Purchase 40 mg benicar overnight delivery
Subsequent local tissue damage blood pressure levels chart discount 40mg benicar mastercard, embolic phenomena, and secondary autoimmune sequelae C. In subacute infection, symptoms include prolonged low-grade fever, weight loss, fatigue, myalgias, nausea, vomiting, and abdominal pain b. Roth spots: retinal hemorrhages with pale center that are caused by immune complex-mediated vasculitis d. Signs of embolic phenomena: cerebral infarction or hemorrhage, pulmonary embolism, and renal infarction g. Possible diagnosis requires 3 minor criteria or 1 major criterion and 1 minor criterion 2. Patients with endocarditis have persistent bacteremia; ~5 blood cultures should be collected in a 2-4-hour period b. Low complement, hematuria, and proteinuria suggest immune complex glomerulonephritis, which occurs with bacterial endocarditis. Vancomycin for empiric therapy; because most cases have positive blood cultures, treatment can be tailored to specific organism 3. Prognosis depends on severity of underlying heart disease and duration of infection 1. Single dose of amoxicillin recommended; cephalexin and clindamycin are alternatives for penicillin-allergic patients 3. Subcutaneous nodules: painless, pea-sized nodules found on extensor surfaces; rare (<2. Differential diagnosis: poststreptococcal reactive arthritis, 1E, juvenile rheumatoid. Symptoms: gradual onset of rhinorrhea, congestion, fever, hoarseness, barky cough,and,eventually,sbidor 2. Mild disease: rhinorrhea, congestion, coryza, fever, hoarseness, barky cough, stridor with agitation b. Signs of impending respiratory failure (rare): lethargy, decreased level of consciousness, severe retractions or stridor, poor aeration, tachycardia, cyanosis or pallor, apnea d. Differential diagnosis (Box 10-5): consider other diseases that present with upper airway obstruction and/or require specific therapies 2. Laboratory testing rarely indicated unless severe illness or need to evaluate for other etiologies b. Racemic epinephrine via nebulizer: requires observation for 3-4 hours after because some children relapse after drug wears off E. Typical clinical course: 1-2 days of upper respiratory symptoms followed by worsening stridor and respiratory distress with gradual resolution over 3-5 days G. Complications: secondary bacterial infection, hypoxemia; rarely respiratory failure, pulmonary edema, pneumothorax: H. Primarily lower airway viral infection, most common in children age <2 years with peak incidence in winter months 2. Affects 20% of all infants; 2% require hospitalization (most common cause of hospitalization ofU. Historical findings (Box 10~7): questions should mostly focus on illness sever~ ity and duration 2. Children age > 1 year may have asthma exacerbation triggered by viral illness; distinguishing these patients is difllcult, and optimal management is controversial b. May lead to increased use of antibiotics, which do not help disease and may harm patient viii. Indicated in severely ill infants and those not following typical disease progression 4. Patients admitted without oxygen requirement should have intermittent pulse oximetry with routine vitals rather than continuously, because transient dips are common in normal infants age <4 months D. Indications for hospitalization: poor hydration, increased respiratory distress, and impending respintory failure 2. In child who persistently desaturates, continuous pulse oximetry and oxygen therapy are indicated to keep pulse oximeter value >90% b. May lead to mild symptomatic improvement but does not affect course of illness in most patients ii. May lead to mild symptomatic improvement but does not affect course of illness in most patients iii. Reduces viscosity of mucus by osmotic pressure, allowing improved airway clearance ii. Several small studies have shown improvement of symptoms and reduced length of stay iii. No clear regimen established and variability of use among pediatric medical centers. Dehydration common because of insensible losses through fever, vomiting, diarrhea, and tachypnea c. Some may improve with respiratory function but be delayed in recovery of appetite, requiring longer hospital stays 6. Moderately effective (reduces likelihood of admission from -8% to +%) but extremely expensive iii. Includes fever, respiratory symptoms, and evidence of parenchymal lung involvement on physical exam or chest radiography 3. In North America, annual incidence of pneumonia is 36-40 cases/1,000 population younger than age 5 years C. True prevalence of various causes of pneumonia is unknown because less invasive tests. In children younger than 5 years old, pneumonia is most often viral in etiology a. Usually less severe clinical course than "typical" bacterial pathogens and often includes nonproductive cough, headache, pharyngitis 5. Ctyptococcus neofof1Tl811s Pneumocystis jiroveci Parasitic infections: Toxoplasma gondii. Results from invasion of virulent organism and failure of natural host defenses 2. Often results from upper or lower respiratory tract viral infection that weakens host defenses and causes decreased respiratory compliance a. Bacterial and viral pneumonias cause different clinical and pathophysiologic manifestations a. Typical bactuial pathogens usually cause lobar pn~ (inflammation and consolidation of lobe) or bronchopneumonia (infection of airways and surrounding interstitium) b. Viral and atypical pneumonias often cause bronchiolitis or interstitial pneumonitis (patterns can overlap) G. Older children: history of fever, cough, and increased work of breathing provide more helpful clues to diagnosis c. Older children: rales (crackles), wheezing, rhonchi, or diminished breath sounds may be heard on auscultation. Moderate to severe cases to determine severity of illness and try to establish etiology b. Includes several infectious and noninfectious diagnoses, especially in younger children i. Anatomic abnormalities: bronchogenic cyst, pulmonary sequestration, congenital cystic malformation, vascular ring ii. Aspiration of gastric contents: predisposing factors include neurologic impairment, neuromuscular weakness, and tracheoesophageal fistula b. In infants: viral bronchiolitis can present similar to bacterial pneumonia with fever, tachypnea, and cough c. In toddlers: foreign body aspiration must always be considered, especially with asymmetric exam on auscultation d. Laboratory studies are usually unnecessary in outpatients with uncomplicated pneumonia b. Various other laboratory studies are useful in specifte circumstances or when looking for more unusual pathogens i.
