Order calcitriol no prescription
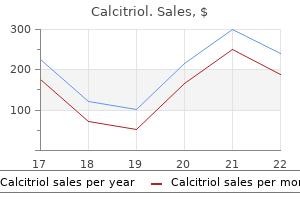
It runs distally and medially from the anterior inferior edge of the lateral malleolus to attach to the talus and is a thin structure treatment 5th metatarsal stress fracture buy calcitriol overnight delivery, approximately the width of the little finger. The bifurcate calcaneocuboid ligament runs from the calcaneus to the cuboid and is often also involved in ankle sprains. It is rounder, so it is more easily palpated than the other two ligaments and less commonly injured. Taping, together with a pressure pad behind the malleolus, helps control swelling. The patient keeps the ankle constantly moving within the pain-free range while elevated, and active and passive mobilization with balance training and instruction on normal heel-toe gait should be administered. A hairline fracture of the fibula should be suspected if pain is worse on weight bearing. If the above regimen has not been followed, and the lesion is in the chronic stage, physiotherapeutic treatment with deep massage, manipulation, exercises to strengthen the peronei and proprioception techniques is probably the best approach. Practice point this is not a common injection because the treatment of choice is early physiotherapy, but is an option when conservative treatment has failed in the chronic stage or the ligament is too painful. The automatic use of crutches in the acute stage should be avoided if at all possible because this tends to reinforce limping and delays normal healing. Slide needle along side of tendon, taking care not to enter into tendon itself Deposit half of the solution while slowly withdrawing needle Insert needle on lateral side and repeat procedure with remaining solution Aftercare Absolute avoidance of any overuse is essential until pain free. In the case of the committed athlete, or if scanning shows significant degenerative changes, a conservative physiotherapeutic approach should be used. This might include an eccentric exercise programme, a glyceryl trinitrate patch, taping, orthotics, deep friction and/or electrotherapy. Practice point It is absolutely contraindicated to infiltrate the body of the tendon because this is a large, weight-bearing, relatively avascular tendon, with a known propensity to rupture. Although there have been reports of tendon rupture after injection here, this has usually occurred as a result of repeated bolus injections of large doses and volumes into the body of a degenerated tendon, followed by excessive exercise postinjection. Because of this recognized risk, we recommend always scanning the tendon before injecting to ascertain the extent of any degeneration (see Section 1, Chapter 6). Tears and degenerative changes within the substance of the tendon would be an absolute contraindication to injection. The longus then divides to pass under the arch of the foot to insert at the base of the big toe, and the brevis inserts into the base of the fifth metatarsal. The division of the two tendons is the entry point for the needle to slide inside the sheath; it can be found by having the patient hold the foot in strong eversion and palpating for the V-shaped fork of the tendons. There should be minimal resistance, and often a sausage-shaped bulge is observed the sheath proximaly towards malleolus Avoid any overuse until symptom free. Resolution of symptoms should then lead to consideration of change in footwear, orthotics and strengthening of the evertors; usually, proprioception retraining is necessary. Practice point this lesion often occurs together with acutely sprained lateral ligaments of the ankle. Examination of the joint should ascertain if one or more ligaments are also affected, and all should be treated if necessary. The same amount of solution is then peppered into the teno-osseous junction by inserting the needle parallel to the skin to touch the base of the fifth metatarsal. Less common is a sprain of the flexor tendons on the medial side of the foot; the signs there will be pain on resisted flexion and inversion. The lesion is invariably found at the medial head, and significant localized tenderness of this area can be elicited by deep pressure with the thumb. Advance at 45 degrees towards calcaneus until touching bone Advise gel heel raises in both ankle boots for men or low-heeled shoes in women after the injection, followed by intrinsic muscle exercise and daily active stretching of the fascia. Rolling the foot on a golf ball or dense squash ball to apply deep friction can be helpful, and orthotics or taping can be applied. Practice point the classic history of pain under the heel when putting the foot to the floor on arising from bed in the morning is usually diagnostic. Although this would appear to be an extremely painful injection, this approach is much kinder than inserting the needle straight through the heel pad. Patients usually tolerate it surprisingly well, and depositing a few drops of the solution as the needle passes through the tissue will give an anaesthetic result. Heel spurs are often seen on x-rays of this area and may be an incidental finding. If this is the cause, the patient complains of pain more on static weight bearing. The use of a pad with a hole in the middle can relieve the symptoms, but a surgical solution might be considered. The history of burning pain, especially at night, and squeezing of the heads or stretching the nerve by hyperextending the toes is usually indicative of this lesion. Placing a small pad just proximal to the metatarsal head to lift the bone and reduce the compression for the first weeks postinjection is helpful. Recurrence of symptoms usually indicates that the patient should discuss operative options with a foot surgeon. Practice point As with all injections around neural tissue, care must be taken to approach the nerve slowly because the sudden sharp pain induced if the nerve is entered may make the patient jump. The drug is deposited around the neuroma, not into the substance of the nerve, which might permanently damage it. A few, however, are unusual presentations with rare diagnoses, which will hopefully challenge you more, as they did us. Clinical findings the information given here is what was found on examination using the routine as described in the text. These are divided into which physical tests provoked pain, loss of power and/or limitation of range. He now complains of constant ache around his left greater trochanter, aggravated by lying on it, walking and sitting for long periods. Since then, he has had severe pain on getting up from sitting, the hip occasionally locks and it seems as if it is about to give way. He takes off at great speed on water skis behind the hotel motor boat, immediately does the splits and feels a searing pain on the inner side of his right groin. She has suffered pain in both buttocks and groins from the age of 14, with no history of trauma. Over the past few years, the pain has occasionally spread down the front of both thighs, right (R) more than left (L), and the riding aggravates this. Pain began after 20 miles and was relieved by high doses of oral anti-inflammatory medication, enabling the patient to complete the competition. He is now complaining of low-level constant groin pain, 4/10, which radiates down the anterior aspect of the thigh when trying to run. It is worse on walking and has become so bad that she is unable to lie down in bed at night, so has to sleep sitting up. He has pain on squatting and turning his body to the left, and occasionally it feels as if the leg is about to give way. It sometimes swells slightly when the pain is pronounced, and the joint temporally locks occasionally. Some months later, she still has pain on twisting and squatting and the knee occasionally feels unstable. All investigations are normal and painkillers help temporally, but an exercise treatment programme has aggravated the condition. He felt a sharp pain at the time of the fall, was taken down the mountain on the blood wagon and the knee was swollen when examined an hour later. His knee is very swollen and warm, and he has constant pain of 8/10, rising to 10/10 on any movement.
Blind Nettle (White Dead Nettle Flower). Calcitriol.
- Are there safety concerns?
- Dosing considerations for White Dead Nettle Flower.
- How does White Dead Nettle Flower work?
- Swelling (inflammation) of the upper airways, sore throat, skin inflammation, vaginal discharge, and other conditions.
