Quality roxithromycin 150 mg
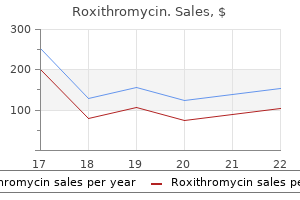
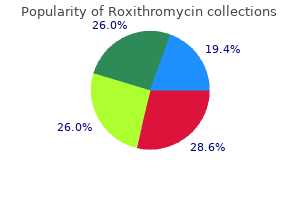
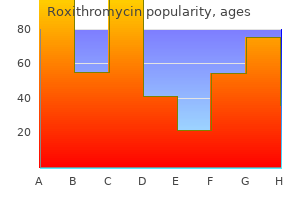
For example antimicrobial needleless connectors roxithromycin 150 mg online, the addition of valpromide, a valproic acid derivative, to the regimen of patients stabilized on carbamazepine causes a marked increase in the serum concentration of the active metabolite carbamazepine-10,11-epoxide, leading to the development of adverse effects [11]. As the serum concentration of the parent drug is not affected by this interaction, monitoring serum carbamazepine concentration provides no clue to the mechanism underlying the adverse effects. Interestingly, in the case of valproic acid, a delay in the onset of suppression of the photoconvulsive response does not necessarily imply a delay in blocking other types of seizure activity, as demonstrated by the relatively rapid onset of effect in some patients with status epilepticus treated with valproic acid (see Chapter 17). The latter observation may be explained by more rapid brain penetration after intravenous dosing, or by a different mechanism underlying drug response in different clinical situations. Note that complete suppression of the photoconvulsive response is delayed with respect to the increase in serum valproic acid levels, and occurs well after the peak in serum valproic acid concentration. In fact, these ranges are simply representative of the serum concentrations at which most patients respond. For the reasons stated in the previous section, there may be a large variation in the degree of response at any given serum drug concentration, and many patients achieve control at concentrations that are below or above the reference ranges quoted in the literature. For example, a drug concentration below the reference range in an individual with uncontrolled seizures and no side-effects will give the clinician greater confidence in increasing dosage, and may help in deciding the magnitude of the dosage increment. Conversely, lower concentrations may be targeted whenever tolerability concerns outweigh concerns of seizure recurrence. More examples of the use of therapeutic drug monitoring in clinical management are given in the section `When should drug concentrations be measured In fact, achieving a desired drug concentration is no 128 Chapter 10 guarantee that an optimal response will be obtained, and many subjects experience therapeutic or toxic effects at concentrations higher or lower than expected. In fact, in clinical practice it is often possible, and even desirable, to establish empirically the serum concentration at which an individual patient exhibits the best response [1,14]. In other words, once dosage has been adjusted on the basis of clinical response and an optimal effect has been achieved, the concentration associated with such an outcome can be measured and considered as an estimate of the therapeutic concentration in that individual. Depending on the characteristics of the individual, an optimal response may be either sustained seizure freedom, or the best compromise between reduction in seizure frequency and adverse effects. The therapeutic concentration in an individual, once established, provides useful information for subsequent management. For example, if a few years later the same individual experiences a seizure breakthrough, a second measurement of the serum drug concentration may provide clues as to the possible causes [15]. In particular, if at the time of the seizure breakthrough the drug concentration is found to be lower than the previously established therapeutic concentration, there is a strong indication that the relapse was caused, depending on clinical context, by either a change in compliance or a change in drug disposition under the influence of physiological factors, disease states or drug interactions [1]. Knowledge of the serum concentration at which that individual had responded in the past will also aid in deciding what dosage adjustments will be needed if the seizure breakthrough was caused by altered drug disposition. Whenever a patient is exposed to conditions known or suspected to alter serum drug concentrations, information on the therapeutic concentration in that individual may be used to prevent recurrence of seizures or drug toxicity. For example, oral contraceptives are known to cause a marked but variable decrease in serum lamotrigine concentration [16]. If the individual therapeutic concentration of lamotrigine is known in a woman with well-controlled epilepsy who is starting an oral contraceptive, serial drug concentration monitoring will enable rapid detection of contraceptive-induced changes in lamotrigine concentration (or the lack of significant changes if the lamotrigine dose was increased pre-emptively by an appropriate degree), and appropriate dosage adjustments can then be made to restore the therapeutic concentration of the drug and thereby prevent possible seizure recurrence. Another example of the application of the therapeutic concentration concept can be found in a recent study on the consequences of a fall in serum lamotrigine concentrations during pregnancy [17]. To ensure optimum accuracy in establishing therapeutic concentrations, sampling time must be standardized carefully, and at least two determinations should be obtained on different dates, in order to assess the variability of the estimate. This may occur as a result of alterations in the pathophysiology of the seizure disorder (particularly during the period of brain maturation), pharmacodynamic interactions with concomitant medications, or changes in drug binding to serum proteins resulting from disease or displacement by interacting drugs [1,14]. Main indications for measuring serum antiepileptic drug concentrations the practice of monitoring serum drug concentrations, introduced in the 1960s, has had a major role in improving the quality of epilepsy care. It should be noted, however, that few patients in that trial were treated with phenytoin, the drug for which measurement of serum concentrations is particularly useful. To start with, if the concept of individualized therapeutic drug concentrations is accepted, a case can be made for determining serum drug concentrations in every individual after reaching steady state on the initial target maintenance, and after any appropriate dose increases if dosage increments were necessary (Table 10. Knowledge of the concentrations that have proved ineffective, and of the concentration that ultimately was associated with an optimal response in that individual (therapeutic concentration) can be very useful for subsequent management, particularly should the patient at a later date show an unexpected change in clinical response or be exposed to conditions causing pharmacokinetic changes. Poor adherence is a common reason for inadequate clinical response in people with epilepsy. Adherence has been reported to be low in 40% of patients with epilepsy [19] and 33% in children with epilepsy [20]. Compliance problems are suggested by unusually low and variable concentrations, which increase following supervision of drug intake. Therefore, children require on average higher doses in milligrams per kilogram body weight to achieve the same drug concentration as adults. Pharmacokinetic variability can be particularly large in paediatric age, and measuring drug concentrations may be useful for optimal management [1,23]. The most pronounced decrease in serum concentrations during pregnancy have been observed for lamotrigine, levetiracetam, the active monohydroxyderivative of oxcarbazepine, and topiramate. Overall, the main situations in which measuring serum drug concentrations are indicated in clinical practice can be summarized as follows (Table 10. In this situation, assessment of the drug concentration will be useful in identifying potential sources of poor response, such as low drug concentrations resulting from unusual pharmacokinetic patterns or poor compliance. In addition to paediatric age, pregnancy, and old age, such conditions include diseases affecting the liver, the kidney and the gastrointestinal tract. If applicable, knowledge of a pre-established individual therapeutic concentration is of particular value in the management of these patients. However, it should be noted that, in some of these conditions, drug binding to serum proteins and pharmacodynamic sensitivity to the drug may also be altered, and this should be taken into account when interpreting concentration data. For example, if an emergent condition resulted in an increased unbound fraction of the drug, therapeutic and toxic effects will be expected to occur at comparatively lower total drug concentrations. When seizure control is unsatisfactory or toxic signs develop in patients on polytherapy, measuring the concentration of individual drugs (or their active metabolites. These determinations should be requested only when there is a sound indication, and dosage adjustments should be made only when there is a clinical need, irrespective of the drug concentration in the blood. Physicians must always remember that the primary aim of therapy is to treat a patient and not a laboratory value. Note not only the non-linear relationship but also the wide variability across patients. For drugs with a long half-life, such as phenobarbital, the daily fluctuation in plasma concentration is negligible and the exact time of sampling is not important. With other compounds, it is preferable to collect the sample in the morning before the first daily dose, when the concentration is usually at its trough. For drugs exhibiting significant variation in serum concentration during the dosing interval, such as carbamazepine, it is at times useful to obtain a second sample at the time of the expected peak concentration, in order to estimate the degree of fluctuation as a potential cause of intermittent adverse effects. Monitoring unbound drug concentrations Although routine analytical methods measure the total concentration of the drug in serum, it is only the free non-protein-bound fraction that is available to equilibrate with receptor sites and to produce pharmacological effects. When the unbound fraction is increased, the total concentration in serum may underestimate the amount of drug that is pharmacologically active, and this should be taken into account when interpreting the serum concentration of highly protein-bound drugs such as phenytoin and valproic acid [1]. An increased unbound fraction of these drugs is observed in conditions associated with hypoalbuminaemia. An increase in unbound fraction may also be caused by drug interactions: valproic acid, for example, increases the unbound fraction of phenytoin by displacing phenytoin from protein binding sites. In all these conditions, therapeutic and toxic effects may be observed at total drug concentrations lower than usual, and failure to recognize this may mislead the clinician into making inappropriate dosage adjustments. The suggestion has been made that in the presence of altered binding to plasma proteins it would be preferable to monitor directly the unbound drug concentration. In practice, however, this is not always necessary because often the increase in unbound fraction may be predicted on the basis of other parameters such as plasma albumin or, in uraemic patients, plasma creatinine concentration. In addition, unbound plasma drug concentrations are much smaller than total concentrations and not always easy to measure. Results may vary depending on the assay technique, and there is a greater possibility of analytical error than with measurements of total drug concentrations.
