Purchase genuine cialis super active line
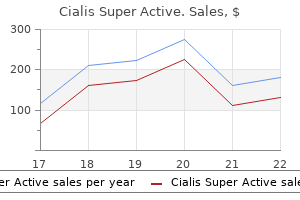
This provides an interesting example of how a highly toxic drug with selectivity toward a specific population (pregnant women) can be used relatively safely with proper precautions impotence with condoms purchase cialis super active once a day. The population at risk for the potential teratogenic effects of thalidomide (all women of childbearing age) was required to use 2 forms of birth control, and also have a negative pregnancy test within 24 hours of beginning therapy, and periodically thereafter. Remarkably, after 6 years of use, only 1 patient actually received thalidomide during her pregnancy. She initially tested negative at the beginning of therapy; on a subsequent test she was identified as positive, and the drug was stopped. Thus, a clear understanding of mechanism of action led to the development of strict prescribing guidelines and patient monitoring, thereby allowing a potentially dangerous drug to be used safely and effectively to treat disease in tens of thousands of patients who would otherwise not have benefited from the therapeutic actions of the drug (Lary et al. In addition to aiding directly in the identification, treatment, and prevention of chemical toxicity, an understanding of the mechanisms of toxic action contributes to the knowledge of basic physiology, pharmacology, cell biology, and biochemistry. The advent of new technologies in molecular biology and genomics now provides mechanistic toxicologists with the tools to explore exactly how humans may differ from laboratory animals in their response to toxic substances. These same tools are also being utilized to identify individuals who are genetically susceptible to factors in the environment or respond differently to a chemical exposure. For example, a small percentage of the population genetically lacks the ability to detoxify the chemotherapeutic drug, 6-mercaptopurine, used in the treatment of some forms of leukemia. Young children with leukemia who are homozygous for this genetic trait (about 1 in 300) may experience serious toxic effects from a standard therapeutic dose of this drug (Weinshilboum et al. Numerous genetic tests for polymorphisms in drug-metabolizing enzymes and transporters are now available that can identify genetically susceptible individuals in advance of pharmacological treatment (Eichelbaum et al. Moving from the single, "candidate gene" approach to genome-wide studies has led to the development of the relatively new fields of pharmacogenomics and toxicogenomics. A descriptive toxicologist is concerned directly with toxicity testing, which provides information for safety evaluation and regulatory requirements. The appropriate toxicity tests (as described later in this chapter and other chapters) in cell culture systems or experimental animals are designed to yield information to evaluate risks posed to humans and the environment from exposure to specific chemicals. The concern may be limited to effects on humans, as in the case of drugs and food additives. Such studies are also a key component of risk assessments that are used by regulatory toxicologists. The development of so-called omics technologies (genomics, transcriptomics, proteomics, metabonomics/ metabolomics, etc) forms the basis of the subdiscipline of toxicogenomics. The application of these technologies to toxicity testing is in many ways "descriptive" in nature, yet affords great mechanistic insights in to how chemicals produce their toxic effects. This exciting area of toxicology is discussed in more detail later in the chapter. This regulation provides direction and financial support for the cleanup of waste sites that contain toxic chemicals that may present a risk to human health or the environment. Regulatory toxicologists are also involved in the establishment of standards for the amount of chemicals permitted in ambient air, industrial atmospheres, and drinking water, often integrating scientific information from basic descriptive and mechanistic toxicology studies with the principles and approaches used for risk assessment (see Chap. In addition to the above categories, there are other specialized areas of toxicology such as forensic, clinical, and environmental toxicology. Forensic toxicology is a hybrid of analytic chemistry and fundamental toxicological principles. It is concerned primarily with the medicolegal aspects of the harmful effects of chemicals on humans and animals. The expertise of forensic toxicologists is invoked primarily to aid in establishing the cause of death and determining its circumstances in a post-mortem investigation (see Chap. Clinical toxicology designates an area of professional emphasis in the realm of medical science that is concerned with disease caused by or uniquely associated with toxic substances (see Chap. Generally, clinical toxicologists are physicians who receive specialized training in emergency medicine and poison management. Efforts are directed at treating patients poisoned with drugs or other chemicals and at the development of new techniques to treat those intoxications. Public information about treatment and prevention is often provided through the national network of poison control centers. Environmental toxicology focuses on the impacts of chemical pollutants in the environment on biological organisms. Although toxicologists concerned with the effects of environmental pollutants on human health fit in to this definition, it is most commonly associated with studies on the impacts of chemicals on nonhuman organisms such as fish, birds, terrestrial animals, and plants. Ecotoxicology is a specialized area within environmental toxicology that focuses more specifically on the impacts of toxic substances on population dynamics in an ecosystem. The transport, fate, and interactions of chemicals in the environment constitute a critical component of both environmental toxicology and ecotoxicology. Knowledge about the toxicological effects of a compound affects consumer products, drugs, manufacturing processes, waste cleanup, regulatory action, civil disputes, and broad policy decisions. The expanding influence of toxicology on societal issues is accompanied by the responsibility to be increasingly sensitive to the ethical, legal, and social implications of toxicological research and testing. The convergence of multiple elements has highlighted the evolving ethical dynamics of toxicology. First, experience and new discoveries in the biological sciences have emphasized our interconnectedness with nature and the need for well-articulated visions of human, animal, and environmental health. One vision is that we have "condition(s) that ensure that all living things have the best opportunity to reach and maintain their full genetic potential" (Gilbert, 2005a). Second, we have experience with the health consequences of exposure to such things as lead, asbestos, and tobacco, along with the detailed mechanistic research to understand the longterm risks to individuals and society. This has precipitated many regulatory and legal actions and public policy decisions, not to mention costly and time-consuming lawsuits. Third, we have an increasingly well-defined framework for discussing our social and ethical responsibilities. There is growing recognition that ethics play a crucial role in public health decision making that involves conflicts between individual, corporate, and social justice goals (Callahan and Jennings, 2002; Kass, 2001; Lee, 2002). Fourth is the appreciation that all research involving humans or animals must be conducted in a responsible and ethical manner. Fifth is managing both the uncertainty and biological variability inherent in the biological sciences. Decision making often includes making judgments with limited or uncertain information, which often includes an overlay of individual values and ethics. Finally, individuals involved in toxicological research must be aware of and accountable to their own individual biases and possible conflicts of interest and adhere to the highest ethical standards of the profession (Maurissen et al. The essence of toxicology is to understand the effects of chemicals on the biotic community. Environmental justice is now an important component of numerous communitybased programs of interest, and is relevant to the field of toxicology (Nweke, 2011). There is growing recognition of the direct financial and indirect costs to individuals and society from environmental exposures that are not equally distributed across society (Landrigan et al. The 4 principle of biomedical ethics-respect for autonomy, beneficence (do good), nonmaleficence (do no harm), and justice (be fair)-became well established as a basis for decision making in health care settings (Beauchamp and Childress, 1994). These principles formed the basis of rules and regulations regarding the conduct of human research. The demands of ethics and science made it clear that the highest standards of care produced the best results in both human and animal research. Rules and regulations regarding the housing and conduct of animal studies evolved similarly. Professional toxicology societies now require their members to adhere to the highest ethical standards when conducting research with humans or animals. A further refinement and expansion of biomedical ethical principles is the development of communitybased participatory research that takes in to consideration community needs to ensure the best results and benefit to the community (Arcury et al. A glance at the daily newspaper confirms the number of current, sometimes controversial issues that are relevant to the field of toxicology. Decisions and action are often demanded or required even when there is a certain level of uncertainty in the toxicological data. The classic example of this challenge is establishing causation of the health effects of tobacco products. In part to address issues related to the health effects of tobacco products, Hill, a distinguished epidemiologist, defined a set of guidelines for evaluating "causation"-for example, whether a causal connection between a particular "exposure" and a particular outcome, condition, or disease can be scientifically established (Hill, 1965). Strength of association (relationship between independent and dependent variables) 2. Specificity of association (cause is tightly linked to an outcome) Although the guidelines provided by Hill were originally designed for interpretation of epidemiological data, they are equally applicable to establishing causation in toxicology, which often relies on a mix of both epidemiological and toxicological data.
