Purchase tranexamic 500 mg fast delivery
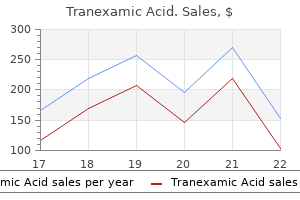
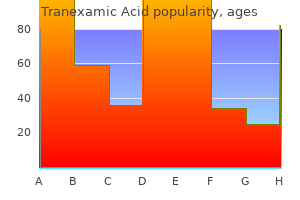
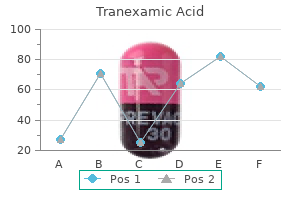
These viruses are genetically identical to the H1N1 viruses that were circulating in 1950 medicine keeper purchase tranexamic without a prescription. In 2009, a new variant of H1N1 viruses, referred to as pH1N1, emerged from pigs and replaced the previous H1N1 viruses. The origin of new pandemic strains has been the subject of intense interest and study, for obvious reasons. The most plausible explanation for their origin takes into account three features of this phenomenon: that the virus has a segmented genome, that pandemics occur only with influenza A viruses, and that influenza A viruses, but not other influenza viruses, maintain a large reservoir of genetic diversity, primarily in birds. Chapter 165 Influenza Viruses, Including Avian Influenza and Swine Influenza Antigenic Drift Incidence of clinically manifest influenza Mean level of population antibody vs. A/ HxNx and A/HyNy represent influenza viruses with completely different hemagglutinins and neuraminidases. Because the nature of influenza epidemics prior to 1918 is known only by serologic means, those boxes are shaded tan. Below the time line are the ages of individuals in 2004 who were alive during the various epidemic periods of earlier influenza subtypes. For example, individuals currently living who are between the ages of 47 and 86 probably experienced their first influenza A infection as an H1N1 virus. Individuals who are 36 years of age or younger have never been infected with H2N2 viruses. In these birds influenza A causes mild illness or may be shed asymptomatically at high levels and for long duration in the feces. These birds may transmit influenza to other animals, including domestic poultry, horses, swine, and marine mammals, which may in turn transmit these viruses to humans. Comparisons of sequence data from animal and human influenza viruses isolates has suggested that the 1918 virus was introduced into humans from such an animal population. Most of these transmission events have been quite limited, with small numbers of persons affected, relatively mild disease, and little or no evidence of person-to-person transmission. In most cases, virus has been transmitted to humans from infected domestic poultry, but cases have also occurred in association with marine mammals and possibly wild birds. These infections have involved primarily viruses of the H7, H5, H9, and H10 subtypes, with H7 and H5 viruses being most common. H5N1 viruses were first recognized in humans in 199782 and have continued to cause substantial numbers of human cases since that time. Patients have ranged in age from 3 months to 75 years, with the median age being 20 years. Half of all cases have been in people younger than 20 years, and 90% of cases have been in people younger than 40 years. The case-fatality rates have been the highest for those in the 10- to 19-year-old age group, lowest for people 50 or older, and in between for children aged <10 years. Activities such as plucking and preparing diseased birds; playing with birds, especially asymptomatically infected ducks; and handling fighting cocks are risk factors for infection. Descriptions of the signs and symptoms of H5N1 infection are mostly from hospitalized patients. Most patients have presented with nonspecific complaints of a fever, cough, and shortness of breath. In many of the patients, there is a progression of symptoms leading to respiratory failure necessitating ventilation and other supportive measures. Atypical symptoms such as nausea, vomiting, encephalopathy, and bleeding gums and nose have been reported. The majority of patients have an abnormal chest radiograph with diffuse and multifocal or patchy infiltration, but pleural effusions are rare. Laboratory abnormalities include significant lymphopenia and leucopenia, mild-to-moderate thrombocytopenia, and elevated transaminases. Pathologic changes include diffuse alveolar damage in the lungs, reactive hemophagocytosis in the marrow, and lymphoid depletion with atypical lymphocytosis in the spleen and lymphoid tissues. Highly pathogenic avian H5N1 viruses have undergone significant genetic diversification and dissemination throughout Asia, the Middle East, and Europe since their initial detection, especially after a large outbreak in birds at Qinghai lake in Western China in 2005. Current human infections have been mainly due to clade 2 viruses, including subclades 2. Sporadic human infections with H7 viruses have been detected for many years, and early infections were typically relatively mild and limited. These outbreaks occurred annually between 2013 and 2017, during the winter with noted cocirculation of seasonal human H3N2 viruses. Coinfection with both H3N2 and H7N9 viruses has been reported,102 but does not appear to have spread reassorted viruses. In contrast to previous outbreaks of avian influenza in humans, the mean age of the affected patients (61 years) was substantially higher, and 42% of those affected were 65 or older. Older age and the presence of chronic medical conditions have been demonstrated to be risk factors for severe illness, somewhat similar to the findings in seasonal influenza. Exposure to infected birds in live bird markets has been identified as a major risk factor for infection. It has been speculated that the older age distribution of human cases may reflect social differences by age in patronizing these markets. Individuals born after 1968, whose primary influenza exposure was due to H3N2 viruses, might be relatively resistant to H7 viruses compared with older individuals whose primary exposure was to an H1N1 virus. Influenza H9N2 virus was isolated from two children in Hong Kong with mild febrile pharyngitis in 1999. Although these isolated incidents have been uncommon, H9 viruses remain a high priority for human surveillance because other threatening avian viruses such as H5 and H7 are often reassortants with H9 viruses. Fortunately, avian influenza A viruses appear to be relatively restricted in their ability to replicate in humans. Extensive sequence analysis has suggested at least two mechanisms by which avian viruses can circumvent these barriers to interspecies transmission. Reassortment would be facilitated by the presence of a third species that is susceptible to infection with both avian and human viruses, such as the pig, which contains both types of receptors. A second mechanism would involve adaptation of avian viruses to the human host by evolution in swine, and this is supported by sequence analysis showing that the 1918 pandemic was most likely the result of direct introduction of an avian or swine influenza A virus into humans. A series of studies have been reported in which various manipulations were attempted to determine whether H5N1 viruses were capable of adapting to ferrets and eventually acquiring the ability to transmit from ferret to ferret. Sequence analysis has suggested that some of these changes may already be present in naturally occurring H5 viruses,120 and it will be important to continue monitoring isolates for sequences suggestive of successful human adaptation. Chapter 165 Influenza Viruses, Including Avian Influenza and Swine Influenza Human Infections With H9 Viruses Factors Controlling Host Range Domestic swine have also been recognized as a potential source of pandemic influenza viruses in man. Genomic data have suggested that influenza A (H1N1) viruses were introduced into swine populations at around the same time that H1N1 viruses emerged in man in 1918. During this time, swine were also occasionally infected with influenza A viruses from humans and from birds, and have always been considered to represent a potential "mixing vessel" in which reassortment between human and avian influenza viruses could occur. This concept was strengthened by the recognition that the swine respiratory tract contains abundant receptors of both the 2-3 and 2-6 types favored by avian and human viruses, respectively. This virus went on to cause a pandemic of influenza with a major impact in children and adolescents, and replaced previous H1N1 viruses as the new seasonal H1N1. Subsequent studies in guinea pigs have identified the Eurasian swine M gene segment as playing a critical role in transmission phenotype of this virus. Influenza viruses that circulate in swine are referred to as "variant" viruses when isolated in humans, designated H3N2v virus. During the period from July to September 2012, a total of 306 cases of human infection with H3N2v influenza viruses were reported. Almost all cases have documented histories of swine exposure, and the majority of cases were associated with attendance at state fairs. The H3N2v viruses isolated from humans are phylogenetically most closely related to human influenza viruses from the mid 1990s, particularly the A/Wuhan/95 and A/Sydney/99 viruses.
Syndromes
- Excessive weight loss
- Betaxolol (Kerlone)
- Heart valve disease (most often the mitral valve)
- If both sides of the brain are being treated, the surgeon will make an opening on both sides of the skull, and two leads will be inserted.
- Male: 97 to 137 ml/min.
