Cheap nifedipine 30mg fast delivery
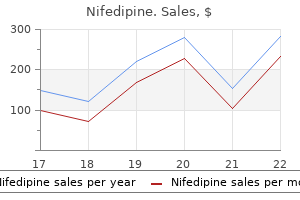
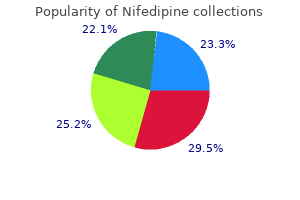
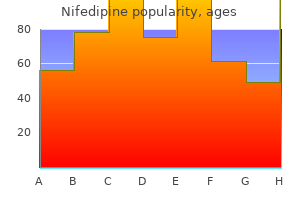
Aegeline Pennyroyal Abortifacient (squawmint oil) Hedeoma pulegoides arrhythmia multiforme safe 20 mg nifedipine, Mentha pulegium Multiple Sassafras albidum Cassia angustifolia Scutellaria Pulegone, monoterpenes Prostata Sassafras Senna Skullcap Prostatism Herbal tea Laxative Anxiolytic Uncertain Safrole Sennoside alkaloids; anthrone Diterpenoids vs. Anthraquinone Traditional Chinese Medicines Jin bu huan Ma huang Shou-wu-pian Sleep aid, analgesic Weight loss Lycopodium serratum Ephedra spp. More disturbing was the finding of undisclosed anabolic steroids in half of the body-building supplements and undisclosed potential hepatotoxins (diclofenac and tamoxifen) in other products. Jaundice was present in 78% and was the most frequent symptom that brought a patient to medical attention. The disease was characterized histologically by centrilobular hepatic congestion with occlusion of the hepatic venules, leading to congestive cirrhosis. Approximately one half of the patients with the acute form recovered spontaneously; transition to a more chronic form of injury occurred in the remainder. At one time, this form of injury accounted for one third of the cases of cirrhosis seen in Jamaica, with death often resulting from complications of portal hypertension in as few as 1 to 3 years. Associated symptoms and signs included fever, fatigue, nausea, pruritus, abdominal pain, hepatomegaly, and jaundice. Liver biopsy specimens from a small number of patients showed a range of histopathologic changes, including lobular hepatitis with prominent eosinophils, mild hepatitis with microvesicular steatosis, and fibrotic expansion of the portal tracts. The injury resolved within a mean of 8 weeks (range, 2 to 30 weeks) but could recur on rechallenge. The cause of germander hepatotoxicity is an interplay between toxic metabolites and immunoallergic mechanisms. Epoxide hydrolase on plasma membranes is a target of germander antibodies, which have been found in the sera of patients who have consumed germander teas over long periods of time. Multiple reports of hepatitis have appeared; most cases have occurred within 1 to 12 months of use and resolved within a few weeks to months of discontinuation. The suspected hepatotoxic ingredient was N-nitroso-fenfluramine, a derivative of the appetite suppressant fenfluramine, which was withdrawn from the U. Usnic acid also is a component of Kombucha tea, which has been associated with hepatic injury. Contamination of the raw material by molds has been cited as an alternative explanation for hepatotoxicity,216 although no hard evidence for aflatoxicosis was found. A majority of the patients have been women who were taking the agent for various dyspeptic complaints. Several reports of hepatocellular (and less often cholestatic) injury have been published, with a latent period ranging from 1 to several weeks, and a clinical presentation that often includes nausea, vomiting, fatigue and jaundice, and instances of severe injury and acute liver failure have appeared. Outcome of liver transplantation for drug-induced acute liver failure in the United States: analysis of the United Network for Organ Sharing database. Hepatotoxicity and mechanism of action of haloalkanes: carbon tetrachloride as a toxicological model. Jaundice after repeated exposure to halothane: a further analysis of reports to the Committee on Safety of Medicines. Mechanism, pathology, and clinical presentation of hepatotoxicity of anesthetic agents. Biotransformation of halothane, enflurane, isoflurane, and desflurane to trifluoroacetylated liver proteins: association between protein acylation and hepatic injury. Exposure assessment, biological monitoring, and liver function tests of operating room personnel exposed to halothane in Hamedan Hospitals, West of Iran. Antibodies to the surface of halothane-altered rabbit hepatocytes in patients with severe halothane-associated hepatitis. Possible association between halothane anesthesia and postoperative hepatic necrosis. Autoantibodies associated with volatile anesthetic hepatitis found in the sera of a large cohort of pediatric anesthesiologists. Absence of antitrifluoroacetate antibody after halothane anaesthesia in patients exhibiting no or mild liver damage. The morphologic spectrum of halothane-induced hepatic injury: analysis of 77 cases. Concordance between trifluoroacetic acid and hepatic protein trifluoroacetylation after disulfiram inhibition of halothane metabolism in rats. Natural killer cells mediate severe liver injury in a murine model of halothane hepatitis. Drug-induced allergic hepatitis develops in mice when myeloid-derived suppressor cells are depleted prior to halothane treatment. Repeated exposure to modern volatile anaesthetics may cause chronic hepatitis as well as acute liver injury. Fatal hepatotoxicity after re-exposure to isoflurane: a case report and review of the literature. Subcellular localization of trifluoroacetylated liver proteins in association with hepatitis following isoflurane. Comparative immunohistochemical assessment of the effect of repetitive anesthesia with isoflurane and sevoflurane on rat liver. Desflurane hepatitis associated with hapten and autoantigen-specific IgG4 antibodies. Sevoflurane hepatotoxicity: a case report of sevoflurane hepatic necrosis and review of the literature. Toxicity due to 2- and 13-wk inhalation exposures of rats and mice to N,N-dimethylformamide. Liver function alterations in synthetic leather workers exposed to dimethylformamide. Abnormal liver function associated with occupational exposure to dimethylformamide and hepatitis B virus. Dimethylacetamide-induced occupational toxic hepatitis with a short-term recurrence: a rare case report. Outcome of sixty four cases of ethylene bromide ingestion treated in a tertiary care hospital. Viral infections and chemical exposures as risk factors for hepatocellular carcinoma in Vietnam. Biochemical and molecular mechanisms of N-acetyl cysteine and silymarin-mediated protection against maneb- and paraquat-induced hepatotoxicity in rats. Ultrastructural, protein, and lipid changes in liver associated with chlordecone treatment of mice. Public health and chronic low chlordecone exposure in Guadeloupe, Part 1: hazards, exposure-response functions, and exposures. Anthropogenic sources of arsenic and copper to sediments in a suburban lake, Northern Virginia. Chronic arsenic toxicity: clinical features, epidemiology, and treatment: experience in West Bengal. Increased serum level of epidermal growth factor receptor in liver cancer patients and its association with exposure to arsenic. Chronic arsenic poisoning in the rat: Treatment with combined administration of succimers and an antioxidant. Iron poisoning: a literature-based review of epidemiology, diagnosis, and management. Pediatric liver transplantation for fulminant hepatic failure secondary to intentional iron overdose. Fatal subacute liver failure after repeated administration of sevoflurane anaesthesia. Safety of propofol in cirrhotic patients undergoing colonoscopy and endoscopic retrograde cholangiography: results of a prospective controlled study. Propofol affinity to mitochondrial membranes does not alter mitochondrial function.
