Buy glycomet canada
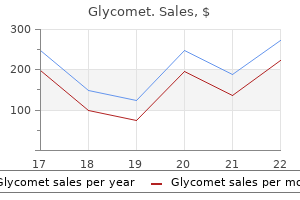
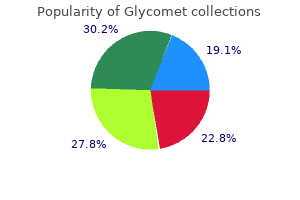
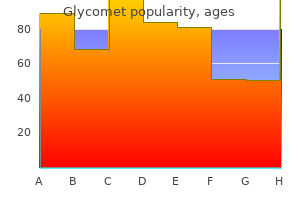
KumagaiH diabetes insipidus and desmopressin glycomet 500 mg line,etal: Efficacy and safety of a novel -agonist for managing intractable pruritus in dialysis patients. YueJ,etal: Comparison of pregabalin with ondansetron in treatment of uraemic pruritus in dialysis patients. Intrahepatic cholestasis of pregnancy, primary sclerosing cholangitis, and hereditary cholestatic diseases such as Alagille syndrome all have pruritus in common. Another disease, primary biliary cirrhosis, is discussed separately next because of its many other cutaneous manifestations. The pathophysiology is not well understood, but it appears that lysophosphatidic acid, formed by the action of the enzyme autotaxin on lysophosphatidylcholine, is central. The serum conjugated bile acid levels do not correlate with the severity of pruritus, and the theory invoking endogenous opioids as the main cause has not been upheld by recent studies. Ursodeoxycholic acid is effective for the pruritus in intrahepatic cholestasis of pregnancy, but not for the itching of primary biliary cirrhosis from other causes. Liver transplantation is the definitive treatment for end-stage disease and provides dramatic relief from the severe pruritus. A B Primary biliary cirrhosis such as acquired perforating disease, lichen simplex chronicus, and prurigo nodularis may develop and contribute to the degree and severity of pruritus. Many patients have concomitant xerosis, and aggressive use of emollients, including soaking and smearing, may help. A trial of -linolenic acid cream twice daily was effective, as was one using baby oil. Naltrexone, topical tacrolimus, and ondansetron also were reported to be useful in initial trials, but subsequent studies indicated these agents are ineffective. Thalidomide, intranasal butorphanol, and intravenous lidocaine are less practical options. Itching may begin insidiously and may be the presenting symptom in a quarter to half of patients. This almost intolerable itching is accompanied by jaundice and a striking melanotic hyperpigmentation of the entire skin; the patient may turn almost black, except for a hypopigmented "butterfly" area in the upper back. Serum bilirubin, alkaline phosphatase, serum ceruloplasmin, serum hyaluronate, and cholesterol values are increased. The disease is usually relentlessly progressive with the development of hepatic failure. DecockS,etal: Cholestasis-induced pruritus treated with ultraviolet B phototherapy. UiboR,etal: Primary biliary cirrhosis: a multi-faced interactive disease involving genetics, environment and the immune response. Polycythemia vera More than one third of patients with polycythemia vera report pruritus; it is usually induced by temperature changes or several minutes after bathing. Aspirin has been shown to provide immediate relief from itching; however, there is a risk of hemorrhagic complications. Paroxetine, 20 mg/ day, produced clearing or near-complete clearing in a series of nine patients. Two new options are being tested based on the knowledge that polycythemia vera results from a Jak2activating mutation. Winter itch is characterized by pruritus that usually first manifests and is most severe on the legs and arms. Extension to the body is common; however, the face, scalp, groin, axillae, palms, and soles are spared. Frequent and lengthy bathing with plenty of soap during the winter is the most frequent cause. This is especially prevalent in elderly persons, whose skin has a decreased rate of repair of the epidermal water barrier and whose sebaceous glands are less productive. Low humidity in overheated rooms during cold weather contributes to this condition. Treatment consists of educating the patient on using soap only in the axillae and inguinal area and lubricating the skin with emollients immediately after showering. Preparations containing lactic acid or urea applied after bathing are helpful in some patients but may cause irritation and may worsen itching in patients with erythema and eczema. For those with more severe symptoms, long-standing disease, or a significant inflammatory component, a regimen referred to as "soaking and smearing" is dramatically effective. The patient soaks in a tub of plain water at a comfortable temperature for 20 min before bedtime. This will trap the moisture, lubricate the skin, and allow for excellent penetration of the steroid component. An old pair of pajamas is then donned, and the patient will note relief even on the first night. The nighttime soaks are repeated for several nights, after which the ointment alone suffices, with the maintenance therapy of limiting soap use to the axillae and groin, and moisturization after showering. Plain petrolatum may be used as the lubricant after the soaking if simple dryness without inflammation is present. KimuraN,etal: Prevalence of asteatosis and asteatotic eczema among elderly residents in facilities covered by long-term care insurance. Pruritusani Pruritus is often centered on the anal or genital area (less frequently in both), with minimal or no pruritus elsewhere. Anal neurodermatitis is characterized by paroxysms of violent itching, when the patient may tear at the affected area until bleeding is induced. Specific etiologic 48 factors should always be sought and generally can be classified as dermatologic disease, local irritants (which may coexist with colorectal and anal causes), and infectious agents. Allergic contact dermatitis is a common dermatologic cause or secondary complication of pruritus ani. It occurs from various medicaments, fragrance in toilet tissue, or preservatives in moist toilet tissue, with one study reporting 18 of 40 consecutive patients being patch test positive. Seborrheic dermatitis, psoriasis, lichen planus, lichen sclerosis, and atopic dermatitis all may cause perianal itching, and an examination of other classic sites of involvement with these conditions should be carefully undertaken. Biopsy of resistant dermatitic-appearing skin should be done in nonresponsive pruritus ani. Irritant contact dermatitis from gastrointestinal contents, such as hot spices or cathartics, or failure to cleanse the area adequately after bowel movements may be causal. Anatomic factors may lead to leakage of rectal mucus on to perianal skin and thus promote irritation. Physical changes such as hemorrhoids, anal tags, fissures, and fistulas may aggravate or produce pruritus. Scrapings are examined directly with potassium hydroxide mounts, and cultures will usually reveal Candida albicans, Epidermophyton floccosum, or Trichophyton rubrum. Other sites of fungal infection, such as the groin, toes, and nails, should also be investigated. Erythrasma in the groin and perianal regions may also occasionally produce pruritus. The use of tetracyclines may cause pruritus ani, most often in women, by inducing candidiasis. Pinworm infestations may cause pruritus ani, especially in children and sometimes in their parents. Pediculosis pubis may cause anal itching; however, attention is focused by the patient on the pubic area, where itching is most severe. Scabies may be causative but often will also involve the finger webs, wrists, axillae, areolae, and genitalia.
Syndromes
- Take any medicines your doctor told you to take with a small sip of water.
- Are you having trouble getting an erection, or keeping erections?
- Ages 60 - 69: 42 - 290 ug/dL
- New spine problems may develop, especially in children who have surgery before their spine has stopped growing.