Cheap 20 mg cialis super active with mastercard
The limited volume of fluid administered with the oral medication is not associated with an increased risk for aspiration pneumonitis tramadol causes erectile dysfunction order cialis super active 20 mg fast delivery. The primary disadvantages of oral sedation are the slow onset, variable response, and prolonged recovery. Injecting a sedative agent in to the back of the throat with a needle-free syringe (when the child does not otherwise accept the medication) has also been associated with adverse consequences. It has been theorized that the drug intended for orogastric administration can be inadvertently aspirated by the crying child. The intranasal route was initially proposed for pediatric sedation because it was believed to avoid first-pass degradation, be rapid in onset, and be less traumatic than the other routes that possessed these same benefits. Medications administered intranasally do result in a rapid rise in the plasma level of a drug. This occurs because the nasal cavity, which functions to warm and cleanse nasal respirations, has a relatively extensive surface area with a thin nasal mucosa and an abundance of capillaries that facilitate the absorption of drug. The intranasal route, although initially thought to be less traumatic than alternative routes, is frequently not well accepted by children. The volume of medication used frequently results in a portion passing in to the pharynx and being swallowed. Therefore, the unpleasant taste of the medication is not avoided, and the drug is subject to firstpass hepatic degradation. Midazolam is the most commonly intranasally administered medication, but the acidic pH is irritating to the nasal mucosa. The minimum epidermal barrier and the vascular supply provide an environment that promotes relatively rapid absorption of drugs. Oral transmucosal administration of a drug also has the advantage of avoiding hepatic first-pass degradation. Transmucosal administration requires cooperation of the patient to keep the drug in contact with the oral mucosa. Induction will be achieved with a single breath, and spontaneous ventilation will resume once a state of general anesthesia is achieved. Some clinicians advocate maintaining the general anesthesia by continuing the administration of the potent vapor agent via a traditional nasal hood. Such an occurrence would necessitate the interruption of the procedure to replace the full facemask to increase the alveolar concentration of the inhalational agent. Although the continued administration of the vapor agent via a nasal hood is not contraindicated, it may result in excessive environmental pollution, even with a scavenger device that is a component of the nasal hood. To avoid these potential problems, especially for longer procedures, the establishment of intravenous access is recommended. The vasodilatory effects of the potent agent may optimize conditions for establishing intravenous access. Once access is set, anesthetic depth can be maintained with intravenous anesthetic agents. The odor may also be minimized if the child breathes through the nose as opposed to the mouth. In addition, inhalation induction is also dependent on the child accepting the facemask. Techniques such as asking the child to inflate a balloon may be employed to distract the child. Any need for mild restraint should be explained to the parent and may be used to facilitate induction in the younger child. If excessive physical restraint is necessary, an alternative technique should be considered. The intramuscular route of administration approximates the rapidity and predictability of onset of intravenous administration. However, for the uncooperative child, it may be the least traumatic method of inducing anesthesia. Four anatomic regions are used for intramuscular administration of drugs: the deltoid muscle, the vastus lateralis muscle, the ventrogluteal area, and the superior lateral aspect of the gluteus maximus muscle. These sites have been identified because they have minimal numbers of nerves and large blood vessels as well as adequate bulk to accommodate the volume of the injected medication. Absorption and onset are also affected by the ionization of the drug and the vehicle in which it is dissolved. At the present time, the only available lozenge that has an acceptable flavor and is commercially available is fentanyl citrate. Palatability can be improved by mixing these medications with a flavored solution that increases their volume; thus, the solution will be bitter or the volume will be excessive, neither of which is advantageous for the transmucosal administration of a liquid/solution. Many, if not most, pediatric patients expectorate the medication or prematurely swallow the liquid medication that is placed within the oral cavity as opposed to keeping it there. Rectal drug administration has been used for the administration of antiemetics, antipyretics, and analgesics to both adults and pediatric patients. Many sedative drugs that are usually administered intravenously, intramuscularly, or orally can be administered rectally. For example, rectal administration of diazepam is an acceptable route for the treatment of seizures. Its blood supply is derived from the inferior rectal arteries and is drained via the superior, middle, and inferior rectal veins. The superior rectal vein drains in to the hepatic portal circulation via the inferior mesenteric vein. The internal iliac vein drains in to the vena cava, thus bypassing the hepatic-portal circulation and avoiding first-pass metabolism by the liver. The absorption of a drug that is administered per rectum is affected by several factors. The variable absorption of the drug may be partially influenced by the venous drainage of the rectum. Therefore, some individuals feel that absorption and subsequent peak plasma level of medication is dependent on the location of deposition of drug within the rectum. However, there are significant anastomoses between the three rectal veins, and peak drug blood level has not clearly been shown to be dependent on the location of agent deposition within the rectum. A more dilute solution with greater volume provides more rapid onset and prolonged duration. Stool within the rectal vault as well as expulsion of an unmeasurable quantity of drug results in delayed or decreased absorption. Alteration in the integrity of the mucosa or the presence of hemorrhoids results in greater absorption. If a child is uncooperative, he or she may tightly close the anal sphincter during any aspect of the administration process. Excessive force in placing or removing the catheter may result in a laceration of the mucosa and cause a greater absorption of drug. Pharmacologic Agents for the Pediatric Patient the objective in selecting a pharmacologic agent is to choose an agent that establishes an appropriate environment to complete the surgical procedure. The effects sought in the pediatric patient include anxiolysis, amnesia, analgesia, immobilization, sedation, and hypnosis. Numerous agents are currently used by oral and maxillofacial surgeons and other practitioners. In this section, we discuss what we feel to be the most appropriate anesthetic agents and the routes by which they should be delivered. The eyes are commonly open with a blank stare and intact corneal and light reflexes. The clinical effect created by ketamine results from a dissociation between the thalamoneocortical and the limbic systems, which disrupts the brain from interpreting visual, auditory, and painful stimuli. This is significant because the effect persists in to the postoperative period and may decrease the need for postoperative analgesia. This minimizes the incidence of upper airway obstruction and hypopneas/apneas and maintains the pulmonary oxygen reserve. In addition to maintaining upper airway muscular tone, ketamine tends to better maintain the pharyngeal and laryngeal airway reflexes. This allows the patient to maintain the ability to swallow and cough, which minimizes the risk of pulmonary aspiration.
