Order vasotec 5mg visa
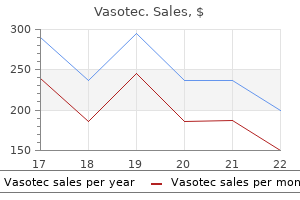
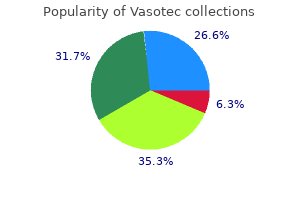
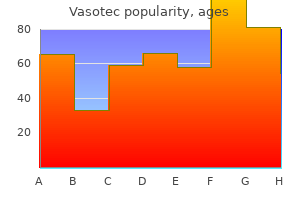
Crohn disease involving the small bowel frequently leads to inadequate energy absorp tion and growth compromise arrhythmia frequency order vasotec american express. In addition, children with Crohn disease will have decreased calorie intake which further contributes to growth failure and short stature. Postviral enteropathy is a prolonged immune response following clearance of the infectious organism. Cow milk and/or soy protein allergy can lead to immune-mediated damage that will reappear with reintroduction of these antigens. If the liver cannot increase synthesis to exceed the excessive losses through the intestine, there is inability to form micelles and consequently fat malabsorption. Primary or secondary lymphangiectasia interferes with the delivery of the bile salts into the proximal small bowel where they are required for nonpolar fat absorption. Malabsorption 179 Extraintestinal causes of malabsorption (pancreatic exocrine insufficiency) Cystic fibrosis, an autosomal recessive disease caused by mutations to the gene for the chloride transporter, is by far the most common etiology for this condition. Pulmonary problems are an even more serious aspect of this disease along with hepatobiliary disease, sweat abnormalities, nasal polyps, and limited reproductive ability. Other methods commonly employed are an increased generation of hydrogen or methane gas measured on breath testing, or finding an acidic pH of the stool which results from bacterial fermentation in the colon of unabsorbed sugar. Once carbohydrate malabsorption is documented then the approach below is employed to determine the etiology of this condition. A history of previous or current infections with gastrointestinal, sinopulmonary, dermatologic, or systemic organisms should be sought. Family history is critical when considering causes such as Crohn disease, celiac disease or cystic fibrosis. Physical examination findings of hepatomegaly, clubbing, and pulmonary, musculoskeletal or dermatologic diseases can provide important clues in evaluating the pathophysiology of malabsorption. Potential noninvasive testing includes serology for celiac disease, serologic evalu- ation for immune function, food allergy testing (IgE or skin prick testing); sweat testing; and possibly mutational analyses for cystic fibrosis. Fecal testing for pH, reducing substances, guaiac, fat, and leukocytes is inexpensive and often elucidating. Additional stool investigations would identify the presence of infectious agents, and measurement of fecal elastase is used as a marker for pancreatic exocrine sufficiency. If there is evidence for compromised protein status a fecal specimen for alpha-1-antitrypsin as a marker for protein-losing enteropathy would be indicated. Endoscopy and biopsy of the duodenum is required to diagnose celiac disease, Crohn disease of the small bowel, Whipple disease, abetalipoproteinemia, certain enteric infections, and lymphoma of the small bowel. Most children with malabsorption will require supplemental and/or simpler forms of nutrients to prevent deficiencies. Malabsorption or deficiencies of carbohydrate, protein or fat will vary in clinical presentation and biochemical profile. Treatment of fat malabsorption related to bile acid deficiency, may require medium chain triglycerides which can be absorbed directly through the intestine without relying on micelle formation. Malabsorption related to pancreatic exocrine insufficiency can be corrected by providing the child with pancreatic replacement enzymes which are taken with meals. This permits adequate digestion of the ingested food so that complete absorption can occur. Celiac disease (gluten), cow milk protein allergy, and soy protein allergy require removal of the triggering antigens to allow the bowel to heal fully. Enteric infections may require prolonged treatment regimens especially when immune dysfunction is contributing to the chronicity. Therapy for specific illnesses such as Crohn disease or intestinal lymphoma will be required when these conditions contribute to intestinal malabsorption. In certain cases, where malabsorption cannot be corrected, amino acid-based diets with glucose polymers are used to permit adequate nutrient absorption. Finally, the child with extensive small bowel disease such as severe short bowel syndrome and motility disorders may have to receive parenteral nutrition when all efforts to provide adequate enteral nutrition are unsuccessful. A subset of these children can ultimately develop enough intestinal function through intensive intestinal rehabilitation programs. The remainder of such patients are candidates for small intestine transplantation. The degree of malabsorption can become severe enough that special diets and special programs are required. Intestinal rehabilitation programs are now reporting that a high proportion of children who enter such programs are able to be discharged on long-term enteral therapy, although some will still require supplemental parenteral nutrition. For children who require intestinal transplant, survival rates have been reported as high as 97% at 1 year and 74% at 3 years post-transplantation. However, only a small proportion of those patients who are on the waiting list will ultimately be able to live long enough to find a suitable donor. This potentially systemic disease is triggered by the ingestion of gluten in genetically susceptible individuals. Unique as an immune-mediated disorder, the primary environmental trigger is not only known, but lifelong removal of this dietary trigger leads to remission of the disease. Associated diseases the highly variable manifestations of celiac disease lead to a broad spectrum of clinical presentations. The classic (malabsorptive) form of celiac disease seen in infants and young children, with chronic diarrhea, muscle wasting, and weight loss, is seen less commonly than those presenting with extraintestinal symptoms or less overt signs of intestinal pathology. In fact, iron deficiency anemia, resistant to oral iron supplementation, is the most common extraintestinal manifestation. While this rate is similarly 1% in the European adult population, European studies have demonstrated an even higher prevalence in children, and the seroprevalence in symptomatic children in the United States is as high as 1:25. Although this disorder is less common in individuals of non-European descent, the prevalence among symptomatic minorities in the United States still remains high. Likewise, the disease is increasingly recognized in the Middle East, India, north Africa, south Asia and Mexico. Celiac disease is triggered by the ingestion of gluten-containing grains (including wheat, rye, and barley) in genetically suscep tible persons. The fact that someone may not develop celiac disease until late adulthood despite being on a lifelong glutencontaining diet, argues for the involvement of environmental cofactors. Environmental cofactors Wheat, and the taxonomically related rye and barley, serve as the environmental trigger in celiac disease patients. Wheat gluten is a protein composite that remains after starch is washed from wheat flour dough. In baking, gluten is responsible for dough elasticity, viscosity (thickness), and increased moisture absorption; however, it is also used as a stabilizing agent in nonbaking products, such as ice cream and ketchup, and as an excipient in many medications. Gluten is a protein composite of gliadins (monomers) and glutenins (polymers), with the gliadin protein being the primary immunogenic and toxic fraction. Barley and rye both possess prolamin fractions equivalent to wheat gliadins (hordeins and secalines, respectively) and demonstrate the same toxic properties in celiac patients. The concordance rate for celiac disease among monozygotic twins is 75%, with a roughly 10% concordance among dizygotic twins. Likewise, the prevalence of celiac disease among firstdegree relatives is as high as 10% in the United States. A United States prospective observational study of at-risk infants demonstrated a decreased risk of celiac disease in children exposed to gluten between 4 and 6 months of life. Whether changing dietary habits reduces the overall risk of disease or simply postpones disease onset is unclear, but it has been hypothesized that the switch from gluten tolerance to that of an immune response depends heavily on the developing intestinal microbiota of infants. Intestinal infections may also contribute to triggering onset of disease, presumably through a rise in small bowel permeability. In symptomatic individuals, the positive predictive value of these tests approaches 1. Current North American guidelines require duodenal biopsies, while on a glutencontaining diet, to make the diagnosis of celiac disease.
