Avana 50mg amex
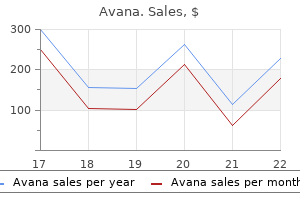
Visualization of the Lateral Meniscocapsular Junction and the Anterior Knee the arthroscope is retracted to visualize the attachment of the lateral meniscus to the capsule erectile dysfunction pills at gnc buy avana without a prescription. Surgeon and arthroscope positioning for performing arthroscopic evaluation of the posterolateral corner of the knee. The popliteus runs superiorly, and the popliteomensical fascicles attach the posterior horn of the lateral meniscus to the popliteus. The lens of the arthroscope is turned medially to visualize the anterior horn of the lateral meniscus. The anterior horn of the medial meniscus may also be seen more medially if the view is not blocked by synovium or the anterior fat pad. Medial Gutter the arthroscope is returned to the suprapatellar pouch, and then the surgeon migrates over the medial femoral condyle to the medial gutter. By lifting his or her hand and aiming the light source so that the arthroscope is angling toward the floor again, the surgeon can visualize the medial gutter (space between the medial femoral condyle and the medial capsule of the knee joint). A medial meniscal cyst and displaced medial meniscal flap tears may be visualized using this view as well. The surgeon probes for softening, fissures, and flaps and checks for plica snapping over the condyle as well. The posterior portion of the medial compartment is usually best visualized with the leg at 30 degrees, with a valgus stress applied to the knee. The medial compartment may widen abnormally with valgus stress so that significant space between the medial tibial plateau and medial femoral condyle exists. This is especially true if the meniscus lifts up off the tibial plateau, indicating significant tibial-sided medial collateral ligament laxity. The surgeon should visualize the posterior root, posterior horn, body, anterior horn, and anterior root of the meniscus. In patients who are not ligamentously lax, the posterior horn periphery may be difficult to visualize. In this case a modified Gillquist maneuver may allow better visualization of the posterior horn of the medial meniscus. Instruments angled up work best in the medial compartment because the tibial plateau is a convex surface. The arthroscope is removed from the sheath and the blunt obturator is placed in the sheath. Arthroscopic view of the posteromedial knee after Gillquist maneuver using a 70-degree arthroscope, including the medial meniscocapsular junction, medial femoral condyle, and medial gutter. Intercondylar Notch the leg is relaxed and allowed to dangle at the side of the bed. The arthroscope and probe can be situated in the intercondylar notch near the medial aspect of the lateral femoral condyle. The leg is placed in a figure 4 position with the knee flexed to 90 degrees while varus stress is applied. Ninety degrees of flexion is the optimal position for visualizing the posterolateral compartment of the knee. When the lateral compartment opens up so there is significant space between the lateral tibial plateau and lateral femoral condyle, the surgeon should suspect a posterolateral corner injury. The undersurface of the meniscus is probed and inspected, and the meniscus is tested with a hoop stress test. The perimeter of the tibial plateau is probed for flipped flap tears of the meniscus. This may require a variation of the modified Gillquist maneuver (mentioned previously). The anterior cruciate ligament is well visualized on the left, with the posterior cruciate ligament on the right more obscured by fat and synovial tissue. The posterior horn of the lateral meniscus, the posterior lateral femoral condyle, the posterior meniscal root, and the capsular attachment are visualized. Shoulder arthroscopy instrumentation and cannula systems can be helpful with more complex surgeries as well. The surgeon should talk to the patient before the surgery and perform an examination under anesthesia to confirm the pathology necessitating surgery. High pump pressures can result in fluid extravasation into the soft tissues, leading to the potential for compartment syndrome. The surgeon may want to consider gravity inflow or lower pump pressures in such situations. Older patients are more likely to sustain an injury to the collateral ligaments when varus or valgus stresses are applied to gain compartment visualization. Some patients have ligamentously tight knees, making it difficult to reach the posterior aspect of the medial and lateral tibiofemoral compartments. The surgeon should use all portals available, including the far medial and lateral as well as the posteromedial and posterolateral portals, to properly address the pathology. Although there is some variation in portal closure, we prefer a simple skin closure with a nonabsorbable monofilament suture. Regardless of suture type or technique, the surgeon should obtain a tight closure. Intra-articular and portal injection of local anesthetic may help with postoperative pain management. Deep vein thrombosis prophylaxis may be accomplished with a compression dressing from the toes to the thigh, elevation, mobilization, and ankle pumps. Regardless of postoperative weight-bearing status, most patients will require crutches for mobility. Cryotherapy has been shown to improve pain scores after knee arthroscopy and is recommended. Complications of arthroscopy and arthroscopic surgery: results of a national survey. Incidence of deep vein thrombosis after arthroscopic knee surgery: a prospective study. The synovial lining undergoes hyperplasia, most prominent in rheumatoid arthritis. Synovitis secondary to inflammatory conditions can lead to painful, swollen, and stiff knees. After medical management has been exhausted, surgery is indicated if the patient experiences continued pain, swelling, and mechanical symptoms. In rheumatoid arthritis, the cervical spine is commonly involved and must be evaluated before surgical intervention. Also, the disease is often not limited to the musculoskeletal system: patients can also have vasculitis, subcutaneous nodules, and pericarditis. During the physical examination the surgeon should look for effusion, tenderness, warmth, mass, and synovial thickening. Lachman test: assesses competence of anterior cruciate ligament Posterior drawer test: assesses competence of posterior cruciate ligament Varus stress test: assesses competence of lateral collateral ligament Valgus stress test: assesses competence of medial collateral ligament Malalignment and ligamentous insufficiencies are noted and will likely preclude arthroscopic synovectomy, given their association with joint destruction. Normal synovium supplies nutrients for the articular cartilage and produces lubricants that bathe the joint surfaces to allow smooth gliding. Histologic hallmarks of chronic synovitis include hyperplasia of the intimal lining, lymphocyte infiltration, and blood vessel proliferation. Patients with chronic synovitis can have localized or diffuse disease, depending on their underlying condition. It presents as an insidious onset of morning stiffness with multiple joint involvement. The synovitis that ensues is likely an acute autoantibody-mediated inflammatory response. Hemophilia is an X-linked deficiency of clotting factors, leading to bleeding of varying severity. The repeated hemarthroses can lead to a chronic, progressive synovial hyperplasia.
