Cheap tetracycline 250mg without a prescription
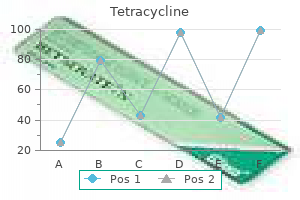
Pineal gland tumors account for 8% of intracranial tumors in children and 1% of tumors in adults; 40% of tumors are germinomas antimicrobial herbs and phytochemicals cheap tetracycline 500mg on-line, followed by pineoblastomas and pineocytomas, teratomas, choriocarcinomas, endodermal sinus tumors, astrocytomas, and metastatic tumors. Tuberous sclerosis is an autosomal dominant disorder associated with hamartomas in multiple organs. Tumors often have intermediate attenuation to intermediate to slightly high attenuation, with contrast enhancement, with or without central and/or peripheral calcifications. Malignant tumors are often larger than benign pineal lesions (pineocytoma), as well as heterogeneous attenuation and contrast enhancement pattern, with or without leptomeningeal tumor. Cortical-subcortical lesion with variable attenuation, calcifications in 50% of older children; contrast enhancement uncommon. Subependymal hamartomas: Small nodules located along and projecting in to the lateral ventricles; calcification and contrast enhancement common. Sessile or pedunculated lesions at the tuber cinereum of the hypothalamus; often intermediate attenuation similar to gray matter; typically no contrast enhancement; rarely contain cystic and/or fatty portions. Axial image shows a lesion in the right frontal lobe that contains calcifications and is associated with adjacent axonal edema. Axial image in a child with tuberous sclerosis shows multiple calcified and noncalcified ependymal hamartomas, as well as cortical tubers and zones of low attenuation in the white matter. Lipomas can occur in many locations, commonly the corpus callosum, cerebellopontine angle cistern, and tectal plate. Circumscribed or invasive lesions, low to intermediate attenuation; variable contrast enhancement, frequent dissemination in to the leptomeninges. Circumscribed lesions involving the cerebral cortex and subcortical white matter, low to intermediate attenuation, with or without small cysts; usually no contrast enhancement. Diffuse leptomeningeal contrast enhancement is another pattern of intracranial lymphoma. Circumscribed tumors usually located in the cerebellum and/or brainstem; small contrast-enhancing nodule with or without cyst or larger lesion with prominent heterogeneous enhancement with or without contrastenhancing vessels within the lesion or at the periphery, Occasionally lesions have evidence of recent or remote hemorrhage. Circumscribed spheroid lesions in the brain; can have various intra-axial locations, often at gray-white matter junctions; usually low to intermediate attenuation; with or without hemorrhage, calcifications, or cysts; variable contrast enhancement. Extra- or intra-axial lesions usually 3 cm in diameter with irregular margins in the leptomeninges or brain parenchyma/brainstem (anterior temporal lobes, cerebellum, thalami, and inferior frontal lobes). Comments Benign fatty lesions resulting from congenital malformation often located in or near the midline; may contain calcifications and/or traversing blood vessels. Increasing incidence related to the number of immunocompromised patients in the population. Rarely occurs in cerebral hemispheres; occurs in adolescents and young and middle-aged adults. Neurocutaneous melanosis Neuroectodermal dysplasia with proliferation of melanocytes in leptomeninges associated with large and/ or numerous cutaneous nevi. Axial image shows a lipoma involving the anterior portion of the corpus callosum (arrow). Pre- (a) and postcontrast (b) images show a large tumor involving the anterior right frontal lobe containing calcifications that has associated mass effect and subfalcine herniation leftward. Axial postcontrast image shows a heterogeneous enhancing lesion in the right basal ganglia with associated mass effect. Circumscribed lesion with a central zone of low attenuation (with or without air-fluid level) surrounded by a thin rim of intermediate attenuation; peripheral poorly defined zone of decreased attenuation representing edema; ringlike contrast enhancement that is sometimes thicker laterally than medially. Findings can vary depending on organism; lesions occur in meninges and brain parenchyma; solid or cysticappearing lesions with decreased attenuation, nodular or ring pattern of contrast enhancement, peripheral zone with decreased attenuation in brain lesions (edema). Formation of brain abscess occurs 2 weeks after cerebritis with liquefaction and necrosis centrally surrounded by a capsule and peripheral edema. Occur in immunocompromised or diabetic patients with resultant granulomas in meninges and brain parenchyma. Cryptococcus involves the basal meninges and extends along perivascular spaces in to the basal ganglia; Aspergillus and Mucor spread via direct extension through the paranasal sinuses or hematogenously and invade blood vessels, resulting in hemorrhagic lesions and/or cerebral infarcts. Louis encephalitis, eastern or western equine encephalitis, and Epstein-Barr virus). Intra-axial lesions in cerebral hemispheres, basal ganglia, and brainstem (adults) and cerebellum (children). Lesions can have decreased attenuation, central zone of low attenuation with a thin peripheral rim of intermediate attenuation; with solid or rim pattern of contrast enhancement; with or without calcification. Caseating intracranial granulomas via hematogenous dissemination; meninges brain lesions. Postcontrast axial images (a,b) in a neonate show poorly defined zones of contrast enhancement involving the superficial portions of the brain with localized destruction and calcification. Axial postcontrast image (c) in a 35-year-old man shows cerebritis with low attenuation involving the right frontal lobe, as well as a left subdural empyema and right frontal sinusitis. Axial postcontrast image (a) shows a ring-enhancing lesion in the right temporal lobe. Axial image (b) shows a ring-shaped lesion with low attenuation centrally and axonal edema peripheral to the abscess rim. Axial image shows a poorly defined zone of decreased attenuation involving the left cerebral hemisphere. Axial image shows poorly defined zones of decreased attenuation in the frontal and temporal lobes. Axial postcontrast image shows diffuse contrast enhancement in the basal meninges (basal meningitis), as well as a ring-enhancing lesion (tuberculoma) in the anterior left temporal lobe. Echinococcus granulosus: Single or rarely multiple cystic-appearing lesions with low attenuation surrounded by a thin wall; typically no contrast enhancement or peripheral edema unless superinfected; often located in vascular territory of the middle cerebral artery. Echinococcus multilocularis: Cystic (with or without multilocular) and/or solid lesions, central zone of intermediate attenuation surrounded by a slightly thickened rim, with contrast enhancement; peripheral zone of decreased attenuation (edema) and calcifications are common. Comments Caused by ingestion of ova (Taenia solium) in contaminated food (undercooked pork); involves meninges brain parenchyma ventricles. Inflammatory disorders Radiation necrosis Focal lesion with or without mass effect or poorly defined zone of low to intermediate attenuation, with or without contrast enhancement involving tissue (gray matter and/or white matter) in field of treatment. Contrast enhancement can be ringlike or nodular, usually in acute/ early subacute phase of demyelination. Poorly marginated intra-axial zone with low to intermediate attenuation; usually shows contrast enhancement with localized mass effect and peripheral edema. Other demyelinating diseases include acute disseminated encephalomyelitis/immune mediated demyelination after viral infection; toxins (exogenous from environmental exposure or ingestion of alcohol, solvents, etc. Early subacute phase (2 d): Hemoglobin becomes oxidized to the iron Fe3 state, methemoglobin, which is strongly paramagnetic. When methemoglobin eventually becomes primarily extra-cellular, the hematoma has high signal on T1-weighted images and high signal on T2-weighted images. Often involve the anterior portions of the temporal and frontal lobes and inferior portions of the frontal lobes. Metastatic intra-axial tumors associated with hemorrhage include bronchogenic carcinoma, renal cell carcinoma, melanoma, choriocarcinoma, and thyroid carcinoma. May be difficult to distinguish from hemorrhage related to other etiologies, such as vascular malformations and amyloid angiopathy. Axial image shows an acute hypertensive-related hemorrhage with high attenuation in the right basal ganglia. Axial image shows a contusion with high-attenuation hemorrhage involving the anterior portion of the right frontal lobe. Cavernous hemangioma Supratentorial cavernous angiomas occur more frequently than infratentorial lesions. Venous angioma Neuroepithelial cyst Cyst walls have histopathologic features similar to epithelium, neuroepithelial cysts; located in choroid plexus choroidal fissure ventricles brain parenchyma. Diffusionweighted images can show positive findings related to decreased apparent diffusion coefficients secondary to cytotoxic edema, absence of arterial flow void, or arterial enhancement in the vascular distribution of the infarct. Signal abnormalities commonly involve the cerebral cortex and subcortical white matter and/or basal ganglia. Vascular occlusion may be secondary to atheromatous arterial disease, cardiogenic emboli, neoplastic encasement, hypercoagulable states, dissection, or congenital anomalies.
