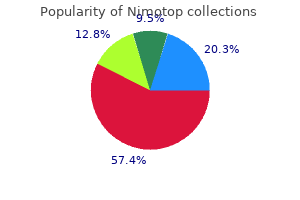
Discount nimotop on line
If the view is suboptimal back spasms 39 weeks pregnant cheap nimotop 30mg mastercard, an assistant can pass the tracheal tube introducer to the operator for placement anterior to the arytenoids and into the larynx. If only the epiglottis is visible, place the introducer, with a 60-degree distal bend, just under the epiglottis and direct it anteriorly. If any portion of the arytenoids is visible and the introducer was seen to pass anterior to them without resistance, the introducer is in the airway. In addition to better visual confirmation, successful passage is indicated, up to 90% of the time, by feeling clicks produced by the angled tip of the introducer as it strikes against the tracheal rings. If there is still any question whether the introducer is in the airway, gently advance it at least 40 cm, at which point resistance should be felt as the introducer passes the carina and stops inside a main bronchus. If the bougie does not stop when advanced approximately 40 cm, the introducer is most likely in the esophagus. The introducer is handed to the clinician after the best glottic view has been obtained. A, the clinician places the introducer (the black line positioned at the teeth indicates the proper introducer depth to ensure stable positioning within the trachea while providing enough length to grasp the end of the introducer before passing the tube). B, An assistant passes the tracheal tube over the introducer as the clinician holds the introducer steady. C, the clinician passes the tracheal tube with a 90-degree counterclockwise rotation as the tube approaches the glottis, and the assistant withdraws the introducer. This is not uniformly appreciated, even in England where the bougie is used commonly. Second, in some cases the bougie will pass through the cords but will become lodged in the anterior trachea and not be able to be advanced further. This will prevent the tip from striking the anterior trachea and allow the bougie to pass to the carina. Fourth, although there may be some benefit to lubricating the distal end of the introducer, in emergency intubations, lubricating the full length of the introducer makes it slippery and hard to handle without conferring any obvious advantage. This often results in difficulty placing the tube because it is displaced posteriorly by the weight of the pharyngeal soft tissues and gets hung up on the laryngeal structures. If the introducer enters the mouth at a significant angle above this line, most often when the clinician is too close to the patient, it may be deflected posteriorly by the lip or intraoral structures and escape the attention of the operator. Once the tube is on the introducer, reinsert the laryngoscope and advance the introducer through the glottic opening. Laryngospasm If the patient is not paralyzed, laryngospasm, or persistent contraction of the adductor muscles of the vocal cords, may prevent passage of the tube. Pretreatment with topical lidocaine may decrease the likelihood of laryngospasm, though this is not routinely performed. After laryngospasm is noted, one option is to spray lidocaine (2% or 4%) directly onto the vocal cords. An infrequent but effective means of achieving tracheal anesthesia is transtracheal puncture and injection of 3 to 4 mL of lidocaine through the cricothyroid membrane. Occasionally, the spasm is prolonged and needs to be disrupted with sustained anterior traction applied at the angles of the mandible, as in the jaw-thrust maneuver. Do not force the tube at any time because it could cause permanent damage to the vocal cords. Prolonged, intense spasm may ultimately require muscle relaxation with a paralyzing drug (see Chapter 5). Because tube movement with both neck flexion and extension averages 2 cm,154 the desired range of tip location is between 3 and 7 cm above the carina. On a portable radiograph, the adult carina overlies the fifth, sixth, or seventh thoracic vertebral body. If the carina is not visible, it can be assumed that the tip of the tube is properly positioned if it is aligned with the third or fourth thoracic vertebra. In children, the carina is more cephalad than in adults, and it is consistently situated between T3 and T5. Inflate the cuff to the point of minimal air leak with positive pressure ventilation. In an emergency intubation, inflate with 10 mL of air and adjust the inflation volume after the patient is stabilized. After placement of the tracheal tube, auscultate both lungs under positive pressure ventilation. Take care to auscultate posterolaterally because auscultation anteriorly can reveal sounds that mimic breath sounds and arise from the stomach. Position the tube at the corner of the mouth, where the tongue is less likely to expel it. Unintentional extubation can have disastrous consequences, particularly if the patient was difficult to intubate initially. Confirm tracheal placement clinically by seeing the tube pass through the vocal cords (Table 4. One may hear "normal" breath sounds if only the midline of the thorax is auscultated. Apply a second piece of tape (sticky side down) to the center of the long piece of tape. The method illustrated can be replaced by using a commercial holder or tracheostomy cloth tie. Because of the angles of takeoff of the main bronchi and the fact that the carina lies to the left of midline in adults, right main stem intubation is most common and is indicated by decreased breath sounds on the left side. When asymmetric sounds are heard, deflate the cuff and withdraw the tube until equal breath sounds are present. Bloch and coworkers163 reported accurate pediatric tracheal positioning if after noting asymmetric breath sounds the tube is withdrawn a defined distance beyond the point at which equal breath sounds are first heard: 2 cm in children younger than 5 years and 3 cm in older children. If known to be in the trachea by other measures, radiography can assess for proper depth of tube insertion. If the tube is placed in the trachea correctly, the plunger will pull back without resistance as air is aspirated from the lungs. If the tracheal tube is in the esophagus, resistance is felt when the plunger is withdrawn because the pliable walls of the esophagus collapse under the negative pressure and occlude the end of the tube. Another device that uses the same principle as syringe aspiration is the self-inflating bulb. In the initial study conducted in an operating room, tube placement was identified correctly in 99 of 100 cases (51 esophageal, 48 tracheal). That tube was removed and found to be nearly totally occluded with purulent secretions. Slight resistance was noted in one patient with right main stem intubation; the resistance decreased when the tube was pulled back. If any connections are loose, the leak may allow the syringe to be withdrawn easily, thereby mimicking tracheal location of the tube. When using the aspiration technique, apply constant, slow aspiration to avoid occlusion of the tube from tracheal mucosa drawn up under the high negative pressure. If the tracheal tube is placed correctly, 30 to 40 mL of air can be aspirated without resistance. If air was initially aspirated and some resistance is then encountered, the tracheal tube should be pulled back between 0. This takes the tube out of the bronchus if it has been placed too deeply and changes the orientation of the bevel if the tube has been temporarily occluded with tracheal mucosa. Air is easily aspirated if the tube was in the trachea, but repositioning it will make no difference if the tube was in the esophagus. The syringe aspiration technique can be used before or after ventilation of the patient. An early study with the Ellick evacuator bulb device reported that 82% of esophageal intubations were identified. Confusion may occur if the esophageal tube is tested more than once because subsequent inflations may be silent. With repeated assessments, false-positive refilling of the bulb may occur as a result of instillation of air during the first attempt. Delayed, though complete refilling of the bulb may occur with bronchial tube placement or placement in the more pliable pediatric airway. The bulb suction modification of the aspiration technique has not been studied as thoroughly as the syringe technique. A significant number of false positives occur with esophageal detection devices (the tube is correctly placed in the trachea, but the device suggests that it is in the esophagus).
