Order bystolic
Ascaris passes through the lung and can initially cause respiratory symptoms; can also cause biliary obstruction; excretes round pulse pressure 44 purchase discount bystolic on line, thickwalled ova. Enterobius is common in children and readily spreads by dust and contaminated linens. Diagnosed when the adhesive cellophane tape test demonstrates worms in the anal area. Under optimal conditions of shade and moisture, eggs excreted in the stool undergo embryonic development within 2-4 weeks. Then, when ingested by humans, the larvae break out of the eggshell and penetrate the intestinal villi of the small intestine. Over 3-10 days, they migrate down to the cecum, and over 1-3 months, they develop into egg-producing adults. Bloody diarrhea, growth retardation, and rectal prolapse are potential complications of a heavy infection. Mebendazole is a highly effective treatment and is seldom associated with side effects. Albendazole is also recommended as first-line therapy; ivermectin or nitazoxanide is an efficacious alternative (see Table 12. In the United States, infections are found predominantly in the southeast, where weather conditions favor egg embryonation. Like Trichuris, Ascaris is a parasite of humans, the infection being contracted by ingesting material contaminated with human feces. Under proper temperature and moisture conditions, eggs develop into infective embryos within 5-10 days. On reaching the capillaries of the lung, they break into the alveoli, crawl up through the bronchi and trachea, and then are swallowed, reentering the gastrointestinal tract, where they mature over a period of 2 months. However, patients with high worm burdens can experience obstruction of the small intestine, accompanied by vomiting and abdominal pain. Heavy infections may also be associated with malabsorption, steatorrhea, and weight loss. A single Ascaris worm can migrate up the biliary tree and obstruct the common bile duct, precipitating symptoms of cholecystitis, including epigastric abdominal pain, nausea, and vomiting. As the worms migrate into the lungs, some patients experience respiratory symptoms and develop pneumonia visible on chest radiographs, accompanied by peripheral eosinophilia (sometimes called Loeffler syndrome). On occasion, worms can migrate to other sites in the body, causing local symptoms. Alternative treatments include pyrantel pamoate, albendazole, and nitazoxanide (Table 12. Alternatively, all school-age children in endemic areas can be treated twice or three times per year to reduce the worm burden, although this approach has not been proven to improve their nutritional status or hemoglobin levels. This infection is very common in children of all socioeconomic groups in the United States. The eggs of this parasite resist drying and can therefore contaminate bed linens and dust. As a result, infection in one young child can lead to infestation of the entire family. After ingestion, the eggs hatch in the duodenum and jejunum, and the larvae mature in the cecum and large intestine. At night, gravid females migrate to perianal area, where they lay eggs and cause localized itching. When this area is scratched, eggs are trapped under fingernails and are subsequently ingested by the host, resulting in repeated autoinfection. The major clinical manifestation is nocturnal itching of the perianal area that often interferes with sleep. Because Enterobius rarely migrates through tissue, this infection is not associated with peripheral eosinophilia. Diagnosis is made by pressing adhesive cellophane tape onto the perianal area in the early morning. Small, white, threadlike worms and eggs become attached to the tape and can be easily identified using a low-power (100x) microscope. Because Strongyloides can cause a fatal hyperinfection syndrome in the immunocompromised host, clinicians need to be familiar with this parasite. Humans become infected as a result of skin exposure to feces or soil contaminated by feces. Walking barefoot on contaminated soil is the most common way of contracting this infection. Subsequently, they become trapped in the lungs, where they enter the alveoli and are coughed up and then swallowed, entering the gastrointestinal tract. The larvae mature in the upper gastrointestinal tract, where females are able to penetrate the bowel mucosa and deposit their eggs. Eggs hatch in the mucosa, releasing rhabditiform larvae that either mature within the intestine, forming filariform larvae capable of penetrating the bowel wall and causing autoinfection, or are passed in the feces. Because Strongyloides can reinfect the human host, an initial infection can persist for 35-40 years. The intensity of the infection depends not only on the initial inoculum but also on the degree of autoinfection. In the immunocompromised host, autoinfection can be intense and can cause severe disseminated illness. Larvae enter the bloodstream, invade the lung, crawl up the bronchi to the trachea, are swallowed, and mature in the small intestine. He had long-standing diabetes mellitus and had experienced multiple myocardial infarcts leading to severe ischemic cardiomyopathy. Following transplantation, he received mycophenolate mofetil, tacrolimus, and high doses of methylprednisolone. One month after transplant, he suddenly developed fever and increasing shortness of breath, associated with a cough productive of clear watery sputum. He had never traveled outside of northern Florida, having lived in the area his entire life. Physical examination showed a blood pressure of 133/72 mmHg, a pulse of 81 per minute, a respiratory rate of 20 per minute, and a temperature of 37. Coarse breath sounds were heard bilaterally in the lungs, and the midline sternal wound was clean and without drainage. Some leg edema was noted (3+ in the left lower leg, and 1+ in the right lower leg), but pedal pulses were intact. A computed tomography scan of the chest shows diffuse interstitial infiltrates consistent with pulmonary edema. Lung biopsy with hematoxylin and eosin stain shows inflammatory cells within the alveoli and a rhabditiform larva (middle of the field). Despite treatment with voriconazole, ganciclovir, and broad-spectrum antibiotics, the patient became hypotensive and remained hypoxic, dying 7 days after the onset of his acute respiratory illness. Occasional filariform larvae were also seen within the sinuses of the hilar lymph nodes and were identified within the myocardial interstitium. Filariform larvae were seen within the walls of the esophagus, stomach, small bowel, and colon, with the heaviest infestation being observed in the colon. As observed with other roundworm infections, most patients with Strongyloides have no symptoms when they harbor only a small number of worms. When the filariform larvae first penetrate the skin, they can cause itching and a papular erythematous rash. Migration into the lungs can cause respiratory symptoms, pneumonia, and peripheral eosinophilia (Loeffler syndrome). Once Strongyloides takes up residence in the gastrointestinal tract, the parasite can cause burning abdominal pain that mimics peptic ulcer disease or a colicky abdominal pain that mimics gallbladder disease. Because the female worm penetrates the bowel mucosa and the filariform larvae can migrate through the bowel wall, the host responds by producing eosinophils, and peripheral eosinophilia is a prominent finding in strongyloidiasis. When larvae penetrate the perianal area, a localized snakelike urticarial rash may be seen. Symptoms may include diffuse pulmonary infiltrates, severe abdominal pain, meningitis, and gramnegative sepsis, the latter manifestation being the result of filariform larvae compromising the integrity of the bowel wall. Periumbilical purpura, diffuse nonpalpable purpura, angioedema, and erythroderma mimicking a drugrelated allergic eruption have all been described. When an immunocompromised patient presents with this clinical constellation and was raised in the rural south or previously lived in a tropical region, hyperinfection with Strongyloides needs to be considered. Lung invasion can produce Loeffler syndrome (cough, wheezing, pneumonia, and eosinophilia).
