Cheap sumycin 250 mg mastercard
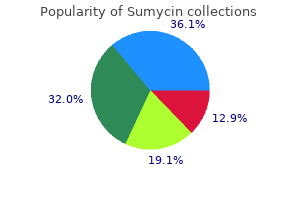
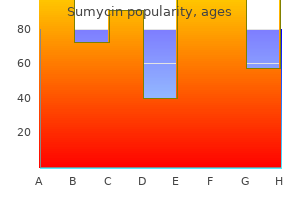
All techniques have limitations antimicrobial therapy for mrsa 500mg sumycin for sale, including need for calibration, sensitivity to motion artifact, and limited applicability in critically ill patients. This was directly proposed more than a half century ago by Eather and associates, who advocated monitoring of "arterial pressure and pressure pulse contours" in anesthetized patients. Others, such as recognition of excessive variation in arterial blood pressure variables as a sign of preload reserve, have only gained significant attention more recently. This bedside examination is a variation on a technique originally described in 1929 to assess arterial stenosis in the hands of patients with thromboangiitis obliterans. Normally, the color will return to the palm within several seconds; severely reduced ulnar collateral flow is present when the palm remains pale for more than 6 to 10 seconds. Although the Allen test is often used to identify patients at increased risk for ischemic complications from radial artery cannulation, the predictive value of this test is poor. Numerous reports of permanent ischemic sequelae note that a normal Allen test result was present before vessel cannulation. Despite its increased risk, cost, and need for technical expertise for placement and management, its utility in providing crucial and timely information outweighs its risks in many cases (Box 45-2). The Australian Incident Monitoring Study of 1993 confirmed the superiority of direct arterial pressure monitoring over indirect monitoring techniques for the early detection of intraoperative hypotension. It appears that the test is unable to provide a cutoff point below which perfusion can be deemed vulnerable. Oximetry is able to detect blood flow at extremely low flows, leading to poor specificity, whereas no established ultrasound criteria are available by which to evaluate radial or ulnar blood flow and identify abnormalities. Dorsiflexion of the wrist should be mild at most to avoid attenuating the pulse by stretch or extrinsic tissue pressure. The course of the radial artery proximal to the wrist is identified by gentle palpation, the skin is prepared with an antiseptic, and a local anesthetic is injected intradermally and subcutaneously beside the artery. Although a soft arm board can be used to maintain the wrist in an anatomically neutral position during arterial pressure monitoring, extreme wrist dorsiflexion should be avoided to prevent injury to the median nerve. Although it is unnecessary to place an additional hole in the back wall of the radial artery for successful cannulation, the technique per se is not associated with a more frequent rate of complications or failure. The ulnar artery is cannulated in a manner similar to that for the radial and has been used safely even following failed attempts to access the ipsilateral radial artery. Bazaral and associates reported more than 3000 brachial artery catheters in patients undergoing cardiac surgery, with only one significant thrombotic complication and no long-term sequelae. However, the risk of cerebral embolization is significantly increased when more centrally located vessels are used. The femoral artery is the largest vessel in common use for monitoring, but its safety appears to be comparable to those for other sites. The risk of distal ischemia may be reduced because of the large diameter of the artery, but risk of atherosclerotic plaque embolization is significant during initial vessel manipulation. Catheterization of the femoral artery is best achieved with a guidewire technique, and the point of vessel entry must be distal to the inguinal ligament to minimize the risk of arterial injury, hidden hematoma formation, or even uncontrolled hemorrhage into the pelvis or peritoneum. Complications of Direct Arterial Pressure Monitoring Large clinical investigations confirm the infrequent incidence of long-term complications after radial arterial monitoring. In most cases, catheter placement was technically difficult or there were contributory factors such as shock or coagulopathy. Furthermore, the anesthesia closed claims study reported claims related to arterial pressure monitoring at any site constitute only 8% of all claims related to any vascular access (2% of total claims). Of these, almost 54% were related to radial artery use (ischemic injury, median or radial nerve injury, or retained wire fragment), less than 8% were associated with use of the brachial artery, and the remainder followed severe thrombotic or hemorrhagic complications after femoral artery monitoring. The fundamental wave (top) added to 63% of the second harmonic wave (middle) results in a pressure wave (bottom) resembling a typical arterial blood pressure waveform (box). Unfortunately, several factors, including extension tubing, stopcocks, flush devices, recorders, amplifiers, and transducers, influence this process and may introduce significant error. The natural frequency of a system determines how rapidly the system oscillates after a stimulus, whereas the damping coefficient reflects frictional forces acting on the system and determines how rapidly it returns to rest after a stimulus. Both variables may be estimated or measured at the bedside and dramatically influence the appearance of the displayed pressure waveform. The displayed arterial blood pressure waveform is a periodic complex wave produced via Fourier analysis of a summation of a series of simpler but diverse propagated and reflected pressure waves. As such, it is a mathematic re-creation of the original complex pressure wave created by stroke volume ejection. Although the pulse rate is measured in beats per minute, fundamental frequency is expressed as cycles per second or Hertz (Hz). The sine waves that sum to produce the final complex wave have frequencies that are multiples or harmonics of the fundamental frequency. A crude arterial waveform depicting a systolic upstroke and peak, dicrotic notch, and so forth can be reconstructed with reasonable accuracy from only two sine waves, the fundamental frequency and the second harmonic. If the original arterial pressure waveform contains high-frequency components such as a steep systolic upstroke, higher-frequency sine waves (and more harmonics) are needed to provide a faithful reconstruction of the original pressure waveform. As a general rule, 6 to 10 harmonics are required to provide distortion-free reproductions of most arterial pressure waveforms. The faster the heart rate and the steeper the systolic pressure upstroke, the greater the dynamic response demands on the monitoring system. All monitoring systems have an intrinsic natural frequency and damping coefficient. Systolic pressure overshoot and additional small, nonphysiologic pressure waves (arrows) distort the waveform and make it hard to discern the dicrotic notch (boxes). The overdamped pressure waveform (A) shows a diminished pulse pressure compared with the normal waveform (B). The slow-speed recording (bottom) demonstrates a 3-minute period of damped arterial pressure. An underdamped pressure waveform displays systolic pressure overshoot and may contain elements produced by the measurement system itself rather than the original propagated pressure wave. In contrast, an overdamped waveform is recognizable by its slurred upstroke, absent dicrotic notch, and loss of fine detail. Catheter-tubing transducer systems in routine clinical use tend to be underdamped but have an acceptable natural frequency that exceeds 12 Hz68. In general, the lower the natural frequency of the monitoring system, the more narrow the range of damping coefficients necessary to ensure faithful reproduction of the pressure wave. If the damping coefficient is too low, the monitoring system will be underdamped, resonate, and display factitiously elevated systolic blood pressure; if the damping coefficient is too high, the system will be overdamped, systolic pressure will be falsely decreased, and fine detail in the pressure trace will be lost. For any specific system, the most rapid possible natural frequency facilitates an optimal dynamic response. Blood clots and air bubbles concealed in stopcocks and other connections have a similar impact on system dynamic response. As a general rule, adding air bubbles to a monitoring system will not improve its dynamic response because any Original waveform 1. Depending on these two parameters, catheter tubingtransducer systems may be classified by their dynamic response range. Systems with an optimal or adequate dynamic response will record and display all or most pressure waveforms encountered in clinical practice. Overdamped and underdamped systems skew measurements in predictable ways, with those having a natural frequency <7 Hz proving unacceptable. The rectangular crosshatched box indicates the ranges of damping coefficients and natural frequencies commonly encountered in clinical pressure measurement systems. Arterial pressure waveforms are displayed, along with superimposed fast-flush square-wave artifacts. A, Original monitoring system has an adequate dynamic response (natural frequency 17 Hz, damping coefficient 0. Somewhat paradoxically, monitoring system resonance may increase and cause even greater systolic pressure overshoot. The fast-flush test provides a convenient bedside method for determining dynamic response of the system and assessing signal distortion. Natural frequency is inversely proportional to the time between adjacent oscillation peaks, calculated as 1 cycle/1. The amplitude ratio thus derived indicates how quickly the measuring system returns to a resting state.