- What is White Dead Nettle Flower?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96362
Cheap 0.25mcg calcitriol with mastercard
No information is given regarding the maximal antihypertensive response to either drug symptoms 7 days pregnant discount calcitriol online visa. The fact that a given response is achieved with a smaller dose of blocker A indicates only that A is more potent than B in the ratio of 500:5. Thus, quantal studies are used to determine the therapeutic index and the variation in sensitivity to the drug in the population studied. Graded (not quantal) dose-response curves are used to determine maximal efficacy (maximal response). Drug A produces 50% of its maximal effect at a lower dose than either B or C and thus is the most potent; drug C is the least potent. Choices involving chemical or physiologic antagonism are incorrect because novamine is said to act at the same receptors as acetylcholine. When given alone, the novamine effect is opposite to that of acetylcholine; so choice C is incorrect. Spare receptors may be defined as those that are not needed for binding drug to achieve the maximal effect. Spare receptors influence the sensitivity of the system to an agonist because the statistical probability of a drug-receptor interaction increases with the total number of receptors. Similarly, no information on efficacy (maximal effect) is presented; this requires graded dose-response curves. Although both drugs are said to be producing a therapeutic effect, no information on their receptor mechanisms is given. Since no data on toxicity are available, the therapeutic index cannot be determined. Sugammadex interacts directly with rocuronium and not with the rocuronium receptor; therefore, it is a chemical antagonist. The binding of a full agonist decreases as the concentration of a partial agonist is increased to very high levels. As the partial agonist displaces more and more of the full agonist, the percentage of receptors that bind the full agonist drops to zero, that is, Curve 5. Curve 1 describes the response of the system when a full agonist is displaced by increasing concentrations of partial agonist. This is because the increasing percentage of receptors binding the partial agonist finally produce the maximal effect typical of the partial agonist. Partial agonists, like full agonists, bind 100% of their receptors when present in a high enough concentration. In contrast, pharmacologic antagonists bind to the agonist site and prevent access of the agonist. The difference can be detected experimentally by evaluating competition between the binding of radioisotopically labeled antagonist and the agonist. High concentrations of agonist displace or prevent the binding of a pharmacologic antagonist but not an allosteric antagonist. Predict the effect of a partial agonist in a patient in the presence and in the absence of Name the types of antagonists used in therapeutics. Describe the difference between an inverse agonist and a neutral pharmacologic antagonist. Specify whether a pharmacologic antagonist is competitive or irreversible based on its effects on the dose-response curve and the dose-binding curve of an agonist in the presence of the antagonist. Give examples of competitive and irreversible pharmacologic antagonists and of Name 5 transmembrane signaling methods by which drug-receptor interactions exert Describe 2 mechanisms of receptor regulation. A drug may have high efficacy but low potency or vice versa the ability to activate (agonism) or inhibit (antagonism) a biologic system or effect. In addition, the binding of a drug may be at the site that an endogenous ligand binds that receptor, or at a different site. Many drugs act on intracellular functions but reach their targets in the extracellular space. On reaching the target tissue, some drugs diffuse through the cell membrane and act on intracellular receptors. Changes in the rates of these processes may be noted as upregulation or downregulation of the receptor numbers and usually take days to accomplish. The major processes involved in pharmacokinetics are absorption, distribution, and elimination. Appropriate application of pharmacokinetic data and a few simple formulas makes it possible to calculate loading and maintenance doses. Units: liters the ratio of the rate of elimination of a drug to the concentration of the drug in the plasma or blood. Units: volume/time, eg, mL/min or L/h the time required for the amount of drug in the body or blood to fall by 50%. For drugs eliminated by first-order kinetics, this number is a constant regardless of the concentration. Units: time the fraction (or percentage) of the administered dose of drug that reaches the systemic circulation the graphic area under a plot of drug concentration versus time after a single dose or during a single dosing interval. The plasma concentration is a function of the rate of input of the drug (by absorption) into the plasma, the rate of distribution into other tissues, and the rate of elimination. These parameters are unique for a particular drug and a particular patient but have average values in large populations that can be used to predict drug concentrations. Because the size of the compartments to which the drug may be distributed can vary with body size, Vd is sometimes expressed as Vd per kilogram of body weight (Vd/kg). Drug A diffuses freely between the 2 compartments and does not bind to macromolecules (heavy wavy lines) in the vascular (volume 1 L) or the extravascular compartments (volume 5 L) of the hypothetical organism in the diagram. With 20 units of the drug in the body, the steady-state distribution leaves a blood concentration of 2 units/L. At equilibrium, only 2 units of the total are present in the extravascular volume, leaving 18 units still in the blood. In each case, the total amount of drug in the body is the same (20 units), but the apparent volumes of distribution are very different. Drug C is avidly bound to molecules in peripheral tissues, so that a larger total dose (200 units) is required to achieve measurable plasma concentrations. At equilibrium, 198 units are found in the peripheral tissues and only 2 units in the plasma, so that the calculated volume of distribution is greater than the physical volume of the system. The Vd of drugs that are normally bound to plasma proteins such as albumin can be altered by liver disease (through reduced protein synthesis) and kidney disease (through urinary protein loss). For example, 50,000 liters is the average Vd for the drug quinacrine in persons whose average physical body volume is 70 liters. The clearance of a particular drug by an individual organ is equivalent to the extraction capability of that organ for that drug times the rate of delivery of drug to the organ. Thus, the clearance of a drug that is very effectively extracted by an organ (ie, the blood is completely cleared of the drug as it passes through the organ) is often flow-limited. For such a drug, the total clearance from the body is a function of blood flow through the eliminating organ and is limited by the blood flow to that organ. In this situation, other conditions-cardiac disease, or other drugs that change blood flow-may have more dramatic effects on clearance than disease of the organ of elimination. The magnitudes of clearance for different drugs range from a small percentage of the blood flow to a maximum of the total blood flow to the organs of elimination. Like clearance, half-life is a constant for drugs that follow first-order kinetics. Disease, age, and other variables usually alter the clearance of a drug much more than they alter its Vd. Since elimination rate is equal to clearance times plasma concentration, the elimination rate will be rapid at first and slow as the concentration decreases. The bioavailability of a drug is the fraction (F) of the administered dose that reaches the systemic circulation. Bioavailability is defined as unity (or 100%) in the case of intravenous administration. The concentration rises smoothly with time and always reaches 50% of steady state after 1 half-life, 75% after 2 half-lives, 87. The decline in concentration after stopping drug administration follows the same type of curve: 50% is left after 1 half-life, 25% after 2 half-lives, and so on. The asymptotic approach to steady state on both increasing and decreasing limbs of the curve is characteristic of drugs that have first-order kinetics.
Buy generic calcitriol 0.25 mcg line
Anti-motion sickness effect parenterally for dystonias Promethazine: H1 blocker with less anti-motion sickness action and more sedative and autonomic effects Cyclizine symptoms acid reflux generic calcitriol 0.25mcg amex, meclizine: H1 blockers with more anti-motion sickness action and less sedative and autonomic effect Chlorpheniramine: H1 blocker with negligible anti-motion sickness, sedative, and autonomic effects H1 blockers, second generation Cetirizine Competitive pharmacologic block of peripheral H1 receptors. Antagonists of these peptides or the enzymes that produce them have useful clinical properties. Many other endogenous peptides with very important actions (eg, insulin, glucagon, opioid peptides) have less or no direct vascular smooth muscle effects. Conversely, renin release is stimulated, a compensatory response, by vasodilators. It also facilitates the release of norepinephrine from adrenergic nerve endings via presynaptic heteroreceptor action (see Chapter 6). Source and Disposition Angiotensin I is produced from circulating angiotensinogen by the enzyme renin. Its major significance is as an endogenous pathophysiologic mediator in some cases of hypertension (high-renin hypertension) and in heart failure. Angiotensin Antagonists As noted in Chapters 11 and 13, 2 types of antagonists are available. A class of drugs that block both enzymes is in clinical trials, and these drugs (eg, omapatrilat) show considerable efficacy in hypertension and heart failure. Unfortunately, these drugs also cause angioedema in a significant number of patients and have not been approved for clinical use. Constrict most vessels, may play a pathophysiologic role in pulmonary hypertension Causes vasoconstriction and stimulates the heart. Source and Disposition Bradykinin is one of several vasodilator kinins produced from kininogen by a family of enzymes, the kallikreins. The peptide is involved in inflammation and causes edema, vasodilation, and pain when released or injected into tissue. Bradykinin can be found in saliva and may play a role in stimulating its secretion. Bradykinin plays an important causative role in hereditary angioedema and some other types of angioedema. Ecallantide, a parenteral kallikrein inhibitor, and icatibant, a parenteral bradykinin B2-receptor antagonist, are approved for use in angioedema. Bradykinin synthesis can be inhibited by the human plasma derivatives Cinryze and Berinert. This drug is approved for intravenous administration in acute heart failure (see Chapter 13) but has very significant toxicity. Endothelins appear to function as autocrine and paracrine hormones in the vasculature. Endothelins are much more potent than norepinephrine as vasoconstrictors and have a relatively long-lasting effect. The peptides also stimulate the heart, increase natriuretic peptide release, activate smooth muscle proliferation, and reduce glomerular filtration rate. The peptides may be involved in causing some forms of systemic hypertension, pulmonary hypertension, and other cardiovascular disorders. Macitentan, a newer dual inhibitor of both endothelin receptors, is also available for use in pulmonary hypertension. A similar peptide, C-type natriuretic peptide, has been isolated from other tissues. Effects and Clinical Role Natriuretic peptides activate guanylyl cyclase in many tissues via a membrane-spanning enzyme receptor. They