Order nifedipine 30mg on-line
Although examination of liver biopsy specimens is still considered the gold standard for establishing the grade of inflammation and stage of fibrosis blood pressure medication good for pregnancy discount 30 mg nifedipine with visa, limitations of liver biopsy include (1) associated morbidity (pain occurs in as many as 30% in some series, and hemorrhage or bile leak occurs in 0. A biopsy should be done with at least a 16-gauge needle, be 15 to 20 mm or more in length, and contain at least 6 portal triads, although 11 or greater is considered optimal. The most frequently used system is transient elastography (FibroScan) to assess liver stiffness, which correlates with the amount of hepatic fibrosis. In a meta-analysis, the area under the receiver operating curve (an estimate of accuracy) of FibroScan for predicting cirrhosis was 0. Most importantly, the degree of hepatic inflammation is not assessed by these tests, and inflammation may significantly alter noninvasive test results. Moreover, although cirrhosis is accurately predicted by several noninvasive tests, the finer discrimination of the fibrosis score is not as reliable as examination of liver biopsy specimens. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Biochemical markers of liver fibrosis in patients with hepatitis C virus infection: a prospective study. Noninvasive assessment of liver fibrosis by measurement of stiffness in patients with chronic hepatitis C. Liver biopsy is not required when cirrhosis is already suggested by clinical findings. The mechanisms by which progression of fibrosis accelerates with aging are not well defined. Changes in the regenerative capacity of the liver, alterations in the immune system, and telomere shortening may play roles. A higher risk for fibrosis progression in patients older than 40 years has been described in patients with various causes of liver disease. Histologic activity and the frequency of cirrhosis are lower in African Americans than in Caucasians. All of these clinical features are nonspecific, however, and are not associated with the severity of liver injury. Studies published since the 1990s have shown remarkably different frequency rates of cirrhosis. Whereas very low rates of cirrhosis were reported in some cohorts like young women infected in the late 1970s through receipt of contaminated antiD immune globulin,155 cirrhosis has been described in up to 69% of patients in hospital-based settings. Several factors reported to influence the liver-related outcomes of chronic hepatitis C remain controversial (Table 80. Still, some of these factors may help estimate the risk of cirrhosis and identify groups of patients who require immediate antiviral treatment. Hepatic decompensation includes ascites, hepatic encephalopathy, variceal hemorrhage, hepatorenal syndrome, or hepatic synthetic dysfunction. A reduction in hepatic iron concentrations does not reduce the risk of progression of fibrosis or improve the response to antiviral treatment. Moreover, type 2 diabetes mellitus has been identified as an important independent risk factor. A morphometric and immunohistochemical study to assess the benefit of a sustained virological response in hepatitis C virus patients with cirrhosis. Different domains in the polymerase protein can be targeted by non-nucleoside polymerase inhibitors, and theoretically, use of a combination of different non-nucleoside polymerase inhibitors is possible. Importantly, there is also no cross-resistance between drugs targeting different polymerase domains. Sofosbuvir is predominantly excreted renally (80%), mostly as an active metabolite. No dose adjustment is required with severe hepatic impairment, thereby allowing sofosbuvir to be administered in patients with decompensated cirrhosis. Although sofosbuvir is not metabolized extensively by the liver, it is transported by P glycoprotein (P-gp); therefore, sofosbuvir should not be co-administered with strong inducers of P-gp, such as rifampin, carbamazepine, phenytoin, or St. If resistance is present, the duration of therapy should be extended (see text) or an alternative regimen should be considered. In contrast to sofosbuvir, ledipasvir is metabolized predominantly in the liver and excreted unchanged in bile. However, ledipasvir can be given safely to patients with severe hepatic impairment with no significant effect on plasma ledipasvir levels or pharmacokinetics. Sofosbuvir/ledipasvir can be administered with antiretrovirals with the exception of tenofovir and ritonavir/cobicistat-containing regimens due to an increase in tenofovir levels, which require monitoring. Grazoprevir exposure is increased greatly with severe hepatic impairment, and therefore, like all protease inhibitors, the drug is contraindicated in patients with Child-Pugh class B or C cirrhosis. Velpatasvir can be administered to patients with severe hepatic impairment without alterations in velpatasvir plasma concentration or pharmacokinetics. As with all protease inhibitors, voxilaprevir exposure is significantly higher with moderate and severe hepatic impairment, and therefore, the drug is not recommended in patients with Child-Pugh class B cirrhosis and contraindicated in those with Child-Pugh class C cirrhosis. Rosuvastatin, in particular, is contraindicated because co-administration was associated with 19fold higher plasma levels of rosuvastatin. Because of significantly higher glecaprevir exposure in patients with moderate and severe hepatic impairment, this combination is contraindicated in those with Child-Pugh class B and C cirrhosis. Therefore, delayed therapy is effective, but early treatment has advantages because fewer patients are lost to follow up. Real-world clinical experience has confirmed the similar efficacy rates of 8 and 12 weeks of sofosbuvir/ledipasvir for this group of patients. Real-world clinical experience has subsequently demonstrated similar efficacy rates for 8 and 12 weeks of sofosbuvir/ledipasvir. Therefore, 12 weeks of glecaprevir/ pibrentasvir is recommended in compensated cirrhotic patients. Therefore, based on these limited data, 12 weeks of glecaprevir/pibrentasvir is recommended for patients who have failed sofosbuvir-containing treatment regimens. The majority of patients had previously received ledipasvir (51%) or daclatasvir (27%). Efficacy was similar among noncirrhotic (99%) and compensated cirrhotic (100%) patients. Hemolytic anemia is reversible and usually resolves within the first month after therapy is stopped. Regimens that are not recommended or contraindicated in decompensated cirrhotics are the paritaprevir-, simeprevir-, grazoprevir-, and glecaprevir-based regimens. Ideally, patients should be on stable immunosuppressive regimens at the time antiviral therapy is initiated. At least 25% of patients will develop cirrhosis within 5 to 10 years after transplantation. Treatment for 24 weeks is recommended in patients with prior treatment experience. Treatment was well tolerated, but immunosuppression was required to be changed in 23% of patients. If this is not possible, then treatment should be initiated in the postpartum period. Global prevalence and genotype distribution of hepatitis C virus infection in 2015: a modeling study. Hepatitis C disease burden in the United States in the era of oral direct-acting antivirals. Rising mortality associated with hepatitis C virus in the United States, 2003-2013. Association between sustained virological response and all-cause mortality among patients with chronic hepatitis C and advanced hepatic fibrosis. Earlier sustained virologic response end points for regulatory approval and dose selection of hepatitis C therapies. Concordance of sustained virologic response 4, 12 and 24 weeks post-treatment with sofosbuvircontaining regimens for hepatitis C virus. Concordance of sustained virologic response at weeks 4, 12 and 24 post-treatment of hepatitis C virus in the era of new direct-acting antivirals: a concise review. Late relapse versus hepatitis C virus reinfection in patients with sustained virologic response after sofosbuvir-based therapies. Cryo-electron microscopy and three-dimensional reconstructions of hepatitis C virus particles. New advances in the molecular biology of hepatitis C virus infection: towards the identification of new treatment targets.
Diseases
- Genu varum
- Hemifacial microsomia
- Ethylmalonic aciduria
- Congenital vagal hyperreflexivity
- Orofaciodigital syndrome type1
- Diffuse idiopathic skeletal hyperostosis
- Webster Deming syndrome
- Levic Stefanovic Nikolic syndrome
Buy cheap nifedipine 20mg on line
Strict precautions including use of gowns and gloves and regular hand washing after patient contact should be observed arteria carotida externa cheap nifedipine online american express. Outbreaks of infection are seen with the emergence of virulent strains, which are highly toxinogenic and resistant to numerous antibiotics including fluoroquinolones. The protective barrier provided by the normal intestinal microbiota is often referred to as colonization resistance; its impairment by antibiotics and subsequent infection with C. Absence of toxin receptor expression on the immature colonic epithelium has been suggested as a mechanism to explain the symptomless carrier state in infants and children. The tcdC gene is transcribed in the opposite direction to tcdA, tcdB, and tcdD, and its gene product appears to decrease toxin production. Following internalization into the host cell cytoplasm, the toxins catalyze the transfer and covalent attachment of a glucose residue from uridine diphosphate glucose to a conserved threonine amino acid on small (20 to 25 kd) guanosine triphosphate-binding rho proteins. Rho proteins are part of the Ras superfamily, are expressed in all eukaryotic cells, and act as intracellular signaling molecules to regulate cytoskeletal organization and gene expression. The rho proteins, RhoA, Rac, and Cdc42, are substrates for both toxins A and B, whereas Rap is a substrate for toxin A only. Toxin A initially was thought to be the only enterotoxin based on studies in animals,69,71,72 whereas toxin B, an extremely potent cytotoxin, appeared to have little independent enterotoxic activity in animals. TcdD (also called TcdR) appears to encode a positive regulator of toxin A and toxin B transcription. TcdE may mediate toxin release through its ability to form pores in the bacterial cytoplasmic membrane. Although binary toxin shows some enterotoxic activity in animal models, its role in the pathogenesis of C. Age was a major risk factor for infection, with rates of 1089 per 1,000,000 population in those aged 85 or older compared with 486 per 1,000,000 for those 65 to 84 years of age, 101 per 1,000,000 for those 45 to 64 years of age, and 28 per 1,000,000 for those 18 to 44 years of age. These factors are often markers of disease severity, older age, or both, and the significance of their association with C. Interaction of the toxin B binding domain (green) with cellsurface receptors (dark blue) induces receptor-mediated endocytosis. The acidic pH of the endosome triggers the first conformational change and results in pore formation by the hydrophobic, translocation domain (red