Order cheapest nimotop
At some point muscle relaxant baclofen purchase 30mg nimotop amex, further attempts at intubation become futile and the benefits of a surgical airway outweigh the risks associated with ongoing hypoxia. The membrane is bordered superiorly by the thyroid cartilage and inferiorly by the cricoid cartilage. The lateral aspects of the cricothyroid membrane are partially covered by the cricothyroid muscles, but the central triangular portion is subcutaneous, which makes it an ideal location to access the airway. Identify the cricothyroid membrane by locating the prominent thyroid cartilage superior to it. The thyroid cartilage consists of two lateral laminae that join at an acute angle in the midline to form the laryngeal prominence. Cricothyrotomy Indications Inability to maintain >90% saturation between intubation attempts or after three attempts Inability to bag-mask-valve ventilate the patient between intubation attempts or after three attempts Multiple attempts at endotracheal intubation fail to secure the airway after failed rescue maneuvers. Higher scores are associated with poor glottic visualization and difficult intubation. A Mallampati score can be determined in cooperative patients who are able to sit upright. In anticipation of a failed airway, it may be reasonable to mark the cricothyroid membrane using ultrasound guidance to prepare for the possibility of a cricothyrotomy. The exact age at which surgical cricothyrotomy can be performed is controversial and not well defined. Various textbooks list the lower age limit from 5 years30 to 10 years31 or 12 years. Some authors also identify tracheal transection or low tracheal obstruction (below the cricoid) as absolute contraindications to cricothyrotomy because of the need to secure the airway below the injury33 (Box 6. Equipment the equipment necessary to perform a traditional surgical cricothyrotomy includes a scalpel with a No. Surgical cricothyrotomy can safely and successfully be performed with minimal cervical spine movement. Prepare the skin of the anterior aspect of the neck with antiseptic solution and create a sterile field with the use of drapes or towels. If the patient is awake or responding to pain, give a subcutaneous and translaryngeal injection of lidocaine with epinephrine as a local anesthetic. Wear sterile gloves and take standard precautions by wearing a mask, goggles, and gown. In a follow-up report in 1989, Erlandson and colleagues38 emphasized the importance of making an initial vertical skin incision and using a relatively small (No. These modifications have generally been accepted and are commonly described as part of the traditional technique. Stabilize the larynx with the nondominant hand by grasping both sides of the lateral thyroid cartilage with the thumb and middle finger. In shorter or more obese patients, or in patients with neck swelling, these landmarks may be more difficult to identify by palpation alone. Immobilize the larynx with your nondominant hand and palpate the cricothyroid membrane with your index finger. With the index finger of the nondominant hand, palpate the cricothyroid membrane through the incision. It is important to understand that the remainder of the procedure should be performed by palpation of the anatomy, not visualization, because bleeding may obscure the field and there is no time to delay while trying to achieve hemostasis. If the cricothyroid membrane cannot be palpated, extend the initial incision superiorly and inferiorly and try to palpate again. Place the nondominant index finger into the stoma momentarily and exchange the scalpel for the tracheal hook. Rotate the handle cephalad while grasping the inferior border of the thyroid cartilage with it. This instrument works opposite that of most ordinary instruments, such as hemostats. This can be confusing the first time you use this instrument, and it is worth practicing before you need it in an emergency. If this instrument is not available in an emergency, Mayo scissors, a hemostat, or even the blunt end of a scalpel handle can be used to dilate the incision in the cricothyroid membrane. If the dilator is left horizontal, the blades of the dilator may impede passage of the tracheostomy tube into the trachea. Because this technique omits dilating the stoma with the Trousseau dilator, it may be more difficult to pass a tracheostomy tube. This method has been further simplified, using ultrasound to localize the cricothyroid membrane. Then, a single horizontal laceration is made, again through the skin, subcutaneous tissue, and cricothyroid membrane. Anatomic distortion will make locating the cricothyroid membrane with a needle more difficult. Be careful not to advance the needle too far because this may result in perforation of the posterior aspect of the trachea. To help recognize when the trachea has been entered, place a small amount of saline in the syringe before the procedure. When the membrane is pierced and the trachea is entered, air will be aspirated into the syringe and air bubbles will appear in the saline. If the needle does not have an overlying catheter, leave the needle in place and remove the syringe. Once the guidewire is placed securely in the trachea, remove the needle or catheter. Once it is through the skin and into the trachea, advance the airway catheter to its hub until it is flush against the neck. These patients often have confounding medical issues, with high morbidity and mortality rates. The cricoid arteries branch from the superior thyroid arteries and anastomose at the anterior superior aspect of the cricothyroid membrane. The laterally running superior thyroid arteries are more often damaged when the initial incision is broad and horizontal. To prevent hemorrhage from these vessels, make the initial skin incision longitudinal as in the traditional technique, and maintain careful awareness of the landmarks. If the opening in the cricothyroid membrane is not carefully stabilized during the procedure, the tube may inadvertently be inserted into subcutaneous tissue. This complication can be recognized by the presence of subcutaneous emphysema when attempting to ventilate the patient. It is essential to recognize this immediately to prevent the development of hypoxia and obliteration of anatomic landmarks. A misplaced tube can pass into any location other than through the cricothyroid membrane, but the most crucial locations are those that do not enter the airway because this will lead to hypoxia and death if not recognized. Aspirate on the saline-filled syringe as you advance; air bubbles will enter the syringe when the trachea is entered. Place the dilator into the airway catheter and thread them over the wire as a unit until it is flush with the skin. As with other cricothyrotomy techniques, extension of the neck (if clinically feasible) exposes the trachea and facilitates the procedure. Since the publication of this latter report, numerous other studies have corroborated their findings that chronic subglottic stenosis is an infrequent long-term complication of surgical cricothyrotomy. It is difficult to successfully perform an emergency surgical airway, and even with proper training and standard experience, not all attempts with this technically difficult procedure will be successful. Although the reported success rate for cricothyrotomy has been quite high (89% to 100%) in most studies,25,37,38,55,62,66,76,87 one study found only a 62. Consensus cannot be drawn from the literature comparing the traditional method with the percutaneous Seldinger (Melker kit) method. Some studies show no difference in time to ventilation or complication rate when the traditional technique is compared with the Seldinger technique.
