Cheap 100 mg pristiq visa
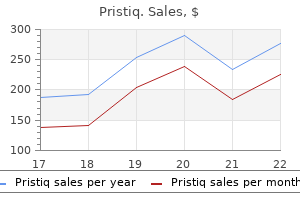
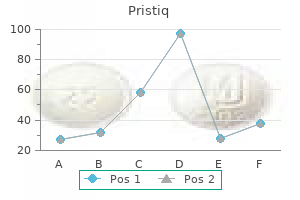
If problem side effects occur symptoms whiplash buy discount pristiq on line, evaluate possibility of tolerance; consider temporary decrease in dose or adjunctive treatment. If unacceptable side effects continue, taper drug over 1 week and initiate new trial; consider potential drug interactions in choice. Evaluate response after 6 weeks at target dose; if response is inadequate, increase dose in stepwise fashion as tolerated. Approximately 40% of primary care patients with depression drop out of treatment and discontinue medication if symptomatic improvement is not noted within a month, unless additional support is provided. A previous response, or a family history of a positive response, to a specific antidepressant often suggests that that drug be tried first. Before initiating antidepressant therapy, the physician should evaluate the possible contribution of comorbid illnesses and consider their specific treatment. In individuals with suicidal ideation, particular attention should be paid to choosing a drug with low toxicity if taken in overdose. The steady-state plasma level achieved for a given drug dose can vary more than 10-fold between individuals, and plasma levels may help in interpreting apparent resistance to treatment and/or unexpected drug toxicity. Ethnic differences in drug metabolism are significant, with Hispanic, Asian, and black patients generally requiring lower doses than whites to achieve a comparable blood level. P450 profiling using genetic chip technology may be clinically useful in predicting individual sensitivity. Second-generation antidepressants are similar to tricyclics in their effect on neurotransmitter reuptake, although some also have specific actions on catecholamine and indolamine receptors as well. Amoxapine is a dibenzoxazepine derivative that blocks norepinephrine and serotonin reuptake and has a metabolite that shows a degree of dopamine blockade. Maprotiline is a potent noradrenergic reuptake blocker that has little anticholinergic effect but may produce seizures. Bupropion is a novel antidepressant whose mechanism of action is thought to involve enhancement of noradrenergic function. It has no anticholinergic, sedating, or orthostatic side effects and has a low incidence of sexual side effects. It may, however, be associated with stimulant-like side effects, may lower seizure threshold, and has an exceptionally short half-life, requiring frequent dosing. Akathisia, involving an inner sense of restlessness and anxiety in addition to increased motor activity, may also be more common, particularly during the first week of treatment. Serotonergic agonists taken in combination should be monitored closely for this reason. Fluoxetine and its principal active metabolite, norfluoxetine, for example, have a combined half-life of almost 7 days, resulting in a delay of 5 weeks before steady-state levels are achieved and a similar delay for complete drug excretion once its use is discontinued. Sexual dysfunction frequently results in noncompliance and should be asked about specifically. Paroxetine appears to be more anticholinergic than either fluoxetine or sertraline, and sertraline carries a lower risk of producing an adverse drug interaction than the other two. Venlafaxine, desvenlafaxine, duloxetine, vilazodone, vortioxetine, and levomilnacipran block the reuptake of both norepinephrine and serotonin but produce relatively little in the way of traditional tricyclic side effects. An extended-release form is available and has a somewhat lower incidence of gastrointestinal side effects. Depending on the specific isoenzyme involved, the metabolism of a number of concomitantly administered medications can be dramatically affected. Fluoxetine and paroxetine, for example, by inhibiting 2D6, can cause dramatic increases in the blood level of type 1C antiarrhythmics, whereas sertraline, by acting on 3A4, may alter blood levels of carbamazepine or digoxin. Common side effects include orthostatic hypotension, weight gain, insomnia, and sexual dysfunction. Electroconvulsive therapy is at least as effective as medication, but its use is reserved for treatment-resistant cases and delusional depressions. Deep brain stimulation and ketamine, a glutamatergic antagonist, are experimental approaches for treatment-resistant cases. Regardless of the treatment undertaken, the response should be evaluated after ~2 months. Three-quarters of patients show improvement by this time, but if remission is inadequate, the patient should be questioned about compliance, and an increase in medication dose should be considered if side effects are not troublesome. If this approach is unsuccessful, referral to a mental health specialist is advised. Strategies for treatment then include selection of an alternative drug, combinations of antidepressants, and/or adjunctive treatment with other classes of drugs, including lithium, thyroid hormone, atypical antipsychotic agents, and dopamine agonists. In patients who have had two or more episodes of depression, indefinite maintenance treatment should be considered. It is essential to educate patients both about depression and the benefits and side effects of medications they are receiving. Advice about stress reduction and cautions that alcohol may exacerbate depressive symptoms and impair drug response are helpful. Patients should be given time to describe their experience, their outlook, and the impact of the depression on them and their families. Occasional empathic silence may be as helpful for the treatment alliance as verbal reassurance. Controlled trials have shown that cognitive-behavioral and interpersonal therapies are effective in improving psychological and social adjustment and that a com- 2717 bined treatment approach is more successful than medication alone for many patients. Some patients suffer only from recurrent attacks of mania, which in its pure form is associated with increased psychomotor activity; excessive social extroversion; decreased need for sleep; impulsivity and impairment in judgment; and expansive, grandiose, and sometimes irritable mood (Table 466-8). In severe mania, patients may experience delusions and paranoid thinking indistinguishable from schizophrenia. One-half of patients with bipolar disorder present with a mixture of psychomotor agitation and activation with dysphoria, anxiety, and irritability. In cyclothymic disorder, there are numerous hypomanic periods, usually of relatively short duration, alternating with clusters of depressive symptoms that fail, either in severity or duration, to meet the criteria of major depression. The mood fluctuations are chronic and should be present for at least 2 years before the diagnosis is made. Manic episodes typically emerge over a period of days to weeks, but onset within hours is possible, usually in the early morning hours. The term rapid cycling is used for patients who have four or more episodes of either depression or mania in a given year. In some cases, rapid cycling is linked to an underlying thyroid dysfunction, and in others, it is iatrogenically triggered by prolonged antidepressant treatment. Approximately one-half of patients have sustained difficulties in work performance and psychosocial functioning, with depressive phases being more responsible for impairment than mania. A distinct period of abnormally and persistently elevated, expansive, or irritable mood and abnormally and persistently increased goal-directed activity or energy, lasting at least 1 week and present most of the day, nearly every day (or any duration if hospitalization is necessary). During the period of the mood disturbance and increased energy or activity, three (or more) of the following symptoms (four if the mood is only irritable) are present to a significant degree and represent a noticeable change from usual behavior: 1. Excessive involvement in activities that have a high potential for painful consequences. The mood disturbance is sufficiently severe to cause marked impairment in social or occupational functioning or to necessitate hospitalization to prevent harm to self or others, or there are psychotic features. Onset is typically between 20 and 30 years of age, but many individuals report premorbid symptoms in late childhood or early adolescence.
Syndromes
- Be selective in the television programs that young children watch (including news broadcasts), which can produce fears and anxiety.
- Cardiac trauma
- Numbness
- Avoid alcohol and caffeine, especially after dinner.
- Eating certain foods?