Diseases
- Roberts syndrome
- Chromosome 9 Ring
- Paraomphalocele
- Marfanoid hypermobility
- Exudative retinopathy familial, autosomal dominant
- Partial gigantism in context of NF
- Sclerotylosis
- Oligodactyly tetramelia postaxial
Cheap benicar on line
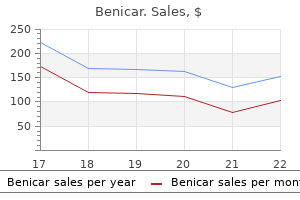
In this meta-analysis heart attack trey songz generic benicar 20 mg amex, a variety of strategies were effective, but the most effective ones were the use of team changes and the use of a case manager. When cost-effectiveness is considered in addition, it appears likely that an amalgam of strategies will be needed. However, the more expensive strategies, such as the use of case managers, probably will be implemented widely only if pay-forperformance takes hold. National State of Quality Measurement In the inpatient setting, quality measurement is now being performed by a very large proportion of hospitals for several conditions, including myocardial infarction, congestive heart failure, pneumonia, and surgical infection prevention; 20 measures are included in all. Analyses demonstrate substantial regional variation in quality and important differences among hospitals. Analyses by the Joint Commission for similar indicators reveal that performance on measures by hospitals has improved over time and that, as might be hoped, lower performers have improved more than higher performers. Public Reporting Overall, public reporting of quality data is becoming increasingly common. There are now commercial websites that have quality-related data for most regions of the United States, and these data can be accessed for a fee. The evidence to date indicates that patients have not made much use of such data but that the data have had an important effect on provider and organization behavior. Instead, patients have relied on provider reputation to make choices, partly because little information was available until very recently and the information that was available was not necessarily presented in ways that were easy for patients to access. Pay-for-Performance Currently, providers in the United States get paid exactly the same amount for a specific service, regardless of the quality of care delivered. The pay-for-performance theory suggests that, if providers are paid more for higher-quality care, they will invest in strategies that enable them to deliver that care. The current key issues in the pay-for-performance debate relate to (1) how effective it is, (2) what levels of incentives are needed, and (3) what perverse consequences are produced. The evidence on effectiveness is fairly limited, although a number of studies are ongoing. One problem is that, if incentives are tied to outcomes, there may be a tendency to transfer the sickest patients to other providers and systems. Another concern is that providers will pay too much attention to quality measures with incentives and ignore the rest of the quality picture. Nonetheless, it appears likely that, under health care reform, the use of various pay-for-performance schemes is likely to increase. A number of available interventions have been shown to improve the safety of care and should be used more widely; others are undergoing evaluation or soon will be. Quality also could be dramatically better, and the science of quality improvement continues to mature. Implementation of pay-for-performance should make it much easier for organizations to justify investments in improving safety and quality parameters, including health information technology. Measures of safety are still relatively immature and could be made much more robust; it would be particularly useful if organizations had measures they could use in routine operations to assess safety at a reasonable cost. Although the quality measures available are more robust than those for safety, they still cover a relatively small proportion of the entire domain of quality, and more measures need to be developed. The public and payers are demanding better information about safety and quality as well as better performance in these areas. The clear implication is that these domains will have to be addressed directly by providers. Industrialized or high-income countries experienced rapid improvement in standards of living, nutrition, health, and health care. Meanwhile, in low- and middle-income countries with much less favorable conditions, health and health care progressed much more slowly. The scale of this divide is reflected in the current extremes of life expectancy at birth, with Japan at the high end (83 years) and Sierra Leone at the low end (47 years). This nearly 40-year difference reflects the daunting range of health challenges faced by low- and middle-income countries. These nations must deal not only with a complex mixture of diseases (both infectious and chronic) and illness-promoting conditions but also, and more fundamentally, with the fragility of the foundations underlying good health. In the last decades of the twentieth century, the need to bridge this global health divide and establish health equity was increasingly recognized. The Declaration of Alma Ata in 1978 crystallized a vision of justice in health, regardless of income, gender, ethnicity, or education, and called for "health for all by the year 2000" through primary health care. While much progress has been made since the declaration, at the end of the first decade and a half of the twenty-first century, much remains to be done to achieve global health equity. This chapter looks first at the nature of the health challenges in lowand middle-income countries that underlie the health divide. It then outlines the values and principles of a primary health care approach, with a focus on primary care services. Next, the chapter reviews the experience of low- and middle-income countries in addressing health challenges through primary care and a primary health care approach. Finally, the chapter identifies how current challenges and global context provide an agenda and opportunities for the renewal of primary health care and primary care. Institute of Medicine encompassed many of these different usages, defining primary care as "the provision of integrated, accessible health care services by clinicians who are accountable for addressing a large majority of personal health care needs, developing a sustained partnership with patients, and practicing in the context of family and community. Primary care performs an essential function for health systems, providing the first point of contact when people seek health care, dealing with most problems, and referring patients onward to other services when necessary. As is increasingly evident in countries of all income levels, without strong primary care, health systems cannot function properly or address the health challenges of the communities they serve. The Declaration of Alma Ata, drafted in 1978 at the International Conference on Primary Health Care in Alma Ata (now Almaty in Kazakhstan), identified many features of primary care as being essential to achieving the goal of "health for all by the year 2000. The declaration drew from the experiences of low- and middle-income countries in trying to improve the health of their people following independence. Commonly, these countries had built hospital-based systems similar to those in high-income countries. This effort had resulted in the development of high-technology services in urban areas while leaving the bulk of the population without access to health care unless they traveled great distances to these urban facilities. Furthermore, much of the population lacked access to basic public health measures. Primary health care efforts aimed to move care closer to where people lived, to ensure their involvement in decisions about their own health care, and to address key aspects of the physical and social environment essential to health, such as water, sanitation, and education. After the Declaration of Alma Ata, many countries implemented reforms of their health systems based on primary health care. Most progress involved strengthening of primary care services; unexpectedly, however, much of this progress was seen in high-income countries, most of which constructed systems that made primary care available at low or no cost to their entire populations and that delivered the bulk of services in primary care settings. This endeavor also saw the reinforcement of family medicine as a specialty to provide primary care services. Even in the United States (an obvious exception to this trend), it became clear that the populations of states with more primary care physicians and services were healthier than those with fewer such resources. However, the target of "health for all by the year 2000" was missed by a large margin. The reasons were complex but partly entailed a general failure to implement all aspects of the primary health care approach, particularly work across sectors to address social and economic factors that affect health and provision of sufficient human and other resources to make possible the access to primary care attained in high-income countries. Furthermore, despite the consensus in Alma Ata in 1978, the global health community rapidly became fractured in its commitment to the far-reaching measures called for by the declaration. Economic recession tempered enthusiasm for primary health care, and momentum shifted to programs concentrating on a few priority measures such as immunization, oral rehydration, breastfeeding, and growth monitoring for child survival. Success with these initiatives supported the continued movement of health development efforts away from the comprehensive approach of primary health care and toward programs that targeted specific public health priorities. By the 1990s, primary health care had fallen out of favor in many global-health policy circles, and low- and middle-income countries were being encouraged to reduce public sector spending on health and to focus on cost-effectiveness analysis to provide a package of health care measures thought to offer the greatest health benefits. Average life expectancy in these countries lags far behind that in high-income countries: whereas the average life expectancy at birth in high-income countries is 74 years, it is only 68 years in middle-income countries and 58 years in lowincome countries. Initially, the situation in poor countries was characterized primarily in terms of high fertility and high infant, child, and maternal mortality rates, with most deaths and illnesses attributable to infectious or tropical diseases among remote, largely rural populations. With growing adult (and especially elderly) populations and changing lifestyles linked to global forces of urbanization, a new set of health challenges characterized by chronic diseases, environmental overcrowding, and road traffic injuries has emerged rapidly 1 Institute of Medicine.
