Proven 135 mg colospa
The remaining 10% may have negative blood cultures spasms right abdomen 135mg colospa fast delivery, possibly suggesting fungal infection. The doctor bases antibiotic selection on sensitivity studies of the infecting organism-or the probable organism, if blood cultures are negative. Be supportive Supportive treatment includes bed rest, antipyretics for fever and aches, and sufficient fluid intake. Severe valvular damage, especially aortic insufficiency, or infection of a cardiac prosthesis may require corrective surgery if refractory heart failure develops. Check dilutions for compatibility with other patient medications, and use a compatible solution. The patient has recovered from endocarditis if he maintains a normal temperature, clear lungs, stable vital signs, and adequate tissue perfusion and can tolerate activity for a reasonable period and maintain normal weight. Stress the importance of taking the medication and restricting activity for as long as recommended. Occasionally, myocarditis is complicated by heart failure and, rarely, it leads to cardiomyopathy. How it happens the myocardium may become damaged when an infectious organism triggers an autoimmune, cellular, or humoral reaction or when a noninfectious cause leads to toxic inflammation. In either case, the resulting inflammation may lead to hypertrophy, fibrosis, and inflammatory changes of the myocardium and conduction system. Feeling the flab Because of this damage, the heart muscle weakens and contractility is reduced. The heart muscle becomes flabby and dilated, and pinpoint hemorrhages may develop. If heart failure occurs, inotropic drugs, such as amrinone, dobutamine, or dopamine, may be necessary. Nitroprusside (Nitropress) and nitroglycerin may be administered to reduce preload and afterload. Upping the ante Treatment with immunosuppressive drugs or steroids is controversial but may be helpful after the acute inflammation has passed. Patients with low cardiac output may benefit from intra-aortic balloon pulsation and ventricular assist devices. Encourage use of a bedside commode because this activity stresses the heart less than using a bedpan. When recovering from myocarditis, the patient should avoid intense exercise or exertion and competitive sports. During recovery, recommend that the patient resume normal activities slowly and avoid intense exercise and competitive sports. Pericarditis Pericarditis is an inflammation of the pericardium, the fibroserous sac that envelops, supports, and protects the heart. How it happens Pericardial tissue damaged by bacteria or other substances results in the release of chemical mediators of inflammation (prostaglandins, histamines, bradykinins, and serotonin) in to the surrounding tissue, thereby initiating the inflammatory process. Histamines and other chemical mediators dilate vessels and increase vessel permeability. Vessel walls then leak fluids and protein (including fibrinogen) in to tissues, causing extracellular edema, and macrophages already present in the tissue begin to phagocytose the invading bacteria and are joined by neutrophils and monocytes. After several days, the pericardial cavity (the space between the epicardium and the fibrous pericardium) fills with an exudate composed of necrotic issue and dead and dying bacteria, neutrophils, and macrophages. Eventually, the contents of the cavity autolyze and are gradually reabsorbed in to healthy tissue. This effusion may produce heart failure effects, such as dyspnea, orthopnea, and tachyarrhythmias. It may also produce ill-defined substernal chest pain and a feeling of chest fullness. This condition compresses the heart and prevents it from filling during diastole, causing a drop in cardiac output. Heart failure results, causing symptoms such as pallor, clammy skin, hypotension, pulsus paradoxus, jugular vein distention and, eventually, cardiovascular collapse and death. The heart becomes encased in a stiff shell, which prevents proper filling during diastole. Left- and right-sided filling pressures increase, leading to a drop in stroke volume and diminished cardiac output. What to look for A patient with acute pericarditis typically complains of sharp, sudden pain, usually starting over the sternum and radiating to the neck, shoulders, back, and arms. Forward feels better the pain is usually pleuritic, increasing with deep inspiration and decreasing when the patient sits up and leans forward. An elevated blood urea nitrogen level and elevated creatinine levels may point to uremia as a cause of pericarditis. The cardiac silhouette may be enlarged, with a water bottle shape caused by fluid accumulation, if pleural effusion is present. If symptoms continue, the doctor may prescribe corticosteroids to provide rapid and effective relief. Corticosteroids must be used cautiously because pericarditis may recur when drug therapy stops. Going in When infectious pericarditis results from disease of the left pleural space, mediastinal abscesses, or septicemia, the patient requires antibiotics, surgical drainage, or both. If cardiac tamponade develops, the doctor may perform emergency pericardiocentesis and may inject antibiotics directly in to the pericardial sac. Understanding pericardiocentesis Typically performed at the bedside in an intensive care unit, pericardiocentesis involves needle aspiration of excess fluid from the pericardial sac. It may be the treatment of choice for life-threatening cardiac tamponade (except when fluid accumulates rapidly, in which case immediate surgery is usually preferred). Pericardiocentesis may also be used to aspirate fluid in such subacute conditions as viral or bacterial infection and pericarditis. Complications Pericardiocentesis carries some risk of potentially fatal complications, such as inadvertent puncture of internal organs (particularly the heart, lungs, stomach, and liver) or laceration of the myocardium or a coronary artery. Emergency equipment should be readily available during the procedure in case of such complications. In this procedure, a window is created that allows fluid to drain in to the pleural space. In constrictive pericarditis, total pericardiectomy may be necessary to permit the heart to fill and contract adequately. Administer supplemental oxygen as needed, based on oxygen saturation or mixed venous oxygen saturation levels. The nature and severity of associated symptoms determine treatment in valvular heart disease. What causes it Mitral insufficiency can result from rheumatic fever, hypertrophic cardiomyopathy, mitral valve prolapse, myocardial infarction, severe left-sided heart failure, endocarditis, untreated high blood pressure, or ruptured chordae tendineae. How it happens In mitral insufficiency, blood from the left ventricle flows back in to the left atrium during systole, causing the atrium to enlarge to accommodate the backflow. As a result, the left ventricle also dilates to accommodate the increased volume of blood from the atrium and to compensate for diminished cardiac output. System failure Ventricular hypertrophy and increased end-diastolic pressure result in increased pulmonary artery pressure, eventually leading to left-sided and right-sided heart failure. Atrial fibrillation or atrial flutter requires beta-adrenergic blockers or digoxin to slow the ventricular rate.
