Purchase vimax on line amex
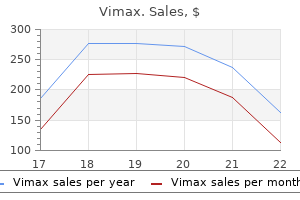
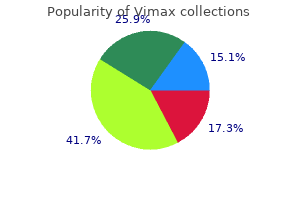
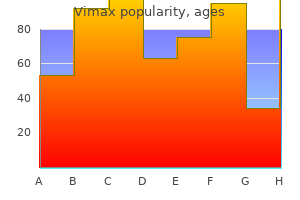
It has been observed that prions accumulate in organs with chronic lymphocytic inflammation impotence 25 years old purchase vimax visa. Rabies, Slow Virus Infections, and Prion Diseases 631 circulating B cells in scrapie-infected sheep. Maximum titers of infectivity are reached in the brain long before neurologic symptoms appear. The disease is characterized by the development of amyloid plaques in the central nervous system of infected animals. These areas represent extracellular accumulations of protein; they stain with Congo red. In the last few years, several studies have generated synthetic prions in vitro that caused disease when inoculated in vivo, further suggesting that prions are infectious proteins. Brain homogenates from patients have transmitted both diseases to nonhuman primates. Kuru occurred only in the eastern highlands of New Guinea and was spread by customs surrounding ritual cannibalism of dead relatives. This occurs with a frequency of approximately one case per million population per year in the United States and Europe and involves patients over 50 years of age. The estimated incidence is less than one case per 200 million for persons under 30 years of age. Scrapie Scrapie shows marked differences in susceptibility of different breeds of animal. Susceptibility to experimentally transmitted scrapie ranges from 0 to over 80% in various breeds of sheep, whereas goats are almost 100% susceptible. The transmission of scrapie to mice and hamsters, in which the incubation period is greatly reduced, has facilitated study of the disease. Infectivity can be recovered from lymphoid tissues early in infection, and high titers of the agent are found in the brain, spinal cord, and eye (the only places where pathologic changes are observed). A particular polymorphism in the amino acid sequence of the human prion protein seems to influence susceptibility to disease. Prions are readily destroyed by (A) Ionizing radiation (B) Formaldehyde (C) Boiling (D) Proteases (E) None of the above 3. The presence in neurons of eosinophilic cytoplasmic inclusion bodies, called Negri bodies, is characteristic of which of the following central nervous system infections Chronic Wasting Disease A scrapie-like disease, designated chronic wasting disease, is found in mule deer and elk in the United States and Canada. It is laterally transmitted with high efficiency, but there is no evidence that it has been transmitted to humans. Infectivity has been detected in feces of deer before they become ill; the agent is retained in the soil, where it can then be ingested by other deer and elk. He develops a severe progressive neurologic disease characterized by psychiatric symptoms, cerebellar signs, and dementia. Rabies virus has a wide host range and the ability to infect all warm-blooded animals, including humans. Infectious scrapie agent can be detected in amyloid plaques in infected brains of sheep and hamsters. The genome of the infectious agent is characterized by which of the following nucleic acid types A 49-year-old man visited a neurologist after 2 days of increasing right arm pain and paresthesias. The symptoms increased and were accompanied by hand spasms and sweating on the right side of the face and trunk. The patient was admitted to the hospital the day after developing dysphagia, hypersalivation, agitation, and generalized muscle twitching. Vital signs and blood tests were normal, but within hours the patient became confused. The most likely explanation for treatment failure is (A) the rabies test results were falsely positive and the patient did not have rabies. Which of the following animals is most commonly reported rabid in the United States What is the best diagnostic test to perform on the patient to rule in rabies as a cause of his illness A 20-year-old man, who for many years had received daily injections of growth hormone prepared from human pituitary glands, develops ataxia, slurred speech, and dementia. At autopsy the brain shows widespread neuronal degeneration, a spongy appearance due to many vacuoles between the cells, no inflammation, and no evidence of virus particles. The most likely diagnosis is (A) Herpes encephalitis (B) Creutzfeldt-Jakob disease (C) Subacute sclerosing panencephalitis (D) Progressive multifocal leukoencephalopathy (E) Rabies Answers 1. C Human Cancer Viruses Viruses are etiologic factors in the development of several types of human tumors, including two of great significance worldwide-cervical cancer and liver cancer. The viruses that have been strongly associated with human cancers are listed in Table 43-1. New cancer-associated viruses are being discovered by the use of molecular techniques. Many viruses can cause tumors in animals, either as a consequence of natural infection or after experimental inoculation. Animal viruses are studied to learn how a limited amount of genetic information (one or a few viral genes) can profoundly alter the growth behavior of cells, ultimately converting a normal cell into a neoplastic one. Tumor viruses are agents that can produce tumors when they infect appropriate animals. Many studies are done using cultured animal cells rather than intact animals, because it is possible to analyze events at cellular and subcellular levels. These discoveries revolutionized cancer biology and provided the conceptual framework for the molecular basis of carcinogenesis. The highly oncogenic (direct-transforming) viruses carry an oncogene of cellular origin. The weakly oncogenic (slowly transforming) viruses do not contain an oncogene and induce leukemias after long incubation periods by indirect mechanisms. Hepatitis C virus, a flavivirus, does not generate a provirus and appears to induce cancer indirectly. Multistep Carcinogenesis Carcinogenesis is a multistep process; that is, multiple genetic changes must occur to convert a normal cell into a malignant one. Intermediate stages have been identified and designated by terms such as "immortalized," "hyperplastic," and "preneoplastic. The natural history of human and animal cancers suggests a multistep process of cellular evolution, probably involving cellular genetic instability and repeated selection of rare cells with some selective growth advantage. The number of mutations underlying this process is estimated to range from five to eight. Observations suggest that activation of multiple cellular oncogenes and inactivation of tumor suppressor genes are involved in the evolution of tumors whether or not a virus is involved. Normal versions of these transforming genes are present in normal cells and have been designated proto-oncogenes. The discovery of cellular oncogenes came from studies with acutely transforming retroviruses. It was found that normal cells contained highly related (but not identical) copies of various retrovirus transforming genes; cellular sequences had been captured and incorporated into the retrovirus genomes. Transduction of the cellular genes was probably an accident, as the presence of the cellular sequences is of no benefit to the viruses. Many other known cellular oncogenes that have not been segregated into retrovirus vectors have been detected using molecular methods. Cellular oncogenes are partly responsible for the molecular basis of human cancer. They represent individual components of complicated pathways responsible for regulating cell proliferation, division, and differentiation and for maintaining the integrity of the genome. Incorrect expression of any component might interrupt that regulation, resulting in uncontrolled growth of cells (cancer). The molecular mechanisms responsible for activating a benign proto-oncogene and converting it into a cancer gene vary-but all involve genetic damage.
Orchanet (Alkanna). Vimax.
- Are there safety concerns?
- Are there any interactions with medications?
- How does Alkanna work?
- What is Alkanna?
- Dosing considerations for Alkanna.
