Allegra 180 mg generic
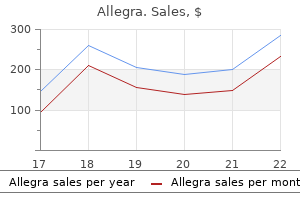
Suspicion of adrenal insufficiency may warrant the use of intravenous fluids and corticosteroids allergy symptoms from nuts purchase online allegra. The decision for surgical intervention is dictated by the location and degree of hemorrhage. If it appears to be retroperitoneal and limited by the perinephric fascia, some recommend blood replacement and careful observation in the hope of spontaneous control by tamponade; often this approach is successful, and surgery is not necessary. If paracentesis reveals blood or if blood loss exceeds replacement, exploratory laparotomy is indicated. Surgery may involve evacuation of hematoma, vessel ligation, and adrenalectomy with or without nephrectomy. When the hemorrhagic process extends to the peritoneal cavity, peritoneal exploration and evacuation of clots are indicated. At 48 hours, fever, icterus, and slow feeding were noted, and a mass was palpable abovetheleftkidney. Prognosis Small hemorrhages are probably often asymptomatic and have no associated significant morbidity, judging from the unexpected discovery of calcified adrenal glands on abdominal radiographs taken for other reasons later in infancy and childhood. If hemoperitoneum or adrenal insufficiency or both develop, the outlook depends on the speed with which diagnosis is made and appropriate therapy instituted. Adrenal function should be tested with adrenocorticotropic hormone stimulation at a later date to determine whether a normal response occurs in the urinary excretion of 17-hydroxycorticosterone. Ultrasonographicexaminationat14daysdemonstratedfluidfilled mass (arrows) superior to left kidney (K), representing adrenal hemorrhage. Etiology Factors that predispose an infant to any form of intraabdominal injury also may affect the kidneys. They include macrosomia, malpresentation (especially breech), and precipitous labor or delivery or both. Differential Diagnosis Adrenal hemorrhage must be distinguished from other causes of abdominal hemorrhage. In addition, when a mass is palpable, the differential diagnosis must include the multiple causes of flank masses in the newborn, such as genitourinary anomaly, Wilms tumor, and neuroblastoma. If the infant is large or the delivery is traumatic or breech, an adrenal hemorrhage is most likely. Neuroblastoma may be distinguished by persistent demonstration of a solid lesion on serial ultrasonographic examinations and by increased excretion of vanillylmandelic acid and Clinical Manifestations the infant may demonstrate the same signs of blood loss and hemoperitoneum noted in the other intra-abdominal lesions. Application of a Doppler probe to the renal hilus and the region of the vessels can assist in assessing renal arterial and venous flow. They include renal tumor with hemorrhage and renal vein thrombosis with infarction. Treatment After providing supportive measures similar to those used in other intra-abdominal injuries, the clinician should consider laparotomy. Possible findings at surgery include kidney rupture or transection, renal pedicle avulsion, and kidney necrosis. Use of an intraoperative Doppler probe can determine the status of renal blood flow. Fair alignment and shortening of less than 1 inch indicate satisfactory closed reduction. Fractures of the long bones in infants always result in epiphyseal stimulation; the closer the fracture to the epiphyseal cartilage, the greater is the degree of subsequent overgrowth. Prognosis Early recognition of possible renal vascular injury may lead to earlier intervention, with the potential for kidney salvage. Etiology this injury, because it was a spiral fracture, was thought to have resulted from rotational maneuvers attempted to alleviate the shoulder dystocia. An alternative explanation is compressive forces related to the shoulder dystocia itself; that is, the affected arm could have incurred an extreme degree of direct compression by the overlying symphysis pubis. Etiology the most common mechanisms responsible are difficult delivery of extended arms in breech presentations and of the shoulders in vertex presentations. Besides traction with simultaneous rotation of the arm, direct pressure on the humerus also is a factor. This may account for the occurrence of fracture of the humerus in spontaneous vertex deliveries. They are often greenstick fractures, although complete fracture with overriding of the fragments occasionally occurs. Clinical Manifestations Physical findings were limited to bruising of the affected forearm. However, as in any long bone fracture, if complete with displacement of fragments, additional findings may include swelling, deformity, tenderness, and crepitation. Treatment In the presence of bilateral fractures, casts may need to be placed on both arms. If it occurs as an isolated injury, without displacement, a radial fracture can be treated with simple immobilization. Clinical Manifestations A greenstick fracture may be overlooked until a callus is noted. A complete fracture with marked displacement of fragments presents an obvious deformity that calls attention to the injury. Often the initial manifestation of the fracture is immobility of the affected arm. Prognosis Radiographs at 2 weeks of age revealed a healed radial fracture and marked callus formation around the humeral fracture. Differential Diagnosis the differential diagnosis includes all the previously noted lesions that cause immobility of the arm. Etiology Fracture of the femur usually follows a breech delivery when the leg is pulled down after the breech is already partially fixed in the pelvic inlet or when the infant is improperly held by one thigh during delivery of the shoulders and arms. Senanayake and associates88 reported on an infant who sustained a midtrimester fracture of the femur. The infant was otherwise normal, with no other fractures and no Treatment the affected arm should be immobilized in adduction for 2 to 4 weeks. This may be accomplished by maintaining the arm in a hand-on-hip position with a triangular splint and a Velpeau bandage, strapping the arm to the chest, or application of a cast. Often an apparent dislocation is actually a fracture displaced through an epiphyseal plate. Because the epiphyseal plate is radiolucent, a fracture occurring adjacent to an unmineralized epiphysis gives a radiographic picture simulating a dislocation of the neighboring joint. Of the true dislocations, those involving the hip and knee are probably not caused by the trauma of the birth process. Most likely, they are either intrauterine positional deformities or true congenital malformations. Recently, radial head dislocation was reported as a late complication years after brachial plexus palsy. This should be done promptly, followed by immobilization of the arm in this position in a circular cast for 2 to 3 weeks. Early recognition and treatment should result in normal growth and function of the elbow. Bayne and associates7 illustrated the importance of establishing an early diagnosis when they described a term infant with a swollen, tender elbow after breech delivery. Radiographs at that time and again at 8 months of age were misinterpreted as normal. Because of several unsuccessful attempts at closed reduction, future osteotomy was required to treat this now permanent deformity. Follow-up through age 6 years revealed normal growth, with no additional fractures. The authors were unable to identify an etiology, other than possible "unnoticed maternal trauma. In addition, failure to identify and document the timing of the fracture may lead to subsequent suspicion of child abuse. Less often, the injury may not be appreciated until several days after delivery when swelling of the thigh is noted; this swelling may be caused by hemorrhage into adjacent muscle. The infant refuses to move the affected leg or cries in pain during passive movement or with palpation over the fracture site. Treatment Optimal treatment is traction-suspension of both lower extremities, even if the fracture is unilateral.
