Discount 250 mg erythromycin with visa
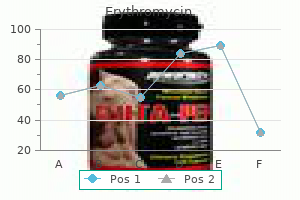
Ater the body is resected antibiotics for dogs home remedy order 250mg erythromycin with mastercard, the spinal column is shortened in such cases to obtain some bony apposition anteriorly. In severe gibbous deformities, decompression is technically more feasible from a posterior approach. For more severe curves, in which substantial correction is necessary, traditionally an anterior approach has been recommended to perform osteotomies of the unsegmented areas, discectomies and fusion, and posterior fusion and instrumentation. For relatively mild deformities, such as those from a wedge vertebra or failure of formation hemivertebra excision, a posterior column-shortening osteotomy, such as Ponte or pedicle subtraction, is suicient. During the procedure, suicient height of anterior reconstruction, avoiding the sagittal translation of the upper and lower vertebrae, keeping a temporary rod in position at all times and intraoperative neuromonitoring, may help to improve the safety. Care should also be taken to control epidural bleeding and keeping the mean arterial blood pressure equal to or above 80 mm Hg during the correction maneuver to prevent neurologic complications. Complete removal of the inferior and superior facets and ligamentum lavum allows the posterior column to be shortened. A combination of cantilever forces and compression is used to obtain correction in Scheuermann kyphosis. In a very young child with congenital deformity, fusion should be as short as possible. Although bracing and casting are not very efective in congenital deformities, alternating with casting may be considered in a very young infant as a temporizing measure to allow further growth before surgery is performed. Overcorrection of a kyphotic deformity can lead to neurologic injury because the spinal cord is lengthened. Avoiding overcorrection, selection of proper fusion levels, and preservation of the supraspinous ligament at the proximal end of the construct have been found to be helpful to prevent a junctional kyphosis. The possibility of a junctional kyphosis should be discussed with the patient and family preoperatively. Not all patients experience progression, and early surgery in the absence of documented progression should be avoided. In patients with congenital scoliosis, the lateral radiograph should be critically examined. With use of modern spinal instrumentation and proper technique, pseudarthrosis rates are low in young children even with allograt and posterior-only fusion. Neurologic Complications he rate of neurologic complications is higher in the surgical treatment of congenital kyphosis than other spinal deformities, especially in older patients with large deformities. Neurologic complications are more likely to occur if attempts are made to obtain maximum correction of the curve with use of instrumentation. Partial correction is preferable; the goal is to obtain a balanced spine in the coronal and sagittal planes, rather than maximal correction. Spinal cord monitoring is mandatory-the use of the wake-up test is recommended if the patient can cooperate. The natural history of Scheuermann disease is generally benign, and most patients do not experience signiicant disability in adulthood. A Milwaukee brace is recommended in skeletally immature patients with curves of 55 to 70 degrees. Surgical indications include a progressive thoracic kyphosis greater than 75 to 80 degrees in a skeletally immature patient; thoracolumbar kyphosis exceeding 50 to 55 degrees that is associated with pain unresponsive to conservative treatment; progression of deformity despite bracing; or cosmetic deformity that the surgeon, patient, and family consider signiicant and unacceptable. Diligent periodic observation of all patients with congenital kyphosis is crucial; without such observation, severe deformities with neurologic sequelae may develop. The natural history of congenital kyphosis, particularly type I deformities, is unfavorable. Insidious progression of the deformity can occur with growth, and surgery is recommended if progression is noted. Goals of treatment are early fusion to prevent severe deformity, halt progression, and achieve head and trunk balance. Classical Scheuermann disease in male monozygotic twins: further support for the genetic etiology hypothesis. Postoperatively, patients should be followed to skeletal maturity to ensure that progression of the primary or compensatory curves does not occur. The results of spinal arthrodesis of congenital spinal deformities in patients younger than ive years old. The authors reviewed the results of spinal fusion for congenital deformity in 49 patients younger than 5 years. The surgical treatment of congenital kyphosis: a review of 94 patients age 5 years or older with 2 years or more follow-up in 77 patients. The authors reviewed the results of spinal fusion for congenital kyphosis in 77 patients older than age 5. This was the irst long-term follow-up study on the natural history of Scheuermann disease. The authors further classiied type 1 deformities into four patterns of malformations. They noted that the posterolateral quadrant vertebra has the worst prognosis, progresses relentlessly, and has a high rate of spinal cord compression. This review article discusses the natural history, diagnosis, and treatment of Scheuermann disease. This is a report on seven patients with early thoracolumbar kyphosis with lumbar hypoplasia. Segmental analysis of the sagittal plane alignment of the normal thoracic and lumbar spines and thoracolumbar junction. Kyphosis of the thoracic and thoracolumbar spine in the pediatric patient: surgical treatment. Are radiologic changes in the thoracic and lumbar spine of adolescents risk factors for low back pain in adults Results of surgical treatment by posterior spine arthrodesis in twenty-two patients. Scheuermann kyphosis: safe and efective surgical treatment using multisegmental instrumentation. A prospective evaluation of pulmonary function in patients with adolescent idiopathic scoliosis relative to the surgical approach used for spinal arthrodesis. Prospective pulmonary function evaluation following open thoracotomy for anterior spinal fusion in adolescent idiopathic scoliosis. Pulmonary function before and ater anterior spinal surgery in adult idiopathic scoliosis. Correction of adolescent hyperkyphosis with posterior-only threaded rod compression instrumentation: is anterior spinal fusion still necessary Comparison of Scheuermann kyphosis correction by posterior-only thoracic pedicle screw ixation versus combined anterior/posterior fusion. Complications ater 147 consecutive vertebral column resections for severe pediatric spinal deformity: a multicenter analysis. Selection of the optimal distal fusion level in posterior instrumentation and fusion for thoracic hyperkyphosis: the sagittal stable vertebra concept. Radiographic spinopelvic parameters in skeletally mature patients with Scheuermann disease. Loss of spinal cord monitoring signals in children during thoracic kyphosis correction with spinal osteotomy: why does it occur and what should you do Hypotension-induced loss of intraoperative monitoring data during surgical correction of Scheuermann kyphosis: a case report. Inluence of induced hypotension and spinal distraction on feline spinal somatosensory evoked potentials. Transverse process hooks at upper instrumented vertebra provide more gradual motion transition than pedicle screws. Biomechanical risk factors for proximal junctional kyphosis: a detailed numerical analysis of surgical instrumentation variables. Incidence and risk factors for proximal and distal junctional kyphosis following surgical treatment for Scheuermann kyphosis: minimum ive-year follow-up. Acute celiac artery compression syndrome ater surgical correction of Scheuermann kyphosis.
