Buy prilosec 10 mg with amex
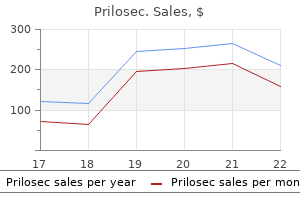
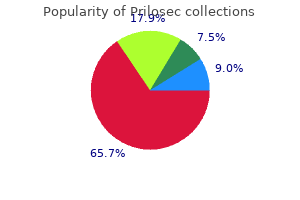
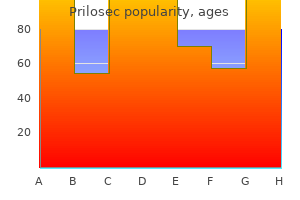
In contrast gastritis diet fruit purchase prilosec 40 mg without a prescription, Jeremitsky et al127 found that there was a higher mortality for patients age < 45 years with hypothermia. Among patients with mass lesions, the outcome was better for epidural hematomas compared with acute subdural hematomas. Age and level of consciousness on admission to neurorehabilitation were two independent prognostic factors. However, in one study, increased international normalized ratio was not related to outcome. If cerebral perfusion is already compromised, anemia can compound the effect and lead to further ischemia. Highest levels were found in patients who had early brain death (within the first week postinjury). Ten percent of their patients had medical complications during the hospitalization. Worse long-term outcome was most closely associated with pulmonary complications and infections. This reduced variability, particularly in the first 24 hours, and state of cardiac uncoupling have been associated with increased mortality and autonomic nervous system failure. Riordan et al179 proposed stratifying mortality risk based on the amount of time that patients had cardiac uncoupling over 24 hours, which they defined as 5-minute heart rate standard deviation between 0. They discovered that blockade had the best effect on patients who were in a cardiac uncoupled state for > 5% of the 24 hours. Propranolol was dosed at 1 mg intravenously every 6 hours and clonidine was dosed at 0. Presence of brainstem injury also correlated with poorer "professional ability," and coordination problems, visual impairment, psychosis, and spasticity appeared to occur more frequently in these patients. The results revealed that there was no difference in the primary end point of ventilator-free days, which is a composite outcome of time on the ventilator and mortality. It has been found to be an independent predictor of poor outcome even after adjusting for injury severity. Betablocker treatment was associated with improved survival in patients with elevated TnI. Gardner and colleagues186 evaluated a total of 51,799 patients with physical trauma. Rather, a drug development strategy that includes receptors or combinations of drugs that may act 30. Prognosis for Traumatic Brain Injury them to experience moderate disability (or, infrequently, even a severe disability) rather than a good recovery. Some individuals never fully recover to their premorbid level of function, and some individuals require ongoing lifetime care and support. However, ongoing investigation into blood and serum biomarkers, and improvements in neuroimaging techniques and technology offer some hope for improved prognostic capabilities for the future. Duration of coma is associated with worse outcome: Severe disability is less likely with coma duration of < 2 weeks. Older age is associated with worse outcome: Good recovery is less likely in individuals > 65 years old. From an outcome perspective, the early mortality rate following penetrating injury is considerably higher than it is for closed head injuries; however, among survivors, there are proportionately fewer people who are left vegetative or severely disabled. Once a person survives the penetrating injury, the chance of good recovery is high. Short-term mortality predictions for critically ill hospitalized adults: science and ethics. Accuracy of decisions to withdraw therapy in critically ill patients: clinical judgment versus a computer model. Bispectral analysis of electroencephalogram signals during recovery from coma: preliminary findings. Detecting consciousness in a total locked-in syndrome: an active event-related paradigm. Brief report: late improvement in consciousness after post-traumatic vegetative state. Predictive and prognostic models: implications for healthcare decision-making in a modern recession. Educating families and caretakers of traumatically brain injured patients in the new health care environment: a three phase model and bibliography. Trends in visits for traumatic brain injury to emergency departments in the United States. Recent trends in hospitalization and in-hospital mortality associated with traumatic brain injury in Canada: a nationwide, population-based study. Preliminary outcome analysis of a long-term rehabilitation program for severe acquired brain injury. Patient age and outcome following severe traumatic brain injury: an analysis of 5600 patients. Prognosis following severe head injury: development and validation of a model for prediction of death, disability, and functional recovery. Predicting survival using simple clinical variables: a case study in traumatic brain injury. Relative prognostic value of best motor response and brain stem reflexes in patients with severe head injury. Predicting course of recovery and outcome for patients admitted to rehabilitation. Effect of severity of post-traumatic confusion and its constituent symptoms on outcome after traumatic brain injury. Psychosocial outcome for the survivors of severe blunt head injury: the results from a consecutive series of 100 patients. Acute predictors of successful return to work 1 year after traumatic brain injury: a multicenter analysis. Comparison of clinical, radiologic, and serum marker as prognostic factors after severe head injury. Prediction of motor status 3 and 6 months post severe traumatic brain injury: a preliminary study. Defining cultural competence: a practical framework for addressing racial/ethnic disparities in health and health care. Traumatic Brain Injury in the United States: Emergency Department Visits, Hospitalizations, and Deaths. Prognostic factors of long-term functioning and productivity after traumatic brain injury: a systematic review of prospective cohort studies. The role of concussion history and gender in recovery from soccer-related concussion. Association between injury indices and outcome after severe traumatic brain injury in children. Outcome after major trauma: 12-month and 18-month follow-up results from the Trauma Recovery Project. Gender and age predict outcomes of cognitive, balance and vision testing in a multidisciplinary concussion center. The role of age and sex in symptoms, neurocognitive performance, and postural stability in athletes after concussion. Sex-specific differences in the severity of symptoms and recovery rate following sports-related concussion in young athletes. Sex differences and self-reported attention problems during baseline concussion testing. Clinical correlates of personality changes associated with traumatic brain injury. Psychiatric disorders and healthrelated quality of life after severe traumatic brain injury: a prospective study.
