Bisoprolol 10mg line
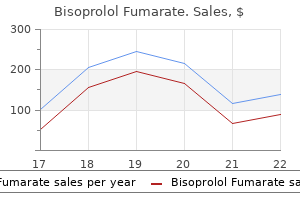
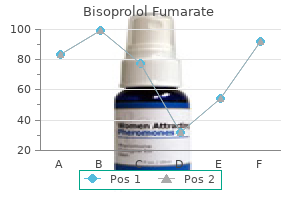
The peak ratings of breathlessness and regression slope of breathlessness as a function of oxygen consumption were significantly higher with naloxone than normal saline arrhythmia gerd buy bisoprolol overnight delivery. All nine studies on systemic opioids and three out of nine nebulized opioid studies were recruited for meta-analysis. The strongest evidence was shown by a double-blind controlled trial by Abernethy et al. Participants of the morphine arm reported significant improvement in dyspnoea scores and sleep. In patients who are already taking opioids for pain control, an increment of 25% of the baseline dosage is supported by one previous study (Allard et al. The use of fast-acting opioids such as oral transmucosal fentanyl requires further study. Communication with patients and families on the indication and adverse effects of opioids is important for an informed choice and to address myths and concerns. The dose of morphine was 10 mg daily for 70% of participants, and the benefit was maintained at 3 months in 33% of all patients. There were no episodes of respiratory depression or hospitalizations as a result of the sustained-release morphine. The authors concluded that sustained-release oral morphine 10 mg once daily is safe and effective for most people. While all patients and family caregivers preferred to continue opioids, most physicians were reluctant to prescribe opioids for refractory dyspnoea. There is limited evidence to support the use of nebulized opioids for controlling breathlessness. The evidence for using opioids for controlling breathlessness in chronic heart failure is conflicting and requires further study. The use of opioids for breathlessness in other life-limiting illnesses such as interstitial lung disease and motor neurone disease are based on anecdotal reports. There is no universally agreed starting dosage of opioids for the control of breathlessness. However, there were reports of successful use of benzodiazepines for the control of breathlessness in people with cancer with or without anxiety. One study reported the effective use of subcutaneous midazolam as adjunct therapy to morphine in the alleviation of severe dyspnoea in people in the last hours or days of life (Navigante et al. In another study, 63 patients were randomized to either oral morphine (starting dose 3 mg) or oral midazolam (starting dose 2 mg) with stepwise titration according to level of dyspnoea in initial in-clinic phase for recent acute onset breathlessness while causes were being investigated. In the subsequent 5 days of ambulatory phase, midazolam was superior to morphine in controlling baseline and breakthrough dyspnoea (Navigante et al. In another prospective, non-randomized study among people with cancer with dyspnoea associated with anxiety, a combination of morphine with lorazepam was shown to be effective in decreasing respiratory rate and dyspnoea intensity, without causing respiratory depression (Clemens et al. There may be a role for benzodiazepines for dyspnoea that is associated with anxiety. While the role of benzodiazepines in relieving breathlessness requires further evaluation, benzodiazepines are widely used (Booth et al. Inhaled furosemide Multiple mechanisms are proposed for the effects of inhaled furosemide in relieving breathlessness, including enhanced pulmonary receptor activity, suppression of the pulmonary irritant activity and vasodilation (Newton et al. Studies performed in people with cancer included one open clinical trial and one case series. A collaborative approach between respiratory team and palliative care team is essential. Inhaled furosemide may exert its effect on the airway and be useful in relieving dyspnoea due to airway diseases, but is not proven to be of benefit for breathlessness in cancer which involves multiple mechanisms. Heliox Helium has a low density and the potential of reducing the work of breathing and improving alveolar ventilation when nitrogen in air is replaced by helium. However, its cost and availability will continue to limit its use in clinical practice. Agitated delirium, dyspnoea, and pain were the most common indications for palliative sedation. The management of depression is an important component in managing patients with chronic dyspnoea. Likewise there is insufficient evidence to support the use of indomethacin and inhaled topical anaesthetics to relief dyspnoea (Parshall et al. Cough can cause physical complications including chest wall pain, fracture of ribs, urinary incontinence, sweating, exhaustion, and disturbance of sleep. Patients may also experience psychological impacts, social embarrassment, and isolation (Molassiotis et al. Conditions with hypersecretion of mucus are associated with cough (see section on airway secretion). Cough reflex protects the airway by clearing the inhaled materials, accumulated airway mucus secretion, and sputum. The efficiency of cough depends on the optimal function of the three phases of cough, mucus properties, and mucociliary clearance all of which may be affected in cancer or chronic lung diseases. Coughing effort is reduced in respiratory muscle weakness or mechanical disadvantage as in general debility, cachexia, steroid myopathy, gross ascites, or hepatomegaly, and neurological conditions affecting conscious level. Dynamic compression of the airway is affected by vocal cord paralysis, presence of tumour, and stent insertion. Changes in mucus properties occur in chronic inflammation or infection of the lungs and dehydration. Assessment of cough in palliative care Despite the prevalence of cough and its appearance with other symptoms such as dyspnoea, insomnia, and fatigue in symptom clusters (Chen et al. A validated tool for cough for systematic assessment in palliative care is lacking (Molassiotis et al. The clinical approach in cough assessment aims at evaluation of the cough symptom and the possible underlying causes. History, physical examination, and chest radiograph remain the mainstay in elucidating the underlying causes of cough. The characteristics of cough should be defined from history taking, including associated sputum production, precipitating factors such as smoking, irritants, drugs, feeding, posture, association with timing of the day, and other associated symptoms such as dyspnoea, insomnia, choking, or fatigue. Cough-specific quality of life (EuroQol) questionnaires have been validated for assessing the impact of cough, such as the Leicester Cough Questionnaire, Cough Quality of Life Questionnaire, Burden of Cough Questionnaire, and Lung Cancer Cough Questionnaire (Molassiotis et al. In patients with suspected aspiration or who fail the bedside swallowing test, referral to a speech therapist for comprehensive assessment should be considered. The C fibres are non-myelinated fibres activated by capsaicin, bradykinin, protons (acid pH), but C-fibre dependent cough is prevented by anaesthesia. Unlike C-fibre dependent cough, the cough receptor-dependent cough is not inhibited by general anaesthesia. It appears to be protective by evoking robust cough efforts in response to touch and acid (Canning, 2011). Higher cortical involvement is suggested by the phenomenon that the urge to cough can be voluntarily suppressed and placebo has a profound effect on cough. Causes of cough in palliative care Tumours are more likely to cause cough with involvement of airways than the lung parenchyma (Kvale, 2006). Cancer involvement of pleura, pericardium, mediastinum, pulmonary lymphatics, and blood vessels may cause cough, and airway hypersecretion is associated with chest infection or inflammation. People with advanced cancer are predisposed to swallowing problems and aspiration Management of cough in palliative care Evidence for cough treatment in advanced cancer has been disappointing, and the approach to cough in palliative care and lung cancer is formulated based on expert consensus and limited evidence (Molassiotis et al. There is also no evidence to support efficacy of nurse-led management (Yorke et al. Treatment for cancer related causes Radiotherapy, chemotherapy, especially with gemcitabine, and endobronchial treatment may palliate cough due to tumours (Kvale, 2006). Data on cough relief by brachytherapy, laser, or photodynamic therapy are limited (Molassiotis et al. Steroids may be useful in reducing tumour-related oedema, airway obstruction, lymphangitis carcinomatosis, or radiotherapyor chemotherapy-induced pneumonitis. A steroid trial may be recommended as an early step in the treatment pyramid for cough in lung cancer after considering disease-specific treatments (Molassiotis et al. Antimicrobial treatment is indicated for chest infections but its outcome may be poor in the presence of drug-resistant pathogens and frail patients especially near the end of life.