Purchase sumycin in united states online
Factors that may enhance the distribution of local anesthetic within the epidural space are small caliber (greater spread in the thoracic space) bacteria exponential growth purchase 250 mg sumycin with visa, increased epidural space compliance, decreased epidural fat content, decreased local anesthetic leakage through the intervertebral foramina. Finally, the direction of drug spread varies with the vertebral level- that is, epidural spread is mostly cephalad in the lumbar region, caudad after a high thoracic injection, and mostly cephalad spread after a low thoracic injection. The rate of elimination is also dependent on the distribution of local anesthetic; greater spread will expose the drug to a larger area for vascular absorption and thus a shorter duration of action. Neuraxial anesthesia evokes blockade of the sympathetic and somatic (sensory and motor) nervous systems, along with compensatory reflexes and unopposed parasympathetic activity. Yet a biphasic response, characterized by an early transient increase followed by an eventual decrease in cardiac output,30 has been observed. This initial increase is caused by a greater magnitude of decline in the systemic vascular resistance than by venous return, especially in elderly patients with preexisting hypertension and high baseline systemic vascular resistance (also see Chapter 80). The extent of the sympathectomy is typically described as extending for two to six dermatomes above the sensory block level with spinal anesthesia and at the same level with epidural anesthesia. In elderly patients with cardiac disease, systemic vascular resistance may decrease almost 25% after spinal anesthesia, whereas cardiac output decreases only 10%. Heart rate may also decrease in the presence of extensive peripheral sympathectomy (T5-L2), with venous pooling in the lower extremity and the abdominal and pelvic viscera. Although hypotension will trigger a compensatory baroreceptor sympathetic response (vasoconstriction and increased heart rate) above the level of blockade, the reduction in venous return and right atrial filling causes a decrease in signal output from intrinsic chronotropic stretch receptors located in the right atrium and great veins,31 leading to a marked increase in parasympathetic activity (vagal tone). The two opposing responses are usually in check with a minimal change in heart rate (or a slight reduction). However, when neuraxial anesthesia is extended to the T1 level, blockade of the cardioaccelerator fibers in addition to a marked reduction in venous return may result in severe bradycardia and even asystole because of unopposed parasympathetic activity. However rare, the likelihood of cardiac arrest appears to be more likely in young, healthy, and conscious patients. The decrease in arterial blood pressure is believed to be more gradual and of less magnitude with epidural than with spinal anesthesia of comparable levels. However, when tetracaine (10 mg) spinal anesthesia was compared with lidocaine (20 to 25 mL of a 1. Venous and arterial vasodilation reduces preload (venous return) and afterload (systemic vascular resistance), respectively. Because of the large amount of blood that resides in the venous system (approximately 75% of the total blood volume), the venodilation effect predominates, owing to the limited amount of smooth muscle in venules; in contrast, the vascular smooth muscle on the arterial side of the circulation retains a considerable degree of autonomous tone. Extraction of oxygen was unchanged because myocardial work, as expressed by myocardial use of oxygen, paralleled the decrease in mean arterial blood pressure and coronary blood flow (16 to 7. However rare, respiratory arrest associated with spinal anesthesia is often unrelated to phrenic or inspiratory dysfunction but rather to hypoperfusion of the respiratory centers in the brainstem. Supportive evidence for this concept is observed after resuscitation, when apnea almost always disappears as soon as pharmacologic and intravascular fluid therapies have restored cardiac output and arterial blood pressure. Treatment the clinical question of what level of decrease in arterial blood pressure after a neuraxial block is acceptable without a significant decrease in organ perfusion. Once arterial blood pressure decreases to a level at which treatment is believed to be necessary, ephedrine, a mixed adrenergic agonist, provides more appropriate therapy for the noncardiac circulatory sequelae of neuraxial block than does a pure -adrenergic agonist (see Chapters 16 and 20), unless the patient has a specific and defined arterial blood pressure requirement. Specifically, 250- to 2000-mL preblock hydration regimens may temporarily increase preload and cardiac output but do not consistently increase arterial blood pressure or prevent hypotension. In a study of elderly patients who had hypotension during bupivacaine spinal anesthesia, Minville and colleagues demonstrated a significant but transient decrease of middle cerebral artery blood flow velocity and an increase in cerebral vascular resistance, both of which suggest a decrease in cerebral perfusion. Whether cerebral autoregulation is impaired in the elderly is still debatable (see Chapter 80). Obesity (Also see Chapter 71) the impact of spinal anesthesia on lung volume variables is significantly reduced compared with general anesthesia49 but is significantly more in overweight patients than in normal-weight patients. Nausea and vomiting may be associated with neuraxial block in as much as 20% of patients and they are primarily related to gastrointestinal hyperperistalsis caused by unopposed parasympathetic (vagal) activity. Spinal anesthesia is most commonly used for patients who require surgical anesthesia for procedures of known duration that involve the lower extremities, perineum, pelvic girdle, or lower abdomen. Descriptions of spinal anesthesia as the primary surgical anesthetic have more recently expanded to include lumbar spine surgery,61 as well as upper abdominal procedures, such as laparoscopic cholecystectomy. Epidural anesthesia can also be used for the lower extremities, perineum, pelvic girdle, or lower abdomen, but by virtue of intermittent or continuous catheter-based local anesthetic delivery, the duration of surgical anesthesia is not necessarily finite as it is with single-injection spinal anesthesia. Continuous catheter-based spinal anesthesia is arguably less conventional than either single-shot spinal anesthesia or catheter-based epidural anesthesia, but may be especially useful when insertion of an epidural catheter is challenging63 or in the setting of severe cardiac disease when the reliability of a single-shot spinal anesthetic must be combined with more hemodynamically stable incremental dosing. For example, in orthopedic patients undergoing hip replacement, bladder catheterization was no more frequent after spinal or epidural anesthesia than it was after general anesthesia and opioid analgesics. In any case, excessive volumes of intravenous crystalloid solutions should not be given to patients undergoing spinal anesthesia. The requirement for voiding before discharge in low-risk ambulatory surgery patients after short-acting spinal or epidural anesthetics should be encouraged. The use of intrathecal and/or epidural opioids either alone or in combination with local anesthetics can provide excellent quality pain relief65,66 and are an analgesic mainstay in labor and delivery,67,68 during and after hip69 or knee replacement,70 in laparotomy,71 in thoracotomy,72 and increasingly even in cardiac surgery. Some of the most important include patient refusal, localized sepsis, and an allergy to any of the drugs planned for administration. The level of anesthesia or analgesia required is of prime importance because the physiologic effects of a high-level block may be untenable. A catheter-based neuraxial anesthetic, whether it is an epidural or intrathecal catheter, allows for the repeated administration of small doses of local anesthetic, with potentially more control over hemodynamic changes, and may be a logical alternative choice. An extension of patients who are preloaddependent, hypovolemic patients may exhibit an exaggerated hypotensive response to the vasodilatory effects of neuraxial blockade. The proof that neuraxial anesthesia or analgesia in the setting of preexisting neurologic deficit can worsen the extent of injury (so-called double-crush phenomenon) is absent. The association between neuraxial techniques and the exacerbation of back pain symptoms is not documented. Patients with spinal stenosis may be at increased risk of neurologic complications after neuraxial blockade,81 but the relative contribution of surgical factors and natural history of the spinal pathology itself is unknown. Previous spine surgery does not predispose patients to an increased risk of neurologic complications after neuraxial blockade. Depending on the severity of the neural tube defect, patients with spina bifida may have a tethered cord and the ligamentum flavum may be absent, thereby increasing the potential for traumatic needle injury to the spinal cord. If a neuraxial technique is undertaken in any of these circumstances, a careful evaluation of neurologic status must first be undertaken and noted along with documentation of the discussion of the risks and benefits. The safety of neuraxial techniques in patients with common bleeding diatheses is not well documented. Hemorrhagic complications after neuraxial techniques in patients with known hemophilia, von Willebrand disease, or idiopathic thrombocytopenic purpura appear infrequently when factor levels are more than 0. A definitive causative relationship between existing systemic infection and meningitis or epidural abscess after a neuraxial technique has never been shown. In fact, a lumbar puncture is a critical component of the investigation of fever of unknown origin, yet there are no definitive data linking lumbar puncture to increased risk of neuraxial infection in this setting. The unpredictable speed and extent to which systemic vascular resistance is reduced after spinal anesthesia may cause many providers to avoid spinal anesthesia in preload-dependent patients and try to prevent a dangerous decrease in coronary perfusion. This concern is borne of theoretic risk and a great deal of caution rather than evidence. American Society of Regional Anesthesia and Pain Medicine Evidence-Based Guidelines (Third Edition), Reg Anesth Pain Med 35:64-101, 2010. Adapted from the German Society of Anaesthesiology and Intensive Care Medicine Consensus guidelines. Yet patients with evidence of systematic infection may safely undergo neuraxial anesthesia once antibiotic therapy has been initiated and the patient has demonstrated a response to the antibiotics. The provider must recall that intraabdominal structures such as the peritoneum (T4), bladder (T10), and uterus (T10) have a spinal segment innervation that may be much more cephalad compared with that of the corresponding skin incision used to operate on these structures. Drug, patient, and procedural factors can all affect the distribution of local anesthetic spread within the intrathecal space, some of which are more clinically relevant than others. Drug Factors the adjustable factors for any given local anesthetic solution are dose, volume, concentration, temperature, and baricity. Density is defined as the mass per unit volume of solution (g/mL) at a specific temperature. Density may be compared between different substances by calculating the specific gravity, which is the ratio of the density of a solution to the density of water.