Diseases
- Patau syndrome
- Cold agglutination syndrome
- Cardiomyopathy cataract hip spine disease
- Bardet Biedl syndrome, type 3
- Amegakaryocytic thrombocytopenia
- Pulmonary valve stenosis
20mg prilosec mastercard
It is after that period of time that babies with anorectal malformations will develop abdominal distention; the intraluminal pressure in the rectum will be high enough to overcome the muscle tone of the sphincter mechanism surrounding the most distal portion of the rectum gastritis and stress buy discount prilosec 20mg. That is also the reason why diagnostic imaging studies designed to determine the position of the rectum in the pelvis should not be done before 24 hours of life. A collapsed rectum is difficult to see even using the most sophisticated imaging technology. Twenty-four hours later, the surgeon must decide whether the patient needs a colostomy or a primary procedure to repair the anorectal malformation. We recommend a descending colostomy, with separated stomas: separated enough to allow the placement of a stoma bag over the proximal (functional) stoma, leaving outside the distal stoma, also called mucous fistula-all of this with the specific purpose to avoid the passing of stool from the proximal to the distal colon. Colostomy 693 a risk of contamination and infection of the operative field after the main repair. Surgical technique for colostomy the recommended incision measures approximately 6 cm, is made in the left lower quadrant, and is oblique. The proximal functional stoma is placed in the upper and lateral portion of the incision, and the mucous fistula (nonfunctional) distal stoma is intentionally created small and placed in the lower and medial portion of the incision. The distal bowel must be irrigated with saline solution during the operation, in order to remove all the meconium. In this way, the distal bowel remains completely clean and collapsed, and the patient does not need any preparation prior to the main repair. The surgeon must carefully identify the piece of intestine that he or she is going to exteriorize to avoid serious mistakes. The most frequent errors in performing colostomies seen by the authors include the following25: 1. The surgeon thinks he or she is opening a transverse colostomy and actually grabs the sigmoid colon and exteriorizes it in the right upper quadrant. In these cases, the bowel was probably handled poorly and may suffer from ischemia and retraction. Choosing the descending colon to create the proximal, functional stoma avoids prolapse because that portion of the colon is normally attached to the posterior wall of the abdomen. The distal colostomy will never prolapse, even when it is performed in a mobile portion of the colon (sigmoid), because we specifically recommend creating a very small stoma, since it will only be used to irrigate the distal bowel and to perform a distal colostogram. Prior to the final repair, it is mandatory to perform a distal colostogram in order to determine the precise type of anatomic defect that the patient has. It is actually very difficult to clean the distal bowel through a transverse colostomy. Makes the distal colostogram easier than when dealing with a more proximal colostomy. It is very difficult to demonstrate the fistula injecting contrast material through a transverse colostomy. Distal colostogram this is, by far, the most important diagnostic study in dealing with anorectal malformations. A Foley catheter is introduced into the distal stoma, the balloon is inflated, and water-soluble Loop colostomies are problematic because they allow feces to pass into the distal stoma, provoking fecal impaction, megarectum, and urinary tract infection. Also, there is 694 Anorectal anomalies contrast material (never barium) is injected by hand, with a syringe, applying enough hydrostatic pressure to overcome the tone of the funnel-like muscle structure that surrounds the lowest part of the rectum. Failure to observe these principles will most likely show the dye staying above the pubococcygeus line, erroneously indicating the presence of a high defect and not showing the fistula, simply because of lack of hydrostatic pressure. When dealing with a case of rectovesical (bladder neck) fistula, the surgeon will be able to predict that the prognosis in terms of bowel function is not going to be as good as in other types of defects. Also, a laparotomy or laparoscopy will be necessary in order to mobilize the rectum. Most importantly, the surgeon will avoid looking for the rectum through a posterior sagittal incision where it will not be found, because that would risk injury to the urinary tract, vas deferens, seminal vesicles, and ectopic ureters. The posterior sagittal approach in this case will be used only to show the trajectory of the pull-through, after its mobilization through laparoscopy or via laparotomy, and to allow tacking of the rectum to the muscle complex. In cases of male newborns, it is important to place a Foley catheter in the bladder during the operation. The purpose of this is to avoid the most common accident seen during these operations, which is the urethral injury. The operation starts by placing multiple sutures and taking the mucocutaneous junction of the fistula. This serves the purpose of exerting uniform traction, which helps in the dissection. The posterior sphincter mechanism is divided to identify the posterior rectal wall; the dissection then is extended to the lateral walls of the rectum. The most delicate part of the operation is the dissection of the anterior rectal wall. Limited posterior sagittal anorectoplasty this procedure is performed in cases of rectovestibular fistula in female newborns. The incision is very similar to the one just described, but it is extended more cephalad as far as necessary to achieve enough bowel mobilization. The main difference with the previous defect is the fact that the rectum and vagina share a rather long common wall. The separation is carried out all the way up, until both structures are completely separated and have a full-thickness normal wall. Lack of adequate rectal mobilization is the main cause of dehiscence after this repair. The separation of the rectum from the vagina requires a meticulous and delicate technique and is performed with a needle-tip cautery, changing from cutting to coagulation where necessary to provide meticulous hemostasis. Once the rectum has been completely separated, the limits of the external sphincter are determined by electrical stimulation. If a colostomy is present, these patients can have oral feedings the same day of surgery and can go home the following day. Posterior sagittal anorectoplasty this technique is used for the repair of a rectourethral fistula or a rectovaginal fistula. The patient is placed as previously described in prone position, with the pelvis elevated and with a Foley catheter in the bladder. Electrical stimulation of the perineum will allow the surgeon to identify the anal dimple, which is the location of the center of the sphincter. The incision runs from the lower portion of the sacrum down and through the anal dimple, staying exactly in the midline, leaving equal amounts of sphincter muscle on both sides. After opening of the skin, one can identify the subcutaneous tissue and then the presence of parasagittal muscle fibers. The incision is deepened, and after another area of fat, the ischiorectal space, one finds the levator muscle. The levator muscle continues with the muscle complex down to the skin of the anal dimple, forming a funnel-like structure. Parasagittal fibers that run on both sides of the midline will close the lumen of the anus once this is reconstructed. Muscle complex fibers run perpendicular to the parasagittal ones and also medially. Parasagittal fibers, muscle complex, and levator muscle have been split in the midline. Definitive repair 697 then opened along its posterior wall between two traction sutures. One must remember that the rectum and urethra share a common wall immediately above the fistula. After approximately 1 cm of submucosal dissection, the dissection continues taking the full thickness of rectal wall. Once the rectum has been separated from the urethra, the fistula is closed with interrupted long-term absorbable sutures. If the catheter comes out accidentally, it is better to leave it out rather than trying to pass it back into the bladder and thus risking a urethral perforation at the urethral suture site.
Discount 40 mg prilosec free shipping
