Buy cialis jelly 20 mg lowest price
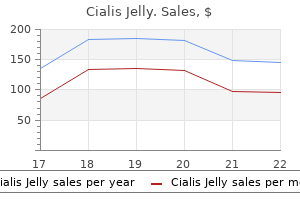
There were no cases of recurrence in the neck when the primary site remained controlled erectile dysfunction icd 9 code 2013 buy generic cialis jelly 20mg on line. All patients who had more than two positive nodes had recurrence either at the primary site or distant metastasis. The most recent guidelines published by the American Thyroid Association state that "prophylactic central-compartment neck dissection (ipsilateral or bilateral) may be performed in patients with papillary thyroid carcinoma with clinically uninvolved central neck lymph nodes, especially for advanced primary tumors (T3 orT4r (103). The overall recurrence rates observed in the dissected side of the neck at 2 years, with the primary tumor under control, was 3. Extracapsular extension of the tumor was present pathologically in 36 patients (34. The dissection was extended to include the prevertebral muscles in only 3% of the cases. The muscles deep to the sternocleidomastoid that may be involved by a tumor are the splenius capitis, the levator scapulae, and the semispinalis capitis muscles. Involvement of these muscles occurs most commonly just lateral to the carotid artery. This is followed distantly by the sympathetic chain (8%), the lingual nerve (7%), the vagus nerve (4%), the superior laryngeal nerve (3%), the phrenic nerve (3%), and the glossopharyngeal nerve (2%) (111). When a nerve is resected, it is advisable to obtain an intraoperative frozen section of the margin of resection even if the appearance of the nerve is normal; perineural tumor spread is initially axial and may not result in thickening of the nerve until late (112). Skin, Musdes, Nerves In a review of 106 cases of extended neck dissections, the largest review on record in the literature, involvement of the skin occurred in 18% of cases (111). Involvement of muscles requiring extension of the neck dissection may affect superficial, prevertebral, and paraspinal muscles. The superficial group is composed of the strap muscles (sternohyoid, sternothyroid, and omohyoid), the mylohyoid, and the digastric/stylohyoid muscle complex. Removal of one or more of these muscles was the reason for extending neck dissections in as many as 62% of the cases studied by Carew and Spiro (111), the digastric muscle being among the structures sacrificed in 51% of cases. This fat pad extends from about the level of the carotid bifurcation to just below the skull base. They are contained within a sliver of fatty tissue located immediately medial to the internal carotid artery. Clinically, involvement of the retropharyngeal nodes by the tumor may be signaled by pain and stiffness in the neck. More ominous and characteristic is an ipsilateral occipitoparietal headache described by the patient as pain located behind the eye. Also ominous is the presence of a Homer syndrome that results from tumor involvement of the cervical sympathetic trunk. Dissection of the retropharyngeal nodes can be performed separately or in continuity with the resection of the primary tumor. When it is done electively, this operation is relatively simple and it takes only a few minutes. The proximity of the nodes to the internal carotid artery and prevertebral structures is such that these structures may be involved as soon as tumor extends beyond the capsule of the lymph nodes. The technique of retropharyngeal node dissection has been described in detail by Vasan and Medina (7). The highest incidence was seen in patients with cancer of the nasopharynx (74%) and the pharyngeal walls (19%). Fourteen of these patients had hypopharyngeal cane~ and the posterior pharyngeal wall was involved in 57% of them. Based on the anatomy of the lymphatic drainage of the different laryngeal sites and on the pertinent clinical observations described in the literature. Treatment/dissection in these cases should include the pretracheal and the paratracheal nodes on both sides. Advanced (T3-T4) glottic carcinomas particularly those with involvement of the anterior commissure and with subglottic extension. In tumors confined to one side of the larynx, treatment/dissection should include the prelaryngeal, pretracheal, and the ipsilateral paratracheal nodes. In tumors involving both sides of the larynx, treatment should include the paratracheal nodes on both sides. Advanced (T3-T4) supraglottic carcinomas, particularly those with involvement of the ventricle/ paraglottic space. In tumors confined to one side of the larynx, treatment/ dissection should include the prelaryngeal, pretracheal, and the ipsilateral paratracheal nodes. In these situations, a neck dissection may need to be extended include the paratracheal and pretracheal lymph nodes; failure to do so may predispose to the development of peristomal recurrence. In addition, lymph node metastases from thyroid carcinomas tend to occur first in the paratracheal nodes regardless of the location of the primary within the thyroid gland (119). Initial reports on carotid artery resection showed very poor results, with approximately 50% of patients suffering either a severe stroke or death. Recent reports have shown a decrease in these events to approximately 25%, with modest improvement in survival compared to those who did not undergo resection. In most patients (70%), the carotid was reconstructed with a vein graft, especially if there was insufficient collateral cerebral circulation. In their more recent cases, the carotid was permanently occluded preoperatively when possible. The mean 1-year disease-free survival rates reported in the literature after resection and reconstruction of the carotid vary between 0% and 44% (121). When considering resection of the carotid the surgeon must make critical preoperative, intraoperative, and postoperative decisions. Preoperative evaluation of these patients requires a clear understanding of the methods available for assessment of the cerebral circulation. Several tests are available that involve occlusion of the carotid artery with either digital pressure (Matas test) or using a balloon during arteriography. The objective of each method is to determine a "critical point" that indicates when reconstruction of the artery is necessary. With the transcranial color Doppler method, the "critical point" is reverse flow from the external carotid artery to the internal carotid. Another method uses Xenon in an aerosolized mixture that is inhaled by the patient. Xenon is concentrated in areas of the brain that are well perfused, correlating with blood flow. Two cr scans are obtained to assess cerebral blood flow: the first one during balloon occlusion and the second after the balloon is released. The "critical point" is a 50% attenuation of the somatosensoryevoked cortical potential in relation to the preoperative exam. Finally, stump pressure measurements can be taken during angiography to determine the pressure on the distal side of the balloon when it is occluded. There is significant individual variability with this measurement, as it is affected by systemic blood pressure. Intraoperatively, patients with frank involvement of the carotid wall whose preoperative evaluation indicates intolerance to carotid ligation should have the carotid reconstructed. Saphenous vein grafts are preferred over prosthetic grafts for reconstruction, and if the skin has been heavily radiated or a portion of skin over the carotid is resected, an appropriate flap should be used to cover the graft. There is still considerable debate regarding the routine use of intraoperative shunts, and to date, there has not been a prospective study to prove their usefulness. However, shunting is clearly indicated when there is angiographic evidence of inadequate flow through the circle of Willis. Postoperatively, delayed strokes can occur in as many as 25% of patients who have undergone carotid artery resection without reconstruction, even if they "passed. Flow from the contralateral side through the circle of Willis prevents a stroke initially. However, the resection creates an arterial stump that begins at the takeoff of the middle cerebral artery and continues down to the level of the resection. This can be a site for thrombus formation, which can then propagate up into the circle of Willis. Alternatively, the thrombus may produce emboli that can travel into the distribution of the middle cerebral artery.