- Fatigue and feeling slow or sluggish
- Spinal cord abscess
- Cramps
- Control the electrical activity of the heart
- Intravenous pyelogram (IVP) - not as commonly used
- The name of the product (ingredients and strengths if known)
Discount glycomet online mastercard
Conclusion Ilioinguinal neuralgia is a chronic pain syndrome that leads to disability and to poorer quality of life managing pre diabetes purchase generic glycomet. The syndrome is diagnostically challenging, so surgeons must have a comprehensive understanding of and familiarity with the anatomic variations of the nerve and the levels of contribution. Points of parietal perforation of the ilioinguinal and iliohypogastric nerves in relation to optimal sites for local anaesthesia. Pulsed radiofrequency of lumbar nerve roots for treatment of chronic inguinal herniorraphy pain. Graham, Gurvinder Kaur, and Aruna Ganju Genitofemoral neuralgia is characterized by chronic pain and paresthesias in the distribution of the genitofemoral nerve. It is a rare condition, as only 35 cases have been reported in the literature since 1942. Although this can be seen following suppurative processes in the retroperitoneum, surgical intervention or trauma to the lower abdominal quadrants can also result in this condition. Symptoms tend to be exacerbated by hyperextension of the hip and ambulation,5 and relief can sometimes be derived from hip flexion or recumbency. It is hypothesized that fibrous adhesions resulting from surgical manipulation, trauma, or chronic inflammation to the retroperitoneum or lower abdominal quadrants causes entrapment of the nerve or its branches. Patient Selection Genitofemoral neuralgia is a predominantly clinical diagnosis; ilioinguinal neuralgia is in the differential diagnosis and should be ruled out. Both the ilioinguinal and genitofemoral nerves innervate the groin; only the latter innervates the proximal medial thigh. In addition, the external spermatic branch, which arises from the genitofemoral nerve, can be affected and thus manifest as impairment of the cremasteric reflex and sensation of the upper medial thigh, neither of which should be present in ilioinguinal nerve entrapment syndromes. Once clinical suspicion is established, local or paravertebral nerve blocks can be performed for both diagnostic and therapeutic benefit. More importantly, these techniques can aid in the differentiation of ilioinguinal and genitofemoral neuralgias. Then the nerve takes a retroperitoneal course on the ventral surface of the psoas muscle body crossing caudal to the ureter. Distally, the nerve typically divides into two branches above the inguinal ligament. In females, the genital branch runs adjacent to the round ligament through the deep inguinal ring and provides sensory innervation to the mons pubis and labium majoris. In males, this branch is also known as the external spermatic branch; it enters the inguinal canal at the deep inguinal ring and provides sensory innervation to the scrotal skin and motor innervation to the cremaster muscle. In both sexes, the femoral branch, otherwise known as the lumboinguinal branch, takes a course lateral to the external iliac artery to enter the lateral aspect of the femoral sheath. The nerve pierces the fascia lata superiorly in the femoral triangle prior to providing sensory innervation to the upper medial thigh over the area of the femoral triangle. The genitofemoral nerve primarily provides sensory innervation to the genitalia and upper medial thigh as well as motor innervation to the cremaster muscle. It is important to note that considerable variation can occur in the anatomy of the genitofemoral nerve. The nerve exists as a single trunk, arising from L1 and L2 or from L2 and L3, in 80% of cases; in the other 20% of cases, the nerve exists as two separate branches, genital and femoral. The operating table is flexed to increase the interval between the lower costal margin and the iliac crest. A curvilinear incision is made on the transverse flank, extending several centimeters from the lateral aspect of the rectus sheath to the anterior axillary line. Using cautery, the external and then internal oblique muscles are identified and divided. Then the transverse abdominis is divided in line with its fibers, allowing entry into the retroperitoneal space. The retroperitoneal fat and peritoneum are retracted medially, exposing the plane anterior to the quadratus lumborum and the psoas major muscles. The ureter is identified and protected; the genitofemoral nerve is usually seen exiting the psoas muscle along its medial edge. A monopolar nerve stimulator can then be utilized to verify the nerve; contractions of the cremaster muscle can be observed with genitofemoral nerve stimulation. Wound closure proceeds in anatomic layers after ensuring that the peritoneum has not been inadvertently violated. There are no established guidelines for the modality or duration of such conservative measures in the literature. When such measures fail, however, surgical intervention may be indicated, and extraperitoneal neurectomy of the genitofemoral nerve is often the treatment of choice. Goal the goal of extraperitoneal neuroectomy of the genitofemoral nerve is to relieve persistent pain and burning sensation in the genitofemoral nerve region after conservative measures have failed and ilioinguinal neuralgia has been ruled out. Conclusion Genitofemoral neuralgia is a rare condition characterized by pain and paresthesias in the groin region and the anterior superior aspect of the thigh. The syndrome is typically diagnosed clinically, and usually occurs following retroperitoneal inflammatory processes, surgery, or trauma to the lower abdominal quadrants. Selective paraspinal and peripheral nerve blocks are useful as both a diagnostic and therapeutic measure. For refractory cases, the lateral retroperitoneal approach for genitofemoral nerve transection is preferred. Patient is positioned supine or lateral with the hip and thorax of the operative side in the nondependent position. A curvilinear incision is made on the transverse flank extending several centimeters from the lateral aspect of the rectus sheath to the anterior axillary line. The external and internal oblique muscles are divided, followed by the transverse abdominis, which allows entry into the retroperitoneal space. The genitofemoral nerve is identified; it is usually seen exiting the psoas muscle along its medial edge. Once the nerve is identified with monopolar nerve stimulator, it is sectioned proximal to the assumed site of entrapment. Surgical management of 10 genitofemoral neuralgias at the Louisiana State University Health Sciences Center. Clinical Case Meralgia Paresthetica A 60-year-old obese woman with a history of diabetes undergoes an elective lumbar decompression and fusion, with an uneventful intraoperative course. Postoperatively, she has resolution of her preoperative concerns, but notes a burning dysesthesia of the lateral thigh that she has not previously experienced. The neurologic exam is notable for a subjectively diminished sensation over the affected region. Her symptoms are improved after treatment with gabapentin, and resolve completely after 2 months. The nerve courses inferiorly lateral to the psoas muscle before crossing the iliacus muscle deep to the iliac fascia. The bifurcation of the nerve into anterior and posterior branches typically is found ~ 5 cm distal to the inguinal ligament, but early nerve bifurcation is noted in 30% of patients; as many as five branches may be identified. The anterior branch becomes superficial ~ 10 cm beyond the inguinal ligament and provides cutaneous innervation of the anterolateral thigh inferiorly to the knee. Meralgia paresthetica can be caused by entrapment of the nerve along any segment, but the inguinal canal is the most common area of compression. Prone positioning with inadequate padding may result in nerve compression and neuropathy. Local trauma may result in meralgia paresthetica via either direct nerve injury or compression by hematoma. Motor weakness or deep tendon reflex changes are not observed in uncomplicated meralgia paresthetica, and suggests other etiologies such as lumbar radiculopathy or femoral neuropathy. Electrodiagnostic studies are generally normal in mild cases, but sensory nerve conduction studies may demonstrate asymmetry or deviation from established baseline measurements. Williams and Trzil15 reported excellent responses to medical treatment in a study of 277 patients with meralgia paresthetica.
Discount glycomet
The administration of ciprofloxacin results in high biliary concentrations and has broad gram-negative and gram-positive coverage diabetes blindness prevention purchase genuine glycomet on-line. Similar results can be observed with other fluoroquinolones, such as norfloxacin and levofloxacin. Prophylactic therapy with oral fluoroquinolone therapy may reduce the frequency of recurrent cholangitis, although no controlled trial has been performed to support this conclusion. Balloon dilation is most effective in patients with acute elevations of serum total bilirubin level or recent onset of bacterial cholangitis. It appears less effective in patients with long-standing jaundice or a history of recurrent bacterial cholangitis. Although some studies have suggested an increased risk of complications following biliary stenting, this finding has not been consistently observed. Therefore temporary biliary stents should be used for strictures refractory to balloon dilation. For strictures related to cholangiocarcinoma, the use of expandable metal stents can be employed for palliative treatment. Pharmacologic agents such as colchicine, corticosteroids, cyclosporine, azathioprine, methotrexate, and mycophenolate mofetil have demonstrated marginal clinical benefit and significant adverse effects. For example, men are less likely to respond than women (72% versus 80%, respectively). In addition, those who present at an older age (older than 70 years) have a response rate of 90% compared with a response rate of 50% among patients who were diagnosed at a younger age (younger than 30 years). Factors that influence the consideration for liver transplantation are deteriorating hepatic synthetic function, the development of comorbid conditions. However, recurrent cholangitis has not been associated with an increase in wait-list mortality. No significant effect on survival, however, has been associated with recurrent histologic disease. Tacrolimus-based immunosuppression is associated with a shorter time-to-recurrence than cyclosporine-based therapy. A mesenteric defect can be created during the biliary reconstruction which is typically a Roux-en-Y choledochojejunostomy. The epidemiology and natural history of primary biliary cirrhosis: a nationwide population-based study. Population-based epidemiology, malignancy risk and outcome of primary sclerosing cholangitis. Pathogenesis of primary sclerosing cholangitis and advances in diagnosis and management. Long-term effects of mid-dose ursodeoxycholic acid in primary biliary cirrhosis: a meta-analysis of randomized controlled trials. This in turn causes an immunologic response through the generation of memory B cells that produce antibodies, which provide varying protection from the pathogen in the future. Immunizations allow for the controlled exposure to pathogens or proteins that induce these protective antibody responses, and have helped control the spread of infectious diseases significantly since their introduction. Inactivated vaccines, also known as killed vaccines are those in which the pathogen stimulates antibody production by triggering an immunologic response. Attenuated vaccines, also known as live vaccines, are made from pathogens that have been disabled from causing active disease. They are still able to stimulate antibody production resulting in protection from the disease, but in patients with compromised immunity this may theoretically result in infection with the pathogen being introduced in the vaccine. How long after receiving the hepatitis A vaccine does it take before one is considered protected against infection There is some evidence of protection in certain individuals within 2 to 4 weeks, but currently 4 weeks is the timeframe recommended before someone can be considered to be protected from hepatitis A. Protection after vaccination has been estimated to last 25 years in those vaccinated as adults and up to 20 years in those vaccinated as children. It has been found to be as effective as Ig, which was previously the only recommended way to protect individuals exposed to hepatitis A prior to 2007. The most common recommendation is to give a three-dose series of hepatitis B vaccine. Give the second dose 1 month after the first dose, and give the third dose approximately 5 months after the second. If there is an interruption between doses of hepatitis B vaccine, does the vaccine series need to be