Some also present with mild facial abnormalities such as a high forehead gastritis or gastroenteritis buy prilosec 10mg with amex, a small nasal tip, and a short columella. Previously, the definitive investigation used to distinguish diffuse and focal forms of the disease was serial venous sampling of insulin. However, this procedure was invasive and time-consuming, and often resulted in inaccurate localization of focal disease. Subcutaneous or intravenous glucagon is used in the acute management of hypoglycemia, often in combination with octreotide. The calcium channel blocker nifedipine has been used successfully in a small number of patients. In mild cases, it may be possible to maintain acceptable levels of blood glucose by dietary measures alone. In the majority of cases, however, intravenous administration of high concentrations of glucose are required to maintain blood glucose levels above 2. In these cases, it is essential to insert a central venous catheter to provide a central route for administration of high concentrations of glucose and to allow frequent monitoring of blood glucose levels. For the laparoscopic approach, a three-trocar technique is used with triangulation centered around the umbilicus. Within the peritoneum, a thorough search is made for sites of ectopic pancreatic tissue. The hepatic flexure is reflected medially and the duodenum Kocherized to expose the head of the pancreas. It is essential for future immunologic competence to preserve the spleen whenever possible. This is accomplished by carefully exposing the short pancreatic vessels passing from the splenic vessels to the pancreas. Should hemorrhage occur from damage to the splenic vein, direct repair should be attempted. In the event of failure to achieve hemostasis, ligation of the splenic vein with preservation of the splenic function can be expected due to collateral supply from the short gastric vessels. The uncinate process is carefully dissected from behind the superior mesenteric vessels, and after positively defining the course of the common bile duct, the head of the pancreas to the left of the common duct and in the concavity of the duodenal loop is excised, leaving a sliver of pancreatic tissue on the surface of the duodenum and on the left wall of the common duct. This represents approximately 5% of the total volume of the pancreas but can vary considerably from patient to patient. Laparoscopic resection is performed in a similar manner, but it is easiest to perform the resection using a hook diathermy in a piecemeal manner, using a stay suture at different intervals along the pancreas as dissection proceeds from the pancreatic tail toward the head. For the transection of the pancreas itself, the harmonic scalpel ensures good hemostasis and occlusion of the pancreatic duct and cut parenchyma. The only remaining pancreatic tissue lies to the left of the common bile duct and a sliver in the C-curvature of the duodenum. In patients undergoing 95% pancreatectomy, the majority will develop insulin-dependent diabetes by the second decade of life. For those that do develop diabetes, novel, minimally invasive treatments such as pancreatic islet transplantation are now achieving excellent results for reversing insulin-requiring diabetes in adults. Neurologic outcomes of 90 neonates and infants with persistent hyperinsulinaemic hypoglycaemia. Perspective on the genetics and diagnosis of congenital hyperinsulinism disorders. Persistent hyperinsulinaemic hypoglycaemia of infancy: A heterogeneous syndrome unrelated to nesidioblastosis. The infant is kept nil by mouth with a nasogastric tube in situ until the postoperative ileus has resolved. Recurrent hypoglycemia can occur as a result of insufficient surgical resection of the diffuse form of the disease, or due to failed localization in the focal form, and should be evident within the first 72 hours after the operation. Other surgical complications include postoperative infection, bleeding, and operative trauma to the bile duct. Delayed diagnosis of bile duct injury can be treated operatively or conservatively depending on the degree of damage and the timing of presentation. Sirolimus therapy in congenital hyperinsulinism: A successful experience beyond infancy. A multidisciplinary approach to the focal form of congenital hyperinsulinism leads to successful treatment by partial pancreatectomy. Laparoscopic vs open pancreatectomy for persistent hyperinsulinaemic hypoglycaemia of infancy. Surgical complications of pancreatectomy for persistent hyperinsulinaemic hypoglycaemia of infancy. Persistent hyperinsulinaemic hypoglycaemia of infancy: Therapy, clinical outcome and mutational analysis. Hyperinsulinaemic hypoglycaemis of infancy (nesidioblastosis) in clinical remission: High incidence of diabetes mellitus and persistent beta-cell dysfunction at long term follow up. Phase 3 trial of transplantation of human islets in type 1 diabetes complicated by severe hypoglycemia. Glucose metabolism in 105 children and adolescents after pancreatectomy for congenital hyperinsulinism. The mortality rate was initially high, and it was only in the mid-1950s that an improved understanding of the pathogenesis and pathology of the condition led to innovative surgical techniques, which resulted in greatly improved surgical outcome. At his instigation, Barnard perfected the experimental model in pregnant mongrel bitches. Mesenteric vascular insults, such as volvulus, intussusception, and interference with the blood supply to a segment of bowel, were created in the dog fetus. The family history may help to identify hereditary forms and conditions that may predispose to atresia, i. The anomaly is usually not genetically determined, although affected monozygotic twins and siblings have been described. Sporadic jejunoileal atresia is different from the familial multiple atresias of the whole gastrointestinal tract seen in severe immune deficiency syndrome, which is an autosomal recessive condition. A classification system for familial intestinal atresia has been proposed that suggests that most cases result from disruption of a normal embryologic pathway in the development of the superior mesenteric artery and its branches. In stenosis, the proximal dilated and narrower distal bowel are in continuity with an intact mesentery, but at the point of junction, there is a short, narrow, somewhat rigid segment with a narrow but patent lumen. The intraluminal pressure in the proximal bowel produces bulging of the web into the distal intestine so that the transition from the distended to the collapsed bowel is conical in appearance-the "windsock" effect. The distal bowel is completely collapsed, and the small intestine is of normal length. More proximally, the bowel distension is less marked, and the bowel assumes a normal appearance. The distal collapsed bowel commences as a blind end, which is sometimes bulbous due to remains of a fetal intussusception. The corresponding intestinal mesentery is normal but may occasionally be deficient, leaving a V-shaped gap. There is always a V-shaped gap in the mesentery, and the total bowel length is reduced. This type is the consequence of an extensive infarction of the midgut secondary to a superior mesenteric artery occlusion just distal to the middle colic origin, producing a proximal jejunal atresia with loss of a varying segment of jejunum. The distal ileum remains viable, receiving an often precarious blood supply from the arterial supply to the right colon, around which the ileum is coiled. In addition, they may have associated bowel anomalies such as malrotation and may develop short bowel syndrome with increased morbidity and mortality. The site of the most proximal atresia determines whether it is classified as jejunal or ileal atresia. In all types, the intestine proximal to the obstruction becomes dilated and hypertrophied. This dilated bowel frequently has a cyanosed appearance and may have some necrotic areas from either sustained intraluminal pressure or secondary volvulus.
Order prilosec 20 mg with mastercard
The vaginal septum is then incised while the outer vaginal orifice is spread open by the nasal speculum and the transverse septum is pushed downward by the Kelly forceps gastritis symptoms+blood in stool best buy for prilosec. If the atretic lower portion of the vagina has been retracted up into the pelvis, it may be desirable to open the vagina through a laparotomy incision to avoid damage to the urethra, bladder, and rectum. Abdominal vaginostomy may be of two types: vaginostomy with an indwelling catheter and tubed vaginostomy. In this procedure, a U-shaped flap of the vagina is used to make a tube that provides drainage through the natural tract (rather than the need for a catheter) till the time of definitive surgery. A tubed vaginostomy avoids the long-term use of any indwelling catheter and at the same time provides an effective drainage. This also provides easy access for performing dye studies to outline the anatomy before doing a definitive surgery. Cases of type V hydrometrocolpos (associated with common cloaca) and a common channel more than 3 cm long require a vaginostomy and also a diverting colostomy. This is to be done keeping the good segment of the sigmoid bowel available for both vaginal replacement and bowel pull-through in the future. Drainage procedure 1129 at surgery, disconnection of the fistula is done followed by total urogenital mobilization. The vagina may be exteriorized onto the perineum, while the urogenital sinus can be made to function as the main urethra. The fistulous communication between the urethra and the vagina cannot be reached through the perineum. The common channel in type V is usually more than 3 cm, mandating a vaginal replacement. In such situations, it would be better to replace the vagina using bowel vaginoplasty. Low anomalies, usually presenting in the newborn period with a hymenal obstruction (rarely the distal vaginal obstruction) and a bulge in the perineum. The diagnosis is made on inspection and needle aspiration of the contents from the bulge under anesthesia. In such cases, there are two openings in the perineum instead of three: the urethra and the anus. The vagina is high up and has a tiny communication with the urinary bladder, usually at the level of the bladder neck. This communication is valvular and allows only one-way flow of urine from the urinary bladder to the vagina. A small amount of urine flows into the vagina during the act of micturition, but the vagina cannot drain it to the urethra due to the valvular effect; thus, there is slow development of hydrometrocolpos. Due to stasis of urine and the vaginal contents, the hydrometrocolpos gets infected, resulting in pyometrocolpos, and the child presents with septicemia. The genitourinary tract is often obstructed due to the effect of pressure, and there is a bilateral hydroureteronephrosis. The patient presents in an emergency with a palpable lump in the lower abdomen, urinary obstruction, sepsis, uremia, and bilateral hydroureteronephrosis. The dirty fluid needs to be drained out urgently using a catheter or by fashioning a formal tube vaginostomy by the suprapubic route. Final surgery, usually after the age of 1 year or so, would require closure of the communication of the channel from the bladder and a vaginal pull-through. It is easier said than done because the vaginal walls are inflamed, thickened, and