Buy rogaine 2 60ml line
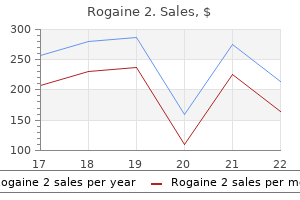
Clusters of comma-shaped bodies are present in nearly onefourth of the histiocytes man health sa discount 60ml rogaine 2 amex. The comma-shaped bodies are formed by two electron-dense membranes of approximately 6 nm, separated by a light space of approximately 8 nm. Where the infiltrate is denser, desmosome-like junctions may be observed among the histiocytes. Slowly the disease subsides spontaneously without a trace or leaving anetoderma-like macules. The papules begin to flatten, and then, after a short period of hyperpigmentation, the lesions disappear without leaving scars. Cutaneous lesions consist of the eruption of hundreds of lesions of two different types: (1) superficial papules and (2) deep nodules. The deep lesions are dermal nodules ranging from 1 to 5 cm, with overlying telangiectasia, mainly located on the trunk. Dense monomorphous histiocytic infiltrate in the papillary and mid-dermis, intermingled with a few lymphocytes. Electron microscopic examination reveals histiocytes with a large indented nucleus. They symmetrically involve the eyelids, trunk, face, and proximal extremities and, in flexures and folds, tend quickly to merge, forming soft plaques. Vasopressin-sensitive transitory diabetes insipidus may be present, but polyuria and polydipsia are generally mild. Prognosis is usually good, but respiratory tract involvement may lead to dyspnea and dysphagia. The lesions are characterized by a mixture of histiocytes, inflammatory cells, and foam cells. The papulonodular lesions range in diameter from a few millimeters to 2 cm and are round, translucent, and yellow-rose or yellow-brown. Grouping of lesions into plaques can give a cobblestone appearance, but lesions are generally scattered and isolated. Erythematous, photodistributed macules and papules have been observed in approximately 15% of cases and may be confused with dermatomyositis. Nail changes, including brittleness, longitudinal ridging, and atrophy, may occur. Almost 50% of affected patients have specific nodular lesions of the oral, nasal, and pharyngeal mucosae. Solitary cutaneous reticulohistiocytosis is characterized by a single firm, rapidly growing nodule varying in color from yellow-brown to dark red. Its most common location is the head, but it may be found in almost any cutaneous site. It occurs without evidence of systemic involvement, and its onset may be preceded by trauma. The lesions symmetrically involve the hands (80% of cases), knees (70%), wrists (65%), and less frequently the shoulders, ankles, elbows, hips, feet, and spine. Involvement of the muscles (myositis, myotonia, and myoatrophy), cardiopulmonary system (pericarditis, cardiac insufficiency, pleuritis, pulmonary infiltration), eyes (exophthalmos, conjunctival infiltration), gastrointestinal system (gastric ulcer), thyroid gland (thyroid nodules), and submandibular salivary glands have occasionally been reported, but histologic documentation of involvement at these sites is rare. Solid tumors such as bronchial, breast, gastric, and cervical carcinomas are most common. Lymphomas and myelodysplastic syndromes have been found less frequently, and malignant melanoma has been reported in three cases. An increase in immunoglobulin G and the presence of cryoglobulinemia and cold agglutinins have occasionally been reported. Histologically, the early lesions may be composed of histiocytes and lymphocytes, and therefore may be confused with other cutaneous histiocytoses. Note the histiocytic infiltrate (A) and multinucleated giant cells with aggregated nuclei and ground-glass cytoplasm (B). The number of giant cells may vary, and the diameter of these cells may reach 100 nm. The nuclei of the multinucleated cells may be arranged haphazardly or they may align along the periphery or cluster in the center. Histochemically, the granular material in histiocytes and giant cells stains with periodic acid-Schiff after diastase digestion, Sudan black, and scarlet red, which indicates the presence of glycolipids and/or glycoproteins and neutral fat. Dermal proliferation of histiocytes with diffuse cytoplasmic granular cell changes has recently been described. Cardiopulmonary manifestations are more frequently reported and may also be fatal. In addition, bones and all the visceral organs may be affected, which leads to weight loss and pyrexia that complicate the potentially mutilating inflammatory polyarthritis. The mucocutaneous lesions have an unpredictable course and may remit spontaneously. In half of the patients, the osteoarticular manifestations become stable, whereas in the other half, they cause progressive destruction. Recently, leflunomide was successful in one patient and therefore it can be considered a therapeutic option. Note "granulomatous" periphery of the lesion, with central ulceration and necrotic material at the base. The lesions are usually multiple and involve, in order of frequency, the face, trunk, and extremities. Areas of severe, clearly defined necrosis are sharply delineated from the surrounding granuloma. Numerous, atypical, very large, bizarrely angulated, multinucleated giant cells may be seen adjacent to the areas of necrosis. Dense, welldefined lymphoid nodules, occasionally containing a germinal center, may be present in the dermis or subcutis. Nausea, vomiting, epistaxis, back pain, and Raynaud phenomenon have also been recorded. The prognosis in given cases is difficult to predict and depends on extracutaneous involvement and the presence of visceral tumors such as multiple myeloma. Lymphocytes, plasma cells, and polymorphonuclear leukocytes, typically eosinophils, may be intermixed in the infiltrate. Emperipolesis (phagocytosis of leukocytes, especially lymphocytes) is a constant feature. In electron microscopic views, most of the histiocytes are rich in phagosomes and may contain clusters of comma-shaped bodies. Cutaneous manifestations are observed in approximately 10% of patients and are polymorphic. They may occur as yellowish macules and patches, reddish-brown papules, and plaques and nodules that may become eroded or ulcerated. In one patient, firm purple nodules and tumors as large as 10 cm in diameter were noted, but in most instances the lesions are much smaller, multiple, widespread, and asymptomatic. Cutaneous lesions may be the initial manifestation and sole presenting feature of the disease. Massive bilateral cervical lymphadenopathy, usually painless, is the hallmark of the condition. Less commonly, axillary, mediastinal, inguinal, and preauricular lymph nodes may be affected. Extranodal disease occurs in approximately 25% of patients and may be the initial manifestation of the disorder. The extranodal noncutaneous sites most commonly affected are the eye, upper respiratory tract, liver, spleen, testes, skeleton, and nervous system.