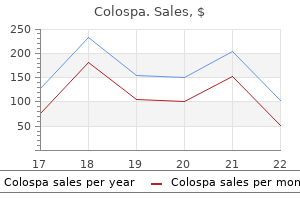
Purchase 135 mg colospa with amex
There is a wide range of histological patterns from solid through small tightly cohesive nests to single infiltrative patterns muscle relaxant discount colospa 135 mg mastercard. Localised areas of special type carcinomas may occur, consistent with intra-tumoural heterogeneity. However, maximal prognostic information is derived from a histopathological refinement of this basic classification system. This includes more accurate pathological measurement of tumour size (pT) and assessment of nodal metastatic load (pN). Histological grading the combined histological grading system of Scarff, Bloom and Richardson (modified by Elston and Ellis) has excellent concordance rates between histopathologists and clinico-pathological correlation (relapse-free and overall survival). A score is provided for each of the following: Numerous other indices have been investigated but not validated for clinical utility. The mean age at diagnosis is between 60 and 70, which is about 10 years older than female breast cancer. The tumour usually presents as a lump, but there can be nipple discharge or retraction. Male breast cancer tends to involve axillary nodes at an earlier stage, possibly due to the smaller volume of breast tissue. Some surgical disorders in childhood are similar to the same condition in adults, and are discussed in those relevant chapters elsewhere in this book. The aspects of paediatric surgery which will be covered in this chapter are those which arise from congenital anomalies, i. Pure genetic causes of anomalies which are surgically treated are uncommon but are seen in achondroplasia (limb lengthening is now offered), cystic fibrosis (with gastrointestinal problems) and haemophilia (venous access is often required). Environmental factors include maternal illness with viruses such as rubella or cytomegalovirus and, depending on the timing of the infection, would lead to different effects on the fetus. Rubella in the first trimester, when the maximum amount of development and differentiation is occurring in the embryo, is often associated with congenital heart disease, deafness, cataracts and developmental delay. The reader needs to be fully conversant with normal development and anatomy in order to be able to recognise and understand congenital anomalies. The relevant information will be covered in each section of this chapter, but it will need to be put in to the overall picture of normal embryological development to be fully understood. The implications of the various anomalies will also be mentioned, but only in the anatomical and clinical management sense. The reader needs to remember the impact any anomaly will have on the patient and more importantly on the family. This particularly affects the mother who has an underlying feeling of failure at having produced a baby which is not perfect. A synopsis of the first eight weeks follows here in brief and will then be expanded in the appropriate later part of the chapter to form the basis of understanding of the congenital anomalies which lead to the fundamentals of paediatric surgery. Fertilisation takes place between a male and female gamete, each containing 23 chromosomes, and their two nuclei coalesce to form a single nucleus containing the usual complement of 46 chromosomes, which then is called the zygote. A series of mitotic divisions then occurs which, through growth and differentiation, eventually leads to the formation of the embryo. This blastocyst continues to divide and develop, and undergoes implantation within the maternal uterine wall. As this occurs, there is differentiation in to two distinct embryonic layers: the bilaminar embryonic disc. The next six weeks sees the most rapid period of development of this embryonic disc in to the true embryo. The bilaminar disc is converted in to a trilaminar disc within the third week by the primitive streak which develops within the embryonic disc and becomes the mesoderm. The embryonic ectoderm gives rise to the epidermis, nervous system, sensory epithelium of eye, ear and nose, and skin. From this primitive streak (or mesenchymal or mesodermal area) of the embryonic disc, cells migrate cranially and caudally as the notochord from the mouth to the cloaca. The embryonic ectoderm overlying this notochord thickens to form the neural plate which will subsequently develop in to the brain, spinal cord and nerves and the neural crest. As the notochord and neural tube form, the adjacent mesoderm forms longitudinal columns called paraxial mesoderm which divide in to paired cuboidal bodies called somites. The first pair of somites develop at the cranial end, and subsequent pairs develop more caudally and develop in to the vertebral column, ribs, sternum and skull and associated muscles. Lateral to this paraxial mesoderm is the mesoderm from which coelomic spaces will develop in to the three body cavities: pericardial, pleural and peritoneal cavities. The three germ layers continue to differentiate during the fourth to the eighth week, and all major internal and external structures and main organ systems appear, although the organ function is minimal. As this is such a crucial period of development, any disturbances during this time in pregnancy (for instance, from maternal teratogens) will give rise to congenital anomalies in the various systems. The embryo folds and converts the flat trilaminar disc in to a c-shaped cylindrical embryo. The original endoderm has developed in to the yolk sac, and part of this is incorporated in to the embryo as the gut. As the cranial end of the embryo folds, it takes the mouth and heart ventrally, and incorporates Developing liver Neural tube Foregut Pharynx Heart Hindgut Midgut Yolk sac. As the caudal end of the embryo folds, the adjacent yolk sac is incorporated as the hindgut, and is carried ventrally as the cloaca, allantois and umbilical cord. The embryo also folds horizontally and incorporates part of the yolk sac as the midgut, which in these early stages is outside the embryo, within the umbilical cord. At the cranial end, six branchial arches develop in pairs, with the ears developing between the first. The limb buds are developing and grow in to limbs with hands and feet, and the tail, which was prominent, has gone before the end of the eighth week. The various important surgical congenital anomalies which can affect the future baby will be discussed below. They each originate from embryological mesenchyme and contain a core of