Syndromes
- Retropharyngeal abscess
- Other conditions that suppress or weaken your immune system
- Podiatrist
- American College of Allergy, Asthma and Immunology - www.acaai.org
- You are not sure whether you or your child should receive the HPV vaccine
- Fainting or feeling light-headed
- Breastfeeding females 14-18 years: 600 mcg/day
- Industrial accidents from falling asleep on the job
Cheap cialis jelly 20 mg free shipping
Comparison between minimally invasive video-assisted thyroidectomy and ronventional thyroidectomy: a prospectm: randomized study does erectile dysfunction get worse with age 20mg cialis jelly. Local recurrence in papillary thyroid carcinoma: is extent of surgical resection important Papillary thyroid carcinoma managed at the Mayo Clinicduringsixdecades (1940-1999): temporal trends in initial therapy and long-term outrome in 2444 consecutively treated patients. The effects of surgery, radioiodine, and external radiation therapy on the clinical outrome of patients with differentiated thyroid carcinoma. Outrome after treatment of high-risk papillary and non-Hurthle-cell follicular thyroid carcinoma. Radioiodine ablation of thyroid remnants after preparation with recombinant human thyrotropin in differentiated thyroid carcinoma: results of an international, randomized, controlled study. Effects of low-iodide diet on postsurgical radioiodine ablation therapy in patients with differentiated thyroid carcinoma. Management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Outromes of patients with differentiated thyroid carcinoma following initial therapy. Management of brain metastases from thyroid carcinoma: a study of 16 pathologically ronfirmed cases over 25 years. Prognostic factors and the dfect of treatment with radioactive iodine and external beam radiation on patients with differentiated thyroid cancer seen at a single institution over 40 years. Vandetanib for the treatment of patients with locally advanced or metastatic hereditary medullary thyroid cancer. Recombinant human thyrotropin-stimulated serum thyroglobulin combined with neck ultrasonography has the highest sensitivity in monitoring differentiated thyroid carcinoma. Clinical usefulness of positron emission tomography-computed tomography in recurrent thyroid carcinoma. Effects of thyroid hormone suppression therapy on adverse clinical outromes in thyroid cancer. Diagnostic follow-up of well-differentiated thyroid carcinoma: historical perspective and current status. Real-time prognosis for metastatic thyroid carcinoma based on 2-[l8F]fluoro-2~e oxy-D-glucose-positron emission tomography scanning. The importance of preoperative laryngoscopy in patients undergoing thyroidectomy: voice, vocal rord function, and the preoperative detection of invasive thyroid malignancy. Prognostic factors in well-differentiated follirular-derived carcinoma and medullary thyroid carcinoma. Approach and safety of comprehensive central compartment dissection in patients with recurrent papillary thyroid carcinoma. Prognosticindicators of outcomes in patients with distant metastases from differentiated thyroid carcinoma. A National Cancer Data Base report on 53,856 cases of thyroid carcinoma treated in the U. The incidence of primary hyperparathyroidism in the United States is approximately 100,000 patients per year. Appropriate management of these patients with hyperparathyroidism requires a thorough understanding of the pathogenesis as well as typical and atypical presentations, knowledge of laboratory tests for proper workup, and interpretation of imaging studies for localization of parathyroid adenomas. Thus, swgical treatment of primary hyperparathyroidism has evolved primarily into minimally invasive single-gland excision. However, bilateral exploration still plays an important role in treatment of secondary and tertiary hyperparathyroidism. This article discusses clinical, laboratory, and radiologic evaluation of the hyperparathyroid patient as well as surgical and postoperative management parathyroid glands. The limited course of the superior glands leads to less variability in location compared to the inferior gland. The inferior parathyroid glands can typically be found inferior, lateral or posterior to the inferior pole of the thyroid, anterior to a plane drawn through the recurrent laryngeal nerve. The superior parathyroid glands are less variable in location, the vast majority of them typically located near the cricothyroid joint, just superior to where the recurrent laryngeal nerve courses medially to enter the larynx. The blood supply to the parathyroid glands is primarily from the inferior thyroid artery, and in some there is contribution from the superior thyroid artery. Approximately 3% to 13o/o of adults have supernumerary glands, and 5% have fewer than four (1). They are usually 2 to 3 mm in width, 1 to 2 mm in thickness, and 4 to 6 mm in length. This calcium-sensing property of parathyroid cells allows for the precise regulation of the extracellular ionized calcium concentration within a narrow range, normally 1. The superior parathyroid glands are derived from the fourth pharyngeal pouch, attach to the posterior surface of the superior or mid portion thyroid and migrate caudally with it. It is important to understand the different causes of elevated P1H in swgical treatment considerations. It predominandy affects those between the ages of 55 and 70 with a female-to-male ratio of2:1. Recent reports &om large series indicate that the etiology is a single parathyroid adenoma in 89% of cases, and hyperplasia or multiple adenomas in the remainder (4). Their cytoplasm is strongly acidophilic; the nucleus is small and uniformly intensely basophilic. These parenchymal cells are arranged in anastomosing chords surrounded by delicate connective tissue septa with abundant capillaries. In addition, renal hydroxylation of vitamin D is impaired leading to hypovitaminosis D. Vitamin D deficiency leads to decreased calcium abso~ption from both the gut and reabso~ption of calcium in the renal tubules. Parathyroid Carcinoma Malignancy of the parathyroid gland is a vecy rare cause of hypeiparathyroidism, representing less than 0. It can rarely ocwrin association with hyperthyroid-jaw bone syndrome Patients with this syndrome are cani. This condition tnJically manifests with extremely high plasma calcium levels, usually greater than 13 mg/dL. While this condition is usually diagnosed at a younger age, it may manifest for the first time in older patients who have not sought medical attention throughout life. It typically has a benign course without the hypercalcemia-induced morbidities and is therefore generally not a surgical disease (15, 16). Musculoskeletal: bone and joint pai~ muscle pain, muscle wealmess, osteopenia, osteoporosis, pseudogout, renal osteodystrophy 2. Gastrointestinal: constipation, peptic ulcers, hearth~ pancreatitis, abdominal pain, nausea 4. Neuropsychiatric: depression, anxiety, confusion, memory loss, impaired thinking or "brain fog" A popular mnemonic for remembering these symptoms is "bones, stones, groans, and psychiatric overtones. Information on use of medications that can cause hypercalcemia should be elicited, specifically thiazide diuretics, lithium, dietary supplemental calcium, and vitamin D. Therefore if the albumin level is low, the plasma calcium should be corrected such that 0. In that setting 24-hour urine for calcium, plasma calcium, serum creatinine and 24-hour urine creatinine levels should be obtained to calculate calcium-creatinine clearance ratio. Some patients may also present with plasma calcium values in the mid to upper normal range but exhibit elevated ionized calcium. In recent yean, a new entity known as normocalcemic hyperparathyroidism has been recognized where calcium level, including ionized calcium, is normal and l! If the calcium level becomes elevated or the PrH level does not correct back down to normal range with vitamin D replacement. The sensitivity of each test varies considerably, depending on the equipment and more importantly how experienced is the individual performing or interpreting the study. In the hands of a highly experienced ultrasonograph~ which can be radiologist, surgeon, or endocrinologist. Generally ultrasound should be able to detect adenomas located dorsal to the esophagus. The limitation of ulttasound is detecting adenomas located rettoesophageally or in 1he mediastinum.
Buy cheap cialis jelly 20mg on line
Wide excision improves the local control impotence drugs buy generic cialis jelly 20mg online, but this is diffirult to perform when dealing with the sinonasal tract. Cranial base surgery may improve the local control of sarcomas of the sinonasal tract. T-cell lymphomas are more common in Asian populations, while B-cell lymphomas are more common in Western populations. The primary sites of occurrence in the sinonasal tract are the maxillary sinus (79%) and nasal cavity (20%) (20). The treatment includes radiation therapy for localized lesions and chemotherapy to prevent systemic recurrence. The biologic behavior is remarkably different in the pediatric and adult populations. Adults suffer frequent relapses, commonly involving the abdomen, and show a 5-year survival rate of around 45%. Distant metastases are often associated with failure to treat with chemotherapy in the primary setting (20). In children, complete remissions are more common, involvement of the gastrointestinal tract is rare, and the 5-year survival rate is close to 75%. Eighty to ninety percent of patients with extramedullary plasmacytoma have involvement of the head and neck region, 40% arise in the sinonasal tract. It tends to spread locally, and can be found in the cervical nodes in less than 25% of the cases. The prognosis is unpredictable, and a variable number of the patients will be diagnosed with multiple myeloma. It is of utmost importance to rule out this diagnosis on the initial presentation. Most of these lesions will respond to radiation therapy in doses of 4,000 to 5,000 cGy administered over 4 to 5 weeks. Metastatic Tumors Metastatic tumors to the sinonasal tract produce symptoms similar to those of primary tumors. More than 100 cases have been reported, metastasizing to the maxillary, ethmoid, frontal, and sphenoid sinus in descending order. The treatment is palliative, using radiation, surgery, or chemotherapy to relieve obstructive and compressive symptoms or pain. This system includes a histologic grading system that differs from the system used for epithelial tumors. Grading is thought to be the most significant prognostic factor in patients with mesenchymal tumors and is based on the number of mitoses, degree of cellularity, amount of stroma, degree of maturation, nuclear pleomorphism, and presence or absence of necrosis. The former is preferred since it provides good access and hemostatic control with less morbidity, and does not contaminate other soft tissues. Tumor invades any of the following: bone of the posterior wall of the max1llary s1nus, subcutaneous t1ssues, floor or med1al. Palliative excision may be considered to alleviate intractable pain, to provide rapid decompression of vital structures, or to debulk a massive lesion, thus freeing the patient from social embarrassment. Surgery as a single treatment modality for malignant tumors of the sinonasal tract has yielded 5-year survival rates from 19% to 86%. Frozen sections must be utilized as the tumor is often removed in a piecemeal fashion. Improvements in functional recovery and long-term survivaL however, are yet to be described. A recent review of 134 patients undergoing endoscopic resection of sinonasal malignancies revealed a 5-year disease-free survival rate 91% and a 59% survival rate for open procedures (21). Rehabilitation after surgical resection may be achieved with a dental prosthesis or reconstructive flaps, such as temporalis muscle flaps with and without the inclusion of cranial bone, pedicled or microvascular free myocutaneous flaps. Flaps are recommended to replace resected skin, to provide support for the orbit or brain, or to isolate the cranial cavity from the upper aerodigestive