oval). Within the cytosol, a second conformational change activates intrinsic protease activity (pink). Autocatalytic cleavage of toxin B releases the catalytic glucosyltransferase domain (light blue) into the cytosol. A correlation was observed between the IgG response to toxin A and the clinical outcome of infection. By contrast, no significant increase was found in serum IgG antitoxin A of patients who experienced recurrent C. In those who had a single episode of diarrhea, IgG antitoxin A levels were generally increased on day 12 of their first episode. Marked thickening of the colonic wall in the sigmoid colon and an accordion-like pattern, produced by a series of broad edematous colonic haustral folds, are evident (arrows). Several large epidemiologic studies indicate that 10% to 21% of hospital inpatients receiving antibiotics in high-risk units are carriers. The incubation period is usually less than a week, with a median time of onset of approximately 2 days. Abdominal plain films might reveal a dilated colon, toxic megacolon, or small bowel ileus with air-fluid levels mimicking intestinal obstruction or ischemia. Flexible sigmoidoscopy or colonoscopy is sometimes indicated to identify pseudomembranous colitis when the diagnosis remains unclear after initial evaluation (see later). Laboratories should choose a toxin test with sensitivity in the upper range of sensitivity. Anaerobic storage or the use of transport media, such as Cary Blair medium, is not necessary. The tissue culture cytotoxicity assay also is sensitive and has high diagnostic accuracy, but it is Whom Not to Test Anaerobic culture followed by determination of toxin production is both sensitive and specific; however, it requires specialized resources and expertise, and results take several days to obtain, leading to it being used in epidemiology studies but seldom in clinical practice. Despite its high sensitivity (67% to 100%) and specificity (85% to 100%), the test is currently seldom used because it requires 48 to 72 hours for completion, is expensive, and requires a tissue culture facility. Therefore, cultured isolates must be tested in vitro for toxin production to improve test specificity, but this is costly and time consuming. Sigmoidoscopy may be normal in patients with mild diarrhea or might demonstrate nonspecific colitis in moderate cases. Pseudomembranes appear as yellow, gray, or white plaques 2 to 5mm in diameter, and in some areas they can coalesce to cover large portions of the mucosal surface. Sigmoidoscopy might not be sufficient to identify all patients with pseudomembranous colitis, because 15% to 20% only have pseudomembranes in the more proximal areas of the colon. In mild disease, colonic mucosal biopsies may be normal or demonstrate only mild and nonspecific acute inflammatory changes with neutrophil infiltration. Patients with protein-losing colopathy and severe hypoalbuminemia can develop peripheral edema, ascites, or anasarca. Antimotility agents such as diphenoxylate plus atropine (Lomotil), loperamide (Imodium), or narcotics often are avoided because of concern for impaired toxin clearance or precipitation of ileus and toxic dilatation, albeit the evidence supporting these concerns is limited and contradictory. Many antimicrobial agents, such as ampicillin or amoxicillin, which have in vitro activity against C. Characteristic raised adherent yellow plaques that vary in size from 2-5mm are visible on the colonic mucosa. There is some erythema of the colonic mucosa between the pseudomembranes, but the epithelium is intact. Focal ulceration of the colonic mucosa is evident (lower arrow), with exudation of a pseudomembrane made up of inflammatory cells, fibrin, and necrotic debris (upper arrow). Bacitracin, teicoplanin, nitazoxanide, rifaximin, and fusidic acid also have been used to treat acute infection but have few, if any, advantages over metronidazole, vancomycin, or fidaxomicin. The advantages and disadvantages of specific therapeutic agents are discussed in the sections that follow. When given orally, vancomycin is neither absorbed nor metabolized significantly and, as a result, high concentrations are achieved in the colonic lumen. Because oral vancomycin is not absorbed appreciably, systemic side effects are rare. The lower dose is recommended for most patients; the higher dose is only recommended for patients with fulminant disease (see later). It is a novel macrocyclic antibiotic, is active in vitro against clinical isolates of C. Several clinical studies before 2000 indicated that metronidazole therapy resulted in resolution of diarrhea and colitis in more than 95% of patients treated. In mild disease, both treatments yielded similar response rates (90% and 98%; P = 0. Metronidazole, unlike vancomycin, is well absorbed in the upper intestine following oral administration. Fecal concentrations are low or absent in healthy persons or asymptomatic carriers of C. Metronidazole also can potentiate the action of warfarin, resulting in prolongation of the prothrombin time. Enigmatically, metronidazole has been identified as the antibiotic agent responsible for causing some cases of C. Response rates after 10 days of therapy were 17 of 22 for nitazoxanide and 20 of 27 for vancomycin (77% vs. In a phase 2 human clinical trial, results with tolevamer were similar to those of vancomycin when used as primary treatment for mild or moderately severe infection. Surgery Surgery is sometimes required in patients with severe colitis not responding to medical therapy, and a surgical consultation should be sought early in patients with severe or fulminant disease. Hence, colon perforation or toxic megacolon are not the sole indicators of a need for surgical intervention. In one study, colectomy appeared to be more beneficial in patients who were not immunosuppressed, were 65 years of age or older, had a leukocytosis of 20,000 cells/mm3, or a lactate between 2. One study reported a different surgical approach whereby a loop ileostomy was fashioned at laparoscopy, and intraoperative colonic lavage was then performed with 8 L of warmed polyethylene glycol colon preparation solution.
Buy nifedipine 20 mg with amex
Maintenance infliximab therapy was similarly beneficial hypertension portal purchase nifedipine 30 mg without a prescription, achieving complete absence of draining fistulas in 36% of patients receiving infliximab compared with 19% receiving placebo. Most abscesses occur adjacent to a diseased segment of the bowel or anastomosis, and are sometimes associated with stenosis and fistulas. Common presenting symptoms are abdominal pain, fever tenderness, and leukocytosis. Traditionally, treatment of intraabdominal abscesses has been surgical drainage followed by resection of the diseased segment; increasingly, however, percutaneous drainage and systemic antibiotics are associated with similar outcomes and avoid the need for surgery in some patients. The scrotum, perianal skin, and buttocks are discolored and hardened by healed fistulas and abscesses. Several studies have examined the efficacy of local injections of various substances into fistula tracts to achieve healing with mixed success. One promising approach appears to be injection of allogenic, adipose-derived stem cells. At week 24, 50% of patients receiving stem cell injections achieved combined clinical and radiologic remission compared with 34% of patients receiving placebo (P = 0. Although some strictures may be asymptomatic, they usually present with abdominal pain or distension with cessation of bowel movements and vomiting in the setting of complete or near complete bowel obstruction. However, nearly 74% of patients required at least 1 more dilation and just under half (43%) underwent surgery. Escalation of medical therapy may be effective in patients who have ongoing inflammation at the site of the stricture. A small study of 18 patients with symptomatic short intestinal strictures (<5 cm) reported complete response in 10 patients with infliximab. Because carcinoma might not be detected on mucosal biopsies, surgical resection of the stricture is advised, particularly in patients with long-standing disease. Loss of contractility from the inflammatory reaction leads to the accumulation of gas and fluid within the lumen and subsequent colonic dilatation. Precipitating factors for toxic megacolon have been reported to include electrolyte imbalance (particularly hypokalemia), use of antimotility drugs including anticholinergic agents and narcotics. Often a very limited insertion will suffice to gauge the mucosal appearance and, if necessary, to allow a biopsy to be done. Medical management for toxic megacolon is directed at treating the underlying inflammation, restoring colonic motility, and preventing free colonic perforation. The transverse colon is dilated (arrow), the colon wall is thickened, and mucosal islands are visible. A, Low-grade dysplasia is characterized by nuclear enlargement, crowding, and hyperchromasia in the colonic epithelial cells. Nuclei are stratified to the surface, and there is a marked increase in nuclear pleomorphism. Branching of the glands in a cribriform pattern and scattered cell necrosis are shown. In general, patients who do not improve after 48 to 72 hours of medical therapy should undergo surgery. Patients with progressive abdominal distention, development of rebound tenderness, or hemodynamic instability should undergo immediate colectomy. Dysplasia, which is unequivocally neoplastic epithelium, is classified both histologically and endoscopically. For these reasons, the diagnosis and grading of dysplasia by pathologists is inherently subjective, which gives rise to very low rates of interobserver agreement. Invisible dysplasia is almost always characterized by flat lesions, whereas visible dysplasia can manifest in a variety of forms, including raised lesions, such as polypoid lesions or masses; flat lesions such as plaques, irregular mucosa, ulcers, or inverted lesions; or strictures. Today, however, the most important issue regarding visible dysplasia is whether the lesion can be removed in its entirety endoscopically, irrespective of location (colitic vs. Traditionally, white light colonoscopy with surveillance biopsies every 10 cm (for a total of at least 32 biopsies) was the standard of care, in addition to targeted biopsies from any raised or potentially dysplastic lesions. Recently, dye spray chromoendoscopy, consisting of applying methylene blue or indigo carmine stains to the mucosal surface has gained popularity and is recommended as the surveillance modality of choice, especially if using standard definition colonoscopies. Challenges with routine adoption of chromoendoscopy include need for operator and supporting staff familiarity with the procedure, longer procedure time, and lack of long-term data on the natural history of chromoendoscopically detected lesions. Recent clinical trials comparing chromoendoscopy to high-definition white light endoscopy have not demonstrated a benefit to the dye-spray technique. In a randomized non-inferiority trial of 270 patients among whom 90 underwent dye-spray examination and 90 high-definition white light, there was no difference in the neoplasia