plastered to the surrounding pelvic structures, and it is not possible to mobilize them to bring them down to the perineum. Thus, it is safe to perform a vaginal replacement and bridge the gap using a segment of the colon or ileum. The patient has only a single opening in the perineum, into which open the urethra, the vagina, and the bowel. In cases with a narrow distal vagina or if the vagina has retracted following its repair, flaps of perineal skin may be used to contribute to the distal vaginal segment. With the V-shaped perineal skin intact, blood supply is created and mobilized sufficiently. Many surgeons prefer the use of a skin graft over a vaginal mold, a cylinder of a prosthetic patch, or a buccal mucosa graft with a mesh to form the neovagina. The vagina may be bifid with a complete or incomplete septum in between with each half of the uterus. The bowel is opened with a fistulous tract either in the vaginal septum or in the bladder neck. In some cases, the whole of the colon is turned into a cesspoollike structure, called a pouch colon, having an abnormal vascular configuration. Surgery is required in the newborn period in emergencies for high-level types of anorectal abnormalities, urinary obstruction, and abdominal lump (hydrometrocolpos or pouch colon) in the form of a transverse colostomy (even ileostomy with the excision of pouch colon), closure of the fistula between the bowel and the bladder, and suprapubic tube vaginostomy to drain the vaginal contents. A part of the vaginal wall adherent to the base of the urinary bladder can be left in situ, and the fistula can be closed to prevent damage to the urinary bladder. Pitfalls and challenges of cloaca repair: how to reduce the need for reoperations. Experience with neonatal hydrometrocolpos in the Niger Delta area of Nigeria: Upsurge or increased recognition Cloaca and hydrocolpos: Laparoscopic-, cystoscopic- and colposcopic-assisted vaginostomy tube placement. The diagnosis of ambiguous genitalia is based on a meticulous perineal exam and gonadal palpation. The masculine phenotype presents a normal-looking penis and two scrotal testicles. The sex of rearing was mainly decided on the basis of what was believed would facilitate the "most functional genitalia and offer the child their best opportunity to reach normality" (Hughes et al. More recent studies have helped us to better understand what actually determines gender identity, but even now, there is a paucity of outcome data for evidence-based approaches to these rare disorders. New scientific acquisitions unveil the ever-evolving complexities of the neurobiological and psychosexual development regarding gender identity. Genital development is constitutively female and nondependent on estrogens prenatally. Gonad development Fifteen years have passed since the discovery of Sry as the primary "testis-determining gene" (Jager et al. Studies in mice are continuing to provide exciting information about differential structural changes and gene expression in normal gonad development (testis versus ovary) as well as the effect of targeted deletion of key genes involved in this process. Androgens the production of androgens by fetal Leydig cells is initially gonadotropin independent. Wolffian duct stabilization is dependent on high local concentrations of testosterone diffusing in a gradient along the duct from the adjacent ipsilateral gonad. It causes involution of the Mullerian ducts and stimulates the Leydig cells to produce testosterone. Tremendous progress has been made in the past 15 years in understanding the role of mutation of factors involved in the steroid genesis process. Considerably more research is needed to be able to translate this new knowledge into effective patient care and to understand the long-term outcome in specific conditions. The term intersex was used till 2005, and subcategories included male pseudohermaphrodite, female pseudohermaphrodite, 1134 Disorders of sexual development and true hermaphrodite. These terms used gender in the nomenclature and were often considered controversial or disparaging. Therefore, revised nomenclature was proposed that incorporated genetic etiology and descriptive terminology while removing gender references. Advances in identification of molecular genetic causes of abnormal sex with heightened awareness of ethical issues and patient advocacy concerns necessitate a reexamination of nomenclature. Terms such as intersex, pseudohermaphroditism, hermaphroditism, sex reversal, and gender-based diagnostic labels are particularly controversial. These terms are perceived as potentially pejorative by patients and can be confusing to practitioners and parents alike. The ideal nomenclature should be sufficiently flexible to incorporate new information yet robust enough to maintain a consistent framework. Terms should be descriptive and reflect genetic etiology when available, and accommodate the spectrum of phenotypic variation.
Teucrium scordium (Water Germander). Prilosec.
- How does Water Germander work?
- Asthma, diarrhea, fever, intestinal parasites, hemorrhoids, and inflamed wounds.
- What is Water Germander?
- Are there safety concerns?
- Dosing considerations for Water Germander.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96116
Discount prilosec uk
Histological analysis of 89 gonads was completed gastritis green tea buy prilosec online now, identifying 52 streak gonads, 32 dysgenetic testes, and 5 ovotestes. Twenty-nine gonads were analyzed: 10 ovotestes, 15 dysgenetic testes, and 4 ovaries. Bilateral gonadoblastoma was found in a 6-month-old patient with bilateral ovotestes Mean age of the 31 patients in G3 was 69. To our knowledge, this is the first report of bilateral gonadoblastoma in ovotestes at a very early age. Although we used to schedule simultaneous gonadal and genitalia procedures with good results encouraged by the laparoscopically better visualization and quicker intraperitoneal access, actually we prefer to avoid resection of any gonad except a classical streak before having definitive histology and to postpone genital surgical procedures. Sometimes, the macroscopic aspect of the gonad and gonaduct as well as the result of a frozen section biopsy strongly favor gonadectomy in patients with previous sex assignment. There is the advantage of a laparoscopic approach in these patients requiring secondary pelvic exploration, especially because many of them are potentially fertile. An additional role of laparoscopy is excision of Mullerian structures and prostatic utricles and orchidopexy in patients raised as males. In patients with a symptomatic utriculus, removal is best performed laparoscopically to increase the chance of preserving continuity of the vas deferens. We still prefer a laparoscopic approach in most of them as it not only enables better visualization of potential Mullerian structures but also allows for treatment of a patent peritoneal sac when removing the gonads, with better cosmetic results. In addition, most of these patients have asymmetric gonads, with one of them being intra-abdominal. Management 1139 There is evidence that innervation of the glans comes from the surrounding skin and plays an important role in sexual arousal, so in the last few years, we have been very careful in preserving most of it, trying to avoid its unnecessary sectioning. We also keep not only the dorsal pedicle but also the ventral skin and mucosal surface, and prefer not to excise the glans in any surface and but to hide it. Recently, a nonablative and potentially reversible technique that dismembers the corporal bodies while keeping them in the labia major has been described in response to new understanding that an intact clitoris plays a crucial role in the development of female sexuality, but no long-term follow-up is available. Cosmetically, a near-normal appearance can now be achieved, but long-term functional results with newer techniques are still unknown. It is now our belief that one-stage total reconstruction can be done in most patients in the early months of life. Nowadays, there is a strong influence of movements toward postponing any kind of surgery in the genitalia until the individual is able to decide and consent. Regardless of the timing or the procedure elected, the surgery must be done meticulously with a clear understanding of the anatomy and only be undertaken in centers with great experience and after all aspects of controversy have been explained in detail to the parents. Initial techniques consisted in total clitorectomy based on the belief that it was necessary to prevent gender dysphoria. However, new understanding that an intact clitoris plays a crucial role in the development of female sexuality has stimulated a more conservative surgical approach, but recession of the clitoris, keeping the corpora, may lead to painful erections during sexual arousal. Glans reduction was accomplished by superficial excise of the epithelium of the glanular groove, avoiding a scar in the glans tissue, which is fixed to the pubis attachment. This has been very helpful for reconstructive understanding, but the vagina is not always high or low and the sphincter not well seen. We have found a wide spectrum of vaginal location, from a normal position to an entrance in the bladder. Low confluence was classically repaired by a flap vaginoplasty and mid to high by a pull-through vaginoplasty. Even in the low type, we advocate for a very aggressive dissection of the posterior vaginal wall, separating it from the rectal wall. The vagina is then cut in the midline well back into its normal caliber, and at this point, a wide cutaneous flap can be sewn using delicate sutures. This maneuver of bringing the vagina out rather than skin in prevents the known complications of the Fortunoff flap (growing of hair and stenosis). Exteriorization of the high vagina in the severely masculinized female is a surgical challenge. We used this principle but in the