act as vasodilators as well as natriuretic (sodium excretion-enhancing) agents. Their renal action includes increased glomerular filtration, decreased proximal tubular sodium reabsorption, and inhibitory effects on renin secretion. Although they lack positive inotropic action, endogenous natriuretic peptides may play an important compensatory role in congestive heart failure by limiting sodium retention. It is found in the central and peripheral nervous systems and in the gastrointestinal tract. The neurokinins, also known as tachykinins, include substance P, neurokinin A, and neurokinin B. It is a potent arteriolar vasodilator and a potent stimulant of veins and intestinal and airway smooth muscle. Highest concentrations of substance P are found in the parts of the nervous system that contain neurons subserving pain. Capsaicin, the "hot" component of chili peppers, releases substance P from its stores in nerve endings and depletes the peptide. Capsaicin has been approved for topical use on arthritic joints and for postherpetic neuralgia. Peripheral administration causes positive chronotropic and inotropic effects in the heart and hypertension. Several receptor subtypes have been identified, but neither agonists nor antagonists of this peptide have found clinical application. Which of the following is a peptide that causes increased capillary permeability and edema In a laboratory study of several peptides, one is found that decreases peripheral resistance but constricts veins. Which of the following endogenous molecules is elevated in heart failure and when given as a drug is a vasodilator with significant renal toxicity A 50-year-old factory worker presents with cardio-respiratory symptoms and careful workup reveals idiopathic pulmonary hypertension. Which of the following binds endothelin receptors and is approved for use in pulmonary hypertension A 60-year-old financial consultant presents with severe pain in a neuronal dermatome region of her chest. In a phase 2 clinical trial in hypertensive patients, an endogenous octapeptide vasoconstrictor was found to increase in the blood of patients treated with large doses of diuretics. Which of the following is a vasodilator that increases in the blood or tissues of patients treated with captopril Capsaicin, the "hot" constituent of hot peppers, is the molecule responsible for release of substance P. Substance P is an important pain-mediating neurotransmitter peptide and appears to be involved in post-herpetic pain as well as arthritic pain. Capsaicin can be used topically to deplete substance P stores from sensory nerves. Aprepitant and ondansetron are both used to reduce or prevent chemotherapy-induced nausea and vomiting. The cough is believed to result from prostaglandins synthesized as a result of increased bradykinin. However, both groups of drugs interfere with renal development in the fetus and are contraindicated in pregnancy. Histamine and bradykinin both cause a marked increase in capillary permeability that is often associated with edema, but histamine is not a peptide. The commercial formulation (nesiritide) is approved for use in severe acute heart failure but has significant renal toxicity. Prostaglandins & Other Eicosanoids the eicosanoids are an important group of endogenous fatty acid autacoids that are synthesized from arachidonic acid, a 20-carbon fatty acid lipid in cell membranes. Classification the principal eicosanoid subgroups are the leukotrienes and a group of cyclic molecules, including prostaglandins, prostacyclin, and thromboxane. The leukotrienes retain the straight-chain configuration of the parent arachidonic acid. Prostacyclin, thromboxane, and other members of the prostaglandin group are cyclized derivatives of arachidonic acid. There are several series for most of the principal subgroups, based on different substituents (indicated by letters A, B, etc) and different numbers of double bonds (indicated by a subscript number) in the molecule. Synthesis Active eicosanoids are synthesized in response to a wide variety of stimuli (eg, physical injury, immune reactions).
Cheap calcitriol line
The effects of blockers and calcium channel blockers on heart size symptoms for pneumonia order 0.25 mcg calcitriol with visa, force, and rate are the same. These observations have been explained as follows: Rapid-acting vasodilators-such as nifedipine in its prompt-release formulation-cause significant and sudden reduction in blood pressure. If coronary blood flow does not increase sufficiently to match the increased requirement, ischemia and infarction can result. Contrast the therapeutic and adverse effects of nitrates, blockers, and calcium channel blockers when used for angina. Explain why the combination of a nitrate with a blocker or a calcium channel blocker may be more effective than either alone. The drugs used in heart failure fall into 3 major groups with varying targets and actions. The fundamental physiologic defect in heart failure is a decrease in cardiac output relative to the needs of the body, and the major manifestations are dyspnea and fatigue. In some cases, it can be ascribed to simple loss of functional myocardium, as in myocardial infarction. It is frequently associated with chronic hypertension, valvular disease, coronary artery disease, and a variety of cardiomyopathies. The remaining cases can be attributed to a combination of systolic and diastolic dysfunction. The natural history of heart failure is characterized by a slow deterioration of cardiac function, punctuated by episodes of acute cardiac decompensation that are often associated with pulmonary or peripheral edema or both (congestive heart failure). Changes in the ventricular function curve reflect some compensatory responses of the body and demonstrate some of the responses to drugs. The homeostatic responses to depressed cardiac output are extremely important and are mediated mainly by the sympathetic nervous system and the renin-angiotensin-aldosterone system. The abscissa can be any measure of preload: fiber length, filling pressure, pulmonary capillary wedge pressure, etc. The ordinate is a measure of useful external cardiac work: stroke volume, cardiac output, etc. In heart failure, output is reduced at all fiber lengths, and the heart expands because ejection fraction is decreased or filling pressure is increased (or both). Compensatory sympathetic discharge or effective treatment allows the heart to eject more blood, and the heart moves to point C on the middle curve. Dashed arrows indicate interactions between the sympathetic and the renin-angiotensin systems. Apoptosis is a later response, and results in a reduction in the number of functioning myocytes. However, because they are not discussed elsewhere in this book, we begin our discussion with this group. Prototypes and Pharmacokinetics All cardiac glycosides are cardenolides (they include a steroid nucleus and a lactone ring); most also have one or more sugar residues, justifying the glycoside designation. The cardiac glycosides are often called "digitalis" because several come from the digitalis (foxglove) plant. Digoxin is the prototype agent and the only one commonly used in the United States. Digitoxin is a very similar but longer-acting molecule; it also comes from the foxglove plant but is no longer available in the United States. Considerable evidence indicates that angiotensin antagonists, certain -adrenoceptor blockers, and the aldosterone antagonists spironolactone and eplerenone also have long-term beneficial effects. The increased intracellular calcium is stored in the sarcoplasmic reticulum and upon release increases contractile force. Digitalis also modifies autonomic outflow, and this action has effects on the electrical properties of the heart. Calcium released from the sarcoplasmic reticulum provides the "activator" calcium that initiates actinmyosin interaction. These beneficial effects permit a decrease in the compensatory sympathetic and renal responses previously described. Electrical effects-Electrical effects include early cardiac parasympathomimetic responses and later arrhythmogenic actions. Toxic responses-Increased automaticity, caused by intracellular calcium overload, is the most important manifestation of digitalis toxicity. Intracellular calcium overload results in delayed afterdepolarizations, which may evoke extrasystoles, tachycardia, or fibrillation in any part of the heart. Congestive heart failure-Digitalis is the traditional positive inotropic agent used in the treatment of chronic heart failure. However, careful clinical studies indicate that while digitalis may improve functional status (reducing symptoms), it does not prolong life. Because the half-lives of cardiac glycosides are long, the drugs accumulate significantly in the body, and dosing regimens must be carefully designed and monitored. The parasympathomimetic action of digitalis often accomplishes this therapeutic objective, although high doses may be required. Alternative drugs for rate control include blockers and calcium channel blockers, but these drugs have negative inotropic effects. Interactions Quinidine causes a well-documented reduction in digoxin clearance and can increase the serum digoxin level if digoxin dosage is not adjusted. Several other drugs have the same effect (amiodarone, verapamil, others), but the interactions with these drugs are not clinically significant. Digitalis toxicity, especially arrhythmogenesis, is increased by hypokalemia, hypomagnesemia, and hypercalcemia. Loop diuretics and thiazides may significantly reduce serum potassium and thus precipitate digitalis toxicity. Digitalis-induced vomiting may deplete serum magnesium and similarly facilitate toxicity. Digitalis Toxicity the major signs of digitalis toxicity are arrhythmias, nausea, vomiting, and diarrhea. Rarely, confusion or hallucinations and visual or endocrine aberrations may occur. Chronic intoxication is an extension of the therapeutic effect of the drug and is caused by excessive calcium accumulation in cardiac cells (calcium overload). Severe, acute intoxication caused by suicidal or accidental extreme overdose results in cardiac depression leading to cardiac arrest rather than tachycardia or fibrillation. The normal clearance of digoxin is 7 L/h/70 kg; volume of distribution is 500 L/70 kg; and bioavailability is 70%. Diuretics Diuretics are the first-line therapy for both systolic and diastolic failure and are used in heart failure before digitalis and other drugs are considered. Furosemide is a very useful agent for immediate reduction of the pulmonary congestion and severe edema associated with acute heart failure and for moderate or severe chronic failure. Thiazides such as hydrochlorothiazide are sometimes sufficient for mild chronic failure. Clinical studies suggest that, unlike other diuretics, spironolactone and eplerenone (aldosterone antagonist diuretics) have significant long-term benefits and can reduce mortality in chronic failure. They have recently been approved for use in type 2 diabetes and have been shown to reduce the risk of cardiovascular death as well as hospitalizations for heart failure in type 2 diabetics. Angiotensin Antagonists these agents have been shown to reduce morbidity and mortality in chronic heart failure. Although they have no direct positive inotropic action, angiotensin antagonists reduce aldosterone secretion, salt and water retention, and vascular resistance (see Chapter 11). They are now considered, along with diuretics, to be first-line drugs for chronic heart failure. Beta1-Adrenoceptor Agonists Dobutamine and dopamine are often useful in acute failure in which systolic function is markedly depressed (see Chapter 9). However, they are not appropriate for chronic failure because of tolerance, lack of oral efficacy, and significant arrhythmogenic effects.
