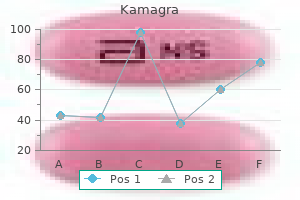
Discount 50 mg kamagra otc
Postvoid residual volumes of the bladder use a urinary catheter placed into the bladder to measure any urine remaining in t he bladder after voiding erectile dysfunction medicine in bangladesh cheap kamagra 50 mg free shipping. Cystoscopy might help identify the presence of bladder tumors, cysts, or foreign bodies. Treatment of incontinence depends on the type of incontinence and may include behavioral techniques, medication, medical devices, therapeutic intervention, and surgery. Incontinence can be managed by wearing sanitary napkins, incontinence pads, adult diapers, or waterproof briefs. Behavioral techniques include activities such as double voiding, scheduled toileting, bladder training, fluid restriction, and accessory muscle exercise. Scheduled toileting involves voiding every two to four hours instead of waiting for the urge to urinate. A urethral insert is a small disposable tampon-like device that is inserted in the urethra to act as a plug to prevent leakage. A pessary may be used to prevent incontinence due to a prolapsed bladder or uterus. This small stiff ring is inserted into the vagina and lifts the bladder to prevent urine leakage. Therapeutic interventions include collagen injec tions, Botox injection, and nerve stimulation. Botox injections into the bladder muscle may benefit people who have an overactive bladder. Nerve stimulators resem ble a small pacemaker and may be implanted under the skin of the buttocks to deliver painless electrical pulses to the sacral nerves which are involved in bladder control. Urinary incontinence surgeries include sling procedure, bladder neck suspension, and artificial urinary sphincter. The sling procedure is often completed laparo scopically and involves using tissue, mesh, or sutures to develop a "sling or hammock" under the urethra or bladder neck. The bladder neck is an area of thickened muscle where the urethra connects to the bladder. This sling attaches to pelvic tissue or the abdominal wall and supports the urethra to help keep it closed. This surgery reinforces the bladder neck so it does not sag and lead to urine leak age. Surgery to insert an artificial urinary sphincter may be necessary to treat males with incontinence often related to prostate surgery or prostate cancer. A small fluid-filled ring (artificial sphincter) is implanted around the bladder neck to hold the urinary sphincter closed. In order to urinate, the male presses a valve implanted under the skin that deflates the ring and allows urine flow. Decreasing risk involves maintaining a healthy weight, not smoking, avoiding bladder irritants such as coffee and alcohol, eating more fiber, and remaining physically active. It usually occurs in males after age 60 and is more common in males than in females. The most important risk factor is cigarette smoking, which increases the chance of cancer proportionate to the number of cigarettes smoked during the life of the affected individual. Other predisposing factors include exposure to industrial chemicals and chronic cystitis. This type of injury occurs when an individual accidentally falls in a straddling position. Instances when straddle injuries can occur include walking a fence or roof beam or, in some cases, riding a horse or motorcycle. Symptoms include hematuria, dysuria, and nocturia, but these symptoms do not usually appear until late in the course of the disease. Neurogenic bladder is dysfunction of the bladder due to some type of injury to the nervous system supplying the urinary tract or bladder. A symptom of bladder cancer is hematuria (blood in the urine) which usually triggers the need for further testing, but hematuria is also found when there are other urinary system disorders such as infections, kidney stones that are passed, and other problems. The study found that the results of the tests varied based on age, gender, and smoking behavior, and that the results should be interpreted considering these factors along with other symptoms in the patient. The recommendations included the need for additional information and careful interpretation of the tests to decide the best intervention for the patient. In the future, these findings might help prevent unnecessary treatment for some patients, especially the elderly who might not tolerate diagnostic or surgical intervention very well. A common trauma that causes neurogenic bladder is a spinal cord injury such as those sustained in motor vehicle accidents or diving accidents. Other traumatic causes include cerebrovascular accidents, strokes, tumors, and herniated lumbar disks. Individuals might have no feeling of the need to void, or they might feel like they need to void all the time. Other symptoms are mild to severe urinary incontinence, difficulty or inability to empty the bladder, and bladder spasms. Intermittent self-catheterization can be taught to individuals unable to empty the bladder to prevent hydronephrosis and possible renal failure. The prognosis of neurogenic bladder depends on the possibility of reversing the nerve damage. Herniated lumbar disks that cause neurogenic bladder are com monly repaired and rapidly restore bladder function. Typ ically, this disease affects young women and is thought to be autoimmune in nature. The inflammation and swelling of the inner lining of the bladder decrease the capacity of the bladder, lead ing to the need to urinate frequently. Other symptoms include pain above the pubic area and lower abdomen, bladder fullness, and urgency. Treatment includes instillation of liquid medica tions into the bladder to distend the bladder and treat the disorder. Treatment can be n eeded for up to 12 weeks, but response to treatment is generally good. It is frequently due to changes in other body systems in the aging process rather than to the urinary system. In older males, benign prostatic hypertrophy is a common disorder that often causes urinary frequency, dribbling, pain or burning with urination, and difficulty starting the urine flow. In older females, the changes in estrogen levels can cause a decrease in vaginal muscle tone and, along with the changes in structure, cause increased frequency and some urine incontinence. Changes in lower abdomen muscle tone, usually the result of multiple pregnancies or obesity, also contrib ute to some urinary incontinence in the older adult female. In other cases, prevention is aimed at rapid diagnosis and treatment of the cause. For instance, fecal impactions that are common in the institutionalized older individual also can cause urinary incontinence. Some medications can cause changes in the ability of the bladder to empty thoroughly, causing overflow incontinence. Many older adults take medications such as antidepressants, narcotic pain relievers, or cardiac drugs that can cause some urinary retention, eventually resulting in incontinence. Individuals who have some difficulty rising from a chair or bed, or who walk slowly, often have periods of incontinence simply because they cannot get to the restroom in time. Lack of mobility causes the individual to be dependent on others for toileting, and this frequently leads to urinary incontinence problems. This system maintains homeostasis in the body by excreting and reabsorbing important electrolytes, compounds, and water. Urinary disorders range from mild infections to very serious diseases such as cancer. The most common disorders of the urinary system include infections and incontinence. Some diseases are diagnosed by urinalysis or urine culture and sensitivity, but radiologic examinations are also used. In the older adult, urinary incontinence is the most frequent problem of the system.
Krameria triandra (Rhatany). Kamagra.
- Are there any interactions with medications?
- Dosing considerations for Rhatany.
- Are there safety concerns?
- How does Rhatany work?
- Intestinal inflammation (enteritis), chest pain (angina), leg ulcers, mild mouth and throat irritation, and other conditions.