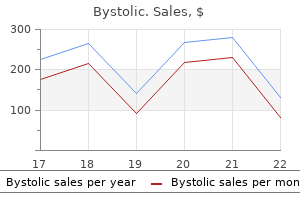
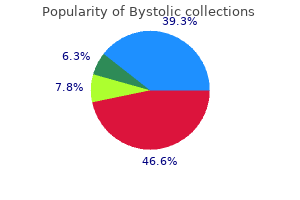
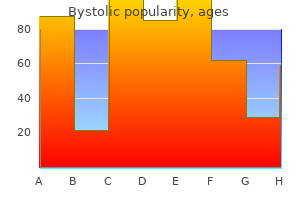
Cheap bystolic 2.5mg mastercard
Necrotizing fasciitis should be considered in diabetic patients with cellulitis who also have systemic signs of infection arteria peronea order bystolic 5mg on-line, such as, tachycardia, leukocytosis, marked hyperglycemia, or acidosis. Diabetic patients can also develop necrotizing fasciitis in other body areas, including the headand-neck region and the perineum. This infection can result from a breach of the integrity of the mucous membranes after surgery or instrumentation, or from an odontogenic infection. These infections begin abruptly with severe pain and may spread rapidly onto the anterior abdominal wall, into the gluteal muscles, and, in males, onto the scrotum and penis. He was admitted to the hospital and intravenous clindamycin and gentamicin were started. On physical examination during the third hospital day, he appeared severely ill and septic. Marked erythema was observed, along with edema of the right ankle that extended up the front and lateral regions of the leg, half way to the knee. A new 1x1-cm patch of dark reddish-purple skin was noted that was exquisitely tender to touch. An emergency surgical exploration revealed an area of necrotic fascia consistent with necrotizing fasciitis. Early diagnosis of necrotizing fasciitis is critical because, as was observed in case 10. Differentiating necrotizing infections from common soft tissue infections such as cellulitis and impetigo is both challenging and critically important (see Table 10. Prompt diagnosis is imperative, because necrotizing infections typically spread rapidly and can result in multiorgan failure, adult respiratory distress syndrome, and death. However, in some patients, signs and symptoms of infection are not initially apparent. However, excruciating pain in the absence of any cutaneous findings may be the only clue for infection in some patients. Within 24 to 48 hours, erythema may develop or darken to a reddish-purple color (as observed in case 10. The bullous stage is associated with extensive deep soft tissue destruction that may result in necrotizing fasciitis or myonecrosis; such patients usually exhibit fever and systemic toxicity. In addition to pain and skin findings, fever, malaise, myalgias, diarrhea, and anorexia may also be present during the first 24 hours. Values of greater than 6 indicate a 50% or greater likelihood of a necrotizing soft tissue infection. Laboratory Risk Indicator Scores for Necrotizing Soft Tissue Infection Necrotizing fasciitis must be distinguished from gas gangrene, pyomyositis, and myositis. Frozen biopsy of the skin and subcutaneous tissue has proven useful for the early diagnosis of necrotic fascia but is often inconvenient and time consuming. Therefore, in most cases, any of the abnormalities described above should be of sufficient concern to prompt surgical exploration. It is critical to proceed with surgery rather than to delay in order to obtain an imaging study or biopsies. Necrotizing soft tissue infection is most effectively diagnosed and treated by surgeons in the operating room. Prompt diagnosis, immediate administration of appropriate antibiotics, and emergent, aggressive surgical debridement of all compromised tissues are critical to reduce morbidity and mortality. The primary indications for surgical intervention are severe pain, sepsis, fever, a high-risk score based on laboratory findings (Table 10. If necrotizing soft tissue infection is a possibility, the only definitive method of diagnosis is surgical exploration. After initial debridement, infection can continue to progress if all necrotic tissues have not been removed. Surgical reexploration is therefore often required and should be performed as often as is necessary. Clindamycin may be more effective because this antibiotic is not affected by bacterial inoculum size or stage of growth. Most experts currently recommend administration of combined therapy with penicillin G and clindamycin when beta-hemolytic streptococci is identified (see Table 10. However, early empiric treatment is necessary: ampicillin-sulbactam (combined with clindamycin or metronidazole) is a reasonable regimen. Broader gramnegative coverage may be necessary if the patient was recently hospitalized or has recently received antibiotic treatment. Because of intractable hypotension and diffuse capillary leak in patients with shock, massive amounts of intravenous fluids (10-20 L daily), plus vasopressors such as dopamine or epinephrine, are often necessary to maintain tissue perfusion. Several recent case reports and a case series suggest a beneficial effect for intravenous administration of high-dose immunoglobulins to neutralize circulating streptococcal toxins. Unfortunately, even with optimal therapy, necrotizing fasciitis is associated with high (20-60%) mortality. This deep subcutaneous infection causes necrosis of the fascia and subcutaneous fat. Severe pain is often the earliest symptom; septic appearance and tachycardia are also suggestive. Myonecrosis Myonecrosis (also called necrotizing myositis) is an uncommon infection of muscle that develops rapidly and is life-threatening. Infections resulting in necrosis of muscle are almost entirely the result of infection by Clostridium species (gas gangrene). These infections typically evolve after contiguous spread from an area of trauma or surgery, or spontaneous spread from hematogenous seeding of muscle. Other conditions associated with traumatic gas gangrene include bowel surgery and postabortion with retained placenta. Clostridial gas gangrene may also be spontaneous and nontraumatic and is often associated with C. Many of the spontaneous cases occur in patients with gastrointestinal portals of entry such as adenocarcinoma. Several other clinical entities may be associated with muscular injury and should be considered in patients presenting with myositis: 1. Vibrio infections can involve the skin, fascia, and muscle and are most common among patients with cirrhosis, consumers of raw seafood, or inhabitants of coastal regions. At the same time, through tissue damage, it produces an anaerobic environment with low oxidation-reduction potential and acid pH, which is optimal for growth of clostridial organisms. In addition, theta-toxin stimulates the production of multiple inflammatory cytokines that lead to blood vessel dilatation and hypotension. Infection with this pathogen usually accompanies a bowel lesion, particularly cecal carcinoma (see case 10. Routine sterilization of tissue allografts may not remove Clostridium spores, explaining this potentially fatal complication. On physical examination, severe tenderness of the left shoulder was elicited, and the patient was given a pain medication for presumed bursitis. A large blister was noted over the left deltoid, and the skin now had a bronze appearance. Crepitus was readily palpated, and subcutaneous air in the arm and left chest wall was noted on X-ray. In many areas, muscle was necrotic and had the appearance of cooked meat, failing to contract with electrical stimulation. Despite aggressive debridement, multiple blood transfusions, and respiratory support, the patient developed irreversible shock and died 18 hours after admission. The mean incubation period may be less than 24 hours, but ranges from 6 hours to several days, probably depending on the size of the bacterial inoculum and the extent of vascular compromise. The skin over the infected area may initially appear pale, but it quickly changes to bronze, and then to purplish-red. These include tachycardia and low-grade fever, followed by shock and multiorgan failure. When clostridial bacteremia occurs, it may be associated with extensive hemolysis. The presence of large grampositive rods at the site of injury help to make a definitive diagnosis. As described earlier for streptococcal gangrene, the combination of penicillin and clindamycin is recommended. This combination would be expected both to reduce toxin production and to kill the organism (see Table 10.