Syndromes
- Breathing help (respiratory support)
- Brain damage
- Have a close family member who has had depression or anxiety
- Feeling hopeless or helpless
- Quinidine
- Broadening of the thumbs and big toes
- Skin irritation
- Come in close contact with a person who has lice
- Thirst
Purchase generic roxithromycin online
Cutting at this level is easy (no preventive clamping is needed) and leads directly to the dorsal aspect of the paraisthmic window antibiotic resistant staphylococcus aureus purchase cheapest roxithromycin and roxithromycin, the ventral aspect of which has been identified previously. The vagina is closed with interrupted sutures after careful evaluation of intraperitoneal hemostasis. Since hemostasis can be difficult to assess vaginally, we go back laparoscopically for inspection of the dissected areas, to complete hemostasis, and to make sure of the integrity of the bladder and the ureters. The same is for constipation, which can be the consequence of neurogenic rectal atony and pre-existing anal problems. Total laparoscopic or robotic-assisted radical hysterectomy might become a better surgical choice. In our own series (unpublished data), the actuarial disease-free 5-year survival was 94. In our own experience (unpublished data), the disease-free 5-year survival was 100% for the 144 patients with tumors less than 2 cm in size versus 87. If not, the frozen sections done on the sentinel nodes retrieved laparoscopically give the answer. Our data seem to demonstrate that the parametrial lymphadenectomy performed during the laparoscopic part of the surgery significantly lowers the risk of recurrences. If the injury concerns the ureter(s) or the bladder floor close to the ureteric orifices, stents should be used. Postoperative complications are similar to those that can occur after all extended pelvic surgery. Bleeding is the first complication, but usually less than with the abdominal approach (Roy and Plante 2011). The incidence of bleeding is lowered by laparoscopic re-evaluation of the abdomen after the vagina is closed. Postoperative pelvic collections of various natures can be observed as a consequence of occult bleeding during the first postoperative days or as a consequence of accumulation of lymphatic fluid in the successive weeks. Fistulas are generally the consequence of undiagnosed injuries, and symptoms appear in the first hours following the surgery. Nevertheless, it is mandatory to investigate by an intravenous pyelogram if injury is suspected. The urinary bladder voiding difficulties observed in the immediate postoperative period can persist at least in the form of loss of the feeling of the need to urinate and a prolonged time to void. The minimally invasive surgery, at first sight, seems to be more "patient friendly," but classical surgery has changed a lot since the new tool appeared and has been developed further: new incisions, new instruments (Ligasure, Biclamp, Ultracision), new wound closure techniques, and new analgesic strategies make the postoperative course much less painful than it was in the past. With more recent use of laparoscopy or robotics in cervical cancer surgery, the future might be "vaginal assisted laparoscopic radical hysterectomy" (Koehler et al. Recurrence in a Schuchardt incision after Schauta-Amreich operation for cervical cancer. Metastasis on a Schuchardt incision after Schauta-Amreich operation for cervical carcinoma. Treatment of the cancers of the ecto-cervix and vagina with preservation of the uterus and adnexae. From laparoscopic assisted radical vaginal hysterectomy to vaginal assisted laparoscopic radical hysterectomy. Laparoscopically assisted radical vaginal hysterectomy versus radical abdominal hysterectomy for the treatment of early cervical cancer. Extraperitoneal lymphadenectomy and radical vaginal hysterectomy for cancer of the cervix (Mitra technique). Laparoscopic radical hysterectomy for invasive cervical cancer: 8-year experience of a pilot study. Modified radical vaginal hysterectomy with or without laparoscopic nerve-sparing dissection: A comparative study. Vaginal radical hysterectomy versus abdominal radical hysterectomy in the treatment of early-stage cervical cancer. Radical vaginal hysterectomy with extraperitoneal pelvic lymphadenectomy in cervical cancer. Laparoscopy-assisted radical vaginal hysterectomy modified according to Schauta-Stoeckel. At the level of the upper endocervix, these two arteries form a network of anastomosis and a rich vascular plexus. At the isthmus, the uterine artery also forms a loop, often referred to as the cross of the uterine artery. This is an important landmark because all efforts should be made to preserve the uterine artery in order to assure a good vascular supply to the uterine body, particularly in the event of a pregnancy. However, bilateral uterine artery ligation is not a contraindication to continuing the trachelectomy, and pregnancies should be allowed to proceed normally; the uterine body usually maintains good vascularization through the utero-ovarian vascular supply. Uterovaginal Endopelvic Fascia the endopelvic fascia refers to the reflections of the superior fascia of the pelvic diaphragm upon the pelvic viscera. This thin layer thus encases respectively the urethra and bladder (urethrovesical fascia), the vagina and lower uterus (uterovaginal fascia), and the rectum (rectal fascia). The uterovaginal endopelvic fascia is of particular importance as it lies in close proximity to the pelvic peritoneum. Cardinal (Mackenrodt) Ligament the cardinal ligament is composed of condensed fibrous tissue and some smooth muscle fibers. This fibrous sheath contains the ureter, the uterine vessels and associated nerves, the lymphatic channels and lymph nodes draining the cervix, and some fatty tissue. The cardinal ligament is in continuity anteriorly to the uterovaginal endopelvic fascia, and posteriorly, fibers are integrated with the uterosacral ligament. Uterosacral Ligaments these ligaments are true ligaments of musculofascial consistency that run from the upper part of the cervix to the sides of the sacrum. So, in terms of quality of life, fertility preservation has become a major issue in the management of young women with early-stage cervical cancer (Plante 2000). It is now recognized as a valuable conservative fertility-preserving surgical procedure for the treatment of selected cases of early-stage cervical cancer. This procedure has the advantage of preserving the uterine body, which in turn allows preservation of childbearing potential. This surgery has been described and first published by Professor Daniel Dargent from Lyon, France (Dargent et al. Data have been reported from nearly 1000 women who have undergone this procedure worldwide (Plante 2013). More than 450 pregnancies have been reported and more than 300 healthy babies have been born so far. The majority of patients have delivered by elective caesarean section and approximately two-thirds were at term. The main obstetrical problem is the risk of premature second trimester birth or miscarriage. Oncologic results are also reassuring, as the risk of recurrences remains less than 5% (Plante 2013). Desire to preserve fertility No clinical evidence of impaired fertility Lesion size less than 2. When a radical hysterectomy is performed abdominally, the uterus is pulled upward, bringing with it the parametrium and the uterine vessels, while the bladder base is mobilized downward. Therefore the uterine vessels lie above the concavity of the ureters as the ureters run into the parametrial tunnel to enter the bladder base. When the radical hysterectomy is performed vaginally, the relationship between the structures is completely the opposite. The uterus is pulled downward and the bladder base along with the ureter is mobilized upward. Vaginal Cuff Preparation A rim of vaginal mucosa is delineated circumferentially clockwise using 8 to 10 straight Kocher clamps placed at regular interval.