Buy erythromycin 250mg visa
Antiepileptic medications such as phenytoin and valproate have been linked to decreased bone turnover and decreased intestinal absorption of calcium infection care plan erythromycin 250mg mastercard, resulting in osteopenia, which may afect implant ixation and should be considered in the selection of construct components. Drugs such as carbamazepine, phenytoin, and valproic acid can result in thrombocytopenia. However, other studies have shown that patients on valproic acid are not at increased risk of bleeding complications at surgery. Manohar and colleagues44 showed in a study of 84 children undergoing craniotomy for resection of seizure focus or hemispherectomy that none of the cohort showed signiicantly abnormal prothrombin time, activated partial thromboplastin time, or platelet count preoperatively. Poor upper airway tone and anatomic deviations can lead to increased risk of airway obstruction during and ater surgery. Patients may require a dietary change, placement of a gastrostomy tube, or a Nissen fundoplication with gastrostomy tube placement to control this aspiration tendency before undergoing spinal surgery. Reactive airway disease is common in these patients and may necessitate the use of preoperative bronchodilators and inhaled steroids. In addition, these patients may have chronic hypoventilation with carbon dioxide retention and poor oxygenation. Vital capacity that exceeds 500 mL and peak expiratory low greater than 180 mL/min are associated with decreased perioperative pulmonary complications. Although surgery may be considered in appropriately selected patients with preexisting respiratory failure, Chambers et al. If a patient cannot be assessed with formal pulmonary function tests, other signs of ventilatory capacity must be used, including crying, laughing, and other vocalizations. Many patients are malnourished secondary to a combination of relux, low calorie intake, and high metabolic demand from frequent illness. Malnourished patients are more prone to perioperative complications such as wound dehiscence, wound infection, and pulmonary complications. Conversely, older patients may be obese, presenting further operative complications associated with their body habitus. Nutritional status should be assessed preoperatively with albumin and total blood lymphocyte levels. Gastrointestinal Because patients with neuromuscular scoliosis are prone to gastrointestinal dysmotility, they are at risk for a postoperative ileus, requiring aggressive hydration, maximized nutritional status, and a rigid daily toilet regimen. In addition, some patients are very thin, and supine positioning and the acute straightening of their deformity put them at risk for superior mesenteric artery syndrome with obstruction of the duodenum. Although less common since the advent of segmental instrumentation and decreased use of casting, this prolonged obstruction carries signiicant morbidity; identifying at-risk patients and maintaining a high index of suspicion when encountering protracted vomiting is essential. Cardiovascular Patients may have cardiac problems secondary to their deformity and other cardiac issues that are comorbidities of the primary disorder. Hematologic Studies have shown that patients with neuromuscular scoliosis have greater blood loss than patients with idiopathic scoliosis undergoing similar procedures. In this neuromuscular group, the underlying disorder plays a major role in determining the extent of blood loss. Much of this diference is due to the requirement for larger fusions in patients with neuromuscular scoliosis, although osteopenia in these patients may also play a role. Patients should have partial thromboplastin time, prothrombin time, and platelet function evaluated as a part of their preoperative blood work. A more aggressive coagulopathy workup should be conducted if the patient has previously shown a tendency toward excessive blood loss. Chapter 28 Neuromuscular Scoliosis 477 For a posterior procedure, 2 to 4 units of packed red blood cells is generally suicient; however, the addition of a kyphectomy or an anterior procedure may increase this requirement. Intraoperative blood work may conirm a dilutional coagulopathy, necessitating the use of fresh frozen plasma, platelets, or cryoprecipitate to correct this imbalance. Several pharmacologic agents have been under investigation for their eicacy in reducing blood loss during surgery. Accurate measurements of the coronal Cobb angle, sagittal Cobb angle, and pelvic obliquity are crucial for complete preoperative planning and postoperative evaluations. In a more recent analysis of the interobserver and intraobserver variability of radiographic measurements of patients with neuromuscular scoliosis, Gupta and colleagues60 found that neuromuscular radiographs can be reliably analyzed with the use of the coronal Cobb angle. With the introduction of the Harrington rod in 1962, use of this instrumentation with fusion of the spine in patients with neuromuscular scoliosis became the standard. Several studies revealed that Luque segmental sublaminar wire ixation had fewer complications than Harrington instrumentation and was stable enough so that most patients required no brace or cast postoperatively. Because of these attributes, the Luque technique became the standard method for posterior spinal instrumentation in patients with neuromuscular spinal deformities. Contouring Luque spinal rods ater the technique introduced by Allen and Ferguson66 (Galveston technique) allowed the rods to be ixed to the pelvis, providing surgeons with a more efective method of controlling pelvic obliquity. Studies of patient outcomes with unit rod ixation have revealed excellent correction and maintenance of correction. Tsirikos and colleagues71 evaluated 287 children treated with unit rod instrumentation to the pelvis Radiographic Assessment Patients should have preoperative anteroposterior and lateral ilms taken of the entire spine, preferably in an upright (sitting or standing) position. For assessment of skeletal maturity, a separate anteroposterior radiograph of the pelvis should be considered because scoliosis ilms oten truncate the anatomy necessary to determine skeletal maturity. Unit rod instrumentation has also been shown to have good results in ambulatory patients, with excellent deformity correction and preservation of ambulatory function at 2. In their comparison study of 30 patients with unit rod instrumentation and sacral fusion and 25 patients with U-rod instrumentation and L5 fusion, McCall and Hayes74 found that the U-rod provided comparable correction of scoliosis and pelvic obliquity in curves with less than 15 degrees L5 tilt at 4 years of follow-up. Regardless of whether the precontoured unit rod or double Luque rods are used, segmental sublaminar wire instrumentation provides simple, inexpensive, and fairly powerful correction of coronal plane deformity. In some circumstances, a hybrid system with a combination of hooks, pedicle screws, and sublaminar wires may provide optimal ixation with maximal correction. Additionally, proximal ixation with sublaminar wires compromises the ligaments above, making junctional kyphosis more likely. Hooks (transverse process) or pedicle screws or both may limit this complication in kyphotic patients at greatest risk. This clinical course emphasizes that ixation challenges are present in patients with neuromuscular deformity, particular hyperkyphosis. Pelvic and Sacral Fixation Severe pelvic obliquity secondary to unbalanced scoliotic curves and lower extremity contractures is common and progressive in patients with neuromuscular scoliosis. Controlling the motion across the lumbosacral joint requires secure ixation to the pelvis to prevent a pseudarthrosis. Reviewing the results of 67 patients, McCarthy and colleagues83 found that this technique had decreased operative time compared with Galveston ixation and achieved excellent clinical results, although in 2 of the 67 constructs, there was migration of the rods into the pelvis. Other techniques of rod contouring to ix to the pelvis include the Warner-Fackler and McCall techniques, both commonly used in the treatment of myelomeningocele-associated kyphosis, in which posterior elements of the lumbar or sacral spine may be absent. In a slight variation of this technique, McCall85 described bending Luque rods to 20 to 40 degrees, passing them through the S1 foramina and bending the protruding portion according to the contour of the anterior sacrum. In 16 myelomeningocele patients with hyperkyphosis, McCall85 found satisfactory correction and maintenance of correction ater 5 years of follow-up. Clinical and biomechanical studies have shown an improved fusion rate and high pullout strengths ater the use of iliac screws for caudad lumbosacral ixation. In a direct comparison of 20 patients with Galveston rod ixation versus 20 patients with iliac screw ixation, Peelle and colleagues90 found that both techniques ofer similar pelvic ixation with the iliac screw construct, allowing additional screw ixation points to the sacrum and lower lumbar vertebrae. Chapter 28 Neuromuscular Scoliosis 481 Tsuchiya and colleagues88; no evidence of degeneration was observed at 5- to 10-year follow-up. Although iliac screws provide a promising alternative to Galveston ixation, several studies have shown diiculty with implant prominence causing skin irritation. A lower proile method of iliac ixation has been developed by Kebaish92 and Whitaker and colleagues93 that starts in the sacral ala lateral to the S1 foramen and traverses the sacroiliac joint before entering the iliac wing. In this study, the authors deined rigid instrumentation as consisting of at least 50% pedicle screw ixation with iliac or sacral alar iliac screw pelvic ixation. Previous studies on this traction technique have been described for patients with idiopathic and congenital scoliosis. In nonambulatory patients with neuromuscular scoliosis, surgeons have relied on rods or screws inserted into the iliac wings by a cantilever method to level the pelvis. In a study of 20 nonambulatory patients with neuromuscular scoliosis with halofemoral traction and 20 matched patients without halofemoral traction, Takeshita and colleagues95 found that halofemoral traction provided signiicantly improved lumbar curve and pelvic obliquity correction at 2-year follow-up.