lithotomy position and without previous opening to prevent bleeding, and never amputate the sinus tissue until the end as it may be used to enlarge the introitus. Each patient must be individualized, and this technique can be combined with a pull-through if required, but it has simplified many of these repairs. We started by placing a balloon catheter (most of the times a Foley one using a catheter as a guide) in the vagina with a cystoscope. The principle consists of placing a Fogarty balloon catheter into the vagina cystoscopically to locate it by palpation deep in the perineum later. The short vagina (which is usually the case in these patients) needed to be exteriorized. The urogenital sinus is mobilized en bloc to the perineum, after it is incised in the ventral wall. Most of them are undervirilized males, and a bowel vagina (colon if possible) is preferred. It is essential to evaluate the effects of early versus later surgery in a holistic manner, recognizing the difficulties posed by an ever-evolving clinical practice. Nevertheless, outcomes from clitoroplasty identify problems related to decreased sexual sensitivity, loss of clitoral tissue, and cosmetic issues. Analysis of long-term outcomes is complicated by a mixture of surgical techniques. The operations we performed have not compromised urinary continence as also previously observed by others. Feminizing genitoplasty as opposed to masculinizing genitoplasty requires less surgery to achieve an acceptable outcome and results in fewer urologic difficulties. Long-term data regarding sexual function and quality of life among those assigned female as well as male show great variability. There are no controlled clinical trials of the efficacy of early (12 months of age) versus late (adolescence and adulthood) surgery or of the efficacy of different techniques. Gender-role change occurs at different rates in different societies, suggesting that social factors may also be important modifiers of gender-role change. Postoperative: the perineum needs to be kept dry and clean for the first week to prevent dehiscence. The risks from vaginoplasty are different for high and low confluence of the urethra and vagina. A midline sagittal incision was made through the anterior anorectal wall and provided an excellent view of the complete urethra and vagina without the need for complex preparation to gain exposure. In this patient, a previous placing of a balloon catheter in the vagina and a total urogenital mobilization were performed in the lithotomy position, and the patient was then turned to prone position. Total mobilization of the urogenital sinus for the treatment of adrenal hyperplasia. Gender dysphoria and gender change in chromosomal females with congenital adrenal hyperplasia. Corporeal sparing dismembered clitoroplasty: An alternative technique for feminizing genitoplasty. Anterior sagittal transanorectal approach to the posterior urethra in the pediatric age group. Understanding these anomalies requires detailed knowledge of the embryology, and particularly the central roles of androgens (in coordinating the masculinization of the anatomy) and formation of the processus vaginalis (which allows descent of the intra-abdominal fetal testis into the scrotum). The endodermal urethral plate canalizes and the inner genital folds fuse to create the male anterior urethra and corpus spongiosum, while the fused outer genital folds make the scrotum. The first phase involves enlargement of the genitoinguinal ligament (or "gubernaculum") and regression of the cranial suspensory ligament. The swollen distal gubernaculum anchors the embryonic testis near the groin during enlargement of the abdominal cavity. The hormonal regulation of this enlargement is by Leydig insulin-like hormone3 (Insl3). Gubernacular migration (with elongation of the processus) to the scrotum is likely to be controlled by the genitofemoral nerve releasing calcitonin gene-related peptide, under stimulation of androgen. After migration is complete, the gubernaculum involutes and the tunica vaginalis becomes adherent inside the scrotum, preventing any further risk of extravaginal torsion. Following testicular descent, the proximal processus vaginalis obliterates, leaving the testis within the tunica vaginalis.
Discount prilosec online american express
This makes the dorsal mesenteric root narrow and puts the bowel at risk of midgut volvulus gastritis diet mango cheap 20mg prilosec with amex. The third stage (12th week) is characterized by the retroperitoneal fixation of the duodenum and colon. The cecum passes to the right and downward and becomes fixed to the posterior abdominal wall. Symptoms can occur at any age, but the classical teaching is that the vast majority of patients with malrotation are symptomatic in the first month of life and 90% will present before 1 year of age. However, a study on 2744 cases of intestinal rotation in children up to 17 years of age has shown that only 30% present by 1 month of age, 58% before 1 year of age, and 75% before 5 years of age. Symptomatic infants, instead, may present with signs and symptoms of acute bowel obstruction due to the development of midgut volvulus, which differ according to the age of presentation. Midgut volvulus results in intestinal strangulation, passage of blood per rectum, and shock. As the strangulation progresses to gangrene, perforation, and peritonitis, the abdominal wall shows signs of edema and discoloration. Older infants and children present with chronic episodic obstructive symptoms, failure to thrive, malabsorption, diarrhea, and/or nonspecific colicky abdominal pain. The intestine develops in utero through three stages that occur during the first trimester. If the physical examination and/or the abdominal radiography is indicative of volvulus with high suspicion, Surgery 589 surgery should be expedited. Alternatively, if the patient is stable, further diagnostic imaging is recommended. Upper gastrointestinal contrast study is the gold-standard investigation for patients presenting with signs of proximal bowel. Frequently it is clear; blood-stained fluid implies bowel ischemia and volvulus; fecal staining indicates bowel perforation and should be cultured. The superior mesenteric artery is identified, and the mesenteric base is broadened as much as possible by division of the peritoneal folds. An appendectomy should be performed, due to the abnormal position of the appendix at the end of the surgery (left upper quadrant). However, it is still a matter of debate whether an appendectomy should be performed in neonates. Some surgeons would opt for an inversion of the appendix; others would leave the appendix untouched to prevent potential additional morbidity. At the end of the procedure, the small bowel is placed in the right hemiabdomen and the large bowel in the left hemiabdomen. The author has reported a technique to deal with mesenteric thrombosis, which causes continuing ischemia of the intestine. This technique includes the following: (1) digital massage of the superior mesenteric vessels after derotation to restore intestinal perfusion and (2) postoperative systemic infusion of tissue-type plasminogen activator. If extensive ischemic bowel of doubtful viability is present, a second-look laparotomy is performed after 24 h in the hope of minimizing the extent of bowel resection required. On lateral view, the fourth part of the duodenum lies anterior to the second part (D2), occasionally showing a corkscrew appearance. Contrast enema has historically been used, especially to study the position of the cecal pole. Abdominal ultrasonography that demonstrates an abnormal orientation of the mesenteric vessels can also be indicative of intestinal malrotation. In a normal situation, the superior mesenteric vein is located to the right of the superior mesenteric artery. Color Doppler ultrasonography may reveal a "whirlpool sign," which is created when the superior mesenteric vein and the mesentery wrap around the superior mesenteric artery in midgut volvulus. Ancillary ultrasonographic findings suggestive of malrotation are found when looking at the third part of the duodenum: dilatation of the proximal portion indicating obstruction and abnormal position between the superior mesenteric artery and the aorta in the retroperitoneal space are suggestive of malrotation. Computed tomography of the abdomen is commonly used in adults as it also provides information on bowel perfusion. However, this imaging technique should not be employed in infants, children, and adolescents due to the radiation exposure risk. All symptomatic patients with positive investigative findings should undergo urgent laparotomy following a brief period of intensive resuscitation, with crystalloids or 5% human albumin in the form of a bolus (20 mL/kg to repeat as required) and maintenance fluids. Care must be taken to correctly identify landmarks such as the duodenum and ascending colon. To gain access to the duodenum, it is useful to raise the head of the operating table and elevate the right flank. After division, the bowel is examined along its length for any further causes of obstruction. Dividing the peritoneal folds broadens the root of the mesentery, and care must be taken in not injuring the superior mesenteric vein. Intravenous fluids are continued, and gastric losses are replaced milliliter for milliliter with normal saline and potassium chloride (20 mmol/L saline). Malrotation and midgut volvulus: A historical review and current controversies in diagnosis and management. The position of the duodenojejunal junction: the wrong horse to bet on in diagnosing or excluding malrotation. Some degree of nonrotation or malrotation is invariably encountered in these patients, and subsequent volvulus is rare. Asymptomatic patients with malrotation in whom the diagnosis is made incidentally during evaluation for nonspecific complaints, prior to fundoplication for gastroesophageal reflux, and in