detection rate between both arms of the study. Manifestations that parallel disease activity usually improve upon successful treatment of the colitis. It classically manifests as single or multiple tender, raised, erythematous nodules on the extensor surfaces of the lower extremities. If possible, the diagnosis should be made clinically without biopsy, because biopsy is associated with increased tendency to form scars. The classic lesion begins as a group of erythematous pustules or nodules that break down, ulcerate, and coalesce into a larger, tender, burrowing ulcer with irregular, violaceous edges. Most cases usually respond to intralesional glucocorticoid injections, mesalamine, glucocorticoids, or tacrolimus, or topical therapy with cromolyn sodium. The latter involves oral mucosa and skin, presenting as pustular dermatitis along with colonic involvement. These lesions usually occur with flares of intestinal inflammation and resolve on control of the bowel disease. Angular stomatitis and a sore tongue may be seen in patients with deficiencies of iron, B vitamins, or other micronutrients. Episcleritis is characterized by painless hyperemia of the sclera and conjunctiva without loss of vision. It typically parallels the activity of bowel disease and usually responds to anti-inflammatory therapy. In contrast, uveitis presents as an acute or subacute painful eye with visual blurring, often accompanied by photophobia and headache. Temporal correlation of uveitis with the activity of the colitis is less predictable than with episcleritis. Patients with uveitis should receive emergent ophthalmologic consultation and treatment with local glucocorticoid ocular drops to prevent progression to blindness. Thus, patients receiving glucocorticoid therapy should be advised to undergo annual ophthalmologic examination. These include hypersensitivity, photosensitivity, and urticarial rashes related to sulfasalazine and less commonly to mesalamine. Patients receiving glucocorticoids often develop acne, which can be distressing cosmetically. There are reports of palmarplantar pustulosis in patients treated with vedolizumab and ustekinumab and with rapid resolution of the eruption if the drug was stopped. The addition of bisphosphonates should be considered for worsening osteopenia or osteoporosis. It is a chronic inflammatory disease of the biliary tree resulting in fibrosis and, eventually, cirrhosis and hepatic failure. The histologic appearance can be variable, however, ranging from chronic inflammatory infiltration in the portal tracts to cirrhosis. A recent study identified more severe histologic inflammation in the proximal colon than in the distal colon, suggesting that this may be the reason for fewer symptoms and the proximal location of neoplasia in these patients. Patients with a dominant extrahepatic biliary stricture can benefit from endoscopic dilatation or stent placement. It usually manifests with acute, selflimited episodes that parallel the underlying bowel disease activity. Type 2 arthropathy is symmetrical and polyarticular, affecting atleast5 joints and typically involving the small joints. This type manifests with persistent symptoms independent of the intestinal inflammatory activity. Rest, physical therapy, intra-articular glucocorticoid injection, and therapeutic arthrocentesis also can help control symptoms. Treatment of axial arthropathy is similar to that for peripheral arthropathy, except that control of the underlying colitis does not alter the progressive nature of ankylosing spondylitis. Renal artery thrombosis, cerebrovascular accidents, coronary artery thrombosis, and venous thrombosis of mesenteric, portal, and hepatic vessels all have been reported. Patients with these complications should be treated with anticoagulants, just as in other patient populations.
Discount nifedipine 20 mg with mastercard
Changing hepatitis D virus epidemiology in a hepatitis B virus endemic area with a national vaccination program blood pressure chart vaughns 1 pagers com order nifedipine no prescription. Prevalence of hepatitis delta infection in the United States: National Health and Nutrition Examination Survey, 1999-2012. Prevalence of hepatitis B and hepatitis D virus infections in the United States, 2011-2016. Delta hepatitis within the Veterans Affairs medical system in the United States: prevalence, risk factors, and outcomes. Prevalence, correlates, and viral dynamics of hepatitis delta among injection drug users. Prevalence of hepatitis D virus infection in sub-Saharan Africa: a systematic review and meta-analysis. Evidence of transmission of hepatitis D virus to spouses from sequence analysis of the viral genome. Sexual practices in the transmission of hepatitis B virus and prevalence of hepatitis delta virus infection in female prostitutes in the United States. Risk factors for hepatitis B in an outbreak of hepatitis B and D among injection drug users. Entry of hepatitis B and hepatitis D virus into hepatocytes: basic insights and clinical implications. Isoprenylation mediates direct protein-protein interactions between hepatitis large delta antigen and hepatitis B virus surface antigen. Isoprenylation masks a conformational epitope and enhances trans-dominant inhibitory function of the large hepatitis delta antigen. Role of the large hepatitis B virus envelope protein in infectivity of the hepatitis delta virion. The middle hepatitis B virus envelope protein is not necessary for infectivity of hepatitis delta virus. Hepatitis delta virus persists during liver regeneration and is amplified through cell division both in vitro and in vivo. Molecular phylogenetic analyses indicate a wide and ancient radiation of African hepatitis delta virus, suggesting a deltavirus genus of at least seven major clades. Genetic diversity and worldwide distribution of the deltavirus genus: a study of 2,152 clinical strains. Genotypes and viremia of hepatitis B and D viruses are associated with outcomes of chronic hepatitis D patients. Genotyping of hepatitis D virus by restriction-fragment length polymorphism and relation to outcome of hepatitis D. Co-treatment with pegylated interferon alfa-2a and entecavir for hepatitis D: a randomized trial. Superimposed hepatitis and the effect on viral replication in chronic hepatitis B. Epidemiologic patterns of infection with the hepatitis B virus-associated delta agent in Italy. An outbreak of delta agent among a group of drug addicts and their close contacts. Chronic delta hepatitis: is the prognosis worse when associated with hepatitis C virus and human immunodeficiency virus infections Clinical outcome of acute and chronic hepatitis delta over time: a long-term follow-up study. Influence of hepatitis delta virus infection on progression to cirrhosis in chronic hepatitis type B. Influence of hepatitis delta virus infection on morbidity and mortality in compensated cirrhosis type B. A population-based study of hepatitis D virus as potential risk factor for hepatocellular carcinoma. A randomized controlled trial of a 12-month course of recombinant human interferonalpha in chronic delta (type D) hepatitis: a multicenter Italian study. Long-term benefit of interferon alpha therapy of chronic hepatitis D: regression of advanced hepatic fibrosis. Treatment of hepatitis delta virus genotype 3 infection with peg-interferon and entecavir. Pathologic and ultrastructural changes of acute and chronic delta hepatitis in an experimentally infected chimpanzee. Immunohistochemical localization of the delta antigen associated with hepatitis B virus in liver biopsy sections embedded in Araldite. Natural history of hepatitis D viral superinfection: significance of viremia detected by polymerase chain reaction. Serum immunoglobulin M antibody to hepatitis D as a surrogate marker of hepatitis D in interferon-treated patients and in patients who underwent liver transplantation. Diagnostic and prognostic significance of the IgM antibody to the hepatitis delta virus. A novel quantitative microarray antibody capture assay identifies an extremely high hepatitis delta virus prevalence among hepatitis B virus-infected mongolians. Pegylated interferon alpha-2b as monotherapy or in combination with ribavirin in chronic hepatitis delta. Treatment of chronic hepatitis D patients with pegylated interferon: a real-world experience. Long-term clinical and virological outcome after liver transplantation for cirrhosis caused by chronic delta hepatitis. A prenylation inhibitor prevents production of infectious hepatitis delta virus particles. In vivo antiviral efficacy of prenylation inhibitors against hepatitis delta virus. Oral prenylation inhibition with lonafarnib in chronic hepatitis D infection: a proof-of-concept randomised, double-blind, placebo-controlled phase 2A trial. Nucleic acid polymers are active against hepatitis delta virus infection in vitro. Phylogenetic analysis of strains of this genus reveals 8 distinct genotypes, 4 of which (genotypes 1 to 4; Table 82. Genotype 1 includes isolates from Asia and Africa, and genotype 2 includes one strain from Mexico and some isolates from western Africa; both of these genotypes are restricted to humans and have been associated with waterborne disease outbreaks. In addition, the infection has also been shown to be associated with chronic liver disease and several extrahepatic manifestations. The Hepeviridae family consists of 2 genera: Piscihepevirus, whose members infect fish, and Orthohepevirus, whose members infect mammals and birds. The outbreaks can be large, causing several hundred to several thousand cases, with overall population incidence rates ranging from 1% to 15%-higher in adults (3% to 30%) than in children (0. Characteristically, the rates of disease and mortality are high in pregnant women. The epidemics vary from single-peaked, short-lived outbreaks to prolonged, multipeaked epidemics lasting more than one year. Waterborne transmission Animal reservoir Well known to occur; most common route No are demographically and clinically similar to those observed during outbreaks. In most outbreaks, epidemiologic investigations have shown an association of disease occurrence with consumption of fecally contaminated drinking water (Box 82. The outbreaks frequently follow heavy rains and floods, but some are related to decreased flow in rivers during summers, with a consequent increase in the concentration of water contaminants. The number of cases appear to peak in the spring and summer, and the disease appears to be more common in residents of coastal and estuarine areas. Case series with similar characteristics have been described from other parts of Europe and, less frequently, North America. The available evidence strongly suggests that most such cases are related to zoonotic transmission from pigs (or other animals). Such transmission appears to occur through consumption of undercooked animal meat, close contact with infected animals, or contamination of water supplies from animal feces. These findings may represent an epidemiologic transition from a high-endemicity pattern to a lowendemicity pattern. Viremia and fecal shedding of the virus last until about 2 and 4 weeks, respectively, after the onset of illness.