Discount avana 100 mg without prescription
The clinical diagnosis of compartment syndrome of the lower leg: are clinical findings predictive of the disorder These injuries account for about 1% of all lower extremity fractures and 5% to 10% of tibial fractures impotence 19 year old purchase avana 50mg overnight delivery. Most orthopedic surgeons will encounter these injuries during the course of their practice; thus, a basic understanding of their characteristics and their management possibilities is important for any practicing orthopedist exposed to trauma. Despite its widespread application in this respect, open treatment presents some difficulties in the management of these fractures because it can compromise the thin soft tissue envelope surrounding the distal tibia. Modern techniques in fracture care are useful in minimizing complications associated with such open treatment in this unique location. The talus is predominantly cartilage-covered and sits in the ankle mortise beneath the tibial pilon. The distinction between fracture patterns is thus attributed to a number of other associated variables, such as the amount of rotational force involved, foot (talus) position during loading, bone quality, and energy of impact. Highly comminuted articular injuries usually occur because of high-energy axial loading forces, while spiral fractures with minimal articular injury are presumed to result from lowerenergy rotational forces. True bending injuries are seen less commonly and may be caused by low- or high-energy causes. Despite the absence of a clear spectrum of injury severity, an estimation of the energy involved in a plafond fracture can be assumed from aspects other than the tibial fracture pattern itself (eg, history, soft tissue injury, associated injuries). About 20% to 40% of plafond fractures are open, reflecting the severity of the injury and the need for aggressive soft tissue management. Associated injuries should be carefully investigated because 5% to 10% of plafond fractures are bilateral, 30% of patients have ipsilateral lower extremity injuries, and 15% have injuries to the spine, pelvis, or upper extremities. Although a number of injury combinations are possible in the distal tibia, characteristic patterns can often be identified. Understanding the pattern of injury is critical to formulating an optimal treatment plan. Lower-energy metaphyseal or diaphyseal involvement of the tibia is spiral in nature with a cortical spike that can guide the reduction. Metaphyseal comminution just above the articular plafond is frequently produced under high-energy axial loading, as the talus impacts into the corresponding weight-bearing surface of the tibia. In such injuries, the anterior plafond is often comminuted and impacted into the adjacent metaphysis. The degree of anterior articular plafond involvement is related to foot (talus) dorsiflexion at the time of impact. The three major types-A (extra-articular), B (partial articular), and C (intra-articular extension with complete separation between the articular fracture fragments and the tibial shaft)-are further divided into subgroups based on the amount of fracture comminution, articular depression, and overall displacement. An anterolateral plafond fracture fragment of varying size separates with its anteroinferior tibiofibular ligament attachment. This anterolateral tubercle of Chaput requires fixation to restore the anatomy and function of the syndesmosis complex. Variable amounts of central or anterocentral articular impaction and comminution are commonly seen. High-energy injuries often result in fracture extension into the tibial diaphysis with fibula fractures proximal to the articular level. Finally, the syndesmosis will be functionally disrupted, secondary to the fibula fracture and anterolateral plafond separation. The syndesmosis anatomy and function can be restored by fixation of both the fibula and anterolateral plafond. Intra-articular injury, if present, is typically simple and without comminution or impaction. On the other end, lowenergy rotational injuries with minimal axial compression produce more straightforward spiral fractures with less soft tissue damage and a more favorable prognosis. Where a particular fracture pattern falls within this spectrum can often predict the eventual outcome of the injury. Unfortunately, determining the outcomes from these fractures is not straightforward as existing classification systems fail to clearly distinguish the spectrum of injury, making a fair comparison of published outcomes difficult to achieve. What is clear is that the surgeon maintains an important role in affecting the final outcome of these injuries, principally by designing a treatment plan that accomplishes the surgical goals set out above while minimizing the risks of complications. Established variables that clearly affect outcome include avoiding complications while restoring a congruent articular surface and the axial alignment of that articular surface relative to the shaft. Occasionally, a patient will simply miss a step on stairs or a curb; this atypical history should initiate an investigation for osteoporosis. All associated injuries must be identified and formulated into the global treatment plan. Low-energy mechanisms should alert the surgeon to suspect osteoporosis and initiate an osteoporosis evaluation. These views should be repeated after all "reductions," including application of temporizing external fixation. Occult vascular injuries, especially of the anterior tibial artery, are not uncommon in patients with high-energy plafond fractures. Description Little or no soft tissue injury Superficial abrasion and mild to moderately severe fracture configuration Deep, contaminated abrasion with local contusional damage to skin or muscle and moderately severe fracture configuration Extensive skin contusion or crushing or muscle destruction and severe fracture 3 Comorbidities such as diabetes mellitus, vascular disease, tobacco use, chronic immune or inflammatory diseases, and others may affect treatment and risk stratification. The medication profile should be assessed for blood thinners, antiinflammatories, and others that may affect surgical risk or bone metabolism. A meticulous examination with special attention to soft tissue and neurovascular status is important in the evaluation and classification of these fractures (Tables 1 and 2). With wound complication rates having a historic potential of 50%,7,14 recognition and appropriate management of the soft tissue injury cannot be overemphasized. The physician should inspect for wounds, swelling, blisters, ischemic skin, and chronic skin and vascular changes. The physician should identify open fractures and establish the "personality" of the injury. Areas of swelling or ecchymosis, breaks in the integument, and the presence or absence of fracture blisters should be identified and documented preoperatively. Findings of vascular compromise may be subtle (such as a one-vessel injury [eg, anterior tibial artery]) owing to collateral or retrograde flow patterns. Rarely, compartment syndrome may also occur, creating the need for urgent operative intervention. This scenario is uncommon, however, as the amount of energy necessary to fracture the tibial plafond typically results in significant fracture displacement and resultant instability. Some consideration may be given to nonoperative treatment in the infirm or neuropathic patient, although the risks of splinting or casting are often greater than for operative treatment. Attempts at casting or splinting unstable plafond fractures in patients considered to be poor candidates for operative treatment (eg, elderly, diabetes, vasculopathy) are fraught with risks for progressive deformity, skin breakdown, and amputation. The presence of other musculoskeletal injuries becomes a strong indication for surgical treatment to the tibia as surgical stabilization may allow for easier mobilization and rehabilitation. Reasonable nonoperative treatment options include nonweight bearing with casting or bracing until radiographic signs of healing are visualized. Regular follow-up radiographic vigilance is recommended to ensure that articular congruity and axial alignment of the lower leg remain satisfactory. Protected weight bearing must be individualized in each case, but usually at least 10 to 12 weeks is necessary to safely expect alignment to be maintained. Low-energy fractures with little comminution or soft tissue compromise may be acceptable for immediate, open surgical stabilization. In most cases, however, the degree of soft tissue injury is not fully appreciated at the time of presentation, and waiting for soft tissues to declare the extent of their injury may be prudent in these situations. This method brings the limb out to length and allows the tissues to "recover" under more physiologic conditions. If profound plantarflexion of the foot exists after reduction of the talus beneath the plafond and restoration of length, a pin can be placed in the first or fifth metatarsal (or both) to optimize positioning of the foot in neutral. If the fibula is to be repaired in this manner, its reduction must be anatomic or there may be difficulty with reducing the tibia at the time of staged pilon reconstruction. The patient should return at regular intervals between 5 days and 3 weeks after injury to schedule and undergo definitive tibial fixation. The return of skin wrinkles, blister epithelialization, and improvement in ecchymosis are several parameters to observe when staging the open tibial procedure. In most cases, the external fixation is removed at the time of internal stabilization.
Diseases
- Leigh disease
- Vasovagal syncope
- Bacterial endocarditis
- Hypomagnesemia primary
- Lowry Yong syndrome
- Selenium poisoning
- Organic mood syndrome
- Mac Dermot Winter syndrome
- Cortada Koussef Matsumoto syndrome
Buy discount avana 200 mg line
The medial trochanteric portal greatly simplifies the access to the proximal femur erectile dysfunction protocol video avana 200mg for sale, and the use of a rigid reamer system minimizes false trajectories and trochanteric iatrogenic fractures. The surgeon should avoid letting the reamer lateralize in the greater trochanter at any time. The medial trochanteric portal uses less radiation and operative time and is preferred in the supine position. Rotation of the trochanteric design nails during the first half of insertion minimizes stress on the greater trochanter and medial cortex of the femur below the lesser trochanteric region in long nail designs. The surgeon should remember to let off traction before final seating of the nail to avoid nailing the femur in distraction. Disruption of the lateral wall places more stress on the construct and should be reconstructed separately from the nail if displaced, or a locking proximal plate may be required. Guidewire insertion and drilling should always be performed with a high speed rate and a slow feed rate. This means that the guidewires and reamers bend and can be misdirected with excessive axial force during drilling. For single-device and integrated screw femoral head fixation, the surgeon should use a center-center position for the large lag screw. For two-device femoral head fixation (reconstruction), the inferior screw is placed first along the medial calcar of the femoral neck; this will ensure room for the proximal screw. Distal locking is usually recommended with a dynamic single screw for short and long nails. Two distal interlocking screws are recommended for comminuted or segmental fractures. If there are adjustments to be made, these are best made while the patient is still under anesthesia. Radiographs should reveal the entire fracture region, including the entire implant construct. Patients are mobilized to a chair upright position the day after the