- Chest x-ray
Pristiq 100 mg without prescription
Hypophosphatemia related to the secondary hyperparathyroidism of vitamin D deficiency usually responds to treatment with vitamin D and calcium alone medications when pregnant cheap pristiq uk. Hemodialysis is the most effective thera- 2461 peutic strategy and should be considered early in the course of severe hyperphosphatemia, especially in the setting of renal failure and symptomatic hypocalcemia. One-half of the 25 g (1000 mmol) of total body magnesium is located in bone, only one-half of which is insoluble in the mineral phase. Almost all extraskeletal magnesium is present within cells, where the total concentration is 5 mM, 95% of which is bound to proteins and other macromolecules. Urinary magnesium excretion normally matches net intestinal absorption and is ~4 mmol/d (100 mg/d). Dietary magnesium deficiency is unlikely except possibly in the setting of alcoholism. A rare genetic disorder that causes selective intestinal magnesium malabsorption has been described (primary infantile hypomagnesemia). Proton pump inhibitors (omeprazole and others) may produce hypomagnesemia by an unknown mechanism that does not involve renal wasting of magnesium. Magnesium depletion is aggravated by metabolic acidosis, which causes intracellular losses as well. Less acute shifts may be seen during rapid bone formation after parathyroidectomy, with treatment of vitamin D deficiency, or with osteoblastic metastases. Large amounts of magnesium may be lost with acute pancreatitis, extensive burns, or protracted and severe sweating and during pregnancy and lactation. Clinical and Laboratory Findings Hypomagnesemia may cause generalized alterations in neuromuscular function, including tetany, tremor, seizures, muscle weakness, ataxia, nystagmus, vertigo, apathy, depression, irritability, delirium, and psychosis. Other electrolyte abnormalities often seen with hypomagnesemia, including hypocalcemia (with hypocalciuria) and hypokalemia, may not be easily corrected unless magnesium is administered as well. Massive exogenous magnesium exposures, usually via the gastrointestinal tract, can overwhelm renal excretory capacity and cause life-threatening hypermagnesemia (Table 423-5). A notable example of this is prolonged retention of even normal amounts of magnesium-containing cathartics in patients with intestinal ileus, obstruction, or perforation. Clinical and Laboratory Findings the most prominent clinical manifestations of hypermagnesemia are vasodilation and neuromuscular blockade, which may appear at serum magnesium concentrations >2 mmol/L (>4 meq/L; >4. Hypotension that is refractory to vasopressors or volume expansion may be an early sign. Nausea, lethargy, and weakness may progress to respiratory failure, paralysis, and coma, with hypoactive tendon reflexes, at serum magnesium levels >4 mmol/L. Vitamin D is synthesized in the skin in response to ultraviolet radiation and also is absorbed from the diet. Cutaneous production of vitamin D is decreased by melanin and high solar protection factor sunblocks, which effectively impair skin penetration by ultraviolet light. The increased use of sunblocks in North America and Western Europe and a reduction in the magnitude of solar exposure of the general population over the last several decades has led to an increased reliance on dietary sources of vitamin D. In the United States and Canada, these sources largely consist of fortified cereals and dairy products, in addition to fish oils and egg yolks. Use of magnesium-free cathartics or enemas may be helpful in clearing ingested magnesium from the gastrointestinal tract. Vitamin D and its metabolites are hormones and hormone precursors rather than vitamins, since in the proper biologic setting, they can be synthesized endogenously. Impairment of this recirculation, which is seen with diseases of the terminal ileum, leads to accelerated losses of vitamin D metabolites. In normal physiologic circumstances, these other metabolites are not thought to stimulate receptor-dependent actions. This hormone is a major inducer of calbindin 9K, a calcium-binding protein expressed in the intestine, which is thought to play an important role in the active transport of calcium across the enterocyte. In addition to being present in the trophoblastic layer of the placenta, the 1-hydroxylase is produced by macrophages associated with granulomas and lymphomas. The elderly and nursing home residents are particularly at risk for vitamin D deficiency, since both the efficiency of vitamin D synthesis in the skin and the absorption of vitamin D from the intestine decline with age. Similarly, intestinal malabsorption of dietary fats and short bowel syndrome, including that associated with intestinal bypass surgery, can lead to vitamin D deficiency. In addition to intestinal diseases, accelerated inactivation of vitamin D metabolites can be seen with drugs that induce hepatic cytochrome P450 mixed-function oxidases such as barbiturates, phenytoin, and rifampin. Impaired 25-hydroxylation, associated with severe liver disease or isoniazid, is an uncommon cause of vitamin D deficiency. A mutation in the gene responsible for 25-hydroxylation has been identified in one kindred. Thus, therapeutic interventions should be considered in patients whose creatinine clearance is <0. This autosomal recessive disorder presents with the syndrome of vitamin D deficiency in the first year of life. Because the receptor mutation results in hormone resistance, daily calcium and phosphorus infusions may be required to bypass the defect in intestinal mineral ion absorption. Mild to moderate vitamin D deficiency is asymptomatic, whereas long-standing vitamin D deficiency results in hypocalcemia accompanied by secondary hyperparathyroidism, impaired mineralization of the skeleton (osteopenia on x-ray or decreased bone mineral density), and proximal myopathy. Vitamin D deficiency also has been shown to be associated with an increase in overall mortality, including cardiovascular causes. In the absence of an intercurrent illness, the hypocalcemia associated with long-standing vitamin D deficiency rarely presents with acute symptoms of hypocalcemia such as numbness, tingling, and seizures. Rickets and Osteomalacia In children, before epiphyseal fusion, vitamin D deficiency results in growth retardation associated with an expansion of the growth plate known as rickets. The proliferation and differentiation of the chondrocytes in the rachitic growth plate are normal, and the expansion of the growth plate is a consequence of impaired apoptosis of the late hypertrophic chondrocytes, an event that precedes replacement of these cells by osteoblasts during endochondral bone formation. Investigations in murine models demonstrate that hypophosphatemia, which in vitamin D deficiency is a consequence of secondary hyperparathyroidism, is a key etiologic factor in the development of the rachitic growth plate. Osteomalacia is also a feature of long-standing hypophosphatemia, which may be a consequence of renal phosphate wasting or chronic use of etidronate or phosphatebinding antacids. This hypomineralized matrix is biomechanically inferior to normal bone; as a result, patients with vitamin D deficiency are prone to bowing of weight-bearing extremities and skeletal fractures. Vitamin D and calcium supplementation have been shown to decrease the incidence of hip fracture among ambulatory nursing home residents in France, suggesting that undermineralization of bone contributes significantly to morbidity in the elderly. Proximal myopathy is a striking feature of severe vitamin D deficiency both in children and in adults. Although vitamin D deficiency is the most common cause of rickets and osteomalacia, many disorders lead to inadequate mineralization of the growth plate and bone. Calcium deficiency without vitamin D deficiency, the disorders of vitamin D metabolism previously discussed, and hypophosphatemia can all lead to inefficient mineralization. Because alkaline phosphatase is necessary for normal mineral deposition, probably because the enzyme can hydrolyze inhibitors of mineralization such as inorganic pyrophosphate, genetic inactivation of the alkaline phosphatase gene (hereditary hypophosphatasia) also can lead to osteomalacia in the setting of normal calcium and phosphate levels. Vitamin D deficiency leads to impaired intestinal absorption of calcium, resulting in decreased serum total and ionized calcium values. This hypocalcemia results in secondary hyperparathyroidism, a homeostatic response that initially maintains serum calcium levels at the expense of the skeleton. This results in hypophosphatemia, which exacerbates the mineralization defect in the skeleton. Paradoxically, levels of this hormone are often normal in severe vitamin D deficiency.
Order pristiq 50 mg without prescription
Remodeling of bone is accomplished by two distinct cell types: osteoblasts produce bone matrix symptoms urinary tract infection buy line pristiq, and osteoclasts resorb the matrix. The noncollagenous portion of the organic matrix is heterogeneous and contains serum proteins such as albumin as well as many locally produced proteins, whose functions are incompletely understood. Transcription factors and other markers specific for various stages of development are depicted below the arrows. As an osteoblast secretes matrix, which then is mineralized, the cell becomes an osteocyte, still connected with its blood supply through a series of canaliculi. They are thought to be the mechanosensors in bone that communicate signals to surface osteoblasts and their progenitors through the canalicular network and thereby serve as master regulators of bone formation and resorption. Mineralization of the matrix, both in trabecular bone and in osteones of compact cortical bone (Haversian systems), begins soon after the matrix is secreted (primary mineralization) but is not completed for several weeks or even longer (secondary mineralization). Although this mineralization takes advantage of the high concentrations of calcium and phosphate, already near saturation in serum, mineralization is a carefully regulated process that is dependent on the activity of osteoblast-derived alkaline phosphatase, which probably works by hydrolyzing inhibitors of mineralization. Runx2 is a transcription factor expressed specifically in chondrocyte (cartilage cells) and osteoblast progenitors as well as in hypertrophic chondrocytes and mature osteoblasts. Runx2-deficient mice are devoid of osteoblasts, whereas mice with a deletion of only one allele (Runx2 +/-) exhibit a delay in formation of the clavicles and some cranial bones. The latter abnormalities are similar to those in the human disorder cleidocranial dysplasia, which is also caused by heterozygous inactivating mutations in Runx2. The paracrine signaling molecule, Indian hedgehog (Ihh), also plays a critical role in osteoblast development, as evidenced by Ihh-deficient mice that lack osteoblasts in the type of bone formed on a cartilage mold (endochondral ossification). Signals originating from members of the wnt (wingless-type mouse mammary tumor virus integration site) family of paracrine factors are also important for osteoblast proliferation and differentiation. Resorption of bone is carried out mainly by osteoclasts, multinucleated cells that are formed by fusion of cells derived from the common precursor of macrophages and osteoclasts. Thus, these cells derive from the hematopoietic lineage, quite different from the mesenchymal cells that become osteoblasts. Factors produced by osteoblasts or marrow stromal cells allow osteoblasts to control osteoclast development and activity. The process of bone remodeling is initiated by contracblasts; actions on all these cells serve to tion of the lining cells and the recruitment of osteoclast precursors. These precursors fuse to form decrease osteoclast number and decrease multinucleated, active osteoclasts that mediate bone resorption. Osteoclasts adhere to bone and subsequently remove it by acidification and proteolytic digestion. After osteoid mineralization, osteoblasts flatten and form a layer of lining cells over new are attached through a specific v3 inte- bone. The osteoclast forms the response of bone to fractures, infection, and interruption of a tight seal to the underlying matrix and secretes protons, chloride, and proteinases into a confined space that has been likened to an extracel- blood supply and to expanding lesions is relatively limited. In injuries that disrupt the organization of the tissue such as a within the osteoclast generates the needed protons. The bone matrix fracture in which apposition of fragments is poor or when motion is resorbed in the acid environment adjacent to the ruffled border by exists at the fracture site, progenitor stromal cells recapitulate the endochondral bone formation of early development and form cartiproteases, such as cathepsin K, that act at low pH. In the embryo and the growing child, bone develops mostly by lage that is replaced by bone and, variably, fibrous tissue. When there remodeling and replacing previously calcified cartilage (endochon- is good apposition with fixation and little motion at the fracture site, dral bone formation) or, in a few bones, is formed without a cartilage repair occurs predominantly by formation of new bone without other matrix (intramembranous bone formation). Remodeling of bone occurs along