Discount benicar line
Therefore arteria vitellina buy benicar 20mg mastercard, the size of the oral dose of such drugs should be reduced in this setting. Another consequence of severe heart failure is decreased gut perfusion, which may reduce drug absorption and, thus, lead to reduced or absent effects of orally administered therapies. Aging also results in changes in organ function, especially of the organs involved in drug disposition. Initial doses should be less than the usual adult dosage and should be increased slowly. Aging also results in a decrease in the size of, and blood flow to , the liver and possibly in the activity of hepatic drug-metabolizing enzymes; accordingly, the hepatic clearance of some drugs is impaired in the elderly. Exaggerated responses to cardiovascular drugs are also common because of the impaired responsiveness of normal homeostatic mechanisms. Conversely, the elderly display decreased sensitivity to -adrenergic receptor blockers. Adverse drug reactions are especially common in the elderly because of altered pharmacokinetics and pharmacodynamics, the frequent use of multidrug regimens, and concomitant disease. For example, use of long half-life benzodiazepines is linked to the occurrence of hip fractures in elderly patients, perhaps reflecting both a risk of falls from these drugs (due to increased sedation) and the increased incidence of osteoporosis in elderly patients. In population surveys of the noninstitutionalized elderly, as many as 10% had at least one adverse drug reaction in the previous year. Drug metabolism pathways mature at different rates after birth, and disease mechanisms may be different in children. In practice, doses are adjusted for size (weight or body surface area) as a first approximation unless agespecific data are available. Candidate gene Studies in Pharmacogenetics Most studies to date have used an understanding of the molecular mechanisms modulating drug action to identify candidate genes in which variants could explain variable drug responses. One very common scenario is that variable drug actions can be attributed to variability in plasma drug concentrations. In this case, the most obvious candidate genes are those responsible for drug metabolism and elimination. Other candidate genes are those encoding the target molecules with which drugs interact to produce their effects or molecules modulating that response, including those involved in disease pathogenesis. However, it is unusual for a drug response phenotype to be accurately measured in more than one family member, let alone across a kindred. Ultra-rapid metabolizers with especially high enzymatic activity (occasionally due to gene duplication;. Polymorphisms in genes encoding drug uptake or drug efflux transporters may be other contributors to variability in drug delivery to target sites and, hence, in drug effects. Ultra-rapid metabolizers may require very high dosages of tricyclic antidepressants to achieve a therapeutic effect and, with codeine, may display transient euphoria and nausea due to very rapid generation of morphine. In addition, some studies suggest that omeprazole and possibly other proton pump inhibitors phenocopy this effect. These variant alleles are associated with increased rates of neurologic complications with phenytoin, hypoglycemia with glipizide, and reduced warfarin dose required to maintain stable anticoagulation. Further, 6-mercaptopurine is itself an active metabolite of the immunosuppressive azathioprine. On the other hand, homozygotes for fully functional alleles may display less anti-inflammatory or antileukemic effect with the drugs. Slow acetylators have an increased incidence of the drug-induced lupus syndrome during procainamide and hydralazine therapy and of hepatitis with isoniazid. Polymorphisms in the 2-receptor gene have also been associated with response to inhaled 2-receptor agonists, while those in the 1-adrenergic receptor gene have been associated with variability in heart rate slowing and blood pressure lowering. In addition, in heart failure, a common polymorphism in the 1-adrenergic receptor gene has been implicated in variable clinical outcome during therapy with the investigational beta blocker bucindolol. Response to the 5-lipoxygenase inhibitor zileuton in asthma has been linked to polymorphisms that determine the expression level of the 5-lipoxygenase gene. Drugs may also interact with genetic pathways of disease to elicit or exacerbate symptoms of the underlying conditions. Tumor and Infectious Agent genomes the actions of drugs used to treat infectious or neoplastic disease may be modulated by variants in these nonhuman germline genomes. Genotyping tumors is a rapidly evolving approach to target therapies to underlying mechanisms and to avoid potentially toxic therapy in patients who would derive no benefit (Chap. Trastuzumab, which potentiates anthracycline-related cardiotoxicity, is ineffective in breast cancers that do not express the herceptin receptor. A decision to adopt pharmacogenetically guided dosing for a given drug depends on multiple factors. The most important are the magnitude and clinical importance of the genetic effect and the strength of evidence linking genetic variation to variable drug effects. The evidence can be strengthened if statistical arguments from clinical trial data are complemented by an understanding of underlying physiologic mechanisms. When the evidence is compelling, alternate therapies are not available, and there are clear recommendations for dosage adjustment in subjects with variants, there is a strong argument for deploying genetic testing as a guide to prescribing. In other situations, the arguments are less compelling: the magnitude of the genetic effect may be smaller, the consequences may be less serious, alternate therapies may be available, or the drug effect may be amenable to monitoring by other approaches. Ongoing clinical trials are addressing the utility of preprescription genotyping in large populations exposed to drugs with known pharmacogenetic variants. Importantly, technological advances are now raising the possibility of inexpensive whole genome sequencing. While barriers to bringing genomic and pharmacogenomic information to the bedside seem daunting, the field is very young and evolving rapidly. Indeed, one major result of understanding the role of genetics in drug action has been improved screening of drugs during the development process to reduce the likelihood of highly variable metabolism or unanticipated toxicity. Interactions must be considered in the differential diagnosis of any unusual response occurring during drug therapy. While it is unrealistic to expect the practicing physician to memorize these, certain drugs consistently run the risk of generating interactions, often by inhibiting or inducing specific drug elimination pathways. Accordingly, when these drugs are started or stopped, prescribers must be especially alert to the possibility of interactions. Drugs such as histamine H2-receptor antagonists or proton pump inhibitors that alter gastric pH may decrease the solubility and hence absorption of weak bases such as ketoconazole. If a drug dose is stabilized in the presence of an inducer that is subsequently stopped, major toxicity can occur as clearance returns to preinduction levels and drug concentrations rise. Individuals vary in the extent to which drug metabolism can be induced, likely through genetic mechanisms. Interactions that inhibit the bioactivation of prodrugs will decrease drug effects (Table 5-1). Interactions that decrease drug delivery to intracellular sites of action can decrease drug effects: tricyclic antidepressants can blunt the antihypertensive effect of clonidine by decreasing its uptake into adrenergic neurons. In contrast to induction, new protein synthesis is not involved, and the effect develops as drug and any inhibitor metabolites accumulate (a function of their elimination half-lives). However, some drugs are especially potent as inhibitors (and occasionally may not even be substrates) of specific drug elimination pathways, and so it is in the use of these agents that clinicians must be most alert to the potential for interactions (Table 5-3). The consequences of such interactions will depend on the drug whose elimination is being inhibited (see "The Concept of High-Risk Pharmacokinetics," above). Similarly, calcium channel blockers have been deliberately coadministered with cyclosporine to reduce its clearance and thus its maintenance dosage and cost. When allopurinol, an inhibitor of xanthine oxidase, is administered with standard doses of azathioprine or 6-mercaptopurine, life-threatening toxicity (bone marrow suppression) can result. A number of drugs are secreted by the renal tubular transport systems for organic anions. Salicylate, for example, reduces the renal clearance of methotrexate, an interaction that may lead to methotrexate toxicity. Renal tubular secretion contributes substantially to the elimination of penicillin, which can be inhibited (to increase its therapeutic effect) by probenecid. Similarly, inhibition of the tubular cation transport system by cimetidine decreases the renal clearance of dofetilide. Thus, coadministration of these nitrates with sildenafil can cause profound hypotension, which can be catastrophic in patients with coronary disease.
Best buy for benicar
Thus arrhythmia high blood pressure order generic benicar online, a negative study is reassuring, but a positive study is a relatively weak predictor of a "hard" perioperative cardiac event. One recent clinical trial further suggests that after 6 months, bare metal and drug eluting stents may not pose a threat. Rather, a discriminative approach based on clinical risk categorization appears to be both clinically useful and cost-effective. However, evidence does not support aggressive attempts to identify patients at intermediate risk who have asymptomatic but advanced coronary artery disease, in whom coronary revascularization appears to offer little advantage over medical therapy. Cardiac events include myocardial infarction, pulmonary edema, ventricular fibrillation, cardiac asystole, and complete heart block. For patients undergoing noncardiac surgery and currently taking statins, statin therapy should be continued to reduce perioperative cardiac risk. A substantial increase in perioperative bleeding and in the need for transfusion in patients receiving dual antiplatelet therapy has been observed. If clinicians elect to withhold antiplatelet agents prior to surgery, these agents should be restarted as soon as possible postoperatively. Inhaled anesthetics have predictable circulatory and respiratory effects: all decrease arterial pressure in a dose-dependent manner by reducing sympathetic tone and causing systemic vasodilation, myocardial depression, and decreased cardiac output. Inhaled anesthetics also cause respiratory depression, with diminished responses to both hypercapnia and hypoxemia, in a dose-dependent manner; in addition, these agents have a variable effect on heart rate. Prolonged residual neuromuscular blockade also increases the risk of postoperative pulmonary complications due to reduction in functional residual lung capacity, loss of diaphragmatic and intercostal muscle function, atelectasis, and arterial hypoxemia from ventilation-perfusion mismatch. Several meta-analyses have shown that rates of pneumonia and respiratory failure are lower among patients receiving neuroaxial anesthesia (epidural or spinal) rather than general anesthesia (inhaled). However, there were no significant differences in cardiac events between the two approaches. Evidence from a meta-analysis of randomized controlled trials supports postoperative epidural analgesia for >24 h for the purpose of pain relief. However, the risk of epidural hematoma in the setting of systemic anticoagulation for venous thromboembolism prophylaxis (see below) and postoperative