Purchase aggrenox caps discount
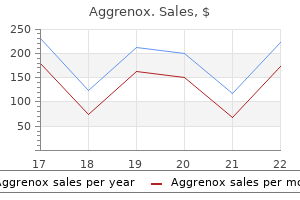
They not only suffer from the effects of radiation on the myocardium that may create a more sustained restrictive effect even after pericardiectomy treatment hemorrhoids quality aggrenox caps 25/200mg, but they also suffer from radiation-induced pulmonary dysfunction. Cardiac tamponade may be easily missed in the early stages as the signs and symptoms are often subtle until reaching a critical state. Decompensated cardiac tamponade is an emergency, requiring either immediate pericardiocentesis or surgical intervention. Tamponade exists when fluid accumulation in the pericardial space dramatically increases intrapericardial pressure and limits filling of the heart. The rate of pericardial fluid accumulation, rather than the absolute fluid volume, is the determinate of tamponade sequelae. One of the reasons for delay in the appreciation of tamponade is the tendency of clinicians to overestimate the sensitivity of clinical signs such as hypotension, pulsus paradoxus, and jugular venous distension. A chest roentogram requires at least 200 mL of fluid to accumulate in the pericardium before the silhouette, known as the water bottle effect, is seen. Pulsus paradoxus may be absent when left ventricular dysfunction, positive pressure breathing, atrial septal defect, or severe aortic regurgitation are present. As diastolic filling begins to disappear, the jugular venous pulse loses a prominent Y descent. A prominent X descent remains by the decrease in intrapericardial pressure that occurs during ventricular ejection. Eventually, the pericardial pressure-volume curve becomes almost vertical, causing any additional pericardial fluid to greatly restrict cardiac filling and to reduce diastolic compliance. Equilibration of these pressures (within 5 mm Hg of each other) merit immediate action to rule out acute tamponade. Echocardiography is the current method of choice and the most reliable noninvasive method to detect pericardial effusion and exclude tamponade. Elevated intrapericardial pressure on the heart during the cardiac cycle is responsible for the hemodynamic changes of cardiac tamponade. Hemodynamic manifestations are primarily due to atrial rather than ventricular compression. Initially with mild tamponade, increased atrial and pericardial pressures limit diastolic filling. Once venous pressure falls below pericardial pressure, the drop in systemic blood pressure is profound and risks inadequate coronary perfusion pressure. Catastrophic hemorrhage can occur suddenly if the atrium or ventricle is perforated, necessitating adequate central venous access. Pericardiectomy via left anterior thoracotomy requires close monitoring of oxygenation because the left lung is severely compressed during dissection. Currently, the anesthetic technique is based on achieving early extubation similar to other cardiac surgical cases, assuming acceptable hemostasis and hemodynamic parameters. Right atrial collapse is a specific finding during echocardiographic examination if it is present for more than one third of the cardiac cycle. Normally, a decrease in intrathoracic pressure during inspiration is transmitted to the pulmonary vasculature and the intrapericardial and intracardiac spaces. In tamponade, this decrease in pressure during inspiration does not occur within the pericardium because of the presence of fluid. Thus the gradient for left-sided filling is decreased, and the early mitral inflow velocity (E velocity) will decrease with inspiration. In addition, right and left ventricular filling display interdependence, similar to that observed in constrictive pericarditis. Echocardiography can also be used to direct needle or catheter placement for pericardiocentesis. Indeed, the bulk of pericardiocentesis is performed under echocardiographic guidance in some centers. Typically, a pigtail catheter is left in the pericardial space for several days until drainage becomes minimal. Failure to recognize the insidious nature of tamponade and to anticipate the progression of hemodynamic changes may lead to a delay in using echocardiography to confirm the diagnosis and begin treatment. Examples include unstable hemodynamics after a penetrating chest injury or an abrupt change in chest tube drainage after cardiac surgery, which should prompt rapid assessment for tamponade and possibly emergency sternal opening. However, the multiple causes of hypotension in the postoperative cardiac surgical patient often complicate the diagnosis. After cardiac surgery, no single clinical, hemodynamic, or echocardiographic finding is sufficient to make a diagnosis of tamponade but requires consideration of the entire clinical picture. Simple arrows represent tamponade sequences; pointed arrowheads represent stimulatory compensatory action; blunt arrowheads represent oppositional compensatory actions. Pericardiocentesis is indicated for life-threatening cardiac tamponade in conjunction with fluid resuscitation to maintain adequate filling pressures. Although pericardiocentesis relieves the symptoms of tamponade, definitive therapy directed at the underlying cause should be pursued. Major complications of pericardiocentesis include coronary artery laceration, cardiac puncture, and pneumothorax. Tamponade attributable to hemorrhage in the patient after cardiac surgery requires immediate mediastinal exploration to determine the source of bleeding and to stabilize hemodynamics. Anesthesia Considerations Severe hypotension or cardiac arrest has followed the induction of general anesthesia in patients with tamponade. The causes include myocardial depression, sympatholysis, decreased venous return, and changes in heart rate that often accompany anesthetic medications and positive pressure ventilation. Pericardiotomy via a subxiphoid incision with only local anesthetic infiltration or light sedation is an option. If intrapericardial injury is confirmed, then general anesthesia can be induced after decompression of the pericardial space. This patient underwent urgent pericardiocentesis under the guidance of echocardiography. On the day of his planned discharge, he was found to have multiple pulmonary emboli and a large lower extremity deep venous thrombosis. Two days later, mechanical extraction of the lower extremity thrombus was undertaken without any known complications. On return to his hospital room after the thrombus extraction, the patient quickly became hemodynamically unstable. He received intravenous fluid administration, however, quickly requiring intubation with mechanical ventilation for respiratory distress. Cardiac arrest resulted, necessitating cardiopulmonary resuscitation and epinephrine administration. He required a period of mechanical ventilation but was ultimately discharged from the hospital in good condition. Combined Carotid and Coronary Artery Disease Patients with concomitant symptomatic coronary and carotid disease are few but a significantly higher risk group than either group of patients with carotid or coronary disease alone. The result is more patients with combined carotid and coronary disease346 but with no consensus regarding their treatment. A large multicenter, randomized trial will be necessary to resolve the management of these patients. Unfortunately, the complexities of such a study with the heterogeneity of patients, varying degrees of coronary and carotid disease, and differing institutional preferences for carotid revascularization decrease its likelihood. Emboli originate primarily from aortic cannulation, aortic cross-clamp release, and cardiac manipulation based on transcranial Doppler ultrasonography. More recently, noninvasive ultrasonography has shown the percentage of persons with severe carotid and coronary disease to be higher than prior studies. In contrast, treatment options for those with active concomitant carotid disease and ischemic heart disease are a combined, synchronous, or staged approach. Without well-defined cardiovascular risks for either the staged or combined approach, the correct decision for the patient is difficult. Individual studies involving concomitant carotid and coronary disease suffer from great variation in the definition of a stroke, selection bias, patient demographics, and surgical techniques that limit the widespread application of study recommendations. To make up for these deficiencies, large systematic reviews of the studies have attempted to provide insight into the optimal practice of concomitant carotid and coronary disease. Others have not only found combined surgery unnecessary but potentially detrimental.