- Feeling detached
Discount tranexamic 500mg overnight delivery
In adults 5 medications post mi purchase tranexamic online from canada, chlamydial eye infection manifests as an acute follicular conjunctivitis, often with a foreign body sensation in the eye. The clinical picture in the first 2 weeks is dominated by hyperemia and a mucoid discharge that becomes purulent. A common scenario for chlamydial ocular infection is conjunctivitis for weeks to months that has not responded to topical antibiotics. The differential diagnosis is primarily conjunctivitis caused by adenovirus or other viruses. Eye-to-eye spread between individuals by transfer of infected secretions without sexual contact may also occur. The condition responds promptly to the administration of appropriate systemic antibiotics such as azithromycin or doxycycline with decreased discharge, hyperemia, and keratitis symptoms within 48 hours. The transmission probability from a single act of unprotected coitus has been estimated to be 0. Recent exposure to a new partner was much more strongly associated with gonorrhea than with chlamydial infection. Both infections present with dysuria, but the urethral discharge with chlamydial urethritis is usually white, gray, or sometimes clear, in contrast to the more purulent discharge observed with gonococcal urethritis. Some patients may deny the presence of discharge but may note stained underwear in the morning. The preferred rapid diagnostic test for urethritis is a Gram stain of the urethral discharge. The absence of urethritis does not exclude chlamydial infection or gonorrhea as the cause of epididymitis. Chlamydial epididymitis is often associated with oligospermia during the acute phase,281 but there are no data indicating that future fertility is impaired. In addition, epididymitis is usually unilateral, and attempts to correlate chlamydial infections with male factor infertility have been unsuccessful. Typically, acute epididymitis presents with unilateral testicular pain and tenderness, hydrocele, and palpable swelling of the epididymis. Many patients can be managed in the outpatient setting, but others require hospitalization for parenteral antibiotics, scrotal elevation, analgesia, and observation. An alternative diagnosis of testicular torsion should always be considered in a young man with acute onset of severe unilateral scrotal pain and should be ruled out with ultrasound. From available data, this bacterium does not appear to play a role in acute prostatitis, which is mainly caused by E. Young age is the single factor most strongly associated with increased risk of chlamydial infection among sexually active females. For example, chlamydial prevalence in sexually active individuals is nearly three times greater among 14- to 24-year-olds compared with 25- to 39-year-olds. Alternatively, oral contraceptive use may be a surrogate marker for increased sexual activity. For example, 68 of 85 (80%) infected but asymptomatic adolescent women were still infected when retested 2 months or more after their initial evaluation. In two large studies, the prevalence of anorectal chlamydial infection among women giving a history of anorectal intercourse was 14. A substantial proportion of chlamydial infections were detected only at the rectal site (44. More research is needed to confirm the frequency and mechanism of rectal carriage in women, to determine whether routine screening at the anorectal site is warranted to increase case finding, and to evaluate the response of anorectal infection to the currently recommended treatment regimens. However, vaginitis can be present in girls because the vagina is lined with transitional cell epithelium before puberty. On examination, the cervix may appear normal or may exhibit edema, erythema, and hypertrophy. Acute urethral syndrome is defined as dysuria and urinary frequency with fewer than 105 organisms per milliliter of urine. Most of the remainder of the women with pyuria and acute urethral syndrome had low urine concentrations of E. Chronic inflammation induced by Chlamydia could also potentially contribute to cancer development. Instead the diagnosis is usually made on a clinical basis in a sexually active woman with lower abdominal pain and cervical, uterine, and adnexal tenderness on pelvic examination. Estimates vary widely, which may be due to differences in the patient populations, with clinic-based studies having more cases of recently acquired incident infections. In a nonhuman primate model, repeated endocervical infections followed by direct tubal inoculation of C. Ten percent of patients and none of the control subjects had confirmed tubal infertility. In one study, women experiencing recurrent spontaneous abortions had high titers of antichlamydial IgG but negative endocervical cultures for C. A major difficulty in these studies is the potential interaction of other infections that may influence pregnancy outcomes, including genital infections caused by Mycoplasma, Ureaplasma, herpesviruses such as cytomegalovirus, and Trichomonas, as well as bacterial vaginosis, urinary tract infections, and vaginal colonization with gram-negative rods. Studies need to evaluate and analyze all of these factors comprehensively, making such studies both large and complex. Considerable clinical data are available on the treatment of uncomplicated urogenital tract infections in both men and women. Questions have been raised about the efficacy of azithromycin for treating chlamydial genital infections. Early repeated chlamydial infection has been reported in up to 5% to 13% of adolescents treated with azithromycin, which could represent reinfection, but treatment failure could not be excluded in some cases. In addition, a metaanalysis of randomized controlled trials suggested a degree of increased efficacy for doxycycline, particularly among symptomatic urethral infection in men. The primary manifestations are anal pruritus and pain and a mucous rectal discharge that may become mucopurulent. The infection remains superficial, is limited to the rectum, and closely resembles gonococcal proctitis. Leukocytes are usually present on rectal Gram stain even if the infection is asymptomatic. Extragenital Infections Proctitis (Rectal Infections) Oropharyngeal Infections Oropharyngeal infections have been documented by cell culture in heterosexual men (3. However, transmission to genital sites likely occurs,356,357 and treatment is recommended if detected. Test of cure after treatment is not necessary in most patients because of high cure rates with first-line antibiotics. It is reserved for specific circumstances, including pregnancy, persistent symptoms, and suboptimal antibiotics (erythromycin or amoxicillin). However, retesting 3 months after therapy is recommended because of the high risk of reinfection in women and men (see "Prevention Strategies" later). Few comparative data exist on the treatment of adult inclusion conjunctivitis, but doxycycline is effective when given for a 2- or 3-week period of time. However, even before the modern antibiotic era, cytoplasmic inclusions, which are identical to those seen in patients with trachoma, had been observed in conjunctival scrapings from neonates with conjunctivitis and subsequently in cells from the cervix of mothers and the urethra of fathers of infected infants. Exceptions include occasional infants who appear to have acquired infection perinatally despite birth by cesarean section, or postnatally from an infected caregiver by hand-to-eye contact. At birth, the conjunctiva lacks a lymphoid layer, so follicles do not develop initially but may become apparent after 3 to 6 weeks. The progression of the disease is similar to inclusion conjunctivitis in adults, with spontaneous resolution occurring in most untreated infants after 3 to 12 months. The primary differential diagnosis in a newborn is gonococcal ophthalmia, which is uncommon in children who receive ocular prophylaxis at birth, but can still occur. Most are afebrile and only moderately ill,405 but half have a history of conjunctivitis and a majority have middle ear abnormalities. Auscultation may reveal scattered crackles, but breath sounds are usually good and wheezing is usually absent. Long-term respiratory sequelae may be significant in more severe cases, as shown by a higher frequency of obstructive airway disease and physician-diagnosed asthma in children who were diagnosed with chlamydial pneumonia in the first 6 months of life. Such a test of cure is not routinely done for chlamydial genital infections but is recommended for pregnant women to ensure therapeutic cure in light of the serious sequelae of neonatal infection. Thus a woman who is positive in the first trimester should receive a test of cure, a follow-up test at 3 months, and a retest during her third trimester. However, chlamydial infection among prepubertal children 3 years and older should be considered indicative of sexual abuse.