- What is Rhatany?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96396
Cheap 100 mg kamagra with amex
Also erectile dysfunction pills generic buy generic kamagra 100mg line, spring-loaded devices, used with syringes, may be helpful for patients who are not accommodated to injections. Insulin pumps can also be used to continuously administer insulin lispro, aspart, or regular insulin. They can eliminate the need for multiple injections every day, allow the utmost flexibility in meal timing, and greatly reduce glucose level variances. Disadvantages of insulin pumps include cost, the fact that they must be worn externally, and mechanical failures that can lead to interrupted insulin supplies. For safe and effective use, insulin pumps must be often and closely self-monitored as to their proper function. Newer oligomeric or liposomal oral insulins, transmucosal forms such as intranasal and oral spray forms, and even transdermal delivery systems are being studied and developed. It is more common when a patient attempts to achieve close glucose control and achieve near-normoglycemia. The symptoms of mild or moderate hypoglycemia include headache, diaphoresis, lightheadedness, palpitations, agitation, blurred vision, and confusion. For older people, hypoglycemia can cause stroke-like symptoms, including aphasia or hemiparesis. Type 1 diabetes patients who have had the disease for a long time may be unaware of hypoglycemic episodes due to lack of awareness of autonomic symptoms, known as hypoglycemia unawareness. The patient must be educated about hypoglycemia symptoms, which usually respond very quickly to ingestion of sugar in candies, juices, or glucose tablets. The patient must check glucose levels 15 minutes following ingestion, and then ingest another 15 g if glucose levels are not more than 80 mg/dL. Hyperglycemia may follow hypoglycemia if excessive sugar was ingested, or because the hypoglycemic condition resulted in a surge of counter-regulatory hormones. When an insulin dose at bedtime is too high, this can cause a counter-regulatory response that results in morning hyperglycemia, known as the Somogyi phenomenon. More commonly, morning hyperglycemia is due to a rise in early Treatment of Diabetes Chapter 11 167 morning growth hormone, known as the dawn phenomenon. When this happens, evening insulin dosing should be increased, replaced with a longer-acting type of insulin, or injected at a later time. With human insulins, local allergic reactions at the injection site are rare, but can still occur if the patient has an allergy to latex, due to the natural rubber latex within the vial stopper. There will be immediate pain or burning, followed by erythema, itching, and induration that can last for days. The majority of reactions disappear on their own after weeks of continued injections, with no specific treatment. A generalized allergic reaction can also occur when insulin is restarted after there has been a treatment lapse. Symptoms occur 30 minutes to 2 hours after injection, including angioedema, urticaria, itching, bronchospasm, and anaphylaxis. If insulin treatment must occur following such a reaction, skin testing is performed, using a panel of purified insulin preparations and desensitization. This is believed to be due to an immune reaction to a component of the insulin form. In type 2 diabetes, insulin resistance is most common, usually because of obesity and genetic factors. This form of insulin resistances may be treated by changing insulin preparations, from animal to human insulin, or by administered corticosteroids if needed. The twice per day regimens use split-mixed doses of rapid- and intermediate-acting insulins. These include single fixed (basal) doses of long-acting insulin and variable prandial (bolus) doses of rapid-acting insulin. Intensive treatment involves glucose monitoring four or more times per day, and three or more injections per day, or continuous insulin infusion. Conventional treatment involves one to two insulin injections per day, with or without monitoring. Intensive treatment is more effective in preventing diabetic nephropathy, neuropathy, and retinopathy. However, it may cause more frequent hypoglycemia and weight gain, and is usually effective only in patients who can and will be very active in their self-care. The remainder is given as a rapid- or short-acting insulin to cover postprandial increases. This is best when doses of rapid- or short-acting insulins are determined using a sliding scale that considers preprandial glucose and the contents of each meal. This allows more lifestyle freedom, since the patient can skin meals, or eat them at different times, and still maintain normoglycemia. After that, regimen choice is usually based on physiologic responses and the preferences of the patient and physician. Glucose levels are often controlled enough with just lifestyle changes or oral medications. Insulin should be added when there is inadequate glucose control by two or more oral medications. Combination therapy is best used when it involves insulin with oral biguanides and insulin sensitizers. Regimens may range from a single injection per day of long- or intermediate-acting insulins, usually at bedtime, to multiple injections. Owing to insulin resistance, some type 2 diabetes patients need very large doses of more than 2 units/kg per day. This is usually due to reduced loss of glucose in the urine, and improvements in metabolism. However, insulin is often added when two or more drugs are not able to give enough glycemic control. They may also help improve peripheral and hepatic insulin sensitivity via reduction of glucose toxicity. With regular use they can potentiate insulin resistance, making them less beneficial. Risk factors include use of drugs with long mechanisms of action, such as chlorpropamide, glipizide, or glyburide; age over 65 years; irregular eating and exercise; and hepatic or renal insufficiency. When hypoglycemia is caused by long-acting drugs, it can last for days after treatment is stopped. The drug chlorpropamide also causes a syndrome of inappropriate antidiuretic hormone secretion. More likely, when insulin secretion and insulin resistance worsen, this is probably more closely linked to diabetes mellitus than to medications used to treat it. Short-Acting Insulin Secretagogues these agents, which include nateglinide and repaglinide, stimulate the secretion of insulin in a way that is similar to the sulfonylureas. They act faster, and may stimulate secretion of insulin more during meals than at other times in the day. This makes them highly effective in the reduction of postprandial hyperglycemia, with lower risks of hypoglycemia. Since nateglinide is slightly less effective, it is best used for patients with only mild hyperglycemia. Biguanides Biguanides decrease hepatic glucose production-both gluconeogenesis and glycogenolysis-to lower plasma glucose. The way they stimulate peripheral glucose uptake may just be an effect of reductions in glucose from their hepatic effects. They may increase beta cell sensitivity to circulating glucose, and also decrease plasminogen activator inhibitor 1 levels, causing an antithrombotic effect. The only biguanide that is commercially available in the United States is metformin, which is just as effective as the sulfonylureas for reducing plasma glucose. It is safely used with insulin and other drugs, and only rarely causes hypoglycemia. Metformin causes no weight gain, and can promote weight loss via appetite suppression. The less common adverse effects of metformin include malabsorption of vitamin B12, without any significant anemia.
Buy discount kamagra on-line
Infants are particularly susceptible to excess vitamin D erectile dysfunction treatment tablets buy kamagra paypal, and if the condition is not corrected, they may develop premature arteriosclerosis, supravalvular aortic stenosis and renal acidosis. The activity of this fat-soluble vitamin is found in a number of dietary constituents, principally in -tocopherol. Dietary deficiency of vitamin E can occur in children as a result of mutations in the -tocopherol transfer protein and in adults with various malabsorption syndromes. The deficiency may present clinically as spinocerebellar ataxia, skeletal myopathy and pigmented retinopathy. In premature infants, hemolytic anemia, thrombocytosis and edema have been associated with vitamin E deficiency. Vitamin E therapy has been reported to improve hemolytic anemia in premature newborns and may reduce the severity but not the incidence of retrolental fibroplasia. Vitamin E is reported to retard development of cirrhosis in infants with congenital biliary atresia. A number of interesting experimental effects are produced by vitamin E, such as inhibition of (1) platelet aggregation, (2) conversion of dietary nitrites to carcinogenic nitrosamines and (3) prostaglandin synthesis. Protection against toxins that exert their activity through production of free radical oxygen species has also been shown. Attempts to use vitamin E as a pharmacologic agent to prevent cancer and coronary artery disease have been unsuccessful. Vitamin D deficiency results from (1) insufficient dietary vitamin D, (2) insufficient production of vitamin D in the skin because of limited sunlight exposure, (3) inadequate absorption of vitamin D from the diet (as in the fat malabsorption syndromes) or (4) abnormal conversion of vitamin D to its bioactive metabolites. It was a disease that affected the urban poor to a much greater extent than their rural counterparts. A partial explanation for this difference lies in the greater exposure of rural residents to Vitamin K Vitamin K, a fat-soluble material, occurs in two forms: vitamin K1, from plants, and vitamin K2, which is principally synthesized by the normal intestinal bacteria. Green leafy vegetables are rich in vitamin K and liver and dairy products contain smaller amounts. However, inadequate dietary intake of vitamin K does occasionally occur in conjunction with chronic illness associated with anorexia. Vitamin K deficiency is common in severe fat malabsorption, as seen in sprue and biliary tract obstruction. Destruction of intestinal flora by antibiotics may also result in vitamin K deficiency. Newborn infants frequently exhibit vitamin K deficiency because the vitamin is not transported well across the placenta and the sterile gut of the newborn does not have bacteria to produce it. Deficiency of vitamin K can be serious, because it can lead to catastrophic bleeding. These amino acids are required in the diet and are considered to be essential amino acids. Another nine amino acids can be synthesized in the human body from simple precursors or from other amino acids. Finally, two amino acids (cysteine, tyrosine) are conditionally dispensable because their synthesis is limited under certain conditions or when adequate quantities of precursors are not available. Table 8-6 lists the 20 amino acids and the extent to which they must be acquired in the diet. Deficiency of essential amino acids is manifest as protein deficiency (kwashiorkor; see above). Leucine (L) Lysine (K) Methionine (M) Phenylalanine (F) Proline (P) Serine (S) Threonine (T) Tryptophan (W) Tyrosine (Y) Valine (V) Increasing Use of Vitamins Recent years have witnessed an explosion of interest in potential pharmacologic uses of vitamins, unrelated to treating dietary or other deficiencies. Consequently, many people are consuming certain vitamins in doses that far exceed what is needed to prevent deficiency diseases. It is likely that studies of such people will provide information regarding both the potential beneficial and toxic effects of large doses of vitamins. An inherited disorder of zinc metabolism, acrodermatitis enteropathica, which is a chronic form of zinc deficiency, is characterized by diarrhea, rash, hair loss, muscle wasting