operative procedure. Ambulation with supervision is allowed, with weight bearing as tolerated with a walker or crutches and emphasis on heel-strike and upright balance exercises. Patients are re-evaluated with an examination and ra diographs at 2 weeks and then monthly thereafter until fracture healing is documented and the patients have maximized ambulatory capabilities, usually by 6 months after the injury. The surgeon should emphasize good nutrition and hip abductor exercises bilaterally. Patients must be counseled to report any increased swelling or respiratory distress as an emergency because of the high risk of thromboembolic disease. Functional recovery is poor in many patients, however, with more than 60% of patients failing to recover their preinjury level of function. Many patients sustain progressive collapse of the hip into varus and shortening of the leg with the current generation of sliding hip screw fixation. It is manifested by collapse of the screw and varus migration of the femoral head construct, with final cutout failure in the worst cases. This occurs to a small degree in all cases, as the sliding impaction was designed to minimize catastrophic cutout. Infection occurs in 1% to 2% of postoperative cases and is minimized by preoperative antibiotics, usually a cephalosporin class of antibiotic. The lateral trochanteric wall: a key element in the reconstruction of unstable pertrochanteric hip fractures. Reliability of classification systems for intertrochanteric fractures of the proximal femur in experienced orthopaedic surgeons. Dynamic hip screw compared with external fixation for treatment of osteoporotic pertrochanteric fractures: a prospective randomized study. Penetration of the distal femoral anterior cortex during intramedullary nailing for subtrochanteric fractures: a report of three cases. A critical analysis of the eccentric starting point for trochanteric intramedullary femoral nailing. Integrity of the lateral femoral wall in intertrochanteric hip fractures: an important predictor of a reoperation. Is there a gluteus medius tendon injury during reaming through a modified medial trochanteric portal Trochanteric versus piriformis entry portal for the treatment of femoral shaft fracture. Avoidance of malreduction in proximal femur fractures: minimally invasive nail insertion technique. Chapter 8 Open Reduction and Internal Fixation of Peritrochanteric Hip Fractures Matthew E. These fractures occur after falls in a substantial number of elderly people (estimated incidence of 250,000 fractures per year) and represent a growing percentage of healthcare expenditures annually. These fractures require operative intervention to achieve stable fracture fixation to allow immediate patient mobilization. However, owing to the pull of the musculature in this region, the fracture will heal in gross malalignment, leading to subsequent functional limitations. Complaints of hip pain before falling may indicate a preexisting pathologic process that requires further evaluation. A thorough global musculoskeletal examination of the patient is necessary because of the high incidence of associated fractures (especially of the wrist and proximal humerus) in the elderly population sustaining hip fractures from simple falls. Examination of the soft tissue overlying the lateral hip, sacrum, and heels is necessary to ensure that no pressure ulcers or abrasions have occurred in these areas. The classic physical finding in a patient with a peritrochanteric hip fracture is a short, externally rotated affected extremity. Patients may have associated musculoskeletal injuries that are not discovered until examined because of the distracting hip injury. Hip rotation assessment: Because of the muscular attachments and gravity, the lower extremity tends to rest externally rotated with a peritrochanteric hip fracture. Passive log-rolling of the leg will elicit pain (particularly with internal rotation, which tightens the hip capsule and causes pain due to the hemarthrosis). This may be an especially helpful finding in occult hip fractures with no obvious fracture deformity. The average femoral neck is anteverted between 10 and 15 degrees (range 0 to 50 degrees) and slightly translated anteriorly (5 to 8 mm) from the axis of the femoral shaft. Multiple muscle groups attach to this region of the femur: Iliopsoas: attaches to the lesser trochanter and exerts a flexion and external rotation force to the hip Abductors and short external rotators: attach to the greater trochanter Adductors: attach to the femoral shaft distal to the peritrochanteric region the blood supply to the peritrochanteric region of the femur is rich and abundant. The medial and lateral femoral circumflex arteries supply the cancellous bone of the trochanteric region through muscle attachments at the vastus origin and the insertion of the gluteus medius. Numerous factors, such as structurally weak bone, less subcutaneous padding, and slowed protective reflexes, lead to increased forces on the hip with falls in the elderly population. Pathologic lesions in the peritrochanteric region are not uncommon and may lead to pathologic fractures after relatively minor trauma. The balance between medical optimization and early operative management in this mostly elderly patient population is delicate. Although a recent study of more than 2600 patients found that a delay in surgery of up to 4 days did not increase patient mortality up to 1 year postoperatively, most studies suggest that delays of more than 2 days may increase patient mortality postoperatively. Group 3 has a fracture geometry that runs in a more transverse or reverse oblique pattern, with the fracture line exiting the lateral cortex below the vastus ridge. Implant selection for fracture fixation should be guided based on fracture pattern and patient age. Recent studies have shown improved patient outcomes and better maintenance of fracture alignment with the use of intramedullary devices in this type of fracture. Sliding hip screw devices are contraindicated in these fractures because of the high incidence of implant failure. A fixed-angle plate (such as a 95-degree blade plate or locked plate), as well as a reconstruction-type nail with a small proximal diameter, will allow for stable fracture fixation, along with preserved proximal femoral bone stock, which is helpful in cases necessitating later revision open reduction and internal fixation. Preoperative planning is vital for a satisfactory outcome when a peritrochanteric fracture is fixed with a blade plate. Multiple views of the nonfractured, contralateral hip and femur, as well as multiple traction views of the fractured hip, are required to properly plan the surgical sequence for this type of fixation. Positioning When fixing a peritrochanteric fracture with a sliding hip screw device, the patient is positioned on a well-padded fracture table, with the nonfractured leg carefully positioned in flexion and external rotation in a well leg holder.
Avana 200mg otc
The ulnohumeral articulation of the elbow is almost a true hinge joint with its constant axis of rotation through the lateral epicondyle and just anterior and inferior to the medial epicondyle erectile dysfunction increases with age discount avana 200 mg visa. The radius articulates with the proximal ulna and rounded capitellum of the distal humerus. The radiocapitellar joint and Intraosseous Vascular Anatomy There are two nutrient vessels in the lateral condyle of the developing elbow. Each vessel extends into the lateral aspect of the trochlea, with one entering proximal to the articular cartilage and the other entering posterolaterally at the origin of the capsule. Although these two vessels communicate with each other, they do not do so with the metaphyseal vasculature. The rapidly expanding capitellar epiphysis in the developing elbow thus receives its blood supply from one or two isolated trans-chondroepiphyseal vessels that enter the epiphysis posteriorly. Cross-section of the elbow showing the round, convex capitellum and the matching concave radial head. The ulnar collateral ligament complex comprises three ligaments: the anterior oblique, posterior oblique, and transverse ligaments. Metaphyseal vascular anastomoses do not make significant contributions to the capitellum until approximately 19 years of age, placing this region at risk for vascular injury. The patient usually complains of the insidious onset of poorly localized, progressive lateral elbow pain in the dominant arm. The throwing athlete may note a reduction in throwing distance or velocity or both. In advanced cases in which a fragment has become unstable or loose body formation has occurred, mechanical symptoms of elbow locking, clicking, or catching may be present. Physical examination methods On examination, there may be tenderness to palpation and crepitus over the radiocapitellar joint. Loss of 10 to 20 degrees of extension is common and mild loss of flexion and forearm rotation may also be seen. Provocative testing includes the "active radiocapitellar compression test," which consists of forearm pronation and supination with the elbow in full extension in an attempt to reproduce symptoms. The examiner should rule out radiocapitellar overload as the result of ulnar collateral ligament insufficiency using the milking maneuver, modified milking maneuver, valgus stress test, or moving valgus stress test. Most cases are seen in high-level athletes who experience repetitive valgus stress and lateral compression across the elbow (eg, overhead throwing athletes, gymnasts, weightlifters). Repeated microtrauma, such as axial loading in the extended elbow or repeated throwing that produces valgus forces on the elbow, results in increased force in the radiocapitellar joint. The repetitive microtrauma caused by these forces has been proposed to weaken the capitellar subchondral bone and result in fatigue fracture. Should failure of bony repair occur, an avascular portion of bone may then undergo resorption with further weakening of the subchondral architecture. This is consistent with the characteristic rarefaction often seen at the periphery of the lesion. The altered subchondral architecture can no longer support the overlying articular cartilage, rendering it vulnerable to shear stresses, which may lead to fragmentation. Some individuals are more susceptible than others, and this may be genetically based. The lesion frequently appears as a focal rim of sclerotic bone surrounding a radiolucent crater with rarefaction located in the anterolateral aspect of the capitellum. Radiographs, however, may not reveal the osteochondral lesions in the earlier stages. In advanced cases, articular surface collapse, loose bodies, subchondral cysts, radial head enlargement, and osteophyte formation may be seen. No reliable criteria exist for predicting which lesions will collapse with subsequent joint incongruity and which will go on to heal without further sequelae. If healing is going to take place, it usually occurs by the time of physeal closure. If healing is not going to take place, repetitive microtrauma and shear stresses to the articular surface of a lesion that has lost its subchondral support may result in further subchondral collapse and deformation with joint incongruity as well as articular cartilage injury, fragmentation, and loose body formation. In advanced cases, degenerative changes accompanied by a decreased range of motion are likely to develop. This technique, however, can potentially provide additional information regarding the status of the articular cartilage and identification of loose bodies. Ultrasonography can also help in the assessment of capitellar lesions, including early stages, but ultrasound is technician dependent. Activity modification consists of avoiding throwing activities and weight bearing on the