Discount tranexamic 500 mg on line
Bleach treatment pink eye order tranexamic without prescription, chlorine dioxide, ethylene oxide, hydrogen peroxide, peroxyacetic acid, methyl bromide, paraformaldehyde, and vaporized hydrogen peroxide all were used to some degree in the federal decontamination process in 2001 and 2002. In the event of widespread contamination of individuals and households where the public will be expected to be performing much of the decontamination efforts, it is likely that household bleach in 1: 10 dilution will be recommended because it is readily available. Contaminated individuals should be advised to remove clothing and place it in a bag either before entering their home or immediately after entering (to minimize spores coming off clothes into the home). Clothes can be decontaminated by washing in hot water with bleach and machine drying. Because it is well known from studies of wool mill workers and nonhuman primates that the innate immune system can eradicate an as yet undefined number of spores, preventing the development of inhalational anthrax, must every spore be removed from every surface There may be an acceptable level of contamination that will allow for a timelier and cost-effective remediation effort after a city-wide exposure without serious compromise to the public health of the community. The National Academy of Sciences reviewed remediation of buildings after anthrax contamination and addressed many of these controversial areas but concluded that it cannot be determined what lowest level of spore contamination is acceptably safe for exposure. Kournikakis B, Ho J Objective assessment of the hazard from anthrax terrorist attacks in an office environment. Chapter 207 Bacillus anthracis (Anthrax) Key References the complete reference list is available online at Expert Consult. Pathology of inhalational anthrax in 42 cases from the Sverdlovsk outbreak of 1979. Massive outbreak of anthrax in wildlife in the Malilangwe Wildlife Reserve, Zimbabwe. Centers for Disease Control and Prevention Expert Panel Meetings on Prevention and Treatment of Anthrax in Adults. A short course of antibiotic treatment is effective in preventing death from experimental inhalational anthrax after discontinuing antibiotics. Bioterrorism-related inhalational anthrax: the first 10 cases reported in the United States. Identifying meningitis during an anthrax mass casualty incident: systematic review of systemic anthrax since 1880. Effects of a reduced dose schedule and intramuscular administration of anthrax vaccine adsorbed on immunogenicity and safety at 7 months: a randomized trial. Meso-scale ecology of anthrax in southern Africa: a pilot study of diversity and clustering. Persistent anthrax as a major driver of wildlife mortality in a tropical rainforest. A major epidemic of anthrax in Zimbabwe: the experience at the Beatrice Road Infectious Diseases Hospital, Harare. The effect of seasonal variation on anthrax epidemiology in the upper Zambezi floodplain of western Zambia. Inhalation anthrax associated with dried animal hides- Pennsylvania and New York City, 2006. Cutaneous anthrax associated with drum making using goat hides from West Africa-Connecticut, 2007. Gastrointestinal anthrax after an animal-hide drumming event-New Hampshire and Massachusetts, 2009. Anthrax infection among heroin users in Scotland during 2009-2010: a case-control study by linkage to a national drug treatment database. American Society for Microbiology, Centers for Disease Control and Prevention, and Association of Public Health Laboratories. Sentinel Level Clinical Microbiology Laboratory Guidelines for Suspected Agents of Bioterrorism and Emerging Infectious Diseases-Bacillus anthracis. The isolation of viable and pathogenic Bacillus anthracis organisms from 200 year old bone fragments from the Kruger National Park. Clinical framework and medical countermeasure use during an anthrax mass-casualty incident. Anthrax toxin protective antigen-insights into molecular switching from prepore to pore. Impaired function of the Tie-2 receptor contributes to vascular leakage and lethality in anthrax. Anthrax lethal toxin disrupts intestinal barrier function and causes systemic infections with enteric bacteria. Sentinel Laboratory Guidelines for Suspected Agents of Bioterrorism and Emerging Infectious Diseases. A two-component direct fluorescent-antibody assay for rapid identification of Bacillus anthracis. Detection of anthrax toxin in the serum of animals infected with Bacillus anthracis by using engineered immunoassays. Evaluation and validation of a real-time polymerase chain reaction assay for rapid identification of Bacillus anthracis. Immune response to Bacillus anthracis protective antigen in patients with bioterrorism-related cutaneous or inhalation anthrax. Serological testing for anthrax antibodies in workers in a goat hair processing mill. A decision analytic approach to the treatment of patients with influenza-like illnesses. Bioterrorismrelated inhalational anthrax: the first 10 cases reported in the United States. Outbreak of oral-pharyngeal anthrax: an unusual manifestation of human infection with Bacillus anthracis. Anthrax toxins inhibit neutrophil signaling pathways in brain endothelium and contribute to the pathogenesis of meningitis. Both lethal and edema toxins of Bacillus anthracis disrupt the human dendritic cell chemokine network. In vitro susceptibility of Bacillus anthracis to various antibacterial agents and their time-kill activity. Antibiotic susceptibilities of 96 isolates of Bacillus anthracis isolated in France between 1994 and 2000. In vivo activity of oritavancin in animal infection models and rationale for a new dosing regimen in humans. Evaluation of combination drug therapy for treatment of antibioticresistant inhalation anthrax in a murine model. In vitro resistance of Bacillus anthracis Sterne to doxycycline, macrolides and quinolones. Antimicrobial treatment for systemic anthrax: analysis of cases from 1945-2014 identified through systemic literature review. The advantage of serum therapy as shown by comparison of various methods of treatment of anthrax. An outbreak of anthrax among drug users in Scotland, December 2009 to December 2010. Analysis of anthrax immune globulin intravenous with antimicrobial treatment in injection drug users, Scotland, 2009-2010. Comparative efficacy of Bacillus anthracis live spore vaccine and protective antigen vaccine against anthrax in the guinea pig. Anthrax vaccination and risk of optic neuritis in the United States military, 1998-2003. Safety, reactogenicity and immunogenicity of a recombinant protective antigen anthrax vaccine given to healthy adults. Immunogenicity and protective efficacy of Bacillus anthracis poly-gamma-dglutamic acid capsule covalently coupled to a protein carrier using a novel triazine-based conjugation strategy. Formaldehyde solution effectively inactivates spores of Bacillus anthracis on the Scottish island of Gruinard. Degradation of biological weapons agents in the environment: implications for terrorism response. Potential for aerosol dissemination of biological weapons: lessons from biological control of insects. Recovery of Bacillus anthracis from the nose and throat of apparently healthy workers. Hoover M Uncertainty and probability distribution analyses for anthrax dispersion and human exposure. Notice to readers: considerations for distinguishing influenza-like illness from inhalational anthrax.
Cheap 500mg tranexamic with visa
The Streptococcus anginosus (milleri) group is a subgroup within the viridans-group streptococci that includes three separate streptococcal species: S medications 3 times a day buy generic tranexamic pills. Within these three distinct streptococcal species, a number of subspecies have been recognized or proposed based primarily on molecular testing rather than phenotypic methods, the latter being highly variable. Microbiologically, members of this group are recognized by their microaerobic or anaerobic growth requirements, their formation of minute colonies, and the frequent presence of a characteristic caramellike odor. Like other streptococci, these organisms may be -hemolytic, -hemolytic, or -hemolytic on sheep blood agar. Phenotypic differentiation of Streptococcus constellatus, Streptococcus intermedius, and Streptococcus anginosus [the Streptococcus milleri group]: association with different body sites and clinical infections. A study of small colony, beta-haemolytic, Lancefield group C streptococci within the anginosus group: description of Streptococcus constellatus subsp. Phenotypic differentiation of Streptococcus constellatus, Streptococcus intermedius, and Streptococcus anginosus (the Streptococcus milleri group): association with different body sites and clinical infections. Most assays require both amplification and sequencing of the targeted region, making the method impractical for routine use. In addition, viridans streptococci are competent-that is, they freely exchange genetic material within and between species. Sialidase, therefore, may be a growth factor and may play a role in the ability of these microorganisms to proliferate in humans. In vitro studies by these and other investigators have confirmed that anaerobes enhance the growth of S. Anginosus group streptococci also possess virulence factors that are likely to be involved in their ability to cause serious invasive infections. Fibrinogen binding may, in turn, aid in platelet aggregation, which would also facilitate the development of endocarditis. The production of pyrogenic exotoxins by other Streptococcus species is well known. Moreover, intermedilysin is essential for the invasion of human hepatic cells and is thus an important factor in the pathogenesis of liver abscesses. One of the most prevalent hydrolytic enzymes is hyaluronidase,53 which has been found in pus54 and shown to be a growth factor. One such factor is an immunosuppressive and B-cell mitogenic protein (P90) that is produced by S. This virulence effect is thought to be mediated by stimulation of suppressor lymphocytes. Multilocus sequence analysis18 and case reports of cervical necrotizing fasciitis involving S. The ability to escape phagocytosis would allow these pathogens to replicate after arriving at and adhering to a site of tissue damage. Superantigens Virulence Factors Resistance to Phagocytosis Cytotoxins Hydrolytic Enzymes Members of the S. The primary species associated with bacteremia in one recent bacteremia study was S. Endocarditis results either from an abnormal heart valve or a prosthetic heart valve, although the exact attachment mechanism is unknown. In addition, these organisms have been found in culture-negative intracerebral abscesses by gene sequencing from direct specimens. Rapid surgical drainage is a critical prognostic factor for effective management of these spinal cord abscesses. Such infections include liver abscesses, peritonitis, pelvic abscesses, subphrenic abscesses, appendicitis, abdominal wound infections, and cholangitis. The proclivity for liver abscess and bacteremia91 and cholangitis92 must be appreciated. Therefore, the addition of an aminoglycoside to a -lactam agent for