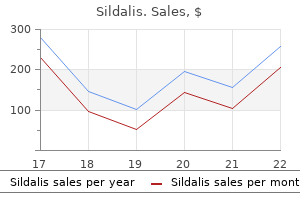
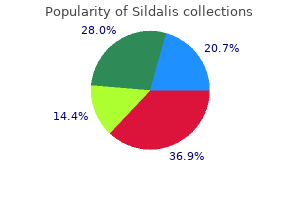
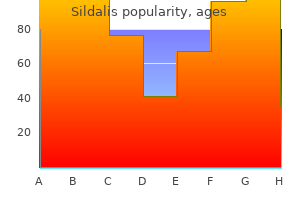
Purchase generic sildalis from india
Posterior border the posterior border is irregularly curved and descends from the posterior superior spine erectile dysfunction with diabetes purchase sildalis 120mg visa, at first forwards, with a posterior concavity forming a small notch. At the lower end of the notch is a wide, low projection: the posterior inferior iliac spine. Here the border turns almost horizontally forwards for approximately 3 cm, then down and back to join the posterior ischial border. Together these borders form a deep notch, the greater sciatic notch, which is bounded above by the ilium and below by the ilium and ischium. The upper fibres of the sacrotuberous ligament are attached to the upper part of the posterior border. The superior rim of the notch is related to the superior gluteal vessels and nerve. The lower margin of the greater sciatic notch is covered by piriformis and is related to the sciatic nerve. Medial border vascular supply the pubis is supplied by a periosteal anastomosis of branches from the obturator, inferior epigastric and medial circumflex femoral arteries. Multiple vascular foramina are present, mainly at the lateral (acetabular) end of the bone, but there is no consistently placed nutrient foramen. It is indistinct near the crest, rough in its upper part, then sharp where it bounds an articular surface for the sacrum, and finally rounded. The latter part is the arcuate line, which inferiorly reaches the posterior part of the iliopubic ramus, marking the union of the ilium and pubis. The smaller, lower part forms a little less than the upper two-fifths of the acetabulum. The upper part is much expanded, and has gluteal, 1343 chaPter ossification 80 the pubic periosteum is innervated by branches of the nerves that supply muscles attached to the bone, the hip joint and the symphysis pubis. The gluteal surface, facing inferiorly in its posterior part and laterally and slightly downwards in front, is bounded above by the iliac crest, and below by the upper acetabular border and by the anterior and posterior borders. It is rough and curved, convex in front, concave behind, and marked by three gluteal lines. The posterior gluteal line is shortest, descending from the external lip of the crest approximately 5 cm in front of its posterior limit and ending in front of the posterior inferior iliac spine. Above, it is usually distinct, but inferiorly it is poorly defined and frequently absent. The anterior gluteal line, the longest, begins near the midpoint of the superior margin of the greater sciatic notch and ascends forwards into the outer lip of the crest, a little anterior to its tubercle. The inferior gluteal line, seldom well marked, begins posterosuperior to the anterior inferior iliac spine, curving posteroinferiorly to end near the apex of the greater sciatic notch. Between the inferior gluteal line and the acetabular margin is a rough, shallow groove. Behind the acetabulum, the lower gluteal surface is continuous Pelvic girdle, gluteal region and thigh with the posterior ischial surface, the conjunction marked by a low elevation. The articular capsule is attached to an area adjoining the acetabular margin, most of which is covered by gluteus minimus. Posteroinferiorly, near the union of the ilium and ischium, the bone is related to piriformis. Gluteus medius is attached between the posterior and anterior lines, below the iliac crest, and gluteus minimus is attached between the anterior and inferior lines. The reflected head of rectus femoris attaches to a curved groove above the acetabulum. Iliacus is attached to the upper two-thirds of the iliac fossa and is related to its lower one-third. The medial part of quadratus lumborum is attached to the anterior part of the sacropelvic surface, above the iliolumbar ligament. Piriformis is sometimes partly attached lateral to the pre-auricular sulcus, and part of obturator internus is attached to the more extensive remainder of the pelvic surface. It is limited above by the iliac crest, in front by the anterior border and behind by the medial border, separating it from the sacropelvic surface. Below it is continuous with a wide shallow groove, bounded laterally by the anterior inferior iliac spine and medially by the iliopubic ramus. The converging fibres of iliacus occupy the wide groove between the anterior inferior iliac spine and the iliopubic ramus laterally and the tendon of psoas major medially; the tendon is separated from the underlying bone by a bursa. The right iliac fossa contains the caecum, and often the vermiform appendix and terminal ileum. The left iliac fossa houses the terminal part of the descending colon and the proximal sigmoid colon. The superior gluteal, obturator and superficial circumflex iliac arteries contribute to the periosteal supply. Vascular foramina on the ilium underlying the gluteal muscles may lead into large vascular canals in the bone. Sacropelvic surface innervation the sacropelvic surface, the posteroinferior part of the medial iliac surface, is bounded posteroinferiorly by the posterior border, anterosuperiorly by the medial border, posterosuperiorly by the iliac crest and anteroinferiorly by the line of fusion of the ilium and ischium. The iliac tuberosity, a large, rough area below the dorsal segment of the iliac crest, shows cranial and caudal areas separated by an oblique ridge and connected to the sacrum by the interosseous sacroiliac ligament. The sacropelvic surface gives attachment to the posterior sacroiliac ligaments and, behind the auricular surface, to the interosseous sacroiliac ligament. The auricular surface, immediately anteroinferior to the tuberosity, articulates with the lateral sacral mass. Its edges are well defined but the surface, though articular, is rough and irregular. The anterior sacroiliac ligament is attached to its sharp anterior and inferior borders. The narrow part of the pelvic surface, between the auricular surface and the upper rim of the greater sciatic notch, often shows a rough pre-auricular sulcus (that is usually better defined in females) for the lower fibres of the anterior sacroiliac ligament. For the reliability of this feature as a sex discriminant, refer to Finnegan (1978) and Brothwell and Pollard (2001). The pelvic surface is anteroinferior to the acutely curved part of the auricular surface, and contributes to the lateral wall of the lesser pelvis. Its upper part, facing down, is between the auricular surface and the upper limb of the greater sciatic notch. Its lower part faces medially and is separated from the iliac fossa by the arcuate line. Though usually obliterated, it passes from the depth of the acetabulum to approximately the middle of the inferior limb of the greater sciatic notch. The periosteum is innervated by branches of nerves that supply muscles attached to the bone, the hip joint and the sacroiliac joint. Ischium the ischium, the inferoposterior part of the hip bone, has a body and ramus. Above, it forms the posteroinferior part of the acetabulum; below, its ramus ascends anteromedially at an acute angle to meet the inferior pubic ramus, thereby completing the boundary of the obturator foramen. The ischiofemoral ligament is attached to the lateral border below the acetabulum (Fuss and Bacher 1991). The lateral border, indistinct above but well defined below, forms the lateral limit of the ischial tuberosity. At a higher level, the femoral surface is covered by piriformis, from which it is partially separated by the sciatic nerve and the nerve to quadratus femoris. The posterior surface, facing superolaterally, is continuous above with the iliac gluteal surface, and here a low convexity follows the acetabular curvature. Inferiorly, this surface forms the upper part of the ischial tuberosity, above which is a wide, shallow groove on its lateral and medial aspects. Above the ischial tuberosity, the posterior surface is crossed by the tendon of obturator internus and the gemelli. The ischial tuberosity is a large, rough area on the lower posterior surface and inferior extremity of the ischium. Though obscured by gluteus maximus in hip extension, it is palpable in hip flexion. The posterior border blends above with that of the ilium, helping to complete the inferior rim of the greater sciatic foramen, the posterior end of which has a conspicuous ischial spine. Below this, the rounded border forms the floor of the lesser sciatic foramen, between the ischial spine and tuberosity. The pelvic surface is smooth and faces the pelvic cavity; inferiorly, it forms part of the lateral wall of the ischio-anal fossa. Muscle attachments 1344 the attachment of sartorius extends down the anterior border below the anterior superior iliac spine.