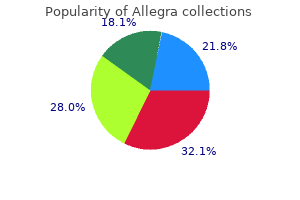
120 mg allegra overnight delivery
Preoperative and intraoperative ultrasounds are crucial to map out the placenta and determine the ideal placement of the uterine incision to optimize exposure and avoid injury to the placenta allergy grocer cheap 120 mg allegra with visa. Typically, fetal exposure is limited to the site specific to the intervention to avoid hypothermia and unnecessary manipulation of the umbilical cord, which is prone to spasm that can result in fatal fetal ischemia. A fetal extremity may also be exposed for placement of an intravenous access if indicated. The uterus should be stabilized within the maternal abdomen to minimize tension on the uterine blood vessels that could impede placental flow. At the conclusion of the procedure, the amniotic fluid is completely restored, and the uterus is closed in multiple layers using absorbable sutures. Postoperatively, the mother and fetus are monitored continuously for uterine contractions and heart rate, respectively. Patients are often dismissed with oral nifedipine as a tocolytic, and close follow-up is arranged. Open fetal surgery requires cesarean section for the current and all future pregnancies owing to the potential for uterine rupture with subsequent births. However, at the conclusion of the case, with an established airway, the fetus is delivered. Anesthetic Considerations Maintenance of uteroplacental relaxation and circulation is a central component to maternal and fetal anesthesia during fetal surgical procedures. In addition, all other tenets of anesthesia must also be considered and applied according to the level of invasiveness associated with a specific procedure to ensure adequate pain control, amnesia (when desired), and appropriate patient monitoring. In all cases, the mother is positioned supine with her left side down to minimize compression of the inferior vena cava by the gravid uterus. Routinely provided is a dose of indomethacin as a tocolytic and a prophylactic dose of cefazolin preoperatively unless there is a maternal contraindication to either medication. The maternal bladder should always be decompressed by either straight catheterization for short procedures or an indwelling bladder catheter for longer or open procedures. Special consideration for spinal anesthesia should be undertaken when an emergency cesarean section is desired by the patient for fetal distress. Spinal anesthesia can cause hypotension, which negatively impacts uteroplacental blood flow; therefore, with spinal anesthesia normotension is maintained with a phenylephrine infusion. Both phenylephrine and ephedrine are effective vasopressors that maintain maternal blood pressure while minimizing the effect on umbilical cord blood flow. When the uterus is open, amniotic fluid volume is maintained with warm, isotonic crystalloid solution to prevent compression of the umbilical cord. For open fetal cases, as the hysterotomy is being closed, the inhaled anesthetic is reduced or turned off and tocolysis with magnesium sulfate is initiated. However, the time needed for fetal levels to reach maternal levels precludes maternal anesthesia from being an adequate source of fetal anesthesia. In the fetus experiencing pain, systemic vascular resistance can increase, which may negatively augment umbilical cord blood flow. A fetal cocktail containing an opioid analgesic in combination with a non-depolarizing paralytic is frequently used, either rocuronium or pancuronium. Rocuronium and pancuronium have vagolytic effects that can offset the bradycardia that may result from opioid administration. The transplacental passage of anesthetic from mother to fetus leads to myocardial depression, which is significant because fetal cardiac output is primarily determined by heart rate. Other environmental factors such as hypothermia and umbilical cord compression can also contribute to demise. Continuous monitoring of fetal heart rate via transcutaneous pulse oximetry and intraoperative fetal echocardiography is recommended. Additional measures include fetal venous access, amnioinfusion, and continuous monitoring of amniotic fluid temperature. Prognostic Criteria Given the risks of fetal interventions, it is widely accepted that they should only be considered in those cases in which a poor prognosis is expected. In one study, survival was 100% in fetuses without liver herniation on prenatal ultrasound, whereas survival dropped to 56% when liver herniation was present. The ultimate advantage was a 75% survival rate with fetoscopic balloon occlusion in the first eight patients compared with a 38% survival rate in historical, case-matched controls managed with postnatal repair. In this study, there was no difference in survival between the tracheal occlusion group and the postnatal care group (73% versus 77%, respectively). Aspiration or thoracoamniotic shunting is reserved for fetuses with a dominant, macrocystic lesion and hydrops at a gestational age that precludes early delivery. In fact, several series have shown that thoracoamniotic shunting results in as much as a 50% to 70% volume reduction in the size of the lesion and up to a 74% survival rate. There were 16 fetuses with hydrops who underwent intervention: 13 underwent open fetal surgery, and three underwent thoracoamniotic shunting. Two of the three survived in the group that underwent shunt insertion, and eight of 13 survived in the open fetal surgery group. Preoperative ultrasound studies showed resolution of the hydrops, and resection was deferred. Predominantly macrocystic lesions are not routinely treated with steroids, as they are unlikely to respond. Maternal steroids can be redosed, but care should be taken because repeated courses of maternal steroids beyond three to five courses can result in untoward effects such as reduced birth weight. Delivery can be particularly difficult when the diagnosis has not been made prenatally, which can contribute to a traumatic delivery resulting in tumor rupture and/or life-threatening hemorrhage. Therefore, prenatal diagnosis and careful obstetrical planning are critical in the management of these fetuses. There was only a single survivor in the other 11 patients with hydrops who did not have a fetal intervention. Of the 10 patients who survived to delivery after fetal intervention, the mean gestational age was 28 weeks, and there was still a 50% neonatal mortality rate. More recently, fetal echocardiographic data have been applied to identify those patients who have early signs of heart failure in order to intervene before the late stages of heart failure manifest as hydrops. The goal of this procedure is not to achieve complete resection, but to debulk enough of the tumor to reduce the vascular shunting. Ultrasound imaging can help in the diagnosis and prognosis by demonstrating polyhydramnios, the lack of a fluid-filled stomach indicating esophageal compression, and a dilated hypopharynx. This measurement is defined as the sum of the lateral and ventral displacement of the trachea and esophagus from the ventral most aspect of the cervical spine. Furthermore, the authors found that the presence of a cervical teratoma or polyhydramnios also increased the risk for a complicated airway. Large masses that cause significant extension of the neck require delivery via cesarean section due to the risk of dystocia. There are very specific considerations that are critical to maintaining uteroplacental circulation. Airway management can be escalated using bronchoscopy or tracheostomy if laryngoscopy is not successful. The trachea is often deviated, and this displacement must be recognized prior to tracheostomy. In cases of large cystic lesions decompression of the cyst may facilitate establishing an airway by relieving any airway compression. Once an airway has been established and confirmed (usually by flexible bronchoscopy), the umbilical cord can be divided and the baby completely delivered. Postdelivery and postresection hypothyroidism and hypoparathyroidism are the most common complications, particularly with cervical teratomas. Given the small malignant potential for cervical teratomas, screening for recurrence should also be implemented by following alpha-fetoprotein levels and obtaining surveillance imaging. Cystic hygromas and other vascular malformations presenting as fetal neck masses can be difficult to manage postnatally given that these lesions have a propensity for significant cervical, oral, and intrathoracic extension, making complete resection difficult, recurrence rates high, and disfigurement likely. Secondary outcomes included neurologic function, which favored the prenatal repair group, with 42% walking without assistance at 30 months compared with 21% in the postnatal repair cohort. In addition, autonomic function is commonly affected, with an inability to control bladder or bowel function. Furthermore, premature rupture of membranes occurred in 46%, which contributed to the high rate of preterm labor. In addition to prematurity, risk to the fetus from prenatal repair included fetal demise, which occurred in 3% of the prenatal repair group. In most cases, especially when the extent of hydronephrosis is minimal, there will be complete resolution. However, 10% will have persistent or progressive disease and require postnatal evaluation.
