Order 10mg glipizide amex
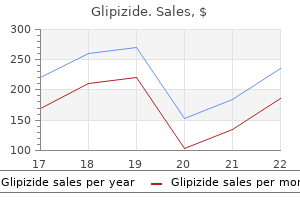
Additional N-methylmelamines formed may also mediate some of the cytotoxicity of this agent signs your diabetes is getting worse glipizide 10 mg without prescription. Altretamine therapy may be associated with some nausea, vomiting, diarrhea, abdominal cramping, and myelosuppression (see Table 27. Biologic and Targeted Agents Since the early 2000s, there have been major efforts toward the incorporation of monoclonal antibodies such as bevacizumab and cetuximab and small-molecule tyrosine inhibitors such as sunitinib, gefitinib, and sorafenib into first-line and recurrent treatment regimens for gynecologic cancers. Although as single-agent therapy the biologic agents have not demonstrated significant activity against gynecologic cancers, there are mounting clinical data to support the implementation of agents such as bevacizumab into first-line and maintenance regimens to improve progression-free survival, specifically for ovarian cancer. As a single agent in the recurrent ovarian cancer setting, bevacizumab has had only a moderate response ranging from 16% to 21% (Cannistra, 2007; Monk, 2006). However, in combination with chemotherapy, bevacizumab has had promising response rates, ranging from 15% to 80% (Micha, 2007; Penson, 2009). Hence, the current recommendation is that patients should not have had recent bowel surgery or a history of significant bowel resections. Bevacizumab has been evaluated in combination with oral cyclophosphamide, paclitaxel, and gemcitabine for the treatment of recurrent ovarian cancer. The integration of bevacizumab into a first-line treatment regimen has focused on the benefits with paclitaxel plus carboplatin followed by maintenance with bevacizumab alone. However, the duration of maintenance bevacizumab remains an area of therapeutic and pharmacoeconomic controversy. Initial studies have demonstrated that it is beneficial in the treatment of malignant ascites. Anticancer Hormone Therapy Hormone therapy has been effectively developed for the treatment of breast cancer. Estrogen and progesterone receptors have been clearly identified in endometrial carcinomas and have been found in other types of gynecologic cancers, particularly ovarian epithelial carcinomas. Progestins such as megestrol (Megace), depot medroxyprogesterone acetate (Depo-Provera), and 17-hydroxyprogesterone caproate (Delalutin), as well as antiestrogens such as tamoxifen and raloxifene, have been used in the treatment of endometrial carcinomas and seem to have their best effects against well-differentiated tumors. Platinum sensitivity is defined by a disease-free interval longer than 6 months after treatment with a platinum agent. If platinum-sensitive, patients can be retreated with a platinum agent, which usually will be single-agent carboplatin because it is tolerated better. Platinum resistance is present when there is tumor progression while receiving a platinum agent or disease relapse within less than 6 months after the completion of chemotherapy, and alternative agents must be considered. The optimal chemotherapeutic agent or regimen in the treatment of platinum-resistant disease is currently unknown. Overall, regardless of the agent, the response rate is low for all the agents in platinum-refractory (resistant) cancer. Because tumor regression is so rare in the recurrent setting, even achieving stable disease is considered a treatment success. If no response is observed after three cycles, an alternative chemotherapy regimen may be selected. A number of trials are necessary to move a new agent from the point of evaluation to allow it to be used in regular medical practice. Unlike other areas of drug development, clinical trials for cytotoxic agents can only be conducted in those with active cancer, often those who have already failed current standard therapy treatment options. In general, patients are poor candidates from clinical trials if their score is 50 or less. The human clinical trial process is a fairly rigorous and costly process to determine not only safety and efficacy but also improvement over the current standard of care for each new agent proposed, sometimes alone or in various combination regimens. At the various doses tested, some therapeutic effects may be observed, although this is not the primary aim of the trial. For example, this trial design assesses whether a new drug therapy is superior, equivalent, or inferior to the chemotherapeutic agent currently used. Numerous programs have been implemented to facilitate drug approval and access to investigational drugs, such as the Fast Track Drug Approval Program and Orphan Drug Approval. Compendia listings are often granted based on peer-reviewed published literature, which expands reimbursement for treatment recommendations. Progress has been slow and unsuccessful in finding a cure for ovarian cancer and recurrent endometrial or cervical cancers. In the absence of a curative treatment for recurrent disease, selecting an investigational trial treatment still remains the best option for ovarian cancer patients. Research is needed to identify and develop new approaches for preventing recurrence and new options for treating advanced primary and recurrent disease. Efforts should especially focus on agents to modulate or overcome drug resistance or new molecular targets to optimize chemotherapy outcomes. Radiation acts on cells primarily in the M phase, making rapidly proliferating cells the most radiosensitive. Normal tissues repair the radiobiologic effects of radiation more effectively than tumor tissue. Uncommon side effects include lowering of the circulating blood cells, dysuria and urinary frequency, diarrhea, bowel injury, and fistula formation. Cytotoxic chemotherapeutic agents act on various phases of the cell cycle, primarily affecting rapidly proliferating cells, and at a given dose destroy a constant fraction of tumor cells. If recurrence is less than 6 months after completion of chemotherapy, the tumor is defined to be platinum or taxane resistant. The antitumor activity of second-line chemotherapy regimens is similar; the choice of treatment for recurrent disease depends on residual toxicities, physician preference, and patient convenience. The prognostic importance of site and type of radiation-induced bowel injury in patients requiring surgical management. Anemia in cervical cancers: impact on survival, patterns of relapse, and association with hypoxia and angiogenesis. An investigation of the molecular basis for the synergistic interaction of tirapazamine and cisplatin. Dose-dense paclitaxel once a week in combination with carboplatin every 3 weeks for advanced ovarian cancer: a phase 3, open-label, randomized controlled trial. The mechanism of action of radiosensitization of conventional chemotherapeutic agents. The relative radiosensitivity of the nucleus and cytoplasm of the Chinese hamster fibroblasts. Long-term follow-up confirms a survival advantage of the paclitaxel-cisplatin regimen over the cyclophosphamidecisplatin combination in advanced ovarian cancer. Targeting the tumor blood vessel network to enhance the efficacy of radiation therapy. Obstetrics & Gynecology Books Full 27 Principles of Radiation Therapy and Chemotherapy in Gynecologic Cancer Kurzeder C, Sauer G, Deissler H. Molecular targets of ovarian carcinomas with acquired resistance to platinum/taxane chemotherapy. Survival benefits with diverse chemotherapy regimens for ovarian cancer: meta-analysis or multiple treatments. Radiosensitization of human breast cancer cells by a novel ErbB family receptor tyrosine kinase inhibitor. International Encyclopedia of Pharmacology and Therapeutics- Inhibitors of Ribonucleotide Diphosphate Reductase Activity. Expression of ribonucleotide reductase after ionizing radiation in human cervical carcinoma cells. Obstetrics & Gynecology Books Full 28 Intraepithelial Neoplasia of the Lower Genital Tract (Cervix, Vagina, Vulva) Etiology, Screening, Diagnosis, Management Mila Pontremoli Salcedo, Ellen S. Schmeler Cervical cancer is a leading cause of cancer and cancer-related deaths among women worldwide, with more than 500,000 new cases and 250,000 deaths annually. Cervical cancer was previously the leading cause of cancer-related death among women in the United States. However, the incidence and mortality has decreased by approximately 70% since the 1970s. This decline is largely due to the introduction in 1941 of the Papanicolaou (Pap) smear, which has led to a systemic effort to detect early cervical cancer and precancerous lesions (Papanicolaou, 1941). Cervical cancer is a preventable disease, with excellent tools for prevention (vaccination) and screening (Pap and human papillomavirus testing). Furthermore, there is a treatable preinvasive phase that lasts several years before progressing to invasive cancer.