treatment of endocarditis caused by members of the S. Of the cephalosporins that are clinically available, cefepime, cefotaxime, and ceftriaxone have been noted to be superior in potency and spectrum for empirical coverage of patients at risk for streptococcal bacteremias. Streptococcus intermedius, Streptococcus constellatus, and Streptococcus anginosus (the Streptococcus milleri group): association with different body sites and clinical infections. Streptococcus intermedius, Streptococcus constellatus, and Streptococcus anginosus ("Streptococcus milleri group") are of different clinical importance and are not equally associated with abscess. Invasive Streptococcus anginosus group infection-does the species predict the outcome Taxonomy of the Anginosus group of the genus Streptococcus and description of Streptococcus anginosus subsp. Interaction between human polymorphonuclear leukocytes and Streptococcus milleri group bacteria. Isolation and characterization of "Streptococcus milleri" group strains from oral and maxillofacial infections. Clinical and microbiological outcomes in patients with Streptococcus anginosus group bacteremia identified through use of a rapid microarray assay. A study of susceptibility of 100 clinical isolates belonging to the Streptococcus milleri group to 16 cephalosporins. Antibiotic susceptibilities of genetically characterized Streptococcus milleri group strains. Species-specific difference in antimicrobial susceptibility among viridans group streptococci. Emended descriptions and recognition of Streptococcus constellatus, Streptococcus intermedius, and Streptococcus anginosus as distinct species. Phenotypic differentiation of Streptococcus intermedius, Streptococcus constellatus, and Streptococcus anginosus strains within the "Streptococcus milleri group". A study of small-colony, beta-haemolytic, Lancefield group C streptococci within the Anginosus group: description of Streptococcus constellatus subsp. Detection of diacetyl (caramel odor) in presumptive identification of the "Streptococcus milleri" group. Lancefield grouping and smell of caramel for presumptive identification and assessment of pathogenicity in the Streptococcus milleri group. A streptolysin S homologue is essential for -haemolytic Streptococcus constellatus subsp. Identification of "Streptococcus milleri" group isolates to the species level with a commercially available rapid test system. Members of a new subgroup of Streptococcus anginosus harbor virulence related genes previously observed in Streptococcus pyogenes. Use of the Phoenix automated system for identification of Streptococcus and Enterococcus spp. The pyogenic potential of the different Streptococcus anginosus group bacterial species: retrospective cohort study. A mechanism of pathogenicity of "Streptococcus milleri group" in pulmonary infection: synergy with an anaerobe. Complicated parapneumonic effusion and empyema thoracis: microbiology and predictors of adverse outcomes. The clinical features of respiratory infections caused by the Streptococcus anginosus group. Case-control study of pneumonia patients with Streptococcus anginosus group bacteria in their sputum. Surface-associated properties of Streptococcus milleri group strains and their potential relation to pathogenesis. Albuminbinding proteins on the surface of the Streptococcus milleri group and characterization of the albumin receptor of Streptococcus intermedius C5. Potential pathogenic properties of members of the "Streptococcus milleri" group in relation to the production of endocarditis and abscesses. Experimental endocarditis induction and platelet aggregation by Streptococcus anginosus, Streptococcus constellatus and Streptococcus intermedius. A cytotoxic toxin specific for human cells of a Streptococcus intermedius isolated from human liver abscess.
500mg tranexamic sale
Palivizumab prophylaxis to prevent respiratory syncytial virus mortality after pediatric bone marrow transplantation: a decision analysis model symptoms 6 weeks pregnant tranexamic 500mg on-line. Drug candidates and model systems in respiratory syncytial virus antiviral drug discovery. Risk of nosocomial respiratory syncytial virus infection and effectiveness of control measures to prevent transmission events: a systemic review. Epidemiology and prevention of pediatric viral respiratory infections in health-care institutions. Medical and economic impact of a respiratory syncytial virus outbreak in a neonatal intensive care unit. Cost-effectiveness analysis of palivizumab in premature infants without chronic lung disease. Reduced-dose schedule of prophylaxis based on local data provides near-optimal protection against respiratory syncytial virus. Impact of the updated guidance for palivizumab prophylaxis against respiratory syncytial virus infection: a single center experience. Sentinel1: an observational study of respiratory syncytial virus hospitalizations among U. Palivizumab prophylaxis, respiratory syncytial virus, and subsequent recurrent wheezing. Development of motavizumab, an ultra-potent antibody for the prevention of respiratory syncytial virus infection in the upper and lower respiratory tract. Efficacy of motavizumab for the prevention of respiratory syncytial virus disease in healthy Native American infants: a phase 3 randomised double-blind placebocontrolled trial. Structure-based design of a fusion glycoprotein vaccine for respiratory syncytial virus. Respiratory syncytial virus transplacental antibody transfer and kinetics in mother-infant pairs in Bangladesh. Impact of placental malaria and hypergammaglobulinemia on transplacental transfer of respiratory syncytial virus antibody in Papua New Guinea. Orthopneumovirus and Metapneumovirus were categorized into separate genera because of different gene numbers and order and because the viruses shared only 40% homology. During fusion, the F protein refolds through a series of unstable intermediates into a highly stable postfusion F conformation. Current evidence suggests that the G protein helps tether virus particles to the cell surface and confers optimal infectivity but is not critical for viral attachment. This pleomorphic form of the virus is stain penetrated, thereby permitting visualization of portions of the virus envelope and nucleocapsid. A border composed of the surface projection proteins may also be seen around the virus periphery. The incubation period is not precisely known, although cases of nosocomial transmission suggest an incubation period of about 5 to 6 days. Lobar consolidation occurs less frequently (18%) and may be due to bacterial complications. In older children, the dominant pathogen associated with asthma exacerbations was rhinovirus. Although healthy older adults generally do not require medical attention, wheezing and dyspnea are more common than in young adults. In contrast, adults with underlying cardiopulmonary conditions are at high risk for hospitalization where illnesses are primarily characterized by severe cough and lack of fever. Chest radiographs most often show bilateral airspace opacities, and computed tomography scan findings consist of patchy areas of ground-glass opacification and multiple nodules. This 23-month-old child admitted to an intensive care unit required mechanical ventilation for 4 days. Overall, prematurity confers the greatest risk for severe disease, with an odds ratio of 13. Several studies suggest that severity or specific symptoms may vary with genotype. Nebulized -adrenergic agents, such as albuterol, have historically been administered to hospitalized children with a history of asthma or wheezing; however, current evidence suggests that this practice does not improve patient outcomes. Oral ribavirin is currently licensed for the treatment of hepatitis C, and intravenous ribavirin has been administered on a compassionate-use basis for the treatment of viral hemorrhagic fevers. An analysis using propensity scores to evaluate the effect of oral ribavirin to treat immunocompromised patients with paramyxovirus infections demonstrated no significant clinical benefit. Although use of shell vial cultures may speed time to identification of virus, delays in diagnosis limit clinical utility. An outbreak of severe respiratory tract infection due to human metapneumovirus in a long-term care facility for the elderly in Oregon. Albuterol use in children hospitalized with human metapneumovirus respiratory infection. A broadly neutralizing human monoclonal antibody exhibits in vivo efficacy against both human metapneumovirus and respiratory syncytial virus. Evaluation of a live attenuated human metapneumovirus vaccine in adults and children. Genetic diversity, seasonality and transmission network of human metapneumovirus: identification of a unique sub-lineage of the fusion and attachment genes. Comparison of nasal cytokine profiles of human metapneumovirus and respiratory syncytial virus. Engineering, structure and immunogenicity of the human metapneumovirus F protein in the postfusion conformation. Epidemiologic characteristics and seasonal distribution of human metapneumovirus infections in five epidemic seasons in Stockholm, Sweden, 2002-2006. The role of human metapneumovirus in upper respiratory tract infections in children: a 20-year experience. Human metapneumovirus infection plays an etiologic role in acute asthma exacerbations requiring hospitalization in adults. Human metapneumovirus viral load is an important risk factor for disease severity in young children. Incidence, morbidity, and costs of human metapneumovirus infection in hospitalized children. Characterization of human metapneumoviruses isolated from patients in North America. Structure and immunogenicity of pre-fusion-stabilized human metapneumovirus F glycoprotein. Human metapneumovirus is capable of entering cells by fusion with endosomal membranes. Residues of the human metapneumovirus fusion (F) protein critical for its strain-related fusion phenotype: implications for the virus replication cycle. Low-pH triggering of human metapneumovirus fusion: essential residues and importance in entry. Potential electrostatic interactions in multiple regions affect human metapneumovirus F-mediated membrane fusion. Human metapneumovirus induces reorganization of the actin cytoskeleton for direct cell-to-cell spread. Mutations in the fusion protein heptad repeat domains of human metapneumovirus impact on the formation of syncytia. Genetic diversity and evolution of human metapneumovirus fusion protein over twenty years. Pathology of human metapneumovirus infection: insights into the pathogenesis of a newly identified respiratory virus. Human metapneumovirus establishes persistent infection in the lungs of mice and is reactivated by glucocorticoid treatment. An outbreak of severe respiratory tract infection due to human metapneumovirus in a long-term care facility. Role of type I interferon signaling in human metapneumovirus pathogenesis and control of viral replication. Functional motifs responsible for human metapneumovirus M2-2-mediated innate immune evasion. Differential production of inflammatory cytokines in primary infection with human metapneumovirus and with other common respiratory viruses of infancy.