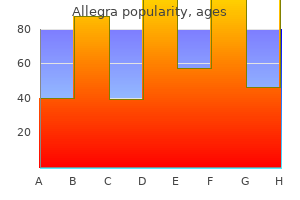
Order line allegra
There is a large body of evidence establishing a strong link between occult upper genital tract infection and spontaneous preterm delivery allergy forecast burlington vt generic 120mg allegra with amex. For example, Watts and associates investigated a series of patients with preterm labor, demonstrating that positive amniotic fluid cultures were present in 19% of women with spontaneous preterm labor and intact membranes despite these women having no clinical evidence of intrauterine infection. Organisms associated with histologic chorioamnionitis include Ureaplasma, Mycoplasma, Gardnerella, Bacteroides, and Mobiluncus species. In contrast, microbial colonization of the upper genital tract appears to play a much less important role in the initiation of parturition at or near term. There is some evidence to support each of these theories, but ascending infection is the most well accepted theory based on data from several sources. For example, in cases of congenital pneumonia, inflammation of the chorioamniotic membrane is present, and the bacteria identified are similar to those found in the genital tract. The mechanism of ascending infection appears to start with excessive overgrowth of certain organisms within the vagina and cervical canal. These microorganisms then gain access to the intrauterine cavity by infecting the decidua, the chorion, the amnion, and then finally the amniotic cavity itself. The fetus then becomes infected by aspirating or swallowing infected amniotic fluid or by direct contact with the organism within the fluid, leading to localized infections such as pneumonitis, otitis, or conjunctivitis. Alternatively, sepsis may result from maternal bacteremia, leading to placental infection with subsequent spread of organisms through the umbilical cord to the fetus. Supporting this theory is the high relative risk of premature birth in the setting of asymptomatic bacteriuria, a risk that is reduced with appropriate treatment of the infection. Intra-amniotic infection can also lead to preterm labor through less direct methods, namely stimulation of prostaglandin. This endotoxin has been found in the amniotic fluid of women with chorioamnionitis, where it has been shown to stimulate prostaglandin synthesis by the amnion and decidua. However, it is unlikely that the quantities of endotoxin within the amniotic fluid of women with chorioamnionitis are sufficient enough to stimulate prostaglandin production. Instead, these endotoxins likely stimulate production of various cytokines by the host, which in turn stimulates prostaglandin production. For example, Neisseria gonorrhoeae infection is associated with an increased risk of preterm birth, with early delivery occurring in up to 25% of patients with positive cultures as compared to 12. Although no differences have been documented in the prematurity rate, premature rupture of membranes, both term and preterm, is more common in women with positive immunoglobulin M (IgM) titers. Furthermore, Andrews and colleagues reported that patients with a diagnosis of chlamydia during pregnancy have an odds ratio of 2 for spontaneous preterm birth. Intravenous ampicillin (2 g initially, and then 1 g every 4 hours) is an acceptable alternative to penicillin G. If the isolate is sensitive to both clindamycin and erythromycin, intravenous treatment with the appropriate agent is recommended (clindamycin 900 mg every 8 hours or erythromycin 500 mg every 6 hours). Van Dyke and co-workers evaluated the implementation of the 2002 guidelines using a multistate, retrospective cohort. These results indicate that the recommendations for universal screening have been successfully implemented. Developing a universal vaccine has proved to be a daunting task, though, because of the variability of serotypes in diverse populations and geographic locations. It is a common lower genital tract infection found in approximately 20% to 40% of African-American women and 10% to 15% of white women. This condition is a clinical syndrome characterized by a decrease in the normal vaginal lactobacilli-dominant microflora and a compensatory predominance of bacteria such as Gardnerella vaginalis, Prevotella, Bacteroides, Peptostreptococcus, Mobiluncus, Mycoplasma hominis, and Ureaplasma urealyticum. Many other maternal infections or colonizations have been reportedly associated with preterm birth. One of the difficult questions to address is whether these relationships are causal or associative. Gonorrhea, chlamydia, trichomonas, syphilis, and other genital pathogens are more frequently found in women who have a spontaneous preterm birth. For example, gonorrhea, chlamydia, and syphilis have all been associated with a twofold increased risk for preterm delivery, and trichomonas has been associated with a 1. Importantly, the women affected by these infections often have other risk factors for preterm birth. Consequently, only about 15% to 20% of patients at risk for preterm birth are true candidates for treatment. A significant volume of research has focused on predicting preterm birth in this cohort of patients. Three main categories of risk factors are explored in the following paragraphs: classic predictors, biochemical predictors, and ultrasound predictors. An association has been noted between the reported presence of contractions and preterm delivery. Beginning in the early 1980s, attempts were made to combine these various factors into a risk scoring system to determine which patients were at jeopardy for preterm delivery. Creasy and co-workers combined socioeconomic factors such as age, height, weight, previous medical history, smoking, work habits, and aspects of the current pregnancy into a risk scoring system. The initial study held promise, with a positive predictive value of 38%, but subsequent studies had much lower positive predictive values in the range of 18% to 22%. One of the limitations of the Creasy risk scoring system is the emphasis placed on previous preterm deliveries, a factor which by itself elevates a patient into a high-risk category. A total score of greater than 10 places the patient at high risk for spontaneous preterm delivery. Perhaps one of the most important biochemical markers identified to date is fetal fibronectin. Clinically, it serves as a prototypic example of a marker of choriodecidual disruption. Fetal fibronectin is usually absent from cervicovaginal secretions starting from the 20th week of gestation until near term. Detection of elevated cervicovaginal levels of fetal fibronectin has therefore been strongly associated with an increased risk for preterm delivery in high-risk patients. For example, Abbott and colleagues evaluated women with preterm labor symptoms, demonstrating an increasing positive predictive value for preterm birth of 19%, 32%, 61%, and 75% with increasing fetal fibronectin thresholds of 10 ng/mL, 50 ng/mL, 200 ng/mL, and 500 ng/mL respectively. Clinically, most experts rely primarily on the negative predictive value of fetal fibronectin, using negative results to justify management of women in an ambulatory fashion, thereby limiting inpatient hospitalization to only women at the highest risk for preterm birth. Estriol is another potential biochemical marker that may be of use in predicting preterm delivery. Levels of this hormone rise throughout pregnancy, with a characteristic exponential increase 2 to 4 weeks before the spontaneous onset of labor at term. Interestingly, patients undergoing induction of labor at term fail to demonstrate this increase in estriol, indicating that it plays a role in the onset of spontaneous labor. This finding has led to the theory that salivary estriol levels may be used to identify patients at risk for preterm delivery. As with many of the other markers, no reduction in the preterm birth rate has been demonstrated with the use of these assays, but they may play a role in limiting hospitalization of women who are ultimately unlikely to deliver prematurely. Each of these markers has been shown to have a modest correlation with spontaneous preterm delivery. This peptide appears to play a role in the initiation of parturition, with elevated levels noted weeks before the onset of preterm labor. Serum levels of these collagenases remain relatively constant until the onset of labor, when a marked increase occurs. This increase appears to be exaggerated in women who deliver prematurely, with an up to eightfold greater elevation in preterm births. In addition to the collagenases, the metalloproteinases and their inhibitors have received increasing interest in regard to their role in predicting preterm birth. The activity of granulocyte elastase has been shown to be increased in the cervix in both term and preterm labor, suggesting that it may be involved in cervical ripening and degradation of fetal membranes. Given the association of occult upper genital tract infection with early spontaneous preterm birth, a variety of serum, amniotic fluid, and cervicovaginal inflammatory markers has also been evaluated as potential markers for the prediction of spontaneous preterm delivery. To safely implement the use of these biochemical markers clinically, tests with improved sensitivity and specificity are needed.
