Purchase metoclopramide paypal
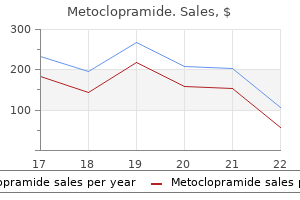
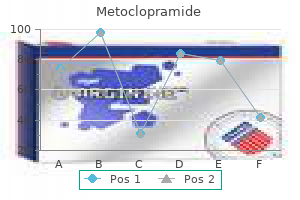
The repeated opening of channels allows a continuous efflux of potassium and influx of sodium gastritis and celiac diet order metoclopramide with a visa, and the resulting abnormal electrolyte balance distorts the function of the junctional membrane. The activity of the sodium-potassium adenosine triphosphatase pump in the membrane increases with increasing intracellular sodium and, by pumping sodium out of the cell and potassium into it, works to restore the ionic balance and membrane potential toward normal. As long as the depolarizing drug is present, the receptor channels remain open and ion flux through them remains frequent. All of these drugs may also have prejunctional effects on the rate and amount of transmitter released and mobilized. Distribution of acetylcholine receptors in developing adult, mature, denervated muscle or in immobilized or inflammationinduced catabolic muscle. A and B, In the early fetal stage, mononucleated myoblasts, derived from the mesoderm, fuse with each other to form multinucleated myotubes. C, As the nerve makes contact with muscle, clustering of the receptors occurs at the synapse and is associated with some loss of extrasynaptic receptors. E, Denervation and some other pathologic states, even without anatomic denervation. These receptor changes are potentially reversible if muscle immobilization, catabolism, and inflammation are restored to normal. Synthesis is directed by nearly all of the nuclei in the cell, and the receptors are expressed throughout the membrane of the muscle cell. As the fetus develops and the muscles become innervated, muscle cells begin to synthesize the mature isoform of receptors, which are exclusively inserted into the developing (future) end-plate area. Next, the nerve-induced electrical activity results in the repression of receptors in the extrajunctional area. Once begun, the process is very stable, and nuclei in the junctional area continue to express mature receptors. After the establishment of a nerve on the muscle, growth factors, including agrin and neuregulins, are released. Neuregulin signaling is essential for Schwann cell survival, and Schwann cells are essential for axonal maintenance. The innervation process progresses somewhat slowly during fetal life and matures during infancy and early childhood. In the active, adult, and normal innervated muscle, just the nuclei under and very near the end plate direct the synthesis of the receptor; only the genes for expressing mature receptors are active. Nuclei beyond the junctional area are not active, and therefore no receptors are expressed anywhere in the muscle cells beyond the perijunctional area. Proteins implicated in the linking of mature receptors to the cytoskeleton include integrin, syntrophin, utrophin, - and -dystroglycan, and rapsyn, just to name a few. Stimulation of a denervated muscle with an external electrical stimulus can prevent the appearance of immature receptors. It has been suggested that the calcium that enters the muscle during activity is important in the suppression process. The synthesis of immature receptors is initiated within hours of inactivity, but it takes several days for the whole muscle membrane to be fully covered with receptors. The changes in subunit composition (versus) in the receptor confer certain changes in electrophysiologic (functional), pharmacologic, and metabolic characteristics. Immature receptors have a smaller single-channel conductance and a twofold to tenfold longer mean channel open time than do mature receptors. The changes in subunit composition may also alter the sensitivity or affinity, or both, of the receptor for specific ligands. Depolarizing or agonist drugs such as succinylcholine and acetylcholine more easily depolarize immature receptors, thereby resulting in cation fluxes; doses one tenth to one hundredth of those needed for mature receptors can effect depolarization. Sensitivity to relaxants can begin to change between 48 and 72 hours after an injury or hospitalization. The resulting hyperkalemia can cause dangerous disturbances in cardiac rhythm, including ventricular fibrillation. However, hyperkalemia and cardiac arrest can occur after the administration of succinylcholine, even in the absence of denervation states. These effects are observed in certain congenital muscle dystrophies in which the muscle membrane is prone to damage by the depolarization produced by succinylcholine, resulting in potassium release via the membrane damage. They include various combinations of -subunits (1 through 10) and -subunits (1 through 4) and one each of -, -, and -subunits. Because a fasciculation is, by definition, the simultaneous contraction of the multitude of muscle cells in a single motor unit and because only the nerve can synchronize all the muscles in its motor unit, it became apparent that succinylcholine must also act on nerve endings. The functional characteristics of prejunctional receptor channels may also be different. For example, the depolarization of motor nerve endings initiated by the administration of acetylcholine can be prevented by tetrodotoxin, a specific blocker of sodium flux with no effect on the end plate. Specific information on the molecular organization of neuronal nicotinic receptors on the motor neuron terminal is still lacking. Some of the subunit composition is similar, but other subunits do not resemble those of the postjunctional receptor. Most strikingly, nervous tissue does not express -, -, or -receptor subunits; it contains genes only for the - and -subunits. The - and -subunit genes in nerve and muscle are not exactly the same; they are variants. To emphasize the distinction between neural and muscle nicotinic receptors, the former are sometimes designated Nn and the latter Nm. With so many different subunits available, possible combinations are many, and it is not known which combinations are found in motor nerves. In other parts of the nervous system, this positive feedback is complemented by a negative-feedback system that senses when the concentration of transmitter in the synaptic cleft has appropriately increased and shuts down the release system. The motor nerve terminal is also known to bear several other receptors, such as opioid, adrenergic, dopamine, purine, and adenosine receptors, as well as receptors for endogenous hormones, neuropeptides, and a variety of proteins. At this point, each junction may have more than one nerve terminal innervating it. Postnatal day 5 (P5): Approximately 5 days after birth, the postsynaptic membrane invaginates to form a gutter and small perforations develop on the plaque. The invaginations or clefts increase in numbers, resulting in more perforations in the pretzelshaped junction. Postnatal day 30 (P30): the neuromuscular junction is completely developed at 30 days after birth. A distinct set of postsynaptic proteins and signaling molecules are selectively transcribed in the subsynaptic area, providing integrity to the neuromuscular junction and efficient neurotransmission. With continued maturation, the plaque is transformed to a multiperforated pretzel-like structure. The polyinnervated end plate is converted to a singly innervated junction because of a retraction of all but one terminal. It is not surprising therefore that neurotransmission is not as efficient in the newborn and in patients with myasthenia gravis. The points of contacts between the prejunctional and postjunctional membrane decrease, resulting in a decline in trophic interactions between nerve and muscle and stimulus transmission. Despite these structural and functional changes associated with aging, the overall margin of safety is better in the older individual than in the neonate. Lennerstrand G, Bolzani R, Tian S, et al: Succinylcholine activation of human horizontal eye muscles, Acta Ophthalmol 88:872-876, 2010. Katz B, Miledi R: Estimates of quantal content during "chemical potentiation" of transmitter release, Proc R Soc Lond B Biol Sci 205:369-378, 1979. Jahn R, Fasshauer D: Molecular machines governing exocytosis of synaptic vesicles, Nature 490:201-207, 2012. Heidelberger R: Neuroscience: sensors and synchronicity, Nature 450:623-625, 2007. Schurch B: the role of botulinum toxin in neurourology, Drugs Today (Barc) 40:205-212, 2004. Schiavo G: Structural biology: dangerous liaisons on neurons, Nature 444:1019-1020, 2006. Karwa M, Currie B, Kvetan V: Bioterrorism: preparing for the impossible or the improbable, Crit Care Med 33:S75-95, 2005. Richtsfeld M, Yasuhara S, Fink H, et al: Prolonged administration of pyridostigmine impairs neuromuscular function with down-regulation of acetylcholine receptors with and without down-regulation, Anesthesiology 119:412-421, 2013. Jonsson M, Gulrey D, Dabrowski M, et al: Distinct pharmacologic properties of neuromuscular blocking agents on human neuronal nicotinic acetylcholine receptors: a possible explanation for the train-of-four fade, Anesthesiology 105:521-533, 2006.