and mental irritability. Similar symptoms are seen in acute zinc deficiency associated with total parenteral nutrition. Zinc deficiency is also seen in diseases that cause malabsorption, such as Crohn disease, celiac disease, cirrhosis and alcoholism. Dietary copper deficiency is rare but may occur in certain inherited disorders, in malabsorption syndromes and during total parenteral nutrition. The most common result is microcytic anemia, although megaloblastic changes have also been described. Manganese deficiency has been described and causes poor growth, skeletal abnormalities, reproductive impairment, ataxia and convulsions. Industrial exposure to manganese causes symptoms closely related to those of parkinsonism. Essential Trace Minerals Are Mostly Components of Enzymes and Cofactors Essential trace minerals include iron, copper, iodine, zinc, cobalt, selenium, manganese, nickel, chromium, tin, molybdenum, vanadium, silicon and fluorine. These are discussed in Chapters 26 and 27, which deal with blood and endocrine diseases, respectively. Chronic zinc deficiency has been reported in Iran and Egypt to result in hypogonadal dwarfism in boys. They have caused more pain, suffering, disability and premature death than any other category of diseases in history. Bacterial and viral diarrheas, bacterial pneumonias, tuberculosis, measles, malaria, hepatitis B, pertussis and tetanus kill more people each year than all cancers and cardiovascular diseases (Table 9-1). Even in the developed countries of Europe and North America, the mortality, morbidity and loss of economic productivity from infectious diseases is enormous. It is estimated that smallpox alone claimed between 300 million and 500 million human lives during the 20th century alone. Although smallpox has been eradicated from the natural environment, a multitude of other infectious agents continue to claim millions of lives each year. Even in industrialized nations, the morbidity and mortality from infectious disease is still substantial. In the United States, sepsis alone is responsible for an estimated 200,000 deaths per year (see Chapter 12). It is instructive that in 1970, the Surgeon General of the United States declared, "The time has come for us to close the book on infectious disease. The recent concern over these and other infectious diseases underscores the facts that the potential for future infectious threats to human existence is real, animal reservoirs of microbes that can be transmitted to humans are bottomless and vigilance can never be relaxed. Finally, the possibility that people may seek to use infectious agents as weapons of warfare should dispel any complacency that we are safe from these pathogens. Infectious Diseases Feature Tissue Damage from an Invading Transmissible Agent Infectious diseases represent many of the familiar taxa: bacteria, fungi, protozoa and various parasitic worms. Viruses cannot replicate by themselves and are obligate intracellular parasites that hijack the replicative machinery of susceptible cells. Likewise, prions, the class of proteinaceous infectious agents, lack nucleic acids and clearly represent a different infectious disease paradigm. Many of these maladies, such as influenza, syphilis and tuberculosis, are contagious. Yet many infectious diseases, such as legionellosis, histoplasmosis and toxoplasmosis, are not contagious but are rather acquired from the environment. Legionella bacteria normally replicate in aquatic amebas but can infect humans via aerosolized water or through microaspiration of contaminated water. Other infectious agents come from many diverse sources: animals, insects, soil, air, inanimate objects and the endogenous microbial flora of the human body. Perhaps the greatest paradox is that certain retroviruses have actually been incorporated into the human genome and are passed from generation to generation. Their function is unclear but their possible activation during placentation has led to speculation that such endogenous retroviruses may have allowed placental mammals to evolve. All these discoveries were made before an intelligible theory of causation of these illnesses existed. That theory arrived with the work of Koch, Pasteur, Lister and Ehrlich, who established the field of microbiology. This feat led directly to identification of agents responsible for many infectious diseases, establishment of effective standards of antisepsis and, eventually, the discovery and development of antibiotics to treat common bacterial, fungal, helminthic and protozoal diseases. The organism must (1) gain access to the body, (2) avoid multiple host defenses, (3) accommodate to growth in the human milieu and (4) parasitize human resources. Many people, particularly blacks, lack these determinants and are not susceptible to infection with P.
100mg kamagra
It also causes watery diarrhea erectile dysfunction at age 21 cheap kamagra on line, probably by interfering with fluid absorption in the colon. Although shigellae extensively damage the epithelium of the ileum and colon, they rarely invade beyond the intestinal lamina propria, and bacteremia is uncommon. The ulcers have a longitudinal orientation because they are located over hyperplastic and necrotic Peyer patches. Bacilli attach to the villi in the small intestine, invade the mucosa and pass to the intestinal lymphoid follicles and draining mesenteric lymph nodes. The organisms proliferate further within mononuclear phagocytic cells of the lymphoid follicles, lymph nodes, liver and spleen. Bacilli are sequestered intracellularly in the intestinal and mesenteric lymphatic system. The intestinal mucosa becomes enlarged and necrotic, forming characteristic mucosal lesions. The intestinal lymphoid tissues become hyperplastic and contain "typhoid nodules"-aggregates of macrophages ("typhoid cells") that phagocytose bacteria, erythrocytes and degenerated lymphocytes. Bacilli proliferate in several organs, reappear in the intestine, are excreted in stool and may invade through the intestinal wall. Necrotic intestinal mucosa sloughs, producing ulcers, which hemorrhage or perforate into the peritoneal cavity. Ulcers appear first on the edges of mucosal folds, perpendicular to the long axis of the colon. A patchy inflammatory pseudomembrane, composed of neutrophils, fibrin and necrotic epithelium, is commonly found on the most severely affected areas. These are small-volume stools that contain gross blood, sloughed pseudomembranes and mucus. Cramping abdominal pain, tenesmus and urgency at stool typically accompany the diarrhea. Cholera Is an Epidemic Enteritis Usually Acquired from Contaminated Water Cholera is a severe diarrheal illness caused by the enterotoxin of Vibrio cholerae, an aerobic, curved gram-negative rod. The organism proliferates in the lumen of the small intestine and causes profuse watery diarrhea, rapid dehydration and (if fluids are not restored) shock and death within 24 hours of the onset of symptoms. The amount of diarrhea is highly variable, but the rapidity and volume loss in severe cases can be staggering. Water and electrolyte loss can lead to shock and death within hours if the volume is not replaced. Replacing lost salts and water is a simple, effective treatment, often achievable by oral rehydration with preparations of salt, glucose and water. Vibrio parahaemolyticus There are several "noncholera" vibrios, of which Vibrio parahaemolyticus is the most common. It is found in marine life and coastal waters around the world in temperate climates, causing outbreaks in the summer. Its range may be expanding, as confirmed cases have occurred in Alaska, more than 1000 miles north of any previous outbreaks. Gastroenteritis is associated with consumption of inadequately cooked or poorly refrigerated seafood. A major pandemic occurred between 1961 and 1974, extending throughout Asia, the Middle East, southern Russia, the Mediterranean basin and parts of Africa. Following the 2010 earthquake in Haiti, an outbreak of cholera occurred, the largest in recent history, which killed 8000 Haitians and hospitalized hundreds of thousands more, while spreading to neighboring nations Cuba and the Dominican Republic. They do not invade the mucosa but cause diarrhea by elaborating a potent exotoxin, cholera toxin, which is composed of A and B subunits. Most fluid secretion occurs in the Campylobacter jejuni Is the Most Common Cause of Bacterial Diarrhea in the Developed World Campylobacter jejuni is the major human pathogen in the genus Campylobacter. The organism is distributed worldwide and is responsible for over 2 million cases annually in the United States. The bacteria inhabit gastrointestinal tracts of many animal species, including cows, sheep, chickens and dogs, which are a significant animal reservoir for infection. Raw milk and inadequately cooked poultry and meat are frequent sources of disease. The agent elaborates several toxic proteins that correlate with the severity of the symptoms. Infection comes from water contaminated with Vibrio cholerae or food prepared with contaminated water. Although they do not invade the intestinal mucosa, vibrios elaborate a potent toxin that induces a massive outpouring of water and electrolytes. In severe cases, infection progresses to small ulcers and patchy inflammatory exudates (pseudomembranes) composed of necrotic cells, neutrophils, fibrin and debris. Epithelial crypts in the colon often fill with neutrophils, forming so-called crypt abscesses. Yersinia Infections Produce Painful Diarrhea Yesinia enterocolitica and Yersinia pseudotuberculosis are gramnegative coccoid or rod-shaped bacteria. A few patients develop a more severe, protracted illness, resembling acute ulcerative colitis. Abdominal pain in the right lower quadrant has led to an incorrect diagnosis of appendicitis. Legionella Cause Mild to Life-threatening Pneumonia Legionella pneumophila is a minute aerobic bacillus that has the cell wall structure of a gram-negative organism but reacts poorly with Gram stains. It was first identified 6 months after an outbreak of a severe respiratory disease of unknown cause at the 1976 American Legion convention in Philadelphia. Subsequently, retrospective studies demonstrated antibodies in sera from previously unexplained epidemics, dating to 1957. They survive chlorination and proliferate in devices such as cooling towers, water heaters, humidifiers and evaporative condensers. The disease is not contagious, and the organism is not part of normal human flora. Predisposing factors are obstructive pulmonary disease in endotracheal tubes, indwelling catheters, debilitating conditions and immunosuppression. Secondary pneumonia caused by these bacteria may complicate influenza or other respiratory viral infections. The pulmonary parenchyma becomes consolidated, and a mucoid exudate of macrophages, fibrin and edema fluid fills the alveoli. Klebsiella and Enterobacter infections may be complicated by fulminating, often fatal, septicemia, and aggressive antibiotic therapy is required. Recently, a group of highly drug-resistant members of the Enterobacteriaceae, including Klebsiella and Enterobacter, have emerged and are spreading throughout the world. The pathogenesis of Legionella pneumonia (Legionnaires disease) is understood in some detail, whereas that of Pontiac fever remains largely a mystery. Legionella pneumonia begins when the organisms arrive in the terminal bronchioles or alveoli, where they are phagocytosed by alveolar macrophages. The bacteria replicate within phagosomes and protect themselves by blocking fusion of lysosomes with the phagosomes. When immunity develops, macrophages are activated and cease to support such intracellular growth. Native respiratory tract defenses, such as the mucociliary blanket of the airway, provide a first line of defense against Legionella infection in the lower respiratory tract.