Generic vasotec 5mg overnight delivery
However blood pressure medication vision changes buy vasotec 10mg cheap, acquired deficiencies of these factors can occur, and acute onset of bleeding could be attributed to antibodies to these factors. Management: Management of vitamin K deficiency varies by the clinical manifestations and underlying cause. Careful attention to maternal anticonvulsants and other medications will help reduce early hemorrhagic disease of the newborn. In this situation, maternal use of vitamin K will be helpful in reversing any possible effects. Classic hemorrhagic disease of the newborn has been effectively eliminated by administration of vitamin K at birth. Parents who choose to not allow their newborn to be given vitamin K at birth may be placing the infant at risk of vitamin K deficiency, particularly if they are breast fed or encounter malabsorption for any reason (including infectious diarrhea) and decreased oral vitamin K intake. Acute treatment of vitamin K deficiency varies and is similar to the treatment for warfarin reversal. Treatment is based upon the screening laboratories and the clinical manifestations. For the patient who cannot swallow oral medications, the vitamin K can be administered subcutaneously, but the absorption is not as reliable when given by this route. Bleeding Risks with Vitamin K Deficiency 751 Finally, vitamin K can be administered intravenously, however this route has occasionally induced anaphylaxis. If there is concern about volume restriction, prothrombin complex concentrates which include most of the vitamin K-dependent factors might be more helpful (see Chapter 39). Prevention of vitamin K deficiency bleeding in breastfed infants: lessons from the Dutch and Danish biliary atresia registries. Immediate post-operative bleeding, both surgical and secondary to platelet dysfunction, is common in patients coming off cardiopulmonary circuits. This is mostly related to surgical bleeding or bleeding secondary to platelet dysfunction. It is rarer to have hemostatic defects associated with cyanotic heart disease or valvular heart disease, but these will also be discussed. Platelet dysfunction can be a result of activation of platelets with subsequent alpha and dense granule release. Platelet dysfunction may also occur with hypothermia that is often induced during surgery and also secondary to the pump and/or filters with subsequent activation of platelets. The dysfunctional platelets are gradually removed from the circulation, so the nadir of the platelet count often is not reached until 1 to 3 days after the operation. Bleeding may also be the result of mild thrombocytopenia (platelet count <100,000/l) induced by this shortened platelet survival, and also by hemodilution, or by platelet consumption during the procedure. A transient decrease in all of the clotting factors can occur immediately after being placed on the bypass circuit secondary to hemodilution. The liver may also be temporarily affected during bypass surgery, with decreased blood flow causing a temporary decrease in hepatic production of clotting factors. Adults also undergo hypothermia, hemodilution of clotting factors/platelets and antifibrinolytic therapy (with resultant kallikrein inhibition). In general, coagulation abnormalities are rare, but occasionally hepatic congestion from an increased hematocrit can lower production of clotting factors. This laboratory artifact can be overcome by drawing the blood into a syringe containing less citrate to compensate for the decreased plasma. In this condition, there is loss of the high molecular weight multimers secondary to a shearing effect on the von Willebrand protein. Paravalvular leaks have also been reported to induce the same hemostasis phenomenon. It remains controversial whether the bleeding complications are entirely attributable to the use of anticoagulants, and their known ability to induce thrombocytopenia. The bleeding associated with cyanotic and non-cyanotic heart disease is usually milder and mucosal in nature (epistaxis, petechiae and purpura). Platelet transfusions will correct the thrombocytopenia and the platelet dysfunction. However, prior to platelet transfusion, heparin should be reversed to allow the hemostatic system to function in the absence of highdose anticoagulant. Heparin Reversal: After the procedure, the anesthesiologist is careful to reverse the effects of heparin with protamine (see Chapter 52). The etiology of protamine toxicity appears to be either IgE mediated anaphylaxis or complement anaphylactoid-mediated, secondary to heparin-protamine or protamineantiprotamine complexes. Protamine contains arginine which, when converted to nitric oxide, may also contribute to the systemic toxicity of this disorder. The D-dimer is always elevated post-operatively due to normal hemostasis following surgery. These screening tests will first confirm the lack of excessive heparin or thrombocytopenia as potential causes for continued bleeding. Since the D-dimer is elevated as a result of normal post-surgical hemostasis, monitoring D-dimer levels and other coagulation parameters over time is essential to assess for 756 Thomas C. In this setting, plasma products and/or cryoprecipitate would be utilized along with consideration of additional anticoagulation therapy. Management: A normal hemostasis screening laboratory panel will help to exclude heparin, dilutional coagulopathy (including low fibrinogen levels) and platelet dysfunction as contributing causes to ongoing bleeding. Since use of an antifibrinolytic agent may also cause thrombosis, careful monitoring is encouraged. Therapy for Inhibitors to Bovine Thrombin: Increasingly, fibrin glue with human thrombin is utilized as a local tissue sealant but topical bovine thrombin may also still be utilized. These antibodies are best treated with appropriate blood product support and with immunosuppressive agents, corticosteroids, intravenous immunoglobulin or plasma exchange. Cardiopulmonary bypass parameters and hemostatic response to cardiopulmonary bypass in infants versus children. In patients post cardiac surgery do high doses of protamine cause increased bleeding Anticoagulation of children undergoing cardiopulmonary bypass is overestimated by current monitoring techniques. Mechanisms of bleeding and approach to patients with axial-flow left ventricular assist devices. Acquired and reversible von Willebrand disease with high shear stress aortic valve stenosis. The association of a prolonged bleeding time, anemia and uremia has been observed since the 1950s. Dialysis and erythropoietin have greatly decreased the bleeding tendency in renal failure patients. This article will focus on the hemostatic disorders associated with chronic renal disease, although acute renal failure can also present with similar bleeding manifestations. The laboratory findings, differential diagnosis, and management issues associated with renal disease will also be addressed. Pathophysiology: Uremic patients consistently demonstrate disordered platelet/ vessel interaction. Several substances present in uremic patients can contribute to this pathophysiology. First, platelet phospholipids are modified, which affect the release of arachidonic acid, which is subsequently converted to thromboxane A2. Finally, increased platelet aggregation and resultant platelet dysfunction occurs when platelets interact with the surface membrane of the dialysis machine. Reversal of heparin at the end of each treatment is standard, but heparin overdose should be considered in the chronic renal disease patient who unexpectedly bleeds after dialysis. Additionally, medications, including various antibiotics and anti-inflammatory drugs, may affect platelet function. Occasionally, this may contribute to clotting within the shunt placed for dialysis. Nephrotic Syndrome: Nephrotic syndrome is described separately due to the myriad of potential coagulation abnormalities seen. The fibrinogen can be qualitatively abnormal and the resultant dysfibrinogen is characterized by a prolonged thrombin time and reptilase time.