Order metoclopramide
As the biologic foundations of behaviors once thought to be exclusively the realm of psychology are unraveled gastritis diet ���� order metoclopramide with a visa, for which anesthetics provide a valuable investigative tool, a comprehensive theory of anesthesia will also develop. Ueda I, Kamaya H: Kinetic and thermodynamic aspects of the mechanism of general anesthesia in a model system of firefly luminescence in vitro, Anesthesiology 38:425-436, 1973. Rudolph U, Antkowiak B: Molecular and neuronal substrates for general anaesthetics, Nat Rev Neurosci 5:709-720, 2004. Devor M, Zalkind V: Reversible analgesia, atonia, and loss of consciousness on bilateral intracerebral microinjection of pentobarbital, Pain 94:101-112, 2001. Tononi G: Consciousness as integrated information: a provisional manifesto, the Bio Bull 215:216-242, 2008. Detsch O, Vahle-Hinz C, Kochs E, et al: Isoflurane induces dosedependent changes of thalamic somatosensory information transfer, Brain Res 829:77-89, 1999. Bullmore E, Sporns O: the economy of brain network organization, Nat Rev Neurosci 13:336-349, 2012. Massimini M, Ferraretti F, Huber R, et al: Breakdown of cortical effective connectivity during sleep, Science 309:2228-2232, 2005. Rudolph U, Crestani F, Benke D, et al: Benzodiazepine actions mediated by specific gamma-aminobutyric acid(A) receptor subtypes, Nature 401:796-800, 1999. Nelson A, Faraguna U, Tononi G, Cirelli C: Effects of anesthesia on the response to sleep deprivation, Sleep 33:1659-1667, 2010. Wiklund A, Granon S, Faure P, et al: Object memory in young and aged mice after sevoflurane anaesthesia, Anesthesiology 109:790798, 2008. Wan Y, Xu J, Ma D, et al: Postoperative impairment of cognitive function in rats: a possible role for cytokine-mediated inflammation in the hippocampus, Anesthesiology 106:436-443, 2007. Avidan M, Evers A: Review of clinical evidence for persistent cognitive decline or incident dementia attributable to surgery or general anesthesia, J Alzheimers Dis 24:201-216, 2011. Zaugg M, Lucchinetti E, Uecker M, et al: Anaesthetics and cardiac preconditioning: I. Huneke R, Jungling E, Skasa M, et al: Effects of the anesthetic gases xenon, halothane, and isoflurane on calcium and potassium currents in human atrial cardiomyocytes, Anesthesiology 95: 999-1006, 2001. Tanaka K, Kawano T, Nakamura A, et al: Isoflurane activates sarcolemmal adenosine diphosphate-sensitive potassium channels in vascular smooth muscle cells-a role for protein kinase A, Anesthesiology 106:984-991, 2007. Yoshino J, Akata T, Izumi K, et al: Multiple actions of halothane on contractile response to noradrenaline in isolated mesenteric resistance arteries, Naunyn Schmied Arch Pharmacol 371:500-515, 2005. Huneke R, Fassl J, Rossaint R, et al: Effects of volatile anesthetics on cardiac ion channels, Acta Anaesthesiol Scand 48:547-561, 2004. Zeller A, Jurd R, Lambert S, et al: Inhibitory ligand-gated ion channels as substrates for general anesthetic actions, Handb Exp Pharmacol 182:31-51, 2008. Nury H, Van Renterghem C, Weng Y, et al: X-ray structures of general anaesthetics bound to a pentameric ligand-gated ion channel, Nature 469(7330):428-431, 2011. Flood P, Ramirez-Latorre J, Role L: Alpha 4 beta 2 neuronal nicotinic acetylcholine receptors in the central nervous system are inhibited by isoflurane and propofol, but alpha 7-type nicotinic acetylcholine receptors are unaffected, Anesthesiology 86:859-865, 1997. Dingledine R, Borges K, Bowie D, et al: the glutamate receptor ion channels, Pharmacol Rev 51:7-61, 1999. OuYang W, Jih T-Y, Zhang T-T, et al: Isoflurane inhibits NaChBac, a prokaryotic voltage-gated sodium channel, J Pharmacol Exp Ther 322:1076-1083, 2007. Kameyama K, Aono K, Kitamura K: Isoflurane inhibits neuronal Ca2+ channels through enhancement of current inactivation, Br J Anaesth 82:402-411, 1999. Takei T, Saegusa H, Zong S, et al: Increased sensitivity to halothane but decreased sensitivity to propofol in mice lacking the N-type Ca2+ channel, Neurosci Lett 350:41-45, 2003. Friederich P, Benzenberg D, Trellakis S, et al: Interaction of volatile anesthetics with human Kv channels in relation to clinical concentrations, Anesthesiology 95:954-958, 2001. Hamaya Y, Takeda T, Dohi S, et al: the effects of pentobarbital, isoflurane, and propofol on immediate-early gene expression in the vital organs of the rat, Anesth Analg 90:1177-1183, 2000. Fujiwara N, Higashi H, Nishi S, et al: Changes in spontaneous firing patterns of rat hippocampal neurones induced by volatile anaesthetics, J Physiol (Lond) 402:155-175, 1988. Bai D, Zhu G, Pennefather P, et al: Distinct functional and pharmacological properties of tonic and quantal inhibitory postsynaptic currents mediated by -aminobutyric acidA receptors in hippocampal neurons, Mol Pharmacol 59:814-824, 2001. Simon W, Hapfelmeier G, Kochs E, et al: Isoflurane blocks synaptic plasticity in the mouse hippocampus, Anesthesiology 94:10581065, 2001. Penttonen M, Buzsaki G: Natural logarithmic relationships between brain oscillators, Thalamus Relat Syst 2:145-152, 2003. Steriade M: Intracellular analysis of relations between the slow (<1 Hz) neocortical oscillation and other sleep rhythms of the electroencephalogram, J Neurosci 13:3266-3283, 1993. Madler C, Keller I, Schwender D, Poeppel E: Sensory information processing during general anaesthesia: effect of isoflurane on auditory evoked neuronal oscillations, Br J Anaesth 66:81-87, 1991. Buzsaki G, Wang X-J: Mechanisms of gamma oscillations, Annu Rev Neurosci 35:203-225, 2012. Antkowiak B, Hentschke H: Cellular mechanisms of gamma rhythms in rat neocortical brain slices probed by the volatile anaesthetic isoflurane, Neurosci Lett 231:87-90, 1997. Szarecka A, Xu Y, Tang P: Dynamics of firefly luciferase inhibition by general anesthetics: gaussian and anisotropic network analyses, Biophys J 93:1895-1905, 2007. Gottschalk A, Haney P: Computational aspects of anesthetic action in simple neural models, Anesthesiology 98:548-564, 2003. Cascio M, Xing Y, Gong D, et al: Mouse chromosome 7 harbors a quantitative trait locus for isoflurane minimum alveolar concentration, Anesth Analg 105:381-385, 2007. Increased uptake (as with a highly blood-soluble drug or high cardiac output) slows the rate by which anesthesia is induced by slowing the rate of rise of Palv. Conversely, low anesthetic solubility in blood is associated with rapid onset and offset of anesthesia. Changes in alveolar volume result in a rapid initial uptake of N2O, which sustains or increases concentrations of other alveolar gases (the second gas effect). The rate of clearance is also context sensitive; that is, equivalent decreases in alveolar and brain anesthetic concentrations are slower after a long exposure to inhaled anesthetics compared with a short period of exposure of equal depth. Significant toxic effects are usually produced in the tissues, such as liver and kidney, in which metabolism occurs. Modern inhaled anesthetics undergo less metabolism than older drugs do, resulting in fewer toxicities. These metabolites covalently modify liver proteins, creating neohaptens that elicit an immune response against hepatocytes. The incidence of the syndrome varies with different anesthetics, paralleling the extent of drug metabolism: halothane >> enflurane > isoflurane > desflurane. Free fluoride in blood can damage kidneys, resulting in high-output renal failure. Renal toxicity is almost exclusively associated with prolonged exposure to methoxyflurane. Sevoflurane metabolism also results in high fluoride levels in blood, but it does not damage kidneys. Factors that enhance the toxicity of methoxyflurane relative to sevoflurane include its high tissue solubility, slow clearance, and high degree of renal metabolism, resulting in high intrarenal fluoride levels for an extended time. Sevoflurane degrades to form compound A, which is associated with renal damage in rodents, but not in humans. This differential toxicity is associated with differential renal metabolism in rodents versus humans. In certain susceptible patients and in patients receiving many anesthetics that include N2O, methionine synthase inhibition can lead to hematologic and neurologic dysfunction. After prolonged N2O exposure, methionine synthase inhibition also increases blood homocysteine, which can increase vascular inflammation and the risk of thrombosis. Definitive clinical trials assessing the effects of N2O on morbidity in vasculopathic patients are lacking. The environmental impact of anesthetics can be lessened by reducing waste through the routine use of low fresh gas flows or with the use of new technologies that trap scavenged anesthetic gases. Reprocessing and reusing trapped anesthetic gases further reduces the environmental impact of drug production. Results from clinical cohort studies in children within the United States and Europe remain inconclusive about an association between early anesthetic exposures and learning or behavioral problems later in life (see Chapter 93). Regarding long-term effects of anesthesia and surgery on the adult brain, see Chapter 99. Optimal delivery of systemic drugs via inhalation requires a full understanding of the factors influencing how gas-phase compounds move into and out of various body tissues and how they are metabolized (pharmacokinetics) together with where and how these drugs and their metabolism affect tissue functions.