Syndromes
- Paralysis
- Fainting or feeling light-headed
- Ringing sounds
- Acute unilateral obstructive uropathy
- Abnormal heartbeat
- Elective abortion is done because a woman chooses (elects) to end the pregnancy.
- Did it start after a viral illness, such as a cold?
- Itching of the mouth, throat, eyes, skin, or any other area
- Syphilis
- AIDS
Cheap nifedipine 20mg mastercard
The opiate receptor antagonist naloxone has shown a clear benefit in a double-blind trial paediatric blood pressure chart uk purchase discount nifedipine line. The serotonin reuptake inhibitor sertraline (75 to 100 mg orally) was associated with relief of pruritus as assessed by a visual analog scale and healing of excoriations. Tacrolimus-based immunosuppression has been the most consistently identified risk factor for disease recurrence. The most important cause is decreased bile acid delivery with insufficient micellar concentration of bile acids in the small intestine. Because each of these causes has specific and different treatments, determining the exact cause of steatorrhea is important. Patients with decreased intestinal bile acid concentrations usually benefit from substitution of medium-chain triglycerides for long-chain triglycerides in their diets and a decrease in total fat intake. Patients with exocrine pancreatic insufficiency will benefit from pancreatic replacement therapy; patients with celiac disease require gluten withdrawal from the diet; and patients with small intestinal bacterial overgrowth should receive intermittent broad-spectrum oral antibiotic therapy. Milder disease stage in patients with primary biliary cholangitis over a 44-year period: a changing natural history. Epidemiology and natural history of primary biliary cholangitis in the Chinese: a territory-based study in Hong Kong between 2000 and 2015. The epidemiology and natural history of primary biliary cirrhosis: a nationwide population-based study. Rising incidence and prevalence of primary biliary cirrhosis: a large population-based study. Increasing prevalence of primary biliary cholangitis and reduced mortality with treatment. Factors associated with prevalence and treatment of primary biliary cholangitis in United States health systems. Expression of adhesion molecules on mature cholangiocytes in canal of Hering and bile ductules in wedge biopsy samples of primary biliary cirrhosis. The Western immunoblotting pattern of anti-mitochondrial antibodies is independent of the clinical expression of primary biliary cirrhosis. Characterization and clinical impact of antinuclear antibodies in primary biliary cirrhosis. Antinuclear antibodies giving the "multiple nuclear dots" or the "rim-like/membranous" patterns: diagnostic accuracy for primary biliary cirrhosis. Profile and clinical significance of anti-nuclear envelope antibodies found in patients with primary biliary cirrhosis: a multicenter study. Epigenetics in the primary biliary cholangitis and primary sclerosing cholangitis. Biliary apotopes and antimitochondrial antibodies activate innate immune responses in primary biliary cirrhosis. Bile salt-phospholipid conjugate ursodeoxycholyl lysophosphatidylethanolamide as a hepatoprotective agent. Identification of 2-nonynoic acid, a cosmetic component, as a potential trigger of primary biliary cirrhosis. Chemical xenobiotics and mitochondrial autoantigens in primary biliary cirrhosis: identification of antibodies against a common environmental, cosmetic, and food additive, 2-octynoic acid. Autoreactive monoclonal antibodies from patients with primary biliary cholangitis recognize environmental xenobiotics. Smoking as an independent risk factor of liver fibrosis in primary biliary cirrhosis. Large-scale characterization study of patients with antimitochondrial antibodies but nonestablished primary biliary cholangitis. The specificity of fatigue in primary biliary cirrhosis: evaluation of a large clinic practice. Fatigue measurements in patients with primary biliary cirrhosis and the risk of mortality during follow-up. Survival and symptom progression in a geographically based cohort of patients with primary biliary cirrhosis: follow-up for up to 28 years. Early primary biliary cirrhosis: biochemical response to treatment and prediction of longterm outcome. Fenofibrate is effective adjunctive therapy in the treatment of primary biliary cirrhosis: a meta-analysis. Systematic review and meta-analysis: bezafibrate in patients with primary biliary cirrhosis [Erratum]. A prospective randomized controlled study of long-term combination therapy using ursodeoxycholic acid and bezafibrate in patients with primary biliary cirrhosis and dyslipidemia. Effects of bezafibrate on outcome and pruritus in primary biliary cholangitis with suboptimal ursodeoxycholic acid response. A pilot, doubleblind, controlled 1-year trial of prednisolone treatment in primary biliary cirrhosis: hepatic improvement but greater bone loss. Oral budesonide in the treatment of patients with primary biliary cirrhosis with a suboptimal response to ursodeoxycholic acid. Colchicine for primary biliary cirrhosis: a Cochrane Hepato-Biliary Group systematic review of randomized clinical trials. Bone disease in patients with primary biliary cirrhosis: independent predictors and rate of progression. Low bone mass and severity of cholestasis affect fracture risk in patients with primary biliary cirrhosis. Parenteral bisphosphonates for osteoporosis in patients with primary biliary cirrhosis. The potent bile acid sequestrant colesevelam is not effective in cholestatic pruritus: results of a double-blind, randomized, placebo-controlled trial. Noninvasive elastography-based assessment of liver fibrosis progression and prognosis in primary biliary cirrhosis. Performance and utility of transient elastography and noninvasive markers of liver fibrosis in primary biliary cirrhosis. Asymptomatic primary biliary cirrhosis: clinical features, prognosis, and symptom progression in a large population based cohort. Development and validation of a scoring system to predict outcomes of patients with primary biliary cirrhosis receiving ursodeoxycholic acid therapy. Antimitochondrial antibody-negative primary biliary cirrhosis: a subset of primary biliary cirrhosis. The long-term effect of ursodeoxycholic acid on laboratory liver parameters in biochemically non-advanced primary biliary cirrhosis. Long-term effects of ursodeoxycholic acid in primary biliary cirrhosis: results of a double-blind controlled multicentric trial. Combined analysis of the effect of treatment with ursodeoxycholic acid on histologic progression in primary biliary cirrhosis. Ursodeoxycholic acid delays the onset of esophageal varices in primary biliary cirrhosis. Primary biliary cirrhosis: incidence and predictive factors of cirrhosis development in ursodiol-treated patients. Influence of ursodeoxycholic acid on the mortality and malignancy associated with primary biliary cirrhosis: a population-based cohort study. Excellent long-term survival in patients with primary biliary cirrhosis and biochemical response to ursodeoxycholic acid. Stratification of hepatocellular carcinoma risk in primary biliary cirrhosis: a multicentre international study. Sex and age are determinants of the clinical phenotype of primary biliary cirrhosis and response to ursodeoxycholic acid. Biochemical response to ursodeoxycholic acid and long-term prognosis in primary biliary cirrhosis. American Association for the Study of Liver Diseases endpoints conference: design and endpoints for clinical trials in primary biliary cirrhosis. Early biochemical response to ursodeoxycholic acid and long-term prognosis of primary biliary 73.