tract. A total maxillectomy defect should not be obliterated at the initial operation; an open cavity facilitates cleansing and direct visual inspection during the follow-up period. Patients requiring a craniofacial resection, especially those needing an orbital exenteration deserve special consideration, since a recurrence after an adequate craniofacial resection is uniformly lethal. From the functional standpoint, patients require immediate separation of the cranial cavity from the upper aerodigestive tract and support of the brain. The temporalis muscle, however, is often devascularized after an infratemporal fossa dissection or its bulk may be inadequate to obliterate the dead space. Under these circumstances, the maxillectomy cavity may be obliterated with a free microvascular flap, offering immediate palliation and oronasal separation without the need for a prosthesis. Radiation Therapy the response of sinonasal tract tumors to radiation varies with the stage and histology of the tumor. Recent reports indicate that postoperative radiation improves local control but not cause specific or absolute survival (22). Radiation therapy is the primary Rehabilitation the main goals of postsurgical rehabilitation are primary wound healing. Preoperative and postoperative radiation therapy seems to produce similar resulta. Nevertheless, the failure of combination therapy, including swgeiy and radiation, to achie11! The skin lndslon begins benuth the medial aspect of the eyebrow and continues 4 to 5 mm anterior to the medial canthus and over the nasal bone along the deepest portion of the nasomaxlllary groove and following the alar crease. To elCpOse the surgical area, the cheek ftap Is elevated subperiosteally owr the maxilla and around the Infraorbital nerve. The anterior wall of the antrum ls penetrated at the canine fossa using a 4-mm chisel. The nasolaaimal duct is divided and the lacrimal sac is opened and marsupialized (C). The first osar otomy involved in the actual removal extends through the piriform aperture at the level of the nasal floor, directed posteriorly until the osteotomy perforates the posterior wall of the antrum. The orbit is retracted laterally, and a second osteotomy is performed at the frontoethmoid suture, extending posteriorly to a point 2 to 3 mm posterior to the posterior ethmoid artery. E: the thin bone of the medial floor of the orbit is sawed following a line that joins the laairnal fossa with the superior osteotomy. First, a 2-mm osteotome is imroducad through the anterior antrostomy and directed through the medial posar rior amral wall. The osteotome is advanced superiorly to reach the level of the superior osteotome and is then pushed medially. F: Heavy curved scissors are then Introduced with one blade ln the nasal cavity and the other ln the superior osteotomy, directed through or along the posterior attachments of the turbinates. Residual ethmoid mucosa Is removed with ethmoid fora~ps, and a 'lllde sphenoldotomy ls opened wlth Kerrison rongeurs. A transfixion Incision Is performed at the membranous septum and Is extended laterally to Join a transcartllaglnous Incision. C: A glnglvobua:al Incision Is performed, extfandlng laterally from the midline to the maxillary tuberosities. These reports, ho~ are vety limited in nature, including small number of patients, and the studies are usually nonrandomized. Patients who represent a poor surgical risk and those who refuse swge:ry, should be considered for enrollment in protocols that include combinations of radiation and chemotherapy. Tumors extending to the paranasal sinuses, those la~ger than 2 em, and those associated with positive surgical margins have been associated wi1h a poor prognosis for which postoperative radiation should be administered. Maxillary Antrum the maxillaJ:Y sinus is the most common site of origin for malignancies of the sinonasal tract. The management of other epithelial and mesenchymal malignancies was disrussed in the pathology section. A total maxillectomy with preservation of the orbit can be performed using incisions identical to lateral rhinotomy incisions wi1fl a lip-splitting extension. Alternatively, a lateral rhinotomy incision may be c;ombined wi111 an ipsilateral degloving approach. The superior incision begins at the lateral canthus and extends medially, passing 3 to 4 mm below the ciliary line.
Discount 20 mg cialis jelly with mastercard
Squamous cell carcinoma of the trachea is notorious for rapid growth and early regional lymph node metastasis erectile dysfunction causes heart disease purchase cialis jelly amex. Synchronous or metachronous lesions are common (30% to 40%) and occur most frequently in the lung, larynx, and oropharynx, regions where smoking-related neoplasms are also common (45). Adenoid Cystic Carcinoma Adenoid cystic carcinoma arises from the minor salivary gland epithelium within the trachea. One study reviewed 208 patients with tracheal tumors and found that those with adenoid cystic carcinoma had symptoms three times as long as patients with squamous cell carcinoma (29). There is low risk for regional lymph node involvement; however, perineural invasion and hematogenous metastasis are encountered frequently. Hematogenous metastasis occurs in approximately 50% of patients and most commonly involves the lungs (46). Recurrence after definitive primary treatment is common and occurs at an average of 51 months compared to 18 months for other tracheal tumors (29). Chemotherapy the role, either adjunctive or palliative, of chemotherapy in the management of tracheal malignancy is poorly defined. Unlike laryngeal cancer, there are no multicenter clinical trial results that define the role of combined radiation and chemotherapy for organ preservation. In unresectable or certain aggressive neoplasms such as basaloid squamous cancer of the trachea. Squamous cell carcinomas and adenoid cystic carcinomas are the most common, occurring in equal proportions. These two carcinomas have been reported to represent between two-thirds and three-fourths of tracheal neoplasms (6,45). There are numerous additional benign and malignant neoplasms that have been described, and this group of heterogeneous lesions comprises the remaining one-fourth to one-third of tracheal tumors (Table 126. Tracheal tumors occur equally among men and women; however, squamous cell carcinoma affects men at least twice as often as women. A history of smoking tobacco is associated with squamous cell carcinom~ but not with adenoid cystic carcinoma. Secondary Tracheal Tumors Tumors from adjacent structures can invade the cervical or thoracic trachea. Cervical trachea invasion can occur from well-differentiated thyroid carcinoma, anaplastic thyroid carcinoma. Although death from thyroid cancer is the exception rather than the rule, when it does occur, tracheal invasion with airway obstruction and bleeding is the cause over 50% of the time (47). Invasion is often identified at the time of thyroidectomy unless luminal invasion has occurred with resulting airway symptoms. Management of tracheal invasion from thyroid carcinoma depends on the extent of invasion, histology, and patient-related factors. Early invasion can be addressed by shaving the tumor from the trachea with the expectation that adjuvant radiotherapy will be given postoperatively. Although controversial, tracheal resection with primary reanastamosis is also an option especially in advanced cases of invasion with intraluminal involvement and may offer more robust disease control (48). Invasion of the trachea or carina can occur from direct extension of a bronchogenic lung cancer. Resection is recommended if there is no regional lymph node involvement or distant metastasis. Tracheal invasion from esophageal carcinoma or metastatic lymph node disease should be considered unresectable, and nonsurgical therapy and palliation is recommended. Squamous Cell Carcinoma this very aggressive epithelial malignancy can be ulcerative or exophytic. Arising from the surface respiratory epithelium, squamous cell carcinomas can occur throughout the entire trachea, and have been known to invade surrounding Chapter 126: Tracheal Tumors 1997 Metastatic Tumors Metastatic tumors of the trachea have been reported and are most commonly from breast cancer, colon cancer, and cutaneous melanoma. Metastasis from renal cell carcinomas, adrenal gland tumors, and testicular cancers has also been described. As with any metastatic disease, prognosis is poo~ and palliative treatment is recommended. Primary tracheal tumors of the neck and mediastinum: resection and reronstruction procedures. Undertreatment of tracheal carcinoma: multidisciplinary audit of epidemiologic data. Primary tracheal tumours: 21 yean of experience at Peking Union Medical College, Beijing. Long-term survival after resection of primary adenoid cystic and squamous cell carcinoma of the trachea and carina. Thmoral and non-tumoral trachea stenoses: evaluation with three-dimensional cr and virtual bronchoscopy. Tracheal and cricotracheal resection fur laryngotracheal stenosis: experience in 54 consecutive cases. Pathologic characteristics of resected squamous cell carcinoma of the trachea: prognostic factors based on an analysis of 59 cases. The long-term outcome and prognostic analysis of surgically treated patients with trachea tumors. Tracheal reconstruction with the use ofradial forearm free flap combined with biodegradative mesh suspension. Squamous cell carcinoma is the predominant histopathology and is aggressive with frequent nodal metastasis. A myriad group of tumors may present in the trachea, which makes accurate biopsy and diagnosis of paramount importance prior to instituting treatment. Treatment of locally advanced adenoid cystic carcinoma of the trachea with neutron radiotherapy. The role of postoperative external-beam radiotherapy in the management of patients with papillary thyroid cancer invading the trachea. Unresectable basaloid squamous cell carcinoma of the trachea treated with concurrent chemoradiotherapy: a case report with review of literanrre. Results and prognostic factors in resections of primary tracheal tumors: a multicenter retrollpective study. Therapeutic bronchoscopy for malignant airway stenoses: choice of modality and survival. Treatment of tracheal and bronchial tumors and tracheal and bronchial stent placement. Management oftracheal obstruction caused by benign or malignant thyroid disease using covered retrievable self-expandable nitinol stents. Prognostic value of pathologic characteristics and resection margins in tracheal adenoid cystic carcinoma. Adenoid cystic carcinoma of trachea treated with adjuvant hypofractionated tomotherapy. Mark Persky Spiros Manolidis Vascular tumors of the head and neck consist of a variety of different entities that are unrelated to each other. This article focuses on acquired vascular tumors that present vexing clinical problems. Based on Batsakis classification of vascular tumors, a differentiation can be made: tumors that are congenital and/or arise on behalf of syndromes and those that are acquired (Table 127. They contain cells that are capable of secreting neuropeptides that have the capability to influence vascular reflexes. These structures are part of the diffuse neuroendocrine system that are derived from neural crest origin cells. Neural crest derivatives, produce the C cell of the thyroid gland, the melanocyte, and the paraganglia. Paraganglia are found in the adrenal medulla or diffusely distributed as the extraadrenal paraganglia (1,2). The latt~ the diffusely distributed extra-adrenal paraganglia are divided into branchiomeric paraganglia and vagal paraganglia. The branchiomeric paraganglia are distributed along arteries and cranial nerves in the head and neck. The jugulotympanic paraganglia arise from the second branchial arch while the carotid paraganglia arise from the third branchial arch. The intravagal paraganglia do not follow this embryologic pharyngeal pouch distribution and are thus classified separately. The carotid body is a chemoreceptor that senses changes in arterial oxygen pressure, pH, and catbon dioxide.