Cheap 120mg allegra amex
Mouth the mouth is a complex structure with component parts that require separate evaluation (see Chapter 76) allergy testing roseville ca buy allegra with a visa. The corners of the mouth may be downturned, as in Prader-Willi syndrome and other conditions with hypotonia. An asymmetric face during crying occurs with congenital deficiency in the depressor anguli oris muscle on one side, and this may be associated with other abnormalities, such as hemifacial microsomia and 22q11deletion/velocardiofacial/DiGeorge syndrome. A cleft upper lip is usually lateral, as in the common multifactorial cleft lip (or palate) anomaly, occurring in the position of one of the philtral ridges. The presence of pits in the lower lip associated with a cleft lip or palate, however, is suggestive of Van der Woude syndrome, which is inherited in an autosomal dominant manner. In fact, there are many diverse syndromes with cleft lip or palate that are important to identify because they may have other associated malformations and relatively high genetic risks for recurrence. Therefore, it is particularly important to evaluate the infant with cleft lip or palate carefully for evidence of other malformations to give accurate recurrence risk and prognostic information to the family. Macroglossia may be relative, as in the Pierre Robin malformation sequence, in which the primary abnormality is mandibular hypoplasia. In other cases, such as hypothyroidism, Beckwith-Wiedemann syndrome, and trisomy 21, the tongue protrudes and is enlarged. A cleft or irregular tongue or oral frenula occurs in various syndromes such as the orofaciodigital syndromes. The lower portion of the mouth is formed by the mandible, which in young infants is relatively small. An excessively small mandible is termed micrognathia, which is a feature of many syndromes. It is a characteristic of the Pierre Robin sequence, which consists of the triad of micrognathia, glossoptosis, and a U-shaped cleft palate, as opposed to the common V-shaped cleft. The Pierre Robin sequence may be part of a syndrome, such as Stickler syndrome (hereditary arthro-ophthalmopathy), and thus other anomalies and a family history must be sought. In other syndromes, the maxilla likewise may be hypoplastic, decreasing the prominence of the upper cheeks (malar hypoplasia). Neck the neck may be short, and limitation of rotation should raise the suspicion of fusion of cervical vertebrae, as in a Klippel-Feil anomaly. In these examples, the excess nuchal skin often represents resolution of a cystic hygroma that was present prenatally. The sternum itself may be unusually short, which is typical in trisomy 18, or it may be altered in shape, as is seen in pectus excavatum or pectus carinatum. The latter anomalies are commonly seen in a variety of skeletal dysplasias and connective tissue disorders (see Chapter 74). Minor external anomalies, particularly of the lower spine, include unusual pigmentary lesions, hair tufts, dimples, and sinuses. Some of these changes, such as hair tufts and sinuses above the gluteal cleft, may be an indication of a more significant deeper anomaly and require further evaluation, such as magnetic resonance imaging. A simple guide to evaluating relative extremity length is to determine where the fingertips are in relation to the thighs when the upper extremities are adducted alongside the body. In the normal infant, the fingertips fall below the hip joint in the midthigh region. A more precise and useful bedside measurement is to determine the ratio of the upper segment to the lower segment. The distance from the pubis to the heel with the leg fully extended constitutes the lower segment. By subtracting the lower segment measurement from the total length, one obtains the upper segment. In normal newborns, the ratio of the upper segment to the lower segment is about 1. A high ratio suggests relative shortening of the extremities, and a low ratio implies either unusually long extremities or a foreshortened trunk, as may occur in spondyloepiphyseal dysplasia. Paired extremities may be asymmetric in either length or overall size, suggesting either atrophy of one or hypertrophy of the other. The distinction may be difficult to make at times, although it is often evident if an extremity is unusually large or excessively small. Hypertrophy of limbs may be a manifestation of Beckwith-Wiedemann syndrome or Klippel-Trunay-Weber syndrome. Isolated hemiatrophy may occur with long-standing corticospinal tract damage as well, as in Russell-Silver syndrome. It is important to identify hemihyperplasia because individuals with this finding are at increased risk for intra-abdominal tumors, such as Wilms tumor, and thus require close monitoring throughout infancy and childhood. Foreshortening of long bones leads to various limb abnormalities, depending on the segments involved. Rhizomelia denotes proximal shortening of the limbs, such as those in achondroplasia. Mesomelia refers to shortening of the middle segment, and acromelia refers to relative shortening of the hands or feet. It results in a characteristic prune-belly appearance in Eagle Barrett syndrome (see Chapter 101). An omphalocele, in which abdominal contents protrude through the umbilical opening, may be part of the Beckwith-Wiedemann syndrome (see Chapter 95) or chromosomal abnormalities such as trisomy 13. Gastroschisis, however, is usually an isolated disruption in which the abdominal contents protrude through the periumbilical abdominal wall. Anomalies of a more minor nature, such as inguinal or umbilical hernias, occur in normal infants, but they are more frequent in various syndromes, particularly in connective tissue disorders. It also can be seen in a number of chromosomal abnormalities or as part of diabetic embryopathy. Genital ambiguity is associated with renal anomalies and an increased risk for Wilms tumor in Denys-Drash syndrome. The hands and feet have epidermal ridges and creases forming a variety of configurations. Normally, there are two deep transverse palmar creases that do not completely cross the palm. In various conditions, such as trisomy 21, there may instead be a single transverse palmar crease. A single phalangeal crease on the fifth finger, instead of the normal two, occurs as a consequence of a hypoplastic middle phalanx and results in clinodactyly (incurving of the digit). Historically, dermatoglyphics, the study of configurations of the characteristic ridge patterns of the volar surfaces of the skin, was sometimes used to aid in the diagnosis of the newborn with congenital anomalies. The scope of this subject is beyond that of this chapter, and the reader is referred to other sources. Congenital lymphedema can also be an autosomal dominantly inherited condition with variable expressivity. Significant anomalies of the underlying structure produce alterations in the normal form of the hands and feet. Absence anomalies are of various types, and the etiology and possible associated malformations vary with the type. Congenital absence of an entire hand is termed acheiria, and absence of both hands and feet is acheiropodia. Ectrodactyly refers to a partial or total absence of the distal segments of a hand or foot, with the proximal segments of the limbs more or less normal. All such anomalies are examples of terminal transverse defects and may occur sporadically or as part of a syndrome. The term ectrodactyly is frequently misused for the lobster-claw anomaly, which is best described as split hand/split foot. In this anomaly, the central rays are deficient, and there is often fusion of the remaining digits. Split hand/split foot may be seen in isolation, when it is of autosomal dominant origin, or it may be seen with other anomalies. It is useful to determine whether the defects involve primarily the radial, or preaxial, side of the limb or the ulnar, or postaxial, side.