Buy sildalis 120mg low cost
The maximum strength of tetanic contraction of a muscle operating at a normal muscle length averages between 3 and 4 kilograms per square centimeter of muscle impotence marijuana facts sildalis 120 mg with mastercard, or 50 pounds per square inch. Because a quadriceps muscle can have up to 16 square inches of muscle belly, as much as 800 pounds of tension may be applied to the patellar tendon. Thus, one can readily understand how it is possible for muscles to pull their tendons out of their insertions in bone. Changes in Muscle Strength at the Onset of Contraction-The Staircase Effect (Treppe). When a muscle begins to contract after a long period of rest, its initial strength of contraction may be as little as one half its strength 10 to 50 muscle twitches later. That is, the strength of contraction increases to a plateau, a phenomenon called the staircase effect, or treppe. Even when muscles are at rest, a certain amount of tautness usually remains, which is called muscle tone. Because normal skeletal muscle fibers do not contract without an action potential to stimulate the fibers, skeletal muscle tone results entirely from a low rate of nerve impulses coming from the spinal cord. These nerve impulses, in turn, are controlled partly by signals transmitted from the brain to the appropriate spinal cord anterior motoneurons and partly by signals that originate in muscle spindles located in the muscle itself. Both of these signals are discussed in relation to muscle spindle and spinal cord function in Chapter 55. Studies in athletes have shown that muscle fatigue increases in almost direct proportion to the rate of depletion of muscle glycogen. Therefore, fatigue results mainly from inability of the contractile and metabolic processes of the muscle fibers to continue supplying the same work output. However, experiments have also shown that transmission of the nerve signal through the neuromuscular junction, which is discussed in Chapter 7, can diminish at least a small amount after intense prolonged muscle activity, thus further diminishing muscle contraction. Interruption of blood flow through a contracting muscle leads to almost complete muscle fatigue within 1 or 2 minutes because of the loss of nutrient supply, especially the loss of oxygen. Muscles operate by applying tension to their points of insertion into bones, and the bones in turn form various types of lever systems. If we assume that a large biceps muscle has a cross-sectional area of 6 square inches, the maximum force of contraction would be about 300 pounds. When the forearm is at right angles with the upper arm, the tendon attachment of the biceps is about 2 inches anterior to the fulcrum at the elbow, and the total length of the forearm lever is about 14 inches. Therefore, the amount of lifting power of the biceps at the hand would be only one seventh of the 300 pounds of muscle force, or about 43 pounds. When the arm is fully extended, the attachment of the biceps is much less than 2 inches anterior to the fulcrum, and the force with which the hand can be brought forward is also much less than 43 pounds. In short, an analysis of the lever systems of the body depends on knowledge of (1) the point of muscle insertion, (2) its distance from the fulcrum of the lever, (3) the length of the lever arm, and (4) the position of the lever. Many types of movement are required in the body, some of which need great strength and others of which need large distances of movement. For this reason, there are many different types of muscle; some are long and contract a long Fulcrum Biceps muscle Lever Muscle Fatigue. The study of different types of muscles, lever systems, and their movements is called kinesiology and is an important scientific component of human physioanatomy. Virtually all body movements are caused by simultaneous contraction of agonist and antagonist muscles on opposite sides of joints. This process is called coactivation of the agonist and antagonist muscles, and it is controlled by the motor control centers of the brain and spinal cord. The position of each separate part of the body, such as an arm or a leg, is determined by the relative degrees of contraction of the agonist and antagonist sets of muscles. For instance, let us assume that an arm or a leg is to be placed in a midrange position. To achieve this position, agonist and antagonist muscles are excited to about an equal degree. Therefore, the elongated muscle on one side of a joint can contract with far greater force than the shorter muscle on the opposite side. As an arm or leg moves toward its midposition, the strength of the longer muscle decreases, whereas the strength of the shorter muscle increases until the two strengths equal each other. Thus, by varying the ratios of the degree of activation of the agonist and antagonist muscles, the nervous system directs the positioning of the arm or leg. We learn in Chapter 55 that the motor nervous system has additional important mechanisms to compensate for different muscle loads when directing this positioning process. Their diameters, lengths, strengths, and vascular supplies are altered, and even the types of muscle fibers are altered at least slightly. Indeed, experiments in animals have shown that muscle contractile proteins in some smaller, more active muscles can be replaced in as little as 2 weeks. Virtually all muscle hypertrophy results from an increase in the number of actin and myosin filaments in each muscle fiber, causing enlargement of the individual muscle fibers; this condition is called simply fiber hypertrophy. Hypertrophy occurs to a much greater extent when the muscle is loaded during the contractile process. Only a few strong contractions each day are required to cause significant hypertrophy within 6 to 10 weeks. It is known, however, that the rate of synthesis of muscle contractile proteins is far greater when hypertrophy is developing, leading also to progressively greater numbers of both actin and myosin filaments in the myofibrils, often increasing as much as 50 percent. In turn, some of the myofibrils themselves have been observed to split within hypertrophying muscle to form new myofibrils, but the importance of this process in usual muscle hypertrophy is still unknown. Along with the increasing size of myofibrils, the enzyme systems that provide energy also increase. This increase is especially true of the enzymes for glycolysis, allowing rapid supply of energy during short-term forceful muscle contraction. When a muscle remains unused for many weeks, the rate of degradation of the contractile proteins is more rapid than the rate of replacement. Proteasomes are large protein complexes that degrade damaged or unneeded proteins by proteolysis, a chemical reaction that breaks peptide bonds. Ubiquitin is a regulatory protein that basically labels which cells will be targeted for proteosomal degradation. Another type of hyper- added as rapidly as several per minute in newly developing muscle, illustrating the rapidity of this type of hypertrophy. Conversely, when a muscle continually remains shortened to less than its normal length, sarcomeres at the ends of the muscle fibers can actually disappear. It is by these processes that muscles are continually remodeled to have the appropriate length for proper muscle contraction. When it does occur, the mechanism is linear splitting of previously enlarged fibers. When a muscle loses its nerve supply, it no longer receives the contractile signals that are required to maintain normal muscle size. After about 2 months, degenerative changes also begin to appear in the muscle fibers. If the nerve supply to the muscle grows back rapidly, full return of function can occur in as little as 3 months, but from that time onward, the capability of functional return becomes less and less, with no further return of function after 1 to 2 years. In the final stage of denervation atrophy, most of the muscle fibers are destroyed and replaced by fibrous and fatty tissue. The fibers that do remain are composed of a long cell membrane with a lineup of muscle cell nuclei but with few or no contractile properties and little or no capability of regenerating myofibrils if a nerve does regrow. The fibrous tissue that replaces the muscle fibers during denervation atrophy also has a tendency to continue shortening for many months, which is called contracture. Therefore, one of the most important problems in the practice of physical therapy is to keep atrophying muscles from developing debilitating and disfiguring contractures. This goal is achieved by daily stretching of the muscles or use of appliances that keep the muscles stretched during the atrophying process. When some but not trophy occurs when muscles are stretched to greater than normal length. This stretching causes new sarcomeres to be added at the ends of the muscle fibers, where they attach to the tendons.
