Purchase levitra 20 mg without a prescription
External compression of the rectum by a massive primary tumor may cause constipation erectile dysfunction pills non prescription generic levitra 10mg amex, but the rectal mucosa is rarely involved at initial diagnosis. Diagnosis, Clinical Evaluation, and Staging Diagnosis the long preinvasive stage of cervical cancer, the relatively high prevalence of the disease in unscreened populations, and the sensitivity of cytologic screening make cervical carcinoma an ideal target for cancer screening. In the United States, screening with cervical cytologic examination and pelvic examination has led to a decrease of >50% in the incidence of cervical cancer since 1975. The American Cancer Society, in conjunction with multidisciplinary working groups, recently updated the guidelines for cervical cancer screening. It is also reasonableto discontinue screening for women older than 65 to 70 years who have three or more consecutive negative studies and have had no abnormal test results in the past 10 years. Annual gynecologic examination might still be appropriate even if cytologic screening is not performed. The sensitivity of individual tests may be improved by ensuring adequate sampling of the squamocolumnar junction and the endocervical canal; smears without endocervical or metaplastic cells are inadequate, and in such cases the test must be repeated. The sensitivity of a screening program is increased by repeated testing; studies of the test frequency required to optimize the sensitivity of screening formed the basis of the American College of Obstetrics and Gynecology recommendations. Following application of a 3% acetic-acid solution, the cervix is examined under 10- to 15-fold magnification with a bright, filtered light that enhances the acetowhitening and vascular patterns characteristic of dysplasia or carcinoma. The skilled colposcopist can accurately distinguish between low- and high-grade dysplasia,205 but microinvasive disease cannot consistently be distinguished from intraepithelial lesions on colposcopy. Although some authorities advocate the routine addition of endocervical curettage to colposcopic examination, it is probably reasonable to omit this step in previously untreated women if the entire squamocolumnar junction is visible with a complete ring of unaltered columnar epithelium in the lower canal. Standard laboratory studies should include a complete blood cell count and renal function and liver function tests. Cystoscopy and proctoscopy should be considered in patients with bulky tumors and patients with imaging findings suggestive of organ involvement. Early studies of diagnostic preradiotherapy lymph node staging were discouraging because of the high complication rates observed when transperitoneal lymph node dissections were combined with large radiation fields. Today, laparoscopic methods are often used to reduce the perioperative morbidity and hospitalization times associated with surgical staging. The use of sentinel lymph node evaluation is expanding in cervical cancer, with high rates of detection of positive nodes in most studies reported. Pelvic lymphadenectomy is indicated for patients undergoing radical hysterectomy but is controversial in other settings. The detection of microscopic para-aortic or common iliac node involvement may identify patients who will benefit from extended-field irradiation, but lymphadenectomy can also add to the morbidity of treatment. Because patients with radiographically positive pelvic nodes are at greatest risk for occult metastasis to para-aortic nodes, these patients may have the greatest chance of benefiting from surgical staging. The use of diagnostic imaging techniques to assess tumor size and local extent is encouraged but not mandatory in the 2009 staging system. Some form of imaging must be performed to evaluate the presence or absence of hydronephrosis, but intravenous pyelography is no longer required. When the stage to which a particular case should be allotted is in doubt, the case should be assigned to the earlier stage. Furthermore, some authors have found that the predictive power of stage diminishes or is lost when comparisons are corrected for differences in clinical tumor diameter. Uterine-body involvement has been associated with an increased rate of distant metastases. Pelvic disease control rates were not correlated with histology, but the incidence of distant metastases was significantly higher in patients with adenocarcinomas. For patients with adenocarcinoma of the cervix, outcome appears to be correlated with the degree of tumor differentiation. Several investigators have correlated low intratumoral oxygen tension levels with a high rate of regional and distant metastasis and poor survival. Selected patients with centrally recurrent disease after maximum radiotherapy may be treated with radical exenterative surgery; isolated pelvic recurrence after hysterectomy is treated with irradiation. Because the risk of pelvic lymph node metastases from these minimally invasive tumors is <1%,232,276 pelvic lymphadenectomy is not usually recommended. Although reports suggest that recurrences are infrequent,277,278 patients who have this conservative treatment must be followed very closely with periodic cytologic evaluation, colposcopy, and endocervical curettage. The likelihood of residual invasive disease after cone biopsy is correlated with the status of the internal cone margin and the results of an endocervical curettage performed after cone biopsy. The authors did not find any correlation between the depth of invasion or the number of invasive foci and residual invasive disease. Therapeutic conization for microinvasive disease is usually performed with a scalpel while the patient is under general or spinal anesthesia. Because an accurate assessment of the maximum depth of invasion is critical, the entire specimen must be sectioned and carefully handled to maintain its original orientation for microscopic assessment. Complications occur in 2% to 12% of patients, are related to the depth of the cone, and include hemorrhage, sepsis, infertility, stenosis, and cervical incompetence. The uterus, cervix, upper vagina, and paracervical tissues are removed after careful dissection of the ureters to the point of their entry to the bladder. The medial halves of the cardinal ligament and the uterosacral ligaments are also removed. With this treatment, significant urinary tract complications are rare, and cure rates exceed 95%. Outcomes appear to be similar for patients treated with radical hysterectomy or radical trachelectomy,283 and successful pregnancies are reported in a significant percentage of patients after radical trachylectomy. This has led to the question of whether more conservative surgery, such as simple trachelectomy or cone with or without a nodal assessment, could be performed. An ongoing international study, ConCerv, is currently testing the safety and feasibility of conservative surgery in patients with low-risk features. Patients who wish to conserve fertility receive cervical cone with lymph node dissection and lymphatic mapping while patients who do not wish to conserve fertility undergo a simple hysterectomy with nodal assessment. Although surgical treatment is standard for in situ and microinvasive cancer, patients with severe medical problems or other contraindications to surgical treatment can be successfully treated with radiotherapy. Depending on the depth of invasion, these early lesions are treated with brachytherapy alone or brachytherapy combined with external beam irradiation, and cure rates exceed 95%. The goal of both treatments is to destroy malignant cells in the cervix, paracervical tissues, and regional lymph nodes. Patients who are treated with radical hysterectomy whose tumors are found to have high-risk disease features may benefit from postoperative radiotherapy or chemoradiation. Because young women with small, clinically node-negative tumors tend to be favored candidates for surgery and because tumor diameter and nodal status are inconsistently described in published series, it is difficult to compare the results reported for patients treated with surgery and those treated with radiotherapy. In the surgery arm, findings of parametrial involvement, positive margins, deep stromal invasion, or positive nodes led to the use of postoperative pelvic irradiation in 54% of patients with tumors 4 cm in diameter and in 84% of patients with larger tumors. Patients in the radiotherapy arm received a relatively low median dose to point A of 76 Gy. With a median follow-up of 87 months, the 5-year actuarial disease-free survival rates for patients in the surgery and radiotherapy groups were 80% and 82%, respectively, for patients with tumors that were 4 cm, and 63% and 57%, respectively, for patients with larger tumors. The authors reported a significantly higher rate of complications in the patients treated with initial surgery, and they attributed this finding to the frequent use of combined-modality treatment in this group. For patients with similar tumors, the overall rate of major complications is similar with surgery and radiotherapy, although urinary tract complications tend to be more common after surgical treatment and bowel complications are more common after radiotherapy. Surgical treatment tends to be preferred for young women with small tumors because it permits preservation of ovarian function and may cause less vaginal shortening. Radiotherapy is often selected for older, postmenopausal women to avoid the morbidity of a major surgical procedure. Because patients with these risk factors have an increased rate of pelvic disease recurrence, surgical treatment is usually followed by postoperative irradiation or chemoradiation, increasing the overall length of treatment and side effects of treatment. Two prospective randomized trials43,296 demonstrated that patients who are treated with radiation for bulky stage I cancers benefit from concurrent administration of cisplatin-containing chemotherapy. A third study suggested that patients who require postoperative radiotherapy because of findings of lymph node metastasis or involved surgical margins also benefit from concurrent chemoradiation. The uterine vessels are ligated at their origin, and the proximal third of the vagina and the paracolpium are resected. Ovarian metastases are rare in the absence of metastases to lymph nodes or other sites. If intraoperative findings suggest a need for postoperative pelvic irradiation, the ovaries may be transposed out of the pelvis. Radical hysterectomy is increasingly being performed using a laparoscopic approach with or without robotic assistance.