epidural catheterization must be considered. The guidelines from the American College of Physicians recommend the following: 1. All patients undergoing noncardiac surgery should be assessed for risk of pulmonary complications (Table 9-5). Graduated compression stockings and pneumatic compression devices are useful supplements to anticoagulant therapy. Patients at higher risk of pulmonary complications should undergo incentive spirometry, deep-breathing exercises, cough encouragement, postural drainage, percussion and vibration, suctioning and ambulation, intermittent positive-pressure breathing, continuous positive airway pressure, and selective use of a nasogastric tube for postoperative nausea, vomiting, or symptomatic abdominal distention to reduce postoperative risk (Table 9-6). Routine preoperative spirometry and chest radiography should not be used routinely for predicting risk of postoperative pulmonary complications but may be appropriate for patients with chronic obstructive pulmonary disease or asthma. Spirometry is of value before lung resection in determining candidacy for coronary artery bypass; however, it does not provide a spirometric threshold for extrathoracic surgery below which the risks of surgery are unacceptable. Pulmonary artery catheterization, administration of total parenteral nutrition (as opposed to no supplementation), or total enteral nutrition has no benefit in reducing postoperative pulmonary complications. Patients whose diabetes is diet controlled may proceed to surgery with close postoperative monitoring. In 2010, according to the Centers for Disease Control and Prevention, 2,468,435 individuals died in the United States (Table 10-1). The epidemiology of mortality is similar in most developed countries; cardiovascular diseases and cancer are the predominant causes of death, a marked change since 1900, when heart disease caused ~8% of all deaths and cancer accounted for <4% of all deaths. It is estimated that in developed countries ~70% of all deaths are preceded by a disease or condition, making it reasonable to plan for dying in the foreseeable future. Cancer has served as the paradigm for terminal care, but it is not the only type of illness with a recognizable and predictable terminal phase. Many patients with illness-related suffering also can benefit from palliative care regardless of prognosis. Ideally, palliative care should be considered part of comprehensive care for all patients. Palliative care can be improved by coordination between caregivers, doctors, and patients for advance care planning, as well as dedicated teams of physicians, nurses, and other providers. The rapid increases in life expectancy in developed countries over the last century have been accompanied by new difficulties facing individuals, families, and society as a whole in addressing the needs of an aging population. These challenges include both more complicated conditions and technologies to address them at the end of life. The development of technologies that can prolong life without restoring full health has led many Americans to seek out alternative end-of-life care settings and approaches that relieve suffering for those with terminal diseases. Over the last few decades in the United States, a significant change in the site of death has occurred that coincides with patient and family preferences. By 2000, the trend was reversing, with ~31% of Americans dying as hospital inpatients. In the last decade, it has been associated with the increased use of hospice care; in 2008, approximately 39% of all decedents in the United States received such care. About 79% of patients receiving hospice care die out of the hospital, and around 42% of those receiving hospice care die in a private residence. Consequently, providing optimal palliative and end-of-life care requires ensuring that appropriate services are available in a variety of settings, including noninstitutional settings. Terminally ill patients have a wide variety of advanced diseases, often with multiple symptoms that demand relief, and require noninvasive therapeutic regimens to be delivered in flexible care settings. Fundamental to ensuring quality palliative and end-of-life care is a focus on four broad domains: (1) physical symptoms; (2) psychological symptoms; (3) social needs that include interpersonal relationships, caregiving, and economic concerns; and (4) existential or spiritual needs. A comprehensive assessment screens for and evaluates needs in each of these four domains. Goals for care are established in discussions with the patient and/or family, based on the assessment in each of the domains. Because failing to address any one of the domains is likely to preclude a good death, a well-coordinated, effectively communicating interdisciplinary team takes on special importance in end-of-life care. The assessment of physical and mental symptoms should follow a modified version of the traditional medical history and physical examination that emphasizes symptoms. Further research on and validation of these assessment tools, especially taking into account patient perspectives, could improve their effectiveness. These instruments are long and may be useful for initial clinical or for research assessments. Shorter instruments are useful for patients whose performance status does not permit comprehensive assessments. Suitable shorter instruments include the Condensed Memorial Symptom Assessment Scale, the Edmonton Symptom Assessment System, the M. Using such instruments ensures that the assessment is comprehensive and does not focus only on pain and a few other physical symptoms. Invasive tests are best avoided in end-of-life care, and even minimally invasive tests should be evaluated carefully for their benefit-to-burden ratio for the patient. Aspects of the physical examination that are uncomfortable and unlikely to yield useful information can be omitted. Regarding social needs, health care providers should assess the status of important relationships, financial burdens, caregiving needs, and access to medical care. Relevant questions will include the following: How often is there someone to feel close to Helpful assessment questions can include the following: How much are you able to find meaning since your illness began In addition, it can be helpful to ask how the patient perceives his or her care: How much do you feel your doctors and nurses respect you If concern is detected in any of these areas, deeper evaluative questions are warranted. Communication Especially when an illness is life-threatening, there are many emotionally charged and potentially conflict-creating moments, collectively called "bad news" situations, in which empathic and effective communication skills are essential. Although these conversations can be difficult and lead to tension, research indicates that end-of-life discussions can lead to earlier hospice referrals rather than overly aggressive treatment, benefiting quality of life for patients and improving the bereavement process for families.
Indian Gentian (Chirata). Benicar.
- Are there safety concerns?
- Dosing considerations for Chirata.
- Fever, malaria, constipation, worm infestations, upset stomach, loss of appetite, skin diseases, and cancer.
- What is Chirata?
- How does Chirata work?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96616
Cheap benicar 40 mg without prescription
Injection studies are sometimes used diagnostically to help determine the anatomic source of back pain iglesias heart attack buy discount benicar 20 mg. The use of discography to provide evidence that a specific disk is the pain generator is not recommended. Pain relief following a glucocorticoid injection into a facet is commonly used as evidence that the facet joint is the pain source; however, the possibility that the response was a placebo effect or due to systemic absorption of the glucocorticoids is difficult to exclude. Another category of intervention for chronic back pain is electrothermal and radiofrequency therapy. Intradiskal therapy has been proposed using both types of energy to thermocoagulate and destroy nerves in the intervertebral disk, using specially designed catheters or electrodes. Radiofrequency denervation is sometimes used to destroy nerves that are thought to mediate pain, and this technique has been used for facet joint pain (with the target nerve being the medial branch of the primary dorsal ramus), for back pain thought to arise from the intervertebral disk (ramus communicans), and radicular back pain (dorsal root ganglia). A few small trials have produced conflicting results for facet joint and diskogenic pain. A trial in patients with chronic radicular pain found no difference between radiofrequency denervation of the dorsal root ganglia and sham treatment. Each of these studies included patients with back pain and a degenerative disk, but no sciatica. Three of the four trials concluded that lumbar fusion surgery was no more effective than highly structured, rigorous rehabilitation combined with cognitive-behavioral therapy. The fourth trial found an advantage of fusion surgery over haphazard "usual care," which appeared to be less effective than the structured rehabilitation in other trials. Food and Drug Administration approved for uncomplicated patients needing single-level surgery at the L3-S1 levels. The disks are generally designed as metal plates with a polyethylene cushion sandwiched in between. The trials that led to approval of these devices compared them to spine fusion and concluded that the artificial disks were "not inferior. Intensive multidisciplinary rehabilitation programs may involve daily or frequent physical therapy, exercise, cognitive-behavioral therapy, a workplace evaluation, and other interventions. For patients who have not responded to other approaches, such programs appear to offer some benefit. Systematic reviews suggest that the evidence is limited and benefits are incremental. These treatments are also not recommended in guidelines from the American College of Physicians and the American Pain Society. On the other hand, exercise therapy and treatment of depression appear to be useful and underused. The term sciatica is used when the leg pain radiates posteriorly in a sciatic or L5/S1 distribution. The prognosis for acute low back and leg pain with radiculopathy due to disk herniation is generally favorable, with most patients showing substantial improvement over months. Serial imaging studies suggest spontaneous regression of the herniated portion of the disk in two-thirds of patients over 6 months. Nonetheless, there are several important treatment options to provide symptomatic relief while this natural healing process unfolds. Randomized trial evidence suggests that bed rest is ineffective for treating sciatica as well as back pain alone. Epidural glucocorticoid injections have a role in providing temporary symptom relief for sciatica due to a herniated disk. However, there does not appear to be a benefit in terms of reducing subsequent surgical interventions. Diagnostic nerve root blocks have been advocated to determine if pain originates from a specific nerve root. However, improvement may result even when the nerve root is not responsible for the pain; this may occur as a placebo effect, from a pain-generating lesion located distally along the peripheral nerve, or from effects of systemic absorption. Surgery is also an important option for patients who have disabling radicular pain despite optimal conservative treatment. For patients who have not improved, randomized trials indicate that, compared to nonsurgical treatment, surgery results in more rapid pain relief. However, after the first year or two of follow-up, patients with sciatica appear to have much the same level of pain relief and functional improvement with or without surgery. Thus, both treatment approaches are reasonable, and patient preferences and needs. Some patients will want the fastest