Cheap aggrenox caps 25/200mg free shipping
Using bar-code technology and medication observation methodology for safer medication administration treatment of criminals purchase discount aggrenox caps on line. Severity of medication administration errors detected by a barcode medication administration system. Multimodal system designed to reduce errors in recording and administration of drugs in anaesthesia: prospective randomised clinical evaluation. A system for anesthesia drug administration using barcode technology: the Codonics Safe Label System and Smart Anesthesia Manager. A controlled trial of smart infusion pumps to improve medication safety in critically ill patients. Network computer-assisted transfusion-management system for accurate blood component-recipient identification at the bedside. Improving transfusion safety: implementation of a comprehensive computerized bar code-based tracking system for detecting and preventing errors. Computerized bar code-based blood identification systems and near-miss transfusion episodes and transfusion errors. Psychological sequelae of surgery in a prospective cohort of patients from three intraoperative awareness prevention trials. Bispectral index monitoring to prevent awareness during anaesthesia: the B-Aware randomized controlled trial. The incidence of intra-operative awareness during general anesthesia in China: a multi-center observational study. Intra-operative awareness in children: the value of an interview adapted to their cognitive abilities. Psychological impact of unexpected explicit recall of events occurring during surgery performed under sedation, regional anaesthesia, and general anaesthesia: data from the Anesthesia Awareness Registry. Intraoperative awareness risk, anesthetic sensitivity, and anesthetic management for patients with natural red hair: a matched cohort study. The directionality and functional organization of frontoparietal connectivity during consciousness and anesthesia in humans. Disruption of frontal-parietal communication by ketamine, propofol, and sevoflurane. Cognitive unbinding: a neuroscientific paradigm of general anesthesia and related states of unconsciousness. Isoflurane causes anterograde but not retrograde amnesia for pavlovian fear conditioning. Isoflurane suppresses stress-enhanced fear learning in a rodent model of post-traumatic stress disorder. Increased risk of intraoperative awareness in patients with a history of awareness. Recall of awareness during cardiac anesthesia: influence of feedback information to the anesthesiologist. Bispectral index monitoring to prevent awareness during anaesthesia: the B-Aware randomised controlled trial. Awareness during anesthesia: risk factors, causes and sequelae: a review of reported cases in the literature. Bispectral analysis measures sedation and memory effects of propofol, midazolam, isoflurane, and alfentanil in healthy volunteers. The effect of the interaction of propofol and alfentanil on recall, loss of consciousness, and the bispectral index. Prevention of intraoperative awareness with explicit recall in an unselected surgical population: a randomized comparative effectiveness trial. Clinical effectiveness and cost-effectiveness of depth of anaesthesia monitoring (E-Entropy, bispectral index and Narcotrend): a systematic review and economic evaluation. Bispectral index values and spectral edge frequency at different stages of physiologic sleep. A multicenter study of bispectral electroencephalogram analysis for monitoring anesthetic effect. Bispectral index monitor prevented intraoperative awareness during partial cardiopulmonary bypass. Bispectral index decreased to "0" in propofol anesthesia after a cross-clamping of descending thoracic aorta. Assessment of intraoperative awareness with explicit recall: a comparison of 2 methods. Breakthrough change for adult cardiac surgery in a communitybased cardiovascular program. Cardiac surgical outcomes improvement led by a physician champion working with a nurse clinical coordinator. The Northern New England Cardiovascular Disease Study Group: a regional collaborative effort for continuous quality improvement in cardiovascular disease. A regional prospective study of in-hospital mortality associated with coronary artery bypass grafting. Improved in-hospital mortality in women undergoing coronary artery bypass grafting. Trends in rates of reexploration for hemorrhage after coronary artery bypass surgery. Effect of preoperative aspirin use on mortality in coronary artery bypass grafting patients. Regional collaboration as a model for fostering accountability and transforming health care. A statewide quality collaborative for process improvement: internal mammary artery utilization. Regional collaborations as a tool for quality improvements in surgery: a systematic review of the literature. A very public failure: lessons for quality improvement in healthcare organisations from the Bristol Royal Infirmary. Measuring organizational cultures: a qualitative and quantitative study across twenty cases. The quantitative measurement of organizational culture in health care: a review of the available instruments. Assessing the impact of total quality management and organizational culture on multiple outcomes of care for coronary artery bypass graft surgery patients. Organizational and strategic predictors of manufacturing technology implementation success: an exploratory study. Diagnosing and Changing Organizational Culture: Based on the Competing Values Framework. A survey of the impact of disruptive behaviors and communication defects on patient safety. The quality and economic impact of disruptive behaviors on clinical outcomes of patient care. A complementary approach to promoting professionalism: identifying, measuring, and addressing unprofessional behaviors. A plan for identification, treatment, and remediation of disruptive behaviors in physicians. Changing perceptions of safety climate in the operating room with the Veterans Health Administration medical team training program. Improving perceptions of teamwork climate with the Veterans Health Administration medical team training program. Measurement of implementation components and contextual factors in a two-state healthcare quality initiative to reduce ventilator-associated pneumonia. Implementation of a surgical comprehensive unit-based safety program to reduce surgical site infections. This article outlines the tasks, challenges, and responsibilities of the cardiovascular anesthesiologist that extend beyond the maintenance of the anesthetic state, focusing on overall organ protection. Ten years prior, a number of insightful perspectives on this important medical landmark accompanied the 50th anniversary of this achievement. From the reservoir, blood is pumped to an oxygenator and heat exchanger unit before passing through an arterial filter and returning to the patient. Additional components of the circuit generally include pumps and tubing for cardiotomy suction, venting, and cardioplegia delivery and recirculation, as well as in-line blood gas monitors, bubble detectors, pressure monitors, and blood sampling ports. Procedures involving the thoracic aorta are often performed using partial bypass in which a portion of oxygenated blood is removed from the left side of the heart and returned to the femoral artery.
Aggrenox caps 25/200mg otc
The hypothesis was that most of the interventions to optimize cerebral oxygen saturation would also influence systemic perfusion symptoms 3 months pregnant 25/200 mg aggrenox caps amex. Further studies are needed to determine whether postoperative cognitive dysfunction can be reduced by treatment of intraoperative cerebral oxygen desaturation. A clear threshold below which the risk of postoperative cognitive dysfunction is increased needs to be defined. Recall is defined as postoperative memory for intraoperative events, an infrequent but wellrecognized phenomenon during general anesthesia. However, the frequent use of inhalation agents and short-acting benzodiazepines in modern anesthetic regimens has reduced the risk of intraoperative awareness for this type of surgery. Most hypnotics, opioids, and volatile agents have been used in different combinations for the induction and maintenance of anesthesia, with good results in the hands of experienced clinicians. Limiting the amount of opioids or use of short-acting drugs is encouraged for patients eligible for fast-tracking and early extubation. With modern cardioplegia techniques and assuming an uneventful intraoperative course, cardiac function typically is well preserved, and the goal should be to extubate the patient within 6 hours postoperatively (Box 20. Unraveling the direct or indirect effects of a particular drug on the heart and circulation is complex because overall effects are based on contractility, vascular tone, and response of the autonomic nervous system and baroreceptors. Additional concerns are the details of the animal preparation (eg, species, acute vs chronic preparation, open vs closed chest) or clinical setting (eg, type and speed of induction). One drug is usually not used exclusively (ie, balanced anesthesia), and all drugs must be titrated to effect with the overall goal of avoiding hypotension, excessive hypertension, tachycardia, and myocardial depression. It is rarely used today, and in the United States, thiopental is no longer available. These effects are thought to result from a combination of direct myocardial depression, venodilation, and a decrease in central sympathetic outflow. Etomidate is often the preferred induction agent in patients with depressed cardiac function because it has minimal or no direct negative inotropic or sympathomimetic effects. Significant pain during injection, particularly in a small superficial vein, is unpleasant for the patient and causes tachycardia and hypertension, both of which increase myocardial oxygen demand. Unless combined with adequate amount of opioids, blunting of the adrenergic response to intubation is poor and may result in hypertension and tachycardia. Even a single dose of etomidate can inhibit adrenal mitochondrial hydroxylase activity, resulting in reduced steroidogenesis245,246; however, outcome differences in cardiac surgery patients have not been documented consistently. These studies reported minimal differences in hemodynamics or the incidence of myocardial ischemia. This effect is thought to be related to the anesthetic preconditioning and postconditioning effects of volatile agents (see Chapter 10). Although there seem to be well-documented advantages for using inhalation anesthetics in patients at risk for myocardial injury, benefits of propofol also have been reported. In states associated with depletion of catecholamines and in isolated preparations, ketamine