Diseases
- Dyskinesia
- Microphthalmia
- Holzgreve Wagner Rehder syndrome
- Jequier Kozlowski skeletal dysplasia
- Ter Haar Hamel Hendricks syndrome
- Transverse limb deficiency hemangioma
Buy erythromycin 250 mg low price
When performing anterior fusion zombie infection jar generic erythromycin 500 mg without prescription, lordosis is achieved by positioning in extension using blanket rolls placed behind the shoulders and by placing distraction pins, which initially converge and, when distracted, tend to lordose the spine. Posteriorly, if reduction does not reduce kyphosis, either compression of the lateral mass screws or use of an interspinous wire can be performed to correct kyphosis. Posterior ligamentous injuries are associated with various anterior column injuries, such as compression or burst fractures. Associated with this injury are varying degrees of posterior ligamentous disruption, facet fracturing, and subluxation. An additional posterior fusion may be indicated in the more displaced and comminuted injuries. Unilateral Facet Dislocations Unilateral facet dislocation occurs when the inferior facet is translated over the superior facet, and is oten associated with facet fracture. Biomechanical studies suggest that signiicant posterior ligamentous and disc anulus injury is required for this injury to occur. Disc disruptions occur universally and disc herniation is present in 56% of patients. In the presence of a facet fracture, especially if it involves more than 40% of the facet, displacement may recur. Posterior fusion is indicated when vertebral body fractures are present and when open reduction is required. Long-term outcomes have been shown to be improved with surgical rather than nonoperative treatment. Bilateral Facet Dislocations Bilateral facet dislocations are highly unstable and result in a minimum of 50% vertebral subluxation. In addition to the facet dislocations, the posterior osteoligamentous complex and disc anulus are disrupted. Fractures of the lamina and spinous process also occur frequently, which may afect treatment decisions. Further, the intervertebral disc is always disrupted and may appear displaced into the spinal canal. In some cases, free disc fragments are located behind the cranial vertebral body wall and may remain ater reduction, causing increased cord compression. In intact patients, there is a small incidence of neurologic worsening from intervertebral disc herniation behind the vertebral body ater reduction. Discoligamentous injuries without neurologic injury can be treated in a cervical orthosis. When associated with central cord syndrome, early decompression-either by anterior or posterior approach-and fusion is recommended. At surgery, the anterior and posterior longitudinal ligaments and disc were disrupted. If the disc appears behind the body, then anterior discectomy and fusion is performed prior to reduction. If reduction cannot be achieved, the patient can be turned prone and an open reduction and posterior fusion performed. Alternatively, a closed reduction can be attempted if the patient is awake and cooperative by carefully monitoring the neurologic function as increasing weight is added. There is a teardrop fracture of the anterior-inferior corner of C5, and the posterior aspect of C5 is rotated into the spinal canal. The fracture is unstable and has a Subaxial Cervical Injury Classiication System score of 9. The postoperative magnetic resonance image shows severe cord edema, hematoma at the site of the injury, and posterior ligamentous disruption. Twelve hours later, she deteriorated and was transferred with central cord syndrome. Traumatic Spondylolisthesis Hyperextension forces can result in bilateral pedicle or pars fractures. With continued forces, the disc anulus is disrupted and vertebral subluxation occurs. Either an anterior or posterior approach can be utilized; in some cases, a combined approach is required. A Hyperextension Subluxations Hyperextension forces can cause disruption of the disc anulus, facet capsules, and even posterior ligaments, resulting in posterior vertebral body subluxation. Treatment may be traction initially but may result in overdistraction, as these injuries may have signiicant ligamentous disruptions. When incompetent from injury, anterior translation may result, with the potential for pain and neurologic injury. Nine of the 15 nonoperatively treated patients developed increased subluxation or kyphosis and needed surgical repair. In a systematic review, Kepler found that 88% of operative compared to 43% of nonoperatively treated patients maintained reduction. Posterior fusion is an alternative and occasionally needed if there is a displaced facet fracture causing radiculopathy requiring foraminotomy. The left and right sagittal computed tomographic sections show facet dislocations. There is 80% anterior translation of C4 on C5, with a fracture of the posterior inferior corner of C4 displaced into the spinal canal. In the center panel, the vertebral bodies realigned with only 25% residual subluxation, and reduction of one of the facet dislocations is seen (white arrows). The patient was turned supine, and anterior decompression and fusion were performed. Manoso reviewed 60 cases and found that 38% had radiculopathy and 18% had spinal cord injury. However, fracture separations are likely to develop subluxation, and careful follow-up is required. An important consideration is whether both segments should undergo fusion or just the level with subluxation. If alignment of the facets can be achieved, then a single-level arthrodesis can be attempted with either the anterior or posterior approach. Vertebral Artery Injury Vertebral artery injuries are common, and may occur in up to 11% of cervical trauma patients. Patients with documented vertebral artery injuries are to be treated with antiplatelet therapy. At the time of injury, there is transient compression of the spinal cord, resulting in a central cord injury. Clinically, patients present with worse neurologic deicits in their arms compared to the legs. Bony injury may be absent, but fractures of spinous processes and laminae, disc distraction, and retrolisthesis of vertebral bodies are oten present. Decompression is warranted in patients with signiicant deicits, instability, or progressive worsening. As the vertebra rotates in lexion, the cranial inferior facets slide upward and may become perched in an almost dislocated position. Perched facets indicate substantial injury to the nuchal ligaments, ligamenta lava, and likely the disc anulus, thus should be considered unstable. Most patients with perched facets should be treated surgically with either anterior or posterior fusion. Special Cases Fractures in Patients With Ankylosed Spines An increasing number of patients who have ankylosed spines due to ankylosing spondylitis, difuse idiopathic skeletal hyperostosis, severe degenerative disease, or from surgical fusion are sustaining cervical fractures. Fusion of additional levels is immaterial, as these patients are already fused by their disease. Traumatic Disc Herniation Rarely, a patient with head or neck trauma sustains a traumatic disc herniation with spinal cord compression. A commitment to patient safety at all stages of care is required to minimize the chance and severity of complications.
Buy generic erythromycin 500mg on-line
Tenderness to palpation of one or two levels is more consistent with bony pathology than tenderness at multiple levels infection from root canal generic erythromycin 500mg with visa. Continuing caudally, the lumbosacral junction and the sacral prominences and sacroiliac joint area can be palpated and percussed. Inlammation in these regions can manifest with sciatica, feigning disc herniation. Spasm can be noted in addition to tenderness; this may be present as a "ball" of contracted muscle in one region. Muscular atrophy can be a sign of long-standing neural compression and is more likely isolated to one motor group. Generalized, symmetric muscle atrophy can suggest a more systemic neurologic disorder, such as a demyelinating disease. Standard dermatomal charts can be helpful, but there is variability among individuals; thus, this is highly subjective. L4 sensory function is tested at the medial ankle; L5, at the irst webspace between the great and second toes; and S1, at the lateral aspect of the sole of the foot. Sensory function should be compared with the contralateral side because this may help detect diferences. In the lower extremity, it is better to test movements rather than speciic muscles. S1 motor function is assessed by testing plantarlexion, whereas L5 is tested by toe dorsilexion, particularly the great toe (extensor hallucis longus), and hip abduction. L4 involvement most oten afects ankle dorsilexion (anterior tibialis), although quadriceps function can be compromised. Motor function is graded as 0 to 5, with 5 being full strength against active resistance (Table 47. In particular, S1 function should be assessed by asking the patient to toe raise repeatedly or toe-walk. Generally, relexes are anticipated to be decreased in response to nerve root compression from a herniated disc. Increased relexes (hyperrelexia), especially if bilaterally symmetric, can indicate spinal cord compression at the thoracic or cervical level. Studies have determined that in the irst 35 degrees of elevation, the slack in the nerves is taken up, and at 35 degrees or more, tension is placed on the nerves. It is not useful for upper lumbar roots, for which a femoral stretch test should be used. If raising the contralateral leg reproduces symptoms in the ipsilateral side, this is highly suggestive for a herniated disc. It should be considered strong evidence of the diagnosis and is more speciic for a free disc fragment. When a patient is initially examined, the patient is usually seated at the side of the examining table with the knees and hips lexed at about 90 degrees. With a herniated fragment causing nerve root tension, the patient relexively extends at the hip and leans back to relieve the ensuing sciatic pain. Diferential Diagnosis he diferential diagnosis should be narrowed based on history, physical examination, and selected imaging tests. Radicular pain can be caused by numerous compressive disorders, such as spinal stenosis, abscess, tumor, or vascular disease. Intrinsic nerve problems, such as nerve tumors or multiple sclerosis, can produce similar symptoms. Peripheral neuropathies, such as tarsal tunnel syndrome, meralgia paresthetica, and obturator or piriformis syndrome, can also lead to similar sciatic-type pain. Diagnostic Imaging We use a simple imaging algorithm for patients with suspected lumbar herniated discs. If the patient presents acutely, within the irst 2 weeks of the incident, the examination is typically masked by a large amount of spasm, back pain, and generalized tenderness. If the mechanism of injury involved substantial trauma, plain radiographs are obtained. For low-energy injury, radiographs can be delayed until the follow-up examination at 6 weeks. Numerous patients will have recovered substantially by 6 weeks, obviating the need for further workup. For patients whose pain has not improved or perhaps has worsened, plain radiographs are obtained. Advanced imaging is reserved for patients in whom pain is persistent, the diagnosis is unclear, or surgical treatment is planned. Other indings that can be noted on plain ilms are changes consistent with disc degeneration, including osteophytes; disc space narrowing; or subtle changes in translation, facet hypertrophy, or changes in sagittal alignment. Most commonly, plain ilms are negative, especially in younger patients with an acute herniation. Plain ilms are important in ruling out obvious underlying problems, such as lytic lesions, tumors, infections, inlammatory spinal disorders, or instabilities. It is crucial to recognize if there is an anomalous number of lumbar vertebrae, such as spines with a "lumbarized" irst sacral segment. Plain ilms can help detect other congenital anomalies, such as spina biida occulta defects, which can inluence surgical exposure and dissection. This makes compression from disc herniations readily visible, as can be visualized in this case of a large extruded paracentral disc herniation. Neural encroachment can be detected within the spinal canal, the foramina, or extraforaminally. Dorsal root ganglion enhancement was found to be nonspeciic, occurring in controls and sciatica patients. Enhancement of the root proper was detected, however, in 11 of 30 symptomatic patients, with patients having a statistical tendency for more severe motor involvement. Komori and colleagues41 studied the signiicance of enhancement around the herniated fragment itself. Patients with marked decrease in size of the herniation showed good clinical resolution. Decrease in fragment size was associated with a gradual increase in the area of enhancement in 17 of 22 sequestered disc herniations, all of which had improvement of radicular pain. Five cases of sequestered discs without enhancement or size decrease had a poor clinical result. Enhancement was less marked in extruded versus sequestered herniations; however, herniations that did show enhancement had a signiicantly better clinical course. From these data, Komori and colleagues41 recommended this test as a prognostic tool in guiding the treatment of patients with extruded or sequestered herniated discs. Because images are traditionally acquired in the supine position, the spine is not axially loaded as it is during everyday activities. Images were obtained in the usual supine position and with a seated lexed and extended posture. Changes in foraminal size and neural compression occurred with lexion and extension. Failures may be related to numerous factors, including psychosocial disturbance, recurrence, infection, wrong-level surgery, poor surgical indications, and improper operative technique. Residual or recurrent back and leg complaints oten prompt practitioners to seek postoperative imaging. Plain radiographs can show overall alignment, with lexion-extension views useful in detecting instability, spondylolisthesis, or disc space collapse, which is a frequent occurrence ater discectomy in adult patients. A herniated disc fragment may eventually enhance if enough time passes before it is imaged. Barrera and colleagues47 compared diferent imaging sequences with and without gadolinium contrast agent. Recurrent symptoms occurred, however, in 84% of patients with focal (extradural, ater the nerve root has exited the cauda equina) enhancement and 86% of patients with nerve root thickening. Enhancement occurred in patients with and without evidence of nerve root displacement by scar or disc. Myelography Plain myelography previously was the imaging modality of choice in detecting herniated discs.