restarted If the vaccine series was interrupted after the first dose, the second dose should be administered as soon as possible. The second and third doses should be separated by an interval of at least 8 weeks. For a person with a normal immune system who has received previous vaccination, booster doses are not recommended. The liver plays a key role within the innate immune response because it encounters ingested pathogens from the gut via circulation from the portal vein system. Cirrhotic patients have a fibrotic and poorly functioning liver with dysfunction of the reticuloendothelial system (Kupffer cells in the liver, macrophages, and monocytes) as well as granulocytes (neutrophils, eosinophils, and basophils). There have been studies demonstrating increased gut permeability of bacteria and associated toxins in patients with cirrhosis leading to spontaneous infections. There is frequently extensive shunting of venous circulation away from the liver in patients with cirrhosis, thus impairing clearing capacity following infections. What vaccine-preventable bacterial infections pose an increased risk for patients with cirrhosis Why is vaccination against hepatitis A and B strongly recommended in patients with cirrhosis When should vaccinations against hepatitis A and B be given to cirrhotic patients For both hepatitis A and B it is recommended that vaccinations be given early in the disease course. Patients have a better immune response to the vaccines when they are given shortly after developing cirrhosis when compared with those who receive it in the later stages of their disease. The patients should receive the standard two doses of the hepatitis A vaccine and three doses of the hepatitis B vaccine per normal guidelines if in the early stages of chronic liver disease, although patients with more advanced disease. Furthermore, studies have demonstrated increased hepatic decompensation in patients with advanced cirrhosis who develop influenza infections. Patients with cirrhosis should receive the pneumococcus vaccine as close as possible to the time of diagnosis, regardless of age. In addition to individuals older than 65 years, pneumococcal infections are more prevalent in patients with cirrhosis and others with chronic liver disease. In patients with concurrent alcoholism and liver cirrhosis, their risk of death from pneumococcal pneumonia, meningitis, or bacteremia is greatly increased. Patients with cirrhosis should receive the standard immunizations that are applicable to an otherwise healthy population. This includes routine diphtheria and tetanus booster immunizations every 10 years, and other age-appropriate vaccines. In general, killed or nonlive vaccines are preferred to live vaccines, when possible. Infections are the most common serious adverse events associated with these therapies. As soon as the diagnosis is made is the best time to address vaccinations, ideally before starting immunosuppressive medications, which may blunt immune responses to vaccines. Most vaccines can be given at any time, but should be timed ideally before the initiation of immunosuppressive therapy. In general, all killed or nonlive vaccines should be given according to routine guidelines. Special considerations are warranted when the risk of natural infection outweighs the risks of the vaccine. Clinical circumstances in which natural infection risk for varicella and zoster are increased include occupations such as preschool teachers and health care workers. Some considerations are necessary for patients with varicella zoster (chicken pox) and herpes zoster (shingles). Given that the varicella and zoster vaccines are live attenuated virus vaccines (the zoster vaccine is a concentrated form of the varicella vaccine), they are generally considered contraindicated in immunocompromised patients. The same holds true for those on low doses of methotrexate, azathioprine, or 6-mercaptopurine. However, if the recipient of a varicella vaccine develops a rash, they should avoid direct contact with the immunosuppressed individual until the rash resolves. It is recommended that household contacts not receive the live influenza vaccine, because there is a theoretical risk of live virus transmission and a killed (injected) alternative is available. It is a live, attenuated vaccine and serious adverse effects have been noted such as encephalitis and multiorgan system failure. If travel to these areas is absolutely necessary, patients should be counseled on the risks of the disease and prevention of mosquito bites, which is the transmission vector for the disease.
Effective 500 mg glycomet
Initial evaluation should include measurement of serum ceruloplasmin and diabetes symptoms glucose level order glycomet 500 mg with mastercard, if abnormal, a 24-hour urinary copper level. Approximately 85% to 90% of patients have depressed serum ceruloplasmin levels, but a normal level does not rule out the disorder. If the ceruloplasmin is decreased or the 24-hour urinary copper level is elevated, a liver biopsy should be performed for histologic interpretation and quantitative copper determination. Although elevated hepatic copper concentrations can occur in other cholestatic liver diseases, the clinical presentation allows an easy differentiation between Wilson disease and primary biliary cirrhosis, extrahepatic biliary obstruction, and intrahepatic cholestasis of childhood. Because D-penicillamine is frequently associated with side effects, trientine also has been used. Patients who present with complications of chronic liver disease or with fulminant hepatic failure should be quickly considered for orthotopic liver transplantation. Wilson disease is an autosomal recessive disorder, and all first-degree relatives of the patient should be screened. If the ceruloplasmin level is reduced, a 24-hour urinary copper level should be obtained, followed by a liver biopsy for histologic examination and quantitative copper determination. Genetic testing can be valuable for family screening if genotyping has been done on the proband and is available to family members. Both disorders involve abnormal metal metabolism and are inherited as autosomal recessive disorders. The mechanism of tissue damage is probably related to metal-induced oxidant stress for both disorders. In hemochromatosis, the heart, pancreas, joints, skin, and endocrine organs are affected; in Wilson disease, the brain, eyes, red blood cells, kidneys, and bone are affected. Both disorders are fully treatable if diagnosis is made promptly before the development of end-stage complications. The reader is referred to Chapter 32, where histologic examples of most of the inheritable forms of liver disease discussed in this chapter can be reviewed. Diagnosis and management of hemochromatosis: 2011 practice guideline by the American Association for the Study of Liver Diseases. Natural history and life expectancy in severe alpha1-antitrypsin deficiency, Pi Z. Survival and causes of death in cirrhotic and noncirrhotic patients with primary hemochromatosis. The use of trientine in preventing the effects of interrupting penicillamine therapy in Wilson disease. Identification of the Wilson disease gene: clues for disease pathogenesis and the potential for molecular diagnosis. Liver disease in alpha-1 antitrypsin deficiency: current understanding and future therapy. Indications include abnormal liver tests of unknown cause, multiple parenchymal diseases, fever of unknown cause, and focal and diffuse abnormalities on an imaging study indicating conditions such as amyloidosis or granulomatous diseases. For example, liver biopsy is often obtained to ascertain control of inflammation prior to steroid dose reduction or discontinuation of immunosuppression therapy for autoimmune hepatitis. What kind of prebiopsy testing and management of medication are necessary before liver biopsy The adequate portal tract number is more than 11, and the minimal requirement is more than 5 portal tracts. Councilman described acidophil bodies in a yellow fever patient for the first time. Injury of intermediate filaments in hepatocytes creates swelling and increases in volume with wisps of cytoplasmic material. Balloon cell degeneration and feathery degeneration resemble each other, and sometimes they are indistinguishable. What kind of abnormal material can accumulate in cytoplasm of hepatocytes and what is the cause Photomicrography of accumulation of abnormal material in cytoplasm of hepatocytes. What kinds of inflammatory cells can be seen in liver biopsy, and what kinds of etiologic factors are suspected The multinucleated cell with molding viral inclusions in the background of hepatocyte necrosis. Fresh tissue is required, and it is useful for the diagnosis of acute fatty liver of pregnancy. Steatohepatitis refers to a histologic constellation of findings with evidence of additional modes of hepatocyte injury such as ballooning degeneration, Mallory-Denk bodies, or necroinflammation. Grade is based on degree of steatosis, hepatocellular ballooning, and lobular inflammation. Chronic hepatitis is a necroinflammatory process in which hepatocytes rather than bile ducts are predominantly injured. Viral hepatitis, autoimmune hepatitis, Wilson disease, and 1-antitrypsin disease show the chronic hepatitis pattern. Variants include cases without plasma cell dominance, acute hepatitis, and unexpected cirrhosis. The lobular activity is mild and consists of spotty necrosis with 1 to 2 mononuclear cells and acidophil bodies. Chronic hepatitis B may show ground-glass hepatocytes, which reflects accumulation of hepatitis B antigen within the endoplasmic reticulum of the hepatocytes. What is the goal for grading and staging systems for chronic hepatitis and what kinds of systems are there The goal is to ensure the same lesions are being evaluated and given similar diagnostic weight regardless of the observers. The biopsy shows centrilobular cholestasis, proliferation of bile ducts associated with neutrophil infiltrate, and portal tract edema. Neutrophils around the bile ducts are related to interleukin-8 expressed by ductular cells, not to infection. It is characterized by biliary epithelial damage, basement membrane destruction, and lymphoplasmacytic infiltrate. Onion skin fibrosis accompanied by reduced number of bile ducts is diagnostic; however, it may be present in fewer than 40% of the liver biopsies. The most common findings on biopsy are nonspecific fibrosis with inflammation of portal tracts and paucity of normal bile ducts or the same histologic finding of extrahepatic bile duct obstruction. The clinical and histologic features of more than one autoimmune process are seen in a patient. Accumulation of iron in hepatocytes indicates genetic hemochromatosis, alcoholic liver disease, and porphyria cutanea tarda. Accumulation of iron in Kupffer cells indicates multiple transfusions or hemolytic anemia. The biopsy shows variable portal inflammation, steatosis, periportal glycogenated nuclei, moderate to marked copper storage, and the presence of Mallory-Denk bodies in periportal liver cells. The patients with nodular regenerative hyperplasia, idiopathic portal hypertension, and hepatoportal sclerosis have portal hypertension without cirrhosis. When the imaging studies are inconclusive, liver biopsy is required to confirm the diagnosis. Some biopsies show a tumor that is probably metastatic but for which no primary tumor is known. In such cases, various immunohistochemical stains can be performed on biopsy tissue to help guide further workup. What are the main histologic features of acute rejection and how are they graded by the Banff scheme Portal inflammation, endotheliitis, and bile duct injury are the three main histologic features. The first is a global assessment of the overall rejection grade (indeterminate, mild, moderate, severe). The second component involves scoring the three main features of acute allograft rejection on a scale of 0 (absent), 1 (mild), 2 (moderate), 3 (severe) to produce an overall rejection activity index. Chronic rejection often occurs as a consequence of repeated episodes of acute rejection that are unresponsive to immunosuppression. The main histologic abnormality is loss of small bile ducts or obliterative vasculopathy affecting large and medium arteries. The former can be diagnosed by biopsy, whereas the latter may require the examination of an explant. Ductpenia is characterized by bile duct loss in more than 50% of portal tracts and is diagnosed through a single biopsy or a series of biopsies. Grading and staging the histopathological lesions of chronic hepatitis: the Knodell histology activity index and beyond. Banff schema for grading living allograft rejection: an international consensus document. Update of the international Banff scheme for liver allograft rejection: working recommendations for the histopathologic staging and reporting of chronic rejection: an international panel.