Buy cialis super active master card
The flap is returned to its original position erectile dysfunction doctors in tallahassee generic cialis super active 20mg on-line, and the initial resorbable suture is placed at the posterior aspect of the second molar. A, Once the soft tissue has been reflected, a small amount of buccal bone is removed with a bur or a hand chisel. B, the tooth is then delivered by a small straight elevator with rotational and lever types of motion. To achieve this goal, prophylactic antibiotics are necessary in some surgical procedures. Most of these procedures fall in to the clean-contaminated or contaminated categories of surgery. The incidence of postoperative infections in a clean surgery is related more to operator technique than to the use of prophylactic antibiotics. Surgery for the removal of impacted third molars clearly fits in to the category of clean-contaminated surgery; however, the exact incidence of postoperative infection is unknown. In the usual sense of the word, infection probably is a rare occurrence after third molar surgery. This means that it is unusual to see pain, swelling, and a production of purulence that requires incision and drainage or antibiotic therapy. In general, a competent, experienced surgeon would expect to have an infection rate in the range of 1% to 5% for all third molar procedures. Although the literature contains many articles that discuss the use of prophylactic perioperative antibiotics, there is essentially no report of their usefulness in the prevention of infection after third molar surgery. This disturbance in wound healing is most likely caused by the combination of saliva and anaerobic bacteria. The use of prophylactic antibiotics in third molar surgery does, in fact, reduce the incidence of dry socket. Other techniques that reduce bacterial contamination of the socket, such as copious irrigation, preoperative rinses with chlorhexidine, and placement of antibiotics in the extraction socket, are also effective. Although systemic antibiotics are effective in the reduction of postoperative dry socket, they are no more effective than local measures. The increase of antibiotic-related complications, such as allergy, resistant bacteria, gastrointestinal side effects, and secondary infections, is not outweighed by the benefits. Therefore, the routine administration of perioperative systemic antibiotics does not seem to be valid. The administration of perioperative steroids may increase the incidence of alveolar osteitis after third molar surgery, but the data are lacking as to the precise degree of increase. The overall incidence of complication and the severity of these complications are associated most directly with the depth of impaction, that is, whether it is a complete bony impaction, and to the age of the patient. The removal of complete bony impactions is likewise associated with increased postoperative pain and morbidity and an increase in the incidence of inferior alveolar nerve anesthesia. Another determinant of the incidence of complications of third molar surgery is the relative experience and training of the surgeon. The less experienced surgeon will have a significantly higher incidence of complications than the trained experienced surgeon. All of these are interpreted by the patient as being unpleasant and should, therefore, be minimized as much as possible. However, despite its extreme importance, this topic has received little significant study. Several authorities have published data on the short-term impact of third molar removal on quality of life. The use of corticosteroids to help minimize swelling, trismus, and pain has gained wide acceptance in the oral and maxillofacial surgery community. The method of usage, however, is extremely variable, and the most effective therapeutic regimen has yet to be clearly delineated. There is little doubt that an initial intravenous dose of steroid at the time of surgery has a major clinical impact on swelling and trismus in the early postoperative period. However, if the initial intravenous dose is not followed up with additional doses of steroids, this early advantage disappears by the second or third postoperative day. Maximum control of swelling requires that additional steroids be given for 1 or 2 days after surgery. Both of these are almost pure glucocorticoids, with little mineralocorticoid effect. In addition, these two appear to have the least depressing effect on leukocyte chemotaxis. Common dosages of dexamethasone are 4 to 12 mg intravenously at the time of surgery. Additional oral dosages of 4 to 8 mg twice a day on the day of surgery and for 2 days afterward result in the maximum relief of swelling, trismus, and pain. Methylprednisolone is most commonly given 125 mg intravenously at the time of surgery followed by significantly lower doses, usually 40 mg orally three or four times a day, later on the day of surgery and for 2 days after surgery. The most important determinant of the amount of postoperative pain that occurs is the length of the operation. There is, however, a strong correlation between postoperative pain and trismus, indicating that pain may be one of the principal reasons for the limitation of opening after the removal of impacted third molars. When a vessel is cut, the bleeding should be stopped to prevent secondary hemorrhage after surgery. The most effective way to achieve hemostasis after surgery is to apply a moist gauze pack directly over the site of the surgery with adequate pressure. In such situations, a variety of techniques can be employed to help secure local hemostasis, including oversuturing and the application of topical thrombin on a small piece of absorbable gelatin sponge in to the extraction socket. Unlike the gelatin sponge, oxidized cellulose can be packed in to the socket under pressure. In some situations, microfibrillar collagen can be used to promote platelet plug formation. Patients who have known acquired or congenital coagulopathies require extensive preparation and preoperative planning. The incidence of infection after the removal of third molars is very low, ranging from 1. Approximately 50% of infections are localized subperiosteal abscess-type infections, which occur 2 to 4 weeks after a previously uneventful postoperative course. Of the remaining 50%, few postoperative infections are significant enough to warrant surgery, antibiotics, and hospitalization. Infections occur in the first postoperative week after third molar surgery approximately 0. This is an acceptable infection rate and would not be decreased with the administration of prophylactic antibiotics. Swelling Postsurgical edema or swelling is an expected sequela of third molar surgery. As discussed earlier, the parenteral administration of corticosteroids is frequently employed to help minimize the swelling that occurs. The application of ice packs to the face may make the patient feel more comfortable but has no effect on the magnitude of edema. Patients who are administered steroids for the control of edema also tend to have less trismus. Like edema, jaw stiffness usually reaches its peak on the second day and resolves by the end of the first week. Tooth Fracture One of the most frequent problems encountered in removing third molars is the fracture of a portion of the root, which may be difficult to retrieve. In these situations, the root fragment may be displaced in to the submandibular space, the inferior alveolar canal, or the maxillary sinus. Uninfected roots left within the alveolar bone have been shown to remain in place without postoperative complications. Aggressive and destructive attempts to remove portions of roots that are in precarious positions seem to be unwarranted and may cause more damage than benefit. The postsurgical pain begins when the effects of the local anesthesia subside and reaches its maximum intensity during the first 12 hours postoperatively. The most common ones are combinations of acetylsalicylic acid or acetaminophen with codeine and its congeners, and the nonsteroidal anti-inflammatory analgesics.
Buy generic cialis super active 20mg on line
Conjunctiva Histology Conjunctival epithelium is a stratified non-keratinising epithelium formed by cuboid-columnar cells and containing mucusproducing goblet cells incidence of erectile dysfunction with age buy cialis super active on line. These cells, together with lachrymal and meibomian glands, maintain hydration and lubrication of the cornea and conjunctiva by producing the tear film. Conjunctival epithelium starts from the eyelid rim, lines the inner eyelid layer, turns at the bottom and continues covering the sclera up to the limbus where the cornea merges with the sclera. The limbus is an important clinical area as it is the point of insertion of the needle for anterior chamber paracentesis. Conjunctival scraping requires local anaesthesia and should be performed by trained ophthalmologists. Conjunctival brush may also be used under local anaesthesia using a small cytobrush Conjunctival epithelial tumours Benign epithelial tumours are principally represented by papillomas, which are composed of a fibrovascular stalk covered by acanthotic squamous epithelium. Cytological diagnosis is rarely requested; papillomas often recur after surgical excision. Scrape cytology sample showing loosely attached conjunctival cells with wide and well defined cytoplasm. Pre-invasive lesions show increased vascularity and thickening of the epithelium, which may be initially misdiagnosed as inflammatory or degenerative processes. Sometimes they may be present without any clinical evidence20 or appear as gelatinous and ill-defined lesions. Smears show immature cells with increased nucleus/cytoplasm ratio; the nuclei are enlarged and hyperchromatic with irregular contours, coarse chromatin and prominent nucleoli. Many high-grade lesions and some invasive carcinomas may show superficial keratinisation, which makes the cytological diagnosis more difficult. The