Discount cialis jelly 20 mg mastercard
Fluctuations in hearing may occur impotence at 30 years old purchase cialis jelly toronto, but the overall course is one of a relentless deterioration in auditory function. Approximately 50% of patients have symptoms of vestibular dysfunction, with 20% of patients experiencing episodes of vertigo consistent with those seen in Meniere disease (34). Sudden hearing loss is an otologic emergency with a treatment window of perhaps 2 to 4 weeks, during which a short burst and taper of corticosteroids are recommended to achieve optimal recovery. Tests of cellular immunity have been advocated by McCabe (lymphocyte migration inhibition assay) and Hughes Chapter 156: Otologic Manifestations of Systemic Disease: Includes Autoimmune Inner Ear Disease 2525 (lymphocyte transformation test) (49). Unfortunately, these tests have never been adequately validated, and their diagnostic accuracy has not been determined. In a prospective controlled study, with well-defined entry criteria, Moscicki and his colleagues demonstrated that 89% of patients with active, rapidly progressive hearing loss did have detectable levels of this antibody, while none of the control patients had positive Western blots (53). Initial therapy for adults consists of a therapeutic trial of prednisone (60 mg daily for 4 weeks). Although patients may occasionally respond early in the 4-week period, many do not begin to improve until late in the month; shorter courses of treatment usually result in relapse. If the threshold has improved by ~15 dB at one frequency or 10 dB at two or more consecutive frequencies, or if the discrimination is significantly improved, patients are considered steroid responders. Responders continue full-dose therapy until monthly audiograms confirm that they have reached a plateau of recovery. Their medication is then slowly tapered over 8 weeks to a maintenance dose of 10 to 20 mg every other day. Clinical observation suggests that patients with a treatment duration of fewer than 6 months are at increased risk of relapse compared with those treated for 6 months or longer. Some patients have improvement in threshold, some in discrimination only, and some in both areas. Some patients with hearing loss fluctuation and progression before therapy show stabilization in their hearing without actual improvement. Historically, these cases have been considered nonresponders, but this issue is currently under reassessment. The majority of responders slowly taper off the steroid dose, wean from steroids, and do well. Some patients, especially in the pediatric age group, may occasionally show steroid-dependent hearing loss. In other words, they cannot be weaned below a certain level of steroid dosage without decline in hearing. Such patients often develop unacceptable side effects of chronic steroid administration. Methotrexate has been used as part of a prednisone-sparing regimen; howev~ a recent randomized, prospective controlled, multicenter trial has shown methotrexate to be no better than a placebo at maintaining a remission in these patients (56). Longterm administration carries a significant risk for gastritis and ulcers, fluid retention and weight gain, blood pressure lability, altered blood sugar metabolism and diabetes, avascular necrosis of the hip, mood changes or psychiatric problems, sleep disturbance, accelerated cataract formation. Although high-dose corticosteroids are associated with serious side effects, with appropriate patient selection, monitoring, and patient education. A number of alternatives to systemic corticosteroids have been proposed, including methotrexate, etanercept, and cyclophosphamide. Low-dose methotrexate appeared to be useful as an adjunct in management of steroiddependent hearing loss (60). Howev~ as noted earlier in this chapter, the recent large trial indicates that it may not serve an effective role as a prednisone-sparing drug. Anecdotally, it appears to work well in combination with methotrexate because of its steroid-sparing effect. As seen in rheumatoid arthritis, etanercept alone does not appear nearly as effective. Toxicity includes severe myelosuppression, opportunistic infection, hair loss, cystitis, infertility, and increased risk of malignancies. Many patients, when confronted with the risk of this medication, would rather consider cochlear implantation. Intratympanic steroid therapy is particularly appealing because it is minimally invasive and enables direct application of the drug to the affected site with low risk of systemic effects (67). There are, however, no published series in which these treatments have been systematically applied. All other immunosuppressants currently employed have not been systematically evaluated and carry with them serious toxicity risks. In a patient who cannot be maintained on corticosteroids because of complications, the possibility of withdrawing treatment, with the intention of inserting a cochlear implant when the hearing becomes significantly impaired, must be considered. Radiologic findings for these patients include thickening of the calvarium with ill-defined densities and poor definition of cortical margins of the inner ear and internal auditory meatus. The conductive portion of this hearing loss is typically down-sloping and 20 to 30 dB in severity. The etiology of this hearing loss is not well explained and cannot be attributed to compressive etiologies as with other diseases of bone. It is believed to arise primarily from changes in bone density and geometry that interfere with normal hearing mechanisms. In addition, patients with Paget can present with tinnitus and mild vestibular complaints. Treatment of Paget disease relies primarily on bisphosphonate therapy, which inhibits osteoclast activity, thereby inhibiting bone reabsorption. There are no surgical treatments to improve conductive hearing loss for these patients. Osteogenesislmperfecta Osteogenesis imperfecta (01), also known as Hoeve-de Kleyn syndrome, is a connective tissue disorder that manifests as a variety of types with vastly differing severity. Type I 01 is the mildest form of the disease and is inherited in an autosomal dominant pattern. This is the classic form of the disease and is the most common type, with an incidence of 1:30,000. It is inherited in an autosomal recessive pattern and has an incidence about half that of type I, 1:60,000. They also demonstrate blue sclera at a young age but this transitions to a normal white sclera later in life. There is no demonstrated association between the severity of peripheral fractures and the presence of hearing loss. Conductive hearing loss results from fractures to the ossicles, most commonly the long process of the incus or the stapes crura. It results from increased activity of osteoclasts and osteoblasts, which manifest as bony hypertrophy and remodeling. Its prevalence increases dramatically with age, with 3% of people over the age of 40 demonstrating histopathologic evidence of the disease and 11% of people over the age of 80 demonstrating histopathologic evidence of the disease (69). The disease is far more common among men than women with relative incidence of about 4:1. Patients with Paget disease typically present in their sixth decade, most commonly with complaints of an enlarging skull, progressive kyphosis, Chapter 156: Otologic Manifestations of Systemic Disease: Includes Autoimmune Inner Ear Disease 2527 loss has been addressed successfully with amplification or ossiculoplasty to replace fractured ossicles. In addition, stapedectomy can be effective but must be performed very delicately due to the fragility of the ossides. It describes the replacement of normal cancellous bone by spicules of woven bone in a fibrous stroma. The affected bone is most commonly a rib, the skull, the proximal femur, or the tibia. The polyostotic form usually presents earlier and will continue to progress throughout life (74). Radiologic findings typical of fibrous dysplasia include radiolucent areas with a well-defined smooth or scalloped edge and a ground-glass appearance. Otologic manifestations of the disease manifest from craniofacial involvement, which occurs far more commonly in the polyostotic (50% to 100%) form than in the monostotic form (10% to 30%). In addition, patients can develop a canal cholesteatoma or involvement of the ossicular chain (75).
