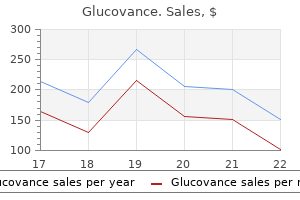
Buy genuine glucovance online
Type B is responsible for about 10% of infections in humans treatment spinal stenosis buy glucovance 400/2.5 mg free shipping, but is not usually associated with epidemics. Type A virus is also classified by the presence of two distinct glycoprotein surface antigens, the hemagglutinin and neuraminidase antigens. Hemagglutinin is responsible for viral binding to cell receptors, and neuraminidase is responsible for the release of virus after replication from the cell. An antigenic "shift," with the development of a new hemagglutinin or neuraminidase antigen, results in pandemic infection at infrequent intervals. In one 10-year study among 209 infants in the first year of life, influenza A (H3N2) occurred most commonly, followed by influenza B and influenza A (H1N1), with infections in 178, 96, and 26 infants. There has been increasing concern that the genome of avian H5N1 influenza A could mix with human influenza A and be able to be transmitted directly from human to human and be able to cause widespread disease. Influenza is rapidly and easily spread person to person by aerosol droplet or by contact with contaminated secretions. Viral shedding and infectiousness are greatest in the 24 hours before onset of symptoms and at the peak of symptoms. The virus may survive in the environment, although the role of fomites in transmitting infection is unclear. School-age children have the highest attack rate and serve as a source of spread to adults and younger children. Infants who are born to pregnant women with influenza have an increased risk of preterm birth, low birth weight, and small size for gestational age, especially when the mother is severely ill. The decreased tidal volume and increased cardiac output, as well as the immunologic changes of pregnancy, put the pregnant woman at higher risk of severe illness requiring hospitalization. All women who may be pregnant during an influenza season should receive inactivated trivalent vaccine. Additionally, the neonatal antibody level is much higher and the infant is much less likely to develop influenza in the first 6 months of life. Infection is less common in the first 6 months of life and usually less symptomatic, probably reflecting the transplacental transference of maternal antibody during pregnancy, which may protect the infant for the first 6 months, and antibody transferred via breast milk. Infants may present with high fever and an upper respiratory tract infection, however, and infection may be indistinguishable from bacterial sepsis. Infants younger than 6 months have also been reported to have the highest mortality. In the 2003 to 2004 influenza season, the mortality of infants younger than 6 months was 0. One third of the infants died at home, and one fourth had co-infections with bacteria. Only one third had conditions recognized as putting the infant at high risk, such as pulmonary or cardiovascular disease or immunosuppression. In a prospective study of the first year of life, one third of the infants were infected, but only 40% of the infants were infected in the first 6 months of life, and most lower respiratory tract disease and otitis media occurred in the latter 6 months, when the transferred maternal antibody would be expected to have waned. One third of infants presenting to the emergency department during influenza epidemics had influenza infection, although they frequently had no respiratory symptoms. In contrast, one third of the infants presenting with a community-acquired pneumonia were also infected with influenza. Low rates of immunization among staff members played a significant role in these epidemics. Prematurity and pulmonary disease, particularly bronchopulmonary dysplasia, seem to be risk factors. It is now approved for use in children as young as 2 weeks of age and up to 1 year of age, at a dosage of 3 mg/kg twice a day for 5 days. Inactivated influenza vaccine, however, is not licensed for infants 6 months or younger because it has not been shown to be immunogenic even though infants, especially infants with bronchopulmonary dysplasia, may be at greater risk than older children. Instead, the risk of exposure to these infants should be minimized by immunizing health care workers and family members and other close contacts. Vaccination of preterm infants after 6 months of age, even in the presence of prolonged hypogammaglobulinemia, does result in a good antibody response. It was initially called swine flu because it seemed to be genetically related to the influenza viruses that occurred in pigs in North America. It has now been shown, however, that novel H1N1 influenza A is a re-assortment virus of two genes that circulate in swine in Europe and Asia and bird (avian) genes and human genes. In April 2009, the United States declared a public health emergency and began working on pandemic alert level; this was based on the spread of the virus rather than its severity. The virus continued to spread, and outbreaks occurred in the United States throughout the summer in 2009. In the Southern Hemisphere, when it entered its influenza season in 2009, cases of novel H1N1 virus spread in addition to the regular seasonal influenza virus. The novel H1N1 virus seems to spread via the same mechanisms as the regular influenza virus, by large particle respiratory droplet transmission, which occurs when a person coughs or sneezes. Influenza virus may also survive and remain infectious on environmental surfaces for 2 to 8 hours. Most importantly, hand washing with soap and water and with alcohol-based hand cleaners is very effective. Individuals should cover their nose and mouth with a tissue when coughing or sneezing; wash their hands frequently; and avoid touching their eyes, nose, and mouth. The symptoms are the same as for seasonal influenza: fever, cough, sore throat, aches, chills and fatigue, headache, running or stuffy nose, and vomiting and diarrhea. Complications may be mild (otitis, febrile seizures) or severe (bacterial co-infection, pneumonia, or worsened baseline conditions) and may progress very rapidly. The novel H1N1 influenza virus is sensitive to the neuraminidase inhibitors, zanamivir and oseltamivir, but resistant to the adamantine medications, amantadine and rimantadine. Treatment should be started as soon as possible after onset of symptoms in all hospitalized patients with suspected, probable, or confirmed novel H1N1 infection, and in patients who are in a high-risk group for seasonal influenza complications. Treatment benefit seems to be greatest when treatment is started within 48 hours of symptom onset, but data from patients with seasonal influenza indicate that there may be some decrease in mortality and hospital stay even when started after 48 hours. There are limited safety data for oseltamivir in children younger than 1 year of age, a group that has had significant morbidity and mortality from seasonal influenza. Premature infants have immature renal function and may have slower clearance of oseltamivir. There are insufficient data to recommend a dose, and drug concentrations that have been measured are highly variable. Pregnant women infected with H1N1 influenza virus in 2009 had higher rates of hospitalization and represented about 6% of all the deaths in the United States. Risk factors for severe disease include obesity, asthma, multiparity, and multiple births. Pregnant women should be vaccinated during prenatal visits and may receive both seasonal flu vaccine and H1N1 flu vaccine at the same time in different sites (one in each arm), when both viruses are in season. Vaccination of the pregnant woman may offer some protection to her newborn infant, which is particularly important, as the vaccine is not licensed for infants less than 6 months of age. Certainly, all caregivers of infants less than 6 months should also be vaccinated in an effort to prevent them from bringing influenza to the infant. Pregnant women should receive the monovalent injectable, inactivated vaccine with or without thimerosal preservative. Breastfeeding is likewise compatible with vaccination and may offer some antibody protection to the infant. The virus has not been shown to cross the placenta to date, but the newborn may be exposed to contaminated secretions at birth. Thus the newborn should be considered exposed rather than infected, and should be carefully observed. The baby may be separated from the mother in an incubator in the same room, or the baby may be put in a separate room until the mother has been treated with antivirals for at least 48 hours and has been free of fever while off antipyretics for at least 24 hours, and can control her cough and respiratory secretions. Breastfeeding should be supported, and the breast milk should be used to feed the newborn. In the 2009 pandemic, more than half of nurseries restricted breastfeeding by the mother while she was ill.
Podophyllum hexandrum (Podophyllum). Glucovance.
- Dosing considerations for Podophyllum.
- Are there safety concerns?
- Treating human papilloma virus (genital and anal warts).
- What is Podophyllum?
- How does Podophyllum work?
