Buy cheap frumil 5mg online
IgA glomerulonephritis associated with microscopic polyangiitis or Churg-Strauss syndrome symptoms lymphoma buy frumil 5 mg without prescription. Pauci-immune crescentic glomerulonephritis superimposed on diabetic glomerulosclerosis. Necrotizing and crescentic lupus nephritis with antineutrophil cytoplasmic antibody seropositivity. Validation of the new classification of pauci-immune glomerulonephritis in a United States cohort and its correlation with renal outcome. Validation of a newly proposed histopathological classification in Japanese patients with anti-neutrophil cytoplasmic antibody-associated glomerulonephritis. The pathologic spectrum of pulmonary lesions in patients with anti-neutrophil cytoplasmic autoantibodies specific for anti-proteinase 3 and anti-myeloperoxidase. Crescentic glomerulonephritis with a paucity of glomerular immunoglobulin localization. Coexistence of anti-neutrophil cytoplasmic antibody-associated glomerulonephritis and membranous glomerulopathy. Vasculitis affecting the kidney: presentation, histopathology and long-term outcome. Antimyeloperoxidase antibodies induce neutrophil adherence to cultured human endothelial cells. Antineutrophil cytoplasmic antibodies stabilize adhesion and promote migration of flowing neutrophils on endothelial cells. Treatment of rolling neutrophils with antineutrophil cytoplasmic antibodies causes conversion to firm integrin-mediated adhesion. Aggravation of anti-myeloperoxidase antibody-induced glomerulonephritis by bacterial lipopolysaccharide: role of tumor necrosis factor-alpha. Complement activation is involved in renal damage in human antineutrophil cytoplasmic autoantibody associated pauci-immune vasculitis. Circulating complement activation in patients with anti-neutrophil cytoplasmic antibody-associated vasculitis. Alternative complement pathway in the pathogenesis of disease mediated by anti-neutrophil cytoplasmic autoantibodies. Inhibition of complement factor C5 protects against anti-myeloperoxidase antibody-mediated glomerulonephritis in mice. The aetiology of mixed cryoglobulinaemia associated with hepatitis C virus infection. Cryoglobulinemic glomerulonephritis: a membranoproliferative glomerulonephritis induced by hepatitis C virus. Vasculitic purpura with antineutrophil cytoplasmic antibody-positive acute renal failure in a patient with Streptococcus bovis case and Neisseria subflava bacteremia and subacute endocarditis. Subacute bacterial endocarditis with positive cytoplasmic antineutrophil cytoplasmic antibodies and anti-proteinase 3 antibodies. Drug-associated antineutrophil cytoplasmic antibody-positive vasculitis: prevalence among patients with high titers of anti-myeloperoxidase antibodies. Successful pregnancy and delivery of a healthy newborn despite transplacental transfer of antimyeloperoxidase antibodies from a mother with microscopic polyangiitis. Pathogenesis of anti-neutrophil cytoplasmic autoantibody associated small vessel vasculitis. Experimental models of vasculitis and glomerulonephritis induced by antineutrophil cytoplasmic autoantibodies. Antineutrophil cytoplasmic autoantibodies specific for myeloperoxidase cause glomerulonephritis and vasculitis in mice. Antineutrophil cytoplasm antibodies directed against myeloperoxidase augment leukocyte-microvascular interactions in vivo. Anti-neutrophil cytoplasmic autoantibodies induce neutrophils to degranulate and produce oxygen radicals in vitro. Reactivity of antineutrophil cytoplasmic autoantibodies with mononuclear phagocytes. Antineutrophil cytoplasmic antibodies induce human monocytes to produce oxygen radicals in vitro. Antibodies to neutrophil cytoplasmic antigens induce monocyte chemoattractant protein-1 secretion from human monocytes. Anti-myeloperoxidase antibodies stimulate neutrophils to damage human endothelial cells. Autoantibodies developing to myeloperoxidase and proteinase 3 in systemic vasculitis stimulate neutrophil cytotoxicity toward cultured endothelial cells. An unusual endocarditis-induced crescentic glomerulonephritis treated by plasmapheresis. Circulating autoantibodies as serological markers in the differential diagnosis of pulmonary renal syndrome. Treatment of glomerulonephritis in microscopic polyangiitis and Churg-Strauss syndrome: Indications of plasma exchanges, meta-analysis of 2 randomized studies on 140 patients, 32 with glomerulonephritis. Glomerulonephritis due to antineutrophil cytoplasm antibody-associated vasculitis: An update on approaches to management. Plasmapheresis therapy for diffuse alveolar hemorrhage in patients with small-vessel vasculitis. Randomized trial of plasma exchange or high-dosage methylprednisolone as adjunctive therapy for severe renal vasculitis. Predictors of relapse and treatment resistance in antineutrophil cytoplasmic antibody-associated small-vessel vasculitis. Singh Renal Involvement in Polyarteritis Nodosa, Kawasaki Disease, Takayasu Arteritis, and Giant Cell Arteritis Background 715 Nomenclature of systemic vasculitis 715 Historical background of necrotizing arteritis 718 Historical background of large-vessel vasculitis 720 Polyarteritis nodosa 721 Clinical presentation 721 Pathologic findings 721 Etiology and pathogenesis 725 Differential diagnosis 726 Clinical course, prognosis, therapy, and clinicopathologic correlations 726 Kawasaki disease 727 Clinical presentation 727 Pathologic findings 727 Etiology and pathogenesis 728 Differential diagnosis 729 Clinical course, prognosis, and therapy 730 Takayasu arteritis 731 Clinical presentation 731 Pathologic findings 731 Etiology and pathogenesis 732 Differential diagnosis 732 Clinical course, prognosis, and therapy 733 Giant cell arteritis 733 Clinical presentation 733 Pathologic findings 733 Etiology and pathogenesis 735 Differential diagnosis 735 Clinical course, prognosis, and therapy 736 through the walls of vessels, usually postcapillary venules, that does not cause pathologic vessel wall injury is not vasculitis. The chronic phase of vasculitis may be characterized by sclerosis without inflammation; thus, in this instance, a diagnosis of vasculitis is made based on evidence indicating that the sclerosis was preceded by inflammation. Nonspecific chronic inflammation with infiltration by predominantly lymphocytes in the setting of arteriosclerosis should not be considered vasculitis. Vasculitis can affect any type of vessel in any organ and thus results in a broad range of clinical signs and symptoms. Because the kidneys have numerous and diverse vessels, they are a frequent target for many types of vasculitis, especially those that affect predominantly small vessels such as capillaries, venules, arterioles, and small arteries. Different names have been used for the same type of vasculitis, and specific types of vasculitis have been given multiple names. The approach used in this chapter is the 2012 Chapel Hill Consensus Conference Nomenclature System Table 17. Three major categories of vasculitis are large-vessel vasculitis, medium-vessel vasculitis, and small-vessel vasculitis. Although these names imply that the size of the vessels affected by inflammation is the major basis for categorizing vasculitides, this is a gross oversimplification because many factors must be taken into consideration to classify a vasculitis precisely, including the type of vessel involved, the pattern of inflammatory injury, distribution of organ involvement, immunopathologic findings in the tissue and blood, and clinical features. Therefore, diagnostic categorization requires a relatively complex integration of not only pathologic data but also immunologic and clinical data to reach the most appropriate diagnosis. Onset usually in patients younger than 50 Arteritis, often granulomatous, usually affecting the aorta and/or its major branches, with a predilection for the branches of the carotid and vertebral arteries. Onset usually in patients older than 50 and often associated with polymyalgia rheumatica Vasculitis predominantly affecting medium arteries defined as the main visceral arteries and their branches. Usually occurs in infants and young children Vasculitis predominantly affecting small vessels, defined as small intraparenchymal arteries, arterioles, capillaries, and venules. Necrotizing vasculitis, with few or no immune deposits, predominantly affecting small vessels. Necrotizing granulomatous inflammation usually involving the upper and lower respiratory tract and necrotizing vasculitis affecting predominantly small vessels. Eosinophil-rich and necrotizing granulomatous inflammation often involving the respiratory tract, and necrotizing vasculitis predominantly affecting small to medium vessels and associated with asthma and eosinophilia. Vasculitis with cryoglobulin immune deposits affecting small vessels (predominantly capillaries, venules, or arterioles) and associated with cryoglobulins in serum. Vasculitis, with IgA1-dominant immune deposits, affecting small vessels (predominantly capillaries, venules, or arterioles). Vasculitis that is associated with and may be secondary to (caused by) a systemic disease. Notice that arteries can be affected by large-, medium-, and small-vessel vasculitis.