cartilage, muscle, an artery and nerve supply from a cranial nerve. The cartilage of the first arch develops in to the malleus and incus (middle ear bones) and an associated ligament, the second in to the stapes (third middle ear bone) and styloid and part of the hyoid bone, the third in to the rest of the hyoid, and part of the fourth and sixth arch in to the larynx, and most of the rest of the cartilage disappears. The muscles of the arches develop in to facial muscles, each keeping their original nerve supply. Persistence or failure of complete regression of the branchial arches gives rise to many congenital abnormalities which are present at birth. A branchial fistula arises from the second arch, from the anterior border of the bottom third of the sternomastoid muscle, and travelling up inside the neck to open in the tonsillar fossa in the pharynx. This fistula may present as a discharging dimple on the neck (as the fistula is lined by mucus-secreting glands), and it needs to be excised (usually requiring two separate neck incisions) in its entirety from the lower neck up to the pharynx to prevent continuous discharge, infection, or the rare possibility of subsequent malignant transformation. This second arch remnant may also present as a skin or cartilaginous tag at the site of the dimple. A branchial cyst also originates from a remnant of the second arch without external connection, and contains the glairy fluid containing cholesterol crystals which typifies the mucus-secreting glands within the cyst.
Buy 135mg colospa with amex
Some believe that irrigation of deep puncture wounds is futile because the irrigant solution does not completely drain out of the wound muscle relaxant 2631 cheap 135mg colospa visa. The approach presented here is reasonable and rational, given the data that are available at this time. Puncture wounds of the foot reportedly have an overall infection rate as high as 15%. The probability of wound infection is increased with deeper penetrating injuries, delayed presentation (>24 hours), gross contamination, penetration through a rubber-soled shoe, outdoor injuries, injuries that occur from the neck of the metatarsals to the web space of the toes, and decreased resistance to infection. Specifically, diabetic patients typically present for care later and have higher rates of osteomyelitis (up to 35%). In one study, they were also 5 times more likely to require multiple operations and 46 times more likely to have a lower extremity amputation as a result of a plantar puncture wound. Joint puncture wounds have the potential to penetrate the joint capsule and produce septic arthritis. Osteomyelitis caused by Pseudomonas aeruginosa remains the most devastating of puncture wound complications. The exact incidence of osteomyelitis remains uncertain and is estimated to be between 0. A nail through the sole of a tennis or sport shoe is known to inoculate Pseudomonas organisms. Any patient who is considered to have penetration of the bone, joint space, or plantar fascia, particularly over the metatarsal heads, should be warned of the potential for serious infection and then referred to an orthopedic surgeon or podiatrist for early followup evaluation. The patient usually wants the ring removed even if it requires cutting the ring off, but occasionally, a patient has a very personal attachment to the ring and objects to its cutting or removal. When a fracture is suspected, order appropriate radiographs, either before or after removing the ring. With substantial injuries, a digital or, preferably, a metacarpal block might be necessary to allow comfortable removal of the ring. Grasping the ring after covering it with a gauze sponge may give you greater traction. If this simple method is not successful, consider several other techniques that preserve the ring. Wrap the cuff with cotton cast padding to keep the Velcro connection from separating, and clamp the tubing to prevent a slow air leak. If necessary, this procedure may be repeated several times until the swelling is adequately reduced. String wrap or string pull technique: A technique that tends to be rather time consuming and only moderately effective (but one that can be readily attempted in the field) is the string wrap or coiled-string technique. Slip the end of a string (kite string is good) under the ring and wind a tight single-layer coil down the finger, compressing the swelling as you go. This will allow traction to be applied, and the string will slide around and around the circumference of the ring as it is pulled, using lubricant, as mentioned previously. Alternatively, two cuts may be made on opposite sides of the ring, allowing it to be removed in halves. Another useful device for removing constricting metal bands is the Dremel Moto-Tool, with its sharp-edged grinder attachment. Repeat until a crack is heard; then continue clamping in different positions until the hard material breaks away. Return the larger pieces to the patient, because they may be able to receive a replacement ring from the manufacturer. For a child who sticks a finger in to a round hole in a plastic toy, sports helmet, or other plastic product and becomes entrapped, release the finger by first cutting around the hole using a standard orthopedic cast cutter. This smaller object can now be removed using any of the earlier techniques or by just protecting the underlying skin and using the cast cutter to cut this plastic ring in half. What Not To Do: Do not insist that a ring must be cut off when a patient requests that the ring not be removed, if the patient is expected to have only transient swelling of the hand or finger and there is no evidence of any vascular compromise of the affected finger. If the patient is vigilant and reliable, he can be warned of the signs of vascular compromise (pallor, cyanosis, pain, and/or increased finger swelling) and instructed to keep his hand elevated above the level of his heart and to apply cool compresses. He should then be made to understand that he is to return for further care if the circulation becomes compromised, because of the possible risk of losing his finger. If it is believed that these consequences are inevitable, be direct with the patient about having the ring removed. It usually requires local anesthesia, dissection, and severing of the deeply embedded fibers with a large-gauge needle and magnifying loupes. By applying hair remover to the hair tourniquet, the constricting bands may be lysed within 10 to 15 minutes. Even when the constricting bands