Purchase vasotec online
Gastrointestinal Disease: Thrombosis resulting in ischemia of the bowel arteria occipital discount vasotec 5 mg with amex, colon, or esophagus with resultant gastrointestinal bleeding, as well as splenic and pancreatic infarction has been reported. Antithrombotic Therapy: Appropriate use of antithrombotic agents requires an assessment of the bleeding risk balanced against the risk of thrombosis. However, a small randomized trial and parallel observational study demonstrated no benefit. When the results of both trials were combined in a meta-analysis, a significant excess of minor bleeding was evident in patients allocated to high intensity warfarin. The risk of recurrence appears to be highest during the first 6 months following warfarin discontinuation, with an event rate of 1. Based on this study, some experts recommend aspirin since no anticoagulant monitoring is required compared to warfarin. Expert recommendations based on these studies suggest using intermediate dose unfractionated heparin. The number of plasma exchange procedures required is unknown, but expert recommendations suggest at least five consecutive treatments. Other investigational treatments include the use of rituximab, other immunosuppressive agents and autologous stem cell transplantation, all of which require further study. Antiphospholipid antibodies and subsequent thrombo-occlusive events in patients with ischemic stroke. A comparison of two intensities of warfarin for the prevention of recurrent thrombosis in patients with the antiphospholipid antibody syndrome. Aspirin for primary thrombosis prevention in the antiphospholipid syndrome: a randomized, double-blind, placebocontrolled trial in asymptomatic antiphospholipid antibody-positive individuals. Combination of heparin and aspirin is superior to aspirin alone in enhancing live births in patients with recurrent pregnancy loss and positive anti-phospholipid antibodies: a meta-analysis of randomized controlled trials and meta-regression. Evidence-based recommendations for the prevention and long-term management of thrombosis in antiphospholipid antibody-positive patients: report of a task force at the 13th International Congress on antiphospholipid antibodies. Schulman S, Svenungsson E, Granqvist S and the Duration of Anticoagulation Study Group. Anticardiolipin antibodies predict early recurrence of thromboembolism and death among patients with venous thromboembolism following anticoagulant therapy. These patients had bleeding symptoms different from classic hemophilia and an autosomal inheritance pattern. The clinical manifestations are varied, but usually comprise mucosal bleeding symptoms and bleeding immediately after invasive procedures or surgery. Glycosylation of the molecule takes place and the C terminal dimers are then N-terminal multimerized up to twenty million daltons in size. This manifests itself as a decrease in both antigen levels and functional activity. Multimer patterns, detected by Western blot, show normal size distribution, but decreased band intensity. This can lead to a mild thrombocytopenia (30% of patients) and a lack of the large molecular weight multimers due to increased binding to and clearance with platelets. Some subjects have a defect in the A3 portion (where collagen binding occurs) of the protein. Type 2N has been called autosomal hemophilia A, as it has some symptoms similar to hemophilia A, but without a sex linked pattern. Without a history of bleeding in the patient or a family history of bleeding, it is difficult to assign a diagnosis. Several investigators have recently proposed a bleeding score based upon the history. This score can be applied to children, but is more difficult to compile as children often have not been carefully questioned nor have they been hemostatically challenged. Screening Laboratory Tests: the most important hint in the diagnosis is a positive bleeding history. Occasionally, one dose of an antifibrinolytic may be all that is needed to stop a nose bleed in a child. Additionally, tranexamic acid has been effective at 25 mg/kg/dose, to a maximum of 1. Occasionally, other topical agents such as gel foam, collagen and topical thrombin and fibrin glue can also be helpful in nose and mouth-related bleeding. Topical vasoconstricting agents have been used in conjunction with cauterization for recalcitrant nose bleeds. The intranasal form is administered as one spray (150 mcg) for a patient less than 50 kg and two sprays (300 mcg) for those over 50 kg. More common side effects include facial flushing and headache and occasionally alteration in blood pressure and abdominal cramps. If the medication is given too frequently (greater than three doses within a few days) tachyphylaxis will occur. Blockade of the Fc receptors of the reticuloendothelial system is best achieved by intravenous immunoglobulin. Occasionally, plasma exchange or immunosuppressive agents such as corticosteroids or cyclophosphamide are utilized. Clinical and molecular predictors of thrombocytopenia and risk of bleeding in patients with von Willebrand disease type 2B: a cohort study of 67 patients. The mutational spectrum of type 1 von Willebrand disease: results from a Canadian cohort study. Hemophilia A has an incidence of approximately 1:5,000 male births and accounts for approximately 85% of cases of hemophilia. Clinical Manifestations: the hallmark of hemophilia-related bleeding is delayed bleeding along with joint and muscle bleeding. In general, the severity of bleeding depends upon the percentage of circulating clotting factor activity. Commonly, patients with severe disease will suffer from spontaneous bleeding while those with mild to moderate disease more typically bleed with trauma or surgery. Differential Diagnosis: Hemophilia A and B are clinically indistinguishable, and individual factor levels must be used to clarify the diagnosis. They are typically staffed with hematologists, orthopedists, physical therapists, nurses, psychologists and social workers who specialize in the care of patients with bleeding disorders. To prevent or minimize long-term sequelae, demand therapy should be given as soon as possible after a bleeding episode is recognized. During a bleeding episode, factor replacement therapy should never be delayed to perform imaging or laboratory studies. Ancillary measures such as compressive dressings, cauterization, packing and splinting should also be implemented when appropriate. Prophylaxis: In developed countries, prophylactic therapy delivered one to four times per week is considered the standard of care, and is the only therapy proven to prevent the long-term complication of degenerative joint disease. It is common practice to begin prophylaxis prior to the onset of recurrent joint bleeding so many patients start prophylaxis before the age of 2 years. Liver Transplant: Liver transplantation has been performed in several patients with hemophilia as a result of severe liver disease. They are more likely to occur in the setting of a positive family history of inhibitors, in association with large gene deletions such as introns 1 and 22 inversions and in non-white patients. Autoantibodies can develop in patients without hemophilia, leading to a condition known as acquired hemophilia (see Chapter 128). These autoantibodies occur most commonly in the setting of pregnancy, malignancy and autoimmune conditions, however 50% of cases are idiopathic.