- Skin diseases, healing leg ulcer wounds, stomach ulcers, and diarrhea.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96601
Purchase vimax master card
Although the number of human cases is small erectile dysfunction nervous generic 30caps vimax, rabies is a major public health problem because it is widespread among animal reservoirs. Rabies virus attaches to cells via its glycoprotein spikes; the nicotinic acetylcholine receptor may serve as a cellular receptor for rabies virus. Ongoing translation is required for replication, particularly of viral N and P proteins. The viral matrix protein forms a layer on the inner side of the envelope, whereas the viral glycoprotein is on the outer layer and forms the spikes. Structure Rabies virus is a rhabdovirus with morphologic and biochemical properties in common with vesicular stomatitis virus of cattle and several animal, plant, and insect viruses (Table 42-1). The particles are surrounded by a membranous envelope with protruding spikes, 10 nm long. Rabies viruses belong to the genus Lyssavirus, whereas the vesicular stomatitis-like viruses are members of the genus Vesiculovirus. The rhabdoviruses are very widely distributed in nature, infecting vertebrates, invertebrates, and plants. Susceptibility varies among mammalian species, ranging from very high (foxes, coyotes, wolves) to low (opossums); those with intermediate susceptibility include skunks, raccoons, and bats (Table 42-2). The virus is widely distributed in infected animals, especially in the nervous system, saliva, urine, lymph, milk, and blood. However, there are strain differences among viruses isolated from different species (raccoons, foxes, skunks, canines, bats) in different geographic areas. These viral strains can be distinguished by epitopes in the nucleoprotein and glycoprotein recognized by monoclonal antibodies as well as by specific nucleotide sequences. There are at least seven antigenic variants found in terrestrial animals and bats. The G glycoprotein is a major factor in rabies virus neuroinvasiveness and pathogenicity. Avirulent mutants of rabies virus have been selected using certain monoclonal antibodies against the viral glycoprotein. A substitution at amino acid position 333 of the glycoprotein results in loss of virulence, indicating some essential role for that site of the protein in disease pathogenesis. Purified spikes containing the viral glycoprotein elicit neutralizing antibody in animals. Antiserum prepared against the purified nucleocapsid is used in diagnostic immunofluorescence for rabies. Hematophagous vampire bats may transmit the virus for months without themselves ever showing any signs of disease. When freshly isolated in the laboratory, the strains are referred to as street virus. Shown here is vesicular stomatitis virus negatively stained with potassium phosphotungstate. However, it is also possible for rabies virus to enter the nervous system directly without local replication. It multiplies in the central nervous system and progressive encephalitis develops. The virus then spreads through peripheral nerves to the salivary glands and other tissues. Other organs where rabies virus has been found include pancreas, kidney, heart, retina, and cornea. There is a higher attack rate and shorter incubation period in persons bitten on the face or head; the lowest mortality occurs in those bitten on the legs. Rabies virus produces a specific eosinophilic cytoplasmic inclusion, the Negri body, in infected nerve cells. The presence of such inclusions is pathognomonic of rabies but is not observed in at least 20% of cases. The importance of Negri bodies in rabies diagnosis has been lessened by the development of the more sensitive fluorescent antibody and reverse transcriptionpolymerase chain reaction diagnostic tests. The clinical spectrum can be divided into three phases: a short prodromal phase, an acute neurologic phase, and coma. General sympathetic overactivity is observed, including lacrimation, pupillary dilatation, and increased salivation and perspiration. A large fraction of patients will exhibit hydrophobia (fear of water) or aerophobia (fear when feeling a breeze). Paralytic rabies occurs in about 30% of patients, most frequently in those infected with bat rabies virus. Rabies should be considered in any case of encephalitis or myelitis of unknown cause even in the absence of an exposure history, and particularly in a person who has lived or traveled outside the United States. Most cases of rabies in the United States are in individuals with no known exposure. Because of the long incubation period, people may forget a possible exposure incident. People who contract bat rabies often have no recollection of being bitten by a bat. The usual incubation period in dogs ranges from 3 to 8 weeks, but it may be as short as 10 days. Clinically, the disease in dogs is divided into the same three phases as human rabies. Both Negri bodies and rabies antigen can usually be found in animals or humans infected with rabies, but they are rarely found in bats. Reverse transcription-polymerase chain reaction testing can be used to amplify parts of a rabies virus genome from fixed or unfixed brain tissue or saliva. Sequencing of amplified products can allow identification of the infecting virus strain. Serology Serum antibodies to rabies can be detected by immunofluorescence or neutralization tests. Such antibodies develop slowly in infected persons or animals during progression of the disease but promptly after vaccination with cell-derived vaccines. Antibodies in cerebrospinal fluid are produced in rabies-infected individuals but not in response to vaccination. Laboratory Diagnosis There are no tests to diagnose rabies infections in humans before the onset of clinical symptoms. Rabies can be diagnosed from euthanized animals by direct fluorescent antibody testing of brain tissue. Viral Isolation Available tissue is inoculated intracerebrally into suckling mice. The central nervous system of the inoculated animal is examined for Negri bodies and rabies antigen. In specialized laboratories, hamster and mouse cell lines can be inoculated for rapid (2- to 4-day) growth of rabies virus; this is much faster than virus isolation in mice. An isolated virus is identified by fluorescent antibody tests with specific antiserum.
Order vimax 30caps without a prescription
One frequently used method is to culture urine using a bacteriologic loop calibrated to deliver 0 erectile dysfunction drug related buy vimax 30 caps on-line. Thus, in the setting of the first such infection in a young woman, definitive identification and susceptibility testing of the bacteria are seldom necessary. Such cases can be treated by a single dose of appropriate antibiotic, based on local or regional antibiograms, but a 3- to 5-day course of therapy yields a lower relapse rate. Recurrent or complicated upper tract infections are best treated with antibiotics shown to be active against the infecting bacteria; definitive identification and susceptibility testing are indicated. Patients with complicated upper tract infections should have evaluations for anatomic abnormalities, stones, and so forth. The wound was cleaned and debrided, the fracture was reduced, and the bone aligned. Pins were placed through the skin and bone proximal and distal to the fracture to allow splinting and immobilization of the leg. One day after surgery, the leg remained markedly swollen; a moderate amount of serous drainage was present on the dressings. Two days later, the leg remained swollen and red, requiring opening of the surgical wound. The patient was treated with intravenous nafcillin for 10 days, and the swelling and redness decreased. Osteomyelitis was diagnosed, and the patient was returned to the operating room, where the fracture site was debrided of necrotic soft tissue and dead bone; the pins and plates were removed. The patient was treated with intravenous nafcillin for 1 month followed by oral dicloxacillin for 3 additional months. After 6 months, there was no x-ray evidence of further osteomyelitis, and the patient was able to bear weight on the leg. A 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Comment Osteomyelitis follows hematogenous spread of pathogenic bacteria from a distant site of infection to bone or, as in this case, direct inoculation of the bone and soft tissue, as can occur with an open fracture or from a contiguous site of soft tissue infection. The primary symptoms are fever and pain at the infected site; swelling, redness, and occasionally drainage can be seen, but the physical findings are highly dependent on the anatomic location of the infection. In children, the onset of osteomyelitis following hematogenous spread of bacteria can be very sudden, while in adults the presentation may be more indolent. Sometimes osteomyelitis is considered to be chronic or of long standing, but the clinical spectrum of osteomyelitis is broad, and the distinction between acute and chronic may not be clear either clinically or on morphologic examination of tissue. Kingella kingae (Chapter 16) is a common etiologic agent in infants and children younger than 4 years. Anaerobic bacteria (eg, Bacteroides species [Chapter 21]) are also common, particularly in osteomyelitis of the bones of the feet associated with diabetes and foot ulcers. Any bacteria that cause infections in humans have been associated with osteomyelitis. Definitive diagnosis of the etiology of osteomyelitis requires culture of a specimen obtained at surgery or by needle aspiration of bone or periosteum through uninfected soft tissue. Culture of pus from the opening of a draining sinus tract or superficial wound associated with the osteomyelitis commonly yields bacteria that are not present in the bone. Blood cultures are often positive when systemic symptoms and signs (fever, weight loss, elevated white blood cell count, high erythrocyte sedimentation rate) are present. Early in the course of osteomyelitis, x-ray films of the infected site are negative. They become positive within a few days after onset and are particularly helpful in localizing the site of infection and determining if there are multiple sites of infection; however, bone scans do not differentiate between fractures, bone infarction (as occurs in sickle cell disease), and infection. Antimicrobial therapy and surgical debridement are the mainstays of treatment of osteomyelitis. Immobilization of infected limbs and fixation of fractures are important features of care. He was rapidly transported to the hospital and immediately taken to the operating room, where the fracture was reduced and the wounds debrided. At admission, results of his blood tests included a hematocrit of 45% and a hemoglobin of 15 g/dL. The immediate postoperative course was uneventful, but 24 hours later, pain developed in the thigh. Physical examination showed an acutely ill young man who was in shock and delirious. Large ecchymotic areas were present near the wound, and there was a serous discharge from the wound. Gas gangrene was diagnosed, and the patient was taken to the operating room for emergency extensive debridement of necrotic tissue. At the time of surgery, his hematocrit had fallen to 27% and his hemoglobin to 11 g/dL; his serum was red-brown in color, indicating hemolysis with free hemoglobin in his circulation. Anaerobic cultures of the specimen obtained at surgery grew Clostridium perfringens (Chapters 11 and 21). The patient developed renal failure and heart failure and died 3 days after his injury. The presence of necrotic tissue and foreign body material provides a suitable anaerobic environment for the organisms to multiply. The extremity or wound shows tenderness, tense swelling, and a serosanguineous discharge. The skin near the wound is pale but rapidly becomes discolored, and fluid-filled blebs form in the nearby skin. In patients such as this one, Gram-stain of fluid from a bleb or of a tissue aspirate shows large Gram-positive rods with blunt ends and is highly suggestive of clostridial infection. The differential diagnosis of clostridial gas gangrene includes anaerobic streptococcal myonecrosis, synergistic necrotizing myonecrosis, and necrotizing fasciitis. These clinically overlapping diseases can be differentiated from clostridial gas gangrene by Gram-stain and cultures of appropriate specimens. The hemoglobin may be low or normal even when the hematocrit is low, consistent with hemolysis and cell-free circulating hemoglobin. Physical examination showed a yellowish mucopurulent discharge from the cervical os. The bimanual pelvic examination showed cervical motion tenderness and adnexal tenderness more severe on the left than on the right. The patient was treated as an outpatient with a single intramuscular dose of ceftriaxone plus oral azithromycin. Hyperbaric oxygen can be used in centers that have experience and the appropriate equipment. When shock and circulating free hemoglobin are present, renal failure and other complications are common and the prognosis is poor. Comment In men, urethral discharge is classified as gonococcal urethritis, caused by N. The diagnosis is based on the presence or absence of Gram-negative intracellular diplococci on stain of the urethral discharge. All patients with urethritis should be tested using nucleic acid amplification methods for both C. Ceftriaxone is frequently used to treat gonococcal urethritis, but quinolones may be used in areas that report low resistance. It is highly recommended that men with gonococcal infection also be treated for chlamydial infection because of the likelihood that both infections may be present.