Purchase kamagra 50mg line
Individual filaments of Actinomyces cannot be discerned with hematoxylin and eosin stain but are readily visible on Gram staining or silver impregnation herbal erectile dysfunction pills canada buy kamagra 50 mg without a prescription. It is caused by a number of anaerobic and microaerophilic bacteria termed Actinomyces. These are branching, filamentous, gram-positive rods that normally reside in the oropharynx, gastrointestinal tract and vagina. Several Actinomyces species cause human disease, the most common being Actinomyces israelii. If infection originates in a tooth socket or the tonsils, it is characterized by swelling of the jaw ("lumpy jaw"), face and neck, at first painless and fluctuant but later painful. In pulmonary infections, sinus tracts may penetrate from lobe to lobe, through the pleura and into ribs and vertebrae. Abdominal or pelvic disease may present as an expanding mass, suggesting an enlarging tumor. Actinomycosis responds to prolonged antibiotic therapy; penicillin is highly effective. Nocardiosis Is a Suppurative Respiratory Infection in Immunocompromised Hosts Nocardia are aerobic, gram-positive filamentous, branching bacteria. They are weakly acid-fast, as distinguished from the morphologically similar actinomycetes. Nocardiosis is most common in patients with impaired immunity, particularly cell-mediated immunity. Trauma can produce tissue necrosis, providing an excellent anaerobic medium for growth of Actinomyces and inoculating the organism into normally sterile tissue. The individual filaments of Actinomyces israeli are readily visible with the silver impregnation technique. Two other pathogenic species of Nocardia, Nocardia brasiliensis and Nocardia caviae, may cause pulmonary nocardiosis resembling that produced by N. If an infected person mounts a vigorous cell-mediated immune response, the infection may be eliminated. In immunocompromised people, however, Nocardia produces pulmonary abscesses, which are frequently multiple and confluent. Direct extension to the pleura, trachea and heart and blood-borne metastases to the brain or skin carry a grave prognosis. Nocardial abscesses are filled with neutrophils, necrotic debris and scattered organisms. With the Gram Spirochetal Infections Spirochetes are long, slender, helical bacteria with specialized cell envelopes that permit them to move by flexion and rotation. Specialized techniques, such as darkfield microscopy or silver impregnation, are needed to visualize them. They have the basic cell wall structure of gram-negative bacteria but stain poorly with the Gram stain. Three genera of spirochetes, Treponema, Borrelia and Leptospira, cause human disease (Table 9-5). They are adept at evading host inflammatory and immunologic defenses, and diseases caused by these organisms are all chronic or relapsing. Urbanization and mass movements of people caused by war contributed to its rapid spread. Originally, syphilis was an acute disease that caused destructive skin lesions and early death, but it has become milder, with a more protracted and insidious clinical course. A silver stain of a necrotic exudate reveals the branching, filamentous rods of Nocardia asteroides. Infection may also spread from an infected mother to her fetus (congenital syphilis). Person-to-person transmission requires direct contact between a rich source of spirochetes. Chronic infection and inflammation cause tissue destruction, sometimes for decades. They appear 1 week to 3 months after exposure, with an average of 3 weeks, and tend to be solitary, with firm raised borders. Chancres, as well as the lesions of the other stages of syphilis, show a characteristic "luetic vasculitis," with endothelial cell proliferation and swelling and vessel walls thickened by lymphocytes and fibrosis. They are painless and may go unnoticed especially in the uterine cervix, anal canal and mouth. Skin: Secondary syphilis most often appears as an erythematous and maculopapular rash of the trunk and extremities, often including the palms. Other skin lesions in secondary syphilis include condylomata lata (exudative plaques in the perineum, vulva or scrotum, which abound in spirochetes). Mucous membranes: Lesions on mucosal surfaces of the mouth and genital organs, called mucous patches, teem with organisms and are highly infectious. Lymph nodes: Characteristic changes in lymph nodes, especially epitrochlear nodes, include a thickened capsule, follicular hyperplasia, increased plasma cells and macrophages and luetic vasculitis. A photomicrograph shows papillomatous hyperplasia of the epidermis with underlying chronic inflammation. Tertiary Syphilis Causes Neurologic and Vascular Diseases After lesions of secondary syphilis subside, an asymptomatic period of years to decades follows. During this time, spirochetes continue to multiply, and the deep-seated lesions of tertiary syphilis gradually develop in one third of untreated patients. Focal ischemic necrosis secondary to obliterative endarteritis is the underlying mechanism for many of the processes associated with tertiary syphilis. These cells infiltrate small arteries and arterioles, producing a characteristic obstructive vascular lesion (endarteritis obliterans). They are surrounded by concentric layers of proliferating fibroblasts, giving the vascular lesions an "onion skin" appearance. Syphilitic aortitis: this disorder results from a slowly progressive endarteritis obliterans of vasa vasorum that eventually leads to necrosis of the aortic media, gradual weakening and stretching of the aortic wall and aortic aneurysm. Syphilitic aneurysms are saccular and involve the ascending aorta, which is an unusual site for the much more common atherosclerotic aneurysms. On gross examination, the aortic intima is rough and pitted (treebark appearance;. The aortic media is gradually replaced by scar tissue, after which the aorta loses strength and resilience. The aorta stretches, becoming progressively thinner to the point of rupture, massive hemorrhage and sudden death. Damage to , and scarring of, the ascending aorta also commonly leads to dilation of the aortic ring, separation of the valve cusps and regurgitation of blood through the aortic valve (aortic insufficiency). Luetic vasculitis may narrow or occlude the coronary arteries and cause myocardial infarction. Neurosyphilis: the slowly progressive infection damages the meninges, cerebral cortex, spinal cord, cranial nerves or eyes. Thus, there are meningovascular syphilis (meninges), tabes dorsalis (spinal cord) and general paresis (cerebral cortex) (see Chapter 32). The ascending aorta exhibits a roughened intima (arrow, "tree bark" appearance), owing to destruction of the media. A patient with tertiary syphilis shows a sharply circumscribed gumma in the testis, characterized by a fibrogranulomatous wall and a necrotic center. The lesions in the late stage include cutaneous gummas, which are destructive to the face and upper airway. These granulomatous lesions have a central area of coagulative necrosis, epithelioid macrophages, occasional giant cells and peripheral fibrous tissue. Gummas are usually localized lesions that do not significantly damage the patient. Congenital Syphilis Is Transmitted from an Infected Mother to the Fetus In this setting, the treponeme disseminates in fetal tissues, which are injured by the proliferating organisms and accompanying inflammatory response.