Cheap erythromycin 500mg online
Efect of various tapping diameters on insertion of thoracic pedicle screws: a biomechanical analysis bacteria that begins with the letter x order 250 mg erythromycin mastercard. Factors afecting the pullout strength of self-drilling and self-tapping anterior cervical screws. Pedicle screw placement at the sacrum: anatomical characterization and limitations at S1. Advantage of pedicle screw ixation directed into the apex of the sacral promontory over bicortical ixation: a biomechanical analysis. Feasibility and biomechanical performance of a novel transdiscal screw system for one level in non-spondylolisthetic lumbar fusion: an in vitro investigation. Can triggered electromyography be used to evaluate pedicle screw placement in hydroxyapatite-coated screws: an electrical examination. Surgical treatment for pyogenic vertebral osteomyelitis using iodine-supported spinal instruments: initial case series of 14 patients. Spinal cord decompression via a modiied costotransversectomy approach combined with posterior instrumentation for management of metastatic neoplasms of the thoracic spine. Transpedicular decompression and stabilization of burst fractures of the lumbar spine. Oxidative stress and heat shock protein response in human paraspinal muscles during retraction. One-year follow-up of a series of 100 patients treated for lumbar spinal canal stenosis by means of HeliFix interspinous process decompression device. Microdiscectomy with and without insertion of interspinous device for herniated disc at the L5-S1 level. Decompression and paraspinous tension band: a novel treatment method for patients with lumbar spinal stenosis and degenerative spondylolisthesis. Biomechanical comparison of an interspinous fusion device and bilateral pedicle screw system as additional ixation for lateral lumbar interbody fusion. Biomechanical analysis of an interspinous fusion device as a stand-alone and as supplemental ixation to posterior expandable interbody cages in the lumbar spine. Posterior tension band wiring and instrumentation for thoracolumbar lexion-distraction injuries. Adolescent idiopathic scoliosis correction achieved by posteromedial translation using polyester bands: a comparative study of subtransverse process versus sublaminar ixation. Hybrid ixation with sublaminar polyester bands in the treatment of neuromuscular scoliosis: a comparative analysis. Braided tubular superelastic cables provide improved spinal stability compared to multiilament sublaminar cables. A comparative biomechanical study of spinal ixation using the combination spinal rod-plate and transpedicular screw ixation system. Orthopedic devices: classiication and reclassiication of pedicle screw spinal systems; technical amendment. A comparison of stress-induced porosity due to conventional and a modiied spinal ixation device. Comparison of loads on internal spinal ixation devices measured in vitro and in vivo. Sacral spinous processes: a morphologic classiication and biomechanical characterization of strength. Clinical eicacy of lumbar and lumbosacral fusion using the Boucher facet screw ixation technique. Outcomes of posterior facet versus pedicle screw ixation of circumferential fusion: a cohort study. Mini-open or percutaneous bilateral lumbar transfacet pedicle screw ixation: a technical note. Neuropathologic changes with experimental spinal instrumentation: transpedicular versus sublaminar ixation. Volumetric spinal canal intrusion: a comparison between thoracic pedicle screws and thoracic hooks. Pullout strength of pedicle screws versus pedicle and laminar hooks in the thoracic spine. Correction of adolescent idiopathic scoliosis using thoracic pedicle screw ixation versus hook constructs. Risk factors for postoperative complication ater spinal fusion and instrumentation in degenerative lumbar scoliosis patients. Single segment of posterior lumbar interbody fusion for adult isthmic spondylolisthesis: reduction or fusion in situ. Posterior reduction and anterior lumbar interbody fusion in symptomatic low-grade adult isthmic spondylolisthesis: short-term radiological and functional outcome. Implant distribution in surgically instrumented Lenke 1 adolescent idiopathic scoliosis: does it afect curve correction Rib hump deformity assessment using the rib index in adolescent idiopathic scoliotics treated with full screw or hybrid constructs: aetiological implications. Posterior-only correction of Scheuermann kyphosis using pedicle screws: economical optimization through screw density reduction. Do anchor density or pedicle screw density correlate with short-term outcome measures in adolescent idiopathic scoliosis surgery Short segment spinal instrumentation with index vertebra pedicle screw placement for pathologies involving the anterior and middle vertebral column is equally efective as long segment stabilization with cage reconstruction: a biomechanical study. Posterior ixation including the fractured vertebra for severe unstable thoracolumbar fractures. Results of treatment of unstable thoracolumbar burst fractures using pedicle instrumentation with and without fracture-level screws. Comparative study of 2 surgical procedures for osteoporotic delayed vertebral collapse: anterior and posterior combined surgery versus posterior spinal fusion with vertebroplasty. A biomechanical assessment of kyphoplasty as a stand-alone treatment in a human cadaveric burst fracture model. Unilateral versus bilateral pedicle screw ixation for degenerative lumbar diseases: a meta-analysis of 10 randomized controlled trials. Unilateral versus bilateral instrumentation in spinal surgery: a systematic review. Clinical outcomes and sagittal alignment of single-level unilateral instrumented transforaminal lumbar interbody fusion with a 4 to 5-year follow-up. Increased incidence of pseudarthrosis ater unilateral instrumented transforaminal lumbar interbody fusion in patients with lumbar spondylosis: Clinical article. Comparison of unilateral versus bilateral pedicle screw ixation in lumbar interbody fusion: a meta-analysis. Biomechanical study of unilateral pedicle screw combined with contralateral translaminar facet screw in transforaminal lumbar interbody fusion. Comparison of transforaminal lumbar interbody fusion performed with unilateral pedicle screw ixation or unilateral pedicle screw-contralateral percutaneous transfacet screw ixation. Pedicle screw placement in the lumbar spine: efect of trajectory and screw design on acute biomechanical purchase. Safety and eicacy of pedicle screw placement using intraoperative computed tomography: consecutive series of 1148 pedicle screws. Monitoring the quality of robot-assisted pedicle screw ixation in the lumbar spine by using a cumulative summation test. Good clinical outcomes and fusion rate of facet fusion with a percutaneous pedicle screw system for degenerative lumbar spondylolisthesis: minimally invasive evolution of posterolateral fusion. Does minimally invasive percutaneous posterior instrumentation reduce risk of proximal junctional kyphosis in adult spinal deformity surgery Neuromonitoring with pulse-train stimulation for implantation of thoracic pedicle screws: a blinded and randomized clinical study. Direct vertebral rotation: a new technique of three-dimensional deformity correction with segmental pedicle screw ixation in adolescent idiopathic scoliosis. A computational biomechanical investigation of posterior dynamic instrumentation: combination of dynamic rod and hinged (dynamic) screw.