Purchase on line sildalis
Each lead is actually a pair of electrodes connected to the body on opposite sides of the heart erectile dysfunction causes mayo purchase sildalis pills in toronto, and the direction from negative electrode to positive electrode is called the "axis" of the lead. Because the electrodes lie exactly in the hori zontal direction, with the positive electrode to the left, the axis of lead I is 0 degrees. The right arm connects to the torso in the upper righthand corner, and the left leg connects in the lower lefthand corner. The polarities of the electrodes are shown by the plus and minus signs in the figure. In this instance, the direction of the vector is +55 degrees, and the voltage of the potential, represented by the length of vector A, is 2 millivolts. In the diagram below the heart, vector A is shown again, and a line is drawn to represent the axis of 140 lead I in the 0degree direction. To determine how much of the voltage in vector A will be recorded in lead I, a line perpendicular to the axis of lead I is drawn from the tip of vector A to the lead I axis, and a socalled projected vector (B) is drawn along the lead I axis. The instantaneous recorded voltage will be equal to the length of B divided by the length of A times 2 millivolts, or about 1 millivolt. In this example, vector A represents the electrical potential and its axis at a given instant during ventricular depolarization in a heart in which the left side of the heart depolarizes more rapidly than the right side. In this instance, the instantaneous vector has a direction of 100 degrees, and its voltage is again 2 millivolts. To determine the potential actually recorded in lead I, we draw a per pendicular line from the tip of vector A to the lead I axis and find projected vector B. Each of these vectors is then analyzed by the method described in the preceding section to deter mine the voltages that will be recorded at each instant in each of the three standard electrocardiographic leads. At this time, the vector is short because only a small portion of the ventricles-the septum-is depolarized. Conversely, when the heart vector has almost exactly the same axis as the lead axis, essentially the entire voltage of the vector will be recorded. Also, the axis of the vector is beginning to shift toward the left side of the chest because the left ventricle is slightly slower to depolarize 142 than is the right ventricle. When it occurs, it is caused by initial depolariza tion of the left side of the septum before the right side, which creates a weak vector from left to right for a frac tion of a second before the usual basetoapex vector occurs. Because the septum and endocardial areas of the ven tricular muscle depolarize first, it seems logical that these areas should repolarize first as well. However, this is not the usual case because the septum and other endocardial areas have a longer period of contraction than do most of the external surfaces of the heart. Therefore, the greatest portion of ventricular muscle mass to repolarize first is the entire outer surface of the ventricles, especially near the apex of the heart. This sequence of repolarization is postulated to be caused by the high blood pressure inside the ventricles during contraction, which greatly reduces coronary blood flow to the endocardium, thereby slowing repolarization in the endocardial areas. Because the outer apical surfaces of the ventricles repolarize before the inner surfaces, the positive end of the overall ventricular vector during repolarization is toward the apex of the heart. At each stage, the vector extends from the base of the heart toward the apex until it disappears in the last stage. At first, the vector is rela tively small because the area of repolarization is small. Finally, the vector becomes weaker again because the areas of depolarization still per sisting become so slight that the total quantity of current flow decreases. These changes also demonstrate that the vector is greatest when about half the heart is in the polar ized state and about half is depolarized. Furthermore, the vector remains generally in this direction throughout the process of normal atrial depolarization. Spread of depolarization through the atrial muscle is much slower than in the ventricles because the atria have no Purkinje system for fast conduction of the depolariza tion signal. Therefore, the musculature around the sinus node becomes depolarized a long time before the muscu lature in distal parts of the atria. Consequently, the area in the atria that also becomes repolarized first is the sinus nodal region, the area that had originally become depolarized first. Thus, when repolarization begins, the region around the sinus node becomes positive with respect to the remainder of the atria. Therefore, the atrial repolariza tion vector is backward to the vector of depolarization. Vectorcardiogram As noted previously, the vector of current flow through the heart changes rapidly as the impulse spreads through the myocardium. It changes in two aspects: First, the vector increases and decreases in length because of increasing and decreasing voltage of the vector. Second, the vector changes direction because of changes in the average direction of the electrical potential from the heart. While the heart muscle is polarized between heartbeats, the positive end of the vector remains at the zero point because there is no vecto rial electrical potential. However, as soon as current begins to flow through the ventricles at the beginning of ventricu lar depolarization, the positive end of the vector leaves the zero reference point. When the septum first becomes depolarized, the vector extends downward toward the apex of the ventricles, but it is relatively weak, thus generating the first portion of the ventricular vectorcardiogram, as shown by the positive end of vector 1. As more of the ventricular muscle becomes depolarized, the vector becomes stronger and stronger, usually swinging slightly to one side. Finally, the ventricles become totally depolarized, and the vector becomes zero once again, as shown at point 5. Vector cardiograms can be recorded on an oscilloscope by con necting body surface electrodes from the neck and lower abdomen to the vertical plates of the oscilloscope and con necting chest surface electrodes from each side of the heart to the horizontal plates. When the vector changes, the spot of light on the oscilloscope follows the course of the posi tive end of the changing vector, thus inscribing the vector cardiogram on the oscilloscopic screen. Note from this vectorcardiogram that the preponderant direction of the vectors of the ven tricles during depolarization is mainly toward the apex of the heart. That is, during most of the cycle of ventricular depolarization, the direction of the electrical potential (negative to positive) is from the base of the ventricles toward the apex. This preponderant direction of the potential during depolarization is called the mean electrical axis of the ventricles. In many pathological conditions of the heart, this direction changes markedly, sometimes even to opposite poles of the heart. The causes of the normal variations are mainly anatomical differences in the Purkinje distribution system or in the musculature itself of different hearts. However, a number of abnormal conditions of the heart can cause axis devia tion beyond the normal limits, as follows. If the net potential of lead I is positive, it is plotted in a positive direction along the line depicting lead I. If the heart is angulated to the left, the mean electrical axis of the heart also shifts to the left. Such shift occurs (1) at the end of deep expiration, (2) when a person lies down, because the abdominal contents press upward against the diaphragm, and (3) quite frequently in obese people whose diaphragms normally press upward against the heart all the time as a result of increased visceral adiposity. Likewise, angulation of the heart to the right causes the mean electrical axis of the ventricles to shift to the right. This shift occurs (1) at the end of deep inspiration, (2) when a person stands up, and (3) normally in tall, lanky people whose hearts hang downward. When one ventricle greatly hypertrophies, the axis of the heart shifts toward the hypertrophied ventricle for two reasons. First, a greater quantity of muscle exists on the hypertrophied side of the heart than on the other side, which allows generation of greater electrical potential on that side. Second, more time is required for the depolarization wave to travel through the hypertrophied ventricle than through the normal ventricle. Consequently, the normal ventricle becomes depolarized considerably in advance of the hypertrophied ventricle, and this situation causes a strong vector from the normal side of the heart toward the hypertrophied side, which remains strongly positively charged. Vectorial Analysis of Left Axis Deviation Resulting from Hypertrophy of the Left Ventricle. Vectorial analysis demonstrates left axis deviation with mean electrical axis pointing in the -15degree direction. In this instance, the axis deviation was caused by hypertension (high arterial blood pressure), which caused the left ventricle to hypertrophy so that it could pump blood against elevated systemic arterial pres sure.