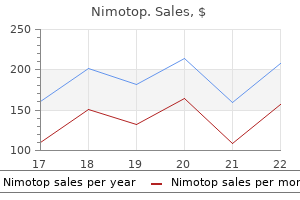
Cheapest nimotop
One consensus panel recommended pancuronium for maintaining paralysis muscle relaxant nerve stimulator generic 30mg nimotop with visa, except in patients with cardiac disease or hemodynamic instability, for whom they recommended vecuronium. This approach, referred to as a "sedated look" or "awake look," is used when the clinician suspects a difficult intubation. This approach allows the clinician to verify that the laryngeal structures are indeed visible and accessible before committing to paralysis. This technique allows the patient to maintain respiratory drive during analysis of the airway. This older practice may create a vulnerable and compromised patient in whom intubating conditions are then problematic. They are particularly useful as adjuncts to nasotracheal and fiberoptic intubation but do not generally provide the degree of analgesia or relaxation desirable for traditional laryngoscopy. In addition, the time required to achieve good topical anesthesia may limit the usefulness of these techniques in emergency situations. Topical anesthesia may be achieved by direct application, by cricothyroid membrane puncture, or by inhalation of a nebulized anesthetic. Direct Application of Topical Anesthetics Achieving anesthesia of the oral and pharyngeal mucosa is a relatively simple procedure that involves the use of commonly available agents such as 4% lidocaine or a combination such as 14% benzocaine, 2% butamben, and 2% tetracaine (Cetacaine, Cetylite Inc. Achieving anesthesia of the hypopharynx is more difficult because optimal results require application of the anesthetic to the epiglottis and vocal cords. If time allows, administer an anticholinergic agent, such as glycopyrrolate, at a dose of 0. It is important to attempt to dry the airway with suction and gauze, as glycopyrrolate will only reduce additional secretions and will not remove existing moisture. An alternative method is to visualize the epiglottis and vocal cords with a laryngoscope and directly spray them with the anesthetic agent. The use of a laryngoscope to visualize the vocal cords, however, is much more stimulating to the patient and often not well tolerated. Another alternative is percutaneous injection of an anesthetic agent into the trachea at the level of the cricothyroid membrane. The availability of relatively effective and safe induction agents makes this a less attractive alternative than in the past, but these techniques may be desirable in specific patients, such as for fiberoptic intubation of a predicted difficult airway. The natural airway is maintained along with spontaneous respiration and a degree of protection from aspiration. The use of sedative agents to produce a state of mild or moderate sedation and adequate topical anesthesia are the principal components needed for awake intubation. Thomas147 likened standard laryngoscopy in an awake patient to the "mouth being held open with a wrench. The upper airway is richly innervated by sensory branches of the 5th, 7th, 9th, and 10th cranial nerves. In addition to pain fibers, there are stretch receptors that stimulate the coughing and gagging reflexes with even minor airway manipulation. It is essential that adequate analgesia be provided before intubation in all but the most extreme circumstances. A new sedative agent, dexmedetomidine (an 2-adrenoreceptor agonist), has been described for use in awake intubation. Patients become sleepy but, if stimulated, can easily be aroused and are generally cooperative. These properties make it seem like an ideal agent for awake intubation, but its use is limited in emergencies by a requisite 10-minute loading dose followed by a maintenance infusion. It preserves spontaneous respirations, does not generally cause hypotension, and can safely provide a deep level of sedation. It may alternatively be used at dissociative doses (> 1 mg/kg) but theoretically can cause more side effects. An attempt to appropriately anesthetize the airway is important as ketamine preserves airway reflexes. The clinician should be prepared for possible laryngospasm during the use of a scope with ketamine. Prepare the skin with an antiseptic and then puncture the cricothyroid membrane in the midline. Advance the needle until air can be aspirated and then rapidly inject 2 mL of 4% lidocaine. In this procedure, identify the cricothyroid membrane immediately below the thyroid cartilage. After antiseptic skin preparation, puncture the overlying tissue and membrane with a 22-gauge needle in the midline and just above the superior border of the cricoid cartilage. Take care to maintain the needle in the midline at all times to avoid injury to the recurrent laryngeal nerves. Advance the needle until air can be aspirated, which indicates placement of the needle in the trachea. Typically, this will precipitate a cough and distribute the anesthetic over the upper part of the trachea, vocal cords, and epiglottis. Whereas more invasive than the other described techniques, intratracheal injection may provide superior local anesthesia,150,151 but there is limited evidence comparing different techniques. Delayed-Sequence Intubation Some patients may be unable to tolerate adequate preoxygenation prior to an initial attempt to intubate. Delayed-sequence intubation has been described as procedural sedation for the procedure of preoxygenation. This allows the patient to tolerate preoxygenation with any appropriate combination of high-flow nasal cannula, bag-valve-mask (preferably with positive endexpiratory pressure valve), non-rebreather mask, or noninvasive ventilator. Deliver the anesthetic via a standard nebulizer and face mask connected to an oxygen source that delivers 4 to 8 L/min. It is critical that the oxygen source not be set to the high-flow rate commonly used to nebulize medications such as albuterol. Doing so will anesthetize the lungs without properly anesthetizing the vocal cords. Nebulize a 4-mL volume of a 4% lidocaine solution over a period of approximately 5 minutes. Bourke and colleagues152 reported achieving consistently good topical anesthesia with this technique, although their patients were often premedicated with combinations of opioids and sedatives. There has been an increasing de-emphasis on the importance of premedications prior to intubation. The importance of avoiding hypotension and hypoxia has caused far less focus on the use of lidocaine, fentanyl, or other medications prior to intubation. An increased emphasis on awake intubations and the new concept of delayed-sequence intubation has further expanded the use of topical anesthetics and ketamine to assist in difficult airways. A mastery of the pharmacology of drugs used to intubate remains a critical skill for all providers that see critically ill patients. Kovacs G, Macquarrie K, Campbell S: Pretreatment in rapid sequence intubation: Indicated or contraindicated Effect on plasma cortisol concentrations of a single induction dose of etomidate or thiopentone. Lignocaine as a pretreatment to rapid sequence intubation in patients with status asthmaticus. Hassani V, Movassaghi G, Goodarzi V, et al: Comparison of fentanyl and fentanyl plus lidocaine on attenuation of hemodynamic responses to tracheal intubation in controlled hypertensive patients undergoing general anesthesia. Green R, Hutton B, Lorette J, et al: Incidence of postintubation hemodynamic instability associated with emergent intubations performed outside the operating room: a systematic review. Morris C, Perris A, Klein J, et al: Anaesthesia in haemodynamically compromised emergency patients: does ketamine represent the best choice of induction agent Clancy M, Halford S, Walls R, et al: In patients with head injuries who undergo rapid sequence intubation using succinylcholine, does pretreatment with a competitive neuromuscular blocking agent improve outcome Loflin R, Koyfman A: When used for sedation, does ketamine increase intracranial pressure more than fentanyl or sufentanil Guldner G, Schultz J, Sexton P, et al: Etomidate for rapid-sequence intubation in young children: hemodynamic effects and adverse events.