Discount nifedipine 30 mg line
Essential nutrients for bone health and a review of their availability in the average North American diet heart attack in men order 20mg nifedipine free shipping. Evaluation, treatment, and prevention of vitamin D deficiency: an endocrine society clinical practice guideline. Vitamin D3 intestinal absorption in vivo: influence of fatty acids, bile salts, and perfusate pH on absorption. Vitamin D-binding protein influences total circulating levels of 1,25-dihydroxyvitamin D3 but does not directly modulate the bioactive levels of the hormone in vivo. Inactivating mutations in the 25-hydroxyvitamin D3 1alpha-hydroxylase gene in patients with pseudovitamin D-deficiency rickets. Enhancing vitamin E in oilseeds: unraveling tocopherol and tocotrienol biosynthesis. The pecking order of free radicals and antioxidants: lipid peroxidation, alpha-tocopherol, and ascorbate. Effects of tocotrienol-rich fraction on exercise endurance capacity and oxidative stress in forced swimming rats. Nitrofurantoin-induced hepatic and pulmonary biochemical changes in mice fed different vitamin E doses. Tocotrienols, the vitamin E of the 21st century: its potential against cancer and other chronic diseases. Isoforms of vitamin E have opposing immunoregulatory functions during inflammation by regulating leukocyte recruitment. Guidelines for the diagnosis and management of chylomicron retention disease based on a review of the literature and the experience of two centers. Neurologic complications of bariatric surgery: involvement of central, peripheral, and enteric nervous systems. Human vitamin E requirements assessed with the use of apples fortified with deuterium-labeled alpha-tocopheryl acetate. Cellular and paracellular magnesium transport across the terminal ileum of the rat and its interaction with the calcium transport. Fe-saturation and proteolysis of human lactoferrin: effect on brush-border receptor-mediated uptake of Fe and Mn. Role of redox systems on Fe3+ uptake by transformed human intestinal epithelial (Caco-2) cells. Effect of acute zinc depletion on zinc homeostasis and plasma zinc kinetics in men. Homeostatic regulation of zinc absorption and endogenous losses in zinc-deprived men. Differences in the plasma transport and tissue concentrations of tocopherols and tocotrienols: observations in humans and hamsters. Studies in humans using deuterium-labeled alpha- and gamma-tocopherols demonstrate faster plasma gamma-tocopherol disappearance and greater gammametabolite production. Vitamin K oxygenation, glutamate carboxylation, and processivity: defining the three critical facets of catalysis by the vitamin K-dependent carboxylase. Vitamin E decreases extra-hepatic menaquinone-4 concentrations in rats fed Menadione or phylloquinone. Vitamin K nutrition, metabolism, and requirements: current concepts and future research. Vitamin K2 colonic and ileal in vivo absorption: bile, fatty acids, and pH effects on transport. Effect of age and the milk sugar lactose on calcium absorption by the small intestine. Effect of 1,25-dihydroxyvitamin D3 on calcium and magnesium absorption in the healthy human jejunum and ileum. Molecular mechanisms for regulation of intestinal calcium absorption by vitamin D and other factors. Segmental heterogeneity of cellular and paracellular calcium transport across the rat duodenum and jejunum. Molecular cloning and characterization of a channel-like transporter mediating intestinal calcium absorption. Studies of zinc transport into brush border membrane vesicles isolated from pig small intestine. The effect of pregnancy and lactation on the absorption of zinc and lysine by the rat duodenum in situ. Metallothionein knockout and transgenic mice exhibit altered intestinal processing of zinc with uniform zinc-dependent zinc transporter-1 expression. Interleukin-6 regulates the zinc transporter Zip14 in liver and contributes to the hypozincemia of the acute-phase response. Copper absorption and copper balance during consecutive periods for rats fed varying levels of dietary copper. Copper absorption and retention in pregnant women fed diets based on animal and plant proteins. Copper absorption and retention in young men at three levels of dietary copper by use of the stable isotope 65Cu. Copper absorption, excretion, and retention by young men consuming low dietary copper determined by using the stable isotope 65Cu. Functional and molecular responses of suckling rat pups and human intestinal Caco-2 cells to copper treatment. Isolation of a candidate gene for Menkes disease that encodes a potential heavy metal binding protein. Selenium concentrations and glutathione peroxidase activities in whole blood of New Zealand residents. Dietary iodide controls its own absorption through posttranscriptional regulation of the intestinal Na+/I- symporter. Benfotiamine blocks three major pathways of hyperglycemic damage and prevents experimental diabetic retinopathy. Impaired intestinal vitamin B1 (thiamin) uptake in thiamin transporter-2-deficient mice. Thiamin-responsive megaloblastic anemia syndrome: a disorder of high-affinity thiamin transport. Identification of a mouse thiamin transporter gene as a direct transcriptional target for p53. Multifaceted role of tocotrienols in cardioprotection supports their structure: function relation. Characterization and partial purification of a ferrireductase from human duodenal microvillus membrane. It is now recognized that many malabsorptive disorders, such as celiac disease, might have subtle clinical presentations or mainly extraintestinal manifestations. Awareness is also increasing that subtle malabsorption of single nutrients such as calcium or vitamin B12 can, if unrecognized, lead to complications that may be difficult to reverse or that are even irreversible. The clinical challenge today is to recognize and treat malabsorption despite its subtle manifestations, a challenge made even more difficult by the restricted availability of tests for malabsorption, such as the 72-hour fecal fat determination. Classically, maldigestion is defined as defective intraluminal hydrolysis of nutrients, and malabsorption is defined as defective mucosal absorption. Although this distinction may be useful on pathophysiologic grounds, the clinical presentation and complications of maldigestion and malabsorption are similar. In this article, the terms digestion and absorption or maldigestion and malabsorption are used separately only in the discussion of pathophysiology. When the distinction between these terms is not of clinical relevance, only the terms absorption and malabsorption are used. Malabsorption can be caused by many diseases of the small intestine as well as by diseases of the pancreas, liver, biliary tract, and stomach (Box 104. In some of these diseases, malabsorption may be the presenting feature; in others, malabsorption may be only a minor clinical problem or detected only as a laboratory abnormality. This article provides an overview of basic pathophysiologic mechanisms that lead to symptoms or complications of maldigestion or malabsorption, reviews the clinical manifestations and complications of malabsorption, describes tests that can be used clinically to evaluate digestive and absorptive function, presents a rational diagnostic approach to the individual patient, and discusses malabsorptive diseases and general measures in the treatment of malabsorption syndrome not covered in other chapters of this book.
Generic nifedipine 30 mg visa
Management consists of withdrawal of the drug and treatment of liver failure (see Table 88 pulse pressure youtube order 20 mg nifedipine with amex. Immunosuppressive treatment is not indicated; the clinical condition improves spontaneously after withdrawal of the causative drug. When serious hepatocellular injury was attributed to celecoxib, female gender was a predisposing factor. Liver biochemical and histology were mostly consistent with a pattern of hepatocellular or mixed liver injury, with rare cases of biliary ductopenia and periductal fibrosis. Risk factors for liver injury include increased treatment duration (>30 days) and higher doses. Liver histology shows centrilobular or bridging necrosis and occasionally bland cholestasis. Hepatomegaly and hepatic tenderness are common; splenomegaly is present in 25% of patients. Extrahepatic features of drug hypersensitivity are common, as is eosinophilia (30%). Liver biochemical test levels are typically mixed because of the infiltrative nature of hepatic granulomas and the frequent presence of some hepatocellular necrosis or cholestasis. Single case reports have implicated many other agents, as referred to briefly in the text. Other causes, including oxyphenisatin and tienilic acid, are now of historical interest. Only 4 cases have been fatal, and 5 cases can reasonably be regarded as chronic hepatitis. A prodromal illness characterized by anorexia, nausea, vomiting, and malaise heralds the onset of liver injury, which usually occurs within 3 months (range 1 to 11 months). Liver histology shows acute lobular hepatitis, and, in severe cases, bridging or confluent necrosis, interface hepatitis, and fibrous expansion of the portal tracts. The prognosis is usually good; resolution occurs after discontinuation of the drug. Patients should be advised to report adverse effects, and clinicians must be aware that diclofenac can cause both acute and chronic hepatitis. Cholestasis without Hepatitis Cholestatic reactions are characterized by bile retention within canaliculi, Kupffer cells, and hepatocytes, with minimal inflammation or hepatocellular necrosis; terms to describe this reaction include pure, canalicular, and bland cholestasis. Other drugs generally associated with cholestatic hepatitis occasionally produce bland cholestasis. Tacrolimus can also cause cholestasis,301 whereas sirolimus has been implicated in cases of mild acute hepatitis. A mild transient prodrome of nausea and malaise may occur and is followed by pruritus and jaundice. Liver biochemical tests should be monitored in hormonal replacement therapy users with liver disease. Recovery usually follows drug withdrawal, but protracted cholestasis with biliary ductopenia can occur. The timely cessation of a causative drug prevents an adverse outcome and avoids unnecessary invasive investigations or surgery. Clinical features include pruritus, dark urine, pale stools, and, in more serious cases, jaundice. Hepatobiliary imaging is critical to exclude biliary obstruction and a hepatic or pancreatic mass lesion. In the absence of such findings, drug-induced cholestasis is more likely, and a liver biopsy is often advisable. When the temporal relationship to drug ingestion indicates a high probability of a drug reaction, the incriminated drug should be discontinued and the patient observed for improvement. Management should focus on symptom relief, with particular attention to pruritus (see Chapter 91). Cholestasis with Hepatitis Cholestasis with hepatitis is a common hepatic drug reaction and is characterized by conspicuous cholestasis and hepatocellular necrosis. This type of reaction overlaps with druginduced acute hepatitis, cholestasis without hepatitis, and cholestasis with bile duct injury. Causative