differential diagnosis must include conjunctival squamous metaplasia (abundant cytoplasm, reduced nuclear/cytoplasmic ratio, pyknotic nuclei) and parakeratosis (dyskeratotic cells and keratohyaline granules). A relatively high correlation between cytology and the corresponding histological diagnoses has been found, while the greatest probability of false negatives is in keratinising squamous cell carcinoma. Conjunctival melanocytic tumours Melanocytic naevi of the conjunctiva are classified in almost the same way as those of the skin, i. Microscopically they are formed by pigmented polygonal cells and are more cellular than their epidermal counterparts. Pagetoid infiltration of the epithelium is indicative of malignant transformation in most cases. Cytological findings: conjunctival melanoma23 Dispersed tumour cells with eccentric nuclei Coarsely granular chromatin and prominent nucleoli Occasional or prominent cytoplasmic melanic granules Occasional spindle-shaped cells. Imprint cytology and Biopore membrane have given excellent diagnostic results, predicting the histological diagnosis by detection of superficial atypical melanocytes and their proportion relative to the conjunctival cells. It is lined with stratified, non-keratinised squamous epithelium and continues in to the sclera at the limbus, where epithelial stem cells proliferate centripetally in a vortex-like fashion, pushing mature and more transparent cells toward the centre. Corneal inflammation is generally diagnosed and treated on the basis of the clinical presentation. Cytology has been used to diagnose unusual clinical presentations or rare infections such as actinomycosis, blastomycosis or acanthamoebic keratitis,8,9 especially when the organisms are superficial. However, in the last few years the accurate identification of ever smaller lesions, mainly choroidal melanomas, and the development of localised therapeutic procedures has allowed a conservative approach to tumour treatment. Retrobulbar or peribulbar anaesthesia is required and the procedure is performed at the slit lamp or under operating microscope guidance. The needles may be connected to an automatic aspiration system to allow the ophthalmologist to place and move them with both hands. In order to make the wound self-healing, the needle is inserted with a slight cut in the sclera and pressure is applied after its withdrawal. The wall of the globe consists of three concentric layers: the external layer is the sclera, composed of scantily vascular collagen tissue, which in the anterior part of the globe, at the limbus, is in continuity with the cornea. The intermediate layer is the uvea, formed by the choroid, which surrounds the whole posterior chamber and is in continuity anteriorly with the ciliary body and iris. The choroid is composed of a pigmented fibrous stroma containing dendritic melanocytes and fenestrated vessels which supply the retinal pigmented epithelium. The crystalline lens, which separates the two segments of the eye, consists of a single layer of epithelium, a basal membrane and a collagenous nucleus. Biopore membrane sample showing numerous hyperpigmented melanoma cells and few conjunctival cells in the upper left corner. Nuclei are hybridised with probes for centromere 3 (green) and centromere 8 (red). Note the presence of one copy of chromosome 3 (split spot) and chromosome 8 again in three cells. Bacterial endophthalmitis may be a postsurgical complication and is characterised by an inflammatory infiltrate including mono and multinucleated histiocytes and lymphocytes. It is clinically important to differentiate phacoanaphylaxis from bacterial endophthalmitis because the latter requires prompt antibiotic therapy. Metastases Metastatic tumours occur less frequently in the anterior chamber than in the posterior chamber; breast, lung and prostate are the most frequent primary tumours. Vitrectomy has since also been used diagnostically; in fact vitrectomy samples may be used for microbiological or cytological examination. Microbiological diagnosis of calcofluor white staining and subsequent immunofluorescent microscopy. Again, this is due to the fear of complications, but also because of the development of highly sensitive and very accurate noninvasive diagnostic tools. At the same time, the identification Tumours Tumours of the anterior segment are rather rare and are represented by melanocytic tumours of the iris, tumours of the posterior segment extending in to the anterior segment, and metastases. Melanocytic lesions of the iris include a spectrum of lesions ranging from naevi to aggressive naevi and melanomas. Amelanotic naevi may be misdiagnosed as melanomas and aggressive naevi may grow and occlude the angle causing glaucoma. As with all uveal melanomas, they are classified as epithelioid, spindle or mixed cell type. Cytological findings: melanoma Dispersed epithelioid cells with large, polygonal, dense, welldefined cytoplasm and one or more eccentrically located nuclei, with coarse chromatin and large nucleoli. Melanic pigment may be present in the cytoplasm of tumoural cells as well as that of macrophages Spindle cell type with oval or even spindle nuclei and bipolar cytoplasmic processes. Spindle cell melanomas generally show a less dispersed pattern and are more monomorphous than the epithelioid variant. One report claims that it is possible to distinguish cytologically aggressive iris naevi from melanomas or metastatic carcinoma,27 but this differential diagnosis can be extremely difficult even in histological sections. Calcofluor white immunofluorescent demonstration of spores and filaments of Candida albicans obtained by vitrectomy with cytocentrifugation. It arises most frequently in the choroid, and a visual deficit is its usual clinical manifestation. The incidence of choroidal melanoma is higher in blue-eyed blond individuals with prevalence in adult males and the Caucasian race. Several cytogenetic changes have been described, with chromosome 8 polysomy and chromosome 3 monosomy being the most frequent and having prognostic significance in terms of survival. Prognostic factors are classically represented by tumour size, vascular pattern, levels of infiltration and histological pattern. It has been proven that monosomy of chromosome 3 and the presence of additional copies of chromosome 8 correlate with reduced survival; these chromosomal anomalies may be Retinoblastoma Retinoblastoma is the most common ocular tumour of childhood. A highly malignant tumour, it arises in the retina and may be unilateral or bilateral; white pupil (leukoria) is the most common clinical sign. Retinoblastoma is genetically determined by the loss of both alleles of the tumour suppressor (Rb) gene on the long arm of chromosome 13. Thanks to timely diagnoses and appropriate therapeutic procedures, retinoblastoma, previously a fatal disease, has become curable in many cases. Bilaterality, optic nerve involvement and invasion of surrounding tissues are the only features significantly associated with an unfavourable prognosis.
Cheap 20 mg cialis super active with visa
In other words erectile dysfunction doctors in orange county purchase 20mg cialis super active with visa, damage to the left occipital lobe means loss of the right visual field because the left half of both retinas receives light waves from the right side of the visual field. Other types of visual loss may occur depending on the point of damage in the visual pathway. Partial loss of vision may lead to inability to coordinate input from right and left visual fields. This may lead to diplopia or double vision as well as loss of depth perception and hand to eye coordination. Dysphasia refers to partial impairment, which is more common, but the term aphasia is frequently used to refer to both partial and total loss of communicating ability. Such a person may be unable to find any intelligible words or construct a meaningful sentence. Aphasia may also be described as fluent or non fluent; in fluent aphasia the pace of speech is relatively normal but contains made-up words and sentences that do not make sense. Non-fluent aphasia is slow and labored speech with short phrases; often small words are omitted. Other types of language disorders include the following: Dysarthria, in which words cannot be articulated clearly, is a motor dysfunction that usually results from cranial nerve damage or muscle impairment. Thorough testing is required before a specific diagnosis can be made of any of these disorders. Compare normal function and coma, using two characteristics of these levels of consciousness. Describe the effects on motor function of damage to the lateral surface of the frontal lobe. Describe the characteristics of expressive aphasia, and state the usual location of the damage. This state may be precipitated by inflammation, hypoxia, or bleeding in the brain. Often the seizure is focal or is related to the particular site of the irritation, but it may become generalized. Frequently the seizure is manifested by involuntary repetitive movements or abnormal sensations. The volume of each of these normally remains relatively constant, thus maintaining a normal pressure inside the cranial cavity. Temporary fluctuations in blood flow and blood pressure may occur with activities such as coughing or bending over. Because the brain is encased in the rigid, non-expandable skull, any increase in fluid, such as blood or inflammatory exudate, or any additional mass, such as a tumor, causes an increase in pressure in the brain. The result is that less arterial blood can enter the "high pressure" area in the brain, and eventually the brain tissue itself is compressed. Both of these effects decrease the function of the neurons, both locally and generally. All of these problems create the same general set of manifestations, which are summarized in Table 22-7. The resulting hypoxia triggers arterial vasodilation in the brain through local autoregulatory reflexes, in an attempt