Safe 0.25 mcg calcitriol
Outcome Definition and Assessment Re-examinations of sick children included assessment of cough symptoms norovirus generic 0.25mcg calcitriol, respiratory rate (if cough was reported), anaemia, temperature and responsiveness. These guidelines are in accordance with the Malawi national guidelines in place at the time of the survey. Given the information available from the re-examination, we defined pneumonia cases as children with cough and fast breathing on re-examination. Providers were asked the diagnosis they assigned following each patient visit as part of the direct clinical observation; results are thus not subject to potentially poor data quality of medical records. Due to limited information from the re-examination, including no indication of stridor, we could not definitively identify children who did not meet the case definition of pneumonia; we thus did not assess specificity of diagnosis. Covariates We identified multiple levels influencing sensitivity of pneumonia diagnosis: contextual factors such as poverty, facility characteristics, provider characteristics and child/visit characteristics. Facility characteristics were defined as infrastructural and environmental factors that might be associated with diagnosis, such as location, facility management, facility type and structural quality, and provider factors such as professional level and technical quality score. Child characteristics considered included child age (infant or not), sex and case severity, where severe case was defined as fever (temperature 37. Among children who met the case definition for pneumonia but did not receive a pneumonia diagnosis, we assessed the proportion who received common alternative diagnoses. We calculated level of sensitivity across the binary and categorical covariates and tested significance of any differences using F tests corrected for the design effect Distribution and Determinants of Pneumonia Diagnosis Using. We then compared average structural and technical quality between children who were correctly and incorrectly diagnosed, determining significance using F tests again clustered by facility. We constructed multivariable models to test the association of the key covariates at each of the levels defined above with sensitivity, controlling for confounding by higher-level factors. Model 1 tested broad facility factors: location (urban or not), management type and facility type; we consolidated facility types into hospitals and non-hospitals following the tiers of the health system in Malawi. Model 3 and Model 4 incorporated provider capacity, including provider cadre and the technical quality of the care received, respectively. We identified child characteristics as factors that might be associated with pneumonia diagnosis, but that should not affect facility or visit characteristics; we tested each for inclusion as a control variable in unadjusted models with sensitivity using a criterion of P <0. We conducted a similar analysis to select contextual factors such as poverty and urban versus rural location due to the small sample size, controlling only for those related to the outcome at P <0. To test whether technical quality was differentially associated with sensitivity in better-equipped facilities, we assessed the association between technical quality and sensitivity of diagnosis only for children who received care in facilities with above-average structural quality for child care. All other analyses, which pertain to the subsample of children with pneumonia symptoms, are unweighted. Other symptoms include diarrhoea, vomit, feeding problem, convulsions, sleeping problem and other. The Harvard University Human Research Protection Program deemed this analysis exempt from human subjects review (protocol no. In total, care was observed for 3248 children under 5 years of age; 112 of these were children under 2 months who were excluded from analysis. Table 1 describes characteristics of facilities providing sick-child care and children receiving care. Children in the sample were 51% male and 49% female, with 64% from 12 to 59 months of age. Children most frequently received care from advanced practice clinicians or paramedical professionals, such as assistant medical officers or clinical officers, in public facilities in rural areas. The majority of sick-child visits (61%) occurred at non-hospitals, such as health centres or clinics, in areas where the proportion Distribution and Determinants of Pneumonia Diagnosis Using. Considerable gaps were evident in structural capacity to provide care: facilities scored an average of just under two-thirds on both general service readiness and childspecific service readiness. Only 118 children (21%) of these children were correctly diagnosed with pneumonia (table 2). Sensitivity was lower in children 12 months to 59 months old, with 78 of 428 (18% sensitivity) diagnosed with pneumonia compared with 40 of 145 cases (28% sensitivity) in children under one. Healthcare workers were more likely to assign the correct diagnosis when children presented with fever, high respiration or both as well as cough: sensitivity among these children (n=206) was 28%. Although prevalence of confirmed fever was equal across age groups, caretakers of children over one were more likely to report fever as a cause for the visit (76. All children 2 months through 59 months Clinician Dx+ 118 241 359 Clinician Dx- 455 2322 2777 573 2563 3136 418 Infectious Diseases: An Evidence based Approach Sensitivity 20. Children 12 months through 59 months Clinician Dx+ 78 122 Clinician Dx- 350 1526 428 1648 Sensitivity 18. Children 2 months through 11 months Clinician Dx+ 40 119 Clinician Dx- 105 796 145 915 Sensitivity 27. Among client demographics and facility characteristics, sensitivity of diagnosis was significantly higher for children <12 months of age, those with fever and/or high respiration, and those seen by clinicians as compared with nurses and other providers. Children seen in dispensaries were less likely to be correctly diagnosed than those seen in hospitals, health centres and clinics; the difference did not reach statistical significance. Analysis of case severity using presence of fever and/or high respiration did not identify differences in the case mix presenting by facility type or clinician qualification (see online supplementary table A1). Average technical quality was significantly higher for children receiving a correct diagnosis of pneumonia (0. Fever and/or tachypnoea confirmed by re-examination Severe case: child has fever and/or tachypnoea Less severe case: child has neither fever nor tachypnoea 28% 16% 0. Child age above and below 1 year, case severity and urban versus rural location met our screening criterion but child sex and poverty did not; we thus controlled for age, severity and location in all models. As shown in column 2 of table 4, probability of correct diagnosis among children with pneumonia symptoms was higher in rural areas and privately managed facilities, but not significantly so. Sensitivity did not vary significantly by general and child-specific structural quality (model 2). In model 3, clinicians were twice as likely to provide the correct diagnosis to children with pneumonia symptoms as nurses and other providers (adjusted relative risk 2. Clinician includes clinical officers, assistant medical officers and medical officers; other includes counsellors and social workers. Service readiness is an index from 0 to 1 comprising basic amenities, equipment, infection prevention, diagnostics and medications. Child service readiness is an index from 0 to 1 comprising staff and training, guidelines, and child-specific equipment and medication. Consistent with prior studies in low-income and middle-income countries, Distribution and Determinants of Pneumonia Diagnosis Using. Missed diagnoses were common irrespective of surrounding poverty level, urban versus rural location and facility type. Providers under-diagnosed pneumonia at both well-equipped and poorly equipped facilities. This evidence suggests a critical quality gap in formal healthcare services in Malawi, one that contributes to excess morbidity and avertable child deaths. Patient factors, such as child age and presenting with fever and/or tachypnoea, were associated with correct diagnosis in bivariable analysis. This is consistent with previous research19 36 and may suggest a lower threshold for diagnosing pneumonia in infants, who experience higher pneumonia incidence and mortality. Healthcare providers may be predisposed to look for pneumonia in infants and malaria in older children; given the incompleteness of physical examinations conducted (five of six children did not have respiratory rate assessed), caretaker report and expected prevalence of disease may form much of the basis for diagnosis. Higher sensitivity among children with fever or tachypnoea suggests providers are responsive to case severity, though three of four children with indications of severe illness were not diagnosed with pneumonia. While few factors were associated with correct diagnosis of pneumonia, provider cadre was a significant determinant, with nurses and other providers demonstrating lower sensitivity compared with clinicians (eg, clinical officers, physicians). Due to massive shortages of physicians in sub-Saharan Africa, nurses compose the majority of providers available for sick-child care at first-level health facilities accessible to rural communities, families in extreme poverty and individuals with limited transport. These findings call into question the effectiveness of non-clinician healthcare workers in appropriately identifying pneumonia cases. Still, even with increased physician or advanced practice clinician presence, sensitivity of pneumonia diagnosis among these providers remains extremely low. As the first nationally representative study on accuracy of pneumonia diagnosis in a low-income country, these results reinforce existing signals of a quality crisis. While reinforcing the need for quality improvement, this study demonstrates mixed results for common strategies. However, the low baseline adherence raises the question of whether and how provider performance can be increased enough to meaningfully improve diagnostic accuracy. The two most prominent interventions-in-service training and supportive supervision-showed only a modest impact on provider adherence to guidelines.