Discount 20mg levitra
Rituximab downmodulates levels of the antiapoptotic protein bcl-2 and may sensitize leukemia cells to fludarabine-induced apoptosis erectile dysfunction age factor discount levitra 20mg fast delivery. This trial achieved the primary end point of demonstrating a significantly higher complete remission rate of 47% in the concurrent group versus 28% in the sequential group. Notably, the incidence of grade 3 to 4 neutropenia was higher in patients who received concurrent fludarabine and rituximab (77%), compared to sequential (41%) treatment. No significant difference was seen in the incidence of infection between the two arms. The largest benefit was seen for patients with Binet stage A and B disease and patients younger than 70. Furthermore, a randomized trial did not show benefit with fludarabine in first-line treatment for these individuals. These molecules are being targeted for inhibition with small molecules as a therapeutic strategy. There was not a difference in activity between the two dose levels; 420 mg once daily is the recommended dose. The overall response rate was 71% (2 complete responses; 58 partial responses) by standard response criteria. Similar responses were noted across risk categories, including for high-risk del(17p), heavily pretreated, and advancedstage disease. Best response was typically achieved by 1 year on treatment, with lymph node responses occurring rapidly, and lymphocytosis requiring longer time to improve. Most patients had transiently increased lymphocytosis upon initiating treatment, which likely represents egress of leukemia cells from lymph nodes and other protective niches. The most common toxicity was diarrhea, occurring in 49% of patients, 95% of which were grade 12. Ibrutinib monotherapy was evaluated as first-line treatment in 31 patients 65 years old or older. This was a very well-tolerated treatment, and the overall response rate was 71%, with 13% complete response and 58% partial response, with durable remissions although limited follow-up. Diarrhea, fatigue, fever, and nausea were the most commonly reported adverse effects experienced by the patients treated with ibrutinib and were mild. For patients with residual disease after purine analoguebased therapy, the marrow is the usual site of involvement. Rituximab was administered to all patients at 375 mg/m2 first dose, 500 mg/m2 every 2 weeks for four doses, then every 4 weeks for three doses (eight total doses). Subsequently, trials evaluated first-line monotherapy, demonstrating tolerability, good responses, and durable disease control. Lenalidomide safety and toxicity concerns have been tumor lysis syndrome and tumor flare reaction, which occur upon initiation of treatment, as well as myelosuppression, which can be dose-limiting and occurs while patients are on treatment. Tumor lysis syndrome and tumor flare reaction have been minimized by initiating lenalidomide at low dose (2. Cellular Therapy for Chronic Lymphocytic Leukemia Chimeric Antigen ReceptorBearing T-Cell Therapy Immune-based cellular therapy takes advantage of the ability of the immune system to seek out and eliminate malignant cells in the body. It potentially provides a mechanism of surveillance to prevent recurrence of disease. Graft-versus-host reactions are avoided with autologous T cells, while inducing and enhancing a graft-versus-leukemia effect. The engineered gene is transduced into autologous T cells and expressed on the surface where it can bind to target antigen and induce T-cell activation, cytokine production, proliferation, and killing of cells expressing the target antigen. On-target effects include a leukemia-specific reaction as well as elimination of normal B cells, resulting in hypogammaglobulinemia. While very robust treatment effects were reported, including durable complete remissions, infusion-related side effects, and more notably, cytokine-release syndrome have been challenging. Hypogammaglobulinemia has inspired a search for better and more specific leukemia-associated or leukemia-specific antigens. A phase 1/2 trial of orally administered navitoclax was conducted and generated promising results. The majority of patients treated in the study had >50% reduction in leukemia counts, and some patients experienced reduction in lymph node size. Immunemodulation Lenalidomide, a thalidomide analogue, has immunemodulatory and antiangiogenic activities. The mechanisms of action and effects on the microenvironment are not well understood. Improvements in the platelet count, neutrophil count, and hemoglobin occurred in 81%, 59%, and 33% of patients, respectively. Because of the high cost of this therapy, monthly intravenous immunoglobulin therapy is best used in patients with hypogammaglobulinemia who experience repeated bacterial infections. Patients present with cytopenias, including neutropenia with accompanying infections, pure red cell aplasia, thrombocytopenia, and anemia. Serologic abnormalities, such as the presence of rheumatoid factor or antinuclear antibody, or both, hypergammaglobulinemia, and high 2-microglobin are frequent. Because lymphocyte counts are usually not elevated, diagnosis requires a high degree of suspicion and a careful examination of the peripheral blood smear and bone marrow. Early data with nonmyeloablative allogeneic transplant indicated almost universal engraftment, although the development of chimerism was slower than with myeloablative transplants. Patients with sensitive disease who were transplanted had a better outcome than those who had resistant disease. These cells are twice as large as normal lymphocytes, with the nuclei showing a loose chromatin pattern and villi-like cytoplasmic projections (best viewed under phase contrast microscopy). Hairy cells infiltrate the bone marrow in an interstitial or focal pattern, with clear zones in between cells ("fried egg appearance"). Multiple series have reported high response rates, with patients remaining in remission for many years. The majority of relapsed patients achieve second remission when retreated with pentostatin or cladribine. The choice of agent may depend on the duration of the first remission: if <3 years, an alternate agent should be used; if >5 years, the same agent may be given. The role of interferon-alpha is currently limited to patients who are unresponsive to nucleoside analogues. Monoclonal Antibody-Drug Conjugate A percentage of patients may relapse with cladribine-resistant disease. Side effects included transient hypoalbuminemia, elevated aminotransferase levels and in 2 of 16 patients, a reversible hemolytic-uremic syndrome developed. Neutralizing antibodies were identified in four (11%) patients, which prevented retreatment. The median number of courses given was four, and no dose-limiting toxicity was observed up to the highest dose tested. Monoclonal B lymphocytes with the characteristics of "indolent" chronic lymphocytic leukemia are present in 3. Unmutated Ig V(H) genes are associated with a more aggressive form of chronic lymphocytic leukemia. Relation of gene expression phenotype to immunoglobulin mutation genotype in B cell chronic lymphocytic leukemia. Integrated mutational and cytogenetic analysis identifies new prognostic subgroups in chronic lymphocytic leukemia. Clonal evolution, genomic drivers, and effects of therapy in chronic lymphocytic leukemia. Monitoring chronic lymphocytic leukemia progression by whole genome sequencing reveals heterogeneous clonal evolution patterns. Guidelines for the diagnosis and treatment of chronic lymphocytic leukemia: a report from the International Workshop on Chronic Lymphocytic Leukemia updating the National Cancer Institute-Working Group 1996 guidelines. Cyclosporin A for the treatment of cytopenia associated with chronic lymphocytic leukemia. A new prognostic classification of chronic lymphocytic leukemia derived from a multivariate survival analysis. Eradication of minimal residual disease in B-cell chronic lymphocytic leukemia after alemtuzumab therapy is associated with prolonged survival. Fludarabine compared with chlorambucil as primary therapy for chronic lymphocytic leukemia.