to improve the blood supply to the brain. However, this adds to the fluid volume inside the skull and is also effective for only a short time. Papilledema can be observed by looking through the pupil of the eye at the retina, where the optic disc provides a "window" in to the brain. Systemic vasoconstriction occurs to increase systemic blood pressure and force more blood in to the brain to relieve the ischemia. Baroreceptors in the carotid arteries respond to the increased blood pressure by slowing the heart rate. Chemoreceptors respond to the low carbon dioxide levels that accompany the accelerated systemic circulation by reducing the respiratory rate. As improved cerebral circulation relieves ischemia, the reflex vasoconstriction momentarily ceases. In other words, the brain responds to ischemia by one mechanism, whereas feedback control for blood pressure uses other mechanisms to protect the rest of the body, resulting in a conflict of interests. Eventually severe ischemia and neuronal death prevent any circulatory control, and the blood pressure drops. Various abnormal respiratory patterns develop, such as Cheyne-Stokes respirations, with alternating apnea and periods of increasing and decreasing respirations, depending on the site of the lesion. With an additional pressure increase, both pupils become fixed and dilated ("blown"). B, Papilledema showing displacement and folding of the retina (arrows) as well as edema and congestion of the optic nerve head. The composition of the fluid may vary with the cause of the problem (see Table 22-1). Cerebrospinal fluid is obtained by inserting a needle in to the subarachnoid space in the lumbar region. Therefore benign tumors as well as malignant tumors can be life threatening, unless they are in an accessible superficial location where they can be removed. In addition, tumors may develop in the meninges (meningioma) or pituitary gland (adenoma, see Chapter 25), causing similar neurologic effects that result from pressure on the brain. Secondary brain tumors are quite common, usually metastasizing from breast or lung tumors, and they cause effects similar to those of primary brain tumors. The combined incidence rate for brain cancer in children and adults is 22,000 in 2008 with 13,000 deaths. Pathophysiology Primary malignant brain tumors, particularly astrocytomas, do not usually have well-defined margins but are invasive and have irregular projections in to adjacent tissue that are difficult to totally remove. There is usually an area of inflammation around the tumor, adding to the pressure. As the mass expands, it compresses and distorts the tissue around it, eventually resulting in herniation. A relatively small tumor in the brain stem or cerebellum can compress the medulla within a short time. However, tumors in the cerebral hemispheres, particularly in "silent" areas (without obvious function), may grow quite large before their effects are noticeable. Etiology Brain stem and cerebellar tumors are common in young children, and research in to the cause of these tumors continues, particularly with regard to prenatal parental exposure to carcinogens and embryonic development. Adults are affected more frequently by tumors in the cerebral hemispheres; predisposing factors have not been established. In transtentorial (central) herniation, the cerebral hemispheres, diencephalon, and midbrain are displaced downward. Cerebellar, or tonsillar (infratentorial), herniation develops when the cerebellar tonsils are pushed downward through the foramen magnum, which compresses the brain stem and vital centers and causes death. Explain why a lesion in the brain stem is more critical than one in the cerebral hemisphere. Clinical assessment routinely includes tools such as the assessment of normal reflexes and the Glasgow coma scale to assess the level of consciousness. Although some overlap occurs, there are major differences in onset, course, and management of the two groups. A, Astrocytoma in right frontal lobe has expanded the gyri (arrows indicate flattening). Lethargy and irritability may develop, along with personality and behavioral changes. In some cases, focal or generalized seizures are the first sign, as the tumor irritates the surrounding tissue. Brain stem or cerebellar tumors may affect several cranial nerves, possibly causing unilateral facial paralysis or visual problems. Pituitary adenomas in the brain usually cause endocrinologic signs, depending on the type of excess secretion (see Chapter 25). Treatment Surgery is the treatment of choice, if the tumor is reasonably accessible.
Pimenta (Allspice). Cialis Super Active.
- Dosing considerations for Allspice.
- Are there safety concerns?
- What is Allspice?
- Intestinal gas, stomachache, vomiting, diarrhea, purging the bowels, fever, flu, colds, heavy menstrual bleeding, and other conditions.
- How does Allspice work?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96125
Discount 20 mg cialis super active with mastercard
In addition fast facts erectile dysfunction order cheap cialis super active on line, the surgical procedure grows more and more difficult as the patient ages owing to more densely calcified bone, which is less flexible and more likely to fracture. There is overwhelming clinical evidence to support the fact that the number of days missed from work and other normal activity after third molar extraction is much higher in the patient older than 40 years compared with patients younger than 18 years. As a general rule, if a patient has a fully impacted third molar that is completely covered with bone, has no obvious potential source of communication with the oral cavity, and has no signs of pathology such as an enlarged follicular sac, and if the patient is older than 40, the tooth probably should not be removed. If the overlying bone is very thin and a removable denture is to be placed over that tooth, the tooth should probably be removed before the final prosthesis is constructed. Compromised Medical Status Patients who have impacted teeth may have some compromise in their health status, especially if they are elderly. As age increases, so does the incidence of moderate to severe cardiovascular disease, pulmonary disease, and other health problems. Thus, the combination of advanced age and compromised health status may contraindicate the removal of impacted teeth that have no pathologic processes. Other factors may compromise the health status of younger people, such as congenital coagulopathies, asthma, and epilepsy. In this group of patients, it may be necessary to remove impacted teeth before the incipient pathologic process becomes fulminant. Thus, not only in the older compromised patient but also in the younger compromised patient, the surgeon occasionally needs to remove asymptomatic as well as symptomatic third molars. Surgical Damage to Adjacent Structures Occasionally, an impacted tooth is positioned such that its removal may seriously compromise adjacent nerves, teeth, and other vital structures. The potential complications must be weighed against the potential benefits of surgical removal of the tooth. In this clinical setting, many clinicians advocate removing only the crown of the impacted tooth and intentionally leaving the roots in place; scientific literature offers substantial support for this approach, particularly for mandibular third molars. In older patients, the surgical extraction of impacted third molars can result in significant bony defects that may not heal adequately and, in fact, may result in the eventual loss of adjacent teeth rather than the improvement or preservation of periodontal health. Typically, the crowns of the teeth are surgically exposed with removal of tissues in the direction most appropriate for crown movement. The teeth were allowed to erupt for up to 24 months or until the greatest diameter of the crown reached the level of the mucosal surface. Of 542 teeth, only 16 were failures (failure to erupt after 24 mo or with other complications). This study found that the teeth tended to show a change of inclination of the longitudinal access by rotation along the root. Age did not appear to be a factor in success, although most patients were younger than 19 years. More commonly, the technique of surgical exposure is combined with attachment of an orthodontic appliance to the tooth, allowing active guidance of the impacted tooth in to an ideal position. Important factors in this technique are prior orthodontic treatment to provide both anchorage and adequate space within the dental arch for the impacted tooth. Many methods have been suggested for making attachment to the impacted tooth, including polycarbonate crowns, attachments such as rare earth magnets, or pins inserted in to the structure of the tooth. The most common method of orthodontic attachment to an impacted tooth is the placement of a bonded orthodontic bracket. Studies have compared simple exposure and packing to maintain a gingival path for eruption with exposure and bonding of a bracket. In a study of impacted premolars, Thilander and Thilander79 showed that surgical exposure alone resulted in eruption, provided that space was present in the arch. However, mesially tipped premolars had a poor prognosis and required orthodontic guidance. Iramaneerat and associates80 found that there was no difference in total orthodontic treatment time for the two techniques. Pearson and colleagues81 found that bracketing was more costly and more likely to require reoperation. Nonetheless, placing a bracket is the more popular technique, perhaps owing to orthodontist preference and patient comfort. Laskin and Peskin82 believe that if exposure of teeth is to result in successful spontaneous eruption, it should be done as soon as it is determined that the tooth is not going to erupt spontaneously. Ranta83 stated that it is typical for impacted second molars to erupt normally when the offending third molar is removed. Vig84 also recommends routine removal of