Cheap bisoprolol amex
A different type of malabsorption that can be seen in palliative care patients treated with antibiotics heart attack vegas purchase discount bisoprolol on-line, or as a complication of gut infection such as Clostridium difficile, is lactose intolerance secondary to changes in the intestinal flora. This will gradually correct itself but meanwhile a lactose-free diet produces prompt resolution of the diarrhoea (Noble at al. If less than 100 cm of terminal ileum is removed, fat malabsorption generally does not occur, as the liver can compensate for the increased biliary loss. A resection of over about 100 cm results in relative bile acid deficiency and hence fat malabsorption, exacerbating the diarrhoea. Ileal resection also produces a disaccharidase deficiency proportional to the length of removed and thus an osmotic diarrhoea due to carbohydrate malabsorption. Such patients require an average of an extra litre of water per day and about 7 g of extra salt to compensate, with special care needed in hot weather. Similar symptoms can also result from an enterocolic fistula, caused either by cancer or as a result of operation (Mercadante, 1992). Alteration of gut anatomy by surgery may also promote diarrhoea through bacterial overgrowth. A colonic or rectal tumour can precipitate diarrhoea through causing partial intestinal obstruction, or loosen stools through increased mucus secretion. Apart from concurrent gastrointestinal disease, the ability of dietary factors to cause diarrhoea should be remembered. Excessive dietary fibre may produce diarrhoea and fruits may do so both by this means and by their content of specific laxative factors. Assessment Malabsorption sufficient to cause diarrhoea may occur in carcinoma of the head of the pancreas or after gastrectomy or ileal resection. Failure of pancreatic secretion leads to reduced fat absorption and consequent steatorrhoea. Gastrectomy can also produce steatorrhoea, presumably as a result of poor mixing of food with pancreatic and biliary secretions. However, the accompanying vagotomy causes increased faecal secretion of bile acids A complaint of diarrhoea demands a careful history, detailing first of all the frequency of defecation, the nature of the stools, and the time course of the problem. Profuse watery stools are characteristic of colonic diarrhoea, whereas the pale, fatty, offensive stools of steatorrhoea indicate malabsorption due 10. The sudden advent of diarrhoea following a period of constipation, perhaps with little warning of impending defecation, should raise the suspicion of faecal impaction. If laxatives are to blame, the error may be of insufficiently regular therapy, resulting in alternating constipation and diarrhoea, or an excessive dose. Too much of a predominantly peristalsis-stimulating laxative tends to produce colic and urgency, and too much of a predominantly stool-softening agent may cause faecal leakage, although at high doses lactulose and docusate have the ability to produce colic and watery diarrhoea in some patients. The occurrence of pyrexia, blood in the stools, or dehydration as features of diarrhoea should be watched out for, as they signal the presence of potentially life-threatening complications and the need for more intensive support and intervention. In a palliative care context this situation is principally likely to arise as a result of recent cytotoxic chemotherapy. Diarrhoea in the presence of neutropenia should suggest the presence of neutropenic enterocolitis in which mucosal ulceration occurs, allowing bacterial and fungal invasion and consequent septicaemia as well as the possibility of intestinal perforation. Although there is evidence that stricter antibiotic and hospital hygiene policies are slowing the rate of rise in incidence, Clostridium difficile diarrhoea is still common and may be life-threatening unless diagnosed and treated with appropriate antimicrobials as directed by stool sample analysis. Proprietary rehydration solutions, containing appropriate electrolyte concentrations and a source of glucose to facilitate active electrolyte transport across the gut wall, are adequate for all but the most severe diarrhoea. Any diarrhoea will benefit from a diet of clear liquids, such as flat lemonade or ginger ale, and simple carbohydrates, as in toast or crackers. Some infective causes of diarrhoea cause transient lactase deficiency and so milk should be avoided in these circumstances (Noble et al. Protein and, later, fats are reintroduced gradually to the diet as the diarrhoea resolves. Neutropenic colitis may also involve fungal infection, principally by Candida spp. Management may also entail administration of granulocyte colony-stimulating factor or resection of the affected bowel (Ullery et al. Examination and investigations Examination should exclude the possibilities of faecal impaction and intestinal obstruction, and should therefore include rectal examination and abdominal palpation for faecal masses. If there is doubt, an abdominal radiograph will make the distinction, but this is rarely necessary. Steatorrhoea is generally clearly suggested in the history and readily confirmed on examination of the stool. Persistent watery diarrhoea, without systemic upset, which would suggest an infective cause, may be more difficult to diagnose. If in doubt, the stool osmolality and sodium and potassium concentrations should be measured. The anion gap, the difference between the stool osmolality and double the sum of the cation concentrations, is over 50 mmol/L in osmotic diarrhoea, because of the presence of an additional non-absorbed solute, for example, a disaccharide from a medicinal elixir. Ileal resection gives rise to a mixed picture, which will become purely secretory if the patient can be fasted. Diarrhoea occurring within 3 days of inpatient admission may be due to community-acquired bacterial enteric pathogens such as Salmonella, Shigella, or Campylobacter, or to viral infection. After this point the infection is likely to have originated in the inpatient unit and stool culture is usually unrewarding; repeating the culture does not improve the diagnostic yield (Chitkara et al. Clostridium difficile is the most commonly detected cause of nosocomial diarrhoea and is associated with antibiotic treatment, particularly quinolones or cephalosporins. It affects predominantly the over 65 age group, in whom its incidence in the United States more than doubled between 2000 and 2005 (Lessa et al. This rise has been accompanied by an increase Specific treatment Specific treatments exist for several causes of diarrhoea. Pancreatin is a combination of amylase, lipase, and protease, which is available in several forms for pancreatic enzyme replacement. The effective dose varies widely between individuals and it may be more effective if gastric acidity is reduced with an H 2-receptor antagonist, in which case enteric-coated preparations should not be used. Cholestyramine is a bile acid-binding resin that is effective in controlling chologenic diarrhoea provided ileal resection has not been too extensive. Sulfasalazine appears in clinical practice guidelines for prophylaxis of radiation-induced diarrhoea (Rubenstein et al. Carcinoid syndrome diarrhoea often responds to general antidiarrhoeals, but peripheral serotonin antagonists, such as methysergide or the less toxic cyproheptadine, have been used against more severe diarrhoea and, sometimes, the accompanying malabsorption. Subcutaneous injection of octreotide may be painful, but continuous subcutaneous infusion is generally well tolerated and the drug can be combined with morphine, diamorphine, haloperidol, midazolam, or hyoscine without apparent loss of efficacy (Riley and Fallon, 1994). Expert consensus has recommended octreotide dose titration as high as 1500 micrograms/24 hours for chemotherapy-induced diarrhoea (Benson et al. Lanreotide has a far more prolonged duration of action and so requires neither frequent injections nor an infusion device, but is also less flexible for use in the continually changing clinical situations of palliative care. Metronidazole remains the first-line antibiotic for Clostridium difficile diarrhoea, and can reasonably be tried also in situations where diarrhoea is suspected to be due to bacterial overgrowth, where it may produce a prompt resolution. General treatment Non-specific antidiarrhoeal agents are numerous, but are either absorbent, adsorbent, mucosal prostaglandin inhibitors, opioids, or somatostatin derivatives. These agents may make illness due to Shigella and Clostridium difficile worse and so should be used with caution if these organisms are known to be present, or if there is blood in the stool, or fever. Absorbent agents absorb water to form a gelatinous or colloidal mass that gives a thicker consistency to loose stools. Bulk-forming agents may have a delay of up to 48 hours in onset of antidiarrhoeal action and are poorly tolerated in ill patients. They have proved useful in the management of colostomies but exacerbate electrolyte loss from ileostomies. The use of pectin is time-honoured and there is some evidence of effectiveness in children (de la Motte et al. Adsorbent agents non-specifically take up dissolved or suspended substances, such as bacteria, toxins, and water, on to their surfaces. Attapulgite has been shown to be better than placebo in acute diarrhoea although significantly less effective than loperamide (DuPont et al. Kaolin is often combined with morphine as an antidiarrhoeal mixture and there is no evidence for efficacy separate from that of the opioid.