has direct negative inotropic and vasodilating effects,265 and it may have a negative lusitropic effect, decreasing diastolic compliance. Contractility was mildly depressed, although afterload was reduced simultaneously, resulting in no net change in the cardiac index. High-dose opioid anesthesia was introduced into cardiac surgery by Lowenstein and coworkers284 in 1969, in an attempt to provide safe anesthesia without myocardial depression in patients with severe valvular heart disease and compromised cardiac function. Although this revolutionized anesthesia for patients with cardiac dysfunction, it was apparent that morphine had several disadvantages: vasodilation from histamine release, increased requirements for fluids and vasoconstrictors, and prolonged respiratory depression. Forty patients were allocated to receive fentanyl or sufentanil boluses, and an additional 40 patients were randomized to sufentanil bolus dosing followed by continuous infusion. Plasma opioid and catecholamine concentrations were obtained after intubation and after sternotomy. In the bolus-only group, the frequency of hemodynamic responders was unrelated to drug and dose administration. Similarly, in the sufentanil-infusion group, the frequency of response was unrelated to plasma sufentanil levels. Although the study had design flaws (eg, small sample sizes, lack of reporting of hemodynamics), it provided some evidence that even high-dose opioids alone could provide incomplete anesthesia. Blood pressure response and plasma fentanyl concentrations during high and very high-dose fentanyl anesthesia for coronary artery surgery. To provide complete anesthesia, the usual practice is to supplement opioids with inhaled or other intravenous agents. This permits a reduction in the total dose of opioid and, particularly with volatile agents, more rapid return of respiratory drive, facilitating early extubation. Specific effectrelated concentrations of fentanyl or sufentanil were targeted by using a computer-assisted infusion pump. By inspecting plots of the data pairs, the investigators were able to ascertain the inflection point at which the isoflurane concentration began to rise rapidly, indicating poor control of hemodynamics by the respective opioid. However, the perioperative use of -blockers, 2-agonists, and other drugs such as benzodiazepines provide additional hemodynamic control. Traditionally, pancuronium was advocated for use with highdose narcotic techniques because it offset opioid-induced bradycardia. Gueret and colleagues333 showed that a single intubating dose of atracurium or cisatracurium provided adequate paralysis and surgical conditions, leading to quicker neuromuscular blockade recovery for cardiac surgical patients. Advocates of this technique also point to potential advantages with regard to prevention of recall (as indicated by patient movement). However, potential disadvantages include the possibility of greater oxygen demand and consumption and movement during surgery. Dexmedetomidine administration was associated with decreased incidences of intraoperative and postoperative tachycardia (5% vs 32% and 4% vs 40%, respectively) compared with placebo. Patients who received dexmedetomidine also were less likely to receive -blocker therapy for tachycardia. These data demonstrate that dexmedetomidine can be effective in attenuating sympathetic stress responses, although the same effect may predispose patients to hypotension. Therapywasinitiated at the time of the initial response, and no further data points were includedforthosepatients. After a short ischemic period (ie, preconditioning signal), the myocardium is rendered more resistant to prolonged ischemia when the subsequent ischemic event occurs within a certain time window. Research has identified two distinct phases, also referred to as early preconditioning (about 2 hours) and delayed or late preconditioning (24 to 72 hours). For example, the commonly used induction agents etomidate and ketamine do not have cardioprotective properties. The exact mechanisms of preconditioning are much more complex and continue to be investigated. After the administration of a preconditioning signal such as ischemia or certain pharmacologic agents, membrane-bound receptors (eg, A1 adenosine, adrenergic, bradykinin, muscarinic, 1-opioid) coupled to inhibitory G-proteins are activated. The delayed phase of myocardial protection, which may last well beyond the documented 24 to 72 hours, probably is based on transcriptional changes of protective proteins,382,383 which may explain the time gap between early and late preconditioning. For example, Belhomme and associates344 exposed patients to 5 minutes of preconditioning with a 2. Brain natriuretic peptide level as an indicator of myocardial dysfunction was significantly decreased in the sevoflurane group. Whether the biochemical markers of improved cardiac outcome translate into reduced mortality rates or improved long-term outcomes is unclear. Garcia and coworkers343 reported the results of a prospective, randomized study of the effect of sevoflurane preconditioning (10 minutes before aortic cross-clamping) on late cardiac events. Several metaanalyses looked at preconditioning and mortality rates or long-term outcomes for patients undergoing cardiac surgery. The results showed that risk-adjusted 30-day mortality rate was significantly reduced when volatile agents were used during cardiac surgery, especially when there was prolonged use of these agents. The optimal timing and duration of inhalation anesthetic administration are uncertain. De Hert and colleagues340 showed that the best results for myocardial protection were achieved when sevoflurane was administered throughout the intraoperative period rather than immediately before the planned myocardial ischemic event. However, Bein and associates401 found that levels of myocardial cell damage and dysfunction were lower in patients who received sevoflurane in an interrupted manner. Frassdorf and coworkers400 also demonstrated that preconditioning-related myocardial protection was superior with multiple periods of sevoflurane administration applied rather than one short period. When sevoflurane was added to the anesthesia regimen after the coronary anastomoses were completed (ie, postconditioning), myocardial recovery was faster compared with propofol-based anesthesia. Nevertheless, patients who received sevoflurane during the entire procedure had the lowest troponin I levels, and the stroke volume changed the least compared with baseline levels.
Discount aggrenox caps 25/200mg otc
Pegorgotein the generation of reactive oxygen species is a well-described pathophysiologic mechanism of ischemic reperfusion injury medications 4 less cheap 25/200 mg aggrenox caps otc. Superoxide dismutase is involved in the catabolism of free radicals, and its mimetics have had beneficial results in the setting of experimental ischemia. Mathew and collegues247 assessed pexelizumab in a 914-patient study aimed at evaluating its effect on myocardial outcome and mortality. A secondary end point of neurocognitive outcome demonstrated that pexelizumab, although having no effect on global measures of cognition, appeared to have a benefit with respect to the visuospatial domain. Platelet-Activating Factor Antagonist: Lexiphant Platelet-activating factor antagonists have demonstrated neuroprotective effects in experimental models of cerebral ischemia. This study was significantly underpowered, which is a recurring and troublesome feature of many studies in this field. Inflammation is considered an important factor in propagating ischemia-mediated brain injury. Furthermore, the administration of steroids has actually worsened cerebral outcome in a large trial (N = 10,000). Hyperglycemia in animal models and several human studies of cerebral injury has been associated with worsened neurologic outcome. There has been renewed interest in ketamine for its potential to reduce the incidence of delirium. Although there is some experimental evidence supporting its role as a neuroprotectant, there is insufficient clinical evidence to support its use for this specific indication. Average daily (diamonds) and unadjusted average peak (triangles) serum creatinine valuesarepresented. Although the physiology of perioperative renal recovery is as yet less studied, emerging data suggest this is also likely to be important. Incriminated particulates other than atheroma include thrombus, platelet fibrin debris, septic vegetations, and even normal vessel wall. Contrast-associated nephropathy is usually heralded by a significant rise in serum creatinine within 5 days after intravascular contrast injection and occurs in approximately 2% to 7% of patients. Use of low-osmolar contrast media and aggressive prestudy hydration have significantly reduced the risk of contrast-associated nephropathy for patients with diabetic nephropathy and other causes of chronic renal disease. For example, in a recent prospective study of 6478 cardiac surgery patients, use of a hydroxyethyl starch 134/0. Nonetheless, despite its limitations as an early biomarker, serum creatinine remains an important clinical tool because of its many other uses. Renal recovery as reflected by declining creatinine levels is highly predictive of short- and long-term outcomes beyond the magnitude of kidney insult. As outlined earlier, commonly used lysine analogue antifibrinolytics (aminocaproic acid and tranexamic acid) mimic this abnormality by selectively blocking kidney tubule receptors, causing a reversible form of this same proteinuria with apparently benign consequences; these biomarkers are considered of little value in most cardiac surgery settings. Profound hypothermia is a highly effective component of the protective strategy used during renal transplantation. Other studies have reported similar patterns and suggest that profound hematocrit change (eg, >50% drop) may be even less well tolerated, highlighting the importance of a clinical strategy including transfusion only after all measures of hemodilution avoidance have been taken. Researchers have performed meta-analyses for many prevalent therapies by combining data from their randomized clinical trials. In some cases, these reports indicate study size concerns may have been warranted. For example, several metaanalyses found N-acetylcysteine not to have renal benefit even in large cardiac surgery populations. Meta-analyses of loop diuretics trials and controlled studies in critically ill patients describe improvements in markers of renal function (urine output, oliguric period), and reduced need for dialysis but also concerning trends toward increased mortality and poorer renal recovery. Additional data, including rationale and existing studies for a number of these therapies, is