Generic vasotec 10mg without prescription
Therefore the clinical status of the neonate blood pressure chart emergency vasotec 5 mg without a prescription, risk of bleeding/intervention, and platelet count must be considered in making recommendations for platelet transfusions. In practice, it is commonly accepted to maintain the platelet count >50,000/l in a neonate with bleeding symptoms. Additional specific therapy depends on clinical presentation including surgical excision, vascular embolization, compression therapy, immunosuppressive therapy, chemotherapy and anti-coagulation. Treatments may include removal of central catheters, thrombectomy, thrombolysis and anti-coagulation. Platelet transfusion in the neonatal intensive care unit: benefits, risks, alternatives. Platelet transfusions in neonates: practices in the United States vary significantly from those in Austria, Germany, and Switzerland. Platelet transfusion practices among neonatologists in the United States and Canada: results of a survey. Platelet transfusions in infants with necrotizing enterocolitis do not lower mortality but may increase morbidity. International consensus report on the investigation and management of primary immune thrombocytopenia. Clinical manifestations of these syndromes range from a severe platelet function defect in patients with a homozygous deficiency, to mild thrombocytopenia in patients with heterozygous deficiency. Benign Mediterranean Macrothrombocytopenia: Mediterranean macrothrombocytopenia is an autosomal dominant disorder characterized by moderate thrombocytopenia, large platelets and a mild bleeding diathesis. Mediterranean macrothrombocytopenia was first described in 1975 in a study that compared 145 asymptomatic Mediterranean and 200 Northern European subjects. In this study, an increased incidence of individuals with thrombocytopenia and large platelets was noted in the Mediterranean population. Sequencing of consecutive patients who presented to an Italian clinic with symptoms of Mediterranean macrothrombocytopenia identified the Ala156Val mutation in six of the 12 patients. The remaining gene mutations responsible for Mediterranean macrothrombocytopenia are unknown. Thrombocytopenia and Velocardiofacial (DiGeorge) Syndrome: Macrothrombocytopenia often occurs in patients with hemizygous deletion of the chromosomal region 22q11. Both result in thrombocytopenia, and both show an enhanced platelet agglutination response to ristocetin that is particularly observable at low ristocetin concentrations. Autosomal dominant macrothrombocytopenia in Italy is most frequently a type of heterozygous Bernard-Soulier syndrome. Reported mutations include point mutations, splice defects, and small deletions and gene inversion. Members of the kindlin family of proteins are essential for normal integrin activation. Since kindlin-3 is the primary kindlin expressed in the hematopoietic lineage, all integrins present on leukocytes and platelets, including 1, 2, and 3, are dysfunctional. Response to the agglutinating agent, ristocetin, Transfusion Medicine and Hemostasis. Hematopoietic stem cell transplantation may also be an effective therapeutic option in severe cases. The role of platelet lysosomes is unclear, but the release of platelet -granules and -granules following platelet activation contributes to propagation and stability of the forming thrombus. Generally these contents promote the adhesion of platelets, and the stimulation of inflammatory and vascular cells. Adhesion proteins, procoagulant molecules, pro- and anti-angiogenic proteins, inflammatory cytokines, platelet receptors, and bactericidal proteins have been identified within the -granule. Release of different -granule components may be differentially regulated depending upon the agonist used. Either a decrease in number of platelet granules or a defect in their release can result in a bleeding diathesis. Bleeding manifestations in patients with storage granule defects are typically mild. Electron microscopy can be utilized to distinguish defects in -granule release and formation. Platelets from patients with no -granules appear gray when evaluated by light microscopy, due to the absence of the basophilic -granule. Fusion of the -granule membrane with the external platelet membrane occurs upon platelet activation. As a result of this membrane fusion, P-selectin is expressed on the platelet surface. The presence of additional systemic manifestations or hematologic findings may also aid in diagnosis. Care of these patients is often more focused on the accompanying systemic manifestations. In another pedigree, the granule deficiency affects other hematopoietic cells, and gray-appearing neutrophils with absent granules are observed. The gene defect responsible for the classical gray platelet syndrome has recently been identified. Other syndromes may also result in a paucity of -granules and a gray platelet phenotype. White Platelet Syndrome: White platelet syndrome is an autosomal dominant disorder characterized by macrothrombocytopenia and decreased -granule content. This syndrome was recently described in a large multigenerational pedigree from Minnesota. The -granule content of the platelets is low, giving some of the platelets a gray appearance. The unique characteristic of platelets in patients with white platelet syndrome is the presence of large, fully developed Golgi complexes. Other Granule Defects: Quebec platelet syndrome is an autosomal dominant bleeding disorder. Degradation of -granule proteins is due to overexpression of urokinase plasminogen activator in the platelet -granule. Release of the ectopically-expressed urokinase in the formed clot may also result in accelerated clot lysis and delayed bleeding manifestations. Patients with absence of both - and - granules have also been reported in the literature. Mutations in platelet receptors, signaling proteins and synthetic pathways have been identified in patients with granule release and aspirin-like defects. Patients with platelet granule release and aspirin-like defects typically have mild mucocutaneous bleeding. Examples of Failure of Granule Release and Aspirin-like Defects: Thromboxane Pathway Defects: Thromboxane (TxA2) is an agonist released by activated platelets which supports the activation of adjacent platelets. The importance of this pathway in thrombus formation is illustrated by the clinical effectiveness of aspirin. Aspirin-like platelet defects are observed in patients with cyclooxygenase deficiency, and a similar phenotype is observed in patients with a deficiency of another enzyme necessary for TxA2 synthesis, thromboxane synthase. Two clinically important anti-thrombotics, clopidogrel and ticolopidine, function by inactivating P2Y12. These receptors depend on the actions of several G-proteins for activation of downstream signaling pathways. A mutation in the G-protein, Gq, has been found in a patient with a mild bleeding diathesis and decreased aggregation to multiple agonists.