| Comparative prices of Sildalis | ||
| # | Retailer | Average price |
| 1 | DineEquity | 580 |
| 2 | Safeway | 118 |
| 3 | Wegman's Food Markets | 438 |
| 4 | Aldi | 481 |
| 5 | Raley's | 172 |
| 6 | Stater Bros. Holdings | 832 |
| 7 | Dollar Tree | 878 |
| 8 | Dillard's | 250 |
Discount sildalis 120mg line
These bands are covered by erectile dysfunction treatment testosterone replacement order 120 mg sildalis free shipping, and blend with, a more superficial fibrous sheet connecting the posterosuperior margin of a rough area posterior to the sacral auricular surface to the corresponding margins of the iliac tuberosity. It consists of several weak fasciculi connecting the intermediate and lateral sacral crests to the posterior superior iliac spine and posterior end of the internal lip of the iliac crest. Inferior fibres, from the third and fourth sacral segments, ascend to the posterior superior iliac spine and posterior end of the internal lip of the iliac crest; they may form a separate long posterior sacroiliac ligament. This ligament is continuous laterally with part of the sacrotuberous ligament and medially with the posterior lamina of the thoracolumbar fascia. Its oblique fibres descend laterally, converging to form a thick, narrow band that widens again below and is attached to the medial margin of the ischial tuberosity. It then spreads along the ischial ramus as the falciform process, whose concave edge blends with the fascial sheath of the internal pudendal vessels and pudendal nerve. The lowest fibres of gluteus maximus are attached to the posterior surface of the ligament; superficial fibres of the lower part of the ligament continue into the tendon of biceps femoris. The coccygeal branches of the inferior gluteal artery, the perforating cutaneous nerve and filaments of the coccygeal plexus pierce the ligament. Ligaments the interpubic disc is strengthened anteriorly by several interlacing collagenous fibrous layers, passing obliquely from bone to bone, decussating with fibres of the external oblique aponeuroses and the medial tendons of the recti abdominis. There are less well developed posterior fibres, sometimes named the posterior pubic ligament. The superior pubic ligament connects the bones above, extending to the pubic tubercles. The arcuate pubic ligament, a thick arch of fibres, connects the lower borders of the symphysial pubic surfaces bounding the pubic arch. It blends superiorly with the interpubic disc and extends laterally attached to the inferior pubic rami. Its inferior edge is separated from the anterior border of the perineal membrane by an opening, which is traversed by the deep dorsal vein of the penis or clitoris. Vascular supply the pubic symphysis is supplied by pubic branches of the obturator, superficial external pudendal and inferior epigastric arteries. Innervation the pubic symphysis is innervated by branches from the iliohypogastric, ilioinguinal and pudendal nerves. Factors maintaining stability the interpubic disc and the superior and arcuate ligaments are the main stabilizing factors of the pubic symphysis. Movements Angulation, rotation and displacement are possible but slight, and are likely during movement at the sacroiliac and hip joints. Some separation occurs late in gestation and during childbirth; on occasion, this is considerable. Relations Anteriorly, the pubic symphysis is related to subcutaneous tissue and skin. Because of the obliquity of the joint, the proximal ends of the penile or clitoral shafts lie anterior to the lower half of the joint. Closer to the joint, the deep dorsal vein of the penis or clitoris passes between the arcuate ligament and the anterior border of the perineal membrane. Posteriorly, the upper part of the joint is separated from the inferolateral surfaces of the urinary bladder by the retropubic fat pad. Inferiorly in the male, the prostatic venous plexus separates the prostate from the lower part of the joint. These relationships explain why traumatic disruption of the anterior bony pelvis may be associated with serious urogenital injury. Fibrous adhesions and gradual obliteration occur in both sexes, earlier in males, and after menopause in females. Radiological evidence of obliteration in normal subjects is occasionally seen before 50 years but is not uncommon thereafter; in old age, the joint may be completely fibrosed and occasionally even ossified. It is partly filled by the emerging piriformis, above which the superior gluteal vessels and nerve leave the pelvis. Below it, the inferior gluteal vessels and nerve, internal pudendal vessels and pudendal nerve, sciatic and posterior femoral cutaneous nerves and the nerves to obturator internus and quadratus femoris all leave the pelvis. Section 9 1354 Articulating surfaces the surfaces are nearly flat in infants, whereas in adults they are irregular, often markedly so, and sometimes undulant. The curvatures and irregularities, greater in males, are reciprocal; they restrict movements and contribute to the considerable strength of the joint in transmitting weight from the vertebral column to the lower limbs. It transmits the tendon of obturator internus, the nerve to obturator internus, and the internal pudendal vessels and pudendal nerve. Psoas major Attachments Psoas major is a long muscle that lies on either side Vascular supply the arterial supply of the sacroiliac joint is derived from the iliolumbar, superior gluteal and superior lateral sacral arteries, with corresponding venous drainage. Innervation Nerve fibres ramify within the joint capsule and adjoining ligaments, but their source is uncertain. It is thought that the joint probably receives branches from the anterior and posterior rami of the first two sacral spinal nerves, and from the superior gluteal nerve, and that there may also be contributions from the obturator nerve and the lumbosacral trunk. The sacroiliac joint has sometimes been implicated as the source of pain in the lower back and buttocks. Diagnosing sacroiliac jointmediated pain is difficult because the presenting complaints are similar to those seen with other causes of back pain. Patients with sacroiliac joint-mediated pain rarely report pain above the level of L5; most localize their pain to the area around the posterior superior iliac spine. Factors maintaining stability the sacroiliac joint is one of the most stable joints in the body and supports the weight of the trunk. The tendency of the sacrum to be forced downwards by the trunk is resisted by the extremely strong posterior ligaments, while the iliolumbar ligaments help to resist displacement of the fifth lumbar vertebra over the sacrum. The sacrotuberous and sacrospinous ligaments oppose upward tilting of the lower part of the sacrum when downward thrust is applied at its upper end. Such movements as do occur are secondarily imposed on the joint as the pelvis moves. Data from living subjects are technically difficult to obtain, and those based on plain radiographs are unreliable. Biplanar radiography has also shown that the axes of movement of the sacroiliac joint during hip movement are oblique, and that the axes differ in flexion and extension. During pregnancy, the pelvic joints and ligaments loosen under the influence of the hormone relaxin. Relaxation renders the sacroiliac locking mechanism less effective, permitting greater rotation and perhaps allowing alterations in pelvic diameters at childbirth, although the effect is probably small. The impaired locking mechanism diverts the strain of weight-bearing to the ligaments, with frequent sacroiliac strain after pregnancy. They include the anterior surfaces and lower borders of the transverse processes of all the lumbar vertebrae. There are five digitations, each from the bodies of two adjoining vertebrae and their intervertebral disc. The highest of these arises from the lower margin of the body of the twelfth thoracic vertebra, the upper margin of the body of the first lumbar vertebra and the interposed intervertebral disc. The lowest arises from the adjacent margins of the bodies of the fourth and fifth lumbar vertebrae and the interposed disc. A series of tendinous arches extend across the narrow parts of the bodies of the lumbar vertebrae between the digitations already described. The lumbar arteries and veins, and filaments from Quadratus lumborum Psoas minor Psoas major Iliacus Anterior superior iliac spine Inguinal ligament Piriformis Coccygeus Levator ani Pubic tubercle Tensor fasciae latae Pectineus Adductor longus Gracilis Sartorius Adductor magnus Relations the sacroiliac joints have many important anterior relations. The internal and external iliac veins join to form the common iliac veins immediately anteriorly, separating the joints from the bifurcations of the common iliac arteries and, more anteriorly, the ureters. The lumbosacral trunk and the obturator nerve cross the anterior aspect of the joint behind the vessels. Piriformis partly attaches to the anterior capsule, separating the joint from the upper part of the sacral plexus. Rectus femoris Iliotibial tract Vastus lateralis Vastus medialis Variants Accessory sacroiliac articulations are not uncommon.