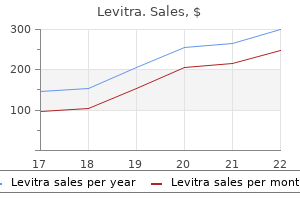
Buy levitra without a prescription
Histology shows a fibroblastic lesion with pleomorphism bph causes erectile dysfunction generic levitra 20 mg line, a characteristic curvilinear vascular pattern, and at least a 10% myxoid component. So-called fibrohistiocytic tumors 1260 Practice of oncology / Sarcomas of Soft Tissue and Bone Fibrous Histiocytoma Fibrous histiocytomas are benign tumors that usually present as solitary, slow-growing nodules, although up to one-third are multiple. Histologically, they consist of fibroblastic and histiocytic cells often arranged in a cartwheel or storiform pattern. When such lesions occur in the skin, they are often called dermatofibromas or sclerosing hemangiomas. Deeper lesions should be resected with a wider margin of normal tissue to prevent local recurrence. In rare cases, fibrous histiocytomas are aggressive ("malignant dermatofibromas"). These lesions have a propensity for local recurrence, have been reported to metastasize, and, in a few patients, can cause death. Copy number alterations have been detected in these tumors, suggesting an underlying molecular aberrancy resulting in an invasive phenotype. Angiomyolipoma the term angiomyolipoma is used for a nonmetastasizing renal tumor composed of fat, smooth muscle, and blood vessels. Angiomyolipomas may be solitary or multicentric, and they may produce abdominal pain or hematuria. Wide excision is curative, but tumors that are asymptomatic and not enlarging may be observed. Xanthoma Xanthoma refers to a collection of lipid-laden histiocytes and is seen in diseases associated with hyperlipidemia. These lesions are generally cutaneous or subcutaneous but may involve deep soft tissues. Liposarcoma Liposarcoma is primarily a tumor of adults, with a peak incidence between ages 50 and 65 years. Liposarcoma may occur anywhere in the body, although the most common sites are thigh and retroperitoneum. Each of these groups has distinctive morphology, natural history, and karyotypic and genetic aberrations, which can be of considerable help in diagnosis. Radiologic imaging typically shows coexistence of fatty and nonfatty solid components, which in the retroperitoneum may be discontiguous. Macroscopically, dedifferentiated liposarcoma consists of large multinodular yellow masses containing distinct nonlipomatous (dedifferentiated) areas, which are solid and often tan-gray. Dedifferentiated liposarcoma appears to have a lower risk of distant metastasis than other highgrade pleomorphic sarcomas. Nevertheless, among 65 patients adipocytic tumors Lipoma Lipomas are the most common benign soft tissue neoplasm. They usually arise in subcutaneous tissue, most frequently in trunk and proximal limbs. Although deep-seated benign lipomas do occur in the mediastinum or retroperitoneum, most fatty neoplasms in the retroperitoneum should be approached surgically as atypical lipomatous tumor/well-differentiated liposarcoma. Most lipomas are soft, painless, slow-growing, and solitary; however, 2% to 3% of patients have multiple lesions that are occasionally seen in a familial pattern. Lipomatosis is a term applied to a poorly circumscribed overgrowth of mature adipose tissue that grows in an infiltrating pattern. They are well circumscribed, being demarcated from surrounding fat by a thin, fibrous capsule. Most subcutaneous, solitary lipomas show reproducible cytogenetic aberrations: translocations involving 12q1315, rearrangements of 13q, or rearrangements involving 6p2133. Intramuscular lipomas differ from their more superficial counterparts by usually being both poorly circumscribed and infiltrative (in 90% of cases). Intramuscular lipomas typically present in midadult life as slow-growing, deep-seated masses most often located in the thigh or trunk. In a patient with a deep-seated fatty tumor, it is important to exclude atypical lipomatous tumor (see "Liposarcoma"), which tends to be more common than intramuscular lipoma. Angiolipomas present as subcutaneous nodules, usually in young adults, and in >50% of cases are multiple. Angiolipomas rarely grow >2 cm, but they often are painful, especially during their initial growth period. Microscopically, these tumors consist of adipocytes with interspersed vascular structures. Hibernoma Hibernoma is a rare, slow-growing, benign neoplasm that resembles the glandular brown fat of hibernating animals. These include losses centered at 3p1421, 3q29, 9p2224, 10p15, 11q2324, 17q21, and 19q13, and gains at 17p11 and 20q11. The 11q2324 loss was associated with genomic complexity and distinct morphology, whereas loss of 19q13 predicted poor prognosis. The tumor consists of small, evenly dispersed oval or plump cells with little cytoplasm in a myxoid matrix containing a variable number of fat cells. A small number of signet-ring cells and multivacuolated lipoblasts are often present but are not required for diagnosis. The myxoidround cell subtype usually occurs in the deep soft tissues of the extremities; in >66% of cases it occurs in the thigh musculature. More than 90% of myxoidround cell liposarcomas have a t(12;16)(q13-14;p11) translocation. In contrast to other liposarcoma types, myxoidround cell liposarcomas tend to metastasize to unusual sites in soft tissue or bone, with multifocal synchronous or metachronous spread to fat pad areas in the retroperitoneum and axilla occurring even in the absence of pulmonary metastasis. Most arise in patients older than 50 years and occur in deep soft tissue of the extremities (lower more frequently than upper). Clinically, they metastasize early to lung in >50% of patients, and these patients usually die within a short time. Pleomorphic liposarcomas typically have high chromosome counts, complex structural rearrangements, and multiple regions of significant copy number amplification and deletion. When they are symptomatic, hormone-regulated tumors can generally be cured by surgical resection; for hormonereceptornegative tumors, surgery is the treatment of choice. In three rare clinical scenarios involving symptomatic leiomyomas, management may be difficult. First, cutaneous leiomyoma is a form that arises from the piloerector muscles of the skin. The nodules most often arise on the extensor surfaces of the extremities, and they may follow a dermatomal distribution. Although these cutaneous leiomyomas are histologically benign, they frequently recur after surgical excision, and they are often so numerous that excision is not possible. Second, intravenous leiomyomatosis is a rare condition in which nodules of benign smooth muscle tissue grow within the veins of the myometrium and may extend into the uterine and hypogastric veins. The third management challenge is with diffuse peritoneal leiomyomatosis, which often occurs in association with pregnancy. Compression of adjacent organs may cause obstruction, as in other instances of sarcomatosis. Venous reconstruction, however, is rarely successful, as vein grafts rarely remain patent for prolonged periods. Moreover, patients generally develop collateral veins during the months after resection. Therefore, venous reconstruction can be deferred even in the context of inferior vena cava resection. Leiomyoma may also occur deep within the extremities, abdominal cavity, or retroperitoneum. Their histologic appearance is benign, with uniform, spindle-shaped nuclei in cells that appear similar to those of normal smooth muscle. Immunohistochemically, the cells are positive for smooth muscle markers such as smooth muscle actin. Angiomyoma is a histologic subtype of leiomyoma that tends to develop on the extremity at ages 30 to 60. Leiomyomas in women often express estrogen and progesterone receptors, which appear to activate Wnt signaling to promote proliferation of tumor stem cells. They are subdivided into adult, fetal, and genital type lesions; cardiac rhabdomyomas are associated with the tuberous sclerosis syndrome. Rhabdomyoma can be distinguished from rhabdomyosarcoma by its lack of nuclear atypia.