Order kamagra online
Some undergo these metamorphoses in different hosts before attaining adulthood erectile dysfunction beat filthy frank buy kamagra once a day, and the human host may be only one in a series that supports this maturation process. Within the human body, the helminths frequently migrate from the port of entry through several organs to a site of final infection. With two exceptions, they do not multiply in the human body, so a single organism cannot become an overwhelming infection. The exceptions are Strongyloides stercoralis and Capillaria philippinensis, which can complete their life cycle and multiply within the human body. For example, morbidity in schistosomiasis, the most destructive helminthic infection, results from granulomatous responses to schistosome eggs deposited in tissue. Primary amebic meningoencephalitis is rare (fewer than 300 reported cases), affecting people who swim or bathe in these waters. Parasitic helminths are categorized based on overall morphology and the structure of digestive tissues: 457 Roundworms (nematodes) are elongate cylindrical organisms with tubular digestive tracts. Flatworms (trematodes) are dorsoventrally flattened organisms with digestive tracts that end in blind loops. Tapeworms (cestodes) are segmented organisms with separate head and body parts; they lack a digestive tract and absorb nutrients through their outer walls. Lymphatic vessels harboring adult worms are dilated, and their endothelial lining is thickened. In adjacent tissues, worms are surrounded by chronic inflammation, including eosinophils. A granulomatous reaction may develop, and degenerating worms can provoke acute inflammation. Microfilariae are seen in blood vessels and lymphatics, and degenerating microfilariae also provoke a chronic inflammatory reaction. After repeated bouts of lymphangitis, lymph nodes and lymphatics become densely fibrotic, often containing calcified remnants of the worms. Adult worms inhabit the lymphatics, most frequently in inguinal, epitrochlear and axillary lymph nodes, testis and epididymis. There they cause acute lymphangitis and, in a minority of infected subjects, lymphatic obstruction, leading to severe lymphedema. These and similar organisms are known as filarial worms, because of their threadlike appearance (from the Latin filum, meaning "thread"). In a small subset, late manifestations of disease appear after two to three decades of recurrent bouts of filarial fevers. Diethylcarbamazine and ivermectin are the agents effective against lymphatic filariasis. Occult filariasis, characterized by indirect evidence of filarial infection (antifilarial antibodies), is the cause of tropical pulmonary eosinophilia. This condition is virtually restricted to southern India and some Pacific Islands. Patients present with cough, wheezing, diffuse pulmonary infiltrates and peripheral eosinophilia. Humans, the only definitive host of these filarial nematodes, acquire infection from the bites of at least 80 species of mosquitoes of the genera Culex, Aedes, Anopheles and Mansonia. After maturing into adult forms over Onchocerciasis Causes Blindness Onchocerciasis ("river blindness") is a chronic inflammatory disease of the skin, eyes and lymphatics caused by the filarial nematode Onchocerca volvulus. The disease is transmitted by bites of Simulium damnosum blackflies, which transmit infectious larvae to humans, who are the only definitive hosts. Onchocerciasis is thus endemic along rivers and streams (hence, "river blindness") in parts of tropical Africa, southern Mexico, Central America and South America. The manifestations of filariasis result from inflammatory responses to degenerating adult worms in the lymphatics. Repeated infections are common in endemic regions and produce numerous bouts of lymphangitis (filarial fevers), which cause extensive scarring and obstruction of lymphatics over years. In its most severe form (<5% of the infected population), this is known as elephantiasis. However, gravid females release millions of microfilariae, which migrate into the skin, eyes, lymph nodes and deep organs, producing corresponding onchocercal lesions. Inflammatory damage to the cornea, choroid or retina causes partial or total loss of vision. Cutaneous inflammation results in microabscess formation and chronic degenerative changes in the epidermis and dermis. In lymph nodes and lymphatics, responses to dying microfilariae produce chronic lymphatic obstruction and localized dependent edema. Active lesions in the eyes and lymphatics all show degenerating microfilariae surrounded by chronic inflammation, including eosinophils. Ocular involvement leads to sclerosing keratitis, iridocyclitis, chorioretinitis and optic atrophy. Rarely, those infected may develop acute generalized loiasis, characterized by obstructive fibrin thrombi, containing degenerating microfilariae in small vessels of most organs. Brain involvement, with obstruction of vessels by filarial thrombi, may cause lethal and sudden diffuse cerebral ischemia. Skin manifestations begin with generalized pruritus, which becomes so intense that it can interfere with sleeping. Continuing damage produces areas of depigmentation, hypertrophy or atrophy of the skin. Chronic lymphadenitis is followed by localized edema, which may cause chronic swelling (elephantiasis) of the legs, scrotum or other dependent portions of the body. Some patients have pruritic, red, subcutaneous "Calabar" swellings, which may be a reaction to migrating adult worms or to microfilariae in the skin. Treatment with microfilariacides may initiate massive death of microfilariae and provoke fever, meningoencephalitis and death. Clinical symptoms occur almost exclusively in patients with very large numbers of worms or who are immunocompromised. Infection spreads from person to person via eggs or larvae passed in the stool or deposited in the perianal region. Infection is most prevalent in settings where hand washing and hygienic disposal of feces are lacking. Warm, moist climates are required for the infectious forms of many intestinal nematodes to survive outside the body. Loiasis Principally Affects the Eyes and Skin Loiasis is infection by the filarial nematode Loa loa, the African "eyeworm. Humans and baboons are the definitive hosts, and infection is transmitted by mango flies. Adult worms (4 cm long) migrate in the skin and occasionally cross the eye beneath the conjunctiva, making the patient acutely aware of this infection. Gravid worms discharge microfilariae, which circulate in the blood during the day but reside in capillaries of the skin, lungs and other organs at night. Ascariasis Is an Infestation of the Small Bowel Ascariasis refers to infection by the large roundworm Ascaris lumbricoides. Infection is worldwide but is most common in areas with warm climates and poor sanitation. Adult worms live in the cecum and upper colon, where females produce eggs that pass in the feces. Ascaris larvae emerge in the small intestine, penetrate the bowel wall and reach the lungs through the venous circulation. They leave the pulmonary capillaries, enter the alveoli and then migrate up the trachea to the glottis, where they are swallowed and again reach the small bowel. Heavy infections may be complicated by vomiting, malnutrition and sometimes intestinal obstruction. On rare occasions, worms enter the ampulla of Vater or pancreatic or biliary ducts, where they may cause obstruction, acute pancreatitis, suppurative cholangitis and liver abscesses. Ascaris pneumonia, which may be fatal, develops when large numbers of larvae migrate within the air spaces. Occasionally, adult worms may pass with the stools or even emerge from the nose or mouth. This invasion causes small erosions, focal active inflammation and continuous loss of small quantities of blood.
Syndromes
- Is it worse after drinking?
- Eat only hot, freshly cooked food
- Adrenal insufficiency
- Serum sodium
- Your body must absorb enough vitamin B12. A special protein, called intrinsic factor, helps your body do this. This protein is released by cells in the stomach.