Discount 10 mg glipizide otc
It is clear that for symptomatic women with ovarian endometriomas best yogurt type 2 diabetes order glipizide overnight, laparoscopic surgical excision should be undertaken. Otherwise for small lesions (2 cm), follicle aspiration can be accomplished avoiding the endometriomas. In general, the presence of endometriomas tends to decrease the number of oocytes aspirated but may not impair oocyte or embryo quality. There has long been a debate as to whether treating mild endometriotic lesions or implants would improve fertility. Data from the Canadian and Italian studies, taken together, suggest that the pregnancy rates improve with implant ablation (Jacobson, 2002). The way these data should be extrapolated into practice is that if a laparoscopy is being performed in a woman wishing to conceive, visible lesions should be ablated if technically possible rather than ignoring them. Apart from the mechanical factors (endometriomas, adhesions, fibrosis) affecting pregnancy rates, in endometriosis, macrophage and cytokine abnormalities are thought to play a significant role in inhibiting fertility. These factors may affect oocyte quality, fertilization, and embryo quality as well as endometrial receptivity. Therefore, in addition to ablating lesions when present, several strategies have been devised to enhance fecundity. Controlled ovarian stimulation along with intrauterine insemination, an approach to enhance fecundity in women with unexplained infertility, has been found to be beneficial in women with endometriosis. Although an older meta-analysis suggested an approximate 20% reduction in pregnancy rates, (Barnhart, 2002) data suggest that pregnancy rates are comparable unless endometriosis is severe (Hamdan, 2015). This reemphasizes the pathophysiologic consequences involved with having endometriosis (described earlier). The role of surgical therapy in the management of endometriosis is very much dependent on the clinical presentation of the patient and her desire for future fertility. Although there can be a beneficial effect for fertility, a detrimental effect can also be seen. Advanced stages of disease, particularly those involving extrapelvic locations (discussed later), are often best managed in a multidisciplinary fashion. Implants that involve the gastrointestinal tract are the most common site of extrapelvic endometriosis but can be the most challenging to manage. The severity and extent of involvement of the bowel by ectopic endometrium varies from the incidental finding of a spot on the serosa of the bowel to obstruction of the rectosigmoid. In the majority of cases, endometriosis of the gastrointestinal tract involves the sigmoid colon and the anterior wall of the rectum, accounting for approximately 90% of cases (see Video 19. In a series of more than 100 consecutive patients with endometriosis, 13% had histologic evidence of endometriosis in the appendix, whereas only 60% of these cases are detected on gross examination. Of note, 48% of patients with rectosigmoid lesions will also have endometriosis of the ovaries, and 84% will have rectocervical lesions (Hemming, 2009). Classic symptoms of endometriosis of the large bowel include dysmenorrhea (cyclic pelvic cramping and lower abdominal pain) and dyschezia (rectal pain with defecation), especially during the menstrual period. Studies have demonstrated that 25% to 35% of women with advanced endometriosis of the large bowel experience episodic rectal bleeding due to endometriosis extending into the submucosa. A distinct dysfunction of the enteric nervous system has been suggested to be the primary cause of the abnormalities of bowel function in women with endometriosis. It is difficult to differentiate the symptoms associated with endometriosis from the overlapping constellation of symptoms associated with inflammatory disease of the colon or malignancy. Women with a gastrointestinal malignancy usually experience intermittent rather than cyclic intestinal bleeding. Physical exam can also help with diagnosis of deep infiltrating endometriosis invading the rectosigmoid such as by palpation of a pelvic mass or "rectal shelf " on rectovaginal examination. Sigmoidoscopy usually demonstrates absence of a mucosal lesion in addition to fixation and immobility of the anterior rectal wall. Donnez and coworkers speculated that endometriosis of the rectovaginal septum is a disease process more closely related to foci of adenomyosis than endometriosis (Donnez, 1997). Surgery should generally be performed in coordination with a multidisciplinary team. Although no consensus exists, bowel resection generally is indicated in symptomatic women when lesions are greater than 2 cm, greater than 30% of the circumference is involved, and when there is invasion into the inner muscularis layer, which may require bowel resection (see Video 19. When surgery is indicated, while still unclear which is better, bowel resection can be done via either segmental or discoid resection. Parameters that should be considered in surgical planning include size, number and depth of lesions, extent of bowel circumference involvement, distance to anal verge, and presence of lymph node involvement. Endometriosis in the female pelvis occasionally produces dysfunction in adjacent pelvic organs. Approximately 10% of women with endometriosis have involvement of the urinary tract, which most commonly involves endometriotic implants and associated retroperitoneal fibrosis located in the peritoneum overlying the ureter or the bladder. In most cases an incidental finding of aberrant endometrial glands and stroma is discovered on the bladder peritoneum and anterior cul-de-sac. The most serious consequence of urinary tract involvement is ureteral obstruction, which occurs in about 1% of women with moderate or severe pelvic endometriosis. Interestingly, approximately 50% of women with endometriosis of the urinary tract have a history of previous pelvic surgery. The lesions may develop from implanted endometrium during cesarean delivery or may be an extension from adenomyosis of the anterior uterine wall. Patients with endometriosis involving the urinary tract have nonspecific clinical presentations. One of three women with documented complete ureteral obstruction secondary to endometriosis has no pelvic symptoms whatsoever. The clinical challenge is to diagnose minimal ureteral obstruction at an early stage, before loss of renal function. The obstruction is almost always in the distal one third of the course of the ureter. The importance of an imaging study to diagnose ureteral compromise in all women with retroperitoneal endometriosis cannot be overemphasized. Endometriosis of the bladder is discovered most often in the region of the trigone or the anterior wall of the bladder (Video 19. Treatment of endometriosis of the peritoneum over the bladder can be accomplished by medical or surgical means. Ureteral obstruction may be intrinsic, from active endometriosis, or extrinsic, from long-standing fibrotic reactions to retroperitoneal inflammation. Extrinsic endometriosis is three to five times more common than the intrinsic form. However, long-term follow-up with serial ultrasound imaging or intravenous pyelograms must be undertaken to ensure that the disease process does not recur. Surgical therapy is the preferred treatment for ureteral obstruction secondary to endometriosis (Video 19. The most common surgical approaches include removal of the uterus and both ovaries and the relief of urinary obstruction by ureterolysis or by ureteroneocystostomy. If ureterolysis is performed, peristalsis in the involved segment of the ureter should be observed, along with adequate resection of the endometriosis and surrounding inflammation in the retroperitoneal space. Ureteroneocystostomy has the advantage of bypassing the urinary obstruction and making it technically easier to resect the area of endometriosis and associated retroperitoneal fibrosis. Obstetrics & Gynecology Books Full 19 Endometriosis 441 A Endometriotic implants B Liver Rt. However, if a patient is symptomatic, the most common presentation of diaphragmatic endometriosis is right-sided catamenial pneumothorax. Other signs and symptoms can include dyspnea, chest pain, shoulder pain, hemoptysis, and the presence of pulmonary nodules. Medical suppressive therapy is the first approach, although surgery, including pleurodesis, may be considered. Possible causal factors of endometriosis include retrograde menstruation, coelomic metaplasia, vascular metastasis, immunologic changes, iatrogenic dissemination, and a genetic predisposition. Grossly, endometriosis appears in many forms, including red, brown, black, white, yellow, pink, or clear vesicles and lesions. Approximately 10% of teenagers who develop endometriosis have associated congenital outflow obstruction.