Diseases
- Chromosome 2, monosomy 2q37
- Chromosome 4, trisomy 4q21
- Pseudohermaphroditism female skeletal anomalies
- Subacute sclerosing leucoencephalitis
- Hereditary hearing loss
- Hallermann Streiff syndrome
Buy vasotec 10mg low price
Factor X deficiency: clinical manifestation of 102 subjects from Europe and Latin America with mutations in the factor 10 gene heart attack symptoms in men purchase vasotec 10mg on-line. Abnormalities of prothrombin: a review of the pathophysiology, diagnosis, and treatment. This article will review the more common congenital and acquired hemostatic disorders affecting pregnancy. Congenital Disorders: Preconception and Prenatal Counseling: Management of pregnancy in women with congenital bleeding disorders is best started prior to conception. Preconception counseling allows for discussion with a hematologist, obstetrician and genetic counselor regarding risks to the mother and fetus. If with treatment, levels 50% are achieved, then Transfusion Medicine and Hemostasis. Accordingly, post-partum treatment plans should include strategies to promote identification and management of delayed bleeding. Levels typically increase by about three-fold, but not all patients respond adequately. Therefore it is preferable to have confirmed a response to desmopressin at both 1 and 4 hours after administration prior to its use at the time of a hemostatic challenge. Tachyphylaxis to this drug occurs, so test administration should be done at least several weeks prior to its intended use. Since hyponatremia is a potential adverse event with desmopressin, fluid intake should be reduced to 75% of normal and drinks with higher NaCl content should replace free water for 24 hours after its use. Desmopressin does not cross the placenta in significant amounts, therefore direct effects on the fetus are not of concern. There is concern regarding neonatal hyponatremia if the mother develops hyponatremia prior to delivery. For patients that do not respond or are intolerant to desmopressin, or have disease types where desmopressin is not effective, i. Bleeding Disorders in Pregnancy 731 Management of Bleeding and Breastfeeding: Desmopressin is minimally excreted into breast milk and poorly absorbed by infants, therefore it is thought to be generally safe for use while breastfeeding. Concentrations of tranexamic acid found in the breast milk are low (1% of maternal serum concentrations) and is thought to be a safe alternative for use while breastfeeding. For those with levels 50%, treatment is necessary before neuroaxial anesthesia and delivery. This increases to up to 8% in women who are not known to be carriers, likely due to use of assistive devices during delivery. The risk of intracranial hemorrhage is reduced, though never zero, when an elective Caesarean section is used for delivery. It is important for the patient and obstetrician to discuss the risks and benefits of elective Caesarean section, since there is no consensus that this option should be the mode of delivery for all children known to have severe hemophilia. Platelet Function Defects: Management of platelet function defects at the time of labor and delivery should be based on the prior history of bleeding, patient preferences 732 Christine L. In general, options for treatment include desmopressin, platelet transfusions, and tranexamic acid. In many cases where the platelet defect is mild, desmopressin alone will be sufficient. The pregnant mother may become sensitized to fetal platelet antigens inherited from the father. If this occurs, the mother may become refractory to platelet transfusions and the antibodies may cross the placenta causing fetal/neonatal alloimmune thrombocytopenia. Plasma-derived fibrinogen concentrates are available (see Chapter 39); however they have not been formally tested in pregnant women. Nonetheless, fibrinogen concentrates are preferred over cryoprecipitate as they are heat-treated and therefore considered safer for repeated infusions. During pregnancy, it has been suggested to maintain the fibrinogen level at >60 mg/dl and increase to >150 mg/dl at the time of labor and delivery. Delivery of a Fetus with a Potential Bleeding Disorder: At the time of delivery, if prenatal testing has not excluded a bleeding disorder in the fetus, then the fetus should be handled as though one is present. Specifically, assisted deliveries using forceps and vacuum extraction should be avoided. The use of forceps and vacuum extraction increases the risk of intracranial hemorrhage and cephalohematoma. Medications and immunizations should be delivered subcutaneously rather than intramuscularly and circumcision should be avoided or delayed until adequate work-up can be performed. If a hemorrhage is detected, this is a potential medical emergency, and a pediatric hematologist should be consulted immediately. They occur most commonly within the first 3 months post-partum, and only approximately 5% ante-partum. Corticosteroid therapy should be considered in all patients to facilitate inhibitor eradication. Cyclophosphamide and other therapies can be reserved for those that fail to respond adequately to corticosteroids (see Chapter 121). Thrombocytopenia: When evaluating gravid women with thrombocytopenia, the same general approach is utilized as in non-gravid patients. It is typically mild (platelet count 70,000/l), occurs late in pregnancy, resolves following delivery, does not affect the fetus and occurs in women without a history of thrombocytopenia (excluding a prior history of gestational thrombocytopenia). The platelet count may progressively decline during pregnancy, reaching a nadir in the third trimester. A platelet count 50,000/l is generally considered safe for vaginal and Caesarean delivery, but some physicians prefer a platelet count 80,000/l for neuroaxial anesthesia. These thresholds are based on limited observational data and the most recent version of the American Society of Hematology guidelines does not endorse a specific platelet count for labor and delivery. With longer corticosteroid exposure, there are increased risks of hypertension, hyperglycemia, osteoporosis, and premature rupture of the membranes. Prednisone, prednisolone or methylprednisolone are favored over dexamethasone because the former are well metabolized by the placenta, exposing the fetus to only 10% of the maternal dose. Regardless of the specific corticosteroid used, one should target the lowest possible dose. The second trimester is the optimal time to perform this intervention, because it can frequently lead to miscarriage or premature delivery in the other trimesters. Immunosuppressive agents such as cyclophosphamide, vincristine, and danazol are contraindicated in pregnancy. Azathioprine has been used in women following organ transplantation; however it remains category D because of the potential for fetal harm. A number of case reports have detailed the safe use of rituximab for treatment of lymphoma during pregnancy. The infants in these cases have had abnormal B-cell development that 734 Christine L. Management of the Fetus or Neonate: Maternal antibodies can affect the fetal platelet count, leading to thrombocytopenia in the newborn. Because of the lack of reliability of platelet counts obtained through fetal scalp vein sampling and the risk associated with percutaneous umbilical blood sampling, fetal platelet count monitoring is not recommended. Mild thrombocytopenia may precede other signs and symptoms, such as right upper quadrant pain and elevated liver transaminases. Acute Fatty Liver of Pregnancy: Acute fatty liver of pregnancy is a rare disorder, with liver failure dominating the clinical picture. The presence of pre-eclampsia, right upper quadrant pain and elevated liver enzymes may point towards other pregnancy-related microangiopathies, although there may be times that this distinction is difficult and the response to therapy, delivery and/or plasma exchange may be the only means to distinguish between these disorders. Gynaecological and obstetric management of women with inherited bleeding disorders. A review of the literature with special reference to the value of steroid and immunosuppressive treatment. Pregnancy outcomes after recovery from thrombotic thrombocytopenic purpura-hemolytic uremic syndrome. The underlying defect is either in the vessels themselves or perivascular connective tissue.