Juglans (English Walnut). Cialis Jelly.
- Preventing heart disease when walnuts are eaten.
- What is English Walnut?
- Reducing the risk of heart disease.
- Are there safety concerns?
- Diarrhea, diabetes, anemia, acne, eczema, ulcers, treating swelling (inflammation) of the skin, treating excessive sweating (perspiration) of the hands and feet, and other conditions.
- What other names is English Walnut known by?
- How does English Walnut work?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96167
Order 20mg cialis jelly visa
For secondary orbital lymphomas erectile dysfunction urologist new york order 20mg cialis jelly with amex, systemic treatment with chemotherapy is used alone or in combination with orbital radiotherapy. However, other studies of orbital lymphomas have failed to detect chronic chlamydia infection, and thus suggest a possible geographic distribution of this association (15). As these features may not distinguish these lesions from other pediatric orbital malignancies in cases presenting prior to systemic leukemic involvement biopsy is often required. A greenish appearance of these lesions on biopsy has been reported in up to 70% of cases (hence the term chloroma) and is due to the exposure of myeloperoxidase to ultraviolet light (16). Touch preparations may be performed on the tissue to stain for cytoplasmic esterase (Leder stain) and myeloperoxidase. The exact histogenesis is unclear, but it is thought to result from mononuclear phagocyte dysregulation. Eosinophilic granuloma is the most common and benign entity and is characterized by unilateral, usually solitary, osseous lesions. The intermediate clinical form is called Hand-Schilller-Christian disease and classically presents as the triad of diabetes insipidus, proptosis, and multifocallytic bone lesions. The disease occurs in children and teens, with a peak incidence between 5 and 10 years of age. Orbital involvement occurs in up to 20% of cases, most frequently presenting as a lytic defect of the superolateral orbit (frontal, zygomatic, or greater sphenoid bones), and causing relapsing episodes of superolateral inflammation with eyelid swelling and erythema that may initially mimic infectious orbital cellulitis. Treatment of isolated orbital bone lesions consists of surgical excision, which may be curative. Intralesional steroid injection or low-dose radiotherapy may be used as adjuncts to surgery. Leukemic infiltrates may involve the orbit, and are more common with myelogenous leukemias than lymphocytic ones. Granulocytic sarcoma (chloroma, myeloid sarcoma) is a primary tissue mass form of acute myeloid leukemia. The tumor mass is composed of granulocytic precursor cells with varying degrees of differentiation. These lesions may occur prior to the development of systemic leukemia in up to 88% of cases, with systemic involvement usually occurring within 1 year (16). The most common presenting clinical sign is proptosis from a rapidly enlarging mass. Up Chapter 130: Orbital Tumors 2069 to 50% are associated with neurofibromatosis, and may be bilateral in this setting. Eye exam findings include an afferent pupillary defect, optic atrophy, optic nerve edema, and strabismus. Although these tumors are generally self-limited or progress slowly, some show aggressive growth. They may extend along the length of the optic nerve but typically do not invade the adjacent dura. Cystic degeneration can lead to sudden tumor enlargement and subsequent vision loss, but does not represent true tumor growth. Characteristic orbital imaging findings are usually sufficient to establish diagnosis. Fusiform enlargement of the optic nerve is seen, with kinking or tortuosity commonly seen. Close observation is indicated when the tumor remains isolated to the orbit and vision is intact Surgical excision with free margins is indicated in cases of aggressive growth in order to prevent chiasm, contralateral optic nerve. Radiation or chemotherapy can be used to retard growth of lesions already affecting the chiasm. Given its adverse effects on childhood development, chemotherapy is preferred over radiation. Orbital Meningiomas Orbital meningiomas represent up to 4% of all orbital lesions. Primary optic nerve sheath meningiomas are much less common than secondary orbital meningiomas, which arise intracranially and extend to the orbit through the optic canal, superior orbital fissure, or bone (17). Gaze-evoked transient visual obscurations, axial proptosis, and ocular motility restriction are possible. An afferent pupillary defect and visual field disturbance can be detected on exam. Optociliary shunt vessels are visible on fundus exam in up to a third of patients; these oollaterals permit retinal venous outflow through the choroidal circulation and thus bypass central retinal vein obstruction secondary to tumor compression. Secondary meningiomas occur in a slightly older population, typically in the fifth decade of life, and also with a female preponderance. Lesions involving the greater sphenoid wing and lateral orbital wall cause proptosis, temporal fossa swelling. Tumors involving the lesser sphenoid wing may lead to early vision loss and visual field defects due to optic nerve involvement (19). Diagnosis can often be established on the basis of characteristic imaging features. Globular enlargement occurs less frequently and is the result of tumor invasion of the adjacent dura. Contrast-enhanced axial cr often reveals a linear central hypointense optic nerve surrounded medially and laterally by a hyperintense nerve sheath-a well-known finding termed Rtram-tracking. Most meningiomas are histologically benign, with aggressive forms occurring most commonly in younger patients. Surgery is indicated for secondary meningiomas when compression of surrounding structures causes significant visual, cosmetic, or intracranial morbidity. Treatment of primary optic nerve sheath meningiomas is dictated by the degree ofvision loss and the presence of intracranial extension, which occurs in up to 15% of patients. Ifvision loss is progressive, vision function can be improved with radiation therapy. Surgical excision is performed when intracranial extension threatens the optic chiasm or contralateral optic nerve, or when the tumor has caused marked vision loss and significant proptosis (7). Schwannoma (Neurilemoma) Schwannomas are uncommon benign tumors of the peripheral nerve sheath. They arise due to proliferation of the myelin-producing Schwann cells and rarely undergo malignant transformation. They occur most commonly in adults between 20 and 60 years of age and are most often found in the superior or intraconal orbit. They can cause slowly progressive proptosis, and location at the orbital apex may cause progressive vision loss. Histopathologically; these lesions are well-encapsulated and are divided into Antoni A type (solid tissue with spindle cells arranged in whorls or palisades) or Antoni B type (loose myxoid tissue containing stellate cells). Long-standing lesions may demonstrate bony remodeling, lower density areas of mucinous cystic degeneration, and calcification. Treatment consists of complete surgical excision of the tumor and capsule (17-19). It can occur in children and adults, and accounts for up to 11% of all orbital lesions (2). Almost any orbital structure may be involved, including one or more extraocular muscles (orbital myositis), the sclera and posterior tenons (sclerotenonitis), or the optic nerve sheath (inflammatory optic neuritis). Ocular motility restriction, diplopia, proptosis, conjunctival inflammation, and eyelid erythema and edema may also occur. Decreased vision may be seen when the optic nerve, sclera, or posterior tenons are involved. Children often present with systemic signs such as fever, emesis, abdominal pai~ and lethargy. In contrast, bilateral involvement in an adult signals an underlying systemic vasculitis (7). A rapid and dramatic response is typically observed within a few days, and steroids are tapered slowly over several weeks to prevent rebound inflammation. Biopsy may be required in patients with atypical symptoms, imaging features, treatment failure.