Cheap roxithromycin 150mg free shipping
A foreign body may be difficult to find virus 24 buy roxithromycin pills in toronto, as may a corneal ulcer, and referral to an ophthalmologist would be in order. In addition, there may be lid problems, particularly in the elderly, and these may constitute ectropion or entropion. If the eye examination is normal, one must consider the possibility of obstruction of the nasolacrimal duct because of trauma, congenital causes, a calculus, neoplasm, or dacryocystitis. Crocodile tears may occur when, because of aberrant nerve regeneration following facial paralysis, the lacrimal gland is stimulated to produce excessive tears while eating. If the eye examination is abnormal or there are problems with the lids, referral to an ophthalmologist is in order. Even if the eye examination is normal, referral to an ophthalmologist would be necessary to determine if obstruction of the nasolacrimal duct is the problem. The patient with hypertension could have either essential or symptomatic hypertension. Be sure to recheck the blood pressure, as other health professionals may miss the auscultatory gap. Next, treat the hypertension and examine the patient for symptomatic hypertension later (page 268). However, when the bleeding is from the posterior nasal areas, one must always consider the possibility of carcinoma. There may be bleeding sites elsewhere to indicate that there is a systemic disorder associated with the epistaxis. If these tests suggest a coagulation disorder, referral to a hematologist can be done for further diagnostic workup. A nasal smear should be done for eosinophils to determine if the patient has chronic allergic rhinitis. When a carcinoma of the nasal pharynx or sinuses is suspected, x-ray of the paranasal sinuses can be done as well as nasopharyngoscopy. Other drugs that are prescribed by physicians may cause euphoria, such as corticosteroids and various narcotics. The patient may demonstrate simple disorientation or disturbance in the thought process or excessive jocularity, as may be seen in Witzelsucht. All these findings may suggest a frontal lobe tumor, a general paresis, or other forms of dementia. When there are long tract signs, such as posterior column or pyramidal tract involvement, one must consider the possibility of multiple sclerosis or a pontine glioma. If the euphoria is intermittent and very brief, one should consider temporal lobe epilepsy. If these tests are negative and the problem persists, the patient should be referred to a psychiatrist. A pulsating eyeball would suggest an arteriovenous fistula, and there should be a loud blowing murmur over the orbit. Fever would suggest acute cellulitis, acute sinusitis, periostitis, or a cavernous sinus thrombosis. Testing for thyrotropin receptor antibody and peroxidase antibodies should be done in these cases. Acute onset would suggest arterial embolism, deep vein thrombophlebitis, and cellulitis. If there is a history of trauma, it would suggest a fracture, sprain, or torn ligament. This is a very important examination, as one would not want to miss a deep vein thrombophlebitis. This would suggest cellulitis, superficial thrombophlebitis, osteomyelitis, lymphangitis, and other types of infections. Tenderness without significant swelling or erythema would be suggestive of bursitis or deep vein thrombophlebitis. If there is clear-cut joint pathology, an x-ray of the joints, arthritis profile, and synovial fluid analysis will usually provide a diagnosis. If a deep vein thrombophlebitis is suspected, venous Doppler ultrasound, impedance plethysmography, or a contrast venogram may be done. Order a phospholipid antibody titer in patients with frequent episodes of thrombophlebitis. In cases of chronic peripheral arteriosclerosis, the ankle-brachial index and arterial Doppler ultrasonography are studies to be ordered first. If a herniated disk or other pathology of the lumbar spine is suspected, plain films of the lumbar spine should be obtained. If these tests are unrevealing, it is wise to refer the patient to a neurologic specialist before more expensive tests are ordered. Bone scans will help diagnose obscure fractures and osteomyelitis, both of the lumbar spine and of the lower extremities. Limitation of motion of a joint would suggest not only various types of arthritis, fracture, or torn ligaments, but also inflammation of surrounding structures such as the bursa or tendons. For example, limitation of motion of the shoulder would suggest impingement syndrome, frozen shoulder, rheumatoid arthritis or osteoarthritis, subacromial bursitis, and a torn rotator cuff. If the limitation of motion is only active, one should suspect tendinitis or bursitis. If the limitation of motion is both active and passive, one should suspect the various forms of arthritis, as well as bone tumors, osteomyelitis, and adhesive capsulitis. Weakness and especially paresthesia suggest a neurologic origin for the pain, and one should be considering brachial plexus neuritis, carpal tunnel syndrome, ulnar entrapment, and radiculopathy. Trophic changes along with vasomotor changes would also suggest a peripheral neuropathy. Diffuse hypoactive reflexes with stocking deficits in the lower extremities would suggest a peripheral neuropathy, whereas hyperactive reflexes in the lower extremities would suggest a cervical cord tumor, cervical spondylosis, or multiple sclerosis. This is an expensive test, but when there are obvious signs of radiculopathy, it is worthwhile. Perhaps dermatomal somatosensory studies should be done when there is confusion about whether a herniated disk is pathologic. When there is intermittent pain, an exercise tolerance test should be done to exclude coronary insufficiency. A stellate ganglion block may be helpful in diagnosing reflex sympathetic dystrophy. Remember that other nerve blocks may be done and one should not hesitate to call an anesthesiologist for help in this area. Various forms of bursitis may be diagnosed by a therapeutic trial of lidocaine and corticosteroid injections. Besides conjunctivitis and scleritis, be sure to look for closed angle glaucoma (dilated pupil) which is associated with nausea and vomiting and is a medical emergency. Without redness, one should suspect disease in the adjacent structures or retrobulbar neuritis. However, contact lens wearers may present with eye pain without redness, but there will be white spots on the cornea. In cases without redness of the eye, is there any abnormality on examination both with the naked eye and with the ophthalmoscope A dilated pupil would certainly suggest glaucoma; ophthalmoscopic examination may show optic neuritis or retinal detachment. A visual field examination may detect optic neuritis, retrobulbar neuritis, and retinal artery occlusion. The primary care specialist may also use fluorescein dye to diagnose a foreign body. Most primary care physicians feel competent to use tonometry to diagnose glaucoma and may feel competent to use a slit lamp. If all tests are negative, a trial of sumatriptan orally or by nasal spray may help diagnose migraine or histamine headaches. However, when there is any doubt about the diagnosis, the most cost-effective approach is to refer the patient to an 236 ophthalmologist. Intermittent pain would suggest trigeminal neuralgia, cluster headaches, or atypical migraine.
Order roxithromycin paypal
Polyuria that is either significant or massive would suggest diabetes insipidus antibiotic vitamins purchase cheap roxithromycin on line, diabetes mellitus, or thyrotoxicosis. Mild or insignificant polyuria may be because of hypercalcemia, hyperparathyroidism, and excessive salt intake. Thrombocytopenia with a normal white count suggests idiopathic thrombocytopenic purpura or drug reaction. Thrombocytopenia with a low white count suggests lupus erythematosus, aplastic anemia, myelofibrosis, drugs, myelophthisic anemia, or pernicious anemia. The most important study is a thyroid technetium-99m or iodine-123 uptake and scan. If the results of these are abnormal, then an endocrinologist or general surgeon should be consulted to assist in the interpretation. If the scan indicates a cold nodule, ultrasonography may be done to determine whether the nodule is cystic or solid. If there are malignant cells or at least suspicious cells for malignancy, surgery should be done. If the scan reveals a hot nodule and there is clinical and laboratory evidence of thyrotoxicosis, the patient should be treated with radioactive iodine or surgery. If the scan shows diffuse uptake of radioactive materials and there is clinical thyrotoxicosis, the patient also may be treated with radioactive iodine or surgery. Objective tinnitus is unusual, but it may indicate glomus tumors, arteriovenous malformations, carotid stenosis, aneurysms, anemia, a patent Eustachian tube, or myoclonus. Objective tinnitus means that both the patient and the examiner can hear the noises. A history of trauma would suggest that the tinnitus is because of whiplash, concussion, or trauma to the middle or inner ear. Drugs that may cause tinnitus include aminoglycosides, tetracyclines, clindamycin, caffeine, and the tricyclic antidepressants. Abnormalities on the ear examination include cerumen, otitis externa, otitis media, mastoiditis, and cholesteatomas. The presence of other neurologic signs along with vertigo and deafness would suggest multiple sclerosis, advanced acoustic neuroma, basilar artery occlusion or insufficiency, brainstem tumors, and central nervous system syphilis. A spinal tap may be helpful in diagnosing multiple sclerosis and central nervous system syphilis. Focal masses, include trauma, herpes simplex, pemphigus, erythema bullosum, carcinoma, angioma, fibroma, lipoma, mucus cyst, papilloma, or syphilitic gumma. If a vitamin deficiency is suspected, a therapeutic trial of vitamins is indicated. There is usually a focal or diffuse inflammation of the tongue or an ulcerating lesion. Diffuse inflammation is found in antibiotic glossitis, glossitis of avitaminosis (pernicious anemia), aphthous stomatitis, thrush, streptococcal glossitis, and acute diffuse glossitis. Focal lesions include cuts and ulcerations from trauma, such as the bitten tongue or burned tongue (hot pizza, etc. Other painful focal lesions are carcinoma, tuberculosis, syphilis (often painless), and herpes simplex ulcers. When the tongue is completely normal, trigeminal neuralgia, polymyositis, trichinosis, and calculus of the submaxillary gland should be considered. Focal lesions that persist should command a referral to a dentist or oral surgeon. The chancre of primary syphilis rarely causes severe pain, so this will often distinguish the lesion from the others. To differentiate the other causes, a smear and culture and, ultimately, a biopsy must be done. Most physicians will find referral to a dentist or oral surgeon is the best course of action when the ulcer persists. Multiple cavities are found in diabetes mellitus, pernicious anemia, and multiparous women. Separation of the teeth may be a clue to hypopituitarism, whereas teeth that taper to a thin edge are typical of the screwdriver appearance of Hutchinson teeth in congenital syphilis. Who has not heard of the dramatic gum hypertrophy associated with phenytoin use in epileptic children In scurvy, the gums become swollen, and the teeth get loose, drop out, or become misaligned. In dental ectodermal dysplasia, the teeth may be partially or completely absent, and, at times, there is no evidence of enamel formation. The dark blue line positioned where the gums meet the teeth is a sign of lead intoxication. Mothers frequently complain that their children grind their teeth, but this is rarely of pathologic significance. Of course, it may be a sign of malocclusion and temporomandibular joint syndrome, especially in adults. Yellow teeth is a sign that a child has been affected by tetracyclines either in utero or early childhood. This would make a subclavian steal syndrome likely causing vertebralbasilar artery insufficiency. If not, remember an atrial myxoma, migraine, epilepsy, and subacute bacterial endocarditis are real possibilities in a transient ischemic attack. Carotid duplex scans, echocardiography, and Holter monitoring would be wise if the above studies are not revealing. Ambulatory blood pressure monitoring may be useful in patients suspected of having paroxysmal hypertension or postural hypotension. Following the algorithm, you ask about weight loss, palpitations, and sweating, and she has none of these symptoms. On your examination, there is no tremor at rest and the tremor is most pronounced on finger to nose testing bilaterally. There are no other neurologic signs, so you rule out multiple sclerosis, hereditary, and neoplastic diseases of the cerebellum. On further questioning, you find that her mother has a similar condition, so you suspect familial or essential tremor. A fine tremor of the outstretched hands, which is sometimes described as tension tremor, would suggest hyperthyroidism. If the patient has tachycardia and an enlarged thyroid, one should consider hyperthyroidism. However, simply tachycardia alone might indicate that the patient is very sensitive to caffeine. Most patients presenting with a mild intention tremor that is symmetrical and not associated with other neurologic findings will probably have familial or senile tremor, and the response to beta-blockers can be determined. In strychnine poisoning, it is a late development, as the twitchings and convulsions are well established before it appears. Trismus may be simulated by impacted wisdom teeth, temporomandibular joint syndrome, scleroderma, and malingering or hysteria. If this ratio is 10:1 or less, one should look for renal diseases or obstructive uropathy. These findings point to obstructive uropathy, particularly bladder neck obstruction. When the smear and culture are negative for gonorrhea, a course of tetracycline can be given as a therapeutic trial to diagnose Chlamydia infection. Other etiologies for nongonococcal urethritis are Ureaplasma genitalium and Trichomonas vaginalis. Alert the laboratory, in advance, if these organisms are suspected because they may require special culture media for isolation. A prostate examination should always be done in males, as acute and chronic prostatitis are common causes of urethral discharge. In teenagers, a urethral discharge may develop from prolonged abstinence or excessive masturbation. Rarer causes of urethral discharge are syphilis, tuberculosis, foreign body, and herpes. Brown urine is usually because of hepatitis or obstructive jaundice, but myoglobin and melanuria may also color the urine brown.