Cheap vasotec 5 mg otc
Investigations such as sigmoidoscopy and colonoscopy may be dangerous in this acute situation and should be deferred until there has been reasonable improvement blood pressure medication harmful purchase vasotec cheap. The blood results show mild microcytic anaemia, suggesting chronic blood loss, low potassium from diarrhoea (explaining in part her weakness) and raised urea, but normal creatinine, from loss of water and electrolytes. If the history was just the acute symptoms, then infective causes of diarrhoea would be higher in the differential diagnosis. Although amoxicillin treatment can be associated with bowel disturbance or even Clostridium difficile infection but it is not relevant here since the diarrhoea was present before taking amoxicillin and did not change afterwards. She should be treated immediately with corticosteroids and intravenous fluid replacement, including potassium. If not, the steroids should be continued until the symptoms resolve, and diagnostic procedures such as colonoscopy and biopsy can be carried out safely. Sulphasalazine or mesalazine are used in the chronic maintenance treatment of ulcerative colitis after resolution of the acute attack. In this case, the colon steadily enlarged despite fluid replacement and other appropriate treatment. The ileorectal anastomosis will be reviewed regularly; there is an increased risk of rectal carcinoma. The palpitations are uncomfortable, rapid and began 2 hours ago whilst in the police station. He is not always adherent with his medications, which include metformin, gliclazide, ramipril, a salbutamol metered dose inhaler and a salmeterol with fluticasone metered dose inhaler. His pulse is 185/minute and irregular, blood pressure is 126/73 mmHg and respiratory rate is 18 breaths per minute. Atrial fibrillation can be secondary to a pulmonary embolism, hyperthyroidism, chronic lung disease and electrolyte abnormalities. Investigations should include measurement of electrolytes, thyroid function tests and a chest radiograph. An echocardiogram should be considered in this patient, as structural heart disease is common in older patients. If coronary artery disease is suspected then a cardiac stress test should be performed. Thrombosis can form in the left atrial appendage and typically embolises to the cerebral arteries. Persistent atrial fibrillation may cause structural changes to the heart muscle resulting in cardiomyopathy. Acute management of atrial fibrillation should be resuscitation and control of heart rate. A beta blocker is recommended to control heart rate in those who are haemodynamically stable. Alternative agents include flecainide (if no underlying coronary heart disease), calcium channel blocker (if a beta blocker is contraindicated), or amiodarone or digoxin (useful if the patient has mild heart failure). Patients with a score of 1 or higher should receive long-term anticoagulation with warfarin. Newer anticoagulants, such as dabigatran, may be used as an alternative to warfarin. Those patients with a contraindication to anti-coagulation should receive anti-platelet therapy such as aspirin or clopidogrel. Selecting patients with atrial fibrillation for anticoagulation: stroke risk stratification in patients taking aspirin. There is no clear difference in mortality between a rate control or rhythm control strategy. Rate control aims to keep the heart rate under 100 beats per minute without the restoration of sinus rhythm. In this patient, rate control was achieved with a calcium channel blocker, as a beta-blocker was contraindicated due to his asthma. A proton pump inhibitor was prescribed with the aspirin to prevent aspirin-induced peptic ulcer disease. A diagnosis of acute pharyngitis was made, presumed streptococcal, and oral penicillin was prescribed. The sore throat gradually improved, but 5 days later the patient noted a rash on his arms, legs and face and painful ulceration of his lips and mouth. These symptoms rapidly worsened; he felt very unwell and presented to the emergency department. He has had sore throats occasionally in the past, but they have resolved with throat sweets from the chemist. There were erythematous tender nodules on his arms, legs and face and ulcers with some necrosis of the lips and buccal and pharyngeal mucosae. The pointers to this diagnosis are the rapidity of onset and its timing related to starting the penicillin, with antibiotics the commonest group of drugs causing this syndrome, and the form and distribution of the lesions. The patient had taken a few doses of paracetamol, leaving the penicillin as the likeliest candidate by far as the cause. In the previous 24 h he had become unwell, feeling feverish and with a painful right knee. He works in an international bank and frequently travels to Asia and Australia, from where he had last returned 2 weeks ago. Otherwise, examination of the cardiovascular, respiratory, abdominal and nervous systems is normal. His right knee is swollen and slightly tender, and there is a small effusion with slight limitation of flexion. The diagnosis is made by microscopy of the discharge, which should show Gram-positive diplococci, and culture of a urethral swab. Immediate treatment on clinical grounds with ciprofloxacin is indicated; penicillin should be reserved for gonorrhoea with known penicillin sensitivity to prevent the development of resistant strains. Septic monoarthritis is a complication of gonorrhoea; other metastatic infectious complications are skin lesions and, rarely, perihepatitis, bacterial endocarditis and meningitis. The patient disclosed that he had had unprotected sexual intercourse with prostitutes in Thailand and Singapore; he had had no intercourse following return to the United Kingdom, so no follow-up of contacts was necessary. The pain was intermittent, worse at night, and relieved by ibuprofen, which she bought herself. She worked part-time stacking the shelves in a supermarket and was a very active and competitive tennis and badminton player. She indicated that the pain was over the vertebrae at T5/6, but there was no tenderness, swelling or deformity. The full blood count, urea creatinine and electrolytes, calcium, alkaline phosphatase and phosphate were all normal, as was urine testing. She was advised that the pain was musculoskeletal due to exertion at work and sport, and she was prescribed diclofenac for the pain. After a few weeks of improvement, the pain began to get worse, being more severe and occurring for longer periods and seriously disturbing her sleep. If there is nothing to suggest osteoporosis or trauma, then the commonest cause of this is a tumour metastasis. The tumours that most frequently metastasize to bone are carcinoma of the lung, prostate, thyroid, kidney, and breast. Urgent biopsy confirmed a carcinoma, and she was referred to an oncologist for further management. Review of the first X-ray after the lesion was seen on the second film still failed to identify a lesion, emphasizing the need to repeat an investigation if there is sufficient clinical suspicion of an abnormality, even if an earlier investigation is normal.