Buy 30caps vimax with amex
However erectile dysfunction medications in india purchase discount vimax, more recent data suggest mortality risk continues to rise for up to 90 days after surgery. On the other hand, if the patient survives the surgical resection and staged procedures, and if the resection margins are clear, then, stage for stage, cancer survival does not differ from patients who have no obstruction. The reason is that the left colon has a narrower calibre than the right, and its contents tend to be less fluid. Furthermore, carcinomas on the right side tend to be soft and friable in consistency, whereas those on the left side tend to be scirrhous and annular. Usually patients present with clinical features of the primary tumour only, but occasionally they may complain of symptoms relating to metastases and deny any abdominal or gastrointestinal problems. The following are the usual clinical features that may be encountered; however, one or any combination of them may present. Broadly speaking, there are two categories of presentation: acute or emergency, and chronic or elective. When patients present electively, the site of the tumour will often dictate the symptom complex. Emergency cases present with one of the complications of the carcinoma, which are usually obstruction, perforation or haemorrhage. The proportion of patients who present to the surgeon in one of these two ways depends on the type 500 Chapter 24 Clinical Features of Colorectal Adenoma and Adenocarcinoma Change in Bowel Habit Change in bowel habit is probably the most common symptom, particularly with left-sided lesions. At the onset, the complaint is often quite trivial; for instance, the frequency of bowel action may increase from once every two days to a daily action. So insidious is the onset of this symptom, that the patient frequently disregards it and does not seek medical advice. Either constipation or diarrhoea may be prevalent, but commonly the two conditions alternate. This may be the result of taking either laxatives or constipating agents to alleviate the principal symptom. Rarely, the volume of mucus is profuse, as in patients with a bulky villous lesion. It is highly unusual, however, for a carcinoma of the colon to cause the syndrome, which may occur with rectal villousneoplasms, and is characterised by dehydration and hypokalaemia. Occasionally, a neoplasm of the transverse colon will invade the stomach and produce symptoms similar to that of a primary gastric carcinoma with anorexia, nausea and weight loss. It may vary from a central or lower abdominal colic to a constant, deepseated ache in one quadrant of the abdomen. Frequently, the patient with abdominal colic complains of nausea and abdominal distension. The latter may be alleviated after several days by the passage of loose stool or flatus. Occasionally the abdominal pain radiates to the back if the patient has a retroperitoneal extension of a tumour from the ascending colon. Lumbar pain may be due to retroperitoneal extension of a tumour in the descending colon. Abdominal Mass Occasionally the patient may become aware of an abdominal mass, but usually if one is present the clinician finds it on palpation. Its site within the abdomen depends on the position of the tumour within the colon; thus, a caecal lesion is felt in the right lower quadrant, a transverse colon lesion is usually felt in the epigastrium, etc. If a sigmoid lesion is mobile and prolapses into the pelvis, it may be felt through the rectal wall on rectal examination. The more proximal the lesion, the more altered the blood will become, with intraluminal blood exerting a laxative effect to cause change in bowel habit. A tumour in the sigmoid or descending colon may produce bright red bleeding of an insignificant amount. The patient may well ignore this symptom, or the doctor may be prepared to attribute it to haemorrhoids. It should be emphasised that even if the practitioner finds haemorrhoids on proctoscopy, the patient must have a more thorough investigation of the rest of the colon and rectum. When occult bleeding occurs, the patient usually presents with symptoms of anaemia, such as fatigue or breathlessness. This form of presentation is frequent with lesions of the caecum and right colon, and indeed anaemia may be the only sign of the underlying colorectal neoplasm. The anaemia is hypochromic and microcytic with a low serum ferritin, due to iron deficiency. It should be stressed that the presence of iron deficiency anaemia in any patient without an obvious cause demands full investigation of the whole gastrointestinal tract, paying particular attention to the colon. Symptoms Related to Metastases Each of the above clinical features emanates usually from the primary growth. Other dermatological problems that may be associated with either a symptomatic or asymptomatic primary colorectal cancer are acanthosis nigricans, dermatomyositis, pemphigoid and pyoderma gangrenosum. Other Modes of Presentation Other less common modes of presentation may result from abscess and fistulation. A sigmoid or descending colon lesion may form a fistula into the bladder and produce a colovesical fistula. The symptoms and signs are identical to those when such a fistula is caused by diverticular disease (see Chapter 49). Very occasionally a colocutaneous fistula results from a colonic carcinoma ulcerating through the abdominal wall. Fistulation into other parts of the gastrointestinal tract may occur, causing a variety of clinical features. Thus, fistula formation between colon and small intestine can Passage of Mucus the passage of mucus is common; it may be separate from the stool or mixed with it. The patient often describes the Evaluation 501 occasionally result in a blind loop syndrome, and a gastrocolic fistula may result in severe diarrhoea and weight loss. Nevertheless, rectal carcinoma tends to be associated with a characteristic symptom complex, and because of its distal site, it can often be palpated per rectum. Bleeding is perhaps the most common symptom and is frequently ignored by the patient. It may be mixed in with the stool or passed separately, and although small amounts are usual, on occasions the volume may be alarming. The patient frequently has the urge to defaecate but on going to the lavatory passes only blood and mucus. It should be stressed that it is not diarrhoea as such, because so often faeculant material is not passed. It should also be stated that this symptom is not always confined to the early morning and may continue throughout the day and even wake the patient during the night. If the growth is constricting the rectum, abdominal colic may be the main complaint. Local anorectal pain is, however, unusual unless there has been spread to local structures, particularly where a tumour has invaded the sacral plexus posteriorly. If this occurs, the patient may feel the most intense discomfort in either the sacral region or in the distribution of one or both sciatic nerves. Pain may also be experienced if the tumour invades downwards and encroaches on the anal canal or perianal skin; this pain is usually aggravated by defaecation in a manner similar to that of an anal fissure. Invasion of the anal canal and sphincter may also lead to incontinence, and invasion of the perineal skin may result in the formation of a fistula-in-ano. Occasionally, the tumour is felt by the patient to be protruding through the anal orifice. Thus, the bladder or urethra may be involved, with the formation of a rectourethral or rectovesical fistula. The patient with this complication often complains initially of recurrent dysuria and urinary frequency, which may lead to pneumaturia. Spread anteriorly in the female may lead to a rectovaginal fistula or, less commonly, a rectouterine fistula.