appear to be completely released, provide for a wound check within 24 hours. There may only be a puncture wound without a clearly visible or palpable foreign body. Be suspicious of all puncture wounds (especially on the foot) that have been caused by a wooden object. If the sliver is visible or easily palpated, locally infiltrate with 1% lidocaine (Xylocaine) with epinephrine, and clean the skin with povidone-iodine solution. Avoid sutures when possible, especially absorbable, buried sutures, because of the increased risk for infection. A more vertical splinter should be approached in the same manner, but the incision will be straight down along the length of the sliver as deep as possible, thereby releasing the entire foreign body from the surrounding tissue. Be careful not to incise any important anatomic structures, such as nerves, vessels, or tendons. Inform the patient that it is often difficult to find such a splinter under the skin ("like a needle in a haystack") and that you will limit your search to about 10 to 15 minutes because further exploration may cause harm. Attempt to stabilize the palpable foreign body with the fingers of your nondominant hand while you cut down on the most superficial point of the sliver with a No. When the splinter is exposed, grab it with plain forceps and release it from the surrounding tissue by cutting down on as much of its length as necessary to free it up. When a sliver is lost under the dermis and cannot be palpated or located using this technique, it can be managed in one of two ways. They will either heal over without consequence or, as with most organic foreign bodies, form an abscess that can be drained, thereby releasing the foreign body. These patients should initially be placed on an antibiotic, such as cephalexin (Keflex), and fully informed of the risks, as well as being included in the decisionmaking process. Alternatively, these patients can have the foreign body removed by a clinician who is skilled in ultrasound-guided techniques. Patients who have larger organic foreign bodies or foreign bodies located in high-risk areas or patients who are at high risk for infectious complications. Even after the foreign body has been found and removed, be cautious about telling the patient that the splinter has been entirely removed. Warn the patient about the signs of infection, and schedule a 48-hour wound check. Prophylactic antibiotics are generally not required when the sliver is thought to be completely removed. For fine cactus spines, briars, or even multiple small splinters, use fine forceps to remove as many of these slivers as possible and then send the patient home to complete treatment. What Not To Do: Do not order plain radiographs unless a suspected sliver is made of glass or metal. In addition, cactus and sea urchin spines, thorns, plastic, and aluminum all tend to be difficult to visualize on plain radiographs. Do not try to pull the sliver out by one end unless you feel confident that the material it is composed of will not fragment or be friable. Otherwise, it is likely to break and leave a fragment behind or leave a trail of debris.
Buy colospa overnight delivery
Before it reaches the stomach spasms kidney order colospa visa, it gives off a hepatic branch which passes in the lesser omentum to the liver and gall bladder and the pyloric branch to the pyloric sphincter. The posterior vagus nerve gives off a coeliac branch which passes to the coeliac plexus before sending a gastric branch to the posterior surface of the stomach. The gastric divisions of both anterior and posterior vagi reach the stomach at the cardia and descend along the lesser curve between the anterior and posterior peritoneal attachments of the lesser omentum. However, with the advent of H2 receptor antagonists and proton pump inhibitors and the discovery of the role of H. However, it is necessary to understand the role of the vagus, as vagotomy is still required in surgery for bleeding peptic ulcer, and also a knowledge of the oesophageal hiatus and the relations of the vagus nerve is required so that these nerves are not inadvertently damaged in repair of hiatus hernia. The vagus nerve constitutes both the motor and secretory nerve supply for the stomach, i. When the nerve is divided in the operation of vagotomy, acid secretion is cut down in the stomach, but so is motility, so that the stomach empties through an intact pylorus only with difficulty. Because of this, total vagotomy (truncal vagotomy) must always be accompanied by some form of drainage procedure: either a pyloroplasty to destroy the pyloric sphincter or a gastrojejunostomy to bypass the pyloric sphincter. In the operation of highly selective vagotomy (proximal selective vagotomy) it is possible to avoid the drainage procedure, as the nerve of Latarjet remains intact and this maintains the innervation of the pyloric antrum and hence its propulsive activity. Structure of the gastric mucosa the surface of the gastric mucosa is covered by columnar epithelial cells that secrete mucus and alkaline fluid that protects the epithelium from mechanical injury and from gastric acid. The surface of the mucosa is studded with gastric pits, each pit being the opening of a duct in to which the gastric glands empty. The cardiac gland area is the small segment located near the gastro-oesophageal junction. Histologically it contains principally mucus-secreting cells, although occasionally a few parietal (oxyntic) cells are present. The remainder of the stomach is divided in to the acidsecreting region (oxyntic gland area) and the pyloric gland area. The oxyntic gland area is the portion containing the parietal (oxyntic cells) and the chief (zymogen) cells. The pyloric end area constitutes the distal 30% of the stomach and contains G cells that produce gastrin. In this region there are few oxyntic and peptic cells, mucus-secreting cells predominating. As in the rest of the gastrointestinal tract the muscular wall of the stomach is composed of an inner circular layer and an outer longitudinal layer. However, in addition there is an incomplete inner layer of obliquely situated fibres which is more prominent near the lesser curvature. The neck of the gland contains many mucus cells, oxyntic cells being most numerous in the midportion of the glands and chief cells predominating in the basal portion. This is approximately 5 cm long and it ascends from the pylorus, being directed superiorly, posteriorly and to the right. Immediately posterior to it lie the portal vein, the common