Order vasotec canada
In all cases blood pressure cuff amazon order vasotec uk, routine use of rating scales completed before the evaluation and reviewed during the office visit greatly facilitates efficient clinical management. Symptoms must be assessed in their developmental context; that is, they must be of greater frequency and severity than what is typical for others of the same sex, age, and cognitive level. Specific impairments should be documented to verify the diagnosis, establish objective treatment targets, and, if necessary justify medication use and expected duration of treatment. The clinical evaluation should review symptoms of oppositional defiant disorder, disruptive mood dysregulation disorder, conduct disorder, anxiety, depression, mania, autism spectrum disorder, specific learning disorders, intellectual disability, substance abuse, and tic disorders. The clinician must assess whether these are healthy adaptations to the disorder or denial of its consequences. Given the potential for adaptation, diagnosis in adults can be based on a history of multiple impairments over the lifetime, rather than concurrent impairment in multiple domains at the time of evaluation. This allows proper consideration of external factors that might affect behavior and helps identify the full range of psychosocial problems that might require intervention. In older patients, it is helpful to understand living arrangements, the nature of personal support networks, and recreational interests. Clinicians should also be mindful that some, particularly younger, patients can be shy in unfamiliar settings, and that failures to engage with the examiner might not represent usual behavior. It remains unclear whether teacher-completed rating scales are as well validated and sensitive in differentiating normal and abnormal levels of hyperactivity in very young children compared to older youth. However, increasing numbers of preschool-age children are being diagnosed and subsequently treated with medication. Clinicians should also assess potential autism spectrum disorders and intellectual disabilities, as well as problems with hearing, speech and language, elimination disorders, family approaches to parenting, and overall psychosocial history. School-Age Children It is useful in assessing a school-age child to determine what is known or expected about the clinic visit. A question like "What did your mom tell you about why you are coming to the doctor today Nonetheless, it is important to include the child in the assessment, both to aid in evaluation and set the stage for treatment adherence. Common comorbid disorders include learning disorders, autism spectrum disorders, oppositional defiant disorder, anxiety, and tic disorders. Parents and teachers might have their own biases that interfere with accurate reporting. One parent might spend more time with the child and be a more accurate informant than the other. Some parents are particularly motivated to obtain medication and/or academic accommodations, while others are strongly opposed to medication or are concerned about stigma if teachers and others find out about the diagnosis. Others resist the diagnosis, sometimes based on negative views of medication or an unwillingness to provide accommodations or special treatment for the student. Teachers are generally better observers of hyperactive-impulsive symptoms than inattention or distractibility. Impairment in younger patients is generally reflected at home, school, and with peers. Since diagnosis requires evidence of symptoms and impairment in multiple settings, it is necessary to consider other sources of information if parent and teacher reports conflict. While teachers rarely make overtly critical comments on report cards, difficulties are sometimes subtly evidenced by less-than-glowing behavioral assessments. In contrast, high levels of parental complaints in the absence of any school-related difficulty suggests that family issues may be of greater concern and emphasizes the importance of a thorough psychosocial assessment. An essential goal of the initial assessment is developing a degree of trust between the adolescent patient and clinician, which is essential in subsequently developing an effective treatment strategy. Good initial questions are "What is your understanding about what this meeting is for today It is not advisable to meet with parents without the teenager present, unless parents convey that there is highly sensitive information that they would otherwise not discuss. Teacher ratings are less valuable once students leave elementary school, as students rotate through different classrooms over the course of the day. Review of past and current academic records can provide important corroborating evidence for the diagnosis, which is particularly helpful if the patient is uncooperative. For example, adolescents might complain of inner restlessness instead of overactivity. Inattention might manifest as problems with motivation, organization, and completing tasks. These risks should be assessed during the evaluation, and opportunities taken, when indicated, to provide counseling toward reducing them. Adults Adults generally come for evaluation from a sense of personal frustration and lack of accomplishment or due to the insistence of third parties such as spouses, partners, parents, or employers. Parents, spouses, partners, and others, if available, can provide useful corroborating information, but their involvement is limited due to privacy needs. Problems with inattention and executive function often have greater relevance for adults. Common difficulties include problems related to organization, distractibility, time management, and following through on important tasks. Common comorbid conditions include lifetime histories of conduct disorder or antisocial behavior, nicotine dependence, other substance abuse or dependence, depression, anxiety disorders, and risky behaviors (see Chapters 3 and). Physicians, regardless of specialty, should conduct a medical assessment as part of their evaluation. This includes review of current and significant past illnesses, surgeries, current and past chronic medication history, major accidents and physical injuries, and possible loss of consciousness. Specialist physicians should confirm that the patient has had necessary primary care and health maintenance, including appropriate physical examinations and immunizations. The clinical interview provides an additional opportunity to counsel patients on reducing these risks, such as the use of seat belts, not drinking and driving, and safe sex practices. Obstructive sleep apnea or other sleep disorders, seizure disorders, and endocrine disorders, such as thyroid disease and diabetes, should be considered in the context of other supportive history. Physical examination is not typically necessary if the patient has received appropriate general medical management. If abnormal motor movements or vocalizations, that is, tics, are present, their nature, frequency, and intensity should be documented. Vision and hearing tests are not standard but might be considered if indicated by specific history. A positive response to any of these suggests the need for further cardiac evaluation prior to medication treatment. In the absence of positive responses, it is generally accepted that additional cardiac workup is unnecessary. The evaluation should review the family history for other evidence of learning and academic difficulties, mood and anxiety disorders, and problems with substance abuse and/or antisocial behavior. It can also prove useful in treatment planning, particularly if one or both parents are also affected. Screening Questions for Identification of Potential Cardiac Risk Factors for Sudden Death Is there any history of: Unexplained shortness of breath with exercise Family history of sudden or unexplained death in first- or second-degree relatives Cardiomyopathy, heart transplant, pulmonary hypertension, or an implantable defibrillator Answering "yes" to any question should prompt review by an appropriate specialist in cardiology prior to initiation of medication. Appropriate tests provide estimates of intellectual ability and academic achievement, as well as adaptive functioning, if there are questions of intellectual disability (Box 6. Learning disabilities are diagnosed when discrepancies exist between measured intellectual level and academic achievement. Screening tests can be sufficient for an initial assessment with an option to follow up with more comprehensive testing if specific difficulties are suspected. Physicians do not typically perform these examinations, which necessitates referral to a psychologist or educational specialist.