Cheap glipizide 10mg with mastercard
Secondary cytoreduction in platinumresistant recurrent ovarian cancer: a single-institution experience diabetes test with urine generic glipizide 10mg otc. Laparoscopic management of early ovarian and fallopian tube cancers: surgical and survival outcome. Immature (malignant) teratoma of the ovary: a clinical and pathologic study of 58 cases. Diaphragmatic peritonectomy versus full thickness diaphragmatic resection and pleurectomy during cytoreduction in patients with ovarian cancer. A review of the close surveillance policy for stage I female germ cell tumors of the ovary and other sites. Rectosigmoid resection at the time of primary cytoreduction for advanced ovarian cancer. Five-year survival for stage Ic or stage I grade 3 epithelial ovarian cancer treated with cisplatin-based chemotherapy. Percutaneous endoscopic gastrostomy tube placement in patients with malignant bowel obstruction due to ovarian carcinoma. Palliative surgery for bowel obstruction in recurrent ovarian cancer: an updated series. Ovarian tumors of borderline malignancy (tumors of low malignant potential): a critical appraisal. Intraperitoneal recombinant interferon gamma in ovarian cancer patients with residual disease at secondlook laparotomy. Pegylated liposomal Doxorubicin and carboplatin compared with paclitaxel and carboplatin for patients with platinum-sensitive ovarian cancer in late relapse. Small cell carcinoma of the ovary with hypercalcemia: report of a case of survival without recurrence 5 years after surgery and chemotherapy. A clinicopathologic multivariate analysis affecting recurrence of borderline ovarian tumors. Risk factors for anstomotic leak after recto-sigmoid resection for ovarian cancer. Pseudomyxoma peritonei in women: A clinicopathologic analysis of 30 cases with emphasis on site of origin, prognosis, and relationship to ovarian mucinous tumors of low malignant potential. Clinical relevance of retroperitoneal involvement from epithelial ovarian tumors of borderline malignancy. Ten-year follow-up of ovarian cancer patients after second-look laparotomy with negative findings. Combined transvaginal B-mode and color Doppler sonography for differential diagnosis of ovarian tumors: results of a multivariate logistic regression analysis. Relationship between lifetime ovulatory cycles and overexpression of mutant p53 in epithelial ovarian cancer. Neoadjuvant chemotherapy for low-grade serous carcinoma of the ovary or peritoneum. Gonadoblastoma: a gonadal tumor related to dysgerminoma (seminoma) and capable of sex hormone production. Conclusions and recommendations from the Helene Harris Memorial Trust Fund Biennial International Forum on ovarian cancer, May 4-7, 1995. Ovarian cysts in premenopausal and postmenopausal tamoxifen-treated women with breast cancer. Different types of rupture of the tumor capsule and the impact on survival in early ovarian carcinoma. Risk factors for progression to invasive carcinoma in patients with borderline ovarian tumors. Relative frequency of malignant paraovarian tumors: Should paraovarian tumors be aspirated The evidence on the effectiveness of management for malignant pleural effusion: a systematic review. Reproductive function after conservative surgery and chemotherapy for malignant germ cell tumors of the ovary. Conservation of in vitro drug resistance patterns in epithelial ovarian carcinoma. Recurrent ovarian granulosa cell tumor: a case report of a dramatic response to taxol. Impact of adjuvant chemotherapy and surgical staging in early-stage ovarian carcinoma: European Organization for Research and Treatment of Cancer-Adjuvant ChemoTherapy in Ovarian Neoplasm trial. A review of four prospective randomized trials including 253 patients with borderline tumors. Cytoreductive surgery in ovarian carcinoma patients with a documented previously complete surgical response. Ovarian cancer screening in asymptomatic postmenopausal women by transvaginal sonography. Epithelial ovarian cancer: Impact of surgery and chemotherapy on survival during 1977-1990. Neoadjuvant chemotherapy or primary debulking surgery in advanced ovarian carcinoma: a retrospective analysis of 285 patients. A Southwest Oncology Group study for the use of a human tumor cloning assay for predicting response in patients with ovarian cancer. Long-term survival after vinblastine, bleomycin, and cisplatin treatment in patients with germ cell tumors of the ovary: an update. Second-look laparotomy in ovarian germ cell tumors: the Gynecologic Oncology Group experience. Adjuvant therapy of ovarian germ cell tumors with cisplatin, etoposide, and bleomycin: a trial of the Gynecologic Oncology Group. Treatment of malignant ovarian germ cell tumors with preservation of fertility: A report of 28 cases. Mucinous tumors of the appendix associated with mucinous tumors of the ovary and pseudomyxoma peritonei. Cis-platinum/vinblastine/bleomycin combination chemotherapy in advanced or recurrent granulosa cell tumors of the ovary. Survival and reproductive function after treatment of malignant germ cell ovarian tumors. Gershenson Fallopian tube and peritoneal cancers have similar clinical characteristics, patterns of spread, response to treatment, and survival rates when compared with ovarian cancer. In addition, the most common histologic type for all three malignancies is high-grade serous adenocarcinoma. However, fallopian tube and peritoneal cancers have several distinct clinical and pathologic findings. This chapter reviews current information on fallopian tube and peritoneal cancer, with particular emphasis on diagnosis, natural history, and clinical management. It diffusely involves the peritoneal surfaces while sparing or minimally involving the ovaries and fallopian tubes. The incidence of peritoneal carcinoma in the United States has been estimated to be 0. Peritoneal cancer is histologically indistinguishable from epithelial ovarian cancer and has similar clinical characteristics, patterns of spread, response to treatment, and survival rates (Fromm, 1990; Halperin, 2001). However, peritoneal cancer has also been associated with older age at diagnosis and increased rates of obesity when compared with ovarian cancer (Barda, 2004; Jordan, 2008). The germinal epithelium of the ovary and mesothelium of the peritoneum arise from the same embryonic origin, and it was previously suggested that primary peritoneal cancer may develop from a malignant transformation of these cells (Lauchlan, 1972). Another proposed theory was a field effect, with the coelomic epithelium lining the abdominal cavity (peritoneum) and ovaries (germinal epithelium) manifesting a common response to an oncogenic stimulus (Parmley, 1974; Truong, 1990). Molecular studies have been inconclusive in determining whether the tumor arises from the ovarian surface epithelium and spreads throughout the peritoneum or if a multifocal malignant transformation process occurs. Peritoneal carcinoma has therefore become a diagnosis of exclusion when a primary ovarian or fallopian tube carcinoma cannot be identified. However, it has been suggested that many cases of ovarian carcinoma may actually arise from the epithelial lining of the fallopian tube fimbria, thereby grossly underestimating the incidence of primary fallopian tube carcinoma (Kindelberger, 2007; Carlson, 2008a). Similar to ovarian cancer, associated risk factors for fallopian tube and peritoneal cancer include infertility, low parity, early menarche, and late menopause (Gates, 2010). Protective factors include oral contraceptive use, multiparity, breastfeeding, and tubal ligation (Cibula, 2011; Tsilidis, 2011).