| Comparative prices of Nimotop | ||
| # | Retailer | Average price |
| 1 | H-E-B | 564 |
| 2 | Kroger | 955 |
| 3 | Nordstrom | 262 |
| 4 | Tractor Supply Co. | 740 |
| 5 | Limited Brands | 167 |
| 6 | Target | 729 |
| 7 | Menard | 752 |
| 8 | Save Mart | 957 |
| 9 | Staples | 783 |
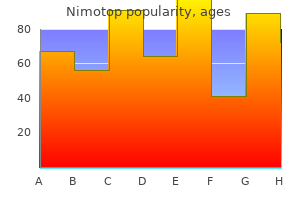
Cheap nimotop 30 mg online
In fasted anesthetized patients spasms below rib cage order generic nimotop online, the incidence of aspiration is very low, approximately 2 per 10,000 cases. Size 3 is yellow and designed for patients 4 to 5 feet in height, size 4 is red and designed for patients 5 to 6 feet in height, and size 5 is purple and designed for patients taller than 6 feet. Introduce the tip of the device into the corner of the mouth while rotating the tube 45 to 90 degrees so that the blue orientation line on the tube is touching the corner of the mouth. As the tip passes under the base of the tongue, rotate the tube back to the midline so that the blue orientation line faces the ceiling. The device is properly placed posterior to the larynx, with the distal end in the proximal esophagus. The distal cuff is inflated in the proximal esophagus and the larger proximal cuff is inflated at the base of the tongue. The proximal portion of the tube is at the lip line and the distal aperture (between the cuffs) is aligned with the glottic opening; oxygen flow from the device to the glottis is depicted by the white arrows. The exact pathology was not determined but was thought to be a pharyngeal or esophageal perforation. Inflate the cuffs with the minimum volume necessary to create a good seal (see the product brochure for maximum cuff volumes). The most serious complication is tracheal placement, which occurred in 10% of cases in one study and is probably significantly underappreciated and underreported. Because an autopsy was denied, the exact injury was never confirmed and may have been related to other interventions during resuscitation. When it is placed blindly the tip will end up in the esophagus in approximately 95% of cases and in the trachea in approximately 5%. The longer lumen or tube is used for ventilation when the tip is in the esophagus. The large proximal cuff or balloon is designed to occlude the pharynx by filling the space between the base of the tongue and the soft palate. Because the King is easier to use and proven to be an effective and reliable primary and rescue airway device, the Combitube is used less frequently than previously. The manufacturer recommends the smaller 37-Fr device for patients from 4 feet to 5 feet 6 inches tall and the larger 41-Fr device for patients taller than 5 feet 6 inches. Studies suggest that the smaller 37-Fr Combitube can be used safely in patients up to approximately 6 feet tall. To insert the Combitube, hold the device in the dominant hand and gently advance it caudally into the pharynx while grasping the tongue and jaw between the thumb and index finger of the nondominant hand. A, Approximately 95% of placements are esophageal, so begin ventilation through the longer (blue) airway tube. When the distal tip is in the esophagus, ventilation occurs through the vent holes between the distal and proximal cuffs (white arrows). B, If the tip of the Combitube is in the trachea, ventilation cannot be accomplished via the long (blue) airway tube. It is essential to recognize this quickly, and use the short (white) tube for ventilations. The large pharyngeal balloon serves to securely seat the Combitube in the oropharynx and creates a closed system in the case of esophageal placement. Because approximately 95% of placements are esophageal, begin ventilation through the longer (blue) airway tube. Alternatively, use a Wee-type aspirator device on the shorter (clear) lumen to confirm that the tip is in the esophagus before ventilation through the longer (blue) lumen. Easy aspiration with the Wee-type device indicates tracheal positioning of the tube and requires changing the ventilation to the shorter (clear) tracheal lumen. Use a more caudal, longitudinal direction of insertion as opposed to an anteroposterior direction of insertion. The Combitube must also be maintained in the true midline position during insertion to avoid blind pockets in the supraglottic area, which can prevent passage of the tube. There are many techniques and devices that can be used to manage emergency airways. In difficult situations, providers will probably have the best success when basic skills are performed excellently. Complications Inappropriate balloon inflation and incorrect Combitube placement can lead to air leaks during ventilation. Combes X, Jabre P, Margenet A, et al: Unanticipated difficult airway management in the prehospital emergency setting: prospective validation of an algorithm. Meier S, Geiduschek J, Paganoni R, et al: the effect of chin lift, jaw thrust, and continuous positive airway pressure on the size of the glottic opening and on stridor score in anesthetized, spontaneously breathing children. Guildner C: Resuscitation-opening the airway: a comparative study of techniques for opening an airway obstructed by the tongue. In Calder I, Pearce A, editors: Core topics in airway management, Cambridge, 2005, Cambridge University Press, p 43. Morikawa S, Safar P, Decarlo J: Influence of the head-jaw position upon upper airway patency. Ayuse T, Inazawa T, Kurata S, et al: Mouth-opening increases upper-airway collapsibility without changing resistance during midazolam sedation. Kobayashi M, Ayuse T, Hoshino y, et al: Effect of head elevation on passive upper airway collapsibility in normal subjects under propofol anesthesia. Isono S, Tanaka A, Tagaito y, et al: Influences of head positions and bite opening on collapsibility of the passive pharynx. Langhelle A, Sunde K, Wik L, et al: Airway pressure with chest compressions versus Heimlich manoeuvre in recently dead adults with complete airway obstruction. Gruber P, Kwiatkowski T, Silverman R, et al: Time to equilibration of oxygen saturation using pulse oximetry. Global Initiative for Chronic Obstructive Lung Disease: Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease, 2011. Dorges V, Wenzel V, Knacke P, et al: Comparison of different airway management strategies to ventilate apneic, nonpreoxygenated patients. Dorges V, Ocker H, Hagelberg S, et al: Optimisation of tidal volumes given with self-inflatable bags without additional oxygen. Reardon R, Ward C, Hart D: Assessment of face-mask ventilation using an airway model. Ikeda A, Isono S, Sato y, et al: Effects of muscle relaxants on mask ventilation in anesthetized persons with normal upper airway anatomy. Harboe M: Lactic acid content in human venous blood during hypoxia at high altitude. Slessarev M, Somogyi R, Preiss D, et al: Efficiency of oxygen administration: sequential gas delivery versus "flow into a cone" methods. Wexler H, Aberman A, Scott A, et al: Measurement of intratracheal oxygen concentrations during face mask administration of oxygen: a modification for improved control. In Walls R, Murphy M, Michael F, editors: Manual of emergency airway management, ed 4, Philadelphia, 2012, Wolters Kluwer/Lippincott Williams & Wilkins Heath. Chanques G, Riboulet F, Molinari N, et al: Comparison of three high flow oxygen therapy delivery devices: a clinical physiological cross-over study. Tiruvoipati R, Lewis D, Haji K, et al: High-flow nasal oxygen vs high-flow face mask: a randomized crossover trial in extubated patients. Ellis Dy, Harris T, Zideman D: Cricoid pressure in emergency department rapid sequence tracheal intubations: a risk-benefit analysis. Aoyama K, Takenaka I, Sata T, et al: Cricoid pressure impedes positioning and ventilation through the laryngeal mask airway. Asai T, Barclay K, McBeth C, et al: Cricoid pressure applied after placement of the laryngeal mask prevents gastric insufflation but inhibits ventilation. Asai T, Barclay K, Power I, et al: Cricoid pressure impedes placement of the laryngeal mask airway and subsequent tracheal intubation through the mask. Brimacombe J: Laryngeal mask anesthesia: principles and practice, Philadelphia, 2005, Saunders. Brimacombe J, White A, Berry A: Effect of cricoid pressure on ease of insertion of the laryngeal mask airway.