bile duct and gastroduodenal artery. The relationship of the gastroduodenal artery to the first part of the duodenum is important because erosion of posterior duodenal ulcers in to the gastroduodenal artery will cause haematemesis and melaena. The bile ducts and main pancreatic ducts enter the second part of the duodenum together at the duodenal papilla on its posteromedial side. The second part of the duodenum is crossed by the transverse colon and lies anteriorly to the right kidney and ureter. Third part the third part of the duodenum is approximately 10 cm long and runs horizontally to the left. It is crossed anteriorly by the root of the mesentery and the superior mesenteric vessels. The mesentery contains the superior mesenteric vessels which enter the mesentery anterior to the third part of the duodenum, the lymph nodes draining the small intestine, and autonomic nerve fibres. At the duodenaljejunal flexure the small intestine leaves the posterior abdominal wall and acquires a mesentery. At surgery the duodenojejunal flexure may be identified by the presence of the suspensory ligament of Treitz. This is a peritoneal fold descending from the right crus of the diaphragm to the termination of the duodenum. These two arteries both lie in the curve between the duodenum and the head of the pancreas, supplying both the duodenum and the head of the pancreas. In the mesentery of the jejunum the arteries form one or two arcades some distance from the free edge of the mesentery, and long straight branches from these arcades run to supply the jejunum. In the ileum the arterial supplies form several rows of arcades in the mesentery, and the final straight arteries to the ileum are shorter than in the jejunum. In general, the jejunum is most likely to be found at or above the level of the umbilicus, while the ileum tends to lie below the level of the umbilicus in the hypogastrium and pelvis. It consists of the caecum, ascending colon, transverse colon, descending colon, sigmoid colon and rectum. The caecum is a dilated blind-ended pouch situated in the right iliac fossa and is usually completely covered with peritoneum. The ileocaecal valve lies on the left side of the junction between the caecum and ascending colon. Tumours may grow to a large size in the caecum without causing any obstruction until they encroach on the ileocaecal junction. The taenia coli, three flattened bands of longitudinal muscle which pass from caecum to rectosigmoid, converge at the base of the appendix. The taenia are shorter than the length of the bowel hence the sacculated appearance of the large bowel. The ascending colon extends from the caecum to the undersurface of the liver where, at the hepatic flexure, it turns left to become the transverse colon. The upper half of the small intestine is termed the jejunum, the remainder being termed the ileum, although the distinction between the two is not sharply defined. The mesentery of the small intestine is about 15 cm long and is attached across the posterior abdominal wall. It commences at the duodeno-jejunal juncture to the left of the second lumbar vertebrae and passes obliquely downwards to the right sacroiliac joint. The transverse colon passes to the left, where it becomes the descending colon at the splenic flexure. It is attached to the anterior border of the pancreas by the transverse mesocolon. Superiorly it is related to the liver, gall bladder, greater curvature of the stomach and the spleen. Posteriorly lie the right kidney, second part of the duodenum, pancreas, small intestine and the left kidney. Between the splenic flexure and the diaphragm is a fold of peritoneum, the phrenicocolic ligament. Posteriorly to the descending colon lies the left kidney, quadratus lumborum and iliacus. The sigmoid colon commences at the pelvic brim and extends to the rectosigmoid junction. It has a mesentery which occasionally is extensive allowing the sigmoid colon to hang down in to the pelvis. The sigmoid loop rests on the bladder in the male and is related to the uterus and the posterior fornix of the vagina in the female. Hence the development of vesicocolic and vaginocolic fistulae in diverticular disease of the sigmoid colon. The taenia coli extend from the base of the appendix to the rectosigmoid junction. The colon, but neither the caecum, the appendix, nor rectum, possesses fat-filled peritoneal tags scattered along its surface. These are called appendices epiploicae and are most numerous in the sigmoid colon.
Proven colospa 135 mg
Regional differences in ventilation Ventilation of the lung does not occur uniformly muscle relaxant high blood pressure order colospa with american express. Indeed dependent regions of the lung are much better ventilated than non-dependent regions of the lung. This force exists because of the strong cohesive forces between molecules along the surface. Its importance in the lung can be demonstrated by comparing the pressure volume behaviour in isolated lungs inflated with either water or air. Lungs inflated with air have a much greater compliance and so are easier to distend than lungs filled with water. Uninhibited, the surface tension within the alveoli would significantly decrease the compliance of the lungs, perhaps by as much as 50%. However, specialised cells within the alveolar epithelium secrete surfactant, a lecithin-rich, detergent-like substance that significantly decreases surface tension. Although these cells are plentiful in adult life they are not productive until a late stage of fetal maturity. Premature babies are very prone to develop respiratory distress, characterised by stiff lungs, atelectasis and pulmonary oedema. In the dependent regions of the lung, resting intrapleural pressure is lower than in the apical regions. The dependent parts of the lung are on the steeper part of the compliance curve and are more easily distended. This situation can be changed dramatically when the lung is ventilating at low volumes. Under these circumstances the lung tissue at the base becomes compressed after full expiration. The intrapleural pressures are now positive at the lung base and much less negative at the apex. When the lung expands, the non-dependent region is in the most advantageous part of the compliance curve, so that its volume will increase rapidly, whilst the dependent lung cannot increase its volume at all until the intrapleural pressures become subatmospheric. Closure of small airways There is another important effect, which can be observed at low lung volumes. As the