outlined next. Dopamine Mesenteric dopamine1 (D1) receptor agonists increase renal blood flow, decrease renal vascular resistance, and enhance natriuresis and 31 Cardiopulmonary Bypass Management and Organ Protection diuresis. However, numerous double-blind, randomized studies in several surgical and nonsurgical settings have failed to demonstrate any renal benefits. Fenoldopam Fenoldopam mesylate, a derivative of benzazepine, is a selective D1receptor agonist. Although first approved as an antihypertensive agent, fenoldopam has shown promise in the prevention of contrast-induced nephropathy. In one prospective, randomized study involving 160 patients with preoperative renal dysfunction, improved renal function with fenoldopam versus placebo was reported after cardiac surgery; however, no long-term benefit was evaluated. Diuretic Agents Diuretics increase urine generation by reducing reuptake of tubular contents. This can be achieved by numerous mechanisms, including inhibiting active mechanisms that lead to solute reuptake (eg, loop diuretics), altering the osmotic gradient in the tubular contents to favor solute remaining in the tubule (eg, mannitol), or hormonal influences that affect the balance of activities of the tubule to increase urine generation (eg, atrial natriuretic peptide). The general renoprotective principle of diuretic agents is that increasing tubular solute flow through injured renal tubules will maintain tubular patency, avoiding some of the adverse consequences of tubular obstruction, including oliguria or anuria and possibly the need for dialysis. Other agentspecific properties (eg, antioxidant effects, reduced active transport) have also been proposed to have beneficial effects in the setting of ischemic renal injury. Loop diuretics, such as furosemide, produce renal cortical vasodilation and inhibit reabsorptive transport in the medullary thick ascending limb, causing more solute to remain in the renal tubule and increasing urine generation. In animal models, administration of furosemide and other loop diuretics has been shown to raise oxygen levels in the renal medulla,416 presumably by reducing oxygen consumption by tubular active transport, but it also results in distal tubular hypertrophy. Although they may facilitate avoidance of dialysis in responsive patients by maintaining fluid balance, there is insufficient evidence to support the routine use of loop diuretics as specific renoprotective agents. However, in situations of severe hemoglobinuria, they may facilitate urine production and tubular clearance of this nephrotoxin. Mannitol, an osmotic diuretic, has been evaluated in several studies of cardiac surgical patients. In an animal model of thoracic aortic clamping, mannitol did not provide evidence of improved renal function after unclamping. The weight of evidence, including four meta-analyses, suggests that potential benefits that may exist with contrast nephropathy are not pertinent to perioperative patients. Despite being positively supported in a second trial,446 clonidine has not gained popular acceptance as a renoprotective agent. The fundamental tenets of this protection center on the judicious use of hypothermia along with the induction and maintenance of chemically induced electromechanical diastolic cardiac arrest. Bigelow and investigators472 were the first to describe the use of hypothermia for this purpose, and this was complemented by subsequent work by Melrose and colleagues,473 who first reported the electromechanical arrest of the heart by the administration of potassium-containing cardioplegia. Despite continued efforts directed at myocardial protection, it is clear that myocardial injury, although reduced, still remains a problem, and with it, the representative phenotype of postoperative myocardial dysfunction. Incidence and Significance of Myocardial Dysfunction After Cardiopulmonary Bypass Unlike other organs at risk of damage during cardiac surgery, it is assumed, because of the very nature of the target of the operation being performed, that all patients having cardiac surgery will suffer some degree of myocardial injury. It is differentiated from the reversible dysfunction associated with chronic ischemia, which is called hibernation. The metabolic consequences of oxygen deprivation become apparent within seconds of coronary artery occlusion. With the rapid depletion of high-energy phosphates, accumulation of lactate and intracellular acidosis in the myocytes soon follows, with the subsequent development of contractile dysfunction. Myocardial Injury From the earliest days of modern cardiac surgery, perioperative myocardial dysfunction, with its associated morbidity and mortality, has been reported. With reperfusion the paradox, represented by the balance of substrate delivery restoration needed for normal metabolism that also can serve as the substrate for injurious free radical production, becomes a significant issue for consideration. Reperfusion causes a rapid increase in free radical production within minutes, and it plays a major role initiating myocardial stunning. Bolli482 identified the importance of this effect by demonstrating that antioxidants administered just before reperfusion significantly diminished myocardial stunning, an effect not observed if the same substance were introduced after reperfusion.
Discount aggrenox caps 25/200mg without prescription
Is the pericardial effusion the sequela of another cardiovascular event or process (ie treatment mononucleosis order aggrenox caps 25/200 mg with amex, aortic dissection or cardiac catheterization) Are invaginations of the free walls of the right atrium, right ventricle, or left atrium present Data Collection Echocardiography is the standard modality for diagnosis of pericardial fluid. Echocardiographic findings consistent with tamponade include the presence of pericardial fluid, compression of the atria, compression of the right ventricle, and loss of normal respiratory variability of ventricular inflow velocities. Location of the effusion is paramount should pericardiocentesis be deemed necessary for acute decompression. The effusion need not be a large circumferential effusion to affect cardiac function significantly. Postcardiotomy pericardial clot may be smaller and more compartmentalized than a chronic circumferential effusion, which may be free flowing. Interpreting the clinical significance of cardiac hemodynamics may be complicated by factors such as lability of hemodynamics, decreased intravascular volume, depressed cardiac function, mechanical ventilation and pulmonary dysfunction, soft tissue changes, and chest tubes that obstruct some of the echocardiographic windows. Doppler imaging is used as a complementary method of demonstrating the hemodynamic derangements of tamponade and to determine the clinical significance of an effusion. Although not specific for tamponade, the changes in respiratory variation of inflow velocity are the hallmarks of increased pericardial pressure. Other important data pertaining to the cause and possible intervention include coagulation status. Echocardiography is portable, quick, and noninvasive, yet it is a sensitive and specific modality for the detection and assessment of a pericardial effusion. The effusion need not be a large circumferential effusion to affect heart function significantly. Small effusions are common after cardiac surgical procedures, especially after removal of chest tubes, and in heart transplant recipients with a mismatch between heart size and pericardial cradle. The presence of a pericardial effusion in the patient who has not undergone cardiotomy must lead to a search for the cause of the effusion. Pericardial effusion mandates close scrutiny of the aortic root for possible aortic dissection. Pericardial effusion in a trauma patient is worrisome for cardiac rupture, ventricular contusion, or foreign body injury. Acute cardiac tamponade in the patient who has not undergone cardiotomy can develop after introduction of as little as 60 to 100 mL of blood. Causes may include type A aortic dissection, myocardial infarction with rupture, acute pericarditis, bleeding from malignant disease, myocardial contusion, or myocardial perforation from penetrating trauma. These life-threatening conditions may manifest with hypotension, tachycardia, plethora, and jugular venous distention. Treatment consists of immediate decrease in pericardial pressure, which can be accomplished through the removal of a relatively small volume of fluid. This temporizing measure can be lifesaving until more definitive therapy is instituted. Development of cardiac tamponade is related to the rate of accumulation of pericardial fluid and the capacity for the pericardium to stretch and accommodate fluid. Chronic pericardial effusions, which occur in cases of malignant disease, uremia, connective tissue disease, Dressler syndrome, and postinfection pericarditis, uncommonly require emergency intervention. Acute pericardial effusions that occur after cardiotomy are usually more ominous and often result in hemodynamic compromise requiring treatment (see Chapters 24 and 38). Hemodynamics may improve temporarily with the administration of volume, thus altering intrathoracic pressure (decreasing peak inflation pressure), but the patient still may require drainage of the effusion. Chronic malignant effusions improve after pericardiocentesis but often require a pericardial window for more definitive therapy. Effusions resulting from acute aortic syndromes or cardiac trauma require timely surgical intervention. Postoperative cardiac surgical patients may require urgent reexploration for evacuation of pericardial hematoma and to address the cause of continued bleeding. If hemodynamics improve after sternotomy but minimal clot is found, the physiologic tamponade may be related to generalized tissue edema and pulmonary dysfunction. In cases of poor cardiac function, the sternal incision may need to remain open and covered with a sterile dressing until edema recedes and cardiac function improves. Because the differential diagnosis of a dilated coronary sinus includes disorders associated with increased right-sided pressures, confirmation should be obtained by injecting agitated saline contrast into an intravenous catheter in the left arm. As a consequence, cannulation of the coronary sinus with administration of retrograde cardioplegia is ineffective for providing cardiac protection during cardiac arrest. If transseptal flow is present across the defect, it is generally from left to right because left atrial pressure is generally greater throughout the cardiac cycle. Bidirectional flow is possible with transient increases of right atrial pressure that can be observed during normal respiratory maneuvers (ie, Valsalva, coughing, and