Order discount tetracycline on-line
Note how polyps on the dependent or posterior wall appear as filling defects in the barium pool (black arrows) antibiotic resistance week discount 250 mg tetracycline, whereas polyps on the non-dependent or anterior wall are etched in white (small white arrows). This patient also has a conglomerate mass of polyps (large white arrows) that could be mistaken for a polypoid carcinoma. Hyperplastic polyps Hyperplastic polyps are by far the most common benign polyps in the stomach, constituting as many as 75 to 90% of all gastric polyps. Hyperplastic polyps typically appear on double contrast barium studies as smooth or slightly lobulated, round or ovoid, sessile lesions less than 1 cm in size. When viewed en face, polyps on the dependent wall appear as filling defects in the thin barium pool, whereas polyps on the non-dependent wall are etched in white. Most patients with hyperplastic polyps have multiple lesions that are predominantly located in the gastric body and fundus. As a result, gastric carcinomas have been reported to occur with increased frequency in patients with hyperplastic polyps. Because polyps arise from the mucosa, they may have a smooth, nodular, or lobulated surface on double contrast studies, and, when viewed in profile, form acute angles with the adjacent gastric wall. In contrast, lesions arising from the submucosa or muscularis propria (also known as submucosal or intramural lesions) usually have a very smooth surface and, when viewed in profile, form right angles or slightly obtuse angles with the adjacent gastric wall. Although large lesions that have a smooth surface are usually submucosal in origin, it is often difficult to determine whether protruded lesions less than 1 to 1. Fundic gland polyps Fundic gland polyps are the second most common type of benign gastric polyps, consisting histologically of cystically dilated pits and glands lined by parietal and chief cells. The polyps typically appear on double contrast studies as smooth, sessile lesions less than 1 cm in size. Adenomatous polyps Adenomatous polyps are relatively uncommon benign neoplasms in the stomach. They may be classified as tubular, tubulovillous, or villous adenomas on the basis of their underlying histologic architecture. Unlike hyperplastic polyps in the stomach, adenomatous polyps are premalignant lesions that may progress to gastric carcinoma via an adenoma-carcinoma sequence similar to that found in the colon. In-situ carcinoma or invasive carcinoma is found in at least 50% of adenomatous polyps larger than 2 cm in size. Most gastric adenomas detected on double contrast studies appear as sessile, lobulated, or pedunculated lesions larger than 1 cm in size. Though most hyperplastic polyps are smaller than 1 cm and most adenomas are larger than 1 cm, it is not always possible to distinguish these lesions on the basis of the radiographic findings. If a polyp is 1 cm or larger in size and has a nodular or lobulated surface, endoscopy and biopsy should therefore be performed to exclude the possibility of an adenoma. Conversely, multiple small, rounded polyps less than 5 to 10 mm in size are almost always hyperplastic, so endoscopy and biopsy are not warranted in these patients. A supine double contrast spot image of the stomach shows a solitary, sessile, slightly lobulated polyp (arrow) on the greater curvature of the gastric antrum. While the terms submucosal and intramural are used interchangeably, it should be recognized that, from a strict pathologic point of view, all submucosal lesions are intramural but not all intramural lesions are submucosal, as they can also arise from the muscularis propria or even the subserosa. These lesions consist histologically of intersecting bundles and whorls of spindle-shaped cells. As the lesions enlarge, however, ischemic necrosis and ulceration of the tumor may cause epigastric pain or upper gastrointestinal bleeding. A supine double contrast spot image of the stomach shows a smooth, rounded submucosal mass (black arrows) as a filling defect in the barium pool on the posterior gastric wall. A small submucosal mass (white arrows) is present on the greater curvature of the distal gastric antrum near the pylorus. This is the characteristic appearance and location of an ectopic pancreatic rest in the stomach. The differential diagnosis for submucosal masses in the stomach includes ectopic pancreatic rests and duplication cysts (which usually arise on the greater curvature of the distal gastric antrum) as well as other uncommon mesenchymal tumors such as lipomas, leiomyoblastomas, hemangiomas, and granular cell tumors. Finally, a benign ulcer with a surrounding mound of edema can sometimes be mistaken for an ulcerated submucosal mass, but edema surrounding an ulcer tends to have more ill-defined borders than a submucosal neoplasm. Ectopic pancreatic rests typically appear on barium studies as small (1 to 2 cm in size), solitary, centrally umbilicated submucosal masses on the greater curvature of the distal gastric antrum within 1 to 6 cm from the pylorus. Early gastric cancer Early gastric cancers are defined histologically as tumors limited to the mucosa or submucosa, regardless of the presence or absence of regional lymphatic metastases. Unlike advanced carcinomas, early gastric cancers are curable lesions, with 5-year survival rates as high as 90 to 95%. Such screening studies are almost never performed in the West, however, because of the much lower incidence of gastric carcinoma. As a result, early gastric cancers are rarely detected on double contrast studies in Western countries, as these studies are almost always performed on symptomatic patients who already have advanced lesions. Note the serrated margins of the ulcer and the nodular, clubbed folds abutting the ulcer crater. Tumors that are ulcerated may be associated with nodularity of the adjacent mucosa and clubbing or nodularity of radiating folds due to infiltration of the folds by tumor. Though some lesions with a suspicious appearance are found to be benign, endoscopy and biopsy are required for all lesions with equivocal radiographic findings in order to avoid missing early gastric cancers. Advanced gastric cancer Most patients with gastric carcinoma develop symptoms such as epigastric pain, anorexia, and weight loss only after they have advanced lesions with local or distant metastases and, as a result, a poor prognosis. Obstructing tumors may cause nausea and vomiting, ulcerated tumors may cause upper gastrointestinal bleeding, scirrhous tumors may cause early satiety, and cardiac tumors may cause dysphagia. Concern about missing gastric cancer on barium studies has sometimes been used as the rationale for performing endoscopy as the initial diagnostic test in patients with upper gastrointestinal symptoms. In one study, however, double contrast barium examinations showed the lesion in 99% of patients with gastric cancer, and malignant tumor was diagnosed or suspected on the basis of the radiographic findings in 96%. Thus, a high sensitivity can be achieved in the radiographic diagnosis of gastric carcinoma without exposing an inordinate number of patients to unnecessary endoscopy. Advanced gastric cancers may be manifested on barium studies as polypoid, ulcerative, infiltrative, or scirrhous tumors. On double contrast studies, polypoid lesions on the dependent or posterior wall are seen as filling defects in the barium pool, whereas polypoid lesions on the non-dependent or anterior wall are etched in white by a thin layer of barium trapped between the edge of the mass and the adjacent mucosa. Occasionally, polypoid carcinomas of the distal gastric antrum may prolapse through the pylorus in to the duodenal bulb, appearing as mass lesions at the base of the bulb. Ulcerated carcinomas are those in which much of the tumor mass has been replaced by ulceration because of necrosis. These lesions are often called malignant ulcers, but the term is a misnomer, as it is not the ulcer but the surrounding tumor that is malignant. The radiographic appearance of malignant gastric ulcers and their differentiation from benign gastric ulcers have been discussed elsewhere (see earlier section, Benign versus