Glipizide 10mg with amex
Diagnostic accuracy of retrograde and spontaneous voiding trials for postoperative voiding dysfunction: a randomized controlled trial blood sugar refers to what molecule circulating in blood buy glipizide 10 mg low cost. Posterior vaginal compartment prolapse and defecatory dysfunction: are they related Long-term outcomes of vaginal mesh versus native tissue repair for anterior vaginal wall prolapse. Successful pregnancies and vaginal deliveries after sacrospinous uterosacral fixation in five of nineteen patients. Comparison of 2 techniques to predict voiding efficiency after inpatient urogynecologic surgery. Massive eversion of the vagina: pathogenesis, diagnosis, and therapy of the "true" prolapse of the vaginal stump. Advanced anterior vaginal wall prolapse is highly correlated with apical prolapse. Laparoscopic sacrocervicopexy for the treatment of uterine prolapse: a retrospective case series report. Lentz the gynecologist frequently consults on and treats urologic problems in the female patient. Perhaps the most commonly seen of these problems involves infection and inflammation of the lower tract. Various prevalence studies have reported that approximately 30% of women noted some degree of incontinence during the preceding 12 months. Ten percent of women suffer from weekly incontinence, and 5% have daily incontinence. Urinary incontinence problems increase in incidence with age and, because the number of older women in our population is increasing, this problem is growing in magnitude. A survey of pelvic floor disorders by (Nygaard, 2008) found at least one pelvic floor disorder in 24% of women. At least monthly urine leakage was reported by 7% of women ages 20 to 39, 17% ages 40 to 59, 23% ages 60 to 79, and 32% 80 years of age and older. This study may actually underpredict the prevalence of these disorders because women in the survey may have been successfully treated and not counted. Overweight and obese women were more likely to report urinary incontinence than women of normal weight. Continence depends on a number of factors, including the neurologic control of micturition, the anatomic relationships of the urinary tract, and the specific effects of a number of systemic, infectious, and neoplastic conditions. Older women have additional challenges to the urinary system with comorbid medical conditions, ambulatory difficulties, and cognitive impairments. Not only does the prevalence of urinary incontinence increase with age, but so does the severity. Incontinence has been associated with depression, increased social isolation, falls, hip fractures, and admission to nursing homes, which has additional morbidity. Furthermore, incontinence decreases quality of life 474 and increases costs to society. This chapter discusses the physiology of normal micturition as well as the evaluation and treatment of female lower urinary tract conditions. It is a balance between bladder storage, which is organized primarily in the spinal cord and coordinates urethral closure and detrusor relaxation, and micturition, which is controlled by reflex mechanisms mediated by the brain. Voluntary voiding is a learned function and is not automatic, like heart rate control. Bladder detrusor contractility is stimulated by the activity of the parasympathetic nervous system, mediated primarily through the neurotransmitter acetylcholine. This stimulates muscarinic (primarily M3) receptors in the bladder wall, which then activate detrusor contraction. Sympathetic nerve receptors within the bladder cause bladder relaxation when stimulated. Bladder contraction may also be affected by irritation and inflammation of the bladder wall lining, causing uninhibited contractions. Inhibitory input to the urethral smooth muscle is conveyed by nitric oxide via parasympathetic nerves. Somatic cholinergic motor nerves supply the striated muscles of the external urethral sphincter from the sacral spinal cord. The act of voiding is under the control of four basic autonomic and somatic nervous system feedback loops. The parasympathetic system is involved in the act of voiding via nuclei in S2 through S4 (micturition center) and mediates its activity through the neurotransmitter acetylcholine, directly stimulating muscarinic receptors in the bladder wall. This signal is transmitted via the pelvic nerve and causes the detrusor to contract. Norepinephrine is secreted via this system, stimulating both - and -adrenergic receptors. The bladder contains primarily receptors, stimulation of which causes relaxation of the detrusor muscle. Estrogen and progesterone receptors are present in the bladder and urethra, although their role in affecting continence has not been fully elucidated. Because the neurogenic control of micturition is so complex and depends on the interaction of so many factors, it is understandable that a host of general systemic diseases or diseases involving the nervous system may affect bladder control. These include, but are not limited to , diabetes mellitus, vascular diseases, obesity, cognitive disorders, normal pressure hydrocephalus, demyelinating diseases. The system can be disrupted by a stroke, which is a suprapontine lesions leading to loss of central inhibition, resulting in detrusor overactivity and reemergence of reflex micturition. A spinal cord injury above the lumbosacral level eliminates voluntary control of voiding, leading to acute urinary retention. Later, neurogenic detrusor overactivity occurs from spinal reflex pathways, which are uncoordinated, so the urethral sphincter may not relax simultaneously, leading to detrusorsphincter dyssynergia. Urinary incontinence in the elderly: physiology, pathophysiology, diagnosis, and treatment. Parasympathetic fibers arising in S2-S4 have long preganglionic fibers and pelvic ganglia close to the bladder and urethra. Sympathetic fibers that have long postganglionic fibers discharge norepinephrine to receptors, primarily in the bladder, and receptors, primarily in the urethra. A radical hysterectomy or subsacral cauda equine lesion might disrupt the local reflexes and lead to overflow incontinence because of detrusor and sphincter hyporeflexia. Compounds with atropine-like effects may interfere with the initiation of micturition, whereas those with cholinergic effects may cause bladder overactivity (Table 21. In summary, bladder control depends on the ability of the bladder to store urine under low pressure, which involves inhibition of the detrusor muscle and contraction of the smooth and striated urethral sphincters. Emptying the bladder requires coordination with pelvic floor and urethral sphincter relaxation and detrusor contraction. For urine to pass through the urethra, the maximum urethral pressure must be lower than the intravesical pressure. Intravesical pressure depends on the following: (1) the volume of fluid in the bladder, (2) the part of the intraabdominal pressure transmitted to the bladder, and (3) the tension in the bladder wall related to muscular and nervous system activity and elastic properties. The resting pressure in the bladder is between 20 and 30 cm H2O due to surrounding intraabdominal pressure with little or no pressure added from tension in the bladder wall in normal bladders. The intraurethral pressure depends on the following: (1) striated muscle fibers of the urethral wall, (2) smooth muscle fibers of the urethral wall (a circular and longitudinal layer), (3) vascular content of the urethral submucosal cavernous plexus, (4) passive elasticity of the urethral wall, and (5) the part of the intraabdominal pressure transmitted to the urethra. The urethra has primarily receptors from the sympathetic nervous system, which, when stimulated, cause contraction of the urethral sphincter. The urethral smooth and striated (skeletal) muscles add to the resting urethral tone, whereas the skeletal fibers react when intraabdominal pressure rises, such as with a cough. Anatomically, the exact border between the bladder and urethra is difficult to determine. The functional length of the urethra, however, is that part in which the urethral pressure exceeds the bladder pressure. Urethral pressure varies with age, increasing up to the age of 20 years and then gradually decreasing until menopause. Asmussen and Ulmsten (1976) have demonstrated that the highest pressure zone in the urethra is approximately at the midpoint of the functional urethral length.