Buy generic calcitriol 0.25mcg online
Methylase production and methylation of the receptor site are established mechanisms of resistance of Gram-positive organisms to macrolide antibiotics treatment quotes cheap calcitriol 0.25 mcg without a prescription. Such enzymes may be inducible by macrolides or constitutive; in the latter case, cross-resistance occurs between macrolides and clindamycin. Such infections may develop slowly because of the long incubation period of chlamydial infection. Treatment with oral doxycycline for 14 d (as originally prescribed) would have eradicated C trachomatis and most other organisms commonly associated with nongonococcal cervicitis or urethritis. Given the limited compliance of this patient, the best course of action would be the administration (in the clinic) of a single oral dose of azithromycin. This patient is in the high-risk category for bacterial endocarditis and should receive prophylactic antibiotics before many dental procedures. The American Heart Association recommends that clindamycin be used in patients allergic to penicillins. Oral erythromycin is not recommended because it is no more effective than clindamycin and causes more gastrointestinal adverse effects. Intravenous vancomycin (not oral), sometimes with gentamicin, is recommended for prophylaxis in high-risk penicillin-allergic patients undergoing genitourinary and lower gastrointestinal surgical procedures. More than 80% of cases are caused by typical pathogens such as S pneumoniae, H influenzae, or M catarrhalis, and 15% are due to the nonzoonotic atypical pathogens such as Legionella species, Mycoplasma species, or C pneumoniae. Preferred initial therapy includes a macrolide, doxycycline, or a quinolone active against respiratory pathogens (Chapter 46). The inhibition of liver cytochrome P450 by erythromycin has led to serious drug interactions. Unlike the tetracyclines, the oral absorption of erythromycin is not affected by cations and the drug does not cause photosensitivity. Because erythromycin undergoes biliary excretion, there is little reason to assess renal function before treatment. Azithromycin has a half-life of more than 70 h, which allows for once-daily dosing and a 5-d course of treatment for community-acquired pneumonia. Unlike other macrolides, azithromycin does not inhibit cytochrome P450 enzymes involved in drug metabolism. Name the most important agents in each drug class, and list 3 clinical uses of each. However, the in vivo effectiveness of some antibiotics, including aminoglycosides, results from a concentrationdependent killing action. Aminoglycosides are also capable of exerting a postantibiotic effect such that their killing action continues when their plasma levels have declined below measurable levels. Consequently, aminoglycosides have greater efficacy when administered as a single large dose than when given as multiple smaller doses. The toxicity (in contrast to the antibacterial efficacy) of aminoglycosides depends both on a critical plasma concentration and on the time that such a level is exceeded. The time above such a threshold is shorter with administration of a single large dose of an aminoglycoside than when multiple smaller doses are given. These concepts form the basis for once-daily aminoglycoside dosing protocols, which can be more effective and less toxic than traditional dosing regimens. With once-daily dosing, peak levels are less important since they will naturally be high. Their penetration through the bacterial cell envelope requires oxygen-dependent active transport, and they have minimal activity against strict anaerobes. Aminoglycoside entry can be enhanced by cell wall synthesis inhibitors, which may be the basis of antimicrobial synergism. Aminoglycosides may also disrupt polysomal structure, resulting in nonfunctional monosomes. However, the primary mechanism of resistance to aminoglycosides, especially in Gram-negative bacteria, involves the plasmidmediated formation of inactivating enzymes. These enzymes are group transferases that catalyze the acetylation of amine functions and the transfer of phosphoryl or adenylyl groups to the oxygen atoms of hydroxyl groups on the aminoglycoside. For example, transferases produced by enterococci can inactivate amikacin, gentamicin, and tobramycin but not streptomycin. However, amikacin is often resistant to many enzymes that inactivate gentamicin and tobramycin. In addition, resistance to streptomycin, which is common, appears to be due to changes in the ribosomal binding site. They are polar compounds, not absorbed after oral administration, and must be given intramuscularly or intravenously for systemic effect. They have limited tissue penetration and do not readily cross the blood-brain barrier. Glomerular filtration is the major mode of excretion, and plasma levels of these drugs are greatly affected by changes in renal function. Dosage adjustments must be made in renal insufficiency to prevent toxic accumulation. Gentamicin, tobramycin, and amikacin are important drugs for the treatment of serious infections caused by aerobic Gram-negative bacteria, including Escherichia coli and Enterobacter, Klebsiella, Proteus, Providencia, Pseudomonas, and Serratia species. These aminoglycosides also have activity against strains of Haemophilus influenzae, Moraxella catarrhalis, and Shigella species, although they are not drugs of choice for infections caused by these organisms. In most cases, aminoglycosides are used in combination with a beta-lactam antibiotic. When used alone, aminoglycosides are not reliably effective in the treatment of infections caused by Gram-positive cocci. Antibacterial synergy may occur when aminoglycosides are used in combination with cell wall synthesis inhibitors. Examples include their combined use with penicillins in the treatment of pseudomonal, listerial, and enterococcal infections. Streptomycin in combination with penicillins is often more effective in enterococcal carditis than regimens that include other aminoglycosides. This combination is also used in the treatment of tuberculosis, plague, and tularemia. Multidrug-resistant strains of Mycobacterium tuberculosis that are resistant to streptomycin may be susceptible to amikacin. Because of the risk of ototoxicity, streptomycin should not be used when other drugs will serve. Owing to their toxic potential, neomycin and kanamycin are usually restricted to topical or oral use (eg, to eliminate bowel flora). Netilmicin has been used for treatment of serious infections caused by organisms resistant to the other aminoglycosides. Its sole use is as a backup drug, administered intramuscularly as a single dose for the treatment of gonorrhea, most commonly in patients allergic to beta-lactams. Ototoxicity Auditory or vestibular damage (or both) may occur with any aminoglycoside and may be irreversible. Auditory impairment is more likely with amikacin and kanamycin; vestibular dysfunction is more likely with gentamicin and tobramycin. Ototoxicity risk is proportional to the plasma levels and thus is especially high if dosage is not appropriately modified in a patient with renal dysfunction. Because ototoxicity has been reported after fetal exposure, the aminoglycosides are contraindicated in pregnancy unless their potential benefits are judged to outweigh risk. This adverse effect, which is often reversible, is more common in elderly patients and in those concurrently receiving amphotericin B, cephalosporins, or vancomycin. Neuromuscular Blockade Though rare, a curare-like block may occur at high doses of aminoglycosides and may result in respiratory paralysis. It is usually reversible by treatment with calcium and neostigmine, but ventilatory support may be required. Skin Reactions Allergic skin reactions may occur in patients, and contact dermatitis may occur in personnel handling the drug. Which of the following statements about the clinical uses of the aminoglycosides is accurate Which statement is accurate regarding the antibacterial action of the aminoglycoside amikacin
Syndromes
- Myotonic dystrophy
- Torsion of the testis
- Difficulty eating and swallowing
- Check how well your liver is working
- Neuroblastoma
- Shortness of breath
Purchase discount calcitriol online