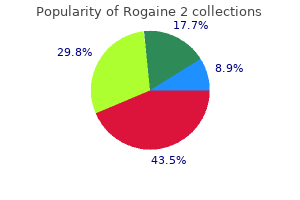
Discount rogaine 2 online
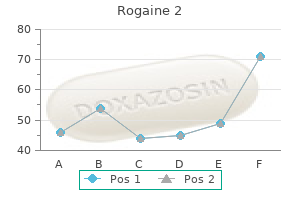
E: the membranous septum is divided into atrioventricular and interventricular components by the septal tricuspid leaflet (arrow) prostate cancer proton therapy buy rogaine 2 60 ml free shipping. The third side is located at the cardiac base and is associated with atrioventricular and semilunar valves. The left ventricle in humans is shaped like a strawberry, here shown whole and in long-axis. Rather than being facetious, this analogy serves to emphasize the complex shape of the chamber. In disease states that are commonly attended by appreciable alterations in ventricular shape, the use of standard formulas may result in determinations that are considerably inaccurate. As a result of this arrangement, systole is characterized by twisting or wrenching contractions that effectively wring blood out of the left ventricle, and diastole creates a vortex that literally sucks blood into the left ventricular chamber. In contrast, the muscular septum forms a rounded peak at its basal summit and becomes thickest at its midportion owing to the contribution of the right ventricular septal band. Then, after thinning a bit, the septum remains relatively constant in thickness and tapers only as it fuses with the apical portion of the free wall. Direct fibrous continuity exists between the anterior mitral leaflet and the left and posterior aortic cusps, and this region is reinforced bilaterally by the right and left fibrous trigones (Section "Base of the Heart"). In some hearts, small bundles of myocytes are embedded in this fibrous tissue and afford a minor degree of muscular separation between the two valves. With persistence of the left parietal band (so-called double conus), this muscle bundle causes appreciable valvular separation as is often seen in a double-outlet right ventricle. However, in contrast, the distances from the apex to the mitral annulus and from the apex to the aortic annulus are similar. The inflow length is appreciably shorter than the outflow length only with atrioventricular septal defects. Thus, in long-axis scans, a line drawn from the point of valvular continuity to the apex will divide the ventricle into an inferior inflow region and an anterosuperior outflow region and allows identification of the site of the membranous septum. The ventricular apex is characterized by small, shallow trabeculations, and the apical one-half to two-thirds of the septal surface is also finely trabeculated. More basally, the septum is smooth walled, and subendocardially, the left bundle branch travels in this region. Because the septal tricuspid leaflet inserts along its midportion, the membranous septum consists of atrioventricular and interventricular components. Their relative sizes vary inversely, depending on the level of tricuspid insertion. Moreover, the entire membranous septum varies considerably in size among individuals and tends to be largest in patients with Down syndrome. Septal defects in this region are generally associated with focal elevation of the tricuspid annulus to the level of the mitral valve so that the communication is interventricular rather than atrioventricular. Abnormalities in any of these structures may be associated with outflow tract obstruction. Examples include the discrete and tunnel forms of subaortic stenosis and hypertrophic cardiomyopathy. Along the anterior free wall, at the entrance to the outflow tract, is found the anterolateral muscle of the left ventricle, a prominent trabeculation that may cause outflow tract obstruction in association with certain anomalies (20,21). Conditions such as aortic stenosis that impose a pressure overload on the left ventricle induce concentric hypertrophy without appreciable dilation (pressure hypertrophy). In contrast, disorders that produce a volume overload, such as chronic aortic regurgitation, are attended not only by concentric hypertrophy but also by chamber dilation (volume hypertrophy). Although pressure and volume hypertrophy each increase the ventricular mass, only pressure hypertrophy is consistently associated with an increased wall thickness. In volume hypertrophy, dilation masks the degree of hypertrophy and wall thicknesses are often normal. Consequently, when the left ventricle is dilated, wall thickness cannot be used as a reliable indicator of hypertrophy. It is also important to recognize that hypertrophy, with or without dilation, decreases myocardial compliance and may hinder diastolic filling. Many forms of congenital heart disease are associated with moderate to marked degrees of ventricular hypertrophy and, as a result, there may be difficulty in achieving adequate myocardial preservation during long operations. Moreover, marked hypertrophy does not always regress significantly following reparative procedures and may become a source for ischemic injury as the individual survives into adulthood. Coarse apical trabeculations, indicative of a right ventricle, are more readily identified by angiography than by echocardiography. A: As shown schematically, compared with the normal state, pressure hypertrophy produces an increase in both wall thickness and surface area, whereas volume hypertrophy (with chamber dilation) increases the surface area but not the wall thickness. B: Compared with a normal heart (center), the heart with pressure hypertrophy (left) has a thick left ventricular wall, but the one with volume hypertrophy (right) has a normal wall thickness. Semilunar Valves General Features the semilunar valves connect the ventricles to the great arteries and serve to maintain unidirectional blood flow. The right and left coronary arteries arise respectively from the right and left aortic sinuses, proximal to this junction. These are often incorrectly called the right and left coronary sinuses; the coronary sinus, of course, is a venous structure that empties into the right atrium. The annulus of each semilunar valve assumes the shape of a triradiate crown, the three points of which attain the level of the sinotubular junction and demarcate the commissures. A commissure, in turn, represents the site at which two cusps meet along the annulus. Because the valvular orifice approximates the level of the sinotubular junction, autopsy measurements of the arterial diameter and circumference at this level correlate well with clinical measurements of orifice size (1). The leading edge of each cusp is its free edge beneath which lies a shallow biscalloped ridge, the closing edge, along the ventricular surface of the cusp. The arterial surface of each cusp, in conjunction with its arterial sinus, forms the valve pocket. B, C: the aortic valve, viewed from above, is shown in simulated opened (B) and closed (C) positions. D, E: Tomographic sections at the level of the aortic valve show adjacent structures as viewed from above (D) and below (E). During isovolumetric ventricular contraction, expansion of the arterial root may produce commissural separation and thereby initiate valvular opening. Pulmonary Valve the pulmonary valve lies closest to the chest wall, near the upper left sternal border, and its orifice is directed toward the left shoulder. Because right ventricular myocardium extends onto the pulmonary sinuses, the valve appears partially submerged within a crater of infundibular muscle. The anterosuperior limb of the septal band extends onto the left pulmonary sinus, and trabeculations parallel to the parietal band insert onto the right pulmonary sinus. In the setting of pulmonary atresia with an intact ventricular septum, failure to recognize these features has resulted in burrowing into the pericardial sac rather than into the pulmonary artery during closed operations (Brock procedure). Although this procedure is no longer performed, it is important to remember this potential complication during cardiac catheter manipulations. Aortic Valve the annulus of the aortic valve is a midline structure, and its orifice is directed toward the right shoulder. Consequently, its systolic murmurs are best heard along the upper right sternal border and radiate toward the neck. The right aortic sinus abuts the basal ventricular septum and right ventricular parietal band and is covered in part by the right atrial appendage. In contrast, the left aortic sinus rests against the anterior left ventricular free wall and a portion of the anterior mitral leaflet, abuts the left atrial free wall, and is covered in part by the main pulmonary artery and left atrial appendage. Finally, the posterior aortic sinus overlies the basal ventricular septum and a part of the anterior mitral leaflet, forms part of the transverse sinus, abuts the atrial septum, and indents both atrial free walls as the torus aorticus (aortic bulge). However, during childhood, the aortic cusps begin to thicken and become more opaque than the pulmonary cusps as a result of higher left-sided pressures.