Vimax 30 caps without prescription
Sugar fermentation and assimilation tests can be used to confirm the identification and speciate the more common Candida isolates erectile dysfunction song purchase 30caps vimax with amex, such as C. Pathogenesis and Pathology Cutaneous or mucosal candidiasis is established by an increase in the local census of Candida and damage to the skin or epithelium that permits local invasion by the yeasts and pseudohyphae. The histology of cutaneous or mucocutaneous lesions is characterized by inflammatory reactions varying from pyogenic abscesses to chronic granulomas. The administration of broad-spectrum antibacterial antibiotics often promotes large increases in the endogenous population of Candida in the gastrointestinal tract as well as the oral and vaginal mucosa. Systemic candidiasis occurs when Candida enters the bloodstream and the innate phagocytic host defenses are inadequate to contain the growth and dissemination of the yeasts. Many nosocomial cases are caused by contamination of indwelling intravenous catheters with Candida. Once in the circulation, Candida can infect the kidneys, attach to prosthetic heart valves, or produce candidal infections almost anywhere (eg, arthritis, meningitis, and endophthalmitis). The critical host defense against systemic candidiasis is an adequate number of functional neutrophils capable of ingesting and killing the yeast cells. During infection, cell wall components-such as mannans, glucans, other polysaccharides, and glycoproteins, as well as enzymes-are released. These macromolecules typically elicit innate host defenses and Th1, Th17, and Th2 immune responses. For example, sera from patients with systemic candidiasis often contain detectable antibodies to candidal enolase, secretory proteases, and heat-shock proteins. Intertriginous infection occurs in moist, warm parts of the body such as the axillae, groin, and intergluteal or inframammary folds; it is most common in obese and diabetic individuals. Before newborns establish a balanced microbiome, they are susceptible to extensive diaper rash and skin infection caused by Candida. Interdigital involvement between the fingers follows repeated prolonged immersion in water; it is most common in homemakers, bartenders, cooks, and vegetable and fish handlers. Candidal invasion of the nails and around the nail plate causes onychomycosis, a painful, erythematous swelling of the nail fold resembling a pyogenic paronychia, which may eventually destroy the nail. As noted above, Candida cells elaborate polysaccharides, proteins, and glycoproteins that not only stimulate host defenses but facilitate the attachment and invasion of host cells. The innate host defense mechanisms include pattern recognition receptors (eg, lectins, Toll-like receptors, and macrophage mannose receptor) that bind to pathogenassociated molecular patterns. A key example is the host cell lectin, dectin-1, which binds to the -1,3-glucan of C. This response is characterized by the production of cytokines, especially tumor necrosis factor-, interferon-, and granulocyte colony-stimulating factor, which activate antifungal effector cells, neutrophils, and monocytes. These activated leukocytes, like macrophages, can phagocytize and kill ingested yeast cells. In addition, the binding of -glucan to dectin 1 on dendritic cells induces the Th17 lymphocytes, which secrete interleukin-17. They are activated by innate, usually mucosal defense mechanisms as well as adaptive immune responses. On a variety of biological and prosthetic surfaces, the accumulation of yeasts and pseudohyphae readily form biofilms. The fungal biofilm is protected by extracellular matrix material that resists penetration by host immune responses and antifungal drugs. Systemic Candidiasis Candidemia can be caused by indwelling catheters, surgery, intravenous drug abuse, aspiration, or damage to the skin or gastrointestinal tract. In most patients with normal innate immune responses and circulating neutrophils, the yeasts are eliminated and candidemia is transient. However, patients with compromised innate phagocytic defenses may develop occult lesions anywhere, especially the kidney, skin (maculonodular lesions), eye, heart, and meninges. Systemic candidiasis is most often associated with chronic administration of corticosteroids or other immunosuppressive agents; with hematologic diseases such as leukemia, lymphoma, and aplastic anemia; or with chronic granulomatous disease. Candidal endocarditis is frequently preceded by the deposition and growth of the yeasts and pseudohyphae on prosthetic heart valves or vegetations and the formation of recalcitrant biofilms. Kidney infections are usually a systemic manifestation, whereas urinary tract infections are often associated with Foley catheters, diabetes, pregnancy, and antibacterial antibiotics. The most common forms present in early childhood and are associated with autoimmunity and hypoparathyroidism. The patients may develop chronic, raised, and crusty highly disfiguring keratitic lesions on the skin, oral mucosa, and scalp. Many patients with chronic mucocutaneous candidiasis are unable to mount an effective Th17 response to Candida. It is a patchy to confluent, whitish pseudomembranous lesion composed of epithelial cells, yeasts, and pseudohyphae, which can lead to the formation of an intractable biofilm. Other risk factors include treatment with corticosteroids or antibiotics, high levels of glucose, and cellular immunodeficiency. Yeast invasion of the vaginal mucosa leads to vulvovaginitis, characterized by irritation, pruritus, and vaginal discharge. This condition is often predisposed by conditions, such as diabetes, pregnancy, or antibacterial drugs that alter the microbiota, local acidity, or secretions. Other forms of cutaneous candidiasis include invasion of the skin, Diagnostic Laboratory Tests A. Specimens and Microscopic Examination Specimens include swabs and scrapings from superficial lesions, blood, spinal fluid, tissue biopsies, urine, exudates, and material from removed intravenous catheters. Sputum cultures have no value because Candida species are part of the oral microbiota. Cultures of skin lesions are confirmatory and distinguish cutaneous candidiasis from dermatophytosis or another infection. The ideal molecular test would detect candidemia early in the course of infection before the yeasts have developed chronic infection in the kidneys and other organs, when blood cultures are usually negative. Serology Serum antibodies and cell-mediated immunity are demonstrable in most people as a result of lifelong exposure to Candida. In systemic candidiasis, antibody titers to various candidal antigens may be elevated, but there are no clear criteria for establishing a diagnosis serologically. The detection of circulating Candida cell wall mannan, using a latex agglutination test or an enzyme immunoassay, is much more specific, but the test lacks high sensitivity because many patients are only transiently positive or because they do not develop significant and detectable antigen titers until late in the disease. The biochemical test for circulating -(1,3)d-glucan, described earlier in this chapter, has become widely used to screen for fungemia in patients at risk who often have negative blood cultures. Although the test is not specific for Candida, most patients with an invasive fungal infection have serum -glucan levels above 80 pg/mL. Other yeast isolates are speciated phenotypically by using any of several commercial kits to test for the metabolic assimilation of a battery of organic substrates. The diagnostic value of a quantitative urine culture depends on the integrity of the specimen and the yeast census. Positive blood cultures may reflect systemic candidiasis or transient candidemia due to a contaminated intravenous line. Unfortunately, only about 50% of blood cultures from patients with systemic candidiasis Immunity the basis of resistance to candidiasis is complex and incompletely understood. Innate immune responses, especially circulating neutrophils, are crucial for resistance to systemic candidiasis. Stimulation of specific Th17 lymphocytes triggers a cascade of cytokines that activate macrophages, inflammation, and enhance phagocytic activity. Treatment Thrush and other mucocutaneous forms of candidiasis are usually treated with topical nystatin or oral ketoconazole or fluconazole. The clearing of cutaneous lesions is accelerated by eliminating contributing factors such as excessive moisture or antibacterial drugs. Systemic candidiasis is treated with amphotericin B, sometimes in conjunction with oral flucytosine, fluconazole, or caspofungin. Chronic mucocutaneous candidiasis responds well to oral ketoconazole and other azoles, but patients have a genetic cellular immune defect and often require lifelong treatment. It is often difficult to establish an early diagnosis of systemic candidiasis-the clinical signs are not definitive, and blood cultures are often negative.