Discount 180mg allegra mastercard
In some institutions allergy medicine overdose fatal cheap allegra 120 mg with amex, the ethics committee as a whole reviews cases; more commonly, a smaller subcommittee, an infant care review team, or an individual ethics consultant undertakes this responsibility. Ethics consultants can be very helpful in working to clarify values and build consensus. In a multidisciplinary ethics committee, team members may disagree among themselves, some members may dominate others, the committee or consultation team may not be qualified to deal with the subject matter, or the team may be overly concerned with the institutional impact of a decision rather than with the specifics of the case. Experience suggests that consultation with individual bioethicists and smaller ethics consultation teams may be of greater benefit to decision makers than the practice of "ethics by committee. When differences of opinion remain and the degree of physician moral compromise is significant, it may be advisable to involve another staff member with whom the parents have formed a therapeutic alliance. Despite these efforts, the moral problem may not be amenable to consensual resolution. Individuals involved in a failed attempt at deriving consensus may experience what Webster and Baylis88 term moral residue-"that which each of us carries with us from those times in our lives when in the face of moral distress we have seriously compromised ourselves or allowed ourselves to be compromised. Rarely physicians seek authority to make unilateral decisions via institutional or legal redress. When ethical conflict seems intractable, an institutional decision may be made to seek legal recourse. This course of action, although sometimes necessary, is generally unsatisfactory: It increases the anguish for patients and families, it destroys the parent-physician relationship, it creates (or increases) conflict between members of the health care team, and it invariably results in a significant drain on staff time and morale. Ideally institutional policies developed by the hospital ethics committee and staff should be in place to minimize the need for judicial intervention. Ethics of Research in the Neonatal Intensive Care Unit Clinical research on sick newborn infants is required to advance clinical care; improvements in the practice of clinical neonatology would not occur without such research. Research in children, let alone newborn infants, has historically been difficult to justify. Until more recently, a very protectionist view prevailed, such that studies in children were justified only if they were unsuitable in adults. This perspective seems to have changed, reflecting the move from the dominance of beneficence or protectionism toward vulnerable groups, such as infants, to a stance based more on the principle of justice as the important consideration whereby individuals who are the subject of a treatment should have an equal opportunity to share the benefits of human research. Despite the imperative for research, there are many challenges to neonatal research. It is difficult to obtain "authentic," morally valid, informed consent from parents, because this requires surrogate decision making by anxious and stressed decision makers, often following an unanticipated, acute emergency. In addition, parents are often young, healthy members of society with little prior medical exposure and familiarity with the concept of medical research. Language and cultural and religious diversity add further complexity, and the act of soliciting consent itself often further exacerbates parental stress. Parents or guardians feel beholden to the caregivers of their vulnerable infants, and in cases in which the relationship between caregiver and researcher is unclear there is the potential for "therapeutic misconception". Informed consent is enshrined as a foundational cornerstone of the ethical practice of protecting human subjects from research risk. Decisions that adults make on their own are morally robust, but decisions made for others cannot have the same degree of authenticity and are necessarily less valid in children. Golec and colleagues31 described various models of consent in neonatal research; this includes the standard model in which parents are solicited when their infant becomes eligible for a study, given written and verbal information, encouraged to ask questions, and required to sign a consent form. Other means of obtaining consent have included a steplike process of consent2; advanced consent, in which parents are approached in anticipation that their infant may meet inclusion criteria at a later date; emergency consent; and randomization without consent, in which randomization occurs before potential participants are approached, and only participants allocated to experimental therapies are informed of the trial and invited to give or withhold consent (Zelen randomization). The optimal model for consent for neonatal research is one that protects and promotes parental autonomy, is sensitive to the vulnerability and stress of the parents, and is beneficent to the infants. Golec and colleagues31 suggested that a "morally optimizing approach to research recruitment" is one in which: 1. Researchers inform parents about research in a continuing process, not as an event. No model of soliciting parental permission is perfect, and the concept of informed consent cannot be the sole safeguard protecting the welfare of the neonate in research studies. The integrity of the researcher, the role of the institutional review board, and safety and monitoring by all individuals involved help to ensure the safety and protection of neonates. Not only are nurses in a strategic position to promote parental understanding and improve the likelihood that the conditions of informed consent are met, but nurses also can help set priorities in neonatal research by playing an active role in the formulation of research policy and being "at the table" where priorities are set. In the broadest terms, these responsibilities are best discharged in the context of a constructive and mutually respectful parent-physician relationship that recognizes that patient and family values and beliefs are integral to the decision-making process. The physician also has an obligation to foster the ethical experience and education of the interdisciplinary team and that of junior staff and trainees. Ideally it should be an open, analytic, selfcritical, and responsive group providing ethically responsible care to pregnant women, newborn infants, and their families. By setting a standard of ethical responsibility for the care of newborns and families, physicians working in neonatal care send a message to society that promotes public confidence and trust in their professional practice and responsible use of expensive resources. Finally, all health care practitioners in neonatal care need to consider their own moral conscience and agency. Ethics is essentially a reflective task that requires participants to be explicit about what they believe and why, and what they value and on what grounds. Policy statement: ethical controversies in organ donation after circulatory death. Perinatal care at the limit of viability between 22 and 26 completed weeks of gestation in Switzerland. Values parents apply to decision-making regarding delivery room resuscitation for high-risk newborns. End-of-life decision-making for infants abandoned in the neonatal intensive care unit. Canadian Paediatric Society, Maternal-Fetal Medicine Committee, Society of Obstetricians and Gynaecologists of Canada. Management of the woman with threatened birth of an infant of extremely low gestational age. Appropriate use of artificial nutrition and hydration-fundamental principles and recommendations. Thinking outside the box-prenatal care and the call for a prenatal advance directive. Parent stress in neonatal intensive care unit and the influence of parent and infant characteristics. End-of-life experiences of nurses and physicians in the newborn intensive care unit. An evidence-based overview of prenatal consultation with a focus on infants born at the limits of viability. Attitudes and preferences of intensivists regarding the role of family interests in medical decision making for incompetent patients. Giving "moral distress" a voice: ethical concerns among neonatal intensive care unit personnel. Medical staff guidelines for periviability pregnancy counseling and medical treatment of extremely premature infants. Using a new analysis of the best interests standard to address cultural disputes: whose data, which values Ethics of resuscitation at different stages of life: a survey of perinatal physicians. Decisions regarding resuscitation of the extremely premature infant and models of best interest. Parental perceptions of forgoing artificial nutrition and hydration during end-of-life care. Making sense of randomization; responses of parents of critically ill babies to random allocation of treatment in a critical trial. Pharmacologic paralysis and withdrawal of mechanical ventilation at the end of life. Refusal of hydration and nutrition irrelevance of the "artificial" vs "natural" distinction. National Institute of Child Health and Human Development Neonatal Research Network: Intensive care for extreme prematurity: moving beyond gestational age. Ethical climate, ethics stress, and the job satisfaction of nurses and social workers in the United States. End of life decisions in newborns in the Netherlands: medical and legal aspects of the Groningen protocol. Death in the intensive care nursery: physician practice of withdrawing and withholding life support.