Generic 500 mg glycomet otc
Because prostate cancer is the most common of these cancers diabetes and alcohol consumption buy glycomet 500 mg visa, most data has been obtained in this group of patients. The peristaltic movement of the small intestine in and out of the field of radiation decreases the degree of injury to the small bowel. The colon, especially the rectosigmoid, is highly susceptible to radiation injury because it is immobile. Brachytherapy, or internal radiotherapy, can deliver high-energy radiation to more focused tissues and therefore causes less damage to the colon than external-beam radiation. Tumors in the pelvic area often require higher dosages of radiation and result in greater risk of damage to the colon. The extent of radiation colitis depends on the cumulative radiation dose, fraction size, technique of radiation delivery, amount of tissue exposed, and presence of other treatments such as surgery or chemotherapy. Radiation damage can be reduced by limiting the dosage and area of exposure while shielding adjacent tissues. Additionally, amifostine has been shown to reduce the incidence of radiation colitis by scavenging free radicals produced during treatment. Acute radiation injury to the colon typically occurs within 6 weeks and is manifested by diarrhea, mucus discharge, tenesmus, and rarely, bleeding. These symptoms are self-limited and typically resolve in 2 to 6 months without therapy. Chronic symptoms of radiation colitis and proctitis (or chronic radiation proctopathy) can occur 9 to 12 months following radiation therapy, but can be delayed by decades after the initial radiation exposure. The primary symptoms associated with chronic injury to the colon and rectum include diarrhea, obstructed defecation, rectal pain, and rectal bleeding. Severe radiation colitis may manifest with bowel necrosis, perforation, fistula development, and uncontrolled rectal bleeding. Colonoscopy may be normal or may show telangiectasias, pallor, and friable mucosa. Early or acute changes include microscopic damage to mucosal and vascular epithelial cells, which may be asymptomatic to the patient. Late changes commonly involve fibrosis with obliterative endarteritis resulting in chronic ischemia, stricture formation, and bleeding. There is limited data on the appropriate treatment for radiation colitis and proctitis. Medications used to treat radiation colitis and proctitis include oral and rectal sucralfate, steroids, 5-acetylsalicylic acid compounds, hyperbaric oxygen, and antibiotics, such as metronidazole. Stool softeners are also recommended, as straining can cause telangiectasias to bleed. The primary goal of endoscopic therapy is to treat telangiectasias, which are the most common source of rectal bleeding. Colorectal surgeons may apply formaldehyde, also known as chemical cautery, to control bleeding. Patients with long or angulated strictures may benefit from surgery as these lesions are more likely to perforate with dilating procedures. Long-term follow-up of colonoscopic fecal microbiota transplant for recurrent Clostridium difficile infection. Decreased diversity of the fecal Microbiome in recurrent Clostridium difficileassociated diarrhea. Microscopic colitis: A common and an easily overlooked cause of chronic diarrhoea. Clostridium difficile: emergence of hypervirulence and fluoroquinolone resistance. Clostridium difficile-associated disease: new challenges from an established pathogen. Probiotics, antibiotic-associated diarrhoea and Clostridium difficile diarrhoea in humans. Other less common sources include esophagitis, angiodysplasia, Mallory-Weiss tears, cancer, gastric varices, portal hypertensive gastropathy, Dieulafoy lesions, and aortoenteric fistulas. The acute loss of 500 mL of blood will not result in detectable physiologic changes. Mild to moderate blood loss (500-1000 mL) results in resting tachycardia, whereas loss of 1000 mL will produce orthostatic changes. A fall in hematocrit is seen over time with fluid resuscitation or replacement of volume with extravascular fluid. Patients with active bleeding or hemodynamic instability should receive volume replacement, initially with crystalloid, to stabilize blood pressure and heart rate. Laboratories including a complete blood count, creatinine and blood urea nitrogen, prothrombin time, and partial thromboplastin time should be obtained. Patients with active bleeding should be typed and cross-matched for packed red blood cell transfusion. Clotting abnormalities and anemia need correcting in certain patients (see Question 8). However, a restrictive transfusion strategy (when hemoglobin <7 g/dL) compared with a liberal transfusion strategy (when hemoglobin <9 g/dL) has been recently found to improve rebleeding and mortality rates in patients with peptic ulcer bleeding or variceal bleeding with Child-Pugh A or B cirrhosis who underwent emergent upper endoscopy with endoscopic treatment. However, patients with brisk bleeding resulting in shock and patients with significant comorbid illness, particularly cardiovascular, cerebrovascular, or peripheral vascular disease, should be transfused more aggressively (goal hemoglobin 9 g/dL). However, guidelines recommend that endoscopy should not be delayed for correction of coagulopathy. A number of scoring systems have been developed to predict the likelihood of adverse outcomes and need for intervention. These scores can be used to triage patients to appropriate levels of care, including urgent endoscopy and early discharge. In general, the higher the number of risk factors, the higher the risk of adverse outcome. A Blatchford score of zero was associated with a low likelihood of the need for urgent endoscopic intervention. The complete Rockall score includes the clinical Rockall score plus endoscopic score. Patient with a clinical Rockall score of 0 or a complete Rockall score or less than or equal to 2 are considered low risk for rebleeding or death. As the number of risk factors accumulate, length of hospital stay, cost, and mortality increases. After initial stabilization and resuscitation is performed (see Questions 7 and 8), intubation and deep sedation should be considered in patients with altered mental status, copious hematemesis, suspicion for variceal bleeding, or alcohol dependence. Endoscopy should be performed within 24 hours of admission, after hemodynamic stabilization and resuscitation. Stigmata of recent hemorrhage describe the appearance of an ulcer at the time of endoscopy. The most commonly used classification system for peptic ulcers is the Forrest classification, which classifies endoscopic stigmata according to the risk of rebleeding and mortality (Table 50-5). Epinephrine therapy is not effective as monotherapy but can be a helpful adjuvant in combination with other modalities. In general, the choice of therapy depends on the type and location of the lesion and the expertise of the endoscopist. If a variceal etiologic factor is suspected, octreotide bolus (50 mcg) with subsequent infusion (50 mcg/h) should be initiated to decrease portal pressures and ongoing bleeding. Patients with cirrhosis are more likely to require correction of coagulopathy and thrombocytopenia, and may develop hepatic encephalopathy, which can be treated with lactulose or rifaximin. Cyanoacrylate glue injection is an alternative endoscopic technique for gastric varices. In patients with recurrent bleeding after endoscopic therapy, approximately 70% will be controlled after a second attempt at endoscopic therapy. Angiography or surgery is recommended in patients who continue to bleed despite two attempts at endoscopic hemostasis.
Liveforever (Houseleek). Glycomet.
- Severe diarrhea; ulcers in the mouth; burns; skin ulcers; warts; itchy, burning skin; and swelling from insect bites.
- Dosing considerations for Houseleek.
- How does Houseleek work?
- What is Houseleek?