lines of force generated by bone formation, chondrocytes proliferate, secrete and mineralize a matrix, enlarge (hypertrophy), and then die, enlarging bone and pro- mechanical stress. The signals from these mechanical stresses are viding the matrix and factors that stimulate endochondral bone for- sensed by osteocytes, which transmit signals to osteoclasts and osteomation. Mechanical forces suppress sclerostin production and thus increase bone formation by osteohormones, such as growth hormone, glucocorticoids, and estrogen. In long bones, deposition of lamellar bone in action of cells with each other and with the environment. Measurement of the products of osteoblast and osteoclast activa concentric arrangement around blood vessels forms the Haversian systems. Growth in length of bones is dependent on proliferation of ity can assist in the diagnosis and management of bone diseases. Osteoblast activity can be assessed by measuring serum bone-specific Growth in width and thickness is accomplished by formation of alkaline phosphatase. Similarly, osteocalcin, a protein secreted from bone at the periosteal surface and by resorption at the endosteal osteoblasts, is made virtually only by osteoblasts. Osteoclast activity surface, with the rate of formation exceeding that of resorption. After digestion by osteoclasts, these cross-linked peptides remodeling of bone (within Haversian systems as well as along the can be measured both in urine and in blood. Thus, bone is an active bility and serves as a reservoir sometimes needed to maintain extracelmetabolizing tissue that requires an intact blood supply. Skeletal calcium bone resorption and formation is a highly orchestrated process carried accretion first becomes significant during the third trimester of fetal out by the basic multicellular unit, which is composed of a group of life, accelerates throughout childhood and adolescence, reaches a peak osteoclasts and osteoblasts. Ranges of values shown are approximate and were chosen to illustrate certain points discussed in the text. Cytosolic calcium does not play the structural role played by extracellular calcium; instead, it serves a signaling function. The steep chemical gradient of calcium from outside to inside the cell promotes rapid calcium influx through various membrane calcium channels that can be activated by hormones, metabolites, or neurotransmitters, swiftly changing cellular function. Alterations in serum protein concentrations directly affect the total blood calcium concentration even if the ionized calcium concentration remains normal. An algorithm to correct for protein changes adjusts the total serum calcium (in mg/dL) upward by 0. The best practice is to measure blood ionized calcium directly by a method that employs calcium-selective electrodes in acute settings during which calcium abnormalities might occur. Intestinal absorption of ingested calcium involves both active (transcellular) and passive (paracellular) mechanisms. Active calcium transport occurs mainly in the proximal small bowel (duodenum and proximal jejunum), although some active calcium absorption occurs in most segments of the small intestine. This is especially true for weakly dissociable calcium supplements such as calcium carbonate. In fact, large boluses of calcium carbonate are poorly absorbed because of their neutralizing effect on gastric acid. In achlorhydric subjects and for those taking drugs that inhibit gastric acid secretion, supplements should be taken with meals to optimize their absorption. Calcium absorption may also be blunted in disease states such as pancreatic or biliary insufficiency, in which ingested calcium remains bound to unabsorbed fatty acids or other food constituents. This daily load of absorbed calcium is excreted by the kidneys in a manner that is also tightly regulated by the concentration of ionized calcium in the blood. Most filtered calcium (65%) is reabsorbed in the proximal tubules via a passive, paracellular route that is coupled to concomitant NaCl reabsorption and not specifically regulated. It then moves across the cell in association with a specific calcium-binding protein (calbindin-D28k) that buffers cytosolic calcium concentrations from the large mass of transported calcium. Conversely, dietary sodium loads, or increased distal sodium delivery caused by loop diuretics or saline infusion, induce calciuresis. This can cause severe hypercalciuria, nephrocalcinosis, progressive renal failure, and hypercalcemia. Phosphate is widely available in foods and is absorbed efficiently (65%) by the small intestine even in the absence of vitamin D.
Discount pristiq 100 mg
The primary goals are development of a rehabilitation plan framed by realistic expectations and attention to the neurologic treatment 4 pimples buy pristiq 100 mg fast delivery, medical, and psychological complications that commonly arise. Many of the usual symptoms associated with medical illnesses, especially somatic and visceral pain, may be lacking because of the destruction of afferent pain pathways. Unexplained fever, worsening of spasticity, or deterioration in neurologic function should prompt a search for infection, thrombophlebitis, or an intraabdominal pathology. The loss of normal thermoregulation and inability to maintain normal body temperature can produce recurrent fever (quadriplegic fever), although most episodes of fever are due to infection of the urinary tract, lung, skin, or bone. Bladder dysfunction generally results from loss of supraspinal innervation of the detrusor muscle of the bladder wall and the sphincter musculature. Surgical options include the creation of an artificial bladder by isolating a segment of intestine that can be catheterized intermittently (enterocystoplasty) or can drain continuously to an external appliance (urinary conduit). Bladder areflexia due to acute spinal shock or conus lesions is best treated by catheterization. Bowel regimens and disimpaction are necessary in most patients to ensure at least biweekly evacuation and avoid colonic distention or obstruction. Patients with acute cord injury are at risk for venous thrombosis and pulmonary embolism. Use of calf-compression devices and anticoagulation with low-molecular-weight heparin is recommended. In cases of persistent paralysis, anticoagulation should probably be continued for 3 months. Prophylaxis against decubitus ulcers should involve frequent changes in position in a chair or bed, the use of special mattresses, and cushioning of areas where pressure sores often develop, such as the sacral prominence and heels. Early treatment of ulcers with careful cleansing, surgical or enzyme debridement of necrotic tissue, and appropriate dressing and drainage may prevent infection of adjacent soft tissue or bone. Drug treatment is effective but may result in reduced function, as some patients depend on spasticity as an aid to stand, transfer, or walk. In refractory cases, intrathecal baclofen administered via an implanted pump, botulinum toxin injections, or dorsal rhizotomy may be required to control spasticity. Despite the loss of sensory function, many patients with spinal cord injury experience chronic pain sufficient to diminish their quality of life. Randomized controlled studies indicate that gabapentin or pregabalin is useful in this setting. Epidural electrical stimulation and intrathecal infusion of pain medications have been tried with some success. A paroxysmal autonomic hyperreflexia may occur following lesions above the major splanchnic sympathetic outflow at T6. Headache, flushing, and diaphoresis above the level of the lesion, as well as hypertension with bradycardia or tachycardia, are the major symptoms. The trigger is typically a noxious stimulus-for example, bladder or bowel distention, a urinary tract infection, or a decubitus ulcer-below the level of the cord lesion. Treatment consists of removal of offending stimuli; ganglionic blocking agents (mecamylamine, 2. Attention to these details allows longevity and a productive life for patients with complete transverse myelopathies. Almost 10 million head injuries occur annually in the United States, about 20% of which are serious enough to cause brain damage. Among men <35 years, accidents, usually motor vehicle collisions, are the chief cause of death and >70% of these involve head injury. Ropper Almost 10 million head injuries occur annually in the United States, about 20% of which are serious enough to cause brain damage. Furthermore, minor head injuries are so common that almost all physicians will be called upon to provide immediate care or to see patients who are suffering from various sequelae. Medical personnel caring for head injury patients should be aware that (1) spinal injury often accompanies head injury, and care must be taken in handling the patient to prevent compression of the spinal cord due to instability of the spinal column; (2) intoxication is frequently associated with traumatic brain injury, and thus testing for drugs and alcohol should be carried out when appropriate; and (3) additional injuries, including rupture of abdominal organs, may produce vascular collapse, shock, or respiratory distress that requires immediate attention. The mechanisms by which a blast injury affects the brain and causes symptoms that are associated with concussion, a problem mainly in military medicine, are not known. The energy of a blast wave can enter the cranium through the openings of the orbits, auditory canals, and foramen magnum. There are not consistent changes in cerebral imaging studies but more subtle indications of tissue disruption have been found, comparable to those of mild concussion. It has been difficult to separate the direct effects of the blast from the consequences of being thrown against fixed objects or injured by flying debris. A surface bruise of the brain, or contusion, consists of varying degrees of petechial hemorrhage, edema, and tissue destruction. Contusions and deeper hemorrhages result from mechanical forces that displace and compress the hemispheres forcefully and by deceleration of the brain against the inner skull, either under a point of impact (coup lesion) or, as the brain swings back, in the antipolar area (contrecoup lesion). Trauma sufficient to cause prolonged unconsciousness usually produces some degree of contusion. Blunt deceleration impact, as occurs against an automobile dashboard or from falling forward onto a hard surface, causes contusions on the orbital surfaces of the frontal lobes and the anterior and basal portions of the temporal lobes. With lateral forces, as from impact on an automobile door frame, contusions are situated on the lateral convexity of the hemisphere. The clinical signs of contusion are determined by the location and size of the lesion; often, there are no focal neurologic abnormalities, but these injured regions are later the sites of gliotic scars that may produce seizures. A hemiparesis or gaze preference is fairly typical of moderately sized contusions. Large bilateral contusions produce stupor with extensor posturing, while those limited to the frontal lobes cause a taciturn state. Contusions in the temporal lobe may cause delirium or an aggressive, combative syndrome. Over a few days, contusions acquire a surrounding contrast enhancement and edema that may be mistaken for tumor or abscess. Glial and macrophage reactions result in chronic, scarred, hemosiderin-stained depressions on the cortex (plaques jaunes) that are the main source of posttraumatic epilepsy. Many patients, however, do not lose consciousness after a minor head injury but instead are dazed or confused, or feel stunned or "star struck," and the term concussion is now applied to all such cognitive and perceptual changes experienced after a blow to the head. Severe concussion may precipitate a brief convulsion or autonomic signs such as facial pallor, bradycardia, faintness with mild hypotension, or sluggish pupillary reaction, but most patients quickly return to a neurologically normal state. The mechanics of a typical concussion involve sudden deceleration of the head when hitting a blunt stationary object. This creates an anterior-posterior movement of the brain within the skull due to inertia and rotation of the cerebral hemispheres on the fulcrum of the relatively fixed upper brainstem. Loss of consciousness in concussion is believed to result from a transient electrophysiologic dysfunction of the reticular activating system in the upper midbrain that is at the site of rotation (Chap. The transmission of a wave of kinetic energy throughout the brain is an alternative explanation for the disruption in consciousness. A brief period of both retrograde and anterograde amnesia is characteristic of concussion, and it recedes rapidly in alert patients. Memory loss spans the moments before impact but may encompass the previous days or weeks (rarely months). With severe injuries, the extent of retrograde amnesia roughly correlates with the severity of injury. Memory is regained erratically from the most distant to more recent memories, with islands of amnesia occasionally remaining. Noncontrast computed tomography scan demonstrating a hyperdense hemorrhagic region in the anterior temporal lobe. These appear to reflect an extreme type of the diffuse axonal shearing lesions that occur with closed head injury. Torsional or shearing forces within the brain cause hemorrhages of the basal ganglia and other deep regions.