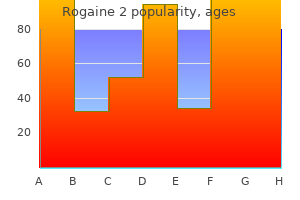
Generic rogaine 2 60ml with visa
Individuals most at risk for toxicity include patients taking systemic vitamin A derivatives for the treatment of dermatologic conditions such as acne mens health xmas gift guide discount rogaine 2 60ml with visa, psoriasis, and ichthyosis. The other population at risk includes vitamin food faddists who consume large quantities of nonprescription vitamin A supplements. A large, blinded randomized controlled study of elderly men with a history of two keratinocytic carcinomas in the 5 years prior to initiation of the study compared topical tretinoin 0. Surprisingly, the study was terminated 6 months early because of a statistically significant increase in all-cause mortality in the tretinoin group compared to the placebo group. Individuals with acute vitamin A toxicity have dry, scaly skin, with large areas of desquamation and fissuring of the lips and angles of the mouth. Other signs and symptoms include headache, fatigue, anorexia, nausea, vomiting, blurred vision, pseudotumor cerebri, myalgias, and arthralgias. An early cutaneous sign of chronic vitamin A toxicity in adults is dryness of the lips, which may progress to diffuse, dry, pruritic, scaly skin with peeling of palms and soles, alopecia, follicular hyperkeratosis, and hyperpigmentation of the face and neck. In children, chronic toxicity presents as coarse hair with diffuse alopecia, coarse skin with generalized exfoliation, hyperpigmentation, and exfoliative cheilitis. Associated pseudotumor cerebri with headaches and papilledema, and in infants may a bulging fontanelle may be present. Skeletal changes are common with vitamin A toxicity, and may present with growth retardation secondary to premature closure of the epiphyses and spontaneous bone fractures. Proposed mechanisms for the pathologic bone findings seen in vitamin A toxicity involves antagonism between vitamin A- and vitamin D-mediated intracellular signaling pathways and interactions with calcium-regulating hormones. Laboratory findings in patients with hypervitaminosis A include elevated levels of calcium and alkaline phosphatase. This alteration in calcium homeostasis can lead to calcification of tendons, ligaments, and soft tissues. Deposition of excess vitamin A in adipose tissue and perisinusoidal fibrosis of the liver, which can lead to cirrhosis, are the most significant effect of long-term vitamin A toxicity. Almost all of the symptoms of vitamin A toxicity subside after the excess vitamin intake is discontinued, with the exception of liver cirrhosis and consequences of pseudotumor cerebri. The condition was described as "carotenemia" in 1919 by Hess and Meyers who reported a connection between yellow skin pigmentation and increased serum carotene levels. Carotenes are not synthesized endogenously and are obtained through intake of carotene-rich foods. Plant carotenes are converted to vitamin A in the gastrointestinal tract, but approximately one-third of carotene is directly absorbed. Several factors can affect carotene absorption, including thyroid hormone, pancreatic lipase and bile acid concentrations, processing of foods, and dietary fat and fiber content. Hypothyroid patients notice an elevation of carotene levels as a result of decreased conversion to retinol. Pancreatic lipase and bile acids digest carotene so that a deficiency of these enzymes due to pancreatic or biliary or hepatic dysfunction could result in elevated carotene levels. Patients with conditions that lead to hyperlipidemia, like diabetes mellitus, nephrotic syndrome, and hypothyroidism, also predispose patients to carotenemia because of a linear relationship between the amount of -lipoprotein and carotene. Impaired conversion of carotene to vitamin A in patients with hypothyroidism and liver disease further contributes to carotenemia. Some patients with anorexia nervosa can present with carotenemia because of increased intake of vegetables. Other groups at risk for carotenemia are food faddists, those with excessive intake of nutritional supplements, dried seaweed (nori), carrots, and papayas, and infants ingesting a large amount of pureed vegetables. Excessive ingestion of carotenes does not result in hypervitaminosis A because the slow conversion of carotene to vitamin A in the intestinal mucosa is not rapid enough to produce toxic amounts of vitamin A. The yellow discoloration of skin secondary to carotenemia is called carotenoderma. The carotene is excreted by sebaceous glands and in sweat, so the yellow pigmentation appears first on the face, predominantly in the nasolabial folds and forehead, and then progresses to manifest diffusely, especially on the palms and soles. Of note, carotenoderma, in contrast to jaundice, spares mucous membranes, like the sclera. Treatment involves discontinuation of excessive carotene intake, and carotenoderma typically fades as the intake of carotene decreases. Vitamin D acts on the gastrointestinal tract to increase dietary calcium and phosphate absorption, stimulates increased bone resorption of calcium and phosphate, and stimulates the renal tubules to increase reabsorption of calcium and phosphate. Humans obtain vitamin D from two sources: (1) dietary intake, and (2) synthesis in the skin from exposure to ultraviolet light. Common dietary sources of vitamin D include fortified milk, fish oil, and fishes such as salmon, sardines, herring, tuna, cod, and shrimp. Vitamin D is essen- vitamin D3 (cholecalciferol), which enters the dermal capillaries. At this point, endogenous vitamin D3 joins with exogenous D2 (ergocalciferol) for hydroxylation in the liver to 25-hydroxyvitamin D. This molecule travels to the kidney where it is again hydroxylated to make mature vitamin D (1,25-hydroxyvitamin D, also known as calcitriol). The most common disorder seen with vitamin D is vitamin D-deficient rickets related to decreased dietary intake of vitamin D. Type I represents an autosomal recessive defect in renal vitamin D-1-hydroxylase, and is therefore treated with supplements of 1,25-hydroxyvitamin D. Supplementation with high doses of 1,25-hydroxyvitamin D and calcium may overcome this resistance. A surge in interest regarding the multisystem effect of vitamin D has spurred numerous studies. Groups at risk for vitamin D deficiency include those with inadequate diet, malabsorption, and decreased exposure to sunlight. This includes the elderly or debilitated who have decreased sun exposure or decreased vitamin intake; patients on anticonvulsant therapy; those with malabsorption from gastrointestinal surgery, celiac disease, or pancreatic or biliary disease; those with chronic renal failure; dark-skinned individuals living in areas with poor sun exposure; and breast-fed babies exclusively breastfed without vitamin supplementation. A recent resurgence in vitamin D-deficient rickets has prompted further evaluation of those at risk. A review of 166 cases of rickets in the United States between 1986 and 2003 showed that most cases presented between 4 and 54 months of age. Given the movement to encourage sunscreen use, there has been concern regarding secondary vitamin D deficiency. Theoretically, regular use of the recommended amount of sunscreen can decrease 25-hydroxyvitamin D levels, but with real-life application of inadequate amounts of sunscreen and the tendency for increased sun exposure in individuals wearing sunscreen, there seems to be no significant impact on the incidence of vitamin D deficiency. Early radiographic signs of rickets include widening of the epiphyseal plate and blurring of the epiphyseal and metaphyseal junction. If the disease progresses, deformities at the growth plate develop, including cupping, splaying, formation of cortical spurs, and stippling. A potentially fatal manifestation of vitamin D deficiency is a dilated cardiomyopathy. In a report of 16 British cases, three infants died and six additional infants were successfully resuscitated from cardiopulmonary arrest. However, within a few months after birth, scalp and body hair are lost with the exception of eyebrows and eyelashes. Small papules and cysts representing abnormal, rudimentary hair structures characteristically develop on the face and scalp. These cysts typically show disintegration of the lower two-thirds of the follicular unit. While the cutaneous features-notably the alopecia and cysts-are phenotypically and histologically identical, these are distinct clinical entities (Table 130-1). The classic manifestations of vitamin D-deficient rickets are skeletal (Box 130-7). Calcium and phosphorus deficiency leads to poor calcification of new bones, resulting in fraying and widening of the metaphysis.