Purchase vimax 30 caps line
Where a bowel resection is envisaged erectile dysfunction kidney failure buy generic vimax canada, every effort should be made to consider the risks and benefits of both a restorative operation and a stoma with the patient pre-operatively, considering what the consequences will be whether a post-operative complication occurs or not. The value of early pre-operative involvement of a stoma therapist in those discussions cannot be overemphasised. That said, particular consideration must be given to the risks and consequences of a colorectal anastomotic leak, a complication with an incidence of up to 29% in some large published series. Severity of anastomotic leakage should be graded according to the impact on clinical management. Patient factors, errors of surgical judgement and intraoperative technical issues contribute to both the occurrence and the consequence of a colorectal anastomotic leak. However, despite both the relative frequency and serious impact of leaks, there is only a limited degree of high level evidence to guide colorectal management. In an elective setting it may be possible to mitigate these risks, for example by optimising enteral intake or draining collections radiologically but correcting severe malnutrition and/or hypoalbuminaemia can take months and may fail in the setting of persisting sepsis. Both smoking and heavy alcohol consumption are associated with an increased risk of colorectal anastomotic leak. There may be some risk reduction if a period of time is spent addressing these factors but the degree of any such benefit is likely to depend on the presence or otherwise of established smoking-, alcohol- or obesityassociated co-morbidities. Respiratory, cardiovascular and renal co-morbidity are all associated with an increased risk of colorectal anastomotic leak, as is diabetes. Perioperative supplemental oxygen of 80% FiO2 has been found to offer some protection against anastomotic leak. The evidence is greatest for corticosteroids, whether used as treatment for underlying inflammatory bowel disease35 or otherwise. Immunosuppression used in transplantation has long been assumed to increase the risk of anastomotic leak, but evidence is largely limited to rodent studies. As described previously, pre-operative mechanical bowel preparation is probably of no benefit in reducing the risk of anastomotic leak from most colorectal anastomoses. Sufficiently large trials to study its possible role specifically in patients undergoing a defunctioned high risk low rectal anastomosis would be of value. Many colorectal surgeons still administer pre-operative mechanical bowel preparation in this situation. There has been a recent increased interest in the role of pre-operative oral administration of non-absorbable antibiotics. Patients receiving a combination of mechanical bowel preparation and oral antibiotics had an odds ratio of anastomotic leak of 0. Animal studies suggest that selective decontamination with oral antibiotics protects against anastomotic leak in the setting of mesenteric ischaemia. More generally, an anastomosis between colon and rectum below the peritoneal reflection is at particularly high risk of leaking in men and women, the risk being higher the closer the proximity to the anus. There have been recent encouraging descriptions in small cohort studies of the use of near infrared angiographic assessment of microvascularisation to determine the site of bowel transection46 and to guide selective defunctioning for low colorectal anastomoses. Instead, most surgeons use a visual assessment to satisfy themselves that neither end of bowel to be anastomosed is chaemic, supplemented sometimes by palpation of mesenteric pulsation close to the prepared ends and/or observation of pulsatile blood flow from the divided ends. Similarly, judging that the anastomosis is not under tension is usually a subjective assessment, involving confirmation that the two ends to be joined can be brought to lie in immediate proximity unheld. Intraoperative events, including surgery prolonged beyond 4 hours and blood transfusion, are associated with increased risk of anastomotic leak,48 as are hypoxia and use of inotropes. Some of these factors are influenced by the performance of the surgeon and/or anaesthetist, but they should also direct intraoperative consideration of the risks and benefits of defunctioning an anastomosis made when intraoperative progress has not been straightforward, or indeed considering whether an anastomosis should be fashioned at all. A sigmoidoscope is introduced into the lower-most rectum and air insufflated whilst holding the bowel join below normal saline. If accessible, further sutures may be placed, but a small inaccessible defect may be better managed by defunctioning. The air test manoeuvre can be reproduced laparoscopically, and many surgeons employ the technique. Importantly, a positive air test, incomplete rings or intraoperative adverse events were exclusions from randomisation. Speculatively, many of the excluded patients may have been defunctioned and yet had an anastomotic leak. Different techniques have been described, including single and double layer, continuous and interrupted, sutured and stapled. Many stapled anastomoses also include sutures, either to underrun or invert/bury staple lines. In choosing a technique, most colorectal surgeons will adopt either handsewn or stapled anastomoses in different circumstances. Early surgical staplers for fashioning colorectal anastomoses were developed in Russia and offer the theoretical benefit of reproducibility in anastomotic technique. On the other hand, since bowel tissue is not identical from patient to patient and indeed may vary in its physical characteristics around its circumference within a single patient, hand-suturing offers a theoretical opportunity to adapt to specific circumstances. Whilst stapling techniques in the pelvis will inevitably vary to accommodate physical constraints, for the surgical trainee in particular there is some merit in becoming highly proficient in one handsewn technique that can then be reliably deployed in almost any situation. Although some size discrepancy can be accommodated with an end-to-end anastomosis, if there is significant difference in the luminal calibres, an end-to-side or side-to-side anastomosis may be preferable. The ends to be anastomosed are positioned in the correct configuration, ensuring no twisting of the mesentery. If enteric content is abundant and liquid, it is prudent to place a non-crushing clamp approximately 10 cm from each cut end, taking care to apply with minimal force and avoiding crushing of the mesentery. The suture is passed from the serosal surface towards the lumen in one limb then back out from the luminal surface to the serosa in the other. The stay sutures facilitate manipulation of the bowel ends and the application of gentle traction for optimal positioning for suture placement. Out-to-in, in-to-out serosubmucosal sutures as described above are then placed at approximately 4 mm intervals from the mesenteric to the anti-mesenteric stay along one side. The stays can then be used to flip the anastomosis over, and the process is repeated along the other side. If the mobility of the ends is limited, it is sometimes easier to place the back wall sutures first with the knots on the luminal surface, rather than attempting to rotate the bowel under tension. Care must be taken to lay the knots squarely with just enough tension to appose the serosal surfaces without strangling the tissues. The entire suture line is inspected to ensure even suture spacing, particularly at the mesenteric border. A stapled side-to-side technique is most commonly used to fashion small bowel or entero-colic anastomoses. A linear stapler cutter places two double rows of staples and divides the tissue between the two rows. The linear stapler cutter chosen must be of sufficient length to fashion an anastomosis of the desired calibre and the correct staple cartridge selected for the depth of tissue. In a common approach, the Wolff technique, the bowel ends to be anastomosed are laid adjacent to each other before resecting the specimen. After ensuring no tension or unwanted mesenteric twist, small enterotomies are made on the anti-mesenteric aspect of the bowel limbs. The linear stapler-cutter device is then passed through the enterotomies along the length of each bowel limb. The stapler is closed and fired after a pause to allow compression of the tissues, creating a side-to-side communication between the two lumen. Many surgeons re-use the reloaded linear stapler cutter to fire a transverse row of staples to excise the specimen and the two enterotomies, completing the anastomosis. However, the linear staplercutter devices are not designed to staple and cut across an existing staple line, and others favour use of a separate transverse stapler for this step. Though there is variation in incidence between colorectal surgeons, it is likely that most experienced colorectal surgeons will have witnessed their patient develop this feared complication. The complication often requires emergency reoperation that frequently involves formation of a stoma that the patient thought they had avoided. Many patients experience a period of critical illness, and for some it is a fatal complication. Although the patient may contribute several risk factors (see above), many anastomotic leaks probably involve some elements of regretted judgement, technical misadventure or both. Whilst investigations play an important role in the assessment of a colorectal patient with a suspected anastomotic leak (see below), departmental strategies to manage the non-technical human factors in decisionmaking may have value in the effective detection and treatment of anastomotic leaks. In many colorectal units, the management of such patients, both inside and outside the operating theatre, now involves support from a surgeon other than the one who undertook the original operation, with potential benefit to both patient and surgeon.
Syndromes
- Mild clouding of the lens often occurs after age 60. But it may not cause any vision problems.
- Speech problems, such as a slow or abnormal speech pattern (slurring of words)
- Fatigue
- You notice blood in your stool
- Determine if the gland and tumor need to be removed
- Excessive bleeding
- Caloric stimulation
- Genetic counselors and psychologists may also be involved.