Buy cheap metoclopramide 10mg on-line
Under normal circumstances chronic gastritis recipes buy metoclopramide 10mg on line, blood from the anterior and posterior circulations does not admix because the pressures in the two systems are equal. The vessels that originate from the circle provide blood flow to welldelineated regions of the brain. However, in pathologic circumstances during which occlusion of one of the arterial branches occurs, the circle of Willis can act as an anteroposterior or side-to-side shunt to increase collateral blood flow to the region of the brain with reduced perfusion. However, substantial variability exists in the anatomy of the circle of Willis, and a significant proportion of individuals may have an incomplete circular loop. However, the space constraints imposed by the noncompliant cranium and meninges require that blood flow not be excessive. These mechanisms, which include chemical, myogenic, and neurogenic factors, are listed in Table 17-1. Rheologic Blood viscosity Neurogenic Extracranial sympathetic and Contribution and clinical parasympathetic pathways significance are poorly defined. Increased synaptic activity with the attendant release of glutamate leads to the downstream generation of a variety of mediators that affect vascular tone. Glia play an important role in flow-metabolism coupling, and their processes make contact with neurons. These processes may serve as conduits for the coupling of increased neuronal activity to increases in blood flow. Oxygen modulates the relative contribution of these pathways, and in the setting of reduced oxygen tension at the tissue level, the release of adenosine can contribute to vascular dilation. The net result therefore on vascular tone is determined by the relative contribution of multiple signaling pathways. These neurotransmitters may also potentially be involved in neurovascular coupling. Flow-metabolism coupling within the brain is a complex physiologic process that is regulated, not by a single mechanism, but by a combination of metabolic, glial, neural, and vascular factors. Synaptic activity leads to glutamate release, activation of glutamatergic receptors, and calcium entry in neurons. The maximum reduction occurs with the dose that results in electrophysiologic silence. At this point, the energy utilization associated with electrophysiologic activity has been reduced to zero, but the energy utilization for cellular homeostasis persists unchanged. The effects of hypothermia on the brain have been reviewed in detail5 (also see Chapter 54). Despite an equivalent or greater degree of reduction in the cerebral metabolic rate with thiopental, cortical evoked responses are better preserved3 than during anesthesia with isoflurane,4 which suggests that the electroencephalographic suppression achieved with different anesthetic drugs should not be assumed to be equivalent electrophysiologic states. The cumulative thiopental doses and expired concentrations of isoflurane and N2O are indicated in this figure. Consequently, a patient who has had a sustained period of hyperventilation or hypoventilation deserves special consideration. The mechanisms mediating cerebral vasodilation during hypoxia may include neurogenic effects initiated by peripheral and neuraxial chemoreceptors, as well as local humoral influences. The response to hypoxia is synergistic with the hyperemia produced by hypercapnia and acidosis. Even within the range over which autoregulation normally occurs, a rapid change in arterial pressure will result in a transient. The limits of autoregulation are conceptual constructs for the purpose of analysis. A continuum of vascular responsiveness in both the lower and upper limits probably exists as the ability of the arteriolar bed to dilate or constrict is exhausted. Furthermore, the morphologic form of the autoregulation is strongly influenced by the background level of vasodilation or vasoconstriction. The precise mechanisms, by which autoregulation is accomplished and its overlap with flow-metabolism coupling are not known. Autonomic innervation of cerebral blood vessels may also contribute to the autoregulation of blood flow (discussed in the next section). An extracranial sympathetic influence via the superior cervical ganglion, as well as parasympathetic innervation via the sphenopalatine ganglion, certainly exists in animals. The intraaxial pathways likely result from innervation arising from several nuclei in animals, including the locus coeruleus, the fastigial nucleus, the dorsal raphe nucleus, and the basal magnocellular nucleus of Meynert. The nature and influence of such pathways in humans are not known, and their manipulation for the purposes of clinical management remains to be systematically investigated. Catecholamine Agonists and Antagonists Numerous drugs with agonist and antagonist activity at catecholamine receptors (1, 2, 1, 2, and dopamine) are in common use. A drug may have direct effects on cerebral vascular smooth muscle or indirect effects mediated by the cerebral autoregulatory response to changes in systemic blood pressure (or both types of effects). The information in the following paragraphs and in Table 17-2 emphasizes data obtained from investigations of vasopressors in intact preparations and gives priority to the results obtained in humans and higher primates. However, this may result not only from a reduction in viscosity but also as a compensatory response to reduced oxygen delivery. In patients with focal cerebral ischemia, a hematocrit of 30% to 34% will result in optimal delivery of oxygen. However, manipulation of viscosity in patients with acute ischemic stroke is not of benefit in reducing the extent of cerebral injury. The actions of anesthetics are discussed in the section, "Effects of Anesthetics on Cerebral Blood Flow and Cerebral Metabolic Rate. Chapter 17: Cerebral Physiology and the Effects of Anesthetic Drugs 395 1-agoniStS. Such increases might occur if autoregulation were defective or its limit exceeded. In anesthetized patients,16-18 phenylephrine administration by bolus modestly reduced cerebral oxygen saturation (Sco2), measured by near-infrared oximetry. Ephedrine, although increasing arterial blood pressure to a similar extent as phenylephrine, did not reduce Sco2, presumably because of its ability to maintain cardiac output. Even a minor change in the volume of arterial and venous volumes within the region of the brain can affect the Sco2 measurement. In the absence of direct measurement of brain tissue oxygenation, a modest reduction in Sco2 in the face of increasing arterial blood pressure cannot be taken as evidence of impairment of cerebral oxygenation. In addition, phenylephrine did not decrease SjVo2, a more global measurement of cerebral oxygenation. Although unlikely, the concern is that 1-agonists might reduce cerebral perfusion in the injured brain. This class of drugs includes dexmedetomidine and clonidine, with the latter being a significantly less specific and less potent 2-agonist. The well-known effect of dexmedetomidine to decrease arterial blood pressure merits careful consideration if used in patients who are critically dependent on collateral perfusion pressure, especially in the recovery phase of an anesthetic. In two investigations in humans, propranolol, 5 mg intravenously,30 and labetalol, 0. The administration of fenoldopam leads to systemic vasodilation and a decrease in arterial blood pressure. In the surgical setting and in the neurocritical care unit, these drugs are administered to control arterial blood pressure acutely. Dendrite branching and volume progressively decrease, and the number of dendritic spines is reduced by approximately 25% to 35%. For instance, barbiturates are cerebral vasoconstrictors, yet some barbiturates actually cause relaxation of cerebral vascular smooth muscle in isolated vessel preparations. The data are derived from human investigations and are presented as percent change from unanesthetized control values. The reference to "reduced compliance" in this text is more correctly described as "increased elastance.
Best metoclopramide 10mg
The juxtaglomerular cells of the renal cortex secrete the proteolytic enzyme renin gastritis journal articles cheap 10 mg metoclopramide fast delivery, which cleaves angiotensinogen, a protein synthesized in the liver, and produces the decapeptide angiotensin I. This converting enzyme is located predominantly in the endothelial tissue of the lung. Lisinopril offers once-daily dosing, which is convenient for long-term use, but the drug can lead to troublesome hypotension if it is not held on the day of surgery and significant intraoperative blood loss occurs. Angioedema, especially after the first dose, affects the face, extremities, lips, mucous membranes, tongue, glottis, or larynx. Chapter 16: the Autonomic Nervous System 377 these agents should not be used at all during the second or third trimester of pregnancy. Their drug action is more specific, with fewer sites affected than with acetylcholine, and their duration of action is generally longer than that of acetylcholine. Unlike adrenergic pharmacology, in which the clinician can select from a wide choice of drugs, relatively few drugs influence parasympathetic function. In general, drugs that affect the parasympathetic system act in one of four ways: 1. As an antagonist by blocking or inhibiting the actions mediated by the cholinergic receptor 3. By inhibiting the enzymatic breakdown of acetylcholine and thereby causing an increased and prolonged effect No effective clinically used drugs act through mechanisms affecting the synthesis of acetylcholine (by inhibiting choline acetyltransferase) or by causing indirect release of acetylcholine. Hemicholinium, which interferes with choline uptake and could deplete acetylcholine stores, is not used clinically. Adenosine may inhibit the release of acetylcholine by decreasing the affinity of binding sites for calcium ions; aminoglycoside antibiotics compete with calcium for membrane calcium channels, as does magnesium. This toxin is sometimes given by local injection to treat strabismus and blepharospasm and has also been used for trigger point injections in pain clinics and to treat age lines. The popularity of offlabel uses of this toxin increases the chance of botulism poisoning. In a full-blown botulism poisoning syndrome, fatalities may result from muscle weakness and respiratory failure. Cholinergic agonists in clinical use have been derived from acetylcholine, but they resist hydrolysis by cholinesterase, which permits a useful duration of action. The different systemic effects of the cholinergic agonists are more quantitative than qualitative, although some limited organ selectivity is useful therapeutically, as seen with the synthetic choline esters bethanechol and carbachol. Methacholine and bethanechol are primarily muscarinic agonists; carbachol has significant nicotinic and muscarinic effects. Adding a methyl group to the position of the choline in acetylcholine produces methacholine, which is almost purely muscarinic and nearly totally resistant to hydrolysis by either of the cholinesterases. An intravenous infusion of methacholine causes hypotension and bradycardia; a small subcutaneous dose causes transient hypotension with a reflex increase in heart rate. The sole current use of methacholine is as a provocative agent in diagnosing hyperreactive airways, thereby making positive use of the deleterious bronchoconstrictive effect of muscarinic agonists. It is administered only by inhalation; serious adverse effects include gastrointestinal symptoms, chest pain, hypotension, loss of consciousness, and complete heart block when the drug is given orally or parenterally. An excessive bronchoconstrictive response should be treated by an inhaled -agonist; coexisting blockade is considered a contraindication to the use of methacholine. The carbamate derivative of methacholine, bethanechol, is occasionally used postoperatively to reinstitute peristaltic activity in the gut or to force the extrusion of urine from an atonic bladder. Bethanechol shows preferential activity at intestinal and urinary receptors relative to cardiac sites, so stimulation of the gastrointestinal tract and bladder is achieved with minimal cardiovascular effects. Bethanechol is usually given orally, but if gastrointestinal function is not adequate to permit absorption of an oral dose, the drug can be given subcutaneously as well. Carbachol is used topically or intraocularly to constrict the pupil for the long-term treatment of wide-angle glaucoma. When used topically, this drug is often better tolerated than the ophthalmic anticholinesterase agents, and it may be effective in patients resistant to pilocarpine and physostigmine. The rapid pupillary constriction is caused by the combination of ganglionic blockade and muscarinic effects. Another natural alkaloid, pilocarpine, was used to treat glaucoma until the advent of more modern drugs. Muscarinic Antagonists Muscarinic antagonists are the active ingredients in some common plants used since antiquity for medicinal and poisonous effects. Despite their age, muscarinic antagonists still represent important drugs in anesthesia and critical care. Muscarinic antagonists compete with neurally released acetylcholine for access to muscarinic cholinoceptors and block its effects. They also antagonize the actions of muscarinic agonists at noninnervated, muscarinic cholinoceptors. Presynaptic muscarinic receptors on the adrenergic nerve terminal may inhibit release of norepinephrine, and muscarinic antagonists may enhance sympathetic activity. As a result of its diffuse, nonselective actions and rapid hydrolysis by acetylcholinesterase and butyrylcholinesterase, acetylcholine has had almost no therapeutic use other than as an intraocular medication for transient constriction of the pupil during ophthalmic surgery. Research has revealed several subtypes of muscarinic receptors, and agonists and antagonists have been synthesized that bind preferentially to one or another of these subtypes. Pirenzepine preferentially blocks the M1 receptor, tripitramine shows highest affinity for the M2 receptor, and darifenacin binds preferentially to the M3 receptor. The distinctive pharmacology of the various antimuscarinic agents has played a major role in the development of new treatments of overactive bladder disorders. Oxybutynin, tolterodine, darifenacin, solifenacin, and trospium have all been developed to optimize the relief of bladder symptoms while minimizing effects on muscarinic receptors outside the bladder. Historically, muscarinic antagonists were used to treat peptic ulcer disease, various forms of spastic bowel syndrome, upper respiratory illness, and asthma. Atropine, once used to treat bronchospasm, was displaced with the introduction of 2-agonist drugs that did not dry secretions or diminish ciliary motility. Topical use of atropine analogues in ophthalmologic practice to dilate the pupil is still common. The addition of a muscarinic anticholinergic drug to anesthetic premedication for decreasing secretions and preventing harmful vagal reflexes was mandatory in the era of ether anesthesia, but it is less important with modern inhaled agents. Routine preoperative use of these drugs as antisialagogues continues in some pediatric and otorhinolaryngologic cases or when fiberoptic intubation is planned. In contrast, one of the synthetic antimuscarinic drugs, glycopyrrolate, does not cross the blood-brain barrier because of its quaternary structure and has gained popularity for this use. The patch preparation of scopolamine can be used prophylactically for motion sickness and for postoperative nausea and vomiting, but like the oral and parenteral forms, it may be associated with adverse eye, bladder, skin, and cognitive and psychological effects. It is very poorly absorbed when inhaled and has few extrapulmonary effects, even in extremely large doses by this route. Ninety percent of the inhaled drug is swallowed, but only 1% of the total dose is absorbed systemically. When administered to normal volunteers, ipratropium provides almost complete protection against bronchospasm induced by a variety of provocative agents. The bronchospastic effects of some agents, such as methacholine or sulfur dioxide, are completely blocked, whereas ipratropium has little effect on leukotriene-induced bronchoconstriction. The onset of bronchodilation is slow, and the maximum effect is less than that seen with -agonists. In general, the therapeutic effect of antimuscarinics, including ipratropium, is greater in patients with chronic obstructive pulmonary disease than in asthmatic patients. However, children depend more than adults on sweating for thermoregulation and can become dangerously hyperthermic when they are given these agents. Moreover, older individuals may not be able to - - 0, No effect; +, mild effect; ++, moderate effect. Increasing doses of atropine or scopolamine cause greater distortions of mentation that progress from thought disorders to hallucinations, delusions, delirium, and severe psychoses. Whether this paradoxical bradycardia is a central or peripheral effect, or both, and the role of muscarinic subtypes are still subjects of debate. Physostigmine may also antagonize the sedative effects of the benzodiazepines, but a specific benzodiazepine antagonist, flumazenil, has supplanted physostigmine for this use. Because these compounds can increase the effect and duration of neurally released acetylcholine, they are useful in situations in which such release is deficient, such as myasthenia gravis. Anticholinesterase drugs are occasionally used to stimulate intestinal function and are applied topically in the eye as a miotic.