Buy generic nimotop
Maggiolini S muscle relaxant drug list purchase cheap nimotop, Bozzano A, Russo P, et al: Echocardiography-guided pericardiocentesis with probe-mounted needle: report of 53 cases. Armstrong W, Feigenbaum H, dillon J: Acute right ventricular dilatation and echocardiographic volume overload following pericardiocentesis for relief of cardiac tamponade. Vandyke W, Jr, Cure J, Chakko C, et al: Pulmonary edema after pericardiocentesis for cardiac tamponade. Chamoun A, Cenz R, Mager A, et al: Acute left ventricular failure after large volume pericardiocentesis. Angouras dC, dosios T: Pericardial decompression syndrome: a term for a well-defined but rather underreported complication of pericardial drainage. Hamaya Y, dohi S, ueda N, et al: Severe circulatory collapse immediately after pericardiocentesis in a patient with chronic cardiac tamponade. If possible, place a backboard under the victim to ensure appropriate thoracic compression. Rotate rescuers aggressively (approximately every 2 to 3 minutes) to avoid deteriorating quality of compressions because of exhaustion. Minimize pauses in chest compressions because even short pauses have profound effects on coronary perfusion pressure and outcomes. Cardiopulmonary Resuscitation and Artificial Perfusion During Cardiac Arrest Benjamin S. Each minute without treatment, however, is associated with a 10% to 15% decrease in the probability of survival. For example, shallow chest compressions have an adverse impact on the success of defibrillation. These guidelines are formulated through a formalized data evaluation process and are updated every 5 years, last updated in 2015. In addition, pauses in chest compressions are too long, and hyperventilation of arrest patients is common. T prevent unwittingly o hyperventilating the patient, one practical technique is to ask the rescuer who is providing ventilations to remove his or her hand completely off the bag-valve-mask apparatus between ventilations. The team leader should be vigilant in the observation of delivery of ventilations and should be ready to verbally prompt rescuers to ventilate the patient at the appropriate rate if hyperventilation is performed. If a pulse cannot be readily felt within seconds, return to chest compressions as soon as possible. Attempt pulse detection at the location of the carotid or femoral artery because peripheral pulse checks during profound shock or cardiac arrest states are notoriously unreliable. To maximize calm and efficiency and to ensure quality of care, establish a team protocol. Designate someone to be the leader of the resuscitation, and make sure that all participants are clearly aware of this designation. The designated team leader should be responsible for monitoring the rhythm, for giving orders to initiate and terminate chest compressions, and for delivery of drugs and other therapies. The team leader should be situated either at the head of the bed or at a place where they can direct the resuscitation. It is important that the team leader does not actually perform compressions, ventilations, or other specific procedures unless absolutely necessary because they may quickly lose control of the resuscitation. Some of these tools directly improve chest compressions, whereas others are less direct and aim to improve human performance or enhance hemodynamics during the delivery of chest compressions. This section describes some of these promising, intuitively useful, yet still unproven techniques. In laboratory studies, this negative pressure enhances venous return to the heart and results in increased cardiac output with each subsequent chest compression. Apply the device and administer ventilations at a rate of 8 to 10 breaths/min as per standard resuscitation guidelines. This is best accomplished with a two-person ventilation technique in which one person holds the face mask and the second person squeezes the bag. This is the Res-Q-Pod; the flashing light indicator is used to time the respiratory rate. The device measures the quality of compressions via a force detector or accelerometer (or both) that determines the rate and depth of chest compressions. The chest compression pad with force detector and accelerometer is indicated (arrow). Such tools have been introduced in previous decades but fell out of favor because of unwieldy design and other practical considerations. One such device uses a "load-distributing compression band" (Autopulse, Zoll Medical Corp. The Autopulse device works via a wide band that is attached to a backboard and battery-powered motor and is placed across the torso. Through cycles of constriction and relaxation, the band compresses the chest in a circumferential manner at a fixed rate and depth consistent with resuscitation guidelines. Such devices have a unique role in out-of-hospital arrest because compressions can be delivered while transporting a patient down stairs or into an ambulance. Venous blood is withdrawn from a central vein (blue arrows), pumped through an oxygenator, and reinfused into a central vein (red arrow). Further research is required in this experimental procedure, which may benefit a select cohort of cardiac arrest victims. Early defibrillation has been linked to better survival rates, but no medications have been shown to improve neurologically intact survival from cardiac arrest. Despite the widespread use of epinephrine and several studies of vasopressin, no placebo-controlled study has shown that any medication or vasopressor given routinely during human cardiac arrest (for any initial arrest rhythm) increases the rate of long-term survival after cardiac arrest. Current evidence in patients with ventricular fibrillation neither supports nor refutes the routine use of intravenous fluids. There is no evidence that any antiarrhythmic drug given routinely during human cardiac arrest increases survival to hospital discharge. There is insufficient evidence to recommend for or against the routine use of fibrinolysis for cardiac arrest. No blood testing is considered routine or standard during the initial stages of cardiopulmonary arrest, although early serum potassium and blood glucose monitoring is prudent if resuscitation is successful. The 2015 resuscitation guidelines recommend continuous waveform capnography for all intubated patients during resuscitation efforts. With advances in ultrasound equipment, properly trained users can portably and accurately monitor cardiac function in real time. Preliminary studies have demonstrated that trained physicians can assess cardiac function and obtain adequate images rapidly by using a subcostal approach to standard echocardiography in the cardiac arrest setting. Use ultrasound during arrest to rapidly diagnose and treat conditions such as cardiac tamponade. Minimize interruptions to perform ultrasound and use it only during resuscitation for specific purposes. Finally, there is ongoing research on the use of transcranial Doppler ultrasound to determine the prognosis after cardiac arrest. One preliminary study concluded that patients with severely disabling or fatal outcomes could be identified within the first 24 hours with this method. Chest compressions and ventilations appear to be deceptively easy to the newly trained, but in fact they are highly complex skills and are difficult to perform well under stress. Valenzuela T, Roe D, Cretin S, et al: Estimating effectiveness of cardiac arrest interventions: a logistic regression survival model. Wik L, Kramer-Johansen J, Myklebust H, et al: Quality of cardiopulmonary resuscitation during out-of-hospital cardiac arrest. Pytte M, Kramer-Johansen J, Eilevstjonn J, et al: Haemodynamic effects of adrenaline (epinephrine) depend on chest compression quality during cardiopulmonary resuscitation in pigs. Hallstrom A, Cobb L, Johnson E, et al: Cardiopulmonary resuscitation by chest compression alone or with mouth-to-mouth ventilation. Skogvoll E, Wik L: Active compression-decompression cardiopulmonary resuscitation: a population-based, prospective randomized clinical trial in out-of-hospital cardiac arrest. Kramer-Johansen J, Myklebust H, Wik L, et al: Quality of out-of-hospital cardiopulmonary resuscitation with real time automated feedback: a prospective interventional study. Krep H, Mamier M, Breil M, et al: Out-of-hospital cardiopulmonary resuscitation with the AutoPulse system: a prospective observational study with a new load-distributing band chest compression device. Forti A, Zilio G, Zanatta P, et al: Full recovery after prolonged cardiac arrest and resuscitation with mechanical chest compression device during helicopter transportation and percutaneous coronary intervention. Nagao K, Kikushima K, Watanabe K, et al: Early induction of hypothermia during cardiac arrest improves neurological outcomes in patients with out-of-hospital cardiac arrest who undergo emergency cardiopulmonary bypass and percutaneous coronary intervention.