Order cheap pristiq online
Focal perimetry and tangent screen examinations should be used to map out visual field defects fully or to search for subtle abnormalities medications 8 rights purchase 100mg pristiq amex. Optic fundi should be examined with an ophthalmoscope, and the color, size, and degree of swelling or elevation of the optic disc noted, as well as the color and texture of the retina. The retinal vessels should be checked for size, regularity, arteriovenous nicking at crossing points, hemorrhage, exudates, etc. To check extraocular movements, ask the patient to keep his or her head still while tracking the movement of the tip of your finger. Move the target slowly in the horizontal and vertical planes; observe any paresis, nystagmus, or abnormalities of smooth pursuit (saccades, oculomotor ataxia, etc. If necessary, the relative position of the two eyes, both in primary and multidirectional gaze, can be assessed by comparing the reflections of a bright light off both pupils. However, in practice it is typically more useful to determine whether the patient describes diplopia in any direction of gaze; true diplopia should almost always resolve with one eye closed. As with other parts of the sensory examination, testing of two sensory modalities derived from different anatomic pathways. Look in particular for differences in the lower versus upper facial muscles; weakness of the lower two-thirds of the face with preservation of the upper third suggests an upper motor neuron lesion, whereas weakness of an entire side suggests a lower motor neuron lesion. Further testing for air versus mastoid bone conduction (Rinne) and lateralization of a 512-Hz tuning fork placed at the center of the forehead (Weber) should be done if an abnormality is detected by history or examination. The pharyngeal ("gag") reflex is evaluated by stimulating the posterior pharyngeal wall on each side with a sterile, blunt object. Assess upper extremity strength by checking for pronator drift and strength of wrist or finger extensors. Assess lower extremity strength by checking strength of the toe extensors and having the patient walk normally and on heels and toes. The motor examination includes observations of muscle appearance, tone, and strength. Although gait is in part a test of motor function, it is usually evaluated separately at the end of the examination. Appearance Inspect and palpate muscle groups under good light and with the patient in a comfortable and symmetric position. Tone Muscle tone is tested by measuring the resistance to passive movement of a relaxed limb. Patients often have difficulty relaxing during this procedure, so it is useful to distract the patient to minimize active movements. In the upper limbs, tone is assessed by rapid pronation and supination of the forearm and flexion and extension at the wrist. Decreased tone is most commonly due to lower motor neuron or peripheral nerve disorders. Increased tone may be evident as spasticity (resistance determined by the angle and velocity of motion; corticospinal tract disease), rigidity (similar resistance in all angles of motion; extrapyramidal disease), or paratonia (fluctuating changes in resistance; frontal lobe pathways or normal difficulty in relaxing). Cogwheel rigidity, in which passive motion elicits jerky interruptions in resistance, is seen in parkinsonism. Strength Testing for pronator drift is an extremely useful method for screening upper limb weakness. The patient is asked to hold both arms fully extended and parallel to the ground with eyes closed. This position should be maintained for ~10 s; any flexion at the elbow or fingers or pronation of the forearm, especially if asymmetric, is a sign of potential weakness. Muscle strength is further assessed by having the patient exert maximal effort for the particular muscle or muscle group being tested. Muscle strength is traditionally graded using the following scale: 0 = no movement 1 = flicker or trace of contraction but no associated movement at a joint 2 = movement with gravity eliminated 3 = movement against gravity but not against resistance 4- = movement against a mild degree of resistance 4 = movement against moderate resistance 4+ = movement against strong resistance 5 = full power However, in many cases, it is more practical to use the following terms: Paralysis = no movement Severe weakness = movement with gravity eliminated Moderate weakness = movement against gravity but not against mild resistance Mild weakness = movement against moderate resistance Full strength Noting the pattern of weakness is as important as assessing the magnitude of weakness. Unilateral or bilateral weakness of the upper limb extensors and lower limb flexors ("pyramidal weakness") suggests a lesion of the pyramidal tract, bilateral proximal weakness suggests myopathy, and bilateral distal weakness suggests peripheral neuropathy. Muscle Stretch Reflexes Those that are typically assessed include the biceps (C5, C6), brachioradialis (C5, C6), and triceps (C7, C8) reflexes in the upper limbs and the patellar or quadriceps (L3, L4) and Achilles (S1, S2) reflexes in the lower limbs. The patient should be relaxed and the muscle positioned midway between full contraction and extension. Reflexes may be enhanced by asking the patient to voluntarily contract other, distant muscle groups (Jendrassik maneuver). For example, upper limb reflexes may be reinforced by voluntary teeth-clenching, and the Achilles reflex by hooking the flexed fingers of the two hands together and attempting to pull them apart. For each reflex tested, the two sides should be tested sequentially, and it is important to determine the smallest stimulus required to elicit a reflex rather than the maximum response. Reflexes are graded according to the following scale: 0 = absent 1 = present but diminished 2 = normoactive 3 = exaggerated 4 = clonus Cutaneous Reflexes the plantar reflex is elicited by stroking, with a noxious stimulus such as a tongue blade, the lateral surface of the sole of the foot beginning near the heel and moving across the ball of the foot to the great toe. With upper motor neuron lesions above the S1 level of the spinal cord, a paradoxical extension of the toe is observed, associated with fanning and extension of the other toes (termed an extensor plantar response, or Babinski sign). However, despite its popularity, the reliability and validity of the Babinski sign for identifying upper motor neuron weakness is limited-it is far more useful to rely on tests of tone, strength, stretch reflexes, and coordination. Superficial abdominal reflexes are elicited by gently stroking the abdominal surface near the umbilicus in a diagonal fashion with a sharp object. They are most helpful when there is preservation of the upper (spinal cord level T9) but not lower (T12) abdominal reflexes, indicating a spinal lesion between T9 and T12, or when the response is asymmetric. Other useful cutaneous reflexes include the cremasteric (ipsilateral elevation of the testicle following stroking of the medial thigh; mediated by L1 and L2) and anal (contraction of the anal sphincter when the perianal skin is scratched; mediated by S2, S3, S4) reflexes. It is particularly important to test for these reflexes in any patient with suspected injury to the spinal cord or lumbosacral roots. Primitive Reflexes With disease of the frontal lobe pathways, several primitive reflexes not normally present in the adult may appear. The suck response is elicited by lightly touching with a tongue blade the center of the lips, and the root response the corner of the lips; the patient will move the lips to suck or root in the direction of the stimulus. The palmomental response is contraction of the mentalis muscle (chin) ipsilateral to a scratch stimulus diagonally applied to the palm. Evaluating sensation is usually the most unreliable part of the examination because it is subjective and is difficult to quantify. In the compliant and discerning patient, the sensory examination can be extremely helpful for the precise localization of a lesion. With patients who are uncooperative or lack an understanding of the tests, it may be useless. For example, in spinal cord, spinal root, or peripheral nerve abnormalities, all major sensory modalities should be tested while looking for a pattern consistent with a spinal level and dermatomal or nerve distribution. In patients with lesions at or above the brainstem, screening the primary sensory modalities in the distal extremities along with tests of "cortical" sensation is usually sufficient. The five primary sensory modalities-light touch, pain, temperature, vibration, and joint position-are tested in each limb. Vibration is tested using a 128-Hz tuning fork applied to the distal phalanx of the great toe or index finger just below the nail bed. The patient is asked to stand with the feet as close together as necessary to maintain balance while the eyes are open, and the eyes are then closed. With a parietal lobe lesion, the patient may be unable to identify the stimulus on the contralateral side when both hands are touched. Other modalities relying on the parietal cortex include the discrimination of two closely placed stimuli as separate (two-point discrimination), identification of an object by touch and manipulation alone (stereognosis), and the identification of numbers or letters written on the skin surface (graphesthesia). Even simple acts require cooperation of agonist and antagonist muscles, maintenance of posture, and complex servomechanisms to control the rate and range of movements. Part of this integration relies on normal function of the cerebellar and basal ganglia systems. However, coordination also requires intact muscle strength and kinesthetic and proprioceptive information. Rapid alternating movements in the upper limbs are tested separately on each side by having the patient make a fist, partially extend the index finger, and then tap the index finger on the distal thumb as quickly as possible. Another cerebellar test in the lower limbs is the heel-knee-shin maneuver; in the supine position the patient is asked to slide the heel of each foot from the knee down the shin of the other leg.