Cheap 2.5 mg bystolic mastercard
In severe infection and meningitis 50 mg/kg/dose 6 times daily to maximum single dose of 2 arteria poplitea purchase bystolic pills in toronto. It can be an effective tool for reducing muscle tone in the appropriately selected patient. The "ideal" patient is the one who has hypertonia that interferes with function, is expected to develop fixed contractures, and requires treatment of only a few muscles at any given time. If more than one muscle group needs to be injected at the same time, this total dose is divided between these muscles. Dose may be repeated when clinical effect diminishes but not within 2 months of previous injection. Cervical dystonia: Inject using a 25, 27 or 30 gauge needle (for superficial muscles) or 22 gauge (deeper musculature). Tailor dosing to individual patient based on the head and neck position, location of pain, muscle hypertrophy, body weight and response. Focal spasticity associated with infantile hemiplegia: Inject using a 25, 27 or 30 gauge needle (superficial muscles) or longer needle for deeper musculature. Multiple injection sites may facilitate more uniform contact with the innervation areas of the muscle, especially in larger muscles. Tailor dose and number of sites based on size, number and location of muscles involved, the severity of spasticity, and the presence of local muscle weakness. Croup: 1 month to 18 years 2 mg with nebulizer when required Bumetanide: oral 1 month to 12 year-0. The dosage of bupivacaine will depend upon the site of injection and the procedure used. Epidural administration should be carried out by, or under the supervision of a consultant anesthetist. At the methotrexate dosages used in most protocols folinic acid rescue will be required. Pneumonia, peritonitis, neutropenia, septicemia-60 mg/kg/day in 3 divided 1180 calamine lotion: Apply to external affected area as needed. Meningitis and life threatening infections-120 mg/kg/day in 3 divided doses (maximum 2 g/ dose). After 12 hours wash in ordinary shampoo, remove dead lice and eggs with comb while the hair is still wet. Give until euthyroid and then taper to once daily dose barely enough to sustain normal thyroid function. Patients with hepatic impairment: not recommended for patients with clinically evident hepatic impairment. Intermittent hemodialysis: due to its high degree of plasma protein-binding, carvedilol is not likely to be significantly removed by hemodialysis. Due to extrarenal elimination it is only necessary to reduce dose in severe renal impairment (creatinine clearance less than 10 mL/ min/1. A normal single dose should be given as a loading dose then the daily dose should be halved without a change in frequency. In hemodialysis: the appropriate maintenance dose should be repeated after dialysis. In patients undergoing dialysis no supplemental dose required but serum concentration monitoring advisable. Reduce dose in severe renal impairment (creatinine clearance less than 10 mL/min/1. Children 50 mg/kg/day (maximum 1 g/day) 4 divided doses-double dose for meningitis, septicemia). In aphthous ulcertation and oral infections use for 48 hours after the infection has cleared. More than 12 years: apply half an inch of gel with massage not more often than every 3 hours. Daily applications should be made over the previous coat and removed every 7 days. Up to 48 weeks of daily applications, weekly trimming by the patient, and monthly professional removal of the unattached, infected nail, are needed. Dose adjustment in renal or liver failure: In severe impairment (creatinine clearance less than20 mL/ min/1. First day-2 drops every 15 min for 6 hour followed by 2 drops every 30 min for the rest of the day. Always consult the current treatment protocol for details of dosage and scheduling. Treatment and postexposure pertussis prophylaxis- (For postexposure prophylaxis, administer to close contacts within 3 weeks of exposure, especially in high-risk patients. Oral dosage: infants more than 6 months and children: 15 mg/kg/day up to maximum of 500 mg twice daily for 7 days.
Bystolic 5 mg otc
Stones are totally radiolucent on X-ray and computed tomography (Ct) prehypertension stress 2.5 mg bystolic sale, but seen on echography [9]. Cola soft drinks, which reduce urine pH, are useful in reducing the formation of crystals and stones [1]. Atazanavir Atazanavir, an azapeptide inhibitor of HiV-1 protease first marketed in 2003, was soon reported as inducing urolithiasis [10] and sometimes acute interstitial nephritis [11]. Other sulfonamides Sulfasalazine, used in the treatment of ulcerative colitis, may induce bilateral stones [19]. Sulfamethoxazole, a component of co-trimoxazole, induces frequent crystalluria but stone formation [18] is infrequent relative to its wide use, likely due to the small size and smooth rhomboid shape of the crystals. Other antibacterial or antiviral drugs Quinolones and aminopenicillins are rarely involved in drug-induced nephrolithiasis (reviewed in [1]). Ciprofloxacin causes frequent asymptomatic crystalluria, especially in alkaline urine (in contrast with first-generation quinolones) but formation of stones is very infrequent [20]. Ceftriaxone is largely used for the treatment of bacterial meningitis, pneumonia or pyelonephritis, especially in children. Guaifenesin, ephedrine, and pseudoephedrine A number of non-prescription oral cough suppressants, expectorants, and decongestants, often in the form of mixed preparations, are available OtC 112 types of Urinary Stones and their Medical Management and freely available via the internet. As a result, new OtC preparations were produced, combining guaifenesin and ephedrine in a 8:1 ratio, and subjects who previously took OtC ephedrine as a stimulant and switched to these new preparations were ipso facto consuming high doses of guaifenesin (some up to 24,000 mg/day). Stones are radiolucent, but visualized on unenhanced helical Ct scan, their weak density leading to frequent misdiagnosis as uric acid urolithiasis. Ephedrine and pseudoephedrine Ephedrine and pseudoephedrine are widely used as decongestants and bronchodilators. However, ephedrine is often used as a stimulant and ephedrine abuse has become popular due to its easy OtC availability (combined with guaifenesin) or as "herbal preparations. Silica-containing drugs, mainly as magnesium trisilicate, used as antacids over long periods, or as colloid silica, used as milk thickener for prevention of esophageal regurgitation in babies, may induce stones made of opaline silica [34]. Carbonic anhydrase inhibitors Carbonic