malignant gastric ulcers, and see. Scirrhous gastric carcinomas typically arise in the distal stomach, gradually extending from the antrum proximally in to the body and fundus. These tumors may be manifested on barium studies by narrowing and rigidity of the stomach associated with mucosal nodularity, thickened folds, and a grossly irregular contour, producing a classic linitis plastica or leather bottle appearance secondary to a marked desmoplastic response incited by the tumor. This circumferentially infiltrating tumor causes irregular narrowing and ulceration of the gastric antrum. There is marked narrowing of the gastric antrum and body with mucosal nodularity, thickened folds, and an irregular luminal contour. These findings are characteristic of a scirrhous tumor with a linitis plastica appearance. With double contrast technique, however, 40% of all scirrhous carcinomas are found to be localized lesions involving the gastric fundus or body with sparing of the antrum. Conversely, other patients with scirrhous tumors may have only minimal loss of distensibility in the stomach, so the diagnosis can be missed if the radiologist relies too heavily on the degree of luminal narrowing as the major criteria for diagnosing these lesions. It is important to be aware of the limitations of endoscopy in diagnosing scirrhous carcinomas of the stomach. There is irregular narrowing of the fundus and body of the stomach with sparing of the antrum. Also note rapid emptying of ingested barium from this rigid, noncompliant stomach in to multiple loops of small bowel. There is focal narrowing of the gastric body with mucosal nodularity, ulceration, and irregular luminal narrowing due to lymphomatous infiltration of the wall.
Cheap tetracycline 250 mg with amex
The total daily dose of immediate-release product may not automatically be equivalent to the daily sustained-release dose; use caution in converting when you need antibiotics for sinus infection buy tetracycline with a mastercard. Increase infusion rate by 25 mL/h every 5 min to a maximum of 150 mL/h until desirable blood pressure lowering is reached. Infusion rate must be decreased to 30 mL/h (3 mg/h) when desirable blood pressure is achieved. If treatment includes transfer to an oral antihypertensive agent other than nicardipine, generally initiate therapy upon discontinuation of the infusion. If oral nicardipine is to be used, administer the first dose of a three times daily regimen 1 h before discontinuation of the infusion. For hospitalized patients under close supervision, dosage may be increased by 10 mg increments over 4-6 h periods until symptoms are controlled. For elderly patients and patients with hepatic impairment, initiate treatment at 10 mg twice daily and monitor carefully. Angina patients maintained on the short-acting formulation (nifedipine capsule) may be switched to the extended-release tablet at the nearest equivalent total daily dose. Nisoldipine (nisoldipine extended release, Sular) Indication Hypertension Dosage Adults Coat-core extended-release tablets Initiate at 20 mg orally once daily; dosage may be increased by 10 mg per week (or at longer intervals) to attain adequate response. For elderly patients and patients with hepatic function impairment, initiate with a dose not exceeding 10 mg daily. Hydrogel extended-release tablets Initiate at 17 mg once daily; dosage may be increased by 8. Administration of this medication with a high fat meal can lead to excessive peak drug concentration and should be avoided. Preparations Nisoldipine (generic, Astra Zeneca, Sciele Pharma): 20, 30, 40 mg extended release tablets Sular (Sciele Pharma): 8. Nimodipine (Nimotop) Indication Subarachnoid hemorrhage Dosage Adults the usual dose is 60 mg q 4 h beginning within 96 h of subarachnoid hemorrhage and continuing for 21 days. Dosage should be reduced to 30 mg q 4 h with close monitoring of blood pressure and heart rate in patients with hepatic cirrhosis. Note: this medication is given preferably not less than 1 h before or 2 h after meals. If the capsule cannot be swallowed (eg, time of surgery, unconscious patient), make a hole in both ends of the capsule with an 18-gauge needle and extract the contents in to a syringe. Sustained-release capsules (Verelan) As an antihypertensive, initiate at 120-240 mg once daily. Dosage may be adjusted in increments of 60-120 mg/d at daily or weekly intervals as needed and tolerated. Dosage may be adjusted in increments of 60120 mg/d at daily or weekly intervals as needed and as tolerated. If response is inadequate, the dose may be titrated upward to 480 mg/d given at bedtime. Note: Less than 1% of patients may have life-threatening adverse responses (rapid ventricular rate in atrial flutter/fibrillation, marked hypotension, or extreme bradycardia/asystole) to verapamil injections. Monitor the initial use of intravenous verapamil and have resuscitation facilities available. An intravenous infusion (5 mg/h) has also been used; precede the infusion with an intravenous loading dose. Elderly Initiate the oral formulation of verapamil at lower dose and titrate to response. Intravenous injections should be given slowly over a longer period of time (at least 3 min) to minimize undesired effects. However, there has been experience with the use of verapamil in the pediatric population. Higher dosage (> 1-2 mg/d) may be required to achieve the desired therapeutic response in patients with renal insufficiency. If the initial diuresis is inadequate, repeated doses may be administered q 4-6 h until the desired diuretic response is achieved or until a maximum daily dosage of 10 mg is administered. An intermittent dose schedule, given on alternate days or daily for 3-4 days with rest periods of 1-2 days in between, may be used for the continued control of edema. Dosage should be kept to a minimum with careful adjustments in dosage for patients with hepatic impairment. If the initial diuresis is inadequate, repeated doses may be administered q 2-3 h until the desired diuretic response is achieved or until a maximum daily dosage of 10 mg is administered. After reconstitution, ethacrynate sodium solution may be infused slowly (over 20-30 min) through the tubing of a running intravenous infusion or by direct intravenous injection over several minutes. If the desired diuresis is not achieved with the first dose of ethacrynate sodium, a second dose may be given after 2-3 h at a new injection site. Children Safety and effectiveness have not been established in children for intravenous administration and in infants for oral as well as intravenous administration. Preparations Edecrin (Merck): 25, 50 mg tablets Edecrin Sodium (Merck): 50 mg/vial, powder for injection 2. Dosage may be adjusted at 2550 mg increments daily until the desired response is achieved or until a maximum dose of 100 mg twice daily is given. A dose of 200 mg twice daily may be required to maintain adequate diuresis in patients with severe refractory edema. An intermittent dose schedule, given on alternate days or daily for 3-4 days with rest periods of 1-2 days in between, may be used for the continued control of edema after an effective diuresis is obtained. Intravenous formulations Intravenous administration of ethacrynate sodium should be reserved for patients in whom a rapid onset of diuresis is desired such as in acute pulmonary edema, or 3. The same dose may be repeated, or adjusted in increments of 20-40 mg q 6-8 h until the desired diuresis is achieved. The effective dose may then be given once or twice daily to maintain adequate fluid balance. For chronic maintenance therapy, furosemide given on alternate days or intermittently on 2-4 consecutive days each week is preferred. A maximum oral dose of 600 mg/d has been used in patients with severe fluid overload. Edema (intravenous formulation) the usual dose is 20-40 mg given as a single injection. The same dose may be repeated or adjusted in 20-40 mg increment q 1-2 h until the desired response is achieved. Furosemide has also been administered as a continuous intravenous infusion in some patients to maintain adequate urine flow. A bolus of 20-40 mg should be given first, followed by an infusion with an initial rate of 0. The