- Are there safety concerns?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96518
Glycomet 500 mg without a prescription
Initial evaluation of the efficacy and safety of endoscopic ultrasound-guided direct Ganglia neurolysis and block diabetes type 2 urine buy glycomet with visa. Endoscopic ultrasound of the upper gastrointestinal tract and mediastinum: diagnosis and therapy. Peak incidence is between 20 and 50 years of age, and it typically has an insidious onset. Pseudoachalasia, or secondary achalasia, is an esophageal motility disorder caused by a distal esophageal obstruction from an infiltrating tumor that may directly intrinsically or extrinsically compress the esophagus Patients exhibit symptoms typical of achalasia, including dysphagia, regurgitation, chest pain, and weight loss. Conventional manometry, endoscopy, and radiologic examination cannot distinguish pseudoachalasia from achalasia. Endoscopy helps rule out the possibility of pseudoachalasia but cannot diagnose a mural or extramural tumor. When this is suspected, based on a history of substantial weight loss (more than 20 lb in 6 months), endoscopic ultrasonography or computed tomography is recommended. The main distinguishing feature is the complete reversal of pathologic motor phenomena following successful therapy of the underlying disorder. Vigorous achalasia is a variant of achalasia in which the esophageal body responds to a swallow with normal or less often high-amplitude contractions that may be multiphasic, but as with classic achalasia, there are no progressive peristaltic waves. Patients with vigorous achalasia are usually younger and have chest pain as a prominent symptom. Most investigators believe that vigorous achalasia is an early form of the disease that presents in some patients. Most myotomies were performed through the chest before the advent of minimally invasive surgery. The transabdominal laparoscopic approach is currently the procedure of choice with good long-term results in 84% to 94% of patients. Five trocars are placed in the upper abdomen in an arrangement similar to that of a laparoscopic antireflux operation. Intraoperative manometry is then used to confirm successful ablation of the pathologic high-pressure zone. A partial fundoplication is performed after the completion of the myotomy around a 52-Fr bougie. There is a general consensus that a complete 360-degree wrap may cause significant obstruction at the distal end of the esophagus and lead to worsening of esophageal function in patients with already impaired peristalsis. The Toupet fundoplication (partial posterior wrap) and Dor fundoplication (partial anterior wrap) are equally popular among surgeons. A randomized trial compared Heller myotomy and Dor fundoplication with Heller myotomy and Nissen fundoplication; the recurrence rate in the Nissen group was significantly higher than the Dor group (15% vs. Patients with mild to moderate reflux after addition of a potential fundoplication can be easily managed medically. How do long-term results of Heller myotomy compare with mechanical esophageal dilatation On the basis of excellent results with laparoscopic Heller myotomy, it is largely considered the optimal treatment for severe symptoms of achalasia. Several large retrospective series have compared the two treatments and favor operative myotomy over pneumatic dilatation. With the introduction of the minimally invasive approach, the historical concerns about the morbidity associated with open surgical techniques have essentially disappeared and the morbidity and mortality of both surgical and nonsurgical options are now nearly identical. The long-term success and safety of laparoscopic myotomy have completed the shift in favor of surgery as the primary therapeutic option for patients with achalasia. However, a recent randomized controlled trial that compared laparoscopic Heller myotomy (with Dor fundoplication added) with pneumatic dilatation revealed that the two techniques are equally effective in a 2-year follow up. The most common complication of a surgical myotomy is esophageal perforation, which is reported in 0% to 4. Previous pneumatic dilatation and botulinum toxin injection increase the technical difficulty in performing a myotomy and may increase the rate of perforation. An unrecognized esophageal perforation may present as persistent fever, tachycardia, or left-sided pleural effusion. These patients require close observation and may need reoperation if conservative measures fail. Early postoperative dysphagia results usually from an incomplete myotomy, whereas causes of late dysphagia also include healing of the myotomy or, more rarely, a reflux-induced peptic stricture. However, in patients in whom the first myotomy was complete, a second myotomy is less likely to be successful and such patients may require esophageal resection. In summary, the treatment options for achalasia are initially medical (nitrates, calcium channel blockers), botulinum toxin injection, and pneumatic dilation. Surgical treatment (laparoscopic Heller myotomy, with Dor fundoplication) is reserved for patients with severe symptoms. Patients who are unwilling to undergo any procedure should be treated with medications. Botulinum toxin injection should be reserved for patients who are unable to tolerate surgery because of significant comorbidities, or patients whose clinical presentation is complicated, putting the diagnosis of achalasia in doubt. Overall, younger patients may choose early surgical intervention to avoid the need for multiple pneumatic dilatations. Peroral endoscopic myotomy has also been gaining popularity as a means of treating achalasia. Patients with achalasia are thought to be at increased risk for the development of squamous cell carcinoma, with risk as high as 140-fold reported. Tumors develop at an age 10 years younger than in the general population and carry a worse prognosis because of late diagnosis. The effect of surgical treatment on the incidence of cancer is not known and surveillance endoscopy is recommended every 2 years. Cancer of the esophagus accounts for 1% of all newly diagnosed cancers in the United States, and the incidence has continued to rise in the last 30 years. An estimated 13,000 new cases of carcinomas of the esophagus were diagnosed in men and 3500 new cases in women in 2009. It is seven times more common in men than women and is the seventh leading cause of death from cancer among men. Whereas squamous cell carcinoma accounted for most cancers of the esophagus 40 years ago, adenocarcinoma now represents more than 70% of such tumors in the United States. This is primarily caused by the striking increase in incidence of adenocarcinoma among white men older than 60 years. Risk factors for squamous cell carcinoma include tobacco use and excessive alcohol consumption, which appear to have a synergistic effect in its pathogenesis. Risk factors for the development of distal esophageal adenocarcinoma are less clear. It is also important that two different pathologists review the slides to increase the yield of the histologic diagnosis per the American Gastroenterological Association 2011 guidelines. That can be accomplished by either medical or surgical management, with the latter shown to be more effective. In addition, the likelihood of developing cancer in the first 3 to 5 years once severe dysplasia has been identified is 25% to 50%. The short gastric and left gastric arteries are ligated, whereas the right gastric artery and right gastroepiploic arcade are carefully preserved to allow a well vascularized gastric conduit to reach to the neck. The main advantage of this approach is avoidance of a thoracic anastomosis because a cervical leak carries much less morbidity than for a thoracic leak. En bloc resection is performed from the hiatus to the apex of the chest just above the azygos vein. Regardless of the incision approach, the same operative procedure is performed, that is, esophagogastrectomy with regional lymph node resection. When is neoadjuvant therapy appropriate in the treatment of patients with esophageal carcinoma There are different modalities of neoadjuvant therapy for esophageal cancer treatment, including either radiation alone (dose used 50 Gy), chemotherapy alone (chemotherapeutic agents used are cisplatin, 5-fluorouracil, carboplatin, paclitaxel, etoposide, or epirubicin), or chemoradiation prior to surgery. Preoperative radiation alone was found to have no significant benefit compared with surgery alone. Clinical trials have shown that neoadjuvant chemoradiation or chemoradiation were found to have statistically significant benefits for survival compared with surgery alone. Chemotherapy versus chemoradiation have been compared in clinical trials but no statistical difference was shown. Potential advantages of neoadjuvant therapy include cancer down-staging, increased resectability, and reduction in micrometastasis. In addition, the chemotherapeutic agents used all possess radiosensitizing properties. However, more studies are needed to verify the effectiveness of this treatment strategy.