anhydrase inhibitors block the reabsorption of bicarbonate and sodium ions, and inhibit the excretion of H+ ions, in the proximal tubule. Such urine composition favors the precipitation of calcium phosphate crystals and formation of phosphate stones [35], mainly in the form of carbapatite [1]. Acetazolamide Acetazolamide, used for a long time in the treatment of glaucoma and more recently epilepsy, provokes the frequent development of nephrolithiasis [35], as do its analogs methazolamide, dorzolamide, and dichlorphenamide (reviewed in [1]). As for acetazolamide, prevention essentially 114 types of Urinary Stones and their Medical Management relies on high fluid intake and thiazides to reduce hypercalciuria, whereas the effectiveness of potassium citrate remains to be evaluated [36]. Concomitant prescription of potassium citrate reduced the prevalence of stones and increased the duration free of symptomatic stones [42]. Calcium and vitamin D supplements Calcium supplementation Calcium supplements, especially when associated with vitamin d, may increase urinary calcium excretion and induce calcium nephrolithiasis, especially in subjects with underlying idiopathic hypercalciuria [43]. At variance with high dietary calcium, which reduces the risk of forming calcium stones, supplemental calcium increased the risk of calcium stone formation by 20% [44]. Other drugs Furosemide therapy in preterm neonates may induce bilateral calcium calculi (and nephrocalcinosis) by rising urinary calcium concentration, unless combined with a thiazide diuretic [52]. Carefully checking the medical history, co-morbidities, and current therapy is essential in every stone-forming patient and may immediately identify the diagnosis. All drug-containing stones are radiolucent on conventional X-ray and need to be differentiated from uric acid, cystine, dihydroxyadenine or xanthine stones. Solubilization of stones or obstructive crystalluria may be achieved by active urine dilution and/or adjustment of urine pH according to the specific pH dependence of the drug. Etiological diagnosis of metabolically induced stones is oriented by medical history, co-morbidities, and composition of stones. Recommendations for the proper use of nonprescription cough suppressants and expectorants in solid-organ transplant recipients. Low serum concentrations of 25-hydroxyvitamin d in older persons and the risk of nursing home admission. Effect of vitamin d repletion on urinary calcium excretion among kidney stone formers. Introduction Patients suffering from renal colic can present in a variety of ways. While there is no formal medical definition of this term, it is generally used to describe an acute-onset, severe flank pain, often radiating to the ipsilateral groin and commonly associated with nausea and vomiting. Prostaglandin E2 also triggers vasodilation of the afferent arterioles, promoting a diuresis which further increases renal pelvic pressure and likely exacerbates the pain [5]. Finally, activation of pain receptors can occur in any organ that shares innervation with the kidney, including the organs of the gastrointestinal tract, thus explaining the frequent association of nausea and vomiting with renal colic [6]. Phase two is marked by efferent arteriolar vasoconstriction that causes a decrease in renal blood flow. At this point the patient often enters the "constant phase" whereby pain is continuous and severe. While costovertebral angle tenderness and flank pain are hallmarks of these alternative conditions, the degree of pain is generally less than that seen for renal colic due to acute ureteral obstruction. Many of these patients will ultimately be diagnosed with non-obstructive intrarenal stones or papillary tip calcifications and rarely may be diagnosed with loin pain hematuria syndrome if noted to have hematuria associated with these episodes. Unfortunately, the benefits of Ct must be measured against the associated ionizing radiation and potential for carcinogenesis. Performance parameters for this diagnostic tool may be lower among obese patients and those with small stones <4 mm in size [18]. Given growing concerns regarding the overuse of Ct, numerous algorithms have been formulated to ideally utilize imaging modalities in the patient with acute renal colic. While this test eliminates the exposure to ionizing radiation, stones are not readily identifiable and must be inferred by the appearance of a filling defect and other secondary signs such as hydroureteronephrosis. One particular instance where this test may be useful is in the case of pregnancy, though White et al. Management of Renal Colic and Medical Expulsive therapy 125 Non-steroidal anti-inflammatory drugs versus narcotic analgesics Non-steroidal anti-inflammatory drugs have a direct effect on pain from renal colic via inhibition of prostaglandin synthesis. A 2004 Cochrane review addressing this subject found that patients using narcotics were more likely to require additional analgesia at earlier times in greater doses [21]. Desmopressin desmopressin has also been investigated for use in renal colic because of its ability to cause vasoconstriction of the afferent arteriole and potentially reduce renal pelvic pressure seen in obstruction [27]. Management of Renal Colic and Medical Expulsive therapy 127 Several other novel therapies have been used to alleviate stent-related discomfort, including botox injections at the ureteral orifices [38] and intravesically administered medications such as oxybutynin, ketorolac, and lidocaine [39]. Medical expulsive therapy the decision to observe versus intervene in the case of an obstructing ureteral stone is a commonly encountered clinical challenge. Ureteral peristalsis, considered to be a promoter of stone passage, becomes disorganized and unco-ordinated in the case of acute obstruction. Furthermore, the stone induces ureteral spasm and edema, further inhibiting the ability of the stone to pass spontaneously [40]. One commonly administered therapy for this purpose is the use of intense hydration and diuretics. Furthermore, there was a shorter time to passage amongst the tamsulosin group (72 versus 120 hours). Conversely, use of -blockers was associated with a 29% increased likelihood of stone passage, which was significant. Corticosteroids have also been studied based on the premise that they might decrease ureteral edema and thus facilitate spontaneous passage. Future efforts must ensure that urologists are not the only members of the medical community with a knowledgeable understanding of this common and treatable problem.