| Comparative prices of Levitra | ||
| # | Retailer | Average price |
| 1 | YUM! Brands | 171 |
| 2 | Delhaize America | 466 |
| 3 | H-E-B | 884 |
| 4 | O'Reilly Automotive | 515 |
| 5 | Neiman Marcus | 321 |
| 6 | Barnes & Noble | 132 |
| 7 | Verizon Wireless | 490 |
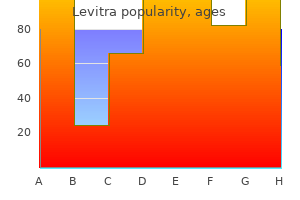
Cheap generic levitra uk
Among all patients erectile dysfunction middle age purchase levitra online from canada, ulceration, recurrent disease at entry, enrollment in E1684, and age >49 years significantly negatively impacted relapse-free survival. However, the interim analysis of E1697 after 1,150 of an originally planned 1,420 patients led to closing the study for futility. Cytotoxic Chemotherapy and Biochemotherapy in Adjuvant Therapy of Melanoma There has been a long list of prospective randomized clinical trials testing single-agent or combination-agent chemotherapy in the adjuvant setting, which have been nearly universally negative in terms of providing a clear clinical advantage over the control arm. Patients were stratified for number of involved nodes (one to three versus four or more), micro- versus macrometastasis, and ulceration of the primary. Pegylation results in substantially slower clearance of interferon after administration. This allows for more stable drug exposure than can be achieved with the shorter-lived conventional interferon- administered on alternating days by subcutaneous injection. Pegylated interferon can be administered less frequently and at a lower dose per injection but maintaining drug exposure over the course of several days. This results in a lower peak concentration after each dose while increasing the interval during which interferon is at biologically active concentrations in blood. Patients were prospectively stratified according to microscopic (N1) versus macroscopic (N2) nodal involvement, number of positive nodes, ulceration and tumor thickness, sex, and center. Despite the anticipation that Experimental Adjuvant Immunotherapy There has been a long list of large adjuvant clinical trials with a variety of immunotherapy approaches for melanoma with negative results. Murine and human data suggest that use of incomplete Freund adjuvant with short peptide vaccines may interfere with protective antitumor T-cell responses by recruiting T cells selectively back to the vaccine site rather than to the tumor. Also, the availability now of clinically effective immune therapies for advanced melanoma promises to open the door to new combination immune therapies in the adjuvant setting that will be explored in clinical trials over the next few years (see Table 94. National/International Guidelines for Follow-Up Recommendations for patient follow-up are largely based on the time-dependent risk of recurrence, the likely sites of metastasis, and historical experience with whether recurrences are commonly identified by the patient, the physician, or by imaging or laboratory studies. However, there is also evidence that follow-up is comforting to patients and decreases psychological stress associated with the diagnosis. Thus, routine clinical follow-up continues to be a part of management, but studies of follow-up have mostly been retrospective, and there is a need for more rigorous studies of the global benefit, risk, and cost of follow-up visits, imaging, and serum markers. Two comprehensive guidelines on melanoma management provide guidance on follow-up based on systematic review of the literature, and expert opinion. These two guidelines are very similar, but differ in the extent of cross-sectional imaging recommended, and the use of ultrasound for evaluation of the node basins. Follow-up visits should include history and physical exam, which should focus on skin exam of the primary site, regional nodes, and in-transit sites. Self-examination by the patient is also recommended, which depends on education of the patient and/ or family about what findings may signal recurrence. Chest X-rays were not recommended, but there was lower consensus (77%) for this than for most other German S3 recommendations. E1609 is an accruing clinical trial randomizing patients to ipilimumab at 10 mg/kg or 3 mg/kg for four doses, compared to a control arm receiving standard high-dose adjuvant interferon therapy. A study of neoadjuvant interferon for patients with palpable regional lymph node metastases was associated with an objective tumor response rate of 55%. Most studies conducted to date were retrospective analyses of patients diagnosed and relapsing in the era when there were very limited truly active treatment options. Therefore, diagnosing patients at an earlier time point had very little chance of improving outcomes other than resulting in a lead time bias in the assessment of survival. Site of first relapse was local/in-transit (28%), regional nodal (21%), or systemic (51%). First relapses were detected by the patient or family in 47% of cases, by the physician in 21%, and by screening radiologic tests in 32%. Distant metastases may include skin or soft tissue metastases distant from a known primary site or visceral, bone, or brain metastases. The prognosis is better for skin and subcutaneous tissue metastases, which are considered M1a, than for lung metastases (M1b) or other distant metastases (M1c). Most patients who develop distant metastases do so after an interval from their original management for clinically localized disease or after management for regionally metastatic disease. Patterns of Metastases Approximately 60% to 80% of first metastases are at local or regional sites including regional nodes. The most common first sites of visceral metastasis are lung and liver (about 10% each), and metastases to distant skin sites are also common. After an initial metastasis, subsequent metastases are more commonly visceral or distant and increasingly become multiple. Common visceral sites of metastasis are lung, liver, brain, gastrointestinal tract (especially small bowel), bone, and adrenal gland. In such patients, a new and growing mass in the chest or abdomen is likely to be metastatic melanoma, but tissue confirmation of metastatic melanoma is usually recommended. If there is a solitary lung mass, and especially if the mass is <1 cm in diameter, then thoracoscopic resection with preoperative localization can be performed with great success and with low morbidity. Fine needle aspiration biopsy of soft tissue masses or lymph nodes can be rapid and accurate diagnostic approaches either at the bedside or with radiologic localization. Similarly, biopsies of many other tissue lesions can be accomplished by minimally invasive techniques. A fine needle aspirate will be diagnostic in most cases, but a core needle biopsy, when feasible, can improve diagnostic accuracy further. It is best to test a metastatic lesion than an archival primary lesion as it cannot be assured that the metastases come from that particular primary lesion. In addition, assay panels that provide results from multiple hot-spot single nucleotide mutations have been developed, as well as assays based on next generation sequencing of a panel of several hundred genes that are commonly associated with cancer. There are numerous clinical scenarios in which surgery may be considered, and it is not possible to address all of them here. Cases in Which the Benefit of Surgery Is Clear Anemia due to occult bleeding from intestinal metastasis Bowel obstruction due to small bowel metastasis Cutaneous or subcutaneous metastasis with ulceration, pain, Lymph node metastasis with neurologic symptoms Symptomatic brain metastasis Life-threatening hemorrhage from metastasis Melanoma frequently metastasizes to the gastrointestinal tract. It usually originates as an intramural lesion but grows into the lumen and through the serosa with time. Nonetheless, when a patient presents with gastrointestinal blood loss or obstruction associated with a small bowel (or other gastrointestinal) metastasis of melanoma, operation is usually indicated. If the tumor involves the mesenteric nodes and is matted, then it may not be feasible or appropriate to resect the entire tumor, but enteroenteric bypass of the obstruction will be palliative. Resection of most or all small bowel metastases can manage bleeding and obstruction effectively. However, if there are numerous small bowel metastases, then excision of large lesions with reanastomosis is appropriate, but small lesions may be excised by partial-diameter excision and stapled (or sewn) closure. If the patient can be rendered surgically free of disease, then there may be long-term survival >5 years in as many as 25% of patients and mean survival >2 years. Because such lesions usually can be resected under local anesthesia with minimal morbidity, it is reasonable to offer resection. Extensive lymph node metastasis with neurologic symptoms is commonly an issue in the axilla, where tumor growth may compress or invade the brachial plexus and axillary vein. Patients with extensive axillary recurrence with neurologic symptoms and patients with other nodal disease and neurologic symptoms should be considered for radical resection of the involved nodal basin. The morbidity of surgery usually is much less than the morbidity of the tumor left untreated. Major risks of tumor growth include paralysis or major neurologic dysfunction of the extremity, intractable lymphedema, disabling pain, and unresectability. Brain metastasis is a particularly ominous sign in terms of future survival, which can usually be measured in months. However, some patients with isolated brain metastasis can have long-term control after surgical resection or stereotactic radiation therapy. For patients with symptomatic brain metastases, the presentation with acute cognitive deficits can be dramatic. Steroid therapy should be instituted immediately (4 mg orally every 6 hours per day initially). However, if this fails, or if the presentation is particularly acute with impending herniation, then surgical resection of the brain metastasis can be therapeutic. Melanoma can metastasize to nodes, adrenal glands, or other sites and then develop spontaneous hemorrhage. Sometimes such bleeding can be trivial, but in some cases, there can be massive hemorrhage into the tissues, with associated hypovolemia.