the third molar when a second molar is impacted. If the tooth is deeply impacted, it may be more appropriate to replace the soft tissue flap, bringing a wire attached to the bonded bracket through the soft tissues near the crest of the ridge. Alternatively, if making attachment to the canine is deemed unnecessary or not possible, the flap may be returned to its original position. A full-thickness soft tissue window is then created over the canine crown, which is then packed open and allowed to epithelialize, leaving the crown visible in the mouth for spontaneous eruption or attachment at a later date. The technique of replacing the flap has been examined for its periodontal consequences. The clinical outcomes show minimal effects of the closed eruption technique on the periodontium. Adequate space in the arch must be established by preliminary orthodontic treatment before canine exposure. A full-thickness mucoperiosteal flap is elevated with mesial and distal releasing incisions extending along the sides of the canine crown. It is often useful to make these incisions more closely parallel than in other circumstances, because widely divergent releasing incisions make repositioning the flap apically more difficult. The crown of the tooth is uncovered, avoiding dissection beyond the cervical line of the tooth. A bonded bracket is attached and the flap is repositioned and secured to cover the cementoenamel junction of the tooth. When the tooth is too far superior to allow an apically repositioned flap, the wire or chain secured to the bracket is brought out from under the flap at the crest of the ridge and the flap is returned to its original position. As the tooth is orthodontically moved in to position, an adequate band of keratinized gingiva either migrates with the tooth or remains in place at the alveolar crest and the tooth is guided to erupt through it. Techniques that involve removal of the attached gingiva, leaving alveolar mucosa surrounding the cervical area of the tooth, are to be avoided. These basic principles of exposure of canines can be generalized to many other impacted teeth. Exposure and orthodontic attachment of maxillary and mandibular premolars can be treated much like maxillary canines. Often, mandibular premolars are located relatively centrally in the alveolar process. When this is the case, exposure from the coronal aspect of the tooth may be indicated. A bonded bracket may be placed on the occlusal surface of the tooth and orthodontic forces applied in a relatively vertical direction until the tooth is exposed sufficiently to place the orthodontic bracket in a more traditional position. Impacted second molars with angulation, root morphology, and available space deemed adequate may be orthodontically uprighted after surgical exposure and bracketing. A conventional button with gold chain may be bonded to the tooth, although a molar bracket with buccal tube has been reported to offer shorter treatment times with excellent outcomes. Impacted lower second molars with incomplete apical closure may be exposed and surgically uprighted according to a method nicely described by Pogrel. This generally creates the necessary space for posterior tipping of the second molar. If no third molar is present, it will likely be necessary to remove bone posterior to the second molar. When doing so, it is important to avoid damage to the cementoenamel junction of the second molar. An extremely important part of this surgical procedure is ensuring that there are no occlusal forces on the repositioned second molar.
Syndromes
- Skin disorders such as pyoderma or dermatophytid
- Skin biopsy
- Traumatic brain injury
- Time it was swallowed
- Congenital dyserythropoietic anemia
- Infection
- Do not give these medicines to children.
- 1/2 teaspoon of salt
- Heat
- Friction of the condom may reduce clitoral stimulation and lubrication, making intercourse less enjoyable or even uncomfortable (using the provided lubricant may help).
Purchase cialis super active from india
Blood flows very slowly through capillaries impotence exercises for men purchase cialis super active 20 mg visa, and precapillary sphincters determine the amount of blood flowing from the arterioles in to the individual capillaries, depending on the metabolic needs of the tissues. Normally, a high percentage of the blood (approximately 70%) is located in the veins at any one time; hence, the veins are called capacitance vessels. Blood flow in the veins depends on skeletal muscle action, respiratory movements, and gravity. Valves in the larger veins in the arms and legs have an important role in keeping the blood flowing toward the heart. The tunica media, a layer of smooth muscle that controls the diameter and lumen size (diameter) of the blood vessel, is the middle layer. The tunica adventitia, or externa, is the outer connective tissue layer and contains elastic and collagen fibers. The vasa vasorum consists of tiny blood vessels that supply blood to the tissues of the wall itself. Normally the large arteries are highly elastic in order to adjust to the changes in blood volume that occur during the cardiac cycle. For example, the aorta must expand during systole to prevent systolic pressure from rising too high, and during diastole the walls must recoil to maintain adequate diastolic pressure. Localized vasodilation or vasoconstriction in arterioles is controlled by autoregulation, a reflex adjustment in a small area of a tissue or an organ, which varies depending on the needs of the cells in the area. For example, a decrease in pH, an increase in carbon dioxide, or a decrease in oxygen leads to local vasodilation. Release of chemical mediators such as histamine or an increase in temperature at a specific area can also cause vasodilation. Norepinephrine and epinephrine increase systemic vasoconstriction by stimulating alpha1-adrenergic receptors in the arteriolar walls. Peripheral resistance is the force opposing blood flow, or the amount of friction with the vessel walls encountered by the blood. Decreasing the diameter (or lumen) of the blood vessel increases the resistance to blood flow. Normally peripheral resistance can be altered by the systemic constriction or dilation of the arterioles. Systemic or widespread vasoconstriction occurs in response to sympathetic stimulation and increases blood pressure. Local vasoconstriction or dilation does not affect the overall systemic blood pressure. Capillary walls consist of a single endothelial layer to facilitate the exchange of fluid, oxygen, carbon dioxide, electrolytes, glucose and other nutrients, and wastes between the blood and the interstitial fluid. Systolic pressure, the higher number, is the pressure exerted by the blood when ejected from the left ventricle. Diastolic pressure, the lower value, is the pressure that is sustained when the ventricles are relaxed. The brachial artery in the arm is used to measure blood pressure with a sphygmomanometer and an inflatable blood pressure cuff. Specific variables include blood volume and viscosity, venous return, the rate and force of heart contractions, and the elasticity of Changes in blood pressure are detected by the baroreceptors and relayed to the vasomotor control center in the medulla, which adjusts the distribution of blood to maintain normal blood pressure. For example, when one rises from a supine position, blood pressure drops momentarily owing to gravitational forces until the reflex vasoconstriction mechanism in the body ensures that more blood flows to the brain. This stimulates the release of renin, which in turn activates angiotensin (vasoconstrictor) and stimulates aldosterone secretion (see Chapter 21). List the compensatory mechanisms (in the correct sequence) that can help return the blood pressure to normal levels following a slight drop such as standing up too rapidly. Differentiate local vasoconstriction from systemic vasoconstriction by: (1) possible causes; (2) area involved; (3) effect on local tissue; and (4) effect on systemic blood pressure. How does vasoconstriction in the skin and viscera result in increased venous return to the heart Common heart diseases include congenital heart defects, hypertensive heart disease, angina and heart attacks, cardiac arrhythmias, and congestive heart failure. There is increasing emphasis on routine preventive measures for all individuals, with a focus on factors such as a healthy diet, regular exercise, moderation in alcohol intake, cessation of smoking, safe sexual practices, immunizations, monitoring body weight and blood pressure, and basic screening tests for cholesterol levels and the presence of cancer. It is a noninvasive procedure and can illustrate the conduction activity of the heart as well as the effects of systemic abnormalities such as serum electrolyte imbalance. In echocardiography, ultrasound, or reflected sound waves, is used to record the image of the heart and valve movements. These tests provide useful information regarding valvular abnormalities, congenital defects, and changes in heart structure or function. Tomographic studies, which illustrate various levels of a tissue mass may be used when available. Nuclear medicine studies can identify dead or damaged areas of myocardial tissues and may be used to assess the extent of myocardial damage after a myocardial infarction. Determination of central venous pressure and pulmonary capillary wedge pressure, which indicate blood flow to and from the heart, can be made with a catheter. Dietary modifications usually include reducing total fat intake and intake of saturated (hydrogenated or animal) fat as well as "trans" fats which are commercially hydrogenated plant oils used to stabilize convenience foods. A regular exercise program is suggested to improve overall cardiovascular function and circulation to all areas of the body. Cessation of cigarette smoking decreases the risk of coronary disease because smoking appears to increase vasoconstriction and heart rate, thus