Buy bystolic toronto
To reduce the risk of spread blood pressure 40 over 20 generic bystolic 5mg visa, aspiration of the cyst is recommended-a procedure that involves removing a fraction of the contents and instilling a hypertonic saline solution (30% NaCl), iodophor, or 95% ethanol to kill the germinal layer and daughter cysts. Surgical resection should be performed 30 minutes after instillation of the solution. In cases with biliary communication, the foregoing cidal agents are not recommended because of the risk of inducing sclerosing cholangitis. As compared with medical treatment alone, debulking of cysts does not improve outcome, but it may relieve symptoms in specific cases. Treatment in the perioperative period with three to four cycles of albendazole 400 mg twice daily for 4 weeks, followed by a 2-week rest period, is generally recommended to limit the risk of intraoperative dissemination. The same medical therapy is recommended for patients with inoperable hydatid cyst (see Table 12. A comprehensive consensus paper describing staging, surgical, and medical management was published in 2010 (see Further Reading). Eggs hatch in the intestine and oncospheres enter the bloodstream, where they migrate to the liver or lung, or (less commonly) to the brain, where they form hydatid cysts. Hydatid cysts survive and grow over decades, causing symptoms when they reach 8-10 cm in diameter. Treatment involves administration of albendazole, combined with surgical resection preceded by instillation of an agent cidal to the germinal layer. Prevalence, Epidemiology, and Life Cycle Taenia solium is another cestode (tapeworm) common in Central and South America, Mexico, the Philippines, Southeast Asia, India, Africa, and southern Europe. This infection can also be contracted eating raw or undercooked pork containing encysted larvae. Once ingested, the encysted larvae are released into the stomach, where they migrate into the intestine and develop into adult worms that can reach 8 m in length. These individuals become chronic carriers who carry the tapeworm, but do not develop cysticercosis unless they accidentally ingest eggs from their own feces. Chronic carriers spread the disease via the fecaloral route, and person-to-person spread is now thought to be the primary mode of transmission of the disease. However, if the eggs released by the worms are ingested, the eggs hatch releasing larvae that penetrate the intestine, enter the bloodstream, and eventually encyst in the brain, causing neurocysticercosis. Cysts may lodge in the cerebral ventricles (causing hydrocephalus), the spinal cord (resulting in cord compression and paraplegia), the subarachnoid space (causing chronic meningitis), or the cerebral cortex (causing seizures). Cysts may remain asymptomatic for many years, becoming clinically apparent only when the larvae die, an event associated with cyst swelling and increased inflammation. Diagnosis and Treatment Computed tomography or nuclear magnetic resonance scan is the preferred diagnostic studies, demonstrating discrete cysts that may enhance following the administration of contrast media depending on the degree of surrounding inflammation. Analysis of the cerebrospinal fluid usually reveals lymphocytes or eosinophils accompanied by low glucose and elevated protein. Serologic tests detecting antibody directed against Taenia solium may be positive, particularly in patients with multiple cysts. The sensitivity of the test depends on the activity of the cysts as well as their number. Computed tomography scan with contrast of the cerebral cortex, showing two typical ring-enhancing lesions of neurocysticercosis (arrow). Albendazole and praziquantel may kill living cysts, but larval death results in increased inflammation and edema, and may exacerbate symptoms. A recent randomized trial and a meta-analysis suggested that in symptomatic patients with cortical lesions, albendazole combined with oral dexamethasone (2 mg three times daily) or oral prednisone (40 mg daily) enhances resolution of the lesions and reduces the incidence of seizures. Surgical resection of cysts may be required depending on the symptoms and size and location of the offending cyst. Antiepileptic medications can be safely withdrawn for solitary lesions, if albendazole treatment results in complete resolution without residual calcification. Contracted by ingesting eggs in fecally contaminated food or encysted larvae in undercooked pork. Symptoms develop after many years when the larvae die, causing increased inflammation. Diagnosis is made by computed tomography scan, magnetic resonance imaging, or serology. Treatment involves administration of albendazole plus corticosteroids for symptomatic disease; surgical resection can be performed in selected patients. Occasionally, fatal during the early stage of infection as a result of a severe serum-sickness syndrome. Primary infection does not occur in the United States because the critical intermediate host-a specific type of freshwater snail-is absent. However, approximately 400,000 imported cases occur in immigrants from Puerto Rico, South America (particularly Brazil), the Middle East, and the Philippines. The parasite is contracted by exposure to freshwater containing infectious cercariae. The fork-tailed cercariae are able to swim to and penetrate the skin of people wading in stagnant infested freshwater pools or rice paddies. Once inside the host, cercariae lose their tails and mature into schistosomulae that enter the bloodstream. From the bloodstream, they penetrate the lung and liver, where over a period of 6 weeks, they mature to adult worms. The adult worms then migrate through the venous plexus to various sites, depending on the Schistosoma strain. Once resident in the host, the worms can live for decades, releasing eggs into the bowel or bladder. Improper handling of contaminated stool and urine leads to egg contamination of water. Eggs hatch in freshwater, forming miracidia whose cilia enable them to swim and infect freshwater snails. Each species of schistosome requires a specific freshwater snail intermediate, which explains the geographic distribution of each strain. Cercariae mature into schistosomulae that enter the bloodstream and migrate to the liver and lung, where they mature. The worms release eggs into stool or urine for many years, resulting in contamination of freshwater. Freshwater snails are infected by miracidia, a necessary step in the production of cercariae and infection of humans. Soon after returning from a 1-week vacation in Malawi, he had an episode of perineal pain associated with painful ejaculation and browncolored ejaculate. Four months before the evaluation, this patient had begun experiencing urinary frequency, with intermittent passage of small blood clots in the urine. A urogram and ultrasound demonstrated a round structure, 8x10 mm in diameter, adherent to the bladder wall. Cystoscopic examination disclosed multiple, slightly raised, polypoid lesions that were less than 5 mm in diameter. Low-power microscopic examination of material from a bladder biopsy revealed a polypoid inflammatory lesion of the bladder mucosa with dense inflammatory infiltrate surrounding clusters of eggs in the submucosa. At higher magnification, the granulomas were found to contain clusters of helminthic eggs surrounded by epithelioid histiocytes, chronic inflammatory cells, and eosinophils. An avian schistosome is also able to penetrate the skin, but it is not capable of entering the bloodstream. Patients develop a serum-sicknesslike syndrome as they react with elevated levels of immunoglobulin E and peripheral eosinophilia to egg antigens. Fever, headache, cough, chills, and sweating are accompanied by lymphadenopathy and hepatosplenomegaly. This clinical constellation has been called "Katayama fever" and is most commonly associated with S.