Purchase generic sildalis line
The abdominal compression reflex is probably much more important than has been realized in the past because it is well known that people whose skel etal muscles have been paralyzed are considerably more prone to hypotensive episodes than are people with normal skeletal muscles erectile dysfunction after age 50 buy sildalis 120 mg without prescription. Increased Cardiac Output and Arterial Pressure Caused by Skeletal Muscle Contraction During Exercise. When the skeletal muscles contract during waves result from several different effects, some of which are reflex in nature, as follows: 1. Many of the "breathing signals" that arise in the respiratory center of the medulla "spill over" into the vasomotor center with each respiratory cycle. Every time a person inspires, the pressure in the thoracic cavity becomes more negative than usual, causing the blood vessels in the chest to expand. This reduces the quantity of blood return ing to the left side of the heart and thereby momen tarily decreases the cardiac output and arterial pressure. The pressure changes caused in the thoracic vessels by respiration can excite vascular and atrial stretch receptors. Although it is difficult to analyze the exact relations of all these factors in causing the respiratory pressure waves, the net result during normal respiration is usually an increase in arterial pressure during the early part of expi ration and a decrease in pressure during the remainder of the respiratory cycle. During deep respiration, the blood pressure can rise and fall as much as 20 mm Hg with each respiratory cycle. The duration of each cycle varies from 26 seconds in the anesthetized dog to 7 to 10 seconds in the unanesthetized human. The cause of vasomotor waves is "reflex oscillation" of one or more nervous pressure control mechanisms, some of which are the following. Even anticipation of exercise tightens the muscles, thereby compressing the vessels in the muscles and in the abdomen. This compression translocates blood from the peripheral vessels into the heart and lungs and, therefore, increases cardiac output. This effect is essential in helping to cause the fivefold to sevenfold increase in cardiac output that sometimes occurs during heavy exercise. The rise in cardiac output in turn is an essential ingredient in increasing the arterial pressure during exercise, an increase usually from a normal mean of 100 mm Hg up to 130 to 160 mm Hg. That is, a high pressure excites the baro receptors, which then inhibits the sympathetic nervous system and lowers the pressure a few seconds later. The decreased pressure in turn reduces the baroreceptor stim ulation and allows the vasomotor center to become active once again, elevating the pressure to a high value. This high pressure then initiates another cycle, and the oscillation continues on and on. It probably plays the major role in causing vasomotor waves when the arterial pressure is in the range of 40 to 80 mm Hg because in this low range, chemoreceptor control of the circulation becomes powerful, whereas baroreceptor control becomes weaker. The record and there is also delay in response time of the guiding mechanism, the plane will oscillate from side to side instead of following a straight course. When the arterial pressure rose to such a high value, the brain ischemia was relieved and the sym pathetic nervous system became inactive. As a result, the arterial pressure fell rapidly back to a much lower value, causing brain ischemia once again. This response repeated itself cyclically as long as the cerebrospinal fluid pressure remained elevated. Thus, any reflex pressure control mechanism can oscil late if the intensity of "feedback" is strong enough and if there is a delay between excitation of the pressure receptor and the subsequent pressure response. The vaso motor waves illustrate that the nervous reflexes that control arterial pressure obey the same principles as those applicable to mechanical and electrical control systems. The body, however, also has powerful mechanisms for regulating arterial pressure week after week and month after month. This long-term control of arterial pressure is closely intertwined with homeostasis of body fluid volume, which is determined by the balance between the fluid intake and output. For long-term survival, fluid intake and output must be precisely balanced, a task that is performed by multiple nervous and hormonal controls and by local control systems within the kidneys that regulate their excretion of salt and water. Indeed, an increase in arterial pressure in the human of only a few mm Hg can double renal output of water, a phenomenon called pressure diuresis, as well as double the output of salt, which is called pressure natriuresis. However, through the stages of evolution, multiple refinements have been added to make this system much more precise in its control. An especially important refinement, as discussed later, has been the addition of the reninangiotensin mechanism. The rising pressure, in turn, causes the kidneys to excrete the excess volume, thus returning the pressure back toward normal. This animal has a low arterial pressure, only 8 to 14 mm Hg, and this pressure increases almost directly in proportion to its blood volume. The hagfish continually drinks sea water, which is absorbed into its blood, increasing the blood volume and blood pressure. However, when the pressure rises too high, the kidney simply excretes the excess volume into the urine and relieves the pressure. Therefore, because the hagfish continues to drink, extracellular fluid volume, blood volume, and pressure all build up again to the higher levels. The curve in this figure is called a renal urinary output curve or a renal function curve. In the human being, at an arterial pressure of 50 mm Hg, the urine output is essentially zero. At 100 mm Hg it is normal, and at 200 mm Hg it is about six to eight times normal. Furthermore, not only does increasing the arterial pressure increase urine volume output, but it also causes an approximately equal increase in sodium output, which is the phenomenon of pressure natriuresis. Then the arterial pressure was suddenly elevated by infusing about 400 ml of blood intravenously. Note the rapid increase in cardiac output to about double normal and the increase in mean arterial pressure to 205 mm Hg, 115 mm Hg above its resting level. Along with this tremendous loss of fluid in the urine, both the cardiac output and the arterial pressure returned to normal during the subsequent hour. Thus, one sees an extreme capability of the kidneys to eliminate excess fluid volume from the body in response to high arterial pressure and in so doing to return the arterial pressure back to normal. Now let us see what happens if the arterial pressure increases above or decreases below the equilibrium point. At this level, the renal output of water and salt is about three times as great as intake. Therefore, the body loses fluid, the blood volume decreases, and the arterial pressure decreases. Furthermore, this "negative balance" of fluid will not cease until the pressure falls all the way back exactly to the equilibrium level. Indeed, even when the arterial pressure is only a few mm Hg greater than the equilibrium level, there still is slightly more loss of water and salt than intake, so the pressure continues to fall that last few mm Hg until the pressure eventually returns exactly to the equilibrium point. If the arterial pressure falls below the equilibrium point, the intake of water and salt is greater than the output. Therefore, body fluid volume increases, blood volume increases, and the arterial pressure rises until once again it returns to the equilibrium point. Furthermore, there are only two ways in which the pressure of this equilibrium point can be changed from the 100 mm Hg level. One way is by shifting the pressure level of the renal output curve for salt and water, and the other is by changing the level of the water and salt intake line. Therefore, expressed simply, the two primary determinants of the long-term arterial pressure level are as follows: 1. Therefore, one can state that if the renal output curve shifts to a new pressure level, the arterial pressure will follow to this new pressure level within a few days.