- Fanconi syndrome
- Cancer
Buy vimax 30caps mastercard
They allow exploration of differences in patients erectile dysfunction medicine from dabur safe 30caps vimax, techniques and management across the cohort to identify areas of practice variability that may result in apparent differences in outcome. It must be noted they do not provide true evidence of causality or the impact of a particular variable, because despite complex multivariable regression modelling, they can never fully control for selection bias effects or the hidden confounders and interaction effects inherent in the complex decision-making processes that underpin surgical care. This said, they can certainly be hypothesisgenerating and identify areas warranting further study in future controlled prospective research or randomised controlled trials. The vast majority of colorectal surgeons now appreciate the central role that clinical research plays in improving outcomes for their patients, and are actively beginning to challenge the historical notions that surgical trials are difficult to conduct and rarely lead to changes in practice. It has been proven previously in the fields of ovarian cancer and coronary artery disease that patients treated at research-active hospitals demonstrate improved survival rates. These findings should serve to further boost the will and determination to create and participate in clinical research in surgery, but there remain major challenges and significant hurdles to overcome. These are a mixture of both genuine methodological challenges peculiar to surgery alongside some historical, environmental and logistical factors. There is increasing recognition that surgery itself is a complex intervention, made up of multiple components that can act independently or inter-dependently to impact on outcomes. Examples relevant here could include pre-operative patient behaviour (such as bathing, skin shaving, nutritional status), anaesthetic management and surgical technique, as well as post-operative ward routines (including dressing removal, staff handwashing, etc. There is also another group of contextual factors relating to the local setting in which the operation/intervention takes place that can impact upon outcomes, such as throughput rates, operating theatre policies and ward geography. However, the risk of delaying definitive evaluation of the technique is that it becomes widely adopted by surgeons and clinical equipoise is lost. Development of surgical practice is largely experiential, and this persists in the development of new surgical techniques or procedures. This methodology does not allow comparison of the new procedure against others, or against non-surgical options. There is an inherently judgemental process of comparing the new technique with the old, to assign a perceived difference in outcomes (or speed, or cost) that determines whether or not the new method is accepted. It must be noted that this ethos of active innovation is not surprising, given that surgeons are specifically trained to undertake constant situational assessment, dynamic decision analysis and improvisation during each and every operation. Modern surgical practice has moved towards the development of efficient patient pathways. Together, these organisational changes decrease the ability of the research team to access patients prior to surgery or enter them into trials and can make follow-up more challenging. The final issue, and perhaps most importantly, has been the lack of experience and infrastructure in surgical research, reflecting a poor funding history, itself secondary to the poor quality of a large proportion of previous surgical research. We are on the verge of a tide-change in clinical research in surgery, and colorectal surgery is best-placed to lead this important charge. The majority of colorectal conditions can be diagnosed at the initial consultation if the clinician is equipped with the ability for judicious clinical evaluation. When coupled with the availability of a myriad of diagnostic tests and a range of interventions that can be administered in an outpatient setting, such as anorectal biopsy, rubber band ligation of haemorrhoids and rigid sigmoidoscopy, it means that a reasonable proportion of patients can actually undergo complete diagnostic evaluation and personalised curative therapy at their first colorectal clinic attendance. Even if this is not possible, a tailored and efficient investigation plan will be created after a careful initial consultation. Exploration of family history is also essential, particularly enquiring about any family members affected by colorectal or lynch-associated cancers or inflammatory bowel disease. Thorough documentation of previous gynaecological, urological, anal and abdominal operations must be recorded. A list of risk factors for anaesthesia and contraindications for day case surgery should be checked: hypertension, diabetes, ischaemic heart disease, previous cerebrovascular accident, renal dysfunction, valvular heart disease, epilepsy and others. Co-existing medical therapy, particularly use of anticoagulants, diabetic medication, anticonvulsants, antihypertensives and immunosuppressants should be recorded. Social circumstances should also be assessed, including the level of support, if any, needed for the patient to complete their own activities of daily living such as washing, dressing, cooking and 38 Chapter 3 Process Delivery in Colorectal Surgical Practice shopping. This gives an estimation of functional status and can be important both in making personalised treatment decisions and in the planning of post-operative discharge arrangements and support requirements. These are discussed in turn: Bleeding Bleeding is one of the commonest symptoms encountered in colorectal clinic, but is always worrying to the patient. The relationship between bleeding, defaecation, straining, scratching, prolapse, constipation and diarrhoea is noted as is the colour of the blood loss and its presence in relation to the stool. Whether blood is on the surface or mixed with the faeces provides a pointer to the pathology. A bleeding source at the level of the anal canal typically produces bright red blood that is often only seen on the toilet paper, although may drip or even squirt into the toilet pan. Bleeding originating from within the colon or rectum produces a blood of variable colour and consistency, depending on the site of the pathology, the colonic transit times and the rate at which blood is being lost. Colonic bleeding may also result in mixing of the blood within the stool and other symptoms such as abdominal pain or altered bowel habit. Bloody stools combined with significant diarrhoea, mucus and abdominal pains may suggest inflammatory bowel disease. Generally speaking, the darker the blood, the more proximal the source is likely to be. Right colonic or caecal pathology will tend to result in altered and very dark red blood, whereas melaena is the passage of black, tarry stools, which have a characteristic and very offensive smell due to the presence of digested blood; it generally indicates a proximal gastrointestinal bleeding source. Abdominal Pain Abdominal pain is an important symptom and the clinician will need to know its site, whether it is related to eating, what relieving factors there are, whether it is constant or colicky and whether there is relief from posture, defaecation or medication. Duration of symptoms must be recorded but severity is difficult to quantify in an objective fashion. When considering abdominal pain, the clinician needs to recall their knowledge of the embryological derivation and neuroanatomy of the gastrointestinal structures and peritoneum. This particularly relates to the poorly localised and midline-based pain, often associated with nausea, that results from irritation or stretch upon the visceral peritoneum overlying the abdominal organs. In addition, pain from the sigmoid colon may radiate to the flank or lower back, and rectal pain may be felt in the sacral region. Continuous abdominal pain, especially of a sharp and well-localised nature, signifies irritation of the parietal peritoneum from any number of sources. Physical examination of the abdomen will allow the clinician to determine presence of peritoneal signs, as well as yield other clues such as masses or organomegaly to help elucidate the underlying diagnosis. Anorectal Pain Anorectal pain is a common symptom seen in colorectal clinics and it can be very disabling for the patient. Careful exploration of the nature, timing and characteristics of this pain can often yield a likely diagnosis prior to any attempt at examination. Information should be sought on the relationship between pain and defaecation, posture or sexual activity, as well as any radiation. Anorectal pain that is exacerbated during and after defaecation is often due to a fissure. Unrelenting and throbbing pain, associated with a palpable perianal lump, is generally due to a thrombosed external haemorrhoid. Pain accompanied by local swelling and tenderness of the perianal tissues, especially alongside fever or signs of systemic sepsis, may suggest a perianal or ischiorectal abscess. It is worth remembering that rectal malignancy rarely causes anorectal pain, unless the lesion invades the anal canal, sphincters or sensate tissues distal to the dentate line. Change in Bowel Habit Details of bowel habit are best ascertained by encouraging the patient to provide the history spontaneously. When taking a history in this area, factors influencing frequency and some details of consistency, stool characteristics and defaecatory difficulty should be sought. A history of straining, self-digitation, rectal sensation, urgency and assisted defaecation by perineal or vaginal pressure may provide valuable information about the pathophysiological problem. A change in bowel habits is important to always ascertain as it is one of the commonest symptoms seen with a colonic neoplasm. The combination of a change in bowel habits alongside colonic-type bleeding is a particularly strong indicator of the presence of a serious underlying pathology.