possible relief and find surgical risks acceptable. Others will be more risk-averse and more tolerant of symptoms and will choose watchful waiting if they understand that improvement is likely in the end. The usual surgical procedure is a partial hemilaminectomy with excision of the prolapsed disk (diskectomy). Fusion of the involved lumbar segments should be considered only if significant spinal instability is present. The costs associated with lumbar interbody fusion have increased dramatically in recent years. There are no large prospective, randomized trials comparing fusion to other types of surgical intervention. In one study, patients with persistent low back pain despite an initial diskectomy fared no better with spine fusion than with a conservative regimen of cognitive intervention and exercise. Artificial disks have been in use in Europe for the past decade; their utility remains controversial in the United States. Many of the prior comments made regarding causes of low back pain also apply to disorders of the cervical spine. Pain arising from the brachial plexus, shoulder, or peripheral nerves can be confused with cervical spine disease (Table 22-4), but the history and examination usually identify a more distal origin for the pain. Cervical spine trauma, disk disease, or spondylosis with intervertebral foraminal narrowing may be asymptomatic or painful and can produce a myelopathy, radiculopathy, or both. The same risk factors for serious causes of low back pain also apply to neck pain with the additional feature that neurologic signs of myelopathy (incontinence, sensory level, spastic legs) may also occur. Motor vehicle accidents, violent crimes, or falls account for 87% of cervical spinal cord injuries (Chap. Immediate immobilization of the neck is essential to minimize further spinal cord injury from movement of unstable cervical spine segments. The Canadian C-spine rule recommends that imaging should be obtained following neck region trauma if the patient is >65 years old or has limb paresthesias or if there was a dangerous mechanism for the injury. These guidelines are helpful but must be tailored to individual circumstances; for example, patients with advanced osteoporosis, glucocorticoid use, or cancer may warrant imaging after even mild trauma. Whiplash injury is due to rapid flexion and extension of the neck, usually in automobile accidents. This diagnosis should not be applied to patients with fractures, disk herniation, head injury, focal neurologic findings, or altered consciousness. Up to 50% of persons reporting whiplash injury acutely have persistent neck pain 1 year later. Imaging of the cervical spine is not cost-effective acutely but is useful to detect disk herniations when symptoms persist for >6 weeks following the injury. Neck pain, stiffness, and a range of motion limited by pain are the usual manifestations. In young adults, acute nerve root compression from a ruptured cervical disk is often due to trauma. Typical patterns of reflex, sensory, and motor changes that accompany cervical nerve root lesions are summarized in Table 22-4. Although the classic patterns are clinically helpful, there are numerous exceptions because (1) there is overlap in sensory function between adjacent nerve roots, (2) symptoms and signs may be evident in only part of the injured nerve root territory, and (3) the location of pain is the most variable of the clinical features. Osteophytes, disk protrusions, or hypertrophic facet or uncovertebral joints may alone or in combination compress one or several nerve roots at the intervertebral foramina; these causes together account for 75% of cervical radiculopathies. When little or no neck pain accompanies cervical cord involvement, other diagnoses to be considered include amyotrophic lateral sclerosis (Chap. The possibility of cervical spondylosis should be considered even when the patient presents with symptoms or signs in the legs only.
Proven benicar 20 mg
Abdominal and rectal examinations should be performed to exclude impaction or acute abdomen prehypertension 133 purchase benicar overnight delivery. A number of constipation assessment scales are available, although guidelines issued in the Journal of Palliative Medicine did not recommend them for routine practice. Radiographic assessments beyond a simple flat plate of the abdomen in cases in which obstruction is suspected are rarely necessary. InterventIon Intervention to reestablish comfortable bowel habits and relieve pain and discomfort should be the goals of any measures to address constipation during end-of-life care. Although physical activity, adequate hydration, and dietary treatments with fiber can be helpful, each is limited in its effectiveness for most seriously ill patients, and fiber may exacerbate problems in the setting of dehydration and if impaired motility is the etiology. Stimulant and osmotic laxatives, stool softeners, fluids, and enemas are the mainstays of therapy (Table 10-5). In preventing constipation from opioids and other medications, a combination of a laxative and a stool softener (such as senna and docusate) should be used. If after several days of treatment, a bowel movement has not occurred, a rectal examination to remove impacted stool and place a suppository is necessary. For patients with impending bowel obstruction or gastric stasis, octreotide to reduce secretions can be helpful. For patients in whom the suspected mechanism is dysmotility, metoclopramide can be helpful. An example of nausea that most likely is mediated by the cortex is anticipatory nausea before a dose of chemotherapy or other noxious stimuli. InterventIon Medical treatment of nausea is directed at the anatomic and receptor-mediated cause that a careful history and physical examination reveals. When a single specific cause is not found, many advocate beginning treatment with a dopamine antagonist such as haloperidol or prochlorperazine. Give a dose every hour until the patient is relaxed, then provide a dose for maintenance 0. Frequently, the specific etiology cannot be identified, and dyspnea is the consequence of progression of the underlying disease that cannot be treated. The anxiety caused by dyspnea and the choking sensation can significantly exacerbate the underlying dyspnea in a negatively reinforcing cycle. InterventIons When reversible or treatable etiologies are diagnosed, they should be treated as long as the side effects of treatment, such as repeated drainage of effusions or anticoagulants, are less burdensome than the dyspnea itself. More aggressive treatments such as stenting a bronchial lesion may be warranted if it is clear that the dyspnea is due to tumor invasion at that site and if the patient and family understand the risks of such a procedure. Low-dose opioids reduce the sensitivity of the central respiratory center and the sensation of dyspnea. If patients are not receiving opioids, weak opioids can be initiated; if patients are already receiving opioids, morphine or other strong opioids should be used. Controlled trials do not support the use of nebulized opioids for dyspnea at the end of life. Benzodiazepines can be helpful if anxiety is present but should be neither used as first-line therapy nor used alone in the treatment of dyspnea. If the patient has pulmonary edema due to heart failure, diuresis with a medication such as furosemide is indicated. There are conflicting data on its effectiveness for patients with proven hypoxemia. But there is no clear benefit of oxygen compared to room air for nonhypoxemic patients. Noninvasive positive-pressure ventilation using a facemask or nasal plugs may be used for some patients for symptom relief. For some families and patients, oxygen is distressing; for others, it is reassuring. More general interventions that medical staff can do include sitting the patient upright, removing smoke or other irritants such as perfume, ensuring a supply of fresh air with sufficient humidity, and minimizing other factors that can increase anxiety. When decreased motility is suspected, metoclopramide can be an effective treatment. Clinicians should attempt prevention of postchemotherapy nausea rather than provide treatment after the fact. Current clinical guidelines recommend tailoring the strength of treatments to the specific emetic risk posed by a specific chemotherapy drug. When a vestibular cause (such as "motion sickness" or labyrinthitis) is suspected, antihistamines such as meclizine (whose primary side effect is drowsiness) or anticholinergics such as scopolamine can be effective. Dyspnea is among the most distressing physical symptoms and can be even more distressing than pain. Consequently, measurements of oxygen saturation through pulse oximetry or blood gases are rarely helpful in guiding therapy. Guidelines recommend visual or analogue dyspnea scales to assess the severity of symptoms and the effects of treatment. Potentially reversible or treatable causes of dyspnea include infection, pleural effusions, pulmonary emboli, pulmonary edema, asthma, and tumor encroachment on the airway. However, the risk-versus-benefit ratio of the diagnostic and therapeutic interventions for patients with little time left to live must be considered carefully before one undertakes etIology the multiple causes of fatigue in the terminally ill can be categorized as resulting from the underlying disease; from diseaseinduced factors such as tumor necrosis factor and other cytokines; and from secondary factors such as dehydration, anemia, infection, hypothyroidism, and drug side effects. Apart from low caloric intake, loss of muscle mass and changes in muscle enzymes may play an important role in fatigue of terminal illness. Finally, depression and other causes of psychological distress can contribute to fatigue. Scales used to measure fatigue, such as the Edmonton Functional Assessment Tool, the Fatigue SelfReport Scales, and the Rhoten Fatigue Scale, are usually appropriate for research rather than clinical purposes. Such a scale allows for assessment over time and correlates with overall disease severity and prognosis. InterventIons For some patients, there are reversible causes such as anemia, but for most patients at the end of life, fatigue will not be "cured. Behavioral interventions should be used to avoid blaming the patient for inactivity and to educate both the family and the patient that the underlying disease causes physiologic changes that produce low energy levels. Practically, this may mean reducing routine activities such as housework and cooking or social events outside the house and making it acceptable to receive guests lying on a couch. At the same time, institution of exercise regimens and physical therapy can raise endorphins, reduce muscle wasting, and reduce the risk of depression. In addition, ensuring good hydration without worsening edema may help reduce fatigue. Discontinuing medications that worsen fatigue may help, including cardiac medications, benzodiazepines, certain antidepressants, or opioids if pain is well-controlled. As end-of-life care proceeds into its final stages, fatigue may protect patients from further suffering, and continued treatment could be detrimental. There are woefully few pharmacologic interventions that target fatigue and weakness. Dexamethasone is preferred for its once-a-day dosing and minimal mineralocorticoid activity. Doses should be given in the morning and at noon to minimize the risk of counterproductive insomnia. Modafinil, developed for narcolepsy, has shown some promise in the treatment of severe fatigue and has the advantage of once-daily dosing. Anecdotal evidence suggests that L-carnitine may improve fatigue, depression, and sleep disruption. Many people believe that depression is normal among seriously ill patients because they are dying. Although sadness, anxiety, anger, and irritability are normal responses to a serious condition, they are typically of modest intensity and transient.