Buy cheap glycomet 500 mg
For patients with chronic liver disease blood glucose test strips optium xceed glycomet 500 mg on-line, when is the appropriate time to refer for liver transplantation The decision to list a patient for transplantation ultimately rests on the judgment and experience of the physicians at the transplant center. Coexistent medical disorders such as coronary artery disease, chronic obstructive lung disease, cardiomyopathy, or pulmonary hypertension may jeopardize successful liver transplantation, especially in older adults. Consequently, patients with comorbid conditions need to be evaluated to determine their candidacy for transplantation. There is no advantage gained by early listing of patients for liver transplantation, because waiting time no longer determines priority for transplantation. Liver transplant recipients fulfilling the Milan criteria have the same 3- to 4-year actuarial survival as patients without malignancy, with a 4-year survival rate of 85%: A. No radiographic evidence of extrahepatic disease Patients who fulfill the Milan criteria are awarded a high priority for transplant with 22 points. In contrast, liver transplants are performed less frequently for chronic hepatitis B, likely as a result of more effective antiviral therapy. Approximately 10% of patients listed for liver transplantation in the United States die each year awaiting a suitable donor organ. In addition, an equal number are removed from the list as "too sick to transplant. Patients typically present with progressive lethargy and jaundice over several days. The most common causes of acute liver failure in the United States, in descending order, are acetaminophen (46%), indeterminate (14%), drug-induced (11%), hepatitis B (6%), autoimmune hepatitis (6%), ischemia (4%), hepatitis A (3%), and other (9%). Acute ingestion of acetaminophen may cause severe hepatic injury via the toxic metabolite, N-acetyl-p-benzoquinone imine, a metabolite of the cytochrome P450 system. Chronic alcohol ingestion may result in induction of the cytochrome P450 system and a reduction in the amount of acetaminophen required to cause hepatotoxicity. Without treatment, an acetaminophen level of more than 300 mcg/mL at 4 hours or more than 45 mcg/mL at 15 hours is associated with a 90% risk of hepatotoxicity. If patients present within 4 hours of ingestion, activated charcoal can reduce acetaminophen absorption. Therefore some centers will not consider such coinfected patients for liver transplantation. Careful recipient and donor selection are important in optimizing outcomes in this population. In most cases, cholangiocarcinoma remains a relative contraindication for liver transplantation; however, some transplant centers have reported acceptable outcomes in selected individuals. Liver transplants are more commonly performed in unresectable cases of early stage perihilar cholangiocarcinoma (tumor size <3 cm, no metastases) in which protocols involving neoadjuvant chemotherapy followed by liver transplantation are associated with recurrence-free survival rates of 68%. In cases of intrahepatic cholangiocarcinoma, liver transplantation is generally not performed because of very high recurrence rates. The decision to perform a liver transplant in a specific patient is based on the judgment and experience of the physicians at the transplant center. Providing a kidney transplant in selected liver transplant recipients can have a major effect on posttransplant survival and quality of life. Recognition of alcoholism by the patient and family members is especially important, and patients demonstrate this through adherence to an alcohol rehabilitation program. Features associated with a low rate of recidivism include absence of comorbid substance abuse, good social function, and absence of family history of alcohol abuse. Which factors measured in the recipient prior to transplant correlate with reduced postoperative survival Pretransplant recipient characteristics associated with an increased risk of liver-related death beyond 1 year after transplant include requirement for retransplantation, renal insufficiency, and diabetes. Current immunosuppressive therapy usually involves two or three agents to prevent allograft rejection in the immediate postoperative period. Corticosteroids are used as first-line therapy in immunosuppression at many centers. However, there is increasing evidence that long-term maintenance corticosteroids may not be necessary to prevent rejection. Therefore most liver transplant recipients are weaned completely off of corticosteroids within a few months after surgery. As a result, posttransplant immunosuppressive regimens are configured to minimize nephrotoxicity. Many centers have introduced the use of rabbit antithymocyte globulin as induction therapy. A liver transplant patient has just sustained a grand mal seizure 36 hours posttransplant. The neurologic side effects are usually reversible with a reduction in dosage or discontinuation of the drug. Medications that induce P450-3A4 lower levels and increase the risk of rejection or require higher doses of the immunosuppressant. What are the histologic findings of acute rejection versus posttransplant hepatitis C on liver biopsy The differentiation between recurrent hepatitis C and acute cellular rejection is one of the most problematic areas in clinical transplantation. In many cases, the histologic findings on the liver biopsy are inconclusive in differentiating these two disorders. The histologic findings may demonstrate a predominant lymphocytic infiltrate in the portal areas rather than the mixed cellular infiltrate of rejection. In contrast, bile duct inflammation and venous endothelial inflammation are more prominent features in rejection. Describe the other posttransplant complications manifested by elevated liver enzymes. The clinical presentation may be variable, but is usually associated with elevated aminotransferases. Cessation of hepatic artery blood flow preferentially causes ischemic damage to the biliary tree, resulting in breakdown of the biliary tree and development of bilomas, bile leaks, and eventually strictures. In hepatic artery thrombosis, retransplantation is usually required for successful long-term outcomes. In the early posttransplant period, portal vein thrombosis may present with signs of graft dysfunction and require immediate revascularization or retransplantation. Late thrombosis may be well tolerated or lead to graft dysfunction or portal hypertension. Balloon angioplasty, stent placement, and thrombolytic infusion have been used to reestablish the portal circulation. Biliary leaks or strictures may be asymptomatic but can also lead to jaundice, bacteremia, or sepsis. Biliary leaks can occur at the biliary anastomosis and within the liver as a result of bile duct destruction. A hepatocellular pattern may occur with azathioprine, nonsteroidal antiinflammatory drugs, and some antibiotics. Tissue invasive disease may cause life-threatening complications when the liver, lungs, or gastrointestinal tract are involved. Chronic allograft rejection is generally characterized by an insidious but progressive rise in alkaline phosphatase and bilirubin. Patients are usually asymptomatic and synthetic function remains intact until the late stages. The pathogenesis of this syndrome remains unclear, but the evidence favors loss of bile ducts and the development of obliterative arteriopathy in the small hepatic arteries. Histologic findings include a normal-appearing parenchyma with few mononuclear infiltrates in the portal areas but absence of bile ducts in almost all of the portal triads. Later in the course, patients develop strictures and dilations in the larger bile ducts resembling primary sclerosing cholangitis. In these cases, the clinical course may be complicated by recurrent attacks of biliary sepsis. Chronic rejection is very uncommon and usually occurs in liver transplant recipients who are noncompliant with their immunosuppressive therapy. The process frequently progresses to graft failure, but recent reports indicate that 20 to 30 percent of patients may respond to additional immunosuppressive therapy. Patients with progressive liver failure caused by chronic rejection may require evaluation for retransplantation.
Cheapest glycomet
Areas of thin intervening epidermis are generally evident between areas of massively hypertrophic adnexal epithelium diabetes prevention health promotion discount glycomet 500 mg online. Ultrastructurally, this zone is composed of four components: the plasma membranes of the basal cells with the specialized attachment plates (hemidesmosomes); an electron-lucent zone called the lamina lucida; the lamina densa (basal lamina); and the fibrous components associated with the basal lamina, including anchoring fibrils, dermal microfibrils, and collagen fibers. Staining in the lower, transient portion of the hair follicle, however, is different. The lack of hemidesmosomes in the deep portions of the follicle may relate to the transient nature of the inferior segment, whereas abundant hemidesmosomes stabilize the upper portion of the follicle. It further serves as a structural support for the epidermis and holds the epidermis and dermis together. The acrosyringium is composed of small polygonal cells with a central round nucleus surrounded by ample pink cytoplasm. In the stratum corneum overlying an actinic keratosis, the lamellar spiral acrosyringeal keratin often stands out prominently against the compact red parakeratotic keratin produced by the actinic keratosis. The straight dermal portion of the duct is composed of a double layer of cuboidal epithelial cells and is lined by an eosinophilic cuticle on its luminal side. The coiled secretory acinar portion of the eccrine sweat gland may be found within the superficial panniculus. In areas of skin such as the back that possess a thick dermis, the eccrine coil is found in the deep dermis, surrounded by an extension of fat from the underlying panniculus. An inner layer of epithelial cells, the secretory portion of the gland, is surrounded by a layer of flattened myoepithelial cells. The secretory cells are of two types: large, pale, glycogen-rich cells and smaller, darker-staining cells. The darker cells may function similar to cells of the dermal duct, which actively reabsorb sodium, thereby modifying sweat from a basically isotonic to a hypotonic solution by the time it reaches the skin surface. Sweat is similar in composition to plasma, containing the same electrolytes, but in a more dilute concentration. Physical conditioning in a hot environment results in production of larger amounts of extremely hypotonic sweat in response to a thermal stimulus. Physiologic secretion of sweat occurs as a result of many factors and is mediated by cholinergic innervation. Heat is a prime stimulus to increased sweating, but other physiologic stimuli, including emotional stress, are important as well. During early development, there is a switch between adrenergic and cholinergic innervation of sweat glands. Cholinergic sweating involves a biphasic response, with initial hyperpolarization and secondary depolarization mediated by the activation of calcium and chloride ion conductance. Vasoactive intestinal polypeptide may also play a role in stimulating eccrine secretion. Hairfollicles During embryogenesis, mesenchymal cells in the fetal dermis collect immediately below the basal layer of the epidermis. The developing follicle forms at an angle to the skin surface and continues its downward growth. At this base, the column of cells widens, forming the bulb, and surrounds small collections of mesenchymal cells. These papillary mesenchymal bodies contain mesenchymal stem cells with broad functionality. At least in mice, they demonstrate extramedullary hematopoietic stem cell activity, representing a potential therapeutic source of hematopoietic stem cells and a possible source of extramedullary hematopoiesis in vivo. Along one side of the fetal follicle, two buds are formed; an upper bud develops into the sebaceous gland, and a lower bud becomes the attachment for the arrector pili muscle. A third epithelial bud develops from the opposite side of the follicle above the level of the sebaceous gland