involved arm. Short-term immobilization (less than 2 to 3 weeks, depending on symptoms) may be considered. Activity modification is continued until the radiographic appearance of revascularization and healing. The surgeon must assess the size, stability, and viability of the fragment and decide whether to remove the fragment or attempt to surgically reattach it. Arthroscopic abrasion chondroplasty or subchondral drilling may be performed to encourage healing. Although symptoms usually improve, about half of all patients will continue to have chronic pain or limited range of motion. Surgical indications for operative management of stable lesions with intact articular cartilage include radiographic evidence of lesion progression and failure of symptom resolution despite a 6-month trial of a conservative, nonoperative regimen. Unstable lesions, characterized by overlying articular cartilage injury and instability as well as collapse or disruption of the subchondral bone architecture, and those with loose bodies are usually managed surgically. They characteristically present with more advanced radiographic changes (including a well-demarcated fragment surrounded by a sclerotic margin). There is controversy as to whether simple fragment excision or reduction (open or arthroscopic) and internal fixation is the preferred treatment. Many authors advocate excision of displaced fragments, often augmented by drilling or microfracture. Critical considerations in operative planning include the size and integrity (viability) of the fragment, the subchondral architecture on the fragment and the opposing bony bed, the poten- tial for anatomic restoration of the articular surface, and the method of fixation if attempted. Internal fixation of the fragment may be performed using metallic screws, bioabsorbable screws or pins, Kirschner wire, bone pegs, and dynamic staple fixation. There have been a few reports of osteoarticular autograft or allograft plugs in the treatment of more advanced lesions, but experience with this method is limited. This is the preferred position, particularly due to the ease of posterior elbow access. The setup of the room is the same and the relative position of the elbow for the surgeon is similar between the prone and lateral positions. Some surgeons prefer this position because it is easier to convert to open surgery and easier anesthesia management; however, posterior arthroscopic access is more difficult in this position. The elbow arthroscope is brought in from the proximal anteromedial portal that provides a direct view of the anterior capitellum and radial head. Examination under anesthesia is performed to assess range of motion and ligamentous stability, particularly valgus laxity, as injury to the ulnar collateral ligament in the athlete may increase the load on the radiocapitellar joint. Diagnostic arthroscopy of the elbow is carried out, using a proximal anteromedial portal, a proximal anterolateral portal, and two posterior portals. This allows for assessment of the entire joint to ensure that loose bodies are not missed. Prone positioning is preferred because it allows easy access to the elbow, reduces the risk of sterility breaks if the arm needs to be in a finger-trap device, as needed for supine elbow arthroscopy, and arthroscopy. The patient is positioned on chest rolls and padding under the knees and feet and ankles. Complete elbow examination is mandatory to look for loose bodies: Proximal anteromedial portal Proximal anterolateral portal Posterior central portal Posterolateral portal Direct lateral portal Loose bodies tend to hide: In the proximal radioulnar joint anteriorly or the gutters In the olecranon fossa or gutters posteriorly, particularly the lateral gutter When looking at the capitellum from the proximal anteromedial portal, instrumentation (shavers, burrs, graspers, and curettes) may be accomplished using the proximal anterolateral portal. Then the arthroscope is brought in from the posterior portals to look for loose bodies. View from the proximal anteromedial portal reveals a flap of cartilage from the capitellum (left) and a slightly deformed radial head (to the right).
Discount avana 200mg with amex
Obstructing cancers or impacted faeces may paradoxically produce diarrhoea as liquid stool leaks through the mass erectile dysfunction treatment side effects order discount avana line. In toxic patients with abdominal distension and diarrhoea, toxic megacolon from overwhelming Clostridium difficile infection must be considered. Pseudo-obstruction describes colonic dysmotility that may be triggered by medications, stress and infection. Patients with pseudo-obstruction usually continue to pass stool and flatus intermittently. Abdominal examination usually reveals a soft abdomen with diffuse mild rebound tenderness without significant guarding. The catheter insertion site should be inspected for erythema or purulent drainage, although these signs may be absent. There may be mild distension and mild diffuse tenderness, but rebound and guarding are unusual. Constipation Chronic constipation causes significant diffuse abdominal pain in elderly patients. In thin patients, dense stool can be palpated in the transverse and sigmoid colon. Rarely, faecal impaction produces the clinical picture of bowel obstruction with nausea, vomiting, abdominal distension and abdominal tenderness. Right Heart Failure Chronic right heart failure may cause hepatic congestion resulting in ascites, hepatomegaly and even splenomegaly. Patients may complain of mild, diffuse or epigastric abdominal pain with associated nausea. Tricuspid stenosis is likely to be present if the pulsations occur just before ventricular systole, while tricuspid regurgitation is more likely if the pulsations occur during systole. Urinary Retention Older patients are also prone to developing acute or chronic urinary retention. Benign prostatic hyperplasia is the most common cause in men, while pelvic floor laxity with the development of a cystocele or rectocele is a common aetiology in women. Some may only report urinary frequency and overflow on questioning as they become accustomed to their chronic symptoms. Physical examination will reveal suprapubic fullness, and palpating the dome of the bladder will make the patient feel an urge to urinate. When the bladder is massively distended, there may be significant tenderness, mimicking peritonitis in some cases. The history may reveal worrisome symptoms such as a change in bowel habit, chronic bloodtinged stools or postmenopausal vaginal bleeding coupled with weight loss, night sweats and fatigue. A firm, palpable mass may be appreciated on abdominal examination if the underlying cancer is sufficiently large. If a rectal cancer is palpated on digital rectal examination, the sphincter tone should be assessed to identify involvement of the sphincter muscles. Ruptured mucoceles of the appendix or ovaries may lead to pseudomyxoma peritonei, in which extensive gelatinous fluid fills the abdomen. The disease is slow to progress, but the presentation is often similar to that of a gynaecological malignancy. Gastroenteritis Fortunately, there are many benign, self-limiting conditions that cause non-acute, generalized abdominal pain. Bacterial or viral gastroenteritis presents with vague, crampy abdominal pain, nausea, vomiting and diarrhoea. Key Points A thorough history and physical examination allow the healthcare provider to formulate a differential diagnosis upon which to base further testing and interventions if necessary. When a patient localizes their abdominal pain to a particular region, the history and physical examination should be tailored to distinguish between the conditions that commonly affect the identified region. Generalized abdominal pain has a vast differential diagnosis, but it is still possible to identify the most likely condition present using detailed history and physical examination skills. A 65-year-old woman presents with complaints of vague, poorly localized abdominal pain over the last 3 weeks. She has also noted some abdominal distension and thin, blood-tinged stools over the last 3 months. A 19-year-old woman complains of progressive right lower quadrant pain over the last 5 days. The abdomen is soft, with tenderness to deep palpation of the right lower quadrant. A 57-year-old man with hypertension and diabetes reports 4 days of right upper quadrant and epigastric pain. The patient has constitutional symptoms suggestive of malignancy and progressive obstructive symptoms without a prior screening colonoscopy. There is no jaundice to suggest cholangitis from choledocholithiasis or cholangiocarcinoma. Gallstone ileus typically presents as a small bowel obstruction, and not with right upper quadrant pain. For each of the following eponyms, select the correct site of the metastatic deposit. Each option may be used once, more than once or not at all: 1 Ovaries 2 Supraclavicular lymph node 3 Rectovesical pouch 4 Periumbilical lymph node a Blumer b Virchow c Sister Mary Joseph d Krukenberg Answers a 3 Rectovesical pouch. It should be remembered that nodal or peritoneal metastases from gastrointestinal malignancies may be palpable on physical examination. Each option may be used once, more than once or not at all: 1 Right heart failure 2 Ovarian cancer 3 Liver failure 4 Colon cancer a Ascites, gynaecomastia, caput medusae b Ascites, a firm palpable left lower quadrant mass, bloody stools c Ascites, a pulsatile liver d Ascites, and a firm adnexal mass Answers a 3 Liver failure. Patients with liver failure due to cirrhosis may demonstrate ascites, gynaecomastia and caput medusae. Patients with advanced colon cancer may have ascites, a palpable mass in the lower left quadrant and bloody stools on rectal examination. The main questions that the clinician needs to answer when evaluating a patient with abdominal pain are `Does the patient have an acute abdomen or not A detailed medical and surgical history and a thorough physical examination help to narrow the differential diagnosis. During the interview, specific characteristics of the pain need to be evaluated (Table 36. It is felt in a precise location corresponding to the somatic innervation of the overlying muscle group and corresponds to the organs that underlie the area anatomically. For example, ipsilateral subscapular or shoulder pain may be felt with diaphragmatic irritation, or pain in the groin or genitalia with the passage of a ureteral stone. The gastrointestinal contents leak into the peritoneal cavity, causing first chemical, then inflammatory and finally infectious peritoneal irritation. The perforation usually develops acutely and presents with a sudden onset of pain that rapidly builds up to maximal intensity. Inflammation may result from infectious (purulent, faeculent) or chemical (bilious) irritation of the peritoneal cavity. Depending on the disease, the peritonitis may be diffuse (from a perforated viscus) or focal (with cholecystitis or an intraabdominal abscess). Torsion is an acute twist of the organ (such as the bowel or ovary) around its axis, usually the vascular pedicle. Initially, the abdomen is soft and the tenderness is localized to the affected organ. Torsion of a segment of the gastrointestinal tract (volvulus) typically results in bowel obstruction. Bowel obstruction is associated with nausea, vomiting, constipation and distension as material fails to pass normally through the gastrointestinal tract. The abdominal pain is of a visceral type and is due to intestinal distension and peristalsis. With overdistension of the bowel, pain and abdominal tenderness may become severe and constant. With ongoing distension (as in complete bowel obstruction), bowel wall ischaemia may develop. With advancing ischaemia, signs of parietal peritoneal irritation and physical findings of guarding develop.