Syndromes
- Impaired perception and motor skills
- Citrus fruits
- Eating enough calories and protein to keep your weight up
- Cloudiness of the front of the eye
- Centers for Disease Control and Prevention - www.cdc.gov/asthma
- Warm-up properly before exercise and sports.
Purchase line erythromycin
While the patient may be positioned prone virus upper respiratory buy 500mg erythromycin free shipping, my preferred technique is to position the patient lateral, under general anesthesia, with the hips and knees lexed and taped in this position. Of note, the spinous processes may oten be diicult to visualize, while the disc spaces are generally better delineated. Over the last decade, clinical studies have been reported comparing various interspinous devices to more traditional approaches. Both study groups required symptoms to be refractory to 6 months of nonoperative care. All patients had to be older than 50 years, able to walk at least 50 feet, and obtain symptom relief with sitting. Outcomes were measured by the Zurich Claudication Questionnaire, Short-Form 36 questionnaire, and radiographic measurements. Complications included incisional pain, hematoma, wound swelling, wound dehiscence, implant dislodgement, implant malposition, spinous process fracture, coronary ischemia, and respiratory distress. Spinous process fracture warrants speciic mention, as clinical outcomes are not always failures. If the fracture obviates stable intraoperative placement or the implant posteriorly displaces in the postoperative period, results may sufer but surprisingly not always or even routinely. Additionally, there was no increase in the degree of spondylolisthesis in the study group. Twenty patients had undergone revision fusion during the study period, while 80% of the patients reported good clinical results. Four of their initial patients showed no improvement in symptoms, while eight patients showed complete resolution of their symptoms. A total of 77% of patients had experienced at least a 15-point improvement in their Oswestry Disability Index, which was maintained at the 4-year postoperative follow-up. More recently, Stromqvist16 presented 100 patients randomized in a prospective controlled study comparing 50 patients treated with the X-Stop and 50 patients undergoing traditional decompressive surgery. However, the X-Stop group had a 26% reoperation rate, while the decompressive group had a 6% reoperation rate. A total of 83% of the Superion group and 84% of the X-Stop reported that they would undergo the same treatment again. Reoperation rates were 23% for the Superion group and 19% the X-Stop group, primarily for inadequate pain relief or return of symptoms. A total of 8 diferent implants were represented with a variety of clinical indications. Chief reasons for reoperation were implant dislocation (20 cases), no improvement (18 cases), spinous process fracture, overdistraction (27 cases), and/or recurrent symptoms ater initial improvement (42 cases). Outcome studies for speciic diagnoses and surgeon opinion, as well as reimbursement, will ultimately deine their relative role in the armamentarium of surgical procedures utilized in the care of the stenosis patient. In 12 patients with 17 distracted levels, the area of the dural sac at these levels increased from 77. The efects of an interspinous implant on the kinematics of the instrumented and adjacent levels in the lumbar spine. The lexion-extension range of motion was signiicantly reduced at the instrumented level. Axial rotation and lateral bending ranges of motion were not afected at the instrumented level. The range of motion in lexion-extension, axial rotation, and lateral bending at the adjacent segments was not signiicantly afected by the implant. At every follow-up visit, X-Stop patients had signiicantly better outcomes in each domain of the Zurich Claudication Questionnaire. Additionally, clinical outcomes data comparing interspinous process devices to more traditional surgical approaches are also lacking. Biomechanical efect of diferent interspinous implants on lexibility and intradiscal pressure. Clinical evaluation of a lumbar interspinous dynamic stabilization device (the Wallis system) with a 13-year mean followup. High failure rate of the interspinous distraction device (X-Stop) for the treatment of lumbar spinal stenosis caused by degenerative spondylolisthesis. X-stop versus decompressive surgery for lumbar neurogenic intermittent claudication: randomized controlled trial with 2-year follow-up. Efectiveness of interspinous implant surgery in patients with intermittent neurogenic claudication: a systematic review and meta-analysis. Interspinous process device versus standard conventional surgical decompression for lumbar spinal stenosis: randomized controlled trial. Interspinous process devices versus standard conventional surgical decompression for lumbar spinal stenosis: cost-utility analysis. Failure rates and complications of interspinous process decompression devices: a European multicenter study. While there is no strict deinition of a minimally invasive technique, the proposed hallmarks include smaller incisions, muscle-splitting rather than muscle stripping, limiting sot tissue damage, and variable sot tissue retraction for visualization. Lumbar spine applications include tubular retractors for decompression and interbody fusions and percutaneous methods for posterior instrumentation. Subperiosteal muscle dissection and sot tissue retraction time and pressure have been shown to induce muscle edema and subsequent muscle necrosis. Proponents of minimally invasive techniques point to early, albeit growing, evidence that these techniques result in less postoperative pain, decreased hospital length of stay, decreased blood loss, fewer surgical site infections, and a quicker return to function. Approach-related morbidity in the cervical spine, while low, still leaves room for improvement. For example, the incidence of dysphagia following cervical surgery has been quoted to be as high as 71%. If minimally invasive techniques can reduce approach-related morbidity and subsequently improve patient recovery and outcomes, there certainly is a growing patient population that may beneit from these techniques. Contraindications to this technique include cervical myelopathy or severe cervical spinal stenosis, large disc herniations (particularly central, requiring near-complete discectomy), bilateral radiculopathy, preexisting cervical instability or fracture, calciied disc herniations, axial neck pain, and signiicant anterior cervical sot tissue scarring. Clinical Evaluation History should focus on the location and quality of unilateral radicular complaints while simultaneously ruling out other potential etiologies for pain. A thorough neurologic examination should also ensure that there are no signs of myelopathy. A towel roll can be placed between the scapulae to aid cervical extension with or without use of Mayield clamps. Skin markings and use of anteroposterior and lateral luoroscopy can help aid localization toward the indicated disc level. A small transverse incision is made in the platysma to allow eventual passage of an initial blunt, thin dilator. With use of an index inger, bluntly sweep subplatysmal structures away through inger dissection. Care should be taken to palpate the trachea, larynx, carotid artery, and the desired cervical disc. Insert the initial blunt dilator to open the prevertebral fascia and sequentially dilate up. Fluoroscopy should conirm docking on the appropriate disc space in anteroposterior and lateral planes. Maintain a thin lateral wall, as this will help to protect the vertebral artery, as well as a thin dorsal edge to protect the exiting nerve root. Alternating use of curettes and a Kerrison rongeur under endoscopic visualization will allow safe removal of disc material until visualization of the posterior longitudinal ligament. Care is taken to remove all herniated disc material using microsurgical instruments under endoscopic visualization. A sot collar can be used for the irst 2 weeks to allow wound healing, ater which the brace can be worn for comfort. Clinical Outcomes and Published Studies Published clinical studies have shown encouraging results. Over the 2-year follow-up, clinical outcomes were noted to be "good" with similar low rates of revision surgery for persistent radicular arm pain (7.