Generic vimax 30 caps with visa
Anticoagulation should be resumed at day 1 or 2 post-operatively or impotence and diabetes vimax 30caps with visa, in high-risk patients, 12 hours post-operatively if the patient is stable and haemostasis is ensured. These include direct thrombin inhibitors (dabigatran) or direct Xa inhibitors (rivaroxaban, apixaban, edoxaban). Bridging therapy is often not required except in patients at increased risk of thrombosis. Adverse events such as cardiac event, stroke or worsening kidney function are twice as common in patients with anaemia. This is regardless of the presence or absence of pre-existing cardiovascular co-morbidities. The practice of restrictive blood transfusion with a Hb level of 7 g/dL or less to trigger transfusion should now be adopted, except in cases where patients are symptomatic or cases of massive haemorrhage when blood transfusion is life-saving. Earlier pre-operative assessment allows earlier detection of anaemia, following which the patients can be considered for oral or intravenous iron therapy. Intra-operative complications are less well-documented and can result in equally significant morbidities or even mortality. They can occur in any operation no matter how well-planned the operation is and how meticulous the surgeon is. It is important to anticipate potential problems in order to be able to recognise and react swiftly, thereby limiting any debilitating damages. The following section describes common problems but is by no means a complete list of complications. Occurrence of major vessel injuries often mandates conversion to open procedure to allow haemorrhage control and repair of injury. Haemorrhagic control is often difficult to achieve, as the vessels are often fragile, under high pressure and not easily accessible. Temporary control with packing may be required to allow adequate resuscitation, followed by the use of occluder pins or bone wax or cement to achieve haemostasis. Occasionally, tight pelvic packing may be required for 24 to 48 hours before any attempt on haemostasis can be made, and in most cases the period of pelvic packing alone will be sufficient in achieving haemostasis. Inadvertent bowel injury may occur in either open or laparoscopic cases, with higher risks of injury in patients with significant adhesions as a result of previous surgery, or in specific cases such as duodenal injury in right hemicolectomy. Serosal tears or even full thickness enterotomies should be repaired primarily when recognised intra-operatively. In some cases, the enterotomies may go unrecognised, leading to peritonitis, formation of an intra-abdominal abscess or entero-cutaneous fistula or the need for bowel resection, stoma and delayed surgery to restore intestinal continuity. Another uncommon yet significant intra-operative complication is that of ureteric injury. Although prophylactic stenting does not prevent ureteric injury, it is a useful adjunct in the intraoperative identification of ureteric injury and should be considered in difficult cases such as re-do pelvic surgery or inflammatory conditions such as severe diverticular disease or proctitis. Intra-operative recognition of the injury allows for immediate primary repair, although in some cases the injury may only be apparent post-operatively with urine leak from perineal wound and confirmed by retrograde urethrogram. Safe and secure positioning is essential to prevent the patient slipping off the operative table, causing significant and potentially life-threatening injuries such as head, vascular or bony injuries. Many methods of patient positioning and fixation have been described including strapping, use of gel mat or use of compressive bean bag. It is therefore important to communicate with anaesthetic and theatre staff when commencing gas insufflation, and to do so at a low flow rate and keeping 4. It is, however, highly fatal, with 1 in 3 deaths in the rare occurrences, and should be kept in mind, especially in patients with sudden unexplained cardiovascular collapse and acute respiratory compromise with difficult ventilation. Preventative measures include regular change in position every 2 hours, use of pneumatic compression device and appropriate use of stirrups and avoiding ankle dorsiflexion. Post-operatively it is a potential complication to be kept in mind, especially in patients with unexplained leg pain and swelling. The obesity paradox: body mass index and outcomes in patients undergoing nonbariatric general surgery. Pre-operative oral carbohydrate loading in colorectal surgery: A randomized controlled trial. Preoperative carbohydrate treatment for enhancing recovery after elective surgery. Systematic review of the literature for the use of oesophageal Doppler monitor for fluid replacement in major abdominal surgery. Improving perioperative outcomes: Fluid optimization with the esophageal Doppler monitor, a metaanalysis and review. Monitoring of peri-operative fluid administration by individualized goal-directed therapy. Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization. Randomized clinical trial comparing laparoscopic and open surgery for colorectal cancer within an enhanced recovery programme. Laparoscopic Versus Open Colorectal Resection Within Fast Track Programs: An Update Meta-Analysis Based on Randomized Controlled Trials. Routine use of dexamethasone for postoperative nausea and vomiting: the case against. Effect of epidural analgesia on bowel function in laparoscopic colorectal surgery: A systematic review and meta-analysis. Transversus abdominis plane blocks and enhanced recovery pathways: Making the 23-h hospital stay a realistic goal after laparoscopic colorectal surgery. Health and Social Care Act 2008 (Regulated Activities) Regulations 2014: Regulation 20; 2015. Influence of oral mannitol bowel preparation on colonic microflora and the risk of explosion during endoscopic diathermy. Bowel preparation with split-dose polyethylene glycol before colonoscopy: A metaanalysis of randomized controlled trials. Polyethylene glycol versus sodium phosphate in bowel cleansing for colonoscopy: A randomized trial. Randomized clinical trial of bowel preparation with a single phosphate enema or polyethylene glycol before elective colorectal surgery. Mechanical bowel preparation for elective colorectal surgery: A multicentre randomised trial. Oral Mechanical Bowel Preparation for Colorectal Surgery: Systematic Review and Meta-Analysis. Evaluation of morbidity and mortality after anastomotic leakage following elective colorectal surgery in patients treated with or without mechanical bowel preparation. Prophylaxis and management of wound infections after elective colorectal surgery: A survey of the American Society of Colon and Rectal Surgeons membership. Nosocomial infection in surgerywards: A controlled study of increased duration of hospital stays and direct cost of hospitalization. A Survey of clinical trials of antibiotic prophylaxis in colon surgery: Evidence against further use of no-treatment controls. Oral Antibiotic bowel preparation significantly reduces surgical site infection rates and readmission rates in elective colorectal surgery. Systematic review of perioperative selective decontamination of the digestive tract in elective gastrointestinal surgery. Comparing mechanical bowel preparation with both oral and systemic antibiotics versus mechanical bowel preparation and systemic antibiotics alone for the prevention of surgical site infection after elective colorectal surgery: A meta-analysis of randomized controlled clinical trials. Oral versus systemic antibiotic prophylaxis in elective colon surgery: A randomized study and meta-analysis send a message from the 1990s.
Discount vimax 30 caps with visa
A pursestring suture has been placed around a taenia and a trocar has been inserted for decompression erectile dysfunction exam video order vimax 30caps with mastercard. It will also facilitate the application of close-fitting stoma appliances, minimising exposure of peristomal skin to irritating effluent. Convexity should be avoided in the peristomal skin, and the summit of any abdominal curvatures should be sought instead. Undue tension can result in deformation of the stoma aperture, retraction and ischaemia. This can be a useful technique if the mesentery is short and the abdominal wall is thick, when a conventional end ileostomy is difficult. Prior to the spouted and everted ileostomy, such stomas were prone to skin injury, stenosis and retraction. The innovation of Brooke in 1952 essentially resolved this issue by simply everting the small bowel to enable spouting and a sound circumferential mucocutaneous junction to be formed. The inherent advantage of the double spout negates the risk of accidently spouting the efferent limb 116 Chapter 8 Stomas 8. Occlusion of the bowel loop will allow distension of the distal limb following air insufflation. Alternatively, visualisation of the endoscopy light source can be used to identify the distal limb. It may also decrease mucous leakage from the distal limb and reduce problems with appliance application. Ideally, shear forces caused by displacement between the deeper and more superficial layers of the abdominal wall must also be avoided, as these can again compromise the lumen. This can be an issue after midline incision, which can cause some displacement between the abdominal wall layers. Turnbull and Weekley237 suggested pre-marking the stoma site with intradermal methylene blue through to the muscle layer in order to guide later straight trephine formation. This issue is reduced in laparoscopic stoma formation due to the maintenance of abdominal wall orientation. The standard trephine for most stomas is sited in the iliac fossae and transgresses the rectus muscle and sheath. Either a cruciate or vertical incision is made in the anterior sheath prior to separating the rectus fibres in the vertical axis. In theory, a trephine can be formed anywhere, and little data exists to support any specific site with regards to eventual stoma function. Siting the trephine should be influenced by the individual patient and their the Stoma Bridge 117 (a) (b) 8. The outer layer of the colon is everted and a series of mucocutaneous sutures are applied. The classical point halfway between the anterior superior iliac spine and the umbilicus is designed to allow passage through the body of the rectus whilst being away from bony prominences. However, in the morbidly obese this may lie over a large abdominal apron, and a higher trephine may be better seen and managed by the patient. A retrospective radiological study found no parastomal hernias in patients with an end colostomy trephine size maintained at less than 25 mm. Given that this does not represent a universal measure, the surgeon must at least ensure that the trephine allows safe delivery of a tension-free end but remains snug whilst not causing congestion or frank ischaemia. In the morbidly obese, this can be difficult to judge and achieve by virtue of the depth of the subcutaneous layer and the encumbrance of a fatty mesentery and epiploica. Cautious debridement of pericolonic fat can be undertaken, but one must avoid devascularisation or serosal injury (especially when diverticulae are present). Delivery of the bowel in difficult cases can be facilitated by using a laparoscopic excision site wound protector209 or a cut surgical glove. Occasionally, in the very hostile abdomen (often at the time of relaparotomy to salvage post-operative sepsis), it may not be possible to produce a safe stoma via a standard trephine. Whilst maturation of an active stoma through a midline wound should be avoided, it is an option when there is no other option. The bridge ends lie on the peristomal skin and provide support to the bowel in an attempt to reduce stoma retraction. Evidently, the presence of a bridge will partially impede the placement of a close fitting peristomal appliance and can also cause soft tissue injury. A bridge is certainly no substitution for ensuring enough mobility to allow a tension-free delivery of the bowel via the trephine. In (a) the terminal ileum has been delivered through a circular trephine in the abdominal wall, and in (b) is being everted prior to completion by mucocutaneous sutures. A small antemesenteric enterotomy is made in the distal limb and, using a pair of Alice tissue forceps, the antemesenteric portion of the apex of the loop is grasped so that the proximal limb can be everted. Mucocutaneous apposition can be undertaken without the use of a rod, using full-thickness bites of the bowel and taking the non-absorbable sutures well away from the skin edge as this facilitates their removal. The bridge helps to maintain stoma orientation and prevent retraction whilst the midline incision is closed (or reinsufflation and inspection during laparoscopy). There is a sizeable quantity of observational data that would support the concept, and despite the varied followup, the effect size would appear to be significant. A metaanalysis of seven studies comparing 250 extraperitoneal stomas to 821 standard colostomies indicates a hernia rate of 6. The technique was developed in the early 1900s following a handful of case reports of lateral space herniation and obstruction (Gabriel 1919; Rankin 1927). Evidence is lacking to support its value above the nonfixation technique, and even when it is undertaken, it does not guarantee the prevention of herniation. The skin is elevated from the rest of the abdominal wall with a Littlewoods tissue forceps and a disc of skin is excised. The optimum site for loop colostomy is selected and a transverse trephine incision made (not shown). The omentum either is partially divided or is dissected off the transverse colon to facilitate delivery of the colon through the abdominal wall. The colon is opened along the taenia with diathermy before suture maturation of the mucocutaneous junction. The lateral gutter should be closed before the ileum is delivered through the abdominal wall trephine. By placement of a long pair of scissors through the trephine in the abdominal wall, lateral retraction is achieved. Further closure of the lateral gutter is achieved by approximating the cut edge of the lateral parietal peritoneum to the cut edge of the small bowel mesentery (not shown). In theory, it confers the perceived advantages of the minimally invasive approach (reductions in length of stay, post-operative ileus, blood loss and readmission rates)90 whilst affording excellent views of the abdominal cavity. Whilst a trephine limits surgical insult, it also limits access to the abdomen for inspection and dissection. This can make delivering the correct segment of bowel, in the correct orientation and with adequate mobility, more taxing. This is particularly the case in obese patients or those who have had multiple abdominal surgeries in the past. Quite often the access incision is larger than that formed at open surgery or laparoscopy, and this may lead to prolapse and higher hernia rates. A tunnel is developed under the cut edge of the lateral peritoneum obliquely towards the previously marked stoma site. With the index finger of one hand in the tunnel, the skin disc and fat are excised to create the trephine. The end of the colon is then delivered through the tunnel and sutured to the skin. A series of sutures to approximate the divided peritoneum and to close the peritoneum over the colon completes the procedure. It should also minimise the risk of mesenteric torsion or maturation of the wrong end of the bowel.