Dumpling Cactus (Peyote). Tranexamic Acid.
- How does Peyote work?
- What is Peyote?
- Fever, arthritis-like pain, bone fractures, wounds, and other conditions.
- Are there safety concerns?
- Dosing considerations for Peyote.
- Are there any interactions with medications?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96482
Purchase tranexamic overnight delivery
The development of respiratory syncytial virus-specific IgE and the release of histamine in naso-pharyngeal secretions after infection symptoms after flu shot purchase tranexamic from india. Beta-chemokines, but neither T helper type 1 nor T helper type 2 cytokines, correlate with severity of illness during respiratory syncytial virus infection. Respiratory syncytial virus infection in children with compromised immune function. Differential response of dendritic cells to human metapneumovirus and respiratory syncytial virus. Viral upper respiratory tract infection and otitis media complication in young children. Prevalence of various respiratory viruses in the middle ear during acute otitis media. Initial radiographic features as outcome predictor of adult respiratory syncytial virus respiratory tract infection. Medically attended respiratory syncytial virus infections in adults aged 50 years: clinical characteristics and outcomes. Modelling estimates of the burden of respiratory syncytial virus infection in adults and the elderly in the United Kingdom. Respiratory syncytial virus infection in older adults: an underrecognized problem. Viral shedding and immune responses to respiratory syncytial virus infection in older adults. Respiratory syncytial virus and influenza A infections in the hospitalized elderly. Mortality associated with influenza and respiratory syncytial virus in the United States. Risk factors for respiratory syncytial virus illness among patients with chronic obstructive pulmonary disease. Importance of viral and bacterial infections in chronic obstructive pulmonary disease exacerbations. Risk factors for respiratory failure associated with respiratory syncytia virus infection in adults. High viral load and respiratory failure in adults hospitalized for respiratory 174. Bacterial complications of respiratory tract viral illness: a comprehensive evaluation. Adults 65 years old and older have reduced numbers of functional memory T cells to respiratory syncytial virus fusion protein. Human metapneumovirus and other respiratory viral infections during pregnancy and birth, Nepal. Viral respiratory infections in children with technology dependence and neuromuscular disorders. Respiratory syncytial virus infection in 406 hospitalized premature infants: results from a prospective German multicentre database. Persistence of morbidity and cost differences between late-preterm and term infants during the first year of life. Palivizumab prophylaxis of respiratory syncytial virus disease from 1998 to 2002: results from four years of palivizumab usage. Respiratory syncytial virus in patients with congenital heart disease: a contemporary look at epidemiology and success of preoperative screening. Environmental and demographic risk factors for respiratory syncytial virus lower respiratory tract disease. The challenge of respiratory virus infections in hematopoietic cell transplant recipients. Community respiratory virus infections in bone marrow transplant recipients: the M. Respiratory syncytial virus infection in patients with hematological diseases: single-center study and review of the literature. Risk factors for severe respiratory syncytial virus disease in children with cancer: the importance of lymphopenia and young age. Community respiratory virus infections among hospitalized adult bone marrow transplant recipients. A multicenter consortium to define the epidemiology and outcome of inpatient respiratory viral infections in pediatric hematopoietic stem cell transplant recipients. A multicenter consortium to define the epidemiology and outcome of pediatric solid organ transplant recipients with inpatinet respiratory virus infection. Changing epidemiology of respiratory viral infection in hematopoietic cell transplant recipients and solid organ transplant recipients. Nosocomial transmission of respiratory syncytial virus in an outpatient cancer center. Detection and control of a nosocomial respiratory syncytial virus outbreak in a stem cell transplantation unit: the role of palivizumab. Respiratory syncytial virus in hematopoietic cell transplant recipients: factors determining progression to lower respiratory tract disease. Outcome of respiratory syncytial virus lower respiratory tract disease in hematopoietic cell transplant recipients receiving aerosolized ribavirin: significance of stem cell source and oxygen requirement. Supplemental oxygen-free days in hematopoietic cell transplant recipients with respiratory syncytial virus. Differing manifestations of respiratory syncytial virus-associated severe lower respiratory tract infections in human immunodeficiency virus type 1-infected and uninfected children. How I treat respiratory viral infections in the setting of intensive chemotherapy or hematopoietic cell transplantation. Guidelines for preventing opportunistic infections among hematopoietic stem cell transplant recipients: focus on community respiratory virus infections. Identifying hospitalized infants who have bronchiolitis and are at high risk for apnea. Aspiration: a factor in rapidly deteriorating bronchiolitis in previously healthy infants Risk of secondary bacterial infection in infants hospitalized with respiratory syncytial viral infection. Concurrent serious bacterial infections in 2396 infants and children hospitalized with respiratory syncytial virus lower respiratory tract infections. Sepsis workup in febrile infants 0-90 days of age with respiratory syncytial virus infection. Lack of usefulness of an abnormal white blood cell count for predicting a concurrent serious bacterial infection in infants and young children hospitalized with respiratory syncytial virus lower respiratory tract infection. Association between respiratory syncytial viral disease and the subsequent risk of the first episode of severe asthma in different subgroups of high-risk Australian children: a whole-of-population-based cohort study. Association between respiratory syncytial virus hospitalizations in infants and respiratory sequelae: systematic review and meta-analysis. Respiratory syncytial virus lower respiratory tract illness in infancy and subsequent morbidity. Respiratory syncytial virus infection provokes airway remodelling in allergen-exposed mice in absence of prior allergen sensitization. Reviewing the evidence for early-life respiratory viral infection as modifiable risk factors to prevent childhood asthma. Comparing nose-throat swabs and nasopharyngeal aspirates collected from children with symptoms for respiratory virus identification using real-time polymerase chain reaction. What is the added benefit of oropharyngeal swabs compared to nasal swabs alone for respirator virus detection in hospitalized children aged <10 years Determining the seasonality of respiratory syncytial virus in the United States: the impact of increased molecular testing. Lack of sensitivity of rapid antigen tests for the diagnosis of respiratory syncytial virus infection in adults. Ribavirin for respiratory syncytial virus infection of the lower respiratory tract in infants and young children. Impact of aerosolized ribavirin on mortality in 280 allogeneic haematopoietic stem cell transplant recipients with respiratory syncytial virus infections. Efficacy of oral ribavirin in hematologic disease patients with paramyxovirus infection: analytic strategy using propensity scores. Comparative effectiveness of aerosolized versus oral ribavirin for the treatment of respiratory syncytial virus infections: a single-center retrospective cohort study and review of the literature.