volume of the lung decreases during expiration the intrapleural pressure in the dependent regions becomes positive. The diagram illustrates the causes of regional differences in ventilation due to the weight of the lung. During normal breathing (right), the base of the lung is on a steeper part of the compliance curve and expands more per unit of negative pressure. The situation is reversed on the left, where, at lower lung volumes, the apex is on the steeper part of the curve. However in patients whose lungs have lost elastic tissue (for example, the elderly or those with emphysema), airway closure occurs at higher lung volumes. The major site of resistance is in the medium-sized bronchi, and the very small bronchioles contribute very little. Most of the pressure drop across the airways occurs up to the seventh generation of bronchi and less than 20% beyond this point. Because the peripheral airways contribute so little to resistance, the detection of lung disease here is made much more difficult. Elastic properties of the chest wall Just as the lung has elastic properties which tend to make it collapse, the chest wall has elastic properties which tend to make it expand. The elastic recoil of the lung is balanced by the tendency of the chest to expand and the lung is at the end of a normal expiration. Conversely at very low lung volume the airway calibre is reduced and airway resistance increased. Patients with significant chronic obstructive airways disease often breathe at high lung volumes in order to decrease airway resistance. The causes of bronchial smooth muscle contraction include irritant gases or allergens such as smoke or pollen. The injection of microemboli or histamine in to the pulmonary circulation results in the constriction of smooth muscle in the alveolar ducts. At high altitude the density of air is reduced, so that airway resistance is also reduced. Conversely, during deeper dives under the ocean, increased pressure increases the density of inspired gases so that airway resistance is increased. When a subject takes a maximal inspiration and then forcefully expires, not only are the lungs compressed but also the small airways. The diagram shows how the variation in resistance and compliance between lung units can cause uneven ventilation. Tissue resistance Just as gas transport within the airways contributes to resistance, so do the frictional forces between tissues. The tissue resistance accounts for about 20% of the total in a fit and healthy adult. The sum of tissue and airway resistance is sometimes called pulmonary resistance to distinguish it from airway resistance. Uneven ventilation within the lungs Until now we have assumed that compliance and resistance within the lung were uniform. Here the volume change in inspiration is both large and rapid, so it is completely filled before expiration begins. Lung unit (b) has stiff walls of low compliance; its volume change is rapid but small, although it is complete before expiration begins. Lung unit (c) has increased airway resistance, so that filling is slow and, therefore, incomplete before expiration begins. Units (b) and (c) contribute to uneven ventilation, but the pattern of inequality will depend on the depth and frequency of respiration. Differences in compliance and resistance are not the only mechanism of uneven ventilation within the lungs. Another mechanism is incomplete diffusion beyond the fifteenth generation of airways. The rate of diffusion of gas molecules is so rapid that differences in concentration are abolished within 1s, despite the very low velocity of gas within this region. Under these circumstances the distances within this region will be greatly increased and diffusion ceases to be an adequate mechanism for gas transport. Five percent is also the efficiency of breathing (as defined by useful work/energy expended). In some patients, where oxygen delivery is critically impaired, paralysing and ventilating the patient can make useful savings in oxygen consumption. Respiratory function tests can be classified according to what they measure: ventilation and lung volumes, compliance, control of ventilation, and diffusion. There are some tests which take in to account many aspects of respiratory physiology. Since work is equal to pressure multiplied by volume, a pressure-volume diagram describes the work done. As the respiratory rate increases, flow rates become faster and the viscous work becomes larger. In patients with reduced compliance, for example, in fibrotic lung disease, breaths tend to be rapid and small. Patients with chronic obstructive lung disease tend to take slower, deeper breaths. Interestingly, at rest a healthy individual is using about 5% of his resting oxygen consumption to breathe. Nitrogen washout is frequently performed in the clinical setting by the anaesthetist, not to measure lung volumes, but to replace all nitrogen in the lungs with oxygen so that, once asleep, a paralysed patient will remain well oxygenated if there is any difficulty in intubation or ventilation.
Buy colospa on line
The anterior cells drain in to the hiatus semilunaris infantile spasms 9 month old buy colospa 135mg, the middle (normally only one or two) on the bulla ethmoidalis and the posterior in to the superior meatus. Acute ethmoiditis in childhood can easily spread in to the orbit through the lamina papyracea and cause proptosis, chemosis, ophthalmoplegia and periorbital oedema. The abscess may be drained through a small incision in the medial part of the orbit. For maxillary sinus wash-out a cannula is inserted in to the sinus via the inferior meatus of the nasal cavity. Nerve supply the sinuses are supplied by the ophthalmic division of the trigeminal nerve via the anterior and posterior ethmoidal nerves of the nasociliary branch. Arterial supply the arterial supply is from the anterior and posterior ethmoidal branches of the ophthalmic artery. Frontal sinus the frontal sinuses are not present at birth but start to appear in the second year of life. It may be a single small air cell above the medial end of the orbit or a cluster of cells extending in to the lateral end of the orbital roof and several centimetres up in to the frontal bone. Nerve supply the maxillary division of the trigeminal nerve supplies the sinus through its infraorbital and superior dental nerves. Arterial supply the maxillary sinus is supplied by branches of the maxillary artery. Infection of the frontal sinus is often associated with infection of the maxillary sinus as their openings