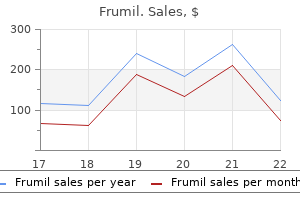
Buy frumil on line
More than half of the patients who initially required replacement dialysis could discontinue dialysis 3 to 18 months later kapous treatment purchase cheap frumil on line. Gross Appearance the kidneys are usually of normal or slightly increased size, although some may be slightly or moderately reduced and scarred because of preexisting arterial narrowing. On cut surface, the paler areas are seen to be minute, wedge-shaped infarcts, much smaller than the usual infarcts seen in the kidney. The surface is finely granular, indicating preexisting renal disease secondary to hypertension. The glomeruli may be unremarkable (A) (periodic acid-Schiff reaction) or may show ischemic features (B) with thickening and wrinkling of the glomerular capillary basement membranes. The lack of staining with methenamine silver (B) in some of the mesangial areas indicates mesangiolysis. Some glomeruli may show little change, whereas others may be congested and infarcted. Accumulation of glomerular intracapillary eosinophilic material with the staining characteristics of fibrin occurs; these fibrin thrombi are localized to the capillary lumina. In other instances, the eosinophilic areas are larger and are referred to as fibrinoid necrosis. The areas of fibrinoid necrosis may contain nuclear debris and ruptured glomerular capillary basement membranes. Fragmented red blood cells can be identified in glomeruli, mostly when intravascular fibrin is present in the glomeruli and small blood vessels. Some glomeruli are sclerosed, either globally or partially, and others show ischemic changes consisting of wrinkling and thickening of the capillary walls with shrinkage and simplification of the glomerular tuft. The juxtaglomerular apparatus is prominent, especially in those cases with severe occlusive arterial and arteriolar lesions. Focal C4d glomerular positivity reported in some of the biopsies in patients with scleroderma renal crisis correlated with tubulointerstitial capillary C4d positivity (549). The characteristic changes in interlobular arteries and smaller arcuate arteries consist of mucoid intimal thickening with concentrically arranged myointimal cellular proliferation ("onion skin" lesion). The mucinous intimal change, which is similar to that seen in severe hypertension, consists of acid mucopolysaccharides of the hyaluronic acid type. Trichrome stain gives either clear reaction or only a weakly blue staining in the thickened mucoid intima indicating no or little mature collagen deposition. This finding is consistent with fibrin with phosphotungstic acid-hematoxylin and Fraser-Lendrum stainings and by immunohistochemical techniques. It represents infiltration of fibrin across the endothelial barrier, incorporation of an intraluminal thrombus into the vessel wall, or coagulation within the vessel wall. In addition, red blood cells or fragments of red blood cells (schistocytes) may be seen in the vascular lumina and permeating the vessel wall. Mucoid intimal hyperplasia of the interlobular arteries with prominent luminal narrowing. A: A small interlobular artery shows luminal narrowing due to pale mucoid intimal thickening and myointimal cellular proliferation. The internal elastic lamina is usually intact, but it may be slightly frayed with no major breaks or gaps. The media and the adventitia of the affected arteries are usually unremarkable; however, the media may be thinned by stretching around the extended intima, and the adventitia has been noted by some authors as being slightly fibrotic (439). Fibrinoid necrosis of the afferent arterioles consists of fibrin in the arterial walls, as seen with small arteries, but the extent of the change is much greater, and the entire wall may be involved. The arteriolar wall may have a smudgy appearance because of swelling of endothelial cells and medial myocytes. Inflammatory cells are usually not seen in fibrinoid necrosis, but such cells may occasionally be present. Sometimes, the arteriolar fibrinoid necrosis is accompanied by luminal thrombus, and on occasion, the process continues into the hilar region of the glomerulus. Arteriolar thrombi were detected in greater frequency than glomerular thrombi in patients with scleroderma renal crisis (549). Diffuse or focal C4d positivity in the renal arteries and arterioles has also been shown in patients with scleroderma renal crisis (549). Tubules are necrotic in the infarcted areas, and sometimes enclaves of necrotic tubules may be found without necrosis of the nearby glomeruli. Extensive (circumferential) fibrin insudation (fibrinoid necrosis) is seen in a small interlobular-size artery. Detachment of the endothelium from the underlying basement membrane is accompanied by subendothelial fibrin deposition in a small interlobularsize artery. There is significant chronicity with extensive tubulointerstitial fibrosis, ischemic glomeruli, and intimal fibroplasia of an interlobular size artery. The patient presented with scleroderma renal crisis; however, she had a long-standing history of systemic sclerosis. This finding does not imply infection but simply represents the normal cellular reaction at the periphery of an infarct; because the infarcts are small, the neutrophilic infiltration appears extensive. The extent of the positivity correlated with worse clinical outcome and also with peritubular capillary leukocyte margination and mild interstitial inflammation. Immunofluorescence Microscopy Fibrin or fibrinogen can be observed along the glomerular capillary walls and sometimes in the mesangium. Glomerular immunostaining with IgM and with C3 is more frequently seen than staining with IgG, IgA, C1q, and C4. Complement factors C3 and C1q are found with the same frequency as IgM, and C4 also has been commonly reported. In one case, scattered hyaline deposits with a periodicity of 9 to 12 nm were found in a subendothelial position in the glomerular capillaries. Glomerular intracapillary thrombi, if present, are composed of fibrin and platelets frequently admixed with fragmented red blood cells. Granular deposits were found in a subendothelial position in the arterioles and were indistinguishable from those seen in patients with hypertension. Fibrin tactoids and fragmented red blood cells can occasionally be seen embedded in the ground substance. Elongated myointimal or smooth muscle cells are present, but no discrete "immunetype" electron-dense deposits corresponding to the positive immunofluorescence findings have been noted. However, differentiation of "immune-type" deposits from areas of hyaline insudation may be difficult. The broad electron-lucent widening between the endothelium and the lamina densa. This widening of the lamina rara interna corresponds to the thickened glomerular capillary walls seen by light microscopy. Thickening and occasional "reduplication" of the glomerular the kidneys of these patients lack distinctive pathologic features and, when seen at autopsy, reveal fibrous intimal arterial thickening with areas of interstitial fibrosis or tubular atrophy. Photomicrograph shows strong fibrinogen positivity in an interlobular size artery (A). IgM positivity is present in the arteriolar wall and also along some of the glomerular capillary walls (B). However, the most severe intimal thickening was observed in patients with scleroderma renal crisis. Of the 44 hypertensive patients, 11 presented with the abrupt onset of severe hypertension associated with rapid deterioration of renal function; they had a poor prognosis-9 died within 2 months and the other 2 underwent bilateral nephrectomy and long-term dialysis. The remaining 33 patients had mild to moderate hypertension, and only 5 died during the follow-up period, the mean of which was 4. There was a longer interval between clinical onset of scleroderma and the development of hypertension in these 33 patients. Presumably, the pathologic features of this group would correspond to what was described in the previous section as the "chronic form," but knowledge of the natural history and pathology of this disorder is limited. The temporal relationship between hypertension and morphologic vascular changes. Considerable evidence indicates that the vascular lesions in patients with scleroderma renal crisis may be the cause of the hypertension rather than the consequence. Four patients had severe vascular changes, two had mild changes, and three had normal vessels. Plasma renin activity was raised in three of the four with severe vascular changes, and further elevation of activity took place in response to cold pressor testing in these four patients, but not in the others.