Buy allegra 180 mg with mastercard
This difference is explained by the higher immunogenicity of the platelet antigen and the smaller size of the platelets allergy forecast killeen buy allegra, which may facilitate their fetomaternal transfusion. In the usual scenario, an asymptomatic woman delivers an otherwise normal infant in an otherwise uncomplicated birth. Most neonates are asymptomatic, and the thrombocytopenia is detected by a blood count performed for other perinatal causes. In some cases, neonates present with generalized petechiae, hemorrhage into abdominal viscera, excessive bleeding after venipuncture or circumcision, or, in extreme cases, abnormal neurologic manifestations secondary to intracranial hemorrhage. The diagnosis of neonatal alloimmune thrombocytopenia involves typing platelet antigens in the newborn and in the parents to show that the mother lacks a platelet antigen that is present on the platelets of the father and the neonate. Testing the infant is generally unnecessary if the father is available for testing. Several techniques are known, and the polymerase chain reaction with sequence-specific primers is used. Older methods that measure the antibody associated with platelets lack adequate specificity, but newer enzyme-linked immunosorbent assays specifically detect the antiplatelet antibody. In antigen capture immunoassays, monoclonal antibodies directed against platelet antigens are used to identify various known platelet antigens individually, although these may be negative in maternal blood 2 to 4 weeks after delivery in 30% of the cases. Establishing the diagnosis of neonatal alloimmune thrombocytopenia has immediate importance and implications for future pregnancies. Management of the Neonate In suspected cases of neonatal alloimmune thrombocytopenia, treatment should be started on the basis of the clinical diagnosis without waiting for the results of the immunologic workup. Management depends on the gestational age of the infant, the severity of the thrombocytopenia, the presence of bleeding, and the presence of additional risk factors for bleeding. This transfusion is compatible in approximately 90% of cases of neonatal alloimmune thrombocytopenia. In any case, the neonatal platelet count should be closely monitored during the first days of life. Management of a Subsequent Pregnancy When the diagnosis of alloimmune thrombocytopenia is established, parents need to be counseled regarding risks and management of future pregnancies. The recurrence rate of neonatal alloimmune thrombocytopenia in a subsequent pregnancy is greater than 90%, and the risk for intracranial hemorrhage is the same or greater than in the previous pregnancy. The difference is, however, that in a subsequent pregnancy the patient and her caregivers are aware of the neonatal alloimmune thrombocytopenia affecting the first child. In the absence of screening (which has very low cost-effectiveness) for the presence of antiplatelet antibodies in maternal blood, the diagnosis is almost impossible without a history of neonatal alloimmune thrombocytopenia in a previous gestation. One exception is an incidental finding of intracranial hemorrhage during an ultrasound scan. Although screening procedures are not indicated to detect neonatal alloimmune thrombocytopenia, a high index of suspicion is needed in certain cases (Box 21-2). Typically, a woman presents in early pregnancy with a history of delivering an infant with neonatal alloimmune thrombocytopenia or presents with some clues to the diagnosis. Failure to treat carries the risk for intrauterine intracranial hemorrhage, which is expected to occur in 30% of cases, with 10% of affected newborns dying and 20% experiencing neurologic sequelae secondary to intracranial hemorrhage. Percutaneous umbilical vein blood sampling has a high risk for miscarriage or fetal death. The operator must be prepared to transfuse platelets if the results show a dangerously low platelet count. Because the survival of transfused thrombocytes is short, performing serial intrauterine transfusions requires repeating the procedure every week or 10 days. The authors calculated a cumulative risk for serial weekly transfusions of approximately 6% per pregnancy, indicating the need to develop less invasive approaches. Intravenous immune globulin also stabilizes endothelial cells and reduces the incidence of intracranial hemorrhage even when the fetal platelet count remains low. The authors found that fetuses with a sibling history of antenatal intracranial hemorrhage or severe thrombocytopenia (a platelet count of <20,000/) had significantly lower pretreatment platelet counts than fetuses whose siblings had less severe thrombocytopenia or postnatal intracranial hemorrhage. None of the fetuses managed by serial platelet intrauterine transfusions had intracranial hemorrhage after treatment. The results of this study suggest that the start of therapy can be stratified on the basis of the sibling history of neonatal alloimmune thrombocytopenia and support the use of maternal therapy as first-line treatment. The infant may present with cardiac, dermatologic, hepatic, and hematologic manifestations. In children with neonatal lupus, there is commonly involvement of only one or two organ systems. The skin lesions on the face and scalp, often in a distinctive periorbital distribution, may be present at birth, but usually develop within the first few weeks of life and tend to resolve in a few weeks or months without scarring. In some instances, this begins as first- or second-degree heart block and progresses to third-degree heart block. The noncardiac manifestations are transient and tend to resolve within months after birth. The recurrence rate of neonatal lupus for a mother with anti-Ro autoantibodies, which are present in almost 95% of patients, is approximately 25%. Maternal anti-Ro and anti-La antibodies and complement components are deposited in fetal heart tissues, leading to inflammation, calcification, necrosis, and fibrosis of the conducting tissue (and, in some cases, of the surrounding myocardium). The process by which maternal anti-Ro or anti-La antibodies begin and propagate inflammation that leads to scarring of the atrioventricular node is not entirely clear. Echocardiography can show the conduction defect and estimate the cardiac function. About 10% of fetuses with congenital heart block are born with hydrops fetalis and congestive heart failure, and their prognosis is poor (see Chapter 24). Neonatal mortality rate in infants born with a congenital heart block ranges from 20% to 30%; however, death may occur from late pacemaker failure later in childhood. Most neonates born with a heart block secondary to neonatal lupus require pacemaker placement in the neonatal period or later in life. Most children with neonatal lupus do not seem to develop rheumatic diseases, but follow-up has been limited to late adolescence. The most common subgroups involved in disease states are anticardiolipin antibodies, lupus anticoagulant antibodies, and antiglycoprotein I antibodies. The hypercoagulability function of these antibodies is epitomized by the fact that they cause "bleeding in the test tube but clotting in the body," referring to their involvement in pathologic clotting. These classification criteria are reported to have a sensitivity of greater than 75% and a specificity of nearly 100%. The potential mechanisms that have been proposed include interference with the function of the coagulation cascade leading to a procoagulant state, cellular immune mechanisms, and the presence of predisposing factors. A "second hit" may be necessary for the clinical manifestation of the syndrome to occur. A woman whose pregnancy fails on a prophylactic regimen should receive full anticoagulation therapy in a subsequent pregnancy. The symptoms include weakness and fatigue of the skeletal muscles of the face and extremities. Because myasthenia gravis typically affects women during reproductive years, the potential for exacerbation, respiratory failure, adverse drug response, crisis, and death during pregnancy is of great concern. Myasthenia gravis has a variable and unpredictable course during pregnancy, including exacerbation, crisis, and remission. In one study, 17% of asymptomatic patients with myasthenia gravis who were not receiving therapy before conception had a relapse; among patients receiving therapy, myasthenia gravis symptoms improved in 39%, remained unchanged in 42%, and deteriorated in 19% of the pregnancies. Therapy is based on anticholinesterase medications and plasmapheresis during a myasthenia gravis crisis. Other medications often have adverse effects on the disease, resulting in a long list of drugs that should be avoided in these patients. Plasmapheresis can be performed during pregnancy, but may be associated with preterm birth. Of special concern are cesarean delivery and the hazards of anesthesia, which might prove very stressful for these patients. Some complications of myasthenia gravis in the form of exacerbation should be anticipated during pregnancy, including anxiety and physiologic stress of pregnancy (mainly present as hypoventilation), infection, a prolonged second stage at delivery (because the patient may become exhausted and be unable to push), and the contraindication to using magnesium sulfate in patients with preeclampsia. Neonatal risks of myasthenia gravis include neonatal myasthenia gravis, prematurity, malformation, and death.