are very close to each other. Acute sinusitis can spread posteriorly in to the anterior cranial fossa causing extradural and subdural abscesses or meningitis. The pus in the sinus can be drained by wash-out through the nose or by a small incision on its wall just below the medial end of the eye brow. Nerve supply the nerve supply is from the ophthalmic division of the trigeminal nerve through the posterior ethmoidal nerve. The root of the neck is the junctional area between the thorax and the neck and contains all the structures going from the thorax to the neck and vice versa. Nerve supply the nerve supply is through the supratrochlear and supraorbital branches of the frontal division of the ophthalmic nerve and the blood supply is via the corresponding branches of the ophthalmic artery. Sphenoidal sinus the sphenoidal sinus, like the maxillary sinus, is very small at birth. The size in the adult is variable and the right and left sinuses may not be symmetrical. It occupies the body of the sphenoid but may extend in to its greater and lesser wings. The pituitary fossa bulges in to the roof in its posterior half and anteriorly the roof separates the sinus from the optic chiasma and the optic nerves. The lateral wall also is thin and separates the sinus form the cavernous sinus and the internal carotid artery. It functions to prevent the lung and pleura rising further in to the neck during respiration. The subclavian artery and vein and the brachial plexus lie on the suprapleural membrane. Subclavian artery the right subclavian artery is a branch of the brachiocephalic trunk and the left arises directly from the arch of the aorta beyond the origin of the left internal Left recurrent laryngeal nerve Phrenic nerve Scalenus medius Stellate ganglion of sympathetic trunk Oesophagus Thoracic duct Trachea Carotid sheath Common carotid artery Scalenus anterior Brachial plexus Upper trunk Middle trunk Lower trunk Subclavian artery Vagus nerve Subclavian vein Internal jugular vein. The carotid sheath and contents are cut and reflected to show the deep structures in the neck. The subclavian vein runs parallel to the artery but in front of the scalenus anterior at a slightly lower level. The roots and the trunks of the brachial plexus lie behind the subclavian artery on the first rib between the scalenus anterior and the scalenus medius muscles. The branches of the subclavian artery are as follows: Subclavian venepuncture can be carried out using an infraclavicular or supraclavicular approach. In the former the needle is inserted below the clavicle at the junction of its middle and medial thirds and advanced upwards and medially behind the clavicle towards the sternoclavicular joint. In the supraclavicular approach the needle is inserted about 2 cms above the clavicle at the junction between its middle and medial thirds at the lateral border of the sternocleidomastoid. The needle is advanced downwards and medially towards the sternoclavicular joint and aspirated for the free flow of blood from the vein. There is the risk of pneumothorax and an inadvertent puncture of the subclavian artery in both of these approaches. A number of approaches are described to block the brachial plexus in the supraclavicular region. In the supraclavicular perivascular method the needle is inserted at the middle of the clavicle just lateral to the subclavian artery pulsation and directed backwards downwards and inwards. In the interscalene approach the needle is inserted at a higher level at the level of the cricoid cartilage and advanced towards the transverse process of the sixth cervical vertebra and the local anaesthetic is injected deep to the prevertebral fascia (the plane containing the nerves). Phrenic nerve paralysis and/or inadvertent injection in to the vertebral artery are complications. It enters the foramen transversarium at the sixth cervical vertebra and ascends through the foramina transversaria of the sixth to the first cervical vertebrae and enters the cranial cavity and branches to supply the brain and spinal cord. The internal thoracic (mammary) artery passes vertically downwards a fingers breadth lateral to the sternum. In the sixth intercostal space it divides in to the musculophrenic artery and the superior epigastric artery. The thyrocervical trunk is a branch of the subclavian artery medial to the scalenus anterior. It divides in to the inferior thyroid artery, the transverse cervical and the suprascapular arteries. The inferior thyroid artery lies behind the carotid sheath and ascends in front of the scalenus anterior. At the level of the transverse process of the sixth cervical vertebra the artery arches medially and enters the postero-medial aspect of the capsule of the thyroid gland at its lower third. The recurrent laryngeal nerve is closely related to the artery and its branches near the lower pole of the thyroid gland. Thoracic duct this duct carries lymph from the whole body except that from right side of thorax, right upper limb, and right side of head and neck. It arises in the abdomen, passes through the thorax and enters the neck lying on the left side of the oesophagus. At the root of the neck it arches laterally lying between the carotid sheath and the vertebral artery. Inadvertent puncture or laceration of the thoracic duct will cause escape of lymph in to the surrounding tissue and occasionally chylothorax. Subclavian vein the subclavian vein follows the course of the subclavian artery in the neck, but lies in front of the scalenus anterior on the first rib. Veins accompanying the branches of the subclavian artery drain in to the external jugular, the subclavian vein or its continuation, the brachiocephalic vein (formed by the union of the subclavian and the internal jugular veins). The superior ganglion lies at the level of C2 & C3, the middle at the level of C6, and the inferior ganglion at the neck of the first rib behind the vertebral artery. Often the inferior ganglion is fused with the first thoracic ganglion to form the stellate ganglion. Grey rami from this reach the upper limb through the roots of the brachial plexus mostly through C7 and C8. The preganglionic input to the cervical ganglia (including the stellate) are from the upper thoracic white rami. The thoracic part of the sympathetic chain can be seen lying on the heads of the upper ribs through a thoracoscope after deflating the lung. Afferents to these nodes are from the superficial tissues of the regions corresponding to those drained by the veins along which they lie.