Buy generic benicar canada
Hyperthyroidism is most difficult to control in the first trimester of pregnancy and easiest to control in the third trimester blood pressure stroke range order benicar mastercard. Part of the reduction in hemoglobin concentration is dilutional, but iron and folate deficiencies are major causes of correctable anemia during pregnancy. Hemoglobinopathies can be associated with increased maternal and fetal morbidity and mortality. Management is tailored to the specific hemoglobinopathy and is generally the same for both pregnant and nonpregnant women. Prenatal diagnosis of hemoglobinopathies in the fetus is readily available and should be discussed with prospective parents either prior to or early in pregnancy. The majority of cases are benign gestational thrombocytopenias, but the differential diagnosis should include immune thrombocytopenia (Chap. Therapy with glucocorticoids should follow the guidelines established for nonpregnant patients. Entrapment neuropathies are common in the later stages of pregnancy, presumably as a result of fluid retention. Carpal tunnel syndrome (median nerve) presents first as pain and paresthesia in the hand (often worse at night) and later with weakness in the thenar muscles. Treatment is generally conservative; wrist splints may be helpful, and glucocorticoid injections or surgical section of the carpal tunnel can usually be postponed. Meralgia paresthetica (lateral femoral cutaneous nerve entrapment) consists of pain and numbness in the lateral aspect of the thigh without weakness. Patients are usually reassured to learn that these symptoms are benign and can be expected to remit spontaneously after the pregnancy has been completed. Restless leg syndrome is the most common peripheral nerve and movement disorder in pregnancy. Hyperemesis gravidarum is a severe form that prevents adequate fluid and nutritional intake and may require hospitalization to prevent dehydration and malnutrition. Ulcerative colitis is associated with disease exacerbations in the first trimester and during the early postpartum period. Medical management of these diseases during pregnancy is similar to management in the nonpregnant state (Chap. In part, this aggravation may be due to pregnancy-induced alteration in the metabolism of bile and fatty acids. Profound pruritus may accompany this condition, and it may be associated with increased fetal mortality. Placental bile salt deposition may contribute to progressive uteroplacental insufficiency. Therefore, regular fetal surveillance should be undertaken once the diagnosis of intrahepatic cholestasis is made, and delivery should be planned once the fetus reaches about 37 weeks of gestation. Acute fatty liver of pregnancy is generally characterized by markedly increased serum levels of bilirubin and ammonia and by hypoglycemia. Management of acute fatty liver of pregnancy is supportive; recurrence in subsequent pregnancies has been reported. Infants born to mothers who are carriers of hepatitis B surface antigen should also receive hepatitis B immune globulin as soon after birth as possible and preferably within the first 72 h. Screening for hepatitis C is recommended for individuals at high risk for exposure. A new or worsening headache, particularly if associated with visual blurring, may signal eclampsia (above) or pseudotumor cerebri (benign intracranial hypertension); diplopia due to a sixthnerve palsy suggests pseudotumor cerebri (Chap. The risk of seizures in patients with epilepsy increases in the postpartum period but not consistently during pregnancy; management is discussed in Chap. The risk of stroke is generally thought to increase during pregnancy because of a hypercoagulable state; however, studies suggest that the period of risk occurs primarily in the postpartum period and that both ischemic and hemorrhagic strokes may occur at this time. Guidelines for use of heparin therapy are summarized above (see "Deep Venous Thrombosis and Pulmonary Embolism"); warfarin is teratogenic and should be avoided. Disease-modifying agents, including interferon, should not be administered to pregnant multiple sclerosis patients, but moderate or severe relapses can be safely treated with pulse glucocorticoid therapy. Many pregnant women have asymptomatic bacteriuria, most likely due to stasis caused by progestational effects on ureteral and bladder smooth muscle and later in pregnancy due to compression effects of the enlarging uterus. However, if asymptomatic bacteriuria is left untreated, symptomatic pyelonephritis may occur. Indeed, ~75% of pregnancy-associated pyelonephritis cases are the result of untreated asymptomatic bacteriuria. All pregnant women should be screened 50 with a urine culture for asymptomatic bacteriuria at the first prenatal visit. Subsequent screening with nitrite/leukocyte esterase strips is indicated for high-risk women, such as those with sickle cell trait or a history of urinary tract infections. While amniotic infection most commonly follows rupture of the membranes, this is not always the case. In general, antibiotic therapy is not recommended as a temporizing measure in these circumstances. If intrauterine infection is suspected, induced delivery with concomitant antibiotic therapy is generally indicated. In penicillin-allergic patients with a low risk of anaphylaxis, cefazolin is recommended. If the organism is known to be sensitive to clindamycin, this antibiotic may be used. Postpartum endomyometritis is more common after cesarean delivery than vaginal delivery and develops in 2% of women after elective repeat cesarean section and in up to 10% after emergency cesarean section following prolonged labor. As most cases of postpartum endomyometritis are polymicrobial, broad-spectrum antibiotic coverage with a penicillin, an aminoglycoside, and metronidazole is recommended (Chap. Women who do not respond to antibiotic treatment for postpartum endomyometritis should be evaluated for septic pelvic thrombophlebitis. Imaging studies may be helpful in establishing the diagnosis, which is primarily a clinical diagnosis of exclusion. All pregnant patients are screened prenatally for gonorrhea and chlamydial infections, and the detection of either should result in prompt treatment. All women who are pregnant or plan to become pregnant in the near future should receive inactivated influenza vaccine. The prompt initiation of antiviral treatment is recommended for pregnant women in whom influenza is suspected. Treatment can be reconsidered once the results of highsensitivity tests are available. Prompt initiation of treatment lowers the risk of admission to an intensive care unit and death. Chorioretinitis, microcephaly, intracranial calcifications, hepatitis, hemolytic anemia, and purpura may also develop. Congenital rubella may be diagnosed by percutaneous umbilical-blood sampling with the detection of IgM antibodies in fetal blood. All pregnant women and all women of childbearing age should be tested for their immune status to rubella. A cohort study of pregnant women without evidence of previous herpesvirus infection demonstrated that ~2% acquired a new herpesvirus infection during the pregnancy. If herpesvirus seroconversion occurred early in pregnancy, the risk of transmission to the newborn was very low. In women who acquired genital herpes shortly before delivery, the risk of transmission was high. The risk of active genital herpes lesions at term can be reduced by prescribing acyclovir for the last 4 weeks of pregnancy to women who have had their first episode of genital herpes during the pregnancy. It is recommended that pregnant women with active genital herpes lesions at the time of presentation in labor be delivered by cesarean section. It rarely causes sequelae, but susceptible women infected during pregnancy may be at risk for fetal hydrops secondary to erythroid aplasia and profound anemia. Prior to the widespread use of antiretroviral treatment, the perinatal transmission rate was in the range of 20%. In women with a good response to antiretroviral treatment, the transmission rate is about 1%.