infusion rate may be titrated up to a maximum of 4 mg/min according to clinical response. If adequate reduction in blood pressure is not achieved in 4-6 weeks, the dose may be increased up to 10 mg once daily. If the blood pressure response is still inadequate, an additional antihypertensive agent should be added. Preparations Demadex (Roche): 5, 10, 20, 100 mg tablets Demadex injection (Roche): 10 mg/mL Hypertension the usual initial dose is 40 mg orally twice daily; dosage should then be adjusted according to clinical response. These patients should be monitored closely to assure efficacy and avoid undesired toxicity. Children Safety and effectiveness have been established in children for the management of edema but not for hypertension. Preparations Furosemide (generic); Lasix (Aventis): 20, 40, 80 mg tablets Furosemide (generic); Lasix (Aventis): 10 mg/mL, 40 mg/5 mL oral solution Furosemide (generic); Lasix (Aventis): 10 mg/mL injection, in 2, 4, and 10 mL single-dose vials Thiazide Diuretics 1. Bendroflumethiazide (Available only in combination with nadolol-Corzide) Indications Hypertension (Corzide) Dosage Adults Hypertension the initial dose is 5 mg bendroflumethiazide + 40 mg nadolol once daily, eventually increasing to 5 mg/80 mg once daily if desired. Preparations Fixed-Dose Combinations for Treatment of Hypertension: Corzide 80/5-Bendroflumethiazide 5 mg/Nadolol 80 mg Corzide 40/5-Bendroflumethiazide 5 mg/Nadolol 40 mg 4. If the diuretic response is inadequate, the dose may be doubled until the desired response is achieved or until a maximum single dose of 200 mg is given. Hepatic cirrhosis the usual initial dose is 5-10 mg once daily administered orally or intravenously along with an aldosterone antagonist or a potassium-sparing diuretic.
500 mg tetracycline with mastercard
This candidate said that he would do an anterior deltopectoral approach to reduce the shoulder and went on to describe the approach bacteria en el estomago sintomas generic 500 mg tetracycline otc. Posterior approach to the shoulder Indications Routine approach to recurrent posterior instability of the shoulder Fixation of scapula and glenoid fractures Tumour surgery. Alternatively, beach chair position, sandbag under medial border scapula, head hand rest. Incision Mark out the outline of the acromion, clavicle and coracoid process beforehand with marker pen. A 5-cm longitudinal incision is made from the anterolateral tip of the acromion and is carried down the lateral aspect of the arm. Incision A linear incision is made over the entire length of the scapula spine, extending to the posterior corner of the acromion. Alternatively, a vertical incision may be used which is more cosmetic but provides poorer exposure of the joint. The incision is centred 2 cm inferomedially to the posterior corner of the acromion. Internervous plane There is no true internervous plane; the lateral approach involves splitting the deltoid muscle. Superficial surgical dissection Split the deltoid muscle in line with its fibres downwards for 5 cm from the acromion. Expose the subdeltoid portion of the subacromial bursa by retracting the deltoid muscle anteriorly and posteriorly. Internervous plane this approach uses the internervous plane between infraspinatus (suprascapular nerve) and teres minor (axillary). The plane between the deltoid and infraspinatus muscles may be difficult to define. Deep surgical dissection the lateral aspect of the upper humerus and its attached rotator cuff lie directly under the deltoid muscle and the subacromial bursa. Split the subacromial bursa and incise longitudinally to provide access to the upper lateral portion of head of humerus. A portion of the anterior deltoid can be reflected off the anterior edge of the acromion but must be carefully repaired at the end of the procedure. Rotating and abducting the arm brings different parts of the rotator cuff in to view in the floor of the wound. The incision can be extended superiorly and medially across the acromion and parallel to the upper margin of the spine of the scapula. Distally the axillary nerve has split at this level and can be identified on the undersurface of the deltoid and protected. Having done this, a second window on to the more distal humeral shaft can be created and is enhanced by partial release of the deltoid from its insertion. Deep dissection Deep dissection involves identifying the interval between infraspinatus and teres minor. This is an important plane that is difficult to define; it is best developed by blunt finger dissection. The fibres of infraspinatus muscle are multipennate, whereas the fibres of teres minor are unipennate. The posterior aspect of the shoulder joint capsule is now exposed and the joint entered by incising the joint capsule close to the glenoid. If a vertical incision is used, the tendon of infraspinatus needs to be divided 1 cm medial to its insertion in to the middle area on the greater tuberosity. During closure, the posterior third of deltoid is reattached to the spine of the scapula with absorbable sutures passed through drill holes in the scapula spine. To enhance access, the infraspinatus muscle can be detached 1 cm from its insertion in to the greater tuberosity. Structures at risk the axillary nerve runs though the quadrangular space beneath the teres minor. Dissection carried out inferior to teres minor can damage the axillary nerve, so it is critical to identify the muscular interval between infraspinatus and teres minor muscles correctly and stay within that plane. The suprascapular nerve passes around the base of the spine of the scapula as it runs from the supraspinous fossa to the infraspinous fossa. The infraspinatus muscle must not be retracted too far medially or neuropraxia may result from stretching the nerve. The posterior circumflex humeral artery runs with the axillary nerve in the quadrangular space and can be damaged, leading to troublesome haemorrhage. The radial nerve leaves the axilla by passing through the triangular interval bounded above by the teres major muscle. The circumflex scapular artery runs in a triangular space and forms part of the extremely rich blood supply to the scapula. Dissection between teres major and minor may damage this vessel, causing haemorrhage that is difficult to control. Internervous plane the anterior approach makes use of two different internervous planes. Proximally the plane lies between the deltoid muscle (axillary nerve) and the pectoralis major muscle (medial and lateral pectoral nerves). Distally the plane lies between the medial fibres of the brachialis muscle (musculocutaneous nerve) and the lateral fibres of the brachialis muscle (radial nerve). Surgical dissection Proximal humeral shaft the superficial and deep fasciae are divided in line with the skin incision. Identify the deltopectoral groove and separate the deltoid and pectoralis major muscles, and develop the muscular interval distally down to the insertion of the deltoid in to the deltoid tuberosity and the insertion of pectoralis major in to the lateral lip of the bicipital groove. Proximally detach the insertion of pectoralis major from the lateral bicipital groove and continue the dissection subperiosteally to expose the upper humerus. The anterior humeral artery crosses the field of dissection in a lateral direction and must be ligated. Proximally the incision can be extended and modified in to an anterior approach to the shoulder. Distal humeral shaft Distally incise the deep fascia of the arm in line with the skin incision. Identify the muscular interval between the biceps and the brachialis, and retract the biceps medially (beneath it is the anterior aspect of brachialis, which cloaks the humeral shaft). Split the fibres of brachialis longitudinally along its midline to expose the periosteum of the anterior surface of the humeral shaft. Anterolateral approach this approach gives access to the proximal and middle thirds of the humeral shaft. Structures at risk the radial nerve is vulnerable at two points as it courses along the humerus: 1. In the spiral groove at the back of the middle third of the humerus, dissect muscle from bone, starting in a subperiosteal plane without straying on to the posterior