Buy allegra 120mg online
As in the 2000 Working Group Recommendations allergy shots tendonitis buy allegra 120 mg online, an increase of 30 mm Hg systolic or 15 mm Hg diastolic blood pressure from baseline in early pregnancy measurements is not included in the diagnostic criteria, because women with these changes alone are not at increased risk for adverse outcomes. In a study of hospitals managed by the Health Care America Corporation, preeclampsia was the secondleading cause of pregnancy-related admission to intensive care units after obstetric hemorrhage. Persistent blood pressure of greater than 140/90 mm Hg is considered hypertension. High blood pressure that persists 6 to 12 weeks postpartum is also classified as chronic hypertension. Diagnosis is often challenging because both blood pressure and urinary protein excretion increase toward the end of pregnancy. High clinical suspicion is warranted given the increase in maternal and fetalneonatal risks. End-organ involvement such as thrombocytopenia, elevated liver transaminase enzymes, or a rapid decline of renal function are also diagnostic of superimposed preeclampsia. Recurrence in Subsequent Pregnancies Recurrence of preeclampsia varies between 7% and 20%. This wide variation in the estimates is based on the quality of the diagnostic criteria used. The risk of recurrent preeclampsia is even higher with two prior preeclamptic pregnancies or with earlier gestational age of preeclampsia onset. A major criticism of the various classification systems is that none have been independently evaluated for the ability to identify the subgroup of women who are at increased risk of adverse pregnancy outcomes. Furthermore, there is disagreement regarding the degree of hypertension, presence or absence of proteinuria, and criteria for disease severity among the different classification systems used internationally. Recent studies have sought to develop clinically relevant definitions guided by the evidence and based on predictors of adverse outcomes. Long-Term Cardiovascular Risks A landmark study published in 1976 demonstrated that women who had eclampsia in any pregnancy after their first had a mortality risk that was two- to fivefold higher over the next 35 years compared with controls. Hypertension, dyslipidemia, insulin resistance, endothelial dysfunction, and vascular impairment have all been observed months to years after the preeclamptic pregnancy, further supporting the link between preeclampsia and cardiovascular disease. Based on these data, women with a history of preeclampsia should have ongoing, close surveillance to prevent or detect cardiovascular disease. Further investigation is needed to resolve whether common risk factors lead to the development of both preeclampsia and subsequent cardiovascular disease or whether preeclampsia itself contributes to this future risk. Epidemiology of Preeclampsia the incidence of preeclampsia is increasing in the United States and is likely related to the higher prevalence of predisposing disorders such as hypertension, diabetes and obesity, and to delay in child-bearing, as well as to the use of assisted reproductive technologies with their associated increase in multifetal gestation. In developing countries, one quarter of stillbirths and neonatal deaths are associated with preeclampsia-eclampsia. Infant mortality is three times higher in low-resource settings compared to high-income countries, largely due to the lack of neonatal intensive care facilities. The associated complications of prematurity are substantial, including neonatal deaths and serious long-term morbidity. The risk of complications is inversely associated with gestational age at delivery. Extremely premature infants (<25 weeks) have the highest mortality rate, and if they survive, they are at substantial risk for long-term issues. These include neurodevelopmental impairment such as impaired cognitive skills, motor deficits with fine and/or gross motor delay, cerebral palsy, vision problems, hearing loss, and behavioral and psychological problems, as well as recurrent hospitalization and chronic lung problems and other health problems. Pregnancy-Specific Characteristics Nulliparity is a strong risk factor, almost tripling the risk of preeclampsia. Excess placental volume, as with multifetal gestations and hydatidiform moles, is also associated with the development of preeclampsia. Maternal Characteristics Extremes of childbearing age have been associated with preeclampsia. Whereas some studies demonstrate a higher risk of preeclampsia among AfricanAmerican women,36,50 larger prospective studies that controlled for other risk factors and rigorously defined preeclampsia did not find a significant association between preeclampsia and African-American race. A family history of preeclampsia nearly triples the risk of preeclampsia, whereas a personal history of preeclampsia in a previous pregnancy increases the risk of recurrence by sevenfold. Obesity increases the overall risk of preeclampsia by approximately two- to theefold. Importantly, it is not only the late or mild forms that are increased, but also early-onset and severe preeclampsia, which are associated with greater perinatal morbidity and mortality. Paradoxically, cigarette smoking during pregnancy is associated with a reduced risk of preeclampsia. Stage 2: Maternal syndrome subtypes may facilitate research and a better understanding of pathophysiology. For example, experts have proposed a "placental preeclampsia" in which placental dysfunction and fetal growth restriction are major features. The placenta, but not necessarily the fetus (as with hydatidiform moles), is requisite for the development of preeclampsia. In normal pregnancy, the cytotrophoblast cells of the developing placenta invade the uterine spiral arteries within the decidua and myometrium of the uterus and remodel the small-caliber, highresistance arteries into large-caliber, low-resistance vessels. Persistence of the uterine artery smooth muscle renders these vessels susceptible to local and circulating vasoconstrictors as well as poor perfusion, which can result in placental ischemia-hypoxia and generation of potentially harmful reactive oxygen species. There is evidence to support the role of angiogenic factors, inflammatory cytokines, circulating placental microparticles, and oxidative stress, to name a few. Classifying preeclampsia into Immunologic/Inflammatory Factors Prior exposure to paternal antigens appears to be protective against preeclampsia, whereas less exposure to paternal antigens is associated with a higher risk of preeclampsia, such as with nulliparous women, new paternity, longer interpregnancy interval, barrier contraceptive use, and pregnancies achieved by intracytoplasmic sperm injection. The immunologic abnormalities observed with preeclampsia have been compared to transplant organ rejection. In a rodent model, injection of these antibodies results in some of the clinical features of preeclampsia, further supporting the pathogenic nature of these autoantibodies. Markers of endothelial dysfunction such as cellular fibronectin, von Willebrand factor, and thrombomodulin are also increased in blood or urine of women with preeclampsia, with some of these changes manifested weeks before the clinically recognized syndrome. In addition, there appears to be increased production of vasoconstrictors such as endothelin-1 and thromboxane as well as a decrease in vasodilators such as prostacyclin and nitric oxide. Immunologic, inflammatory, and angiogenic components are also important contributors. This is in contrast to marked lowering of vascular resistance during normal pregnancy. In an untreated group of preeclamptic women, the systemic hemodynamics were characterized as a low outputigh resistance state. Genetics Epidemiologic associations of preeclampsia with positive family history, preeclampsia in a prior pregnancy (see "Risk Factors"), or male partner who has fathered a preeclamptic pregnancy indicate a genetic basis for preeclampsia. A number of candidate genes have been studied with positive findings in small cohorts, but subsequent larger studies have not confirmed their association with preeclampsia. Genome-wide association studies have been performed and have shown modest associations, but the findings are not consistent across different populations. Recent investigations are turning toward evaluating environmental influences such as hypoxia and epigenetic modifications that may be associated with preeclampsia. Handling of proteins and other substances such as uric acid and calcium are altered. Urinary protein excretion is increased owing to the impaired integrity of the glomerular barrier as well as altered tubular handling of filtered proteins. Glomerular endotheliosis is considered a renal pathologic lesion characteristic of preeclampsia. Features include endothelial swelling, loss of fenestrations, and occlusion of the capillary lumina. Endothelial Dysfunction the endothelium, an important modulator of vascular tone, is dysfunctional in preeclampsia and contributes to the increased peripheral vascular resistance. Ex vivo investigations using subcutaneous resistance arteries have demonstrated reduced to absent flow-mediated and endothelium-dependent vasodilatory responses in women with preeclampsia relative to normal Brain Headaches, visual symptoms, and seizures are thought to be related to pathophysiologic changes in the brain. Cerebral edema and ischemia with or without hemorrhagic changes in the posterior hemispheres are often observed on computed tomography and magnetic resonance imaging. Hepatic Periportal hemorrhage and intraparenchymal hepatic infarction associated with intense vasospasm are the major hepatic histopathologic lesions associated with preeclampsia. Placenta A common finding in the preeclamptic placenta is acute atherosis, which refers to fibrinoid necrosis of the vessel wall and accumulation of lipid-laden macrophages, and a mononuclear perivascular infiltrate. The syncytiotrophoblast contains areas of apoptosis and necrosis, whereas the cytotrophoblast cells are increased in number and have higher mitotic activity; these changes are thought to be associated with hypoxia. Clinical Presentation of Preeclampsia the clinical presentation and course of disease progression can be quite variable. Approximately 25% of women will present with, or develop features of, severe preeclampsia; however, the degree of hypertension and proteinuria and presence/ absence of severe features are highly variable (see Table 18-1).