Erythromycin 250mg mastercard
Biomechanical analysis of bone mineral density antibiotic ear infection 250mg erythromycin visa, insertion technique, screw torque, and holding strength of anterior cervical plate screws. Initial stability of cervical spine ixation: predictive value of a inite element model. Efects of disc height and distractive forces on grat compression in an anterior cervical discectomy model. One-stage internal ixation and anterior fusion in complex cervical spinal disorders. Vocal fold paralysis ater anterior cervical spine surgery: incidence, mechanism, and prevention of injury. Anterior screw ixation of odontoid fractures comparing younger and elderly patients. Endoscopic endonasal atlantoaxial transarticular screw ixation technique: an anatomical feasibility and biomechanical study. Anterior cervical instrumentation enhances fusion rates in multilevel reconstruction in smokers. Anterior decompression and arthrodesis of the cervical spine: long-term motor improvement. Banked ibula and the locking anterior cervical plate in anterior cervical fusions following cervical discectomy. Biomechanical analysis of a new concept: an add-on dynamic extension plate for adjacent-level anterior cervical fusion. A new stand-alone cervical anterior interbody fusion device: biomechanical comparison with established anterior cervical ixation devices. Loosening at the screw-vertebra junction in multilevel anterior cervical plate constructs. Biomechanical rigidity of cadaveric cervical spine with posterior versus combined posterior and anterior instrumentation. Initial intervertebral stability ater anterior cervical discectomy and fusion with plating. Short-term comparison of cervical fusion with static and dynamic plating using computerized motion analysis. Use of a bioabsorbable anterior cervical plate in the treatment of cervical degenerative and traumatic disk disruption. Bioresorbable polylactide interbody implants in an ovine anterior cervical discectomy and fusion model: three-year results. Early failure of bioabsorbable anterior cervical fusion plates: case report and failure analysis. Pseudarthrosis failures of anterior subaxial cervical spine fusion using a plate with a single screw per vertebral body: a case series. A comparison of fusion rates between single-level cervical corpectomy and two-level discectomy and fusion. Pedicle screws enhance primary stability in multilevel cervical corpectomies: biomechanical in vitro comparison of diferent implants including constrained and nonconstrained posterior instumentations. Cervical spinal stenosis: outcome ater anterior corpectomy, allograt reconstruction, and instrumentation. Anterior cervical allograt arthrodesis and instrumentation: multilevel interbody grating or strut grat reconstruction. Enhancement of stability following anterior cervical corpectomy: a biomechanical study. Anterior decompression combined with corpectomies and discectomies in the management of multilevel cervical myelopathy: a hybrid decompression and ixation technique. Comparison of outcomes for unstable lower cervical lexion teardrop fractures managed with halo thoracic vest versus anterior corpectomy and plating. Single level arthrodesis as treatment for midcervical fracture subluxation: a cohort study. Biomechanical analysis of anterior cervical spine plate ixation systems with unicortical and bicortical screw purchase. Biomechanical comparison of anterior cervical spine locked and unlocked plate-ixation systems. Systematic review of the efect of dynamic ixation systems compared with rigid ixation in the anterior cervical spine. Efects of a cervical compression plate on grat forces in an anterior cervical discectomy model. Cervical spine loading characteristics in a cadaveric C5 corpectomy model using a static and dynamic plate. Biomechanical evaluation of Caspar and Cervical Spine Locking Plate systems in a cadaveric model. Anterior cervical plate ixation: a biomechanical study to evaluate the efects of plate design, endplate preparation, and bone mineral density. Stress-shielding compared with load-sharing anterior cervical plate ixation: a clinical and radiographic prospective analysis of 50 patients. Anterior cervical discectomy and fusion with a locked plate and wedged grat efectively stabilizes lexion-distraction stage-3 injury in the lower cervical spine: a biomechanical study. Efect of age on the perioperative and radiographic complications of multilevel cervicothoracic spinal fusions. A simple method to ensure proper screw position and plate size selection using the Morscher cervical spine locking plate. Adjacent level ossiication development ater anterior cervical fusion without plate ixation. Anterior correction of cervical spine lordosis using an adjustable depth tap: technical note. Failure of a titanium anterior cervical plate implant: microstructural analysis of failure. Reoperation rates for acute grat extrusion and pseudarthrosis ater one-level anterior corpectomy and fusion with and without plate instrumentation: etiology and corrective management. A randomized study, with or without plate ixation, using radiostereometry in 27 patients. A review of the utility of obtaining repeated postoperative radiographs following single-level anterior cervical decompression, fusion, and plate placement. Changes in cervical spine curvature ater uninstrumented one- and two-level corpectomy in patients with spondylotic myelopathy. Plate ixation adds stability to two-level anterior fusion in the cervical spine: a randomized study using radiostereometry. Treatment of unstable lower cervical spine injuries by anterior instrumented fusion alone. Biomechanical testing of circumferential instrumentation ater cervical multilevel corpectomy. Does anterior plating of the cervical spine predispose to adjacent segment changes Delayed esophageal injury without instrumentation failure: complication of anterior cervical instrumentation. Asymptomatic esophageal perforation caused by late screw migration ater anterior cervical plating: report of a case and review of relevant literature. Persistent swallowing and voice problems ater anterior cervical discectomy and fusion with allograt and plating: a 5- to 11-year follow-up study. Risk factors for dysphagia ater anterior cervical spine surgery: a two-year prospective cohort study. Inluence of anterior cervical plate design on dysphagia: a 2-year prospective longitudinal follow-up study. Primary stabilizing efect of interbody fusion devices for the cervical spine: an in vitro comparison between three diferent cage types and bone cement. A new anterior cervical instrumentation system combining an intradiscal cage with an integrated plate: an early technical report. Comparative biomechanical analysis of a cervical cage made of an unsintered hydroxyapatite particle and poly-L-lactide composite in a cadaver model. Debridement and spinal instrumentation as a single-stage procedure in bacterial spondylitis/ spondylodiscitis. Corpectomy followed by the placement of instrumentation with titanium cages and recombinant human bone morphogenetic protein-2 for vertebral osteomyelitis.
Buy cheap erythromycin 500mg on line
Other antibiotics you cannot take with methadone order erythromycin on line amex, less common approaches have also been described for upper thoracic disc herniations. Relative contraindications include previous tube thoracostomy or previous thoracotomy. At 1-year follow-up, 76% of patients related satisfactory results; 24% of patients reported dissatisfaction or no change. In a further extension of their series, Anand and Regan30 reported outcomes on 100 consecutive cases with minimal 2-year follow-up. In 100 patients, 117 discs were excised; 40 patients underwent fusion: 27 with autologous rib strut and 13 with a threaded interbody fusion cage. Mean operative time was 173 minutes, mean blood loss was 259 mL, and average length of stay was 4 days. Intercostal neuralgia occurred in six patients (6%) early in the series and declined subsequent to use of sot lexible intercostal trocars. One patient incurred a 2500-mL blood loss; open conversion to thoracotomy was done in one patient. Five patients underwent reoperation: four for secondary fusion secondary to discogram-positive intractable axial pain and one for pseudarthrosis with a threaded interbody fusion device that was removed and replaced with a rib grat strut. Of the 68 who responded to the patient satisfaction survey, 18% rated their procedure satisfaction as excellent, 54% as good, 16% as fair, and 12% as poor. Oswestry scores improved with 36% of patients with preoperative scores greater than 50 and 23% of patients with preoperative scores less than 50. Six patients showed a transient postoperative intercostal neuralgia; the incidence diminished with subsequent use of sot trocars. Atelectasis or efusion resulting in a prolonged hospital stay was seen in ive patients. Penetration of the right hemidiaphragm occurred in one case, with mild parenchymal laceration to the liver repaired thoracoscopically without postoperative sequelae. Intraoperative conversion to open thoracotomy was required in one patient secondary to scarring from a previous costotransversectomy. In 11 of the patients, there was no deinitive plane between the calciied disc and the dura. Minimally Invasive Techniques here have been several more recent reports of using minimally invasive techniques for the surgical treatment of thoracic disc herniations. Following that, Lidar and colleagues129 used the technique on 10 patients with myelopathy secondary to thoracic disc herniation. No complications were reported, with a mean operative time of 153 minutes per level and hospital stay of 21 hours. Reported outcomes were excellent or good in 13 (81%), fair in 1 (6%), and poor in 2 (13%). Of asymptomatic adults, 73% have positive anatomic indings, including 37% with disc herniation and 29% with spinal cord deformation. For symptomatic central thoracic disc herniation, the transthoracic approach is probably the safest. Surgical treatment of thoracic disc herniation by laminectomy has a 28% chance of worsening symptoms. Blood supply to the spinal cord is tenuous in the thoracic spine, especially from T4 to T9, and ligation of blood vessels within the neural foramina should be avoided whenever possible because this may cause paralysis. Diagnosis is diicult owing to myriad symptoms, and there is no clear-cut clinical syndrome. Most herniations occur in the lower thoracic region; central protrusions are more frequent than lateral protrusions. In most cases, the cause is a degenerative process, but a history of trauma can be elicited in approximately one-third of cases; an association with Scheuermann disease has been suggested by several authors. Radiologic evaluation is essential for the diagnosis, but plain ilms are helpful only if disc calciication is present. Laminectomy is no longer indicated for treatment of thoracic disc herniation because of a high risk of neurologic deterioration and the fact that it may compromise the results of later anterior decompression. Discectomy may be performed by various surgical approaches: costotransversectomy, transthoracic, posterolateral, or video-assisted. Posterolateral techniques are ideal for lateral lesions and may be the best choice for herniated discs with coexistent stenosis. Upper thoracic lesions are more diicult to approach through the chest and may be managed best by costotransversectomy. Depending on the experience of the surgeon, video-assisted approaches can provide an alternative with reportedly less surgical morbidity. Newer minimally invasive approaches are also being developed that may ofer less pain and quicker recovery. The true incidence of thoracic