Cheap roxithromycin 150 mg free shipping
In patients with poor or unknown functional capacity antibiotics lactose intolerance buy roxithromycin online from canada, the number of active clinical risk factors should guide the need for further testing. Step 5: Supplemental Preoperative Evaluation Supplemental testing allows the clinician to obtain prognostic information, further guiding therapy and perioperative management. There are no randomized controlled trials to support routine coronary revascularization prior to noncardiac surgery exclusively to reduce perioperative cardiac events (McFalls et al. In situations where noncardiac surgery is necessary, a consensus decision regarding the relative risks of surgery and antiplatelet therapy can be helpful. Perioperative cardiac risk is directly linked to the extent of jeopardized viable myocardium identified by stress cardiac imaging (Beattie et al. Cardiopulmonary exercise perioperative medical management Several randomized control trials have suggested perioperative beta-blockade reduces cardiac events in high-risk patients during noncardiac procedures. If an emergency, then determine the clinical risk factors that may influence perioperative management and proceed to surgery with appropriate monitoring and management strategies based on the clinical assessment (see Section 2. In those patients with unknown functional capacity, exercise stress testing may be reasonable to perform. Initiating perioperative beta-blockade in patients at intermediate or high risk for myocardial ischemia as determined by preoperative risk stratification may be reasonable (Boersma et al. The majority of data on perioperative statin use is derived from observational studies demonstrating a protective effect on cardiac complications (Lindenauer et al. If urgent surgery is required within this time period, antiplatelet therapy should be continued unless the relative risk of bleeding outweighs the benefit of the prevention of stent thrombosis. If the antiplatelet therapy must be discontinued, it is recommended to continue aspirin and to restart antiplatelet therapy as soon as possible after surgery. Perioperative planning should be determined in concert with the entire medical team to optimize therapy plans and outcomes. The initiation or continuation of aspirin is not beneficial in patients undergoing elective, noncardiac, noncarotid surgery in those without stents unless the risk of ischemic events outweighs the risk of surgical bleeding (Fleisher et al. In patients requiring surgery, the risks of bleeding must be weighed against the benefit of remaining on anticoagulants. In procedures with minimal risk of bleeding, it may be reasonable to continue the anticoagulants perioperatively. Of note, vitamin k response is delayed, including a delayed return to therapeutic level of anticoagulation, when the antagonists are restarted. Vitamin k antagonists should be discontinued 5 days preoperatively, with bridging therapy at the same time, if utilized. Vitamin k antagonist therapy may then be reinitiated 12-24 hours postoperatively following confirmation of adequate hemostasis. For procedures with an elevated risk of surgical bleeding, it is recommended to discontinue the inhibitors 48 hours or more prior to the procedure (Fleisher et al. Thromboembolic disease is the most frequent cause of postoperative death in patients with uterine or cervical carcinoma (Martino et al. Risk stratification, dependent upon patient-specific and procedural-specific risk factors, may be implemented within models to determine the need for therapy, balanced with the risk of bleeding (Geerts et al. One such model, the Caprini score, estimates risk according to a point system (Caprini 2005). An adaptation provided in the American College of Chest Physicians consensus statement published in 2012 categorizes risk as very low (0-1 point), low (2 points), moderate (3-4 points), or high (5 points) (Gould et al. Commonly placed within the highest risk categories, the cancer patient is often subject to additional risks including chemotherapy, radiation therapy, and hormonal treatment, further necessitating the need for long-term thromboprophylactic therapy. Options for perioperative thromboembolic prophylaxis include pharmacologic and mechanical methods. Dual prophylaxis with pharmacologic and mechanical methods may benefit the high-risk oncology patient, and is possibly cost-effective (Agnelli et al. Moderaterisk patients should have at least one type of preventative measure (mechanical or pharmacologic). High-risk patients subjected to a major cancer procedure or with multiple risk factors should receive thromboprophylaxis after hospital discharge for up to 28 days postoperatively. Extended prophylaxis for this is supported by the American College of Chest Physicians and American College of Gynecologists (Geerts et al. Although rare, patients with a strong family history of clots who are negative for Factor V Leiden or prothrombin mutation should consider additional testing (Rosendaal 2005). Antiphospholipid syndrome is an acquired thrombophilia associated with arterial and venous thrombosis. Testing for antiphospholipid syndrome includes serum analysis for lupus anticoagulant and anticardiolipin antibodies (de Groot and Derksen, 2005). Increasing sensitivity of dynamic contrast-enhanced computerized tomography has confirmed the replacement of the prior gold standard of pulmonary arteriogram in the diagnosis of pulmonary embolism. Some patients on thrombogenic chemotherapy regimens may benefit from lifelong anticoagulation. Approximately 25% of morbidity in the early postoperative period is pulmonary related, including atelectasis, pneumonia, respiratory failure, and exacerbation of underlying chronic lung disease (Fisher et al. Major abdominal surgery induces a 20% to 30% overall risk of pulmonary complications (Ferguson 1999). Vital capacity is reduced by 45% and functional residual capacity is reduced by 20% with laparotomy (Qaseem et al. The supine position results in a reduction of functional residual capacity below alveolar closing volume, significantly increasing the postoperative risk of atelectasis. Several additional intraoperative factors increase the risk of perioperative pulmonary complications (Table 2. Procedural-based pulmonary risk factors include duration of surgery, choice of anesthetic, the emergent nature of the procedure, and incision location. Risk factors specific to the patient include increasing age, chronic lung disease, cigarette use, functional status, obesity, congestive heart failure, asthma, obstructive sleep apnea, poor mental status, alcohol use, and neurologic impairment (Doyle 1999, Smetana et al. If the stress test is abnormal, consider coronary angiography and revascularization depending on the extent of the abnormal test. Risk reduction strategies in the postoperative period include pulmonary expansion by means of incentive spirometry, chest wall expansion, deep breathing, and cough, none of which has been proven to be superior to the others. Increased use of bronchodilators and steroids, exacerbations, and smoking are risk factors for perioperative bronchospasm. Prophylaxis in reactive airway disease is with perioperative inhaled beta agonists by inhaler or nebulizer therapy. Steroid therapy should be reserved for those patients already using them as a part of their current regimen, which may decrease inflammation preoperatively and minimize bronchospasm postoperatively. Prophylactic antibiotics have no place in perioperative therapy to prevent pulmonary complications. Patients on oral steroids for prolonged periods of time should receive preoperative stress dose steroids (see below; "Adrenal Suppression"). Preoperative consultation with an anesthesiologist may be helpful in this patient population for planning medication use, optimization of therapy, and communication. Smoking increases the risk of postoperative complications even in the absence of chronic lung disease. Perioperative pulmonary risk is particularly increased in those who have been smoking more than 20 years, and is highest in patients still smoking within 2 months of surgery (Moller et al. Obstructive sleep apnea increases risk for airway management difficulties in the immediate perioperative period; however, with the epidemic of obesity, almost all patients are at risk for some complication. Patients with a history of asthma or other restrictive lung diseases are at a minimal risk for postoperative complications (Smetana et al. There is no predictive value in obtaining a chest x-ray in a well, normal adult and it should not be included in the preoperative evaluation. Alternatively, patients at increased risk for perioperative pulmonary complications, including those older than 50 years of age and those with diagnosed lung disease, may benefit from a baseline chest x-ray. Patients with longstanding restrictive lung disease are at a significantly elevated risk for pulmonary hypertension. Spirometry may be helpful in diagnosing obstructive lung disease; however, it has not been proven to be predictive of postoperative pulmonary complications. Management may be determined in concert with the anesthesiologist, and may require cancellation or pulmonary rehabilitation. A low serum albumin (<35g/L) is an additional marker for increased risk of postoperative pulmonary assessment of endocrinologic risk Diabetes Mellitus Perioperative hyperglycemia has been found to increase the risk of adverse events in patients undergoing elective noncardiac surgery (Frisch et al. Postoperative glucose levels greater than 200 mg/dL are associated with prolonged hospital stays and increased risk of postoperative complications including wound infections and cardiac arrhythmias (Ramos et al. Diabetes-associated perioperative risk can be determined by evaluating the extent of the disease.
Cnidium Fruit (Cnidium). Roxithromycin.