Discount nimotop 30 mg online
Reinsertion or placement of a second tube may be indicated if the first tube is not functioning properly muscle relaxer kidney pain cheap 30mg nimotop visa. In general, if a chest tube is not functioning properly and the patient is deteriorating, remove the tube and insert another one. Manipulating the tube by pushing it deeper into the chest cavity can lead to an increased risk for infection. A rare complication of tube thoracostomy is unilateral reexpansion pulmonary edema. The pulmonary edema ranges from mild to severe, but fatalities have been reported. A common factor in these cases seems to be a prolonged period between the development of a pneumothorax and the onset of treatment, but the exact time frame is quite variable. Proposed mechanisms include anoxic damage to the alveolar-capillary basement membrane from prolonged pulmonary collapse, loss of surfactant, or rapid fluid shifts. Reintroduction of air back into the pleural space and temporary occlusion of the ipsilateral pulmonary artery are other suggested, but unproved interventions. Wilson H, Ellsmere J, Tallon J, et al: Occult pneumothorax in the blunt trauma patient: tube thoracostomy or observation Havelock T, Teoh R, Laws d, et al: Pleural procedure and thoracic ultrasound: British Thoracic Society pleural disease guideline 2010. Lichtenstein dA, Meziere G, Biderman P, et al: the lung point: an ultrasound sign specific to pneumothorax. Chambers A, Scarci M: In patients with first episode primary spontaneous pneumothorax, is video-assisted thoracoscopic surgery superior to tube thoracostomy alone in terms of time to resolution of pneumothorax and incidence of recurrence Marimoto T, Fukui T, Koyama H, et al: Optimum strategy for the first episode of primary spontaneous pneumothorax in young men-a decision analysis. Engdahl O, Boe J, Sandstedt S: Intrapleural bupivacaine for analgesia during chest drainage treatment for pneumothorax. Horsley A, Jones L, White J, et al: Efficacy and complications of small-bore, wire-guided chest drains. Niinami H, Tabata M, Takeuchi y, et al: Experimental assessment of the drainage capacity of small Silastic chest drains. Rainer C: Breast deformity in adolescence as a result of pneumothorax drainage during neonatal intensive care. As an example, a 60-year-old man cannot usually mount a sinus tachycardia higher than 160 beats/min in response to sepsis, exercise, fever, anxiety, or adrenergic stimulation. Faster rates would indicate a pathologic cardiac rhythm, not a physiologic response. Tachycardias can be benign or can have significant physical effects on the patient. The pacemaker impulse traverses across and depolarizes the atria, which causes atrial contraction or systole. There may also be an abnormal conduction pathway between the atria and the ventricles. To facilitate the diagnostic process, discrimination between atrial and ventricular electromechanical activity must be attempted. This article provides a framework to facilitate the decision-making process with a focus on emergency interventions for various tachydysrhythmias. Techniques for unmasking, identifying, and treating the various forms of tachyarrhythmias are presented in Box 11. Immediately thereafter, this depolarizing wave accelerates as it travels down the bundle of His to the Purkinje fibers and causes ventricular depolarization and contraction systole. Parasympathetic input to the heart is provided by the vagus nerve (cranial nerve X) fibers. These are usually normal, benign physiologic responses to various stimuli or triggers. These foci may develop as a result of increased irritability or automaticity of atrial myocytes secondary to electrolyte abnormalities, hypoxia, pharmacologic agents, or atrial stretch caused by volumetric overload. If these foci are not treated or suppressed and the atrial depolarization rate proceeds to accelerate to rates greater than 150 beats/min. Treatment of this tachycardia can be achieved pharmacologically by suppressing the automaticity of myocytes with medications. This can lead to an unstable patient with signs and symptoms such as confusion, altered mental status, or persistent chest pain. Reentry describes a condition whereby a depolarization impulse is being propagated down a pathway in which some of the myocytes are still in the effective refractory period and a unidirectional block is present and preventing the impulse from traveling normally down this pathway. However, as the impulse travels around the area of the unidirectional block, the tissue allows the depolarization front to travel in the opposite (antidromic) direction, back to the initial point of entry into this pathway. Sodium influx decreased, calcium influx decreased/potassium efflux still present Phase 4: Steady state. A, Normal depolarization down path 1 and 2 that will "extinguish" or "cancel out" at point 3. As a result, the patient could be treated inappropriately with calcium channel blockers or -blockers, resulting in vasodilation, loss of inotropy, and ultimately cardiac arrest. The clinician must have a means of slowing down and sorting out these physiologic events so that appropriate diagnosis and treatment or intervention decisions can be made. With the application of vagal maneuvers, in some cases the activity of the atria and ventricles may be isolated enough to facilitate a correct diagnosis. An understanding of the underlying pathophysiology will guide appropriate treatment. Adenosine may be used for the same diagnostic purpose in these situations as well. Sinoatrial slowing, which occurs in approximately 75% of cases and leads to sinus arrest approximately 3% of the time. Atrial conduction defects, as manifested by an increase in width of the P wave on the electrocardiogram. Complete asystole, defined as sinus arrest without ventricular escape lasting longer than 3 seconds, which occurs in 4% of cases. Because it shares many characteristics with sick sinus syndrome, it has been suggested that both are manifestations of the same disease. Note the atrial rate slowing from 102 to 88 beats/min whereas the ventricular rate is unaffected. The upper strip resembles atrial flutter or atrial fibrillation with ventricular ectopic beats. The lower strip shows paroxysmal atrial tachycardia with variable block at an atrial rate of 166 beats/min. Prolonged periods of asystole may produce anxiety in physicians waiting for the resumption of a sinus pacemaker. This can guide use and dosage of the medication before initiating treatment with digoxin. Note the obvious flutter waves with an atrial rate of 300 and a long period of ventricular standstill. The patient remained asymptomatic, and a normal sinus rhythm was established spontaneously within a few seconds. If asystole is prolonged, ask the patient to cough vigorously (cough-induced cardiopulmonary resuscitation) or apply a precordial thump. Gentle pressure was applied to the carotid sinus for 3 seconds, which resulted in a pause of approximately 7 seconds in sinus rhythm. Keep a defibrillator/pacemaker at the bedside in anticipation of a worsening dysrhythmia. Administer oxygen for the procedure, especially if conscious sedation is anticipated. The procedure is likely underused by clinicians but should be routinely considered as an initial intervention. It takes advantage of the accessible position of this baroreceptor for diagnostic and therapeutic purposes. Adapted from Braunwald E, editor: Heart disease: a textbook of cardiovascular medicine, ed 6, Philadelphia, 2001, Saunders, p 642.