- Failure to produce breast milk (in women)
- Swallowing difficulties
- From mother to child -- a pregnant woman can spread the virus to her fetus through their shared blood circulation, or a nursing mother can transmit it to her baby through her breast milk
- Sleep problems
- Fever
Purchase kamagra 50mg overnight delivery
One of the enterotoxins is structurally and functionally similar to cholera toxin erectile dysfunction in the military buy kamagra discount, and another acts on guanylyl cyclase. In severe cases, fluid and electrolyte loss can lead to extreme dehydration and even death. The organism is responsible for diarrheal illness in poor tropical areas, especially in infants and young children. Although it has virtually disappeared from developed countries, it still produces sporadic outbreaks of diarrhea, particularly among hospitalized infants younger than 2 years. The organism is not invasive and brings on disease by adhering to and deforming the microvilli of the intestinal epithelial cells. Bacteria adhere to colonic mucosa and elaborate an enterotoxin, virtually identical to Shigatoxin (see below), that destroys the epithelial cells. Most strains are intestinal commensals, well adapted to growth in the human colon without harming the host. An electron micrograph shows adherence of the bacteria to the intestinal mucosal cells and localized destruction of microvilli. As in shigellosis, the mucosa of the distal ileum and colon is acutely inflamed and focally eroded and is sometimes covered by an inflammatory pseudomembrane. Patients have abdominal pain, fever, tenesmus and bloody diarrhea, usually for about a week. Because the shorter female urethra provides a less effective mechanical barrier to infection, women are much more prone to urinary tract infections. Infections involving the bladder or urethra manifest as urinary urgency, burning on urination (dysuria) and leukocytes in the urine. If infection ascends to involve the kidney (pyelonephritis), patients develop acute flank pain, fever and elevated leukocyte counts. An infiltrate of neutrophils spills from the mucosa into the urine, and the blood vessels of the submucosa are dilated and congested. Chronic infections exhibit an inflammatory infiltrate of neutrophils and mononuclear cells. Chronic renal infection may lead to chronic pyelonephritis and renal failure (see Chapter 22). Chronically ill or severely stressed persons elaborate a salivary protease that degrades fibronectin, allowing gram-negative enteric bacteria to overcome the normal gram-positive flora and colonize the oropharynx. Inevitably, droplets of the resident oral flora are aspirated into the respiratory tract. Debilitated patients often have weak local defenses and cannot destroy these organisms. Decreased gag and cough reflexes, abnormal neutrophil chemotaxis, injured respiratory epithelium and foreign bodies, such as endotracheal tubes, all facilitate entry and survival of the aspirated organisms. The agents cause two important human diseases, namely, Salmonella enterocolitis and typhoid fever. Increased malaise, fever and labored breathing are often the first signs of pneumonia. Infection is typically acquired by eating food containing nontyphoidal Salmonella strains and is commonly called Salmonella food poisoning. Together with other enteric gram-negative rods that normally reside in the human colon, E. In healthy individuals, macrophages and circulating neutrophils phagocytose these bacteria. People with ruptured abdominal organs or acute pyelonephritis suffer gram-negative sepsis because the large numbers of organisms that gain access to the circulation overwhelm the normal defenses. If these foods are not cooked, pasteurized or irradiated, the bacteria persist and proliferate, particularly at warm temperatures. Although such dissemination is infrequent among adults, it is common among small children in daycare settings or within families. The nontyphoidal Salmonella species elaborate several toxins that injure intestinal cells. The mucosa of the ileum and colon is acutely inflamed and sometimes superficially ulcerated. Both colonize the vagina, and newborns acquire them on passage through the birth canal. It is postulated that the organisms spread to the bloodstream from the gastrointestinal tract and then seed the meninges. Typhoid Fever Typhoid fever is an acute systemic illness caused by infection with Salmonella typhi. Paratyphoid fever is a clinically similar but milder disease that results from infection with other species of Salmonella, including Salmonella paratyphi. The disease is spread primarily by ingestion of contaminated water and food, especially dairy products and shellfish. Infected food handlers with poor personal hygiene and urine from patients with typhoid pyelonephritis can be a significant source of spread. Typhoid fever accounts for over 25,000 annual deaths worldwide but is uncommon in the United States. Invasion tends to be most prominent in the ileum in areas overlying Peyer patches. The organisms are engulfed by macrophages, after which they block the respiratory burst of the phagocytes and multiply within these cells. Infected cells spread first to regional lymph nodes, then throughout the body via the lymphatics and bloodstream, affecting mononuclear macrophages in lymph nodes, bone marrow, liver and spleen. Fastigium: Fever and malaise increase over several days until the infected person is prostrate. Lysis: In patients destined to survive, fever and toxic symptoms gradually diminish. Gastrointestinal bleeding and intestinal perforation at sites of ulceration may occur in any stage but are most common during lysis, which commonly lasts a week. Convalescence: Fever abates and patients gradually recover over several weeks to months. Ten to 20% of untreated patients die, usually of secondary complications, such as pneumonia. In some cases, intestinal lymphoid hyperplasia progresses to capillary thrombosis, causing necrosis of overlying mucosa and the characteristic ulcers oriented along the long axis of the bowel. These ulcers frequently bleed and occasionally perforate, producing infectious peritonitis. Systemic dissemination of the organisms leads to focal granulomas in the liver, spleen and other organs, termed typhoid nodules. These are composed of aggregates of macrophages ("typhoid cells") containing ingested bacteria, erythrocytes and degenerated lymphocytes. Infection usually occurs through ingestion of fecally contaminated food or water but can be acquired by oral contact with any contaminated surface. As a result, endemic shigellosis is more common in areas with poor hygiene and sanitation. It is also spread in closed communities, such as hospitals, barracks and households. In the United States, about 300,000 cases occur annually, but the incidence of the disease is much higher in countries lacking sanitary systems for human waste disposal. Like other diarrheal illnesses, shigellosis is a significant cause of childhood mortality in developing countries.
Buy generic kamagra from india
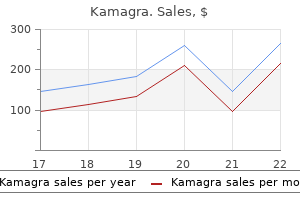
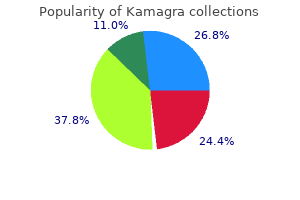
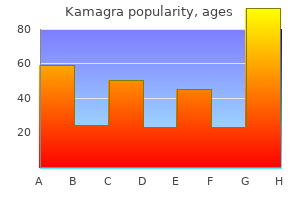
Diagnosis is commonly confirmed by ney stones includes administering pain medication and increasing fluid intake with the hope the stone will pass Copyright 2019 Cengage Learning erectile dysfunction and diabetes ppt generic 50 mg kamagra with amex. In the past, the most common individuals afflicted with kidney stones were middle aged males but now health care providers are seeing new cases, most commonly in teenagers, women, and African Americans. However, women over their lifetime have had a 45% increase in the chance of developing kidney stones. Future research might help explain this trend and give health care providers some guidelines for assisting patients to prevent kidney stone development. Urine is often strained through a filtering device in an effort to catch the stone for identification. Even though stones feel like they should be quite large to the individual passing them, the ones that are voided and filtered are usually quite small, ranging in size from a grain of salt to a small piece of rice. If the urinary tract is totally obstructed, emergency surgery must be performed to prevent hydronephrosis and kidney damage. Surgery called a stone basket procedure can be performed in which a retrieval instrument is passed through the urethra, bladder, and ureter to remove the stone. Another method is to break the stones into pieces for retrieval or in h opes that the pieces can be passed. This breaking of the stone is called lithotripsy (litho = stone, tripsy = breaking). Prevention of further stone devel- causative metabolic conditions, and increasing water intake. Polycystic disease is a slow, progressive disease that affects teenagers and young adults, usually leading to renal failure by age 30 or 40. As the disease progresses, kidney tissue is destroyed and function becomes increasingly paired. Renal failure is the failure of the kidneys to cleanse the blood of waste products. The primary method of cleansing the body of waste involves the formation of urea in the liver, which the kidneys filter out of the blood and excrete in urine. A high urea level in the blood is called uremia, meaning, literally, urine in the blood. Blockage of urine flow, caused by tumors, stones, or enlarged prostate, also can lead to acute failure. Reversal of acute renal failure, which involves treating the cause of the failure, is usually quite successful. Individuals in acute renal failure are placed on a limited diet to allow the kidneys to rest and regenerate function. Long-term substance abuse, alcoholism, and diabetes also can cause chronic renal failure. Symptoms can include those of acute failure and problems of infertility; impotence; and bone weakness, leading to pain and fractures. Dialysis is a procedure that cleanses the blood of waste products when the kidneys have failed or are failing to perform this function. There are two types of dialysis; both require the same components: the Copyright 2019 Cengage Learning. This machine is filled with semipermeable, cello phane-like material and dialyzing solution. As blood passes through the machine, the waste products diffuse through the membrane into the dialyzing solution to cleanse the blood. This procedure involves performing a paracentesis to instill dialyzing solution into the peritoneal cavity. This type of dialysis uses the membrane that lines the peritoneal cavity to act as the semipermeable membrane. The dialyzing solution is allowed to stay in the abdomen for varying amounts of time (dwell time), during which waste products diffuse out of the peritoneal capillaries and into the dialyzing solution. Peritoneal dialysis can be performed by several methods such as the following: Copyright 2019 Cengage Learning. Also, access to an artificial kidney machine might be limited to large metropolitan areas. Renal transplantation is a procedure to transplant a kidney of a donor into a recipient. This is a relatively simple surgical procedure performed on individuals with chronic renal failure commonly due to