Buy vimax 30 caps on line
Closure was possible through the stomal incision in 64 of 67 patients best erectile dysfunction pills review trusted vimax 30caps, and a laparotomy was needed in only three. They used a stapling technique for closure in 49 patients and suture closure in 18. Two patients developed leakage following closure, causing an enterocutaneous fistula that closed spontaneously in five and seven days. Stapled closure effectively creates a side-to-side ileo-ileal anastomosis by suture or staples. Likewise, Amin and others6 reported a 14% complication rate using stapled closure. By contrast, the Minnesota group found that resection and sutured closure had the highest incidence of post-operative bowel obstruction, 12%, followed by stapled closure alone, 8%, whereas suture closure carried only a 2% rate of bowel obstruction. A randomised trial to compare suture with stapled ileostomy closure indicated a significantly shorter operating time and fewer complications, particularly bowel obstruction, with stapled closure. A circumferential incision is made between the ileostomy and the skin, keeping as close to the bowel as possible. The serosa of the two limbs of the ileostomy is freed from the subcutaneous fat, the rectus sheath and, finally, the peritoneum. This ensures that the ileum can be easily replaced into the peritoneal cavity after closure. For a sutured closure, the everted ileostomy bud is turned back by scissor and gauze dissection. The opening on the anti-mesenteric border of the ileum is closed using a series of single-layer inverting interrupted sutures or a continuous extra-mucosal suture. For a stapled anastomosis, this also facilitates passage of a linear stapler blade down the limb of an often previously collapsed distal limb. In these circumstances it is often safer to resect the traumatised segment between bowel clamps after dividing the small bowel mesentery; a single layer end-to-end anastomosis is then fashioned. The ileum is gently eased back into the peritoneal cavity through the trephine in the rectus muscle. The rectus sheath is then closed using interrupted sutures, and the skin defect is either left open and packed or closed. The authors prefer to use a subcuticular absorbable purse string to reduce the skin aperture prior to packing. Healing times were longer in the purse-string group at 24 versus 35 days, but wound satisfaction scores were comparable. Wound satisfaction scores and healing times were also significantly better after purse-string closure. A recent meta-analysis including two additional trials and over 300 patients reports an infection rate of 25. A linear staple cutter is advanced down both loops of bowel to fashion a side-to-side ileoileal anastomosis. Two diamondshaped segments of skin are excised on both lateral aspects of the skin circle. A series of subcutaneous sutures are used to bring the skin edges together so as to complete a transverse skin closure. However, most patients will be able to leave hospital four to five days, or even earlier, after closure. Anti-diarrhoeals may precipitate obstruction and increase the risk of leakage from the suture line. These agents should therefore be avoided in the first two weeks after closure, despite severe diarrhoea and perianal excoriation. If anti-diarrheals must be prescribed, ispaghula or methylcellulose is preferred to loperamide or codeine in the early post-operative period. Some authors now advocate ileostomy closure as a day-case procedure; in this way, costs are reduced by a third and only two of 28 patients needed to be readmitted. A much higher complication rate is recorded following closure of a loop ileostomy utilised in the diversion proximal to a pelvic ileal pouch, since there may be persistent pelvic sepsis, stricture or a fistula from the pouch or the ileo-anal anastomosis. If infection occurs in a sutured wound, the stitches should be removed and the wound opened. There may or may not be signs of peritonitis, abscess, ileus or a fistula through the wound. The dehiscence usually resolves spontaneously, unless there is an abscess, a type-2 fistula, peritonitis or a low distal obstruction. In the first instance, conservative treatment with intravenous fluids and antibiotics is advised for dehiscence. If a fistula does develop, it usually closes spontaneously if there is no obstruction and provided there is no cavity between the hole in the ileum and the skin. Management should involve withholding oral fluids, total parenteral nutrition, drainage of any abscess and appropriate stoma therapy to contain the fistula. Intestinal obstruction is a common complication following ileostomy closure, particularly after decompression for a pelvic pouch, and should be treated conservatively by intravenous fluids and nasogastric decompression. If there is no resolution with medical therapy, there may be a distal mechanical obstruction. In these circumstances, laparotomy should then be performed early because of the risks of infarction (see Chapter 66). Other complications of ileostomy closure include hernia at the abdominal wall trephine, fistula from the original operation site and chronic sepsis around a nonabsorbable suture. Trephine site hernia has been documented at a rate of 30%, although only half of all detected hernias are subsequently repaired. One retrospective study suggests a significant effect size in terms of subsequent hernia formation after mesh placement,161 but further prospective research is currently required to clarify this. A recent series from Vilnius reports realistic rates of complications after ileostomy closure in 132 patients. Post-Operative Management 147 these results compare well with a systematic review of 48 studies including 6,107 patients44: obstruction 7%, wound infection 5%, peritonitis 1. Method of Closure Meticulous mechanical preparation of the proximal and distal colon should minimise the risks of colostomy closure. There should be no evidence of obstruction distal to the stoma or residual disease on sigmoidoscopy or contrast radiology. Consideration should be given to using local anaesthesia in selected patients having loop colostomy closure. The skin over the closure site can be closed primarily, but again the authors prefer the subcuticular purse-string. Details of restoring intestinal continuity after Hartmann resection can be found in Chapter 52. A distal colostomy irrigation is used after a rectal washout to clear the distal bowel. The mucocutaneous junction is incised around the circumference of the stoma with a small blade. The rectus muscle is then dissected free from the stoma so that it is completely mobile and can be replaced in the peritoneal cavity with ease. Although resection is not necessarily superior to simple closure, there are occasions when simple closure is suboptimal. Resection of the colostomy is indicated if the loop of colon is damaged during mobilisation from the abdominal wall, if there is evidence of stenosis, an abscess or ischaemia or if there is a fistula adjacent to the colostomy. If there is any difficulty in mobilising the bowel, the abdomen should be explored through a laparotomy incision, the bowel ends completely freed and the stoma resected so that the ends can be safely anastomosed. The mesentery is then closed, and the abdominal wall sutured as already described. Reference has already been made to stapling techniques used for closure of a loop ileostomy. The principle is to perform a side-to-side anastomosis using a linear staple cutter through the colotomy followed by closure of the mucocutaneous junction with a transverse stapler. The anastomosis, if it lies in the sigmoid, can be tested by insufflating air through the rectum. The skin may be left open and packed with a proflavine swab, or it may be closed transversely.