Discount 120mg sildalis with mastercard
These parts are often referred to as separate muscles but the boundaries between each part cannot be easily distinguished and xarelto erectile dysfunction order genuine sildalis online, moreover, they perform many similar physiological functions. Ischiococcygeus (coccygeus) lies immediately cranial to levator ani and is contiguous with it. Pubococcygeus is often subdivided into separate parts according to the pelvic viscera to which each part relates (puboperinealis, puboprostaticus or pubovaginalis, puboanalis, puborectalis). Levator ani arises from each side of the walls of the pelvis along the condensation of the obturator fascia (the tendinous arch of levator ani). Fibres from ischiococcygeus attach to the sacrum and coccyx but the remaining parts of the muscle converge in the midline. Fibres from iliococcygeus join by a partly fibrous intersection and form the iliococcygeal raphe posterior to the anorectal junction. Closer to the anorectal junction, and elsewhere in the pelvic floor, the fibres are more nearly continuous with those of the opposite side, such that the muscle forms a sling (iliococcygeus, puborectalis). The most posterior fibres are attached to the tip of the sacrum and coccyx, but the majority join fibres from the contralateral side to form a raphe that is effectively continuous with the fibroelastic anococcygeal ligament, which is closely applied to its inferior surface; some muscle fibres may attach into the ligament. The raphe provides a strong attachment for the pelvic floor posteriorly and must be divided to allow wide excisions of the anorectal canal during abdominoperineal excisions for malignancy. An accessory slip may arise from the most posterior part and is sometimes referred to as iliosacralis. Puborectalis Puborectalis lies lateral to pubococcygeus and cannot been seen from inside the pelvis. It originates from the inner surface of the ischiopubic rami immediately adjacent to , and sometimes arising in part from, the perineal membrane. Its fibres pass lateral to those of iliococcygeus and pubococcygeus to decussate posterior to the rectum at the anorectal junction. The border between puborectalis and some fibres of the external anal sphincter is indistinct. Ischiococcygeus Ischiococcygeus may be referred to as a separate muscle, sometimes named coccygeus. It lies as the most posterosuperior portion of levator ani, and arises as a triangular musculotendinous sheet with its apex attached to the pelvic surface and tip of the ischial spine, and base attached to the lateral margins of the coccyx and the fifth sacral segment. Ischiococcygeus is rarely absent, but may be almost completely tendinous rather than muscular. It lies on the pelvic aspect of the sacrospinous ligament and may be fused with it, particularly if it is mostly tendinous. The sacrospinous ligament may represent either a degenerate part or an aponeurosis of the muscle, since muscle and ligament are coextensive. Attachments the attachments for pubococcygeus, iliococcygeus and puborectalis are as follows. Pubococcygeus Pubococcygeus originates from the posterior aspect of the body of the pubis and passes back almost horizontally. The most medial fibres run directly lateral to the urethra and its sphincter as it passes through the pelvic floor; here, the muscle is correctly called puboperinealis, although, because of its close relationship to the upper half of the urethra in both sexes, it is often referred to as pubourethralis; despite this, no direct connection with the urethra is present. In males, some of these fibres lie lateral and inferior to the prostate and are referred to as puboprostaticus (levator prostatae). In females, fibres run further back and attach to the lateral walls of the vagina, where they are referred to as pubovaginalis. In both sexes, fibres from this part of pubococcygeus attach to the perineal body; a few elements also attach to the anorectal junction. Some fibres, sometimes called puboanalis, decussate and blend with the longitudinal rectal muscle and fascial elements to contribute to the conjoint longitudinal coat of the anal canal. Behind the rectum, other fibres of pubococcygeus form a tendinous intersection as part of the levator raphe. Relations the superior, pelvic, surface of levator ani is separated only by fascia (superior pelvic diaphragmatic, visceral and extraperitoneal) from the urinary bladder, prostate or uterus and vagina, rectum and peritoneum. Its inferior, perineal, surface forms the medial wall of the ischio-anal fossa and the superior wall of the anterior recess of the fossa, both being covered by inferior pelvic diaphragmatic fascia. The medial borders of the two levator muscles and the inferior ischiopubic rami border the levator hiatus, through which pass the urethra, vagina (in the female) and anus. In the female, that portion of the hiatus that lies anterior to the perineal body is referred to as the urogenital hiatus. Vascular supply Levator ani is supplied by branches of the inferior gluteal, inferior vesical and pudendal arteries. Innervation the nerves to levator ani originate mainly from the third and fourth sacral spinal segments, with lesser contributions from the second segment. These nerves enter the pelvis just above, and sometimes pierce, ischiococcygeus to pass along the ventral surface of ischiococcygeus and pubococcygeus, supplying these muscles and sending fibres to puborectalis (Sato 1980, Roberts and Krishingner 1967). The 1222 secTion 8 True pelvis and pelvic floor pudendal nerve also may supply pubococcygeus from its lateral surface through its inferior rectal and perineal branches. It is connected to the posterior part of the arcuate line of the ilium and is continuous with iliac fascia. Anterior to this, as it follows the line of origin of obturator internus, it is gradually separated from the attachment of the iliac fascia, and a portion of the periosteum of the ilium and pubis spans between them. It arches below the obturator vessels and nerve, investing the obturator canal, and is attached anteriorly to the back of the pubis. Above the attachment of levator ani, the fascia is thin and is effectively composed only of the epimysium of the muscle and overlying connective tissue; posteriorly, it forms part of the lateral wall of the ischio-anal fossa in the perineum, and anteriorly, it merges with the fasciae of the muscles of the deep perineal space, which is continuous with the ischio-anal fossa. The obturator fascia is continuous with the pelvic periosteum and, thus, the fascia over piriformis. Actions Pubococcygeus and puborectalis pull the pelvic and perineal structures ventrally and cranially, occluding the levator hiatus. In the female, this action occludes the vaginal canal and prevents prolapse of the pelvic organs through the urogenital hiatus. The constant baseline activity of the levator muscles is similar to that of the anal sphincter, modulated to adjust to the loads placed on them. The action of puborectalis and pubococcygeus also reinforces the external anal sphincter and helps to create the anorectal angle. Iliococcygeus and, to a lesser extent, the less muscular ischiococcygeus form a relatively horizontal diaphragm, especially in the dorsal half of the pelvis, that assists puborectalis in achieving anorectal and urinary continence. Levator ani must relax appropriately to permit expulsion of urine and, particularly, faeces; it contracts with the abdominal muscles and the abdominothoracic diaphragm to raise intra-abdominal pressure. It forms much of the muscular pelvic diaphragm, which supports the pelvic viscera. Like the abdominothoracic diaphragm, but unlike the abdominal muscles, levator ani is also active in the inspiratory phase of quiet respiration. In the pregnant female, the shape of the pelvic floor may help to direct the fetal head into the anteroposterior diameter of the pelvic outlet. The fascia over the inner aspect of piriformis is very thin, and fuses with the periosteum on the front of the sacrum at the margins of the anterior sacral foramina. It ensheathes the anterior primary rami of the sacral nerves that emerge from these foramina; the nerves are often described as lying behind the fascia. The internal iliac vessels lie in front of the fascia over piriformis; their branches draw out sheaths of the fascia and extraperitoneal tissue into the gluteal region, above and below piriformis. In humans, ventral to the lateral attachment of the pelvic organs, a portion of it is derived from the degener- Both surfaces of levator ani have a fascial covering; the combination of the two fascial layers and the intervening muscle is called the pelvic diaphragm. On the inferior surface, the thin fascia is continuous with the obturator fascia below the tendinous arch of levator ani laterally. It covers the medial wall of the ischio-anal fossa and blends below with fasciae on the urethral sphincter and the external anal sphincter. The superior fascia of the pelvic diaphragm is markedly thicker than the inferior fascia and is attached anteriorly to the posterior aspect of the body of the pubis, approximately 2 cm above its lower border. It is continuous posteriorly with the fascia over piriformis and the anterior sacrococcygeal ligament. Medially, the superior fascia of the pelvic diaphragm blends with the visceral pelvic fascia to contribute to the endopelvic fascia. This band extends on the inner surface of levator ani and joins the tendinous arch of levator ani to the ischium, just above the spine. The attachment of the paravaginal tissue to the pubic bones is sometimes called the pubourethral ligament, which is a misnomer since it is not attached to the urethra. The attachment of the anterior vaginal wall to the tendinous arch of the pelvic fascia, the paravaginal attachment, helps to provide support to the vagina, urethra and bladder.