Discount 30mg nimotop with visa
Scalp veins can be very useful for venous sampling in small infants when other options are not possible or readily available yorkie spasms buy nimotop 30mg on-line. The anatomic considerations and technique are discussed later (see sections on Peripheral Venous Catheterization: Percutaneous and Peripheral Venous Catheterization: Venous Cutdown). Complications Complications of venipuncture include hematoma formation, arterial puncture, local infection, injury to adjacent structures, and phlebitis. Use special care when attempting to puncture the external jugular or femoral vein. Inadvertent deep puncture in the neck can injure the carotid artery, vagus nerve, phrenic nerve, or apex of the lung. The femoral artery or nerve can be injured during puncture of the area around the femoral triangle. Often two people are required-one to hold the arm and insert the needle and the other to aspirate the blood. Arterial blood may be drawn for routine laboratory analysis or blood culture if venous blood is difficult to obtain. Avoid puncture of an artery if the overlying skin is infected, burned, or otherwise damaged. In addition, consider the presence of adequate collateral circulation and any potential coagulation disorders. Equipment and Setup For arterial puncture in infants and children, a small-gauge butterfly needle is preferable to a needle and syringe. Ask an assistant to restrain the infant in a supine position with the head and neck extended over the edge of the bed. Cleanse the skin surrounding the area to be punctured with alcohol or another antiseptic solution. The neck is extended, either over the side of the bed or by placing a rolled towel under the shoulders. Some clinicians prefer to use a 25-gauge needle connected to a syringe, but a butterfly allows better control of the needle while an assistant aspirates the syringe. Technique Potential sites for arterial blood sampling include the radial, brachial, dorsalis pedis, and posterior tibial arteries. The radial artery has several advantages that make it the most commonly used artery for blood sampling. Second, no vein or nerve is immediately adjacent to the radial artery, minimizing the risk of obtaining venous blood or damaging a nerve. Another advantage of the radial artery is the presence of good collateral circulation from the ulnar artery. The brachial artery has little collateral circulation and should be avoided unless an arterial sample is absolutely necessary and no other options are available. As a general rule, do not use the femoral artery for obtaining routine blood samples. Because the radial artery is used most frequently to obtain percutaneous arterial blood samples, the technique for radial artery puncture will be described. Apply pressure for a minimum of 5 minutes after the procedure and monitor for bleeding. Radial Arterial Blood Sampling Median nerve Radial artery Ulnar artery Ulnar nerve Palm A the radial artery is preferred for sampling procedures. Its superficial location is easy to palpate and puncture, and there are no immediately adjacent nerves or veins that may be injured or accidentally punctured. These lines are used to provide fluids for resuscitation and maintenance needs and for the administration of medications. Select the appropriate gauge and length of the catheter based on the size of the child and the clinical situation. In general, use the smallest-gauge catheter that is appropriate for the clinical situation. Attach T-connector extension tubing to the catheter after insertion to facilitate blood collection. An arm or leg board appropriate for the size of the child provides stabilization of the extremity after insertion. Macrodrip tubing and liter bags are inappropriate for use in infants because they can result in the inadvertent infusion of large amounts of fluid. An infusion pump is an ideal way of limiting fluid infusion while keeping the vein open. Vein Imaging Devices A variety of imaging modalities, including ultrasound, transillumination, and infrared technologies, can be used to help locate peripheral veins for cannulation. In adults, data support the use of ultrasound to facilitate peripheral vein cannulation in those with difficult access. Theoretically, knowledge of the location of the venous valves and the course of the vessel can assist the clinician in selecting the best area to be cannulated. If the needle has traversed both walls of the artery, blood will be obtained as the needle is slowly withdrawn into the arterial lumen. Do not overextend the wrist because this can cause loss of the arterial pulse during palpation. Make a small indentation in the skin with a fingernail to mark the insertion site. The topical anesthetic options discussed previously may be used if the clinical situation permits. In contrast to performing the procedure in adults, provide continuous, but gentle suction with the plunger of the syringe in infants. Pulsating or rapidly flowing blood that appears in the hub of the needle is a good indication that the radial artery has been punctured. Some clinicians prefer to attach the syringe to the butterfly needle only after blood return is noted. If resistance is met while pushing the needle deeper, withdraw the needle slowly because both walls of the artery may have been punctured, but the tip may reenter the lumen on withdrawal. If no blood returns, withdraw the needle slowly to the point at which only the distal tip of the needle remains beneath the skin. Repeat the procedure after checking the location of the pulse and reorienting the needle. After the desired amount of blood is obtained, remove the needle and apply pressure for 5 minutes or longer to prevent hematoma formation. Complications Complications of radial artery puncture include infection, hematoma, arterial spasm, tendon injury, and nerve damage. The veins on the dorsum of the hand are relatively straight and are easily stabilized because they lie flat on the metacarpals. Veins in the antecubital fossa (cephalic and basilic veins) are easily accessible; however, the angulation across the fossa makes advancement of the catheter difficult. Tributaries of the dorsal venous arch on the dorsum of the foot, like those on the dorsum of the hand, are relatively straight, and the extremity is easily immobilized after insertion. Because indwelling catheters in this location prevent mobility, consider using this site only in preambulatory patients or after attempts at other sites have been unsuccessful. The scalp veins are easy to cannulate, but their use is primarily limited to small infants. The particular site is a matter of preference, so choose the vein that appears to be the easiest to cannulate. If an extremity location is chosen, place a tourniquet proximal to the planned site of insertion. After 1 ml of saline has been flushed through the line, inspect the site for swelling, which may indicate infiltration. If an artery is entered during placement of the needle and fluid is infused, blanching will occur in the area.