herniated discs is unknown; many cases are unrecognized, or patients are asymptomatic. The pathogenesis of neurologic compromise secondary to herniated thoracic discs is believed to be a combination of direct neural compression and vascular insuiciency. A thorough neurologic examination is mandatory; the examiner should pay close attention to long tract signs and other evidence of myelopathy. Indications for surgery include progressive myelopathy, lower extremity weakness or paralysis, bowel or bladder dysfunction, and radicular pain refractory to conservative measures. The recommended extent of bone and disc removal varies from a relatively small trough in the posterior aspect of the disc to complete discectomy with partial corpectomy of adjacent bodies. The prognosis of patients who have herniated thoracic discs treated surgically is favorable, and early operative intervention is advised in cases of myelopathy or refractory radicular pain. The authors describe the technique and clinical outcome of video-assisted thoracic disc decompression. This review of the literature details the clinical presentation and progression of thoracic disc herniation. This article describes the technique of transthoracic disc decompression and clinical outcomes. The clinical method and the outcome of nonoperative thoracic disc herniation treatment are presented. This article is a summary of the early experience of the authors of this chapter using the transthoracic approach for treating patients with symptomatic thoracic herniated discs. Spinal cord compression caused by a protruded thoracic disc: report of a case treated with anterolateral fenestration of the disc. Case reports and technical notes on transthoracic removal of thoracic disc: report of three cases. Microsurgical anatomy and related techniques to an anterolateral transthoracic approach to thoracic disc herniations. A technical report on video-assisted thoracoscopy in thoracic spine surgery: preliminary description. Video-assisted thoracoscopic excision of herniated thoracic disc: description of technique and preliminary experience in the irst 29 cases. Removal of a protruded thoracic disc using microsurgical endoscopy: a new technique. Injury of the spinal cord due to rupture of an intervertebral disc during muscular efort. Spinal compression caused by enchondrosis of the intervertebral ibrocartilage with a review of the recent literature. Complications in thoracoscopic spinal surgery: a study of 90 consecutive patients. A calciied thoracic intervertebral disk with herniation and spinal cord compression in a child: case report. Multiple protrusions of intervertebral disks in the upper thoracic region: report of case. Chapter 45 Thoracic Disc Disease lumbar spine: insights into the etiopathogenesis of spinal degeneration. Protrusion of intervertebral discs: study of their distribution, characteristics and efects on the nervous system. Asymptomatic versus symptomatic herniated thoracic discs: their frequency and characteristics as detected by computed tomography ater myelography. Post-operative pain-related morbidity: video-assisted thoracic surgery versus thoracotomy.
Best buy for erythromycin
Melvill and Baxter14 used the intertransverse approach for discectomy in 40 patients with extraforaminal herniations antimicrobial epoxy paint discount generic erythromycin canada. Melvill and Baxter14 noted a ibrous band that was present tethering the nerve root to the lateral aspect of the disc in an associated cadaveric study. Assuming uniformity of the deinition of instability and indications for fusion in these cases, this inding is supportive of the hypothesis by McCulloch and Transfelt31 that lateral disc herniations were a precursor to the development of degenerative spondylolisthesis. A thorough knowledge of the anatomy in this region is imperative to performing an efective discectomy without undue bleeding or injury to the nerve root. Identiication of the correct level of incision is crucial in minimizing the length of the incision. It is more common with central herniation (27% of central herniations), although it can occur with paracentral or lateral herniations as well. Proponents of laminectomy believe that this provides superior visualization of the dura and avoids excessive traction. Although a number of studies have reported that surgical decompression within 48 hours of the onset of symptoms is a safe time point within which to perform surgery, more recent systematic reviews have concluded that there is no strong support for the oten-cited 24- or 48-hour thresholds nor that the earlier the decompression, the better the outcomes. Still, endoscopic discectomy remains a technically demanding procedure, and the results depend heavily on surgeon experience. A study by Pan and colleagues did not show a signiicant diference in patient-reported pain when comparing endoscopic and traditional open discectomy, though postoperative inlammatory markers such as interleukin-6 and C-reactive protein were reduced in the endoscopic group. Using a lateral decubitus position, the technique uses a small paramedian incision for introduction of the instruments. Dilators are used to strip the muscles subperiosteally from the adjacent lamina as far lateral as the facet joint. A shaver is used to remove bone within the interlaminar window until the attachments of the ligamentum lavum can be visualized. A root retractor pulls the nerve root and dura medially, allowing access to the disc space. Yeung and Tsou80 reported results of 307 endoscopically assisted transforaminal discectomies. A standard discogram is performed irst, injecting blue dye into the disc space to help identify the herniated tissue. Six patients (2%) had lower extremity dysesthesia that lasted longer than 6 weeks, two had thrombophlebitis, two had discitis, and one had a dural tear that did not require repair. Yoshimoto and colleagues demonstrated transforaminal microendoscopic decompression to be efective for treating far-lateral disc herniations. Several authors have sought to compare the results of microendoscopic discectomy with more traditional techniques. Percutaneous Automated Discectomy Because of the evolution of percutaneous techniques of discectomy, there is considerable "overlap" in the names of different procedures. Although endoscopic discectomy can be considered percutaneous, it is not what is typically considered percutaneous automated discectomy. Chapter 47 Lumbar Disc Herniations 863 Using a posterolateral approach, a tissue-removing device is introduced into the disc space in a similar path as the needle of a discogram; this is guided by intraoperative luoroscopy. Earlier techniques used a direct lateral approach that led to (or raised concern of) viscous perforation in some patients. Shapiro93 showed only partial improvement of leg pain in 57% of patients undergoing this procedure. In contrast, Hoppenfeld94 reported more successful results, with relief of sciatica and sensory deicit in 86% of patients. He determined, however, that patients with sequestered discs do not reliably respond well to the procedure. Kotilainen and Valtonen95 treated 41 patients with small protrusions or prolapses (bulges) with percutaneous automated discectomy. From these data, it can be inferred that automated discectomy can be reasonably efective in patients with small disc bulges or protrusions that are in direct continuity with the remaining nucleus. Only in this select group of patients is there the possibility of relieving the neural compression. Most lumbar disc herniations respond well to conservative treatment within the irst 3 months from the onset of symptoms. In patients who fail conservative treatment, surgery consistently showed better outcomes than continued nonoperative care. The type and size of disc herniations and psychosocial factors are the primary determinants of outcomes after discectomy. Although minimally invasive techniques, such as endoscopic and percutaneous laser discectomy, can be efective in experienced hands, it is unclear whether they would ever replace the gold standard operation of open discectomy (with or without the use of a microscope). Patients with extraforaminal (far lateral) and central disc herniations should be advised that surgical outcomes may be inferior compared with outcomes for more common and typical paracentral herniations. Patients should be informed that a lumbar discectomy is primarily indicated for leg pain. Recurrent disc herniations, which can occur in 18% of patients, remain problematic and may be more prevalent in patients who have large annular defects after discectomy. Although simple discectomy for a recurrent disc herniation can yield outcomes equivalent to the index procedure, the addition of fusion may be considered after a second recurrence. Patients should be carefully counseled preoperatively on the risk and beneits of surgery so that they may make a well-informed decision according to their speciic functional demands and expectations. Positioning a patient in a lexed or kneeling position can help open the interlaminar window to allow easier entry into the spinal canal. Regardless of the technique of discectomy, a successful operation is contingent on adequate exposure that enables careful and minimally traumatic identiication of the cauda equina, descending nerve root, and exiting nerve root before retraction to retrieve the herniated fragments. The spinal canal and disc space should be thoroughly inspected before closure to avoid retained disc fragments. Chemonucleolysis Chemonucleolysis involves the chemical digestion of nucleus material via injection of an agent, such as chymopapain, into the intervertebral disc. Ideally, the agent not only decompresses the central aspect of the disc space (producing a similar efect as percutaneous automated discectomy), but also might directly attack the herniated fragment. Chemonucleolysis has been rigorously examined in numerous clinical investigations. In a randomized prospective trial comparing chemonucleolysis and standard discectomy, Muralikuttan and colleagues98 concluded that it leads to inferior results. Crawshaw and colleagues178 found extremely high failure rates-47% to 52%-ater chemonucleolysis compared with 11% with open surgery. Salvage discectomy ater failed chemonucleolysis leads to worse results than primary surgery. This article details the 10-year follow-up results from the Maine lumbar spine study that prospectively evaluated patients with operative and nonoperative treatment for lumbar disc herniations. In this nonrandomized study, surgical treatment produced better results than nonoperative treatment, and the beneits were maximally appreciated at the 2-year mark. In this analysis, surgery resulted in better outcomes than nonoperative treatment. In this article, intention-to-treat analysis showed no statistical diferences between surgery and nonoperative treatment of lumbar disc herniations. This trial has been widely criticized for its high crossover rate between groups, however. This classic study was a randomized controlled trial of operative versus nonoperative treatment for lumbar disc herniations. It showed statistically better results with surgery at 1-year and 4-year follow-up but no diference at 10-year follow-up. This article correlates the size of a disc herniation (at least 6 mm anteroposterior dimension) with better outcomes after surgery. Factors predicting the results of surgery for lumbar intervertebral disc herniation. Elective discectomy for herniation of a lumbar disc: additional experience with an objective method. Evolution of disc degeneration in lumbar spine: a comparative histological study between herniated and postmortem retrieved disc specimens.