Discount 250 mg sumycin with visa
Heart Failure Heart failure affects 4 to 5 million people in the United States and is a significant risk factor for postoperative mortality and adverse events infection the game purchase sumycin in united states online. Diastolic failure accounts for almost half of all cases, but little science guides the perioperative care of these individuals. Ischemic heart disease is the most common cause of systolic dysfunction in developed countries (50% to 75% of cases). The goal in the preoperative evaluation is to identify and minimize the effects of heart failure. Recent weight gain, complaints of shortness of breath, fatigue, orthopnea, paroxysmal nocturnal dyspnea, nocturnal cough, peripheral edema, hospitalizations, and recent changes in management are all significant. Patients with decompensated heart failure feel like they are "suffocating" or have "air hunger. In general, elective surgery should not be performed until at least 1 year following drug-eluting stent implantation. If urgent surgery is needed, strong consideration is given to continuing dual antiplatelet drug therapy throughout the perioperative period (see Box 38-3). Antiplatelet drugs should not be interrupted in patients with coronary stents without consultation with a cardiologist familiar with coronary stents, as well as an in-depth discussion with the surgeon and the patient regarding the risks of stopping these drugs. Digoxin levels are not routinely determined unless toxicity, undertreatment, or noncompliance is suspected. One must determine trough levels of digoxin, and this is not always possible in a preoperative evaluation setting. Normal left ventricular ejection fraction is greater than 50%; mildly diminished is 41% to 49%, moderately diminished is 26% to 40%, and severely diminished is 25% or less. In addition, severely affected individuals or those with decompensated heart failure may need the help of a heart failure specialist. Medical therapy, including -adrenergic blockers, hydralazine, nitrates, and digoxin, must be optimized and continued preoperatively. Continuation of loop diuretics on the day of surgery does not increase the risk of intraoperative hypotension or adverse cardiac events. Continuing all medications for patients with severe dysfunction who are scheduled for minor procedures is probably best. In these cases, potent diuretics should be discontinued on the morning of surgery. As indicated previously, surgery should be postponed in patients with decompensated or untreated heart failure, unless the situation is truly an emergency. No consensus exists on how long such patients remain at risk after resolution of an acute exacerbation of heart failure. Murmurs and Valvular Abnormalities Clinical goals in preoperative assessment include determining the cause of cardiac murmurs and distinguishing between significant murmurs and those that are clinically unimportant89 (see Chapter 67). Functional murmurs occur from turbulent flow across the aortic or pulmonic outflow tracts. These benign murmurs occur with highflow states such as hyperthyroidism, pregnancy, or anemia. It is often not easy for noncardiologists to distinguish benign from pathologic murmurs. In general, regurgitant valvular lesions are better tolerated perioperatively than is stenotic disease. Nonetheless, the usefulness of this approach is debatable because severe lesions can be associated with soft murmurs and vice versa. The location of the murmur, as well as changes in intensity associated with maneuvers, can guide diagnosis (Table 38-6). Severe aortic stenosis is associated with increased perioperative cardiac risk, especially in combination with other risk factors for perioperative cardiac complications. Aortic sclerosis, which also causes a systolic ejection murmur similar to that of aortic stenosis, is present in 25% of people 65 to 74 years old and in almost half of those 84 years old or older. The cardinal symptoms of severe aortic stenosis are angina, heart failure, and syncope, although patients are much more likely to complain of a decrease in exercise tolerance and exertional dyspnea. Aortic stenosis causes a systolic ejection murmur, best heard in the right upper sternal border and often radiating to the neck. A delayed carotid upstroke and a paradoxically split S2 (second heart sound) are noted. The pattern of radiation of the murmur can help rule out aortic stenosis; specifically, the absence of murmur radiation to the right clavicle is associated with a negative likelihood ratio of 0. This is especially true if general anesthesia or an intermediate- or high-risk procedure is planned. Aortic stenosis severity is based on the valve area and mean transvalvular pressure gradient (Table 38-7). A limitation of using the pressure gradient alone to assess severity is that the gradient may decrease if the left ventricle begins to fail. Echocardiography is recommended annually for patients with severe aortic stenosis, every 2 years for moderate stenosis, and every 5 years for mild stenosis. Patients with moderate to severe aortic stenosis have an increased risk of bleeding. The cause appears to be acquired von Willebrand syndrome, resulting from mechanical disruption of von Willebrand multimers during turbulent blood flow through a narrowed valve. Prophylaxis for infective endocarditis in patients with aortic stenosis is no longer recommended. Insufficiency of the aortic valve occurs with true valvular disease affecting the leaflets, aortic root dilation, or both. Rheumatic heart disease, bicuspid valves, collagen vascular diseases, and endocarditis can all lead to valvular disease. Aortic root dilation can complicate ankylosing spondylitis, osteogenesis imperfecta, syphilis, hypertension, age-related degeneration, Marfan syndrome, and collagen vascular diseases. Acute aortic insufficiency can also result from trauma, infections, or aortic dissection; this is an emergency. The intensity of the murmur does not correlate with the severity of regurgitation. Other signs include de Musset sign (head bob with each heart beat), Duroziez sign (systolic and diastolic bruit heard over the femoral artery when it is partially compressed), Quincke pulses (capillary pulsations in the fingertips or lips), and Mueller sign (systolic pulsations of the uvula). Left atrial hypertrophy and left axis deviation along with premature atrial and ventricular contractions are not uncommon. Generally, chronic aortic insufficiency is well tolerated in the perioperative period. Patients with good functional status and preserved left ventricular systolic function have a low risk of complications of anesthesia. Mitral stenosis is much less common than aortic stenosis and is usually associated with a history of rheumatic heart disease. A normal mitral valve has an area of 4 to 6 cm2; stenosis is mild when the area is 1. A resting mean transvalvular gradient of 10 mm Hg or more also denotes severe stenosis. Symptoms typically occur 10 to 20 years after acute rheumatic fever and often are precipitated by pregnancy or illness. Unrecognized mitral stenosis should be included in the differential diagnosis of pulmonary edema. Dyspnea, fatigue, orthopnea, pulmonary edema, and hemoptysis result from increased left atrial pressures and decreased cardiac output. Atrial fibrillation can result from a dilated left atrium, which can precipitate heart failure in the short term and cause thrombosis in the long term. Patients with atrial fibrillation also require anticoagulation to avoid a left atrial thrombus. Pulmonary Chapter 38: Preoperative Evaluation 1103 hypertension (suggested by a loud S2 heart sound) and right-sided heart failure may occur in patients with significant stenosis. Physical examination involves looking for rales and for signs of right-sided heart failure such as jugular venous distention, peripheral edema, hepatomegaly, right ventricular heave, and ascites.