Purchase bystolic 2.5mg online
Monitoring Systolic function should be directly assessed intraoperatively with trans-esophageal echocardiography arrhythmia management discount 2.5 mg bystolic with visa, while invasive arterial pressure monitoring should subsequently be established [2]. Right atrial or central venous pressure should be monitored, as well as measurement of left atrial or pulmonary artery wedge pressures. In particular, one should pay attention to the relationship between right and left atrial pressures, in case of isolated right or left ventricular dysfunction. In recipients with a prior history of pulmonary hypertension, particular attention should also be given to pulmonary artery pressure as high pulmonary artery pressures may lead to right ventricular failure. Intermittent measurement of cardiac output is considered prudent, along with continuous measurement of arterial oxygen saturation [2]. Hemodynamics Most important in determining post-transplant survival is the ability of the newly transplanted heart to generate sufficient cardiac output in the early hours and days following transplantation. As initial donor heart dysfunction is relatively common, with reports of occurrence in up to 50% of Inotropic and Vasoactive Support for Ventricular Dysfunction Hemodynamic instability early post-transplant is relatively common and may be secondary to graft reperfusion injury, post-bypass inflammation, 9 Immediate Post-operative Management After Heart Transplantation 97 hyperacute rejection, cardiac tamponade, primary graft dysfunction, elevated pulmonary vascular resistance or labile fluid status. As such, inotropic and vasoactive pharmacologic support is routinely necessary to augment the marginal cardiac output mediated by ventricular dysfunction and associated systemic hypotension. Furthermore, the catecholamine stores of the newly transplanted heart are often depleted, requiring exogenous supplementation [3]. Continuous infusions of isoproterenol, dobutamine, dopamine and/or milrinone all increase left ventricular contractility as well as right ventricular function if applicable, without the negative Table 9. Luu vasoconstrictive effects of alpha-adrenergic agonists such as norepinephrine and epinephrine. However, occasionally there may be incidences of low systemic vascular resistance where mean arterial pressures remain low following cardiopulmonary bypass. In this situation, continuous infusion of alpha-adrenergic agonists including phenylephrine, norepinephrine and/or epinephrine may be used to maintain adequate mean arterial pressure. Low dose vasopressin or methylene blue may also be used to treat cases of vasodilatory shock, where alpha-agonists have been ineffective in countering low systemic vascular resistance [2]. In cases where hemodynamic instability is profound, with persistently poor ventricular function and low systemic vascular resistance despite maximal inotrope/vasoactive agent use, underlying causes such as cardiac tamponade or hyperacute rejection should be considered. Direct surgical exploration should be used to check for tamponade, while hyperacute rejection should be treated aggressively (see below). Factors such as risk of infection, immobility and the need for anti-coagulation should be considered [2]. Treating Specific Causes or Features of Early Hemodynamic Instability Hyperacute Rejection Hyperacute rejection, though now rare, is mediated by preformed antibodies to the allograft in the recipient. The development of the modern prospective cytotoxic crossmatch, and subsequently the virtual cross-match (mentioned in Chap. In addition to aggressive inotropic and mechanical support for the ailing graft if necessary, aggressive treatment consisting of high dose intravenous corticosteroids, plasmapheresis, intravenous immunoglobulin, anti-thymocytye globulin as well as immediate initiation of immunosuppression maintenance therapy (calcineurin inhibitor, anti-proliferative) should also be administered. The role of complement blockade in hyperacute rejection has not yet been established. Cardiac Tamponade the sudden appearance of right or left ventricular dysfunction during the first few days posttransplant may indicate the accumulation of blood or other fluid in the mediastinum. Cardiac tamponade should be excluded as a possible cause by direct surgical exploration in the event of persistent hemodynamic instability, and if present, evacuated appropriately. Primary Graft Dysfunction Primary Graft Dysfunction is defined as left, right or biventricular dysfunction developed within 24 h after completion of cardiac surgery with no identifiable etiology. It is the most frequent cause of death in the first 30 days after transplant, occurring on average in 7% of patients [1]. The cause is thought to be multifactorial, and has been speculated to include trauma from brain death in the donor, insufficient preservation, hypothermic ischemia during transport, reperfusion injury and adverse systemic factors in the recipient such as persistent hypotension [1]. Classification is determined by the level of pharmacologic or mechanical support required in the patient. The donor right ventricle is particularly vulnerable to periprocedural myocardial strain, ischemia, cardioplegia, and surgical trauma. Such a situation might also be further exacerbated by a donor heart that is too small for a larger recipient. After stabilization of graft function, the aim is then to wean the patient from ventilatory and pharmacologic therapy as soon as possible. However, to specifically target pulmonary vascular hypertension, systemic vasodilators with pulmonary vasodilating properties have also been demonstrated to be useful in this setting; such agents include nitroglycerine and sodium nitroprusside, which may be used in the absence of systemic hypotension (see Table 9. At some institutions, they are used as a first-line treatment and may be administered perioperatively. Examples of selective vasodilators include prostaglandin E1 analog alprostadil, the prostaglandin I2 derivatives epoprostenol or iloprost, inhaled nitric oxide, and sildenafil (see Table 9. Generally, milder cases of right ventricular dysfunction will respond favorably to a vasodilating agent with concomitant inotropic support. Post-transplant Rate and Rhythm While the majority of transplanted hearts exhibit normal sinus rhythm in the operating room shortly after reperfusion and clinically important arrhythmias are rare in the proceeding weeks, sinus node dysfunction post-transplant is very common with prevalence as high as 50% [15]. The parameters affected may include prolonged sinus node recovery time, prolonged corrected sinus node recovery time, and abnormal sinoatrial conduction time. While the etiology is unclear, sinus node dysfunction is believed to be multifactorial in origin, including surgical trauma, cardiac denervation, myocardial ischemia and preservation injury [16]. Sinus node dysfunction is seen more commonly with the biatrial cuff surgical technique due to manipulation of the sinus node of the donor heart during implantation. Sinus bradycardia is also common for patients on preoperative amiodarone as this medication has a 30-day half-life and can temporarily slow the sinus node of the donor heart early after transplant. Furthermore, it is recommended that both atrial and ventricular temporary epicardial 102 J. Luu pacing wires should be placed at the time of heart transplantation, even if the initial rhythm is sinus. Management Post-transplantation bradycardia resulting from sinus node dysfunction is perhaps the most common rate disorder after transplantation. Such pharmacologic chronotropic agents may include isoproterenol, terbutaline or theophylline, an adenosine receptor antagonist, while awaiting return of normal sinus node function. Asymptomatic transient arrhythmias, both atrial and ventricular, are common posttransplantation. Persistent post-operative tachyarrhythmias, regardless of being atrial or ventricular, should prompt investigation for possible rejection, and if rejection is absent, electrophysiology and coronary angiography evaluation. Ventricular arrhythmias may result from ischemia-reperfusion injury and metabolite disturbances, but are rarely malignant except when seen in the presence of hyperacute rejection. It is important to note that prolonged anti-arrhythmic therapy (>3 months) is generally not indicated, as most arrhythmias post-transplant are transient. Furthermore, amiodarone is associated with significant drug interaction with calcineurin inhibitors, requiring close monitoring of drug levels; beta blockers and calcium channel blockers should also be used cautiously, due to the risk of bradycardia and interactions with immunosuppressants. Although sinus node dysfunction is typically transient [21], some patients display permanent sinus node dysfunction and require permanent pacing. Pacemaker implantation is usually delayed until the third week post-transplantations. Renal Function and Fluid Balance Renal Function Renal reserves are often impaired prior to transplantation simply due to the prolonged low cardiac output and chronic administration of diuretics that occurs in end-stage heart failure. Hence, appropriate management in order to maintain sufficient cardiac performance (as detailed 9 Immediate Post-operative Management After Heart Transplantation 103 above) is particularly important in minimizing negative renal outcomes. Due to the factors mentioned above, oliguria (<50 ml/h) and an increase in serum creatinine (>1. This may occur particularly in patients who were on high-dose diuretics prior to transplantation due to end-stage heart failure. In these oliguric patients, aggressive diuretic therapy targeting urine output of >50 ml/h may be required. Patients with pre-existing renal insufficiency (serum creatinine >2 mg/dl) may receive a course of antithymocyte globulin, a polyclonal immunosuppression agent (see Chap. Should renal dysfunction remain severe and refractory to pharmacologic treatment despite adequate cardiac output, temporary hemodialysis is an option until renal function improves.