Cheap erythromycin 250mg mastercard
In a longitudinal follow-up of the same patients at 3 years first line antibiotics for sinus infection purchase erythromycin overnight delivery, 14% were noted to have changed type. Conversely, other studies have found better correlation between back pain and Modic changes than the correlation between back pain and discography. Of all the incidental diagnostic indings, only moderate or severe Modic changes of the vertebral end plates were found to be weakly associated with subsequent development of a disabling episode of back pain. Interestingly, psychosocial, neurophysiologic (chronic nonlumbar pain), and occupational factors strongly predicted future disabling episodes and consultations for back pain. Clinical indings in patients with radiographic evidence of disc degeneration without Modic changes were not signiicantly diferent from the baseline population. Discography Discography is another diagnostic modality for the evaluation of the integrity of the lumbar disc. Discography is the only widely available physiologic modality used to determine if a speciic disc is a pain generator. Although several attempts have been made to explain the pathogenesis of pain provocation during discography, the precise pathomechanism is not well understood. Most authors feel that to be diagnostic the pain should be concordant on low-pressure injection and a normal control disc should be pain free. Although 17% of the normal discs were found to be morphologically abnormal, there were no positive pain responses. Presumably asymptomatic discs in symptomatic individuals on pressure-controlled discography demonstrated pain levels and responses similar to the control group, whereas patients with true-positive discography demonstrated pain characteristics concordant with their usual symptoms. In contrast to reports of high false-positive rates, two recent meta-analyses of low-pressure discography reported strong evidence to support the role of discography in identifying Chapter 46 Lumbar Disc Disease 821 patients with discogenic pain. Chronic pain was not found to be a confounder, and strength of evidence was reported as level 2 in support of the diagnostic accuracy of discography. Finding a gold standard to which discography results can be compared remains a problem. Few studies have compared the use of discography and outcomes ater surgical fusion, which is perhaps the best measure for the validity of discography. Seventy-two percent of the spondylolisthesis patients met the highly efective success criteria for surgery versus only 27% of patients with discogenic pain. In an attempt to improve on the poor reliability of discography, interest has turned to functional anesthetic discograms, also called discoblocks. Regardless of the details of how discography is performed, some authors have posed the question of potential ill efects resulting from perforating the lumbar disc. Ten-year follow-up demonstrated that discs that had been punctured had a greater progression of disc degeneration (35% vs. Psychosocial factors and chronic nonlumbar pain have also been shown to alter the diagnostic capabilities of the procedure. Finally, consideration of the consistent reports of the high false-positive rates, as well as new indings of accelerated degeneration in discs that undergo discography, make it diicult to recommend the procedure for the diagnosis of discogenic back pain. Indeed, the validity of lumbar discography is very much in doubt, which is underscored by a recent practice recommendation published by the American Pain Society. All available information should be used in formulating a treatment plan to ensure a successful outcome. Sole reliance on individual clinical indings or imaging studies drastically lowers the success rate because the incidence of disc abnormality in asymptomatic patients approaches 30% to 40% and increases with advancing age. In 2009, the American Pain Society published ive practice guidelines regarding the management of chronic nonradicular back pain based on the best available evidence for the various diagnostic and treatment modalities available. Nonoperative Treatment Nonoperative treatment of lumbar disc disorders has been extensively discussed in the literature. Among the study population of 282 patients, 33% reported using bed rest, and 8% remained in bed for longer than 4 days. Behavioral factors, catastrophizing, and fear of injury were associated with use of prolonged bed rest. History of back pain and pain intensity was not associated with patient use of prolonged bed rest. A Cochrane Review244 of patient education and advice to stay active demonstrated strong evidence that individual instructional sessions of 2. Education sessions of shorter duration or written information was no more efective than no intervention. Another metaanalysis245 of 39 randomized controlled studies evaluated whether advice to stay active alone was as efective as advice in combination with other interventions such as "back school" or speciic exercise routines. Orthotics Bed Rest and Advice to Stay Active he use of bed rest and its duration has long been debated in the literature. Another common conservative management technique involves the use of lumbar supports. Moderate evidence was found that braces are no more efective than no treatment or physical training in preventing episodes of back pain. Physical Therapy A large number of physical therapy modalities and routines have been described in the literature. Adjunctive modalities include ultrasound, iontophoresis, transcutaneous electrical nerve stimulation, and heat and cold therapy. Exercise programs commonly use aerobic exercise, stretching, lexion and extension routines, core conditioning, and back stabilization protocols. Patients oten respond diferently to physical therapy so treatment programs must be tailored to the individual. Patients should also be educated on proper body biomechanics, lifestyle, and healthy living habits such as weight control, proper nutrition, stress relaxation, and cessation of smoking. Several published randomized controlled trials have supported diferent therapy routines or programs. Although a comprehensive review of all the various programs is not in the scope of this chapter, some critical updates in recent years are worthy of discussion. Recent prospective randomized trials comparing physical therapy to fusion have emphasized the importance of a multidisciplinary approach with cognitive therapy, fear-avoidance counseling, and intensive exercise programs. Intensive interdisciplinary rehabilitation with emphasis on cognitive and behavioral intervention is one of the treatment recommendations by the American Pain Society. Noninterdisciplinary or "traditional" physical therapy is also eicacious in this patient population, but no one speciic program, method, or technique is signiicantly better than another. A recent study of 3094 patients treated with physical therapy for back pain concluded that the treatment is safe but did not reach minimally efective clinical level. Functional status and kinesiophobia were improved at 3 months, but there was no diference in pain intensity and perception of recovery among the groups. A 2004 systematic Cochrane Review257 concluded there was moderate evidence suggesting that back schools in an occupational setting reduce pain and improve function and return-to-work status compared with other forms of therapy such as exercises, manipulation, myofascial therapy, advice, placebo, and waiting list controls. A European economic evaluation of a randomized controlled study258 of intensive group therapy found no signiicant cost diference between intensive group therapy and standard physiotherapy. Although low-intensity back school and programs in a work setting may have a beneit versus other forms of nonoperative treatment, most of the current literature demonstrates that back schools ofer little beneit over standard physiotherapy and cognitive therapy. Outcomes using the Roland-Morris scale and subjective assessment of symptoms demonstrated no statistically signiicant improvement in patients who underwent alternative therapies. Although less than 20% of the patients experienced overall relief of pain and diferences in outcome measures were not clinically signiicant, patients in the chiropractic group were more likely to perceive that their symptoms had improved. Other alternative medical therapies such as acupuncture, prolotherapy, and massage have also been evaluated. A Cochrane Review of acupuncture271 showed superiority to placebo sham therapy and also a short-term beneit that did not extend beyond irst follow-up when acupuncture was used in conjunction with other conventional therapies. Prolotherapy is a technique that attempts to regenerate ligamentous and tendinous structures of the spine via injections of various irritant solutions. Most practitioners use various combinations of saline, dextrose, glycerin, phenol, and lidocaine. Reports of the eicacy of prolotherapy are conlicted among many randomized trials and systematic reviews. Opioid formulations are also commonly used to treat back pain, but considering their widespread use there is a surprising paucity of high-quality randomized controlled data available on their eicacy. A Cochrane meta-analysis277 of opioid use found only four studies, three of which focused on the use of tramadol. Pooled data found that tramadol, an atypical opioid, was more efective than placebo for pain relief and showed a slight improvement in functional scores.