- Raised areas on the tongue and mouth in people with immune system diseases (hairy leukoplakia), liver problems, cancer, and other conditions.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96783
Cheap 400/2.5 mg glucovance mastercard
All infants were receiving cow milk formula medicine allergic reaction buy 500/5mg glucovance fast delivery, which provided 3 to 4 g of protein per kilogram of body weight per day. This observation suggests that excessive protein content of cow milk formula results in endogenous acid production beyond the excretory capacity of the premature kidney, which is limited by urinary bicarbonate losses and reduced phosphate excretion. Kalhoff and colleagues28 also described a decrease in renal net acid excretion in infants with low birth weight and examined the effect of bicarbonate supplementation. When randomly assigned to control or bicarbonate therapy groups, infants in the control group who had a persistent urine pH less than 5. In recent years late metabolic acidosis is less common, which may reflect increased human milk intake and alterations to the composition of formulas for preterm infants. When metabolic acidosis occurs, it is often self-limited and resolves with further renal maturation. Isotonic versus hypotonic fluid supplementation in term neonates with severe hyperbilirubinemia-a double-blind, randomized, controlled trial. Impact of changes in serum sodium levels on 2-year neurologic outcomes for very preterm neonates. The effects of thermal environment on heat balance and insensible water loss in low-birthweight infants. Combined effect of radiant warmer and phototherapy on insensible water loss in low-birthweight infants. Effect of fluid administration on the development of symptomatic patent ductus arteriosus and congestive heart failure in premature infants. High-volume fluid intake predisposes premature infants to necrotising enterocolitis. Phases of fluid and electrolyte homeostasis in the extremely low birth weight infant. Transepidermal water loss and skin hydration in preterm infants during phototherapy. A randomized controlled trial of fluid supplementation in term neonates with severe hyperbilirubinemia. Acetazolamide therapy for hypochloremic metabolic alkalosis in pediatric patients with heart disease. Effects of prenatal steroids on water and sodium homeostasis in extremely low birth weight neonates. Type 2 pseudohypoaldosteronism: new insights into renal potassium, sodium, and chloride handling. Regulation of sodium metabolism and extracellular fluid volume during development. New insights into the pathogenesis of renal tubular acidosis-from functional to molecular studies. Renal handling of water and sodium in infancy and childhood: a study using clearance methods during hypotonic saline diuresis. Extracellular fluid volume changes in very low birth weight infants during first 2 postnatal months. Sodium balance and extracellular volume regulation in very low birth weight infants. Randomized controlled trial of oral versus intravenous fluid supplementation on serum bilirubin level during phototherapy of term infants with severe hyperbilirubinaemia. Studies on the renal concentrating and diluting mechanisms in the premature infant. Type I pseudohypoaldosteronism includes two clinically and genetically distinct entities with either renal or multiple target organ defects. Indomethacin responsiveness of patent ductus arteriosus and renal abnormalities in preterm infants treated with indomethacin. Whole-body hypothermia for term and near-term newborns with hypoxic-ischemic encephalopathy: a randomized controlled trial. Influence of antenatal steroids and sex on maturation of the epidermal barrier in the preterm infant. Decreased growth rate of low-birth-weight infants with prolonged maximum renal acid stimulation. Effect of oral diuretics on pulmonary mechanics in infants with chronic bronchopulmonary dysplasia: results of a double-blind crossover sequential trial. Fluid restriction for term infants with hypoxic-ischaemic encephalopathy following perinatal asphyxia. Evaluation of urine acidification by urine anion gap and urine osmolal gap in chronic metabolic acidosis. Improved care and growth outcomes by using hybrid humidified incubators in very preterm infants. Postnatal development of renal hydrogen ion excretion capacity in relation to age and protein intake. Insensible water loss in preterm infants: changes with postnatal development and non-ionizing radiant energy. Human development is sufficiently resilient to withstand some disturbance of the normal postpartum sequence of events that initiate attachment; however, significant problems of either the infant (prematurity; congenital anomalies; transitional problems such as asphyxia, trauma, or peripartum infection) or the mother (complications of pregnancy, depression) have more substantial capacity to disrupt normal processes. These complications carry a risk for adverse effects on long-term neurodevelopment9 in addition to risks related to prematurity or underlying anomalies. This chapter reviews the complex subject of supporting infants and their families during a particularly vulnerable time of human development. Klaus and Kennell, the original authors of this chapter, are pioneers in identifying the importance of this subject, and much of their work remains relevant and constitutes a core of this knowledge. Although husbands/ partners and female relatives routinely accompany the mother to the delivery room, they usually have little experience in providing labor support and may need support themselves. The clinical value of continuous emotional and physical care during childbirth by a trained woman called a doula is supported by the results of the 22 randomized clinical trials conducted over more than two decades. In addition, they were less likely to have intrapartum analgesia or a baby with a low 5-minute Apgar score. Beneficial findings are consistent across the studies despite different cultural, medical, and social practices. Life stresses that leave the mother feeling unloved or unsupported or that precipitate concern for the health and survival of either her infant or herself may delay preparation for the infant and retard bond formation. Increased level of oxytocin throughout pregnancy facilitates the formation of an emotional bond between mother and infant in humans by acting to reduce anxiety and to ameliorate responses to external stresses. Mothers who have a less anxious state of mind are more able to increase their focus on infant care and recognize and respond effectively to nonverbal infant cues. Vigorous infants with meconiumstained amniotic fluid may need suctioning of the mouth and nose with only a soft bulb syringe. The ability to move a hand in a reaching motion enables the infant to claim the nipple. Oxytocin production in mothers is maintained postnatally by lactation and also in response to innate infant behaviors such as suckling, clinging, facial expressions, and vocal calls. The first feelings of love for the infant are not instantaneous with the initial contact. Many mothers express distress and disappointment when they do not experience feelings of love for their infant in the first minutes or hours after birth. In a study of 100 primiparous mothers interviewed within 72 hours of delivery, 39% developed positive feelings prenatally, 42% on the first day, and 19% on the second or third day. The beginning of parent-infant interactions has foundation in autonomic, neurologic, and endocrinologic systems in the mother and infant, and each become sensitized to the temporal patterns of the other, leading to the formation of a unique bond. Maternal cues of her voice, touch, and body rhythms in response create a synchronized "dance" between the mother and infant. When fathers are given the opportunity to be alone with their newborns, they not only spend almost exactly the same amount of time with the infants as mothers do, but also respond to infant cues as effectively. Additionally, when fathers had more extended postpartum hospital contact with their infants, they were more involved in infant caretaking responsibilities. Hospital routines should minimize unnecessary separation of newborns from their parents. Parent-infant synchrony and the construction of shared timing; physiological precursors, developmental outcomes, and risk conditions. Evidence for a neuroendocrinological foundation of human affiliation: plasma oxytocin levels across pregnancy and the postpartum period predict mother-infant bonding.
Buy genuine glucovance on line
These infants are usually born at term and have appropriate size and normal Apgar scores moroccanoil oil treatment cheap glucovance 500/5 mg mastercard. Although these babies might be asymptomatic at delivery, respiratory distress, cyanosis, and hypoxemia progress quickly to respiratory failure in more than half of these patients within hours after delivery. Intubation and mechanical ventilation, drainage of pleural and peritoneal effusions, and correction of hypoxia, acidosis, and shock might be needed in the delivery room for stabilization. The prognosis appears to depend on the severity of symptoms in the immediate newborn period. Although traditionally thought to be fatal, there are reports of survival in some patients presenting with respiratory failure, chylothorax, and hydrops fetalis in the immediate neonatal period. Later presentation carries a better prognosis with the possibility of spontaneous resolution, although respiratory morbidity might be common. Mechanical ventilation and drainage of the chylothorax might be needed in patients with large effusions, and nutritional support using total parenteral nutrition is essential. Several treatment strategies have been described for cases with persistent chylothorax, including pleurodesis, ligation of the thoracic duct, and pleuroperitoneal shunt. There is growing evidence from uncontrolled case studies suggesting a markedly positive effect of somatostatins, particularly octreotide, in the treatment of chylothorax with minimal side effects. In the absence of a controlled trial evaluating safety and efficacy, this therapy should be reserved for persistent and severe cases and not as first line of treatment. It is a rare entity, with a reported incidence of 1: 10,000 births, and affects males more than females (2: 1). Secondary chylothoraces are most commonly associated with trauma during thoracic surgery, but can also be the result of increased superior vena caval pressure caused by venous thrombosis. Clinical presentation is that of respiratory distress secondary to lung compression, pulmonary hypoplasia, or symptoms of the underlying pulmonary or cardiac disease. Many cases of congenital chylothorax are diagnosed by prenatal ultrasound, and antenatal management consists of thoracocentesis or thoracoamniotic shunt placement to try to prevent the development of pulmonary hypoplasia. However, even with prenatal treatment, these infants can still present with significant respiratory distress at birth as fluid reaccumulates, requiring postnatal treatment. Physical examination is significant for decreased breath sounds on the affected side with shifting of the cardiac apex to the contralateral side. Chest radiograph shows a pleural effusion, compression of the lung on the affected side, and displacement of the heart to the opposite side. In neonates with established feedings, chylothorax appears milky in color; however, in non-fed neonates, it is clear. These lesions can be identified on prenatal ultrasound, but the classification of the lesion should wait until postnatal examination and histology are available. These lesions should be followed closely in utero as some of these lesions can predispose the fetus to develop hydrops, and when this occurs in the second trimester, fetal intervention is warranted. Intervention includes repeated cyst aspiration, thoracoamniotic shunting, sclerotherapy, fetal surgery, or more recently, maternal betamethasone treatment. However, fetal intervention is relatively rarely needed as many of these cystic lung lesions appear to regress in utero. Congenital Cystic Adenomatoid Malformation Congenital cystic adenomatoid malformation constitutes multiple different hamartomatous lesions arising from the abnormal branching of the immature bronchial tree. This entity was first described by Chin and Tang in 1949,23 and since then, the term has been evolving as our understanding of the entity improves. Congenital cystic adenomatoid malformation is the most common congenital cystic lung disease, occurring in 1 in 11,000 to 30,000 live births, and affecting more males. In addition to the classification system described in the preceding, some have suggested classifying the lesions, at least during the prenatal period, as microcystic versus macrocystic based on the gross anatomy and antenatal ultrasound appearance. Whereas the latter classification has poor correlation with histologic features, it has a much better prognostic value, with microcystic lesions (cysts <5 mm) having a poorer prognosis than macrocystic lesions (>5 mm). These infants also have other associated lesions, including cardiovascular anomalies, renal hypoplasia, and focal dermal hypoplasia. Microscopically, the tissue consists almost entirely of irregular bronchial-like structures lined by pseudostratified ciliated columnar