physical straining). Detection of a primum or sinus venosus defect requires a more involved surgical procedure, and associated anomalies must be addressed. Alternatives to operative closure are increasing as transvenous percutaneous closure devices become increasingly applicable. The cause of this lesion is attributed to poor growth of the secundum septum or excessive absorption of the primum septum. Only 11% of surgeons converted a planned off-pump procedure to an on-pump procedure to close the defect, but the rate of closure increased to 96% if the patient had a history of possible paradoxical embolism. Sometimes surgical intervention requires a significant alteration of the surgical plan that may significantly increase operative risk. Major focal and nonfocal neurologic deficits, cognitive decline, and coma are common postoperatively. The pathogenesis of cerebral damage is multifactorial, with embolism considered a major contributor. Other factors include hypotension, low flow, reperfusion injury, and inflammation. Embolic events are strongly associated with the severity of atherosclerotic disease, characterized by plaque thickness of greater than 4 mm, ulcerated plaques, and mobile protruding plaques in the aorta. The clinical consequence of distal embolization depends on the number, composition (eg, air bubbles, fat particles, platelet aggregates, and calcium deposits), size, and location of the emboli (see Chapters 14, 15, 18, 20, 21, 23, 31, and 40). Epiaortic ultrasound examination can provide high-definition imaging of these otherwise hidden portions of the aorta. A common practice is the interrogation of the descending thoracic aorta for high-grade atheroma. In the absence of atheromatous disease in the descending aorta, the ascending aorta and locus of aortic cannulation are significantly less likely to have high-grade disease. A 67-year-old patient was scheduled to undergo triple coronary artery bypass grafting. Epiaortic scanning takes time and expertise in its interpretation and poses the potential risk for wound contamination. Data are insufficient to support its use in all cardiac patients, although high-risk patients (advanced age, diabetes, hypertension) are the most likely to benefit. Echocardiographers working in the operating room need the skill set to interrogate the aorta by handheld ultrasound scanning and the ability to guide the surgeon in performing the examination. A diagnostic scan of the ascending aorta and arch to evaluate the location of possible cannulation and clamp sites can be performed in several minutes. Standardized approaches to a comprehensive organized intraoperative epiaortic and epicardial examination are useful guides. The patient is transferred to the operating room table, and everyone turns to the anesthesiologist-echocardiographer for guidance. The attending surgeon asks, "I need to know is this an anterior injury with heart contusion, injury to the ascending aorta, tamponade with blood in the pericardium, or a transected aorta at the isthmus or arch, or is this a nonoperable injury The patient is positioned in the left lateral decubitus position, and the operation proceeds to save a young life. Few more crucially important decisions are posed to the intraoperative echocardiographer than to diagnose the nature and extent of acute aortic injury quickly and accurately.
Locust Bean (Carob). Aggrenox.
- Are there safety concerns?
- Nutritional disorders, celiac disease, obesity, diarrhea, heartburn, intestinal inflammation, and vomiting during pregnancy.
- How does Carob work?
- What is Carob?
- Dosing considerations for Carob.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96341
25/200mg aggrenox caps visa
That said treatment lyme disease trusted 25/200mg aggrenox caps, abnormalities in platelet function and life span have on occasion been reported. Cyanotic erythrocytotic patients have excessive hemoglobin turnover, and adults have an increased incidence of calcium bilirubinate gallstones. Biliary colic can develop years after cyanosis has been resolved by cardiac surgery. These factors include increased tissue capillary density, elevated systemic venous pressure, aortopulmonary and transpleural collaterals that have developed to increase pulmonary blood flow, and prior thoracic surgery. Despite the elevated uric acid levels, urate stones and urate nephropathy are rare. Paradoxical emboli can occur even through shunts that are predominantly left to right, because during the cardiac cycle there can be small transient reversals of the shunt direction. A healed childhood brain abscess can provide the nidus for the development of seizures throughout life. Surgery at the apices of the lungs is particularly associated with the risk of nerve damage. Nerves that are susceptible to injury include the recurrent laryngeal nerve, the phrenic nerve, and the sympathetic chain. They can affect the suitability of vessels for cannulation by the anesthesiologist or measurement of correct pressures. Some lesions, particularly when associated with heterotaxy (polysplenia) have discontinuity of the inferior vena cava; Will not be able to pass a catheter from the groin to the right atrium. Distal blood pressure will be low in the presence of coarctation of the aorta or following subclavian flap repair (subclavian artery only), and variably so if postoperative recoarctation; pulses can be absent or palpable with abnormal blood pressure. Blood pressure low with classic Blalock-Taussig shunt on that side, and variably so with modified Blalock-Taussig shunt. Blood pressure artifactually high with supravalvular aortic stenosis (Coanda effect). Moderate or severe renal dysfunction (estimated glomerular filtration rate of <60 mL/ min/m2) carries a five-fold increased risk of death at 6-year follow-up compared with patients with normal glomerular filtration rate and a three-fold increase over those with mild elevations in glomerular filtration rate 50 Renal dysfunction is particularly prevalent in cyanotic patients and those with poor cardiac function. Although cardiac complications, spontaneous abortions, premature delivery, thrombotic complications, peripartum endocarditis, and poor fetal outcomes can occur,63 successful pregnancy to term with vaginal delivery is possible for most patients with congenital defects. Up to 47% of cyanotic women have worsening of functional capacity during pregnancy. The increases in stroke volume and cardiac output during pregnancy can stress an already pressure-overloaded ventricle. The decrease in systemic vascular resistance that accompanies pregnancy is better tolerated by women with regurgitant lesions and typically offsets the added insult of pregnancyrelated hypervolemia. The decrease in systemic vascular resistance can, however, increase right-to-left shunting. Maternal cyanosis is associated with increased incidences of prematurity and intrauterine growth retardation. Women on long-term anticoagulation will likely need peripartum modifications, and postpartum thromboembolism is a potential significant problem. Anesthesiologists will generally encounter pregnant patients well into the last trimester. Most of the major physiologic changes associated with pregnancy occur before the third trimester, and if patients have maintained good functional status to this point, they will have demonstrated themselves to be in a relatively low-risk group. Pregnancy is a stress test, and if they have successfully arrived at the mid-to-late third trimester, it is more likely that they will successfully tolerate delivery. There is no a priori reason to favor an instrumented or cesarean delivery over a vaginal one. Furthermore, avoidance of second-stage pushing is an option as long as progress is being made and can be combined with a maneuver such as low-outlet vacuum or forceps to facilitate delivery. The third stage can be accompanied by an autotransfusion of placental blood or potentially with hypovolemia with uterine atony and hemorrhage. These rapid changes in loading conditions can be poorly tolerated in mothers with fixed cardiac output, and pulmonary edema or heart failure can develop. Some mothers will be taking medications for their cardiac condition, including antiarrhythmics. Maternal cardioversion would appear to be safe for the fetus at all stages because of the low intensity of the electrical field at the uterus. Bodies that carry scars from prior surgery and physical limitations can complicate the bodyconscious teenage years. While they are children, these patients rely on their parents to ensure regular cardiac appointments are kept and surveillance echocardiograms are done. Cardiac Issues the basic hemodynamic effects of an anatomic cardiac lesion can be modified by time and by the superimposed effects of chronic cyanosis, pulmonary disease, or the effects of aging. Although surgical cure is the goal, true universal cure, without residua, sequelae, or complications, is uncommon on a population-wide basis. Postoperative arrhythmias are common, particularly when surgery entails long atrial suture lines, and the incidence of atrial arrhythmias increases with time, either as a primary sequela or as an indicator of diminished cardiac function. The reader is referred to one of the current texts on pediatric cardiac anesthesia for more detailed descriptions of these lesions, the available surgical repairs, and the anesthetic implications during primary repair. Both short-term and long-term results from older series can differ significantly from contemporary results. Aortic Stenosis Valvar aortic stenosis is the most common congenital heart defect but is often not seen in that light because it typically does not cause problems until adulthood. Most aortic stenosis in adults is due to a congenitally bicuspid valve that does not become problematic until late middle age or beyond, although endocarditis risk is lifelong. Congenital aortic stenosis can on some occasions, however, become severe enough to warrant surgical correction in adolescence or young adulthood, in addition to those severely affected valves that present in infancy. Once symptoms (angina, syncope, near-syncope, heart failure) develop, survival is markedly shortened. Median survival is 5 years after the development of angina, 3 years after syncope, and 2 years after heart failure. Most mothers with aortic stenosis can successfully carry pregnancies to term and have vaginal deliveries. Hemodynamic monitoring during delivery with maintenance of adequate preload and avoidance of hypotension is critical. When intervention is required during pregnancy, percutaneous balloon valvuloplasty is an attractive option compared with aortic valve replacement. Additionally, there is a risk of stroke from calcium that embolizes from the valve during balloon dilation. Aortopulmonary