate may be associated with lower rates of colon and rectal cancer. Animal studies have shown a correlation between methionine restriction and inhibition of colorectal carcinogenesis. Certain medications have been associated with a lower risk of developing adenomas and colorectal cancer. The daily use of aspirin for 5 years or longer has been associated with a risk reduction of 32% to 49%. All jointly recommend starting screening at the age of 50 for average-risk individuals, although with some discrepancies regarding frequency, preferred method, and the recommended age at which to discontinue screening. The preferred screening and therapeutic test for the prevention of colorectal cancer is colonoscopy. If the findings of modalities for screening other than colonoscopy are abnormal, a full colonoscopic examination is necessary. For individuals with a nonhereditary family history of colorectal cancer or adenomatous polyps in first-degree relatives younger than 60 years, or in two or more first-degree relatives of any age, colonoscopic screening should be carried out every 5 years and should begin at age 40 or 10 years earlier than the age of the youngest affected relative, whichever is earlier. For patients with first-degree relatives diagnosed at older than 60 years, or with two or more second-degree relatives of any age, screening should begin at age 40 and the recommendations for average-risk individuals should be followed. Incidence rates for the development of cancer correspond to cumulative probabilities of 2% by 10 years, 8% by 20 years, and 18% by 30 years. Relative risk for cancer in relation to ulcerative proctitis has been estimated to be 1. In relation to the general population there is an overall eightfold higher risk of colorectal cancer, with a 19-fold higher risk in patients with extensive colitis. Roughly 17% of all deaths in ulcerative colitis are the result of colorectal cancer. The American Gastroenterological Association and British Society of Gastroenterology share international guidelines recommending surveillance colonoscopies every 1 to 2 years starting 8 to 10 years after a diagnosis of pancolitis, or 12 to 15 years after left-sided colitis. Polyps, predominately found in the rectum and left colon, develop in adolescence and are present in up to 15% of patients by 10 years of age and 75% by age 20. If untreated, the risk of colorectal malignancy is nearly 100% by 35 to 40 years of age. With the predilection for polyp development in the left colon and rectum, a yearly flexible proctosigmoidoscopy can be performed instead of a formal colonoscopy, although if adenomatous polyps are appreciated a formal colonoscopy should then be performed. With the predilection for polyp development in the right side of the colon, a formal colonoscopy is recommended. Polyps are most commonly found in the left side of the colon and present in patients at a median age of 48. If no polyps are found, endoscopy should be repeated every 3 to 5 years, and more frequently if polyps are present. The risk of developing colon and rectal cancer is increased, with rates of up to 30% to 50% documented in those with multiple polyps. The risk of malignancy increases with age (13-fold higher than in the general population), with the most common cancers being colorectal, breast, pancreatic, and genitourinary. Polyps can be found throughout the gastrointestinal system, with the colon and rectum affected 100% of the time. Colorectal cancer is the most common associated malignancy, with lifetime rates as high as 39%. Asymptomatic patients should begin with screening colonoscopy by 15 years of age, and earlier for those with symptoms. If no polyps are detected, evaluation can be repeated every 2 to 3 years, otherwise annually. The mean age of diagnosis is 42, with a lifetime risk of developing colorectal cancer of around 80%. For those with a family or personal history, colonoscopic screening should begin at 20 to 25 years of age, or 10 years younger than the index case, and should continue every 2 years until the age of 40, then annually. The diffusely infiltrating type is the rarest and presents similarly to linitis plastica of the stomach; there is diffuse thickening of the rectum with preservation of the layers of the intestinal wall. Regardless of the surgical resection performed (proctectomy or local excision), certain histologic features are essential in determining prognosis and must be evaluated. Histologic grade is determined by the degree of differentiation of the tumor and is a stage-independent prognostic factor. A diagnosis is made when more than 50% of cells in the tumor have signet ring features. Graham and colleagues determined that a tumor bud count of 10 corresponded to an approximately 2. Tumor deposits found in pericolonic fat are not directly associated with lymph nodes and confer a worse prognosis. Intramural spread in the wall of the rectum beyond 2 cm and nodal spread in the mesorectum beyond 3 to 4 cm is rare. In an attempt to determine an adequate distal resection margin based on intramural spread, Shirouzu and colleagues retrospectively reviewed 610 consecutive rectal cancer specimens not treated with neoadjuvant chemoradiation. Extramural lymphatic drainage and spread generally follow the cephalad direction of the inferior mesenteric vessels. Although the rectum drains primarily to the inferior and paraaortic nodes, the distal portion can also drain to the internal iliac chains by way of the middle hemorrhoid vessels. Retrograde lymphatic drainage, although rare, can occur if anterograde pathways are blocked. Inguinal nodal involvement is exceedingly rare and typically seen only with involvement of the anal canal and specifically the dentate line. Full-thickness involvement of the rectal wall with invasion of adjacent structures beyond the enveloping fascia propria of the mesorectal compartment occurs around 10% of the time. The administration of intravenous contrast material has not been shown to improve accuracy or provide additional prognostic staging information. Overall accuracy for depth of invasion was 75%; nodal stage, 71%; and circumferential margin involvement, 94%. Up to 90% of nodes with irregular borders harbor metastasis in comparison with those with smooth regular borders, which are benign nearly 94% of the time. The sensitivity and specificity range from 54% to 79% and 74% to 96%, respectively. For patients with signs and symptoms, bleeding is the most common and occurs around 60% of the time. Others presentations include a change in bowel habits (43%), occult bleeding (26%), abdominal pain (20%), bowel obstruction (9%), malaise (9%), pelvic pain (5%), perforation or peritonitis (3%), and jaundice from liver metastasis (<1%). In addition to a detailed medical, surgical, family, and social history, the duration of symptoms, presence of pain, alteration of bowel function, changes in weight, issues with continence, genitourinary dysfunction, and level of fitness are ascertained. Patients with a family history suspicious for or meeting the criteria for a heritable syndrome should be referred to a genetic counselor. For women with anteriorly located tumors, a full pelvic and vaginal examination should be carried out. Palpation of the inguinal regions is performed to evaluate for the presence of lymphadenopathy. An abdominal examination is pursued to check for liver and other palpable abnormalities. A full colonoscopic examination is performed and provides the opportunity to directly visualize the lesion and document the size, gross appearance, degree of luminal involvement, anatomic orientation, and lower margin distance from the anal verge.