Cheap frumil
The lumen is nearly totally occluded 714x treatment effective frumil 5 mg, resulting in collapse of the glomerulus being fed by the vessel. The renal arterioles and small arteries show intimal thickening, often with a mucoid appearance resulting in marked narrowing of their lumina. As suggested in the name, thrombotic occlusion of the lumen is often superimposed on this narrowing. The question of the primacy of malignant levels of hypertension in the pathogenesis of these microangiopathic lesions is still controversial. Most of the cases I see now that have the changes I consider representative of malignant nephrosclerosis are superimposed on the kidneys with primary glomerular disease. In these patients, severe renal parenchymal disease is present, and the history is consistent with preexistence of the glomerular disease before the onset of the malignant levels of hypertension. However, I have also seen a patient with IgA nephropathy and the changes of malignant nephrosclerosis in whom glomerular disease was not severe and the tubules and interstitium showed only focal fibrosis and atrophy. Nevertheless, the arteries showed changes consistent with the malignant hypertension, which was present clinically. In that case, I believe that the malignant hypertension was separable from the renal parenchymal disease and was thus primary or essential malignant hypertension. In most cases with microangiopathic changes, malignant hypertension is prominent clinically. In one particularly memorable case of scleroderma renal crisis, the patient never had a recorded blood pressure exceeding 120/80 mm Hg yet had spectacular fibrinoid necrosis of both glomeruli and arterioles. Ultrastructural studies of intimal thickening of larger arteries in hypertension show that the intimal cells are myofibroblasts as characterized by both abundant rough endoplasmic reticulum and myofibrils distributed along the periphery of the cell. Electron microscopy also demonstrates the presence of extracellular proteoglycans (small granules), which are responsible for imparting the mucoid appearance to the thickening (122,138). The most common reactant seen in immunofluorescence studies of malignant hypertension is fibrinogen (134). It may be noted in areas of fibrinoid necrosis, as would be expected, but it is also seen in glomerular capillary loops and in larger vessels without obvious fibrinoid necrosis. On occasion, other immunoglobulins can be identified, presumably accumulating nonspecifically in areas of injury. The mesangium may be intact or show areas of loosening of the matrix, sometimes with finely granular material. Red blood cell fragments, platelets, and fibrin thrombi may be found in arterioles and capillaries. Endothelial cells may be swollen or, in more severely affected areas, they may become necrotic and disappear. The widened subendothelial space contains flocculent material of variable density, sometimes with fibrin tactoids. Ultrastructural studies have suggested that the smooth muscle cells of the media are hypertrophied (122). Furthermore, such studies have also shown the presence of cells with smooth muscle features in the intima (122). Ultrastructural studies of vessels in severe hypertension confirm the presence of fibrin within fibrinoid necrosis, with frequent tactoids noted (122). Smooth muscle cells are necrotic or show various degenerative changes, including loss of microfibrils, vacuole formation, and increased numbers of autophagosomes. In those areas where the endothelium remains intact, one may see swelling of these cells or increased microfilaments, so-called stress fibers, at either the luminal surface or near its attachment to the basal lamina (140,141). An increase in the number of cellular organelles and myofilaments has been shown to occur in vascular endothelium when exposed to shear stress in vitro (142,143). Etiology and Pathogenesis Pathophysiology of Hypertension the pathogenetic mechanisms of essential hypertension are complex, but it is recognized that sodium and fluid balance and vasomotor tone are the major determinants of blood pressure. The electron-lucent area between the two basement membranes contains flocculent material, most notably to the left. Resistance is inversely related to the fourth power of the diameter of the blood vessels (144). Arteriolar diameter is the most powerful determinant of resistance in the short term. In the long term, other factors, such as an increased wall-to-lumen ratio, which affects lumen diameter, and rarefaction, which results in a decrease in the number of arterioles and capillaries, also become important. Furthermore, the level of activation is directly related to severity of hypertension and is associated with greater cardiovascular morbidity and mortality (145). These changes shift the pressure-natriuresis curve to the right so that there is a resetting of arterial pressure up in order to reestablish sodium balance (146,147). A number of mutations in genes associated with sympathetic activation have been recognized in essential hypertension as well as in experimental models of hypertension (61,145). Renal denervation was associated with long-term lowering of arterial pressure in a proof of principle study in patients with hypertension that had been difficult to control (149). Endothelial dysfunction was initially defined as impaired vasodilation in response to such substances as acetylcholine or bradykinin. Other factors involved in endothelial dysfunction include oxidative stress and up-regulation of inflammatory mediators. Endothelial dysfunction has been described in humans with hypertension and in families prior to the onset of hypertension (154). Some subsets of patients with hypertension do not show endothelial dysfunction (153). It is not yet clear whether endothelial dysfunction is a cause or effect in hypertension. RhoA, a member of the Rho family of small G proteins, plays a role in control of vascular tone (157). Oxidative stress is defined by an imbalance between the concentration of free radicals and antioxidant defenses. Numerous epidemiologic papers including several longitudinal studies have established an associative risk between hyperuricemia and essential hypertension (161). This effect is more striking in young and middle-aged populations than in the elderly (96). Furthermore, they showed that the arteriolar lesions that developed were followed by the development of salt sensitivity that was independent of the level of serum uric acid (163). Chapter 20 Renal Disease Caused by Hypertension 865 Numerous studies have demonstrated elevated circulating inflammatory markers in patients with hypertension (166,167). These molecules are also elevated in prehypertensive states and indicate increased risk of developing hypertension (167). Several authors in various reviews have suggested schemas that weave many of these strands into a common pathway to understand the pathogenesis of essential hypertension (161,166,171). However, as arteriolar lesions develop due to effects from these various stimuli, ischemia results as well as defective autoregulation. Another contributing factor to the impairment of autoregulation may be a reduction in nephron number (172,173). Arteriolar injury then reduces blood flow to glomeruli shifting the pressurenatriuresis curve and resulting in increased salt sensitivity and increased blood pressure. Advances in our knowledge of molecular biology have led to the uncovering of these substances and enhanced our understanding of their differing functions and interactions. Although we now can list many of the substances that play an important part in its genesis, we still do not understand all of the interrelationships among them. In this model, the clipped kidney is protected in the short term from hypertension, while the nonclipped kidney is exposed to the elevated systemic pressure and, as a result, manifests both glomerular and vascular injury. Changes in the nonprotected glomeruli include segmental or global necrosis with adhesions and eventual total sclerosis of the tuft. Many different experimental models of hypertension have been developed and are summarized by Dornas and Silva (17). Addition of sodium chloride to the diet exacerbated the hypertension and the glomerular injury (178). The glomerular lesions included glomerular collapse, segmental necrosis, and segmental glomerulosclerosis. Those glomeruli that showed collapse had decreased perfusion, whereas those glomeruli with either sclerosis or necrosis had been exposed to increased pressures.