Shunts Depending on their age, adult patients may have had one or more of several aortopulmonary shunts to palliate cyanosis during childhood. All were inherently inefficient, because some of the oxygenated blood returning through the pulmonary veins to the left atrium and ventricle would then return to the lungs through the shunt, thus volume loading the ventricle. It was difficult to quantify the size of the earlier shunts, such as the Waterston (side-to-side ascending aorta to right pulmonary artery) and Potts (side-to-side descending aorta to left pulmonary artery). If too small, the patient was left excessively cyanotic; if too large, there was pulmonary overcirculation with the risk of developing pulmonary vascular disease. The Waterston, in fact, could on occasion stream blood flow unequally, resulting in a hyperperfused, hypertensive ipsilateral (right) pulmonary artery and a hypoperfused contralateral (left) pulmonary artery. Takedown of Waterston shunts often required a pulmonary arterioplasty to correct deformity of the pulmonary artery at the site of the anastomosis, and the posteriorly located Potts anastomoses could not be taken down from a median sternotomy. Patients with a classic Blalock-Taussig shunt almost always lack palpable pulses on the side of the shunt and arm length and strength can be mildly affected. To ensure a valid measurement, preoperative blood pressure should be measured in both arms (Table 22. Theanastomosesare(1),modified Blalock-Taussig, (2) classic Blalock-Taussig, (3) Waterston (WaterstonCooley), and (4) Potts. The most common type- and, if otherwise undefined, the presumptive type-is the secundum type located in the midseptum. The primum type at the lower end of the atrial septum is a component of endocardial cushion defects, the most primitive of which is the common atrioventricular canal (see later). The sinus venosus type, high in the septum near the entry of the superior vena cava, is almost always associated with partial anomalous pulmonary venous return, most frequently drainage of the right upper pulmonary vein to the low superior vena cava.
Syndromes
- Swelling at site of sting
- Recent neurosurgery
- Lymphoma
- Inflammation of the area between the lungs (mediastinitis)
- Infection
- X-rays of the abdomen, barium contrast studies, and CT scans may help diagnose a blockage of the intestines caused by adhesions.
- Peppermint and spearmint
- Severe malnutrition caused by feeding difficulty, leading to failure to thrive
- Women at high risk for heart disease should take omega-3 fatty acid supplements.
Order 25/200 mg aggrenox caps free shipping
Flow cytometric analysis of platelet surface glycoproteins: phenotypically distinct subpopulations of platelets in children with chronic myeloid leukemia symptoms quadriceps tendonitis 25/200 mg aggrenox caps otc. Studies on platelet membrane glycoproteins and platelet function during hemodialysis. Platelet-activated clotting time does not measure platelet reactivity during cardiac surgery. Platelet surface glycoproteins: studies on resting and activated platelets and platelet membrane microparticles in normal subjects, and observations in patients during adult respiratory distress syndrome and cardiac surgery. Evaluation of coagulation during cardiopulmonary bypass with a heparinase-modified thromboelastographic assay. The role of desmopressin acetate in patients undergoing coronary artery bypass surgery: a controlled clinical trial with thromboelastographic risk stratification. Thromboelastography is a suboptimal test for determination of the underlying cause of bleeding associated with cardiopulmonary bypass and may not predict a hypercoagulable state. Coagulation abnormalities in the trauma patient: the role of point-of-care thromboelastography. Rapid thrombelastography delivers real-time results that predict transfusion within 1 hour of admission. Initial experiences with point-of-care rapid thrombelastography for management of life-threatening postinjury coagulopathy. Impact of new oral or intravenous P2Y12 inhibitors and clopidogrel on major ischemic and bleeding events in patients with coronary artery disease: a meta-analysis of randomized trials. A novel modification of the Thrombelastograph assay, isolating platelet function, correlates with optical platelet aggregation. Comparison of modified Thrombelastograph and Plateletworks whole blood assays to optical platelet aggregation for monitoring reversal of clopidogrel inhibition in elective surgery patients. Point of care testing in cardiac surgery: diagnostic modalities to assess coagulation and platelet function. Perioperative assessment of platelet function by Thromboelastograph platelet mapping in cardiovascular patients undergoing non-cardiac surgery. Viscoelastic clot strength predicts coagulation-related mortality within 15 minutes. Evaluation of the coagulation profile among oral and vaginal combined hormonal contraceptive users using Sonoclot coagulation analyzer. Assessment of heparin anticoagulation by Sonoclot Analyzer in arterial reconstruction surgery. Impact of Sonoclot hemostasis analysis after cardiopulmonary bypass on postoperative hemorrhage in cardiac surgery. Evaluation of post-cardiopulmonary bypass Sonoclot signatures in patients taking nonsteroidal anti-inflammatory drugs. Comparison of Thromboelastograph and Sonoclot coagulation analyzer for assessing coagulation status during orthotopic liver transplantation. Interoperator and intraoperator variability of whole blood coagulation assays: a comparison of thromboelastography and rotational thromboelastometry. Correlations between global clotting function tests, duration of operation, and postoperative chest tube drainage in pediatric cardiac surgery. Validation of rotational thromboelastometry during cardiopulmonary bypass: a prospective, observational in-vivo study. The value of rotation thromboelastometry to monitor disturbed perioperative haemostasis and bleeding risk in patients with cardiopulmonary bypass. A comparative evaluation of rotation thromboelastometry and standard coagulation tests in hemodilution-induced coagulation changes after cardiac surgery. Comparison of whole blood fibrin-based clot tests in thrombelastography and thromboelastometry. Point-of-care testing: a prospective, randomized clinical trial of efficacy in coagulopathic cardiac surgery patients. Comparison of three point-of-care testing devices to detect hemostatic changes in adult elective cardiac surgery: a prospective observational study. Changes in transfusion therapy and reexploration rate after institution of a blood management program in cardiac surgical patients. Thromboelastometry-guided administration of fibrinogen concentrate for the treatment of excessive intraoperative bleeding in thoracoabdominal aortic aneurysm surgery. First-line therapy with coagulation factor concentrates combined with point-of-care coagulation testing is associated with decreased allogeneic blood transfusion in cardiovascular surgery: a retrospective, single-center cohort study. Thromboelastometry based early goal-directed coagulation management reduces blood transfusion requirements, adverse events, and costs in acute type A aortic dissection: a pilot study. Reduction of fresh frozen plasma requirements by perioperative point-of-care coagulation management with early calculated goal-directed therapy. An audit of red cell and blood product use after the institution of thromboelastometry in a cardiac intensive care unit. Comparison of structured use of routine laboratory tests or near-patient assessment with clinical judgement in the management of bleeding after cardiac surgery. Reduced haemostatic factor transfusion using heparinase-modified thrombelastography during cardiopulmonary bypass. Thromboelastometrically guided transfusion protocol during aortic surgery with circulatory arrest: a prospective, randomized trial. The role of point-of-care assessment of platelet function in predicting postoperative bleeding and transfusion requirements after coronary artery bypass grafting. Inhibition of platelet aggregation by abciximab but not by aspirin can be detected by a new point-of-care test, the hemostatus. Validation of a VerifyNow-P2Y12 cartridge for monitoring platelet inhibition with clopidogrel. Comparison of methods to evaluate clopidogrel-mediated platelet inhibition after percutaneous intervention with stent implantation. A comparison of platelet function tests and thromboxane metabolites to evaluate aspirin response in healthy individuals and patients with coronary artery disease. Efficacy and safety of intensified antiplatelet therapy on the basis of platelet reactivity testing in patients after percutaneous coronary intervention: systematic review and meta-analysis. Posttreatment platelet reactivity on clopidogrel is associated with the risk of adverse events after off-pump coronary artery bypass. Routine assessment of on-clopidogrel platelet reactivity and gene polymorphisms in predicting clinical outcome following drug-eluting stent implantation in patients with stable coronary artery disease. Are in-vitro platelet function tests useful in predicting blood loss following open heart surgery Perioperative evaluation of primary hemostasis in patients undergoing mitral valve repair. Patients with severe aortic valve stenosis and impaired platelet function benefit from preoperative desmopressin infusion. Utility of platelet function analyzer as a screening tool for the diagnosis of von Willebrand disease in adolescents with menorrhagia. The effect of acetylsalicylic acid resistance on prognosis of patients who have developed acute coronary syndrome during acetylsalicylic acid therapy. Point-of-care whole blood impedance aggregometry versus classical light transmission aggregometry for detecting aspirin and clopidogrel: the results of a pilot study. A comparison between the Plateletworks-assay and light transmittance aggregometry for monitoring the inhibitory effects of clopidogrel. Plateletworks platelet function test compared to the thromboelastograph for prediction of postoperative outcomes. Correlation between point-of-care platelet function testing and bleeding after coronary artery surgery. Comparison of platelet function tests in predicting clinical outcome in patients undergoing coronary stent implantation. Platelet dysfunction as measured by a point-of-care monitor is an independent predictor of high blood loss in cardiac surgery. A new point-of-care method for monitoring anti-platelet therapy: application of the cone and plate(let) analyzer. Platelet concentrates transfusion in cardiac surgery and platelet function assessment by multiple electrode aggregometry. An evaluation of cyclooxygenase-1 inhibition before coronary artery surgery: aggregometry versus patient self-reporting.