Cheap benicar 10mg with mastercard
Family history of menstrual or other gynecologic problems or bleeding disorders C blood pressure chart in pregnancy cheap benicar 20 mg visa. Hematologic disorders History of easy bruising or bleeding, epistaxis, gingival bleeding Vaginal discharge. Testing for von Willebrand disease (not necessary if platelet count is normal because this is platelet adhesion problem). Primary dysmenorrhea: painful menses with clear physiologic etiology and no identifiable pelvic pathology b. Secondary dysmenorrhea: painful menses associated with underlying pelvic abnormality 3. Primary dysmenorrhea is due to release of prostaglandins from endometrium after progesterone withdr. Prostaglandins lead to potent vasoconstriction and uterine contractions, which leads to ischemia and pain ii. Causes of secondary dysmenorrhea are more prevalent in adulthood but should still be considered in adolescents i. Pain is usually just before or after onset of menstrual flow, usually worse in first 2 days 3. Usually in lower abdomen but can radiate to lower back, buttocks, rectum, or legs 4. To be most effective, should be started before or at onset of menses, then continued for at least 2+-48 hours 6. Primary dysmenorrhea is the leading causa of recurrent absences from school or work in young women. U D Chronic pelvic pain may also be due to nongynecologic causes, especially if not only anociated with menses. Therefore, recurrent pain since the onset of menarche should raise suspicion for congenital maHormations such as bicornuate uterus with partialob~uction. Primary dysmenorrhea: nausea, vomiting, diarrhea, breast tenderness, bloating, fatigue, headache, light~headedness, and mood changes b. Mild suprapubic tenderness possible with primary dysmenorrhea at time of menses; otherwise nonnal b. Speculum exam allows visualization of vagina and cervix but may not be necessary if history is consistent with primary dysmenonhea and remainder of physical exam is witltin normal limits b. Rectovaginal exam can evaluate for endometriosis, which can be associated with mild posterior uterine or rectouterine pouch tenderness and uterosacral nodularity D. Allows for direct visualization of pelvic and peritoneal cavity; can diagnose adhesions b. Oral contraceptives: limit endometrial proliferation so less tissue available for prostaglandin production c. History of thrombotic disorder or migraines with aura is contraindication to estrogen-containing methods ii. Screening for thrombotic disorders is not necessary before starting estrogencontaining methods, unless there is a family history of thrombotic events c. Quick start (begin today): reduces chance of becoming pregnant before next period 2. Follow up in 3 months after starting birth conttol to assess compliance, tolerance of method 3. Educate patients about emergency contraception in case of contraceptive failure, such as condom breaking or missed birth control pills 6. Menses is dependent on ovulation, esttogen, and progesterone (secretion and withdrawal) b. Ovaries not producing sufficient esttogen to proliferate uterine lining or induce ovulation i. Vaginal exam (if tolerated) (a) Vagina ending in "blind pouch": indicates absent uterus d. Organize differential based on presence or absence of breasts and/or uterus (Tables 13-6, 13-7, and 13-8) i. Absent breast development indicates inadequate estrogen production (consider if problem is at level of hypotb. Hypergonadotropic and hypogonadottopic hypogonadism necessitate estrogen and progesterone replacement. Because undescended testes have a high malignancy potential, they should be surgically removed. Excluding congenital disorders, much overlap exists between causes of primary and secondary amenorrhea B. If absent, evaluate for hypothalamic-pituitary insufficiency or ovarian failure D. Psychological intervention for eating disorders, significant psychosocial stressors 2. Can use pill with drospirenone as progestin component; has antiandrogen properties b. However, diagnosis is made baaed on elevated free and/ or total testosterone levels. Other organisms include Streptococcus species, Eschmchfa coli, Mycoplasma hombtis, Ureaplasma urealyticum, Bacttroidts species, and other anaerobes +. Chlamydia and gonorrhea have predilection for columnar cells that predominate in area surrounding cervical os in adolescents (cervical ectropion); these cells transform to squamous epithelium as the adolescents enter adulthood U. Less likely to use banier contraception due to cognitive stage, sense of invincibility b. Inflammatory disruption of cervical banier permits ascension of inciting bacteria into uterus c. Multiple vaginal organisms follow, creating polymicrobial upper tract infection d. Decreased motility of fallopian tubes due to inflammation leads to collections of fluid (hydrosalpinx) or pus (pyosalpinx) f. Patient may or may not have had symptoms of cervicitis prior to presentation (see Box 13-3 for clinical presentation of cervicitis) 2. Differential diagnosis includes causes of abdominal pain originating from multiple organ systems a. Gynecologic: pregnancy, dysmenorrhea, endometriosis, mittelschmerz, ovarian cyst, ovarian torsion, ovarian tumor c. Laparoscopy can visualize swollen fallopian tubes, allow for bacterial culture of pelvic fluid or abscesses D. Bacteria, inflammatory cells, fluid accumulate in fallopian tube, then spread beyond fuubriated end of tube to encompass adjacent ovary ii. Disruption of normal vaginal flora and/or altered pH leads to overgrowth of other flora. Adherence to vaginal epithelial ceUs leads to cellular damage and mucosal inflammation B. Ask about onset, duration, color, odor, consistency, and quantity of vaginal discharge b. The higher glucose content of vaginal secretions and altered immune function permit increased proliferation of Candida species. Instruct patients to abstain from sexual intercourse until completion of therapy, resolution of symptoms 5. Eating yogurt and other sources of live lactobacilli not shown to significantly prevent infections d. Transmitted through sexual contact: vaginal or anal sex, genital-genital contact, manual-genital contact b. Can lead to cellular dysplasia and even anogenital and cervical carcinoma, although much less likely in adolescents B. Patients may report "bumps" in genital region; may occasionally itch or bleed at site of lesion d.