Cheap frumil 5 mg free shipping
Mild interstitial expansion in patients with long-standing type 1 diabetes is largely due to an increase in interstitial cell component that antedates interstitial fibrosis (135) in treatment order 5mg frumil visa. This is different from the glomerular lesions where mesangial matrix accumulation is the primary cause of mesangial widening even at the early stages of the disease. The extent and/or severity of interstitial fibrosis and global glomerulosclerosis have also been shown to correlate with the clinical manifestations of diabetic nephropathy in patients with type 1 diabetes (137,196). The extent of interstitial fibrosis has long been advocated as an independent predictor of chronic renal dysfunction as characterized by elevated serum creatinine not only in patients with diabetes including those with type 2 diabetes but also in a number of nondiabetic glomerular, tubulointerstitial, and vascular diseases (133,588). In a recent review, Najafian and Mauer (106) state that morphometric techniques are useful predictors of renal functional decline in type 1 diabetes only in later stages and not early in the course of disease. As a corollary, structural-functional correlations in patients with type 2 diabetes are less conclusive than those in patients with type 1diabetes due to the greater morphologic heterogeneity of the renal lesions in these patients. Differential Diagnosis Many features of diabetic nephropathy may occur in other glomerular diseases. For example, the presence of the hyalinosis lesion is not at all specific for the identification of diabetic nephropathy. This lesion may be seen in focal segmental glomerular sclerosis, in chronic pyelonephritis, and in other forms of glomerulonephritis as well. The diffuse lesion, particularly in its early stage of evolution, may also be confused with mesangioproliferative glomerular diseases. However, the lack or slight degree of hypercellularity in diabetic nephropathy may aid in its distinction from these forms. The addition of immunofluorescence and electron microscopic findings to the presence of the diffuse lesion may secure the diagnosis. If severe hyaline arteriolosclerosis is also present, then these findings are virtually specific for diabetic glomerulosclerosis even in the absence of the nodular lesion. The nodular form of diabetic glomerulosclerosis is a distinct entity that should not be confused with other conditions. The more common entities are amyloidosis, immunoglobulin deposition disease, immunotactoid and/ or fibrillary glomerulonephritis, and membranoproliferative glomerulonephritis. The second and third are discussed in Chapters 13 and 27, respectively, and are not considered further here. An algorithmic approach to diagnosis of diseases with organized deposits, which frequently show glomerular nodules, is provided by Herrera and TurbatHerrera (172). Amyloidosis Amyloidosis is the easiest of the three diseases to separate from diabetic glomerulosclerosis. Although similar to the nodules of diabetes in distribution and irregularity of size, the mesangial nodules in this condition are virtually acellular. Furthermore, they stain with Congo red and appear apple green under examination with polarized light. Capillary loops show variability in thickness unlike the uniform thickening seen in diabetic nephropathy. Electron microscopy demonstrates the classic appearance of rigid nonbranching fibrils measuring 8 to 10 nm in diameter. Because these do not stain with Congo red, differentiation from diabetic glomerulosclerosis is more difficult. This difficulty is verified by the fact that the condition was not identified until the late 1970s (594). Before that time, most cases of this condition were diagnosed as either diabetic glomerulosclerosis (in the absence of diabetes) or an anomalous form of membranoproliferative glomerulonephritis. The renal lesion in immunoglobulin deposition disease is characterized by increased lobulation of the glomeruli with nodules forming in the mesangium. Furthermore, the light or heavy chains frequently accumulate in the tubular basement membranes and produce thickening of these structures and a picture similar to diabetic glomerulosclerosis. These nodules and the materials around tubular basement membranes do not stain with silver (see Table 21. This condition is defined by immunofluorescence studies using kappa and lambda light chains or the four subclasses of IgG (595). Immunotactoid and/or Fibrillary Glomerulonephritis Immunoglobulin Deposition Investigators now recognize that certain patients who excrete light or heavy chains of immunoglobulins in the urine, often in association with a plasma cell dyscrasia, may deposit these light chains in the kidney not as fibrils with the configuration of -pleated sheets as in amyloid but as granular Although these lesions may show nodules, they more frequently simulate the diffuse mesangial lesion of diabetes. However, early in these diseases, capillary loops tend to be variably thickened, rather than showing the uniform alteration typical of diabetes. Electron microscopy provides the definitive diagnosis with the characteristic fibrils or microtubules measuring between 15 and 60 nm in diameter. Third, increased cellularity is the typical finding in the mesangium of membranoproliferative pattern of injury, whereas in diabetes, one often sees only a mild increase in the number of cells, which are characteristically situated at the periphery of the nodule. Electron microscopy demonstrates the presence of subendothelial and mesangial immune deposits in type I membranoproliferative glomerulonephritis and C3 glomerulopathies (596). Mesangial increase and nodules are seen in both glomeruli accompanied by cellular proliferation. First, membranoproliferative pattern of injury affects all glomeruli to a similar degree, in contrast to the nodular change of diabetic glomerulosclerosis, which affects only some of the glomeruli. Second, the change of membranoproliferative pattern of injury is uniform with respect to size of nodules and usually is manifest in all or most of the lobules of a given glomerulus. In all cases, the diagnosis of diabetic nephropathy must be excluded on clinical criteria. The patients were most frequently older white men who presented with renal insufficiency and nephrotic range proteinuria. Additional common clinical features included hypertension, history of smoking, hypercholesterolemia, and vascular disease outside the kidneys. The pathology shows many of the characteristic findings of diabetic nephropathy including diffuse mesangial expansion with nodules, microaneurysms, capsular drops, and hyaline arteriolosclerosis. However, their patients also had increased incidence of obesity (60%) and overweight (27%) suggesting that these may be additional risk factors for this condition. In summary, the well-formed nodular lesion with hyaline arteriolosclerosis is virtually pathognomonic of diabetes. However, the pathologist must exclude renal amyloidosis, immunoglobulin deposition disease, immunotactoid and/or fibrillary glomerulonephritis, membranoproliferative glomerulonephritis, and idiopathic nodular glomerulopathy. These lesions may be present independent of diabetic glomerulosclerosis or superimposed on it. In addition, both minimal change disease and focal segmental glomerular sclerosis have been reported (182,607,608), although the occurrence of these two entities can only be definitely established in the absence of diabetic nephropathy. Whether the incidence of any type of glomerular disease is increased in the diabetic population or whether the coexistence of diabetic glomerulosclerosis with other glomerular lesions is a chance occurrence is not known. No studies in human beings have addressed the issue of increased susceptibility of diabetic glomeruli to the formation or deposition of immune complexes. Note numerous capillaries forming within centers of nodules as well as at periphery of nodules. Higher reported frequencies are seen in biopsy studies because unusual clinical features suggestive of nondiabetic renal disease often prompt a biopsy (189). Unbiased studies with proteinuria as the only criterion for biopsy show a frequency of 9% for nondiabetic renal disease (603). In type 2 diabetes, vascular disease especially renal artery stenosis may complicate the clinical picture. Most categories of renal disease may be seen, including glomerulonephritis, pyelonephritis, papillary necrosis, and vascular disease. They found that absence of retinopathy had the highest sensitivity (87%) and specificity (93%) followed by diabetes duration of less than 5 years with sensitivity of 75% and specificity of 70%. These include membranous glomerulonephritis, acute postinfectious glomerulonephritis, IgA nephropathy, Whether diabetic patients have an increased occurrence of renal and urinary tract infections is debated. The incidence of acute infection at autopsy is increased in diabetic patients as compared with nondiabetic patients (609). However, acute renal infection may occur as a terminal event in the diabetic patient and may be related to decreased host resistance to bacterial and fungal infections (610).