Prasterone (Dhea). Pristiq.
- Improving ability to achieve an erection in men with sexual dysfunction.
- Improving thinking in healthy older people.
- Improving muscle strength in elderly people.
- Is Dhea effective?
- Dosing considerations for Dhea.
- Improving sexual arousal in healthy women.
- Treating male hormone (androgen) deficiency in women with thyroid disease.
- Are there safety concerns?
- What is Dhea?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96350
Cheap 100 mg pristiq otc
Unfortunately medicine wheel wyoming buy 50mg pristiq, no other reading tests were included, so this study adds little on the reading front to what was already known. This means, of course, that the ability to read low frequency irregular words varies significantly in the normal population, a factor that is very important to take into account when assessing single patients. The standard explanation for surface dyslexia is that regularizations suggest a lack of semantic knowledge, which begs the question: are surface dyslexia and semantic impairments inextricably linked Interestingly, the patients were impaired on non-word reading too, even the relatively mildly impaired cases, although these scores did not correlate significantly with semantic knowledge. The relationship between composite semantic score and low-frequency exception word reading accuracy are impressive with R2 = 0. Repeated observations for each patient are connected by lines to indicate progression over time. Phonological dyslexia Phonological dyslexia-in its Platonic form-serves as a counterpoint to surface dyslexia. He was especially poor on non-words, unable to read any (0/20) of the four or five letter examples correctly. His errors were mainly close phonological non-words, but he did attempt to turn a few into real words. He was able to read suffixed words as well as the other classes of words, but could not read the suffixes alone. This, combined with his ability to read functors, differentiated his reading behavior from that of patients with deep dyslexia (Table 18. In its purest form (an inability to read non-words only) phonological dyslexia looks like a neurological curiosity that should have little, if any, impact on normal reading. An important and as yet still unresolved issue is what is the root cause of phonological dyslexia. The most illuminating study to have examined this question used data from 31 stroke patients. Overall, the phonological composite scores proved to be powerful predictors of written language performance, accounting for 67 per cent of the variance in reading accuracy and 61 per cent of the variance in spelling accuracy. All the patients had a central alexia of a pattern in which both low-frequency exception word and non-word reading were comparably compromised. They found that their phonological error rate significantly correlated with reading performance. The strength of this relationship was similar for low-frequency exception words and non-words, suggesting that reading deficits for these two types of items in this disorder shared a common cause: a progressive impairment of phonological processing. In this case the correlation was a positive one, that is, the better the patients were on a given reading task, the greater their grey matter density. Exception word reading (irregular words, read via the direct or lexical route) correlated with greater internalmedicinebook. Phonological dyslexia and dysgraphia: cognitive mechanisms and neural substrates, pp. Maps of significant correlation are superimposed the 3D rendering of the Montreal Neurological Institute standard brain. Reading disorders in primary progressive aphasia: A behavioral and neuroimaging study, pp. Deep dyslexia Deep dyslexia is related to phonological dyslexia but in its canonical form is clearly different. Patients make semantic errors when reading real words which are striking when they occur. From a 1930 account, the patient was shown the word [Cat] and, after each error, was asked to try again, `Mice. The usual pattern of increasing difficulty that patients with deep dyslexia have, in terms of part-of-speech is: concrete > abstract > functors > nonwords. These phenomena all suggest a problem with the way that the semantic system supports reading in these patients. The underlying assumption seems to be that little change is to be expected in their impairment profile, but this is unlikely to be the case. Friedman pointed this out when she described five patients whose reading evolved from deep to phonological. The patients had all suffered a stroke and were recruited on the basis of demonstrating the following when reading aloud: (a) a lexicality effect, (b) an imageability effect, or (c) production of semantic paralexias. In short, they could find no clear cut-offs between phonological and deep dyslexia. They proposed a two-dimensional space in which acquired dyslexic patients might be found. The peripheral alexias Hemianopic alexia Hemianopic alexia is the most peripheral of the peripheral alexias. These graphs can be conceived of as a set of performance/resource curves with the x-axis reflecting the amount of phonological resources available to the different patient subgroups. Patients with homonymous, hemifield defects that encroach within five degrees of fixation, which the majority do,27 can be expected to have some form of hemianopic alexia; although those with left-sided hemianopias are less likely to be impaired than those with right-sided hemianopias when reading languages that are written (and thus read) from left-to-right. The amount of visual sparing is important as there is a clear, monotonic relationship between this and reading speed. Unlike all the others, visual word form and linguistic processes are preserved, so the various therapies are all based around retraining eye movements. The disorder is selective in the sense that other language functions, including writing, are intact. However, subtle visual deficits have been reported to accompany pure alexia in many patients. Typically, patients read slowly, but can identify most letters, words, and nonwords correctly. In the more severe condition of global alexia, word reading and letter identification is very impaired, and most words and nonwords cannot be identified. Pure alexia is in many ways a simple syndrome: it is the result of focal brain injury, affects only one function (word recognition), and commonly patients have residual function so that reading is not abolished but merely deficient. It would seem, then, that pure alexia should be an easy target for rehabilitation efforts. Unfortunately, it has proven rather difficult to help patients with pure alexia read better. There are a whole host of therapeutic approaches that have been tried with varying success. There are, however, two forms of acquired reading disorders that may result from lesions to the non-dominant hemisphere, or bilateral damage: neglect alexia and attentional alexia. As the names imply, these deficits are thought to reflect attentional dysfunctions, rather than being core reading deficits. Neglect alexia is seen in patients with damage to occipito-parietal areas, most commonly in the right hemisphere. The core symptom of these patients is that they ignore the contralesional (left) side of words and/or text. Neglect alexia is commonly seen in the context of more generalised unilateral neglect syndrome (inattention to contralesional space), but may in some instances be seen as an isolated symptom. The core symptom of attentional alexia, migration errors, is almost never observed in pure alexia. Initially, errors tend to be visual in nature with crowding effects, but as the disease process moves anteriorly, the ventral visual stream can be affected leading to pure alexia-like errors (letter confusability). Their classification mirrors that for reading and depends on both part-of-speech effects (which classes of words are more or less affected), and error types so a patient with phonological dysgraphia will be more likely to make errors on low frequency words or abstract words. One has to be particularly careful in enquiring about premorbid spelling ability before reading too much into mild written errors, as there is good evidence to suggest that writing errors may show up sooner than speaking errors in degenerative disorders. In brief, they propose a form of short-term exaptation47 whereby cultural inventions invade evolutionarily older brain circuits and inherit many of their structural constraints. Small ischemic lesions of this region have been reported as causing acute, seemingly pure, dysgraphia. But one could argue that as well as being linguistically pure, the syndrome must also be differentiated from a general motor output disorder affecting the dominant hand (a patient with a recently fractured dominant hand will be partially agraphic, but not in any clinically meaningful way). With this in mind, the most useful classification is to borrow that from acquired alexia and think about central dysgraphias, where linguistic functions are impaired, (such as phoneme-to-grapheme conversion); and peripheral dysgraphias, where the stages of letter selection and the planning and implementation of the motor movements break down. The peripheral dysgraphias When the stages of letter selection or the planning and implementation of the motor movements involved in writing break down in isolation, then the patient is said to have an isolated peripheral alexia. Some patients have well formed letters but these are produced in the wrong order, have extra elements or transpositions.