Cheap 5mg vasotec overnight delivery
Options for prevention and treatment of adverse reactions will be described blood pressure medication depression side effects cheap generic vasotec canada, as well as the proper documentation and reporting of such reactions. In addition, fresh products are transfused prior to the final post-processing culture results. The risk of contamination has also been shown to be higher in products collected by large volume leukapheresis, as opposed to standard apheresis. The pathogenicity of the identified organism is of great importance, with gram negative rods raising particular concern. The time to growth and the number of positive cultures add further information to the significance of the culture result. Of the 434 patients, however, one patient who received a product contaminated with Bacillus cereus developed septic shock, highlighting the serious risk of infusing products contaminated with pathogenic organisms. The clinical manifestations are characterized by dyspnea, hypoxia, hypertension, and jugular venous distention. Theoretically, the incidence may be higher than that seen with red blood cell transfusion given the large volume of the product, which is often greater than a liter. Upper and lower airway obstruction and frank anaphylaxis may occur during more severe reactions. Allergic reactions can often be prevented by premedication with antihistamines, steroids, or a combination of both. The primary clinical features are fever and chills, although hypertension is also a commonly-associated symptom. The pathogenesis is due to the accumulation of cytokines in the product or to anti-leukocyte antibodies in the recipient that react with the leukocytes in the product. Reactions Specific to Allogeneic Products: Allogeneic transplants, with the exception of cord blood, are generally infused into the recipient shortly (within 48 hours) after collection from the donor. In the interim, the allogeneic product is maintained at room temperature or refrigerated. The rate of adverse effects during infusion of non-cryopreserved products is lower than that of cryopreserved products. Hemolysis Related to Red Blood Cell Antigen Incompatibility: While the overall rate of infusion-related toxicity is lower, there are several considerations that are unique to allogeneic transplants. The signs and symptoms of acute hemolysis include fever, hypotension, hemoglobinuria, flank pain, and disseminated intravascular coagulopathy. Fortunately, product processing is generally able to prevent significant hemolysis. Therapeutic plasma or red cell exchange of the recipient for major and minor incompatibilities, respectively, may be useful in dire situations. The usual clinical manifestations are dyspnea, hypoxia, fever, tachycardia, and hypotension. The laboratory may be able to plasma reduce the product if the pathogenic antibody is donor-derived. These components are present in varying amounts depending on the collection method and donor characteristics. Furthermore, the amount of granulocytes has been correlated with the severity of infusion toxicity. One study found that products with higher total nucleated count and clumping were more likely to cause reactions. The authors hypothesized that clumps, resulting from cell aggregation, might induce the release of cytokines upon infusion. Of note, both recipient age and gender have been associated with infusion-related toxicity, with more side effects occurring in older patients and in females. Differences in premedication regimens, product composition and volume, infusion rates, and symptom reporting may all contribute to the wide distribution of frequencies. Severe Adverse Events: the severe adverse events related to cryopreserved products can generally be categorized into neurologic or cardiac complications. There have been numerous case reports describing serious infusion-related neurotoxicity, including reversible encephalopathy, transient global amnesia, seizure, and cerebral infarction. Reported incidence ranges from 1 in 51 to 1 in 208 recipients of cryopreserved stem cells. Although most bradycardic events are asymptomatic, requiring no intervention other than close monitoring, there have been rare case reports of fatal bradyarrhythmias. While severe, even fatal, toxicity has occurred, the great majority of the adverse events are mild to moderate in severity and self-limited. Occurrence and severity of adverse events after autologous hematopoietic progenitor cell infusion are related to the amount of granulocytes in the apheresis product. Recovery, viability and clinical toxicity of thawed and washed haematopoietic progenitor cells: analysis of 952 autologous peripheral blood stem cell transplantations. What is the clinical significance of infusing hematopoietic cell grafts contaminated with bacteria Adverse events after infusions of cryopreserved hematopoietic stem cells depend on non-mononuclear cells in the infused suspension and patient age. Sterility testing of hematopoietic progenitor cell products: a single-institution series of culture-positive rates and successful infusion of culture-positive products. Red blood cell-incompatible allogeneic hematopoietic progenitor cell transplantation. Modern cell-based therapies include regenerative medicine, which is the process of replacing or regenerating human cells, tissues or organs to restore or establish normal function. With these advances, a need existed to incorporate quality systems and regulatory oversight into their use. While the basics of quality and quality systems are the same for blood banking/transfusion services and cellular therapies, there are some distinct differences. As additional uses for cell therapies are found, it is expected that there will be further expansion of regulatory oversight (Table 87. Because cellular therapy products often are exchanged internationally, these requirements help to ensure consistency in product quality worldwide. On-site inspections are conducted by inspectors who are qualified by training and experience and who have working knowledge of the industry. These international standards cover all phases of cord blood collection, processing, testing, selection and release and distribution. The Standards cover all aspects of collection, processing, storage, and administration of bone marrow and cells derived from peripheral blood. For umbilical cord blood products, these Standards only apply to the administration of the cellular product. The Standards for Cellular Therapy Products are similar to those for Blood Banks and Transfusion Services with an emphasis on a quality system composed of 10 elements (Table 87. Organization Resources Equipment Agreements Process Controls Documents and Records Deviations and Nonconforming Products or Services Internal and External Assessments Process Improvements Safety and Facilities the Standards and is focused on donor eligibility, collection, processing, storage and distribution. Regulation is focused on safety and efficacy: safety issues include sterility, purity, identity, segregation and tracking, whereas efficacy includes potency and stability. To determine the cost-effectiveness of a drug therapy relative to other traditional and new therapies. Donor eligibility determination should be performed according to written procedures and is required prior to transplant. Personnel should have the education, experience and training to perform their assigned tasks and should only be assigned tasks for which they are trained and deemed competent. Procedures: Well-written procedures that are compliant with regulations are required for all steps in the manufacturing process. These procedures must be reviewed and approved by a responsible person and must be available and easily accessible to those who are doing the work. Facilities: Facilities must be of suitable size and orientation to prevent contamination or mix-ups; facilities must be maintained in a clean and sanitary condition. The manufacturing operations should be performed in clearly defined areas with adequate lighting, ventilation, plumbing, drainage and access to sinks and toilets. Written procedures governing maintenance and cleaning should be in place and followed, and cleaning records should be retained for a defined period of time that is no less than three years.