Diseases
- Dandy Walker malformation with mental retardation, macrocephaly, myopia, and brachytelephalangy
- Hyperlipoproteinemia type I
- Aggressive fibromatosis
- Microcephaly developmental delay pancytopenia
- Billard Toutain Maheut syndrome
- Usher syndrome, type 3
- Peanut hypersensitivity
- Trichomoniasis
- Mucolipidosis type 4
Purchase bisoprolol 10 mg mastercard
A recent Cochrane systematic review concluded that drugs absorbed from the gastrointestinal tract appeared to be more effective than drugs not absorbed from the gastrointestinal tract (Worthington et al arrhythmia chest pain discount bisoprolol online. It should be noted, however, that the evidence for the effectiveness of individual antifungal drugs in treating cancer patients is somewhat limited (Worthington et al. The choice of treatment depends on a number of factors (Finlay and Davies, 2005): 1. Extent of disease: topical agents are appropriate for treating localized disease, whilst systemic agents are more appropriate for treating multifocal/generalized disease. Immunocompetence: systemic agents are more appropriate for treating immunosuppressed patients than topical agents. Drug resistance: resistance to the polyenes is uncommon, although resistance to the azoles is becoming increasingly common. Concomitant disease: the azoles have a number of relative/absolute contraindications, which may limit their usage. Concomitant drug treatment: the azoles have a number of drug interactions, which may limit their usage. Patient adherence with medication: topical agents are associated with greater non adherence than systemic agents. Denture-related problems Denture-related problems are again common in patients with advanced cancer. Suitable for treating pseudomembranous candidosis, denture stomatitis and angular cheilitis Miconazole is also active against staphylococci, which may be present in some cases of angular cheilitis Drug needs to be kept in contact with lesions. Denture-related fungal infections are also common in patients with advanced cancer. Oral care in terminal phase Oral care often takes prominence during the terminal phase of the illness. However, the oral care protocols in these pathways are not evidence based, and are reported to produce somewhat disappointing outcomes (Fowell et al. This is very obtrusive for patients (and families), and very time consuming for health-care professionals. Some patients may require this frequency of care, although many patients require much less frequent care, to maintain oral comfort. Thus, the frequency of oral care should be determined on an individual basis, rather than on the basis of a protocol. Some family members relish this task, whilst others find it difficult and/or distressing. It is important, if appropriate, that families are given the opportunity to provide oral care. Furthermore, health-care professionals must provide adequate instructions, and ongoing support and supervision, for families that do undertake this task. One of the most common problems amongst unconscious patients is the presence of a desiccated oral mucosa. Family members (and health-care professionals) often perceive this as a source of discomfort, although this is unlikely to be the case in an unconscious patient. However, this strategy is largely ineffective, since the water rapidly dissipates as a result of swallowing and/ or evaporation. A more effective intervention involves the regular application of a suitable water-based moisturizing gel. The philosophy of care in the terminal phase should be the maintenance of patient comfort (Sweeney, 2005). Thus, health-care professionals should always ask patients about their experiences of oral care, that is, whether the oral care makes them feel better, whether the oral care causes any problems. Nevertheless, it is much less easy to determine the merits of oral care in unconscious patients. However, if an intervention causes or appears to cause distress, then that intervention should be discontinued. Comparison between saliva stimulants and saliva substitutes in patients with symptoms related to dry mouth. A comparison of artificial saliva and chewing gum in the management of xerostomia in patients with advanced cancer. An Investigation into the Relationship Between Salivary Gland Hypofunction and Oral Health Problems in Patients with Advanced Cancer. Objective and subjective efficacy of saliva substitutes containing mucin and carboxymethylcellulose. Physical and psychosocial impact of xerostomia in palliative cancer care: a qualitative interview study. Comparison between saliva stimulants and a saliva substitute in patients with xerostomia and hyposalivation. Clinical trial of a mucin-containing oral spray for treatment of xerostomia in hospice patients. Measuring the symptom experience of seriously ill cancer and noncancer hospitalized patients near the end of life with the Memorial Symptom Assessment Scale. Interventions for treating oral candidiasis for patients with cancer receiving treatment. A comparison of artificial saliva and pilocarpine in the management of xerostomia in patients with advanced cancer. Parasympathomimetic drugs for the treatment of salivary gland dysfunction due to radiotherapy. A comparison of artificial saliva and pilocarpine in radiation-induced xerostomia. Insomnia is the most prevalent sleep disorder and can become a persistent problem for patients with serious or life-threatening illnesses. The burden of chronic sleep disturbances is heavy for patients, caregivers, and health-care providers and its impact can affect physical, psychological, occupational, and economic well-being (Morin and Benca, 2012). Assessment and management of sleep disorders is necessary when treating chronically ill patients. Sleep is generated by two opposing processes that interact together to strengthen sleep: the homeostatic drive for sleep and the circadian system that regulates wakefulness (Borbely and Achermann, 1999;Kryger et al. The homeostatic drive for sleep involves mutually inhibitory interactions between sleepand arousal-promoting systems and increases with the length of time that an individual has been awake. The circadian system is known as the wake-promoting system because it determines the timing of sleep propensity and wakefulness (Borbely and Achermann, 1999). Individuals who sleep in phase with their circadian rhythm obtain a better quality of sleep, with minimal time to fall asleep and fewer awakenings, than those who sleep outside of their circadian chronotype. The central pacemaker of the circadian system for all physiological processes (including the modulation of sleep and wakefulness) is located in the suprachiasmatic nucleus of the hypothalamus. A complicated neural pathway links the suprachiasmatic nucleus to the pineal gland, where melatonin is secreted in a circadian pattern with onset of the secretion in the early evening, peak levels occurring in the middle of the night, and very low or non-existent melatonin levels during the day. In the mammalian circadian system, melatonin serves as a chemical messenger of the circadian pacemaker. Central melatonin receptors are concentrated primarily in the suprachiasmatic nucleus, where melatonin functions in a feedback loop (Borbely and Achermann, 1999). Sleep physiology Sleep is a state that shows alternating patterns of neural activity controlled by homeostatic and circadian mechanisms interacting in complex ways. Sleep architecture varies widely from person to person in terms of the amount of time spent in each sleep stage, the number of cycles, and the amount of interruption by waking. There are individuals who, because of their circadian Prevalence of sleep disorders the reported prevalence of sleep disturbances depends on the definitions used and the underlying pathology (Roth, 2007). A general consensus has emerged from population-based studies that approximately 30% of adults report one or more of the symptoms of insomnia: difficulty initiating sleep, difficulty maintaining sleep, waking up too early, and, in some cases, non-restorative or poor quality sleep (Roth, 2007). Clinicians caring for patients with serious illness should have a stronger foundation in at least those disorders for which medically ill patients often seek care-insomnia, excessive daytime sleepiness, obstructive sleep apnoea syndrome, and restless legs syndrome.
Discount 10mg bisoprolol fast delivery
The effect of intravesical instillations can be maximized with urinary diversion (percutaneous nephrostomy tubes and ureteral occlusion) in order to minimize the effects of urokinase heart attack under 30 10 mg bisoprolol with mastercard, a clot inhibitor present in urine (Sneiders and Pryor, 1993; Zagoria et al. An alternative to intravesical agents in the treatment of haematuria from a malignant source includes radiation therapy. In one study, up to 59% of patients with advanced bladder cancer had resolution of haematuria and 73% had pain reduction after case of stricture, balloon dilation or laser endoureterotomy are reasonable options (Banner and Pollack, 1984). Intractable haematuria Intractable haematuria in the palliative care patient can be difficult to control and may be life-threatening (see also Chapter 8. Depending on the source of bleeding, symptoms can be painful or painless, accompanied by lower urinary tract symptoms, clot retention, or infection. If untreated, patients will continue to have anaemia requiring frequent transfusions, clot retention, and secondary obstructive uropathy, and eventually haemorrhagic shock and death. Risk factors in this population include bleeding diatheses due to impaired synthetic function, anticoagulant medication, and poor wound-healing ability. Management depends on the aetiology and location within the upper or lower urinary tract (Garber and Wein, 1989). For upper urinary tract bleeding involving the kidneys or ureters, sources include renal cell carcinoma, urothelial carcinoma, arteriovenous malformation, angiomyolipoma, haemorrhagic cysts, or metastatic disease. While rare, upper urinary tract communications with nearby vessels (ureterovascular, pyelovascular, and renovascular fistulae) can cause brisk bleeding and require quick intervention with transfusion, and angioembolization. Ureterovascular fistulae, although rare, occur with risk factors that are more common in the palliative care population, such as chronic ureteral stents, vascular stents, significant atherosclerosis, arterial aneurysms, or history of radiation. Renovascular or pyelovascular fistulae are usually iatrogenic after percutaneous kidney surgery. The clinician must have a high level of suspicion in order to detect this pathology, as presentation and diagnostic studies can be elusive. If the bleeding source is localized to a lesion in the collecting system, then ureteroscopy and endoscopic fulguration with or without excision is a reasonable approach. If bleeding recurs despite endoscopic treatment or if the source of bleeding is not amenable to endoscopic fulguration, then selective arterial embolization is recommended. In the setting of life-threatening haemorrhage, haemodynamic stabilization and blood transfusion should be followed quickly by angiography with selective arterial embolization. Surgical exploration to control bleeding is an option if endovascular embolization is not possible. For bleeding renal masses that cannot be managed endoscopically or endovascularly, palliative nephrectomy or nephroureterectomy could be considered in very select patients. For ureterovascular fistulae, control of the communicating vessel can be achieved by endovascular stenting, open reconstruction, embolizing, or ligating with or without arterial bypass (Rovner, 2012). Consideration must be taken for infection due to urine contamination, and treated as needed. Control of the urinary tract can be achieved via urinary diversion, least invasive of which would be placement of a nephrostomy tube with 8. Reprinted from the Journal of Urology, Volume 174, Issue 4, Part 1, Joon-Ha Ok et al. In another study, complete palliation of locally advanced bladder cancer was found in 43% of patients (Salminen, 1992). Although bladder and bowel complications are possible, radiation therapy is generally well tolerated. Chemotherapy has not been as well studied for palliation of pain or bleeding in advanced bladder cancer. If conservative methods fail, embolization or surgical ligation of hypogastric arteries may be required. Palliative cystectomy with urinary diversion such as an ileal conduit