surface of the bone. In the anterior compartment of the distal third of the arm as it pierces the lateral intermuscular septum and lies between brachioradialis and brachialis muscles. Split brachialis along its midline; the lateral portion of the muscle then serves as a cushion. Axillary nerve with over-retraction of the deltoid Anterior circumflex humeral vessels cross the operative field and have to be sacrificed. Skin incision A longitudinal incision from the tip of the coracoid process extending laterally and distally along the deltopectoral groove to the deltoid tuberosity on the lateral aspect of the humerus, halfway down its shaft. Anterolateral approach to the distal humerus Exposes the distal quarter of the humerus. The major advantage over the brachialis-splitting anterior approach is that it can be extended both proximally and distally, whereas the brachialis-splitting approach cannot be extended distally. A sandbag is placed under the affected shoulder and there is no tourniquet as it will get in the way. Incision A longitudinal midline incision is made on the posterior aspect of the arm from 8 cm below the acromion to the olecranon fossa. Incision A curved longitudinal incision is made over the lateral border of biceps starting 10 cm proximal to the flexor crease of the elbow and ending just above the flexor crease of the elbow.
Diseases
- Post-infectious myocarditis
- Non functioning pancreatic endocrine tumor
- Hemochromatosis type 3
- Thiopurine S methyltranferase deficiency
- Membranoproliferative glomerulonephritis (type II)
- Polycystic kidney disease, adult type
- Renal dysplasia diffuse autosomal recessive
- Virus associated hemophagocytic syndrome
- Schereshevskij Turner
Order cheap tetracycline
The treatment is usually closed reduction antibiotics used for sinus infections uk discount tetracycline 250 mg overnight delivery, though more comminuted and displaced fractures will need open reduction and fixation. It results from a fall on a flexed wrist or a direct blow to the dorsum of the wrist. Photograph of the classic "dinner fork" deformity seen with dorsal radius fractures (left). Barton Fracture Barton fracture is a distal radius fracture in which the carpus displaces volarly with the radial fragment. A reverse Barton fracture is actually more common in which the carpus displaces dorsally with a fragment of the distal radius. Injuries may encompass two fractures at similar or separate sites or may involve a single fracture with ligamentous injury, with or without dislocation. Careful examination of the wrist and elbow joints is imperative, as these are commonly involved sites. Some common patterns are seen in forearm fractures and thus knowledge of these injury patterns is important. Both bones fractures (involving both the radius and ulnar shafts) are often seen in children secondary to falls on an outstretched hand. They are only rarely seen in adults and are then from high-energy mechanisms or severe direct impact. Closed reduction is often successful in children because small amounts of residual angulation will resolve with bone remodeling. Complete fractures are more common in adults, and open reduction is often required. The Monteggia fracture complex, first described in 1814, is a proximal ulnar fracture with an associated radial head dislocation. The injury is caused by forced pronation of the forearm during a fall on an outstretched hand. Radiographs easily reveal the proximal ulnar fracture, and in these cases the radial head should be carefully evaluated. In the normal position, the radial head should align with the capitellum when a line is drawn through the radial shaft. The injury occurs with a fall on an outstretched hand with wrist in extension and the forearm forcibly pronated, or with a direct blow to the dorsoradial aspect of the wrist. The anteroposterior radiograph reveals a fracture of the radius at the junction of the middle and distal thirds, and an increase in the joint space between the distal radius and ulna may be seen. In proximal ulnar fractures, the radial head should be carefully examined to exclude the presence of a Monteggia fracture. Associated injuries are rare but include compartment syndrome and vascular injury. Most undisplaced fractures are treated with plaster immobilization, while displaced fractures (>50% of width of ulna) may need open reduction. They are usually the result of a fall on an outstretched hand with arm extended and abducted. Most elbow dislocations (>90%) are posterior, and the patient will present with the elbow in 45 degrees of flexion, with a prominence of the olecranon process posteriorly. The collateral ligaments are torn, and careful neurovascular assessment is important as brachial artery and median nerve injuries can complicate this injury. Most often the coronoid process will slip posteriorly, but occasionally a fracture of the process will be noted. Reduction is performed under conscious sedation by countertraction with flexion of the elbow. The injury can result in damage to the articular surface, depression of the radial head, or an angulated fracture of the radial head and neck. Often a fracture is seen on radiographs, but they may reveal only a fat pad sign indicative of an effusion and an occult fracture. Nondisplaced or minimally displaced fractures are treated with a sling or posterior splint. Fractures that are displaced more than 3 mm or involve more than one-third of the joint surface are usually treated operatively with the insertion of small screws. Comminuted fractures are treated conservatively, though the treatment of severely comminuted and displaced fractures is controversial and includes excision of fragments and / or the radial head with or without the insertion of Silastic implants. Radial nerve injuries complicate up to 20% of humerus fractures, though median and ulnar nerves are rarely injured. Plain radiographs are most often diagnostic, and conservative treatment is used for the majority of closed injuries. Open fractures, severely comminuted fractures, and fractures that are not adequately aligned by closed reduction are treated with open reduction. Fractures of the humeral head most often occur in older patients after minor falls. Shoulder dislocations can be classified as anterior, posterior, or inferior (luxatio erecta). They are usually the result of a fall on an outstretched hand with the arm abducted, extended, and externally rotated. The humeral head is palpable anteriorly, and a slight hollow is noticed in the shoulder laterally. Standard radiography includes anteroposterior and lateral views and either a transscapular Y view or an axillary view. In addition, a small anteroinferior glenoid rim fracture called a Bankart lesion may be seen. They can be difficult to diagnose, and up to 50% are thought to be initially misdiagnosed. The injury occurs with an axial load on an adducted internally rotated and forward flexed arm, direct blow to the shoulder, or severe muscular contractions as from a seizure or electrical injury. The arm is usually internally rotated on exam, and the patient is unable to elevate the arm above 90 degrees. The anteroposterior radiograph may look nearly normal, and thus the transscapular Y view or the axillary view is necessary to exclude the diagnosis. There are four important radiographic findings associated with posterior shoulder dislocation: the "light bulb" sign (rotation of the trochanters in to an anteroposterior plane leaving the humeral head with the appearance of a light bulb), the deep sulcus sign (>6 mm distance between the humeral head and the glenoid rim), the "trough" sign (compression fracture of the humeral head resulting in two vertical parallel lines), and the rim or ellipse sign (loss of the usual elliptical overlap of the humeral head and the glenoid rim). Not all signs are present in a single patient but the presence of any of these signs suggests a posterior dislocation. Reduction is accomplished by slow in-line traction, usually with general anesthesia. Inferior dislocation, also known as luxatio erecta, is a very rare dislocation forming <1% of all shoulder dislocations. The injury occurs with forced abduction of the arm, and the patient presents with a fully abducted arm and the elbow flexed with the forearm on or behind the head. Neurovascular compromise is common because these structures are inferior to the joint. Plain radiographs easily demonstrate the dislocation, and closed reduction is usually successful with a two-stage procedure. First the dislocation is rotated downward with in-line traction and converted in to a simple anterior dislocation. In a minority of cases interposition of soft tissues makes closed reduction impossible and open reduction is required. Open shoulder dislocation is rare but invariably results in severe disruption of the brachial plexus and vascular supply to the arm because the skin is the last structure to tear. Localized tenderness is found on examination, and radiography easily delineates the fracture.