Order aggrenox caps 25/200 mg overnight delivery
Simulation is medicine vial caps purchase 25/200mg aggrenox caps free shipping, first and foremost, changing the face of medicine from "see one, do one, teach one to an approach in which students and residents practice on References 201, 213, 222, 223, 228, 262, 311, 312. Using simulation, procedures such as intubation, laparoscopic operations, and bronchoscopy are learned and, hopefully, perfected before attempted in patients. Finally, adequate performance in simulated events is a part of medical and nursing licensure. In a voluntary survey of 10,806 anesthetic cases in 2 hospitals in New Zealand,361 the overall rate of drug error was 1 in 133 anesthetic cases (0. The receiving nurse ensures the bed space is set up according to the monitoring, ventilation, and other requirements specified on the Patient Transfer Form. Phase 2: Information handover the anesthetist, then the surgeon, speak alone and uninterrupted, providing the relevant information about the case, using the Information Transfer Aid Memoir. Safety check: the receiving nurse and doctor should use the Information Transfer Aid Memoir to check that all necessary information has been obtained and ask appropriate questions. Phase 3: Discussion and plan the surgeon, anesthetist, and receiving team discuss the case as a group. The receiving physician manages the discussions and identifies anticipated problems, and anticipated recovery is discussed. Patient handover from surgery to intensive care: using Formula 1 pit-stop and aviation models to improve safety and quality. A similar survey in Canada found that 85% of anesthesiologists reported that they had made at least 1 drug error or "near miss," with 4 deaths in the 1038 reported errors. Additional reports from Australia,364 Japan,365,366 and South Africa367 suggest that anesthetic drug error continues to be a significant problem around the world. The incidence of drug administration errors in an academic practice in the United States appears to be similar to that reported from elsewhere in the world. In a self-reporting study performed in a single center in the United States, Cooper and associates368 found a rate of error of 0. The majority of reported drug errors can be classified as Webster and colleagues361 proposed (Table 30. Equipment misuse or failure accounted for 26%, incorrect route for 14%, and communication error for 4%. Rarely, the perfusionist also may be an anesthesiologist (particularly in Australia), but whether the anesthesiologist even supervises the perfusionist in the administration of drugs varies depending on the particular practice setting. In a voluntary survey of incidents during perfusion, 29% of perfusionists in Australia and New Zealand reported related incidents during bypass. An updated survey by the same researchers found a total of 4882 events that occurred over 2 years; 63 events were related to medication errors, and 10 were related to incorrect units of blood. In these cases of serious harm, succinylcholine was the primary drug in 17% of the cases and epinephrine in 8%. Drug administration errors involving epinephrine were particularly dangerous, with death or major morbidity resulting in 11 of the 17 epinephrine-related cases. An informative case report describing the nearly fatal results of inadvertent epinephrine administration resulting from an ampoule swap has been published. Human ingenuity has found a way to place a catheter into virtually every location in the body; human error has found a way to make every possible misconnection between infusion type and access line, often with disastrous outcomes (Table 30. Accidental injection of vincristine into the subarachnoid space was first reported in 1968; since then at least 58 deaths have occurred worldwide, despite extensive publicity of the danger. However, as any anesthesiologist can attest, many were related to poor user interface design or human factors issues. Compliance with the drug library is critical for prevention of error, but a systematic review found numerous studies showing high rates of user override of soft alerts, as well as a variable compliance rate with drug library use. A review evaluated the evidence for various measures for reducing drug administration errors in anesthetic practice and made recommendations. Pharmacy involvement was believed to be critical to reducing errors, from educational duties to managing the entire dispensing process from ordering of drugs to providing them to the anesthesiologists. Several studies of the use of bar code scanning systems in hospital nursing units suggested that errors may be reduced. Only approximately 90% of drugs arrive at a pharmacy with a bar code; the linear bar codes mandated are easily rendered illegible, the locations of bar codes on inhalers render them unreadable when inserted in the administration device, and so on. These new requirements may increase the price of many drugs but could improve patient safety-but only if hospitals fully implement bar code scanning across the delivery process. No significant differences in errors occurred when the system was used compared with conventional methods, primarily because of sample size but also due to user error or violation. In a subset analysis, significantly fewer errors occurred when the system was used as intended, including that users scanned the bar code of each drug before administration and kept the voice prompt active (a computer voice speaks the name of the drug after the bar code is scanned). Although no comprehensive assessment of the incidence and nature of errors related to infusion pumps has been made, it is clear from the available evidence that programming errors are significant sources of error. Some infusion pumps use drug libraries with predefined dosing limits and warn the practitioner if the dosing parameters entered will result in a dose that is outside the predefined dosing limits. Smart infusion pumps, although not perfect, repeatedly have been shown to intercept and prevent errors, primarily wrong rate and dose. However, the evidence for the effectiveness of pumps with drug libraries is mixed, with some studies suggesting benefit and others not. The drug library intended to prevent programming errors was bypassed 25% of the time. This study demonstrated that technology alone may not solve a problem; close attention to the details of implementing the technology and making it work properly are essential. Many errors were related to bolus dosing and failure to monitor and respond to drug-related problems adequately. These investigators did not conclude that smart pumps should be abandoned, but they advocated for smarter and more capable pumps. Although smart pumps can alert to programming errors that may result in an incorrect dose, they do not recognize that a wrong drug has been placed in the pump or that the drug is being administered to the wrong patient. Furthermore, if the pump is connected to the electronic medical record, the dosing information from the pump can be automatically documented in the record. Application of bar code scanning to infusion pumps is a relatively new and evolving technology. Transfusion Safety Although bar coding of drugs has received greater publicity, bar coding of blood units and the use of bar coding to ensure accurate matching of blood component to recipient comprise a promising technology. The system also improved the efficiency of blood component management and reduced the outdate rate on red blood cells from 3. Prevention of Intraoperative Awareness An early report of patients who had experienced awareness during anesthesia was made in 1961 by Meyer,413 who described the patients as "Expressionless and staring. Patients often are reticent to speak of the experience and frequently do not report it unless specifically queried, and they may not be able to verbalize the experience for days or weeks. This delay in the appearance of explicit memory has led many anesthesiologists to be skeptical about an incidence of 0. However, most cases of awareness cannot be traced to such obvious events,429 but they are likely related to complex differences among patients in response to anesthetic drugs. Certain subtypes confer resistance to the memory inhibition of isoflurane while not changing the immobilization or hypnotic effects. Specific types of surgical procedures also increase the risk: cardiac surgical procedures increase the risk of intraoperative awareness from the overall level of approximately 0. Ghoneim and Block and their colleagues445,446 confirmed that cardiac surgical procedures are associated with an increased risk. Administration of neuromuscular blocking drugs, ubiquitous in cardiac surgical patients, also increases the risk for intraoperative awareness. No difference was reported in the incidence of intraoperative awareness in the two groups. Small doses of muscle relaxant usually obliterate high-frequency artifact caused by muscle activity, but not that associated with electrocautery. The propensity of response to a surgical stimulus is more likely with inhaled agents and less likely if opioids are present. No single foolproof method to avoid all instances of intraoperative awareness exists, but multiple elements that must be considered and managed (Box 30. Anesthesia providers should also therefore be alert to and elicit any experience of awareness from patients, by using a modified Brice interview. However, most quality improvement initiatives in cardiac surgery represent comprehensive, multidisciplinary, and multiunit approaches. Doran and colleagues466 used the Institute for Healthcare Improvement Breakthrough model of rapid cycle improvements in a community cardiac surgical program and found significant improvements in length of stay, ventilator time, patient satisfaction, and cost.