Generic cialis jelly 20mg with mastercard
Although fungi may be the primary pathogens erectile dysfunction names best buy for cialis jelly, they are usually superimposed on chronic bacterial infection of the external canal or middle ear. Secondary otomycosis tends to recur if the underlying primary infection is not controlled. Pruritus is the primary clinical complaint the otoscopic examination commonly reveals a white, black, or dotted gray membrane. Thorough cleaning under a microscope with the patient supine to remove any fungal debris is the first and absolutely most important step in therapy. Thorough aural toilet is supplemented by the topical application of an acidifying solution such as aluminum sulfatecalcium acetate (Domeboro) or by a drying powder such as boric add. Metacresyl acetate (Cresylate) may be painted on the margin of a perforation or an infected ventilation tube. This medication should not enter the middle ear cleft because it is quite irritating. In recalcitrant infections, a foreign body such as a ventilation tube acts as the nidus for infection and should be removed. Tympanoplasty is best performed to close a perforation that intermittently drains with a superimposed fungal infection. Gentian violet is usually well tolerated in patients with mastoid cavities, although it is best left out of the middle ear cleft in the presence of a perforation. Because it will permanently stain sldn and clothing, small amounts are used with adequate protection of the surrounding area. Treating physicians should realize that all drops are formulated with moisture and do not persist indefinitely in an homogenized state. Eventually, the water component will separate from the precipitate of the active medical ingredient. In these cases, an acidifying powder such as boric acid or a compounded powder, as described below, will often help dry up a refractory ear. Many patients with refractory otomycotic infections may have had previous mastoid surgery. Due to moderate to severe hearing loss, the patient may need to wear a hearing aid with a closed mold. This is a significant problem because the patient relies on the aid virtually all day and is reluctant to leave the instrument out Careful instruction to the patient. Ointments in cavities with closed hearing aids may promote fungal growth due to the accumulation of moisture. In refractory cases, gentian violet or metacresyl acetate (Cresylate) is used topically. Involvement of the facial nerve may produce paresis or paralysis (herpes zoster oticus or Ramsay Hunt syndrome), named after Dr. Many patients excoriate the blisters, and bacitracin ointment or a suitable substitute should be applied to prevent superinfection. Acyclovir, famciclovir, and valacyclovir have been shown to ameliorate herpetic infections, especially herpes zoster oticus. The latter two have easier dosing schedules and are better absorbed orally than acyclovir. However, it will cause a transitory rise in hepatic enzyme production and must be used with caution. Dermatoses Allergic and irritant contact dermatoses may mimic diffuse external otitis. These result when the susceptible patient comes in contact with any type of agent that can produce a cutaneous response. Irritants may be absolute, so noxious that a reaction occurs in everyone exposed. Allergic contact dermatitis refers to delayed hypersensitivity reactions resulting from substances such as poison ivy, nickel compounds (earrings), and rubber compounds (headphones). The typical reaction presents as erythema, weeping, and vesiculation accompanied by itching. Treatment consists of removal of the causative agent and the use of topical steroids and astringents. Unfortunately, once auricular cartilage has been lost and reparative scarring has begun, the auricle is doomed to reparative malformation. The lesions may be discrete or confluent Although chemotherapy, radiotherapy, and interferon-a have been used for therapy, treatment of auricular and canal lesions is rarely necessary. Sharp Trauma to the Auricle Sharp trauma to the auricle may be as small as a tom ear lobe piercing to complete avulsion of the auricle, usually as a result of motor vehicular trauma. The auricle has a plentiful blood supply and as a general rule will heal if the cartilaginous and soft tissue structures remain even partly attached, less so if complete avulsion has occurred. If remnants or the entire auricle can be salvaged, these should be cleansed and an attempt made to reimplant in the acute situation. Tom lobules may occur by gravity in which a heavy earring works its way over time through the lobule or by acute injury in which an earring is tom through the lobule. The tom lobule may be repaired in the office; the lobule may be repierced at a later stage. Broad-spectrum antibiotic coverage for the most likely oral flora including microaerophilic streptococci and anaerobes such as Bacteroides is indicated. If remnants of the auricle have been salvaged, these may be thoroughly washed, decontaminated and reattached with sutures. If only the auricular cartilage remains, it should be cleaned of soft tissue attachments, decontaminated, and buried in a subcutaneous pocket (postauricular, forearm, abdomen. If part or whole of it appears viable, it is worth an attempt at surgical reattachment. The patient must then be counseled regarding the main steps of auricular reconstruction (costochondral cartilage harvest. Another very good option in these severe cases is the insertion of osseointegrating Traumatic Disorders of the External Ear Blunt Injuries Shearing forces to the auricle. The lobule is composed primarily of fat covered with skin and is less susceptible to injury. If uninfected, a small seroma of the auricle may be observed, a larger one aspirated. If the seroma reaccumulates, it should be treated under sterile conditions with drainage and a bolster type dressing using dental rolls and through-and-throu~ nonabsorbable sutures placed to obliterate the potential space for reaccumulation of the seroma. If infected there is a risk that cartilage itself may become necrotic and lost the ear must be incised and drained with broad-spectrum antibiotic coverage; drains may need to be placed. Because the cartilaginous frame is at greater risk, the hematoma should be drained and a compressive dressing applied with dental rolls sutured on either side. If the hematoma reaccumulates Chapter 146: Diseases oftne External Ear 2347 titanium posts for the anchoring of an aurirular prosthesis. A well-made aurirular prosthetic for the properly selected patient is an excellent option with very acceptable cosmetic results. This type of repair must be chosen carefully with regard to the age and usual activities of the recipient. Thermal Injuries (Thermal Burns, Frostbite) Bums of the auricle are classified by nature of the bum (thermal, ultracooling due to frostbite) and the degree of the injury to the skin: first degree leading to erythema, second degree (blistering), and third degree (full thickness). In first- and second-degree bums, pain is present; in third-degree bums, the sensory nerve endings have been destroyed, and the affected area is anesthetic. It is of great importance to elicit a detailed history about the nature and time course of the injury. Upon inspection, the area may be erythematous and blistered (first- and second-degree bums), blackened with eschar (third degree), or white, hard, and cold (frostbite) due to extreme vasoconstriction. It is important to suspect that the extent of the injury extends greater than that apparent on inspection. Cooling a thermal bum should be done quickly with cold/ iced compresses to waste the built-up heat within the tissue in an attempt to prevent necrosis by cell expansion and disruption. If frostbite extends to larger areas of the body, the patient may be placed in a warming bath or warming intravenous solutions may be used.
Generic 20mg cialis jelly fast delivery
Adequate gastroesophageal reflux preventive measures are initiated in all patients as reflux may impair wound healing erectile dysfunction shake recipe purchase cialis jelly online now, promote granulation tissue formation, and prolong edema. Wound healing is usually complete in 4 to 6 weeks following which voice rehabilitation therapy is scheduled. A small number of patients with persistent granulation or granuloma formation may require a second-look laryngoscopy. Complications: Secondary hemorrhage is rare following resection of glottic tumoiS and can be managed conservatively if minor or with cautecy at microlaryngoscopy. C Postoperative lacyngeal or tongue edema can occur particularly after resection of bulky T2 tumoiJ with supraglottic spread to arytenoids. The aiJway obstruction may necessitate tracheostomy but is frequently managed by administration of intravenous corticosteroids and aerosolized topical vasoconstrictoiS. In certain patients, wound healing elicits a strong inflammatory response and formation of exuberant granulation tissue. If the granulation persists for more than 6 to 12 weeb or is a source of compromised voice quality, surgical removal may be required. Endoscopic laser excision for early glottic tumors does not usually require any reconstruction of the glottic defect as in open conservation swgecy. Howeve:t in Chapter 123: Early Laryngeal Cancer cordectomies requiring vocal muscle excision, poorer voice quality may result due to an aerodynamic glottic insufficiency caused by the concavity of the neocord (81). Subcutaneous emphysema has been reported as one of the complications and can be prevented by pressure dressing and a wound drain. Hemilaryngectomy: this procedure involves resection of the ipsilateral thyroid cartilage, arytenoid, true cord and false cord, underlying muscle, and mucosa from the aryepiglottic fold to the upper border of the cricoid cartilage from the posterior to anterior midline. Frontolateral vertical hemilaryngectomy: the procedure is indicated for T1 cord lesions approaching or extending to the anterior commissure and not more than 1 to 2 mm of the contralateral cord. The thyrotomy incisions are made bilaterally on either side of the midline and the larynx is entered through the cricothyroid membrane. The resection includes true and false cords and ventricle on the ipsilateral side, arytenoid when necessary, anterior commissure, and anterior conttalateral cord. The conttalateral mucosa is sutured to the external perichondrium in order to resurface the larynx. Lcu:yngofissure and cordectomy are indicated for T1 lesions of vocal cord limited to the membranous cord when transoral resection is not possible. An endoscopy is performed prior to the surgery to reevaluate the suitability of the tumor for the procedure. A transverse skin incision is made at the level of midportion of the thyroid cartilage Superior and inferior flaps are raised, strap muscles are retracted, and the thyroid cartilage is exposed in the midline. A midline vertical thyrotomy is performed and the larynx is entered through a short incision in the cricothyroid membrane. The thyroid ala is retracted laterally and the anterior ends of vocal folds are separated in the midline at the anterior commissure. The resection can include the true and false cords anterior to the vocal process of arytenoid, underlying thyroarytenoid muscle. The anterior commissure is reconstructed by anchoring the anterior end of the uninvolved cord to the thyroid lamina. The vertical midline portion of the thyroid cartilage, inner perichondrium, true cord, false cord, and ventricle up to the vocal process, bilaterally, are included in the resection. Reconstruction is performed by silastic or keel insertion to allow epithelialization on either side without web formation. Reconstruction after partial laryngectomy: the glottic defect from open partial laryngectomy procedures may result in unsatisfactory voice outcomes. Resurfacing and reconstruction of the glottic defect enable better ftmctional restoration. Several techniques are described of which more commonly applied are strap muscle llaps. Mucosal llaps, external thyroid perichondrium flap, a muscle-based cartilage flap, or imbrication laryngoplasty are alternatives. Postoperative cam: Care of the tracheostomy tube to maintain a patent airway is important in patients undergoing vertical hemilacyngectomy. Complications: Airway obstruction after vertical hemilaryngectomy from prolapse of supraglottic tissue or formation of excessive granulation tissue is managed by maintenance of the tracheostomy. Progression to glottic stenosis is a possible complication in postradiation cases, which may need to be addressed by surgical intervention. Dysphagia and aspiration may occur in immediate postoperative period, particularly in patients with arytenoid resection. In a study of 438 patients comparing outcomes for different surgical approaches, a lower complication rate of 1. T stage, anterior commissure involvement, and epidermal growth factor receptor expression are correlated with poorer local control in