epithelium surrounded by thick cartilage plates and bundles of smooth muscle fibers. Usually all lobes of the lung are involved; thus this diagnosis is usually lethal. However, many of these cysts collapse as pregnancy progresses, allowing normal lung growth of the unaffected lobes. Radiographically, they appear as either a single or multiple air-filled or air/fluid-filled cysts in one or (much less frequently) multiple lobes. Depending on size, there can be flattening of the diaphragm, mediastinal shift and compression of adjacent lung. These malformations are of bronchiolar origin and consist of multiple small cysts (0. These are of bronchiolar/alveolar duct origin and almost exclusively seen in males. These lesions were the original congenital adenomatoid malformation described by Chin and Tang in 1949. The lesion primarily consists of large (up to 10 cm) air-filled, thinwalled cysts usually located at the lung periphery. This lesion can be asymptomatic at birth, and presents from the neonatal period to 4 years of age. Often, this will be an incidental finding on an x-ray that was taken for other reasons, such as acute respiratory distress related to a tension pneumothorax, or pneumonia. This lesion can be confused with pleuropulmonary blastema; therefore, blastemas must be looked for histologically. The unpredictability of the in utero growth of these lesions requires careful follow-up. Midgestation, these lesions can grow quite rapidly, which can cause mediastinal shift, pulmonary hypoplasia, and impaired venous return leading to hydrops. However, there is still some debate over the appropriate management of those lesions that are asymptomatic at birth. There are justifications for prophylactic surgery: preventing chest infections and sepsis; preventing malignancy; early rather than delayed surgery may encourage compensatory lung growth; reduction in postoperative complications (compared with emergency surgery). Usually, these structures are not connected to the main airway, and their blood supply arises from the systemic circulation. Intralobar sequestration occurs when the accessory bud arises before the establishment of the pleura and is contained within the normal lung. Extralobar sequestrations are usually located supradiaphragmatic; however, a small portion (<10%) are located infradiaphragmatic. Bronchopulmonary sequestration appears on chest radiograph as a posterior thoracic mass mostly on the left. If the sequestration is large, it can act as a space-occupying lesion and present as respiratory insufficiency either from pulmonary hypoplasia or lung compression and may require emergent surgical repair. If asymptomatic in the neonatal period, sequestrations can present later with recurrent pneumonia, atelectasis, bleeding, or high-output congestive heart failure. It is felt that asymptomatic patients should undergo elective resection to prevent complications of malignancy or infection. Symptoms, if present, are secondary to mass effect on the airways, gastrointestinal tract, or cardiovascular system. Even though major airway obstruction is uncommon, subcarinal lesions can present with severe obstruction. On the other hand, obstruction of smaller airways can cause air trapping, overdistension, and a clinical picture mimicking congenital lobar emphysema. Cases not diagnosed in the neonatal period usually present in older children or adults with pneumonia, hemoptysis, pneumothorax, dysphagia, or signs of caval obstruction. In symptomatic patients, this is performed after immediate clinical stabilization. Simple aspiration should be considered as a temporizing measure in patients with severe compromise, but complete resection is subsequently required. Only a few patients develop life-threatening complications before surgery and have a poorer outcome. There are no long-term complications related to the resection of a bronchogenic cyst. The left upper lobe is most frequently affected (42%), followed by right middle lobe (35%) and the right upper lobe (21%).
500/5 mg glucovance free shipping
For enteral medications the bioavailability depends on biochemical properties of the drug medicine university buy discount glucovance on-line, the formulation, and patient-specific factors such as gastric acidity, gastric emptying time, and intestinal transit time. Bioavailability is reduced by incomplete absorption and also by first-pass metabolism that takes place as the drug travels through the liver. Neonates have unique absorption properties that differ with maturity because of differences in their gastric acidity, gastric emptying time, intestinal transit time, hepatic blood flow, and rates of drug metabolism. Bioavailability after intramuscular and subcutaneous administration can be affected by tissue perfusion and drug permeability. Site of action "Receptors" Bound Free Tissue reservoirs Free Bound Distribution Absorption Bioavailability Systemic circulation Free drug Bound Metabolites Excretion Renal Biliary Pulmonary phase, drugs distribute into the more peripheral muscle and adipose tissue. Once in the circulation, drugs can disperse into several compartments, including the extracellular water stores, adipose tissue, brain, and muscle. The apparent volume of distribution (Vd) for a drug is defined as the hypothetical fluid volume through which drug is dispersed. This is a hypothetical Vd because when drug plasma concentrations are very low, the apparent Vd may be more than physiologic. Drugs can have extraordinarily large Vd if they are bound to proteins in the peripheral tissues or sequestered in adipose tissue. For example, digoxin has a very large Vd because of low concentrations in the plasma because it is sequestered in the peripheral tissue where it is bound to proteins in skeletal and cardiac muscle. Additionally, many physiologic and pathologic factors influence the distribution of drugs in the body. Limited adipose tissue in extremely premature infants limits distribution of drugs to adipose tissue. Drugs that are highly bound to plasma proteins, such as vancomycin, stay within the circulation, thus limiting their distribution outside the circulation and their volume of distribution. Preterm infants have deficient serum protein concentrations, resulting in an increased fraction of free drug and often an increased distribution of free drug outside the circulation. Drugs enter the systemic circulation as free drug, where they can then be bound by plasma proteins, react at the site of action with receptors, or travel to tissue reservoirs. Initially, drugs rapidly diffuse to well-perfused organs such as the heart, liver, and kidneys. Then, in the second Biotransformation is the process that typically converts a drug molecule into a more polar, hydrophilic derivative. Metabolism of drugs most often produces inactive metabolites, but can also produce active metabolites (theophylline is methylated to caffeine), or even toxic metabolites (acetaminophen toxicity from N-acetyl-p-benzoquinone imine). The metabolism of drugs is typically classified into two phases, nonsynthetic phase 1 and synthetic or conjugation phase 2. The cytochrome P450 enzymes found in the liver and other tissues are primarily responsible for phase 1 oxidative metabolism. Biotransformation may be enhanced or impaired by multiple factors, including maturity, postnatal age, coenzyme induction or inhibition, prostaglandins, hepatic blood flow and function, and even the effects of other disease states. Glomerular filtration increases with maturation, with newborns having the lowest glomerular filtration rate compared with children and adults. Drug secretion in the proximal tubules uses transport systems that typically eliminate 100 90 80 70 60 50 40 30 20 10 0 0 organic anions. Secretion transporters are used to secrete and thus eliminate drugs conjugated with glucuronic acid, glycine, and sulfate, including penicillin and furosemide. The proximal renal tubules also use transport systems for organic cations or peptides. Tubular secretion is lower in newborns, thereby explaining the prolonged half-life of furosemide and penicillin. Membrane transporters in the distal tubule actively reabsorb drugs from the tubular lumen back into the systemic circulation, typically through nonionic diffusion. Glomerular filtration rate typically improves with maturation faster than tubular mechanisms. The liver uses four mechanisms of drug elimination: drug metabolism, excretion into bile, fecal elimination, and enterohepatic recirculation. Patients with hepatic insufficiency have decreased elimination of drugs because of alterations in protein levels and protein binding, decreased liver blood flow, and altered hepatic enzymatic reaction. Patients with hepatic insufficiency, however, exhibit marked variability in drug metabolism and elimination. Nonetheless, infants with hepatic insufficiency typically benefit from lower doses of drugs that are eliminated by hepatic biotransformation, and when possible, drug plasma concentrations should be monitored. Similarly, when infants with low protein stores receive a highly proteinbound medication, they will likely have a higher proportion of active, unbound drug and typically a lower volume of distribution, faster elimination, and shorter half-life. Patients with significant renal disease also accumulate organic acids in the plasma that can compete with protein-bound drugs for albumin binding, thereby altering the volume of distribution. Patients with liver disease or hepatic congestion accumulate active drugs owing to their diminished metabolic capabilities and decreased first-pass metabolism. Patients with liver disease typically have low albumin or altered glycoprotein levels that may affect fractional protein binding of drugs, thereby altering volume of distribution. Cardiac dysfunction significant enough to cause altered perfusion, edema, and/or hepatic congestion can affect drug metabolism. Drug metabolism and elimination from the body exhibit marked complexity and interpatient variability. In general, the rates of biotransformation and elimination are often slower in the newborn period. The expected changes in drug metabolism with maturation are often extremely variable and depend on both the drug and the metabolic pathways. Pharmacokinetic Models Describe Concentration of Drug over Time Pharmacokinetics describes the mathematical relationship between the dose of a medication administered to a patient and the concentration of a drug in the plasma over time after a given dose. In reality, most drugs distribute through various compartments in the body beyond the circulation and into the brain, muscle, fat, and organ systems. Therefore, even though we measure drug concentrations in the plasma or serum, these measurable levels are associated with the drug concentrations at sites of action or in tissue reservoirs. Most drugs follow first-order kinetics, and mathematical equations used from this point forward are appropriate for drugs that are eliminated using properties of first-order kinetics (Table 51-1). Most drugs used in neonates follow first-order kinetic properties, including ampicillin, gentamicin, and phenobarbital. These medications have an exponential decrease in the serum concentration over time and therefore represent a linear relationship on a logarithmic scale. For example, if 50% of the drug is removed per unit of time, then a larger amount of drug is removed in first interval than in last interval. Rarely, drugs may follow what is called zero-order kinetics, or nonlinear, saturable kinetic properties. In drugs that follow zero-order kinetics, a constant amount of drug is metabolized or eliminated per unit of time regardless of concentration. There is a maximum yet constant amount that the body can eliminate at any given time. Small increases in dose can yield large increases in levels because the amount of drug removed is constant and not proportional to the dose. The elimination rate constant (Kel) is highly variable, with a smaller percentage of the drug eliminated at the beginning and a higher percentage of the residual drug eliminated toward the end. The half-life of drugs whose elimination follows zero-order kinetics is dependent on drug dosage; larger doses yield a longer half-life. The drug concentration follows a linear decrease of serum concentration over time. Phenytoin is another zero-order kinetic drug, owing to saturable kinetics of the metabolizing enzymes. The mathematical principles that describe the firstorder kinetics of the dose-to-concentration relationship over time often use a compartmental approach that best represents how a drug distributes through the body and the different rates of concentration changes in the body over time. In one-compartment models, a drug hypothetically distributes instantaneously in a homogeneous fashion into one compartment representing the entire body, and then the concentration declines linearly with one elimination rate constant (Kel) as drug is eliminated. This one-compartment approach is most appropriate for drugs that do not distribute widely into extravascular tissue. Two different exponential rates of clearance are demonstrated by a change of slope in the semi-logarithmic plot of a concentration-versus-time graph. Finally, the distribution and elimination properties of widely distributed drugs that enter and exit numerous compartments may require multi-compartment models.