those with heterotaxy syndromes. This term was created by Laidlaw8 in 1938, and described the histological finding of islet cells proliferating by budding off the pancreatic ductal tissue within pancreases of infants with severe symptoms of hypoglycemia. This results in the calcium channels remaining closed, preventing any calcium influx or consequent insulin release. This outlines the importance of all neonates undergoing blood glucose testing shortly after birth. Perforation may develop antenatally, leading to meconium peritonitis, or may occur as a postnatal event, especially if diagnosis is delayed. The peristaltic movements in the proximal segment are subnormal and ineffective, and histologic and histochemical abnormalities can be observed up to 20 cm cephalad to the atretic segment. The grossly dilated obstructed bowel tapers proximally into intestine of normal calibre. The distal collapsed bowel illustrates how difficult it may be to assess the length of this segment. Up to 38% of patients with proximal jejunal atresia display polyhydramnios, which is less frequent in more distal cases. Many babies with intestinal atresia are diagnosed by ultrasound investigation of the fetus, which shows a dilated, echogenic, and thickened bowel loop with increased peristalsis. Note the precarious blood supply of the terminal portion of the distal bowel and the grossly dilated proximal jejunum. In general, the higher the level of obstruction, the earlier and more forceful the vomiting, whereas in low intestinal obstruction, the vomiting may be delayed. Abdominal distension is frequently present, more so with the distal ileal intestinal atresias, where the distension is generalized, compared with the more proximal jejunal atresias, where it is confined to the upper abdomen and is relieved by nasogastric tube aspiration. In delayed diagnosis or where perforation has occurred, the distension may be severe and associated with respiratory distress. Constipation is usually not absolute, and the meconium passed varies from normal in color to the more common grey plugs of mucus.
Order prilosec us
Esophageal atresia and diaphragmatic hernia the lower segment of the esophagus in patients with esophageal atresia is characterized by an abnormal or absent propulsive peristalsis chronic gastritis recipes buy prilosec online pills. The long acid clearance time may cause already in this age group a chronic esophagitis. A spontaneous normalization of the pathology cannot be expected; therefore, surgical correction is usually necessary. Mechanisms of gastroesophageal reflux in preterm and term infants with reflux disease. Guidelines for evaluation and treatment of gastroesophageal reflux in infants and children: Recommendations of the North American Society for Pediatric Gastroenterology and Nutrition. Gastrooesophageal reflux disease in preterm infants: Current management and diagnostic dilemmas. Although these symptoms usually become clinically evident only in later childhood, vomiting, recurrent respiratory tract infections, as well as failure to thrive are, in small babies, are strong indicators that the underlying pathology is accompanied by a significant reflux problem. These findings support again the hypothesis that pathological reflux is strongly connected with a dysfunction of the regulation centers in Conclusion 533 11. Gastroesophageal reflux disease in infants: How much is predictable with questionnaires, pH-metry, endoscopy and histology Correlation between manometric and roentgenologic findings of diseases of the esophagus in infants and children. Gastro-oesophageal reflux monitoring: Review and consensus report on detection and definitions of acid, non-acid, and gas reflux. Twenty-fourhour esophageal impedance-pH monitoring in healthy preterm neonates: Rate and characteristics of acid, weakly acidic, and weakly alkaline gastroesophageal reflux. Challenges in the diagnosis of gastroesophageal reflux disease in infants and children. The effect of body positioning on gastroesophageal reflux in premature infants: Evaluation by combined impedance and pH monitoring. The effect of thickened-feed interventions on gastroesophageal reflux in infants: Systematic review and meta-analysis of randomized, controlled trials. A systematic review of nonpharmacological and nonsurgical therapies for gastroesophageal reflux in infants. Natural history of infant reflux esophagitis: Symptoms and morphometric histology during one year without pharmacotherapy. Proton pump inhibitors for reflux therapy in infants: Effectiveness determined by impedance pH monitoring. Effect of proton pump inhibition on acid, weakly acid and weakly alkaline gastro-esophageal reflux in children. Are proton pump inhibitors indicated for the treatment of gastroesophageal reflux in infants and children Laparoscopic Nissen fundoplication for gastro-esophageal reflux disease in infants. Surgical treatment of gastroesophageal reflux in children: A combined hospital study of 7467 patients. Reoperation after Nissen fundoplication in children with gastroesophageal reflux: Experience with 130 patients. Comparison of outcomes twelve years after antireflux surgery or omeprazole maintenance therapy for reflux esophagitis. Recurrent gastroesophageal reflux in neurologically impaired patients after fundoplication. Infant apnea and gastroesophageal reflux: A critical review and framework for further investigation. Combined disturbance of respiratory regulation and esophageal function in early infancy. Gastroesophageal reflux and diaphragmatic motility after repair of congenital diaphragmatic hernia. Gastroesophageal reflux in patients treated for congenital diaphragmatic hernia: Short- and long-term evaluation with multichannel intraluminal impedance. Part Gastrointestinal 5 51 52 53 54 55 56 57 58 59 60 61 62 63 64 65 66 67 68 69 Pyloric atresia and prepyloric antral diaphragm Alessio Pini Prato, Vincenzo Jasonni, and Girolamo Mattioli Infantile hypertrophic pyloric stenosis Prem Puri, Balazs Kutasy, and Ganapathy Lakshmanadass Gastric volvulus Alan E. Minkes Duodenal obstruction Yechiel Sweed and Alon Yulevich Intestinal malrotation Augusto Zani and Agostino Pierro Congenital hyperinsulinism Paul R. Millar, Alp Numanoglu, and Sharon Cox Colonic and rectal atresias Tomas Wester Meconium ileus Guido Ciprandi and Massimo Rivosecchi Meconium peritonitis Jose L. Mortell, and Farhan Tareen Mesenteric and omental cysts Benno Ure and Christoph Zoeller Neonatal ascites Prem Puri and Elke Ruttenstock Necrotizing enterocolitis Stephanie C. Saxena and Praveen Mathur 537 543 558 565 571 588 591 597 610 618 624 631 642 648 653 660 667 684 701 536 Gastrointestinal 70 71 72 73 74 Congenital segmental dilatation of the intestine Yoshiaki Takahashi, Yoshinori Hamada, and Tomoaki Taguchi Intussusception Spencer W. Beasley Inguinal hernia Thambipillai Sri Paran and Prem Puri Short bowel syndrome and surgical techniques for the baby with short intestines Michael E. Pathology There are three main different types of pyloric obstruction: (1) type A, pyloric membrane or web; (2) type B, longitudinal segmental atresia. However, some sonographic signs suggest the possibility of significant cutaneous desquamation and blister formation in a fetus, especially when there is positive amniotic acetylcholinesterase coupled with elevated alphafetoprotein. This association is usually fatal during the first few weeks or months of life, even following surgical correction of intestinal obstruction. Preoperative management Usually, newborns are referred to the hospital and admitted within the first 48 hours of life. Preoperative preparation should consist of gastric decompression by nasogastric tube insertion. An intravenous infusion should be started to correct dehydration, electrolyte imbalance, and metabolic alkalosis observed in most cases. Diagnosis A plain x-ray of the abdomen will usually confirm the clinical diagnosis. The radiological diagnosis is based on the identification of three radiological signs: the single gas bubble sign, the absence of beak sign (typical of hypertrophic pyloric stenosis), and the presence of the pyloric dimple sign on a contrast study. The ultrasonographic examination can be helpful and demonstrates the absence of normal pyloric muscle and canal, which is specific for the diagnosis of this entity. For longer atresia, the procedure of choice is excision and end-to-end gastroduodenostomy. Careful exploration and search of other intestinal atresias are performed at this site. A blunt dissecting forceps, which is inserted into the lumen, is useful at this stage. Care must be taken that no inadvertent damage is done to the posterior wall of the stomach or duodenum. The greater length on the gastric side is necessary because of the thicker gastric wall in order to properly align both margins of the incision in the transverse direction. The duodenal lumen is inspected, and a catheter is pushed down to exclude further distal atresias. The abdomen is closed in two layers, and the nasogastric tube is left in the stomach for decompression. A total of about 150 cases have been reported, divided between pediatric and adult age ranges. The authors described a successful and satisfactory outcome and suggested laparoscopy as an alternative option to the conventional laparotomic procedure. Pathology There are three groups of patients: a neonatal group with complete or partial obstruction, a group presenting later in childhood, and a group not diagnosed until later in life. History, presentation, and diagnosis In the neonatal group, nonbilious vomiting is the predominant presenting symptom. Prolonged retention of foreign bodies can lead to the diagnosis is older children. Gastroscopy has recently been noted to be of use in confirming clinical and radiological evidence of the web in Complications Complications are uncommon but include strictures, leakage, adhesions, infections, and bleeding as with any other abdominal surgery.