Purchase tetracycline us
On the anteroposterior radiograph bacteria jeopardy tetracycline 250 mg low price, compression fracture is seen as a loss of height of the vertebral body compared with the adjacent ones, loss of space between adjacent spinous processes, or loss of distance between the pedicles above and below the fracture. Separation of the pedicles laterally compared with those above or below suggests a burst fracture of the vertebral body. Consequently, plain radiographs reveal loss of vertebral height, increased anteroposterior and lateral diameters, and loss of the normal lordotic lines of alignment. The presence of both anterior and posterior step-offs is diagnostic for burst fracture. All suspicious findings on the initial three-view C-spine series must be delineated further. Treatment is immobilization of the neck for comfort with either a soft or hard cervical collar, as well as appropriate analgesia. Isolated fractures of a single pedicle or lamina are usually due to penetrating injury, most commonly a gunshot wound. Displacement of pedicle or laminar fragments medially can result in direct spinal cord injury. The lateral masses represent the lateral articulations of the spinal column and contain the facet joints. They also form the bony margins of the neural foramina through which nerve roots enter and exit the spinal cord. Consequently, fractures of the lateral masses are often associated with nerve root injury. If sufficient flexion or rotation occurs, one superior facet will become locked anterior to the inferior facet on that side. Oblique radiographs of the spine will often more clearly demonstrate the dislocation. Subluxation of the vertebral bodies is less than 50%, and approximately 25% will have associated spinal cord injury. Bilateral facet dislocation results from forced flexion of the neck, causing the superior facets to glide anteriorly on their inferior counterparts. Once the facet joints reach the peak of the inferior facet, they are said to be "perched" atop the inferior facet. If the superior facet continues anteriorly, it becomes locked in the dislocated position. Bilateral facet dislocation results in greater than 50% subluxation of the superior vertebral body on the inferior one and almost inevitably results in complete spinal cord injury. Both superior facets (C-5) are seen resting atop the lower facets (C-6), a condition known as perched facets. X-ray shows complete bilateral facet dislocation of C-3 on C-4 with significant anterior subluxation and angulation of C-3 (superior facets are lying anterior to the lower facets; see arrow). Consequently, it is essential to visualize this area with plain radiographs on the initial examination prior to clearing the cervical spine. Visualization of this area is difficult to accomplish in children, patients with large, muscular shoulders, and those with upper extremity injuries that make it difficult to pull on the arms for a lateral x-ray. The differential diagnosis, besides thoracic aortic injury and fracture of the sternum, should include fracture of the thoracic spine. Plain radiograph showing compression fracture of T-10 with anterior subluxation of T-9 on T-10 and a small fracture of the anterosuperior aspect of T-10 body. In addition, the anatomy of the thoracic vertebrae inherently limits lateral movement and extension. Fractures in this segment of the spine are commonly associated with spinal cord injury because of the limited amount of space for the cord within the spinal canal in this area. Penetrating injury in this area is another relatively common etiology for thoracic cord injury. Associated thoracoabdominal injuries may take precedence for stabilization, so it is important not to overlook the possibility of concurrent spinal injury. The chest x-ray often shows a widened upper mediastinum because of the presence of hematoma around the fracture. The radiological appearance is very similar to that in blunt trauma to the thoracic aorta. Visualization of the thoracic spine by plain radiographs is difficult on account of numerous overlying structures. The L-1 vertebral body shows a comminuted fracture with intrusion of bony fragments in to the spinal canal. The second group is made up of younger patients who sustain severe hyperflexion of the lumbar spine, usually during a fall from height. In these patients, associated injuries, such as calcaneal, acetabular, and other lower extremity fractures, mesenteric or renal arterial injury, aortic avulsion, and additional spinal column injuries, are common. Lumbar compression fracture occurs as a result of acute hyperflexion at the waist, resulting in an anteriorly wedge-shaped vertebral body. The posterior wall of the vertebra is intact, and spinal cord injury is very rare. Collapse of more than 30% of the anterior height may result in progressive collapse of the vertebral body and increasingly severe kyphosis. Consequently, fractures with greater than 30% anterior compression are treated more aggressively. Radiographically, these fractures appear wedge-shaped with loss of anterior vertebral height on the lateral view. The presence of 244 Spinal Injuries a burst fracture should be suspected if the anteroposterior view shows separation of the pedicles. Fractures of the transverse process, lateral mass, or vertebral body in the lumbar spine from L-2 to L-4 may be associated with renal injury. The patient sustains acute hyperflexion at the waist around the axis of the lap belt. The normal flexion point of the spine is located in the center of the vertebral body. An improperly worn lap belt shifts the flexion point anteriorly and acts as a fulcrum that pries apart the vertebral elements from back to front. There are several variations of Chance fracture, depending on the course of the fracture line. The impact on spinal stability is identical regardless of the exact course of the fracture because both posterior and anterior elements are disrupted. F fractures are commonly associated with blunt intestinal injury, and patients should be investigated for this possibility. The presence of a seatbelt sign on the lower abdomen should alert the clinician to the possibility of Chance fracture as well as intestinal injury. Nerve fibers supplying the pelvis and lower extremities continue distally as the cauda equina. Injuries to the lower lumbar vertebrae may produce injury to this structure, resulting in the cauda equina syndrome. This syndrome is characterized by the presence of asymmetric weakness and numbness of the lower extremities, often with saddle anesthesia of the perineum, as well as sphincter dysfunction of bowel and bladder. As with compression fractures, injury to the kidneys, ureters, and other retroperitoneal structures must be considered with lumbar fracture-dislocations. Pediatric Spinal Injury Cervical spine fractures are relatively rare in children because of the inherent flexibility of the pediatric spine. Soft tissue thickness may vary considerably depending on the phase of respiration. Incompletely calcified vertebrae cause vertebral bodies to appear wedge-shaped, suggesting possible compression fracture. Physiologic anterior subluxation of C-2 on C-3 or C-3 on C-4 occurs in up to 50% of children and persists until mid adolescence in 10% of patients. It is often difficult to obtain adequate open-mouth views of C-1 and C-2 in children because of their small mouths and inability to cooperate.