Buy 50mg pristiq with mastercard
Patients with large postvoid residual urine volumes are predisposed to infections medications contraindicated in pregnancy buy pristiq 50mg otc. Prevention by urine acidification (with cranberry juice or vitamin C) inhibits some bacteria. Prophylactic administration of antibiotics is sometimes necessary but may lead to colonization by resistant organisms. Fatigue may improve with assistive devices, help in the home, or successful management of spasticity. Patients with frequent nocturia may benefit from anticholinergic medication at bedtime. Cognitive problems may respond to the cholinesterase inhibitor donepezil hydrochloride (10 mg/d). Heat sensitivity may respond to heat avoidance, air-conditioning, or cooling garments. Sexual dysfunction may be helped by lubricants to aid in genital stimulation and sexual arousal. Management of pain, spasticity, fatigue, and bladder/bowel dysfunction may also help. No controlled trials of therapy exist; high-dose glucocorticoids, plasma exchange, and cyclophosphamide have been tried, with uncertain benefit. Longitudinally extensive cord lesion extending over 3 or more vertebral segments 2. Brain magnetic resonance imaging normal or not meeting criteria for multiple sclerosis 3. Seropositive patients have a very high risk for future relapses; more than half will relapse within 1 year if untreated. Aquaporin-4 is localized to the foot processes of astrocytes in close apposition to endothelial surfaces, as well as at paranodal regions near nodes of Ranvier. Postinfectious encephalomyelitis is most frequently associated with the viral exanthems of childhood. Worldwide, measles encephalomyelitis is still common, although use of the live measles vaccine has dramatically reduced its incidence in developed countries. Some patients may have a nonspecific upper respiratory infection or no known antecedent illness. In addition to measles, postvaccinal encephalomyelitis may also follow the administration 2674 of vaccines for smallpox (5 cases per million), the Semple rabies, and Japanese encephalitis. Fever reappears, and headache, meningismus, and lethargy progressing to coma may develop. Lymphocytic pleocytosis, generally 200 cells/L or greater, occurs in 80% of patients. Occasional patients have higher counts or a mixed polymorphonuclear-lymphocytic pattern during the initial days of the illness. Patients who fail to respond within a few days may benefit from a course of plasma exchange or intravenous immunoglobulin. The first goal is accomplished by obtaining a thorough history, neurologic examination, and electrodiagnostic and other laboratory studies. While gathering this information, seven key questions are asked (Table 459-1), the answers to which can usually identify the category of pathology that is present (Table 459-2). If the patient has only weakness without any evidence of sensory or autonomic dysfunction, a motor neuropathy, neuromuscular junction abnormality, or myopathy should be considered. Some peripheral neuropathies are associated with significant autonomic nervous system dysfunction. Symptoms of autonomic involvement include fainting spells or orthostatic lightheadedness; heat intolerance; or any bowel, bladder, or sexual dysfunction (Chap. There will typically be an orthostatic fall in blood pressure without an appropriate increase in heart rate. Autonomic dysfunction in the absence of diabetes should 459 peripheral Neuropathy Anthony A. Diseases can affect the cell body of a neuron or its peripheral processes, namely the axons or the encasing myelin sheaths. Most peripheral nerves are mixed and contain sensory and motor as well as autonomic fibers. Motor axons are usually large myelinated fibers that conduct rapidly (approximately 50 m/s). Large-diameter sensory fibers conduct proprioception and vibratory sensation to the brain, while the smaller-diameter myelinated and unmyelinated fibers transmit pain and temperature sensation. Thus, peripheral neuropathies can impair sensory, motor, or autonomic function, either singly or in combination. Peripheral neuropathies are further classified into those that primarily affect the cell body. These different classes of peripheral neuropathies have distinct clinical and electrophysiologic features. This chapter discusses the clinical approach to a patient suspected of having a peripheral neuropathy, as well as specific neuropathies, including hereditary and acquired neuropathies. Neuropathy Chapter 459 Peripheral Neuropathy History and examination compatible with neuropathy Rarely, a pandysautonomic syndrome can be the only manifestation of a peripheral neuropathy without other motor or sensory findings. Delineating the pattern of weakness, if present, is essential for diagnosis, and in this regard two additional questions should be answered: (1) Does the weakness only involve the distal extremity, or is it both proximal and distal The importance of finding symmetric proximal and distal weakness in a patient who presents with both motor and sensory symptoms cannot be overemphasized because this identifies the important subset of patients who may have a treatable acquired demyelinating neuropathic disorder. Findings of an asymmetric or multifocal pattern of weakness narrow the differential diagnosis. In the absence of sensory symptoms and signs, such weakness evolving over weeks or months would be worrisome for motor neuron disease. The patient may have loss of sensation (numbness), altered sensation to touch (hyperpathia or allodynia), or uncomfortable spontaneous sensations (tingling, burning, or aching) (Chap. Neuropathic pain can be burning, dull, and poorly localized (protopathic pain), presumably transmitted by polymodal C nociceptor fibers, or sharp and lancinating (epicritic pain), relayed by A-delta fibers. A neurologic examination revealing a dramatic loss of proprioception with vibration loss and normal strength should alert the clinician to consider a sensory neuronopathy/ganglionopathy (Table 459-2, Pattern 8). In particular, if this loss is asymmetric or affects the arms more than the legs, this pattern suggests a non-length-dependent process as seen in sensory neuronopathies. If the patient presents with symmetric distal sensory symptoms and signs suggestive of a distal sensory neuropathy, but there is additional evidence of symmetric upper motor neuron involvement (Chap. The most common cause for this pattern is vitamin B12 deficiency, but other causes of combined system degeneration with neuropathy should be considered. It is important to determine the onset, duration, and evolution of symptoms and signs. On examination, the feet may show arch and toe abnormalities (high or flat arches, hammertoes); scoliosis may be present. In suspected cases, it may be necessary to perform both neurologic and electrophysiologic studies on family members in addition to the patient. A final diagnosis is established by using other clues such as the temporal course, presence of other disease states, family history, and information from laboratory studies. The electrophysiologic data provide additional information about the distribution of the neuropathy that will support or refute the findings from the history and physical examination; they can confirm whether the neuropathic disorder is a mononeuropathy, multiple mononeuropathy (mononeuropathy multiplex), radiculopathy, plexopathy, or generalized polyneuropathy. Finally, the electrophysiologic data can help distinguish axonopathies from myelinopathies as well as axonal degeneration secondary to ganglionopathies from the more common length-dependent axonopathies. This is important, because the most likely cause of small-fiber neuropathies, when one is identified, is diabetes mellitus or glucose intolerance. Amyloid neuropathy should be considered as well in such cases, but most of these small-fiber neuropathies remain idiopathic in nature despite extensive evaluation.
Generic 50 mg pristiq visa
Coronal diffusion-weighted image demonstrates high signal intensity indicating restricted diffusion involving the right medial temporal lobe and hippocampus (arrows) as well as subtle involvement of the left inferior temporal lobe (arrowhead) medicine tramadol discount pristiq 100mg overnight delivery. This is most consistent with neuronal death and can be seen in acute infarction as well as encephalitis and other inflammatory conditions. The suspected diagnosis of herpes simplex encephalitis was confirmed by cerebrospinal fluid polymerase chain reaction analysis. Serious injuries have been caused, however, by attraction of ferromagnetic objects into the magnet, which act as missiles if brought too close to the magnet. Likewise, ferromagnetic implants, such as aneurysm clips, may torque within the magnet, causing damage to vessels and even death. Metallic foreign bodies in the eye have moved and caused intraocular hemorrhage; screening for ocular metallic fragments is indicated in those with a history of metal work or ocular metallic foreign bodies. All health care personnel and patients must be screened and educated thoroughly to prevent such disasters because the magnet is always "on. These provide a vascular flow map rather than the anatomic map shown by conventional angiography. Noncontrast computed tomography scan shows one hyperdense lesion in the right hemisphere (arrow). Susceptibility-weighted image shows numerous low-intensity lesions consistent with hemosiderin-laden cavernous malformations (arrow). Slower-flowing blood, as occurs in veins or distal to arterial stenosis, may appear high in signal. However, using special pulse sequences called gradient echo sequences, it is possible to increase the signal intensity of moving protons in contrast to the low signal background intensity of stationary tissue. Proper technique and timing of acquisition relative to bolus arrival are critical for success. It has also proved useful in the noninvasive detection of intracranial aneurysms and vascular malformations. Relative cerebral blood volume, mean transit time, and cerebral blood flow maps are then derived. Delay in mean transit time and reduction in cerebral blood volume and cerebral blood flow are typical of infarction. In the setting of reduced blood flow, a prolonged mean transit time of contrast but normal or elevated cerebral blood volume may indicate tissue supplied by collateral flow that is at risk of infarction. This technique has great potential in the assessment of brain maturation as well as disease entities that undermine the integrity of the white matter architecture. It has proven valuable in preoperative assessment of subcortical white matter tract anatomy prior to brain tumor surgery. Neuronal activity elicits a slight increase in the delivery of oxygenated blood flow to a specific region of activated brain. Further studies will determine whether these techniques are cost effective or clinically useful, but currently, preoperative somatosensory and auditory cortex localization is possible. This technique has proved useful to neuroscientists interested in interrogating the localization of certain brain functions. Increased cerebral flow is more easily identified than slow flow, which can be sometimes difficult to quantify. This technique has also been shown useful in detecting arterial venous shunting in arteriovenous malformations and arteriovenous fistulas. It is also quite sensitive for detecting dying or dead brain tissue secondary to encephalitis, as well as abscess formation. Images are obtained with fat-suppressed fast spin echo imaging or short inversion recovery sequences. Images reveal differences in regional glucose activity among normal and pathologic brain structures. Concerns have been raised that diskography may contribute to an accelerated rate of disk degeneration. ContraindiCations Myelography is relatively safe; however, it should be performed with caution in any patient with elevated intracranial pressure, evidence of a spinal block, or a history of allergic reaction to intrathecal contrast media. If myelography is necessary, only a small amount of contrast medium should be instilled below the lesion in order to minimize the risk of neurologic deterioration. Lumbar puncture is to be avoided in patients with bleeding disorders, including patients receiving anticoagulant therapy, as well as in those with infections of the overlying soft tissues (Chap. A higher incidence is noted among younger women and with the use of larger gauge cutting-type spinal needles. If significant headache persists for longer than 48 h, placement of an epidural blood patch should be considered. Vasovagal syncope may occur during lumbar puncture; it is accentuated by the upright position used during lumbar myelography. Adequate hydration before and after myelography will reduce the incidence of this complication. Intrathecal contrast reactions are rare, but aseptic meningitis and encephalopathy are