should only be considered if all other options have failed or are not feasible, as it is the most invasive treatment associated with the greatest morbidity. Surgical diversion with an ileal conduit or formal fistula repair are more involved and only appropriate in select patients. For vesicoenteric fistulas, a diverting colostomy or the use of rectal stents may temporize symptoms (Harford et al. Depending on the severity of the fistulae, conservative measures may or may not alleviate symptoms. Pelvic and bladder pain Pelvic and bladder pain can cause significant distress with symptoms of suprapubic pressure, urgency, or dysuria. Diagnostic work-up includes drawing a urinalysis and culture, pelvic exam, imaging with X-ray and ultrasound to evaluate for obstructing urolithiasis or bladder stones. Cystoscopy can be performed to identify an intravesical mass, bladder stone, or fistula. If the patient has a known malignancy as the source of pelvic pain, extensive work-up may be unnecessary. Invasive pelvic masses cause pain due to the loss of bladder capacity and compliance, leading to high filling pressure, urgency, frequency, incontinence, and infection. Extrinsic compression on the bladder can cause similar lower urinary tract symptoms. Initial treatment includes placement of a urethral catheter to facilitate drainage. Ongoing bladder pressure and spasms despite drainage could be treated with analgesics, antimuscarinic medication, or belladonna and opium suppository. Urinary diversion with nephrostomy tubes could further alleviate symptoms of voiding dysfunction; however, it may not address pain from mass effect. Neuropathic pain caused by mass compression onto the lumbosacral plexus can be treated medically with analgesics, antidepressants, or antiepileptics (Jaeckle et al. Symptoms of fistulae involving the urinary tract include pneumaturia, urinary tract infection, suprapubic pain, and incontinence. Untreated, these symptoms lead to rash, skin breakdown, ulcers, chronic infection, and sepsis. Goals of palliative management of urinary fistulas include symptom management and containment of urinary leakage. Palliative percutaneous and endoscopic urinary diversion for malignant ureteral obstruction. Palliative treatment of intractable hematuria in context of advanced bladder cancer: a systematic review. Infection Control: Prevention of Healthcare-Associated Infections in Primary and Community Care. Types of urethral catheters for management of short-term voiding problems in hospitalized adults: a short version Cochrane review. Percutaneous nephrostomy drainage in the treatment of severe hemorrhagic cystitis. Radiation, chemotherapy, or surgery is appropriate in very select patients, to reduce the size of the mass. Transurethral resection of invasive prostatic or bladder malignancy could be considered as well. Alternative treatment of pain from cystitis includes oral pentosan polysulphate sodium (Elmiron). Intravesical agents include dimethyl sulphoxide, heparin, and hyaluronic acid, which have variable success. Management of haematuria related to radiation cystitis is addressed earlier in this chapter. Selection of tests and treatment modalities should be based on using the least invasive means to achieve the most relief in suffering. Some genitourinary conditions in this setting are potentially fatal, such as urinary tract haemorrhage and renal failure, and in the acute or subacute setting, require re-evaluation of the end-of-life goals and wishes of the patient and family. Initial experience with full-length metal stent to relieve malignant ureteral obstruction. High failure rate of indwelling ureteral stents in patients with extrinsic obstruction: experience at 2 institutions. Davies Introduction to oral care Epidemiology Oral symptoms are common in patients with advanced cancer (see below) (Davies and Epstein, 2010). Oral symptoms are also common relative to other symptoms in patients with advanced cancer (Davies and Epstein, 2010). Indeed, xerostomia (dry mouth) is consistently ranked as one of the five most common symptoms in this group of patients.
Bisoprolol 10mg with visa
Nutritional supplements Various nutritional supplements such as Ginseng quinquefolius (American ginseng) best blood pressure medication kidney disease safe bisoprolol 10 mg, Paullinia cupana (guarana), co-enzyme Q10, and L-carnitine, have been investigated in cancer patients to manage fatigue with various levels of success. Three hundred and sixty-four participants were enrolled from 40 institutions in United States. Changes from baseline in the general subscale of the Multidimensional Fatigue Symptom Inventory-Short Form were 14. Greater benefit was reported in patients receiving active cancer treatment vs those who had completed treatment. In another study by de Oliveira Campos and colleagues, patients with progressive fatigue after their first cycle of chemotherapy were randomized to receive either Paullinia cupana (guarana) 50 mg by mouth twice daily (32 patients) or placebo (43 patients) for 21 days (de Oliveira Campos, 2011). After a 7-day washout period, patients Conclusion Fatigue in cancer patients is now accepted as a symptom that should be studied in its own right. Unfortunately, few studies have addressed fatigue in palliative cancer populations. Consequently, most of the insight into the complexity of fatigue must be based upon extrapolation from studies performed with patients earlier in the disease trajectory. To improve treatment, we must gain a better understanding of the many aspects of fatigue. Thus, identifying the pathophysiological mechanisms that cause fatigue is important. Assessment and staging tools that are valid and reliable are needed to assist in clinical practice and research. Clinical syndromes of fatigue (cognitive, affective, and physical) also must be better characterized. Effects of methylphenidate on fatigue and depression: a randomized, double-blind, placebo-controlled trial. Psychostimulants for the management of cancer-related fatigue: a systematic review and meta-analysis. Acupuncture for cancer-related fatigue in patients with breast cancer: a pragmatic randomized controlled trial. Physical exercise for cancer patients with advanced disease: a randomized controlled trial. The potential of agents such as eicosapentaenoic acid, thalidomide, and anabolic steroids must be explored in studies in which fatigue is a primary endpoint. Finally, the role of psychostimulants should be further researched, and the importance of counselling, rest, and exercise in cancer patients receiving palliative care should be clarified. Wisconsin Ginseng (Panax quinquefolius) to improve cancer-related fatigue: a randomized, double-blind trial, N07C2. Sham Introduction to dyspnoea and other respiratory symptoms in palliative care A breath is a vital sign of a living creature. Hence a breath may be filled with physiological, psychological, and spiritual signals. Breathlessness serves as a warning signal in responding to the metabolic demand on a person. When the respiratory system is compromised by diseases, every breath may become laborious. Every day, millions of people throughout the world are distressed by breathlessness and other respiratory symptoms. Dyspnoea becomes an important factor predicting the will to live in the terminally ill while approaching death (Chochinov et al. Relieving distress related to respiratory symptoms is key to addressing suffering. In a cohort of 5682 palliative care patients, breathlessness increased from around 50% at 3 months before death to 65% at the time of death, with severe breathlessness increased from less than 10% to 26% at the two time points respectively. Two patterns of dyspnoea have been reported by cancer patients: the breakthrough-only dyspnoea in 61%, and constant dyspnoea in 39% of patients, among which 20% presented as breakthrough episodes (Reddy et al. The majority of patients with breakthrough episodes presented with fewer than five episodes daily, with each episode frequently lasting for less than 10 minutes. Episodic breathlessness could be triggered by exertion, emotion, or environment; or occur spontaneously without trigger. However, episodic breathlessness was only reported as a primary outcome in eight among 27 studies (Simon et al. Dyspnoea along the trajectory of life-limiting illnesses has been evaluated by several longitudinal studies. The experience is derived from interactions among physiological, psychological, social, and environmental factors, and may induce secondary physiological and behavioural responses. Perception entails conscious recognition and interpretation of sensory stimuli and their meaning (Parshall et al. Dyspnoea is a term we use for a symptom that patients often describe as breathlessness. Dyspnoea prevalence, pattern, and trajectory Dyspnoea is common among patients with advanced cancers and non-cancer life-limiting illnesses. The prevalence of dyspnoea varies with the site of primary cancers and the stage of illness. Similar to the pain model, it is postulated that dyspnoea consists of multiple dimensions, including the independent component of sensory dimension (sensory intensity and sensory quality), immediate affective stage which trigger immediate behaviour, and a stage of cognitive evaluative and emotional response which affects long-term behaviour (Lansing et al. Against the traditional neurochemical and neuromuscular model, a neuromatrix-gated model has been proposed to unify multiple factors by recognizing different inputs from afferents at receptor levels and inputs from different areas of the brain (Williams, 2011). Patients with non-cancer diagnoses had significantly higher levels of breathlessness at all three time points, while cancer patients had less breathlessness initially but increased significantly at day 10 and day 3 before death. In another cohort of over 10,000 cancer patients, the trajectories of performance status and symptom scores during the last 6 months of life were evaluated (Seow et al. Breathlessness increased in severity over time, particularly in the month before death. Qualities of dyspnoea and neurophysiology There are at least three separate qualities of dyspnoea: air hunger or unsatisfied inspiration; work or effort; and tightness (Lansing et al. This classification depends on different perceptual qualities with distinct afferent sources: 1. Air hunger or unsatisfied inspiration: this is the conscious perception of the urge to breathe. This sense of air hunger can be experimentally induced by hypercapnia, hypoxia, exercise, or acidosis, all leading to increase in respiratory drive. The signal comes from the motor drive of the respiratory centres in the brainstem, and is conveyed to the cerebral cortex as corollary discharge. When this is not matched by an adequate ventilatory response by feedback from afferent receptors throughout the respiratory system, individuals perceive air hunger or unsatisfied inspiration. Afferent information about the pulmonary ventilation achieved from mechanoreceptors in the lungs, airways, and chest wall can relieve or inhibit air hunger or unsatisfied inspiration. The sense of work or effort can be produced experimentally by external resistive or elastic load, volitional hyperpnoea, or by weakening of the respiratory muscles. The sensation of tightness arises from pulmonary afferents through the stimulation of airway receptors. The most consistent and the strongest area of activation is in the right anterior insula (Lansing et al. Other activations can be seen in the left anterior insula, anterior cingulate, supplementary motor area, prefrontal cortex, cerebellum, and amygdala (Parshall et al. Dyspnoea is associated with activation of cortico-limbic structures, which overlap with that observed the impact of dyspnoea Breathlessness correlates with survival and is a predictor of poor prognosis in cancer. In a systematic review of the value of symptom assessment to predict survival in people with advanced cancer, dyspnoea was evaluated in 35 studies involving 9155 patients (out of 44 studies included). Dyspnoea was correlated with survival in 22 studies in univariate analysis, and in ten studies in multivariate analysis. Dyspnoea is one of six parameters used in the Palliative Prognostic Score that predicts 30-day survival of palliative care patients (Pirovano et al. Previous studies have shown that dyspnoea often brings panic, fear, anxiety, depression, hopelessness, sense of loss of control, and impending death to patients (Gysels et al.