How drugs can cause side-effects 3: auto-immune reactions Some drugs produce certain side-effects only in genetically susceptible individuals medicine uses order calcitriol 0.25 mcg with visa. Many of these drugs induce an immune reaction that instead of defending the body, attacks it. The mechanisms whereby these auto-immune responses cause damage are complex and many are not fully understood so we will just list them here in Table 3. This explains some of the common side-effects such as dry mouth, hair loss, gastro-intestinal disturbance and neutropaenia (low levels of circulating neutrophils). In addition to interfering with normal cell division, many of the anti-cancer drugs are intrinsically toxic and need careful monitoring as they can cause damage to the heart, nervous tissue, lungs and kidneys. Nausea and vomiting are frequent side-effects of anti-cancer treatment and are very distressing to patients. Some drugs, such as cisplatin and cyclophosphamide, are notorious for this problem. Cancer is a very serious, life-threatening disease and some of the drugs used to treat it have a fairly brutal mechanism of action on the body, so it is not surprising that their side-effects are among the most unpleasant of all drug groups. However, as they can be life-saving or at least life-prolonging, their benefit generally outweighs the disagreeable side-effects they may cause. Epithelial cells are those that line the parts of the body exposed to the external environment, including the skin, lungs and digestive tract. Lining cells inside the body such as those that line blood vessels are called endothelial cells. Patients may be suffering from diabetes, rheumatic pains, hypertension, fluid retention and digestive problems so inevitably different drugs will be prescribed for each of these disorders. Multiple prescribing, or polypharmacy as it is sometimes called, can result in some drugs interacting with other drugs and this can cause additional side-effects for the patient. Drug interactions are not rare and a glance at Appendix 1 of the current British National Formulary will show the extent of the problem, with around 150 pages listing how one drug can interact with another. Interactions between drugs will either increase or decrease the activity of one of those drugs. However, to be worthy of interest, an interaction must be of clinical significance. For example, drug A may marginally decrease the activity of drug B but if this does not produce any measurable change in the therapeutic effectiveness of drug B or change its side-effects profile then the interaction is of little or no clinical relevance. Those drugs where a small change in concentration can have severe consequences are more likely to have serious interactions. These drugs include some of the anticoagulants (anticlotting drugs) and antiarrhythmics (drugs to restore normal heart rhythm). This is especially a problem for the elderly who often have multiple problems, each requiring its own range of drugs. Interactions involving hepatic P450 enzymes Cytochrome P450 enzymes in the liver specialise in metabolising unwanted substances, making them more soluble and easier for the kidneys to excrete. The liver can detect an increase in these unwanted substances in the blood and responds by increasing the production of P450 enzymes specific to that substance. The unwanted substances are metabolised more quickly, hastening their elimination from the body. Some drugs can induce P450 protein synthesis, causing an increase in enzyme activity that results in substrates for those enzymes (including drugs) being metabolised more quickly. When a particular P450 enzyme is inhibited, drugs that are substrates for that enzyme are metabolised more slowly. As a general rule, inducers have a more general action as they tend to induce a wide range of P450 enzymes. Induction is also generally a slower process than inhibition, often taking several days for its effects to become evident. As an example, the antibacterial rifampicin can induce P-gp efflux pumps in the wall of the gut. Drugs that are substrates for these pumps are returned more quickly to the lumen of the gut for faecal elimination. This reduces the rate of absorption of drugs such as digoxin which lowers its bioavailability. For example, the antibacterial erythromycin can inhibit P-gp efflux pumps in the wall of the gut. This reduces the rate at which drugs are returned to the lumen of the gut so absorption of drugs such as digoxin is enhanced which increases its bioavailability. The antiarrhythmic verapamil is another potent P-gp inhibitor affecting many drugs, including the immunosuppressant, sirolimus. Other mechanisms of drug interactions There are many other mechanisms whereby drugs interact. The anticoagulant drug warfarin is susceptible to interactions with both antibiotics and common foods. Warfarin competes with vitamin K for the active site of vitamin K reductase, an enzyme that produces reduced vitamin K, a cofactor in the production of various circulating coagulation proteins. Normally, these friendly bacteria produce vitamin K so, if levels of this vitamin fall due to rifampicin, the effectiveness of warfarin is enhanced. Conversely, a rise in vitamin K levels has the opposite effect, decreasing the effectiveness of warfarin and promoting coagulation. In fact phytomenadione (vitamin K) is used to counteract the effects of excess warfarin. This also explains why patients on warfarin are warned against suddenly consuming large amounts of vitamin K-rich leafy green vegetables such as cabbage, broccoli and kale. Drugs with a similar therapeutic activity can cause problems if administered together. This is called additive or summative action and an example would be the co-administration of the anticoagulants warfarin and aspirin. Although their mechanisms of action are different, when given together they can result in an increased risk of haemorrhage and can be especially problematical if the patient develops a peptic ulcer, which can cause bleeding into the stomach. Another herbal remedy worth mentioning here is the maidenhair tree, Ginkgo biloba, which is reputed to improve cerebral circulation. As the ginkgolides contained in its leaves have an anticoagulant action, it would be inadvisable to use this herb with either aspirin or warfarin because of the potential additive effect causing unwanted bleeding. Drugs that have a similar effect can produce an additive effect if taken together. Herbal remedies and even common foodstuffs, such as grapefruit juice and cabbage, can interact with drugs. Ideally, where treatment is to last several days or weeks, the rate of administration should match the rate of elimination so that the amount of drug in the body remains fairly constant. Water is coming in via the taps (drug administration) and water is leaving via the plughole (drug elimination). The only way to keep the level constant is to ensure that water is going in at the same rate as it is leaving the bath. Administration, on the other hand, tends to be periodic, either by regular injections or by ingestion. The therapeutic index Once the rate of elimination has been determined, it is possible to calculate the dose required to reach therapeutic levels. This level of drug in the body is important because if levels are too low, the drug will be ineffective and if levels are too high, the drug may produce toxic effects. This is the minimum amount of drug that will produce the desired therapeutic effect. This is the maximum amount of drug that can be tolerated before it starts to produce toxic effects. Correct drug administration should ensure that the level of circulating drug is maintained between these two values for the period determined to be required for the course of treatment. After each dose, levels rise and then fall as the drug is metabolised and eliminated from the body. In real life, it is not possible to determine absolute values because drugs behave differently in each individual which is why, on the graph, the blue therapeutic-zone is depicted as having blurred edges. Achieving the therapeutic dose generally, the aim of drug administration is to reach a steady plasma concentration within the therapeutic window.