Purchase sumycin 250 mg without a prescription
Acupuncture stimulates high-threshold infection quarantine purchase 250mg sumycin visa, small-diameter nerves that activate the spinal cord, brainstem. Studies using positron emission tomography have demonstrated that the thalamic asymmetry present in patients suffering from chronic pain was reduced after acupuncture treatment. Although acupuncture was used clinically for centuries, the first trial of acupuncture for anesthesia was performed in China around 1960. Because anesthesia produced by acupuncture varies and takes too long to induce,174 acupuncture has been used rarely as anesthesia for surgery175 and more for pain relief afterward. Since 1970, clinical studies have been conducted on acupuncture for postoperative pain,176 lower back pain,177 osteoarthritis of the knee,178 chronic headache,179 shoulder pain,180 and neck pain. Drugs, the mainstay of management, have limited effectiveness, are associated with adverse effects, and can be costly. The P6 acupuncture point is located between the palmaris longus and flexor carpi radialis muscle tendons, 4 cm proximal to the distal wrist crease and 1 cm below the skin. Data to compare the effectiveness, safety, and costs of different methods of stimulation are inadequate. Stimulation of the acupuncture point should be initiated before induction of anesthesia. Some anesthesiologists anecdotally report tapping a small needle cap or other piece of smooth plastic over the P6 point as an effective means of acupressure stimulation. With this method, a subject consciously slows breathing and focuses on taking deep breaths. Slow, deep breathing relaxation exercises Music therapy is the clinical, evidence-based use of music interventions to accomplish individualized therapeutic goals. Because music can be used for diverse applications, music therapists practice in a variety of health care and education settings. The increase of endogenous opioids through music may be the reason for pain relief. Patient-selected music can reduce patient-controlled sedative requirements during spinal anesthesia and analgesic requirements during lithotripsy. Sections also contain safety, industry, and regulatory information this site contains fact sheets about alternative therapies, consensus reports, and databases the site contains an extensive phytochemical database with search capabilities Although this site addresses all aspects of health care, there is a considerable amount of information covering complementary and herbal therapies this site focuses on health fraud with a position paper on over-thecounter herbal remedies this site contains information on numerous herbal medications, with evidence for activity, warnings, preparations, mixtures, and mechanisms of action. This site is maintained by a corporation that conducts independent laboratory investigations of dietary supplements and other health products frequency and intensity compared with usual care. To manage herbal medications in the perioperative period, their possible direct and indirect effects should be recognized based on an understanding of the underlying pharmacology. Surgery and anesthesia can usually proceed safely if potential complications are anticipated and can be minimized. These modalities are easy to administer, have a rapid onset of action, are cost effective, and produce minimal side effects. Food and Drug Administration: Draft guidance for industry: dietary supplements: new dietary ingredient notifications and related issues, July, 2011. Chapter 40: Anesthetic Implications of Complementary and Alternative Medications 182. Food and Drug Administration: Draft guidance for industry: dietary supplements: new dietary ingredient notifications and related issues, 2011. A randomized, double-blind, placebo-controlled trial, Ann Intern Med 137:939, 2002. Munekage M, Kitagawa H, Ichikawa K, et al: Pharmacokinetics of daikenchuto, a traditional Japanese medicine (kampo) after single oral administration to healthy Japanese volunteers, Drug Metab Dispos 39:1784, 2011. Gawande S, Kale A, Kotwal S: Effect of nutrient mixture and black grapes on the pharmacokinetics of orally administered (-)epigallocatechin-3-gallate from green tea extract: a human study, Phytother Res 22:802, 2008. Gleitz J, Beile A, Wilkens P, Ameri A, Peters T: Antithrombotic action of the kava pyrone (+)-kavain prepared from Piper methysticum on human platelets, Planta Med 63:27, 1997. Pongrojpaw D, Chiamchanya C: the efficacy of ginger in prevention of post-operative nausea and vomiting after outpatient gynecological laparoscopy, J Med Assoc Thai 86:244, 2003. Kruth P, Brosi E, Fux R, et al: Ginger-associated overanticoagulation by phenprocoumon, Ann Pharmacother 38:257, 2004. Vale S: Subarachnoid haemorrhage associated with Ginkgo biloba, Lancet 352:36, 1998. Rosenblatt M, Mindel J: Spontaneous hyphema associated with ingestion of Ginkgo biloba extract, N Engl J Med 336:1108, 1997. Woelkart K, Feizlmayr E, Dittrich P, et al: Pharmacokinetics of bilobalide, ginkgolide A and B after administration of three different Ginkgo biloba L. Meyer) on acute glycemia: results of two acute dose escalation studies, J Am Coll Nutr 22:524, 2003. Pharmacokinetics of ginsenosides in the rabbit, Eur J Drug Metab Pharmacokinet 5:161, 1980. Bent S, Kane C, Shinohara K, et al: Saw palmetto for benign prostatic hyperplasia, N Engl J Med 354:557, 2006. Kerb R, Brockmoller J, Staffeldt B, et al: Single-dose and steadystate pharmacokinetics of hypericin and pseudohypericin, Antimicrob Agents Chemother 40:2087, 1996. Leuschner J, Muller J, Rudmann M: Characterisation of the central nervous depressant activity of a commercially available valerian root extract, Arzneimittelforschung 43:638, 1993. Taavoni S, Ekbatani N, Kashaniyan M, Haghani H: Effect of valerian on sleep quality in postmenopausal women: a randomized placebo-controlled clinical trial, Menopause 18:951, 2011. Zhou S, Chan E: Effect of ubidecarenone on warfarin anticoagulation and pharmacokinetics of warfarin enantiomers in rats, Drug Metabol Drug Interact 18:99, 2001. Zhou Q, Zhou S, Chan E: Effect of coenzyme Q10 on warfarin hydroxylation in rat and human liver microsomes, Curr Drug Metab 6:67, 2005. Spigset O: Reduced effect of warfarin caused by ubidecarenone, Lancet 344:1372, 1994. Shalansky S, Lynd L, Richardson K, et al: Risk of warfarin-related bleeding events and supratherapeutic international normalized ratios associated with complementary and alternative medicine: a longitudinal analysis, Pharmacotherapy 27:1237, 2007. Persiani S, Rotini R, Trisolino G, et al: Synovial and plasma glucosamine concentrations in osteoarthritic patients following oral crystalline glucosamine sulphate at therapeutic dose, Osteoarthritis Cartilage 15:764, 2007. Volpi N: Oral absorption and bioavailability of ichthyic origin chondroitin sulfate in healthy male volunteers, Osteoarthritis Cartilage 11:433, 2003. Dyerberg J: Platelet - vessel wall interaction: influence of diet, Philos Trans R Soc Lond B Biol Sci 294:373, 1981. Abraham J: Acupressure and acupuncture in preventing and managing postoperative nausea and vomiting in adults, J Perioper Pract 18:543, 2008. Arnberger M, Stadelmann K, Alischer P, et al: Monitoring of neuromuscular blockade at the P6 acupuncture point reduces the incidence of postoperative nausea and vomiting, Anesthesiology 107:903, 2007. Boehler M, Mitterschiffthaler G, Schlager A: Korean hand acupressure reduces postoperative nausea and vomiting after gynecological laparoscopic surgery, Anesth Analg 94:872, 2002. Stewart E: To lessen pain: relaxation and rhythmic breathing, Am J Nurs 76:958, 1976. Chalaye P, Goffaux P, Lafrenaye S, Marchand S: Respiratory effects on experimental heat pain and cardiac activity, Pain Med 10:1334, 2009. Tsunoda Y, Sakahira K, Nakano S, et al: Antagonism of acupuncture analgesia by naloxone in unconscious man, Bull Tokyo Med Dent Univ 27:89, 1980. Mori H, Nishijo K, Kawamura H, Abo T: Unique immunomodulation by electro-acupuncture in humans possibly via stimulation of the autonomic nervous system, Neurosci Lett 320:21, 2002. Gerhard I, Postneek F: Auricular acupuncture in the treatment of female infertility, Gynecol Endocrinol 6:171, 1992. Shen J: Research on the neurophysiological mechanisms of acupuncture: review of selected studies and methodological issues, J Altern Complement Med 7(Suppl 1):S121, 2001. Taguchi R: Acupuncture anesthesia and analgesia for clinical acute pain in Japan, Evid Based Complement Alternat Med 5:153, 2008. Weidenhammer W, Linde K, Streng A, et al: Acupuncture for chronic low back pain in routine care: a multicenter observational study, Clin J Pain 23:128, 2007. Witt C, Brinkhaus B, Jena S, et al: Acupuncture in patients with osteoarthritis of the knee: a randomised trial, Lancet 366:136, 2005. Manias P, Tagaris G, Karageorgiou K: Acupuncture in headache: a critical review, Clin J Pain 16:334, 2000. Ekblom A, Hansson P, Thomsson M, Thomas M: Increased postoperative pain and consumption of analgesics following acupuncture, Pain 44:241, 1991. Gunta K, Lewis C, Nuccio S: Prevention and management of postoperative nausea and vomiting, Orthop Nurs 19:39, 2000.