Diseases
- Fitz-Hugh Curtis syndrome
- Hailey Hailey disease
- Kosztolanyi syndrome
- Palsy cerebral
- Polydactyly postaxial
- Dwarfism thanatophoric
- Chagas disease
- Potassium deficiency (hypokalemia)
Buy generic glipizide line
Hoffman and associates noted that 14 of 15 patients with inguinal lymph node metastases smaller than 36 mm2 survived free of disease at 5 years compared with 12 of 29 whose lymph node metastases measured more than 100 mm2 (Hoffman diabetes vertigo generic glipizide 10mg with visa, 1985). These results should be taken into consideration when planning additional therapy for patients with positive nodes. If tumor spread to the regional inguinofemoral nodes is identified, further treatment should be considered. If only one node is microscopically involved with tumor and the woman has undergone a complete lymph node dissection of the groin, no further therapy is usually needed, particularly if only a small volume is present. However, if one node is microscopically positive and the woman has undergone a superficial inguinofemoral lymph node dissection, many clinicians would be uncomfortable not treating the groin with adjuvant radiation therapy. If three or more nodes are involved, pelvic radiation as outlined is usually prescribed. For patients with only two nodes involved, the decision for further therapy will depend on the location of the nodes, extent of groin dissection performed, and size of the metastatic deposit of tumor, although most clinicians would opt for radiotherapy in such cases. In such cases, it may be necessary to remove the anus or urethra as part of a primary operative procedure, in which case diversion of the urinary or fecal stream is required (see the discussion of exenterative surgery for carcinoma of the cervix in Chapter 29, Malignant Diseases of the Cervix). For tumors that encroach on the urethra or anus, making procurement of negative margins improbable, multidisciplinary organ-sparing approaches may be used in an effort to reduce the morbidity of exenterative procedures. A useful therapeutic approach has been to treat large vulvar tumors with external radiation and then, after the tumor has been reduced in size, to remove the residual tumor surgically, usually by radical vulvectomy. External radiation is used to deliver approximately 4000 cGy to the tumor and 4500 cGy to the pelvis and inguinal nodes. The operation is usually performed approximately 5 weeks after the completion of radiation therapy. Although a large series of patients have not been treated by this technique, a sufficient number have been treated to demonstrate that marked tumor regression does occur. The primary cancer can be eradicated by a procedure that does not require diversion of the urine or feces. Boronow and associates initially summarized the treatment of 26 patients with primary carcinoma of the vaginal vulvar area with this technique and noted a 5-year survival rate of 80% (Boronow, 1987). Recurrences are more likely if the resection margins were within 1 cm of the tumor. Actuarial 3- and 5-year survival rates in this small group were 59% and 49%, respectively. Other complications reported include stenosis of the introitus, urethral stenosis, and rectovaginal fistula, but this technique is an effective alternative to primary exenteration for large vulvar vaginal carcinomas and is preferred in most treatment centers, although success with exenteration can occasionally be achieved. Radiation Therapy and Recurrences In a few cases, the medical condition of the woman precludes surgery, and radiation therapy may be used as the sole treatment. However, the vulvar skin is prone to radiation dermatitis, fibrosis, and ulceration, making irradiation as the sole form of therapy a less desirable treatment. Therefore irradiation is seldom used as the sole treatment of carcinoma of the vulva. Piura and colleagues analyzed 73 patients whose disease recurred only on the vulva (Piura, 1993). Salvage was achieved with wide radical local excision, which appeared to be successful in 30 patients in whom the recurrence was only on the vulva. As may be expected, the risk of recurring carcinoma rises as the stage of the disease increases. Radiation therapy or additional operations for local vulvar recurrences usually provide effective control and yield 5-year survival rates of approximately 50%. The risk of recurrence of the disease in the vulva requires careful attention to the surgical resection margins at the time of initial operation. Combined chemotherapy and radiation has been used for primary treatment of late-stage advanced vulvar tumors, as noted. It has also been applied to recurrences, especially those near the anus or urethra. Radiation alone may also be used for vulvar recurrences, although chemoradiation would appear to be a more effective choice. Treatment of patients with disseminated disease requires chemotherapy but, unfortunately, no chemotherapeutic regimen has been successful for treatment of this disease. Squamous cell carcinomas of the female genital tract have generally not been responsive to cytotoxic chemotherapy; the protocols followed are similar to those described for recurrent squamous cell carcinomas of the cervix (see Chapter 29). Quality of Life and Vulvar Carcinoma There have been few studies regarding quality of life in patients with vulvar cancer. Body image disturbance is significant and may account for decreased or absent sexual activity in women who have undergone vulvectomy. Interestingly, Green and colleagues noted that the extent of surgery or type of vulvectomy performed does not correlate well with the degree of sexual dysfunction (Green, 2000). They demonstrated a significant need to address sexual problems with all women undergoing any type of vulvectomy. Perhaps this tool can be used to help assess quality of life and also facilitate vital communication about quality-of-life issues in women with this disease. Lymphatic Mapping and Sentinel Lymph Node Biopsy As noted, regional lymph node dissections are routinely performed in the surgical treatment of vulvar cancer because the status of regional lymph nodes is essential for therapeutic planning and overall prognosis. Lymphatic mapping and sentinel lymph node biopsy, as used for the treatment of patients with melanoma and breast cancer, are appealing techniques for patients with vulvar cancer. The sentinel nodes are those that directly drain the primary tumor and are thought to predict the metastatic status of the upper echelon or nonsentinel nodes in the groin. If the sentinel node is negative, in theory, all the other groin nodes would also be negative and surgeons could abandon full groin dissections, thereby greatly reducing the associated morbidities of lymphocyst, lymphedema, and wound separation. Women enrolled in this study underwent a sentinel node biopsy, with omission of complete inguinofemoral lymphadenectomy if no metastatic disease was found. Patients with negative sentinel nodes were triaged to no further therapy and observed for recurrence. In an accumulation of data from smaller studies on the subject, Frumovitz and colleagues reviewed the combined data on 279 patients with vulvar cancer who had undergone lymphatic mapping and sentinel lymph node identification (Frumovitz, 2008). They found the overall sensitivity of the sentinel node for detecting metastatic disease in patients with vulvar cancer to be 97. Although these numbers are promising, at this time, lymphatic mapping and sentinel lymph node biopsy are considered experimental, with the standard of care remaining full inguinofemoral node dissection. However, staging is not as useful a prognostic indicator as is the depth of invasion. A staging system for vulvar melanoma analogous to that used by Clark for cutaneous melanomas has been adopted. These tumors are treated similarly to primary squamous cell carcinoma of the vulva; radical vulvectomy with bilateral inguinofemoral lymphadenectomy is the treatment of choice. Basal Cell Carcinoma Basal cell carcinoma can arise in the vulva, as it can arise in the skin elsewhere in the body. Therapy consists of wide local excision of the lesion, which is generally ulcerated. They are a special variant of squamous cell cancer, with distinctive histologic features. Histologically, they consist of mature squamous cells and extensive keratinization, with nests that invade the underlying vulvar tissue. It is often necessary to perform multiple biopsies of the condylomatous lesion to establish a diagnosis of malignancy. Radiation therapy is ineffective and can worsen the prognosis by causing anaplastic changes in the tumor and is therefore contraindicated. In 24 cases of verrucous carcinoma, Japaze and coworkers noted no lymph node metastases (Japaze, 1982). Recurrences developed in nine patients, five of whom had previous radiation therapy. Depending on the size and location of the tumor, simple vulvectomy may be needed, but a radical vulvectomy or inguinal node dissection is not indicated. The 17 patients treated surgically and reported by Japaze and colleagues had a 5-year survival rate of 94%. This is particularly important when dealing with a malignant-appearing tumor from a biopsy specimen that has been reported as benign, which can lead to incorrect therapy for condyloma acuminatum. Conversely, too shallow a biopsy may fail to show areas of squamous cell carcinoma that can coexist with verrucous carcinoma, but in the presence of areas of squamous cell carcinoma, local excision is inadequate therapy. Verrucous tumors with squamous cell carcinoma elements can metastasize to regional nodes; these tumors should not be treated as true verrucous carcinomas. As is true elsewhere in the body, melanomas arise from junctional or compound nevi.