anlage and gives rise to the apocrine gland. The uppermost portion of the follicle, which extends from its surface opening to the entrance of the sebaceous duct, is called the infundibular segment. It resembles the surface epidermis, and its keratinocytes may be of epidermal origin. The portion of the follicle between the sebaceous duct and the insertion of the arrector pili muscle is the isthmus. The inferior portion includes the lowermost part of the follicle and the hair bulb. Throughout life, the inferior portion undergoes cycles of involution and regeneration. Primary follicles are surrounded by the appearance of two secondary follicles; other secondary follicles subsequently develop around the principal units. The density of pilosebaceous units decreases throughout life, possibly because of dropout of the secondary follicles. In mouse models, signaling by molecules designated as ectodysplasin A and noggin is essential for the development of primary hair follicles and induction of secondary follicles. Arrector pili muscles contained within the follicular unit interconnect at the level of the isthmus. The actual hair shaft, as well as an inner and an outer root sheath, is produced by the matrix portion of the hair bulb. The hair shaft and inner root sheath move together as the hair grows upward until the fully keratinized, inner root sheath sheds at the level of the isthmus. The epidermis of the upper part of the follicular canal is contiguous with the outer root sheath. The upper two portions of the follicle (infundibulum and isthmus) are permanent; the inferior segment is completely replaced with each new cycle of hair growth. Most sites on the body have a much shorter anagen and much longer telogen, resulting in short hairs that Apocrineunits Apocrine units develop as outgrowths not of the surface epidermis, but of the infundibular or upper portion of the hair follicle. Although immature apocrine units are found covering the entire skin surface of the human fetus, these regress and are absent by the time the fetus reaches term. The straight excretory portion of the duct, which opens into the infundibular portion of the hair follicle, is composed of a double layer of cuboidal epithelial cells. The coiled secretory gland is located at the junction of the dermis and subcutaneous fat. It is lined by a single layer of cells, which vary in appearance from columnar to cuboidal. Apocrine coils appear more widely dilated than eccrine coils, and apocrine sweat stains more deeply red in H&E sections, contrasting with the pale pink of eccrine sweat. The apices of the columnar cells project into the lumen of the gland and in histologic cross section appear as if they are being extruded (decapitation secretion). Controversy surrounds the mode of secretion in apocrine secretory cells, whether merocrine, apocrine, holocrine, or all three. Protein, carbohydrate, ammonia, lipid, and iron are all found in apocrine secretion. It appears milky white, although lipofuscin pigment may rarely produce dark shades of brown and gray-blue (apocrine chromhidrosis). Apocrine sweat is odorless until it reaches the skin surface, where it is altered by bacteria, which makes it odoriferous. Apocrine secretion is mediated by adrenergic innervation and by circulating catecholamines of adrenomedullary origin. Vasoactive intestinal polypeptide may also play a role in stimulating apocrine secretion. Apocrine excretion is episodic, although the actual secretion of the gland is continuous. In other species, it has a protective as well as a sexual function, and in some species, it is important in thermoregulation as well. Outer root sheath Inner root sheath Hair shaft Hair cuticle Cortex Medulla Bulb with matrix cells Dermal papilla Crosssection 6 stay in place for long periods without growing longer. Most commonly, telogen effluvium is the result of early release from anagen, such as that induced by a febrile illness, surgery, or weight loss. Pregnancy is typically accompanied by retention of an increased number of scalp hairs in anagen, as well as a prolongation of telogen. Soon after delivery, telogen loss can be detected as abnormally prolonged telogen hairs are released.
Order glycomet 500 mg on-line
Other Toxicodendron-related dermatitides Lacquer dermatitis is caused by a furniture lacquer made from the Japanese lacquer tree diabetes symptoms blood in urine buy generic glycomet line, used on furniture, jewelry, or brica-brac. Antique lacquer is harmless, but lacquer less than 1 or 2 years old is highly antigenic. Cashew nutshell oil is extracted from the nutshells of the cashew tree (Anacardium occidentale). The liquid has many commercial applications, such as the manufacture of brake linings, varnish, synthetic glue, paint, and sealer for concrete. Many persons who have been so exposed, however, whether or not they had dermatitis from it, are sensitized by one or a few episodes of contact with the peel of the mango fruit. The palms carry the allergen, so the eyelids and the male prepuce are often early sites of involvement. Ginkgo tree dermatitis simulates Toxicodendron dermatitis with its severe vesiculation, erythematous papules, and edema. The causative substances are ginkgolic acids from the fruit pulp of the ginkgo tree. Ginkgo biloba given orally for cerebral disturbances is made from a leaf extract so it does not elicit a systemic contact allergy when ingested. A severe inflammatory reaction with bulla formation may be caused by the prairie crocus (Anemone patens L. Several species of ornamental "bottle brush" from Queensland (Grevillea banksii, G. Contact dermatitis may be caused by handling many other flowers, such as the geranium, scorpion flower (Phacelia crenulata or P. The poinsettia and oleander almost never cause dermatitis, despite their reputation for it, although they are toxic if ingested. Treatment of all these plant dermatitides is the same as that recommended for toxicodendron dermatitis. Parthenium hysterophorus, a photosensitizing weed, was accidentally introduced into India in 1956 and has spread over most of the country; it is also spreading in Australia, parts of Africa, China, and Argentina. The well-deserved reputation for harmfulness of dieffenbachia, a common, glossy-leafed house plant, rests on the high content of calcium oxalate crystals in its sap, which burn the mouth and throat severely if any part of the plant is chewed or swallowed. Severe edema of the oral tissues may result in complete loss of voice, thus its common nickname, "dumb cane. The castor bean, the seed of Ricinus communis, contains ricin, a poisonous substance (phytotoxin). Its sap contains an antigen that may cause anaphylactic hypersensitivity and also dermatitis. Flowers and houseplants Among the more common houseplants, the velvety-leafed philodendron, Philodendron crystallinum (and its several variants), known in India as the "money plant," is a frequent cause of contact dermatitis. The eruption is often seen on the face, especially the eyelids, carried there by hands that have watered or cared for the plant. English ivy follows philodendron in frequency of cases of occult contact dermatitis. Primrose dermatitis affects the fingers, eyelids, and neck with a punctate or diffuse erythema and edema. Primin, a quinone, is the causative oleoresin abounding in the glandular hairs of the plant Primula obconica. The popular cut flower, the Peruvian lily, is the most common cause of allergic contact dermatitis in florists. When handling flowers of the genus Alstroemeria, the florist uses the thumb and second and third digits of the dominant hand. Because it is chronic, fissured hyperkeratotic dermatitis results, identical to the "tulip fingers" seen among sensitized tulip workers. Chrysanthemums frequently cause dermatitis, with the hands and eyelids of florists most often affected. The -methylene portion of the sesquiterpene lactone molecule is Fruit and vegetables Many vegetables may cause contact dermatitis, including asparagus, carrot, celery, cow-parsnip, cucumber, garlic, Indian bean, mushroom, onion, parsley, tomato, and turnip. Onion and celery, among other vegetables, have been incriminated in the production of contact urticaria and even anaphylaxis. Several plants, including celery, fig, lime, and parsley, can cause a phototoxic dermatitis because of the presence of psoralens. Trees Trees with timber and sawdust that may produce contact dermatitis include ash, birch, cedar, cocobolo, elm, Kentucky coffee tree, koa, mahogany, mango, maple, mesquite, milo, myrtle, pine, and teak. Melaleuca oil (tea tree oil), which may be applied to the skin to treat a variety of maladies, can cause allergic contact dermatitis, primarily through the allergen D-limonene. The exotic woods, especially cocobolo and rosewood, and tea tree oil are prominent among allergens that may produce erythema multiforme after cutaneous exposure. Toxicodendron, various medicaments, and a variety of other allergens may induce this reaction. Plant-associated dermatitis Phototoxic contact dermatitis from plants is discussed in Chapter 3. Randox (2-chloro-N,N-diallyl-acetamide) has been reported as the cause of hemorrhagic bullae on the feet of farmers. Lawn care companies spray herbicides and fungicides throughout the spring, summer, and fall. Dryene, thiuram, carbamates, and chlorothalonil are potential sensitizers in these workers, whose clothing frequently becomes wetted while spraying. Barbs, bristles, spines, thorns, spicules, and cactus needles are some of the mechanical accessories of plants that may produce dermatitis. It also occurs in persons handling Indian figs in Israel, where the condition is seen from July to November. Agave americana is a low-growing plant used for ornamental purposes in many southwestern U. Trimming during landscaping can induce an irritant dermatitis caused by calcium oxalate crystals. The stinging nettle is a common weed that bears tiny spines with biologically active substances such as histamine that produce itching and urticaria within minutes of contact. Tree-associated plants Foresters and lumber workers can be exposed to allergenic plants other than trees. Foresters and wood choppers exposed to these lichens growing on trees may develop severe allergic contact dermatitis. Exposure to the lichens may also occur from firewood, funeral wreaths, and also fragrances added to aftershave lotions (oak moss and tree moss). Sensitization is produced by D-usnic acid and other lichen acids contained in lichens. The leafy liverwort (Frullania nisquallensis), a forest epiphyte growing on tree trunks, has produced allergic dermatitis in forest workers. The protein fraction causes the respiratory symptoms of asthma and hay fever, and the oil-soluble portion causes contact dermatitis. Ragweed oil dermatitis is a seasonal disturbance seen mainly during the ragweed growing season from spring to fall. Contact with the plant or with wind-blown fragments of the dried plant produces the typical dermatitis. The oil causes swelling and redness of the lids and entire face, and a red blotchy eruption on the forearms that, after several attacks, may become generalized, with lichenification. It closely resembles chronic atopic dermatitis, with lichenification of the face, neck, and major flexures, and severe pruritus. The distribution also mimics that of photodermatitis, with ragweed dermatitis differentiated by its involvement of the upper eyelids and the retroauricular and submental areas. Chronic cases may continue into the winter, although signs and symptoms are most severe at the height of the season. Coexistent sensitization to pyrethrum may account for prolongation of ragweed dermatitis. Men outnumber women in hypersensitivity reactions; farmers outnumber patients of all other occupations. Plant derivatives Marine plants 98 Numerous aquatic plants are toxic or produce contact dermatitis. The onset is within a few minutes of leaving the ocean, with severe itching and burning, followed by dermatitis, blisters, and deep, painful desquamation that affects the areas covered by the bathing suit, especially the scrotum, perineum, and perianal areas and occasionally the breasts in women). Patch tests with the alga are neither necessary nor helpful because it is a potent irritant.