Buy cheap calcitriol
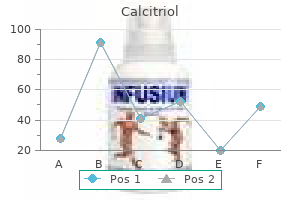
Although initial responses to monotherapy usually are good medicine in the civil war effective calcitriol 0.25 mcg, secondary failure within 5 years is common. Increasingly, noninsulin antidiabetic agents are being used in combination with each other or with insulin to achieve better glycemic control and minimize toxicity. Long-acting drugs (sulfonylureas, metformin, thiazolidinediones, exenatide, sitagliptin, some insulin formulations) help control both fasting and postprandial blood glucose levels, whereas short-acting drugs (-glucosidase inhibitors, repaglinide, pramlintide, rapid-acting insulins) primarily target postprandial levels. As is the case for type 1 diabetes, clinical trials have shown that tight control of blood glucose in patients with type 2 diabetes reduces the risk of vascular complications. Obesity predisposes patients to hypertension as well as to type 2 diabetes, so many patients suffer from both diseases. Both diseases damage the kidney and predispose patients to coronary artery disease. A large clinical trial of patients with type 2 diabetes suggests that poorly controlled hypertension exacerbates the microvascular disease caused by long-standing diabetes. Because of these links, it is important to consider the treatment of hypertension in diabetic patients. Identify the major drug groups used for chronic treatment of essential hypertension. Which of these drug groups have special implications for the treatment of patients with diabetes Chemistry, mechanism, and effects-Glucagon is a protein hormone secreted by the A cells of the endocrine pancreas. Acting through G protein-coupled receptors in the heart, smooth muscle, and liver, glucagon increases heart rate and force of contraction, increases hepatic glycogenolysis and gluconeogenesis, and relaxes smooth muscle. Clinical uses-Glucagon is used to treat severe hypoglycemia in diabetics, but its hyperglycemic action requires intact hepatic glycogen stores. In this patient, metformin should either be avoided or used with extreme caution because the combination of metformin and ethanol increases the risk of which of the following Which of the following drugs is taken during the first part of a meal for the purpose of delaying the absorption of dietary carbohydrates Which of the following drugs is most likely to cause hypoglycemia when used as monotherapy in the treatment of type 2 diabetes A 13-year-old boy with type 1 diabetes is brought to the hospital complaining of dizziness. Laboratory findings include severe hyperglycemia, ketoacidosis, and a blood pH of 7. Which of the following agents should be administered to achieve rapid control of the severe ketoacidosis in this diabetic boy Which of the following is the most likely complication of insulin therapy in this patient A 24-year-old woman with type 1 diabetes wishes to try tight control of her diabetes to improve her long-term prognosis. Which of the following patients is most likely to be treated with intravenous glucagon Because of the risk of brain damage, the most important complication of insulin therapy is hypoglycemia. Insulin regimens for tight control usually take the form of establishing a basal level of insulin with a small amount of a long-acting preparation (eg, insulin glargine) and supplementing the insulin levels, when called for by food intake, with short-acting insulin lispro. Less tight control may be achieved with 2 injections of intermediate-acting insulin per day. Because intake of glucose is mainly during the day, longacting insulins are usually given in the morning, not at night. Glipizide is a second-generation sulfonylurea that promotes insulin release by closing potassium channels in pancreatic B cells. Insulin lowers serum glucose concentration in part by driving glucose into cells, particularly into muscle cells. Biguanides, especially the older drug phenformin, have been associated with lactic acidosis. Thus, metformin should be avoided or used with extreme caution in patients with conditions that increase the risk of lactic acidosis, including acute ethanol ingestion. To be absorbed, carbohydrates must be converted into monosaccharides by the action of -glucosidase enzymes in the gastrointestinal tract. Acarbose inhibits -glucosidase and, when present during digestion, delays the uptake of carbohydrates. When activated, these receptors translocate to the nucleus, where they regulate the transcription of genes encoding proteins involved in the metabolism of carbohydrate and lipids. The insulin secretagogues, including the sulfonylurea glyburide, can cause hypoglycemia as a result of their ability to increase serum insulin levels. The biguanides, thiazolidinediones, -glucosidase inhibitors, and canagliflozin are euglycemics that are unlikely to cause hypoglycemia when used alone. Glucagon acts through cardiac glucagon receptors to stimulate the rate and force of contraction of the heart. Because this bypasses cardiac adrenoceptors, glucagon is useful in the treatment of -blocker-induced cardiac depression. Angiotensin receptor antagonists may have similar protective effects in patients with diabetes. Beta-adrenoceptor blockers can, in theory, mask the symptoms of hypoglycemia in diabetic patients; however, many patients with diabetes and cardiovascular disease are successfully treated with these drugs. A large clinical trial showed that control of hypertension decreases diabetes-associated microvascular disease. Thiazide diuretics impair the release of insulin and tissue utilization of glucose, so they should be used with caution in patients with diabetes. List the prototypes and describe the mechanisms of action, key pharmacokinetic features, and toxicities of the major classes of agents used to treat type 2 diabetes. Give 3 examples of rational drug combinations for treatment of type 2 diabetes mellitus. Agents That Affect Bone Mineral Homeostasis Calcium and phosphorus, the 2 major elements of bone, are crucial not only for the mechanical strength of the skeleton but also for the normal function of many other cells in the body. Secondary disease most commonly results from chronic kidney disease Bone cell that promotes bone formation Bone cell that promotes bone resorption A condition of abnormal mineralization of adult bone secondary to nutritional deficiency of vitamin D or inherited defects in the formation or action of active vitamin D metabolites Abnormal loss of bone with increased risk of fractures, spinal deformities, and loss of stature; remaining bone is histologically normal A bone disorder, of unknown origin, characterized by excessive bone destruction and disorganized repair. In animals with vitamin D deficiency, active metabolites of vitamin D produce a net increase in bone mineralization by increasing the availability of serum calcium and phosphate. The action of vitamin D metabolites is mediated by activation of 1 or possibly a family of nuclear receptors that regulate gene expression. Active vitamin D metabolites are required for normal mineralization of bone; deficiencies cause rickets in growing children and adolescents and osteomalacia in adults. Vitamin D, vitamin D metabolites, and synthetic derivatives are used to treat deficiency states, including nutritional deficiency, intestinal osteodystrophy, chronic kidney or liver disease, hypoparathyroidism, and nephrotic syndrome. They are also used, in combination with calcium supplementation, to prevent and treat osteoporosis in older women and men. Ergosterol undergoes similar transformation to vitamin D2 (ergocalciferol), which in turn is metabolized to 1,25-dihydroxyvitamin D2 and 24,25-dihydroxyvitamin D2. In patients with conditions that impair vitamin D activation (chronic kidney disease, liver disease, hypoparathyroidism), an active form of vitamin D such as calcitriol is required. All cause less hypercalcemia and, in patients with normal renal function, less hypercalciuria than calcitriol. Oral and parenteral doxercalciferol and oral paricalcitol are approved for treatment of secondary hyperparathyroidism in patients with chronic kidney disease. These and other analogs are being investigated for use in various malignancies and inflammatory disorders. The primary toxicity caused by chronic overdose with vitamin D or its active metabolites is hypercalcemia, hyperphosphatemia, and hypercalciuria. Bone formation is not impaired initially, but ultimately both formation and resorption are reduced. Calcitonin is approved for treatment of osteoporosis and has been shown to increase bone mass and to reduce spine fractures.
Generic calcitriol 0.25mcg fast delivery
In this case medicine used for adhd order calcitriol with paypal, we can surmise that this unintentional interaction will result in specific side-effects. These side-effects may be common or rare but the practitioner will be aware that there is the possibility that the patient may experience them. Type B side-effects are an unpredictable individual response to a particular drug when administered at the correct therapeutic dose. The patient has an adverse reaction to a drug, probably caused by an immune response to the drug specific to that individual. This is a common phenomenon but precisely why it happens is not always easy to determine. There are also differences within the body, in particular the way that our bodies deal with drugs. Most of these differences manifest themselves at a cellular level, which is where drugs interact with the body. The way that our bodies absorb, metabolise and eliminate drugs also varies between individuals, perhaps because of age or disease, and this can result in variations in the amount of drug circulating in the blood. Some drugs regularly cause minor inconveniences such as nausea or constipation but rarely cause any serious problems. Other drugs quite regularly cause unpleasant side-effects and need monitoring carefully. The message is that every drug is different and it will behave differently in each individual patient. This is not, of course, to imply that there is a complete lack of predictability with the drugs that we administer but, because of individual differences, there will inevitably be some variation between patients both with regard to their therapeutic response and their susceptibility to side-effects. The most common side-effects include abdominal pain, dyspepsia, nausea, headache, constipation and diarrhoea. The mechanism whereby drugs cause these problems is often not well understood but we should not be surprised that the introduction of a foreign compound into the body causes disturbance in its normal functioning. How drugs can cause side-effects 1: tipping the balance too far Individuals react differently to drugs and their response can vary with factors such as age, disease and simply the normal genetic variability between people. Manufacturers are aware of this and during the testing process they decide the appropriate dosage that will provide the optimum therapeutic effect with the minimum of side-effects. Sometimes, however, variability in response to a drug means that the drug delivers a more pronounced therapeutic effect than originally intended. Now you might think that this is a good thing because a patient who experiences an enhanced therapeutic effect will automatically be better off, but this is not always the case. If the house is too cold you turn up the thermostat, but if you turn it up too far, an hour later you are sweating. This is like a drug that has a greater effect than intended and tips the balance the other way. The anticlotting drugs warfarin and heparin need to be used carefully or they can tip the balance of blood coagulation too far in the other direction and cause haemorrhage (unwanted bleeding). Stimulant laxatives such as senna can prove to be too effective and cause diarrhoea. Codeine phosphate used for acute diarrhoea can work too well and cause constipation. Most examples of drugs tipping the balance too far are dependent on the dose; therefore we say that the effect is dose-related. The greater the dose, the more pronounced is the action of the drug and the greater is the side-effect produced. These protein targets seldom exist as solitary individuals, but are mostly members of a larger group, a family of similar proteins. Each family will have core similarities in molecular structure that define their group. This means that drugs targeting one member of the family are quite likely to bind to other members of that family because of these similarities in molecular structure. When a drug binds to these unintentional targets then unintended things happen in the form of side-effects. Within these families are classes and sub-classes of receptor but as these receptors are all related, they have key similarities in structure. While allocating specific receptors to specific tissue helps explain how drugs work, in reality a tissue may express more than one type of receptor. The heart, for example, expresses not only beta-1 adrenergic receptors but also beta-2 receptors. These form part of a complex regulatory mechanism beyond the scope of this introductory book. To further complicate matters, diseases such as chronic heart failure can change the ratio of these receptors and this affects the way that some drugs act on the heart. It can produce two different effects depending on which lock (receptor) it goes into. The key will fit into your car door lock and open the door and also fit into your ignition lock and start your engine. This specificity is what is required from drugs because we want heart drugs to target the heart, lung drugs to target the lungs and so on. Atenolol can precipitate bronchospasm and also block the action of beta-2 bronchodilators. Both actions could be serious for asthmatics and so the use of beta-blockers such as atenolol is cautioned in patients with asthma. As well as an example of a sideeffect (bronchospasm) this is also an example of a mechanism of interaction where the two drugs compete for the same receptor. It should be noted however that there is variation in selectivity within drug groups. Other beta-blockers such as carvedilol are non-cardioselective but their ability to bind to alpha adrenergic receptors on arterioles makes them useful in treating hypertension. This produces beneficial results such as lowering blood pressure, relieving inflammatory pain and reducing blood cholesterol. However, these enzymes are often members of families of enzymes and drugs can stray off target, bind to other members of the family and cause side-effects. This results in an accumulation of bradykinin, irritating the bronchioles and causing a dry cough. By interfering with various processes such as sodium balance, this reduces blood pressure. How this relieves inflammation and pain is complex and is explained in more detail in Chapter 6.