- Increasing sexual performance and libido, erectile dysfunction, infertility, body building, increasing energy, cancer, osteoporosis, infections, itchy skin, rashes, eczema, and ringworm.
- How does Cnidium work?
- What is Cnidium?
- Are there safety concerns?
- Dosing considerations for Cnidium.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=97044
Purchase roxithromycin cheap online
Treatment of locally advanced vaginal cancer with radiochemotherapy and magnetic resonance image-guided adaptive brachytherapy: Dose-volume parameters and first clinical results bacteria use restriction enzymes to order roxithromycin 150mg with mastercard. The relationship between brachytherapy dose and outcome in patients with bulky endocervical tumors treated with radiation alone. Excellent long-term survival and absence of vaginal recurrences in 332 patients with low-risk stage I endometrial adenocarcinoma treated with hysterectomy and vaginal brachytherapy without formal staging lymph node sampling: Report of a prospective trial. Primary radiotherapy for nonsurgically managed Stage I endometrial cancer: Utilization and impact of brachytherapy. Multichannel vaginal cylinder brachytherapyImpact of tumor thickness and location on dose to organs at risk. Trends in the utilization of brachytherapy in cervical cancer in the United States. Vaginal brachytherapy for postoperative endometrial cancer: 2014 Survey of the American Brachytherapy Society. Surgical-pathologic variables predictive of local recurrence in squamous cell carcinoma of the vulva. Radiation therapy versus pelvic node resection for carcinoma of the vulva with positive groin nodes. Definitive radiotherapy for treatment of primary vaginal cancer: Effectiveness and prognostic factors. The Vienna applicator for combined intracavitary and interstitial brachytherapy of cervical cancer: Design, application, treatment planning, and dosimetric results. Treatment preferences and involvement in treatment decision making of patients with endometrial cancer and clinicians. Endometrial carcinoma: High dose-rate brachytherapy in combination with external irradiation; a multivariate analysis of relapses. For locally advanced cervical and vaginal cancer, brachytherapy delivers high doses to the tumors while keeping normal tissues to limited doses. Incorporation of brachytherapy into the treatment of these patients results in increased tumor control and overall survival with reasonable rates of toxicity. Close pre-, intra-, and post-operative collaboration between surgeon and radiotherapist will best guide this application. Vaginal brachytherapy for postoperative endometrial cancer decreases the rates of vaginal recurrence at very modest rates of toxicity. Postoperative external irradiation and prognostic parameters in stage I endometrial carcinoma: Clinical and histopathologic study of 540 patients. Carcinoma of the intact uterine cervix treated with radiotherapy alone: A French cooperative study: update and multivariate analysis of prognostics factors. Preoperative intensity-modulated radiotherapy and chemotherapy for locally advanced vulvar carcinoma. American Brachytherapy Society consensus guidelines for interstitial brachytherapy for vaginal cancer. Definitive radiotherapy for carcinoma of the vagina: Outcome and prognostic factors. Surgery and postoperative radiotherapy versus surgery alone for patients with stage-1 endometrial carcinoma: Multicentre randomised trial. The Vienna applicator for combined intracavitary and interstitial brachytherapy of cervical cancer: Clinical feasibility and preliminary results. Clinical use of the Utrecht applicator for combined intracavitary/interstitial brachytherapy treatment in locally advanced cervical cancer. Definitive radiation therapy for invasive carcinoma of the vagina: Impact of high-dose rate intracavitary brachytherapy. Postoperative high dose-rate intravaginal brachytherapy combined with external irradiation for early stage endometrial cancer: A long-term follow-up. Precis de curietherapie, endocurietherapie et plesiocurietherapie, Paris, France: Masson. Clinical and pathological prognostic factors in squamous cell carcinoma of the vulva. Long-term follow-up of a randomized trial comparing concurrent single agent cisplatin, cisplatin-based combination chemotherapy, or hydroxyurea during pelvic irradiation for locally advanced cervical cancer: A Gynecologic Oncology Group Study. Consensus statement for brachytherapy for the treatment of medically inoperable endometrial cancer. The role of interstitial brachytherapy in the treatment of vaginal and vulvar malignancies. Uterine perforation - 5-year experience in 3-D image guided gynaecological brachytherapy at Institute of Oncology Ljubljana. American Brachytherapy Society consensus guidelines for adjuvant vaginal cuff brachytherapy after hysterectomy. External pelvic and vaginal irradiation versus vaginal irradiation alone as postoperative therapy in medium-risk endometrial carcinoma-A prospective randomized study. Postoperative vaginal irradiation with high dose rate afterloading technique in endometrial carcinoma stage I. Interstitial brachytherapy in the treatment of advanced and recurrent vulvar cancer. The quality of cervical cancer brachytherapy implantation and the impact on local recurrence and disease-free survival in radiation therapy oncology group prospective trials 0116 and 0128. American Brachytherapy Society consensus guidelines for locally advanced carcinoma of the cervix. The dosage distribution in the pelvis in radium treatment of carcinoma of the cervix. Martino Hospitals are also now dealing with a changing healthcare system where our economic model is shifting from fee-for-service to fee-for-performance (James 2012). By 2016, over 80% of all reimbursement by Medicare will be driven by performancebased metrics, and healthcare costs will become more shared by individuals and employers (medicare. With so many variables in the future of training, reimbursement, and surgical volume, validated surgical training programs are of utmost importance. Since the majority of hysterectomy procedures as of 2013 were performed through a robotic-assisted approach, standardizing this training platform is essential to safely teach future surgeons how to utilize emerging technologies such as robotics. Minimally invasive surgery has significantly changed the way surgeons care for patients, with the vast majority of gynecologic oncology patients receiving minimally invasive approaches to help manage complex gynecologic conditions. What have not changed through the years are the basic surgical principles that are needed to accomplish a surgical procedure safely. The key points that Halsted illustrated in the nineteenth century, including gentle handling of tissue, meticulous hemostasis, preservation of blood supply, strict aseptic technique, minimum tension on tissues, accurate tissue apposition, and obliteration of dead space, have been taught to every surgical trainee in one form or another for decades (Polavarapu 2013). What has changed over time is how those skills translate into minimally invasive surgical technique and how to appropriately teach and validate those skills in our trainees. Robotic assisted surgery remains a unique training arena where both surgeons (teacher and student) are not simultaneously doing surgery at the patient bedside. Thus many traditional training curricula are inherently not customized for these new surgical procedures. Residency and fellowship programs throughout the country are adapting and building innovative methods to teach and train in minimally invasive surgery with validated programs. While training programs are dealing with this new paradigm, challenges exist as to how best to teach and evaluate surgical skills with an objective and validated approach. Duty hour restrictions now require residents to average no more than 80-hour work weeks over the course of a month. Although there are many benefits for residents with these restrictions, multiple studies within general surgery programs have shown that mandated work-hour guidelines have decreased the number of operative cases for residents (Carlin 2007, Kairys 2008). One study within gynecology identified no changes in overall volume of cases with duty hour restrictions, but noted a difference in types of cases. Gynecology residents had more hysteroscopy and laparotomy procedures, but less total abdominal hysterectomies and total vaginal hysterectomies (Kane 2010). With decreasing surgical volume and limited time in the workday, innovative curricula have been optimized to be both efficient and simulation-based. This is best illustrated through the board certification process, which requires a written and oral examination to all generalists and subspecialists.