Purchase line sumycin
British Thoracic Society Bronchoscopy Guidelines Committee: a Subcommittee of Standards of Care Committee of British Thoracic Society: British Thoracic Society guidelines on diagnostic flexible bronchoscopy antimicrobial 5 year plan purchase sumycin paypal, Thorax 56(Suppl 1):i1-i21, 2001. Weiler N, Heinrichs W, Dick W: Assessment of pulmonary mechanics and gastric inflation pressure during mask ventilation, Prehosp Disaster Med 10:101-105, 1995. Isono S, Tanaka A, Ishikawa T, Tagaito Y, Nishino T: Sniffing position improves pharyngeal airway patency in anesthetized patients with obstructive sleep apnea, Anesthesiology 103:489-494, 2005. Asai T, Brimacombe J: Review article: cuff volume and size selection with the laryngeal mask, Anaesthesia 55:1179-1184, 2000. Brimacombe J, Clarke G, Keller C: Lingual nerve injury associated with the ProSeal laryngeal mask airway: a case report and review of the literature, Br J Anaesth 95:420-423, 2005. Isono S: Common practice and concepts in anesthesia: time for reassessment: is the sniffing position a "gold standard" for laryngoscopy Takenaka I, Aoyama K, Iwagaki T, Ishimura H, Kadoya T: the sniffing position provides greater occipito-atlanto-axial angulation than simple head extension: a radiological study, Can J Anaesth 54:129-133, 2007. Cattano D, Cavallone L: Airway management and patient positioning: a clinical perspective, Anesthesiology News 37:17-23, 2011. Asai T, Shingu K: Difficulty in advancing a tracheal tube over a fibreoptic bronchoscope: incidence, causes and solutions, Br J Anaesth 92:870-881, 2004. Nileshwar A, Thudamaladinne A: Comparison of intubating laryngeal mask airway and Bullard laryngoscope for oro-tracheal intubation in adult patients with simulated limitation of cervical movements, Br J Anaesth 99:292-296, 2007. Sorbello M, Paratore A, Morello G, et al: Bonfils fiberscope: better preoxygenate rather than oxygenate! Aziz M, Metz S: Clinical evaluation of the Levitan Optical Stylet, Anaesthesia 66:579-581, 2011. Bouvet L, Da-Col X, Rimmele T, et al: Optimal remifentanil dose for laryngeal mask airway insertion when co-administered with a single standard dose of propofol, Can J Anaesth 57:222-229, 2010. Nakayama S, Osaka Y, Yamashita M: the rotational technique with a partially inflated laryngeal mask airway improves the ease of insertion in children, Paediatr Anaesth 12:416-419, 2002. Weber S: Traumatic complications of airway management, Anesthesiol Clin North America 20:503-512, 2002. Burgard G, Mollhoff T, Prien T: the effect of laryngeal mask cuff pressure on postoperative sore throat incidence, J Clin Anesth 8:198-201, 1996. Brimacombe J, Costa e Silva L: Pharyngeal necrosis with the laryngeal mask airway, Eur J Anaesthesiol 20:502-503, 2003. Handa-Tsutsui F, Kodaka M: Propofol concentration requirement for laryngeal mask airway insertion was highest with the ProSeal, next highest with the Fastrach, and lowest with the Classic type, with target-controlled infusion, J Clin Anesth 17:344-347, 2005. Biro P, Battig U, Henderson J, Seifert B: First clinical experience of tracheal intubation with the SensaScope, a novel steerable semirigid video stylet, Br J Anaesth 97:255-261, 2006. Greif R, Kleine-Brueggeney M, Theiler L: Awake tracheal intubation using the Sensascope in 13 patients with an anticipated difficult airway, Anaesthesia 65:525-528, 2010. Jungbauer A, Schumann M, Brunkhorst V, Borgers A, Groeben H: Expected difficult tracheal intubation: a prospective comparison of direct laryngoscopy and video laryngoscopy in 200 patients, Br J Anaesth 102:546-550, 2009. Maassen R, Lee R, Hermans B, Marcus M, van Zundert A: A comparison of three videolaryngoscopes: the Macintosh laryngoscope blade reduces, but does not replace, routine stylet use for intubation in morbidly obese patients, Anesth Analg 109:1560-1565, 2009. Cattano D, Artime C, Maddukuri V, et al: Endotrol-tracheal tube assisted endotracheal intubation during video laryngoscopy, Intern Emerg Med 7:59-63, 2012. Dupanovic M: Maneuvers to prevent oropharyngeal injury during orotracheal intubation with the GlideScope video laryngoscope, J Clin Anesth 22:152-154, 2010. Popat M, Mitchell V, Dravid R, et al: Difficult Airway Society Guidelines for the management of tracheal extubation, Anaesthesia 67:318-340, 2012. Falzon D, Foye R, Jefferson P, et al: Extubation guidelines: Guedel oropharyngeal airways should not be used as bite blocks, Anaesthesia 67:919, 2012; author reply 921-922. Despite these similarities, there are significant technical, physiologic, and pharmacologic differences. In contrast, epidural and caudal anesthesia progress more slowly (>20 minutes) after a large mass of local anesthetic that produces pharmacologically active systemic blood levels, which may be associated with side effects and complications unknown to spinal anesthesia. The introduction of combined spinal and epidural techniques blurs some of these differences, but also adds flexibility to clinical care. Single-injection spinal or epidural anesthesia with local anesthetic is most commonly used for surgery to the lower abdomen, pelvic organs. Continuous catheter-based epidural infusions of dilute local anesthetics and opioids are used for obstetric labor analgesia and postoperative pain relief after major surgery. Evidence demonstrating that epidural analgesia can reduce cardiovascular and pulmonary morbidity and mortality in high-risk patients undergoing major thoracic and abdominal surgery served to propel the practice of epidural analgesia at the beginning of the millennium. Caudal blocks are mostly performed for surgical anesthesia and analgesia in children, and for therapeutic analgesia in adults with chronic pain. Indwelling spinal catheters can be applied long term (from months to years) for the treatment of chronic malignant and nonmalignant pain. Spinal anesthesia using ropivacaine and levobupivacaine was introduced in the 1980s. The year 1901 marked the first reported use of intrathecal morphine described by Racoviceanu-Pitesti, as well as the first description of caudal anesthesia reported by Cathleen. Despite the extensive experience using neuraxial techniques throughout the past century, several events caused major setbacks along the way, including the Woolley and Roe case detailing paraplegia after spinal anesthesia in 1954,4 the reports of persistent neurologic deficits and adhesive arachnoiditis with spinal chloroprocaine in the early 1980s, and cauda equina syndrome with continuous spinal lidocaine anesthesia in the early 1990s. This distal termination varies from L3 in infants to the lower border of L1 in adults because of differential growth rates between the bony vertebral canal and the central nervous system. Surrounding the spinal cord in the bony vertebral column are three membranes (from innermost to outermost): the pia mater, the arachnoid mater, and the dura mater. The pia mater is a highly vascular membrane that closely invests the spinal cord and brain. Surrounding the dura mater is the epidural space, which extends from the foramen magnum to the sacral hiatus and surrounds the dura mater anteriorly, laterally, and posteriorly. The epidural space is bound anteriorly by the posterior longitudinal ligaments, laterally by the pedicles and intervertebral foramina, and posteriorly by the ligamentum flavum. Contents of the epidural space include the nerve roots and fat, areolar tissue, lymphatics, and blood vessels including the well-organized Batson venous plexus. Posterior to the epidural space is the ligamentum flavum (the so-called yellow ligament), which also extends from the foramen magnum to the sacral hiatus. B, Oblique view of the lumbar vertebrae showing the ligamentum flavum thickening in the caudad extent of the intervertebral space and in the midline. Superior articular process Spinous process C Inferior articular process comprised of two ligamenta flava-the right and the left-which join in the middle and form an acute angle with a ventral opening. Ligament thickness, distance to the dura, and skin-to-dura distance vary with the area of the vertebral canal. The two ligamenta flava are variably joined (fused) in the midline, and this fusion or lack of fusion of the ligamenta flava even occurs at different vertebral levels in individual patients. Extending from the external occipital protuberance to the coccyx posterior to these structures is the supraspinous ligament, which joins the vertebral spines. The vertebral arch, spinous process, pedicles, and laminae form the posterior elements of the vertebra, and the vertebral body forms the anterior element. The vertebrae are joined together anteriorly by the fibrocartilaginous joints with the central disks containing the nucleus pulposus, and posteriorly by the zygapophyseal (facet) joints. The thoracic spinous process is angulated steeply caudad as opposed to the almost horizontal angulation of the lumbar spinous process. This is a clinically important distinction for needle insertion and advancement in the thoracic versus lumbar levels. The sacral canal contains the terminal portion of the dural sac, which typically ends at S2. Variation is found in this feature as well, with the termination of the dural sac being lower in children. In addition to the dural sac, the sacral canal contains a venous plexus, which is part of the valveless internal vertebral venous plexus. The volume of the caudal canal in adults, excluding the foramina and dural sac, is about 10 to 27 mL.