reported complications. The latter is usually dose related and associated with contrast entering the intracranial subarachnoid space. Risk factors include a preexisting seizure disorder and the use of a total iodine dose of >4500 mg. Other reported complications include hyperthermia, hallucinations, depression, and anxiety states. These side effects have been reduced by the development of nonionic, water-soluble contrast agents as well as by head elevation and generous hydration following myelography. Angiography carries the greatest risk of morbidity of all diagnostic imaging procedures, owing to the necessity of inserting a catheter into a blood vessel, directing the catheter to the required location, injecting contrast material to visualize the vessel, and removing the catheter while maintaining hemostasis. Therapeutic transcatheter procedures (see below) have become important options for the treatment of some cerebrovascular diseases. The decision to undertake a diagnostic or therapeutic angiographic procedure requires careful assessment of the goals of the investigation and its attendant risks. To improve tolerance to contrast agents, patients undergoing angiography should be well hydrated before and after the procedure. Because the femoral route is used most commonly, the femoral artery must be compressed after the procedure to prevent a hematoma from developing. The puncture site and distal pulses should be evaluated carefully after the procedure; complications can include thigh hematoma or lower extremity emboli. CompliCations A common femoral arterial puncture provides retrograde access via the aorta to the aortic arch and great vessels. Thrombus can form on or inside the tip of the catheter, and atherosclerotic thrombus or plaque can be dislodged by the catheter or guide wire or by the force of injection and can embolize distally in the cerebral circulation. Risk factors for ischemic complications include limited experience on the part of the angiographer, atherosclerosis, vasospasm, low cardiac output, decreased oxygen-carrying capacity, advanced age, and prior history of migraine. The risk of a neurologic complication varies but is ~4% for transient ischemic attack and stroke, 1% for permanent deficit, and <0. Ionic contrast media are less well tolerated than nonionic media, probably because they can induce changes in cell membrane electrical potentials. Patients with dolichoectasia of the basilar artery can suffer reversible brainstem dysfunction and acute short-term memory loss during angiography, owing to the slow percolation of the contrast material and the consequent prolonged exposure of the brain. Rarely, an intracranial aneurysm ruptures during an angiographic contrast injection, causing subarachnoid hemorrhage, perhaps as a result of injection under high pressure.
Order pristiq 100 mg otc
Excessive vitamin ingestion can lead to disease; examples include vitamin A and pseudotumor cerebri or pyridoxine and peripheral neuropathy symptoms 3 days after embryo transfer pristiq 50 mg on line. Many patients are unaware that over-the-counter sleeping pills, cold preparations, and diet pills are actually drugs. Alcohol, the most prevalent neurotoxin, is often not recognized as such by patients, and other drugs of abuse such as cocaine and heroin can cause a wide range of neurologic abnormalities. Use the opportunity while taking the history to form an impression of the patient. Are there any clues to problems with language, memory, insight, comportment, or behavior The neurologic assessment begins as soon as the patient comes into the room and the first introduction is made. Mastery of the complete neurologic examination is usually important only for physicians in neurology and associated specialties. However, knowledge of the basics of the examination, especially those components that are effective in screening for neurologic dysfunction, is essential for all clinicians, especially generalists. There is no single, universally accepted sequence of the examination that must be followed, but most clinicians begin with assessment of mental status followed by the cranial nerves, motor system, reflexes, sensory system, coordination, and gait. Whether the examination is basic or comprehensive, it is essential that it be performed in an orderly and systematic fashion to avoid errors and serious omissions. The detailed description that follows describes the more commonly used parts of the neurologic examination, with a particular emphasis on the components that are considered most helpful for the assessment of common neurologic problems. Each section also includes a brief description of the minimal examination necessary to adequately screen for abnormalities in a patient who has no symptoms suggesting neurologic dysfunction. First, in recording observations, it is important to describe what is found rather than to apply a poorly defined medical term. If the complaint is of dizziness when the head is turned in one direction, have the patient do this and also look for associated signs on examination. If pain occurs after walking two blocks, have the patient leave the office and walk this distance and immediately return, and repeat the relevant parts of the examination. The mental status examination is under way as soon as the physician begins observing and speaking with the patient. If the history raises any concern for abnormalities of higher cortical function or if cognitive problems are observed during the interview, then detailed testing of the mental status is indicated. Using age-adjusted values for defining normal performance, the test is ~85% sensitive and 85% specific for making the diagnosis of dementia that is moderate or severe, especially in educated patients. Individual elements of the mental status examination can be subdivided into level of consciousness, orientation, speech and language, memory, fund of information, insight and judgment, abstract thought, and calculations. When the patient is not fully awake, the examiner should describe the responses to the minimum stimulus necessary to elicit a reaction, ranging from verbal commands to a brief, painful stimulus such as a squeeze of the trapezius muscle. Responses that are directed toward the stimulus and signify some degree of intact cerebral function. Orientation is tested by asking the person to state his or her name, location, and time (day of the week and date); time is usually the first to be affected in a variety of conditions. A typical testing sequence is to ask the patient to name successively more detailed components of clothing, a watch, or a pen; repeat the phrase "No ifs, ands, or buts"; follow a three-step, verbal command; write a sentence; and read and respond to a written command. Memory should be analyzed according to three main time scales: (1) immediate memory is assessed by saying a list of three items and having the patient repeat the list immediately; (2) short-term memory is tested by asking the patient to recall the same three items 5 and 15 min later; and (3) long-term memory is evaluated by determining how well the patient is able to provide a coherent chronologic history of his or her illness or personal events. Fund of information is assessed by asking questions about major historic or current events, with special attention to educational level and life experiences. Abnormalities of insight and judgment are usually detected during 2537 the patient interview; a more detailed assessment can be elicited by asking the patient to describe how he or she would respond to situations having a variety of potential outcomes. Abstract thought can be tested by asking the patient to describe similarities between various objects or concepts. With eyes closed, ask the patient to sniff a mild stimulus such as toothpaste or coffee and identify the odorant. As a screening test, it is usually sufficient to examine the visual fields of both eyes simultaneously; individual eye fields should be tested if there is any reason to suspect a problem of vision by the history or other elements of the examination, or if the screening test reveals an abnormality. Instruct the patient to look directly at the center of your face and to indicate when and where he or she sees one of your fingers moving. Beginning with the two inferior quadrants and then the two superior quadrants, move your index finger of the right hand, left hand, or both hands simultaneously and observe whether the patient detects the movements. A single small-amplitude movement of the finger is sufficient for a normal response. Watching the patient walk is the most important part of the neurologic examination. Normal gait requires that multiple systems-including strength, sensation, and coordination-function in a highly integrated fashion. Unexpected abnormalities may be detected that prompt the examiner to return in more detail to other aspects of the examination. The examination may reveal decreased arm swing on one side (corticospinal tract disease), a stooped posture and shortstepped gait (parkinsonism), a broad-based unstable gait (ataxia), scissoring (spasticity), or a high-stepped, slapping gait (posterior column or peripheral nerve disease), or the patient may appear to be stuck in place (apraxia with frontal lobe disease). The laboratory assessment may include (1) serum electrolytes; complete blood count; and renal, hepatic, endocrine, and immune studies; (2) cerebrospinal fluid examination; (3) focused neuroimaging studies (Chap. The anatomic localization, mode of onset and course of illness, other medical data, and laboratory findings are then integrated to establish an etiologic diagnosis. In other patients, an inadequate history may be overcome by a succession of examinations from which the course of the illness can be inferred. In perplexing cases it is useful to remember that uncommon presentations of common diseases are more likely than rare etiologies. Here, the imperative is to rapidly identify patients likely to have nervous system infections, acute strokes, and spinal cord compression or other treatable mass lesions and arrange for immediate care. Lowenstein 438e-1 Chapter 438e the Neurologic Screening Exam Knowledge of the basic neurologic examination is an essential clinical skill. Although the components of the examination may appear daunting at first, skills usually improve rapidly with repetition and practice. In this video, the technique of performing a simple and efficient screening examination is presented. Samuels 439e-1 Chapter 439e Video Atlas of the Detailed Neurologic Examination the comprehensive neurologic examination is an irreplaceable tool for the efficient diagnosis of neurologic disorders. Mastery of its details requires knowledge of normal nervous system anatomy and physiology combined with personal experience performing orderly and systematic examinations on large numbers of patients and healthy individuals. In the hands of a great clinician, the neurologic examination also becomes a thing of beauty-the pinnacle of the art of medicine. In this video, the most commonly used components of the examination are presented in detail, with a particular emphasis on those elements that are most helpful for assessment of common neurologic problems. In addition, an increasing number of interventional neuroradiologic techniques are available, including angiography catheter embolization, coiling, and stenting of vascular structures, and spine diagnostic and interventional techniques, such as diskography, transforaminal and translaminar epidural and nerve root injections, and blood patches. As the x-ray beam, collimated to the desired slice width, rotates around the patient, it passes through selected regions in the body. The resolution of an image depends on the radiation dose, the detector size, collimation (slice thickness), the field of view, and the matrix size of the display. Single or multiple (from 4 to 320) solid-state detectors positioned opposite to the x-ray source result in multiple slices per revolution of the beam around the patient. The table moves continuously through the rotating x-ray beam, generating a continuous "helix" of information that can be reformatted into various slice thicknesses and planes. The use of iodinated contrast agents carries a small risk of allergic reaction and adds additional expense. The most frequent complications are those associated with use of intravenous contrast agents. While two broad categories of contrast media, ionic and nonionic, are in use, ionic agents have been largely replaced by safer nonionic compounds. Contrast nephropathy may result from hemodynamic changes, renal tubular obstruction and cell damage, or immunologic reactions to contrast agents. A rise in serum creatinine of at least 85 mol/L (1 mg/dL) within 48 h of contrast administration is often used as a definition of contrast nephropathy, although other causes of acute renal failure must be excluded.