Generic rogaine 2 60ml fast delivery
Congenital heart surgery nomenclature and database project: Hypoplastic left heart syndrome prostate cancer 70 year old buy rogaine 2 online from canada. Hypoplastic left heart syndrome diagnosed in fetal life: Associated findings, pregnancy outcome and results of palliative surgery. Borderline left ventricles in prenatally diagnosed atrioventricular septal defect or double outlet right ventricle: Echocardiographic predictors of biventricular repair. Foramen ovale size in the normal and abnormal human fetal heart: An indicator of transatrial flow physiology. Fetal aortic valve stenosis and the evolution of hypoplastic left heart syndrome: Patient selection for fetal intervention. Development of hypoplastic left heart syndrome after diagnosis of aortic stenosis in the first trimester by early echocardiography. Hypoplastic left heart syndrome: Progression of left ventricular dilation and dysfunction to left ventricular hypoplasia in utero. Low rate of prenatal diagnosis among neonates with critical aortic stenosis: Insight into the natural history in utero. Hypoplastic left heart syndrome with intact atrial septum: Utilization of a hybrid catheterization facility for cesarean section delivery and prompt neonatal intervention. Hypoplastic left heart syndrome with intact or highly restrictive atrial septum: Surgical experience from a single center. Optimization of preoperative status in hypoplastic left heart syndrome with intact atrial septum by left atrial decompression and bilateral pulmonary artery bands. Hypoplastic left heart syndrome with atrial level restriction in the era of prenatal diagnosis. Prediction and perinatal management of severely restrictive atrial septum in fetuses with critical left heart obstruction: Clinical experience using pulmonary venous Doppler analysis. Aortic stenosis and severe mitral regurgitation in the fetus resulting in giant left atrium and hydrops: Pathophysiology, outcomes, and preliminary experience with pre-natal cardiac intervention. Prenatal diagnosis and risk factors for preoperative death in neonates with single right ventricle and systemic outflow obstruction: Screening data from the Pediatric Heart Network Single Ventricle Reconstruction Trial. Outcome after prenatal diagnosis of hypoplastic left-heart syndrome: A case series. Fetal diagnosis of hypoplastic left heart, associations and outcomes in the current era. Tricuspid valve disease with significant tricuspid insufficiency in the fetus: Diagnosis and outcome. Outcomes and Predictors of Perinatal Mortality in Fetuses With Ebstein Anomaly or Tricuspid Valve Dysplasia in the Current Era: A Multicenter Study. Left ventricular function and geometry in fetuses with severe tricuspid regurgitation. Prenatal findings in total anomalous pulmonary venous return: A diagnostic road map starts with obstetric screening views. Spectrum of cardiovascular disease, accuracy of diagnosis, and outcome in fetal heterotaxy syndrome. Outcome of antenatally diagnosed cardiac rhabdomyoma: Case series and a meta-analysis. Diagnosis and management of fetal cardiac tumors: A multicenter experience and review of published reports. The outcome of monochorionic diamniotic twin gestations in the era of invasive fetal therapy: A prospective cohort study. Endoscopic laser surgery versus serial amnioreduction for severe twin-to-twin transfusion syndrome. Limited prognostic value of a staging system for twin-to-twin transfusion syndrome. The twin-twin transfusion syndrome: Spectrum of cardiovascular abnormality and development of a cardiovascular score to assess severity of disease. The outcome of twin reversed arterial perfusion sequence diagnosed in the first trimester. Intrafetal laser treatment for twin reversed arterial perfusion sequence: Cohort study and meta-analysis. Clinical characteristics and outcomes of patients with cardiac defects and congenital diaphragmatic hernia. Congenital diaphragmatic hernia and associated anomalies: Their incidence, identification, and impact on prognosis. Extracorporeal membrane oxygenation in infants with congenital diaphragmatic hernia and cardiac malformations. Congenital heart anomaly in newborns with congenital diaphragmatic hernia: A single-center experience. Prognostic factors of congenital diaphragmatic hernia accompanied by cardiovascular malformation. Preferential streaming of the ductus venosus and inferior caval vein towards the right heart is associated with left heart underdevelopment in human fetuses with left-sided diaphragmatic hernia. Left heart structures in human neonates with congenital diaphragmatic hernia and the effect of fetal endoscopic tracheal occlusion. Minimally invasive therapy for fetal sacrococcygeal teratoma: Case series and systematic review of the literature. Isolated cardiomegaly in the second trimester as an early sign of fetal hydrops due to intracranial arteriovenous malformation. Pentalogy of Cantrell: Two patients and a review to determine prognostic factors for optimal approach. Echocardiographic screening in neonates undergoing surgery for selected gastrointestinal malformations. Congenital heart disease and fetal thoracoabdominal anomalies: associations in utero and the importance of cytogenetic analysis. Assessment of fetal atrioventricular time intervals by tissue Doppler and pulse Doppler echocardiography: normal values and correlation with fetal electrocardiography. Reference values for time intervals between atrial and ventricular contractions of the fetal heart measured by two Doppler techniques. Relation between persistent atrial arrhythmias and redundant septum primum flap (atrial septal aneurysm) in fetuses. Perinatal outcome in fetuses with heterotaxy syndrome and atrioventricular block or bradycardia. Doppler echocardiographic isovolumetric time intervals indiagnosis of fetal blocked atrial bigeminy and 2:1 atrioventricular block. Mechanisms in fetal bradyarrhythmia: 65 cases in a single center analyzed by Doppler flow echocardiographic techniques. Autoimmune-associated congenital heart block: Demographics, mortality, morbidity and recurrence rates obtained from a national neonatal lupus registry. Isolated atrioventricular block in the fetus: A retrospective, multinational, multicenter study of 175 patients. Transplacental fetal treatment improves the outcome of prenatally diagnosed complete atrioventricular block without structural heart disease. Perinatal outcome of fetal atrioventricular block: Onehundred-sixteen cases from a single institution. Prenatal anti-ro antibody exposure, congenital complete atrioventricular heart block, and high-dose steroid therapy: Impact on neurocognitive outcome in school-age children. Fetal supraventricular tachycardia complicated by hydrops fetalis: a role for direct fetal intramuscular therapy. Noninvasive prenatal testing: a replacement for chorionic villus sampling and amniocentesis for advanced maternal age Fetal ventricular pacing for hydrops secondary to complete atrioventricular block. Effects of maternal-fetal hyperoxygenation on aortic arch flow in a late-gestation human fetus with closed oval foramen at risk for coarctation. First successful case of non-invasive in-utero treatment of twin reversed arterial perfusion sequence by high-intensity focused ultrasound. Cardiac intervention using high-intensity focused ultrasound: Creation of interatrial communication in beating heart of an anesthetized rabbit.
Buy rogaine 2
Group L Streptococci (often carried by pigs prostate oncology journals rogaine 2 60ml visa, cattle, and poultry) have been responsible for impetigo, secondarily infected wounds, and paronychias in meat handlers. The incidence of invasive complications (lymphangitis, suppurative lymphadenitis, bacteremia) of streptococcal infections of the skin has decreased in the antibiotic era. Distinct differences exist between acute rheumatic fever and acute glomerulonephritis in the site of the antecedent infection, the length of the latent period, and the streptococcal serotypes involved. In contrast, acute nephritis may follow infection of either the skin or the upper respiratory tract. A longer latent period of approximately 3 weeks is characteristic of acute nephritis associated with streptococcal pyoderma. Group A Streptococci are classified into over 80 subtypes, based on the antigenicity of their M proteins (fibrillar structures extending out from the cell surface). Although there is no strong evidence of an association between infection with any specific group A serotypes and the subsequent development of rheumatic fever as yet, several serotypes (particularly mucoid strains of types 1, 3, and 18) have been implicated in a few outbreaks of streptococcal sore throat complicated by this sequela. Type 12 is the classic serotype responsible for pharyngitis-associated acute nephritis, but other serotypes, such as 1, 4, 25, and 49, have been implicated. The pyoderma-associated nephritogenic strains generally belong to different serotypes: types 2, 49, 42, 55, 56, 57, and 60. The distinction between nephritogenic and other strains of Streptococci that might be associated with rheumatic fever can be seen in studies from Trinidad, a hyperendemic area for pyoderma-associated nephritis. There the streptococcal serotypes causing outbreaks of nephritis differed from the serotypes associated with sporadically occurring cases of acute rheumatic fever in the same population. Almost all rheumatic fever outbreak-associated strains belong to serotypes of class I and require a precursor nasopharyngeal infection. Current evidence indicates differences among class I organisms that may relate to their capacities to induce rheumatic fever: class I nasopharyngeal isolates appear to lack human IgG-binding activity, whereas nearly all impetigo isolates of the same class bear human IgG receptors. Streptococcal infection is usually defined as a positive throat culture with a serologic response to group A Streptococcus and the streptococcal carrier state by a positive throat culture and no serologic response. After streptococcal pharyngitis, specific antibodies develop to many of the extracellular enzymes of the Streptococci. Eighty-five percent of patients with acute rheumatic fever and a proven preceding streptococcal infection have an elevated or increasing antistreptolysin O titer. Antibodies to extracellular products, with the exception of antibody to the erythrogenic toxin of scarlet fever, appear to have no effect on the manifestations of illness. Streptococcal immunity is type specific (but not group specific), long