agents include chlorpromazine (see later), antidepressants and other psychotropic agents, erythromycins and other macrolides,310 and related ketolide antibiotics (telithromycin,311 clindamycin,312 sulfonamides, oxypenicillins,313 ketoconazole [see earlier],219 sulfonylureas, sulindac,314 ibuprofen, piroxicam,315 cefazolin,316 captopril,167 flutamide,317 enalapril,168 pravastatin,171 atorvastatin,172 ticlopidine,318 ciprofloxacin and other fluoroquinolones,319 and metformin320). The onset can be rapid (median 8 days; range 1 to 39 days) or may be delayed for up to 30 days after the antibiotic course is completed. The range of hepatic reactions includes asymptomatic liver biochemical test abnormalities in 20% to 50% of recipients and rare cases of fulminant hepatic necrosis. Reactions do not appear to be more common with increasing age but are rare in children. The onset is within 1 to 6 weeks after the drug is started but can be delayed by 5 to 14 days after its discontinuation. Pruritus is common and occurs later with chlorpromazine hepatitis than with drug-induced bland cholestasis. Most patients recover completely: one third within 4 weeks, another third between 4 and 8 weeks, and the remainder after 8 weeks. Cholestatic Hepatitis with Bile Duct Injury Bile duct (cholangiolytic) injury is observed with several drugs that cause cholestatic hepatitis, such as chlorpromazine300 and flucloxacillin. Compounds associated with this syndrome include carbamazepine,333 dextropropoxyphene,334 and methylenediamine, an industrial toxin responsible for an outbreak of jaundice (Epping Jaundice) associated with intake of bread made from contaminated flour (see Chapter 89). The illness is often heralded by abdominal pain, which may be severe and simulates other causes of cholangitis. Liver biopsy specimens demonstrate cholestasis with expansion of the portal tracts by inflammation and mild fibrosis; portal tract edema also may be present. Other features include irregularity and necrosis of the biliary epithelium, together with an infiltrate of neutrophils and eosinophils on the outer surface of bile ducts. Recovery is the rule, with liver biochemical test levels returning to normal within 1 to 3 months. Features of hypersensitivity such as fever, skin rash, and eosinophilia are seen in 30% to 60% of patients. Bile duct injury (usually mild) and perivenular cholestasis with lipofuscin deposits are often present. Other histologic features include hepatic granulomas, biliary ductopenia, and cirrhosis. Continuing jaundice, dark urine, and pale stools are possible but not invariable findings and may resolve despite persistence of liver biochemical abnormalities. In severe cases, intestinal malabsorption, weight loss, and bruising caused by vitamin K deficiency may occur; xanthelasma, tuberous xanthomata, and other complications of severe hypercholesterolemia also have been noted. Firm hepatomegaly may be found on physical examination, but splenomegaly is unusual unless portal hypertension develops. Most cases resolve, but there are rare reports of severe biliary ductopenia and biliary cirrhosis. Compounds that stimulate hepatic fibrosis include arsenic, vitamin A, and methotrexate. Hepatic storage of amiodarone also produces phospholipidosis, a storage disorder characterized by enlarged lysosomes stuffed with whorled membranous material (myeloid bodies). In animals fed amiodarone, the development of phospholipidosis is time and dose dependent. The treatment duration and possibly the total dose,357,360 but not the incremental dose, are risk factors for chronic liver disease. Hepatomegaly, jaundice, ascites, bruising, and other features of chronic liver disease may be present. In severe cases, jaundice, hypoalbuminemia, and prolongation of the prothrombin time are evident. Determining the cause of abnormal liver biochemical test results and hepatomegaly is often difficult in patients taking amiodarone, and a liver biopsy may be indicated. Liver histologic findings include phospholipidosis, steatosis, focal necrosis with Mallory hyaline, infiltration with neutrophils, and pericellular fibrosis. Preventing and managing amiodarone-induced liver disease is problematic because abnormal liver biochemical test levels are common in persons taking amiodarone, especially in those with heart failure.
Buy nifedipine 20mg online
Assessment of the influence of hydrogen nonexcretion on the usefulness of the hydrogen breath test and lactose tolerance test hypertension yoga order genuine nifedipine. An upstream polymorphism associated with lactase persistence has increased enhancer activity. Meta-analysis: the diagnostic accuracy of lactose breath hydrogen or lactose tolerance tests for predicting the North European lactase polymorphism C/T-13910. A novel polymorphism associated with lactose tolerance in Africa: multiple causes for lactase persistence Measurement of short-chain fatty acids in human faeces using high-performance liquid chromatography: specimen stability. Evidence for impaired assimilation and increased colonic fermentation of protein, related to gastric acid suppression therapy. The Lundh test and faecal elastase 1 determination in chronic pancreatitis: a comparative study. Effect of molecular structure on bile acid-induced alterations in absorptive function, permeability, and morphology in the perfused rabbit colon. Fibroblast growth factor 19 and 7alpha-Hydroxy-4-Cholesten-3-one in the diagnosis of patients with possible bile acid diarrhea. A new mechanism for bile acid diarrhea: defective feedback inhibition of bile acid biosynthesis. Studies of the prevalence and significance of radiolabeled bile acid malabsorption in a group of patients with idiopathic chronic diarrhea. Accurate enzymatic measurement of fecal bile acids in patients with malabsorption. Rapid intestinal transit as a primary cause of severe chronic diarrhea in patients with amyloidosis. Use of 23-selena-25-homocholyltaurine to detect bile acid malabsorption in patients with ileal dysfunction or diarrhea. Cellobiose/mannitol test: physiological properties of probe molecules and influence of extraneous factors. Comparative clinical evaluation of the 13C mixed triglyceride breath test as an indirect pancreatic function test. Methodology and indications of H2-breath testing in gastrointestinal diseases: the Rome Consensus Conference. Hydrogen and methane-based breath testing in gastrointestinal disorders: the North American Consensus. Oral xylose isomerase decreases breath hydrogen excretion and improves gastrointestinal symptoms in fructose malabsorption-a double-blind, placebo-controlled study. The role of artificial and natural sweeteners in reducing the consumption of table sugar: a narrative review. Conjugated bile acid replacement therapy reduces urinary oxalate excretion in short bowel syndrome. Absence of dysfunctional ileal sodium-bile acid cotransporter gene mutations in patients with adult-onset idiopathic bile acid malabsorption. Accelerated regional bowel transit and overweight shown in idiopathic bile acid malabsorption. Review article: gastrointestinal amyloidosis - clinical features, diagnosis and therapy. Endoscopic and biopsy findings of the upper digestive tract in patients with amyloidosis. An investigation of gastrointestinal disturbances in familial amyloidosis with polyneuropathy. Use of olmesartan and enteropathy outcomes: a multi-database study Severe intestinal malabsorption associated with olmesartan: a French nationwide observational cohort study Immunopathogenesis of olmesartan-associated enteropathy. The effect of pancreatic enzyme supplementation in patients with steatorrhoea after total gastrectomy. Vitamin E malabsorption and neurological consequences after gastrectomy for gastric cancer. Ingestion of guar gum hydrolysate, a soluble fiber, increases calcium absorption in totally gastrectomized rats. An evaluation of the importance of gastric acid secretion in the absorption of dietary calcium. Developmental patterns of small intestinal enterokinase and disaccharidase activities in the human fetus. Intestinal disaccharidase activities in relation to age, race, and mucosal damage. An enhancer activates the pig lactase phlorizin hydrolase promoter in intestinal cells. Biogenesis of intestinal lactase-phlorizin hydrolase in adults with lactose intolerance. Evaluation of the pathogenesis of flatulence and abdominal cramps in patients with lactose malabsorption. Lactose malabsorption in Greek adults: correlation of small bowel transit time with the severity of lactose intolerance. Lactose absorption and malabsorption in healthy Italian children: do the quantitiy of malabsorbed sugar and the small bowel transit time play a role in symptom production Lactose handling by women with lactose malabsorption is improved during pregnancy. Genetic predisposition for adult lactose intolerance and relation to diet, bone density, and bone fractures. Adult-type hypolactasia and calcium availability: decreased calcium intake or impaired calcium absorption Fructose-sorbitol malabsorption and symptom provocation in irritable bowel syndrome: relationship to enteric hypersensitivity and dysmotility. Fructose malabsorption may be gender dependent and fails to show compensation by colonic adaptation. Fructose and sorbitol malabsorption in ambulatory patients with functional dyspepsia: comparison with lactose maldigestion/malabsorption. Colonic bacterial activity determines the symptoms in people with fructose-malabsorption. The contribution of malabsorption to the reduction in net energy absorption after long-limb Roux-en-Y gastric bypass. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient-2013 update: cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery. Small-bowel bacterial overgrowth in elderly people: clinical significance and response to treatment. Lactose malabsorption in the elderly: role of small intestinal bacterial overgrowth. Small bowel bacterial overgrowth in systemic sclerosis: detection using direct and indirect methods and treatment outcome. Hypereosinophilic syndrome presenting with diarrhoea and anaemia in a patient with systemic lupus erythematosus. Malabsorption due to cholecystokinin deficiency in a patient with autoimmune polyglandular syndrome type I. Pernicious anemia and widespread absence of gastrointestinal endocrine cells in a patient with autoimmune polyglandular syndrome type I and malabsorption. Gastrointestinal pathology in patients with common variable immunodeficiency and X-linked agammaglobulinemia. The significance of duodenal mucosal atrophy in patients with common variable immunodeficiency: a clinical and histopathologic study the enteropathy associated with common variable immunodeficiency: the delineated frontiers with celiac disease. The enteropathy associated with common variable immunodeficiency: the delineated frontiers with celiac disease. A cross-sectional study of the prevalence of gastrointestinal symptoms and pathology in patients with common variable immunodeficiency. The gene involved in Xlinked agammaglobulinaemia is a member of the src family of protein-tyrosine kinases. Symptom clustering in subjects with and without diabetes mellitus: a population-based study of 15,000 Australian adults.