Purchase glipizide in united states online
Abdominal Pregnancy this is a rare situation; from an analysis of 11 abdominal pregnancy-related deaths and an estimated 5221 abdominal pregnancies in the United States diabetes mellitus natural treatment buy glipizide us, it has been estimated that there were 10. There were five cases of an intraabdominal abscess in the 14 patients in whom the placenta had been left in situ. Maternal outcomes were documented in 26 cases with seven deaths; 27 fetal outcomes were documented in 22 cases with three fetal deaths (13. Treatment is always surgical and interventional radiology and endovascular surgery must be considered for assistance. Cervical Pregnancy Surgical treatment of cervical ectopic pregnancies consists of evacuation with dilatation and curettage or vacuum aspiration. This often occurs after methotrexate treatment, which facilitates the decrease in size and vascularity of the pregnancy. Cesarean Scar Pregnancy Surgical treatment of cesarean scar pregnancies also consists of evacuation with dilatation and curettage or vacuum aspiration under transabdominal ultrasound guidance. To prevent hemorrhage, temporary laparoscopic bilateral artery occlusion with silicone tubing has been described (Wang, 2015). Hysteroscopy coupled with curettage followed by uterine artery embolization is also an alternative surgical approach for these cases (Qian, 2015). Treatment of tubal ectopic pregnancy by salpingotomy with or without tubal suturing and salpingectomy. They concluded that this procedure is safe and effective in interstitial pregnancy with the advantage of preserving reproductive function compared with cornual resection (Choi, 2009). The ectopic is evacuated after a linear incision is made and the defect is sutured as shown. After fimbrial expression or tubal abortion, the incidence of persistence ranges from 12% to 15%. Persistent tubal ectopic gestation: patterns of circulating beta-human chorionic gonadotropin and progesterone, and management options. Surgical management should be utilized for women who develop symptoms of persistent lower abdominal pain. Graczykowski and Mishell performed a randomized trial in which a single dose of methotrexate or placebo was given within 24 hours after salpingostomy. For medical and surgical therapy, rates of tubal pregnancy (62% to 90%) and recurrence rates (8% to 15%) are comparable. The multidose regimen is more successful but involves more dosing and therefore potentially has more side effects. It also includes the use of leukovorin (folinic acid), an antagonist to Obstetrics & Gynecology Books Full 17 Ectopic Pregnancy Table 17. Mol and associates performed a systematic review and meta-analysis comparing laparoscopic salpingostomy and methotrexate. They concluded that the clinical treatment is more cost effective with less hospitalization, faster recovery, and no significant difference in subsequent spontaneous conception rates or recurrent ectopic pregnancies (Mol, 2008). A two-dose regimen has been proposed as well, which is intermediate between the high and multiple-dose regimens. Between 3 and 7 days after initiating therapy, severe pelvic pain lasting up to 12 hours frequently occurs. This symptom, probably caused by tubal abortion, must be differentiated from the symptoms of tubal rupture. Serial monitoring of vital signs and measurement of hematocrit levels are helpful. If the woman remains hemodynamically stable and the pain disappears, a tubal abortion has probably taken place and no further therapy is necessary. To avoid the toxicity of systemic methotrexate administration, a smaller dose of the drug has been administered directly into the tube with either laparoscopic or ultrasound visualization. Because of the lower success rate and need for direct needle placement with local injection, most clinicians are now using systemic methotrexate. There have also been several reports of direct intratubal injection of other substances, including potassium chloride, hypertonic glucose, and prostaglandins, but use of these agents is generally less successful than the use of methotrexate. Methotrexate plays an important role in the treatment of the nontubal ectopic pregnancies. It can be used be administrated intramuscularly or intraamniotically and may also be combined with other therapeutic means, such as intraamniotic administration of potassium chloride, vaginal mifepristone, or uterine artery embolization. Some new drugs are being studied for the clinical management of the ectopic pregnancies, with drugs such as selective progesterone receptor modulators. Expectant Management Although this is not a preferred plan of management, it is useful to know that certain ectopics may resolve without treatment. This group comprised one fourth of all the women with the diagnosis of ectopic pregnancy seen at their institution during 3 years. It has been reported that when serial sonography is performed, some of the tubal pregnancies can increase in size and become more vascular as they resolve. In this scenario, methotrexate therapy is preferred unless the ectopic pregnancy involves a known hydrosalpinx, in which case salpingectomy should be preferred. The Cochrane database has shown that methotrexate therapy is equivalent to laparoscopic surgery; it has also been deemed more cost effective. Overall, the subsequent conception rate in women following all ectopic pregnancies is about 60%, with the other 40% remaining infertile. About one third of the pregnancies occurring after the initial ectopic pregnancy or another ectopic pregnancy, and one sixth are spontaneous abortions. Therefore only about half the pregnancies are viable, and only one third of all women with an ectopic pregnancy have a subsequent live birth. The subsequent fertility rate is significantly Obstetrics & Gynecology Books Full 17 Ectopic Pregnancy 367 1. On the other hand, women with high parity (more than three births) who develop an ectopic pregnancy have a relatively high rate, about 80%, of subsequent conception. The subsequent conception rate is lower in women who have a history of salpingitis, as well as those who have visual evidence of pathologic changes in the opposite oviduct as a result of previous salpingitis. Future fertility is significantly higher in women who have an unruptured tubal pregnancy than in those with tubal rupture, so early diagnosis is desirable. Only 65% of women with a ruptured ectopic pregnancy subsequently conceive, whereas the conception rate in women with an unruptured tubal pregnancy is approximately 82%. In two large groups of women with unruptured ectopic pregnancy treated by conservative surgery, a high incidence of subsequent fertility (80% to 86%) and a low incidence of subsequent ectopic pregnancy (11% to 22%) have been reported. Most studies in the literature indicate that the overall subsequent ectopic pregnancy rate is similar among women treated by salpingostomy or salpingectomy, and the data suggest that conservative surgery is most beneficial for women with evidence of contralateral tubal damage or a history of infertility. When comparing salpingostomy outcomes after laparoscopy or laparotomy, the women treated by laparoscopy conceived sooner than those treated by laparotomy, and there were more ectopic pregnancies in the latter group. In women with an unruptured ectopic a history of infertility (particularly resulting from tubal disease), previous salpingitis, a prior ectopic pregnancy, or the presence of only one tube were each independent factors that decreased the rate of subsequent fertility and also increased the risk of subsequent ectopic pregnancy. It has been suggested therefore that if more than one of these factors were present it would be preferable to perform a salpingectomy than to perform a salpingostomy, as 80% of the recurrent ectopic pregnancies occurred in the same tube as the initial ectopic pregnancy. The rate of repeat ectopic pregnancies after a single ectopic pregnancy ranges from 8% to 27%, with a mean of about 20%. Because the overall pregnancy rate is in the 60% to 80% range, about one of three to four conceptions after an ectopic pregnancy is a repeat ectopic pregnancy. Women with an ectopic pregnancy who become pregnant again should be monitored by ultrasound early in pregnancy. Only about one of three nulliparous women who have had an ectopic pregnancy ever conceives again (35%), and about one third of these conceptions are an ectopic pregnancy, for an overall rate of 13%. Risk factors for a repeat ectopic pregnancy were ectopic pregnancy as the first pregnancy, age younger than 25, evidence of tubal infection, and history of infertility (see Table 17. With two ectopic pregnancies, the subsequent fertility rate decreases even further. There have been several reports on salpingostomy or salpingotomy in women with an unruptured tubal pregnancy in the only remaining tube. In the great majority of the subjects, the other tube had been removed because of another ectopic gestation. About one fourth of the women who conceived had a subsequent ectopic pregnancy, which is similar to the rate among all ectopic pregnancies. Thus conservative surgery or medical therapy may be considered when an unruptured ectopic pregnancy occurs in the only remaining tube.