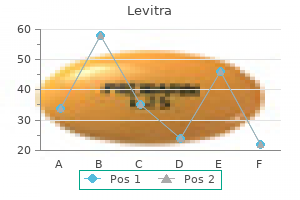
Generic levitra 10 mg with mastercard
Partial pancreaticoduodenectomy can provide cure for duodenal gastrinoma associated with multiple endocrine neoplasia type 1 otc erectile dysfunction pills walgreens levitra 20 mg for sale. Determinants of metastatic rate and survival in patients with Zollinger-Ellison syndrome: a prospective long-term study. Surgery for asymptomatic pancreatic lesions in multiple endocrine neoplasia type 1. Gastric carcinoid tumors in multiple endocrine neoplasia-1 patients with Zollinger-Ellison syndrome can be symptomatic, demonstrate aggressive growth, and require surgical treatment. Unilateral adrenalectomy for pheochromocytoma in multiple endocrine neoplasia type 2 patients. The characterization of pheochromocytoma and its impact on overall survival in multiple endocrine neoplasia type 2. Peak incidence of pheochromocytoma and primary hyperparathyroidism in multiple endocrine neoplasia 2: need for age-adjusted biochemical screening. Surgical curability of medullary thyroid cancer in multiple endocrine neoplasia 2B. There is currently no evidence of genotype phenotype correlations, and interfamilial and intrafamilial variability is the rule. These tumors occur in 80% to 95% of patients by the age of 50 years,5,810 and are typically multiglandular and often hyperplastic. These tumors are usually multicentric and can arise in the pancreas or more commonly as small (<0. A full review of surgical options is outside the scope of this review, but this topic has been reviewed elsewhere. Parathyroid abnormalities are the least common finding, occurring in up to 30% of patients. For families that do not have a detectable mutation, management recommendations can be based on the clinical features in the affected individual and in the family. There are six or more facial papules, of which three or more must be trichilemmoma, or b. Two or more major criteria, but one must include macrocephaly or LhermitteDuclos disease; or 3. Four minor criteria Operational diagnosis in a family where one individual is diagnostic for Cowden syndrome: a. Given their rarity, and their recent discoveries, less is known about their clinical presentation. Mutations fibrocystic disease in 40% to 75% of females), gastrointestinal polyps (80%), macrocephaly (80%), and uterine fibroids (25% to 44% of females). It has an estimated birth incidence of 1 in 36,000 per year105 and is inherited in an autosomal dominant manner with a high degree of interfamilial and intrafamilial variability. Several clinical and genetic screening algorithms have been proposed to assist clinicians in deciding which genes to test and in which order,52,109,110 as testing for mutations in five different genes in every patient may not be feasible or cost-effective. A number of algorithms have been proposed whereby testing decisions are based on a variety of factors including presence of clinical features, early age at diagnosis, location and laterality of tumor(s), positive family history, and presence of malignancy. For at-risk patients with known mutations, there are no consensus guidelines as to the appropriate screening protocols. The variable penetrance and spectrum of manifestations of multiple endocrine neoplasia type 1. Hyperparathyroidism presenting as the first lesion in multiple endocrine neoplasia type 1. Parathyroid carcinoma in multiple endocrine neoplasia type 1 with a classic germline mutation. Gastrinomas in the duodenums of patients with multiple endocrine neoplasia type 1 and the ZollingerEllison syndrome. Determinants of metastatic rate and survival in patients with ZollingerEllison syndrome: A prospective long-term study. Prospective endoscopic ultrasonographic evaluation of the frequency of nonfunctioning pancreaticoduodenal endocrine tumors in patients with multiple endocrine neoplasia type 1. Multiple endocrine neoplasia type 1 in patients with recognized pituitary tumours of different types. Multiple endocrine neoplasia type 1 and ZollingerEllison syndrome: A prospective study of 107 cases and comparison with 1009 cases from the literature. Multiple endocrine neoplasia type 1 gene maps to chromosome 11 and is lost in insulinoma. Germ-line mutation analysis in patients with multiple endocrine neoplasia type 1 and related disorders. Role of multiple endocrine neoplasia type 1 mutational analysis in clinical practice. Care for patients with multiple endocrine neoplasia type 1: the current evidence base. Medullary thyroid cancer: Management guidelines of the American Thyroid Association. Medullary carcinoma of the thyroid: Prognostic factors and treatment recommendations. Prognostic significance and impact on treatment of clinical and pathologic variables. Medullary thyroid carcinoma: Clinical characteristics, treatment, prognostic factors, and a comparison of staging systems. Multiple endocrine neoplasia type 2B (mucosal neuroma syndrome, Wagenmann-Froboese syndrome). Multiple endocrine neoplasia 2B syndrome due to codon 918 mutation: Clinical manifestation and course in early and late onset disease. Localisation of the gene for multiple endocrine neoplasia type 2A to a 480 kb region in chromosome band 10q11. Genetic linkage studies map the multiple endocrine neoplasia type 2 loci to a small interval on chromosome 10q11. Comparison of diagnostic accuracy of urinary free metanephrines, vanillyl mandelic acid, and catecholamines and plasma catecholamines for diagnosis of pheochromocytoma. Pheochromocytoma: recommendations for clinical practice from the First International Symposium. Current and future anatomical and functional imaging approaches to pheochromocytoma and paraganglioma. Estimated risk of pheochromocytoma recurrence after adrenal-sparing surgery in patients with multiple endocrine neoplasia type 2A. GeneReviews at GeneTests: Medical Genetics Information Resource [database online]. Germline mutations and variants in the succinate dehydrogenase genes in Cowden and Cowden-like syndromes. Genetics and clinical characteristics of hereditary pheochromocytomas and paragangliomas. Paraganglioma after maternal transmission of a succinate dehydrogenase gene mutation. The succinate dehydrogenase genetic testing in a large prospective series of patients with paragangliomas. The genetics of phaeochromocytoma: using clinical features to guide genetic testing. Endocrine cancer predisposition syndromes: Hereditary paraganglioma, multiple endocrine neoplasia type 1, multiple endocrine neoplasia type 2, and hereditary thyroid cancer. Clustering of features of von HippelLindau syndrome: evidence for a complex genetic locus. Clinical predictors and algorithm for the genetic diagnosis of pheochromocytoma patients. They pose a significant therapeutic challenge because about 50% of patients with newly diagnosed sarcoma eventually die of disease. Sarcomas also pose significant diagnostic challenges because there are more than 70 histologic subtypes with unique molecular, pathologic, clinical, prognostic, and therapeutic features.