Order tranexamic with a visa
It can be anticipated that infection caused by coagulase-negative staphylococci will parallel the increasing use of such devices treatment yeast infection home purchase 500 mg tranexamic overnight delivery. It is therefore not surprising that coagulase-negative staphylococci, whose chief virulence determinant is the ability to elaborate a biofilm, have been incriminated as a cause of a variety of 2442 blood generally obtained (0. A particularly common problem, conjunctivitis, is reported to occur in 4% to 22% of neonates. Erythema toxicum neonatorum, a benign self-limited eruption, may be caused by an innate immune response to coagulase-negative staphylococci that have colonized the hair follicles. Staff should adhere to appropriate protocol in caring for the catheter site and in accessing the catheter, including thorough disinfection of the catheter connector valve or hub. A meta-analysis of five randomized controlled trials that evaluated the safety and efficacy of prophylactic vancomycin in preventing late-onset sepsis in neonates has confirmed a beneficial effect. There were insufficient data to evaluate the risk of development of vancomycin-resistant organisms. Similarly, a trial of a vancomycin-heparin catheter lock solution proved beneficial in preventing bloodstream infections. Rare cases of native valve endocarditis, endophthalmitis, and septicemia have been cited in the literature. Companion animals have been noted to be colonized with antibiotic-resistant strains of S. Unfortunately, with the increased use of medical devices, the challenge of coagulase-negative staphylococcal infections is not likely to diminish. Chapter 195 Staphylococcus epidermidis and Other Coagulase-Negative Staphylococci the increasing prevalence of multidrug-resistant S. Antimicrobials from human skin commensal bacteria protect against Staphylococcus aureus and are deficient in atopic dermatitis. Coagulase-negative staphylococcal strain prevents Staphylococcus aureus colonization and skin infection by blocking quorum sensing. Evidence for autolysin-mediated primary attachment of Staphylococcus epidermidis to a polystyrene surface. Clinical significance of coagulase-negative staphylococci isolates from nosocomial bloodstream infections. Staphylococcus haemolyticus - an emerging threat in the twilight of the antibiotics age. Distribution and persistence of Staphylococcus and Micrococcus species and other aerobic bacteria on human skin. Matrix-assisted laser desorption ionization-time of flight mass spectrometry: a fundamental shift in the routine practice of clinical microbiology. Identification of a variety of Staphylococcus species by matrix-assisted laser desorption ionization-time of flight mass spectrometry. Evaluation of the FilmArray blood culture identification panel: results of a multicenter controlled trial. Phylogenetic study of Staphylococcus and Macrococcus species based on partial hsp60 gene sequences. Staphylococcus epidermidis esp degrades specific proteins associated with Staphylococcus aureus biofilm formation and host-pathogen interaction. Staphylococcus epidermidis esp inhibits Staphylococcus aureus biofilm formation and nasal colonization. Coagulasenegative staphylococcal strain prevents Staphylococcus aureus colonization and skin infection by blocking quorum sensing. Ongoing revolution in bacteriology: routine identification of bacteria by matrix-assisted laser desorption ionization time-of-flight mass spectrometry. Comparison of two matrix-assisted laser desorption ionization-time of flight mass spectrometry methods with conventional phenotypic identification for routine identification of bacteria to the species level. Susceptibility patterns of coagulase-negative staphylococci to several newer antimicrobial agents in comparison with vancomycin and oxacillin. Comparative in vitro activity profile of oritavancin against recent gram-positive clinical isolates. New developments in the management of severe skin and deep skin structure infections - focus on tedizolid. Surveillance of tedizolid activity and resistance: in vitro susceptibility of gram-positive pathogens collected over 5 years from the united states and Europe. Decreased susceptibilities to teicoplanin and vancomycin among coagulase-negative methicillin-resistant clinical isolates of staphylococci. Heterogeneously vancomycin-resistant Staphylococcus epidermidis strain causing recurrent peritonitis in a dialysis patient during vancomycin therapy. Heterogeneous resistance to vancomycin in Staphylococcus epidermidis, Staphylococcus haemolyticus and Staphylococcus warneri clinical strains: characterisation of glycopeptide susceptibility profiles and cell wall thickening. High prevalence of heterogeneously glycopeptide-intermediate coagulase-negative staphylococci in sternal wounds. Molecular epidemiology of a vancomycin-intermediate heteroresistant Staphylococcus epidermidis outbreak in a neonatal intensive care unit. Clinical and Laboratory Standards Institute: Performance standards for antimicrobial susceptibility testing: twenty-third information supplement. Modality of bacterial growth presents unique targets: how do we treat biofilm-mediated infections Multiple combination bactericidal testing of staphylococcal biofilms from implant-associated infections. Efficacy of daptomycin versus vancomycin in an experimental model of foreign-body and systemic infection caused by biofilm producers and methicillinresistant Staphylococcus epidermidis. Staphylococcus aureus biofilms prevent macrophage phagocytosis and attenuate inflammation in vivo. Chapter 195 Staphylococcus epidermidis and Other Coagulase-Negative Staphylococci 2443. Targeting macrophage activation for the prevention and treatment of Staphylococcus aureus biofilm infections. Comparison of molecular typing methods for characterization of Staphylococcus epidermidis: proposal for clone definition. Extreme genetic diversity of methicillin-resistant Staphylococcus epidermidis strains disseminated among healthy Japanese children. Inferring a population structure for Staphylococcus epidermidis from multilocus sequence typing data. Clonal analysis of Staphylococcus epidermidis isolates carrying or lacking biofilm-mediating genes by multilocus sequence typing. Multiple-locus variable-number tandem repeat analysis for typing of Staphylococcus epidermidis. Rapid and high-throughput genotyping of Staphylococcus epidermidis isolates by automated multilocus variable-number of tandem repeats: a tool for real-time epidemiology. Characterization of Staphylococcus epidermidis polysaccharide intercellular adhesin/hemagglutinin in the pathogenesis of intravascular catheter-associated infection in a rat model. Characterization of the importance of polysaccharide intercellular adhesin/ hemagglutinin of Staphylococcus epidermidis in the pathogenesis of biomaterial-based infection in a mouse foreign body infection model. Molecular basis of intercellular adhesion in the biofilm-forming Staphylococcus epidermidis. Regulated expression of pathogen-associated molecular pattern molecules in Staphylococcus epidermidis: quorum-sensing determines pro-inflammatory capacity and production of phenol-soluble modulins. Genomewide analysis of gene expression in Staphylococcus epidermidis biofilms: insights into the pathophysiology of S. Insights on evolution of virulence and resistance from the complete genome analysis of an early methicillin-resistant Staphylococcus aureus strain and a biofilm-producing methicillinresistant Staphylococcus epidermidis strain. Identification and characterization of a novel autolysin (aae) with adhesive properties from Staphylococcus epidermidis. Characterization of the importance of Staphylococcus epidermidis autolysin and polysaccharide intercellular adhesin in the pathogenesis of intravascular catheter-associated infection in a rat model. Pathogenic implication of a fibrinogen-binding protein of Staphylococcus epidermidis in a rat model of intravascular-catheter-associated infection. Accumulation-associated protein enhances Staphylococcus epidermidis biofilm formation under dynamic conditions and is required for infection in a rat catheter model. Role for the A domain of unprocessed accumulation-associated protein (aap) in the attachment phase of the Staphylococcus epidermidis biofilm phenotype.

Cheap 500 mg tranexamic overnight delivery
Chapter 211 Neisseria meningitidis Outbreak Immunoprophylaxis Cases of invasive meningococcal disease can occur in communities or organizations medicine 19th century tranexamic 500 mg on-line. Thus, meningococcal vaccination is an adjunct to expanded chemoprophylaxis when an outbreak is caused by a vaccine-preventable serogroup. The occurrence of meningococcal outbreaks during the Hajj and Umrah pilgrimages has been related to high meningococcal transmission and carriage in pilgrims. In one historic study from Mecca, meningococcal carriage rates were as high as 80%. In 2000 and 2001, two large outbreaks caused by meningococcal serogroup W529,530 resulted in the inclusion of a quadrivalent (A, C, Y, W) vaccine, either polysaccharide within 3 years or conjugate vaccine within 5 years, as a requirement for a Hajj or Umrah visa. Prevention of meningococcal disease in those receiving eculizumab is a special concern. Eculizumab is a humanized monoclonal antibody that binds C5 and inhibits the terminal complement pathway. Antibiotic chemoprophylaxis is recommended, but development of resistance to oral penicillin regimens has been reported. Challenges are the costs and other barriers to worldwide implementation of the meningococcal conjugate and MenB vaccines, gaps in vaccine coverage. Of note, meningococcal vaccine work may provide potential new insights into gonococcal vaccine strategies. Current epidemiology and trends in meningococcal disease-United States, 1996-2015. Protecting the herd: the remarkable effectiveness of the bacterial meningitis polysaccharide-protein conjugate vaccines in altering transmission dynamics. Laboratory Methods for the Diagnosis of Meningitis Caused by Neisseria meningitidis, Streptococcus pneumoniae, and Haemophilus influenzae. Virulence evolution of the human pathogen Neisseria meningitidis by recombination in the core and accessory genome. Lipooligosaccharide structures of invasive and carrier isolates of Neisseria meningitidis are correlated with pathogenicity and carriage. A journey into the brain: insight into how bacterial pathogens cross blood-brain barriers. Meningococcal disease among men who have sex with men-United States, January 2012-June 2015. Serogroup C invasive meningococcal disease among men who have sex with men and in gay-oriented social venues in the Paris region: July 2013 to December 2014. Clinical features, outcome, and meningococcal genotype in 258 adults with meningococcal meningitis: a prospective cohort study. The role of particular strains of Neisseria meningitidis in meningococcal arthritis, pericarditis, and pneumonia. Meningococcal pneumonia: characterization and review of cases seen over the past 25 years. Global and regional risk of disabling sequelae from bacterial meningitis: a systematic review and meta-analysis. The clinical features and long-term sequelae of invasive meningococcal disease in children. Population-based surveillance of Neisseria meningitidis antimicrobial resistance in the United States. Emergence of