Buy discount allegra online
It enters the anterior edge of the tentorium cerebelli allergy shots skin reactions order allegra no prescription, continues in an anterior direction in the lateral wall of the cavernous sinus. The trigeminal nerve exits from the anterolateral surface of the pons as a large sensory root and a small motor root. These roots continue forward out of the posterior cranial fossa and into the middle cranial fossa by passing over the medial tip of the petrous part of the temporal bone. In the middle cranial fossa the sensory root expands into the trigeminal ganglion. The ganglion is in a depression (the trigeminal depression) on the anterior surface of the petrous part of the temporal bone in a dural cave (the trigeminal cave). The motor root is below and completely separate from the sensory root at this point. It arises in the midbrain and is the only cranial nerve to exit from the posterior surface of the brainstem. After curving around the midbrain, it enters the inferior surface of the free edge of the tentorium cerebelli, continues in an anterior direction in the lateral wall of the cavernous sinus. Ophthalmic nerve [V1] the ophthalmic nerve [V1] passes forward in the dura of the lateral wall of the cavernous sinus. The ophthalmic nerve [V1] carries sensory branches from the eyes, conjunctiva, and orbital contents, including the lacrimal gland. It also receives sensory branches from the nasal cavity, frontal sinus, ethmoidal cells, falx cerebri, dura in the anterior cranial fossa and superior parts of the tentorium cerebelli, upper eyelid, dorsum of the nose, and the anterior part of the scalp. Maxillary nerve [V2] the maxillary nerve [V2] passes forward in the dura mater of the lateral wall of the cavernous sinus just inferior to the 445 Head and Neck ophthalmic nerve [V1]. The maxillary nerve [V2] receives sensory branches from the dura in the middle cranial fossa, the nasopharynx, the palate, the nasal cavity, teeth of the upper jaw, maxillary sinus, and skin covering the side of the nose, the lower eyelid, the cheek, and the upper lip. Mandibular nerve [V3] the mandibular nerve [V3] leaves the inferior margin of the trigeminal ganglion and leaves the skull through the foramen ovale, and enters the infratemporal fossa. The motor root of the trigeminal nerve also passes through the foramen ovale and unites with the sensory component of the mandibular nerve [V3] outside the skull. Thus the mandibular nerve [V3] is the only division of the trigeminal nerve that contains a motor component. Outside the skull the motor bers innervate the four muscles of mastication (temporalis, masseter, and medial and lateral pterygoids), as well as the tensor tympani, the tensor veli palatini, the anterior belly of the digastric, and the mylohyoid muscles. The mandibular nerve [V3] also receives sensory branches from the skin of the lower face, cheek, lower lip, anterior part of the external ear, part of the external acoustic meatus and the temporal region, the anterior twothirds of the tongue, the teeth of the lower jaw, the mastoid air cells, the mucous membranes of the cheek, the mandible, and dura in the middle cranial fossa. The motor and sensory roots cross the posterior cranial fossa and leave the cranial cavity through the internal acoustic meatus. Near this point the nerve enlarges as the geniculate ganglion, which is similar to a spinal ganglion containing cell bodies for sensory neurons. It arises from the brainstem between the pons and medulla and passes forward, piercing the dura covering the clivus. Continuing upward in a dural canal, it crosses the superior edge of the petrous temporal bone, enters and crosses the cavernous sinus. The two divisions combine into the single nerve seen in the posterior cranial fossa within the substance of the petrous part of the temporal bone. Within or immediately outside the jugular foramen are two ganglia, the superior (jugular) and inferior (nodose) ganglia, which contain the cell bodies of the sensory neurons in the vagus nerve [X]. It is a unique cranial nerve because its roots arise from motor neurons in the upper ve segments of the cervical spinal cord. These bers leave the lateral surface of the spinal cord and, joining together as they ascend, enter the cranial cavity through the foramen magnum. It then descends in the neck to innervate the sternocleidomastoid and trapezius muscles from their deep surfaces. Within the jugular foramen, and before exiting from it, the rootlets merge to form the glossopharyngeal nerve. This branch re-enters the temporal bone, enters the middle ear cavity, and participates in the formation of the tympanic plexus. Within the middle ear cavity it provides sensory innervation to the mucosa of the cavity, pharyngotympanic tube, and mastoid air cells. As part of the vagus nerve [X], they are distributed to the pharyngeal musculature innervated by the vagus nerve [X] and are therefore described as being part of the vagus nerve [X]. It arises as several rootlets from the anterior surface of the medulla, passes laterally across the posterior cranial fossa and exits through the hypoglossal canal. This nerve innervates the hyoglossus, styloglossus, and genioglossus muscles and all intrinsic muscles of the tongue. Thus an understanding of the unique organization of the various structures between the superciliary arches superiorly, the lower edge of the mandible inferiorly, and as far back as the ears on either side- the area de ned as the face-is particularly useful in the practice of medicine. They are in the super cial fascia, with origins from either bone or fascia, and insertions into the skin. This organizational arrangement into functional groups provides a logical approach to understanding these muscles. Orbital group Two muscles are associated with the orbital group-the orbicularis oculi and the corrugator supercilii. The orbicularis oculi is a large muscle that completely surrounds each orbital ori ce and extends into each eyelid (Table 8. The second muscle in the orbital group is the much smaller corrugator supercilii (Table 8. Procerus Trans vers e part Nas alis Alar part Nasal group Three muscles are associated with the nasal group-the nasalis, the procerus, and the depressor septi nasi (Table 8. The largest and best developed of the muscles of the nasal group is the nasalis, which is active when the nares are ared (Table 8. The procerus is a small muscle super cial to the nasal bone and is active when an individual frowns (Table 8. The orbicularis oris is a complex muscle consisting of bers that completely encircle the mouth. The buccinator forms the muscular component of the cheek and is used every time air expanding the cheeks is forcefully expelled (Table 8. They include the orbicularis oris and buccinator muscles, and a lower and upper group of muscles. Levator labii s uperioris alaeque nas i Levator anguli oris Levator labii s uperioris Zygomaticus minor Zygomaticus major Modiolus Ris orius Platys ma Buccinator Depres s or anguli oris Depres s or labii inferioris Mentalis Orbicularis oris Lower group of oral muscles Parotid duct (cut) the muscles in the lower group consist of the depressor anguli oris, depressor labii inferioris, and mentalis (Table 8. The depressor labii inferioris depresses the lower lip and moves it laterally, and the mentalis helps position the lip when drinking from a cup or when pouting. Upper group of oral muscles Buccinator mus cle Pterygomandibular raphe Superior pharyngeal cons trictor mus cle the muscles of the upper group of oral muscles consist of risorius, zygomaticus major, zygomaticus minor, levator labii superioris, levator labii superioris alaeque nasi, and levator anguli oris (Table 8. The risorius helps produce a grin; the zygomaticus major and zygomaticus minor help produce a smile; the levator labii superioris deepens the furrow between the nose and the corner of the mouth during sadness; the levator labii superioris alaeque nasi may assist in aring the nares; and the levator anguli oris elevates the corner of the mouth and may help deepen the furrow between the nose and the corner of the mouth during sadness. The platysma is a large, thin sheet of muscle in the super cial fascia of the neck. It tenses the skin of the neck and can move the lower lip and corners of the mouth down. Three muscles associated with the ear are also in the group of "other muscles of facial expression. The occipitofrontalis is the nal muscle in this category and is associated with the scalp (Table 8. Parotid gland the parotid glands are the largest of the three pairs of main salivary glands in the head and numerous structures pass through them. They are anterior to and below the lower half of the ear, super cial, posterior, and deep to the ramus of mandible. They extend down to the lower border of the mandible and up to the zygomatic arch. Posteriorly they cover the anterior part of the sternocleidomastoid muscle and continue anteriorly to halfway across the masseter muscle. Maxillary Trans vers e facial artery and vein Superficial temporal artery and vein artery and vein Anterior auricular Pos terior auricular.