diabetes, hypertension, and glomerulonephritis. An identical twin provides the greatest probability of match, with a fraternal twin, sibling, parent, and biological child the next best matches, in that descending order. The greatest problems with renal transplant are obtaining a kidney that is histocompatible with the recipient and dealing with postoperative organ rejection and complications with lifelong administration of immunosuppressant medications. Controlling risk factors and conditions that cause kidney failure is the best preventive method. Because kidney disease is often caused by hypertension and diabetes, keeping these under control is important. Other preventive activities include not smoking, maintaining a healthy weight, eating healthy, and exercising regularly. If metastasis has occurred, chemotherapy and radiation also might be employed, but prognosis varies with the extent of spread. Cure might be possible if no metastasis has occurred, but with metastasis, prognosis is poor. Kidney cancer might not be preventable, but Adenocarcinoma of the Kidney Description. These tumors are more common in men than in women and usually affect men 55 years of age or older. The cause of this tumor is unknown, although cigarette smoking is considered to be a risk factor. Adenocarcinoma of the kidney frequently metastasizes to the liver, brain, and bone before symptoms appear. The most common initial symptom is controlling risk factors by living a healthy lifestyle, including not smoking, eating more fruits and vegetables, staying active, maintaining normal body weight, and controlling blood pressure, might be helpful in prevention. Later, as the tumor increases in size, the individual experiences flank pain and fever. As males age, the prostate is often enlarged, leading to urinary dribbling, the inability to control flow. Sleeping pills, antihistamines, muscle relaxants, and medications to control hypertension also might cause urinary incontinence. Often, the fear of urinary accidents drives affected individuals away from social activity and into a life of seclusion. Stress incontinence is the inability to hold urine when the bladder is stressed by coughing, sneezing, or laughing. Overflow incontinence is caused by the bladder not properly emptying and leaking when overfilled. Incontinence affects all areas of an indi- bladder every hour for 7 to 10 days, and then gradually increasing the length of time until one is toileting every three to four hours. Fluid restriction involves reducing the overall amount of fluids consumed during the day, not drinking any fluids around bedtime, and avoiding fluids containing alcohol and caffeine. Accessory muscle exercise employs frequently emptying the bladder and exercising the pelvic muscles and external sphincter to strengthen these structures. This exercise is performed by tightening or contracting the pelvic muscles as one would do to hold or stop urine flow. Medications may calm an overactive bladder, treat urge incontinence, relax the bladder neck, and improve tone in the urethra and vagina. Female stress incontinence can be improved with estrogen therapy because low estrogen levels weaken the urethral sphincter. Specialized urodynamic testing uses cystometry to measure anatomic and functional status of the bladder and urethra. Urinary disorders can be the result of urinary system pathology or of disease or malfunction of other body systems. Which diagnostic tests are most commonly used to determine the type and cause of urinary system disorders Match the disorders listed in the left column with the correct definition in the right column: Urethritis Pyuria Oliguria Anuria Nocturia Cystectomy Dysuria Nephrectomy Urinalysis Pyelonephritis Glomerulonephritis a.
Buy cheap kamagra on-line
Familial clustering suggests a genetic predisposition erectile dysfunction caused by performance anxiety kamagra 100 mg mastercard, although this is poorly understood. Syphilitic aneurysms are the common variety in the ascending aorta, which is usually spared by the atherosclerotic process. Berry aneurysms are seen in the circle of Willis, mainly at branch points; their rupture leads to subarachnoid hemorrhage. Mycotic aneurysms occur almost anywhere that bacteria can deposit on vessel walls. However, it is thought that the disease is actually multifactorial, involving inflammation and dysregulation of matrix remodeling and repair. They occur much more often in men than in women, and half of patients are hypertensive. Occasionally, aneurysms may be found in all parts of the thoracic aorta and in iliac and popliteal arteries. They may occur at almost any age but are most common in the sixth and seventh decades. Almost all patients have a history of hypertension, and associated conditions include atherosclerosis, bicuspid aortic valve and idiopathic aortic root dilation. Aneurysms that extend above the renal arteries may occlude the origin of the superior mesenteric artery and the celiac axis. Most abdominal aortic aneurysms are lined by raised, ulcerated and calcified (complicated) atherosclerotic lesions. The majority contain mural thrombi of varying degrees of organization, portions of which may embolize to peripheral arteries. Infrequently, a thrombus itself enlarges enough to compromise the lumen of the aorta. The adventitia is thickened and focally inflamed as a response to severe atherosclerosis. In some cases the condition is brought to medical attention by the onset of abdominal pain, which often reflects expansion of the aneurysm. Abrupt occlusion of a peripheral artery by an embolus from a mural thrombus presents as sudden ischemia of a lower limb. The most dreaded complication of aortic aneurysms is rupture and exsanguination into the retroperitoneum (or chest), in which case the patient presents with pain, shock and a pulsatile mass in the abdomen. This is an acute emergency, and half of patients die, even with prompt surgical intervention. Therefore, even asymptomatic large aneurysms are often replaced by or bypassed with prosthetic grafts. Aneurysms of Cerebral Arteries Cause Subarachnoid Hemorrhage the most common type of cerebral aneurysm is a saccular structure known as berry aneurysm, because it resembles a berry attached to a twig of the arterial tree. Berry aneurysms occur due to congenital defects in arterial walls and tend to arise at branches in the circle of Willis or one of the arterial junctions. The most common sites are between the anterior cerebral and anterior communicating arteries; the internal carotid and posterior communicating arteries; and the first main divisions of the middle cerebral artery and the bifurcation of the internal carotid artery. The changes were originally described as cystic medial necrosis (of Erdheim), because focal loss of elastic and muscle fibers in the media leads to "cystic" spaces filled with a metachromatic myxoid material. These spaces are not true cysts but are rather pools of matrix collected between the cells and tissues of the media. However, genetic studies have linked some cases to specific disorders, including Marfan, EhlersDanlos and Loeys-Dietz syndromes, and to filamin mutations. In Marfan syndrome, a systemic connective tissue abnormality, specific mutations in the gene encoding fibrillin (an extracellular matrix protein) have been identified (see Chapter 6). Aging also results in mild degenerative changes in the aorta, with focal elastin loss and medial fibrosis. Patients with dissection of the thoracic aorta show decreased expression of fibulin-5, an extracellular protein that regulates elastic fiber assembly. In animals, defective cross-linking of collagen induced by a copper-deficient diet (lysyl oxidase is a copper-dependent enzyme) causes dissecting aneurysm of the aorta. The same lesion is produced by feeding -aminopropionitrile, an inhibitor of lysyl oxidase. People with Wilson disease who are treated with penicillamine, a copper chelator, also may develop medial necrosis of the aorta. Taken together, these data suggest that the common factor in these several situations is a molecular defect that brings on weakness of aortic connective tissue. Dissecting Aneurysm Features Blood in the Arterial Wall the dissection occurs on a path along the length of the vessel. Although the lesion is usually designated an aneurysm, it is actually a form of hematoma. Dissecting aneurysms most often affect the aorta, especially the ascending portion, and its major branches. Thoracic dissections may involve the ascending aorta alone (type A) or only the distal aorta (type B). Over 95% of cases have a transverse tear in the intima and internal media, and it is widely held that spontaneous laceration of the intima allows blood from the lumen to enter and dissect the media. Alternatively, it has been proposed that hemorrhage from vasa vasorum into a media weakened by cystic medial necrosis initiates stress on the intima, which in turn leads to the ubiquitous intimal tear. Dissection in the media occurs within seconds and separates the inner 2/3 of the aorta from the outer third. It can also involve coronary arteries, great vessels of the neck and renal, mesenteric or iliac arteries. Atherosclerotic aorta with dissection along the outer third of the media (elastic stain). Inflammation of Aortic Vasa Vasorum Causes Syphilitic Aneurysms Syphilis was once the most common cause of aortic aneurysms, but as the infection has become less common, so has syphilitic vascular disease, including aortitis and aneurysms. Syphilitic aneurysms mainly affect the ascending aorta, which shows endarteritis and periarteritis of vasa vasorum. These vessels ramify in the adventitia and penetrate the outer and middle thirds of the aorta, where they become encircled by lymphocytes, plasma cells and macrophages. Obliterative changes in the vasa vasorum cause focal medial necrosis and scarring, and disruption and disorganization of elastic lamellae. The depressed medial scars create a roughened intimal surface, a "tree bark" appearance. Loss of one or more arterial pulses is common, as is a murmur of aortic regurgitation. Whereas hypertension is a frequent finding in patients with dissecting aneurysms, hypotension is an ominous sign and suggests aortic rupture. Before antihypertensive and surgical treatment became available, more than a third of patients with aortic dissection died within 24 hours, and 80% succumbed by 2 weeks. The thoracic aorta is dilated, and its inner surface shows the typical "tree bark" appearance. Other factors that raise venous pressure in the legs can cause varicose veins, including pelvic tumors, congestive heart failure and thrombotic obstruction of the main venous trunks of the thigh or pelvis. In the pathogenesis of varicose veins, it is not clear whether incompetence of the valves or dilation of the vessels comes first. Once the process begins, the varicosity extends progressively throughout the length of the affected vein. As each valve becomes incompetent, increasing strain is put on the vessel and valve below. The role of inflammation is not well studied, although elevated expression of leukocyte-endothelial adhesion molecules is reported in affected veins.