Metoclopramide 10 mg on line
Mangano and associates also reported that gastritis dietitian order metoclopramide 10mg without a prescription, after myocardial revascularization, patients receiving intense postoperative analgesia with sufentanil (1 g/kg/hour) experienced a lower incidence and severity of electrocardiographically documented ischemia compared with patients receiving intermittent intravenous morphine (2. However, the concomitant neural, cellular, immune, and biochemical changes have been Chapter 31: Opioid Analgesics 883 allodynia were observed for several days after cessation of morphine administration (40 mg/kg/day for 6 days). Intraoperatively, 70% N2O administration significantly reduced postoperative opioidinduced hyperalgesia in patients receiving propofol (120 g/kg/minute) and remifentanil (0. Genetic analysis in mice suggested that genetic variants of the 2-adrenergic receptor gene seem to explain some of the differences among various strains of mice in the development of opioid-induced hyperalgesia, and the selective 2-adrenergic receptor antagonist butoxamine was shown to reverse opioid-induced hyperalgesia in a dose-dependent manner. The conditions under which opioidinduced hyperalgesia is expressed should be clarified, and its clinical significance remains to be elucidated. Because underestimation and undertreatment of pain are common in opioid-dependent patients, it is important to identify the goals of short-term pain management in these patients (Box 31-3). No ideal anesthetic approach exists for a patient with a chronic addiction or a patient with an acute opiate overdose. One treatment for opioid addiction is rapid detoxification with a high dose of naloxone or naltrexone. For this treatment, general anesthesia is induced before the start of opioid antagonism and is maintained for several hours to prevent perception of withdrawal symptoms by the patient. If renal function does change during opioid anesthesia and surgery, this is probably the result of secondary changes in systemic and renal hemodynamics. The mechanism by which opioids cause urinary retention is incompletely understood. Effects of opioids on the lower urinary tract include disturbances of micturition characterized by urinary retention, especially after intrathecal opioid administration. Long-term morphine administration causes adrenal hypertrophy and impairs corticosteroid secretion. Not all opioid agonists behave similarly, and morphine appears to be particularly potent with regard to producing urodynamic problems. Malinovsky and associates compared the urodynamic effects of intravenous morphine (10 mg), buprenorphine (0. Methylnaltrexone, a quaternary naloxone derivative that does not cross the blood-brain barrier, can attenuate morphine-induced delays in gastric emptying, thus suggesting a peripheral mechanism in the opioid effect on gastrointestinal tract. Intravenous, but not intramuscular, metoclopramide (10 mg) also can reverse morphine-induced delays in gastric emptying. Transit time from mouth to ileum may not be significantly altered by morphine because morphine enhances ileal propulsion before decreasing motility. In rats, pretreatment with epidural or intraperitoneal morphine attenuated ischemia-induced inhibition of bowel motility. However, the clinical consequences of opioid-induced biliary tract actions are usually minimal. Although traditional teaching dictates that morphine induces "spasm" in the sphincter of Oddi and should not be used in patients with acute pancreatitis, no study or evidence indicates that morphine is contraindicated for use in acute pancreatitis. Oddi sphincter manometry through choledochoscopy demonstrated that the regular dose of morphine could increase common bile duct pressure, whereas pethidine had no effect, and tramadol inhibited motility of the sphincter of Oddi. Chapter 31: Opioid Analgesics 885 the duodenum and showed that remifentanil delays the drainage of dye from the gallbladder into the duodenum, but the delay is shorter than that reported after morphine or meperidine. Remifentanil pretreatment can attenuate liver injury induced by ischemia and reperfusion. This effect is mediated by inducible nitric oxide synthase expression and exhausting reactive O2 species but does not involve opioid receptors. The etiology, treatment, and prevention of postoperative nausea and vomiting have been extensively investigated. Opioids stimulate the chemoreceptor trigger zone in the area postrema of the medulla, possibly through receptors, and thereby lead to nausea and vomiting. When compared with approximately equipotent doses of fentanyl and sufentanil, alfentanil is associated with a lower incidence of postoperative nausea and vomiting. The teratogenic actions of opioids, including fentanyl, sufentanil, and alfentanil, at least in animal models, appear to be minimal. The parenteral administration of opioids before delivery remains a common method of analgesia. Nociception as a result of uterine cervical distention was able to be suppressed by - and -agonists in rats,280 but the analgesic effect of -agonist but not -agonist was reduced by estrogen. Fatal manifestations of maternal opioid administration include decreases in heart rate variability. Adverse neonatal effects can occur after administration of either morphine or meperidine to mothers. Attempts to minimize neonatal effects of opioids include restricting opioid administration to the first stage of labor. In one report, the short-acting opioid alfentanil administered before cesarean delivery attenuated the maternal stress response but led to a slightly reduced Apgar score. The chemoreceptor trigger zone and the emetic center with the agonist and antagonist sites of action of various anesthetic-related agents and stimuli. Investigators showed that the sheep fetus absorbs sufentanil after intraamniotic instillation, and significantly greater plasma concentrations were achieved in the fetal lamb than in the ewe. Newborns of addicted mothers can exhibit opioid withdrawal and require observation and appropriate treatment. In 32% of heroin addicts who died suddenly after heroin injection, the concentration of tryptase was elevated (>10 g/L), but no correlation was found between the immunoglobulin E levels and tryptase, a finding supporting the hypothesis that mast cell degranulation was not mediated by allergic reactions. Remifentanil (1 g/kg) combined with propofol (2 mg/kg) or thiopental (5 mg/kg) was reported to be effective for prevention of intraocular pressure change after succinylcholine and tracheal intubation. Topical morphine application significantly reduced the number of myofibroblasts and macrophages in the closing wound. Pharmacokinetic parameters govern the relationship between opioid dose and the opioid concentrations in blood (or other body fluid). Pharmacodynamic parameters describe the relationship between the Chapter 31: Opioid Analgesics 887 opioid concentration in blood (or other fluid) and opioid effect. When dissolved in solution, opioids are dissociated into protonated and free-base fractions, with the relative proportions depending on the pH and ion dissociation constant (pKa). High lipid solubility facilitates transport of opioid into the biophase or site of action. However, because the opioid receptor "recognizes" an opioid molecule in the protonated form, the intensity of opioid effects is closely related to the ionized concentration of drug in the biophase. All opioids are to some extent bound to plasma proteins, including albumin and 1-acid glycoprotein. Only the un-ionized, unbound fraction constitutes the diffusible fraction and provides the concentration gradient that promotes diffusion of opioid from blood to the tissue of interest. Thus, the speed of onset of opioid effect is affected by both the lipid solubility and protein binding. Morphine Morphine pharmacokinetics is notably different from that of the fentanyl congeners. Penetration of morphine into and out of the brain is presumably slower than that of other opioids. Morphine is principally metabolized by conjugation in the liver, but the kidney plays a key role in the extrahepatic metabolism of morphine. Morphine-3-glucuronide (M3G) is the major metabolite of morphine, but it does not bind to opioid receptors and possesses little or no analgesic activity. M3G may actually antagonize morphine, and this effect may contribute to both variability in response and resistance to morphine analgesic therapy. Except for renal function, M6G accumulation was shown to be affected by transmembrane transporters inhibited by probenecid. The lungs exert a significant first-pass effect and transiently take up approximately 75% of an injected dose of fentanyl. Fentanyl is relatively long acting, in large part because of this widespread distribution in body tissues.