lasting, and depends on the production of bactericidal antibodies to the specific M proteins of the over 80 different serotypes of group A organisms. Although recurrent pharyngeal infections caused by the same serotype are most unusual, repeated clinical infections caused by different types are not uncommon. Early treatment of streptococcal upper respiratory tract disease with antibiotics may suppress the appearance of type-specific antibody (and immunity), as well as the development of antibody to the extracellular products of the organism. In contrast to pharyngeal infections, the antistreptolysin O response with streptococcal skin infections or pyoderma-associated nephritis is weak. Although pyoderma strains of Streptococci produce M proteins, and although type-specific antibody may develop in patients with pyoderma-associated nephritis, the frequency of production of such antibodies and their role in protection against reinfection are unclear. Although pharyngeal reinfection with the same streptococcal serotype is probably unusual, some evidence suggests that the same serotype can be associated with repeated episodes of pyoderma. Specific diseases caused by group A (and other) Streptococci are listed in Box 176-8. Streptococcal pyodermas include all types of superficial streptococcal skin infections except erysipelas-that is, impetigo, ecthyma, and secondary infections of preexisting skin lesions. Streptococcal intertrigo such as streptococcal perianal "cellulitis" can occur primarily or secondarily in underlying conditions such as inverse psoriasis. Impetigo caused by group A Streptococcus is a highly communicable infection and occurs predominantly in preschool-aged children (usually before the age of 2 years except in highly endemic areas). Nongroup A (groups B, C, and G) Streptococci may be responsible for rare cases of impetigo; group B Streptococci are associated with impetigo in the newborn. Whereas, many different serotypes of group A Streptococci may cause pharyngitis, a limited number of newly described types predominate in impetigo (types 49, 52, 53, 55, 56, 57, 59, and 61). Streptococci are recovered from the respiratory tract of approximately 30% of children with skin lesions, but there is no clinical evidence of streptococcal pharyngitis. Thus, the sequence of spread in a given patient is from normal skin to lesions and eventually to the respiratory tract. When exposed to an infectious contact, preexisting lesions, such as scabies, varicella, or eczema, predispose to the appearance of infected lesions. Crowding, poor hygiene, and neglected minor skin trauma contribute to the spread of streptococcal impetigo in families. Although the majority of cases occur in children, particularly of preschool age, young adults are also affected. The inflammatory process of impetigo is superficial, with a unilocular vesicopustule located 2141 29 between the stratum corneum above and the stratum granulosum below. Impetigo caused by group A Streptococcus presents as a crusted superficial infection of the skin; an initial vesicular phase has been described but is rarely detected. Although the latent period after impetigo is longer than that after pharyngeal infection, the mildness of the illness delays or negates the seeking of medical attention. Practically, however, the majority of cases of nonbullous impetigo are caused by S. Perianal (group A) streptococcal "cellulitis" occurs principally in children, presenting with intense perianal erythema. Guttate psoriasis has also occurred in children, associated with perianal streptococcal infection. A Gram-stained smear of early vesicle fluid reveals Gram-positive cocci in chains. Culture of the weeping area or of the area beneath an unroofed crust reveals group A Streptococci or a mixture of Streptococci and S. If untreated, the process may persist and new lesions may develop over the course of several weeks; thereafter, the infection tends to resolve spontaneously unless there is some underlying cutaneous disorder such as eczema. If untreated, some lesions become chronic and deeper, such as ecthyma (see Section "Staphylococcal Ecthyma"). Topical treatment (removal of dirt, crusts, and debris by soaking with soap and water) is a valuable adjunct. Mupirocin ointment appears to be as effective as parenteral or oral penicillin for treatment of impetigo. A sharply marginated erythematous and oozing plaque in the axilla, which was also present in the other axilla, inframammary area, and inguinal folds, was painful in this human immunodeficiency virus-infected woman. The lesion may be more proximally located on the finger or extend to involve the nail folds. Blistering distal dactylitis may be treated with oral penicillins or erythromycin and release of subungual pus is often required. Staphylococcal blistering distal dactylitis has been reported with an identical clinical picture. Acute lymphangitis is an inflammatory process involving the subcutaneous lymphatic channels. It is most often caused by group A Streptococci, but occasionally may be caused by S. Well-demarcated erosive erythema in the perianal region and perineum in an 8-year-old boy who complained of soreness. Group A Streptococcus is responsible for the majority of cases of blistering distal dactylitis, also called bulla repens, usually occurring in children and adolescents. A large, tense blister develops, filled with seropurulent fluid, over the volar skin pad of distal fingers or toes. The systemic manifestations of infection may occur either before any evidence of infection that is present at the site of inoculation or after the initial lesion has subsided.
Liquorice (Licorice). Rogaine 2.
- Are there any interactions with medications?
- Muscle cramps, arthritis, lupus, infections, hepatitis, infertility, cough, stomach ulcers, prostate cancer, weight loss, atopic dermatitis (eczema), chronic fatigue syndrome (CFS), and other conditions.
- Upset stomach (dyspepsia), when a combination of licorice and several other herbs is used.
- Are there safety concerns?
- What other names is Licorice known by?
- What is Licorice?
- How does Licorice work?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96849
Generic 60 ml rogaine 2 visa
Hand-held ultrasound may augment what is learned from physical examination alone and may aid in detection of clinically silent abnormalities such as decreased systolic function androgen hormone oestrogen buy rogaine 2 60 ml on-line, ventricular dilation, pericardial effusions, and some mild valvular abnormalities. Further study of hand-held ultrasound, including its cost-effectiveness is needed to determine its clinical utility in congenital heart disease (20). Despite its availability, hand-held ultrasound will not supplant physical examination as a clinical assessment tool. Policy Statement: Endorsement of Health and Human Services recommendation for pulse oximetry screening for critical congenital heart disease. The genesis of gallop sounds: investigation by quantitative phono- and apex cardiography. Frequency analysis of heart murmurs correlates to severity of ventricular septal defect. Evaluation of transient heart murmur resembling pulmonary artery stenosis in term infants by Doppler and M-mode echocardiography. Handheld ultrasound versus physical examination in patients referred for transthoracic echocardiography for a suspected cardiac condition. Paridon Over the last 30 years, there has been a significant increase in the rates of overweight and obesity in children in developed countries. Concurrently, there has been a decline in physical activity in children and adolescents. Much more commonly, it happens to those athletes not previously suspected of having cardiac abnormalities. What information is available is restricted to adolescents and young adults, and, importantly, current recommendations are restricted to competitive sports. It also discusses the differences and various types of physical activity such as those of daily living, leisure sports, and organized competitive athletics. As well, differences in physiologic requirements of various athletic activities and their associated risks are discussed. Finally, what is known about the ability to participate in and the risks of athletic activities for the individual groups of congenital cardiac defects is discussed with emphasis on what is known about preathletic screening and recommendations for activities of daily living, leisure and recreational athletics, and participation in competitive sports. These in turn may be influenced by a number of factors such as age, sex, height, weight, and especially cardiovascular conditioning. The ability to successfully and safely undertake a given athletic activity depends on the combination of these factors and the requirements of the activity. All athletic activities can be roughly broken down into their "static" and "dynamic" components (8). The cardiovascular effects of high dynamic activity are quite different from static activity. To meet this oxygen demand, cardiac output may rise fivefold or more in well-conditioned athletes. In truth, there are no pure "static" or "dynamic" activities, and all athletic activities are to some degree, a combination of both types. It is important to remember that the values for this table refer only to competitive sports in adolescents and adults. The contents of this table have little or no relevance to competitive sports participation in the preadolescent population. Much of preadolescent competitive sport training focuses on learning basic skills and coordination. Any parent will tell you that soccer played by a group of 7-year-olds bears almost no relationship to soccer being played by a group of 17-year-olds. Types of Physical Activity Physical activities can be divided into three broad types of activities: (a) activities of daily living, (b) leisure and recreational sports, and (c) competitive sports. Activities of Daily Living "Activities of daily living" is an inclusive term that encompasses all the physical activities required by an individual as part of his or her routine daily tasks. These studies used various types of motion detectors as well as recall questionnaires. It is also worth noting that most children tend to overestimate the amount of physical activity they perform (17,18). There is at least some evidence that this is due to activity restrictions that have been imposed by physicians, parents, and in some cases by the children themselves (19). Obesity in this population mirrors that of the general pediatric population and occurs even in populations with