Order 500mg tetracycline amex
Therapy of Lisfranc fractures usually involves closed reduction with internal fixation using percutaneous Kirschner wires and casting virus 78 purchase 250 mg tetracycline free shipping. Avulsion fractures usually occur with sudden inversion of the plantar flexed foot. The insertion of the peroneus brevis has been implicated in these fractures by causing avulsion of the styloid process. Diaphyseal fractures usually occur with running or jumping injuries, and transverse fractures within 15 mm of the proximal bone are often termed Jones fractures. Complications of this diaphyseal fracture are common and include delayed union, nonunion, and recurrent fracture. These include bilateral calcaneal injuries, lower leg injury, and vertebral fractures. Typically, significant pain and deformity around the heel is noted, and weight-bearing is impossible. This angle is seen on the lateral view and is the angle between lines connecting the three highest points of the calcaneus. In addition, subtalar joint involvement is important to recognize, as many of these patients are treated operatively. Despite optimal therapy, chronic pain and joint dysfunction is seen in 50% of patients. Spoonamore and Demetrios Demetriades One of the most devastating consequences of trauma is spinal cord injury. In the United States, approximately 10,000 spinal cord injuries yearly result in permanent disability. In the United States most spinal cord injuries are caused by motor vehicle accidents (40%), violence (30%), falls (20%), and sports accidents (6%). Although spinal fractures can occur in any age group, the peak incidence is in males from ages 18 to 25. Certain conditions predispose to spinal fracture or dislocation: old age, rheumatoid arthritis, osteoporosis, and spinal stenosis. Forces that injure the spinal column include flexion, extension, axial loading, shear force, and rotational acceleration. The type and site of spine injuries depend on the mechanism of injury and the age of the victims. High-level falls are associated with spinal trauma in about 24% of cases and usually involve the lower thoracic and lumbar spine. Cervical spine injuries pose a special challenge because of the potential catastrophic consequences of any associated cord injury. The overall incidence of cervical spine injuries in blunt trauma is about 3% and increases with age. In the presence of severe head trauma the incidence of cervical spine trauma increases to about 9%. Very young or very old patients are more likely to suffer injuries of the upper cervical spine than younger adults who are more likely to have lower cervical injuries. In about 85% of blunt cervical spine injuries there is a fracture, in about 10% there is subluxation without fractures, and in about 4% there is isolated cord injury without fracture or dislocation. Very young or very old patients are more likely to suffer cord injuries without skeletal trauma than young adults. Clinical Examination All trauma victims must be thoroughly evaluated for the possibility of a spinal injury. Blunt trauma patients should have the spine immobilized at first medical contact and remain in spinal immobilization until the integrity of the cord and spinal column can be verified. In patients with multiple severe injuries, the spinal clearance can be deferred until more critical injuries have been addressed, provided that immobilization of the spine and adequate precautions are maintained. Patients with spinal fractures experience pain, and examination will reveal spinal tenderness on palpation and ecchymosis on inspection. However, patients who are unable to report pain because of concomitant head injury or intoxication may harbor occult spinal injuries and should remain immobilized until they can be accurately evaluated. Patients with spinal cord injury manifest symptoms according to the spinal cord level affected. With complete cord transection, all motor and sensory function below the level of the lesion is lost. The highest intact sensory level should be marked on the patient to determine whether the cord lesion is progressing proximally on subsequent examinations. Assessment of rectal tone and perianal sensation is important in detecting any sparing of lower cord segments which significantly improves the prognosis. Spinal shock is common in the immediate period after injury and consists of loss of all spinal reflexes and flaccid 207 paralysis below the level of the lesion. During this phase the bulbocavernosus reflex (anal sphincter contraction with stimulation of the glans or urethra) is absent. In many cases, no definitive prognostication regarding the severity or level of the spinal cord lesion can be made while spinal shock is present. Once the bulbocavernosus reflex returns, spinal shock is resolved, reflexes become spastic, and the lesion is complete. Priapism is common in males after complete cord transection but resolves quickly in most cases. Neurogenic shock is the hemodynamic effect of sympathetic denervation that results in vasodilation and hypotension. In high cervical cord injuries the hypotension is associated with severe bradycardia, because of disruption of the sympathetic innervation to the heart. Regardless of the presence of neurogenic shock, hypotension must be assumed to be due to hemorrhage and a diligent search for sources of blood loss must be made. Incomplete cord syndromes may present with a confusing pattern of neurologic deficits. In central cord syndrome, the hands and arms sustain a much denser bilateral paralysis than the lower extremities. With anterior spinal cord syndrome, there is preservation of posterior column function (position and vibration sense) bilaterally, but all other functions are lost. Neurologic deficits may be delayed many hours, and by definition, radiographs are normal. Investigations Trauma patients requiring cervical spine clearance can be classified in to one of three categories: asymptomatic, symptomatic, or nonevaluable (obtunded/ comatose). Patients who are fully alert, not intoxicated, have no significant distracting injuries, and who are asymptomatic (no neurological symptoms, no neck pain) can be cleared safely based on clinical examination alone without imaging studies. Trauma patients who present with neck pain, tenderness, spinal deformity, and/or neurologic symptoms or dysfunction require radiographic imaging. The standard radiological evaluation in a multiple trauma patient used to include a cervical spine series (anteroposterior, lateral, open mouth view). The clearance of the cervical spine in obtunded and comatose trauma patients remains controversial. Many serious complications occur during transportation of the critically injured patients.