Order benicar mastercard
The involvement of heme explains why the drug is selectively toxic to malaria parasites arrhythmia lecture discount benicar 10 mg free shipping. The World Health Organisation has recommended artemisinin combination therapies be the first-line therapy for Plasmodium falciparum malaria worldwide. Combinations are effective because the artemisinin component kills the majority of parasites at the start of the treatment, while the more slowly eliminated partner drug clears the remaining parasites Artemisinin is not used for malaria prophylaxis because of short half-life. The drug is potent anthelmintic active against many trematodes including different species of Schistosoma, Clonorchis sinensis, Fasciola hepatica, and Opisthorchis viverrini. It is more common in people who live in tropical areas with poor sanitary conditions. Only about 10% to 20% of people who are infected with Entamoeba histolytica become sick from the infection. The symptoms often are quite mild and can include loose stools, stomach pain, and stomach cramping. Amebic dysentery is a severe form of amebiasis associated with stomach pain, bloody stools, and fever. Even less commonly, it spreads to other parts of the body, such as the lungs or brain. Life cycle of Entamoeba histolytica includes ingestion of cysts, the formation of trophozoites, the penetration of intestinal wall, the multiplication of trophozoites within the colon wall, excretion of cysts with feces. If amoebas enter the blood and travel to another organs, they cause systemic invasion. Devyatkina Tinidazole Emetine hydrochloride Chloroquine Luminal amebicides Iodoquinol Tetracyclines Diloxanide furoate Quiniodochlor. In the case of metronidazole, reduced ferredoxin appears to be the primary electron donor responsible for its reduction. Aerobic microbes use other electron transport systems and are not sensitive to metronidazole. Spectrum of action Protozoa (Giardia lamblia, Entamoeba histolytica, Trichomonas vaginalis, Leishmania), anaerobic cocci, anaerobic Gram (+) and Gram (-) bacilli (Bacteroides spp. Side-effects A loss of appetite An unpleasant taste in the mouth Nausea, vomiting Diarrhea Headache, reversible polyneuropathy Skin rash, itch Leukopenia Red-brown discoloration of urine Changes in pharmacokinetics of some other drugs. It is a systemic amebicide; is used in a conjugation with metronidazole and diloxanide to treat and prevent amebic liver abscesses. Diloxanide furoate is a luminal amebicide; is used to treat intestinal amebiasis; is well tolerated, but may cause flatulence, dry mouth, itch, urticaria; is contraindicated to pregnant women and children younger than 2 years of age. Trichomoniasis is caused by the single-celled protozoan parasite, Trichomonas vaginalis. The vagina is the most common site of infection in women, and the urethra (urine canal) is the most common site of infection in men. Trichomoniasis can usually be cured with nitroimidazole derivatives (metronidazole, tinidazole or ornidazole) and nitrofuran derivatives (furozolidone). Although the illness most frequently occurs in developing countries, giardiasis is also one of the most common causes of waterborne illness in the United States. When symptoms occur, they typically start one to three weeks after exposure and include a sudden onset of watery diarrhea, abdominal cramping, bloating, nausea, gas. Although most people will recover from giardiasis without treatment, medica-tions, such as metronidazole, quinacrine hydrochloride (Mepacrine) or furazolidone (furoxone), are used to treat giardiasis. Metronidazole and furazolidone are described in detail as amebicides and chemotherapeutics of different chemical structure. Toxoplasmosis passes from animals to humans, sometimes without causing any symptoms. Toxoplasmosis infections in people fall into three basic patterns: congenital toxoplasmosis, in which a child becomes infected before birth; 2) toxo-plasmosis in otherwise healthy kids (with the same symptoms a pregnant woman may have); 3) toxoplasmosis in kids with weakened immune systems. Toxoplasmosis is treated with pyrimethamine which is described as an antima-larial agent and its combinations with sulfonamides (sulfadiasine). It is caused by infection with Leishmania parasites which are spread by the bite of infected sand flies. The most common forms are cutaneous leishmaniasis which causes skin sores, and visceral leishmaniasis which affects some of the internal organs of the body. Some other preparations for the treatment of leishmaniasis (quinacrine, metronidazole, amphotericin B) are presented in other parts of this Chapter and in Chapter 30. The blood shizonticides are all the drugs, except: Chloroquine Primaquine Quinine Pyrimethamine Mefloquine. The correct statements concerning antiprotozoals are: Quinine is used for the radical cure of malaria Chloroquine is used for malaria and amebiasis Metronidazole may cause disulfiram-like adverse reaction Sodium stibogluconate is antimony compound for leishmaniasis Sodium stibogluconate is a folate antagonist for toxoplasmosis. A patient with an acute attack of malaria was presctibed with an erythrocytic shizonticidal fast acting drug. In addition to antimalaial effect, this drug has anti-inflammatory properties and is used in the treatment of rheumatoid arthritis and lupus erythematosus. There are several main spe-cies of parasitic worms causing human helminthic infections. They are tapeworms (cestodes): Taenia saginata, Taenia solium, Hymenolepis nana, and Echionococcus species; roundworms (nematodes): Ascaris lumbricoides, Enterobius vermicularis, Ancilostoma duodenale, Necator americanus, Trichinella spiralis; trematodes: Schistosoma mansoni, Schistosoma haematobium. Intestinal helminthiasis is an infestation with one or more intestinal parasitic worms. Infected people excrete helminth eggs in their feces which then contaminate the soil in areas with inadequate sanitation. Other people can then be infected by ingesting eggs or larvae in contaminated food, or through the penetration of the skin by infective larvae in the soil (hookworms). Infestation can cause morbidity, and sometimes death, by compromising nutritional status, affecting cognitive processes, inducing tissue reactions, such as granuloma, and provoking intestinal obstruction or rectal prolapse. Control of helminthiasis is based: on drug treatment improved sanitation health education. For extraintestinal nematodoses Diethylcarbamazine Ivermectin Drugs for treatment of cestodoses For intestinal cestodoses Niclosamide (Phenasal) For extraintestinal cestodoses Albendazole Drugs for treatment of trematodoses For intestinal trematodoses Perchloroethylene For extraintestinal trematodoses Praziquantel Chloxyl Drugs of wide spectrum of action Chapter 34. Pharmacokinetics is taken orally is poorly absorbed in the gut (10%); absorption is increased in the presence of fatty meals is rapidly metabolized is excreted with urine and bile within 24-48 hrs. Mechanism of action It inhibits the polymerization of helminth tubulin that leads to inhibiting the synthesis of microtubules in parasitic worms, and destroying extant cytoplasmic microtubules in their intestinal cells. Thus, the drug interferes with microtubule-dependent functions, such as a glucose uptake. The effect takes time to develop and the worms may not be expelled for several days. Pinworm (Enterobius vermicularis), roundworm (Ascaris lumbricoides), guinea worm (Dracunculus medinensis), Trichinella spiralis, hookworm (Ancilostoma duodenale, Necator americanus), whipworm (Trichuris trichiura). Indications Infection caused by pinworm Infection caused by roundworm Infection caused by guinea worm Trichiniasis Infection caused by hookworm Infection caused by whipworm. Is given as a single dose for threadworm, and twice daily for 3 days for hookworm and roundworm infestations. Side-effects Gastrointestinal disturbances, elevated liver enzymes, low white blood cell count, low platelet count, and hair loss. Contraindications Should not be given to pregnant women and children under 2 years old. Oral absorption of albendazole is small and depends on gastric pH and increases with a fatty meal. For systemic parasites, it acts as a prodrug, while albendazole sulfoxide (active metabolite) reaches systemic circulation and acts as the real antihelminthic. The drug leads to impaired uptake of glucose by parasites, and depletes their glycogen stores. It prevents the formation of spindle fibers needed for cell division, which in turn blocks egg production and development. Onchocerca volvulus, roundworms, whipworms is the first choice of the drug for filarial infection, onchocerciasis (river blindness), infestation by Wuchereria bancrofti caused elephantiasis is well tolerated, but may cause skin rash, fever, headache, pain in muscles and joints. Examples of naturally occur-ring anthelmintics include: Tobacco (Nicotiana tabacum), black walnut (Juglans nigra), wormwood (Arthemisia absynthium, Arthemisia cina), clove (Syzygium aromaticum), tansy tea (Tanacetum vulgare), hagenia (Hagenia abyssinica), garlic (Allium sativum), pine-apple (Ananas comosus), kalonji (Nigella sativa) seeds, male fern (Dryopteris filix-mas), plumeria (P. Many natural anthelminthics are poisonous and, in improper dosages, dangerous for humans, as well as for parasites. Some medicinal plants used as antihelminthics: A Dryopteris filix-mas; B Allium sativum; C Arthemisia cina; D Cucurbita pepa. All the listed drugs are antihelminthics, except: Mebendazole Metronidazole Niclosamide Pyrantel pamoate Piperazine adipinate 2. The antihelminthic affecting microtubular function in nematodes is: Praziquantel Niclosamide Piperazine adipinate Mebendazole Ivermectin.