Purchase nifedipine overnight
Cimetidine blood pressure guidelines 2015 nifedipine 20 mg with mastercard, ranitidine, and famotidine can cause acute hepatitis, mostly mild and often with cholestatic features. Other histologic findings include occasional cholestatic hepatitis with bile duct injury and microvesicular steatosis. In persons in whom hepatitis develops, the latent period from exposure to disease ranges from 1 week to more than 6 months (median, 8 weeks), and, in severe cases, 12 weeks. Prodromal symptoms occur in one third of patients and include malaise, fatigue, and early symptoms of hepatitis, such as anorexia, nausea, and vomiting. Jaundice appears several days later and is the only feature in approximately 10% of cases. Serum bilirubin levels usually are elevated; values that are increased more than 10-fold indicate a poor prognosis. In one study,193 one third of patients had a prolonged prothrombin time, and 60% of these cases were fatal. Liver histology shows hepatocellular injury, which is focal in one half of the cases, often with marked hydropic change in residual hepatocytes. In the remainder, hepatocellular necrosis is zonal, submassive, or massive, with inflammation confined to the portal tracts. Cholestasis and lobular regeneration suggestive of early cirrhosis are rare features. New regimens are gaining favor for treating latent tuberculosis infection; a 4-month rifampin schedule was less hepatotoxic than the traditional isoniazid course. Effective prevention depends on awareness of early symptoms, no matter how nonspecific. Recovery is usual with discontinuation of the drug, although prolonged cholestasis with ductopenia has been reported. Rare cases of severe hepatic necrosis have been ascribed to fluconazole, but other causes were not excluded. Patients who take combinations that include isoniazid and pyrazinamide can develop particularly severe liver injury. In a network meta-analysis of treatment protocols for latent tuberculosis, pyrazinamide-based regimes carried the highest risk of hepatic injury. Evidence that preexisting liver disease or other drugs predispose to troglitazone hepatotoxicity is lacking, although a progressive course in one patient was attributed to concurrent use of simvastatin and troglitazone. Serious liver injury is rare with the second-generation thiazolidinediones, rosiglitazone and pioglitazone. Women (with a female-to-male ratio of 2:1) and persons older than 40 years of age are particularly susceptible to liver injury. Continued ingestion of ketoconazole after the onset of symptoms leads to an adverse outcome. Jaundice occurs in 50% of patients in whom acute hepatitis develops, and up to one third may present with nonspecific symptoms, such as nausea, anorexia, and vomiting. By contrast, a French pharmacovigilance study concluded that the risk of hepatic reactions with these drugs was similar to that reported with other oral hypoglycemic drugs. Persons in whom jaundice developed with troglitazone should not take other thiazolidinediones. Fatal liver failure has been reported in 2 cases, including one with underlying cirrhosis. Gliclazide245 and glibenclamide have also been associated with hepatocellular injury and, with the latter drug, hepatic granulomas. By promoting weight gain, some of these drugs (clozapine, olanzapine) also promote hepatic steatosis. Postmarketing surveillance has identified 3 additional patients with acute hepatocellular injury. Thereafter, the frequency of testing is left to the discretion of the treating doctor. With bentazepam, the clinicopathologic pattern resembled chronic hepatitis, but without autoantibodies or other immunologic features. Minor degrees of hepatocellular injury were noted in up to 50% of cases, but tolerance eventually developed. The mechanism of liver injury is unclear, but mitochondrial injury was observed in an animal model of tacrine hepatotoxicity. Dantrolene, a skeletal muscle relaxant, causes hepatitis in about 1% of exposed persons, with a case-fatality rate of approximately 28%. One third of patients are asymptomatic, and the remainder present with jaundice and symptoms of hepatitis. Other idiosyncratic hepatotoxins include tizanidine (a centrally acting muscle relaxant),271 alverine (a smooth muscle relaxant),272 and riluzole. Two cases 88 Drugs Used for Psychiatric and Neurologic Disorders Several neuroleptic agents have been associated with drug hepatitis. Some reactions appear to be immunoallergic, whereas others are related to metabolic idiosyncrasy, depending on the drug structure. Such reactions have been reported for commonly used antidepressants, such as fluoxetine,247,248 paroxetine,249 venlafaxine,250 trazodone,251 tolcapone,252 and nefazodone. The hydrazine substituent (which iproniazid shares in part with isoniazid, ethionamide, pyrazinamide, and niacin) was determined to be the hepatotoxic moiety. Tricyclic antidepressants bear a structural resemblance to the phenothiazines and are occasional causes of cholestatic or, less commonly, hepatocellular injury. Recovery following cessation of the drug is usual, but amitriptyline254 and imipramine255 can cause prolonged cholestasis. Liver enzyme elevations have been observed in asymptomatic persons taking fluoxetine and paroxetine. Liver biochemical test elevations resolved rapidly after riluzole was discontinued. Small-vessel vasculitis is another potential complication and may involve the kidneys, bone marrow, skin, and lungs; the mortality rate is high. For drug reactions, however, the definition often has been made inappropriately on hepatic histologic features alone. The histologic features include interface hepatitis, bridging necrosis, and fibrosis. Because these features may be present as early as 6 weeks after the onset of severe reactions, they do not confirm chronicity. The diagnosis of chronic hepatitis is more convincing when clinical or biochemical evidence of hepatitis has been present for more than 3 months and when clinical and laboratory features of chronic liver disease or histologic evidence of established hepatic fibrosis are present. Nevertheless, recognition of a drug cause remains important for preventing a poor outcome by timely withdrawal of the drug. Chronic hepatitis is more common in women (4-fold) and in older patients (as illustrated by nitrofurantoin) but is rare in children. Drugs associated with chronic hepatitis more commonly cause acute hepatitis, and the latent period to recognition tends to be longer in cases of chronic hepatitis; therefore, the duration of drug ingestion may be a risk factor for chronic hepatitis. In the first, cases are identical to acute hepatitis but more severe, more prolonged, or later in onset, perhaps due to failure of recognition. Clinical and laboratory features of chronic liver disease are rare, and hallmarks of autoimmunity are absent. Recognized causes include intralesional formalin therapy of hepatic hydatids and intra-arterial infusion of floxuridine for metastatic colorectal carcinoma. After several months of floxuridine infusion, the frequency of toxic hepatitis or bile duct injury, or both, was as high as 25% to 55% but has declined considerably (to 5%) with the advent of current protocols. Ischemia has been suspected, and toxicity to biliary epithelial cells is another possibility. Other drugs associated with steatohepatitis include irinotecan (in the setting of colorectal cancer)381 and 2 other agents that are no longer used, perhexiline maleate and coralgil (4,4-diethylaminoethoxyhexestrol). Liver biochemical test monitoring has been recommended,382 but there is no evidence to support the efficacy of this approach in preventing severe reactions. Calcium channel blockers have rarely been associated with steatohepatitis,364 and methyldopa has been reported to be associated with cirrhosis in obese middle-aged women365; however, these associations may have been fortuitous. Several forms of liver injury have been attributed to tamoxifen,368 including cholestasis, hepatocellular carcinoma,369 peliosis hepatis,370 acute hepatitis, massive hepatic necrosis,368 steatosis, and steatohepatitis, occasionally with cirrhosis. Reduction in the severity of hepatic steatosis has been documented with bezafibrate, a peroxisome proliferator-activated receptor- agonist.