early glottic cancer (84). In addition, overall treatment time greater than 50 days and total dose less than or equal to 65 Gy, especially for T2 tumors, have been found to be significant for reduced local control in studies of early glottic cancers treated by definitive Rf (84). Also, in patients with T2 neoplasms, good local control ranging from 75% to 85% for local control has been observed in patients with T2 neoplasms (87,94-97). A comparison of outcomes for external versus endoscopic approach for patients with early glottic tumors revealed similar oncologic results. The group treated by laser surgery, however, was found to have a shorter clinical course, lower complications, and the best possibility of salvage therapy in the case oflocal recurrence (83,98,99). In a study investigating prognostic factors for local recurrence, the anterior commissure was the site of recurrent tumor in 54% of the cases, vocal muscle infiltration and subglottic involvement correlated with poor disease-free survival, and 91% of the recurrent cases could be retreated successfully (100). Outcome for lesions involving anterior commissure: Involvement of the anterior commissure is considered to be a poor prognosticator for local control in early glottic cancer irrespective of the treatment modality. The observed rates for local control in T1 carcinoma with anterior commissure extension vary from 57% to 89% (102-107). The organ preservation rate in this study was high ranging from 93% for Tla to 88% in T1 b and 93% in T2lesions (112). Unlike open procedures, there is no disruption of structural integrity including the cartilaginous framework or the strap muscles. This results in better protection of the airway and swallowing that facilitate faster functional recovery. Furthermore, avoidance of Rf preserves salivation and pharyngeal lubrication that assists in speech (104). The quality of voice is affected by the extent of cordectomy (114) and unsatisfactory outcome can be improved using phonomicrosurgical techniques. Whereas some authors advocate better voice outcomes with radiation than laser surgery (115), others have observed dysphonia due to Rf-induced scarring and dryness of normal mucosa (116). Excision biopsy using transorallaser alone has been observed to yield a 92% recurrence-free survival at 3 years forTl glottic cancers (71). Moreover, biopsy for making the histologic diagnosis is quite likely to remove the entire tumor in early localized lesions even before the initiation of radiation treatment (123). In a retrospective study of 30 patients, better 3-year local control rate could be achieved only when chemoradiotherapy was combined with transoral debulking microsurgery (95%) versus chemoradiotherapy alone (61 %) (127). Suitable candidates for radiation in early glottic cancer may include elderly patients with poor general health who are at greater risk of surgery-related complications, tumor extending to both cords, or when the physician lacb surgical expertise. Other complications include xerostomia, pmistent laryngeal edema, cervical fibrosis, glottic stenosis, hypothyroidism, chondronecrosis, and radiation-induced malignancy. Radiation-recurrent tumors are also, frequently, submucosal and discontinuous in nature. The results may also be affected by tumor extension to the anterior commissure or the arytenoids (133,135). The photosensitizer is delivered intravenously, topically, or orally followed by subsequent treatment with a pulsed dye laser. Food and Drug Administration approved for clinical treatment of early glottic cancers; howevet; its application as a single-modality, minimally invasive treatment modality is still limited. About 68% of patients were reported to present with early subglottic cancer in a series of 39 patients (137); however, most of the other published studies have observed 60% to 80% of the tumors presenting at late stages with dyspnea and stridor that may necessitate tracheostomy (138,139).
Buy generic cialis jelly 20 mg
The facial nerve is protected in this approach because it will always lie medial to the ossicular heads erectile dysfunction doctor atlanta order cialis jelly online from canada. Second, care should be exercised as the canal is enlarged in the posterior-inferior direction because of the more anterior and lateral course of the mastoid segment. Chronic Infection Normal migration of keratin debris is lacking in the skingrafted ear canal. Protective secretions from sebaceous and apocrine glands are also absent As a consequence, the incidence of canal infections is higher than in the normal ear. A widely patent meatus and membranous canal are important for aeration and cleaning, which may be required once or twice annually. Most patients are not restricted with regard to water activities, although use of an alcohol- or acetic add-based ear drop after swimming is often recommended. Some degree of narrowing of the membranous canal requiring local care in the office. Occasionally, a significant stenosis occurs, trapping squamous epithelium and causing infection. In such cases, attempts to dilate the canal with soft or hard stents are usually ineffective, and a secondary meatoplasty with skin grafting is necessary. This potential problem can be minimized by generously debulking soft tissue from the auricle before the meatoplasty, thus decreasing the length of the membranous canal. In addition to Kenalog injections, the application of mitomycin C has been suggested as a method to prevent or reduce excess fibrosis within the ear canal (38-40). In some patients, the lateral canal may be narrowed by displacement of the pinna rather than by fibrous proliferation. Because the reconstructed auricle has more mass and less muscular and soft tissue support than the normal pinna, it can shift, usually anteriorly or inferiorly, after surgery. If there is concern about proper alignment of Conductive Hearing Loss Persistent or recurrent conductive hearing loss is the most common negative outcome in aural atresia surgery. The causes of the former are varied and include inadequate mobilization of the ossicular mass from the atretic bone, an unrecognized incudostapedial joint discontinuity, or a fixed stapes footplate. Wide exposure of the ossicular mass at surgery is necessary to ensure chain mobility and to facilitate assessment of chain integrity. Recurrence of a conductive hearing loss after an initial satisfactory improvement in air-conduction thresholds is usually secondary to refixation of the ossicular chain or to tympanic membrane lateralization. At least a 2- to 3-mm wide area of bone removal around the ossicular mass (except at the fossa incudis) is desirable, because bony regrowth can occu~; especially as children enter puberty. In several male patients with initial excellent hearing results for 8 to 10 years, complete closure of the bony canal has been observed during their rapid growth spurt of adolescence. Anchoring the fascia graft beneath a bony ledge and/ or the use of a Silastic disc help minimize graft lateralization. The incidence of tympanic membrane perforation or middle ear adhesions approximates that encountered in routine tympanoplastic procedures. Bone-Anchored Hearing Implant A bone-anchored hearing aid is an alternative rehabilitative strategy for patients with unilateral or bilateral aural atresia, and especially for those patients who are marginal or poor surgical candidates. This approach uses an osseointegrated titanium fixture, placed in the mastoid area. The osseointegration allows more efficient transfer of sound than can be achieved with a traditional bone-conduction hearing aid (42). As in patients with otosclerosis, this hearing aid option should be discussed in tandem with surgical Chapter 148: Congenital Malformation of the Ear 2397 intervention. Less commonly, skin overgrowth necessitating surgical revision of the implant site and failure to osseointegrate can occur (43). This device provides an alternative to the traditional bone-conduction hearing aid and should be considered in children born with bilateral aural atresia. A thorough knowledge of the anatomic variations that can occur with abnormal development of the temporal bone is essential, and the nuances of audiometric and radiographic interpretation must be mastered. Hearing results that are consistently excellent cannot yet be achieved in atresia surgery, but with adherence to strict selection criteria and with further refinements in surgical technique, this goal is realistic. Boneconduction auditory brainstem response can provide objective data on ear-specific cochlear function in these cases and help with operative selection. The latter can occur because of inadequate mobilization of the ossicular mass from the atretic bone, lateralization of the tympanic membrane graft, or refixation of the ossicular chain by bony regrowth or fibrous tissue. The intratemporal course of the facial nerve and its influence on the development of the ossicular chain. If incomplete, this process can result in a stenotic membranous canal laterally, with a more normal caliber bony canal and tympanic membrane medially. The significant defect in the minor malformation group involves the middle ear, especially the ossicular chain. In most cases of microtia and atresia of the ear canal, the cochlear and vestibular labyrinths are normally formed. Dehiscence of the tympanic segment with or without inferior displacement is often seen. The mastoid segment of the facial nerve often makes a more acute angle at the second genu, resulting in anterior and lateral displacement; it may obscure the round window. The preventive effect of mitomycinC on the external auditory canal fibrosis in an experimentally induced animal model. Intraoperative use of mitomycin C in fibrous atresia of the external auditory canal. Middle ear dimensions in congenital aural atresia and hearing outcomes after atresiaplasty. Congenital aural atresia: ernbtyOlogy, pathology, classification, genetics, and surgical management. In the vast majority of cases, the pathologic process is self-limited, or resolves with antibiotic therapy. Although these complications are rare today, they occur in developed countries at approximately the same frequency as in underdeveloped countries, and are associated with high rates of serious morbidity and mortality (4). Prompt diagnosis and rapid, effective therapy are critical to minimizing these sequelae. Exposure to pathogens can be increased or altered by exposure to day care environments, or crowded or unhygienic living situations. The specific microbiologic flora is strongly influenced by prior individual and community antibiotic treatment (5). Different pathogens have varying degrees of pathogenicity and disease progression. Eustachian tube function varies widely in otherwise normal individuals, but is reduced in patients with cleft palate, exposure to smoke (smokers and passive exposure), allergic rhinitis, neoplastic processes involving the cranial base, acromegaly, and many other conditions. Abnormally patent eustachian tubes result in reflux of nasopharyngeal contents into the middle ear. If a patient develops cholesteatoma, the local anatomy has a direct effect on how the cholesteatoma grows and what bony destruction it causes. The cholesteatoma and associated inflammation can then, in tum, directly or indirectly impact eustachian tube function. It is important to understand the anatomy in which these infections exist, their routes of spread, and the characteristic patterns of disease. Infection can spread via direct extension, via venous structures, or hematogenously. However, the primary pathogenesis seems to be a complex interaction between the specific organisms and the host (8). Chronic otorrhea with or without cholesteatoma Mixed aerobic (also occasionally including S. Anaerobic organisms (Peptococcus, Peptostreptococcus, Bacteroides fragilis) Bacterial meningitis in children Streptococcus pneumonia Haemophilus influenzae, type B Neisseria meningitidis Intracranial Extradural granulation tissue or abscess Sigmoid sinus thrombophlebitis Occluding Non occluding Brain abscess Otitic hydrocephalus Meningitis Subdural abscess An important host response leading to complication is the production of tissue edema and granulation tissue that subsequently becomes obstructive to drainage and aeration. This creates an environment conducive to the growth of anaerobic organisms and the destruction of bone. Important microbiologic factors seem to pivot about the synergistic pathogenicity of anaerobic organisms (9). The epidemiology and microbiologic behavior of the organisms found in complications offer some insight into the pathogenesis and pathophysiology of these complications (Table 149. Uncomplicated chronic otorrhea characteristically cultures Pseudomonas aernginosa, Staphylococcus aureus, and a variety of other Gram-negative organisms, such as Proteus sp. Multiple organisms are found in 57% of chronically draining ears with cholesteatoma, with an average of three different organisms.