10mg glipizide mastercard
These changes diabetes diet review order glipizide online pills, unusual in adolescence, are most common in women of reproductive age (20 to 50 years) and unusual after menopause unless associated with exogenous hormone replacement. Clinical signs include increased breast engorgement and density, excessive breast nodularity, fluctuation in the size of cystic areas, increased tenderness, and infrequently spontaneous nipple discharge. Associated mastalgia is bilateral, often difficult to localize, and most frequent in the upper, outer breast quadrants. The pathophysiology that produces these symptoms and signs includes cyst formation, epithelial and fibrous proliferation, and varying degrees of fluidretention. The latter two conditions have symptoms that are not cyclic and unrelated to the menstrual cycle. Note: Fibrosis (F), adenomatous changes with increased ductal tissue (A), and cysts (C). There may be multiple areas of seemingly ill-defined thickening or areas of palpable lumpiness that seem more two-dimensional than the three-dimensional mass usually associated with a carcinoma. There are three general clinical stages of fibrocystic change, with each stage having characteristic histologic findings. Clinically these stages are variable and overlap, but they are described to assist in the understanding of the natural history. The first stage, mazoplasia (mastoplasia), is associated with intense stromal proliferation and occurs in the early reproductive years (20s). Breast pain is noted primarily in the upper, outer breast quadrants with most tenderness in the axillary tail. The cystic phase is the last stage and typically occurs another decade later in women in their 40s. Typically there is no breast pain unless a cyst increases rapidly in size with associated sudden pain, point tenderness, and a lump. Although breast cysts may occur at any age, they are generally simple and may be managed with aspiration alone. Complex cysts have internal septations, debris, or solid components and may require core needle biopsy if stability cannot be documented. The fluid aspirated from a large cyst is typically straw colored, dark brown, or green, depending on the chronicity of the cyst. Women with a clinical diagnosis of fibrocystic change have a wide variety of histopathologic findings. The histology of fibrocystic change is characterized by proliferation and hyperplasia of the lobular, ductal, and acinar epithelium. Usually, the proliferation of fibrous tissue occurs and accompanies epithelial hyperplasia. Many histologic variants of fibrocystic change have been described, including cysts (from microscopic to large, blue, domed cysts), adenosis (florid and sclerosing), fibrosis (periductal and stromal), duct ectasia, apocrine metaplasia, intraductal epithelial hyperplasia, and papillomatosis. Ductal epithelial hyperplasia with atypia and apocrine metaplasia with atypia are the most prominent histologic findings directly associated with the subsequent development of breast carcinoma. If either of these two conditions is discovered on breast biopsy, the chance of future breast carcinoma is increased fivefold. Clinical management of fibrocystic change is age dependent and includes appropriate use of breast imaging. First and foremost, malignancy should be excluded, particularly in the presence of a mass or with a concerning or uncertain examination. Initial therapy for fibrocystic change involves mechanical support utilizing a firm support or sports bra. Although confirmatory medical studies evaluating the benefit of these dietary changes are lacking, there seems to be little harm to trying this inexpensive option for 3 to 6 months. The only dietary substance that seems, at this time, to correlate with fibrocystic symptoms is dietary fat, particularly saturated fat. Incorporating a low-fat, nutrient-dense diet makes sense, and limiting intake of saturated fat intake should be considered as a simple therapeutic tool for the management of women with symptomatic, refractory fibrocystic changes. Additionally, some advocate limiting or eliminating alcohol consumption to lessen estrogen levels. Diuretics are sometimes prescribed during the premenstrual phase and may lessen symptoms of breast discomfort/engorgement. Oral contraceptives or supplemental progestins administered during the secretory phase of the cycle have also been used to treat fibrocystic changes. Oral contraceptives are reported to decrease the incidence of fibrocystic changes by 30% (Schindler, 2013). Unfortunately, virilizing side effects such as hirsutism, acne, and voice changes frequently limit its use. Oral tamoxifen, 20 mg daily, is superior to placebo in randomized, double-blind trials, and pain relief is reported to be sustained in 72% of women for >1 year after discontinuation. Tamoxifen administration restricted to the luteal phase of the menstrual cycle abolishes pain in 85% of women; however, adverse side effects are frequent (21%). Breast pain is typically divided into cyclic pain, related to the menstrual cycle, and noncyclic pain. Noncyclic breast pain should be evaluated, particularly in older women, as there is a small association with malignancy. Thedifferentialdiagnosis includes a cyst, chest-wall pain, radicular pain, costochondritis, mastitis, pregnancy-related pain, prolactinomas, and medication exposure (Box 15. Breast cysts occur in as many as 7% of women during their lifetime and may be therapeutically aspirated if they are simple. Recurring simple cysts can be followed with ultrasound, typically withholding repeat aspiration for symptomatic cysts. Complex cysts should have a tissue diagnosis with core needle biopsy if they are symptomatic or show progressive changes on serialsonography. Breast pain treatment is directed at the cause; however, nonsteroidal anti-inflammatories are often useful when pain is idiopathic. Although decreasing in overall incidence, mastitis, infection of the ductal systems or smaller sebaceous glands, is most commonly related to Staphylococcus aureus. Continued breast-feeding or manual pumping of the affected breast is recommended to decrease engorgement. Obviously, one should always consider and exclude the presence of malignant breast disease, particularly inflammatory cancer. Nipple piercing, particularly in smokers, is associated with mastitis and a 20-fold increase in subareolar abscess formation. As with any infection, the clinician should strongly consider removal of the foreign body. The American College of Obstetricians and Gynecologists recommends counseling women who are planning to get piercings to have a prepiercing hepatitis-B vaccine and tetanus vaccinations. Thisdisease may present with a mass, abscess, inflammation, or granuloma formation. The granulomas are often found within the lobules and on biopsy are noted to be sterile. Skin scarring and residual small abscesses may remain, frequently necessitating surgical treatment. Chronic inflammatory diseases, such as lupus, sarcoid, and Wegner granulomatosis, are rare causes of noninfectious mastitis, and evaluation for these diseases should be performed if antibioticsarenoteffective. Importantly,anybreastinflammationnot responsive to adequate antibiotic treatment warrants a tissue diagnosis. Core needle biopsy is frequently performed when there is a lack of response to antibiotics. The diagnosis is frequently made when the biopsy demonstrates sterile granulomas after excluding other causes of granulomatous mastitis such as tuberculosis. The majority have a benign etiology; however, 55% present with a coexisting mass of which 19% are malignant. Age is important, as an underlying malignancy is present in 3% of women under 40, 10% of women between 40 and 60, and 32% of women over 60 when nipple discharge is the only presenting symptom. Intraductal papilloma and fibrocystic changes are the two most common causes of spontaneous nonmilky discharge. Galactorrhea is likely when breast discharge is bilateral, copious, pale milky in color, and occurs from multiple ducts.