Syndromes
- Clay-colored stools
- Bulging fontanelles in babies
- Able to communicate needs such as thirst, hunger, need to use the restroom
- Swollen hands and feet
- If part of the ear has been cut off, keep the part. Get medical help immediately.
- Complete blood count (CBC), clotting tests, platelet count, and other laboratory tests
- Rinse your mouth with mild, over-the-counter mouthwashes or salt water.
- Joint pain (arthralgia)
- Urinary tract infection
- Bacterial or fungal infection of skin lesions
Purchase genuine bisoprolol line
Some children may benefit from an 8-hourly dose of long-acting opioid preparations rather than the standard 12-hourly regimen (Hunt et al blood pressure charts readings purchase on line bisoprolol. This occurs in neonates and infants up to the age of 12 months who, amongst other pharmacokinetic differences, have reduced renal clearance of morphine. Neonates and infants (under 12 months) are, therefore, prescribed a lower starting dose of opioid at longer intervals, for example, 6- or 8-hourly. Impaired renal function is another indication to approach opioid dosing cautiously. It is sensible to use immediate release opioids at a dosing schedule of 8- or 12-hourly or even as needed initially until titration of dose interval to requirements in the individual patient is established. Effectively the immediate release opioid has a longer acting duration as excretion is delayed. Using the appropriate route of administration: by the mouth the least invasive route, the oral route, is usually preferable in children. As such, palatability, availability of oral solutions, size of tablets, and frequency of dosing become factors to consider to ensure compliance and, consequently, good symptom management. Unless these factors are reviewed regularly, administering medication in children can become a major issue and may be a source of conflict between child and parent/carer. Some manufacturers have developed concentrated oral solutions to facilitate administration of medication for children who are unable (or unwilling) to take tablets. Many children with complex neurological disease, or those receiving cancer treatment, may have a gastrostomy in situ. Although these devices can be incredibly helpful, negating palatability and dose frequency issues, other problems may arise as several commonly used medications cannot be given via gastrostomy due to interaction between the medication and the device. There are several situations when the enteral route might not be suitable and an alternative route must be sought, for example: poor absorption: vomiting, disordered gastrointestinal motility inability to comply: unconscious; severe nausea, poor swallow; risk of aspiration, medication refusal pain crisis requiring rapid titration of opioids. The choice of alternative routes of administration when the oral route is not possible should be based on clinical judgement, availability, feasibility, and patient preference. The transmucosal route has become an increasingly popular means to deliver medication in children. Drugs absorbed through the transmucosal membrane of the nose or buccal cavity avoid the first-pass metabolism of the gastrointestinal tract and are absorbed rapidly. This mode of delivery is particularly effective for drugs such as midazolam, which is now available for this use in a concentrated buccal form. Diamorphine has also been used very effectively via this route for breakthrough pain although intranasal fentanyl has received more attention in the literature (Crellin et al. Although alternative opioids are available for sublingual, transmucosal, and nasal use, there are often issues regarding the practicalities of appropriate dosing, particularly in younger children when lower doses of opioid preparations for nasal, sublingual, or buccal use may be very helpful for rapid relief of symptoms. End-of-life symptoms including pain, dyspnoea, agitation, and seizures have been controlled successfully via the transmucosal routes but unfortunately literature supporting this is scarce. Other routes of medication administration in children Alternative routes of administration of analgesics in children include the subcutaneous, intravenous, or transdermal routes. The intramuscular route is practically obsolete in children as the injection itself is a cause of pain and may result in under-reporting of pain. The availability of short-gauge, indwelling, non-metallic needle systems has been very useful and made the subcutaneous route popular in paediatric practice. Ease of insertion, the possibility of numerous sites for access, and avoidance of recurrent intravenous cannulation offer obvious benefit. Indwelling percutaneous intravenous catheters or central venous access devices are used frequently for children requiring long-term therapy, recurrent blood product transfusion, and/or parenteral nutrition. They can be useful in the palliative setting towards the end of life for delivery of analgesia and other medications, particularly if higher-volume infusions are needed. The successful use of patient (or proxy) controlled analgesia has been reported in children at the end of life (Schiessl et al. Although the minimum quantity of opioid required for use might provide a barrier in smaller children, the more recent manufacture of lower-dose, matrix-based patches has enabled more children to gain from the clear advantages offered by this route. Medication delivered by the rectal route may be advantageous in some instances but many children dislike this way of giving medications. It can be a very useful route in the infant and younger child to avoid parenteral routes in the short term. Additionally some immediate and sustained release opioid preparations can be readily absorbed from the rectal mucosa. Anticonvulsants have Adapting treatment to the individual: by the child this principle promotes individualized treatment according to the assessed need of the child. In a child already receiving opioids the current dose of opioid should be used as a basis for calculation. The correct dose of opioid is determined in partnership with the child and carers until the best possible pain relief is achieved, with the fewest side effects. Maintenance: is established once a dose that provides adequate relief of pain is achieved. For many children, long-acting morphine preparations (granules) are convenient and offer flexible dosing. Internationally the availability of child appropriate dosage formulations is often very limited and prohibits optimal analgesia. Opioid switching Opioid switching should be considered in children who have opioid dose limiting side effects. Fentanyl has been reported as causing less constipation than other opioids (Finkel et al. Pruritus as a side effect of opioids is not uncommon in infants and children and occurs frequently around the nose and face. Standard management for pruritus can be trialled, however if it persists an opioid switch may be required (Drake et al. Myoclonus is an involuntary muscle contraction that occurs as a consequence of either opioid toxicity or long-term use of opioids. It is not infrequent in children and usually prompts opioid switching or treatment with a benzodiazepine or muscle relaxant, depending upon the circumstances. Urinary retention is seen in children particularly after rapid dose escalation and spinal or epidural opioids. Anecdotally, children seem to experience urinary symptoms (usually hesitancy) not infrequently; however, a small case series indicated that one in seven children (14%) had overt symptoms of retention (Mashayekhi et al. External bladder massage/pressure, heat packs, voiding in a warm bath, and, if necessary, intermittent catheterization or cholinergic agent may be required. Opioid side effects Children may not report adverse effects voluntarily, for example, constipation, nausea, and itching, so careful attention must be paid to these problems when assessing opioid efficacy. If opioids are titrated appropriately, respiratory depression is a very rare occurrence. In palliative care patients, opioid toxicity is more likely to occur when there is sudden removal of a pain stimulus, such as following radiation therapy to a bone metastasis or the insertion of an intrathecal pump for metastatic spinal disease. In these situations it is helpful to revert to short-acting opioids, or an opioid infusion, to enable close monitoring of opioid requirements. The onset of renal failure and an inability to excrete opioid metabolites is another potential reason for respiratory compromise, as is the inadvertent administration of higher doses of opioid than those prescribed, such as ingestion of sustained-release medication in the place of short-acting opioids. If respiratory depression occurs then small, frequent doses of naloxone (an opioid antagonist) may be necessary at a starting dose, in opioid-tolerant patients, of 1 microgram per kilogram, titrated over time. A low-dose infusion of naloxone may be required until the adverse effect of the opioid resolves. Administration of naloxone must be done with caution as reversal of analgesia will precipitate extreme pain and opioid withdrawal syndrome. Assisted ventilation for respiratory depression may be indicated in palliative care patients in this situation. Psychostimulants such as methylphenidate have been used in adults to reverse opioid-induced sedation, despite a recent review stating that robust data are lacking (Stone and Minton, 2011).