Buy genuine levitra on line
Rare sites of primary lymphoma include the orbit erectile dysfunction treatment natural in india cheap generic levitra canada, heart, breast, salivary glands, the thyroid, and the adrenal gland. Diagnosis and Initial Management After the initial biopsy, a careful history and physical exam should be done to help assess the extent and pace of disease. Concurrent illness that may impact therapy or monitoring on therapy should be ascertained, including a history of diabetes or congestive heart failure. Laboratory studies should be obtained, including complete blood count, routine chemistries, liver function tests, and serum protein electrophoresis to document the presence of circulating monoclonal paraproteins. A bone marrow biopsy should be considered for staging and prognostic purposes depending on the disease histology and the results of other laboratory and staging studies. Imaging studies depend on the histology of the lymphoma as well as the clinical presentation. The prognosis is more dependent on histology and clinical parameters than the stage at presentation. Four risk groups were identified based on the number of risk factors: low risk (0 or 1); low intermediate (2); high intermediate (3); and high (4 to 5). Patients 60 years with zero, one, two, or three risk factors had 5-year survival rates of 83%, 69%, 46%, and 32%, respectively. Survival rates for those age >60 years with the same scores were 56%, 44%, 37%, and 21%, respectively. Within that model, the 4-year progression-free survival is 94%, 80%, and 53% for zero and one, two, or three or more risk factors, respectively. The 10-year survival rates for patients with zero to one (low risk), two (intermediate risk), or three or more (high risk) of these adverse factors averaged 71%, 51%, and 36%, respectively. These prognostic indices take into account the proliferative index and cell surface markers, respectively. Restaging after treatment is typically done 6 to 8 weeks following the completion of chemotherapy (or chemoimmunotherapy), or 8 to 12 weeks after the completion of radiotherapy or combination chemotherapy and radiotherapy, to assess for disease response to treatment. The most important prognostic factor is the achievement of a complete response to therapy. Restaging at the completion of treatment is often with the repetition of studies that were abnormal at diagnosis. It should be noted that patients with certain lymphomas or bulky disease may not have complete regression of their lymphadenopathy despite there not being any remaining active lymphoma. Patients are usually adolescent or young adult males who present with lymphadenopathy in cervical, supraclavicular, and axillary regions (50%) or with a mediastinal mass (50% to 75%). These masses can be associated with superior vena cava syndrome, tracheal obstruction, and pericardial effusions. Less commonly, patients present with extranodal disease (skin, testicular, or bony involvement). Although the bone marrow can be uninvolved at presentation, virtually all patients develop bone marrow infiltration and a subsequent leukemic phase indistinguishable from T-cell acute lymphoblastic leukemia. B-cell lymphoblastic lymphoma is a very rare entity, with patients having a median age of 39 years. The treatment of precursor B-cell and T-cell lymphoblastic leukemia/lymphoma is detailed in Chapter 110. The clinical aggressiveness of the tumor correlates with the number of centroblasts that are present. Involvement of the peripheral blood with malignant cells is commonly seen, and morphologically, these cells have notches and have been referred to as buttock cells. Cytologically, both are composed of blasts with a high nuclear-to-cytoplasmic ratio, scant cytoplasm, and nuclei with slightly coarse chromatin with multiple small nucleoli. Approximately 85% to 90% of lymphoblastic lymphomas are of the T-cell lineage, with the remainder being of the B-cell type. Both are comprised of tumor cells with immunophenotypes that correspond to stages of pre-T and pre-Bcell development, respectively. Most lymphoblastic tumors are positive for TdT, a specific marker of immature lymphoid cells that can be detected by flow cytometry or immunohistochemistry. Bone marrow involvement is present in 70% of patients, whereas involvement of other nonlymphoid organs is uncommon. In a small subset of patients, the disease presents in the intestine; such patients usually have an early stage and a favorable prognosis. Treatment of Advanced Stage Disease the overwhelming majority of patients have advanced stage disease at diagnosis. This approach is supported by randomized prospective trials of observation versus immediate treatment. One of the largest trials compared immediate treatment with chlorambucil to observation. Similar results have been noted in other prospective trials of initial treatment versus observation. A retrospective analysis of good risk patients who were either observed or received single-agent rituximab97 found no negative impact of watchful waiting. The median time to next treatment was 34 months in the watch and wait patient but was not reached in the rituximab-treatment arm. The important issues of time to second therapy, quality of life, impact on histologic transformation, cost, toxicity, and future responses to rituximab are not yet addressed. These studies, which have observed an impact on the prognosis of reactive macrophages and T cells, need additional study in larger data sets and a prospective design with uniformly treated patient populations. However, significant neutropenia and opportunistic infections were observed with these regimens. The 151 patients with responding or stable disease at week 12 were randomized to no further treatment or prolonged rituximab maintenance every 2 months for four doses. At a median follow-up of 35 months, patients who received the prolonged rituximab maintenance had a twofold increase in event-free-survival (23 months versus 12 months). With a longer follow-up, 45% of newly diagnosed patients in this study were in remission at 8 years with the addition of maintenance rituximab. Maintenance rituximab has also been shown to benefit patients who received chemotherapy without rituximab as part of the initial treatment. However, in the context of current induction therapy that includes chemotherapy and rituximab in the majority of patients, it is uncertain if the response data to single-agent rituximab is as high or durable as in patients who received chemotherapy without rituximab as induction therapy. Given the current paradigm of chemoimmunotherapy and maintenance, the applicability of these data to presently treated patients is uncertain. Retreatment with these agents remains controversial, with uncertainty of delivery of full dose and concerns of second malignancies. There are no significant side effects of treatment, even in the head and neck region where higher doses would cause xerostomia and mucositis. Although single institution studies suggested that reinfusion of tumor-free stem cells led to a decreased relapse rate, it remains controversial as to whether there is a benefit, particularly now with rituximab treatment. Unfortunately, myeloablative conditioning has a treatment related mortality of up to 40%; however, the relapse rate is less than 20%. This includes monoclonal antibodies, idiotype vaccines, immunomodulatory agents, and novel drugs such as kinase inhibitors. These include several humanized antibodies that are designed to have less infusion toxicity and a better antibody-dependent cell-mediated cytotoxicity effector function. In a series from Stanford, previously untreated patients and patients with limited disease and no prior therapy at transformation had improved prognoses. Patients with histologic transformation can have later relapses with indolent lymphoma. These agents are undergoing additional study, in combination with chemotherapy and as maintenance following remission induction, to better define their role. It is histologically defined by the presence of more than 15 centroblasts per hpf. Cytogenetic abnormalities include trisomy 12, which is present in about 40% of cases, as well as 13q deletions (45% to 55% of cases), 11q deletions (17% to 20% of cases), and 17p deletions (7% to 10% of cases). Cases with 13q deletions have the most favorable prognosis, whereas those with del(11q) or del(17p) have an unfavorable prognosis. A serum paraprotein is found in about 20% of cases, and hypogammaglobulinemia is present in about 40%. The diagnosis is made by an examination of involved tissue, such as the lymph node or bone marrow. These larger lymphoid cells are usually clustered together in so-called proliferation centers, which are pathognomonic. In some cases, patients present with mixed cryoglobulinemia, possibly related to concurrent hepatitis C virus infection.