Syndromes
- Fatigue
- Clean the area around where urine leaves the body. Men or boys should wipe the head of the penis. Women or girls should wash the area between the lips of the vagina with soapy water and rinse well.
- Ethinyl estradiol and ethynodiol diacetate (Demulen)
- You have diabetes or a weakened immune system (for example, HIV) and have developed warts.
- Urinalysis
- Erythrocyte sedimentation rate (ESR)
- Inflammation of the blood vessels (rheumatoid vasculitis), which can lead to skin, nerve, heart, and brain problems
- Stage 2 is called early disseminated Lyme disease. The bacteria have begun to spread throughout the body.
- Fluid buildup in the brain (hydrocephalus)
Effective avana 100 mg
In one cohort of 189 patients erectile dysfunction causes smoking purchase generic avana pills, 61% of first-time dislocations occurred during sports activity. On the other hand, patients presenting with recurrent patellar instability are much more likely to continue experiencing additional dislocations than patients who present with their first dislocation. The risk of a repeat dislocation in patients presenting with a history of prior patellar dislocation is about 50% over a 2- to 5-year period. Crosby and Insall3 reported that degenerative changes were uncommon after patellar dislocation. In a more recent study, however, the incidence of degenerative changes was significantly higher at 6- to 26-year follow-up in first-time dislocators treated nonoperatively. The patellotibial and patellomeniscal ligament complex play a secondary role in restraining lateral patellar displacement, whereas the medial patellofemoral retinaculum contributes little to patellofemoral stability. Patients may report that something "popped out" medially, as the uncovered medial femoral condyle becomes prominent. The knee usually gives way secondary to pain inhibition of the quadriceps and disruption of the mechanical advantage of the extensor mechanism, and the patient falls down. Increased laxity is signified by more than two quadrants of translation; 10 mm or more of lateral translation; or the absence of an endpoint. Inability to fully translate the patella laterally because of patient guarding may lead to a falsenegative result. The patella abruptly translates laterally as the knee is fully extended, moving in an upside-down "J" pattern. A tense effusion or hemarthrosis (on aspiration) after an acute dislocation raises suspicion for an osteochondral fracture. Pivot shift also may be attempted, but may be difficult to perform on an acutely injured knee. Medial patellar instability can occur following prior lateral retinacular release. Medial patellar instability can be distinguished from lateral instability by the DeLee sign. The DeLee sign is positive if the application of a laterally directed force on the patella (which reduces the patella from its subluxated position) eliminates the pain caused by flexion of the knee. Diagnosis of extensor mechanism disruption should be obvious based on an inability to straight-leg raise and actively extend the knee. On the lateral radiograph, patellar height is measured according to the method of Caton and Deschamps (ie, the ratio between the distance from the lower edge of the patellar articular surface to the upper edge of the tibial plateau and the length of the patellar articular surface). Trochlear morphology can be assessed on the true lateral radiograph (the posterior borders of both femoral condyles are strictly superimposed). The axial patellar view may demonstrate lateral patellar subluxation or even frank dislocation. It may demonstrate medial patellar avulsion fractures, although these may be missed on plain radiographs. With the knee flexed to 30 degrees, an axial patellar view is taken with a laterally directed force applied to the medial side of the patella. Lateral offsets of 20 mm or more should be corrected with medialization of the tibial tubercle. On a true lateral radiograph, trochlear dysplasia is evident when the floor of the trochlea crosses the anterior borders of both femoral condyles (ie, the "crossing" sign). Measurement of the trochlear prominence on the lateral view according to Dejour et al. X and Y are lines tangential to the anterior and posterior cortices of the distal femoral metaphysis, respectively. Line Z crosses the most prominent point of the line of the trochlear groove (point B) and the upper aspect of the posterior border of the condyles. Line Z crosses the anterior aspect of the lateral condyle (point A) and line X (point C). Note that the floor of the trochlea lies anterior to the line tangential to the anterior cortex of the distal femur. Partial injury, with surrounding edema, to the midsubstance of the patellar retinaculum (open arrow) also is seen. A complete tear (open arrow) is seen in the patellar insertion of the medial patellar retinaculum. A large joint effusion with layering (black arrows) is present, consistent with hemarthrosis. Plain radiographs should be reviewed for the presence of trochlear dysplasia (ie, crossing sign and trochlear prominence of 3 mm or more), avulsion fractures, and loose bodies. Offset of 20 mm or more should be treated with medialization of the tibial tubercle. The patella should displace more than 10 mm laterally from the centered position with the knee flexed 30 degrees, and there should be a soft endpoint or no endpoint with the knee extended. Randomized prospective studies comparing operative and nonoperative treatment of initial patellar dislocation found no benefit from immediate medial retinacular repair. As a result, nonoperative management relies on brace protection during early progressive moblization and functional rehabilitation. After an acute dislocation, patients initially are placed in knee immobilizers for comfort and weight bearing as tolerated. Patients are encouraged to continue wearing the patellastabilizing brace during participation in pivoting activities and sports. Surgical management usually is indicated for any patient with at least two documented patellar dislocations and a physical examination demonstrating excessive lateral patellar laxity. A superolateral portal is used to facilitate viewing of the patellar articular surface and passive patellar tracking and mobility. Specifically, the patellofemoral compartment is assessed for the severity of articular cartilage injury and the presence of degenerative changes. After dissection through the subcutaneous tissue, the superficial medial patellar retinaculum (layer 1) is identified. The deep synovial layer (layer 3) can be dissected off the deep surface of the ligament to aid in inspection. The knee is then flexed to 30 degrees with the patella manually reduced in the trochlear groove. With the knee extended, a laterally directed force should reproduce a firm endpoint ("check rein" sign). Patellar mobility is assessed by applying medial and lateral forces of about 5 pounds with the knee flexed to 30 degrees. If lateral displacement is less than 5 mm or more than 10 mm, then the medial repair is retensioned. Alternatively, the origin may be approached through a separate posterior incision centered between the medial epicondyle and the adductor tubercle. The dissection is carried down through the subcutaneous tissue, and the injured medial retinacular tissue is identified. Augmented repair of avulsion-tear type medial patellofemoral ligament injury in acute patellar dislocation. Identify and isolate both the gracilis (proximal) and semitendinosus (distal) tendons from their deep aspect, ie, from within the bursal layer. Apply tension to the semitendinosus while freeing it from the crural fascia at the posteromedial corner with tissue scissors. Once all tendinous slips have been freed, harvest the semitendinosus tendon using a closed (preferred) or open tendon stripper. Baseball stitches are placed on both free ends for later graft passage throught the two patellar tunnels. The graft is prepared on the back table by first sizing the graft to 240 mm, then folding it in half, leaving a doubled graft of 120 mm. Patellar Tunnel Placement A longitudinal incision the length of the patella is made at the junction of the medial and middle thirds of the patella (in line with the medial border of the patellar tendon at the distal patellar pole). The medial 8 to 10 mm of the patella is exposed by subperiosteal dissection with a no.