Generic glucovance 400/2.5 mg fast delivery
If an additional source of quality donor organs became available through xenotransplantation or tissue or stem cell engineering treatment 0f gout buy glucovance 400/2.5mg online, it would likely change the face of therapy for this disease. As it stands now, most cardiac transplants are being done either for cardiomyopathy, the highest-risk subpopulations with congenital heart disease, or those who have undergone failed surgical palliation. With the success of newer immunosuppression regimens, long-term survival after heart transplant has improved dramatically over the last 15 years. In addition, there is good evidence that neonatal heart transplant recipients have even better survival than older children, probably because of immune system immaturity with decreased incidence of antibodymediated rejection. They have been shown to have less graft vasculopathy,64 require less immune suppression,20 and have improved overall survival after transplant. Because of the limited supply of donor hearts and the fact that congenital heart defects can often be associated with other malformations, including chromosomal abnormalities, every attempt should be made to assure that only the most viable candidates receive the organs. For this reason, extensive screening is done before placing an infant on the transplant list. These investigations often include viral serologies, chromosomal analysis, cranial ultrasound, renal ultrasound, cardiac catheterization, and neurologic evaluation, as well as some consideration regarding the social surroundings and quality of care the infant will receive after transplant. These quality-of-care issues include screening the family for social support systems, psychologic issues, the ability to adjust to highpressure demands, including, but not limited to , administering medications, high-intensity medical follow-up including drug levels and surveillance endomyocardial biopsies, as well as the need for superb vigilance and attention to potential early signs of rejection. A list of relative and absolute contraindications to infant cardiac transplantation is shown in Table 87-4. Even after a suitable match between candidate and quality donor organ, significant challenges remain, such as opportunistic infections and prophylactic antibiotic use, as well as graft-versus-host disorders. In addition, close supervision of blood cell counts and electrolyte levels is extremely important because immunosuppressive agents have known side effects of renal and bone marrow suppression. With adequate care, the 10-year survival rate for infants undergoing heart transplant is 83% for patients with cardiomyopathy and 67% for patients with congenital heart disease. However, those who are refractory to medical therapy may be candidates for retransplantation. Some of the common indications that now remain for purely diagnostic catheterizations are shown in Table 87-5. Just as diagnostic catheterization has been decreasing, the last 30 years has brought a revolution of catheterbased interventions for heart disease. Rashkind and Miller in 1966 for palliation in infants with transposition of the great vessels in whom there was inadequate intercirculatory mixing. A balloon catheter was inserted through the femoral vein, advanced across the atrial septum, inflated in the left atrium, and forcibly pulled across the atrial septum in order to enlarge the communication and allow increased atrial-level mixing. With that procedure, a new era of innovation in treatment for congenital and structural heart disease was ushered in, and a wide range of attractive, less invasive alternatives to surgery have emerged. As catheter manufacturing becomes more miniaturized, more financially feasible, and, perhaps most importantly, as regulatory agencies become more streamlined in their approval processes for children, the risk/benefit ratio for further interventions will likely continue to tip even further in favor of catheter-based advances rather than traditional surgical techniques. A summary of the clinical problems in the neonate that can be addressed with catheter-based interventions is shown in Table 87-6. If there are other intracardiac mixing lesions such as a ventricular septal defect or patent ductus arteriosus or if the atrial septum itself is already nonrestrictive, a septostomy may not be necessary. However, approximately one third of babies with transposition of the great arteries require a septostomy before arterial switch. Because there is no adequate forward pathway for flow on the left side of the heart, a restrictive septum leads to pulmonary venous hypertension and pulmonary edema. A mild amount of septal restriction may actually limit pulmonary overcirculation to some extent, but in general, pulmonary overcirculation is better tolerated and easier to control medically than is atrial septal restriction, so many of these infants will undergo atrial septostomy before the Norwood procedure. Just as opening the atrial septum may be necessary in those with an inadequate left heart, it may also need to be performed in those with inadequate forward flow through the right side of the heart. The most obvious examples of this include tricuspid atresia or pulmonary atresia with intact ventricular septum, wherein there is complete right heart obstruction and there would be no systemic flow at all without shunting at the atrial level. Other examples of inadequate right heart output include Ebstein anomaly, in which the right ventricle does not develop normally because of apical displacement of the septal leaflet of the tricuspid valve. Septostomy is necessary to maintain cardiac output by providing a path for blood, albeit deoxygenated, to be pumped systemically. In all of these cases, maintaining a patent ductus arteriosus is, of course, also necessary to maintain adequate pulmonary blood flow. An additional situation in which a septostomy may be indicated is in total anomalous pulmonary venous return. If there is a restrictive atrial septum in this condition, as the pulmonary venous blood returns anomalously to the right side of the heart, cardiac output can be severely decreased until a septostomy again provides a path for forward systemic flow. Providing a pressure pop-off of left-to-right flow across the atrial septum may lead to improved respiratory dynamics by decreasing pulmonary edema and improved hemodynamics by decreasing rightsided pressures. A, Left atrium opacified with contrast, with a small interatrial communication noted around the catheter. The advantage to performing the procedure in the catheterization laboratory is the availability of a wide range of tools should the procedure be anything other than straightforward. For d-transposition of the great arteries, the most common lesion requiring septostomy, the septostomy is usually straightforward, and it has been shown that a bedside, echocardiography-guided approach is as safe and significantly more cost effective than taking the patient to the catheterization laboratory. If no interatrial communication is present, one may have to be created using either radiofrequency perforation of the septum or with a transseptal needle. In the absence of any of these hemodynamic consequences, even severe pulmonic stenosis Other Strategies to Maintain Interatrial Communication In conditions other than d-transposition of the great arteries, the atrial septum can be thick or even intact and other strategies may be employed to create and maintain communication. B,Anangiogram is performed to confirm appropriate stent location before deployment in the septal communication. It was first performed in older children, and was soon expanded to the neonatal population with critical pulmonic stenosis. Although a much more difficult procedure in the neonate because of the smaller effective valve orifice, it is still associated with significant reduction in gradient and very good mid- and late-term results with high freedom from reoperation. This is usually temporary and can be managed with increased intravascular volume and beta blockers. Once the valve is perforated, a wire is passed and snared from the aortic side, creating a rail over which the valvuloplasty balloon can be advanced. A certain number of these patients can have right ventricular hypoplasia because of in utero lack of forward pulmonary blood flow, but many show significant growth of the right ventricle when sufficient outflow is established. During this time, they may need to remain on prostaglandins, as they can remain ductal-dependent until the ventricle is large enough to supply sufficient pulmonary blood flow on its own. In some extreme patients, weeks or even months may be necessary to allow sufficient right ventricular remodeling, so strategies to supplement pulmonary blood flow may be considered, including an aortopulmonary shunt or stenting of the ductus. This allows discontinuation of the prostaglandins and may palliate the patient until the time when biventricular circulation can be safely completed. If the obstruction is related to the surgical repair, it can often become apparent during or immediately after the surgery and can be revised surgically. Sometimes, however, what could be a minor stenosis or kink can become a nidus for thrombus secondary to turbulent blood flow. The most common occurrences, however, are minor narrowings that do not severely limit blood flow in the immediate postoperative period but that lead to progressively decreasing saturations over time because of decrease in pulmonary blood flow relative to the growth of the patient. Whatever the cause of decrease in shunt flow, catheterbased interventions can be performed to attempt to maximize shunt lumen. These interventions include simple balloon dilation, thrombus evacuation, or, more commonly, stent placement within the shunt. However, in some institutions where neonatal repair is not performed or when significant co-morbidities necessitate avoidance of cardiopulmonary bypass, catheter-based interventions can serve to palliate a child until a time when a complete repair is safer. These catheter-based interventions may include pulmonary balloon valvuloplasty if there is a component of valvar obstruction as well as the normal subvalvar obstruction. Under extreme circumstances, the right ventricular outflow tract can also be stented, although this necessitates obliteration of the valve and does not allow for a future valve-sparing repair. Pulmonary Artery Stenosis It is rare for isolated pulmonary arterial obstructions to necessitate intervention in the neonatal period. However, if the patency of one of the arteries is threatened, balloon angioplasty can be performed. Most operators attempt to avoid stent placement because of the limited growth potential going forward, although they can either be removed at future surgeries or "unzipped" by fracturing them with larger balloons in a relatively controlled manner. Isolated Pulmonary Artery Anomalous origin of the pulmonary artery can occur in isolation or, more commonly, in association with tetralogy of Fallot. Most often, the left pulmonary artery originates from ductal tissue off the aortic isthmus. As the ductus arteriosus closes, the pulmonary artery is at risk of isolation from the circulation and the related lung is at risk for underperfusion.