Discount bystolic 2.5mg with amex
Moxifloxacin is also partially metabolized by the liver heart attack meme order bystolic 5 mg without prescription, and gemifloxacin is metabolized primarily by the liver. All quinolones demonstrate similar tissue penetration, being concentrated in prostate tissue, feces, bile, and lung tissue. As a result of an excellent gram-negative spectrum, ciprofloxacin is one of the primary antibiotics recommended for treatment of urinary tract infections. It is the drug of choice for Salmonella typhi (typhoid fever), and it also is recommended for treatment of Salmonella gastroenteritis when antibiotic treatment is necessary. Ciprofloxacin is the recommended treatment of cat scratch disease caused by Bartonella henselae. With the exception of gemifloxacin, these agents can also be used in soft tissue infection in which a combination of gram-positive and gram-negative organisms is suspected. Given the worse toxicity profiles of the three newer agents (moxifloxacin, gatifloxacin, and gemifloxacin), levofloxacin should probably be the fluoroquinolone of choice for those infections. Gatifloxacin and moxifloxacin demonstrate moderate in vitro activity against anaerobes and may be considered for the treatment of mixed infections thought to include anaerobes. Fear of selecting for resistant pathogens has led to their use being restricted in some hospitals. Also covers many other gramnegative organisms including Escherichia coli, Salmonella, Shigella, Neisseria, and Legionella. Levofloxacin, gatifloxacin, moxifloxacin, gemifloxacin: a) Greater activity against Streptococcus pneu-moniae, covers highly penicillin-resistant strains. These agents bind to the 50S ribosome at a site similar to that used by chloramphenicol. The oxazolidinones are bacteriostatic against staphylococcal species and enterococci. Reversible thrombocytopenia has been reported in association with prolonged therapy, and monitoring of platelet count is recommended for patients receiving two or more weeks of linezolid. Because this agent is a weak inhibitor of monoamine oxidase, hypertension has been reported in association with ingestion of large amounts of tyramine. Pseudoephedrine and selective serotonin reuptake inhibitors should be prescribed with caution. Like chloramphenicol, binds to the 50S ribosome subunit; inhibits the initiation of protein synthesis. Thrombocytopenia common with treatment exceeding 2 weeks; inhibitor of monoamine oxidase; avoid tyramine, pseudoephedrine, and serotonin uptake inhibitors. A combination of 30:70 quinupristin:dalfopristin has synergistic activity and has been named Synercid. These two agents inhibit bacterial protein synthesis by binding to the 50S bacterial ribosome. Quinupristin inhibits peptide chain elongation, and dalfopristin interferes with peptidyl transferase activity. Daptomycin has a mechanism of action that is distinctly different from that of other antibiotics. It binds to bacterial membranes and causes rapid depolarization of the membrane potential. This antibiotic is cidal and causes rapid concentration-dependent killing, but it does not result in the systemic release of cell membrane or cell wall contents. Synergy with aminoglycosides, -lactam antibiotics, and rifampin has been observed. Less commonly, daptomycin administration has resulted in neuropathy associated with a slowing of nerve conduction velocity. More recently, daptomycin treatment has also been associated with eosinophilic pneumonia. This antibiotic is approved for the treatment of complicated skin and soft tissue infections by susceptible strains and for S. Daptomycin is inactivated by surfactant and should not be used for the treatment of pneumonia. Toxicities include muscle pain and weakness associated with creatine phosphokinase leak; no coadministration of statins. Within a bacterium, this antibiotic acts as an electron acceptor and is quickly reduced. Metronidazole is not recommended in pregnancy, and it should usually be avoided in patients on Coumadin, because it impairs metabolism of that drug. Antabuse-like reaction can occur; mutagenic effects not proven in mammals, but the drug should be avoided in pregnancy. Metronidazole is cidal for most anaerobic bacteria, and it is the antibiotic of choice for covering anaerobes. Because metronidazole has no significant activity against aerobes, it is usually administered in combination with a cephalosporin for aerobic coverage. Metronidazole is the drug of choice for treatment of pseudomembranous colitis attributable to overgrowth of C. Alterations in the sulfonyl radical determine many of the pharmacokinetic properties of the compounds. Trimethoprim consists of two 6-member rings, one of which has two nitrogens and two amino groups, the other having three methoxybenzyl groups. Sulfonamides should be avoided in the last month of pregnancy because they displace bilirubin bound to plasma albumin and increase fetal blood levels of unconjugated bilirubin. Competitively inhibit para-aminobenzoic acid incorporation, blocking folic acid synthesis; trimethoprim inhibits dihydrofolate reductase, potentiating sulfonamide activity. Broad spectrum of activity for gram-positive and gram-negative organisms, but resistance is common. Trimethoprim-sulfamethoxazole combination is the drug of choice for Pneumocystis prophylaxis and treatment. All are metabolized by the liver, undergoing acetylation and glucuronidation, with the metabolites being excreted in the urine. Trimethoprim is excreted primarily by the renal tubules, and very high concentrations of active drug are found in the urine. The half-life of trimethoprim is 9-11 hours matching the half-life of sulfamethoxazole. Sulfonamides have proved to be effective for the empiric treatment of uncomplicated urinary tract infections; however, because of widespread resistance, they are seldom used as empiric therapy in other infections. Sulfonamides are the treatment of choice for Nocardia asteroides, and are useful in combination with other agents for the treatment of M. It can be used to treat a number of other gram-positive and gram-negative pathogens. However, plasmid-mediated resistance is common, and treatment of most pathogens should be initiated only after sensitivity is confirmed by microbiologic testing. Colistin this antibiotic was discovered in the 1980s, but abandoned because of fears of undue nephrotoxicity. Because of the progressive increase in multiresistant Gram-negative bacilli, the use of colistin has been revisited. Complex mixture of polymyxins and natural polypeptides that bind to bacterial lipopolysaccharide and disrupt the membrane barrier 2. Narrow spectrum, used to treat multiresistant Pseudomonas aeruginosa, Acinetobacter baumannii, Stenotrophomonas maltophilia, and Klebsiella pneumoniae. The polymyxins all have a strong positive charge and a hydrophobic acyl chain that binds with high affinity to the lipopolysaccharide bacterial membrane. Upon binding, colistin acts as a cationic detergent that disrupts the membrane barrier causing leakage of cell contents and eventual death of the bacterium. Risk factors for this complication include older age, preexisting renal insufficiency, low serum albumin, and coadministration of nonsteroidal antiinflammatory drugs or vancomycin. The onset of renal dysfunction usually occurs within the first week of administration and is reversible upon discontinuation in nearly 90% of patients. In cystic fibrosis patients, colistin may be less nephrotoxic than aminoglycosides. Other rarer neurological manifestations associated with administration include seizures, vertigo, muscle weakness, confusion, hallucinations, partial deafness and visual loss. These neurological side effects have been reported to quickly resolve upon discontinuing the drug. The half-life of the drug is approximately 14 hours and once per day therapy may be preferable; however until clinical studies demonstrate no increase in toxicity once per day administration, q12h dosing is the preferred dosing interval.