otherwise excellent cardiac repair and normal or near normal exercise capacities (3,4,19). There is at least some evidence that the amount of obesity is related to daily amounts of physical activity (21). The intensity of physical activity can obviously vary greatly from individual to individual depending on the nature of their employment. Although this may seem obvious, the little research available would suggest that patients and physicians largely ignore this aspect of care. Of concern is the finding that the most common reason patients do not seek information about appropriate level of physical activities is a mistaken belief that all activities are safe to perform (22). Clearly, the intensity with which these leisure activities are performed may vary widely with the age and circumstances in which they are undertaken (13). This also highlights the importance of understanding the difference and intensity of sports at a recreational level as opposed to a competitive level. For example, intramural flag football has little in common with competitive high school football. Competitive Sports Competitive sports are those that are generally organized, coached, and played at high skill levels. The intensity with which an individual participates in competitive sports is influenced by their personal motivation as well as the outside influences of the coach, other team members, parents and other family members, as well as spectators. The end result is the potential for the individuals to push themselves to participate beyond the level they might otherwise choose to or which might be considered safe by their physician (12). For example, weight training and physical conditioning undertaken by high school athletes playing baseball may easily exceed the intensity of the activity they achieve in the actual game. It is also important to remember, as stated earlier, that "competitive" does not necessarily mean the same thing for all ages. None of the factors that influence high levels of performance in adolescents and adults, such as coaching and spectators, are likely to have much of an effect on young children. Especially at early ages, children are very unlikely to perform beyond a level that they would otherwise choose to self-limit. As such, these "competitive" sports should be thought of more as activities to teach basic physical skills rather than true competitive athletics (12,23). As will be discussed later in this chapter, this is a level of physical activity that is often achieved in recreational activity or in many cases through competitive sports and is both safe and desirable for many individuals with simple congenital heart defects. The need and the rationalization for these tests will be discussed for the individual defects. In patients with complex defects and residual cardiac dysfunction, studies from the adult heart failure literature suggest that they would still benefit from routine regular physical activity. However, these patients may need physical activity programs that are more specifically designed for their degree of cardiac fitness (25,26,27). This can be used to instruct the patient in the types and intensity of activities that are both safe and beneficial. All four factors should be included when generating an exercise prescription and address both activities with primarily dynamic and static components to assure optimal physical conditioning (28). Other cardiac diseases, including myocarditis, other cardiomyopathies, electrical abnormalities. Published reports have relied on public media, catastrophic insurance claims, the U. Young athletes participating in competitive sports had an estimated risk of sudden death approximately 2. As well, a recent nonforensic analysis of collegiate athletes found a frequency of 2. The American Academy of Pediatrics recently published guidelines for preparticipation screening, with the goal to "uncover conditions that might require further investigation or treatment" that would hinder the health and safety of the athlete (41). Treatment may include activity restriction, pharmacotherapy, electrophysiology studies and procedures, implantable cardioversion defibrillator placement, and in some cases, surgical repair. The limited value of history and physical examination alone was noted in a retrospective analysis of 115 high school and collegiate athletes who died suddenly.
Syndromes
- Injury to self or others caused by mental state (confusion/delirium)
- They still have foot problems after treatment
- Chronic unilateral obstructive uropathy
- Shortness of breath
- Fatigue
- Surgery to treat bleeding in some areas
- Chronic pain (rarely)
- Open brain surgery, called a posterior craniotomy
Buy cheap rogaine 2 60 ml online
Promotion of physical activity for children and adults with congenital heart disease: a scientific statement from the American Heart Association mens health 10 week challenge buy discount rogaine 2 online. Recommendations for physical activity, recreation sport, and exercise training in paediatric patients with congenital heart disease: a report from the Exercise, Basic & Translational Research Section of the European Association of Cardiovascular Prevention and Rehabilitation, the European Congenital Heart and Lung Exercise Group, and the Association for European Paediatric Cardiology. Physical activity, sports participation and aerobic fitness in children who have undergone surgery for congenital heart defects. Physical activity levels of school-age children with congenital heart disease in Taiwan. Aerobic exercise training intensity in patients with chronic heart failure: principles of assessment and prescription. Ventilatory efficiency and aerobic capacity predict event-free survival in adults with atrial repair for complete transposition of the great arteries. Prevalence of sudden cardiac death during competitive sports activities in Minnesota high school athletes. Sudden death in young adults: an autopsy-based series of a population undergoing active surveillance. Relationship of race to sudden cardiac death in competitive athletes with hypertrophic cardiomyopathy. Does sports activity enhance the risk of sudden death in adolescents and young adults Incidence of sudden cardiac death in National Collegiate Athletic Association Athletes. Recommendations and considerations related to preparticipation screening for cardiovascular abnormalities in competitive athletes: 2007 update: a scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism: endorsed by the American College of Cardiology Foundation. American Academy of Family Physicians, American Academy of Pediatrics, American College of Sports Medicine, et al. Prospective screening of 5,615 high school athletes for risk of sudden cardiac death. Efficacy of personal symptom and family history questionnaires when screening for inherited cardiac pathologies: the role of electrocardiography. Study Group of Sport Cardiology of the Working Group of Cardiac Rehabilitation and Exercise Physiology and the Working Group of Myocardial and Pericardial Diseases of the European Society of Cardiology. An electrocardiogram should not be included in routine preparticipation screening of young athletes. Sudden cardiac death and preparticipation screening: the debate continues-in support of electrocardiogram-inclusive preparticipation screening. A Scientific Statement from the American Heart Association and the American College of Cardiology. Normal electrocardiographic findings: recognizing physiologic adaptations in athletes. Abnormal electrocardiographic findings in athletes: recognizing changes suggestive of cardiomyopathy. Abnormal electrocardiographic findings in athletes: recognizing changes suggestive of primatery electrical disease. Relation of race to electrocardiographic patterns in elite American football players. Ethnic differences in left ventricular remodeling in highly trained athletes relevance to differentiating physiologic left ventricular hypertrophy from hypertrophic cardiomyopathy. Comparison of electrocardiographic criteria for detection of cardiac abnormalities in elite black and white athletes. Is there evidence for recommending electrocardiogram as part of the preparticipation examination Cost-effectiveness of preparticipation screening for prevention of sudden cardiac death in young athletes. Preparticipation screening of young competitive athletes for cardiovascular disorders. Ventilatory anaerobic threshold for evaluating exercise performance in children with congenital left-to-right intracardiac Shunt. Lower exercise capacity in children with asymptomatic atrial septal defect associated with circulatory impairment. Is it worth closing the atrial septal defect in patients with insignificant shunt Atlantoaxial instability in individuals with Down syndrome: epidemiologic, radiographic, and clinical studies. The value of cardiopulmonary exercise testing in individuals with apparently asymptomatic severe aortic stenosis: A pilot study. Postoperative exercise training develops normal levels of physical activity in a group of children following cardiac surgery. Exercise training in adults with congenital heart disease: feasibility and benefits. Sudden unexpected death after balloon valvuloplasty for congenital aortic stenosis. Usefulness of bicuspid aortic valve phenotype to predict elastic properties of the ascending aorta. Natural history of asymptomatic patients with normally functioning or minimally dysfunctional bicuspid aortic valve in the community. Muscular strength training is associated with low arterial compliance and high pulse pressure. Aortic root size and prevalence of aortic regurgitation in elite strength trained athletes. Self-estimated physical functioning poorly predicts actual exercise capacity in adolescents and adults with congenital heart disease. Long-term follow-up after aortic coarctation repair: the unsolved issue of exercise-induced hypertension. Prevalence and long-term predictors of left ventricular hypertrophy, late hypertension, and hypertensive response to exercise after successful aortic coarctation repair. Predictors of exaggerated exercise-induced systolic blood pressures in young patients after coarctation repair. Vascular dysfunction after repair of coarctation of the aorta: impact of early surgery. Functional and haemodynamic assessment of mild-tomoderate pulmonary valve stenosis at rest and during exercise. Improved exercise performance and quality of life after percutaneous pulmonary valve implantation. Impaired cardiac reserve in asymptomatic patients with moderate pulmonary restenosis