meningococci with reduced susceptibility to third-generation cephalosporins. Low immunogenicity of quadrivalent meningococcal vaccines in solid organ transplant recipients. Serogroup B meningococcal disease outbreak and carriage evaluation at a college-Rhode Island, 2015. Effectiveness of meningococcal B vaccine against endemic hypervirulent Neisseria meningitidis W Strain, England. Effectiveness of a group B outer membrane vesicle meningococcal vaccine against gonorrhea in New Zealand: a retrospective case-control study. Appendix B: evaluation and management of suspected outbreaks of meningococcal disease. Changes in Neisseria meningitidis disease epidemiology in the United States, 1998-2007: implications for prevention of meningococcal disease. Clonal descent and microevolution of Neisseria meningitidis during 30 years of epidemic spread. Zur differential diagnose des erregers der epidemischen cerebrospinalmeningitis und der gonorrhoea. Uber die aetiologie und pathologische anatomie der meningitis cerebrospinalis epidemica. The results of the serum treatment in thirteen hundred cases of epidemic meningitis. Etude de quelques germes isoles du rhino-pharynx, voisans du meningocoque (parameningocoques). Epidemiological study of 383 cases of meningococcus meningitis in the city of Milwaukee, 1927-1928 and 1929. Cerebrospinal fever: analysis of 3575 case reports, with special reference to sulphonamide therapy. Reference strains for the serologic groups of meningococcus (Neisseria meningitidis). Biology and pathogenesis of the evolutionarily successful human bacterium Neisseria meningitidis. Protecting the herd: the remarkable effectiveness of the bacterial meningitis polysaccharideprotein conjugate vaccines in altering transmission dynamics. Multilocus sequence typing: a portable approach to the identification of clones within populations of pathogenic microorganisms. Clonal diversity of Neisseria meningitidis from a population of asymptomatic carriers. Uncloaking the meningococcus, the dynamics of meningococcal carriage and meningococcal disease. Epidemiology and risk factors for serogroup X meningococcal meningitis during an outbreak in western Kenya, 2005-2006. Frequent interspecific genetic exchange between commensal Neisseriae and Neisseria meningitidis. Comparative genomics of Neisseria meningitidis: core genome, islands of horizontal transfer and pathogen specific genes. Molecular characterization and expression in Escherichia coli of the gene complex encoding the polysaccharide capsule of Neisseria meningitidis group B. An IgG monoclonal antibody to group B meningococci cross reacts with developmentally regulated polysialic acid units of glycoproteins in neural and extraneural tissue. Population structure and capsular switching of invasive Neisseria meningitidis isolates in the pre-meningococcal conjugate vaccine era-United States, 2000-2005. Capsule switching of Neisseria meningitidis sequence type 7 serogroup A to serogroup X. Attachment of Neisseria meningitidis to human mucosal surfaces: influence of pili and type of receptor cell. Genetic basis for biosynthesis, structure, and function of meningococcal lipooligosaccharide (endotoxin). Innate immune response to lipoologosaccharide: pivotal regulator of the pathobiology of invasive Neisseria meningitidis infections. Meningococcal endotoxin in lethal septic shock plasma studied by gas Chapter 211 Neisseria meningitidis 2607. Transcriptomic data from two primary cell models stimulating human monocytes suggest inhibition of oxidative phosphorylation and mitochondrial function by N. Effect of Neisseria meningitidis fur mutations on global control of gene transcription.
Order tranexamic cheap online
Infant-to-infant spread within nurseries probably occurs by the hands of personnel engaged in mouth care medicine in the civil war discount 500 mg tranexamic otc, gavage feeding, and other activities requiring close direct contact. Enlargement of the liver is more often due to congestive heart failure than to viral hepatitis. The overall mortality rate for neonatal myocarditis is 30% to 50%, and death usually occurs within a week of onset. Myocardial function rapidly improves in surviving infants after defervescence, generally by 1 week, although in a few infants, convalescence is prolonged for several weeks. Some surviving infants develop dilated cardiomyopathy with ventricular aneurysm formation. Infants dying of myocarditis have enlarged, dilated hearts, extensive myonecrosis, and a variable degree of cardiac inflammation. Hepatitis the initial symptoms of severe neonatal hepatitis are lethargy, poor feeding, and increasing jaundice that progress in many infants, within 1 to 2 days, to jaundice, ecchymoses, bleeding from puncture sites, and 2234 metabolic acidosis. Hepatic transaminases may rise rapidly to extremely high levels, and markedly prolonged prothrombin times and partial thromboplastin times confirm profound hepatic failure. More than half of infants with severe neonatal E hepatitis die within days after the onset of symptoms despite therapy with blood products and intensive supportive care. The long-term prognosis for surviving infants is not well known, although hepatic fibrosis and chronic hepatic insufficiency develop early in life in some. Persistent skeletal muscle involvement causes a dermatomyositis-like syndrome in more than half of these patients, and some also have chronic hepatitis. Autopsy findings have included chronic meningitis and encephalitis, with lymphocytic perivascular cuffing, focal loss of neurons, and gliosis of both gray and white matter. However, widespread destruction of motor neurons, such as that seen in poliomyelitis, has not been observed. The experimental antiviral drug pleconaril has been used in this setting, but the reported experience with it is uncontrolled and limited to a small number of patients. Neonatal myocarditis is sometimes mistaken for congenital heart disease because, in both conditions, murmurs and evidence of congestive heart failure may be present. However, fever and electrocardiographic evidence of acute myocardial injury are absent in patients with congenital heart disease. The early features of myocarditis and severe hepatitis resemble those of bacterial sepsis. Infants in congestive heart failure require judicious fluid management and administration of inotropic agents and diuretics. The profuse bleeding that results from hepatic failure necessitates frequent replacement therapy with packed red blood cells, platelets, and fresh-frozen plasma. Some epidemics of conjunctivitis in the Far East have involved both viruses sequentially or concurrently. Epidemiology Clinical Manifestations Nervous system manifestations may be totally absent, or mild nuchal rigidity, headache, lethargy, papilledema, seizure disorders, motor weakness, tremors, and ataxia may be present. These neurologic abnormalities may fluctuate in severity, disappear, or steadily progress. Within weeks, about 2500 cases occurred, largely among disadvantaged persons living in Miami. Postepidemic antibody prevalence rates of nearly 50% have been observed in Ghana and Indonesia but only in 6% of affected populations of Japan. Antibody prevalence rates are highest in children younger than 10 years, whereas attack rates for clinical disease are greatest in young adults, which indicates that many infections in children must be inapparent or mild. Burning, foreign body sensation, ocular pain, photophobia, eyelid swelling, and watery discharge begin in one eye and rapidly progress to the other eye. Conjunctival edema is said to be more common in elderly people; hemorrhage is more profuse in young patients. In most cases corneal erosion or a fine punctate epithelial keratitis can be demonstrated by slit-lamp examination after staining with fluorescein. The ocular discharge is serous or seromucoid and contains abundant neutrophils in the first 24 hours. Preauricular lymph nodes are often enlarged and tender by the second day of illness. Recovery is usually noticeable by the second or third day and is complete in most cases in 10 days, although discoloration from the hemorrhages sometimes persists for many days. Contagion can be prevented by careful hand washing, use of separate towels, and sterilization of ophthalmologic instruments. Evidence is somewhat stronger that certain Es, particularly E-11, E-14, and E-18, have occasionally been responsible for epidemic diarrhea in young infants. However, inconsistency regarding this finding has been noted across different studies. Infants and young children who develop a rhombencephalitis have a high mortality related to rapid cardiovascular collapse and pulmonary edema. Primary isolation is most successful in African green monkey kidney cell culture, although a cytopathic effect may take 5 to 8 days to develop. Aseptic meningitis among infants less than two years of age: acute illness and neurologic complications. Enterovirus-associated encephalitis in the California encephalitis project, 1998-2005. Epidemiology and clinical characteristics of acute flaccid paralysis associated with non-polio enterovirus isolation: the experience in the Americas. Epidemiology and clinical findings associated with enteroviral acute flaccid paralysis in Pakistan. Enterovirus co-infections and onychomadesis after hand, foot, and mouth disease, Spain, 2008. Detection of viruses in myocardial tissues by polymerase chain reaction: evidence of adenovirus as a common cause of myocarditis in children and adults. Survival of neonates with enteroviral myocarditis requiring extracorporeal membrane oxygenation. Apollo 11 disease or acute hemorrhagic conjunctivitis: a pandemic of a new enterovirus infection of the eyes. Isolation of Coxsackievirus A24 variant from patients with hemorrhagic conjunctivitis in Cuba, 2008-2009. Efficacy, safety, and immunology of an inactivated alum-adjuvant enterovirus 71 vaccine in children in China: a multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. Observations on viral excretion, seroimmunity, intrafamilial spread and illness association in coxsackie and echovirus infections. Association of clinical presentation, laboratory findings, and virus serotypes with the presence of meningitis in hospitalized infants with enterovirus infection. Syndrome of inappropriate secretion of antidiuretic hormone in enteroviral meningitis. Prospective investigation of a large outbreak of meningitis due to echovirus 30 during summer 2000 in Marseilles, France. Lack of cerebrospinal fluid pleocytosis in young infants with enterovirus infections of the central nervous system. Shift in cerebrospinal polymorphonuclear cell percentage in the early stage of aseptic meningitis. Cerebrospinal fluid mononuclear cell predominance is not related to symptom duration in children with enteroviral meningitis. Management of central nervous system infections during an epidemic of enteroviral aseptic meningitis. Viral central nervous system disease: an etiologic study conducted at the los Angeles County General Hospital. A clinical, epidemiologic and laboratory investigation of aseptic meningitis during the four-year period, 1955-1958. An epidemic of aseptic meningitis due to echovirus type 30: epidemiologic features and clinical and laboratory findings. Diagnosis of enteroviral meningitis by use of polymerase chain reaction of cerebrospinal fluid, stool, and serum specimens.