Buy 135mg colospa free shipping
The inferior surface of the tongue is smooth and shiny and in the midline has the frenulum of the tongue spasms right upper abdomen discount 135 mg colospa overnight delivery. The posterior third of the tongue faces the oropharynx and the laryngeal part of the pharynx. There are a number of elevations seen here which form the lingual tonsil, a lymphoid aggregation embedded in the musculature. Fractures of the mandible Fractures of the mandible happen more often than those of the upper facial skeleton. The condyle of the mandible can fracture due to a blow to the chin and this may result in dislocation of the temporo-mandibular joint. Fractures of the angle can run downwards and forwards, or downwards and backwards. However, if the fracture line runs downwards and backwards, muscular contraction tends to displace the posterior fragment upwards. Fractures of the body of the mandible are most common in the canine region as the length of the root of the canine tooth weakens the bone in this position. These attach the tongue to the mandible, hyoid bone, styloid process and the soft palate respectively. The lingual nerve which is a branch of the mandibular division of the trigeminal (nerve of the first branchial arch) carries common sensation from the anterior two-thirds. The sensory supply of the posterior third, including the vallate papillae, is by the glossopharyngeal nerve which is the nerve of the third branchial arch. Fimbriated fold Deep lingual vein Frenulum Blood supply Arteries the tongue is supplied by the lingual artery, a branch of the external carotid artery the course of which is illustrated in. The dorsal lingual arteries are branches which supply the mucous membrane as well as the palatine tonsil and the soft palate. At its commencement, the hypoglossal nerve and its companion vein crosses superficial to the artery. At the posterior third, branches from the tonsillar artery (branch of the facial) and ascending pharyngeal artery anastomose with those of the lingual artery. There is only a poor communication between the two lingual arteries across the median septum. Muscles the intrinsic muscles A midline fibrous septum divides the tongue in to right and left halves. In the anterior two-thirds there is only minimal communication of lymphatics across the midline septum so that metastases from this portion tend to be ipsilateral. Posterior third lymphatics form extrinsic networks and facilitate early bilateral metastases. Lymphatics from the tip of the tongue pass to the submental nodes and from there to the lower deep cervical nodes. From the mid portion lymphatics pass to the submandibular nodes and then to the deep Hyoglossus muscle Occipital artery Dorsal lingual arteries. From the posterior third the drainage is to the upper deep cervical of both sides. The anterior part of the tongue rests on the mucosa covering the floor of the mouth. In the midline, the frenulum of the tongue is seen on the floor connecting the tongue to the mandible. On either side of the frenulum is the sublingual papilla on which the submandibular gland duct opens. More posteriorly between the mylohyoid and the tongue lies the hyoglossus muscle which in fact is the side wall of the tongue. On the hyoglossus it breaks up in to branches to supply all the muscles (both extrinsic and intrinsic) of the tongue except the palatoglossus. Paralysis of the hypoglossal nerve is manifested as fibrillation of the tongue as well as wasting of the muscles. The anterior twothirds is bony, forming the hard palate and the posterior third, the soft palate, is muscular. The palatine process of the maxilla and the horizontal plate of the palatine bones form the hard palate. The tensor palatini, the levator palatini, the musculus uvuli, the palatoglossus and the palato-pharyngeus form the muscular core of the soft palate. The tensor palatini winds round the pterygoid hamulus of the medial pterygoid plate to enter the cavity of the pharynx and its tendon spreads out to become the palatine aponeurosis to be attached to the posterior aspect of the hard palate. The levator palatini takes origin from the base of the skull inside the pharynx and is inserted to the palatine aponeurosis. Both the tensor and the levator palatini in their upper part are attached to the cartilaginous part of the Eustachian (auditory) tube. Their contraction opens the tube to transmit air from the pharynx to the middle ear. Children with cleft palate may develop deafness as this mechanism is often affected. The mucosa of the palate has stratified squamous epithelium on the oral surface and ciliated columnar epithelium on the surface facing the nasal cavity. The sensory nerve supply of the palate is by branches from the maxillary nerve and the motor supply is by the cranial part of the accessory nerve transmitted through the vagus as its pharyngeal branch. The deep part of the submandibular gland and the submandibular duct are described on page 418. The lingual nerve, a branch of the mandibular division of the trigeminal nerve, runs forward above the mylohyoid. It gives off a gingival branch which supplies the whole of the lingual gingiva and the mucous membrane of the floor of the mouth. The lingual nerve winds round the submandibular duct (page 418) before getting distributed to the mucosa of the anterior two-thirds of the tongue. The submandibular ganglion is suspended from the lingual nerve as it lies on the hyoglossus. Before reaching the floor of the mouth the lingual nerve lies against the periosteum of the alveolar process closely related to the 3rd molar tooth. The hypoglossal nerve descends between the internal jugular vein and the internal carotid artery, giving branches to thyrohyoid and geniohyoid muscles. It supplies the superior limb of the ansa cervicalis (C1) to innervate the infrahyoid muscles. Superficial surface Tongue There is natural plane of separation between the skin and the superficial surface. Anteromedial surface This, in fact, is U-shaped extending from the lateral surface of the masseter to the medial surface of the medial pterygoid muscle winding round the posterior border of the mandibular ramus. Where this surface meets the superficial surface is the convex anterior border from which emerges the parotid duct and the five branches of the facial nerve. The stylomandibular ligament separates the deep aspect of this surface from the submandibular gland. Sternocleidomastoid Submandibular gland Submandibular duct Sublingual gland Sublingual ducts. Posteromedial surface region and solidified around a number of important structures. The story emphasises the complex configuration and relations of the gland which will no doubt be appreciated by a surgeon doing a total parotidectomy. The parotid gland lies between the mastoid process and the sternocleidomastoid posteriorly, and the ramus of the mandible, which it clasps anteriorly. The upper pole of the gland is a small concave surface and it adheres to the cartilaginous part of the auditory tube and it is wedged between the latter and the capsule of the temporomandibular joint. The parotid gland is enclosed in a tough capsule derived from the investing layer of the deep fascia.