Diseases
- Hirschsprung microcephaly cleft palate
- Game Friedman Paradice syndrome
- X chromosome, duplication Xq13 1 q21 1
- Dermatofibroma
- XYY syndrome
- Hoepffner Dreyer Reimers syndrome
- Langerhans cell histiocytosis
Discount frumil 5mg with visa
Immunofluorescence staining for IgM and C1q tends to be quite inconspicuous symptoms zinc deficiency husky 5mg frumil amex, but segmental IgG deposits (probably nonspecific) are not unusual. Bright fibrinogen staining can help to identify focal segmental necrotizing lesions or crescents. In one of these patients, large intraluminal and subendothelial cryoglobulin-like deposits were noted but without microtubular substructure (428). Etiology and Pathogenesis Antibodies against staphylococcal antigens have been proposed in the pathogenesis already in the 1970s. Polyclonal elevation of serum IgA and IgG, as well as circulating immune complexes, is frequently detected (120,414,418). A: the glomeruli showed only mild mesangial hypercellularity and occasional intracapillary polymorphonuclear leukocytes. The same group from Japan developed an experimental model of IgA nephropathy in mice following biweekly immunization of the animals with antigens derived from S. The enterotoxin is usually staphylococcal enterotoxin C, A, or the toxic shock syndrome toxin-1. Also, the superantigen can directly bind to the T-cell receptor V beta region of a large percentage of the total T-cell population, irrespective of the antigen specificity of the receptor. These superantigens are strongly mitogenic for the T cells causing marked T-cell proliferation, and subsequent release of large amounts of lymphokines/ cytokines. These cytokines, in turn, will cause polyclonal B-cell activation and immune complex formation and, eventually, glomerulonephritis. They conclude that in addition to superantigens, conventional Staphylococcus antigens also play a role in the pathogenesis of glomerulonephritis. Staphylococcal enterotoxins acting as superantigens are also implicated in other diseases such as staphylococcal toxic shock syndrome. The differential diagnosis is possible only if detailed clinical data, particularly bacterial culture results and serologies, are available. The differential diagnosis from idiopathic IgA nephropathy or IgA vasculitis can be quite difficult. Of course, as indicated above, theoretically, it is possible that a subset of IgA nephropathy cases are related to staphylococcal infection (422). In our experience, it is more common to see adult IgA-dominant glomerulonephritis associated with purpuric skin lesions in patients with staphylococcus infection. Therefore, if an adult patient presents with symptoms of IgA vasculitis and a renal biopsy shows IgAdominant glomerulonephritis, an underlying staphylococcal infection should always be taken into consideration. The clinical presentation can be quite helpful in making the differential diagnosis. As pointed out above, just based on morphologic findings, the diagnosis of IgA nephropathy will likely be made. As pointed out above, blood cultures are frequently positive and the site/origin of infection may be quite difficult to identify. We always raise the possibility of an underlying staphylococcus infection if we see IgA and C3 codominant glomerulonephritis with an acute clinical presentation. Although IgA nephropathy can show exacerbations with episodic gross hematuria following upper respiratory tract infections, most of these patients do not develop acute kidney injury or heavy proteinuria, and sometimes, C3 staining is mild or even absent. In typical cases of progressive IgA nephropathy, the patients have a protracted, slowly progressive clinical course with persistent microscopic hematuria, hypertension, and gradually worsening proteinuria. Renal biopsy findings usually show a mixture of chronic and active glomerular lesions, including segmental or global glomerular sclerosis, glomerular scars, adhesions, and old fibrous crescents. Rare cases of pauci-immune crescentic and necrotizing glomerulonephritis have been reported in association with staphylococcal infection (417,422). Fortunately, such cases are rare, but the clinical management can be quite problematic because if a pauci-immune crescentic and necrotizing glomerulonephritis is secondary to staphylococcus infection, treatment with cyclophosphamide and steroid may be contraindicated. Fortunately, in most instances, the obvious clinical history of infection, fever, and positive cultures make the differential diagnosis relatively easy. The goal of treatment should be eradication of the infection and management of additional comorbidities that these elderly patients commonly have, such as diabetes, hypertension, congestive heart failure, and surgical complications (2,167,410). Appropriate antibiotics (for methicillin-resistant or methicillin-sensitive staphylococcus), surgical debridement of the infected wounds, or infection sites such as cellulitis, osteomyelitis, are important (421,438). In severe cases of diabetes, even amputation of the infected lower extremity may be required to bring the infection under control. Some antibiotics (such as high doses of vancomycin) used for staphylococcal infections can themselves be nephrotoxic and can cause acute tubular injury and interstitial nephritis. In such instances, it can be difficult to determine the cause(s) of the renal dysfunction. Antibiotic levels, especially vancomycin levels in the blood, may have to be monitored, and the antibiotic may have to be changed to reverse the drug-induced nephrotoxicity. There are no randomized prospective clinical trials on the role of steroids in this condition. However, the patients subsequently may develop sepsis without improvement in renal function (432). Glomerular subepithelial humps are found, and C3 and pneumococcal antigens can be detected in the mesangial regions and along the glomerular capillaries by immunofluorescence (354,355). In view of these findings, it was suggested that the alternative pathway of complement activation had been stimulated by the pneumococcal polysaccharide. Meningococcal infections may cause acute proliferative glomerulonephritis (358,359). Patients with this infection may not have clinical evidence of glomerulonephritis, but they undergo biopsy because of laboratory evidence of circulating immune complexes. Klebsiella capsular polysaccharide antigens, immunoglobulins, and complement have been demonstrated in the glomerular capillaries and in the mesangial regions of a patient with focal proliferative glomerulonephritis and pneumonia caused by Klebsiella organisms (360). In this case, the eluate of the glomerular-bound IgG had antibody specific to Klebsiella.