Buy metoclopramide 10mg on-line
These ulcers usually occur in the proximal gastritis chronic nausea discount metoclopramide online visa, acid-secreting portion of the stomach. Examination of the intravital microcirculation during sepsis reveals vascular wall edema, local hemorrhages, arteriole-venule shunting, reverse flow in capillaries and venules, blood flow redistribution within microunits, leukocyte-endothelial interaction, and transmigration through the capillary walls. Some micro-areas are hyperperfused and others are hypoperfused; arteriovenous shunting of blood is increased. This often is associated with a relatively normal or even increased total blood flow, but severely decreased nutritive blood flow to the intestinal walls, particularly to the mucosa. During sepsis, metabolic demand for oxygen within the intestines is increased, and nutritive blood flow is decreased despite profound vasodilation. Sepsis is associated with severe inflammatory response leading to an increase in permeability and impaired immunologic barrier function within the intestines. Ischemia, increased permeability, and impaired intestinal barrier play an important role in subsequent amplification of distant organ dysfunction. The term oxygen delivery might not precisely reflect oxygen content in the arterial blood and flow (cardiac output). Oxygen output might be a better term, because in reality this oxygen is not delivered to cells, but bypasses them via arteriovenous shunting. Effects of Spinal and Epidural Anesthesia on Gastrointestinal Blood Flow and Volume the degree of arterial hypotension induced by spinal or epidural anesthesia is directly related to the extent of the blockade, the dose of local anesthetic used, and baseline hemodynamics. The constriction of the proximal part of the splanchnic vasculature shifts blood volume from the splanchnic system into the systemic circulation and usually results in preservation of stressed volume and blood pressure. Thoracic epidural anesthesia is associated with pronounced mesenteric vasodilation and arterial hypotension, whereas intestinal blood flow and oxygen consumption are maintained. A study using labeled red cells demonstrated that epidural anesthesia with sensory block at T4-T5 increased blood volume in both the intrathoracic and splanchnic vasculature. The authors estimated that the use of a vasoconstrictor during thoracic epidural anesthesia led to a shift of approximately 1 L of blood from the splanchnic area into the thoracic and systemic circulation. Infusion of fluid increases total (stressed and unstressed) blood volume, whereas adrenergic agonists move existing blood volume from unstressed to stressed. In many situations, the use of -adrenergic agonists might be more beneficial than infusion of fluid. Role of M cells in transepithelial transport of antigens and pathogens to the mucosal immune system, Am J Physiol 274:G785, 1998. Camilleri M: Integrated upper gastrointestinal response to food intake, Gastroenterology 131:640, 2006. Thorn K, Thorn S-E, Wattwil M: the effects of cricoid pressure, remifentanil and propofol on esophageal motility and the lower esophageal sphincter, Anesth Analg 100:1200, 2005. Chapman M, Fraser R, Vozzo R, et al: Antro-pyloro-duodenal motor responses to gastric and duodenal nutrient in critically ill patients, Gut 54:1384, 2005. Rauch S, Krueger K, Turan A, et al: Determining small intestinal transit time and pathomorphology in critically ill patients using video capsule technology, Intensive Care Med 35:1054, 2009. Van Oudenhove L, McKie S, Lassman D, et al: Fatty acid-induced gut-brain signaling attenuates neural and behavioral effects of sad emotion in humans, J Clin Invest 121:3094, 2011. Mayer E: Gut feelings: the emerging biology of gut-brain communication, Nat Rev Neurosci 12:453, 2011. Schaefer N, Tahara K, Von Websky M, et al: Role of resident macrophages in the immunologic response and smooth muscle dysfunction during acute allograft rejection after intestinal transplantation, Transpl Int 21:778, 2008. Laine L, Takeuchi K, Tarnawski A: Gastric mucosal defense and cytoprotection: bench to bedside, Gastroenterology 135:41, 2008. Gelman S: the pathophysiology of aortic cross-clamping and unclamping, Anesthesiology 82:1026, 1995. Aliverti A, Uva B, Laviola M, et al: Concomitant ventilatory and circulatory functions of the diaphragm and abdominal muscles, J Appl Physiol 109:1432, 2010. Schafer M, Sagesser H, Reichen J, et al: Alterations in hemodynamics and hepatic and splanchnic circulation during laparoscopy in rats, Surg Endosc 15:1197, 2001. Redistribution of the venous reservoir as a cause of decompensation, Circ Heart Fail 4:669, 2011. Clemente A, Carli F: the physiological effects of thoracic epidural anesthesia and analgesia on the cardiovascular, respiratory and gastrointestinal systems, Minerva Anestesiol 74:549, 2008. Stanton-Hicks M, Hock A, Stuhmeler K-D, et al: Venoconstrictor agents mobilize blood from different sources and increase intrathoracic filling during epidural anesthesia in supine humans, Anesthesiology 66:317, 1987. The portal vein delivers 75% of total hepatic blood flow; the hepatic artery provides the rest. The liver has a highly compliant, distensible vasculature that is central to its role as an important, rapidly accessible reservoir of blood volume. Without this reservoir function, mild losses of intravascular volume can result in severe hypotension. Kupffer cells reside in hepatic sinusoids; they filter the venous effluent of the gastrointestinal tract; and they avidly remove bacteria and other harmful substances, preventing their entry into the systemic circulation. Blood perfusing zone 1 is rich in O2 and nutrients; zone 3 hepatocytes are perfused with effluent blood from zones 1 and 2, which is relatively O2 poor. Hepatocytes secrete bile acids, which flow through a series of hepatobiliary ducts that drain into the duodenum via the common bile duct. Enterocytes of the terminal ileum efficiently take up bile acids and return them to hepatocytes via the portal blood. Depletion of liver glycogen during prolonged fasting, for example, promotes hepatic gluconeogenesis, enabling the liver to nourish glucose-dependent tissues. Starvation accelerates the oxidation of fatty acids and formation of ketoacids, which are released from the liver and used as energy substrates by most of the extrahepatic tissues. Such products, being more hydrophilic than their unconjugated precursors, are more readily excreted in the urine or feces. Ammonia is highly toxic to the central nervous system and can be eliminated only by the liver. Hepatocytes are uniquely equipped with the urea cycle enzymes required to metabolize ammonia to urea, which is readily excreted and much less toxic than ammonia. Albumin is the most abundant plasma protein; it is the main determinant of plasma oncotic pressure and an essential plasma transporter of exogenous substances and endogenous compounds, such as unconjugated bilirubin and free fatty acids. For diagnostic purposes, results of such tests must be interpreted in clinical context and often with supplemental radiologic and endoscopic information. Portosystemic shunting occurs, circumvents the hepatic filtering mechanism, and thereby allows drugs, nitrogenous waste, and toxins to enter the central circulation. Additional liver injury leads to life-threatening pathophysiologic derangements, including variceal hemorrhage, hepatic encephalopathy, and the hepatorenal and hepatopulmonary syndromes. The only definitive treatment for end-stage hepatic disease is liver transplantation. The liver is an essential part of the gastrointestinal tract that filters, excretes, and modifies an enormity of gut-derived substances. It is also a key component of the monocyte-macrophage system; Kupffer cells within liver sinusoids avidly remove bacteria and other harmful substances from portal blood, preventing their entry into the systemic circulation. The liver is the most vascular organ in the body; it has a unique dual blood supply and receives nearly 30% of the total cardiac output. Because of its highly compliant, distensible vasculature, the liver serves as a rapidly exchangeable blood reservoir that promotes homeostasis of the circulating blood volume. Moreover, the liver is the epicenter of intermediary metabolism and energy homeostasis; it is uniquely equipped to meet the nutritional needs of tissues throughout the body during times of both feast and famine. The liver plays an indispensable role in the excretion of endogenous wastes-most notably, ammonia and bilirubin-and eliminates a wide range of xenophobic substances, including most of the drugs and toxins that enter the body. For these reasons, a fundamental understanding of hepatic physiology is a prerequisite for health care providers. Liver disease, particularly when severe, has pervasive clinical ramifications and imposes complex therapeutic challenges. Being highly malleable, the liver allows its less pliable neighbors to determine its topography. For example, on its posterior surface, the liver shows imprints of the inferior vena cava and diaphragmatic attachments, such as the coronary and triangular ligaments and the interstitial matrix at the bare area of the liver.