Discount tranexamic 500mg on line
Antibiotic prophylaxis may be useful but is limited to cases of medicosurgical procedures in the area of welldefined infective foci (see Chapter 83 for details) 8h9 treatment order tranexamic with a visa. Thus, detection of patients with risk factors, and respect for proper hygiene and antisepsis measures, remain the cornerstones of S. Dyspnea may be present from congestive heart and from septic pulmonary emboli in the case of right-sided endocarditis. General signs such as arthralgia or myalgia, back pain, and pleuritic pain are present in 10% to 50% of cases. A defect in atrioventricular conduction may represent a mycotic aneurysm of the sinus of Valsalva, usually the noncoronary cusp. However, the risk of embolization rapidly decreases within the first days of efficacious therapy. Larger septic emboli from broken-off vegetations can occlude the coronary or peripheral arteries, especially in the brain. Mycotic aneurysms are found in up to 15% of patients with bacterial endocarditis, and probably more frequently in S. They may arise either from direct invasion of the arterial wall by the infecting organisms, from septic embolization of the vasa vasorum, or from the deposition of immune complexes that trigger local inflammation and weakening of the arterial wall. Cerebral complications are frequent, occurring in 15% to 25% of patients517,519 and are associated with poor outcome. On the other hand, glycopeptides (vancomycin or teicoplanin) should not be used for short-course treatment because of their lack of bactericidal activity and poor vegetation penetration. This decision is difficult because anticoagulation therapy during extracorporeal circulation and after valve replacement puts the patients at increased risk of secondary intracerebral hemorrhage. Postoperative meningitis usually appears as hospitalacquired infection in young people, and most cases are associated with ventricular shunt devices,530 recent neurosurgery, or cerebrospinal fluid leak. On the other hand, spontaneous meningitis is a community-acquired infection associated with a variety of clinical sources (primary bacteremia, infective endocarditis, osteomyelitis) that mainly affects older patients with severe underlying conditions. The volume of blood cultures is critical because persistent bacteremia in infective endocarditis is often of low level, representing 1 to 100 bacteria per milliliter of blood. For each culture, 8 to 12 mL of blood should be drawn, with careful antiseptic precautions. Spinal epidural abscess is a rare infection of the central nervous system, usually occurring after operation or trauma, that can be associated with damage to the spinal cord and nerve roots. Agents proven appropriate for 2-week treatment of right-sided endocarditis are nafcillin and oxacillin. Some authors do not start rifampin until 3 days of effective therapy have been given, hoping to reduce the chance of secondary rifampin resistance. The infection may result either from airborne contamination or aspiration or from hematogenous seeding during bacteremia or right-sided endocarditis. In both cases, the pulmonary infection can lead to local complications, such as abscesses and pleural empyema. Demonstration of a pleural air-fluid level in the absence of a previous thoracocentesis suggests a bronchopleural fistula, another feared complication of S. However, deescalation therapy should occur whenever possible; in particular, a switch to a more rapidly bactericidal -lactam agent should be done whenever possible according to susceptibility testing. In the case of surgical drainage of empyema, the treatment duration is adjusted according to cultures and persistence of the pleural effusion. In the case of right-sided endocarditis, therapy is prolonged to 4 weeks according to standard recommendations for endocarditis treatment (see previous discussion). In one pediatric case review, the mortality rate decreased from more than 30% before the introduction of sulfa derivatives (years 1936 through 1940) to approximately 13% afterward (from 1941 to 1945). Other risk factors include individuals with an increased risk of bacteremia, such as patients undergoing hemodialysis or intravenous drug users, and immunosuppression. Osteoarticular Infections Pathogenesis Osteomyelitis Epidemiology Osteomyelitis has been described since antiquity. Its epidemiology has, however, dramatically changed over the last decades, in parallel with the increased use of medical devices in orthopedic surgery; the higher incidence of chronic disease, especially diabetes mellitus; and the emergence of resistant bacterial strains. The two ways by which bacteria can infect the bones are: 1, hematogenous seeding; and 2, contiguous contamination. In children with hematogenous osteomyelitis, the disease is usually located at the distal end of the long bone metaphysis, including the humerus, femur, and tibia. Terminal arterioles followed by stagnant blood in the venous sinusoids may facilitate the settlement of 2429 blood-borne staphylococci. In addition, microtrauma (or macrotrauma) to bone may facilitate infection by affecting the local blood supply or exposing host matrix proteins to which staphylococci can adhere. Chapter 194 Staphylococcus aureus (Including Staphylococcal Toxic Shock Syndrome) Clinical Features Osteomyelitis can be classified according to pathogenesis, to localization, to the presence of an implant, or to anatomy and comorbidity. Acute osteomyelitis is defined as a first episode that responds to medical treatment within 6 weeks. Symptoms are those of an acute septic syndrome with chills, high fever, malaise, and local pain and swelling. Blood cultures are positive in about 50% of cases, and blood or tissue cultures in 65% of cases. Chronic osteomyelitis is considered in all other situations, including the relapse of previously treated or untreated disease and infection arising by contiguity. The process can evolve over months or even years and is characterized by low-grade inflammation, the presence of necrosis, sequestra, pus, fistula, and recurrences. Diabetes-related osteomyelitis and vascular-related osteomyelitis principally involve the feet. They complicate chronic ulcers, which may be paradoxically painless because of associated neuritis. The ulcerative lesion should be explored gently, but in depth, with a surgical probe. Cultures of deep tissues and bone biopsy are mandatory for microbiologic diagnosis. Cultures of surface swabs and fistula fluids mostly yield skin contaminants but not the responsible pathogen. Diagnosis A Diagnosis of osteomyelitis integrates clinical signs, radiology, and microbiology. Important to note, chronic infection may be associated with persistent forms of S. The duration of drug treatment in most studies is 4 and 6 weeks but may vary up to 10 weeks or more in complicated situations. A series comparing 131 children showed equivalence 2430 between short (total of 20 days) and long (total of 30 days) treatment durations. Oral treatment is currently not recommended in adults, although newer quinolones may be appropriate because of their high bioavailability. Although controversial, some workers use ceftriaxone (2 g once a day), which was shown to be effective against S. Although vancomycin is still recommended as first-line therapy, daptomycin and linezolid are good alternatives. The disease may follow both hematogenous seeding and local trauma and may be of iatrogenic nature in the case of joint puncture or arthroscopy. Postarthroscopic septic arthritis has a prevalence of around 14 cases per 10,000 procedures. Joint destruction occurs within a few days from both bacterial and host inflammatory factors and probably also ischemic lesions from the increased intraarticular hydrostatic pressure. Therefore, patients with underlying arthritis with acute pain in a single joint should undergo aspiration immediately; the fluid should be examined for cell count, chemistry, and gout crystals (if appropriate), and culture should be performed. In adults, the mortality rate is around 11%429 and the prognosis is mostly associated with that of the underlying disease. Open joint drainage is usually unnecessary, except for hip infections in children, where it may help prevent necrosis of the femoral head. Although early symptoms may be acute, patients with low-grade or chronic infection may have few general symptoms, and the clinical signs may become centered around local pain and loosening of the prosthesis. Prosthetic joints remain susceptible to hematogenous seeding during their entire lifetime. Cultures of the fluid from the artificial joint are critical, preferably with broth culture, but can have negative results as well.