Trusted 150mg roxithromycin
However antibiotics for treatment of uti in pregnancy generic roxithromycin 150 mg fast delivery, if there are cranial nerve signs, one must consider a brain stem tumor as well as other degenerative diseases of the brain and brain stem. If there are no findings on the examination to indicate a level, then, of course, the entire spine would have to be covered. The spinal tap with analysis of the 74 fluid for myelin basic protein and gamma globulin levels should be done if multiple sclerosis is suspected. Finally, the most cost-effective approach to a patient with ankle clonus is to refer the patient to a neurologic specialist. There is no cough or night sweats to suggest tuberculosis, carcinoma, or other pulmonary conditions. Acute anorexia would most likely be caused by an acute febrile disease or acute psychiatric disturbance. The most likely abdominal mass to produce anorexia as the only symptom would be an early pancreatic neoplasm. Other neoplasms may be felt and/or metastasize to the liver and cause hepatomegaly. If there is a chronic cough, one should consider tuberculosis or carcinoma of the lung. Hepatomegaly without any other masses present in the abdomen would certainly bring to mind cirrhosis. Also, the hepatomegaly may be related to a collagen disease or metastatic carcinoma. A complete endocrinologic workup by an endocrinologist may be indicated if all the above studies are negative. Patients with a normal physical examination and normal diagnostic studies should be referred to a psychiatrist. If the anosmia or unusual odor is intermittent, then one should consider psychomotor epilepsy. A skull fracture, particularly if it involves the cribriform plate, may interrupt the olfactory nerves and cause anosmia. If there is unilateral anosmia, one should consider an olfactory groove meningioma. Multifocal neurologic signs should suggest multiple sclerosis, and additional neurologic signs such as memory loss should suggest an olfactory groove meningioma or parietal lobe tumor. Many systemic diseases may cause anosmia, including hypothyroidism, diabetes, renal failure, hepatic failure, and pernicious anemia. This symptom is often delusional, so a psychiatrist may need to be consulted at the outset. Sulfonamides are notorious for causing renal failure, but one must also consider amphotericin B, gold compounds that might be administered in arthritis, and lead and other drugs or heavy metals. If there is hypertension and anuria, one should consider acute or chronic glomerulonephritis, polycystic kidneys, and acute tubular necrosis. If there is a low blood pressure, one should consider prerenal causes of anuria such as dehydration, blood loss, the acute abdomen, and other causes of shock. If there is chest pain, one should consider myocardial infarction or pulmonary infarction. If there is chest or abdominal pain with hypertension, then one should consider dissecting aneurysm. Enlargement of both kidneys should suggest bilateral hydronephrosis or polycystic kidneys. Enlarged bladder would make one think of bladder neck obstructions due to prostatic hypertrophy or carcinoma or a urethral stricture. Occasionally, what is thought to be an enlarged bladder is actually a pelvic mass that is obstructing the ureters. Hematuria would suggest glomerulonephritis, acute tubular necrosis, intravascular hemolysis, and nephrolithiasis. A Foley catheter should be passed and attached to drainage to determine the urine output. If there is obstructive uropathy due to bladder neck obstruction, this will obviously determine the diagnosis, as there will be a large volume of urine and it should be taken off gradually. Then studies of obstructive uropathy can be done, including cystoscopy and 80 retrograde pyelography. If the obstructive uropathy is caused by obstruction of the ureter, renal ultrasonography can be reliable in detecting the dilated calyces or dilated ureter. If the patient presents with anuria and hypotension, the most important thing is to reestablish the blood pressure with a bolus of normal saline or dopamine drip. If the anuria does not cease at this point, high-dose furosemide or a mannitol infusion can be started. The clinician should examine the urinary sediment himself, and this will identify cases of acute glomerulonephritis, lupus erythematosus, and acute tubular necrosis with considerable accuracy. If intravascular hemolysis is suspected, serum haptoglobins and serum hemoglobin tests should be done. Renal angiography and aortography should be done in cases of suspected dissecting aneurysm or bilateral renal artery stenosis. Abdominal ultrasound will also be helpful in diagnosing polycystic kidneys and pelvic masses that may be obstructing the ureter. In difficult cases, a renal biopsy may be necessary to diagnose the various collagen diseases and the various forms of glomerulonephritis. Intermittent anxiety suggests the possibility of psychomotor epilepsy, a pheochromocytoma, or insulinoma. It is also possible that the patient is suffering from an intermittent cardiac arrhythmia such as paroxysmal supraventricular tachycardia or atrial fibrillation. The young or middle-aged patient is more likely to be suffering from a psychiatric disorder, whereas the older patient may be suffering from cerebral arteriosclerosis or some other type of dementia. Tachycardia that is sustained during sleep would suggest hyperthyroidism, caffeine effects, or other drug effects. Sustained tachycardia with weight loss makes hyperthyroidism a very likely possibility. If routine laboratory studies and physical examination are normal, a trial of selective serotonin reuptake inhibitors may be warranted before launching on an expensive diagnostic workup. A 24-hour urine collection for catecholamines should also be done to rule out a pheochromocytoma. Twenty-four-hour Holter monitoring may be necessary to rule out a paroxysmal cardiac arrhythmia. If these are not revealing, perhaps 24-hour Holter monitoring may be of some value. It may be even wiser to consult a psychiatrist before undertaking an expensive workup. Episodic aphasia, apraxia, or agnosia would suggest epilepsy, transient ischemic attacks, migraine, or hypertensive encephalopathy. Acute onset of aphasia, apraxia, or agnosia would suggest a cerebral vascular accident, or if there is fever, the onset of a cerebral abscess. The gradual onset of aphasia, apraxia, and agnosia would suggest a tumor or other type of space-occupying lesion. Headaches with aphasia, apraxia, and agnosia might suggest migraine, but one should not forget a brain tumor. Fourvessel angiography may need to be considered, but a neurologist should be consulted before this is done. If there is associated dyspnea, one should look for congestive heart failure, pulmonary emphysema, and other cardiopulmonary conditions. Edema in the lower extremities along with significant proteinuria certainly suggests a nephrotic syndrome, whether it is caused by glomerulonephritis, diabetes, or a collagen disease. If there is no significant proteinuria, then a primary peritoneal condition such as tuberculous peritonitis or peritoneal carcinomatosis must be considered. A peritoneal tap with analysis of the fluid to determine whether it is a transudate or exudate, and cell block studies as well as amylase, culture and sensitivity should be done; an elevated amylase indicates pancreatic disease. Laparoscopy is useful in differentiating peritoneal carcinomatosis from tuberculous peritonitis. As the diagnostic tests become more expensive, the clinician should consider a referral to a gastroenterologist, nephrologist, or hepatologist before proceeding.
Buy discount roxithromycin online
Theoretic concerns include unnecessary exposure of the fetus to radiation from the prophylactic catheter placement and technical malfunction of the catheterization equipment infection after abortion discount roxithromycin uk. Surgical management of postpartum hemorrhage requires a thorough knowledge of pelvic anatomy, vascular perfusion, and pathophysiology of pregnancy. Uterine compression sutures for postpartum hemorrhage: Is routine postoperative cavity evaluation needed The ability of the Haemonetics@ 4 Cell Saver System to remove tissue factor from blood contaminated with amniotic fluid. The B-Lynch surgical technique for the control of massive postpartum hemorrhage: An alternative to hysterectomy Prophylactic use of intravascular balloon catheters in women with placenta accreta, increta and percreta. Perioperative temporary occlusion of the internal iliac arteries as prophylaxis in cesarean section at risk of hemorrhage in placenta accreta. Uterine compression sutures for preserving fertility in severe postpartum hemorrhage: An overview 13 years after the first description. The introduction of intra-operative cell salvage in obstetric clinical practice: A review of the available evidence. Risk of synechiae following uterine compression sutures in the management of major postpartum haemorrhage. Transcatheter endovascular techniques for management of obstetrical and gynecologic emergencies. Fertility and pregnancy outcomes following uterine devascularization for severe postpartum haemorrhage. The role of interventional radiology in reducing haemorrhage and hysterectomy following caesarean section for morbidly adherent placenta. Vaginal cancer can be treated with an intracavity single- or multichannel vaginal cylinder for superficial and early stage tumors (Chyle et al. Interstitial brachytherapy should be performed for locally advanced and deeply invasive vaginal cancer (Beriwal et al. Brachytherapy for vulvar cancer can be performed with interstitial techniques, though there is potentially an increased risk of necrosis with brachytherapy for vulvar cancer compared to other gynecologic sites (Tewari et al. Interstitial Brachytherapy Interstitial brachytherapy involves placement of catheters into or surrounding a tumor. In gynecologic cancers, these catheters are most commonly needles that are placed through a perineal template to optimize proper needle spacing. The vaginal obturator acts as an anchor for the template and a guide for the needles that are most proximate to the vagina. For patients with an intact uterus, an intrauterine tandem can be placed through the cervix with the obturator placed over the tandem. This allows for dose to be delivered to the uterus and cervix, as in cases of locally advanced or recurrent cervical cancer with parametrial or pelvic sidewall involvement. More recently applicators have been developed that combine intracavitary and interstitial techniques, known as hybrid applicators. These applicators have been developed by groups from Vienna and Utrecht and named after those cities, respectively. These applicators use an intrauterine tandem and vaginal ring (Vienna) or ovoids (Utrecht) which act as a template for interstitial needles to be placed improving the geometry of the implant (Kirisits et al. Radiation therapy can be broadly categorized as either teletherapy (tele, Greek for far) or brachytherapy (brachy, Greek for near). Teletherapy can be delivered by a linear accelerator or by a radioactive source in the treatment machine such as a Cobalt-60 unit. Brachytherapy most commonly utilizes radioactive sources placed in a patient cavity (intracavitary) and/or in patient tissues (interstitial). Both intracavitary and interstitial applications of brachytherapy are integral to treat malignancies of the gynecologic tract. The purpose of this chapter is to outline the various disease sites, applicators, techniques, and treatment planning for gynecologic brachytherapy. Intracavitary Brachytherapy Gynecologic intracavitary brachytherapy generally involves placing an applicator through the cervical os into the uterine cavity, in the vaginal canal or vaginal fornices, or both. There are numerous applicators that can be chosen by the brachytherapist to individualize treatment delivery for the patient. Commonly used applicators for intracavitary cervical brachytherapy include tandem and ovoids, tandem and ring, tandem and vaginal mold, tandem and cylinder, and Miami applicator (tandem and multichannel cylinder). These applicators can be placed in the operating room with general anesthesia or in a brachytherapy suite with deep or conscious sedation. Brachytherapy is a crucial component of the treatment course for curable cervical cancer patients. Those patients not undergoing brachytherapy have a comparative decrease in overall survival (Eifel et al. In addition, increased brachytherapy dose and quality implants have been shown to improve overall survival and disease-free survival, respectively (Viswanathan et al. Despite the progresses of external beam radiotherapy, brachytherapy affords patients outcomes that cannot be matched with other modalities of radiotherapy. The goal of brachytherapy for cervical cancer is to choose a procedure and corresponding applicator to deliver the desired dose to the tumor and at-risk adjacent structures. Another way to prescribe brachytherapy dose in cervical cancer is milligram radium equivalent-hours. This method uses the total implant activity (unit of milligram radium equivalent) multiplied by the number of hours the implant is loaded. Advocates of this method prefer the direct manipulation of the two factors that affect dose-activity and time (Pierquin 1964, Walstam 1954). Both of these methods can be planned with dose prescribed based on orthogonal planar x-rays. More recently, the use of volumetric imaging to design and even individualize treatment plans has increased. The goal of intracavitary brachytherapy is to surround the tumor and cervix with the applicator so that a very high radiation dose can be delivered. The steps for classic placement of the intracavitary applicator are shown in Table 37. The procedure is routinely performed under anesthesia, ranging from conscious sedation to general anesthesia. A good examination under anesthesia is important prior to the procedure, as this will direct treatment planning. Manual and visual examination of the cervix and extent of tumor should be performed. A rectovaginal examination should focus on presence and extent of parametrial or pelvic sidewall involvement. If there is significant parametrial involvement or extension to the pelvic sidewall, then interstitial brachytherapy should be considered. Once prepped and draped, the cervix should be visualized and grasped with a tenaculum. Fiducials act as a soft tissue surrogate of the cervix and ensure that applicator positioning remains optimal on intraoperative plain films after vaginal packing has been completed. The cervix and should be dilated, preferentially under ultrasound guidance, to help ensure that the dilators and ultimately the tandem are placed in the uterine canal (Small et al. Uterine perforations are common given that the cervix and cervical os are often obliterated following tumor growth and subsequent treatment. Ultrasound guidance of tandem placement has been shown to decrease rates of uterine perforation, and it is especially beneficial in patients with challenging anatomy (Segedin et al. The uterine canal should be sounded and measured to determine the length from the external cervical os to the uterine fundus. The cervical stopper (phlange) should be placed at that distance from the tip of the tandem to prevent the tandem from perforating through the uterine fundus upon tandem placement. The largest ring or ovoids that fit snugly in the right and left vaginal fornices should be placed. The system should be assembled and manipulated to maximize the distance between the two halves of the ring or the ovoids. The intracavitary brachytherapy applicator comprises a tandem that is placed transvaginally through the cervical os extending to the uterine fundus. A vaginal ring, two colpostats (ovoids), or mold is placed in the vaginal fornices. The catheter is clamped and the bladder filled with sterile water or saline; Foley balloon is filled with 7 cc of radiopaque solution. Ultrasound with a transabdominal probe can expedite insertion process, assist with accurate placement, and prevent perforation.