Diseases
- Mitochondrial PEPCK deficiency
- Porphyria, acute intermittent
- Thumb stiff brachydactyly mental retardation
- Beriberi
- Cystin transport, protein defect of
- Sociophobia
- Myopathy, centronuclear
- Humero spinal dysostosis congenital heart disease
- Somatostatinoma
- Melanosis neurocutaneous
Buy generic metoclopramide 10 mg online
Body Weight Many opioid pharmacokinetic parameters gastritis eating before bed order metoclopramide discount, especially clearance, appear to be more closely related to lean body mass (see also Chapter 71). This means that opioid dosage regimens may best be based on lean body mass and not on total body weight. Clinically, context-sensitive half-times are not significantly different between obese and lean subjects. Mounting evidence suggests that lean body mass is a better predictor of metabolic capacity than is total body weight. For the fentanyl congeners, the clinical importance of renal failure is less marked. Morphine is an opioid with active metabolites that depend on renal clearance mechanisms for elimination. Morphine is principally metabolized by conjugation in the liver, and the water-soluble glucuronides (M3G and M6G) are excreted by the kidney. The clinical pharmacology of the fentanyl congeners is not grossly altered by renal failure, although a decrease in plasma protein binding may potentially alter the free fraction of the fentanyl class of opioids. In the presence of renal impairment, fentanyl, alfentanil, sufentanil, and remifentanil do not deliver a high active metabolite load, and their clearance is not significantly prolonged. The increase in total body water and the edema of advanced liver disease may alter the distribution characteristics of a drug. Enzyme induction, such as that observed in early alcoholism, can actually increase the metabolic capacity of the liver. Morphine pharmacokinetics is relatively unchanged by developing liver disease, such as liver cirrhosis and hepatic carcinoma, because of the substantial compensatory extrahepatic metabolism of morphine. A reduction in hepatic blood flow would be expected to slow the decline in morphine plasma concentrations. A computer simulation of the context-sensitive halftimes (50% decrement times) and 80% decrement times of remifentanil in obese versus lean subjects. In clinical terms, the curves are not grossly different in obese and lean subjects. Although the elimination of normeperidine is also decreased in these patients, the ratio of normeperidine to meperidine is generally low, and the narcotic effects of meperidine usually predominate. A significant decrease in clearance of alfentanil was demonstrated in patients with mild to moderate cirrhosis when compared with volunteers from the historical control group. The graphs show the time-dependent change of the serum concentration of morphine and its metabolites in patients with renal failure (A) and in patients with normal renal function (B) who received 0. Time-dependent changes of blood concentration of remifentanil in patients with liver disease (A) and in control subjects (B). Binding of drugs to components of the bypass circuit can also alter opioid pharmacokinetics. These effects are more intense for fentanyl than for sufentanil and for sufentanil than for alfentanil. The pH dependence of plasma protein binding of the opioids significantly correlates with their partition between an organic and aqueous phase, thus suggesting the hydrophobic character of the interaction between plasma proteins and opioids. Increased ionization decreases the amount of fentanyl available for hepatic metabolism or renal excretion. Intraoperative hyperventilation during surgical procedures can significantly influence the pharmacokinetics of sufentanil and can result in an increased distribution volume and prolonged elimination half-time. Thus, both intraoperative respiratory alkalosis and respiratory acidosis, especially in the immediate postoperative period, can prolong and exacerbate opioidinduced respiratory depression. Hemorrhagic Shock Common practice is to administer reduced doses of opioids to patients in hemorrhagic shock to minimize adverse hemodynamic consequences and to prevent a prolonged opioid effect (see also Chapter 81). This prolonged drug effect is at least partially attributable to a pharmacokinetic mechanism. Analysis of pigs receiving fentanyl suggested that central clearance and central and second compartment distribution volumes were significantly reduced in hemorrhagic shock, with higher fentanyl concentrations for any given dosage and a prolonged context-sensitive half-time. A computer simulation of the context-sensitive halftimes (50% decrement times) and 80% decrement times of fentanyl in animals in shock versus control animals. The graph indicates spectral edge measurements for control animals and for animals in hemorrhagic shock, respectively. Without considering effect-site drug concentrations over time, the choice of opioid and the amount, method, and frequency of its administration cannot be optimal. Lundy suggested that a balance of anesthetic agents and techniques be used to produce the different components of anesthesia. Anesthesia with a single agent can require doses that produce excessive hemodynamic depression. The inclusion of an opioid as a component of balanced anesthesia can reduce preoperative pain and anxiety, decrease somatic and autonomic responses to airway manipulations, improve hemodynamic stability, lower requirements for inhaled anesthetic agents, and provide immediate postoperative analgesia. Opioids interact synergistically and markedly reduce the dose of propofol and other sedative-hypnotics required for loss of consciousness and during noxious stimulation such as skin incision354. Although the intent of combining opioids with sedative-hypnotics or volatile anesthetic agents is to produce anesthetic conditions with stable hemodynamics before and after noxious stimulation, this ideal is not always achieved. Giving a large dose of any opioid shortly before the end of a surgical procedure is very likely to result in postoperative respiratory depression. Intravenous boluses of fentanyl (1 to 3 g/kg), alfentanil (10 to 20 g/kg), or sufentanil (0. Plasma concentrations of opioids necessary for various purposes are listed in Table 31-6. Changes in the excitability of central neurons play an important role in the establishment of pain. In rats, low doses of fentanyl blocked the synaptic form of central sensitization in the spinal cord in vivo, a finding suggesting the possibility of preemptive analgesia by fentanyl, but higher doses do not have this effect. A, Measured arterial propofol and fentanyl concentrations at which patients did and did not respond to a verbal command at 10 minutes after the initiation of the infusion of these drugs. The solid lines represent the modeled concentration of propofol, according to decade of age when combined with the measured fentanyl concentrations, at which 50% of patients did not respond to verbal command (Cp50s). Alfentanil and remifentanil provide the greatest ability to titrate opioids rapidly because of their extremely rapid time to onset (1 to 2 minutes) of peak effect. Sufentanil, alfentanil, and remifentanil are arguably superior to fentanyl in most respects. Antagonism of opioid action with naloxone for troublesome respiratory depression is required less frequently after alfentanil and sufentanil compared with fentanyl. Fentanyl Anesthetic induction is usually achieved by combining a loading dose of fentanyl (2 to 6 g/kg) with a sedative-hypnotic, most commonly thiopental or propofol, and a muscle relaxant. Maintenance of anesthesia can be achieved with N2O (60% to 70%) in O2, low concentrations of potent inhaled anesthetic agents, and additional fentanyl (intermittent boluses of 25 to 50 g every 15 to 30 minutes or a constant infusion of 0. The plasma concentration of fentanyl required for postoperative analgesia was approximately 1. In patients undergoing spine fusion, to keep the mean arterial pressure within 15% of the control value when fentanyl was infused to maintain the plasma concentration at 0, 1. Investigators reported that fentanyl dose based on total body weight may cause overdosing in obese patients. Repeated doses or continuous infusions of fentanyl are most likely to result in significant depression of spontaneous ventilation. In patients undergoing coronary artery bypass grafting, sufentanil doses larger than 1. This property explains how low doses (10 to 30 g/kg) of alfentanil, administered just before or simultaneously with a sedative-hypnotic, are effective. In balanced anesthetic techniques in which potent inhaled anesthetic agents are also employed, relatively low plasma alfentanil concentrations. Remifentanil Very short duration of action of remifentanil mandates that an infusion (0. Remifentanil can reliably suppress automatic, hemodynamic, and somatic responses to noxious stimulation. A randomized double-blind placebo-controlled study demonstrated that the combination of 0. In combination with propofol for induction of anesthesia in children, bolus administration of sufentanil 0. Neuroleptanalgesia is characterized by analgesia, absence of clinically apparent motor activity, suppression of autonomic reflexes, maintenance of cardiovascular stability, and amnesia in most patients. The addition of an inhaled anesthetic, usually N2O, improves amnesia and has been called neuroleptanesthesia.
Order metoclopramide in india
The risk of nephrotoxicity increases exponentially with the number of risk factors and nephrotoxic combinations gastritis questionnaire cheap metoclopramide 10mg fast delivery. Nephrotoxic acute renal failure is usually nonoliguric, with loss of concentrating ability and slowly progressive azotemia. However, the prognosis for recovery is good if these agents are discontinued in time and no coexistent organ failure exists. Their nephrotoxicity is directly related to their polycationic status, so that neomycin (six cationic sites) is more destructive than gentamicin (five sites) or streptomycin (three sites). In animal studies, administration of antioxidants such as melatonin ameliorates nephrotoxicity. Once-daily administration of aminoglycosides to achieve a high therapeutic level with an adequate trough period for renal recovery may limit the occurrence of nephrotoxicity. In platelets, the impact lasts for the lifetime of these cells (7 to 10 days), but the kidney resynthesizes cyclooxygenase within 24 to 48 hours. Short-term postoperative analgesia with a single analgesic such as ketorolac is extremely unlikely to cause injury in a relatively young, healthy, well-hydrated patient. The risk of nephrotoxic injury increases exponentially with the addition of concomitant nephrotoxins. However, the proposed decreased risk of nephrotoxic injury compared with nonselective cyclooxygenase inhibitors has not been shown. Calcineurin Antagonists (Cyclosporine A, Tacrolimus) Cyclosporine A is a remarkably potent immunosuppressive drug; together with steroids and azathioprine, it is routinely used to prevent rejection after organ transplantation. Indeed, heart, lung, and liver transplantation increased exponentially after the release of cyclosporine A in 1981. It causes renal injury in part because it induces sympathetic hyperreactivity, hypertension, and renal vasoconstriction. Preexisting renal dysfunction, hypovolemia, and other nephrotoxic insults exacerbate its nephrotoxic effects. However, renal biopsy studies in pancreas transplant patients indicate that the risk of nephrotoxicity does not differ between tacrolimus and cyclosporine A. Most transplant immunologists will avoid this drug interaction, but it may actually be beneficial. In patients undergoing cadaveric renal transplantation, the calcium channel blocker diltiazem was added to the graft preservative solution, infused into the donor for 48 hours, and then given orally. Diltiazem impairs cyclosporine metabolism so that plasma cyclosporine levels are higher, but this results in fewer episodes of early acute rejection, and calcium channel blockade protects against cyclosporine nephrotoxicity. An alternative approach that is gaining some traction is to replace cyclosporine A or tacrolimus with a noncalcineurin agent, sirolimus, which appears to have similar immunosuppressive effects with considerable less potential to induced renal injury. Subsequent studies either did not confirm these results260 or found that N-acetylcysteine provided better protection than saline alone only when a low dose of contrast dye was used. Direct cytotoxicity almost certainly plays a role as well, because contrast agents are water soluble and readily gain access to the urinary space of the glomerulus and renal tubules. The potential toxicity of radiocontrast media was thought to be directly related to their osmolality. However, metaanalysis has failed to disclose a renoprotective benefit of iso-osmolar contrast compared with a pooled group of low-osmolar contrast agents. This provides a clear warning to defer elective surgery to ameliorate the risk of perioperative acute renal failure. Intravenous mannitol has been used for many years but may exacerbate injury if it induces dehydration though excessive osmotic diuresis. Rhabdomyolysis and Myoglobinemia Muscle necrosis (rhabdomyolysis) occurs most commonly with direct trauma involving major crush or thermal injury. However, it also occurs with acute muscle ischemia induced by vascular disease or injury, or by prolonged immobilization. They are particularly likely to occur with major hemorrhage in an extremity or when vascular insufficiency coexists with tissue edema. Dramatic increases in metabolic rate (severe exercise, prolonged fever, status epilepticus, or myoclonus), severe hypophosphatemia, or direct proteolysis (acute pancreatitis) can all precipitate rhabdomyolysis. Because of the associated hypercatabolic state, oliguria is associated with acute hyperkalemia, hypocalcemia, anion-gap metabolic acidosis, and rapid azotemia. The most important