Purchase 10mg levitra with visa
The two- and threedrug combinations of novel agents described previously for newly diagnosed patients remains an important option erectile dysfunction treatment in jamshedpur purchase generic levitra pills. In this age group, which most of the time is not considered eligible for transplant, the combination of bortezomib, or lenalidomide, or both with dexamethasone is considered the preferred option. To manage toxicity, the dose of therapeutic agents, including dexamethasone, needs to be reduced in patients >75 years of age. With hydration, control of hypercalcemia, and effective therapy, it is reversible in 50% cases. Renal dysfunction of <6 months duration and the rapid initiation of therapy with a reduction in monoclonal protein are associated with a higher likelihood of improvement in renal function. Improved renal function is observed mainly in patients with light chain cast nephropathy and light chain deposition disease; therefore, renal biopsy is used to identify these reversible conditions and the need for aggressive treatment. This includes steroids, melphalan,341 cyclophosphamide, bortezomib,294,342 and thalidomide. Ease of administration, limited toxicity, and effectiveness make these novel agents the primary modes of therapy for myeloma patients with renal failure. In one retrospective analysis, 24 patients on dialysis were treated with bortezomib or bortezomib-based combinations. One patient was spared dialysis, and three other patients became independent of dialysis following bortezomib-based treatment. Because the pharmacokinetics of melphalan are unaltered by renal failure, such patients have been previously considered as potential candidates for high-dose therapy. Dose reduction and close monitoring are therefore needed to ensure the safety of the procedure, and the role of transplantation in the setting of renal failure remains investigational. Although the proportion of patients achieving complete responses has increased, all patients eventually relapse. Importantly, all three studies show a small increased incidence of second primary malignancy in the arms receiving lenalidomide compared to placebo. This has prompted a careful evaluation and discussion with the patient of the benefit of lenalidomide maintenance. Because of its significant benefit, lenalidomide is considered the standard of care for maintenance therapy in myeloma. Additionally, almost 50% 1-year mortality has limited use of this procedure to only a highrisk patient population. This study showed a superior median survival outcome for patients undergoing autotransplants compared to allogeneic transplants (34 versus 18 months, respectively). Case-matched comparative studies from other single institutions have also failed to show a survival advantage for allotransplants. However, patients undergoing syngeneic transplantation had significantly superior median survival time compared with autologous (72 months versus 25 months; p = 0. Allogeneic Transplantation Allogeneic transplantation has remained a difficult procedure in myeloma. Results from larger published studies evaluating nonmyeloablative regimens with allogeneic transplantation are listed in Table 112. The treatment was performed in an outpatient setting with a low 100-day mortality (2%). Treatment-related mortality did not differ significantly between the two groups, (p = 0. These results suggest a role for allografting, especially in patients with high-risk disease where improvement in longterm outcome has been limited. Bisphosphonates the second- and third-generation bisphosphonates, pamidronate and zoledronate, reduce skeletal complications and bone pain in myeloma Table 112. Preliminary reports of pamidronate administered alone frequently (every 2 weeks) have shown a response or delay in disease progression in occasional patients. For example, a randomized phase 3 multicenter international study has confirmed that the combination of bortezomib and pegylated liposomal doxorubicin is superior to bortezomib alone for both overall response (50% versus 42% respectively; p = 0. Lenalidomide has been evaluated in two large phase 3 studies comparing it in combination with dexamethasone to high-dose dexamethasone and placebo. Lenalidomide was equally active in patients with or without previous exposure to bortezomib or thalidomide. A pilot phase 1/2 study in relapsed refractory myeloma has evaluated the combination of lenalidomide and bortezomib in 38 patients. Thalidomide has also been an active agent, both alone and in combination with dexamethasone in relapsed patients (see Table 112. Although lenalidomide activity has been demonstrated in patients relapsing after thalidomide, it is unclear whether patients relapsing after lenalidomide will respond to thalidomide. A further analysis of this data suggested that its continued use beyond 2 years was beneficial. Interestingly, the study also showed that zoledronic acid reduced mortality by 16% versus clodronic acid (p = 0. Rates of complete, very good partial, or partial response did not differ significantly between the zoledronic acid and clodronic acid groups. Renal dysfunction induced by pamidronate affects mainly tubules and manifests first as proteinuria followed by a rise in creatinine, whereas zoledronic acid affects glomeruli and manifests as a rise in creatinine without proteinuria. Even mild renal dysfunction requires bisphosphonate dose adjustment, and renal effects of bisphosphonates can be partly prevented by extending the duration of infusion. Due to the increased detection of this complication, a prophylactic dental checkup and follow-up is recommended. In this study, 95% of 266 patients were refractory to their last therapy and 80% refractory or intolerant to both bortezomib and lenalidomide. Overall survival at 6 months was 78% and 67% in the 2- and 4-mg cohort, respectively. Among the 38 patients enrolled (including 22 with added dexamethasone), 42% achieved a minimal response or better, 21% achieved a partial response or better, and 3% achieved a complete response. The combination of bortezomib and Akt inhibitor perifosine is able to overcome bortezomib resistance. Detailed oncogenomic studies are identifying novel targets and pathways operative in myeloma, and ongoing studies are determining mechanisms of action of novel agents at a gene and protein level in order to provide the framework for rational combination clinical trials that will overcome drug resistance and improve patient outcomes. On a new substance occuring in the urine of a patient with mollities and fragilits ossium. Racial differences in the prevalence of monoclonal gammopathy in a community-based sample of the elderly. Prevalence of monoclonal gammopathy of undetermined significance among men in Ghana. A long-term study of prognosis in monoclonal gammopathy of undetermined significance. Role of Helicobacter pylori infection in the incidence and clinical course of monoclonal gammopathy of undetermined significance. Risk of multiple myeloma and monoclonal gammopathy of undetermined significance among white and black male United States veterans with prior autoimmune, infectious, inflammatory, and allergic disorders. Monosomy 13 is associated with the transition of monoclonal gammopathy of undetermined significance to multiple myeloma. Progression in smoldering myeloma is independently determined by the chromosomal abnormalities del(17p), t(4;14), gain 1q, hyperdiploidy, and tumor load. Dysregulation of cyclin D1 by translocation into an IgH gamma switch region in two multiple myeloma cell lines [see comments]. Activated fibroblast growth factor receptor 3 is an oncogene that contributes to tumor progression in multiple myeloma. Diverse karyotypic abnormalities of the c-myc locus associated with c-myc dysregulation and tumor progression in multiple myeloma. Rearrangements of the c-myc oncogene are present in 15% of primary human multiple myeloma tumors. Telomerase inhibition and cell growth arrest by G-quadruplex interactive agent in multiple myeloma. A validated gene expression model of high-risk multiple myeloma is defined by deregulated expression of genes mapping to chromosome 1. Prediction of survival in multiple myeloma based on gene expression profiles reveals cell cycle and chromosomal instability signatures in high-risk patients and hyperdiploid signatures in low-risk patients: a study of the Intergroupe Francophone du Myelome.