Generic 20mg cialis jelly visa
Effect of heated humidification on compliance and quality of life in patients with sleep apnea using nasal rontinuous positive airway pressure impotence under hindu marriage act purchase cialis jelly cheap. Time course of changes in driving simulator performance with and without treatment in patients with sleep apnoea hypopnoea syndrome. Long-term cardiovascular outromes in men with obstructive sleep apnoea hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Severe bradyarrhythmias in patients with sleep apnoea: the effect of rontinuous positive airway pressure treatment. Cardiac rhythm disturbances and Sf-segment depression episodes in patients with obstructive sleep apnea-hypopnea syndrome and its mechanisms. Association of nocturnal arrhythmias with sleep-disordered breathing: the Sleep Heart Health Study. Therapy Insight interactions between atrial fibrillation and obstructive sleep apnea. Effect of rontinuous positive airway pressure on ventricular ectopy in heart failure patients with obstructive sleep apnoea. Controlled trial of continuous positive airway pressure in obstructive sleep apnea and heart failure. Case-control study of 24 hour ambulatory blood pressure in patients with obstructive sleep apnoea and normal matched control subjects. Obstructive sleep apnoea syndrome as a risk factor for hypertension: population study. Predictive factors for the need for additional humidification during nasal continuous positive airway pressure therapy. Craniofacial changes after 2 years of nasal continuous positive airway pressure use in patients with obstructive sleep apnea. Continuous positive airway pressure therapy is associated with an increase in intraocular pressure in obstructive sleep apnea. Practice parameters for the treatment ofsnoring and obstructive sleep apnea with oral appliance. Comparison of a custom-made and a thermoplastic oral appliance fur the treatment of mild sleep apnea. Mandibular advancement oral appliance therapy fur obstructive sleep apnea: effect on awake caliberofthevelopharynx. Nasopharyngoscopic evaluation of oral appliance therapy for obstructive sleep apnea. A randomized, controlled study of a mandibular advancement splint foro bstructive sleep apnea. Mandibular advancement appliances and obstructive sleep apnea: a randomized clinical trial. Efficacy of positive airway pressure and oral appliance in mild to moderate obstructive sleep apnea. Effect of oral appliance therapy on neurobehavioral functioning in obstructive sleep apnea: a randomized controlled trial. Yoshida K Effect on blood pressure of oral appliance therapy for sleep apnea syndrome. Yoshida K Effects of a mandibular advancement device for the treatment of sleep apnea syndrome and snoring on respiratory function and sleep quality. Mandibular advancement devices in 630 men and women with obstructive sleep apnea and snoring. Impact of sleep nasendoscopy on the outcome of mandibular advancement splint therapy in subjects with sleep-related breathing disorders. Sleep nasendoscopy: a diagnostic tool for predicting treatment success with mandibular advancement splints in obstructive sleep apnoea. Sleep nasendoscopy as a predictor of treatment success in snorers using mandibular advancement splints. Treating obstructive sleep apnea and snoring: assessment of an anterior mandibular positioning device. A short term controlled trial of an adjustable oral appliance for the treatment of mild to moderate obstructive sleep apnoea. A randomized crossover study of an oral appliance va nasal-continuous positive airway pressure in the treatment of mild-moderate obstructive sleep apnea. Nasal congestion secondary to allergic rhinitis as a cause of sleep disturbance and daytime fatigue and the response to topical nasal corticosteroids. Effects of nasal surgery on sleep quality in obstructive sleep apnea syndrome with nasal obstruction. Influence ofnasal resistance on oral appliance treatment outcome in obstructive sleep apnea. Differences in upper airway soft tissue anatomy in normal subjects and patients with sleep-disordered breathing. A novel volumetric magnetic resonance imaging paradigm to study upper airway anatomy. Enlargement of the lateral pharyngeal fat pad space in pigs increases upper airway resistance. Mechanical properties of the velopharynx in obese patients with obstructive sleep apnea. Waking genioglossal electromyogram in sleep apnea patients versus normal controls: a neuromuscular rompensatory mechanism. Didgeridoo playing as alternative treatment for obstructive sleep apnoea syndrome: randomized rontrolled trial. Effects of oropharyngeal exercises on patients with moderate obstructive sleep apnea syndrome. Sleep fragmentation attenuates the hypercapnic (but not hypoxic) ventilatory responses via adenosine A1 receptors in awake rats. Effects of alrohol and sleep restriction on simulated driving performance in untreated patients with obstructive sleep apnea. Prospective randomized study of patients with insomnia and mild sleep disordered breathing. Objective evidence that bariatric surgery improves obesity-related obstructive sleep apnea. Effects of sleep posrure on upper airway stability in patients with obstructive sleep apnea. Fasting glycemia in sleep disordered breathing: lowering the threshold on oxyhemoglobin desaturation. Sleep-disordered breathing and cardiovascular disease: an outmme-baserl definition ofhypopneas. The complex interaction between respiratory control, arousal thresholds, neuromuscular tone. Simply put, the upper airway including the pharynx and to a lesser degree the nasal cavity can be thought of as a collapsible tube. The flow of air through the upper airway is influenced by the difference in upstream, downstream, and intraluminal forces. The role of surgical intervention has classically been viewed as an attempt to influence the structures involved with airway collapse. An alternative and perhaps more accurate way of looking at the role of surgery is that of a reconstructive approach. The goal of airway reconstruction is to improve the patency of the tube and the flow of air. In adults, a single anatomic structure is not usually the sole cause of obstruction, and multiple sites or levels of the airway often require treatment for optimal results. A vast array of surgical treatments are described and variable reported responses to them exist. This is in part due to the distinct character of each airway based on the craniofacial anatomy, neuromuscular tone, influence from other soft tissues, and physiologic elements. Impacting only one of these factors surgically may be inadequate to achieve the desired end state. Ideally, the surgical approach is tailored to a patient rather than the application of a one method suits all approach. Obstruction and narrowing of both the upper pharyngeal (retropalatal) and lower pharyngeal (retroglossal) airways occurs in 70% to 80% of patients (1). Obstruction occurs in the pharynx for most events but obstruction of laryngeal tissues as a primary site is uncommon (4,5). Ultimately, the common finding is an upper airway that is structurally vulnerable to collapse.