Vedhari (Cissus Quadrangularis). Sumycin.
- Obesity and weight loss, diabetes, metabolic syndrome, and high cholesterol, bone fractures, osteoporosis, scurvy, cancer, upset stomach, hemorrhoids, stomach ulcer, menstrual discomfort, asthma, malaria, pain, and body building.
- Are there safety concerns?
- What is Cissus Quadrangularis?
- How does Cissus Quadrangularis work?
- Dosing considerations for Cissus Quadrangularis.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=97110
Buy genuine sumycin
This volume includes arteries antibiotic justification form cheap generic sumycin uk, capillaries, and veins and has a predominantly venous weighting. Buccal microvascular Hb saturation has been associated with survival in patients with sepsis. Because no gold standard exists for cerebral oximetry, it is difficult to compare the accuracy of the devices, and each device has its own set of "normal" values. For this reason, acquisition of baseline values for each patient at the start of the procedure is recommended. A reduction of rSo2 to less than 20% to 25% of the baseline, or lower than an absolute value of 50%, is a recommended threshold for intervention. Intraoperative reductions in rSo2 correlate well with changes in transcranial Doppler variables,124-128 electroencephalographic waveforms,129-131 and stump pressure,128,132 which are consistent with ischemia. Although some studies indicate that reductions in rSo2 that are less than 20% of baseline are well tolerated, data are lacking for a clear rSo2 threshold for carotid shunt placement (see also Chapter 69). Its presence in the sample cell decreases the amount of infrared light at this wavelength that reaches the detector in proportion to its concentration. In addition, the light source is completely blocked at various points during the revolution of the chopper disk. The two general categories of capnometers are sidestream (diverting) and mainstream (nondiverting). Schematics of sidestream (A) and mainstream (C) capnometry sampling methods, along with corresponding representative time capnograms (red curves in B and D) following a step increase in carbon dioxide concentration (blue lines). Rise time (T70) corresponds to the time required for either sensor to change from 10% to 70% of its final value. A delay time is observed for the sidestream analyzer, corresponding to the aspiration rate of the sampled gas and the washout of the analyzing chamber. Typical tubing length for this aspiration may be 6 feet, and gas withdrawal rates may vary from 30 to 500 mL/minute. This lost gas volume may need to be considered during closed-circuit anesthesia or during ventilation of neonates and infants. The volume can be returned to the circuit, or it can be routed to a scavenger to prevent contamination of the environment with anesthetic or waste gases. Gases must also pass through various filters and water traps before they are presented to the sample cell. Thus, the inspiratory or expiratory gases pass directly through the infrared light path. Well-ventilated and well-matched V/Q regions tend to have lower Pco2 and shorter time constants, and they empty earlier during the expiratory phase. The method used to determine this number is not universal and varies according to the manufacturer of the particular capnograph in use. For example, Petco2 may simply be (1) the Pco2 value just before inspiration, (2) the largest Pco2 value during a single exhalation cycle, or (3) the Pco2 value at a specified time in the capnogram averaged across several breaths. In healthy individuals with homogeneous ventilation, the difference between Paco2 and Petco2 is usually less than 5 mm Hg, thereby expressing the equilibration between alveolar and pulmonary capillary blood. Several disease states compromise this equilibration and produce increased Paco2 - Petco2 difference (Box 51-2). In some situations, Petco2 can be greater than Paco2, especially in the presence of severe ventilation heterogeneity and lung units with very low V/Q. This section focuses on the use of arterial blood gases to assess oxygenation and ventilation. In healthy adults breathing room air at sea level, PaO2 ranges between 80 and 100 mm Hg. Hypoventilation V/Q mismatching Right-to-left shunt Diffusion limitation Diffusion-perfusion mismatch the first three causes explain most cases of hypoxemia in the perioperative setting. D, Cardiogenic oscillations at the end of exhalation as flow decreases to zero and the beating heart causes emptying of different lung regions and back-and-forth motion between exhaled and fresh gas. V/Q mismatch, right-to-left shunt, and alveolar diffusion limitation affect the efficiency of O2 exchange. Diffusion limitation plays a role in conditions that thicken the alveolar-capillary barrier, such as interstitial lung diseases, and in hypoxemia induced by exercise or altitude. Representative time capnograms trended over many breaths that illustrate various abnormalities in ventilation or perfusion, or both. C, sudden interruption in pulmonary perfusion, as may occur during cardiac arrest. The volume capnogram is a plot of the fraction of carbon dioxide (Fco2) in exhaled gas versus exhaled volume. The total area below the horizontal line (denoting the Fco2 of a gas in equilibrium with arterial blood) can be divided into three distinct areas: X, Y, and Z. Representative single-breath volume capnograms illustrating various abnormalities in ventilation or perfusion, or both. Right-to left shunt is the amount of blood that flows from the pulmonary artery to the systemic arterial circulation without undergoing pulmonary gas exchange. Effect of different ventilation-perfusion V/Q regions on partial pressure of arterial oxygen (PaO2). Because of the shape of the oxyhemoglobin dissociation curve, regions of lung with low V/Q have a disproportionately greater effect on lowering the arterial saturation than do regions of lung with normal or higher V/Q to increase Pao2. Based on the oxyhemoglobin dissociation curve, however, the average saturation of the arterial blood is 89%, producing an average PaO2 equal to 7. In healthy awake spontaneously breathing subjects, intrapulmonary shunt is negligible,159 and a small (<1% of cardiac output) extrapulmonary shunt results from drainage of the bronchial and thebesian veins into the arterial side of the circulation. The effect of the shunt on PaO2 is a function of the magnitude of the shunt, and the cardiac output. Increases in FiO2 have a small effect on PaO2 in the presence of a large true right-to-left shunt. Cco2 is calculated using Equation 1 and assuming equilibration between the end-capillary blood and alveolar gas. When FiO2 is 100%, the effects of V/Q heterogeneity on O2 exchange are eliminated, and the equation exclusively yields the right-to-left shunt fraction. Other Indices of Oxygenation the calculation of the shunt fraction is a fundamental measure of O2 exchange impairment. For this reason, indices of oxygenation have been developed that rely on less invasive measures. The lung is represented as three functional units: alveolar dead space, "ideal" alveoli, and venous admixture (shunt). The model does not differentiate between true shunt or true dead space and components of shunt and dead space that are caused by ventilation-perfusion (V/Q) mismatch. This is because the (A-a) Po2 is unchanged under conditions of decreased FiO2 and hypoventilation but increased with V/Q mismatch, shunt, and diffusion limitation. Another limitation is the fail ure of these indices to account for changes in V/Q matching resulting from changes in the FiO2. Additionally, the normal value of the (A-a)Po2 is less than 10 mm Hg in young adults breathing room air, and it increases with age and the administration of supplemental O2. In this way, compensatory hyperventilation can be used to reduce elevations in Paco2. As with the discussion on shunt, the dead space fraction characterizes not only real anatomic dead space, but also areas of inefficient ventilation. The electrode consists of a cathode (electron source, platinum or gold) and an anode in an electrolyte bath, surrounded by a thin O2-permeable membrane. The electrode is inserted into the sample, and O2 diffuses through the membrane and is reduced by the cathode, thus generating a current. Two strategies have been developed for the management of arterial gas partial pressures under these conditions: alpha-stat and pH-stat. Potential benefits of alpha-stat management include the preservation of cerebral autoregulation and the maintenance of protein function. The theoretic benefits of pH-stat management are increased cerebral vasodilation leading to more homogenous cerebral cooling. Two common sources of error are delays in sample analysis and the presence of air in the sampling syringe. The presence of an air bubble in the syringe can lead to a change in the measured PaO2 toward the Po2 of the bubble and a decline in Paco2. The transport of air to the alveoli and alveolar gas to the environment requires the creation of a pressure gradient, which will result in volume changes in the elastic components of the respiratory system, flow in the airways, velocity in moving tissues, and acceleration of air and tissues.