Purchase online frumil
All paraffin sections medicine in the middle ages purchase frumil in united states online, immunoperoxidase stains; no counterstain (A, E), all other with hematoxylin counterstain. Note that a single patient may suffer from different amyloid diseases simultaneously. It is feasible that the existence of amyloid deposits may induce polymerization of another potentially amyloidogenic (amyloidogenesis-prone) protein. Testing for light chains should be done routinely on all native kidney biopsies, at least on those from adult patients. Interestingly, a low-grade monoclonal gammopathy was detected in 24% of these patients. Thus, both careful clinicopathologic correlation as well as the exclusion of other amyloid types are important. On rare occasion, both light and heavy chain immunoglobulins have been detected by immunofluorescence or mass spectrometry in amyloid deposits (290,362,363). While such reports are intriguing, additional studies are needed to establish whether such a combination Various nonantibody-based analytical tools, derived from proteomics, have been tried in the typing of amyloid deposits. The aim was to develop techniques that would be applicable to the small biopsies that are typical among clinical specimens. The rationale for the application of proteomics methods to amyloid typing lies in the relative abundance of amyloid protein in the tissue, where it is frequently the dominant protein. Although the initial approach was to study the entire proteome (shot gun proteomics), over the years, the techniques have been refined to include sample enrichment methods, such as laser microdissection, and the identification of specific protein targets (targeted proteomics), in order to increase specificity. While the details are beyond the scope of this book, the salient features are summarized below. The amino acid sequences are deduced from a comparison of the observed fragmentation pattern of each peptide with the theoretical fragmentation pattern of all human tryptic peptides predicted by the human genome. A probability score is calculated for individual peptides and ultimately for a given protein. To increase the specificity of the method, multiple peptides from a given protein are analyzed. Given the challenges encountered with amyloid typing in paraffin sections, this is indeed a welcome development. Identification of the amyloid protein is based on the premise that this protein is the most abundant species within the analyzed sample. However, other proteins may be present within amyloid deposits, such as amyloid P component, apolipoprotein E, and various serum proteins. Conversely, small amyloid deposits may be associated with low-abundance proteins/peptides in the examined tissue and, thus, may be obscured by more abundant proteins. The observed peptide fragmentation data must be matched to known protein sequences that are available in public databases, and hence, certain germ-line polymorphisms or somatic mutations may not be identified. These limitations notwithstanding, it has been possible to identify virtually all known amyloid protein types, and thus, the number of cases with undetermined amyloid type has been markedly reduced to 7% with 3% of samples being deemed to be insufficient for analysis (367). Thus, it has now been demonstrated that the C region may be involved in initiating aggregation and providing a template for V region deposition (368). However, additional studies are needed in order to establish that this truly represent a new entity as has been done for other proposed new entities (360,369). Currently, the latter approach would seem to be a safer and more reasonable choice. For antibody-based testing, the intensity of each stain (in relation to amyloid distribution) should be reported; the results of additional studies, if performed/known, should also be included. A scoring system for amyloid involvement of the kidney has been proposed, but, thus far, it has been neither validated nor widely accepted. It has also been critical for the typing of cases with limited antibody reactivity and in the discovery of new protein types and identification of their variants. At high resolution, exceeding that used in diagnostic pathology, amyloid fibrils consist of fibrillary subunits, termed "protofilaments. Typical ultrastructural appearance of amyloid fibrils seen in the mesangium (A and B) and extending into the peripheral glomerular capillary wall and occupying a subepithelial location (C). They may also extend into the peripheral capillary walls, occupying the subendothelial or subepithelial spaces (375). Infiltration of the basement membrane by amyloid may be associated with the loss of argyrophilia and the fraying seen by light microscopy. In endstage amyloidosis, the entire lamina densa of the glomerular basement membrane may be replaced by amyloid, and amyloid may be found in the urinary space and the Bowman capsule. Extremely rare cases of amyloidosis may exhibit massive aggregates of amyloid fibrils in subendothelial and mesangial areas, arranged in tightly packed electron-dense structures, which can be confused with other entities, including membranoproliferative glomerulonephritis, cryoglobulinemic glomerulopathy, and even diffuse proliferative lupus nephritis (374,376,381). Such cases show the expected tinctorial characteristics of amyloid and are typically associated with monoclonal light chains. In the few documented cases of regression of amyloidosis, the glomerular basement membrane remains as a complicated lattice of basal lamina, and there may be a few remaining fibrils or amorphous debris in between the lacunae left behind by the lamellated lamina densa (375). Amyloid is defined as "mainly" an extracellular accumulation of fibrils sharing similar staining and ultrastructural features (267). Various intracellular structures, some with complete (neurofibrillary tangles) and others with partial (inclusion bodies) properties of amyloid, have been encountered in various degenerative diseases (267). Small intracellular aggregates with amyloid properties have been demonstrated in the choroid plexus, in the adrenal cortex, and in the Sertoli cells (383). Early electron microscopic studies also suggested intralysosomal formation of amyloid fibrils (384). Fibrillary amyloid-like structure of crystalline inclusions was also observed in rare cases of light chain proximal tubulopathy (385). Two additional cases of light chain proximal tubulopathy with intracellular lysosomal-like structures exhibiting Congo red positivity and green birefringence were also recently reported (104,386). It is quite possible that in the future, the pathologic definition of amyloid will be extended to include intracellular structures as well. It should be added that the molecular definition of amyloid differs from that used in pathologic diagnosis. At the molecular level, amyloid is defined on the basis of the characteristic conformational arrangement of the proteins, consisting of highly ordered cross-beta sheet structures. This definition therefore extends to synthetic peptides and proteins forming amyloid in vitro. In 1872, Adams documented an association between renal amyloidosis and myeloma (387). The first case of amyloidosis in a patient with myeloma was published in 1902 by Jochmann and Schumm (388), and 15 years later, Glaus (389) reported a second case of amyloidosis associated with myeloma. Approximately 50 years later, Schmiedeberg described the amino acid composition of amyloid and noted that it resembled that of serum globulin (270). The Congo red stain was introduced in 1933 by Bennhold as a diagnostic clinical test and later used as a histologic stain (390,391). Six years later, Divry and Florkin reported green birefringence when amyloid was stained with Congo red and then viewed under polarized light (392). In 1931, Magnus-Levy first suggested a relationship between amyloid and light chain proteinuria (393).