Buy 50 mg kamagra free shipping
End-diastolic volume may also increase erectile dysfunction treatment south florida buy kamagra 50mg otc, causing a large increase in cardiac output. If a heart is injured, overall cardiac function tends to be depressed in the basal state. Higher than normal filling pressures are then required to maintain cardiac output (curve Y in. Moreover, in cardiac failure, catecholamine stimulation is often present in the basal state. Comparable increases in cardiac output thus require greater increases in atrial pressure in failing hearts than in normal ones. The most prominent feature of heart failure is abnormally high atrial filling pressure relative to stroke volume. However, the absolute values of stroke volume and cardiac output are generally well maintained. However, the downslope of this curve is reached only at very high left atrial pressures. The curve may shift upward to position X or downward to position Y, depending on whether contractility has increased. There is a distinction between physiologic hypertrophy, which develops in highly trained athletes, and pathologic hypertrophy, which occurs because of injury or disease. These disparities are not well understood but may reflect the fact that the demands of exercise are intermittent, while those of disease. Events mediated by -adrenergic receptors are implicated in the transition from compensatory hypertrophy to heart failure. Ligands, signaling cascades, downstream targets and mechanisms mediating the hypertrophic response are described below (see also Chapter 1). It also develops as a response to primary injury of cardiac myocytes as in cardiomyopathies (see below). Until recently, this had been thought to occur without an increase in the number of cardiac myocytes, but it is now known that cardiac progenitor cells exist with at least the potential to contribute to hyperplastic growth (see below). Hypertrophy at first entails compensatory and possibly reversible mechanisms, but with persistent stress, the myocardium becomes irreversibly enlarged and dilated. Contractile cells respond to mechanical stimuli, such as stretching or pressure overload, by releasing ligands that activate receptormediated signaling pathways to produce hypertrophy. Interstitial fibrosis, which occurs in virtually all forms of heart failure, is an obligatory feature of the hypertrophic response. After myocardial infarction, fibrosis is important in replacing necrotic myocytes and preventing cardiac rupture. It can also lead to remodeling of electrical conduction pathways, and so is a major factor in the pathogenesis of atrial fibrillation and ventricular tachycardia. This isoform helps mediate physiologic hypertrophy in response to exercise training, promotes cell survival, inhibits cardiac fibrosis and attenuates pathologic hypertrophy. Desensitization of -adrenergic receptors contributes to sluggish responses of a failing heart to exercise. Chronic overstimulation leads to decreased numbers and responsiveness of -adrenergic receptors and a defect in coupling to adenylyl cyclase. Although 1-adrenergic receptors are desensitized in heart failure, treatment to block this receptor class reduces mortality and improves contractile function in patients with advanced heart failure. Expression and function of key Ca2+-regulating proteins in cardiac myocytes are altered. As a result, impaired Ca2+ sequestration in diastole leads to impaired relaxation. Transcription of proto-oncogenes helps to reexpress fetal protein isoforms in the hypertrophic heart. In cardiac hypertrophy induced by hemodynamic overload, many of these genes are reexpressed. Cardiac hypertrophy also elicits reexpression of fetal isoforms of several contractile proteins. In experimental cardiac hypertrophy, "fast" -myosin is replaced by "slow" -myosin, leading to impaired myocardial contractility. However, this change in myosin gene expression is also adaptive, as it increases the tension generated during systole and improves contraction efficiency, thus conserving energy. Hypertrophied hearts exhibit similar, but not identical, changes in myosin isoforms. Ventricles contain only slow myosin, and hypertrophic hearts change from fast to slow myosin only in the atrium. Current research focuses on strategies to exploit this capacity in order to replace damaged or necrotic muscle. After birth, however, the heart downregulates glycolytic enzymes and increases expression of genes that encode proteins mediating -oxidation of fatty acids derived from breast milk. The failing heart reverts to using glucose by reexpressing fetal patterns of genes for energy generation. Recent advances in understanding the molecular pathogenesis of heart failure have identified a role for histone acetylases and deacetylases in stress-activated myocyte signaling pathways. This switch entails changes in subcellular localization and activities of histone acetylases and deacetylases, suggesting that manipulation of histone-modifying enzymes may be useful in preventing heart failure. Apoptosis of cardiac myocytes increases 5-fold in animal models of heart disease, and senescent rats have 30% fewer cardiac myocytes than do young ones. Pathologic hypertrophy is generally associated with greater cardiac myocyte apoptosis, which may help transition from compensated hypertrophy to heart failure. Thus, diverse signaling pathways in cardiac hypertrophy may exert both proapoptotic and antiapoptotic influences, the final outcome depending on the balance between them. These increase in number with age or in disease, indicating a capacity for nuclear division. However, it is clear that cardiac stem cells exist in adults and that during a lifetime, the heart continuously replaces myocytes, endothelial cells and fibroblasts at a slow rate (see Chapter 1). Ischemic heart disease is by far the most common cause of cardiac failure, accounting for more than 80% of deaths from heart disease. Most of the rest are caused by nonischemic heart muscle disease (cardiomyopathies) and congenital heart diseases. Ventricular hypertrophy is seen in virtually all conditions associated with chronic heart failure. Initially, only the left ventricle may be hypertrophied, as in compensated hypertensive heart disease. But when the left ventricle fails, some right ventricular hypertrophy usually follows, as the increased workload is imposed on the right ventricle by the failing left ventricle. In most cases of clinically apparent systolic heart failure, the ventricles are conspicuously dilated. The distribution of endorgan involvement depends on whether the heart failure is predominantly left sided or right sided. Left-sided heart failure is more common, as the most common causes of cardiac injury. To compensate for left ventricular failure, left atrial and pulmonary venous pressures rise, resulting in passive pulmonary congestion. Alveolar septal capillaries fill with blood and small ruptures allow erythrocytes to escape. As a result, alveoli contain many hemosiderin-laden macrophages (so-called heart failure cells). If capillary hydrostatic pressure exceeds plasma osmotic pressure, fluid leaks from capillaries into alveoli. Resultant pulmonary edema (see Chapters 16 and 18) may be massive, with alveoli being "drowned" in a transudate. Interstitial pulmonary fibrosis results when congestion is present over an extended period. Right-sided heart failure most commonly complicates left-sided failure, but it can develop independently due to intrinsic lung disease or pulmonary hypertension.