Purchase cheap prilosec on-line
Normal urinary function requires balanced neurogenic input to bladder and sphincter muscles gastritis diet x1 discount prilosec line, requiring integrated central and peripheral system coordination, which may be disrupted by brain trauma. Even if the bladder is functioning well, the individual must have enough cognition intact to perceive the need to void and plan the steps for successful continent voiding, and 360 Jallo and Loftus, Neurotrauma and Critical Care of the Brain, 2nd Ed. Neurorehabilitation after Brain Injury if unable to accomplish this independently, then the individual must be able to consistently communicate to a provider the need for toileting assistance. Urinary incontinence may lead to complications such as skin breakdown, urinary tract infection, and avoidance of social situations. While indwelling Foley catheters are commonly used in the acute medical setting, they are less desirable in a social setting and can be associated with complications such as trauma to the lower urinary tract and infection. Formal urodynamic studies are rarely indicated, but checking postvoid residuals after catheter removal is essential to monitor for urinary retention particularly in patients who would be unable to communicate lower abdominal discomfort. Timed voids may be an initial management strategy to provide regular bladder emptying as recovery continues and may need to be combined with pharmacotherapy options such as anticholinergic medications (although limited by cognitive and balance side effects in this population). Common complications including gastroparesis, gastric ulcers, cognitive impairment, and nausea compound nutritional deficit. Supplementing with serum protein product evaluations and/or 24-hour urea nitrogen levels can provide useful windows into the nitrogen balance. Bedside swallow evaluations have poor sensitivity, missing up to 40% of "silent" aspirations. Patients who are unsafe to take oral nutrition may require long-term enteral nutrition. Factors such as increased age, tracheostomy tubes, and aphonia are associated with greater risk of requiring a feeding tube. These professionals can also make recommendations for compensatory strategies to improve functional independence with swallowing. Careful fluid and electrolyte management is usually effective in the acute stages; however, more aggressive strategies including oral or intravenous medications may be required. Attention to fluid and salt balance is key to mitigate risk of excessive brain swelling, which may lead to poorer outcomes. With the exception of sodium monitoring, no guidelines exist for the screening of neuroendocrine dysfunction. Patients with concerning symptoms should be screened to determine morning cortisol, thyroid axis, folliclestimulating hormone, luteinizing hormone, testosterone (in men), and estrogen (in women) levels. Although initial screening and management may occur in the primary care setting, some cases may require referral to an experienced neuroendocrinologist. Nonpharmaceutical and pharmaceutical methods are used for management of these behaviors. This caloric expenditure in acute rehabilitation has been estimated at 40 to 69% above premorbid baseline. Patients receiving exclusively oral nutrition are at higher risk for energy and protein deficits. This state occurs in the absence of other physical, medical, or psychiatric causes. Posttraumatic aggression is likely multifactorial that include structural lesions, biochemical imbalance, and environmental factors. Presentation can include motor restlessness with the patient continuously moving between sitting and standing position, dismantling objects/furniture, or screaming. Another measurement tool is the Overt Agitation Severity Scale-modified for Neurorehabilitation, which also reported good reliability. Acute alcohol and opioid withdrawal symptoms can cause the patient to become agitated. The environment should be quiet and calming, with decreased stimuli such as loud monitors, television, and other noises. The general consensus when starting any medication is to always adjust the environment first and then if necessary start medications at the lowest dose and go slow. In acute agitation where patient may be a danger to self and others, sedative neuroleptic (loxapine) and/or benzodiazepine is recommended. Motor restlessness, involuntary yawning, drowsiness, and waning attention over a therapy session may suggest inadequate arousal. Medications used to treat agitation, anxiety/depression, and spasticity such as antiepileptics, antipsychotic, and antispasticity medications can suppress wakefulness and worsen hypoarousal. Nonpharmacological management can include frequent breaks and promoting proper sleep hygiene. Therapists can alternate between challenging and less intense tasks during sessions to prevent worsening fatigue in patients. Other medications that have been used are levodopa/carbidopa, sertraline, modafinil, and pramipexole, but the studies are limited by small sample size. Some screening questionnaires include Beck Depression Inventory, Hamilton Depression Inventory, and Zung Depression Inventory. Selective serotonin reuptake inhibitors, such as sertraline and citalopram, are usually first-line treatments. Educating the patient and family about depression is also important to allow them to feel empowered in the recovery process. Riley found higher rate of depression and stress in caregivers were associated with severe behavior issues. They may also be impulsive, unable to shift flexibly between tasks, or perseverate. Impaired self-awareness is common and may result in the individual asserting unrealistic goals and seeing no purpose for the use of compensatory strategies. Additionally, cognitive issues may be evident in areas of orientation, processing speed, language, visuoperceptual skills, and motor dexterity and/or speed. Language problems may include those in verbal fluency, word finding, confrontational naming, and/or misnaming (paraphasic errors). Other communication-relevant skills may be impacted such as appreciation for subtle social and interpersonal nuances, often referred to as "pragmatics. Rehabilitation services for cognitive deficits are "directed to achieve functional changes by (1) reinforcing, strengthening, or re-establishing previously learned patterns of behavior, or (2) establishing new patterns of cognitive activity or compensatory mechanisms for impaired neurological systems. For instance, "attention process training" demonstrates improvements in attention, memory, and other neuropsychological measures. Interventions to teach time management strategies facilitate compensation for slowed information processing and handling multiple information sources. Provision of categorical, multiple choice, or even phonemic cues may be necessary to retrieve information that was previously encoded. Executive functioning represents a broad cognitive domain that includes abilities of abstraction, reasoning, problem solving and hypothesis testing, foresight and planning, organization, flexibility, initiation, behavioral inhibition, persistence, and self-awareness. Consider a referral to psychiatric services to assess the appropriateness of medication management of emotional or behavioral problems. If uncertain as to whether the etiology of emotional/behavioral problems are neurologic versus psychogenic, referral to a neurologist or neuropsychologist may be indicated. Research has demonstrated that unrelenting stress on the family from caregiving demands, the uncertain course of recovery, and losses in social, emotional, financial, and functional domains place family caregivers at high risk for experiencing psychological distress. One study surmised that even 2 years after injury some families do not realize the full extent of the 364 Jallo and Loftus, Neurotrauma and Critical Care of the Brain, 2nd Ed. Psychological interventions for ambiguous loss focus on family and community-based interventions in which the fundamental goal is to build resiliency and competence. Normalizing the reaction to ambiguous loss mobilizes the family toward accepting a new but more realistic future. Ambiguous loss correlates with the spiritual injuries, the change in perception of self. Often times, rehabilitation programs are not equipped to manage the spiritual challenges a person with brain injury experiences. As such, it is important for psychologists, chaplains, and/or social workers to be integrated into the team and be skilled at discussing ambiguous loss and spiritual injuries. The trajectory of awareness across the first year after traumatic brain injury: the role of biopsychosocial factors. The experience of discharge for patients with an acquired brain injury from the inpatient to the community setting: a qualitative review.