late after relief of severe pulmonary stenosis: evidence for diastolic dysfunction. Physical activity intervention studies: what we know and what we need to know: a scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity); Council on Cardiovascular Disease in the Young; and the Interdisciplinary Working Group on Quality of Care and Outcomes Research. Recommendations for competitive sports participation in athletes with cardiovascular disease: a consensus document from the Study Group of Sports Cardiology of the Working Group of Cardiac Rehabilitation and Exercise Physiology and the Working Group of Myocardial and Pericardial Diseases of the European Society of Cardiology. Usefulness of cardiopulmonary exercise to predict long-term prognosis in adults with repaired tetralogy of Fallot. Biventricular response after pulmonary valve replacement for right ventricular outflow tract dysfunction: is age a predictor of outcome Effect of pulmonary artery angioplasty on exercise function after repair of tetralogy of Fallot. Right and left ventricular systolic function late after repair of tetralogy of Fallot. A pilot study of exercise training in adult patients with repaired tetralogy of Fallot. Habitual exercise correlates with exercise performance in patients with conotruncal abnormalities. Relation of systemic ventricular function quantified by myocardial performance index (Tei) to cardiopulmonary exercise capacity in adults after Mustard procedure for transposition of the great arteries. Failure of stroke volume augmentation during exercise and dobutamine stress is unrelated to load-independent indexes of right ventricular performance after the Mustard operation. The cardiologic status of youngsters and young adults after neonatal arterial switch operation with a simple transposition of big vessels. Exercise performance after the arterial switch operation for Dtransposititon of the great arteries. Follow-up outcomes 10 years after arterial switch operation for transposition of the great arteries: comparison of cardiological health status and healthrelated quality of life to those of the a normal reference population.
Rogaine 2 60 ml fast delivery
However androgen hormone ovulation proven rogaine 2 60ml, as stated above, the risks of physical activities in this group of patients are unknown. For the very rare patient with exceptionally good function who desires to participate in a recreational sport at a high level, comprehensive individual evaluation by their cardiologist should be undertaken prior to participation. Asymptomatic patients repaired by the arterial switch operation with only minor residual lesions and with no significant arrhythmias at rest or during exercise and no evidence of exercise-induced myocardial ischemia may participate in competitive sports without restrictions. Sports with a combined high dynamic and high isometric component are not contraindicated, but are discouraged. Their cardiologist may prescribe sports with low-dynamic and low- isometric components depending upon the residual lesions and the needs of the patient. There are insufficient data on the exercise performance after the so-called "double switch" operation. A maximal graded exercise test is useful to measure physical working capacity, aerobic capacity, chronotropic response, and presence of arrhythmias. This decision should be based on preparticipation evaluations and exercise testing. Frequent assessment of such patients is needed to assure safe participation in more vigorous activities. Diminished muscle bulk and function may also contribute to reduced exercise tolerance (167). This finding may reflect the limited ability of this physiology to maintain ventricular preload at higher heart rates (165). Energy loss through the Fontan circuitry due to turbulence may limit the ability to augment cardiac output with exercise (168,169). A significant decline in aerobic performance has been associated with onset of symptomatic heart failure and cardiac death or need for heart transplantation (27). A graded exercise test is extremely useful to measure aerobic and physical working capacities. Evaluating pulmonary function at rest and exercise may be quite useful in unmasking associated pulmonary abnormalities that may impact on exercise performance. On formal exercise testing, up to 25% to 30% of patients with Fontan physiology will have aerobic capacities within the range of normal for healthy age-matched peers. At the other extreme is a significant portion of patients with Fontan physiology who have quite limited exercise performance. Patients should be allowed to rest when fatigued, maintain adequate hydration, and avoid bodily collision if taking antithrombotic medication. Principle for Recreational Activities and Exercise Training in Children and Adolescents with Fontan Procedurea F. Ordinary physical activity does not cause undue dyspnea or fatigue, chest pain, or near syncope. Less than ordinary daily activities result in excessive dyspnea, fatigue, chest pain, or near syncope. Therefore, the recommendations of the Bethesda Conference restricting them from those activities are a reasonable default position (82). Because there are exceptional patients in this age range with normal exercise capacity, a case-by-case evaluation should be made for these patients who may wish to compete at higher levels of intensity. As previously mentioned, preadolescent patients with Fontan physiology may often have normal or near normal exercise capacity. Also, as discussed earlier in this chapter, the nature of competitive sports in this population is significantly different from that of adolescent and adult level sports. Some patients should not participate in competitive sports in which a risk of bodily collision could result in significant injury: Those patients taking antithrombotic medication and those who are pacemaker-dependent or have an implantable cardioverter/defibrillator. Class 2 patients are symptomatic with leisure activities and some activities of daily living. Even those patients who are Classes 1 and 2 may be at significant risk with physical activity. Evaluation Prior to Exercise and Sports Participation this population is at high risk for adverse events with exercise even if they are completely asymptomatic. Evaluation of exercise performance is very useful in both initial risk stratification and subsequent monitoring of disease progression and therapeutic interventions. Leisure Activities and Activities of Daily Living Because of the broad range of symptoms and the unpredictable risk of sudden death in many of these patients, it is very difficult to make any generalized recommendations regarding physical activity in this population. With rare exceptions, activity should be of low intensity and have both a low dynamic and P. This may initially need to be in a structured and monitored location rather than a home-based program. Many patients will have a marked improvement in the symptoms with onset of therapy. For this reason, the need to frequently reassess exercise capacity and recommendations in this population cannot be overemphasized (177). Principle for Recreational Activities and Exercise Training in Children and Adolescents with Pulmonary Hypertensiona F. Exercise capacity is often limited by both cardiac and peripheral factors (177,179). However, as stated above, these patients are at less risk for sudden drops in systemic cardiac output and blood pressure. Careful and frequent monitoring of exercise symptoms and capacity are still essential (177). Special circumstances may occur when participation in low static and dynamic sports may be considered on an individual basis for Class 1 patients. There are, however, no significant data that would allow accurate assessment of risk for an individual patient. Heart Transplantation Exercise capacity as measured by both aerobic capacity and musculoskeletal strength is significantly decreased in the pediatric population following heart transplantation. These values are not significantly different from those reported in the adult population. This may be due to systolic impairment but more importantly to diastolic dysfunction with high cardiac filling pressures. Abnormalities of autonomic innervation and function also impact on cardiac output during exercise. This significantly decreases chronotropic reserve and blunts the time course of the chronotropic response. Limitations of the peripheral exercising musculature are likely at least as important as central mechanisms in limiting aerobic capacity. This may reflect the marked deconditioning in these patients that occurs prior to transplantation but may also be the result of immunosuppressant therapy. Use of ongoing immunosuppressant medications may continue to exacerbate the problem of demineralization. Serial studies of exercise performance following pediatric heart transplant are limited. The reason for these discrepant findings are unclear but are probably the combined improvement of systolic and especially diastolic function in the immediate posttransplant period as well as the longer-term improvement in musculoskeletal conditioning, even in the absence of formal rehabilitation. There are no significant data on the risks and benefits of exercise training in pediatric heart transplant recipients. Studies in adults consistently show significant improvement in maximal aerobic capacity. There is also some evidence from small studies that suggest that high-intensity interval training is more effective in this population than prolonged moderate intensity training (187,188,189,190,191,192). Principle for Recreational Activities and Exercise Training in Children After Heart Transplantation without Coronary Artery Disease F. Exercise aims at correct technique and breathing pattern to avoid the Valsalva maneuver. They should be evaluated for physical activity by physicians and healthcare providers who have specialized knowledge in this area. These children usually benefit from exercise testing and a thorough physical therapy evaluation. Often a structured rehabilitation program that transitions to a home activity program is desirable for patients immediately after cardiac transplant. Leisure Activities and Activities of Daily Living There are no evidence-based studies assessing the types, safety, or benefit of sports and exercise participation in children following heart transplantation. In a very small interview study of mixed solid organ transplant patients, Olausson et al. They stated, "physical rehabilitation and return to normal lifestyle has been nearly 100%.