Order glucovance 500/5 mg mastercard
Black children have a 35% seroprevalence by age 5 compared with 18% in white children treatment xdr tb purchase glucovance no prescription, and the seroprevalence remains twice as high through the teen years, but is equivalent by 60 years of age. Primary genital infection may cause localized pain and burning of the labia and vaginal mucosa 2 to 7 days after contact. These vesicles break down easily, forming shallow ulcers and releasing numerous infectious virus particles. Not only was this seroprevalence largely unsuspected among these pregnant women, but asymptomatic viral shedding also occurred among them at a rate (roughly 1% viral shedding at any time in pregnancy) similar to that in women with symptomatic recurrences. Oral sex has become more popular among teens because they believe it is safer sex. Primary and recurrent maternal infections have been associated with congenital infection. Maternal neutralizing antibodies may also be partially protective for a newborn in recurrent infections and may not yet be present (and available to cross the placenta) in a primary maternal infection. The amount of neutralizing antibody also affects the severity of neonatal disease. Infants who do not receive much transplacental transfer of antibody are more likely to develop disseminated disease. Prolonged rupture of membranes (>4-6 hours) also increases the risk of viral transmission, presumably from ascending infection. Delivery via cesarean section, preferably before rupture of membranes, but at least before 4 to 6 hours of rupture, can reduce the risk sevenfold. The father and the mother and maternal breast lesions have been implicated in neonatal infections. Removal of health care workers with other lesions would pose significant risk to neonates because it would cause significant disruption of care. Orolabial lesions should be covered with a mask, and skin lesions should be covered with clothing or a bandage. Congenital infections are described throughout pregnancy and after primary and recurrent infections, but are most likely with a primary infection, or if the mother has disseminated infection and is in the first 20 weeks of pregnancy. The manifestations probably result from destruction of normally formed organs rather than defects in organogenesis because the lesions are similar to lesions of neonatal herpes. A few children, usually in association with prolonged rupture of membranes, have isolated skin lesions that may be more amenable to antiviral therapy. Half of the infants are born prematurely, usually between 30 and 37 weeks of gestation, and many have complications of prematurity, particularly respiratory distress syndrome. Two thirds of the term newborns have a normal neonatal course and are discharged before the onset of disease. One fourth of the infants present on the first day of life, and two thirds present by the end of the first week. Disseminated infections may involve virtually every organ system, but predominantly involve the liver, adrenal glands, and lungs. Infants usually present by 10 to 12 days of life with signs of bacterial sepsis or shock, but often have unrecognized symptoms several days earlier. Although the presence of cutaneous vesicles is helpful in diagnosis, 20% of infants never develop vesicles. Disseminated intravascular coagulation with decreased platelets and with petechiae and purpura are common, and bleeding often occurs in the gastrointestinal tract. Respiratory distress, often with pneumonitis or pleural effusion on the chest x-ray, has a poorer prognosis. These infants may present with irritability, apnea, a bulging fontanelle, focal or generalized seizures, opisthotonos, posturing, or coma. Death usually occurs at about 2 weeks of age, roughly 1 week from the onset of symptoms, and often involves respiratory failure, liver failure, and disseminated intravascular coagulation with shock. Encephalitis may occur as a component of disseminated disease, via blood-borne seeding of the brain, resulting in multiple lesions of cortical hemorrhagic necrosis often in association with oral, eye, or skin lesions, at 16 to 19 days of life. Lethargy, poor feeding, irritability, and localized or generalized seizures may be the presenting manifestations. Disease was found in the temporal lobes, cerebellum, brainstem, and deep gray nuclei. Infants with disease localized to the skin, eyes, or mouth usually present by 10 to 11 days of life. More than 90% of these infants have skin vesicles, usually over the presenting part at birth and appearing in clusters. Infants at risk should be monitored for localized infections (vesicles) of the oropharynx. One third of these infants later develop neurologic sequelae indicative of undiagnosed neurologic involvement. Serologic testing is not useful in neonatal disease because transplacentally transferred maternal antibody confounds the interpretation. Polymerase chain reaction can also be used to test blood, scrapings of lesions, the conjunctiva, or the nasopharynx. High-dose acyclovir resulted in a much improved survival rate: Infants with disseminated infection had an odds ratio of survival of 3. Acyclovir, a deoxyguanosine analog, is preferentially taken up by virusinfected cells and phosphorylated by thymidine kinase, which is encoded in the virus. National Institute of Allergy and Infectious Diseases Collaborative Antiviral study Group: Predictors of morbidity and mortality in neonates with herpes simplex virus infections. Initiation of therapy in the high-dose acyclovir trial usually began 4 to 5 days after onset of symptoms, which is no better than occurred in the low-dose trial. Oral suppressive acyclovir therapy for 6 months after completion of treatment has been used to decrease recurrences in infants. Repetitive cervical cultures do not predict whether a mother will be shedding virus at delivery. Mothers should be counseled regarding the signs and symptoms of disease, and some may then recognize infection. If rupture of membranes has been present longer than 6 hours, some experts still recommend cesarean delivery in the face of genital lesions, but data are lacking, and controversy exists. There is also no consensus for treatment with ruptured membranes in a mother with lesions except for a very immature fetus. If an infant is delivered vaginally to a mother with recurrent genital lesions (5% risk of infection), most experts do not recommend treating the infant. The mother needs to be taught the signs and symptoms of neonatal disease because the cultures do not always detect neonatal disease. If it is a recurrent infection, the acyclovir may be discontinued after a negative evaluation. In situations where this is not possible, the approach detailed in the algorithm will have limited, and perhaps no, applicability. When a genital lesion is strongly suspicious for HsV, clinical judgment should supersede the virological test results for the conservative purposes of this neonatal management algorithm. Targeting women for testing who are at high risk for infection misses too many seronegative women. Although no major malformations have been associated to date with the use of acyclovir in pregnancy, the safety to the fetus has not been determined. In a Cochrane Database meta-analysis of third-trimester antiviral prophylaxis, women were less likely to have a recurrence at delivery (relative risk 0. The virus is highly species specific, and humans are the only known reservoir for disease. After primary infection, the virus enters a latent state, from which reactivation may frequently occur. Reinfection may also result from any of the thousands of human strains, which are homologous, but not identical. The differing antigenic makeup of the various strains may make it possible to identify the source of the viral infection. It also allows re-infection to occur with other strains in an already seropositive individual. This capsid is surrounded by amorphous material, which is surrounded by a lipid envelope, probably acquired during budding through the nuclear membrane. The virus is named for the intranuclear and paranuclear inclusions seen with symptomatic disease-cytomegalic inclusion disease.
Syndromes
- Numbness
- Do you use a hair dryer? What type? How often?