Buy 500 mg glycomet mastercard
The femoral nerve can be exposed from its appearance at the edge of the psoas muscle to its exit under the inguinal ligament through an anterior lateral extraperitoneal approach diabetes prevention curriculum generic glycomet 500 mg without a prescription. A skin incision is made just above and parallel to the iliac crest, and the abdominal wall is opened in layers, exposing the pre- and retroperitoneal fat. The femoral nerve emerges from within the psoas muscle and passes under the inguinal ligament lateral to the femoral artery. Retracting the peritoneal contents anteriorly will readily expose the lateral femoral cutaneous and femoral nerves, which lie under the iliac fascia and the branches of the genitofemoral nerves as they perforate the psoas muscle. This exposure can be extended anteriorly to expose the femoral nerve in the thigh. Several modifications of this approach have been described that offer a better exposure of the more proximal intrapsoas portion of the femoral nerve; the upper lumbar roots, which form the femoral nerve; or the proximal lower lumbar roots, which contribute to the sciatic nerve. More proximal exposure of the upper lumbar plexus is achieved by an incision that begins just below the lateral rib cage and extends transversely to just below the umbilicus. The external oblique muscle is split and the deeper abdominal wall layers are cut. Again the peritoneal contents are swept forward, allowing the upper lumbar roots to be traced through the psoas muscle to their exit from the spine. In male patients, care should be taken not to injure the sympathetic chain, which lies in the gutter between the psoas muscle and the vertebral body, because this can result in retrograde ejaculation. The cutaneous nerve is found lying on the iliacus muscle lateral to the femoral nerve beneath the iliac fascia. The small incision and the approach through the retroperitoneal fat minimize blood loss and approach-related morbidity. The femoral nerve can be exposed in the thigh by a vertical incision made parallel and lateral to the femoral artery. Proximal exposure of the femoral nerve is obtained by curving the incision laterally along a line connecting the anterior superior iliac spine with the pelvis symphysis. The more proximal femoral nerve is exposed by opening the muscular abdominal wall into the retroperitoneal space. The saphenous nerve can be exposed at the knee by an incision made parallel and lateral to the tendon of the sartorius muscle. The main trunk of the saphenous nerve may be hidden behind the saphenous vein because these two structures maintain an intimate relationship down the leg. The infrapatellar branch travels from lateral to medial just below the level of the tibial plateau. Obturator Nerve the obturator nerve takes its origin from the ventral division of the ventral rami of L2, L3, and L4. The nerve forms in the psoas major muscle, but unlike the femoral nerve it passes behind the common femoral vessels lateral to the internal iliac artery. As it passes through the obturator foramen into the anterior thigh, the nerve divides into an anterior and a posterior branch. A branch joins the medial cutaneous nerve, providing sensation to the medial upper thigh. Motor branches pass to the adductor longus, adductor brevis, and gracilis muscles. This nerve enters the popliteal fossa along with the femoral artery to innervate the knee joint. Fortunately, surgeons rarely need to repair the nerve within the pelvis, where its deep location makes repair quite difficult. The obturator mononeuropathy most frequently occurs after urologic, gynecologic, or orthopedic procedures. The interval between the pectineal and the adductor longus, both of which originate from the pectineal line of the pubis, is developed. If it is difficult to open this plane, the medial interval between the adductor longus and adductor magnus can be opened and the adductor longus can be mobilized. The proximal pectineus may need to be detached to afford a good look at the nerve. The anterior division of the obturator nerve is seen passing over the obturator brevis muscle. Exposure of the posterior division may require partial sectioning of the obturator brevis muscle. The combined sural nerve then travels along the lateral border of the Achilles tendon, passing between that tendon and its lateral malleolus. Motor branches from the tibial nerve are given to the posterior tibialis, flexor hallucis longus, and flexor digitorum longus muscles, and the nerve travels behind the soleus muscle. The tibial nerve emerges from the medial side of the tendon calcaneus to pass between that tendon and the lateral malleolus under the flexor reticulum. The calcaneal branch to the heel can originate from the posterior tibial nerve, the lateral plantar nerve, and, rarely, from the medial plantar nerve. Beneath the flexor retinaculum the tibial nerve lies posterior to the posterior tibial artery. The medial and lateral plantar nerves enter the foot within adjacent but separate canals. The roof of the canal for the lateral plantar nerve is the aponeurosis of the foot, and the roof for the canal of the medial plantar nerve provides the origin of the abductor hallucis brevis. The two lumbar nerves L4 and L5 combine to form the lumbosacral branch, which crosses the ala of the sacrum to join the upper three sacral roots forming the sciatic nerve. The sciatic nerve exits through the greater sciatic notch below the piriformis muscle and above the superior gemellus under the cover of the gluteus maximus muscle. The fibers destined to form the peroneal nerve segregate lateral to the fibers destined to form the tibial nerve. The sciatic nerve travels down the thigh posterior to the exterior rotators of the hip (the obturator internus, the gemellus, and the quadratus femoris) and the adductor magnus. The nerve is flanked medially by the semitendinous muscle and laterally by the short head of the biceps femoralis, and is crossed posteriorly by the long head of the biceps femoralis muscle because that muscle makes its way from the ischial tuberosity to the head of the fibula. Soon after exiting from the sciatic notch, the sciatic nerve provides innervation to the hamstring muscles with branches to the semimembranous, semitendinous, long head of the biceps, and adductor magnus originating from the tibial division, and branches to the short head of the biceps originating from the peroneal division. Most commonly the sciatic nerve divides into a medial tibial division and a smaller lateral peroneal division in the lower third of the thigh proximal to the popliteal fossa. The nerve leaves the popliteal fossa, passing between the heads of the gastrocnemius muscle, and continues distally, sandwiched anterior to the soleus muscle and behind the posterior tibialis muscle, emerging 4 cm above the ankle from the medial side of the tendon calcaneus. Muscular branches to the gastrocnemius and soleus muscles originate at approximately the level of the medial epicondyle of the femur, and 3 to 5 cm proximal to the knee joint the tibial nerve contributes to the sural nerve. This cutaneous branch passes between the head of the gastrocnemius muscle before Exploration of the Intrapelvic Sciatic Nerve Because of the slope of the sacrum away from the surgeon, exploration of the sacral plexus is difficult through the retroperitoneal approach. A transperitoneal approach affords a good exposure of the proximal sciatic nerve and control of the adjacent vasculature. The peritoneal cavity is opened through a midline or transverse approach, and the peritoneal contents are displaced superiorly with moist sponges exposing the posterior peritoneum. The descending portion of L4 joins the L5 root anterior to the promontory of the sacrum. The three upper sacral roots join this trunk, separated from the sacrum by the origin of the piriformis muscle. Branches of the internal iliac artery and the superior gluteal, inferior gluteal, and internal pudendal arteries pass through the proximal sacral plexus. Exposure of the Proximal Extrapelvic Sciatic Nerve An extensive approach described by Henry12 lifts the gluteus maximus muscle to expose the entire proximal portion of the sciatic nerve. The posterior femoral cutaneous nerve, which travels down the posterior midthigh, must be avoided. The gluteus muscle is detached from its insertion into the femur and the iliotibial track, the interval between the gluteus medius and gluteus maximus is developed, and the gluteus maximus muscle is lifted, hinged on its medial origin, into the posterior gluteal line of the ileum and the dorsal sacrum. The sciatic, superior gluteal, inferior gluteal, posterior femoral cutaneous, and pudendal nerves can be seen. The sciatic and posterior femoral cutaneous nerves are seen exiting the pelvis under the piriformis muscle and then traveling caudally over the short external rotators of the hip. For lesions localized to the gluteal region, a transgluteal approach can be accomplished by a muscle-splitting approach through the gluteus maximus muscle.