Buy 200 mg avana otc
This in turn is more commonly associated with additional injuries of concerning severity erectile dysfunction treatment herbs buy avana with a mastercard. In such cases anterior external fixation may effectively manage hemodynamic instability but does not offer structural posterior stability. An immediate presurgical pelvic radiograph is obtained to assess the impact of retained bowel gas or contrast on imaging capability (if required). Preparation is done from the umbilicus to the anterior thighs, including both iliac crests. One or both lower extremities are included circumferentially as required to effect rehearsed closed reduction maneuvers. Approach Adequate fixation and accordingly proper pin placement are the principal requirements for restoring pelvic stability when applying an external fixator. Pin placement within the iliac crest is more expeditiously performed and lacks significant regional anatomic hazards. On occasion, this area may be compromised by soft tissue concerns or proximity to fracture planes. Pins and frames in this lower position may offer improved access to the abdomen and unlike pins placed within the iliac crest are less irritating to anterolateral abdominal soft tissues. The dense bone of the supra-acetabular region offers stability of fixation as good as or better than the iliac crest. Some authors investigating the biomechanical performance of these pins (supra-acetabular) demonstrated superior purchase within bone and diminished displacement of posterior portions of the pelvic ring. The device is indicated in both rotationally and vertically unstable pelvic ring injuries. It is contraindicated in lateral compression injuries and fractures involving comminution of the iliac wing or sacrum. If the device is used in lateral compression-type injuries, it may accentuate the deformity. Use of the pelvic antishock clamp with iliac wing fractures may lead to the pins traversing the fracture sites, subsequently causing internal injury. This device, applied posteriorly, may offer more stability to vertically unstable injury patterns than anteriorly applied frames. Anterior versus posterior provisional fixation in the unstable pelvis: a biomechanical comparison. These do not permit abdominal access, they require skill and familiarity, and they conceal the abdomen. The simple application of a circumferential bed sheet may be considered during the resuscitation of the hemodynamically unstable patient. The sheet may be positioned to allow assessment of abdominal and lower extremity regions. The position of sheet application is directed more at the level of the greater trochanters of the hips than more proximally at the injured pelvis. Its use in such situations may aggravate deformity, resulting in internal visceral injury and posterior neurologic compression. Pelvic circumferential compression devices may offer the simplicity and effectiveness of sheeting with the benefit of feedback controlled force. An 8- to 10-cm oblique wound adjacent and parallel to the iliac crest anteriorly is established. Dissection continues through skin and subjacent soft tissues, allowing palpation of the underlying iliac crest. Exposure of the inner and outer tables continues within the confines of the surgical wound. The first pin is placed anteriorly within the anterior pillar, about 1 to 2 cm posterior to the anterior superior iliac spine. A unicortical drill hole, no more than 1 to 2 cm deep, initiates access within the crest. The second pin and the third if applicable are inserted one fingerbreadth posterior to the previous pin. The narrow and curved profile of the crest does not allow parallel pin insertion and on occasion accommodates no more than two pins. In an effort to retain intrapelvic tamponade, pins may be introduced through a similar approach without elevation of periosseous muscular attachments. Small Kirschner wires or spinal needles are directed along the iliac fossa to orient proper pin placement. The "rule of thirds" (cross-sectional junction of inner third and outer two thirds of the crest) aids in establishing the preferential pin entry point. Alternatively, pins may be placed through percutaneous wounds subjacent to the open surgical incision. Pins should converge on the supra-acetabular region while remaining within the anterior pillar. Fluoroscopic guidance facilitates proper pin placement within the inner and outer tables. This orientation diminishes undesirable soft tissue tension around the pin on pelvic reduction and greatly enables pin tract release in the event of impending pin tract infection. After completing the skin incision, dissection continues by spreading a surgical clamp, clearing away subcutaneous fat. Through these small wounds, Kirschner wires or spinal needles can be introduced along both sides of the iliac wing. This provides a targeting method to accurately position the pins within the two tables of the ilium. Guided by the spinal needles, a soft tissue trocar assembly is introduced and situated medial of the midline to account for lateral overhang ("rule of thirds"). This requires that the drill be held more cephalad (directed caudad) than expected to allow proper position within the desired supra-acetabular bone (superior and cephalad to the acetabulum), rather than the thin bone of the ilium. The fixation pin is inserted, allowing the cortical walls of the ilium to establish direction. Stab wounds (1 to 2 cm long) are established perpendicular to the iliac crest in the direction of the umbilicus. Safe introduction and proper positioning of the pin require the assistance of fluoroscopic guidance. The open approach for pin placement begins with a vertically oriented 5- to 10-cm incision, depending on patient body habitus and prereduction pelvic deformity. A smaller transverse incision has been described in addition to entirely percutaneous techniques of pin insertion. This vertical approach begins along the lateral border of the anterior superior iliac spine, extending distally and lateral to the anterior inferior iliac spine. Tissue planes are developed with blunt dissection and the anterior inferior spine is palpated. The lateral femoral cutaneous nerve is most commonly identified medial to the anterior iliac spine. Anatomic studies have demonstrated the lateral femoral cutaneous nerve to have a variable course, often within 10 mm of inserted pins. Supra-acetabular pins should be inserted no less than 2 cm proximal to the joint to avoid intra-articular pene- tration. An obturator oblique view with slight cephalad angulation (obturator outlet view) is first obtained. The trocar assembly is positioned under fluoroscopic control superior to the hip joint. The drill, followed by the pin, is directed within the pelvis, avoiding intra-articular penetration of the hip joint. Pin angulation is typically 20 degrees medial from the vertical axis and slightly cephalad. The drill is directed toward and superior to the sciatic notch (30 to 45 degrees in the sagittal plane). The interval between the sartorius and the tensor fascia lata is established (lateral femoral cutaneous nerve protected (*).
Purchase avana with american express
Sutures are passed in 20 degrees of flexion for medial tears and 90 degrees of flexion for lateral tears erectile dysfunction prevention generic avana 200mg fast delivery. Programs should be individualized for each patient in terms of protection, weight bearing, range of motion, and return to activities. In the operating room, our patients are placed in a knee immobilizer or hinged brace locked in extension. A patient with an isolated meniscus repair will remain partially weight bearing with crutches for about 1 month. Typically, range of motion is limited to 90 degrees for the first 3 weeks for nondisplaced meniscus tears and 4 to 6 weeks for displaced bucket-handle tears. Crutches are discontinued when the patient shows good quadriceps function and no antalgia. Henning et al19 reported on 260 repairs in 240 patients with follow-up of about 2 years. On arthroscopic secondlook or arthrogram evaluation, inside-out repairs had a 62% success rate, with 17% incompletely healed and 21% not healed. Rodeo et al17 found an overall success rate of 87% with use of the outside-in technique in 90 patients. Studies have shown inside-out vertical mattress suture placement to be the strongest fixation technique, whereas the all-inside suture fixators provide excellent repair strength. The all-inside first-generation fixators have shown inferior results compared to the newer fixators. Biomechanical testing of longitudinal tears in adult porcine meniscus showed mean load to failure of inside-out vertical mattress sutures to be 80. They found seven failures in each group, but the mean time to follow-up was 68 months for the inside-out repairs and only 27 months for the all-inside group. They found an increasing rate of significant complications in addition to meniscus repair failure, including chondral scoring, fixator breakage, and joint-line irritation. There are published reports of an increased incidence of infection associated with intra-articular corticosteroid injections given intraoperatively. The most common complications associated with the insideout and outside-in techniques are traumatic neuropathy to the saphenous or peroneal nerves. The all-arthroscopic implant fixators can be associated with complications such as retained fragments that fail to resorb, broken implants, fixator migration, and inflammatory responses to the implant. A retained implant may cause further chondral damage secondary to implant abrasion. Septic arthritis following arthroscopy, clinical syndromes and analysis of risk factors. The microvasculature of the meniscus and its response to injury: an experimental study in the dog. Meniscal tears: the effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee: a preliminary report. Deteriorating outcomes after meniscal repair using the Meniscus Arrow in knees undergoing concurrent anterior cruciate ligament reconstruction: increased failure with long-term followup. Prospective comparison of arthroscopic medial meniscal repair technique: inside-out suture versus entirely arthroscopic arrows. Although meniscus preservation is always preferable, large irreparable tears often require partial or subtotal meniscal excision. Many patients will become symptomatic in the meniscaldeficient compartment as the result of increased articular cartilage contact stresses and progressive cartilage deterioration. Meniscal allograft transplantation is an option in the carefully selected patient with symptomatic meniscal deficiency. Traumatic tears often include unstable longitudinal tears in the vascular zone, which are optimal candidates for meniscal repair. Degenerative tears this is a more complex tear pattern that typically occurs in patients older than 35. Irreparable tear patterns or failed previous meniscal repairs often necessitate arthroscopic meniscal excision of the tear component. Only the peripheral third of the meniscus is vascularized (10% adjacent to popliteal hiatus). Blood is supplied via the perimeniscal capillary plexus with contributions from the superior and inferior medial and lateral geniculate arteries. Medial meniscus the medial meniscus covers a smaller percentage of medial compartment surface than the lateral meniscus. Lateral meniscus the lateral meniscus covers a relatively larger percentage of the articular surface in its respective