- Sensory changes
- X-ray of the knee
- Chest x-ray
- Seizures
- Difficulty swallowing
Purchase discount glucovance
Platelet-activating factor primarily resides on the cell surface symptoms and diagnosis purchase glucovance 400/2.5mg amex, where it acts as an intercellular messenger. Chemokines are the largest family of cytokines and are involved in the activation and recruitment of a wide variety of cell types. Chemokine receptors belong to the seven transmembrane-spanning family of G-proteincoupled receptors. Chemokines are constitutively produced in organs, where cell attraction is required for maintenance of local homeostasis. In inflammatory states, chemokines are responsible for navigation and homing of effector leukocytes. Role of chemokines and chemokine receptors in regulating specific leukocyte trafficking in the immune/inflammatory response. Considerable data suggest that chemotactic factor generation is deficient in newborn infants. Coordinated Inflammatory Response in Neonatal Sepsis In human bacterial sepsis, cytokines are released in a sequential manner, resulting in a cytokine cascade. Other proinflammatory cytokines are released shortly afterward, and anti-inflammatory mediators follow in close sequence. In general, cytokines are not stored in intracellular compartments; they are synthesized and released in response to an inflammatory stimulus. Proinflammatory and anti-inflammatory cytokines or molecules are produced in response to an inflammatory stimulus. Counter-inflammatory molecules include soluble cytokine receptors (resulting from proteolytic cleavage of the extracellular binding domain), antiinflammatory cytokines. Through this mechanism, endothelial cells are activated to produce other cytokines and mediators. Toll-like receptors are pattern recognition receptors that recognize pathogen-associated molecular patterns. Pathogen-associated molecular patterns are shared by many pathogens, but are not expressed in host cells. Activated, macrophages synthesize and secrete the cascade of proinflammatory cytokines, chemokines, and mediators described earlier. Some of these cytokines activate neutrophils to release proteases and free radicals that have the capacity to damage endothelium and promote capillary leak. Upregulation of adhesion molecules on the neutrophils allows them to bind to counterreceptors on the endothelial cells and migrate to sites of inflammation. The proinflammatory cascade is interrupted by the initiation of counter-regulatory mechanisms. Anti-inflammatory cytokines (which appear later in the cascade) are found in most of these infected individuals. This is a response of the host to limit the toxicity of proinflammatory substances. Shortly after the onset of an infectious episode, the mononuclear cell becomes refractory and is unable to respond to proinflammatory cytokines. Innate immunity and Toll-like receptors: clinical implications of basic science research. Each lymphocyte expresses a cell surface receptor that recognizes a particular antigen. Each lymphocyte is engineered to express a receptor that is specific for only one antigen. In this way, the lymphocyte population as a whole can recognize a wide range of antigens. The antigen receptors are generated during development by a process known as somatic mutation and recombination involving a few germline genes. B cells recognize an unmodified antigen molecule, either free in solution or on the surface of other cells. An antigen selects the clones of B and T cells that express the cell surface receptors that recognize the antigen. Because the number of different lymphocyte antigen specificities is large, the number of lymphocytes available to recognize each antigen is relatively small-only a few hundred lymphocytes in an adult. In addition, because so few cells are insufficient to eradicate an invading pathogen, the first step toward the generation of a specific immune response involves a rapid expansion of antigen-specific lymphocytes. This step is followed by further differentiation of antigen-specific cells into effector cells. These events underlie the difference between primary and secondary immune responses. During the primary response, the small number of specific cells increases, and the cells undergo differentiation. If the antigen is encountered again (or persists), there is a larger population of specific cells to react with the antigen, and these cells are able to respond more quickly because they have already undergone several steps along their differentiation pathway. These lymphocytes that have been stimulated by antigen (primed) and their progeny either may differentiate fully into effector cells or may form the expanded pool of cells (memory cells) that can respond more efficiently to a future (secondary) challenge with the same antigen. T cells develop and differentiate in the thymus before seeding the secondary lymphoid tissues. The balance of activity between these subsets is related in part to how antigen is presented to the cells, and it ultimately determines the type of immune response that develops. Lymphocytes destined to become T cells must undergo several maturational steps in the thymus before they become mature effector T cells. In humans, the thymus develops embryologically as an outgrowth from the third and fourth pharyngeal pouches between weeks 6 and 7 of gestation. The cortex and medulla of the thymus begin to differentiate by the 10th week of gestation, and Hassall corpuscles appear by the 12th week of gestation. In the thymus, T-cell maturation is accompanied by the sequential appearance of surface phenotypic markers (see Table 54-7). Mice lacking Notch-1 have blocked T-cell development with B cells developing in the thymus instead, suggesting that Notch signaling may play an important role in early T-cell commitment and differentiation. Developmental immunology and role of host defenses in neonatal susceptibility to infection. The combined costimulatory signal prevents T-cell apoptosis or the induction of anergy (unresponsiveness) that may occur in response to activation of either signal alone. This differential pattern of cytokine expression contributes to differences in the function of these two subsets of T cells. Th1 cells are inflammatory cells responsible for mediating cell-mediated immunity. The decision of a na T cell to mature into either Th1 or Th2 is partly regulated by the interaction between growth factors/ cytokines and their receptors and transcription factors. T-regulatory cells (Tregs) downregulate T-cell responses to both foreign antigens and self-antigens. The T-follicular helper (Tfh) cells are a distinct class of helper T cells that are normally found in B-cell follicles in secondary lymphoid organs. These cells are controlled by the Bcl-6 transcription factor and mediate B-cell activation and assist in germinal center formation. The synthesis and secretion of this cytokine is triggered by the activation of mature T cells. This high-affinity receptor is found on T cells, B cells, mast cells, myeloid cells, fibroblasts, muscle cells, neuroblasts, stromal cells, endothelial cells, and monocytes. Treg cells are interestingly higher in cord blood of preterm compared with term infants or adults. Thus with antigenic stimulation there is immediate release of Th2 cytokines and development of Th2 effector cells. This is also observed in neonatal mouse studies, where altering the dose of the viral antigen or addition of costimulatory molecules, leads to a deviation from the expected Th2 to an adult type Th1 response. This diversity is retained throughout the first year of life and then decreases gradually over the first decade of life. Dendritic cell populations have been grown from separated hematopoietic precursors, suggesting that there is a common granulocyte-monocyte-dendritic cell progenitor. Yet, this leaves the neonate susceptible to infections from viruses and other intracellular pathogens that need effective Th1 defenses for clearance. Adult-level cytokine production can be elicited in human neonatal T cells by increasing the magnitude of Th1promoting costimulatory signals. These findings could be exploited in the future to generate vaccines for the treatment of viral infections.
Generic glucovance 500/5mg visa
The lower Cmax is because drug is being eliminated during the same time drug is being infused medications 3601 order online glucovance. In this case, more complicated exponential equations would be necessary to estimate the Vd while taking drug elimination into account (see Table 51-1, Eqs. Fortunately, most neonates receive drugs with short infusion times relative to the slow drug elimination rate; therefore only a very small quantity of drug is eliminated during the actual infusion, allowing the use of simplified calculations. The half-life, T1 2, is the time it takes to reduce the drug concentration [C] in half (Ln([C1]/[C2]) = Ln2 as shown in Eq. Clearance is formally defined as the volume of blood from which all drug is removed per unit of time. In practice, total body clearance is often estimated using the dose per dosing interval divided by the average steady-state drug concentration (see Table 51-1, Eq. Formulas accounting for relatively short infusions are most appropriate (see Table 51-1). If the peak concentration is obtained 30 minutes after the end of the infusion to allow for rapid distribution phase, then multiply Cmax by the decay factor (e-kt where t = 0. Clinicians can predict the concentration at any time relative to Cmax at the end of infusion by adjusting the time parameter "t" in the decay factor (e-kt) (see Table 51-1, Eq. Different formulas can be used that incorporate both the dosing interval referred to as tau and the number of doses (n). If multiple doses have been administered, but it is not known if steady-state has been reached, then formulas allow for calculation of Cmax after n doses. Many drugs, such as dopamine, bind to physiologic receptors; agonists mimic the effects of endogenous ligands, whereas antagonists block the effects of endogenous ligands. The pharmacodynamics of receptor-binding drugs is altered during development because of changes in receptor binding, receptor density, and downstream signal transduction. Disease states, maturity, and concomitant medications can also alter drug pharmacodynamics. Lack of efficacy may be caused by the dose being too small and thus yielding subtherapeutic concentrations. Alternatively, the dose may have achieved the desired concentration, but in the young infant that plasma concentration did not correlate with the desired response. Once a drug has been chosen, the hard part is choosing the right dose to accomplish these goals. Infant factors such as immunocompetence, bacterial load, and drug concentration at the site of infection are also important, but they are difficult to modify. Gentamicin is concentration dependent; therefore the higher the dose, the higher the Cmax, the more killing is achieved. Gentamicin also has a significant postantibacterial effect, meaning that the higher the Cmax, the more bacterial growth is subsequently suppressed after levels decrease. Finally, bacterial killing with vancomycin is independent of concentration; however, there is a modest post-antibacterial effect such that higher levels are associated with prolonged killing even as levels decrease. Neonates are notorious for their susceptibility to meningitis and severe abdominal infections associated with ascites and large fluid shifts. Decreased renal toxicity is attributed to the reduction in renal drug accumulation because of saturable drug uptake. A-C, Mary, Jack, and Ava are three babies who all receive gentamicin for presumed sepsis. Ava has the lowest renal clearance such that after three doses, gentamicin accumulates to higher peak and trough concentrations. Repeat peak and trough levels may be warranted if treatment is continued beyond two doses. Conclusion the success of drug therapy is determined by complex interactions between the administered drug and its drug exposure profile, the host, and the disease process or the pathogen. Use equations in Table 51-1 to estimate what dose and interval she would need to have a desired peak of 8-10 mg/L and the desired trough concentration of less than 2 mg/L. Predicting efficacy of antiinfectives with pharmacodynamics and Monte Carlo simulation. Pharmacokinetics, pharmacodynamics, and Monte Carlo simulation: selecting the best antimicrobial dose to treat an infection. Pharmacokinetics and pharmacodynamics: optimal antimicrobial therapy in the intensive care unit. Association of aminoglycoside plasma levels with therapeutic outcome in gram-negative pneumonia. The association of aminoglycoside plasma levels with mortality in patients with gram-negative bacteremia. Optimizing therapy with antibacterial agents: use of pharmacokinetic-pharmacodynamic principles in pediatrics. Drug disposition and clinical practice in neonates: cross talk between developmental physiology and pharmacology. Neonatal pharmacology: extensive interindividual variability despite limited size. In comparison to today, medical practice in 1900 was not dramatically different from that practiced in ancient Rome. Since then, however, medication management has increased in complexity at the same time that diagnostic techniques and patient monitoring have increased. With the dramatic increases in technology, diagnostics, and monitoring, there has been an equal explosion of medications to ease pain or treat disease. The combination of these factors has led to a modern health care system that has the potential to do as much harm as good. Few people expect to have severely grave outcomes when entering an ultramodern hospital. Based on several studies from Colorado, New York, and Utah, the report estimated that between 44,000 and 98,000 people die each year as a result of preventable medical errors. The report also details that an estimated 7,000 people a year die from medication-related adverse events, either in or out of the hospital. In addition, nonlethal medicationrelated errors are estimated to cost upward of $2 billion each year. Specific to pediatrics, there are several studies that describe the rate of medication-related problems. Indeed, that rate holds true for every 49 admissions: seven of those patients would be harmed. Before this study, medical practitioners would not have imagined that the harm caused to their patients by medication 676 errors would have been that significant. A study from 2001 reported that pediatric patients were found to be at a three times higher risk of having an adverse drug event than adult patients. First, weight-based dosing, required for pediatric patients, necessitates more calculations than adult dosing. Second, dispensing drugs in pediatrics is also error-prone because pharmacists often must dilute stock solutions. Third, neonatal and pediatric patients generally are not able to advocate on their own and cannot alert practitioners to adverse drug reactions. Fourth, all children, especially neonates, may have more limited internal reserves than adults with which to buffer errors. As a follow-up to the report, many hospitals at this point have such a reporting system. More important than simply having a reporting system is what is done with the reports that are entered by hospital employees. The important principles of error reporting are: (1) the person who made the error needs to know that an error was made, (2) others in the work group need to know the details of the error but not the details of who made the error, (3) errors need to be reviewed in aggregate to look for trends that could point to a collective weakness in the system, and (4) any events that resulted in serious harm need to be investigated for possible root causes and implications for other parts of the hospital. In our current medical practice there is much to be gained from employees who have seen an error and who feel free to report unsafe conditions that they see, errors that they have almost committed, or errors they have actually committed. Although this contention is impossible to prove, it stands to reason that every person who has worked in a hospital has made a mistake at some point. This statement should not be discouraging to current medical practitioners; on the contrary, it should be empowering. Knowing that they will personally make mistakes should cement in clinicians a relentless drive to discover the part of the process in which they participated that is broken and needs to be fixed to provide safe patient care.
Order glucovance
It is no surprise that the ideal composition of intravenous amino acid mixtures is unknown treatment wasp stings order 500/5mg glucovance free shipping. Whether the goal should be to match amino acid concentrations of term, breastfed infants or some other standard is not known. Clearly, the ultimate goal is to achieve plasma amino acid concentrations in response to provision of parenteral nutrition that optimize both growth and neurodevelopment without toxicity. To optimize nutrition and growth, particularly in a premature infant, the requirements for specific amino acids need to be more precisely defined. Cysteine, tyrosine, and arginine are often considered conditionally essential amino acids for premature infants. Tyrosine is not present in appreciable amounts in currently available amino acid solutions because of its low solubility. Snyderman found lower rates of weight gain, nitrogen retention, and plasma concentrations of tyrosine in premature infants given a tyrosine-deficient diet. The activity of this enzyme in premature infants was thought to be inadequate for growth and nitrogen retention without tyrosine supplements. However, stable isotope studies have demonstrated active phenylalanine hydroxylation in very premature (26 weeks) and premature (32 weeks) infants. However, it remains unclear whether enough tyrosine can be endogenously produced from phenylalanine in premature infants to support normal rates of protein accretion. N-acetyl tyrosine, although currently added to TrophAmine, is not highly bioavailable. Nonetheless, several studies provide indirect evidence that N-acetyl tyrosine improves protein accretion in preterm infants. Cysteine may be a conditionally essential amino acid for premature infants, but is not contained in currently available amino acid solutions. Some studies have shown that the fetal liver lacks the enzyme system to convert methionine into cysteine and that infants on a cysteinefree diet demonstrate impaired growth and low plasma cysteine levels. Other studies have demonstrated that there is enough cystathionase in extrahepatic tissues of the fetus and premature infant to synthesize cysteine when an adequate amount of methionine is provided. Studies using stable isotope techniques have demonstrated active endogenous cysteine synthesis in low birth weight infants. However, it is important to note that cysteine hydrochloride supplements can produce metabolic acidosis unless appropriately buffered with acetate. Glutamine is one of the most abundant amino acids in both plasma and human milk, yet it is not supplied by currently available amino acid solutions because glutamine is unstable in aqueous solution. Glutamine is a major energy substrate for small intestinal mucosa, as proved by a high glutamine uptake from the lumen and from arterial blood during the newborn period in rats. Several studies suggest that parenteral glutamine supplementation is of benefit in selected populations of critically ill adults. It is present in large concentrations in the retina and brain of the fetus, reaching a peak concentration at birth. When newborn nonhuman primates are fed taurine-deficient formula, growth is depressed, but this does not occur in human preterm infants, despite declining plasma and urine taurine levels. Nevertheless, there is some limited evidence that taurine supplementation might influence auditory brainstem evoked responses. It is important to note that currently available amino acid solutions have not been modified for more than 20 years and that none were designed specifically to meet the needs of extremely premature infants. Future research efforts should be directed at designing a fourth generation of amino acid solutions to optimize amino acid nutrition provided to the most vulnerable infants. As discussed earlier in this chapter, rates of glucose production and utilization in term infants are approximately 3 to 5 mg/kg per minute, whereas an extremely premature infant has a much greater need, 8 to 9 mg/kg per minute. Infants who weigh 1000 g or more usually tolerate a 10% glucose solution initially, whereas infants weighing less than 1000 g probably need to be started on a 5% glucose solution, given their higher total fluid requirements and predisposition toward hyperglycemia. The definition of hyperglycemia also varies but is generally set at a plasma level above 150 mg/dL (8. Alternatively, a lower concentration of dextrose solution can be used, although solutions less than 2. The appropriate balance of glucose and lipid in parenteral nutrition is critical for achieving maximal nutritional benefit. In fact, nutrient and protein retention is maximal if the nonprotein caloric balance between carbohydrate and lipid is approximately 60: 40. This more closely mimics the fat content of breast milk and minimizes excess energy expenditure, which can occur if a disproportionate amount of nonprotein calories is given as glucose. Even at higher protein intakes, a parenterally fed infant with extremely low birth weight may need 80 to 90 kcal/kg per day for nonprotein energy supplies. The caloric requirements of a parenterally fed neonate are much lower than those fed enterally. It is important to realize that providing excessive calories via parenteral nutrition does not correlate with higher rates of growth. In addition, it should be emphasized that it is not difficult to provide adequate nonprotein energy, and it can be done without using highly concentrated glucose solutions. They are made up of neutral triglycerides, egg yolk phospholipids to emulsify, and glycerol to adjust the tonicity. Emulsions containing fish oil provide a direct source of very long chain omega-3 fatty acids as docosahexaenoic acid and eicosapentaenoic acid. The early administration of intravenous lipids to preterm infants has been the subject of discussion and debate primarily centered on the acute metabolic effects of early intravenous lipids and potentially adverse effects, such as chronic lung disease and bilirubin toxicity as a result of free fatty acids displacing bilirubin from albumin binding sites. A meta-analysis found no increase in chronic lung disease resulting from early lipid administration to premature infants. Triglyceride concentrations are most often used as an indication of lipid tolerance, and maintaining triglyceride concentrations below 200 mg/dL seems prudent. Intravenous lipid emulsions may undergo lipid peroxidation, which may form organic free radicals and potentially initiate tissue injury. Light, especially phototherapy, may play some role in increasing lipid peroxidation in intravenous lipid emulsions. However, multivitamin preparations included in the intravenous solutions are a major contributor to a generation of peroxides, and lipid emulsions may have only a minor additive effect. Based on these studies, some clinicians protect intravenous lipid solutions from light, although the importance or efficacy of this practice is unclear. Lipid particles supplied by intravenous lipid solutions are similar in size to endogenously produced chylomicrons. Like chylomicrons, clearance of these lipid particles also depends on the activity of lipoprotein lipase. Heparin theoretically releases lipoprotein lipase from the endothelium into the circulation, but there is no evidence that this increases lipid utilization in preterm infants. In addition, increased lipoprotein lipase activity may produce high levels of free fatty acids and be in excess of the clearance capacity of the premature infant. Consequently, the routine addition of heparin to lipid emulsions for this purpose (to stimulate lipolysis) is not recommended on the basis of currently available evidence. Carnitine facilitates transport of long chain fatty acids through the myocardial membrane, and as such plays an important role in the oxidation of these long chain fatty acids. Premature infants receiving parenteral nutrition have low carnitine levels, but the clinical significance of this remains uncertain. A Cochrane review found no evidence to support the routine supplementation of parenterally fed neonates with carnitine. Human Milk Fortifiers Human milk does not completely meet the nutritional needs of premature infants; insufficient protein, calcium, phosphorus, sodium, zinc, vitamins, and possibly energy are provided by human milk to optimally support most premature infants. Human milk fortifiers have been developed to address many of these inadequacies (Tables 43-6 and 43-7). Evaluation of the available evidence has shown that multicomponent fortification of human milk improves postnatal weight gain, linear growth, and head circumference growth. It is important to point out the significant difference in protein content (1 g/100 kcal) between the two bovine human milk fortifier products currently available. If the product containing the lower concentration of protein is used, an additional source of protein will be needed in infants less than 1 kg to meet estimated protein requirements. The use of powdered products is to be avoided, given potential risk of infectious complications. Benefits found in preterm infants with weight less than 1250 g included improvements in weight and linear growth at 28 days compared with infants randomized to a control powdered human milk fortifier. A small, multicenter, randomized clinical trial evaluated the use of an exclusive human milk diet compared with maternal milk fortified with bovine human milk fortifier and preterm formula.