Discount roxithromycin master card
If the appendix is retrocecal antibiotic resistance of helicobacter pylori in u.s. veterans buy discount roxithromycin on line, the cecum is mobilized by incising the peritoneum along the peritoneal reflection. The appendiceal artery is isolated, doubly clamped, cut, and secured with 2-0 suture. Single-layer continuous versus two-layer interrupted intestinal anastomosis: A prospective randomized trial. Colorectal stents for palliation of large-bowel obstructions in recurrent gynecologic cancer: An updated series. Comparison of continuous single layer polypropylene anastomosis with double layer and stapled anastomoses in elective colon resections. Single-layer continuous colon and rectal anastomosis using monofilament absorbable suture: Study of 500 cases. A comparison of end and loop colostomy for fecal diversion in gynecologic patients with colonic fistulas. Prophylactic ureteric catheterization has been suggested to allow better identification of the ureter intraoperatively. In one large series consisting of over 3000 patients, of which 15% underwent prophylactic ureteric catheterization, no significant difference in rates of injury was found, albeit the rate of injury was very low overall (Kuno et al. A small but randomized control trial also demonstrated no significant difference in injury rates with the use of ureteric catheterization (Chou et al. Furthermore, in a decision analysis study it was determined that while insertion was not costly, because of the low rates of injury there was no cost savings from prophylactic insertion (Schimpf et al. However, the authors themselves clearly state there is no evidence of benefit from insertion. Routine cystoscopy at the time of surgery has also been investigated in a number of studies, however there is also a lack of well-designed studies in this area (Patel and Bhatia 2009). Cystoscopy, although not preventative, may allow for early detection of vesical injury; this is of paramount importance, as this early detection leads to lower morbidity, a decreased need for additional surgeries, and less long-term sequelae (Dowling et al. In a meta-analysis, intraoperative cystoscopy allowed for a superior rate of detection of ureteric and bladder injuries compared to surgeries without cystoscopy (ureteric 89% vs. In a prospective series, the rates of detection were also shown to be greatly improved with utilization of cystoscopy (Vakili et al. While there is a small cost associated with it and it requires an expanded skill set, the benefit gained from early recognition of potential injuries surely makes routine cystoscopy a wise choice. Furthermore, intraoperative consultation with a urologist or a gynecological oncologist can help improve identification of potential injuries (Aviki et al. There has also been recent work using fluorescent dyes in animal models, which appears promising for intraoperative identification (Korb et al. So, although to date we may not have identified significant preventative measures, we can optimize early detection, which greatly decreases the morbidity of injuries. Traditionally, laparoscopic approaches have been associated with a lower rate of immediate recognition of ureteral injuries (Grainger et al. However, this has not been studied in the more contemporary setting where the impact of the learning curve has now been overcome. Given their anatomical proximity to gastrointestinal and reproductive organs, urological structures are innately prone to iatrogenic injury during obstetric and gynecological procedures. Among a large series of iatrogenic ureteral injuries, gynecological surgery was identified as the primary operation associated with injury in 73% of the cases (Dobrowolski et al. Rates of genitourinary injuries for specific gynecological surgeries vary greatly, especially among contemporary series, due in large part to the impact of the introduction of laparoscopic and robotic approaches (Brummer et al. However, three large population studies, either retrospective or prospective in nature, found rates of only 0. The improvement is most likely due to a number of factors, including modifications in surgical techniques, greater experience and training with minimally invasive techniques, use of adjunctive tools for identification of injury, and a greater emphasis on early recognition and prevention (Adelman et al. In addition, there has been greater emphasis on identifying putative risk factors for injury and possible preventative measures to avoid injury. This chapter focuses on two main subjects, ureteric injuries and use of urinary diversion. Injuries occur in one of two settings: either (1) it is oncologically necessary or (2) iatrogenic injury occurs due to poor visualization, difficult anatomy, or surgical error, which can be influenced by the risk factors mentioned. The latter may possibly be attenuated or avoided by utilization of preventative measures. However, rates of injury were no lower with preoperative intravenous pyelogram (Piscitelli et al. A number of studies have demonstrated that a more meticulous approach to intraoperative identification of the ureter is of greater benefit than preoperative imaging (Kuno et al. Maintaining an awareness of the pelvic anatomy and a high suspicion of injury will allow for prompt identification. Management of Ureteric Injuries Management of ureteric injuries is dependent on time of recognition, anatomical location, and extent of injury. Generally, if identified promptly, either intraoperatively or within the early postoperative period, these injuries can be managed with prompt surgical correction. Otherwise, if and when the injury is discovered in the delayed setting, the morbidity and quality of life of the patients is significantly affected. The mechanisms of injury during gynecologic oncology surgery include contusion, transection, ligation, crushing, obstruction, and avulsion. Management can require a range of interventions from intraoperative inspection of urinary structures to possible renal autotransplantation or ligation of the ureter and percutaneous drainage. Contusions of the ureter can generally be handled with observation and conservative management. An indwelling ureteric stent should be placed whenever compromise of the ureter is suspected. If there is severe or extensive contusion, this is often associated with future stricture formation or possible necrosis. Similarly, in the case of ligation, if recognized, a trial period of intraoperative observation after release of the suture or clip may be reasonable. Again, indwelling ureteric stenting should be placed for 4 to 6 weeks with any ureteral repair. More severe injuries, including transections, can be managed as per the algorithm Table 30. Upper ureteric injuries are unlikely to occur during gynecological oncology surgery, thus the algorithm focuses on mid- and distal ureteric injuries. General principles to abide by in repair of ureteric injury are listed in Table 30. Anatomy the most common sites of ureteric injury during hysterectomy are along the pelvic wall lateral to the uterine artery, the uretrovesical junction, and the base of the infundibulopelvic ligament (Liapis et al. Vascular Supply the superior and inferior vesical arteries, both branches from the anterior internal iliac artery, provide the majority of the vascular supply to the bladder. The ureter takes its supply from the vessels it is in proximity to , namely the abdominal aorta, the internal and external iliacs, and the vesical arteries. It is helpful to remember during injury and reconstruction that the majority of the vascular supply for the distal ureter comes from the lateral aspect, while more proximately it arises medial to the ureter. Innervation Sympathetic and parasympathetic afferent and efferent fibers from the vesical plexus innervate the bladder. Ureteroureterostomy Management of ureteric injuries requiring ureteroureterostomy can be approached in two ways. If there has been a laceration with less than 50% transection, primary repair may be indicated. If a laceration is present but there is healthy tissue at the site of injury, closure in a transverse fashion to offset the risk of stricture, and using absorbable, monofilament sutures in an interrupted fashion will allow for the least complex repair. If transection is greater than 50%, we recommend dividing completely and spatulating the ends of the ureter in an opposing manner. Most urologists employ interrupted anastomotic sutures for the initial portion of the approximation. Given the rapid uptake of robotic surgery in the United States, more and more procedures are performed robotically. These injuries are manageable robotically, and most urologists have robotic experience.