compartment than the medial meniscus. The anterior and posterior horn attachments are closer to each other than the medial meniscus without a ligament insertion footprint interposed between the two sites. This makes the lateral meniscus more amenable to a bone bridge transplantation technique. These increases in joint contact stress often lead to premature cartilage deterioration and the development of osteoarthritis. Although patients often remain relatively asymptomatic until they have advanced degenerative changes, many patients (who tend to be younger and more active) develop pain earlier in the degenerative process. Lateral meniscectomy is considered to have a poorer prognosis than medial meniscectomy. The views expressed in this article are those of the authors and do not reflect the official policy or position of the Department of the Navy, Department of Defense, or the United States Government. Meniscus implantation decreases peak stresses and improves contact mechanics but does not restore perfect knee mechanics. A detailed history includes specific symptoms, prior injuries, and subsequent surgery. Arthroscopy pictures are helpful in determining the degree of meniscal resection and the condition of the articular cartilage. Symptomatic postmeniscectomy patients typically present with joint line pain (sometimes subtle), swelling, and pain associated with barometric pressure changes. The physical examination should focus on determining pain location, ligament stability, and alignment, assessing the cartilage, and ruling out elements of the differential diagnosis. Sharp pain on the McMurray test may indicate recurrent meniscal injury or chondral lesion versus meniscal insufficiency (dull ache). Concerns about malalignment and gait problems necessitate long-leg alignment films. The consistent relationship between meniscal size and landmarks in plain radiographs often is used by tissue banks for allograft sizing. By using measurements of the length and width of the medial and lateral tibial plateaus, McDermott et al determined that meniscal size can be predicted with a mean error rate of 5%. Upper limit is generally age 50 for highly active patients who are not good candidates for arthroplasty. Meniscal allografts are procured under strict aseptic conditions within 12 hours of cold ischemic time in accordance with standards established by the American Association of Tissue Banks for donor suitability and testing (Table 2). Weight-bearing 45-degree flexion posteroanterior view: Look for subtle joint space narrowing. Table 2 Preservation Method Fresh grafts Meniscal Allograft Preservation Methods Strengths and Weaknesses Can be stored for only up to 7 days, making graft sizing and serologic testing difficult. Despite lack of donor cell viability, allograft survival and outcome of meniscal transplant have not been affected. They maintain a cell viability of 10% to 40% and are invaded by host cells as early as 4 weeks after transplantation. Allows indefinite storage but produces alterations in the biomechanical properties and the size of the allografts. Ethylene oxide may cause soft tissue synovitis and gamma irradiation negatively affects the mechanical properties of collagen-containing tissues. For a lateral meniscal transplant, there is the option of a figure 4 position versus the leg over the table break for femoral distractor application (see Approach). For the medial meniscus, a medial parapatellar arthrotomy with posteromedial meniscus repair approach is used. Always use the bone bridge-in-slot technique; it maintains the bridge of bone between the anterior and posterior insertion sites. Mark the superior surface of the meniscus and the popliteal hiatus with a surgical marker.
Generic avana 100 mg with visa
Alternatively erectile dysfunction treatment edmonton avana 200 mg without a prescription, if arthrosis is a concern, a distal clavicle excision can be performed. The deltotrapezial fascia is meticulously closed using interrupted nonabsorbable sutures, taking care to leave the knots on the posterior aspect of the trapezius. Making clear full-thickness flaps during the approach and using tagging sutures allows for secure coverage of the grafts and clavicle. The short limb of the graft representing the conoid ligament is folded laterally and sewn to the graft base representing the trapezoid ligament. The long limb representing the trapezoid ligament can be taken laterally and used to augment the acromioclavicular ligament fixation. Alternatively, a "hockey stick" incision can be made laterally from the acromion along the midportion of the clavicle, ending in a hockey stick fashion down toward the corocoid. Periosteal flaps are elevated and a tagging suture can be placed at the medialmost aspect of the flap for accurate closure. Two heavy nonabsorbable sutures are placed at the end of the ligament using a whipstitch. If adequate arthroscopic resection has not already been performed, an oscillating saw is used to make an oblique cut on the clavicle, leaving more bone superiorly rather than inferiorly, at the level of the previously marked site. Full-thickness flaps are made from the midline of the clavicle both posteriorly and anteriorly, skeletonizing the clavicle. After a distal clavicle resection, two 2-mm unicortical drill holes are placed in the posterosuperior surface of the distal clavicle, exiting through the intramedullary canal. One clamp is turned clockwise while holding the other end until the sutures are intertwined together for the entire length of the sutures. The three sets are intertwined counterclockwise in the same fashion, resulting in a cord of nine total sutures. If ligament augmentation was used, the ligament is wrapped in a figure 8 fashion and sutured to itself using heavy nonabsorbable sutures. If the suture cord was used, the suture cord that was passed around the coracoid and through the clavicle is tied. The ends of the suture cord are unraveled and each individual suture limb is tied to prevent unraveling of the cable. The sutures are placed through the drill holes and tied over the top of the clavicle. If this is done correctly, the ligament should be taut and not overstuffed inside the pocket. Draping is similar to the open procedures, with wide exposure and the arm draped free. An anterosuperior portal is made using an outside-in technique, using a spinal needle to confirm positioning. Release of the superior glenohumeral ligament and partial release of the middle glenohumeral ligament may be required for adequate exposure. An anteroinferior portal is made near the tip of the coracoid, again with the outside-in technique, using a spinal needle to confirm positioning and ensuring that the base of the coracoid can be reached using this portal. If the 30-degree arthroscope is used, the arthroscope position is changed to the anterosuperior portal. Drilling the assembled "Adapteur Drill Guide C-Ring with the Coracoid Drill Stop and Graduated Guide Pin Sleeve" (Arthrex, Inc. With the drill stop placed at the base of the coracoid (as close to the scapula as possible), the corresponding area is marked on the superior aspect of the clavicle for the guide pin sleeve. Using the Adapteur Drill Guide C-Ring with the Coracoid Drill Stop under direct visualization, a guide pin is placed through the clavicle and coracoid, engaging the drill stop. The pin should be centered on the clavicle and the coracoid and should exit the coracoid base as close to the scapula as possible. The surgeon should take care to stop at the drill stop and not advance past the coracoid base. The power drill is detached and the cannulated drill is used as a portal to pass an 18-inch Nitinol suture passing wire. The limb of the Nitinol passing wire is brought out of the anteroinferior portal, leaving the loop superior to the clavicle. The Nitinol suture passing wire is used to deliver the white traction sutures through the clavicle and coracoid and out of the anteroinferior portal. While holding the blue TightRope suture tails, pulling on one of the white suture tails flips the oblong button to a vertical position, allowing passage of the TightRope through the clavicle and coracoid. Once past, independent pulling on the white sutures flips the oblong button back to a horizontal position, anchoring it underneath the coracoid. Suture Passage and Tying the power drill is detached, leaving the cannulated drill in place. After reduction of the clavicle, sequential pulling on the blue TightRope suture tails delivers the round button down to the superior clavicle, holding the reduction firmly. The blue TightRope suture tails of the round button are held firmly with one hand. Clavicle Reduction the surgeon pulls on the blue suture tails to advance the round button down to the clavicle. An alternative is to displace the clavicle anteriorly with a towel clip to allow access for conoid tunnel drilling. Graft management Semitendinosus ends are bulleted to allow for easy graft passage. Sutures are passed under the coracoid either from medial to lateral or lateral to medial. If passing lateral to medial, the surgeon should make sure that the medial coracoid base is exposed and should insert a Darrach retractor on the medial base to "catch" the passing device. Once the graft is passed under the coracoid, the limbs are crossed before they are passed through the clavicle tunnels. When the power driver is disconnected, the surgeon should pull the reamer out manually to ensure that the tunnel is a perfect circle and not widened by uneven reaming. The tenodesis screw is inserted anterior to the graft to equally recreate posterior coracoclavicular ligaments. These braces are recommended to counter the pull on the shoulder complex by gravity. For the first 6 to 8 weeks, the brace may be removed for grooming and supine gentle passive range of motion only. Active and passive range-of-motion exercises are started at 8 weeks after surgery. If painless range of motion is obtained, strength training is started at 12 weeks. Postoperative radiographs show that the mean difference in the coracoclavicular distance is 2. Weaver-Dunn Outcomes are difficult to compare due to the variations in the Weaver-Dunn method used and the makeup of the type of patients and severity of injury within study groups. Arthroscopic reconstruction with the TightRope System: preliminary results of an ongoing study: 29 patients with a mean age of 31 years and 6-month follow-up Mean Constant score 91. Decision making: operative versus nonoperative treatment of acromioclavicular joint injuries. The acromioclavicular capsule as a restraint to posterior translation of the clavicle: a biomechanical analysis. Anatomy of the clavicle and coracoid process for reconstruction of the coracoclavicular ligaments. Chapter 13 Arthroscopic Acromioclavicular Joint Reduction and Coracoclavicular Stabilization: TightRope Fixation Michael S. Overall incidence of the injury is 3 to 4 per 100,000 in the general population, with up to 52% of cases occurring during sporting events. Determination of the injury type will guide operative versus nonoperative management. Evaluation of the neck and a complete neurologic examination are essential, as higher-grade injuries may manifest with brachial plexus compromise. Increased deformity is commonly seen as the injury grade increases, but acutely the deformity may be masked by swelling. Pain at the posterior aspect of the shoulder or the lateral shoulder might indicate other pathology.