Buy levitra 10 mg with visa
Prognosis after ipsilateral breast tumor recurrence and locoregional recurrences in patients treated by breast-conserving therapy in five National Surgical Adjuvant Breast and Bowel Project protocols of node-negative breast cancer erectile dysfunction vitamin b12 discount 20mg levitra with mastercard. The annual incidence rate for recurrence elsewhere in the breast increased slowly to a rate of approximately 0. However, even when correction is done for the differing incidence of the pathologic features of the primary tumor between the age groups, young age is still associated with an increased likelihood of recurrence in the breast. Patients with breast cancer with a mutation have a substantial risk of contralateral and late ipsilateral breast cancers. In patients with a mutation, the option of bilateral mastectomy should be strongly considered to avoid the long-term risk of a second breast cancer in either breast. Patients with breast cancer most likely to benefit from bilateral mastectomy are those who are young and have early-stage disease. A close deep margin is not significant if the breast resection was carried down to the pectoral fascia; the same is true for a close anterior margin if the resection extended to the deep dermal surface. The results of randomized trials, reproducibility of margin assessment, and current patterns of multimodality care were also considered. This increased risk was not mitigated by favorable biology, endocrine therapy, or a radiation boost. Treatment-Based Risk Factors Other important treatment risk factors are the use of a boost and the use of adjuvant systemic therapy. A boost or supplementary irradiation to the area of the primary site is generally used. A negative margin is defined by absence of cancer cells at inked surfaces, but Practice of oncology 1130 Practice of oncology / Cancer of the Breast figure 79. The area of the primary in the upper outer quadrant is contoured in magenta and the heart is contoured in red. Note that for the actual treatment a block was used to block irradiation of her heart, which also blocked out some breast tissue well away from the primary cancer. Right upper is an axial view of the treatment fields in the center of the treatment fields. Other than the surgical scar, there is minimal difference between the treated and the untreated breast. Evolution of the untreated breast, such as change in size because of weight gain and the normal ptosis seen with aging, continue to affect the symmetry. The major factor determining the cosmetic result is the extent of surgical resection. For example, although the removal of a large tumor in the lower portion of the breast often results in distortion of the breast contour, this is only apparent with the arms raised and is acceptable to most women. A similar distortion in the upper inner quadrant of the breast, which is visible in most types of clothing, might not be as acceptable. If the mass is associated with microcalcifications, an assessment of the extent of the calcifications within and outside the mass should be made using magnification views. Mammography of the contralateral breast is also standard at the time of diagnosis to exclude synchronous lesions. However, women whose breasts are preserved have more positive attitudes about their body image and experience fewer changes in their frequency of breast stimulation and feelings of sexual desirability. Thus, an evaluation of both surgical margins and the extent of viable tumor elsewhere in the specimen is essential and may dictate resection of additional breast tissue even when margins are apparently tumorfree. The lack of a survival benefit for neoadjuvant therapy and the increased complexity in determining the appropriate extent of resection suggest that for women who are candidates for breast conservation at presentation, neoadjuvant therapy outside the context of a clinical trial offers little benefit. Examination of subsets of patients by age and tumor size did not find any statistically significant differences. Newer markers are needed to more reliably identify patients who can be safely treated with wide excision alone. Tamoxifen alone has its greatest appeal in older patients (older than 70 years)129 where competing risks of other illnesses are substantial. In a subset analysis, conventional fractionation had better results in patients with high-grade cancers. There is controversy whether cosmetic results are compromised relative to conventional whole breast external beam treatment. It found that rates of major coronary events increased linearly with the mean dose to the heart by 7. It is important to note the major limitations of the study; mainly, it is a case-control study and as such, it does not provide the highest level of evidence. For 50-year-old women without cardiac risk factors, the lifetime increased risk was 0. Notwithstanding these study limitations and improvements in technique, radiation oncologists should operate on the principle that there is no totally safe radiation dose to the heart, and that the heart dose should be kept as low as possible. A number of maneuvers, such as using cardiac blocks, prone techniques, and deep inspiration breath holds, make radiation delivery much safer in current practice. The mastectomy used today is a total or complete mastectomy, with removal of the breast tissue from the clavicle to the rectus abdominous and between the sternal edge and the latissimus dorsi muscles. The majority of postmastectomy recurrences occur in the skin or subcutaneous fat of the chest wall and present as palpable masses in the skin flap, so detection is not affected by the presence of the reconstruction. This finding is consistent with prior observations that the extent of skin removal in patients treated with mastectomy alone is not a major determinant of the risk of chest wall recurrence. Intraoperative frozen section of the tissue beneath the nipple is often used to minimize the risk of residual cancer. This is rarely the case for women with large, ptotic breasts, further limiting the application of this procedure. In summary, immediate reconstruction with preservation of the skin envelope of the breast has not been shown to alter the outcome of mastectomy or to delay the administration of systemic therapy. Immediate reconstruction has the advantages of avoiding the need for a second major operative procedure and the psychological morbidity of the loss of the breast. The two major reconstructive techniques involve the use of implants and/ or tissue expanders or the use of myocutaneous tissue flaps to create a new breast mound. Since that time, several epidemiologic studies have failed to demonstrate an increased incidence of connective tissue disorders in women with implants compared with matched control populations. Silicone implants are again available for use in patients with breast cancer, but many patients opt for saline implants or flap reconstructions as a result of the adverse publicity surrounding silicone implants. There is considerable variability in outcome reported in the medical literature for the same approaches, and there are no prospective studies reported to date. The figures for nonirradiated patients were 88% (p = not significant) and 85%, respectively. Implant loss occurred in 11% of patients with irradiated implants and 6% of nonirradiated pa- tients. In patients with significant cosmetic deformity, a secondary flap reconstruction is performed. This approach has the advantage of allowing preservation of the breast skin and providing the patient with a breast mound during what may be a prolonged course of postoperative cancer therapy. However, additional favorable experience with irradiation of expanders or implants at other institutions is needed. Complete flap loss is rare, but fat necrosis, fibrosis, and volume loss can occur. As in the native breast, the full cosmetic impact may not be evident until 3 years posttreatment. This is an area that continues to evolve, and multidisciplinary consultation between the oncologic surgeon, reconstructive surgeon, and radiation oncologist will help to ensure optimal patient outcomes. Initially, this was thought to be a critical component of the surgical cure of breast cancer. Complications of sentinel node biopsy are infrequent, with anaphylaxis to lymphazurin blue dye observed in 0. Care should be taken to excise any palpably abnormal nodes intraoperatively because lymph nodes that contain a heavy tumor burden may not take up the mapping agent. Caution should be used in proceeding directly to dissection without pathologic confirmation because the false-positive rate of physical examination is approximately 20%. Multicentric cancers and T3 primary tumors were initially thought to be contraindications to lymphatic mapping, but studies have shown that sentinel node biopsy is accurate in these circumstances. In one study with a median follow-up of 31 months, isolated axillary first failure was seen in only 3 of 4,008 patients (0.