Purchase line sildalis
The lumbar part of the lumbosacral trunk contains part of the fourth and all of the fifth lumbar ventral rami; it appears at the medial margin Common iliac nodes Posterior trunk nodes Branches of the sacral plexus the branches of the sacral plexus are shown in Table 73 impotence from priapism surgery best sildalis 120mg. The course and distribution of most of the branches of the sacral plexus are covered fully in Section 9. L4 root L5 root Lumbosacral trunk S2 root Superior gluteal nerve S3 root S4 root Inferior gluteal nerve Sciatic nerve Obturator nerve Nerve to piriformis Perforating cutaneous nerve Coccygeal nerve(s) Nerve(s) to levator ani and coccygeus Pudendal nerves Posterior femoral cutaneous nerve Nerve to obturator internus and superior gemellus Nerve to quadratus femoris and inferior gemellus 1229 cHapTer 73 S1 root True pelvis, pelvic floor and perineum Pudendal nerve (in the pelvis) the pudendal nerve arises from the ventral divisions of the second, third and fourth sacral ventral rami and is formed just above the superior border of the sacrotuberous ligament and the upper fibres of ischiococcygeus (Klink 1953, Sato 1980). In the posterior part of the canal, it gives rise to the inferior rectal and perineal nerves; the dorsal nerve of the penis or clitoris continues ventrally from this origin. Anococcygeal nerves arise from it and form a few fine filaments that pierce the sacrotuberous ligament to supply the adjacent skin. It lies medial or anterior to the anterior sacral foramina and has four or five interconnected ganglia. The right and left trunks converge below the lowest ganglia and unite in the small ganglion impar anterior to the coccyx. Grey rami communicantes pass from the ganglia to sacral and coccygeal spinal nerves but there are no white rami communicantes. Sacral muscular branches Several muscular branches arise from the fourth sacral ventral ramus to supply the superior surface of levator ani and the upper part of the external anal sphincter. The branches to levator ani enter the superior (pelvic) surface of the muscle whilst the branch to the external anal sphincter (also referred to as the perineal branch of the fourth sacral nerve) reaches the ischio-anal fossa by running either through ischiococcygeus, or between ischiococcygeus and iliococcygeus. Vascular branches Coccygeal plexus the coccygeal plexus is formed by a small descending branch from the fourth sacral ramus and by the fifth sacral and coccygeal ventral rami. The fifth sacral ventral ramus emerges from the sacral hiatus, curves round the lateral margin of the sacrum below its cornu, and pierces ischiococcygeus from below to reach its upper, pelvic, surface. Here it is joined by a descending branch of the fourth sacral ventral ramus; the small trunk so formed descends on the pelvic surface of ischiococcy- Preganglionic fibres for the vessels supplying the pelvis and lower limb are derived from the lower three thoracic and upper two or three lumbar spinal segments. They reach the lower thoracic and upper lumbar ganglia through white rami communicantes and descend through the sympathetic trunk to synapse in the lumbar ganglia. Postganglionic fibres pass from these ganglia via grey rami communicantes to the femoral nerve, which carries them to the femoral artery and its branches. Some fibres descend through the lumbar ganglia to synapse in the upper two or three sacral ganglia, from which postganglionic axons pass through grey rami communicantes to the roots of the sacral plexus. Those in the pudendal and superior and inferior gluteal nerves accompany the arteries of the same name to the gluteal and perineal tissues; branches may also supply the pelvic lymph nodes. Those joining the tibial nerve are carried to the popliteal artery and distributed via its branches to the leg and foot. It is usually described as if from the position of an individual lying supine with the hip joints in abduction and partial flexion. The surface projection of the perineum and the form of the skin covering it vary considerably, depending on the position of the thighs, whereas the deep tissues themselves occupy relatively fixed positions. The perineum is bounded anteriorly by the pubic symphysis and its arcuate ligament, posteriorly by the coccyx, anterolaterally by the ischiopubic rami and the ischial tuberosities, and posterolaterally by the sacrotuberous ligaments. The deep limit of the perineum is the inferior surface of the pelvic diaphragm, and its superficial limit is the skin that is continuous with that over the medial aspect of the thighs and the lower abdominal wall. An arbitrary line joining the ischial tuberosities (the inter-ischial line) divides the perineum into an anterior urogenital triangle and a posterior anal triangle. Ischio-anal fossa Anal triangle the structure of the anal triangle is similar in males and females, the main difference reflecting the wider transverse dimension of the triangle in females that is associated with giving birth. The anal triangle contains the anal canal and its sphincters, and the ischio-anal fossa and its contained nerves and vessels. The ischio-anal fossa is an approximately horseshoe-shaped region filling the majority of the anal triangle. Above them, the medial limit of the fossa is formed by the deep fascia over levator ani. The outer boundary of the fossa is formed anterolaterally by the fascia over obturator internus and the periosteum of the ischial tuberosities. Posterolaterally, the outer boundary is formed by the lower border of gluteus maximus and the sacrotuberous ligament. There is an anterior recess to the ischio-anal fossa that lies cranial to the perineal membrane and transverse perineal muscles. It extends anteriorly as far as the posterior surface of the pubis, below the attachment of levator ani. Posteriorly, the fossa contains the attachment of the external anal sphincter to the tip of the coccyx; above and below this, the adipose tissue of the fossa is uninterrupted across the midline. These continuations of the ischio-anal fossa mean that infections, tumours and fluid collections within not only may enlarge relatively freely to the side of the anal canal, but also may spread with little resistance to the contralateral side and deep to the perineal membrane. The internal pudendal vessels and accompanying nerves lie in the lateral wall of the ischio-anal fossa, enclosed in fascia forming the pudendal canal. The inferior rectal vessels and nerves cross the fossa from the pudendal canal and often branch within it. The ischio-anal fossa is an important surgical plane during resections of the anal canal and anorectal junction for malignancy. It provides an easy, relatively bloodless, plane of dissection that encompasses all of the muscular structures of the anal canal and leads to the inferior surface of levator ani, through which the dissection is carried. External anal sphincter superficial fascia of the anal triangle the superficial fascia (subcutaneous tissue; tela subcutanea) of the region is thin and is continuous with the superficial/subcutaneous fascia of the skin of the perineum, thighs and buttocks. The external anal sphincter is a band of striated muscle that surrounds the lowest part of the anal canal (Oh and Kark 1972, Dalley 1987, Lawson 1974b). The uppermost (deepest) fibres blend with the lowest fibres of puborectalis; the two are seen to be contiguous on endoanal ultrasound and magnetic resonance imaging. Anteriorly, some of these upper fibres decussate into the superficial transverse perineal muscles. On the left side, the skin and superficial fascia of the perineum only have Dorsal artery of the penis been removed. The posterior scrotal (perineal) artery has been Deep artery of the penis shown as it runs forwards into the scrotal tissues. On the right side, the corpora cavernosa and Artery of the bulb corpus spongiosum and their associated muscles, the Deep transverse superficial perineal muscles and perineal muscle perineal membrane have been Puborectalis removed to reveal the underlying Internal pudendal artery deep muscles and arteries of the Levator ani (iliococcygeal) perineum. Some fibres from each side of the sphincter decussate in these areas to form a sort of commissure in the anterior and posterior midline. The anterior and posterior attachments of the external anal sphincter give the muscular tube an oval profile lying anteroposteriorly. A subcutaneous portion encircles the anal verge and creates the radial skin creases surrounding the anus. The lower fibres lie below the level of the internal anal sphincter and are separated from the lowest anal epithelium by submucosa. Recent detailed histological examination of serial cross-sections supports the concept of the perineal membrane as part of a larger interconnected support apparatus. It has distinct dorsal and ventral portions that are intimately connected with levator ani: the dorsal portion is related to the support of the perineal body and lateral vaginal wall by its attachment to the ischiopubic ramus, and the ventral portion is contiguous with the urethral supportive apparatus (Stein and DeLancey 2008). The perineal membrane is particularly thick where it is attached to the arcuate ligament of the pubis, and is here referred to as the transverse perineal ligament. The posterior border of the perineal membrane is continuous with the deep part of the perineal body at its dorsal margin, and is continuous with the fascia over the superficial transverse perineal muscles. In the female, the perineal membrane is divided almost into two halves by the vagina and urethra, such that it forms a triangle on each side of these structures. The lateral margins of the vagina are attached to the perineal membrane at the level of the hymenal ring, and levator ani lies on its cranial surface. The iliococcygeal raphe (the decussation of the posterior fibres of iliococcygeus) lies just above the anococcygeal ligament and is separated from the rectum by presacral fascia. Division of the anococcygeal raphe may cause descent of the anal canal and a lowering of the posterior part of the anal triangle, but does not demonstrably interfere with the process of defecation. Urogenital triangle the urogenital triangle is bounded posteriorly by the inter-ischial line, which usually overlies the posterior border of the transverse perineal muscles.