Buy pristiq with a visa
Unlike hereditary fructose intolerance medicine jar paul mccartney order pristiq 50mg with visa, this deficiency usually is not associated with an aversion to sweets, and renal tubular and liver functions are normal. Later, avoidance of fasting and elimination of fructose and sucrose from the diet prevent further episodes. A slowly released carbohydrate such as cornstarch is useful for the long-term prevention of hypoglycemia. It is a serious disease with an incidence of 1 in 60,000 and an early onset of symptoms. The newborn infant normally receives up to 40% of caloric intake as lactose (glucose + galactose). Without the transferase, the infant is unable to metabolize galactose 1-phosphate. After the first feeding, infants can present with vomiting, diarrhea, hypotonia, jaundice, and hepatomegaly. Patients with galactosemia are at increased risk for Escherichia coli neonatal sepsis; the onset of sepsis often precedes the diagnosis of galactosemia. The prevalent genetic mutations for each disease may vary in different ethnic populations, but clinical symptoms are remarkably similar and treatment guidelines apply to all populations. The practice of newborn screening should be considered worldwide to intercept the rapid progression of many of these disorders. The most common and clinically important is phenylketonuria (frequency 1:10,000), which is an autosomal recessive disorder characterized by an increased concentration of phenylalanine and its by-products in body fluids and by severe mental retardation if untreated in infancy. The accumulation of phenylalanine inhibits the transport of other amino acids required for protein or neurotransmitter synthesis, reduces synthesis and increases degradation of myelin, and leads to inadequate formation of norepinephrine and serotonin. Phenylalanine is a competitive inhibitor of tyrosinase, a key enzyme in the pathway of melanin synthesis, and accounts for the hypopigmentation of hair and skin. Untreated children with classic phenylketonuria are normal at birth but fail to attain early developmental milestones, develop microcephaly, and demonstrate progressive impairment of cerebral function. Hyperactivity, seizures, and severe intellectual disability are major clinical problems later in life. Electroencephalographic abnormalities; "mousy" odor of skin, hair, and urine (due to phenylacetate accumulation); and a tendency to develop hypopigmentation and eczema complete the devastating clinical picture. In contrast, affected children who are detected and treated at birth show none of these abnormalities. Eight amino acids, referred to as essential, cannot be synthesized by humans and must be obtained from dietary sources. Each amino acid has a unique degradative pathway by which its nitrogen and carbon components are used for the synthesis of other amino acids, carbohydrates, and lipids. The features of inherited disorders of amino acid catabolism are summarized in Table 434e-1. In general, these disorders are named for the compound that accumulates to highest concentration in blood (-emias) or urine (-urias). In the aminoacidopathies, the parent amino acid is found in excess, whereas products in the catabolic pathway accumulate in organic acidemias. Which compound(s) accumulates depends on the site of the enzymatic block, the reversibility of the reactions proximal to the lesion, and the availability of alternative pathways of metabolic "runoff. Five distinct forms of hyperphenylalaninemia, nine forms of homocystinuria, and methylmalonic acidemia are recognized. At the other extreme, complete deficiency of ornithine transcarbamylase is lethal in the untreated neonate. Protein-induced vomiting, neurologic dysfunction, and hyperammonemia occur in many disorders of urea cycle intermediates. Metabolic ketoacidosis, often accompanied by hyperammonemia, is a frequent presenting finding in disorders of branched-chain amino acid metabolism. Some disorders produce focal tissue or organ involvement such as liver disease, renal failure, cutaneous abnormalities, or ocular lesions. The analysis of plasma amino acids (by ion-exchange chromatography), urine organic acids (by gas chromatography/mass spectrometry), and plasma acylcarnitine profile (by tandem mass spectrometry) is commonly used to diagnose and monitor most of these disorders. The clinical manifestations in many of these conditions can be prevented or mitigated if a diagnosis is achieved early and appropriate treatment. For this reason, newborn screening programs seek to identify several of these disorders. Infants with a positive screening test need additional metabolic testing (usually suggested by the newborn screening program) to confirm or exclude the diagnosis. Confirmed cases should be referred to a metabolic center for initiation of therapy. The parents need to be counseled about the recurrence risk of the disease in future pregnancies. In some cases, parents need testing to exclude metabolic alterations seen in carriers for some of these disorders (such as some forms of homocystinuria) or because they might have a disorder themselves (such as glutaric acidemia type 1, methylcrotonyl coenzyme A carboxylase deficiency, or fatty acid oxidation defects). Some metabolic disorders can remain asymptomatic until adult age, presenting only when fasting or severe stress require full activity of affected metabolic pathways to provide energy. For this reason, most newborns in North America, Australia, and Europe are screened by determinations of blood phenylalanine levels. Dietary phenylalanine restriction is usually instituted if blood phenylalanine levels are >360 mol/L (6 mg/dL). Treatment consists of a special diet low in phenylalanine and supplemented with tyrosine, since tyrosine becomes an essential amino acid in phenylalanine hydroxylase deficiency. With therapy, plasma phenylalanine concentrations should be maintained between 120 and 360 mol/L (2 and 6 mg/dL). A number of women with phenylketonuria who have been treated since infancy will reach adulthood and become pregnant. If maternal phenylalanine levels are not strictly controlled before and during pregnancy, their offspring are at increased risk for congenital defects and microcephaly (maternal phenylketonuria). After birth, these children have severe intellectual disability and growth retardation. Pregnancy risks can be minimized by continuing lifelong phenylalanine-restricted diets and assuring strict phenylalanine restriction 2 months prior to conception and throughout gestation. Classic homocystinuria, the most common (frequency 1:200,000), results from reduced activity of cystathionine -synthase. Defects in methyl transfer or in the subsequent metabolism of homocysteine by the pyridoxal phosphate (vitamin B6)dependent cystathionine -synthase increase plasma methionine levels. This occurs through methionine synthase, a reaction requiring methylcobalamin and folic acid. Deficiencies in these enzymes or lack of cofactors is associated with decreased or normal methionine levels. In an alternative pathway, homocysteine can be remethylated by betaine:homocysteine methyl transferase. Some patients develop a marfanoid habitus and radiologic evidence of osteoporosis. Life-threatening vascular complications (affecting coronary, renal, and cerebral arteries) can occur during the first decade of life and are the major cause of morbidity and mortality. Classic homocystinuria can be diagnosed with analysis of plasma amino acids, showing elevated methionine and presence of free homocystine. Treatment consists of a special diet restricted in protein and methionine and supplemented with cystine. Folate and vitamin B12 deficiency should be prevented by adequate supplementation. Betaine is also effective in reducing homocystine levels in pyridoxineunresponsive patients. The other forms of homocystinuria are the result of impaired remethylation of homocysteine to methionine. This can be caused by defective methionine synthase or reduced availability of two essential cofactors, 5-methyltetrahydrofolate and methylcobalamin (methylvitamin B12). Hyperhomocysteinemia refers to increased total plasma concentration of homocysteine with or without an increase in free homocystine (disulfide form). Hyperhomocysteinemia, in the absence of significant homocystinuria, is found in some heterozygotes for the genetic defects noted above or in homozygotes for milder variants.