increasing the workload on the heart. Smoking increases platelet adhesion and the risk of thrombus formation, as well as increasing serum lipid levels. Common medications include: Vasodilators, such as nitroglycerin or long-acting isosorbide, reduce peripheral resistance systemically and therefore the workload for the heart and also act as coronary vasodilators. These actions provide a better balance of oxygen supply and demand in the heart muscle. Vasodilators may cause a decrease in blood pressure, resulting in dizziness or syncope and a flushed face. A person should sit quietly for a few minutes after taking nitroglycerin sublingually. Members of the group may be used as agents to decrease cardiac contractility, as an antidysrhythmic particularly for excessive atrial activity, or as an antihypertensive and vasodilator. Some drugs such as diltiazem are more selective for the myocardium and reduce both conduction and contractility. There is some risk with this procedure, but it has proved beneficial in many instances. Current research using very tiny ultrasound instruments within the vessels has proved more effective in diagnosing obstructions. Obstructions can be assessed and then treated with the basic catheterization procedure, with injected thrombolytic agents or laser therapy to break down clots, or balloon angioplasty to open a narrow coronary artery mechanically. Hemoglobin, hematocrit, blood cell counts, and the differential count for white cells are also routine aspects of blood tests. Other specific tests are mentioned under the appropriate topic and in Ready Reference 5 at the back of the book. Note that these drugs do not affect skeletal muscle contraction because more calcium is stored in skeletal muscle cells. Digoxin, a cardiac glycoside, has been used for many years as a treatment for heart failure and as an antiarrhythmic drug for atrial dysrhythmias. Digoxin improves the efficiency of the heart because it also is inotropic, increasing the contractility of the heart. Because the effective dose is close to the toxic dose, patients must be observed for signs of toxicity, and blood levels of the drug must be checked periodically. Combinations of drugs from various classifications are frequently prescribed to effectively lower blood pressure. Some of these drugs do cause orthostatic hypotension, a drop in blood pressure accompanied by dizziness, when arising from a recumbent position. These drugs may be used for treatment of essential hypertension or congestive heart failure or after myocardial infarction. These drugs, such as enalapril (Vasotec), ramipril (Altace), and captopril (Capoten), reduce both peripheral resistance (vasoconstriction) and aldosterone secretion (thus decreasing sodium and water retention). Diuretics remove excess sodium and water from the body through the kidneys by blocking the reabsorption of sodium or water (see Chapter 21).
Order cheapest cialis super active
Patients should be monitored because of an increased incidence of intestinal lymphoma erectile dysfunction forums buy cialis super active canada. Prevalence is estimated in the range of 500,000 cases in the United States, ranging from mild to severe. These diseases are characterized by remissions and exacerbations as well as considerable diversity in the severity of clinical effects. Inflammation occurs in a characteristic distribution called "skip lesions," with affected segments clearly separated by areas of normal tissue. Initially inflammation occurs in the mucosal layer with the development of shallow ulcers. The ulcers tend to coalesce to form fissures separated by thickened elevations or nodules, giving the wall a typical "cobblestone" appearance. The progressive inflammation and fibrosis may affect all layers of the wall (transmural), leading eventually to a thick, rigid "rubber hose" wall. This change leaves a narrow lumen ("string sign"), which may become totally obstructed. Granulomas indicative of chronic inflammation may be found in the wall and the regional lymph nodes. The damaged wall impairs the ability of the small intestine to process and absorb food. The inflammation also stimulates intestinal motility, decreasing the time available for digestion and absorption. Interference with digestion and absorption in the small intestine may lead to hypoproteinemia, avitaminosis, malnutrition, and possibly steatorrhea. Adhesions between two loops of intestine may develop when the subserosa is inflamed. Fistulas, a connecting passage between two structures, may form as the ulcer erodes through the intestinal wall. Anorexia, weight loss, anemia, and fatigue are associated with malabsorption and malnutrition. Children experience delayed growth and sexual maturation resulting from lack of adequate protein and vitamins, particularly fat-soluble vitamins A and D. In addition, many psychological implications are characteristic of this type of chronic illness. Ulcerative Colitis Pathophysiology the inflammation commences in the rectum and progresses in a continuous fashion proximally through the colon. In an attempt to heal, granulation tissue forms, but it is vascular and fragile and bleeds easily. When the ulcers coalesce, large areas of the mucosa become denuded, but there are residual "bridges" of intact mucosa over the ulcers. This tissue destruction interferes with the absorption of fluid and electrolytes in the colon. In severe acute episodes, a serious complication, toxic megacolon, may develop, as inflammation impairs peristalsis, leading to obstruction and dilation of the colon, usually the transverse colon. A concern with long-term ulcerative colitis is the increased risk of colorectal carcinoma, which may be predicted by detection of metaplasia and dysplasia in the mucosa. C, Photograph showing narrowing ("garden-hose") and inflammation-ulceration of bowel. During severe exacerbations, blood and mucus alone may be passed frequently, day or night, accompanied by tenesmus (persistent spasms of the rectum associated with a need to defecate). Rectal bleeding may be considerable and contributes to severe iron deficiency anemia. It is helpful to identify and remove, if possible, the specific factors that apply in each individual. These drugs may be administered systemically, both orally and parenterally, or topically, as an enema or suppository. Total parenteral nutrition (intravenous) may be required during severe exacerbations. The recommended diet is usually high in protein, vitamins, and calories but low in fat. In some cases, surgical intervention may provide a temporary rest for the intestine and can be reversed to normal anatomy later. Pathophysiology the development of appendicitis usually follows a pattern that correlates with the clinical signs, although variations may occur because of the altered location of the appendix or underlying factors. Obstruction of the appendiceal lumen by a fecalith, gallstone, or foreign material or from twisting or spasm is commonly an initiating factor. The increasing congestion and pressure within the appendix leads to ischemia and necrosis of the wall, resulting in increased permeability. B, Smear of drainage from a ruptured appendix showing infection by fecal flora and gram-positive and gram-negative bacteria. This breakout of bacteria leads to abscess formation or localized bacterial peritonitis. An abscess may develop when the adjacent omentum temporarily walls off the inflamed area by adhering to the appendiceal surface. Localized infection or peritonitis develops around the appendix and may spread along the peritoneal membranes. Increasing pressure inside the appendix causes increased necrosis and gangrene in the wall (infection in necrotic tissue). The appendix ruptures or perforates, releasing its contents in to the peritoneal cavity. Signs and symptoms Sometimes appendicitis develops "silently" or manifests with significant variations. In classic cases, a sequence of signs occurs, as follows: General periumbilical pain related to the inflammation and stretching of the appendiceal wall occurs initially. Localized pain results from involvement of the parietal peritoneum over the appendix. The location of the appendix does vary among individuals, and this can be diagnostically misleading. General periumbilical pain increasing in severity as inflamed appendix is distended 3. Treatment Surgical removal of the appendix and administration of antimicrobial drugs are the standard treatment. It is a common problem in the Western world, affecting primarily older individuals. Pathophysiology Diverticula form at gaps between bands of longitudinal muscle that coincide with openings in the circular muscle bands that permit passage of blood vessels through the wall. Longitudinal muscle also occurs in three bands, rather than as a continuous sheet. These weaker areas of the wall bulge outward when pressure is increased, frequently inside the lumen of the intestine, for example, in the presence of strong muscle contractions. Consistently low-residue diets, irregular bowel habits, and aging lead to chronic constipation and then to muscle hypertrophy in the colon, with elevated intraluminal pressures, and finally to the gradual development of diverticula. Potential complications include intestinal obstruction, perforation with peritonitis, and abscess formation. Sometimes there is mild discomfort, diarrhea, or constipation and flatulence, which can be excused for other reasons. For specific information on the tests that are being used and the rationale for the use of each, see the American Cancer Society web site. The United States Congress has mandated screening for colorectal cancer as part of the "Welcome to Medicare" physical to be done within 6 months of qualifying for Medicare benefits. Pathophysiology Most malignant neoplasms develop from adenomatous polyps, of which there are a diversity of types. A polyp is a mass, often on a stem, that protrudes in to the lumen, and many polyps represent genetic abnormalities.