Buy cheapest frumil
Fibrin thrombi can also be seen in the glomerular capillaries and in the lumina of renal arterioles and small arteries symptoms 3 days dpo discount frumil online. In addition, a particulate or flocculent electrondense material is present in the widened subendothelial region of the glomerular capillary wall. The exact nature of the subendothelial material is not known, but it is clearly related to fibrinogen (or fibrin) or other coagulation proteins and probably some matrix proteins. Endothelial Damage Endothelial damage is the crucial feature that precedes the development of additional vascular lesions. All of these factors may contribute to platelet aggregation, thrombus formation, and impaired removal of fibrin with subsequent severe vascular and organ damage. Although the pathogenetic pathways of the endothelial injury for some of the causative agents have been well delineated, for most of the proposed causative agents, the exact mechanism by which the endothelium is injured is still not fully understood. Some factors thought to play a major role in the endothelial injury in the pathogenesis are discussed. The Stx family comprises two main groups, Stx1 and Stx2, each of which contains an increasing number of variants, such as Stx1c, Stx2c, Stx2d, Stx2e, Stx2f, and Stx2g (134). Structurally, both Stxs are composed of an enzymatically active A subunit of 32 kDa and a homopentameric 7. Upon binding of Shiga toxin (Stx) to its specific endothelial receptor Gb3, the endothelial cells acquire a proinflammatory and prothrombotic phenotype, leading to endothelial injury and microvascular thrombosis (T). Binding to the receptor is followed by internalization of the toxin, trafficking via endosomes, and subsequent retrograde transport from the Golgi complex to the endoplasmic reticulum (357). Trafficking of the toxin from the endosomes to the Golgi can be blocked by manganese as shown recently (358). Cessation of protein synthesis initiates a cascade of reactions called the ribotoxic stress response, resulting in cell death (361). It is also well documented that Stx can trigger programmed cell death signaling pathways in various cell types, including human microvascular endothelial cells (362,363). Complement activation in response to Stx generated an increased amount of C3a that caused further endothelial P-selectin expression, loss of endothelial thrombomodulin, and thrombus formation (377). Stx1 and Stx2 bind to different epitopes of the Gb3 receptor with differences in the binding affinity and kinetics. Binding of Stx2 to the receptor is slower; however, dissociation from the receptor is also slower than for Stx1 allowing longer time for internalization (381). This might explain the significantly higher in vitro toxicity of Stx2 on human endothelial cells. It has also been demonstrated that up-regulation of the genes encoding proinflammatory molecules is more efficient when mediated by Stx2 than Stx1 (366,382,383). In general, there is a higher association of more severe disease caused by bacteria producing Stx2 than those producing Stx1 (119). Stxs gain access to systemic circulation via translocation across polarized intestinal epithelial cells, a process facilitated by neutrophil transmigration (387,388). Although erythrocytes, platelets, and monocytes can all bind Stx, both in vitro and in vivo data seem to support polymorphonuclear leukocytes as the carriers of the toxin within the circulation (390,391). Patients with high amounts of Stx on polymorphonuclear leukocytes showed preserved or slightly impaired renal function, whereas cases with low amounts of Stx usually presented evidence of acute renal failure (392). The authors of this paper hypothesized that high amounts of Stx could induce a reduced release of cytokines by the renal endothelium, with a consequent lower degree of inflammation. Conversely, low toxin amounts can trigger the cytokine cascade, provoking inflammation, thereby leading to more significant tissue damage. In vivo studies also suggest that the organ distribution of Stx receptors determines the localization of microvascular lesions in rabbits injected with Stx1 (394). However, cells other than endothelial cells such as renal tubular epithelial cells expressing high levels of Gb3 may also be targeted by Stxs and may contribute to tissue injury (395). The role of anti-Stx antibodies has also been hypothesized in the development of neurologic complications as well as enhancing the toxic effects of Stx on the endothelial cells (79). Inherited and acquired abnormalities of the alternative complement system account for approximately 70% of cases, affect most patients with the familial and the sporadic forms of the disease, and also affect a few cases with the secondary forms (11,36,247). The complement system is part of the innate immune system with a primary role of protecting against infections. The alternative pathway in the plasma is continuously activated by hydrolysis of C3 (so-called "C3 tickover") with the formation of anaphylatoxin C3a and the opsonic fragment C3b, which is being deposited onto plasma-exposed surfaces, including endothelial cells (405). Thrombomodulin, a transmembrane protein with anticoagulant and anti-inflammatory properties, regulates complement activation on cell surfaces (406). In all these forms, endothelial cell injury with acquired prothrombotic phenotype and exposure of the subendothelial surface due to retraction or cell death trigger platelet activation, intravascular coagulation, and thrombus formation (409). Inflammation, also secondary to complement activation, as well as endothelial cell apoptosis, can further exacerbate the injury. The disease will only manifest in patients who have complement abnormalities coupled with a triggering event usually in the background of at-risk haplotypes (408). Most of the mutations are heterozygous clustering in the C-terminal of the molecule with diminished cofactor activity due to low binding of mutant forms to glycosaminoglycans on the endothelial cells or to surface-bound C3b (411,412). Plasma C3 level is decreased in 30% to 50% of patients with heterozygous mutations (11). Most of the mutations are heterozygous and approximately 25% are homozygous or compound heterozygous. The mutant forms may show decreased C3b binding capability, decreased cofactor activity, or decreased expression on blood leukocytes (76,420). Others disrupt cofactor activity with altered degradation of C3b/C4b in the fluid phase and on surfaces (421). The mutated forms bind excessively to C3b, induce an increased stability and activity of the C3 convertase, with enhanced formation and deposition of C5b-9 complexes at endothelial cell surfaces (423). Permanent activation of the alternative pathway results in very low C3 levels in these patients. In two large independent cohorts with 152 patients, the penetrance of disease phenotype was reported to be approximately 50% (424b). A possible explanation for the incomplete penetrance is that polymorphic changes in complement regulatory proteins may act as modifiers. In one of the two cohorts of patients included in the study of FremeauxBacchi et al. In addition, a heterozygous mutation of factor H was found in the patient who developed chronic renal failure but not in her sister who presented with exclusive neurologic symptoms. However, there are individuals with the predisposing genetic mutation(s) who remain asymptomatic pointing to additional extrinsic and/or intrinsic factors in the development of the disease. The familial forms with complement abnormalities reveal genetic heterogeneity, and a significant proportion of the sporadic forms also have genetic abnormality. The pathogenesis has been attributed to the action of neuraminidase to expose the usually hidden T-crypt antigen (Thomsen-Friedenreich antigen) by removing part of the protective glycocalyx (Nacetylneuraminic acid) from membrane surfaces (89). Because most people have preformed circulating IgM antibodies to this antigen, the antigen-antibody reaction followed by complement activation through the classical pathway damages endothelial, red-cell, and platelet surfaces (89,434) and leads to intravascular thrombosis, hemolysis, and thrombocytopenia. Thrombocytopenia is caused by consumption of activated platelets in microthrombi and mechanical destruction in peripheral, damaged microvessels. Locally-produced cytokines can augment microvascular injury by up-regulation of the endothelial Stx receptor Gb3 and also via amplification of the inflammatory response (371). Direct interaction of the inflammatory cells with activated endothelial cells can further contribute to the endothelial cell injury. Polymorphonuclear leukocytes stimulated by Stx induce apoptosis in cocultured endothelial cells (474). Distinction might be aided by the apparent discrepancy between the morphologic severity of such lesions and the severity of the hypertension. Morphologic findings that were available from 32 patients indicated fibrin thrombi in the glomerular capillaries, arterioles, and interlobular arteries in 75%, 46%, and 33% of cases, respectively. The correlation between the presence of intraglomerular thrombi and anticardiolipin antibodies was also significant. Antiphospholipid syndrome nephropathy was statistically associated with lupus anticoagulants, and it was also an independent risk factor for more severely altered renal function. There is also evidence indicating that some of the antiphospholipid antibodies can hinder inactivation of procoagulant factors and resolution of clots by binding to proteases involved in hemostasis and fibrinolysis, such as plasmin, tissue plasminogen activator, and activated factor X (493,494).