Purchase discount rogaine 2 on-line
Cardiac involvement can include myocarditis mens health survival of the fittest buy cheap rogaine 2 60 ml on-line, coronary arteritis, endocarditis, and valvular disease. A wide spectrum of renal manifestations can occur, varying from minimal change disease to proliferative glomerulonephritis and rapidly progressive crescentic glomerulonephritis. Gastrointestinal complaints can be a symptom for aphthae throughout the gastrointestinal tract and can rarely result in perforation and peritonitis (0. Significant neurologic manifestations occur in approximately 10% of patients and may be delayed in onset. Meningoencephalitis, cerebral venous sinus thrombosis, benign intracranial hypertension, cranial nerve palsies, brainstem lesions, and pyramidal or extrapyramidal lesions have been described. Poor prognosis is associated with a progressive course, relapses after treatment, repeated attacks, and cerebellar symptoms or parenchymal disease. Further symptoms include gait disturbance, dysar- thria, vertigo, and diplopia as well as hyperreflexia, epileptic seizures, hemiplegia, ataxia, or a positive Babinski reflex. Psychiatric symptoms, such as depression, insomnia, or memory impairment, are also signs of neurologic involvement. Biopsies from early mucocutaneous lesions show a neutrophilic vascular reaction with endothelial swelling, extravasation of erythrocytes, and leukocytoclasia or a fully developed leukocytoclastic vasculitis with fibrinoid necrosis of blood vessel walls. The neutrophilic vascular reaction should be considered the predominant histopathologic finding. Broader pathergy phenomena also include the occurrence of aneurysms around vascular anastomoses as well as local recurrence of ulcers after resection of affected bowel segments. Blindness can often be prevented with early aggressive therapy of posterior uveitis. Lethal outcome has been seen in 0 to 6% of affected patients in different ethnic groups. Central nervous system and pulmonary and large vessel involvement, as well as bowel perforation, are the major life-threatening complications; death may also result as a complication of immunosuppressive therapy. Spontaneous remissions of certain or all manifestations of the disease have been observed. Ophthalmic and neurologic sequelae are leading causes of morbidity, followed by severe vascular and gastrointestinal manifestations, and their effects on morbidity may be cumulative. Electroencephalographic detection of diffuse -waves is considered a positive finding. There can be a delay of up to several years before the diagnosis is made, and this may influence the prognosis. Recurrent aphthae are most often treated with palliative agents, such as mild diet, avoidance of irritating agents, and potent topical glucocorticoids and local anesthetics,48,49 lately topical hyaluronic acid 0. They can also be beneficial on panuveitis and cystoid macular edema as a single intravitreal injection (triamcinolone acetonide 4 mg). Additional treatments have been successful in studies with a lower grade of evidence (eBox 166-3. A synergistic effect with cyclosporine A has been described in patients with ocular involvement. A rapid relapse often occurs after discontinuing cyclosporine A, interferon-, dapsone or infliximab. Ann Rheum Dis 68:1528, 2009 2042 Section 28:: the Skin in Inflammatory and Other Vascular Disorders Chapter 167:: Kawasaki Disease:: Anne H. Major symptoms are prolonged high fever, conjunctival injection, oral mucosal changes such as red lips and pharynx and strawberry tongue, redness and swelling of the hands and feet, erythematous polymorphic rash, and cervical lymphadenopathy. Inflammation in the coronary arteries can lead to aneurysms with subsequent myocardial infarction, aneurysm rupture, and sudden death. Long-term complications are confined to the heart and vascular tree, primarily thrombosis and stenosis of the major coronary arteries with myocardial ischemia. About 25% of untreated children develop coronary artery abnormalities, including dilatation and aneurysms that can lead to myocardial infarction and sudden death. However, incomplete forms of illness are well-recognized, in which a child manifests prolonged fever with fewer than four other clinical features of the illness and subsequently develops coronary artery abnormalities. The existence of these incomplete forms of illness results in a major diagnostic dilemma for physicians in establishing the diagnosis accurately in children with prolonged fever of uncertain cause. Tomisaku Kawasaki, a Japanese pediatrician who first recognized the clinical features of the illness. Oral mucosal changes, including red, dry, cracked lips, pharyngeal erythema, and/or strawberry tongue 3. Changes of the hands and feet: erythema of palms and soles and/or swelling of the hands and feet during the acute phase, and/or periungual desquamation of the fingers and toes during the subacute phase 4. Genetic predisposition is a common theme in susceptibility and host response to infectious diseases. Immune complexes, although detectable in serum in the subacute phase, are not deposited in tissues and do not appear to play a prominent role in pathogenesis. Kawasaki described the illness in the English-language literature in 1974; this report was closely followed by a description of the same illness, observed independently in the early 1970s in Hawaii by Dr. Therefore, it is important to query parents and physicians who saw the patient during the course of a prolonged febrile illness as to the presence of the other five clinical features of the illness: (1) conjunctival injection, (2) oral mucosal changes, (3) changes of the hands and feet, (4) rash, and (5) cervical adenopathy. Bullae, vesicles, and ulcerative lesions are not observed, but a fine micropustular rash, especially on the extensor surfaces, occasionally occurs. In the acute febrile phase of illness, groin erythema and desquamation are commonly observed. The skin changes in the groin can be seen both in children in diapers and toilet-trained children. Classic periungual desquamation of the fingers and toes does not begin until the second to third week after fever begins, and can progress to involve the entire hand and foot. In the third to sixth week after illness, transverse lines across the fingernails (Beau lines) are often apparent. Palmar and plantar erythema is a common feature, and there can be an abrupt transition from marked erythema to normal skin at the wrists and ankles. In particular, arthritis can occur during the acute febrile phase, involving the small interphalangeal joints and larger joints, or may occur during the subacute phase of illness, usually involving the larger joints such as the knees and ankles. Patients with anemia and low albumin levels may be at higher risk of developing coronary artery disease. Gallbladder hydrops, with accompanying right upper quadrant abdominal pain, resolves spontaneously and does not require surgical intervention. Some centers perform an additional echocardiogram at 1 year after onset, but it is rare to find any evidence of coronary artery abnormalities at 1 year that were not present within the first two months after fever began. In areas where measles is still prevalent, differentiating the two disorders can be difficult. Later in the course of measles infection, the rash becomes diffuse and Koplik spots are no longer visible.