500mg tetracycline with mastercard
There also is marked luminal narrowing (white arrow) by the band with distention of the gastric pouch above the band and slow emptying of barium in to the remaining stomach antibiotics for uti in babies generic tetracycline 250 mg line. A barium study shows distal slippage of the band (black arrows), with marked narrowing and obstruction of the gastric antrum (small white arrow) where it traverses the band. The stomach proximal to the band has twisted on itself with associated narrowing of the distal esophagus (large white arrows). The resulting gastric volvulus places the patient at high risk for gastric infarction and perforation, necessitating emergent surgery. In the operating room, the distended stomach was found to be quite cyanotic, but blood flow was immediately restored after the band was removed. A barium study shows how the laparoscopic band (black arrows) has eroded in to the lumen, so that it is surrounded on all sides by barium. Also note dilatation of the distal esophagus (white arrows) due to obstruction at the gastroesophageal junction by the migrated band. Intraluminal band erosion is an unusual complication that occurs when high intraluminal pressures generated by the band cause focal pressure necrosis and breakdown of the adjacent gastric wall, enabling the band to erode partly or even completely in to the lumen. Rarely, the band can even migrate in a retrograde fashion to the gastroesophageal junction, causing distal esophageal obstruction. Distribution of gastric ulcers by double-contrast barium meal with endoscopic correlation. Radiographically diagnosed antral gastritis: findings in patients with and without Helicobacter pylori infection. Serpiginous gastric erosions caused by aspirin and other nonsteroidal antiinflammatory drugs. Hypertrophied antral-pyloric fold: reassessment of radiographic findings in 40 patients. Lymphoid hyperplasia of the stomach: radiographic findings in five adult patients. The spectrum of radiographic features of aberrant pancreatic rests involving the stomach. Gastric mucosa-associated lymphoid tissue lymphoma: radiographic findings in six patients. Hyperirritable stomach as a cause of nausea and vomiting: clinical and radiographic findings. Usefulness of high-density barium for detection of leaks after esophagogastrectomy, total gastrectomy, and total laryngectomy. Complications after total gastrectomy and esophagojejunostomy: radiologic evaluation. Detection of strictures on upper gastrointestinal tract radiographic examinations after laparoscopic Roux-en-Y gastric bypass surgery: importance of projection. Using radiography to reveal chronic jejunal ischemia as a complication of gastric bypass surgery. Utility of routine barium studies after adjustments of laparoscopically inserted gastric bands. Intraluminal erosion and retrograde migration of laparoscopic gastric band with high-grade obstruction at gastroesophageal junction. Most ulcers detected on double contrast studies are less than 1 cm in size and some are as small as several millimeters. A major advantage of double contrast technique is its ability to demonstrate these tiny ulcer craters. In contrast, giant duodenal ulcers are defined as ulcers greater than 2 cm in size (see later section, Giant duodenal ulcers). Location About 90% of duodenal ulcers are located in the duodenal bulb and the other 10% in the postbulbar duodenum. Unlike gastric ulcers, which rarely develop on the anterior wall, as many as 50% of duodenal ulcers are located on the anterior wall of the bulb (the other 50% are on the posterior wall). A supine left posterior oblique spot image shows an ulcer (arrow) filling with barium on the posterior wall of the duodenal bulb. Morphologic features Bulbar ulcers Unlike gastric ulcers, duodenal ulcers are virtually always benign. The ulcers are often surrounded by a smooth radiolucent mound of edema and/or straight, symmetric folds that radiate directly to the edge of the ulcer crater. As in the stomach, ulcers on the posterior wall of the bulb generally fill with barium on routine double contrast radiographs obtained with the patient in supine or supine oblique positions. In contrast, ulcers on the anterior wall may appear as ring shadows due to barium coating the rim of the unfilled, non-dependent ulcer craters. In such cases, prone views with graded compression (using an inflatable compression balloon to thin out the barium pool) should be obtained to demonstrate filling of these anterior wall ulcers. Duodenal ulcers are often associated with considerable deformity of the bulb caused by edema and spasm accompanying the ulcer or by scarring from a previous ulcer. Conversely, an ulcer crater may be simulated by trapping of barium in portions of the deformed bulb, limiting the accuracy of the radiographic study. Nevertheless, symptomatic patients with a deformed bulb should probably be treated for an active ulcer because of the high risk of ulcer disease whether or not an ulcer is demonstrated with certainty. A supine left posterior oblique spot image shows a ring shadow (arrow) due to barium coating the rim of a nondependent anterior wall ulcer in the duodenal bulb. A prone compression view shows the anterior wall ulcer (arrow) filling with barium. There is an ulcer (arrow) on the medial wall of the proximal descending duodenum just above the papilla. Also note a large indentation of the lateral wall due to a marked degree of edema and spasm accompanying this postbulbar ulcer crater. There is marked narrowing (white arrows) of the proximal descending duodenum just above the papilla due to circumferential edema and spasm caused by a flat postbulbar ulcer (black arrow) that is barely visible on this image. Unlike bulbar ulcers, postbulbar duodenal ulcers are often greater than 1 cm in size. A large ulcer (large arrow) is seen in the proximal descending duodenum with marked narrowing (small arrows) proximal and distal to the ulcer because of severe edema and spasm. The presence of multiple ulcers in the distal duodenum should suggest Zollinger-Ellison syndrome, as uncomplicated postbulbar ulcers are almost always located above the papilla. This patient has a short, eccentric stricture (arrow) in the proximal descending duodenum due to scarring from a previous postbulbar ulcer. Focal scarring and fibrosis associated with healing of postbulbar ulcers can eventually lead to the development of a short segment of eccentric narrowing (also known as a ring stricture) in the proximal descending duodenum. Nevertheless, the duodenal bulb would be expected to change in size and shape at fluoroscopy, whereas these giant ulcers will have a fixed, unchanging configuration. There is a short segment of eccentric narrowing (arrow) with spiculated folds in the descending duodenum due to asymmetric compression by an annular pancreas. This patient has a long, tubular stricture (arrows) with an extremely smooth contour and tapered margins extending from the apex of the duodenal bulb in to the distal descending duodenum. There is an enormous ulcer crater (arrows) replacing almost the entire duodenal bulb. However, the fixed, unchanging size and shape of this collection at fluoroscopy should suggest the correct diagnosis. Ulcer healing and scarring Duodenal ulcers usually heal rapidly on treatment with antisecretory agents. Ulcer healing often leads to the development of an ulcer scar, manifested by radiating folds, bulbar deformity, or both. When radiating folds are present, they almost always converge at the site of the previous ulcer. In some cases, marked bulbar deformity may cause uninvolved segments of the bulb to balloon out between areas of fibrosis as one or more pseudodiverticula, producing a classic cloverleaf duodenum. Marked scarring of the duodenal bulb from previous ulcer disease has resulted in the development of multiple outpouchings or pseudodiverticula (arrows) between areas of retraction, producing a cloverleaf appearance. Pyloric channel ulcers Pyloric channel ulcers should be treated as gastric ulcers rather than as duodenal ulcers in terms of the need for aggressive evaluation to rule out an ulcerated carcinoma.