Order cheap bisoprolol on line
In this way blood pressure pills kidney failure order bisoprolol with amex, high doses of radiation close to , or beyond, those tolerated by surrounding normal tissues can be given. Conventional treatment schedules deliver a single dose of radiation, often called a fraction, on a daily basis, Monday to Friday. This treatment may be accelerated, that is, given two or three times a day over a relatively shorter period, to produce greater tumour damage by reducing the opportunity for tumour repopulation. Treatment acceleration is limited by the increase in the acute reaction of normal tissue. Hyperfractionation, which delivers the total dose in an increased number of fractions over the same period dividing the usual daily dose into two or three smaller doses, may be employed to deliver higher doses with greater sparing of normal tissues. For patients with limited life expectancy, however, more pragmatic schedules are appropriate. Sixty to 80% of tumour cells are killed by the first one or two radiation doses, and when the intent of treatment is palliative, this initial effect may be more than adequate for long-term symptom control. Indeed, in some scenarios, for example, metastatic bone pain, symptom response is independent of tumour shrinkage. The delivery of short, relatively low-dose schedules results in less acute reaction and a minimal risk of late damage to normal tissues within the expected life span of the patient. The most frequently used forms of ionizing radiation are X-rays produced from an X-ray machine or linear accelerator and gamma rays produced from a radioactive source. Particle radiation also is sometimes used, particularly electrons for superficial treatments and beta particles from systemic radioisotopes. Indirect damage is the more important cause of cell death, which may occur from either reproductive failure or apoptosis following derangement of cell regulatory mechanisms. When very high single doses (> 10 Gy) of radiation are delivered, damage to endothelial cells occurs and the resulting interruption in blood flow may be another mechanism for cellular injury. In clinical practice, radiation is delivered to maximize tumour cell kill whilst minimizing normal tissue damage by exploiting differences between normal and malignant cells. Factors that influence response other than repair capacity include oxygenation (hypoxic cells are relatively radioresistant), the number of cells actively dividing (cells in certain phases of the cell cycle are more sensitive than others; non-cycling cells are relatively radioresistant), and the rate of repopulation within the tumour. These parameters of repair, re-oxygenation, repopulation, and redistribution within the cell cycle, are the fundamental influences on the cellular response to radiation. Radiotherapy in clinical practice the most common type of radiotherapy is external beam irradiation Table 12. Alternative means to deliver radiation-brachytherapy and systemic radioisotopes-are used in specific circumstances. In brachytherapy, the radioactive source is placed directly onto or within the area to be treated Table 12. Systemic radioisotopes target a specific tissue or pathophysiology, for example, radioiodine for thyroid cancer and strontium for bone metastases. To direct radiation as accurately as possible to the tumour whilst minimizing exposure to normal tissue requires a systematic process that defines the treatment volume and optimal technique. The simulator is an X-ray machine identical to the therapy machine in its geometric specifications and movement, which emits a diagnostic X-ray beam and produces an image of the proposed therapeutic beam. Dosimetric planning: once the volume has been defined, the means of treatment delivery is determined. For simple treatments, such as those for bone metastases, a single beam or two opposing beams to treat a block of tissue will be all that is required. For internal volumes, more complex, three- or four-field arrangements may be optimal. Immobilization: it is necessary to immobilize the patient when small movements could result in the irradiation of critical structures, for example, the eye. Although a simple technique, such as sandbags, may suffice, more complex treatments may require a plastic shell with an individualized face mask. With simple superficial fields, clinical measurement and observation are adequate. Accurate documentation of the beam position with indelible marking of defined skin entry points on the patient will facilitate this and ensure accurate day-to-day reproducibility when more than one fraction is to be given Table 12. These are minimized by reducing the A linear accelerator produces high-energy radiation at a rate of around 1 Gy per minute. This means that most treatments, even those using large single fractions in the palliative setting, last for only a few minutes. There are no accompanying symptoms provided the patient is comfortable at the outset. Many patients require help in achieving the required position and lying still during treatment. Unfortunately, many patients experience discomfort related to immobilization, the use of hard wooden flat couch, and the need for staff to leave the patient isolated whilst radiation delivery is taking place. The judicious administration of an analgesic or anxiolytic drug prior to treatment always should be considered. Side effects of radiotherapy the side effects of radiotherapy are categorized into two groups based on their timing relative to the radiation exposure. Late effects are rarely seen before 9 months after treatment and the risk of a late complication continues indefinitely. The common clinical manifestations of acute and late radiation toxicity are shown in Table 12. This results in skin erythema or desquamation, and depending on the site of treatment, oropharyngeal mucositis, oesophagitis, cystitis, or gastrointestinal irritation. Repair of the denuded surface with new epithelial cells occurs once treatment is completed, provided that the underlying stem cell population has not been damaged irreparably. This most often occurs in vulnerable sites, such as the back or the lower leg, where skin healing appears less efficient. Poor healing after radiotherapy may also be seen where there is secondary infection or trauma, and it is these events that predispose to the rare occurrence of radionecrosis. Late effects cause of treatment-related loss of function and even mortality in patients receiving radical radiotherapy. One of the reasons for the complex planning systems which have evolved for radiation delivery is the strenuous effort required to avoid exceeding these doses whilst delivering effective doses to nearby tumour. Unfortunately there are genetically predisposed individuals to radiation damage where even a conventional tolerance dose may result in late damage. Late radiation injury is due to vascular damage, specifically progressive endarteritis obliterans. In the pelvis, the bowel or bladder may be damaged, resulting in fibrosis and bowel perforation or fistula formation between the bladder, bowel, or vagina. In the central nervous system, there is very limited ability to repair damage and catastrophic necrosis may occur if dose limits are exceeded. Management of radiation side effects Acute side effects are common and management is focused on relief of symptoms whilst allowing the affected area to heal. The use of topical preparations such as gentian violet is to be discouraged, and talcum powder and proprietary creams containing metallic salts should be avoided at all costs during treatment as these can enhance the reaction. Starch powder, as found in proprietary baby powders, may be helpful in keeping the surrounding skin dry and comfortable. For example, single radiation doses given to the lumbar spine or pelvis produce an exit dose of radiation to the abdomen, and a prophylactic regimen of dexamethasone 8 mg and ondansetron 8 mg or granisetron 2 mg given 30 minutes before treatment is effective in avoiding severe symptoms. Radiation-induced acute diarrhoea may respond to a low residue diet, avoiding fruit and other fibre-containing foods. When required, loperamide or codeine phosphate on a regular basis three to four times daily is helpful. The use of an alpha blocker such as tamsulosin may be helpful when there is severe bladder spasm. Potassium citrate or cranberry juice are both time-honoured remedies, which may be of supportive value but have no evidence for efficacy.
Order bisoprolol 10 mg visa
Other markers and immunocytochemical techniques have not been found to have clinical value (Chamberlain blood pressure jokes discount 10mg bisoprolol with visa, 2006). This pain may be associated with paroxysmal episodes of lancinating or throbbing pain. The quality of the pain only rarely can mimic classical trigeminal neuralgia, an atypical facial pain is more common (Cheng et al. This is a sign of disease of the jaw or, more frequently, of the base of the skull, leptomeninges carcinomatosis, and local perineural spread of lip carcinoma. Glossopharyngeal nerve the typical patient has throat and neck pain, which radiates to the ear and is aggravated by swallowing. Pharyngeal and other carcinomas of the neck can present with odynophagia with reflex otalgia. Although it has been described with leptomeningeal disease, it commonly results from local nerve infiltration in the neck or base of the skull. Pain was reported in the inner aspect of the arm and paraesthesiae in the 5th and 4th finger. Left side: the arrows show the tumour mass invading the tissue planes in the area of the brachial plexus. Right side: the tumour is invading the left upper lobe, the arrows show the tumour invading one thoracic vertebral body. The pain of a root lesion is usually focal and radiates in the distribution of the affected root. Herpes zoster and post-herpetic neuralgia are common in patients with cancer and should always be considered in the differential diagnosis of painful radiculopathies. Cervical plexopathy Infiltration of the cervical plexus by tumour can be a result of compression by head and neck neoplasms or metastases to cervical nodes. Symptoms usually include local lancinating or dysaesthetic pain referred to the retro-auricular and nuchal areas, the shoulder, and the jaw. Sensory abnormalities define the affected (greater auricular and greater occipital) nerves (Vecht et al. The diagnosis in patients with head and neck cancer may be difficult because of the postoperative and post-radiation changes often found in these patients. Brachial plexopathy Five per cent of the neurological consultations at a comprehensive cancer centre were found to be initiated by brachial plexopathy (Burt et al. The plexus can be compressed or infiltrated by tumour lying in contiguous structures, such as axillary or supraclavicular nodes, or the apex of the lung. The hallmark of the syndrome is the neuropathic nature of the pain with numbness, paraesthesia, allodynia, and hyperaesthesia. All patients with symptoms of brachial plexopathy should have a scan of the contiguous paravertebral region before radiation therapy, since extension of disease in this region is common (13/41 cases in one series). While use of both techniques can give helpful complementary information in doubtful cases, sometimes neither is helpful even in cases of proven metastatic plexopathy (Krol, 1993). Comparative data on specificity and sensitivity of the two techniques are lacking. Radiation fibrosis is important in the differential diagnosis of brachial plexopathy in cancer Table 14. Lumbosacral plexopathy Lumbosacral plexopathy is one of the most disabling complications of cancer. Although it is commonly associated with colorectal, cervical, and other pelvic malignancies (bladder, uterus, prostate, sarcoma, lymphoma), it can also be caused by breast or lung cancer, or melanoma. It is usually followed by numbness, paraesthesia, weakness, and, later, leg oedema. The pain is usually aching or pressure-like in quality, and is rarely burning or dysaesthetic. Reproduced from Hematology and Oncology Clinics of North America, Volume 10, Issue 1, Caraceni, A. Anal sphincter 0 weakness Although electrodiagnostic studies and imaging may distinguish radiation-induced plexopathy from malignant invasion (Harper et al. Selective involvement of the L1, iliohypogastric, ilioinguinal, or genitofemoral nerves can produce pain and paraesthesia in the inguinal and scrotal region. A sacral plexopathy, often overlapping a sacral polyradiculopathy, can be produced from direct extension of a presacral mass invading the sacrum, as sometimes occurs with rectosigmoid and bladder carcinomas. Tumour is often found in the lumbar vertebrae, sacrum, or pelvis of patients with lumbosacral plexopathy (45/76 patients) and epidural extension is also common, especially with retroperitoneal tumours. Motor involvement is bilateral in 80% of cases and electromyography can be a useful diagnostic tool. Other differential diagnoses include leptomeningeal carcinomatosis, and cauda equina compression. Related to chemotherapy and radiation Mononeuropathy Mononeuropathy is less common than plexopathy or radicular lesions (Anoine and Camdessanche, 2007). It is caused by compression or infiltration of a nerve by bony lesions, or by soft tissue masses in the limbs. Intercostal nerve neuropathy from invasion of the chest wall is the most common of the mononeuropathies caused by cancer. Obturator, femoral, and sciatic neuropathies are seen when tumour involves the soft tissue along the nerve distribution in the pelvis and thigh. Peroneal mononeuropathy can occur with bony lesions of the head of the fibula and sarcoma of the popliteal fossa. Clinical experience suggests that dexamethasone can be particularly effective for pain due to compression and oedema of peripheral nerves. Peripheral polyneuropathy Polyneuropathy in cancer patients can be caused by chemotherapy, metabolic disturbance or nutritional deficiency, or paraneoplastic syndromes (Box 14. Peripheral neuropathy is characterized by a stocking-glove distribution of negative sensory and positive sensory symptoms. Loss of sensation may predominate, or there may be painless paraesthesia or distressing burning dysaesthesia, allodynia, and hyperalgesia. Early sensory loss and later motor signs (weakness) are characteristic of some drug-induced sensorimotor neuropathies (vincristine, paclitaxel). Sensory involvement can be selective in neuropathies associated with cisplatin or paraneoplastic syndromes. Often the only early sign of polyneuropathy is reduction or loss of the ankle reflex. Muscle cramps may be associated with neuropathy and can sometimes be prominent symptoms in vincristine neuropathy. Paraneoplastic sensory neuropathy and sensory neuropathy caused by vincristine or paclitaxel is often more painful than that caused by cisplatin. Cisplatin induces a sensory neuropathy mainly affecting the cells of the dorsal root ganglia. There is predominant involvement of the large fibre functions (proprioception), which causes sensory ataxia rather than pain. Vinca alkaloids and paclitaxel produce a mostly sensory axonopathy with some motor component. New antineoplastic drugs that interfere with specific metabolic pathways, such as bortezomid, also have distinct toxic effects on the peripheral nervous system (Anoine and Camdessanche, 2007). They can affect central or peripheral nervous systems, neuromuscular junction, or muscle (Darnell and Posner, 2003; Viaccoz and Honnorat, 2013) Table 14. The specific antibodies and their pathogenic role need to be evaluated carefully by highly specialized professionals (Darnell and Posner, 2003; Viacozz and Honnorat, 2013). The clinical course is independent of that of the original tumour, which in 50% of cases is found after the onset of neurological symptoms.
Cheap bisoprolol online visa
For example blood pressure medication and memory loss buy 10 mg bisoprolol overnight delivery, a patient may use a long-acting opioid preparation, such as morphine, for background pain and a fast-acting fentanyl preparation for breakthrough pain. This group is often satisfied to use a standard opioid such as immediate (normal)-release morphine, 30 minutes in advance of such activity. Opioid toxicity Opioid toxicity is a spectrum which at one extreme may involve sleepiness, poor concentration, and vivid dreams while at the other end of the spectrum may involve hallucinations, confusion, agitation, and even a paradoxical increase in pain known also as hyperalgesia. A survey of inpatients in a regional cancer centre showed 50% of patients to have some symptoms of opioid toxicity, 13. Most of the evidence for opioids with faster onset of analgesia and faster peak plasma analgesic levels is limited to fentanyl (Zeppetella and Ribeiro, 2006). Specific pharmacological or non-pharmacological interventions for the breakthrough pain. It is generally agreed that one of the main problems with breakthrough pain due to bone metastases is that multiple breakthrough doses of opioid to control pain on movement and/or spontaneous pain at rest, usually leave the patient with frank, unacceptable opioid side effects, especially sedation, or with frank opioid toxicity. Twenty-five patients admitted to a palliative care unit with movement-related breakthrough pain were titrated with intravenous morphine to background pain relief. The morphine dose was then increased further until patients began to experience unacceptable side effects at which point the increase was either stopped, or the morphine dose reduced. Ideally, rescue medication should have an onset/duration of action appropriate for the pain, should have a potency of effect appropriate for the pain and be easily administered. Rescue medication should be offered soon after the pain has started in cases of unpredictable pain, and before the pain has started in cases of predictable pain. Morphine, hydromorphone, and oxycodone are the most common oral opioids used, and a fixed proportion of the daily dose is usually advised. One study formally addressed the use of a fixed dose of rescue medication (Mercadante et al. A total of 172 episodes of pain were assessed and most patients had a 33% reduction in their pain within 18 minutes. However, with an onset of action of approximately 30 minutes, a relatively long duration of action, and dose-limiting adverse effects, they are not ideally suited to the management of breakthrough pain. There are no studies to suggest that they are effective in this clinical scenario. These studies confirmed the efficacy of this delivery system for the management of breakthrough pain (Farrar et al. It is a heterogeneous phenomenon, although it is typically of fast onset and short duration as previously discussed. Despite implementation of guidelines, patients continue to have inadequate pain control and often express a variety of problems secondary to this. Three principles have been proposed for the management of general breakthrough pain, not specifically related to bone metastases (Portenoy, 1997): 1. The mechanism by which bisphosphonates cause short-term pain relief is unclear, but is likely to be related to their effect on tumour growth factors and other nociceptive agents. A Cochrane systematic review addressing the (acute) analgesic effect of bisphosphonates was first published by Wong and Wiffen (2002). The data were subsequently updated to create a Health Technology Report for the Canadian Coordinating Center of Health Technology Assessment (Wong et al. The data support the fact that bisphosphonates provide moderate relief of pain within 12 weeks of therapy. While there was a trend towards pain relief at weeks 4 and 8, this only became statistically significant at week 12. This differs from usual practice of prescribing one-sixth of the 24-hour opioid dose as a breakthrough dose. It is, however, hardly surprising that when an opioid dose is carefully titrated for breakthrough pain in the context of a clinical trial, that the individual effective doses vary between patients and rarely work out as one-sixth of the 24-hour opioid dose. Bisphosphonates for bone pain Over the years, a number of different bisphosphonates have been developed, with the newer agents exhibiting increased potency as compared to the original agents (Wong, 2007). Bisphosphonates have a number of actions, which account for their anti-resorptive properties (Santini et al. They inhibit dissolution of hydroxyapatite crystals, have an effect on osteoclasts and osteoblasts, and also can have an effect on the underlying tumour. Bisphosphonates can inhibit the differentiation of stem cells to osteoclasts, affect the structure and function of osteoclasts, and cause apoptosis of osteoclasts (Santini et al. The latter actions rely on the bisphosphonate being taken up into the osteoclast by a process of endocytosis. In addition, bisphosphonates can inhibit the growth of tumour cells, stimulate the immune system (against the tumour), and cause apoptosis of tumour cells (Santini et al. The inhibition of growth is achieved by a reduction in the adhesion of tumour cells to bone, a reduction in the secretion of tumour growth factors into the bone (secondary to a reduction in bone resorption), and an inhibition of tumour angiogenesis. Bisphosphonates delay the development of skeletal events, particularly in patients with breast cancer, multiple myeloma, and prostate cancer (Bloomfield, 1998; Michaelson and Smith, 2005). However, bisphosphonates can also improve pain secondary to established bone lesions: many patients only respond after months of treatment, whilst other patients respond soon after treatment is initiated. The mechanism by which bisphosphonates cause Results for different bisphosphonates Five randomized trials provided direct comparisons between different bisphosphonates. All of them compared pamidronate against a different bisphosphonate: three compared it with clodronate (Zhang et al. Based on the limited data available, pamidronate appears to be a better choice than clodronate with a greater response rate and a greater magnitude of pain relief. Further studies are necessary to elucidate the relative merits of pamidronate and the more potent bisphosphonates, such as ibandronate and zoledronate (Cameron et al. Clinical data tolerability Bisphosphonate side effects commonly described include flu-like syndromes and injection site reactions. Randomized trials with standard doses did not identify excessive gastrointestinal toxicities, although concern has been raised about this (Lanza, 2002). Rapid infusions may result in renal toxicity, especially in patients with renal compromise. Pamidronate infusions (90 mg) are typically delivered over a period of 2 hours, while zoledronate infusions (2 mg) are typically delivered over 15 minutes. Ibandronate does not appear to possess the same renal toxicity concerns and can be used in patients with varying degrees of renal impairment (Jackson, 2005; von Moos, 2005). Adverse ocular events including uveitis, scleritis, and conjunctivitis have been reported with amino-bisphosphonate use, particularly pamidronate use (Leung et al. Bisphosphonate-associated osteonecrosis of the mandibular and maxillary bone has been described (Migliorati et al. The pathophysiology of this condition is unknown, but the risk factors include dental extraction, local trauma, local infection, and systemic chemotherapy. The condition has been reported with pamidronate and zoledronate and usually appears after many 13. Appropriate prophylactic dental assessment and management, along with antibiotic therapy if indicated, are keystone to minimizing occurrence of this complication. The latter procedure allows enough time for the bone marrow from the un-irradiated half of the body to re-populate the marrow cavity in the irradiated half of the body (van As and Huddart, 2007). There is continued interest in this form of therapy with newer agents being developed (Yuan et al. Despite evidence, they are not widely used currently and while there are a number of potential reasons for low use of radioisotopes, cost may be an issue in many countries. A positive effect of delaying these skeletal events is an overall reduction in pain secondary to bone resorption and its complications. In addition, bisphosphonates also provide relief of bone pain, although the magnitude of the effect is modest in the short term and can take up to 12 weeks to work. Further work is underway to evaluate the utility of the potent bisphosphonates such as ibandronate in achieving acute pain relief (Ibrahim et al.