Buy generic avana pills
An alternative method of examination to palpate the kidney is to turn the patient onto their side with the affected side uppermost and repeat the bimanual examination erectile dysfunction treatment in bangkok discount 200mg avana overnight delivery. This physical test is unnecessary as it can cause considerable discomfort and does not elicit any further clinical information than that obtained with gentle palpation. In most cases, the only abnormality detected on physical examination is suprapubic tenderness. Complicating factors include prostatic enlargement, calculi, urinary tract malignancy, strictures, fistulas and bladder dysfunction. It is therefore important that a thorough urological examination is performed in all men who present with cystitis. Prostatitis Prostatitis is inflammation of the prostate gland that clinically presents as several syndromes with a range of clinical symptoms and investigative findings (Table 39. Prostatitis is a common urological diagnosis, with approximately 50 per cent of men experiencing symptoms of prostatitis during their lifetime. Despite this, acute bacterial prostatitis is relatively unusual in that it accounts for less than 5 per cent of cases of prostatitis. The condition classically presents with fever, chills, pelvic and back pain, urinary frequency, dysuria, urgency and occasionally urinary retention. It forms either by direct extension secondary to pyelonephritis, by haematogenous seeding from other sites of infection or as a superimposed infection in a perirenal haematoma. Patients who receive haemodialysis for polycystic kidney disease are particularly susceptible to perinephric abscess formation. Typically, a perinephric abscess presents with symptoms similar to those of acute pyelonephritis, including fever, flank and abdominal pain, weight loss, malaise and gastrointestinal symptoms. In contrast to most patients with an uncomplicated pyelonephritis, those who present with a perinephric abscess have usually been symptomatic for at least a week. Physical findings include abdominal tenderness and a flank mass, especially if the abscess is large and located in the region of the inferior pole of the kidney. During movement, the patient may experience pain on flexion of the contralateral thigh and lateral flexion of the spine. The condition requires prompt diagnosis and management as any delay can result in sepsis, irreversible renal impairment and death. Patients may present with asymptomatic bacteruria or, more commonly, infective urinary symptoms, loin pain and a fullness or mass in the flank. Treatment is with a combination of intravenous antibiotics and decompression of the renal pelvis by placing a percutaneous nephrostomy tube or less frequently an endoscopically inserted ureteric stent. Through the centre of the prostate passes the first part of the urethra (prostatic urethra), into which the prostatic glands drain and the ejaculatory ducts pass to open adjacent to the verumontanum. The examination is commonly performed with the patient in the left lateral position, with the knees and hips flexed so that the buttocks are near the edge of the examining couch or bedside. Using a generous amount of lubricant gel, the gloved index finger is inserted into the rectum and then turned to face the anterior surface, where the lobes of the prostate can be palpated through the rectal mucosa. The seminal vesicles and vasa, neither of which is palpable in the normal individual, lie cranial to the prostate. It is important to assess the size of the prostate, document the maximum transverse distance between the lobes, as well as the consistency, and check for the presence of tenderness, nodules and asymmetry. If the prostate feels boggy, this suggests the presence of a prostatic abscess, and radiological imaging should be requested. If the patient is systemically unwell, prostatic massage for bacteriology is contraindicated and only the midstream urine is collected for urine culture. Urinary retention should be managed using a suprapubic catheter to avoid instrumentation of the prostatic urethra. About 5 per cent of cases of acute bacterial prostatitis progress to chronic bacterial prostatitis, which is characterized by recurrent genitourinary and back pain with associated urinary frequency, urgency and dysuria. In contrast to acute bacterial prostatitis, the physical findings in chronic bacterial prostatitis are often normal. The diagnosis is often made by the culture of urine samples taken before and after prostatic massage. The prostatic massage should be performed during the rectal examination and often requires firm palpation to obtain prostatic secretions from the urethral meatus. Bacilli can spread into the lower urinary tract from renal granulomas that erode into the calyceal system. Involvement of the bladder usually initially manifests in the region of the ureteric orifices with fibrosis and obstruction or ureteric reflux. Tuberculosis of the epididymis and vas characteristically causes nodular beading and may result in infertility if there is bilateral obstruction. In severe cases of infection of the scrotal contents, a discharging sinus may form. Schistosomiasis It is estimated that over 200 million people worldwide are infected with organisms of the genus Schistosoma, with 97 per cent of cases of centred around North and West Africa and the Middle East. Urinary tract schistosomiasis is caused by infestation with a trematode fluke, the most common species being Schistosoma haematobium, S. Travel to endemic areas and swimming, bathing and wading in contaminated water can result in infection. Schistosomiasis is the result of direct penetration of the skin by free-swimming cercariae released from freshwater snails. The cercariae enter the venous system, traverse the pulmonary circulation and migrate to the perivesical veins. On their way, they induce a granulomatous response leading to ulceration of the mucosa on the release of the eggs into the lumen. However, most infected patients exhibit haematuria and, on cystoscopic examination, have typical perioval granulomas visible on the mucosal surface. Lower ureteric involvement is a feature of heavy or prolonged infection and leads to obstruction and hydronephrosis. Epididymitis and Orchitis Epididymitis and orchitis are inflammation, usually secondary to infection, of the epididymis and testicle, respectively. Infection of the epididymis that progresses to the adjoining testicle is referred to as epididymo-orchitis. Both pathologies typically present with scrotal pain and swelling, which develop over a couple of days, in contrast to torsion of the spermatic cord, which presents within hours. Associated symptoms include dysuria, urinary frequency, urgency and occasionally fever and urethral discharge. A common cause of isolated orchitis is mumps, in which testicular pain is usually preceded by fever, malaise and parotiditis. On examination, orchitis and epididymitis are characterized by swelling and tenderness of the respective tissue with erythematous and oedematous overlying scrotal skin. In advanced cases, a reactive hydrocele may occur, making scrotal examination more difficult. The most common presenting features are urinary frequency, nocturia, dysuria, fever, suprapubic pain, flank pain, haematuria and pyuria. Delayed diagnosis and intervention often results in significant morbidity and occasionally death. The source of the infection is usually the large bowel, urinary tract or skin of the genitalia. Patients often have multiple comorbidities that compromise the immune system, which precipitates and augments the infection. Sexually Transmitted Infections Gonorrhoea Gonorrhoea is a common infectious condition caused by the bacterium Neisseria gonorrhoeae. Approximately 10 per cent of infected men and 50 per cent of infected women are asymptomatic. The latter is usually caused by infection with Chlamydia trachomatis, Ureaplasma urealyticum, Mycoplasma hominis or Trichomonas vaginalis. In primary genital herpes, the patient typically starts to experience constitutional symptoms (fever, headache, malaise) and local symptoms (pain, dysuria, itch, urethral and vaginal discharge) after an incubation period between 1 day and 3 weeks. Recurrent genital herpes is common, occurring in up to 90 per cent of patients within the first 12 months. Infection has been associated with changes in the cervical epithelium that may progress to cervical intraepithelial neoplasia and later to invasive carcinoma. The primary route of infection is through sexual contact, but it may also be transmitted from mother to fetus in utero or at birth (congenital syphilis). During the latent phase, which may last many years, affected individuals are usually asymptomatic.