Cheap frumil generic
Some fungi 9 medications that cause fatigue generic frumil 5 mg without prescription, for example, Aspergillus, tend to be angiocentric, as opposed to Candida, which tends to be glomerulocentric. Infections originate from mucosal surfaces of the oral cavity, upper respiratory tract, digestive tract, and vagina, followed by hematogenous dissemination. The mean time of onset of systemic Candida infections is 22 days after hospitalization. Furthermore, when skin/mucosal barriers are breached by medical devices or surgery, it opens a portal of entry for pathogens like C. For instance, major abdominal surgery poses an increased risk for systemic Candida infections, which is underlined by the observation that in a cohort of 107 patients with candidemia, 50% underwent recent surgery (134). Presenting symptoms are those of severe renal infection, with low-grade fever, flank pain, costovertebral angle tenderness, hematuria, hypotension, progressive loss of renal function, and acute renal failure. Fungus balls may develop in the pelvis and calyces (135), and their passage may result in ureteral colic. Recovery of Candida from urine specimens, together with positive blood culture, suggests disseminated infection. However, in comparison with other fungi, invasion of blood vessels by Candida is less common, and cortical infarction Candidiasis Pathogenesis Granulomas are the hallmark of mycobacterial infection, but fungi, parasites, and even viruses cause granulomatous inflammation. The mycobacterial granuloma seems to be a host defense mechanism for walling off the bacilli, but microorganisms can survive within macrophages that compose the granulomas and persist in a latent form until immunosuppression and other triggers cause reactivation and dissemination. An understanding of the pathophysiology of granulomas is critical for the design of new drugs and vaccines. Animal models including mice, guinea pigs, rabbits, and monkeys, and in vitro systems were developed that reproduce granulomatous inflammation (132). In addition, the role of innate immunity Chapter 24 Pyelonephritis and Other Infections, Reflux Nephropathy, Hydronephrosis, and Nephrolithiasis 1057 where through surface receptors bind to extracellular matrix components. These include patients with defective T-cell function or immunosuppression who are unable to adequately contain the fungus. To colonize surface epithelia, Candida organisms adhere to epithelial cells through mannoproteins, hydrophobic forces (137), and proteins that bind iC3b receptors. Unless phagocytosed, Candida organisms reach the subepithelial layer Candida glabrata (previously classified as Torulopsis glabrata) (140) is an opportunistic yeast-like fungus present in the normal microflora of the oropharynx, gastrointestinal tract, skin, urethra, and vagina. The kidneys are usually involved as part of disseminated infections, but they may be the site of a primary infection through the ascending route, particularly in diabetic patients. Aspergillosis Aspergillosis can be caused by various species of aspergilli, but the most common pathogen is A. Bundles of fungal pseudohyphae invade the interstitium and tubules; fungal spores are focally present (arrow); an inflammatory response is lacking. Autopsy kidney from a 49-year-old man who died abruptly from disseminated candidiasis involving multiple organs. Renal aspergillosis is frequently the result of hematogenous dissemination, usually from invasive bronchial infection, necrotizing pneumonitis, or infarct by aspergilli. Patients receiving corticosteroids, neutropenic patients, diabetics, and immunocompromised patients (26) are particularly at risk. Renal parenchymal infections may produce symptoms comparable to those of acute pyelonephritis. The urinary tract may be obstructed by growth of mycelium, and fungus balls may be passed into the urine. Renal involvement occurs in 30% to 40% of patients who die of disseminated aspergillosis (136). The involvement may be bilateral in systemic infections and in those with isolated renal involvement. Multiple small abscesses, a few millimeters in diameter and each surrounded by a red rim, are most common. However, extensive abscess formation with vascular invasion, thrombosis, and infarction may occur. Microscopic examination reveals inflammation with mononuclear cells and neutrophils. Abscess formation and infarcts containing typical septate branching hyphae are also seen. The mechanism of Aspergillus infection involves adherence to epithelial surfaces and release neutrophil phagocytosis. Cryptococcosis Cryptococcus neoformans, the agent of cryptococcosis, is a yeastlike fungus encountered in avian habitats, particularly those contaminated with pigeon dropping. Pulmonary infection is common, particularly in immunosuppressed and neutropenic patients. Hematogenous dissemination results in central nervous system and organ-based infection, including the kidneys. Renal involvement may be clinically silent or may manifest with costovertebral angle tenderness, pyuria, and gross hematuria. Yeast forms can be cultured from the urine and can be recognized in the urinary sediment by negative staining with India ink. Renal involvement is found in about 50% of patients who die of disseminated cryptococcosis (136). Small parenchymal abscesses, or granulomas, with central necrosis involving the cortex and medulla have been described (136). The organism may elicit little inflammation despite extensive tubular destruction. Eliminating cryptococci from sites of infection involves growth inhibition, a process that depends on nitric oxide production by phagocytes, and phagocytosis by macrophages, a complement-dependent mechanism modulated by cytokines. Histoplasmosis Histoplasmosis, caused by Histoplasma capsulatum, is endemic in South and Central America and in the Ohio River and Mississippi River valleys in the United States (136). Infection is caused by inhalation of dust particles from soil contaminated with bird or bat droppings containing the fungus. Yeast within glomeruli and tubules are separated by clear halos corresponding to their thick capsule. Renal involvement is usually clinically silent, and compromise of renal function is uncommon. The kidneys are involved in about 40% of patients as a result of progressive disseminated histoplasmosis. Grossly, lesions range from one or more well-circumscribed nodules to diffuse inflammation and necrosis. Microscopically, small aggregates of yeast-laden macrophages may be present in all renal compartments, usually associated with granulomas. The histologic diagnosis of histoplasmosis can be confirmed by immunofluorescence with antibodies to polysaccharide antigens of H. Coccidioidomycosis, caused by Coccidioides immitis, is endemic in the southwest and western United States. Sporadic cases of disseminated coccidioidomycosis have been reported in nonendemic areas. In nature, the fungus is in a mycelial form, but it produces arthroconidia, which is the infective form. Although not contagious, coccidioidomycosis is transmissible during autopsy procedures, presumably through aerosolization of endospores (145). The kidneys are involved in one third of patients who die of disseminated infection (136). Coccidioides immitis organisms are easily found in active lesions within macrophages or giant cells as thick-walled spherules, about 100 m in diameter, containing endospores that are 5 to 30 m in diameter (136). Disease progression has been equated with attenuation of cellular immunity from antigen overload, suppressor cells, immune complexes, and immunosuppressive factors released from the fungus. Containment of infection depends on cellular immunity that, through release of lymphokines, enhances phagosome-lysosome fusion and killing of the fungus as described above for other fungi. North American blastomycosis, caused by Blastomyces dermatitidis, is endemic in the Ohio and Mississippi River valleys and the southeastern United States (136). Primarily, a pulmonary infection disseminates through blood to various organs, including the kidneys. In severe infections, fever, weight loss, chest pain, cough, costovertebral angle tenderness, flank pain, renal insufficiency, and chronic discharging sinuses or subcutaneous abscesses have been reported. The diagnosis can be established through culture or by identifying the organism in fluids or tissue sections. Involvement is often bilateral and varies from small, circumscribed nodules to diffuse inflammation and necrosis (136).