Purchase cialis super active in india
Carcinomatous metastases in the skeleton are mainly derived from the breast erectile dysfunction treatment supplements cialis super active 20mg free shipping, kidney, lung, prostate thyroid and liver. Cutaneous and extracutaneous malignant melanoma are another important source of metastases. The cytological features in skeletal metastases are the same as those of the primary tumours. When bone deposits are the first manifestation of the tumour, immunocytochemistry may help to disclose the primary site. Cytological findings: osteomyelitis Highly cellular yields Neutrophils Debris Histiocytes Epithelioid histiocytes in granulomatous inflammation. Tuberculous osteomyelitis must be suspected when clusters of epithelioid histiocytes are mixed with the neutrophils. They have pale greyish-blue cytoplasm with indistinct cell borders and their elongated kidney-shaped nuclei are also pale staining. Small lymphocytes may also be noted but typical giant cells of Langerhans type as found histologically are seldom observed and caseation necrosis is not easily recognised. In these circumstances, the cytological diagnosis becomes the most important parameter in determining further management. At our musculoskeletal tumour centre, this double approach has proved to be successful. The role of fine-needle aspiration biopsy in the primary diagnosis of mesenchymal lesions. Accuracy, limitations and pitfalls in the diagnosis of soft tissue tumors by fine needle aspiration cytology. Combined radiology and cytology in the diagnosis of bone lesions: a retrospective study of 370 cases. Unique cytological features and chromosome aberrations in chondroid lipoma: a case report based on fine-needle aspiration cytology, histopathology, electron microscopy, chromosome banding, and molecular cytogenetics. A cytologic-histologic study with clinical, radiologic, electron microscopic, and cytogenetic correlations. Fine-needle aspiration cytology and core needle biopsy in the preoperative diagnosis of desmoid tumors. Solitary fibrous tumour: clinicopathological, immunohistochemical, and ultrastructural analysis of 12 cases arising in soft tissues, nasal cavity and nasopharynx, urinary bladder and prostate. Elastofibroma has distinct cytomorphologic features making diagnostic surgical biopsy unnecessary: cytomorphologic study with clinical, radiologic, and electron microscopic correlations. Fineneedle aspiration of primary and recurrent benign fibrous histiocytoma: classic, aneurysmal, and myxoid variants. Cytologic findings in granular cell tumors, with emphasis on the diagnosis of malignant granular cell tumor by fine-needle 2. Fine-needle aspiration in liposarcoma: cytohistologic correlative study including well-differentiated, myxoid, and pleomorphic variants. Comparative fine-needle aspiration and pathologic study of malignant fibrous histiocytoma: cytodiagnostic features of 95 tumors in 71 patients. Cytologic features of primary, recurrent, and metastatic dermatofibrosarcoma protuberans. An analysis of the most common cytologic findings and the value of ancillary techniques. The new international rhabdomyosarcoma classification, its progenitors, and considerations beyond morphology. Paratesticular spindle cell rhabdomyosarcoma diagnosed by fine needle aspiration cytology: A case report. Rhabdomyosarcoma: cytogenetics of five cases using fine-needle aspiration samples and review of the literature. Findings in fourteen fine needle aspiration biopsy specimens and one pleural fluid specimen. Cytohistologic correlations in angiosarcoma including classic and epithelioid variants: the Institute Curie experience. The clinical use of fine needle aspiration cytology for diagnosis and management of children with neuroblastic tumours. Fine needle aspiration cytology in the diagnosis and management of children and adolescents with Ewing sarcoma and peripheral primitive neuroectodermal tumor. Fine needle aspiration cytology in diagnosis and management of childhood small round cell tumours. Cytogenetic characterisation of Ewing tumors using fine needle aspiration samples, a 10-year experience and review of the literature. Fine-needle aspiration biopsy diagnosis of gastrointestinal stromal tumors using morphology, immunocytochemistry and mutational analysis of c-kit. Fine-needle aspiration of synovial sarcoma: criteria for diagnosis: retrospective examination of 37 cases, including ancillary diagnostics. Aspiration cytology of pulmonary small cell variant of poorly-differentiated synovial sarcoma metastatic from the tongue: a case report. The complex cytological features of synovial sarcoma in fine needle aspirates, an analysis of four illustrative cases. Reverse transcriptase polymerase chain reaction on fine needle aspirates for rapid detection of translocations in synovial sarcoma. Fine needle aspiration cytology and core biopsy in the diagnosis of alveolar soft part sarcoma presenting with lung metastases. Cytologic features of clear cell sarcoma (malignant melanoma) of soft parts: a study of fine needle aspirates and exfoliative specimens. Clear cell sarcoma diagnosis by fine-needle aspiration: cytologic, histologic, and ultrastructural features; potential pitfalls; and literature review. Extraskeletal myxoid chondrosarcoma with neuroendocrine differentiation: a case report with fine-needle aspiration biopsy, histopathology, electron microscopy, and cytogenetics. Malignant rhabdoid tumor of the liver diagnosed by fine needle aspiration cytology. Intraabdominal desmoplastic small round cell tumor: Cytopathologic finding in two cases. Intraabdominal desmoplastic small round cell tumor: report of a case with fine needle aspiration, cytologic diagnosis and molecular confirmation. Chondroblastoma of bone: use of fine-needle aspiration biopsy and potential diagnostic pitfalls. Low risk of recurrence of enchondroma and low grade chondrosarcoma in extremities. Light and electron-microscopic examination of fine-needle aspiration in the preoperative diagnosis of cartilaginous tumours. Potential sampling error in fine-needle aspiration biopsy of dedifferentiated chondrosarcoma: a report of 4 cases. Fineneedle aspiration of spinal osteoblastoma in a patient with lymphangiomatosis. Small cell osteosarcoma of the ribs: immunohistochemical, and ultrastructural study with literature review. Chordoma: diagnosis by fine-needle aspiration with histologic, immunocytochemical, and ultrastructural confirmation. Fine needle aspiration biopsy of soft tissue sarcomas: utility and diagnostic challenges. The role of fine needle aspiration biopsy in the initial diagnosis of pediatric bone and soft tissue tumors: an institutional experience. Fine-needle aspiration cytology of sarcoma: retrospective review of diagnostic utility and specificity. Fine-needle aspiration biopsy in the diagnosis and management of bone lesions: a study of 450 cases. Concordance of histopathologic and cytologic grading in musculoskeletal sarcomas: can grades obtained from analysis of the fine-needle aspirates serve as the basis for therapeutic decisions Fine-needle aspiration biopsy of soft tissue sarcomas: a cytomorphologic analysis with emphasis on histologic subtyping, grading, and therapeutic significance. Soft tissue sarcomas: the usefulness and limitations of fine-needle aspiration biopsy. The diagnostic utility of fine-needle aspiration biopsy of soft-tissue sarcomas in the core needle biopsy era. Histologic prognostication in soft tissue sarcomas: grading versus subtyping or both Freemont and John Denton Chapter contents Introduction Synovial fluid cytology the cytocentrifuge preparation Cells Clinical applications of synovial fluid microscopy and the value of diagnostic algorithms the place of synovial fluid microscopy in clinical management Summary layer of cells. This means that there is no intact basement membrane, which in other tissues is a significant physical and chemical barrier to the movement of molecules and cells. It also means that the matrix of cartilage and synovium are in contact with the synovial fluid, allowing a relatively homogeneous chemical environment to develop within the joint.