Purchase genuine sumycin online
Patients with bacteria eating flesh sumycin 500mg mastercard, or suspected of having, pulmonary hypertension must be managed by a pulmonary hypertension specialist (see the later section on pulmonary hypertension). A maneuver that decreases diastolic volume or increases contractility increases the intensity of the murmur. Thus, passive leg raising and squatting decrease the intensity, whereas the Valsalva maneuver increases it. Many patients are treated with -adrenergic blockers to decrease contractility; these medications should be continued perioperatively. The most important preoperative issues in patients with prosthetic heart valves are determinations of the underlying condition requiring replacement, the type of prosthesis, the need for anticoagulation, and the planned anticoagulation management of such patients in the perioperative period. In descending order of risk, the risk of thrombosis is greatest with multiple valves, mitral valve replacements, and aortic valve replacements. Bioprosthetic valves such as Carpentier-Edwards or Hancock brands generally do not require long-term anticoagulation. Prophylaxis for infective endocarditis is recommended for specific procedures and is discussed in the next section. A Guideline from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group, Circulation 16:1736-1754, 2007. Prophylaxis is recommended because prosthetic material is endothelialized within 6 months after the procedure. Current guidelines have dramatically scaled back the range of conditions and procedures warranting prophylaxis. Prophylaxis to prevent endocarditis is also no longer recommended for patients with valvular abnormalities (other than transplant recipients). Patients who are having procedures on infected skin or musculoskeletal tissues and who also have one of the conditions listed in Box 38-7 receive prophylaxis. Many procedures involving the gastrointestinal and genitourinary tracts may cause transient bacteremia; however, reports of endocarditis associated with these procedures are anecdotal. The current guidelines recommend prophylaxis only for at-risk patients (see Box 38-7) undergoing urinary tract procedural manipulation. If the procedure is elective, infection should be eradicated before the procedure is performed. No prophylaxis is recommended for upper and lower gastrointestinal diagnostic endoscopic procedures. Rhythm Disturbances on the Preoperative Electrocardiogram Arrhythmias and conduction disturbances are common in the perioperative period. Supraventricular and ventricular arrhythmias are associated with a higher risk of perioperative adverse events, both because of the arrhythmias themselves and because they are markers for cardiopulmonary disease. Uncontrolled atrial fibrillation and ventricular tachycardia are high-risk clinical predictors, and elective surgery is postponed until evaluation and stabilization are complete. New-onset atrial fibrillation, uncontrolled atrial fibrillation (rates >100 beats/minute), symptomatic bradycardia, or high-grade heart block (second- or third-degree heart block), warrants postponement of elective procedures and referral to cardiology for further evaluation. Mobitz type I, or Wenckebach block, is more benign, rarely progresses to complete heart block, and is easily responsive to atropine. Third-degree or complete heart block is complete dissociation between the atrial and ventricular beats and requires a pacemaker unless a reversible source is identified. Two general factors are considered when determining the need for a pacemaker: an arrhythmia associated with symptoms and the location of the conduction abnormality. Syncope or near syncope associated with bradycardia or conduction delays is generally an indication for pacemaker placement. Disease in the His-Purkinje system is generally less stable and likely benefits from permanent pacemaker placement. Indications for perioperative pacemaker placement are the same as those in nonsurgical patients (Box 38-8). They can be normal variants, or they can result from aging or fibrosis of the conducting system, ischemia, pulmonary disease, radiation, and cardiomyopathies. If congenital heart disease, pulmonary hypertension, or Brugada syndrome is suspected, a cardiology consultation is indicated. Most patients with atrial fibrillation require long-term anticoagulation, which entails perioperative management. Patients with atrial or ventricular thrombi, mechanical heart valves, or a history of previous thromboembolic events are at higher risk for stroke. Any -adrenergic blockers, digoxin, calcium channel blockers, or antiarrhythmic medications used for atrial fibrillation should be continued perioperatively. Food and Drug Administration in 2006, and reports of adverse events with droperidol resulted in a black box warning and subsequent removal of the drug from the U. Brugada syndrome is a rare cause of sudden cardiac arrest that occurs without structural heart disease. Brugada syndrome is an autosomal dominant disorder that is much more common in men and rarely diagnosed in children. The most significant clinical manifestations are ventricular arrhythmias, syncope, and sudden death. These patients may also be at increased risk of atrial arrhythmias, especially atrial fibrillation. The syndrome has no proven pharmacologic treatment; indeed, class I antiarrhythmic medications. The preoperative evaluation should determine the type of device, as well as features. Patients frequently carry a wallet card with important designations and phone numbers. Equally important is the need to evaluate the coexisting cardiac disease because these patients invariably have conditions such as heart failure, ischemic heart disease, valvular heart disease, or potentially lethal arrhythmias. Special features such as rate-adaptive mechanisms and antitachyarrhythmia functions must be disabled, or the device must be reprogrammed to an asynchronous pacing mode before surgical procedures where interference may occur. It is inappropriate to have industry-employed allied health professionals independently develop this prescription. Communication and guidance with an electrophysiology specialist comprise the preferred approach for managing these patients. Patients with Marfan syndrome or Ehlers-Danlos syndrome may have aneurysmal disease without other risk factors. Renal insufficiency and cerebrovascular disease are also common in these patients. For example, in a study of 1000 consecutive patients scheduled for major vascular surgery, almost 60% had critical stenosis in at least one major coronary vessel. If significant vascular disease is diagnosed during an examination for nonvascular surgery, referral to a vascular specialist is needed. Auscultation for bruits over the abdomen and femoral arteries, as well as palpation for abdominal masses, should be part of the vascular examination. A creatinine concentration should be determined before procedures involving injection of radiocontrast dye. Many patients take aspirin or dipyridamole, Chapter 38: Preoperative Evaluation 1109 a vasodilator with antiplatelet effects that are reversible on discontinuation. Continuation of antiplatelet drugs is preferable for almost all vascular procedures. Asthma Asthma is a chronic inflammatory disease characterized by obstruction of the airways that is partially or completely reversible with treatment or spontaneously. Asthma is classified as intermittent, persistent mild, persistent moderate, and persistent severe, based on the degree of impairment and on whether symptoms are intermittent or constant. Patients with mild, well-controlled asthma have no greater perioperative risk than do individuals without asthma. A history of asthma should be associated with further questioning about shortness of breath, chest tightness, cough (especially nocturnal), recent exacerbations, therapy (especially steroids), prior hospitalizations or emergency department visits, critical care unit admissions, and endotracheal intubations. Patients with asthma can estimate their breathing capacity based on their estimated percentage at which they are currently functioning. The quality of breath sounds, quantity of air movement, and degree of wheezing are important. The degree of wheezing does not always correlate with the severity of bronchoconstriction.