Buy sildalis 120 mg line
The degree to which the ligament of the head of the femur offers functional stability to the adult hip is uncertain erectile dysfunction remedies fruits buy sildalis 120 mg overnight delivery, although it is likely to be secondary to that provided by the capsular ligaments and muscle activation. Free nerve endings have been identified within this ligament, suggesting that this structure may be a source of pain when it is injured or degenerating (Leunig et al 2000). The afferent innervation in the healthy state may serve as a source of proprioception or protection of the joint (Bardakos and Villar 2009). The thick capsule is reinforced by the three major ligaments: iliofemoral, pubofemoral and ischiofemoral. The iliofemoral ligament is the strongest, and is progressively tightened when the femur extends to the line of the trunk. The pubofemoral and ischiofemoral ligaments also tighten when this happens and, as the joint approaches the close-packed position, resistance to an extending torque increases rapidly. The transverse acetabular ligament and ligament of the head of the femur also contribute to stability. Only slight separation of the articular surfaces can be achieved by strong traction on the joint. To aid insertion of an arthroscope, a needle is first inserted into the joint to eliminate the suction effect; the joint will subsequently open sufficiently with traction. Traumatic dislocation usually occurs only when the joint is subjected to extreme force. Synovial membrane Starting from the femoral articular margin, the synovial membrane covers the intracapsular part of the femoral neck, and then passes to the internal surface of the capsule to cover the acetabular labrum, the ligament of the head of femur and fat in the acetabular fossa. It is thin on the deep surface of the iliofemoral ligament where it is compressed against the femoral head, and sometimes is even absent here. The biomechanical features of the human lower limb, whose function is primarily to allow stance and bipedal propulsion, are very different from those of the quadruped lower limb, and these differences are reflected in the anatomy and biomechanics of the human hip, knee, ankle and foot joints. This articulation is innately limited in its capacity for translational motion in anteroposterior, transverse and vertical directions. Bursae the hip joint may communicate with the subtendinous iliopectineal bursa through a circular aperture between the pubofemoral ligament and the descending part of the iliofemoral ligament. More distant bursae are associated with the tendons of distal attachment of glutei medius and minimus at the greater trochanter, and between gluteus maximus and vastus lateralis. Femur the femur is essentially a tubular structure with distortions that consist of bows and twists. The most notable is the anterior bow in its mid portion, where the radius of curvature is relatively constant along the length of the femoral shaft. Lymphatics from the anterior aspect of the hip joint drain to the deep inguinal nodes, while those from the medial and posterior aspects of the joint travel with the obturator and gluteal arteries, respectively, to reach the internal iliac nodes. The posterior capsule is innervated by the sciatic and superior gluteal nerves, and by the nerve to quadratus femoris (Birnbaum et al 1997, Gardner 1948). Head N Neck B Greater trochanter Hip and groin pain Pain emanating from the hip and groin has many possible causes. Pain over the lateral aspect of the hip usually suggests a local problem such as trochanteric bursitis. Pain in the buttock is only occasionally derived from the hip joint; most frequently, it is referred from the lumbosacral spine or may be caused by vascular claudication. Attritional chronic overload of the anterior abdominal wall at its attachments to the pubis and inguinal ligament, or of external oblique at the superficial inguinal ring, is a common occurrence. In addition, in most hips, a line nearly perpendicular to S from the tip of the greater trochanter (B) passes through the centre of the femoral head. This approximation can be utilized in judging the position of the femoral osteotomy in hip arthroplasty. Since the growth plate is avascular, the only blood supply to the femoral head is conveyed through the retinacular vessels, which are mainly tributaries of the medial circumflex femoral artery. These retinacular arteries enter the joint capsule in the trochanteric fossa and ascend the femoral neck on its outer aspect superiorly and posteriorly. A minor contribution to the vascular supply comes from the ligament of the head of the femur. The yellow arrow shows posterior displacement of the femoral head in the slipped capital femoral epiphysis. The red arrow indicates the course of the retinacular vessels along the posterior aspect of the femoral neck. The body therefore tends to incline posteriorly but this is counterbalanced by ligamentous tension and congruence and compression of the articular surfaces within the hip joints in the close-packed position. Under increased loading of the trunk or leaning posteriorly, these resistive but passive factors are assisted by active force produced by the hip joint flexors. The posture adopted, or the rate of change of posture, is largely controlled by the hamstrings, which, besides being powerful flexors of the knee, are strong extensors of the hip. Gluteus maximus becomes particularly active when the thigh is extended against resistance, as in rising from a bending position or during climbing. Abduction is produced by glutei medius and minimus, assisted by tensor fasciae latae, piriformis and sartorius. The motion is limited by adductor muscle tension, the pubofemoral ligament and the extreme medial bands of the descending part of the iliofemoral ligament. The abductor muscles, most notably glutei medius and minimus, are active periodically at precise phases of the walking or running cycle to ensure coronal plane stability of the pelvis. Adduction is produced by adductors longus, brevis and magnus and by gracilis assisted by pectineus, quadratus femoris and the inferior fibres of gluteus maximus. The range of adduction is limited by the increasing tension in the abductor muscles, the transverse part of the iliofemoral ligament and the fascia lata of the thigh. Medial rotation is produced by the anterior fibres of glutei minimus and medius, and assisted by tensor fasciae latae and most adductor muscles. The strength of medial rotation naturally increases as the hip is flexed because this position increases the moment arm of most medial rotator muscles (Delp et al 1999). Medial rotation is limited by tension in lateral rotator muscles such as piriformis, the ischiofemoral ligament and the adjacent posterior joint capsule (Wagner et al 2012). Lateral rotation is produced by gluteus maximus, obturator internus, superior and inferior gemelli, quadratus femoris and piriformis, and it is assisted by obturator externus and sartorius. Lateral rotation, a stronger motion than medial rotation, is limited by tension in the medial rotator muscles and the transverse part of the iliofemoral ligament (Myers et al 2011). The degree of anteversion affects many aspects of lower limb biomechanics, including the moment (lever) arms of the hip abductor and medial rotator muscles (the perpendicular distance from the centre of rotation of the femur to the line of action of the resultant muscle force); patellar tracking (the motion of the patella relative to the femur); and foot orientation. Forces acting on the hip In quiet upright standing, the femoral heads support the weight of the trunk, upper limbs and head. About two-thirds of body weight is located above the hips, and so each femoral head normally accepts about one-third of body weight. This force is compressive in nature, as gravity pulls the acetabula against the femoral heads. When viewed in the sagittal plane, minimal muscle forces suffice to maintain equilibrium as long as the weight of the upper body is directed over the femoral heads. If the upper body leans anteriorly, shifting the upper body weight vector anteriorly beyond the femoral heads and thereby producing a hip flexion moment, posterior thigh muscles can counter such rotation. As the capsular ligaments of the hip slacken in flexion, none of them is able to resist the forward lean. During walking, hip joint compression force varies from one-third of body weight, when both feet are on the ground, to some four times body weight when the other foot is lifted. The large compression forces generated while walking originate primarily from two sources: gravity and muscle activation. During the stance phase, gravity pulls the upper body and acetabulum inferiorly on the femoral heads (as described above for quiet standing). More significantly, each femoral head is pushed superiorly against its socket as the foot strikes and then pushes against the ground.