Buy discount glipizide 10mg on-line
Generally blood sugar under 100 discount 10 mg glipizide, if the supports of the bladder neck are adequate, the urethra is adequately supported. If a cystocele and urethrocele are present, it invariably follows that the bladder neck is not supported. Although determining the type of anterior vaginal wall prolapse-central or lateral/paravaginal-is no longer as important as once thought, a ring/sponge forceps can be used with the split speculum. If supporting the lateral anterior vaginal walls to the arcus tendineus fascia pelvis with an open ring forceps causes the cystocele to disappear with straining, a paravaginal defect is present. If apical support with the ring forceps causes the cystocele to resolve with straining, an apical or central defect is present. Pelvic floor muscle bulk, symmetry, and function should be assessed during the bimanual exam by asking the woman to tighten her muscles like she is trying to inhibit voiding or flatus. Urethroceles should be differentiated from inflamed and enlarged Skene glands and urethral diverticula. Cystoceles must be differentiated from bladder tumors and bladder diverticula, both of which are rare but may occur. With diverticula or Skene glands, it may be possible to express pus from the urethra when they are palpated. In such cases, gonococcal, chlamydial, and other bacterial infections should be considered. Occult stress urinary incontinence and the effect of vaginal vault prolapsed on abdominal leak point pressures. With a comfortably full bladder (ideally around 300 mL), usually in the standing position, the patient is asked to cough while the prolapse is replaced in its normal anatomic position. If she leaks during this test, she has latent or occult stress urinary incontinence that is likely to present after surgical repair of the prolapse. Women with negative preoperative prolapse reduction stress tests in this trial had a 38. With this information, the patient and physician can decide whether or not to do an anti-incontinence procedure at the time of prolapse repair. Management Treatment of anterior vaginal wall prolapse may be nonoperative or operative depending on patient preferences and goals. If the patient is not bothered by the prolapse, it can be left alone and managed expectantly unless it is causing urinary retention or renal hydronephrosis. Pelvic floor physical therapy can also treat associated urinary, bowel, and sexual dysfunction. In one study, 447 women were randomized to receive individualized pelvic floor muscle training or a prolapse lifestyle advice leaflet with no muscle training (control group). This supervised training led to a 44% increase in muscle strength, a 15% increase in muscle thickness, a decreased levator hiatus area, shortened muscle length, and elevation of the bladder and rectum position. It took 6 months of muscle hypertrophy training to achieve these results, so this option requires motivated patients. A follow-up study by the same group reported that 11 (19%) of women in the exercise group improved one stage on the Pelvic Organ Prolapse Quantification system compared with 4 (8%) of controls. This did correlate with reduced frequency and bother of vaginal bulging and heaviness by 74% and 67%, respectively. Women who have performed Kegel exercises on their own and have not improved may still benefit from working with a physical therapist. In an older woman, the use of a vaginal estrogen product may improve vaginal atrophy and patient comfort if the prolapsed vaginal epithelium is irritated or ulcerated. Behavioral modification may help urinary symptoms such as urgency and will be discussed in Chapter 21. E of a large tampon (pessaries are discussed in more detail under Uterine Prolapse in this chapter). If pelvic floor strengthening and pessary do not adequately control the prolapse symptoms or if a patient declines these options, then surgery can be considered. A young woman should be encouraged to avoid operative repair until she has completed her family. If pessary management is not adequate and the abnormality is so uncomfortable that repair must be performed before childbearing is complete, cesarean delivery should be considered for subsequent pregnancies. Operative repair of anterior vaginal wall prolapse is generally performed in conjunction with the repair of all other pelvic support defects. It is unusual for anterior supports of the vagina to relax without an accompanying relaxation of the apical compartment. Repair therefore usually consists of an anterior colporrhaphy as well as correction of uterine descensus or apical defect posthysterectomy. Anterior wall repair (colporrhaphy) is performed by plicating the connective tissue of the anterior vaginal in the midline. After placement of a Foley catheter, the vaginal epithelium is incised from just distal to the anterior lip of the cervix or cuff to just proximal to the urethrovesical junction or bladder neck, which can be identified using the inflated bulb of a Foley catheter. If the woman has undergone a hysterectomy in the past, the incision may be made approximately 1 to 1. The longitudinal incision is made by through the vaginal epithelium to but not through the underlying connective tissue. When the longitudinal incision is complete, the cut edge of the vagina is held under tension, and the fibromuscular tissue underneath (sometimes called pubocervical fascia, although it is technically not fascia) is separated from it using sharp and blunt dissection. The connective tissue is imbricated in the midline by placing absorbable or delayed absorbable 0 or 2-0 sutures laterally on each side of the defect and tying them in the midline. The excess vaginal epithelium can be trimmed and then closed over the repair using absorbable suture such as 2-0 polyglycol. C, Dissection of the vaginal epithelium off the underlying connective tissue and fibromuscular layer. Midurethral sling surgery for associated stress urinary incontinence or stress urinary incontinence on prolapse reduction (occult or latent stress incontinence) can then be performed through a separate incision over the midurethra. In this case, the longitudinal incision can be continued under the urethra and the Kelly plication performed prior to the anterior colporrhaphy. A suture over the bladder neck (Kelly stitch) brings together the connective tissue on either side. The stitch should be placed as lateral as possible without tension, parallel to the urethra on each side, and then tied. The suprapubic technique is simple to use and seems to have a lower incidence of infection than does transurethral catheterization, but patients may complain of extravasation of urine around the site and occasionally of hematoma formation. On the other hand, women should be able to resume other nonstrenuous normal activities as soon as they feel ready. However, although it may improve the anatomic result compared to traditional native tissue anterior colporrhaphy, it is associated with increased complications such as mesh exposure, pelvic pain, and dyspareunia. A 2013 Cochrane Database systematic review concluded that the risk of recurrent prolapse symptoms and anterior vaginal wall prolapse on examination are decreased with the use of biologic or synthetic grafts, but disadvantages include longer operative times, greater blood loss, prolapse in other areas of the vagina, new onset stress urinary incontinence, and an 11% rate of vaginal mesh exposure (Maher, 2013). The 5-year cumulative risk for repeat surgery has been found to be higher after anterior prolapse surgeries that involved mesh than those that did not (15. Certainly careful patient selection, detailed patient counseling, and a skilled surgeon with proper training is needed for these procedures and to manage the complications. Recurrent anterior vaginal wall prolapse remains a frustrating problem for gynecologic surgeons and patients. Because there is a risk of urinary retention immediately after surgery, a voiding trial should be performed after removing any vaginal pack and prior to discharging the patient. For the back fill, the bladder is retrograde filled with 300 mL of sterile saline, and then the catheter is removed. For auto fill, the catheter is removed, and the bladder is allowed to fill spontaneously. The voided volume is measured, and the residual volume is measured with a bladder ultrasound or straight catheterization in either type of voiding trial, or it can calculated after a back fill. The patient can be considered to have passed the voiding trial if she voids at least two thirds of the total bladder volume. Two randomized trials of the two voiding trial techniques revealed that the back fill technique was a better predictor of adequate postoperative bladder emptying than the auto fill technique, and it was also preferred by patients (Pulvino, 2010; Geller, 2011). Notably, 40% or more of patients had an unsuccessful voiding trial after prolapse or incontinence surgeries and were discharged home with a catheter. It is helpful to counsel women on this high chance of going home with a catheter, given short hospital stays after these procedures.