aid to the diagnosis of rhabdomyolysis is a high index of suspicion. The serum is clear because of the low renal threshold for myoglobin excretion, whereas in hemoglobinemia the larger hemoglobin molecule is poorly filtered and accumulates in serum, coloring it pink. Urine flow should be kept between 100 to 150 mL/hour by osmotic diuresis with intravenous mannitol, 6. However, because there are no prospective data that confirm the beneficial effect of urinary alkalinization, urine pH should not be increased at the expense of causing significant acid-base imbalance. Jaundice and Bilrubinemia There is a direct correlation between the degree of preoperative obstructive jaundice and postoperative renal dysfunction. This situation is analogous to hepatorenal syndrome and sepsis, in which circulating endotoxins induce renal vasoconstriction and damage (vasomotor nephropathy). However, in a prospective, randomized study in patients with obstructive jaundice undergoing surgery, Plusa and Clark270 found no difference in renal outcome between these two regimens. Nevertheless, mannitol provokes a brisk osmotic diuresis, and it is important to replace urinary losses appropriately. It may induce renal damage by altered hypotension and vasomotor nephropathy and through the direct and indirect effects of endotoxin, and renal function may deteriorate progressively without defined episodes of hypotension. In addition, sepsis predisposes the kidney to further ischemic and nephrotoxic insults. The severity of renal dysfunction is directly related to the severity of sepsis and the degree of plasma renin activation. Prostaglandin F2, which mimics the action of thromboxane, is formed during leukostasis when arachidonic acid is oxidized by free oxygen radicals. Endotoxin causes leukocyte arachidonic acid to undergo lipoxygenation to form leukotrienes; it also impairs their biliary elimination. This complex is too large to be filtered by the kidney and undergoes metabolism in the liver. When free hemoglobin production is excessive, it overwhelms the haptoglobin system and accumulates in the plasma. The hemoglobin molecule is small enough to be filtered by the glomerulus and enters the tubule, where it scavenges endothelium derived nitric oxide, subsequently releasing iron and causing tubular occlusion with hemoglobin cast formation. The released free iron is nephrotoxic, through the generation of reactive oxygen species. However, renal damage is thought to be predominantly due to red blood cell stroma rather than to free hemoglobin. Chapter 23: Renal Physiology, Pathophysiology, and Pharmacology 583 increases urinary loss of tubular enzymes. It causes sequestration of leukocytes in peritubular capillaries, induces endothelial lesions by releasing neutrophil-derived elastase (enhanced by reperfusion injury), and potentiates renal ischemia such that brief hemodynamic instability causes rapid loss of renal function. The changes caused by endotoxin are mimicked by the cytokine, tumor necrosis factor-. It has been estimated that about 10% to 26% of septic patients receiving aminoglycoside antibiotics will develop nephrotoxic renal insufficiency. In the presence of these and other risk factors (see earlier), alternative nonnephrotoxic antibiotics should be considered to cover gram-negative infections, including penicillins (ticarcillin), cephalosporins (ceftazidime), carbapenems (imipenem), or monobactams (aztreonam). In cases of sepsis, low-dose dopamine is also administered in combination with more potent pressors (dobutamine, epinephrine, and norepinephrine) in the hope of enhancing hepatic, renal, and mesenteric perfusion. In patients with sepsis syndrome (signs of sepsis without hypotension), low-dose dopamine infusion doubled urine flow rate and increased creatinine clearance by 60% without any change in systemic hemodynamics. In patients with established septic shock who required catecholamines for blood pressure support, lowdose dopamine did not alter systemic hemodynamics or renal function. Most studies have examined its role in splanchnic and hepatic perfusion rather than in renal protection. Administration of the selective inhibitor either before or 30 minutes after surgery prevented deterioration in creatinine clearance, urinary sodium excretion, and urine flow rate. Beneficial effects have also been observed with aprotonin, perhaps through its antiinflammatory action. Supranormal Oxygen Delivery Over the last decade there has been considerable controversy in the concept of supranormal oxygen delivery to the tissues to overcome the defect that exists in oxygen utilization by septic tissues. The benefits of supranormal oxygen delivery on outcome have been disputed, and high-dose inotropic and vasopressor support may themselves have adverse consequences.
Order metoclopramide 10mg with amex
In contrast to the inotropic receptors that directly couple to ion-selective channels gastritis and gastroparesis diet order metoclopramide with visa, G proteins act as indirect molecular switches to relay information from activated plasma membrane receptors to appropriate intracellular targets. Chapter 25: Inhaled Anesthetics: Mechanisms of Action 629 initiated by changes in reactive oxygen species as the critical second messenger. A comparison of the effects of three mechanistically diverse anesthetics (isoflurane, propofol, and ketamine) on critical intracellular protein phosphorylation signaling pathways that are known to integrate multiple second messenger systems reveals both shared and agent-specific actions in vivo. Gene Expression the ability of general anesthetics to alter gene expression in the brain was first observed for the highly reactive immediate early genes c-fos and c-jun. Neurons show considerable diversity, and therefore anesthetic effects vary between neuronal populations with the state of the individual neuron and its network-that is, whether it is hyperpolarized or depolarized, stimulated by synaptic inputs, or quiescent. Therefore it should be recognized that results obtained even from traditional acute slice preparations only incompletely reflect anesthetic effects on neurons in vivo. The intrinsic excitability of lumbar spinal motoneurons in vivo appears to be little affected by halothane. The effects of anesthetics on tonic inhibition have been characterized in the hippocampus, which is critically involved in learning and memory. Thus these receptors provide a potential substrate for the amnesic properties of anesthetics. The relative contributions of presynaptic compared with postsynaptic anesthetic effects on synaptic transmission have been difficult to resolve, probably because the effects are transmitter and synapse specific. B, General anesthetics prolong channel opening and increase postsynaptic inhibition. Anesthetics and benzodiazepines increase the tonic conductance as indicated by the inward shift in the current. Experiments in various slice preparations indicate that reduced excitation is primarily caused by presynaptic mechanisms. The mechanisms for the presynaptic effects of inhaled anesthetics, like those for their postsynaptic effects, are complex and involve multiple targets. Although a synapse-specific contribution of presynaptic Ca2+ channels is likely, presynaptic Na+ channels are more sensitive than the Ca2+ channels coupled to glutamate release. This is consistent with observations that the predominant Ca2+ channel coupled to neurotransmitter release at hippocampal glutamatergic synapses (P/Q-type) is insensitive to isoflurane. Halogenated anesthetics enhance inhibitory and depress excitatory synaptic transmission. B, Redrawn from Perouansky M, et al: Effects of halothane on glutamate receptor-mediated excitatory postsynaptic currents: a patch-clamp study in adult mouse hippocampal slices, Anesthesiology 83:109-119, 1995. The relative importance of anesthetic effects on excitatory versus inhibitory synaptic transmission, and the mechanisms of these effects, is likely to differ for different anesthetics and for specific synapses and networks. These approaches are essential for integrating reductionist observations of the multiple molecular effects of anesthetics into functional models relevant to behavioral end points. Brain slices preserve native connections but usually lack natural inputs and outputs. These "organotypic slice cultures" preserve a high degree of synaptic connectivity and display spontaneous network activity, typically absent from "acute slices. Anesthetics affect excitation and inhibition simultaneously in opposite directions. Halothane depresses the excitatory depolarization and augments the inhibitory hyperpolarization in both hippocampal pyramidal cells and interneurons. The net result will depend on the underlying neuronal state, the neuronal network, and its function. Synaptic Plasticity Paired-pulse depression and paired-pulse facilitation are examples of short-term plasticity in response to external stimulation. Enhancement of paired-pulse facilitation has been attributed to the presynaptic depressant effect of volatile agents. Isoflurane blocks the induction of synaptic plasticity in vitro (a model of learning and memory). Spontaneously Active Circuits Spontaneous neuronal activity is decreased by volatile anesthetics both in vivo and in cortical brain slices. However, changes in raw neuronal firing rates do not provide a precise quantitative measure of higher cognitive function, which is better reflected by the relationship of firing patterns to strength and phase of cortical rhythms (see next section). Anesthetic effects have also been tested on the circuitry underlying locomotion, a well-studied central pattern generator. Lower frequency rhythms allow for integration over longer time periods and typically engage larger areas of the brain. By contrast, higher frequency rhythms allow for higher temporal resolution on local scales. Crossfrequency modulation allows for integration of both aspects of information processing. Although their physiologic roles are not clear, brain rhythms reflect, subserve, and/or constitute fundamental higher-order processing, such that their modulation by anesthetics is of great interest. The current nomenclature of brain rhythms reflects historical conventions and is not based on underlying mechanisms. Slower frequency rhythms are termed Slow-1 to Slow-4, with the higher numbers referring to slower rhythms. All oscillations are behavioral state dependent, and -Rhythms Chapter 25: Inhaled Anesthetics: Mechanisms of Action 633 anesthetic-induced amnesia. Isoflurane slows the frequency of evoked -oscillations (30 to 90 Hz, also known as "40- Hz rhythms") in humans. However, the interaction between anesthetics and behaviorally relevant network effects is likely to be complex because flash-evoked -oscillations in the primary visual cortex are not affected by inhaled agents,54 whereas feedback information transfer at -frequencies between the visual and frontal cortices is disrupted. The nature of their modulation by anesthetics as well as relevance is far from clear. Some strategies that should facilitate understanding of anesthetic mechanisms include use of agonists or antagonists in vivo, nonanesthetics or nonimmobilizers, transgenic animals, and high-resolution imaging of the functioning brain. In this approach, a receptor may be tested for its contribution to a specific end point. For example, the tuberomammillary nucleus (part of the endogenous sleep pathway) mediates the sedative component of anesthesia for some intravenous anesthetics. Computer simulations of anesthetic effects on integrated outputs can thereby be generated. These compounds have the potential to provide insights beyond the initially envisaged receptorlevel studies by allowing the separation of sedation from amnesia for the study of underlying network activity in vivo. This agent has similar (although not identical) physicochemical properties as isoflurane. When irradiated at a wavelength of 300 nm, azi-isoflurane reacts with amino acid residues surrounding putative isoflurane-binding sites. Use of azi-isoflurane and similar agents could help identify binding sites of inhaled agents on anesthesia-relevant molecular targets. Examples of this strategy are targeted mutations that alter the sensitivity of specific neurotransmitter receptors to anesthetics. Subsequently, transgenic animals rendered resistant to anesthetics, either by deletion of a putative target protein from the genome or by expressing a target receptor engineered to be insensitive to an anesthetic, were used to test behavioral relevance of the altered gene product for the production of anesthesia. Forward genetics, by contrast, is a discovery process that involves the study of randomly generated mutations (either experimentally induced or naturally occurring polymorphisms) in a population that affect the phenotype of interest. Because 1 is the most widely expressed subunit in adult animals, it is unlikely that action at glycine receptors plays an important part in the immobilizing action of inhaled agents. Interestingly, responses to pentobarbital are unaffected, indicating that the mutation does not cause a generalized resistance to anesthesia. Knockout and Knock-in Animals In the knockout approach, expression of the gene encoding a protein of interest is disrupted by a specific deletion or insertion. A well-recognized problem with the global knockout approach is that extensive compensatory changes can be induced, from anomalies that are lethal in utero to insidious (but experimentally confounding) influences that might be expressed only at maturity. A complementary strategy is the conditional knockout, in which the genetic deletion is restricted-either anatomically (limited to certain brain regions) or temporally (at a known point in time). These strategies can minimize developmental anomalies and reduce the likelihood of compensatory changes. In the knock-in approach, a mutation, usually of a single amino acid residue, is targeted to produce a protein with altered sensitivity to a drug of interest.