Purchase 0.25mcg calcitriol fast delivery
Opioid peptides are also found in the adrenal medulla and neural plexus of the gut symptoms 9f anxiety generic calcitriol 0.25 mcg on-line. Absorption and Distribution Most drugs in this class are well absorbed when taken orally, but morphine, hydromorphone, and oxymorphone undergo extensive first-pass metabolism. In most cases, opioids can be given parenterally, and sustained-release forms of some drugs are now available, including morphine and oxycodone. They cross the placental barrier and exert effects on the fetus that can result in both respiratory depression and, with continuous exposure, physical dependence in neonates. Metabolism With few exceptions, the opioids are metabolized by hepatic enzymes, usually to inactive glucuronide conjugates, before their elimination by the kidney. However, morphine-6-glucuronide has analgesic activity equivalent to that of morphine, and morphine-3-glucuronide (the primary metabolite) is neuroexcitatory. The ingestion of alcohol causes major increases in the peak serum levels of several opioids including hydromorphone and oxymorphone. Meperidine is metabolized to normeperidine, which may cause seizures at high plasma levels. However, long-acting formulations of some drugs may provide analgesia for 24 h or more. Remifentanil (an ester) and alfentanil, congeners of fentanyl, are metabolized rapidly and have very short half-lives (minutes to tens of minutes). On the left, sites of action on the pain transmission pathway from the periphery to the higher centers are shown. On the right, actions of opioids on pain-modulating neurons in the midbrain (D), rostral ventral medulla (E), and the locus coeruleus indirectly control pain transmission pathways by enhancing descending inhibition to the dorsal horn. Receptor Mechanisms Opioid analgesics inhibit synaptic activity partly through direct activation of opioid receptors and partly through release of the endogenous opioid peptides, which are themselves inhibitory to neurons. All 3 major opioid receptors are coupled to their effectors by G proteins and activate phospholipase C or inhibit adenylyl cyclase. At the postsynaptic level, activation of these receptors can open potassium ion channels to cause membrane hyperpolarization (inhibitory postsynaptic potentials). Analgesia the opioids are the most powerful drugs available for the relief of acute pain. Drugs with mixed agonist-antagonist actions (eg, buprenorphine, see below) may antagonize the analgesic actions of full agonists and should not be used concomitantly. Codeine, hydrocodone, and oxycodone are partial agonists with mild to moderate analgesic efficacy. Propoxyphene, a very weak agonist drug, is also available combined with acetaminophen. Sedation and Euphoria these effects may occur at doses lower than those required for maximum analgesia. At higher doses, the drugs may cause mental clouding and result in a stuporous, or even a comatose, state. Respiratory Depression Opioid actions in the medulla lead to inhibition of the respiratory center, with decreased response to carbon dioxide challenge. With full agonists, respiratory depression may be seen at conventional analgesic doses. Increased Pco2 may cause cerebrovascular dilation, resulting in increased blood flow and increased intracranial pressure. Antitussive Actions Suppression of the cough reflex by unknown mechanisms is the basis for the clinical use of opioids as antitussives. This action can be obtained with the use of doses lower than those needed for analgesia. Nausea and Vomiting Nausea and vomiting are caused by opioid activation of the chemoreceptor trigger zone and are increased by ambulation. Gastrointestinal Effects Constipation occurs through decreased intestinal peristalsis, which is probably mediated by effects on opioid receptors in the enteric nervous system. This powerful action is the basis for the clinical use of these drugs as antidiarrheal agents. Smooth Muscle Opioids (with the exception of meperidine) cause contraction of biliary tract smooth muscle, which can result in biliary colic or spasm, increased ureteral and bladder sphincter tone, but a reduction in uterine tone, which may contribute to prolongation of labor. Miosis Pupillary constriction is a characteristic effect of all opioids except meperidine, which has a muscarinic blocking action. Miscellaneous Truncal rigidity occurs in response to several opioids and can cause significant resistance to mechanical ventilation. Opioid analgesics, especially morphine, can cause flushing and pruritus through histamine release. Exaggerated responses to opioid analgesics may occur in patients with adrenal insufficiency or hypothyroidism. Tolerance Marked tolerance can develop to the just-mentioned acute pharmacologic effects, with the exception of miosis and constipation. Although there is crosstolerance between different opioid agonists, it is not complete. This provides the basis for "opioid rotation," whereby analgesia is maintained (eg, in cancer patients) by changing from one drug to another. Dependence Physical dependence is an anticipated physiologic response to chronic therapy with drugs in this group, particularly the strong agonists. Physical dependence is revealed on abrupt discontinuance as an abstinence syndrome, which includes rhinorrhea, lacrimation, chills, gooseflesh, muscle aches, diarrhea, yawning, anxiety, and hostility. A more intense state of precipitated withdrawal results when an opioid antagonist is administered to a physically dependent individual. Hyperalgesia When used for a prolonged period, some opioids, including morphine, fentanyl, and remifentanil, may exacerbate pain. Analgesia Treatment of relatively constant moderate to severe pain (eg, fractures, cancer pain, etc) is the major indication. Prolonged analgesia, with some reduction in adverse effects, can be achieved with epidural administration of certain strong agonist drugs (eg, fentanyl and morphine). Fentanyl has also been used by the transdermal route providing analgesia for up to 72 h. Cough Suppression Useful oral antitussive drugs include codeine and dextromethorphan. Large doses of dextromethorphan may cause hallucinations, confusion, excitation, increased or decreased pupil size, nystagmus, seizures, coma, and decreased ventilation. Treatment of Diarrhea Selective antidiarrheal opioids include diphenoxylate and loperamide. Management of Acute Pulmonary Edema Morphine (parenteral) may be useful in acute pulmonary edema because of its hemodynamic actions; its calming effects probably also contribute to relief of the pulmonary symptoms. Anesthesia Opioids are used as preoperative medications and as intraoperative adjunctive agents in balanced anesthesia protocols. High-dose intravenous opioids (eg, morphine, fentanyl) are often the major component of anesthesia for cardiac surgery. Opioid Dependence Methadone, one of the longer acting opioids, is used in the management of opioid withdrawal states and in maintenance programs for addicts. In withdrawal states, methadone permits a slow tapering of opioid effect that diminishes the intensity of abstinence symptoms. Buprenorphine (see later discussion) has an even longer duration of action and is sometimes used in withdrawal states. In maintenance programs, the prolonged action of methadone blocks the euphoria-inducing effects of doses of shorter acting opioids (eg, heroin, morphine). Treatment of overdose involves the use of antagonists such as naloxone and other therapeutic measures, especially ventilatory support. Concomitant use of certain opioids (eg, meperidine) with monoamine oxidase inhibitors increases the incidence of hyperpyrexic coma. Meperidine has also been implicated in the serotonin syndrome when used with selective serotonin reuptake inhibitors. Analgesic Activity the analgesic activity of mixed agonist-antagonists varies with the individual drug but is somewhat less than that of strong full agonists like morphine. Buprenorphine, butorphanol, and nalbuphine afford greater analgesia than pentazocine, which is similar to codeine in analgesic efficacy.