Purchase sumycin amex
The signals are very small antibiotics starting with z generic 250mg sumycin mastercard, and each recording electrode records only information generated directly beneath the electrode. The electroencephalographer can accurately identify consciousness, unconsciousness, seizure activity, stages of sleep, and coma. In the absence of significant changes in anesthetic technique, the electroencephalographer also can accurately identify inadequate oxygen delivery to the brain (from either hypoxemia or ischemia). Evoked potentials are electrical activity generated in response to either a sensory or a motor stimulus. Measurements of evoked responses may be made at multiple points along an involved nervous system pathway. It contains a passive thermistor (T1) that measures brain temperature and is located outside of the area influenced by the active thermistor. The energy required to maintain that increase in temperature is proportional to cerebral blood flow. The initial rate of propagation of the thermal field is used to establish the fixed conductive component of heat transfer. Because fever is a frequent complication, particularly in patients with severe brain disease, the inability to monitor during a febrile episode may constitute a true limitation of the technique. Localized monitoring of tissue Po2 is based on an oxygen-sensitive electrode originally described by Clark. Currently available catheter-based electrodes provide stable recording conditions over long periods. Motor-evoked responses are generally larger and commonly do not require averaging. Responses may be recorded proximally over the stimulated nerve, the spinal cord, and the cerebral cortex. The recorded responses assess the function of the peripheral nerve, the posterior and lateral aspects of the spinal cord, a small portion of the brainstem, the ventral posterolateral nucleus of the thalamus, the thalamocortical radiation, and a portion of the sensory cortex. Responses are most commonly recorded from electrodes applied to the scalp, although more invasive direct recordings from auditory structures and nerves may also be made. Recordings are made from cortically placed electrodes and assess visual pathways from the optic nerve to the occipital cortex. Electrical stimuli to activate motor tracts also may be applied at the level of the spinal cord, but this method of stimulation is controversial (see later). International 10-20 system of electrode placement for recording electroencephalogram and sensory-evoked responses. Alternatively, subdermal needle electrodes may be used, particularly when sterile application of an electrode close to a surgical field is necessary. When electrodes are applied directly to the surface of the brain, impedance is minimized by close electrode contact and saturation of the area with an electrolyte solution. This system is a symmetric array of scalp electrodes placed systematically based on the distance from the nasion to the inion and from the pretragal bony indentations associated with both temporomandibular joints. Based on 10% or 20% of these distances, recording electrodes are placed systematically over the frontal (F), parietal (P), temporal (T), and occipital (O) regions at increasing distances from the midline. Left-sided electrodes are given odd number subscripts, and right-sided electrodes are given even number subscripts. The large spikes (arrows) are muscle artifact from eye blinks and hence are best visible in channels that incorporate frontal electrodes (designated F). Recordings also may be made from electrodes placed on the surface of the brain (electrocorticography) or from microelectrodes placed transcortically to record from individual neurons. Amplitude is the size, or voltage, of the recorded signal and ranges commonly from 5 to 500 V (versus 1 to 2 mV for the electrocardiogram signal). Frequency can be thought of simply as the number of times per second the signal oscillates or crosses the zero voltage line. This highfrequency and usually low-amplitude signal is common from an alert attentive brain and may be recorded from all regions. With eye closure, higher-amplitude signals in the alpha frequency range (8 to 13 Hz), seen best in the occipital region, appear. Regional asymmetry can be seen with tumors, epilepsy, and cerebral ischemia or infarction. Factors affecting the entire brain may produce symmetric abnormalities of the signal. Many of the normal global pattern changes produced by anesthetic drugs are similar to pathologic patterns produced by ischemia or hypoxemia. This qualitative approach was used simply because the waveforms could not be described mathematically in a time frame that would make such information of any practical use. Computer hardware has dramatically improved in speed and size, and real-time signal processing is now possible and commonly used. Display of the activity of both hemispheres is necessary to delineate unilateral from bilateral changes. These monitors display the data in two general forms, either compressed spectral array or density spectral array. In compressed spectral array, frequency is displayed along the x-axis, and power is displayed along the y-axis with height of the waveform equal to the power at that frequency. Density spectral array also displays frequency along the x-axis; time is displayed along the y-axis, and power is reflected either by the density of the dots at each frequency or by a spectrum of colors. Each display format provides the same data, and choice depends on the preference of the user. Many changes that occur during anesthesia and surgical procedures are reflected as changes in amplitude, frequency, or both. These changes can be clearly seen in these displays if adequate and appropriate channels are monitored. The example at the bottom of the figure shows compressed spectra of the alpha rhythm from a normal subject. Power analysis is a sensitive and reliable monitor in the hands of experienced operators using an adequate number of channels. In addition, parameters obtained from power analysis have been investigated as monitors for depth of anesthesia39-42 (see Chapter 50). If a long epoch length is chosen, the waveform can be described precisely, but the time required for data processing is long and not real time. If a short length of data is sampled, analysis may be done in near-real time, but the epoch chosen for analysis may not be representative of the overall waveform. With better and faster computers, continuous monitoring of 2-second epochs and now even longer epochs is possible. Because motor pathways are often adjacent anatomically to these sensory pathways or are supplied by the same blood vessels, or both, function of motor pathways may be inferred, albeit imperfectly, from function of these sensory pathways. With this technique, signal recording is timelocked to the application of the sensory stimulus. This enhancing effect increases directly with the square root of the number of responses added into the averaged response. Interpeak latency may be measured between two peaks in the same channel or between peaks in different channels (shown in figure). The example shows a recording of posterior tibial somatosensory-evoked potentials. Each tracing is reproduced twice because reproducibility of a waveform helps distinguish signal from artifact. Left and right posterior tibial nerves are stimulated at 0 and 90 msec, respectively. As a far-field potential, the potential looks similar for right- and left-sided stimulation. The primary cortical responses are recorded from the contralateral hemisphere (labeled P35 and N40). Because the current spreads diffusely throughout the conducting medium, it is more difficult to locate the source of the recorded signal, and the electrode position has little effect on the morphology of the recorded evoked potential. More responses must be averaged to record far-field potentials (several thousand) than near-field potentials (50 to 100). Subcortical responses may arise from many different structures depending on the type of response, including peripheral nerves, spinal cord, brainstem, thalamus, cranial nerves, and others. Subcortical-evoked responses also may be recorded as far-field potentials from scalp electrodes or, as appropriate, from electrodes placed over the spinal column or peripheral nerve.