Purchase metoclopramide 10 mg line
Obstructive lung disease can result in diversion of inspired air into (nonobstructed) ventilated helicobacter pylori gastritis diet order cheap metoclopramide on line, but poorly perfused, regions of the lung. The components of overall impedance to breathing results from elastance (the reciprocal of compliance), resistance, and inertia. Under normal circumstances, inflation of the lung is maintained because although the pressure inside (alveolar pressure) is zero, the outside pressure. The inward force is the "elastic recoil" of the lung and emanates from the elastic lung tissue fibers, contractile airway smooth muscle, and alveolar surface tension. The outward force is developed by passive recoil from the ribs, joints, and muscles of the chest wall. First, inflating an already opened (inflated) lung is easier than when the lung is already deflated. This is because complete collapse results in liquid-only surfaces interfacing in alveoli (high surface tension), whereas alveoli in partially inflated lung have air-liquid interfaces (lower surface tension). Second, although perfusion in the lung is phasic, the frequency is rapid and the oscillations in flow are low, resulting in nearly continuous flow. Ventilation is different: the frequency is far slower and the size of the oscillations far larger. Chest wall mechanics can be measured only if complete relaxation of the respiratory muscles can be achieved26; however, during mechanical ventilation the respiratory muscles can be completely relaxed. Values of chest wall compliance are about the same as that of the lung and are reduced with obesity, chest wall edema, pleural effusions, and diseases of the costovertebral joints. The major component of resistance is the resistance exerted by the airways (large and small), and a minor component is the sliding of lung and the chest wall tissue elements during inspiration (and expiration). Resistance (R) is calculated as driving pressure (P) divided by the resultant gas flow (F): R = P/F the value of airway resistance is approximately 1 cm H2O/L/sec, and is higher in obstructive lung disease. Two factors explain why most (approximately 80%) of the impedance to gas flow occurs in the large airways. Second, in tubes that are large, irregular or branched, the flow is often turbulent, not laminar. When flow is laminar: F(lam) = P/R In contrast, when flow is turbulent: F(turb) = P/R2 Therefore, for a given radius, far more pressure is required to achieve comparable flow where flow is turbulent; thus, the effort required is greater and if prolonged or severe, respiratory failure is more likely. First, resistance lessens as lung volume increases; this is intuitive as increasing volume (positive pressure or spontaneous breathing) stretches the diameter of the airways; because this is the key determinant of resistance, the resistance falls to a small extent. In fibrosis, the slope of the curve is flatter, reflecting considerable increases in pressure variation and in respiratory work. In asthma or bronchitis, there is a parallel (upward) shift of the pressure-volume curve, indicating an increase in lung volume but no change in compliance. In emphysema, the slope of the curve is steeper, reflecting tissue loss and possible increased compliance. However, in emphysema, asthma, or bronchitis, the airway resistance is increased; this increases work of breathing and overrides any benefit from increased compliance. This results in different positions on the pressure volume curve of the upper (flatter, less compliant) versus lower (steeper, more compliant) lung regions. Schematic drawing of airflow resistance against lung volume at different flow rates. Therefore, the point along the airway tree at which pressure inside the airway has decreased to less than that outside the airway (equal to pleural pressure) is moved from smaller collapsible airways toward the mouth to noncollapsible, cartilaginous airways. With the application of some expiratory muscle effort, pleural pressure (Ppl) is positive, 4 cm H2O (0. The elastic recoil pressure (Pst) of the alveoli (6 cm H2O) and the pleural pressure add together to yield intraalveolar pressure (Palv) (10 cm H2O). At some point downstream toward the airway opening, airway pressure (Paw) has dropped by 6 cm H2O, so intraluminal pressure and pleural, extraluminal pressure are the same. From this point to the mouth, intraluminal airway pressure is lower than the surrounding, extraluminal pressure and the airway may be compressed. The increased resistance to expiratory flow requires increased expiratory effort to maintain gas flow. Thus, pleural pressure is increased in comparison to the normal conditions (Ppl = 20 cm H2O). Alveolar elastic recoil pressure (Pst) is the same as in the earlier condition, provided that lung volume is the same. If expiratory flow is of the same magnitude as during normal breathing, pressure along the airway falls to the same extent as during normal breathing. During inspiration, the intrathoracic airways are exposed to extraluminal pressure. Tissue Although not intuitively obvious, resistance of the lung tissue is the applied pressure on tissue divided by the resulting velocity of tissue movement. This component is minor, however, and can hardly be measured under normal breathing, regardless of whether the lungs are healthy. Nonetheless, tissue inertia is large during rapid ventilation,38 and it could be important during the rapid, shallow breathing characteristic of weaning failure or during high-frequency oscillation. Because the pleural pressure gradient is oriented according to gravity, the distribution of ventilation changes with body position. Indeed, experimentally induced weightlessness decreases inhomogeneity in the distribution of ventilation41, but does not eliminate it; therefore, nongravitational. Because compliance at the start of inflation is less in the (already more aerated) apex, ventilation is preferentially directed to the base. In contrast, at high airflow, resistance (not compliance) is the key determinant of distribution; because the resistance is lower in upper, more expanded lung regions, increasing flow rate equalizes the distribution of ventilation, as shown by distribution of 133Xe gas in humans47,48. This is important during exercise or stress because greater amounts of the alveolar-capillary surface area will be used. In the resting lung, the basal (dependent) regions are less aerated than the apical (nondependent) regions; therefore, they have the capacity to undergo greater expansion. During inspiration, most gas goes to the basal units (dorsal, when supine; lower right lung when in the right lateral position). Three applications of this important principle are of key relevance to anesthesia. Schematic of regional alveolar and airway volume at an upper (A) and a lower (B) lung level (left panel). The right panel shows the distribution of ventilation and perfusion ratios from the multiple inert gas elimination technique. A "normal" mode of ventilation and blood flow (A) can be seen corresponding to the open and ventilated alveoli in the upper parts of the lung. Distribution of ventilation to upper versus lower lung regions as inspiratory flow is altered. Flow is through multiple generations of bronchi, and the net resistance falls with each division. After the fourteenth generation, airways merge with alveoli and participate in gas exchange (respiratory bronchioles). Because the number of gas molecules is constant, the velocity falls rapidly, which by the time the gas enters the alveoli is miniscule (0. In the lung base, blood flow is decreased possibly because of increased interstitial pressure that compresses extra alveolar vessels. The traditional thinking about lung perfusion emphasized the importance of gravity58; however, factors other than gravity are also important. The height (base to apex) of an adult lung is approximately 25 cm; therefore, when a person is standing, the hydrostatic pressure at the base is 25 cm H2O. The mean pulmonary arterial pressure is approximately 12 mm Hg at the level of the heart, and the pulmonary artery pressure at the lung apex can therefore approach zero. Thus, less blood flow will occur at the apex (versus the base), and in the setting of positive pressure ventilation, the apical alveoli can compress the surrounding capillaries and prevent any local blood flow. In the apex (zone I), the key issue is that pulmonary arterial pressure is less than alveolar pressure; therefore, no perfusion occurs. First, the downstream blood flow in the pulmonary capillaries is pulsatile, in contrast to the more constant systemic capillary flow. Whereas an abrupt increase in the pulmonary arterial (or venous) pressure can cause breaks in the capillaries,54 slower increases. The distributions from ventral to dorsal are similar, irrespective of position, suggesting that that anatomic features (and not simply gravity) determine the distribution of flow.