Order prilosec 20mg on line
Histologically gastritis from diet pills buy generic prilosec from india, in the proliferative phase, endothelial hyperplasia with incorporation of H-thymidine and large numbers of mast cells can be observed. Clinical presentations of the various lesions described above overlap considerably. Some, however, remain asymptomatic and are discovered on routine prenatal or postnatal imaging performed for unrelated reasons. The most common presenting features are an abdominal mass, hepatomegaly, and anemia. It is more common in the diffuse type, but has been noted in multifocal and large solitary hemangiomas. Rarely, hemorrhagic shock with or without disseminated intravascular coagulation may follow a rupture of the lesion. Endovascular modalities are now used to outline the vasculature of tumors in a subgroup of infants who present with high-output cardiac failure for whom a high-flow shunt amenable to embolization is suspected. It consists of multifocal and confluent masses of homogenous liver nodules with peripheral enhancement. This can be every 1 to 2 months until the lesion is stable, after which scans can be performed two to three times a year until involution is demonstrated. If there are signs of asymptomatic shunts, a closer follow-up schedule can be implemented. Multifocal lesions have a similar natural history to that of focal lesions and can be similarly observed. The mechanism of propranolol is to hasten tumor involution, reducing cardiac failure and hypothyroidism. Embolization may be required for lesions with large arteriovenous shunts resulting in heart failure. If the diagnosis is unclear, a percutaneous needle biopsy may be necessary to rule out malignancy. In addition to the above, an early consultation with the transplant team should be considered for patients whose disease progresses despite medical management. Response rates in the literature vary, with good responses ranging from 30% to 75% for multifocal and diffuse disease. The duration of therapy is guided by serial imaging and generally ranges from 5 to 8 months. The high content of tubulin in the endothelial cells of hemangiomas makes this tumor particularly sensitive to vincristine. Hemangiomas can derive collaterals from any of the hepatic, phrenic, intercostal, superior mesenteric, or adrenal arteries. It has also been employed to shrink large hemangiomas symptomatic by the mass effect causing caval compression or abdominal compartment syndrome. An angiographic classification has been proposed based on the number of lesions; flow characteristics (high vs low); presence; type of shunt (arteriovenous, arterioportal, or portovenous); and major anomalies of hepatic Benign liver tumors 939 vessels (particularly venous varices). Hemangiomas with extensive portal venous supply are more difficult to treat and may require multiple embolizations. The expertise required to perform and interpret angiography in this group of infants is generally found only in highly specialized referral centers. They used hepatic artery embolization as a second line of treatment, with one death from postoperative hemorrhage among nine patients who underwent surgery. Because these patients may be those most likely to benefit from liver transplantation, early involvement of the transplant team has been advocated if there is a poor response to initial pharmacotherapy. Prospective characterization of patients will further the understanding of these uncommon tumors. About 50% are multicystic, with the intervening myxoid stroma containing fibroblasts, blood vessels and lymphatics, collagen, bile ductules, and islands of hepatocytes. Less commonly, the cysts can be very small and sometimes absent, resulting in a predominantly solid tumor. Mesenchymal hamartomas are usually well circumscribed and are surrounded by a rim of compressed hepatic parenchyma but are devoid of a true capsule. Small satellite lesions at the margins of the tumor have been described and may explain recurrent disease after excision of the main tumor. Aneuploidy has been detected by flow cytometry in two of eight mesenchymal hamartomas in one study. Mesenchymal hamartomas present most commonly as abdominal distention or an upper abdominal mass. Large tumors can cause respiratory distress or compression of the inferior vena cava with distended superficial abdominal veins or lower limb edema. The tumor can be detected on prenatal ultrasound and may cause fetal hydrops, polyhydramnios, and fetal demise. Levels return to normal after tumor removal, but may take up to a year due to liver regeneration. The typical finding of a multiseptated cystic tumor with distinct margins is rarely seen in other pediatric tumors and is diagnostic of a mesenchymal hamartoma. While spontaneous regression has been described, there is a lack of longterm follow-up and the safety of this approach cannot be determined. In the past, recommendations were made for nonradical resection, but there have been reports of late recurrence. Retroperitoneal tumors have been found to extend to involve the liver, porta hepatis, pancreas, and mesentery. Mortality may be as high as 60% for those tumors that involve the retroperitoneum. Areas that do undergo involution often appear as fibrotic and firm capillary malformation. Heparinization is not indicated because of bleeding risk and minimal platelet effects. Should the patient develop hypofibrinogenemia (<100 mg/dL), fresh frozen plasma or cryoprecipitate can be administered. It is an infrequent diagnosis in newborns and has been reported in association with other hepatic lesions of both benign and malignant categories. On microscopic analysis, the proliferating cells are practically identical to the surrounding hepatocytes. The tumors typically have normal accumulation of 99mTc sulfur colloid on liver scintigraphy. In symptomatic patients, where biopsy is nondiagnostic, or On histology, there are sheets or lobules of spindled endothelial cells and dilated lymphatic channels that show aggressive infiltration of normal tissue. Vascular lumens are filled with erythrocytes and hemosiderin suggestive of stasis. Other defining characteristics include an ill-defined and infiltrative tumor penetrating multiple contiguous layers. The tumor has small feeding and draining 942 Hepatic tumors patients in whom the diagnosis of malignancy has not been definitively ruled out, surgical excision is required. The mass is usually hypoechoic on ultrasound but may be hyperechoic; the mass is not typically cystic. In contrast-aided studies, the arterial phase is usually homogeneous in enhancement and the portal phase is hypodense. The common pattern observed is mild signal hypointensity in the T1-weighted images and hyperintensity in the T2-weighted images. Subsequently, complete surgical resection is recommended when technically feasible. Contemporary management has included percutaneous radiofrequency ablation as an additional modality for treatment. Using a 16-gene signature that correlated with the phase of liver development, they established a tight correlation between the stage of hepatic differentiation and clinical behavior-notably, vascular invasion, metastatic spread, and patient survival.