Buy bystolic now
Heart-Lung Transplant: Specific Complications For heart-lung transplants heart attack lyrics 007 generic bystolic 2.5mg with amex, the approach to mitigating and managing complications is similar to that for isolated heart transplant patients, detailed in Chaps. However, cardiologists should also be aware of the potential lung-specific complications in this cohort, as most complications following dual heart-lung transplant are lung-related. Interestingly, both cardiac rejection rates and cardiac allograft vasculopathy rates in heart-lung patients are reduced compared to rates in isolated heart transplant patients [27], although the exact reason for this phenomenon is not known. In many programs, routine surveillance heart biopsies are reduced as a result of less observed rejection. Exact incidences are difficult to determine, as many cases are clinically silent and only discovered by surveillance bronchoscopic biopsies, which are not regularly performed from center to center. In stable asymptomatic patients, regular home surveillance by spirometry is still needed, as "silent" rejection may be detected by a drop in spirometry. In this system, a severity grade is assigned to both the perivascular/interstitial component (a-grade) and airway component (b-grade). In addition, other pathological processes that lead to chronic rejection have been identified. While the exact etiology is unknown, there is strong evidence to suggest that it is mediated by immunologic injury [34]. Diagnosis is most definitively made with a surgical biopsy, but in practice most patients are diagnosed clinically. Patients show progressive airflow obstruction that cannot be attributed to any specific cause [35]. Many treatment strategies have been tried, including augmentation of immunosuppression, total lymphoid irradiation, and photopheresis [38]. There is lymphoid hyperplasia around the airways and eventually this progresses to bronchiectasis. Survival after Heart-Lung Transplantation Since the early 1980s, when the dual heart-lung transplant was first performed, the outcomes have improved with each subsequent era [3]. A common theme is that although late survival has improved, the most significant improvements are noted during the early post-transplant period. Early mortality is worse in combined heartlung compared with single heart or single lung transplantation. Late mortality, however, is better than for single lung transplantation but still worse than single heart transplantation. In patients who survive the first year post-transplant, the conditional median survival is 10. Over the years, better patient selection, refinement of surgical techniques, immunosuppressive therapy preventing graft rejection, and improved understanding of risk factors for morbidity and mortality have all contributed to these improved outcomes [3]. While longer-term outcomes after dual heartlung transplant are very similar to outcomes after lung transplantation, they are significantly worse than after heart transplantation; most complications after heart-lung transplant are lung-related. Despite limited data, risk factor analyses of mortality demonstrate that patients reliant on mechanical ventilation or circulatory support prior to dual heart-lung transplant suffer worse outcomes that those not reliant [19]. Given that most complications are lung-related in the heart-lung population, it would seem prudent to infer that these factors might also lead to increased mortality in a dual heart-lung transplant cohort. For the same reasons, patients with primary endstage renal failure and coexisting severe heart disease have often been overlooked for transplantation. Furthermore, calcineurin inhibitors, a mainstay of immunosuppression, are known to exert nephrotoxic effects. However, the improvement in long-term outcomes over the past 25 years has led to this rare procedure being performed more frequently. Selection While there are no established guidelines on selecting heart-kidney transplant candidates, patients being considered for this procedure typically fall into three different categories: those with combined primary end-stage heart disease and intrinsic (primary) kidney disease; severe renal dysfunction secondary to severe heart failure; and end-stage intrinsic kidney disease with secondary heart disease. Most common is the patient with co-existing combined end-stage primary heart and kidney disease. Common causes of the primary cardiac disease include idiopathic dilated cardiomyopathy and ischemic heart disease, while common causes of the renal disease include diabetes mellitus and chronic glomerulonephritis [42]. The majority of combined heart-kidney transplants, and hence the majority of data on this topic, have been performed on this cohort of patients [40]; it is considered more controversial to transplant patients with secondary renal or cardiac dysfunction. Many centers have used this procedure with no worse outcomes than either organ transplanted alone. Diagnosis of Rejection With regard to frequency of rejection after combined heart-kidney transplant, there is limited data; however, an early multicenter report demonstrates a lower incidence of acute cardiac and renal rejection than expected when compared to rates of rejection for the transplantation of each individual organ [42]. Rejection is often clinically diagnosed on the basis of increasing creatinine or dysuria. There have been less than 200 heart-liver transplants performed in the history of transplantation in the United States, and hence this is a rare topic. Potential candidates are those with endstage heart and liver disease of varying etiology, end-stage heart and liver disease of related etiology [48], and end-stage heart disease where liver transplantation is needed in order to correct an underlying metabolic disorder. Other examples include biliary atresia and iron deposition disorders such as homozygous betathalassemia and genetic hemochromatosis. It is hypothesized that the liver confers protection by absorbing donor specific antibodies. The exact mechanism has not been demonstrated but could be through the phagocytic action of Kupffer cells. Survival is comparable to single orthotopic heart transplantation with 1- and 5-year survival at 83. Outcomes Multiple studies have actually demonstrated superior outcomes in heart-kidney recipients compared to isolated heart transplant recipients in terms of long-term survival [40, 42, 44, 45], especially in end-stage heart failure patients dependent on dialysis. Heart-lung transplantation: successful therapy for patients with pulmonary vascular disease. State of the art of combined heart-lung transplantation for advanced cardiac and pulmonary dysfunction. Right and left ventricular area and function determined by two-dimensional echocardiography in adults with the Eisenmenger syndrome from a variety of congenital anomalies. Heart-Liver Transplantation the first combined heart-liver transplant occurred in 1984, described by Starzl et al. Medical management of heart failure and candidate selection: comparison of the hemodynamics and survival of adults with severe primary pulmonary hypertension or Eisenmenger syndrome. Quantitative ultrasonic tissue characterization of myocardium in cyanotic adults with an unrepaired congenital heart defect. A clinical perspective in a new therapeutic era of pulmonary arterial hypertension. Repair of congenital heart lesions combined with lung transplantation for the treatment of severe pulmonary hypertension: a 13-year experience. Lung and heart-lung transplant practice patterns in pulmonary hypertension centers. Indications for and results of single, bilateral, and heart-lung transplantation for pulmonary hypertension. Comparative outcome of heart-lung and lung transplantation for pulmonary hypertension. Long-term outcome of double-lung and heart-lung transplantation for pulmonary hypertension: a comparative retrospective study of 219 patients. Prognosis in chronic obstructive pulmonary disease: results from multicenter clinical trials. Impact of extracorporeal membrane oxygenation or mechanical ventilation as bridge to combined heart-lung transplantation on short-term and long-term survival. Does donor arterial partial pressure of oxygen affect outcomes after lung transplantation Dual ex vivo lung perfusion techniques ameliorate airway hypoxia in lung grafts in rats. A consensus statement of the International Society for Heart and Lung Transplantation. Multiorgan transplantation: is there a protective effect against acute and chronic rejection Analysis of time-dependent risks for infection, rejection, and death after pulmonary transplantation. Analysis of risk factors for the development of bronchiolitis obliterans syndrome. Risk factors for the development of bronchiolitis obliterans syndrome after lung transplantation.