Purchase genuine nimotop on line
Injuries to health care personnel during cardioversion or defibrillation include mild shock and burns spasms in intestines nimotop 30mg sale. Patient complications are dose related and may involve the airway, heart, or chest wall, or they may be psychological. Hypoxia may develop in patients if sedation is excessive or the airway becomes compromised. Chest wall burns resulting from electrical arcing are generally superficial partial-thickness burns, although deep partialthickness burns have occurred. Paddles should not be placed over medication patches or ointments, especially those containing nitroglycerin, because electrical discharge may cause ignition and result in chest burns. In the moderate energy levels used most commonly, the hemodynamic effects are small. At higher energy levels, however, complications include dysrhythmias, hypotension, and rarely, pulmonary edema, which may occur several hours after the countershock. Pediatric Cardioversion Pediatric cardioversion is similar to adult cardioversion. However, the energy levels for pediatric cardioversion are different from those for adults. If needed, repeated cardioversion may be attempted at 2 J/kg, again while the defibrillator is in the synchronized mode. Remember to resynchronize the defibrillator after each cardioversion attempt and look for the appropriate markers on the monitor to ensure that the current is delivered at the appropriate phase of the cardiac cycle. If medication is needed, amiodarone at a dose of 5 mg/kg intravenously over a 60-minute period or procainamide at a dose of 15 mg/kg over a 60-minute period can be used (do not give these drugs together). Holmberg M, Holmberg S, Herlitz J: Incidence, duration and survival of ventricular fibrillation in out-of-hospital cardiac arrest patients in Sweden. International Liaison Committee on Resuscitation: 2005 International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Nanson J, Elcock D, Williams M, et al: Do physiologic changes in pregnancy change defibrillation energy requirements Wu D, Amat-y-leon F, Denes P, et al: Demonstration of sustained sinus and atrial re-entry as a mechanism of paroxysmal supraventricular tachycardia. Kuisma M, Suominen P, Korpela R: Paediatric out-of-hospital cardiac arrests: epidemiology and outcome. Waldecker B, Brugada P, Zehender M, et al: Dysrhythmias after directcurrent cardioversion. Fortunately, the increased reliability of these devices has precluded a marked increase in patients with true emergencies related to device malfunction, but such patients clearly have serious underlying medical problems that must be considered. These devices are complicated and emergency physicians are not expected to be experts in all complications; therefore appropriate consultation is often necessary depending on the clinical situation. The pulse generator is hermetically sealed with a lithium-based battery device that weighs approximately 30 g and has an anticipated lifetime of 7 to 12 years. The generator is connected to sensing and pacing electrodes that are inserted into various locations in the heart, depending on the configuration of the pacemaker. Newer models are programmable for rate, output, sensitivity, refractory period, and modes of response. Pacemakers are classified according to a standard five-letter code developed by the North American Society of Pacing and Electrophysiology/British Pacing and Electrophysiology Group (Table 13. In normal practice, only the first three letters are used to describe the pacemaker. The terminal electrodes, which may be unipolar or bipolar, travel from the generator unit to the heart via the venous system. In a unipolar system, the lead electrode functions as the negatively charged cathode, and the pulse generator case acts as the positively charged anode into which electrons flow to complete the circuit. The pulse generator casing must remain in contact with tissue and be uninsulated for pacing to occur. The cathode is at the tip of the lead, and the anode is a ring electrode roughly 2 cm proximal to the tip. Bipolar leads are thicker, draw more current than unipolar leads, and are commonly preferred because of several advantages, including a decreased likelihood of pacer inhibition as a result of extraneous signals, and decreased susceptibility to interference by electromagnetic fields. The typical entry point for inserting the leads is the central venous system, which is generally accessed via the subclavian or cephalic vein. The terminal electrodes are placed either in the right ventricle or in both the right ventricle and the atrium under fluoroscopic guidance. When the battery is low, the rate generally begins to drop and gets slower as the battery fades. The pacing electrical stimulus is a triphasic wave consisting of an intrinsic deflection, far-field potential, and an injury current, which typically delivers a current of 0. Pacemakers have a reed switch that may be closed by placing a magnet over the generator externally on the chest wall; this inactivates the sensing mechanism of the pacemaker, which then reverts to an asynchronous rate termed the magnet rate. Several innovations in rate regulation have been incorporated into some pacemakers. When present, the hysteresis feature causes pacing to be triggered at a rate greater than the intrinsic heart rate. To illustrate, were the hysteresis feature of the pacemaker set at 50 beats/min, an intrinsic rate lower than 50 beats/min would trigger ventricular pacing. Unlike a standard ventricular pacemaker, the hysteresis feature might be set to offer a ventricular pacing rate at 70 beats/min or greater once the pacer is triggered. Rate modulation by sensor-mediated methods is an additional feature triggered and mediated by a sensed response to various physiologic stimuli. The primary application for this rate modulation feature is in patients with pacemakers who continue to engage in vigorous physical activity. Many transvenous systems consist of a single lead containing a distal sensing electrode and one or more defibrillation electrodes in the right atrium and ventricle. The left side is preferred because of a smoother venous route to the heart and a more favorable shocking vector. It has voltage converters and resistors, capacitors to store charge, microprocessors and integrated circuits to control analysis of the rhythm and delivery of therapy, memory chips to store electrographic data, and a telemetry module. This energy is high enough that a discharge is very obvious and often distressing to the patient. They often have difficulty identifying atrial arrhythmias, which can result in inappropriate defibrillation of atrial tachycardias. In most studies, dual devices have been found to offer improved discrimination between ventricular and supraventricular arrhythmias, thus decreasing inappropriate shocks as a result of rapid supraventricular rhythms or physiologic sinus tachycardia. The advent of technology has allowed placement of a single device that can perform both pacemaker and defibrillator functions. They are programmed with specific algorithms that identify and treat specific rhythms. Ventricular arrhythmias may initially be converted (or undergo attempts at conversion) with antitachycardiac pacing as opposed to immediate defibrillation. This overdrive pacing may terminate the rhythm without the need for electrical defibrillation in up to 90% of events. It is most successful for terminating monomorphic ventricular tachycardia with a rate of less than 200 beats/min. Overdrive pacing is better tolerated by patients than cardioversion and reduces the risk for inducing atrial fibrillation. These events may be silent, not felt by the patient, and discovered only by interrogating the device. This works best for ventricular rates higher than 150 and lower than 240 beats/min. Traditionally, the energy level of the first shock is set at least 10 J above the threshold of the last defibrillation measured. If the first shock fails a backup shock may be required, but this may induce or aggravate ventricular arrhythmias (see the later section on Pacemaker-Mediated Tachycardia). Unlike the proarrhythmic effects of medication, these arrhythmias are almost never fatal, although they may be associated with increased morbidity. There are three leads-the first is positioned in the right atrium, the second is in the right ventricular apex, and the third courses posteriorly in the coronary sinus and into the posterolateral cardiac vein. B1, the ventricular lead is passing through an atrial septal defect into the left ventricle. C, A dual-chamber implantable cardioverter-defibrillator with active fixation leads has been implanted via a transvenous approach to place the atrial lead in the systemic venous atrium and the ventricular lead across the baffle into the morphologic left ventricle.