Purchase 25/200mg aggrenox caps free shipping
The Doppler-calculated gradient is subject to the same flow limitation as invasively calculated gradients counterfeit medications 60 minutes cheap aggrenox caps online master card. The preferred method requires only two Doppler-generated velocities: those proximal or distal to the stenotic valve. Several studies have demonstrated the reliability of these Doppler-determined valve areas. The increase of wall tension is thought to be the direct stimulus for the further parallel replication of sarcomeres, which produces the concentrically hypertrophied ventricle characteristic of chronic pressure overload. Second, the slope of the diastolic limb is steeper, reflecting the reduced left ventricular diastolic compliance that is associated with the increase in chamber thickness. Echocardiographic and radionuclide studies have documented that diastolic filling and ventricular relaxation are abnormal in patients with hypertrophy from a variety of causes, and significant prolongation of the isovolumic relaxation period is the most characteristic finding. Clinical studies have confirmed that ejection performance is preserved at the expense of myocardial hypertrophy, and the adequacy of the hypertrophic response has been related to the degree to which it achieves normalization of wall stress, in accordance with the Laplace relation. This in no way excludes the possibility that a subset of patients also may experience some intrinsic depression of myocardial contractility. In most patients, load-insensitive indices of contractility (ie, endsystolic stress-diameter determinations) are virtually identical before and after the development of hypertrophy, suggesting that the increase in chamber thickness compensates for the afterload stress and that myocardial contractility is therefore normal, albeit appropriate for the higher afterload. Left ventricular relaxation and filling pattern in different forms of left ventricular hypertrophy: an echocardiographic study. The box size indicates myocardial mass, and the circle area indicates the cross-sectional area of coronary vasculature. Concentric hypertrophy normalizes wall stress, and contractility remains unchanged. The latter may accompany hypertrophy-induced left ventricular chamber or mitral annular enlargement. Intrinsic contractility is commonly preserved, and the major threat to the hypertrophied ventricle is its exquisite sensitivity to ischemia. The possibility of ischemic contractile dysfunction in the inadequately hypertrophied ventricle arises from increases in wall tension, which directly parallels the imbalance between the increased peak systolic pressure and the degree of mural hypertrophy. Mural thickening enhances systolic performance, maximizing the mechanical work performed while minimizing its metabolic cost. The price of systolic efficiency is relatively inadequate growth of the coronary microcirculation, which contributes to relaxation abnormalities, diastolic dysfunction, and the potential for superimposition of ischemia-induced abnormalities of systolic dysfunction (Table 21. The findings of these studies also emphasize that contractile reserve is an important prognostic indicator for these patients and that dobutamine challenge may help select patients for valve replacement. Left ventricular contractile reserve appears to be a critical variable for prognosis. This treatment can effectively alleviate to some extent the left ventricular dysfunction component of the complete syndrome. Surgical therapy is unlikely to benefit these patients because the underlying pathology is a weakly contractile myocardium. Moderate or severe valvular calcification along with a rapid increase in aortic-jet velocity identify patients with a very poor prognosis. They should be considered for early valve replacement rather than delaying until symptoms develop. Nitroprusside in critically ill patients with left ventricular dysfunction and aortic stenosis. In these patients, the additional precaution of administering supplementary oxygen may obviate the possibility of a similarly pronounced response to the sedative effects of the premedicant. Hemodynamic monitoring is controversial, and few prospective data are available on which to base an enlightened clinical decision. Intraoperative fluid management should be aimed at maintaining appropriately increased left-sided filling pressures. Keeping up with intravascular volume losses is particularly important in noncardiac surgery, in which the shorter duration of the operation may make inhalation or potentially vasodilating regional anesthesia preferable to a narcotic technique. The principal benefit of a narcotic induction is assurance of an adequate depth of anesthesia during intubation, which reliably blunts potentially deleterious reflex sympathetic responses capable of precipitating tachycardia and ischemia. The negative inotropy of inhalation anesthetics is a theoretical disadvantage for a myocardium faced with the challenge of overcoming outflow tract obstruction. Occasionally, surgical stimulation elicits a hypertensive response despite the impedance posed by the stenotic valve and a seemingly adequate depth of narcotic anesthesia. In these patients, a judicious trial of low concentrations of an inhalation agent, used purely for control of hypertension, may prove efficacious. The temptation to control intraoperative hypertension with vasodilators should be resisted in most cases. Given the risk for ischemia, nitroglycerin seems to be a particularly attractive drug. Intraoperative hypotension, regardless of the primary cause, should be treated immediately and aggressively with a direct -adrenergic agonist such as phenylephrine. Most attention has been focused on the potential for irreversible cellular damage occurring during the period of ischemic cardiac arrest. Although these changes are observed in patients whose clinical course is seemingly unremarkable, ischemic cellular damage also may underlie the frequent occurrence of postoperative low-output syndromes and the greater mortality rates associated with valvular operations. Because the operation requires an ascending aortotomy, many surgeons routinely use direct coronary ostial cannulation for the delivery of the cardioplegic solution. Problems associated with this approach are uncommon but include the inherent hazard of injury to the coronary ostia and cannula-induced late stenosis of the left main coronary artery. These problems are obviated by the use of cardioplegia delivery through the coronary sinus. The retrograde technique commonly is used in conjunction with an initial dose of antegrade cardioplegia; the latter provides for a more immediate electromechanical arrest. A common clinical problem is the elderly, asymptomatic patient with a harsh systolic ejection murmur who is scheduled for noncardiac surgery. For these patients, a two-dimensional Doppler echocardiographic examination allows a noninvasive assessment of the severity of stenosis57 and some quantification of contractile function (see Chapters 14 and 15). In the clinical setting, the overall picture often dictates that the anesthesiologist proceed with the originally planned operation, albeit at increased risk for perioperative cardiac morbidity (see Chapter 27). The hypertrophy initially develops in the septum and extends to the free walls, often giving a picture of concentric hypertrophy. For more than 40 years, the standard treatment has been the ventricular septal myotomy-myomectomy of Morrow, in which a small amount of muscle from the subaortic septum is resected. In one series, patients with a resting gradient of more than 40 mm Hg or a dobutamine-induced gradient of more than 60 mm Hg were included. The coronary septal branches were cannulated with a small balloon-equipped catheter. Depending on the septal branch size and area of septal hypertrophy, a dose of 2 to 5 mL of ethanol was injected slowly through the balloon catheter lumen. The cause and exact pattern of inheritance of the disease remain unknown, although it appears to be an autosomal dominant trait expressed with a high degree of penetrance. Each emphasizes some aspect of the disease that may or may not be a prominent feature of its manifestation in an individual patient. Echocardiography has unquestionably increased the number of asymptomatic patients who carry the diagnosis. Follow-up remains an important problem for cardiologists because sudden death or cardiac arrest may occur as the presenting symptom in slightly more than one-half of previously asymptomatic patients. The symptoms may share a similar pathophysiologic basis (eg, poor diastolic compliance) in the two conditions. Although cardiac arrest may be an unheralded event, some patients may have a stable pattern of angina or intermittent syncopal episodes for many years. These patients are at risk for sudden death, although those with a family history of this problem form an especially high-risk group. It also would explain the female predominance of the disease because mitral annular calcification is more common in elderly women.