Purchase glucovance overnight delivery
Performance of a Fetal Echocardiogram Each fetal echocardiogram must be individualized stroke treatment 60 minutes generic glucovance 400/2.5 mg on-line, depending on the nature of the suspected cardiac lesion, as well as the status of the mother and fetus. At a minimum, it must involve a thorough examination of the four-chamber view, both arterial outflow tracts, three vessels and trachea view, and an assessment of pulmonary venous return. There is broad variation in anatomy in different congenital heart diseases, including situs inversus, ventricular inversion, transposition of the great arteries, heterotaxy syndromes, and a host of other complex configurations of the heart. The first step is to determine the fetal position in space and establish a right-left and cranial-caudal axis. This allows for good assessment of biventricular function, mitral valve abnormalities, pulmonary venous return, outflow tracts, conal septal defects, and branch pulmonary arteries. If a thymus cannot be visualized, one must investigate the fetus for 22q11 deletion syndrome and all the cardiac disorders associated with it. Other means are simultaneous Doppler interrogation of inflow and outflow tracts or venous and arterial Doppler. Pulsed-wave Doppler interrogation of all valvular, arterial, and venous structures must be obtained in a complete fetal echocardiogram. Venous structures to be sampled include the systemic venous inflow superior vena cava and the inferior vena cava, at least two pulmonary veins, the ductus venosus, and the umbilical vein. Other structures that may be helpful to assess include the middle cerebral artery, hepatic veins, and any abnormalappearing Doppler signal. Fetal Pathology Fetal heart failure is associated with placental edema and resultant hypoxia. The mature heart response to hypoxia is to increase the heart rate, but the fetus decreases its heart rate in response to hypoxia. The differential diagnosis of the underlying cause of hydrops is broad (Box 82-1). Chemoreceptors in the fetal aorta respond to aortic pO2 below 18 to 19 mm Hg, inducing bradycardia. The blood flow to the myocardium, adrenals, and brain is increased (sampling of the middle cerebral artery may show increased diastolic velocities, the so-called "brain sparing effect") while the flow to the renal system, skin, muscle, bones, and gastrointestinal system is decreased. Doppler of the umbilical artery shows decreased diastolic flow and increased resistance. Theatrialwall motion (A) is in a one-to-one relationship with the ventricular wall motion(V). Immune Rh incompatibility leading to anemia Infection Viral hepatitis leading to decreased protein production Viral infection leading to anemia (parvovirus) Cardiac Congenital heart disease with severe tricuspid regurgitation. Adapted from Wieczorek A, Hernandez-Robles J, Ewing L, et al: Prediction of outcome of fetal congenital heart disease using a cardiovascular profile score. However, postnatal studies have shown abnormalities in vascular compliance and increased pulse wave velocities of the donor twin. Donor hormones from the response to hypovolemia are transferred across the placenta to the recipient twin. These include the cardiac function, cardiac size, the systemic venous Doppler profile of the ductus venosus or umbilical vein, atrioventricular valve regurgitation, and presence of pericardial effusions, pleural effusions, ascites, or skin edema. This should include resolving abnormal peripheral impedance and treating high output failure, myocardial dysfunction, arrhythmia, anemia, or twin-twin transfusion. Although the overall mortality did not differ in the prenatal versus postnatal groups, prenatal diagnosis was associated with fewer adverse neurologic events compared with those with postnatal diagnosis. Further studies into markers of outcome in these patients and improved survival may depend on fetal intervention. This attempt was successful and the infant eventually underwent a biventricular repair. Ideally, fetal cardiac interventional procedures are performed percutaneously to limit maternal risks. The least invasive technique involves maternal sedation with percutaneous access to the fetus. More invasive methods, which increase maternal risk, have the benefit of better fetal position. The underlying hypothesis in support of many fetal cardiac interventions is that the left ventricle Impact of Prenatal Diagnosis the goal of early detection of a pathologic state is to alter the long-term outcome in a favorable way. All of the patients who were diagnosed prenatally survived, whereas only 65% of the patients who were diagnosed postnatally survived. In addition, the patients diagnosed prenatally had a lower incidence of preoperative acidosis, tricuspid regurgitation, and ventricular dysfunction, and were less likely to need preoperative inotropic medications or bicarbonate. This, combined with altered coronary perfusion caused by a longer retrograde pathway and the elevated subendocardial wall stress, may be the cause of myocardial damage and replacement with fibrous tissue. Criteria for selection for fetal aortic valve balloon dilation currently include a large left ventricle with persistent patency of the aortic valve, a normal-appearing mitral valve, reversed flow in the aortic arch, and a left-to-right shunt at the atrial level. Postnatal mortality is extremely high in this group of patients, with reported rates of 48% to 80%. This suggests that mortality risk may be associated with intrapulmonary arterial or venous changes. Likewise, the spatial position and orientation of interventional devices inside the fetal heart was far better demonstrated with this novel imaging modality. The fixed intraesophageal position of the catheter permits alignment with the interventional needle shaft during percutaneous transthoracic fetal cardiac access. Conventional maternal transabdominal echocardiogram remains instrumental during this critical procedural step. By offering color Doppler, pulsed-wave Doppler, and continuouswave Doppler interrogation of the fetal heart from the esophagus, fetal transesophageal echocardiography may permit immediate assessment of the results of intracardiac manipulations as well as fetal hemodynamics. Comparison between pulsedwave Doppler- and tissue Doppler-derived Tei indices in fetuses with and without congenital heart disease. Utility of fetal echocardiography in postnatal management of infants with prenatally diagnosed congenital heart disease. Guidelines for the evaluation of heart failure in the fetus with or without hydrops. Fetal transesophageal echocardiography: clinical introduction as a monitoring tool during cardiac intervention in a human fetus. Intervention for severe aortic stenosis in the fetus: altering the progression of left sided heart disease. Assessment of left ventricular endocardial fibroelastosis in fetuses with aortic stenosis and evolving hypoplastic left heart syndrome. Novel Approaches to Prenatal Diagnosis of Congenital Heart Disease Just as with fetal intervention, there continue to be advances in the diagnostic realm. Promising results have been seen in performing fetal echocardiograms during the first trimester. The sensitivity of these early echocardiograms compared with the standard study was calculated as 60. Newer indices of ventricular performance, the Tei index or myocardial performance index, are currently being evaluated in the fetus. The Tei index is widely used as a measure of global (systolic and diastolic) myocardial function in adults and children. However, pitfalls of poor frame rates and false-positive results are still an issue. Screening fetal echocardiography in diabetic mothers with normal findings on detailed anatomic survey. Intrauterine pulmonary venous flow and restrictive foramen ovale in fetal hypoplastic left heart syndrome. Improved surgical outcome after fetal diagnosis of hypoplastic left heart syndrome. Although essential to normal fetal physiology, it normally constricts, closes, and becomes a fibrous remnant after birth. Failure of those processes, resulting in persistent ductal patency into childhood or adulthood, has been recognized as a significant pathology for many years. Evidence of benefit from those interventions has been slow to develop, however, and concerns have arisen about adverse effects of medical or surgical closure of the ductus. Although consensus regarding many aspects of management is lacking, the current approach consists of recognition of pathologic persistence of ductal patency, evaluation of hemodynamic consequences, and selection of strategies to minimize deleterious effects.