Roxithromycin 150 mg on-line
Moreover antibiotic john hopkins purchase roxithromycin 150mg overnight delivery, it has been found that molecular interactions with modulatory proteins or drugs can partially rescue the function of Na+ channels with mutations that normally lead to a complete loss of function [26]. This evidence further shows that more research is needed to clarify the functional effects of channel mutations in vivo and the variability of the phenotypes resulting from Na+ channel mutations. Mechanisms of Epileptogenesis 41 Unlike Na2+ and Ca2+ channels, which are large monomeric proteins that include four homologous repeats, K+ channels are made by the assembly of four proteins each of which contain six transmembrane domains and is therefore similar to one Na+ or Ca2+ repeat, thus the resulting structure is similar to that of Na+ and Ca2+ channels, but the number of possible subtypes is much higher because of the large number of possible combinations. Although it is assumed that there are subtle functional differences between the different subtypes, the currents flowing through the K+ channels are grouped in a relatively limited number of physiological categories. Disrupted K+ channel function is involved in the epileptogenesis in some spontaneously occurring human epilepsies. However, this is difficult to prove experimentally for three reasons: (i) given its paramount importance for protein synthesis and metabolism, a considerable amount of Ca2+ is stored in the cytoplasmic reticulum and any artificial change in its concentration in an experimental preparation can mobilize it from the storage compartment to the ionized free fraction, thus leading to complex effects on cell excitability that are further complicated by metabolic effects, which are often difficult to resolve; (ii) the role of Ca2+ in promoting vesicle fusion at nerve terminals adds a presynaptic effect that has to be taken into account when evaluating membrane excitability as a function of Ca2+ concentration; and (iii) a number of the Ca2+-dependent K+ currents contributing to cell excitability may be impaired when Ca2+ concentration is artificially lowered, thus leading to indirect and somehow unpredictable consequences that may obscure the direct effect of Ca2+ movement across the membrane. The characterized Due to the fact that neuronal membrane needs a perfect balance of ionic currents to regulate intrinsic the physiological excitability, malfunctioning of other voltage sensitive channels can be critical to 42 Chapter 3 generate pathological oscillations and paroxysmal events. Ligand-gated channels Ligand-gated channels, or receptors, are molecular complexes that include a pore region or ionophore, which becomes permeable to some ions when the relevant ligand binds to a specific binding site. Ligand-gated channels are classified according to a scheme based on the ligand (neurotransmitter or neuromodulator), with a number of functionally distinct subtypes being differentiated in each category based on pharmacological (affinity for artificial ligands) or physiological criteria (selective ion permeability). Pharmacological agents acting on receptors can affect not only the primary epileptogenic process, but also its effects in regions beyond the epileptogenic area. The amino acids glutamate and aspartate are the two main excitatory neurotransmitters in the cerebral cortex and act through various receptor subtypes, the subunit composition of which determines the selective ionic permeability and kinetics of the respective ionic currents [47]. Five subunits from seven subunit subfamilies (, and) assemble to form a heteropentameric Cl-permeable channel. Furthermore, the hyperexcitable dentate gyrus removed from patients with temporal lobe epilepsy retains bicuculline-sensitive synaptic inhibition [53]. Membrane ion channels as targets for antibodies in acquired autoimmune disorders Antibodies to neuronal surface proteins have been found in patients with seizures presenting as symptom of paraneoplastic or autoimmune encephalopathies [66,67]. The precise mechanisms of seizures resulting from the synthesis of antibodies against channel or receptors remain incompletely understood [68]. In fact, the possibility of a direct action of the antibody on the channel and/or receptor has been hypothesized for Rasmussen encephalitis [69] but not ultimately demonstrated. Channel and receptor trafficking and plasticity the efficient delivery of cellular constituents to their proper location is of fundamental importance for all cells and has a pivotal role in normal neuronal functions. Protein trafficking is essential in developmental processes and plasticity and includes neurotransmitters release by exocitosis, recycling of synaptic vesicle proteins and regulation of receptor signalling. Neuronal function can be significantly modified by alterations in the levels of receptors, ion channels and transporters at both pre- and postsynaptic level and defective protein trafficking can be a significant mechanism in sustaining excitability changes and epileptogenesis. A main topic relating to trafficking defect in epilepsies arise from observation made on genetically determined channelopathies, which can be assumed as a general model of excitability changes resulting from disturbed protein function and interaction which can also occur as a consequence of epileptogenic events supporting epileptogenic progression. Its pore region has a pentameric structure consisting of various hetero- or homologous combinations of eight -subunits and three -subunits. As the 4-subunit is widely distributed in the mammalian brain, it is puzzling how the mutation can cause a focal hyperexcitability syndrome. Some mutations in Na+ channel function directly lead to hyperexcitability thus accounting for the occurrence of seizures; however, other mutations lead to loss-offunction that often results from folding and/or trafficking defects capable of reducing channel expression. Some of these mutations appear to act through decreasing binding of calmoduline which impairs the exit of Kv7. The possibility that the genetic background or modifying genes have a role in influencing trafficking dependent defects may account for different phenotypic expression of the same gene mutation, which effect can be attenuated or increased by modulatory proteins. This can open novel therapeutic possibilities acting by rescuing trafficking-defective mechanisms using appropriate drugs or interacting proteins. These therapeutic strategies may be targeted to amend specific genetic defects but can also model future treatments for acquired epilepsies. In fact, beside inherited channelopathies, evidence obtained in models of acquired epilepsies also point toward excitability dysfunction resulting from defective trafficking of ionic channels. For instance, decreased availability of A-type potassium ion channels found in models of temporal lobe epilepsy has been attributed to result from transcriptional (loss of channels) and post-translational (increased channel phosphorylation by extracellular signal-regulated kinase) mechanisms [76]. The knowledge of protein trafficking defects and adaptive mechanisms taking place during epileptogenic processes might open new strategies in the therapeutic interventions. K+ channels the synchronization of large populations of synaptically connected neurons. The physiology of this multisynaptic system and its relevance to epilepsy have been a focus of intense research. In this section the role of local circuits regional networks and system are considered. Such networks can be discretely localized or more widely distributed within one hemisphere [83]. The concept of an epileptogenic network as seizure generator typically applies to limbic epilepsies. Their physiological and pathophysiological properties relevant to epileptogenesis are further commented upon here. Some information concerning the significance of integrative hippocampal activities has come from studies of the correlations between cell activities and behaviour. Above all, these have demonstrated a fundamental relationship between the discharging properties of hippocampal cells and arousal, the most important finding being the modifications created during the acquisition of conditioned responses. Thanks to these properties, the limbic (and particularly hippocampal) circuits are capable of recording and storing traces of information originating from the various sensory systems by constructing a cognitive map that is continuously updated on the basis of experience [86]. The relevance of hippocampal plasticity in the pathophysiology of temporal lobe epilepsies was first demonstrated by Graham Goddard [87]. The role of such an epileptogenic plasticity in determining the progressive course of some types of epilepsies is discussed further in the next section. The arrows in parts (a) and (b) indicate efferent and afferent connections, respectively. Sensory information reaches the amygdala through the lateral nucleus and is then distributed in parallel to the various other nuclei by means of a system of highly organized intra-amygdaloid circuits. Amygdala discharges are often associated with oral feeding automatisms (chewing movements) that are sometimes accompanied by salivation [89], less frequently with unmotivated fear and even more rarely with the emotional expressions of anger and aggressiveness described in classic animal studies [90]. Cingulate gyrus the cingulate region appears to be involved in conditioned responses presumably connected with the acquisition of avoidance reactions. The symptomatology of epileptic seizures originating from the anterior cingular region includes terror, screams, aggressive verbal expressions, complex gestural automatisms, vegetative disturbances and visual hallucinations associated with only partial alterations in consciousness [91]. The anatomical basis underlying the motor expression of the responses are the connections between this region and the caudate nucleus, the ventral pontine nuclei, the ventral part of the periaqueductal grey matter and the deep strata of the superior colliculus. The posterior or retrosplenial cingulate region seems to be particularly involved in the processes of spatial discrimination associated with visual information. Among the limbic structures many networks can be identified that account for the clinical manifestations of limbic seizures and for the spread of the generating discharges inside and outside the limbic area possibly resulting in secondary generalization. What makes the system prone to seizure generation is matter for hypothesis-driven investigations, putative mechanisms include genetic and developmental factors and their interaction, but also environmental factors that electively affect the excitable properties of the relevant system. In this sense the SystE hypothesis provides a conceptual alternative to the current views based on the double dichotomy: focal versus generalized/idiopathic versus symptomatic epilepsies. One condition that exemplifies well the concept of SystE is absence epilepsy and its relationship with thalamo-cortical system. Recent evidence indicates that a non-inactivating Na+ current component may act synergistically with the T-type Ca2+ current [101]. Both the thalamic the organization of the fibre connections within the brain is so rich that the number of circuits that one can identify is virtually unlimited. Yet the claims of a given circuit as the basis for a given type of seizures should be accepted only when sound proof of its responsibility is provided. Among the corticocortical fibre bundles, specific mention should be made of the frontal callosal projections that have a role of in the interhemispheric synchronization of epileptic discharges. They obtained different types of pseudogeneralized discharges depending on the location of the bilateral frontal loci, a finding that correlates well with the marked tendency towards the bilateral expression of seizures with a frontal origin in humans.