Purchase bisoprolol pills in toronto
Hence pulse pressure mitral stenosis bisoprolol 10mg otc, many patients continue to receive relatively ineffective treatments for their oral problems. However, there is a wealth of evidence for the efficacy of various interventions in the non-palliative care population, and increasingly in the palliative care population (Davies and Finlay, 2005; Davies and Epstein, 2010). It is recommended that a small-headed brush, which has soft-to-medium texture bristles is used. Powered toothbrushes with a rotation-oscillation action appear to be better at removing dental plaque than manual toothbrushes (and other types of powered toothbrushes) (Robinson et al. The recommended life span of a toothbrush is about 3 months, but it should be replaced sooner if the filaments of the brush become softened and/or misshapen. Toothbrushes should be replaced sooner if the patient is immunosuppressed or receiving chemotherapy. Furthermore, toothbrushes should be immediately replaced if the patient has experienced any type of oral infection. Most toothpaste contains a foaming agent, which may prove problematic for those patients who have difficulty swallowing (and who are at risk of aspiration). If patients cannot tolerate the use of toothpaste (due to oral discomfort), then they can simply use water during toothbrushing. Denture care Denture hygiene must be carried out regularly and should be incorporated into a daily oral care routine (Sweeney and Davies, 2010). All dentures must be cleaned outside the mouth, and the soft tissues of the mouth cleaned separately (see below). The denture should first be held under running water to remove debris, and then be brushed thoroughly with a large toothbrush, denture brush, or personal nailbrush to dislodge any remaining debris or plaque. Commercial products are available for cleaning dentures, but soap and water, or water on its own, is usually satisfactory. Ordinary toothpaste should not be used, because they are quite abrasive and may damage the polished surface of the denture. Dentures should ideally be rinsed under running water after every meal, and the lining of the mouth checked for food debris before re-inserting the dentures. Calculus may irritate/damage the underlying oral mucosa, and should be professionally removed as soon as it is noticed. In order to maintain a healthy oral mucosa, it is advisable to leave dentures out of the mouth overnight. Plastic dentures should be soaked in a dilute solution of sodium hypochlorite (1 part Milton sterilizing fluid to 80 parts water). This allows disinfection of the denture, and reduces the likelihood of denture stomatitis. Interdental cleaning Interdental aids are designed to remove dental plaque from the areas between teeth that cannot be reached by a toothbrush. Ideally, some form of interdental cleaning should be used on a daily basis (Sweeney and Davies, 2010), although this may not be achievable or appropriate for some patients. The types of cleaning aids available include dental floss, dental tape, wood sticks, and interdental brushes. Chemical plaque control For some patients, mechanical control of dental plaque is extremely difficult because of their level of debilitation and/or the presence of oral pathology. In such cases chemical control of dental plaque may be considered for maintenance of oral hygiene (Sweeney and Davies, 2010). The chlorhexidine molecule has a positive charge at either end, and binds readily to negatively charged sites on the dental enamel pellicle, mucosal cells, and bacterial cells. Chlorhexidine is slowly released from such surfaces, so maintaining its antimicrobial activity (a property known as substantivity). Indeed, there are no indications for using chlorhexidine more than twice a day (see earlier). It is important to realize that chlorhexidine will not remove established dental plaque-this must be physically removed by a dentist or dental hygienist. The most common side effect associated with long-term use of chlorhexidine is staining of the teeth and the dorsal surface of the tongue. Other problems include the taste of the mouthwash, and the alcohol content of some mouthwashes (which may cause mucosal discomfort). These problems may be overcome by Care of the oral mucosa the oral mucosa should be cleaned three to four times per day, ideally after each meal (Sweeney and Davies, 2010). For those patients who are able, rinsing the mouth with water is adequate to remove any debris. For those who are unable to rinse, the mucosa should be cleaned mechanically with a water-moistened gauze or foam stick. Xerostomia is usually the result of a decrease in the volume of saliva secreted. However, xerostomia may also result from a change in the composition of the saliva secreted. There are good reasons for prescribing saliva stimulants rather than saliva substitutes. Moreover, in studies that have compared saliva stimulants with saliva substitutes, patients have generally expressed a preference for the saliva stimulants (Bjornstrom et al. Nevertheless, some patients do not respond to treatment with saliva stimulants, and so will require treatment with saliva substitutes. Saliva stimulants Chewing gum Chewing gum increases salivary flow by two mechanisms; approximately 85% of the increase is related to stimulation of chemoreceptors within the oral cavity. However, side effects can occur, and may be related to (a) chewing, for example, jaw discomfort, headache; (b) inappropriate ingestion, for It is important to emphasize that there may be a discrepancy between the symptoms experienced by patients and the signs identified by health-care professionals. The classic signs of salivary gland hypofunction include dryness of the oral mucosa, dryness of the lips, absence of a pool of saliva in the floor of the mouth, fissuring of the oral mucosa (especially of the tongue), and cracking of the lips. However, patients with xerostomia, and some patients with salivary gland hypofunction, may have no obvious abnormalities on examination. Chewing gum is an acceptable form of treatment for most patients, including most elderly patients (Davies, 2000a). Organic acids Various organic acids have been used as saliva stimulants, including ascorbic acid (vitamin C), citric acid (the acid in citrus fruits), and malic acid (the acid in apples and pears). Organic acids increase salivary flow through stimulation of chemoreceptors within the oral cavity. Thus, organic acids should not be used in patients with dry mucosae, cracked mucosae, stomatitis, and/or mucositis. Thus, organic acids should not be used in patients with teeth, and should be used with caution in patients with dental prostheses. The other choline esters that have been used in clinical practice include bethanechol, carbacholine, and cevimeline (Davies, 2010a). The cholinesterase inhibitors that have been used in practice include distigmine and pyridostigmine (Davies, 2010a). In spite of this, many patients choose to use water rather than other saliva substitutes. The reasons for this phenomenon include familiarity, efficacy (moderate), tolerability, availability, and affordability. The use of water is not associated with side effects per se, although polydipsia is inevitably associated with polyuria (and nocturia). It should be noted that there is no scientific rationale, and indeed no research evidence, to support the use of chilled or frozen water. Parasympathomimetic drugs Parasympathomimetic drugs stimulate the part of the autonomic nervous system responsible for the secretion of saliva from the salivary glands. The side effects of pilocarpine are usually related to generalized parasympathetic stimulation, and include sweating, headache, urinary frequency, and vasodilatation. The incidence of side effects is dose related, that is, the higher the dose of pilocarpine, the higher the incidence of side effects. A number of commercial products have been developed, which differ in formulation. Moreover, it should have a neutral pH (to prevent demineralization of the teeth), and contain fluoride (to enhance remineralization of the teeth). However, there are positive studies in the literature involving patients with advanced cancer of a specific mucin-based artificial saliva (Sweeney et al. Artificial saliva is generally well tolerated, although some patients report local problems.